HCS Highlights
SPRING 2023





The 2023 Regular Session officially convened on January 9, 2023. However, most of you know that the work began in the Spring of 2022. HCS proposed several items for this session, including increasing the Personal Needs Allowance (PNA) for our clients served in medical institutions and residential settings from $70 to $100. I was so excited to see this bill passed by both the House and the Senate – it proves that our Legislature is invested in helping to lift our clients out of poverty.
With the Governor’s recent signing of the bill, this law will go into effect on July 1, 2023. It will increase each year after that in line with the Social Security Administration’s cost of living adjustments. The additional PNA supports clients with their needs, including phone service, a haircut, gifts for grandchildren, or even a meal out.
Other legislation of note includes:
• $6 million for hunger relief in the current fiscal year
• Changes to home care aide certification
• Addressing home care workforce shortages by modifying training and certification requirements for home care workers
• Working with CMS to create a waiver for spouses to be paid caregivers

• Creating a program for individuals found incompetent to stand trial due to an intellectual or developmental disability, traumatic brain injury, or dementia to receive services and supports in communitybased settings.
• Collaborating with the Health Care Authority to expand a difficult-todischarge pilot at Harborview to other hospitals around the State.
The conference budget the Legislature penciled out left a healthy balance in the wake of the declining revenue forecast. While the decline was noted, it’s essential to recognize that the overall state budget is still anticipated to grow between the 2023-25 and 2025-27 biennia. In the 2021-23 Washington State Operating budget universe, DSHS long-term care continues to be a significant portion of the state budget, following K-12 Public Schools and HCA – Low Income Health Care.
Cathy Kinnaman DirectorSome highlights for the 2023 legislative HCS budget include the following:
• Mandatory workload adjustments increasing the number of field staff
• Funding to hire staff to assist with community housing transitions
• Expand the Senior Farmers Market Nutrition Program and ongoing increase senior nutrition services
• Increase to the rate paid to Area Agencies on Aging (AAAs) for case management services
• One-time funding to expand efforts to support individuals with dementia and their families
• Kinship care support, including an increase in kinship navigator rates
• Ten additional non-citizen personal care slots
• Continued funding of Transitional Care Center of Seattle through the fiscal year 2025
• Funding to continue the rapid response nursing team program through the end of the fiscal year 2024
• One-time funding for staff support of the difficult-to-discharge task force and to develop home and community assessment timeliness requirements for pilot participants in cooperation with the Health Care Authority
• Additional staff to assist with reporting, auditing, and dispersal requirements of Medicaid funds
In addition to funding, the Legislature also included requests for reports and pilots from HCS, including continuing the homeless senior’s pilot, funding for staff support to the difficult-to-discharge task force, and a report on enhanced behavior supports to name a few.
This year we welcomed Jovi Sanchez in her role as Legislative Coordinator at HCS. I thank Jovi for her steadfast support during this year’s fast-paced and long session. Now the hard work begins to implement the investments the Legislature has made into LTSS, recruit and hire new staff to keep up with the increasing demand for our services and implement the new initiatives from the session.
As this work begins, take a moment to think about all the incredible work you all contribute to every day – we need every one of you to achieve our daily mission of transforming the lives of the people we serve.
Seven years ago, Region 1 started an experimental in-training team to better prepare staff to do the work of a social services specialist within HCS. With this experiment, we started hiring employees who met the SSS2 work experience rather than the higher SSS3 work experience criteria. In 2021, the program was expanded to the entire region, taking training out to the entire field via MS TEAMs and some in-person as needed.
Tami Rucker, Region 1 Administrator
The Region 1 Training Team now consists of three Social and Health Program Consultants, one Data Social and Health Program Consultant, two Supervisors in Spokane who have in-training staff on their teams for one year and a Program Manager.
Since the advent of the in-training team in 2016, 49 people have been hired and trained. Twenty-seven are still with HCS, a 55% retention rate. The in-training team works to train staff on all HCS programs, and we have seen several staff move from one discipline to another. One has gone on to become a Program Manager and one has promoted to an SSS5!
The training team has provided support to supervisors and new staff who need CARE shadow visits and QA monitoring. They have provided focus reviews for residential case management teams and have developed trainings quickly to address any QA findings using “Over the Cubicle Wall” 30-minute presentations on topics such as: Shared Rooms in ALFs, LTC Chapter update reviews, and Management Bulletin Synopses. The team has worked extensively with ensuring ProviderOne payments are accurate, and helping staff understand the P1 system. The training team is here to support all staff and to hire, assist, and train where staff need it, whether new or seasoned.
Another significant element of the training team has been the creation of a Training Library in One Note where the trainings they have developed and provided are stored for future use whenever a “brush-up” is needed. Supervisors can go to the library and select a topic to train to a specific need
on their team or when something is requested. The trainings include guest speakers who train on their areas of expertise such as Residential Support Waiver, Adult Protective Services, Nurse Delegation, TEMS, Adult Day Health, AIDA, Supported Employment, and Durable Medical Equipment.
The Region 1 Training Team has been vital as we progress through our hiring and training of larger numbers of staff than is typical as we come out of the pandemic. They are committed to providing quality materials for staff training and are passionate about our social services learning. We are fortunate to have them as part of our journey here in Region 1!

For the first time since 2020 our Region 2 Acute Care Hospital team is on top of our game! Assessments are timely, Long length of stay (LLOS) lists are down, and cases are transitioning out from the hospital and back into the community. We have had peaks of up to 456 referrals per month and LLOS clients over 250 days at times, our average length of stay currently rests at 38 days in the past few months. What an improvement!


A mighty thank you for our R1, R2, R3 and HQ helpers for all the support provided. My Region 2 partners, so many of you were enlisted for assistance and we would not have been able to do this without you. R2D2 has also helped to keep the discharge process streamlined and flowing. My very own Acute hospital teammates who have weathered the storm and are still with me, I give my heartfelt gratitude. We have rebuilt ourselves into a bigger, stronger, and more efficient machine, and we will continue this path to grow and flourish!
Submitted by Cindy Nomura, ACH PM
Sonya Sanders, Region 2 AdministratorI recently listened to a podcast that was discussing how the past few years have been a steady flood of adrenaline and cortisol into our systems resulting in an epidemic of exhaustion and burn out. I know I have heard that a lot in my Region. Yet even though many of us feel exhausted, we keep going, we keep doing, we keep giving.
Referencing the book “Burnout – The Secret to Unlocking the Stress Cycle, by Emily and Amelia Nagoski they discussed the symptoms of burn out, the difference between stress and stressors and how to complete the stress cycle to help find relief.

Symptoms of burnout include, but are not limited to emotional exhaustion, depersonalization (e.g., you want to care, but there is nothing left) and feeling like nothing you do makes a difference.
The Nagoski sisters differentiate between stressors and stress. Stressors are outside of us and includes things like relationship issues, money issues, work issues, traffic jams, looming deadlines, etc. Stress on the other hand, is what is happening to our bodies and minds on the inside.
It doesn’t matter what the stressor is, the body reacts and needs to complete what they call the “stress cycle.” If the stressor is an unpaid bill that you are worried you cannot afford, paying the bill does not complete the stress cycle in your body. The stress of the experience remains unprocessed until you complete the cycle. The cycle has a beginning, middle and end. However, many of us stay stuck in the middle and do not know how to bring it to an end and so it builds up in in our bodies and causes burnout.
The idea is to allow the emotions and stress cycle out of your body rather than holding on to it.
A podcaster described it as “taking out the trash” – we cannot prevent the trash (stress) from coming in, but it is important to take it out, not just let it pile up and pretend it doesn’t exist. There are actions you can take to complete the stress cycle, these include:
• Physical Activity
• Breathing
• Laughter
• 20 second hugs
• Connection with others
• Crying and,
• Creative Expression.
By completing the stress cycle, we allow the stress to move through us and not accumulate in our bodies.
As author Ann Lamott said, “Almost everything will work again if you unplug it for a few minutes, including you.”
Every May, we join with the Administration for Community Living to celebrate Older Americans Month, when we recognize the positive contributions that older Washingtonians have on our communities. This year, Governor Jay Inslee signed a proclamation honoring the state’s older residents and proclaiming May to be Older Americans Month in Washington.
This year’s theme, Aging Unbound, offers an opportunity to explore a wide range of aging experiences and to promote the importance of enjoying independence and fulfillment by paving our own paths as we age.
This May, join us as we recognize the 60th anniversary of OAM and challenge the narrative on aging. Here are some ways we can all participate in Aging Unbound:
• Embrace the opportunity to change. Find a new passion, go on an adventure, and push boundaries by not letting age define your limits. Invite creativity and purpose into your life by trying new activities in your community to bring in more growth, joy, and energy.
• Explore the rewards of growing older. With age comes knowledge, which provides insight and confidence to understand and experience the world more deeply. Continue to grow that knowledge through reading, listening, classes, and creative activities.
• Stay engaged in your community. Everyone benefits when everyone is connected and involved. Stay active by volunteering, working, mentoring, participating in social clubs, and taking part in activities at your local senior center or elsewhere in the community.
• Form relationships. As an essential ingredient of well-being, relationships can enhance your quality of life by introducing new ideas and unique perspectives. Invest time with people to discover deeper connections with family, friends, and community members.
For more information, visit the official OAM website, follow ACL on Twitter and Facebook, and join the conversation using #OlderAmericansMonth.



I want to use this space today to share a little more about our commitment to wellbeing in ALTSA. The pandemic brought wellbeing into sharp focus for all of us as a country, an organization, and individuals. According to the World Health Organization, our country has lost 1,121,819 people to covid since the beginning of the pandemic. When faced with our own mortality, most of us did some serious rethinking about our priorities with wellbeing rising to the top for many of us.
As an organization, we already knew wellbeing was important. We’ve talked about and supported workplace wellness in ALTSA for many years. But with the shift to remote and hybrid work, we really had to think about wellbeing differently. Wellbeing “in the workplace” means wherever you do your work. It means your whole health. It means your sense of belonging, connection, work/life balance and integration. It means being flexible and supportive. It means creating psychological safety, being vulnerable and honest as well as helping people grow and thrive in their careers. Here is a great article from Gallup about what employee wellbeing is and why it matters.
To reflect our commitment to wellbeing in ALTSA, we felt it was important to “name it and claim it.” This meant adding a Welling goal to our 2023-2025 Strategic Plan and getting a question added to the annual Employee Survey so we can measure our success. Watch for opportunities to learn about and give feedback on ALTSA’s 2023-2025 Strategic Plan in June and July and plan to engage in the Employee Survey, which will run this fall. Your voice and feedback are crucial to our success in expanding and embracing wellbeing in ALTSA
If you missed the Wellness message in the winter edition of this magazine, click here and go to page 13 to find links to some great resources and learn more about what we are doing to promote wellness in ALTSA.
Amy Besel By Michelle Joseph, ALTSA EDAI Administrator
By Michelle Joseph, ALTSA EDAI Administrator
I recently attended a train-the-trainer leadership workshop on the Americans with Disabilities Act (ADA). Cornell University has vetted and approved the curriculum provided for our use for training across the United States. It was such an honor to learn so much through this program. Here is a summary of the program:
The ADA Trainer Network (ADA TN) is a group of individuals nationwide who use a curriculum provided by the ADA National Network to educate local communities about the ADA. As our partners, they help to spread the word about the rights and responsibilities of employers, service providers, municipal entities, and private businesses under the ADA. The curriculum has more than 40 modules, each with its own facilitator’s guide. The curriculum covers all Titles of the ADA, disability awareness, serving customers with disabilities, and information about accessible technology. ADA TN members participate in “train-the-trainer” events through their regional ADA Center to learn to effectively deliver the materials, including how to customize training sessions to particular audience needs. We believe ADA TN members are excellent resources within their communities and that their training helps foster relationships between individuals with disabilities and entities with responsibilities under the ADA locally. (ADA Leadership Network, n.d.)
At the end of the program, which was so well organized, detailed, and facilitated by two passionate individuals, we had to submit a project. The project was for each person to create and present a Uniquely YOU project. The project involved completing a logo/symbol that embodied what differentiates us from others. The challenge was to think of a time at work when you felt you had a powerful and positive impact on people with differing abilities. The idea for this thought process was for the participants to consider their training style when presenting material that has
been provided to them, emphasizing staying within the path or intent of the material. The first thing that came to mind was the magnitude in which we compare our ability to that of others. So often, we focus on how a person delivers their training, how they deliver their speech, how they conduct their meetings, and how they structure their teams. It all flows seamlessly and without effort. So, we imitate and compare our delivery to that of others. I encourage you to take your unique approach to delivery. You are unique in your way! Taking pointers or advice on best practices to deliver a training, speech, or presentation is perfectly fine! However, take those pointers and show up uniquely you! You’ll feel much better, and your audience will be able to connect with you for who you are authentically! You’ve got this! Make it your own! That’s what our class did! Here are some examples of the Uniquely You projects.
To learn more about ADA, consider the following resources/web-based courses:
• ADA National Network
• ADA Foundations (formerly ADA Basic Building Blocks)
• ADA Title I: Employment Requirements
• ADA Title II Tutorial
• Architectural Accessibility Laws
• At Your Service: Welcoming Customers with Disabilities
• Federal Court Concepts Training Module
• Overview of Disability Rights


On April 10, 2023, Lori Rolley received a recognition of service for 45 years of faithful service to the State of Washington.
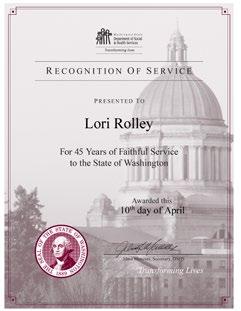
Lori Rolley is the Financial Policy Analyst for the Washington State Department of Social and Health Services (DSHS), Aging and Long-Term Support Administration (ALTSA).
She grew up in Port Angeles and was inspired to work with older adults and people with disabilities by her mother, an RN who was the Director of Volunteer Hospice of Clallam County for over 35 years. She started working for DSHS in Spokane as a college intern in 1977. In 1980 Lori began working primarily with the Institutional and SSI-related Medicaid programs at Medical Assistance Administration (now called Health Care Authority) and Home and Community Services in Olympia. She is the program lead for Chapter 182-513 WAC (Institutional) and Chapter 182-515 WAC (Home and Community-Based
Lori is affectionate and known to her unit members as “M.O.M.” not only because she has mentored them in their current roles but because she is the “Mother of Medicaid.”
Waiver). Lori enjoys hiking in the forest, walking on the beach, kayaking in Puget Sound, and playing with her kitties Gracie and Sir Walter “Wally” Rolley.In April, I had the joy of virtually interviewing Patty and Debbie, two clients who regularly attend an Adult Day Health (ADH) Center in Everett. The unique pair met at the ADH center five years ago and have been inseparable since then. The ladies were sincere, honest, and cheerful throughout the interview, and they were excited to share their experiences.

Full Life Care has two Adult Day Health Care centers, one in Seattle and one in Everett. Their programs provide health and wellness services that that work to challenge minds, keep bodies moving and lift the spirits of each participant.
Their centers have programs that run five days a week for four hours a day. They offer skilled nursing and rehab services, including wound care,medication management and diabetic care, and tube feedings. They have occupational therapists that can help with fitting wheelchairs or other assistive devices, Falls Prevention, and general exercises tailored to the individual client’s
needs. They also have case managers and social workers They aim to keep folks living independently in the community or at the lowest level of care possible.
Please tell us about yourselves.
Patty: I am currently handicapped and in a wheelchair. I like to do beadwork and arts and crafts. I say I think I’m kind of interesting. Maybe a little bit of a pain, but that’s OK. *laughs* I come by it naturally and am a bit of a comedian.
Debbie: I like reading, doing word search puzzles, and watching TV. Some favorite shows are Wheel of Fortune, Jeopardy, Walker Texas Ranger, and The Bachelorette. I like the Mariners, Kraken, and the Seahawks.
Tell us about the first time you met at this center and briefly describe how your friendship formed.
Patty: I remember meeting around Halloween one year and dressing up like a clown.
Left to Right: Debbie and PattieDebbie: I dressed up as a Seahawk cheerleader.
Patty and I have been friends for a long time. I go to Patty’s house for lunch. Patty’s brother is my boyfriend, and we have been dating for eight months. We met at Patty’s place.
Patty: We (Debbie and I) like to hang out together and have fun.
What is the most valuable thing you enjoy about coming to this center.
Debbie: I like meeting new people, making friends. Expect friendships. There is a welcome committee. If someone new comes in right away, we welcome them. We want them to feel at home and ease. The staff is very nice and supportive.

Patty: Interacting with the staff and being creative. I like the arts and crafts. And sometimes, they exercise, but only some of the time. The center has dance parties every week and the music style change every week. They can expect plenty of exercises, be wellrespected, and be appreciated.
I knew someone that used to come here. She was scared to death the first day she arrived. So, I went over and told her, “Don’t be scared. You’re OK. I’ll keep you company.” We’ve been friends ever since then. They’re all good people here. If someone gets out of line here, staff will let you know to “knock it off,” *laughs*
When did you first hear about this Adult Day Health Center (ADH)? What attracted you to this center?
Debbie: My family was looking for a place with activities. We found this place and called. I came in for an interview, and I was accepted. I needed something to do because I was bored at home. I needed activities and friendships. Everybody here is open and friendly here. The staff is very supportive. If you need something, they’ll take their time with you; they encourage us.
Patty: I mainly wanted to get out of the house and come, socialize, exercise, and do something healthy.
Debbie: Emily or someone will ask if we liked the lunch. The staff receives feedback from the clients, and if we do not like something, they (staff) will take it out of the menu.
Patty: For lunch, we have stuff like rice, chicken, vegetables, and fruit, and milk always comes with our meals. They are healthy meals.
What was your life like before coming to this Adult Day Health Center?
Patty: Before coming to the center, life was boring. I was lying around, watching tv. I used to smoke. I don’t do that anymore. The center has improved our lifestyle. The staff makes you want to come back. The team is very supportive and ensures we are doing OK or if there’s any change in our health.
Staff gives Pattie a makeover for Valentine’s DayDebbie: It was very dull and boring (life). I have very supportive siblings, and they encourage me all the time. I highly recommend anyone that qualifies.
How has this program changed you?
Patty: It’s taught me patience. How to work with other people. The staff is good about letting us know what we are doing is wrong, but they don’t embarrass us in front of other clients. They take us to the side and talk to us. We have nurses here on hand, so if we need medical attention, they’ll come and check us and see what’s wrong. They keep an eye on our blood pressure and weight. The staff makes sure we are doing good at home too. And that we have good caregivers.
Debbie: It’s taught me to relax (laughs) and patience, too. If staff is available and you need to talk, they will speak to you. Emily, our manager, is available to talk to you. I do a lot of crafts with a staff member. I will use the exercise bike when I meet with the OT students in training. I recommend all these staff members. Friendly and supportive. If I am trying to lose weight, a nurse will check my weight and give me tips on what to do. They will weigh me once a week and check my oxygen and heart rate. The nurse on staff here is good, too. The team made themselves
available here and at home too. Make sure that we are safe and healthy.
Is there anything else you would like to share with us?
We really enjoy coming here and being able to socialize with our friends. Nursing students came over for Valentine’s Day and gave us a “makeover,” and did our hair and nails. The staff treats us like family. They let us know that we are appreciated.

Acknowledgements:
Thanks to Susan Worthington, Nursing Services and Adult Day Services Program Manager, for putting me in contact with the Adult Day Health Center staff.
And special thanks to Stacy Christ, Adult Day Health Program Development Director, and Emily Roberts, Program Manager, for helping me coordinate the interview with Debbie and Pattie.
Nursing student is giving Debbie a manicure for Valentine’s DayThe Washington State Health and Human Services Coalition – a cohort of Washington state health and social services agencies – has just published the Washington State Action Plan for Removing Barriers to Health and Human Services.
The Washington Plan for Removing Barriers to Health and Human Services sets forth a future where accessing benefits is simple and seamless. Cathy Kinnaman, HCS Director, and Babs Roberts, CSD Director, worked together to lead work around establishing a humancentered design (HCD) community of practice and developing recommendations on streamlining applications for assistance programs. “The opportunity to research innovative policy options to streamline eligibility and enrollment while also learning how to proactively seek out and include the voices of our clients in the systems we design was an irresistible combination for me,” said Cathy Kinnaman, “This work is so important and will truly make a difference to the people who need to access our services.”
The plan outlines two goals:
• Remove client barriers to accessing benefits. We imagine a future where clients can seamlessly apply for multiple programs (Apple Health, SNAP, TANF, and WCCC) in less than 20 minutes and immediately know their eligibility status.
• The state and its programs comprehensively view clients and share information across organizations to offer other benefits for which the client may qualify proactively.
“With the right technology in place, individuals should no longer need to spend hours navigating multiple complicated systems,” said Christine Nolan, deputy chief information officer at the Washington State Health Care Authority. “Our north star is to provide the most complete care possible, connect people to services, and ensure they maintain access to those services.”
Human-centered design principles drive this vision. Human-centered design is an approach to problemsolving that puts people’s needs, wants, and limitations at the center of the design process. It involves understanding the end-users perspectives and incorporating their feedback to create products, services, and experiences that are more effective,
usable, and desirable. Michael Sheehan, Unit Manager in the Training, Communication, and Workforce Development Unit at HQ, was crucial in helping this work get rolling. He provided initial overview training to workgroup members on human-centered design and participated throughout the plan’s development. Other HCS HQ staff joined him on a sub-workgroup to create training opportunities on HCD by partnering with the University of Washington, Evans School of Public Policy and Governance. The goal is to provide recommendations to the HHS Coalition on opportunities to expand expertise in HCD across multiple state agencies. It has led to implementation of a new, crossagency Community of Practice.
The HHS Coalition worked closely with Benefits Data Trust (BDT) to create the action plan. This national nonprofit improves health and financial security by harnessing the power of data, technology, and policy to provide dignified and equitable access to assistance. BDT guided the development of the Action Plan and provided expertise in reducing barriers to accessing benefit programs.
“Washington is applying innovative strategies to improve the ways families learn about, apply to, and access benefit programs,” said Trooper Sanders, CEO of Benefits Data Trust. “We applaud the HHS Coalition’s commitment to comprehensive improvement of benefits access and look forward to helping Washingtonians connect to the programs they need in a way that is dignified, equitable, and proactive.”
In 2018, to promote service coordination, the leaders of Washington’s state health and human services organizations decided that increased collaboration on IT investments is critical to improving the health and well-being of the people, families, and communities of Washington. The decision established the HHS Coalition as a collaborative to govern IT project investments across Washington’s state HHS organizations, and the Washington Legislature formally recognized the HHS Coalition in the 2019 legislative session. The HHS Coalition includes the Department of Children, Youth, and Families, the Department of Health, the Department of Social and Health Services, the Washington Health Benefit Exchange, the Health Care Authority, and Washington Technology Solutions. The Office of Financial Management is an exofficio member advising on issues around state financial budget and legislative processes.

Home and Community Services (HCS) utilizes nursing facility case managers to actively work with Medicaid residents from admission to a nursing facility to achieve the resident’s transition goals and potential. This includes meeting face-to-face with residents early in their admission and working with families and staff at the nursing facility to advocate for therapies, treatments, and education provided in a way that supports the resident’s transition goals and timelines. By ensuring nursing facility residents (and their informal supports) have information about community long-term services and supports, the NFCM collaborates with the nursing facility to create a transition plan and a community care plan which provides services in the least restrictive, most appropriate setting that meets the person’s care needs while honoring choice and preference.
ALTSA embraces the belief that individuals with very high care needs can be cared for and supported in various settings by implementing waivers and state plan services that provide alternatives to nursing facility care. Nursing Facility Case Managers play an essential role in ALTSA’s Mission to transform lives by promoting choice, independence, and safety through innovative services and a vision that people are healthy, safe, and supported and state taxpayer resources are guarded.
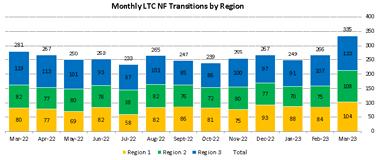
We would like to shine a light on a remarkable break through with our statewide NFCM transition work, all 3 regional NFCM teams have achieved triple digit transition counts for the month of March!
This is remarkable for a number of reasons, but most importantly, we have not seen all 3 regions achieve triple digit transition numbers in one month since March of 2020 or pre-pandemic.
Our NFCM teams continue to pull together in this very complex institutional community transition work and the results of these efforts are clearly demonstrated in the following,
NFCM, Yachna Chumber, worked to support a 47-year-old individual transition from a Skilled Nursing Facility (SNF) to an Adult Family Home (AFH) close to family. The client had been residing at the SNF since March 2022. The previous discharge attempts had failed as the client exhibited behavioral challenges, including being physically abusive to staff and other residents. The client was assigned a 1:1 sitter to help the client safely manage his behaviors. The client also had functional deficits requiring assistance with most personal care and went to dialysis three times a week.
Region 1: Karen Mendoza transitioned 9 individuals back out to the community. Commella Prigan & Sally Wilkins each transitioned 8 individuals to their preferred community homes. Sharon Sneed transitioned 7 clients to their community homes. Carol Bannister, Nenita Bosnar, Kayla Cordova, & Yvette Housley each transitioned 6 individuals to the community settings of choice. The average age of R1 client transitions: 71 yrs. old (Age Range: 24 - 99 yrs. old). The average SNF length of stay: 146 days (Length of Stay Range: 8 days to 9+ years) Amazing!
Region 2: Lorraine Howard & Dipa Trivedi each transitioned 9 individuals to their community settings of choice. Rosa Casas, Nichole Kyle, & Deanna Weathermon each transitioned 6 Medicaid recipients back out to the community. The average age of R2 client transitions: 73 yrs. old (Age Range: 34 - 102 yrs. old). The average SNF length of stay: 156 days (Length of Stay Range: 9 days to 5+ years) Awesome!
Region 3: Jamie Hanson transitioned 13 Medicaid recipients to their preferred community settings. Carolyn Jacoby transitioned 11 clients to their community settings of choice. Michelle Bellah & Rebecca Swafford each transitioned 9 individuals back out to the community. Christina Tarnowski transitioned 6 folks to their community homes. The average age of R3 client transitions: 70 yrs. old (Age Range: 30 - 94 yrs. old). The average SNF length of stay: 152 days (Length of Stay Range: 13 days to 3+ years!) Excellent!
An AFH provider visited the client, who expressed interest in moving forward with the client transitioning to their AFH. NFCM confirmed that AFH held a Specialized Behavior Support contract and had experience managing residentcomplex behavioral needs. NFCM referred the client to RSW-SBS as the client already had 1:1 support at SNF to manage behaviors. SBS would provide continued 1:1 support in the AFH setting. NFCM coordinated with the dialysis social worker, SNF social worker, and AFH provider for discharge planning to ensure continuity of care and ensure the client had appropriate durable medical equipment to have a greater likelihood of a successful transition. NFCM also coordinated with the dialysis social worker to move the client to a different dialysis run time that would work with the AFH schedule. Otherwise, AFH would have needed more time to accept the client due to the early morning run time.
One day before discharge, the client struck his nurse at dialysis, which resulted in dialysis having a meeting to determine the future of the client’s continued services at their center as he had also exhibited multiple behaviors at dialysis towards staff. NFCM communicated the incident to AFH and was able to follow up to ensure that the behavioral health provider client was referred to also had a prescriber on staff as requested by AFH. SNF social worker coordinated a hospital bed delivery and delivered the client’s belongings to the AFH. On the day of discharge, NFCM ensured the dialysis social worker had contact information for the AFH provider to relay new dialysis center/treatment times for continuity of care over the weekend. NFCM also staffed the case with receiving RCCM to ensure receiving RCCM was aware of the client’s behaviors before the file transfer. The client was discharged as planned and is living in the community.
