Essential Update: Type 2 Diabetes Management 2025
Why Every Physician Needs This Synopsis


Why Every Physician Needs This Synopsis


Paradigm Shift
Move from glucose-centric to cardio-renal protection-first approach
Early Intervention
SGLT2i/GLP-1RA now recommended independent of HbA1c in high-risk patients
Evidence-Based
Comprehensive review of 126 studies including major cardiovascular outcome trials
Guideline Convergence
Updated recommendations from 9 major professional societies (ADA, ESC, ACP, WHO, IDF)
Technology Integration
New evidence on CGM, insulin pumps, and digital health tools

Cardiovascular Events
Reduction with specific SGLT2i/GLP-1RA
Heart Failure
Reduction in hospitalizations
Kidney Disease
Reduction in progression
Diabetes Remission
Up to 46% rates with intensive lifestyle interventions

Update your treatment algorithms today
Patient Safety
Reduce cardiovascular events and hypoglycemia
Cost-Effectiveness
Optimize medication selection and monitoring
Align with latest evidence-based standards

Source: Kalyani RR, et al. Diagnosis and Treatment of Type 2 Diabetes in Adults:
A Review. JAMA. 2025;doi:10.1001/jama.2025.5956


SGLT2 inhibitors and GLP-1 receptor agonists should be initiated early (often independent of HbA1c levels) in patients with established atherosclerotic cardiovascular disease, heart failure, or chronic kidney disease, based on proven outcome benefits.
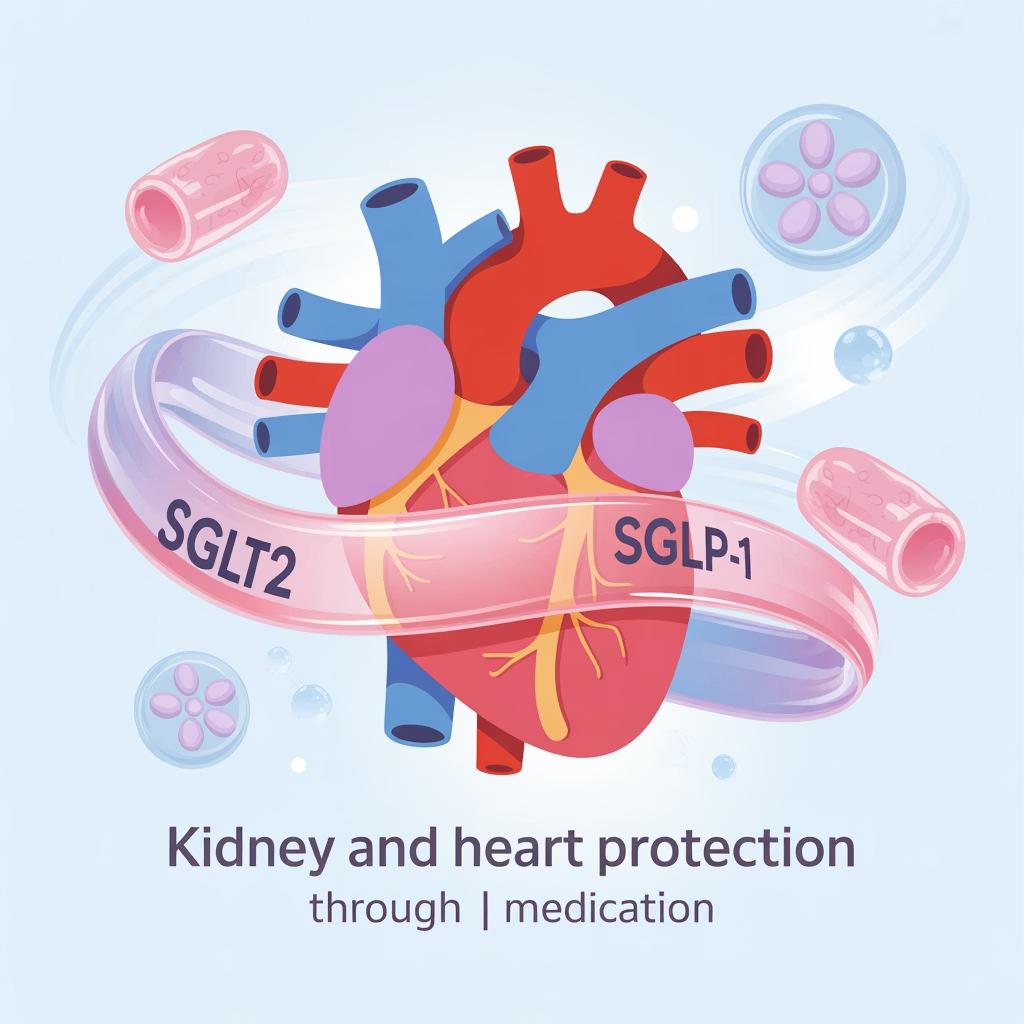


While metformin continues as first-line therapy for most patients without comorbidities, guidelines now support starting SGLT2i or GLP-1RA concurrently with or prior to metformin in high-risk patients.


Standard Target
Target HbA1c <7% for most adults
Younger, Healthier Patients
Individualize to <6.5%
Older Adults
7.5-8.5% for older adults or those with limited life expectancy/high hypoglycemia risk

When injectable therapy is needed, prefer GLP-1RA or dual GIP/GLP1RA over insulin due to lower hypoglycemia risk and weight loss benefits, unless severe hyperglycemia (HbA1c >10%) or symptoms are present.



CGM reduces HbA1c by ~0.31% compared to fingerstick monitoring and should be offered to insulin-treated patients and considered for others on glucose-lowering therapy.


Intensive lifestyle interventions can achieve diabetes remission in up to 46% of patients at 12 months.
No single diet is superior, but structured programs with significant calorie restriction show remarkable results.


Avoid glyburide in older adults; prefer shorter-acting sulfonylureas (glimepiride, glipizide) when cost is a concern.
Consider deintensification when adding SGLT2i or GLP-1RA to insulin/sulfonylurea regimens.


1 Screening
Screen all adults g35 years every 3 years (annually if prediabetes).
2 Stable Monitoring
Monitor HbA1c every 6 months when stable.
3 Therapy Adjustment
Monitor HbA1c every 3 months when adjusting therapy.

Consider insulin pumps with automated delivery systems for appropriate patients on multiple daily injections. Diabetes technology may warrant endocrinology consultation.



Education
Refer all patients for diabetes selfmanagement education
Nutrition
Medical nutrition therapy for all patients
Consider endocrinology referral for complex insulin regimens, lack of expected response, or when screening for other diabetes types is needed
These points reflect the evolution toward more aggressive early intervention for cardiovascular/kidney protection while maintaining individualized glycemic targets and emphasizing comprehensive care approaches.