Associate Professor of Medicine
Director of Education, DHM
Associate Residency Program Director, MSH
Acting Internship Clerkship Director
Director of the Career Hospitalist Advisement Program

Associate Professor of Medicine
Director of Education, DHM
Associate Residency Program Director, MSH
Acting Internship Clerkship Director
Director of the Career Hospitalist Advisement Program



Thinking about the last 5 years, what changes have you noticed in how we teach and train in the era of digital medicine—both in terms of trainee education and your own teaching practices?


While it has been ongoing for several years, the digital transformation was accelerated by the COVID-19 pandemic. Physical distancing mandates created a vacuum in traditional inperson didactic curricula, spurring a rapid proliferation in digital platforms and content. In this new educational landscape, the digital space has become integral to how we access information and communicate with one another. Thus, the modern medical educator must be able to deliberately appraise both the advantages and pitfalls of the digital world and traditional modalities. Our challenge now is to thoughtfully integrate digital and traditional platforms to help the modern learner effectively acquire information and build community

❑ Increased use of Technology (EMR/APP’s)
❑ Expansion of E-Learning and Virtual Platforms
❑ Simulation Based Learning ( AR/VR )
❑ Social Media Based Medical Education
❑ Artificial Intelligence Boom
❑ Learning Analytics and Personalized Education



“Machines, for all their capabilities, cannot provide the empathetic touch, a comforting hand, or supportive words during difficult diagnoses. Dr. Abraham Verghese of Stanford Medicine has stressed the importance of not overly focusing on the "iPatient"—the virtual representation of a patient based on tests and data—since it cannot replace the act of physically examining a patient or building a personal connection”.

“I wish we had more time for bedside teaching”
“I only wish all faculty could equally deliver high yield teaching points that are patient related and time conscious”
“We need a better balance of education on work rounds”
“Some of the best faculty have a true talent for physical exam skill development”

Step 1: Disrupt the Digital Drag/Bedside 2.0
❑ Set clear expectations for device use

❑ Model appropriate use
❑ Incorporate technology into learning
❑ Shift focus on mindfulness and “being present”
❑ Designate “Tech-Free” zones or times
❑ Call attention to key learning moment



Planned Breaks
Minimize Cognitive load
Brief Digital Checks
Clear Urgent Messages

Case Presentations

Active Participation
Clinical Reasoning Management

Methods: Recruited faculty from 10 institutions including clerkship directors + prior research experience in medical education and conducted bedside rounds

Data Collection/Analysis: Digitally recorded one to one interviews identifying themes and categories generating a codebook to facilitate analysis
Results: All 10 institutions participated 34 interviews conducted focus was directed at key thematic areas
Journal of Teaching and Learning in Medicine Vol. 25, Iss. 4, 2013




















❑Preparation is everything
❑Create a safe and welcoming environment
❑ Email welcome before you come on service
❑Set clear expectations from day one
❑Identify your learners' strengths/interests
❑Use icebreakers
❑Draw a mental image your time together

❑ Chart check the night before and get in early on your first day
❑ “Stealth Round” virtually on your new admissions (EMR efficiency)
❑ Pick 1 or 2 topics that you want to tackle that day
❑ Plan and map out your teaching session: -Organization/Timing -How will you engage the learner -Take home points -Homework assignments -Digital engagement plan -Prepare your technology







❑ Personal investments in your learner and who they are as human beings

❑ Take some time for those “weekend plans” and “fun facts”
❑ Check in on the pulse of your team often
❑ Let your team leads lead









❑ Diagnostic assessor
❑ Content curator
❑ Technology adopter
❑ Learner Navigator
❑ Professional coach
❑ Clinical role model
❑ Learning environment designer/implementer






❑ Demonstrate efficient workflow
❑ Review “smart setup” of dashboards
❑ Template and smart phrase review
❑ Highlight best practices
❑ Set key standards for note writing
❑ Integrate decision support tools (order sets, drug interactions, best practice alerts)












Featured Technical Tools: Chat GPT4o and Loom AI for Video Screen Capture
Practical Uses: Create curated podcast links for targeted clinical scenarios that can easily be shared with UME/GME trainees. Consider prompt engineering if you are looking for a specific Podcast.
Example: Mr. Johnson is a 70 year old male with a known history of advanced COPD who presented with acute hypoxic respiratory failure was admitted to the MICU, course was complicated by an acute stroke requiring a tracheostomy and a PEG tube placement and he remains ventilator dependent. He is transferred to gen med teaching for continued care.


Technology driven
Board review focused
Knowledge development
Allows for corrective guidance
Example:
55-Year-old male with ETOH-Cirrhosis presenting with hypotension, acute blood loss anemia in the setting of an acute variceal bleed.



❑ LLM Natives are coming
❑ 30% of undergraduate students use AI
❑ 20% of matriculating MS4’s use Chat GPT
❑ 67% of younger generations have a positive view of AI
❑ By 2034: 50-70% of learners could be using LLM’s in general education and 60-80% in medical education.
Real-time assessment and feedback: for all physicians at all levels of training
❑ Technological improvement: longer text windows, entire patient chart analysis, fewer technical errors, HIPPA compliant models.
Cognitive tasks: LLM will surpass human performance in a variety of cognitive tasks
❑ Residency Integration: ambient listening, note generation, patient portals
❑ Textual analysis: letters of support, feedback, core integration into analytic workflow
Patient engagement: routine engagement with LLM
❑ Educational implications: explosion of new LLM driven learning tools which will disrupt the education landscape
Physician Experience: change in the overall experience at all levels of training


❑ Assessment of Clinical Reasoning: development and validation of machine learning models for assessment of resident clinical reasoning based on H&P
❑ Communication Improvement: enhanced communication strategies for difficult case scenarios (i.e., Pancreatic CA case)
❑ Predictive Outcomes/Procedures: assist with gesture analysis and prediction of clinical outcomes using video assessment (i.e., robotic prostatectomy)
❑ Bias Assessment: Used to detect and mitigate bias in text
University of Cincinnati (AAIM Conference)


❑ Quick Lesson Plan Generation
❑ Clinical Guidelines and Evidence
Summaries
❑ Landmark Trial Summary for dissemination
❑ Clinical Guidelines/best practice review
❑ Clinical case simulation
❑ Interview Prep
❑ LLM’s to explore:
-BioGPT (literature focus)
-MedPalm (clinical questions)












“Medicine is a science of uncertainty and an art of probability, and in the digital age, data can turn the art into precision.”
Adapted from William Osler
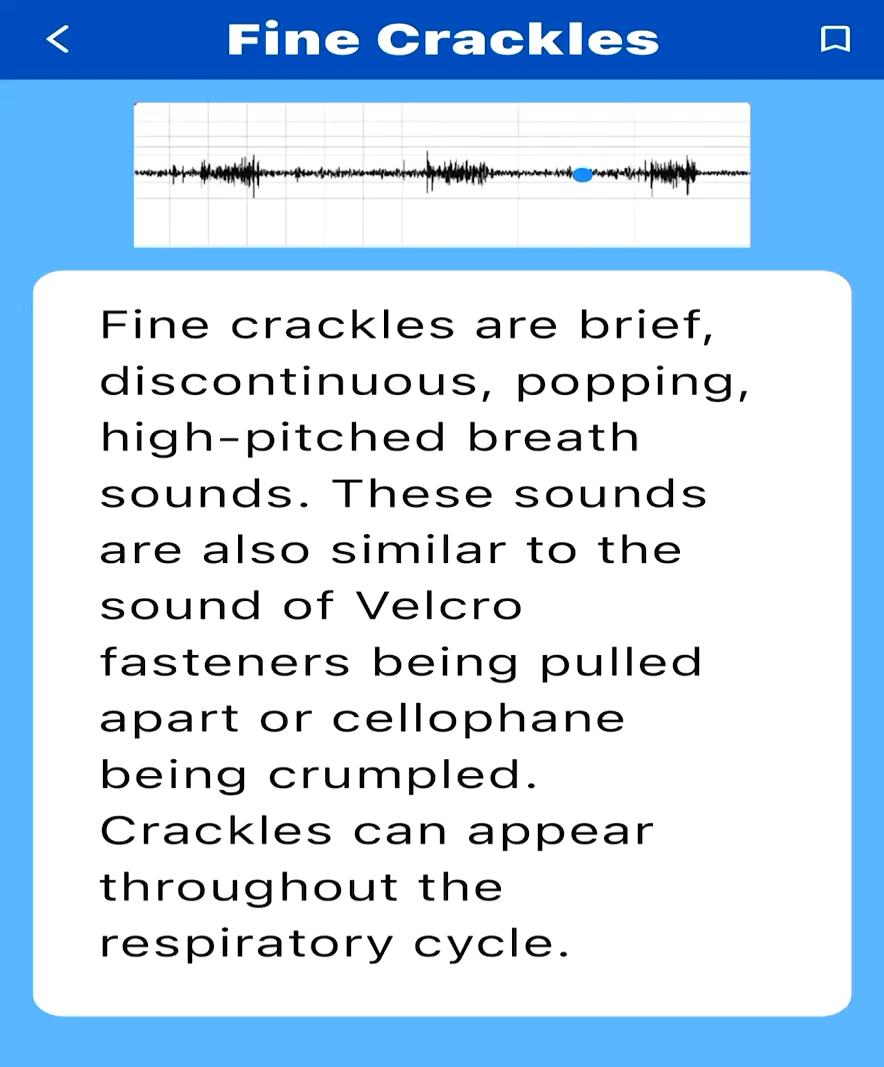
SMART DEVICE APPS:
❑ Auscultation Heart Sound
https://play.google.com/store/apps/details?id=com.rer.medapps.au scultation&hl=en_US
❑ Lung/Heart Sounds
https://apps.apple.com/us/app/lung-heart- sounds/id6477601947
❑ Poll Everywhere
https://www.polleverywhere.com/
WEB BASED RESOURCES:
❑ Radiopaedia-Radiology resources
https://radiopaedia.org/
❑ Perplexity Notion
http://perplexity.ai
❑ Notion
http://notion.so
PODCASTS:
❑ Curbsiders
https://thecurbsiders.com/
❑ Core IM
https://www.coreimpodcast.com/
❑ Clinical Problem Solvers
https://clinicalproblemsolving.com/
❑ Core IM
https://www.coreimpodcast.com/
❑ Annals On Call
https://www.acpjournals.org/topic/webexclusives/annals-on-call
