


















Dear Friends of FirstHealth,
Happy spring! Spring is a season of growth—a perfect time to re ect on how far we have come and look ahead to the future. It’s tting, then, that this spring issue of FirstHealth Magazine marks a milestone in FirstHealth’s journey: our 30th anniversary as a health system.
For me, this celebration is especially meaningful. In 1994, I received an internship at FirstHealth while nishing up my undergraduate degree, and I was hired upon graduation. Just a year later, in 1995, I was working in corporate education when FirstHealth of the Carolinas was o cially formed.
To return 25 years later as CEO has been one of the greatest honors of my life.

Over the past three decades, FirstHealth has grown from a single hospital into a nationally recognized health system. Our commitment to providing high-quality care has remained constant, and we have expanded our reach in ways that continue to strengthen the communities we serve. From milestones such as the creation of FirstHealth Dental Care to the opening of the Reid Heart Center, our focus has always been on meeting the needs of our patients, even beyond traditional hospital walls.
This spirit of innovation and dedication has propelled us forward. Today, we are preparing to break ground on a new hospital in Montgomery County, ensuring rural health care remains a priority. We are also investing in the future of our workforce through FirstFutures, a program designed to inspire and support the next generation of health care professionals.
FirstHealth.org
FIRSTHEALTH OF THE CAROLINAS
Cindy Goodman, Ed.D., Chair
David Wood, Vice Chair
Arthur Medeiros, Corporate Secretary
Ray Allen, Treasurer
Gary VonCannon, Immediate Past Chair
Mickey Foster, MHA
Matthew Harmody, M.D.
Beth Jones
Susan Keller
Jefferson Kilpatrick, M.D.
Charles Kuzma, M.D.
Wayne Lucas, M.D.
James Obi Tom Pashley
Sushma Patel, M.D.
Alexander “Sandy” Stewart, Ph.D.
Elizabeth Webster
Chief Executive Officer
FirstHealth of the Carolinas Mickey W. Foster, MHA
President, FirstHealth Physician Group Daniel R. Barnes, D.O.
Chief Information Officer
FirstHealth of the Carolinas Chris Beasley, MBA
President, Eastern Region Susan K. Beaty, MSN, R.N.
Chief Medical Officer
FirstHealth of the Carolinas Jenifir Bruno, M.D.
Chief Financial Officer
FirstHealth of the Carolinas Jeffrey A. Casey
President, The Foundation of FirstHealth Dana L. Casson, CFRE
Chief Operating Officer
FirstHealth of the Carolinas Jonathan Davis, MPH, FACHE
Vice President, Finance
FirstHealth of the Carolinas Chris Fraley, CPA
Chief Strategy and Innovation Officer







I invite you to read more about FirstHealth’s incredible journey in this issue of FirstHealth Magazine. As we celebrate 30 years, I am grateful to the providers, employees, volunteers and community members who have shaped FirstHealth into the organization it is today. I look forward to what we will accomplish together in the years to come.

FirstHealth of the Carolinas Amy Graham, MHA
President, Western Region Kerry Herbine, FACHE
President, Southern Region Christy Land, MSN, R.N.
Chief Quality Officer
FirstHealth of the Carolinas Cindy McNeill-McDonald, R.N.
Vice President, Operations
FirstHealth Moore Regional Hospital Matthew Prestwood, MHA
Chief People Officer
FirstHealth of the Carolinas Berni Szczepanski, MBA
FirstHealth of the Carolinas, a not-for-profit health system, is headquartered in Pinehurst, North Carolina, and comprises Moore Regional Hospital, Montgomery Memorial Hospital, Moore Regional Hospital – Richmond, Moore Regional Hospital – Hoke, The Foundation of FirstHealth and the FirstHealth Physician Group. Comments on the FirstHealth magazine or changes of address should be directed to (800) 213-3284 or Marketing@FirstHealth.org.
FirstHealth is published by the Strategic Marketing and Communications Department. For more information on any of the programs or services offered by FirstHealth of the Carolinas, please call (800) 213-3284 or visit FirstHealth.org.



Designer Eric Baker
Photographer Eddie Harris, CPP
Writers Emily Sloan, Derek Medlin, Camryn Quick, Rebecca Hummel


FirstHealth Moore Regional Hospital, including its Hoke and Richmond campuses, has been recognized as one of America’s 100 Best Hospitals for Orthopaedic Surgery by Healthgrades, the leading resource consumers use when searching for a doctor or hospital. Moore Regional also earned the 2025 Orthopaedic Surgery Excellence award, placing the hospital among the nation’s top 10% for overall orthopaedic services. These achievements place Moore Regional in the upper echelon of hospitals for orthopaedic care nationwide.
FirstHealth also received the following awards from Healthgrades this year:
H Named One of America’s 50 Best Hospitals for Outpatient Joint Replacement for Two Years in a Row
H Five-Star Recipient for Outpatient Total Knee Replacement for Two Years in a Row
H Five-Star Recipient for Total Knee Replacement for 2025
H Five-Star Hip Fracture Treatment for Four Years in a Row
H Five-Star Recipient for Outpatient Hip Replacement for Two Years in a Row
H Five-Star Recipient for Pacemaker Procedures in 2025
H Five-Star Recipient for Treatment of Diabetic Emergencies in 2025 for Three Years in a Row
H Five-Star Recipient for Outpatient Prostate Care Excellence in 2025
H Named One of America’s 50 Best Hospitals for Outpatient Prostate Excellence
H Recipient of the Healthgrades Outstanding Patient Experience Award for 17 Years in a Row (2008-2024)
In November, FirstHealth’s Montgomery Memorial Hospital earned a 2024 Performance Leadership Award for excellence in quality. Compiled by The Chartis Center for Rural Health, the Performance Leadership Awards recognize top quartile performance (75th percentile or above) among rural hospitals in quality, outcomes and/or patient perspective.
FirstHealth of the Carolinas is happy to announce that we have once again earned a distinguished three-star rating from The Society of Thoracic Surgeons (STS) for patient care and outcomes in isolated coronary artery bypass grafting (CABG) procedures. The three-star rating, which is the highest category of quality, places FirstHealth’s Cardiovascular & Thoracic Surgery program among the elite for heart bypass surgery in the United States and Canada.
Earlier this year, William C. Kitchens, M.D., was named surgical director of the Chest Center of the Carolinas. In this role, Dr. Kitchens will collaborate with our team of surgeons and pulmonologists to develop a robust thoracic surgery program focused on advancing patient care. Under Dr. Kitchens’ leadership, we aim to expand the robotic thoracic surgery program by working closely with multidisciplinary teams to provide expert, minimally invasive surgical care for patients with lung cancer.

FirstHealth welcomed Dana L. Casson, CFRE, as president of The Foundation of FirstHealth in October 2024. Casson was chosen for the position after Kathy Stockham announced her retirement after 35 years of dedicated service. Casson joins FirstHealth with more than 20 years of executive fundraising experience, having held key leadership roles in several leading health care organizations.
FirstHealth has expanded its specialty services in Chatham County. Patients with neurology needs can now be seen by certified physician assistant Amy Gonzales, PA-C, at our FirstHealth clinic in Pittsboro. Gonzales has more than 16 years of health care experience in neurology, psychiatry and pain management.
In the spirit of advancement, there have also been some changes in the Imaging Department at FirstHealth’s Montgomery Memorial Hospital. According to MMH Imaging Director Pam Duncan, nuclear medicine studies have moved to in-house scans, making them more accessible to patients in Montgomery County. Before, FirstHealth patients could only receive this type of imaging intermittently through a mobile service. Nuclear medicine can diagnose and treat conditions like heart disease, lung disease, bone disease, brain disease, blood disorders and cancer. We are excited to help ease the wait time for nuclear medicine throughout the system.
FirstHealth has invested in its Imaging Department by acquiring new equipment to better serve clinicians and patients, including a 256-slice CT scanner and a pioneering MRI machine. The CT scanner features ultramodern AI technologies, upgraded hardware, and faster scanning times, while the new MRI prioritizes patient comfort first with the ability to personalize the scanning experience. Both machines help our clinicians find, diagnose and treat various diseases and disorders, including cancer and heart disease.

EliteCare in Hope Mills has now joined FirstHealth, creating our second primary care practice in Cumberland County, Family Medicine - EliteCare. Travis Ross, PA-C, is the established primary care provider offering family medicine and walk-in appointments.


Migraines are a neurological condition affecting millions of people worldwide, with symptoms that can be debilitating. Amy Gonzales, PA-C, a provider at FirstHealth Neurology, discusses the cause of migraines and what you can do to treat them.
Q: What is a migraine?
A: A migraine is a type of headache that is typically more intense than a regular headache. It often causes severe, throbbing pain, usually on one side of the head. Migraines can also be accompanied by other symptoms such as nausea,
vomiting, sensitivity to light and sound, and visual disturbances (known as an aura). They are caused by abnormal brain activity that a ects the nerves, blood vessels and chemicals in the brain.
Typical migraines can last between 4 and 72 hours.
Q: What causes migraines?
A: While we don’t fully understand the cause of migraines, several factors can trigger or contribute to them. These include genetics, environmental factors, hormonal changes, stress, diet and sleep disturbances.
Q: How can FirstHealth help me manage migraine pain?
A: There are several ways to manage and relieve migraine pain, including over-the-counter pain relievers, prescription medications and antinausea medications. Providers can also
prescribe medications to reduce the frequency and severity of attacks for people who have frequent migraines.
Lifestyle changes can also help. Getting highquality sleep is important to reduce the risk of migraines, and relaxation techniques like meditation, yoga or deep breathing can help lower the chance of a migraine.
If you are su ering from migraines, don’t hesitate to seek medical help and explore treatment options that might work best for you. Migraines are a complex condition, but our providers are committed to nding personalized care plans to help you manage migraines and enjoy life.
FirstHealth Neurology is proud to o er innovative and comprehensive neurology care, with caring and compassion, close to home. We diagnose and treat all common neurological conditions, as well as sleep issues and balance.


Hormone Replacement Therapy (HRT) is a medical treatment commonly used to manage menopause symptoms, though it can also address other conditions related to hormone imbalances.
William Terry, M.D., an OB/GYN at FirstHealth OB/GYN with Southern Pines Women’s Health Center, discusses how HRT can enhance overall quality of life.
Q: What is hormone replacement therapy?
A: Hormone replacement therapy involves supplementing or replacing hormones such as estrogen, progesterone and occasionally testosterone. These hormones often decrease naturally with age, particularly for women experiencing menopause. For women, HRT can alleviate common menopause symptoms,
including hot ashes, night sweats, mood swings, vaginal dryness and sleep disturbances. HRT can also assist individuals undergoing medical treatments like chemotherapy, which can a ect hormone levels.
Q: Who is a candidate for HRT?
A: Anyone experiencing symptoms due to hormonal imbalances may be a candidate for HRT. Our OB/GYN providers collaborate with patients to create personalized care plans, ensuring that any hormone treatments align with an individual’s medical history and needs.
HRT is primarily used to support those going through menopause, those with hormone imbalances or those at a higher risk of osteoporosis.
Q: Are there risks to consider?
A: While HRT can provide signi cant bene ts, it also carries risks, including an increased likelihood of blood clots, stroke and certain types of cancer. Individuals with a history of breast, uterine or ovarian cancer may not be suitable candidates for hormone replacement therapy.
If you are considering HRT, it’s important to consult with your primary care provider or OB/GYN to nd out what is best for you.

Aubrey Kinsman, PA-C, with the FirstHealth Heart Failure Clinic, talks about the relationship between sodium, the heart and the brain.
Q: What is sodium and how does it a ect the body?
A: Sodium is a mineral and electrolyte that helps regulate uid balance, nerve function and muscle contraction. The body can have too much or too little sodium.
Q: How does sodium a ect heart disease and heart failure?
A: Sodium has a signi cant impact on the heart. Increased amounts of sodium can increase blood pressure because it causes the body to hold on to more uid, which in turn will increase the volume of blood in the vessels. When blood pressure is increased, it will increase the workload on the heart, which will increase the risk of heart disease such as coronary artery disease and heart failure.
Q: How is sodium related to stroke?
A: Increased sodium intake has been linked to increased risk of stroke due to its e ect on blood pressure. Chronically elevated blood pressure is the leading risk factor for both ischemic and hemorrhagic stroke.
Q: How important is it to monitor your sodium intake?
A: It is important to monitor your sodium intake to maintain overall health. Consuming too much sodium can increase the risk of high blood pressure signi cantly, which then raises the likelihood of heart disease and stroke. It is recommended to limit sodium intake to 15002000 mg of sodium daily. If diet modi cation alone is not enough, there are medications that can also help.
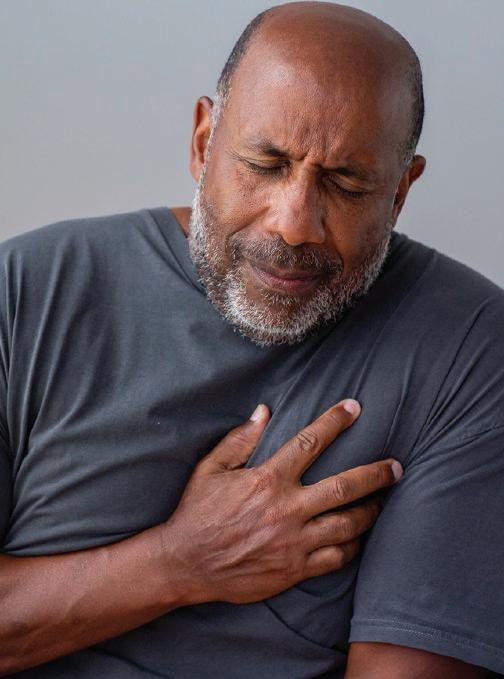

Medical emergencies are always scary, and that’s especially true when someone is alone and away from home. Anxiety and fear can set in quickly, and questions are endless –what is happening with my body? Can I safely drive myself to get medical care? Is there a hospital nearby?
All these questions and many more were running through Doug Peterson’s mind in October 2024 after he started experiencing chest pains following a day of work in Lee County. Peterson was far from his home.
“I work for a company that installs security equipment, and on Monday, Oct. 28, I left my home in Dover, Delaware, to install a security camera at a job site in Sanford. I left at 4 a.m., drove straight to the site and finished up my work around 3:30 that afternoon. When I started packing up, I noticed a feeling that reminded me of bad indigestion.”

threw up my lunch and the medication I took, and sweat was rolling off my forehead,” Peterson recalled. “I attempted to lie down, thinking I might be able to sleep it off, but a few minutes later, I called my wife, and she told me to get to a hospital because I might be having a heart attack.”

Peterson’s wife, Melanie, who spent more than two decades working as a nurse, was right. Peterson was in the midst of a heart attack, and his harrowing journey was just beginning.
“I asked the hotel staff to call 911, and by the time the FirstHealth EMS crew got to the hotel I was in a bad way,” Peterson said.
At this point, Peterson met Vince Duke, a FirstHealth paramedic who would be more important than he could have imagined.
On his way to the hotel he picked for the night, Peterson stopped at a pharmacy to buy antacid medication, hoping to get some relief.
“By the time I got to the hotel, I was feeling nauseous. I checked in, and once in the room I only got worse. I
Peterson said he was immediately struck by Duke and the crew’s calm demeanor and how they quickly sprang into action.
“His expertise was evident, and after he took an EKG, he told me I was having a heart attack. When we discussed where I should go, Duke mentioned FirstHealth’s Reid Heart
Center, which has a catheterization lab and heart specialists who could help me and deliver top-notch care. I told him I was at his mercy and to do what he thought was best. Within moments, we were rolling.”
During the 35-minute drive from Sanford to Pinehurst, Duke and his team continued to care for Peterson both physically and emotionally. He was given pain medications and reassured that they would be at Reid Heart Center soon.
“I heard them call the hospital and tell them they were coming and that I would need to go straight to the Cath Lab,” Peterson said. “Even though I was still in pain, I was extremely worried about my wife not knowing that I was possibly dying. You could only imagine her anxiety being back in Delaware with no additional information. The last time she had heard from me was when she told me to get to a hospital.”
Again, Duke was ready to help, calling Peterson’s wife and explaining both what was going on and where the ambulance was headed.
“He calmed her down, and she felt that I was receiving the best care I could get,” Peterson said. “The last parts of the ride are foggy to me, and there were times I felt like I was slipping away. I remember at least once Duke calling to me and saying, ‘Stay with me, Doug.’”
Duke said taking care of a patient during an emergency often includes care of their family, too.
Continued on page 8
“It happens on a lot of calls. We always try to think about the full patient picture, which involves the family,” Duke said. “Another bonus is that when we can engage a patient and get information to their family, it can take their mind off what is happening in the moment and put them in a position where they can provide care to someone themselves.”
Upon arrival at Moore Regional Hospital’s emergency department, Duke continued to advocate, making sure Peterson was taken to the Cath Lab as quickly as possible.
“I was medicated and possibly dreaming but I know Vince kept pushing to get me into Reid Heart Center, and he stayed with me in the room until I was taken back,” Peterson said.
occlusion (clot), and we were able to successfully open it with a single stent,” Kim said. “After Doug’s trip to Reid Heart Center from Sanford, we were able to open his artery about half an hour after he got here.”
When Peterson woke up following the procedure and met Dr. Kim, another phone call to his wife helped ease both of their minds again.

M.D.
“Dr. Kim agreed when I asked to call Melanie as he was explaining everything, and he was so patient in explaining everything to her. He must have spent 15 minutes talking through everything, and I’d never seen that happen before,” Peterson said.
“That was an incredible few minutes, and it was really meaningful for Melanie to have Dr. Kim take the time to do that.”
From there, Reid Heart Center’s team of heart care specialists, including interventional cardiologist Sun Moon Kim, M.D., took over, discovering that a 100% blockage in Peterson’s right coronary artery had caused his heart attack.
“Doug had a 100% thrombotic
Kim said it’s common for members of the heart team to help make sure family members know what is going on with a patient’s care from a distance.
“In this case I was able to speak with Doug’s wife, update her on his condition, the success of the procedure and what she could expect
moving forward,” Kim said. “Although difficult at times, we do our best to communicate with family members when we have permission from patients.”
Peterson spent an additional 36 hours in Reid Heart Center before being discharged on Wednesday, and his care team helped him get 30 days’ worth of medicine he needed as he and his wife worked to identify a follow-up appointment with a cardiologist in Delaware. Peterson says his recovery continues to go well, and his experience has reminded him that “real-life heroes” still exist.
“What sort of care would you expect in such a scary moment? You would want qualified people who are on your side and advocating for you the entire way. That’s just what I got,” Peterson said. “I never saw Vince after I was rolled into the Cath Lab, but without him and his crew, I would not be here. I owe my life to him, and Melanie and I are so grateful for the care I received.”
Duke said EMS crews approach each call with the mindset of delivering high-quality care.
“Our teams take their patient contact very personally. We advocate for our patient and do our best to provide the type of care we would want for our own family,” Duke said.





On-demand video visit with a FirstHealth provider for urgent but non-emergency care like rash, flu, pink eye and more.
• For all ages
• Available 6 a.m. to midnight
• No appointment needed
• $0-45 depending on your health plan
• For new and established patients
When wait times at Convenient Care are longer than expected, we now offer patients the option to use an in-clinic video visit with one of our licensed FirstHealth providers. You may be offered this option if you need to be seen for:
• Allergies
• Cold
• Flu
• Cough
• UTI
• Insect bites
• Pink eye
• Rash

• Sinus
• Sore throat
• Yeast infections
• COVID


MyChart Online Scheduling for Established Primary Care Patients
Established patients can now see your preferred FirstHealth provider through an appointment that is scheduled through MyChart.
• For all ages
• Available with participating providers by appointment
• For established FirstHealth patients
Access to a Virtual Primary Care Provider FirstConnection
For those who do not have a primary care provider and have medical needs that cannot be met when visiting the emergency room or convenient care. We connect you with a provider while virtually offering the following:
• Order labs, tests & imaging
• Make referrals to specialists
• New prescriptions, medication refills or dose changes
• Treat acute & chronic illnesses
FirstHealth’s core purpose is To Care for People. That purpose drives all the ways we care for our communities, and it also drives innovation across our system that makes care more accessible, especially to those in need.
In recent years, FirstHealth’s care delivery has gone virtual. The goal? We want to give patients quick and seamless access to our providers and care teams, allowing them to avoid time-consuming clinic visits or unnecessary trips to the emergency room.
With FirstHealth MyChart you can Save Your Spot at the nearest Convenient Care, schedule an appointment, start a virtual visit with On the Go , pay bills, view test results and more. Need help? Contact us at (910) 715-2434 or MyChartSupport@FirstHealth.org
Ready to learn more about virtual care options at FirstHealth? Visit our website to see how we can take care of you.

FirstHealth of the Carolinas is Born
Moore Regional Hospital in Pinehurst and Montgomery Memorial Hospital in Troy merge to create FirstHealth of the Carolinas.



FirstHealth EMS
FirstHealth begins offering Emergency Medical Services in Montgomery County. FirstHealth EMS now serves Montgomery, Lee, Chatham and Richmond counties.


Expanding in Richmond County
FirstHealth acquires Richmond Memorial Hospital, later renamed FirstHealth Moore Regional Hospital-Richmond and builds a new $4.8 million ED in 2003.
The community raises $11 million through The Foundation of FirstHealth’s In Love and Service campaign to fund at MRH:
• Nursing tower
• Inpatient cancer center
• Emergency department
• Parking deck


Reid Heart Center Opens
Consolidating specialty services under one roof, offering innovative treatments like TAVR and MitraClip.
The newly built house welcomes its first guests, offering a comforting, caring and affordable place to stay for FirstHealth outof-town patients, families and caregivers.

Since its inception in 1995, FirstHealth of the Carolinas has grown to a regional health care system and trusted provider of world-class care across the mid-Carolinas. Here’s a look back on some of the pivotal milestones over the last three decades:
















The 30-plus acre Hospice Campus opens with a Hospice House, Chapel and Grief Resource and Counseling Center.




A new medical office building and fitness center opens in Sanford.
FirstHealth Moore Regional Hospital-Hoke opens, bringing inpatient care and a 24/7 emergency department to Raeford.

FirstHealth Cancer Center
The four-story, 120,000-square-foot center brings a full spectrum of cancer care to one location, enhancing accessibility for patients across the region.

FirstHealth remains committed to its core purpose To Care for People, with a focus on employee engagement, patient safety and delivering the highest quality medical excellence.




See the full 30-year Timeline. Visit FirstHealth.org/30years for a complete look at FirstHealth’s history and milestones.








It’s no secret that a cancer treatment journey is challenging.
From the diagnosis onward, patients often experience several unique but related challenges – it could be side e ects of chemotherapy or radiation, the stress associated with such an abrupt change in lifestyle or the emotional challenge of dealing with a scary situation. The inherent lack of control during the journey can be overwhelming at times.
That’s what makes comprehensive care so critical, and it’s a feature of the approach at FirstHealth’s Cancer Center in Pinehurst.


In 2024, the center made the next step in its ability to deliver care by introducing an Integrative Oncology & Survivorship program.
Put simply, the groundbreaking program o ers evidence-informed therapies that complement conventional cancer treatments. Chasse BaileyDorton, M.D., the program’s director, collaborates with each patient’s oncologist, who directs and oversees the primary cancer treatment plan.
“With integrative oncology, we are trying to optimize health and quality of life. We are thinking about the link between mind and body, so we consider therapies that ease stress as critical to quality care,” she said.

“Maybe that looks like art therapy, yoga, music therapy or changes to a person’s diet. We also work with patients to manage cancer treatment side e ects like hot flashes, neuropathy and anxiety. Very often these complementary pieces don’t involve an additional prescription medication.”
The program also provides some of the following:
• Healthy lifestyle recommendations for reducing cancer recurrence and managing other health conditions
• Guidance on safe use of supplements, herbs and vitamins
• Nutritional counseling in collaboration with the Cancer Center’s dietitian team
• Physical activity recommendations with support from the Cancer Wellness team
• Referrals to additional integrative therapies


FirstHealth’s program is available to high-risk individuals for preventative consultation, patients undergoing active cancer treatments and survivors in surveillance phase who want long-term health guidance.
“In the past, survivorship has always been described to start at the end of treatment. We need to start it at the beginning and follow them all the way through,”



Bailey-Dorton said. “But cancer is also changing. We now have some patients who are never going to be o treatment, and they don’t really fit into that prior survivorship model.”
Bailey-Dorton emphasized the importance of integrative oncology in modern cancer care. Research in the field supports this approach, indicating that integrative methods combined with traditional treatments can significantly enhance patient experiences and outcomes.


“Integrative oncology needs to become standard of care for our patients. Some studies have shown improved outcomes and certainly improved patient satisfaction,” she said. “Many patients use alternative treatments, but few share this information with their providers. Our program gives patients the opportunity to discuss and explore these therapies safely.”

FirstHealth’s program follows standard care guidelines developed by the Society of Intergrative Oncology and the American Society of Clinical Oncologists to provide pathways that bring integrative therapies in line with standard care approaches.
“Developing this program in a community hospital is groundbreaking and demonstrates the commitment to excellent patient care here in our community,”

Bailey-Dorton said.



Bailey-Dorton’s journey into integrative oncology was influenced by her own experience as a patient.
“I was diagnosed with breast cancer at age 39 and went through surgery, chemotherapy, radiation therapy and endocrine therapy,” she said.

Prior to her diagnosis, Bailey-Dorton provided full-spectrum family medicine care to patients, including obstetrics care and work in the hospital setting in her South Carolina hometown.
“I was drawn to this field first to help myself and, ultimately, to better help my patients,” she said.



Today, Bailey-Dorton said she’s glad to see integrative oncology becoming more mainstream. She knows it can be a gamechanger for patients and their caregivers.



“The experience shifted my focus to the care of cancer survivors.”
Dr. Bailey-Dorton earned her medical degree from East Carolina University School of Medicine, completed her family medicine residency at ECU Health Medical Center, and pursued advanced training in integrative medicine through a fellowship at the Andrew Weil Center for Integrative Medicine in Tucson, Arizona.
“You can see the patient who, when they’re first diagnosed, it’s like they are thrown into the middle of a hurricane. Things happen fast and it can be scary. Patients feel like they have no control,” she said.
“My goal is to help empower them to partner with us and their oncologist in their care, to give them things they can do to help them decrease side e ects. It gives them agency in the process, and you can definitely see the impact it has on patients both physically and emotionally.”

M.D.

For more information about the Integrative Oncology Program, please call (910) 715-0998 or visit FirstHealth. org/IntegrativeOncology.





It’s no secret that in today’s world, sleep often takes a backseat to work, social activities and the constant pull of our screens – both big and small.
But sleep isn’t a luxury. It’s a necessity, and its importance is hard to overstate. It is crucial for our physical and mental well-being and making it a true priority in your routine can help you live a healthier, happier life.
Family Nurse Practitioner Autumn Grimm, who focuses on sleep medicine at FirstHealth Neurology, said people should think more actively about cultivating good sleep health habits.
“Sometimes it may be easy to think of sleep as a passive thing, but we have agency and can make choices to prioritize our own sleep habits and, by extension, our well-

being,” she said.
When you sleep, your body isn’t just resting; it’s repairing, rejuvenating and recharging. Good sleep can also help promote proper cell function and balance a person’s stress responses.
Sleep is one of the most important factors in maintaining physical health. Research has shown that inadequate sleep is associated with a higher risk of developing chronic conditions like heart disease, high blood pressure, diabetes and obesity. One reason for this is that sleep helps regulate critical bodily functions like blood
sugar levels and inflammation. When you’re sleep-deprived, your body’s ability to balance these functions is compromised, increasing the likelihood of disease.

“Without enough restorative sleep, your body won’t function at its best,” Grimm said.
“This may look like fatigue, irritability or a general sense of feeling off, but the effects of poor sleep can go much deeper than that.” Poor sleep habits can hinder your ability to concentrate, problemsolve or make sound decisions.
Grimm says one of the first steps for improving sleep is to understand the different stages of sleep.
Sleep stages include light sleep, deep sleep and REM (Rapid Eye Movement) sleep. Each stage serves a different purpose, and it’s the deep sleep and REM stages that are particularly important for restoration and cognitive function. If your sleep is constantly interrupted or if you don’t get enough of these crucial stages, you won’t experience the full benefits of sleep.
“Chronic sleep deprivation has even been linked to an increased risk of mood disorders,” Grimm said. “The relationship between sleep and mental health can become cyclical. A lack of quality sleep might exacerbate stress and negative emotions, while poor mental health can disrupt sleep patterns, creating a vicious cycle.”

Looking to improve your sleep habits? Grimm says the following tips are a great starting point:
Stick to a Routine: Go to bed and wake up at the same time every day, even on weekends. This helps regulate your body’s internal clock.

Create a Sleep-Friendly Environment: Keep your bedroom dark, cool and quiet. Minimize distractions like phones and electronics, as the blue light emitted by screens can interfere with your body’s production of melatonin, a hormone that promotes sleep.
Exercise Regularly:
Physical activity can promote deeper sleep, but try not to exercise too close to bedtime, as it may leave you feeling too energized to fall asleep.
Manage Stress:
Incorporate relaxation techniques like deep breathing, meditation or journaling to calm your mind before bed.
A calm mind is essential for restful sleep.
Limit Ca eine and Alcohol:
Both caffeine and alcohol can interfere with your ability to fall asleep and stay in deep sleep.
In a world where productivity and multitasking are highly valued, it’s easy to neglect sleep in favor of more “active” pursuits. However, prioritizing quality sleep is one of the best things you can do for your physical and mental health.

Your gut is more than just where food is digested, it’s a powerhouse that a ects nearly every aspect of your health. From digestion to immunity, mood and even metabolism, maintaining a healthy gut is essential for overall well-being.
So, what is gut health? A healthy gut means a balanced microbiome, a community of trillions of microorganisms that support digestion, produce essential
nutrients and protect against harmful bacteria.
Wayne Lucas, M.D.
Lifestyle and eating habits are the most important factors in maintaining a healthy microbiome, explained Wayne Lucas, M.D., gastroenterologist with Pinehurst Medical Clinic.
“Unfortunately, many of the eating habits popularized in the 1950s have harmed gut health. The highly processed, high-carb
American diet, fueled by the “food pyramid” of the 1970s, has been a significant contributor to the obesity and Type 2 diabetes epidemic,” Lucas said.
Experts now agree that a Mediterranean-style diet, rich in fresh, whole foods, is one of the best ways to promote a healthy gut microbiome. This approach to eating o ers numerous health benefits, including improved heart and brain health, reduced inflammation and a lower risk of obesity and chronic diseases.
Signs of a Healthy Gut
How can you tell if your gut is thriving? Signs of a healthy gut include regular bowel movements, minimal digestive discomfort, stable weight and even healthier skin and energy levels. Conversely, symptoms of an unhealthy gut include frequent bloating, gas, diarrhea, constipation and unexplained weight changes. Poor gut health can also manifest as fatigue, skin issues like eczema and mood disorders such as anxiety and depression.
While digestion is its most well-known function, your gut also plays critical roles in the endocrine, immune and nervous systems.
• Endocrine System:

Your gut microbiome is home to trillions of microorganisms, including bacteria, viruses and fungi. This ecosystem plays a vital role in digestion, breaking down complex carbohydrates and fibers while producing essential nutrients like vitamin K and B12.

The gut is the body’s largest endocrine organ, producing more than 30 hormones that regulate metabolism. For example, L-cells in the small intestine secrete glucagon-like peptide 1 (GLP-1), a hormone that helps balance blood sugar levels and has gained attention for its role in diabetes and obesity treatments.
• Immune System:
More than 70% of your immune cells reside in the gut, where they protect against infections and help regulate inflammation.
• Nervous System:
Known as the second brain, the gut houses the enteric nervous system, which communicates with the brain through the gut-brain axis. This complex network influences mood, stress levels and even serotonin production—the “feel good” neurotransmitter.
fatigue, weight gain and mood disorder.
The best way to nourish your microbiome is through your diet. There are many foods that are rich in healthy gut microorganisms including:
“The microbiome is a living system, and we should treat our bacterial friends the same way we would treat the family pet,” Lucas advised. “Feed your microbiome daily with healthy foods and plenty of water. Don’t feed your microbiome harmful foods like highly refined carbohydrates and sugary food, artificial sweeteners, fried foods, trans-fat rich foods, excess alcohol and excess red or processed meats.”
Lucas added that studies have shown that eating three di erent servings of fruit a day can improve your microbiome health.
“Consider a variety of fruits like berries, apples, grapes, papaya and citrus fruits to provide a rich mix of essential nutrients that support gut health and overall health,” he said.
A healthy microbiome helps regulate inflammation, supports immunity, and even protects against harmful bacteria like Clostridioides di cile (C. di ), a dangerous infection often triggered by antibiotic use.
• Vegetables like asparagus, broccoli and leafy greens
• Fruits such as berries, apples, grapes, papaya and citrus fruits
• Whole grains, nuts and seeds
• Yogurt with live cultures
• Fermented foods like kombucha, kimchi, sauerkraut and kefir
“A healthy gut is the foundation of overall health,” concluded Lucas. “By making mindful choices about what you eat and how you care for your microbiome, you can improve not only your digestion but also your immune system, energy levels and mental wellbeing.”

However, an imbalance in the microbiome, known as dysbiosis, can damage the gut lining or barrier, allowing toxins to be absorbed into the bloodstream. Dysbiosis can lead to symptoms like bloating and irregular bowel habits and may also increase the risk of chronic inflammation,
Wayne Lucas, M.D., is a board certified gastroenterologist with Pinehurst Medical Clinic Gastroenterology and Endoscopy, a trusted leader in digestive health o ering advanced care in clinic locations in Pinehurst, Sanford and Pittsboro. The team of specialists diagnose and treat a full range of GI conditions, from shortterm concerns to lifelong diseases. Pinehurst Medical Clinic’s Endoscopy Centers are nationally recognized for quality and accredited by the AAHC, ensuring the highest standard of care for patients.










Cardiovascular Thoracic Surgery
Blaine Buchanan, PA-C
FirstHealth Cardiovascular Thoracic Surgery




ANESTHESIA – FIRSTHEALTH
ANESTHESIA
Karis Comiskey, CRNA
Hanna Greene, CRNA
ANESTHESIA – PROVIDENCE
ANESTHESIA ASSOCIATES
Aryn Rooney, D.O.
FIRSTHEALTH CONVENIENT CARE
Jenny Baucom, PA-C
Dinah Oxendine, PA-C
Jamie Speight, PA-C
FIRSTHEALTH INPATIENT DERMATOLOGY
Natalie Davies, M.D.

Family Medicine
Tracy Bullard,




EMERGENCY MEDICINE –SANDHILLS EMERGENCY
PHYSICIANS
Jeffrey Alex Gross, M.D.
John A. Cook, M.D.
Jaclyn Bell, PA-C
Ryan McAvoy, PA-C
FIRSTHEALTH OB HOSPITALISTS
Tammy G. Lucas, AGACNP
PULMONOLOGY – PINEHURST MEDICAL CLINIC
Danielle Shellman, AGACNP-BC
RHEUMATOLOGY – PINEHURST MEDICAL CLINIC
Konrad Dziamski, M.D.
INTERNAL MEDICINE
Phillipp C. Wirth, M.D.
ORAL & MAXILLOFACIAL SURGERY – ASPEN DENTAL
Joseph D. Park, MDDS
NEPHROLOGY – PINEHURST NEPHROLOGY ASSOCIATES
Christina Revels, PA-C

On Oct. 16, 2024, my wife Mary Lou and I traveled to FirstHealth Montgomery Memorial Hospital in Troy for what we thought would be a routine CT scan. We arrived at 9 a.m. and expected to be back home in Southern Pines by noon. It did not work out that way for a number of reasons. She had some difficulties and ended up in the emergency department where she spent the next several hours with wires attached and nurses and a doctor checking on her periodically. We are so fortunate that we were so well taken care of, and we want to thank those who made us as comfortable as possible in the hospital setting. Our thanks go out to Pam, Christine and Val in the imaging areas and in the ED we offer our sincere thanks to Ronda, Zona, Amy, Nancy, Abagaile, Chris and Dr. Lundberg. We are so grateful for the care and compassion that each of these professional staff members provided for us. If we did not include anyone in this letter, please pass on our thanks to them as well. We arrived home around 4:30 p.m.
Helm and Mary Lou Wilden Southern Pines, N.C.


Your Feedback is Valuable!
Would you consider sharing your experience online? It’s one of the many ways we love to recognize our employees when they deliver on our core purposeTo Care for People.





















The distinguished three-star rating awarded from The Society of Thoracic Surgeons denotes the highest category of quality, placing FirstHealth among the elite for heart bypass surgery in the United States.






