




As we embrace the fall season, we are reminded of the importance of gratitude and the spirit of Thanksgiving.
our lives, and I am profoundly grateful for the dedication, skill and compassion of our FirstHealth team. Every day, they demonstrate why FirstHealth is an award-winning health system that has been named to the 100 Top Hospitals eight times since the inception of the program.
Just last month, FirstHealth was recognized by Healthgrades as one of America’s 100 Best Hospitals for our dedication to clinical excellence and distinguishes Moore Regional Hospital as one of the nation’s leading hospitals for orthopaedic surgery.
I am immensely proud to acknowledge the remarkable unwavering commitment to excellence in patient care has earned us this distinction. Additionally, we could not have achieved this recognition without our physician partners and the outstanding orthopaedic surgeons at Pinehurst Surgical Clinic, who share in our pursuit of excellence in health care. Together, we have achieved remarkable success in delivering the highest standards of care to our patients.
I am also pleased to share other recent accolades from Healthgrades, including:
•2025 Orthopaedic Surgery Excellence Award
•Top 10% in the Nation for Overall Orthopaedic Services in 2025
•Five-Star Recipient for Total Knee Replacement in 2025
•Five-Star Recipient for Pacemaker Procedures in 2025

In addition to these recognitions, this edition of the FirstHealth magazine also highlights our recent awards for stroke care, home care, hospice, cardiology and cardiothoracic surgery.
On the topic of cardiothoracic surgery, you will not want to miss the heartwarming story of Peter Ellman, M.D., FirstHealth cardiothoracic surgeon, and his journey through a life-changing kidney transplant. on new programs and facilities at FirstHealth that are further enhancing the exceptional care we provide.
We remain committed to providing the highest quality of care at FirstHealth and improving the health and well-being of those we serve. Thank you for your continued trust and support in our mission to care for you and your loved ones.
With gratitude,
Mickey W. Foster, MHA
FirstHealth of the Carolinas
Cindy
Goodman, Ed.D., Chair
David Wood, Vice Chair
Arthur
Medeiros, Corporate Secretary
Ray Allen, Treasurer
Gary
VonCannon, Immediate Past Chair
Mickey Foster, MHA
Matthew Harmody, M.D.
Jason Jerry, M.D.
Ben Jones
Susan Keller
Jefferson Kilpatrick, M.D.
Wayne Lucas, M.D.
Brian McMurray
James Obi
Tom Pashley
Sushma Patel, M.D.
Elizabeth Webster
Chief Executive Officer
FirstHealth of the Carolinas .
President, FirstHealth Physician Group
Chief Information Officer
FirstHealth of the Carolinas
President, Eastern Region
Chief Medical Officer
FirstHealth of the Carolinas
President, FirstHealth Montgomery Memorial Hospital and Western Region
Chief Financial Officer
FirstHealth of the Carolinas
Chief Operating Officer
FirstHealth of the Carolinas
Vice President, Finance
FirstHealth of the Carolinas
Chief Strategy and Innovation Officer
FirstHealth of the Carolinas
President, Southern Region
Chief Quality Officer
FirstHealth of the Carolinas
Vice President, Operations
.Mickey W. Foster, MHA
Daniel R. Barnes, D.O.
Chris Beasley, MBA
Susan K. Beaty, R.N.
Jenifir Bruno, M.D.
Rebecca Carter, R.N.
Jeffrey A. Casey
Jonathan Davis, MPH, FACHE
Chris Fraley, CPA
Amy Graham, MHA
Christy Land, MSN, R.N.
Cindy McNeill-McDonald, R.N.
FirstHealth Moore Regional Hospital Matthew Prestwood, MHA
President, The Foundation of FirstHealth
Chief People Officer
FirstHealth of the Carolinas
Kathleen Stockham
Berni Szczepanski, MBA
FirstHealth of the Carolinas, a not-for-profit health system, is headquartered in Pinehurst, North Carolina, and comprises Moore Regional Hospital, Montgomery Memorial Hospital, Moore Regional Hospital – Richmond, Moore Regional Hospital – Hoke, The Foundation of FirstHealth and the FirstHealth Physician Group. Comments on the FirstHealth magazine or changes of address should be directed to (800) 213-3284 or Marketing@FirstHealth.org. © Copyright 2024 FirstHealth of the Carolinas, Inc. No part of this publication may be reproduced or transmitted in any form or by any means without written permission from FirstHealth of the Carolinas, Inc. Articles in this publication are written by professional journalists who strive to present reliable, up-todate health information. However, personal decisions regarding health, finance, exercise and other matters should be made
What’s Happening at FirstHealth
ASK THE EXPERTS: Sleep 101, A Silent Killer, New at FirstHealth: Certified Hand Therapy
New Ultrasound Technology Promotes Faster Relief for Hospice Patients
The Reimagining of Montgomery Memorial Hospital
Welcome to a Higher Level of Surgical Care
The Remarkable Story Behind a Local Kidney Transplant
Weight-Loss Surgery: The Transformation Is More than Just Physical
Functional Medicine Reveals Root Causes of Illness and Forges Path to Wellness
Tackling Mental Health Concerns in Our Community
FirstHealth in the Community 20 Welcome New Providers on FirstHealth's Medical Staff
22 KUDOS: Dear Foundation of FirstHealth; Dear Dr. Bruno, Chief Medical Officer





by Krames, a WebMD Ignite solution
FirstHealth hospitals have again earned stroke care awards from the American Heart Association for our demonstrated commitment to ensuring stroke patients receive the most appropriate treatment according to nationally recognized, research-based guidelines. This year, FirstHealth hospitals achieved the following awards for stroke care:
Moore Regional Hospital
Get With The Guidelines® – Stroke Gold Plus With Target: Stroke Honor Roll Elite and Target Type 2 Diabetes Honor Roll
Get With The Guidelines® – Rural Stroke Silver
Get With The Guidelines® – Rural Stroke Bronze
Moore Regional Hospital – Richmond
Get With The Guidelines® – Stroke Silver Plus With Target: Type 2 Diabetes Honor Roll
Get With The Guidelines® – Rural Stroke Bronze
Moore Regional Hospital – Hoke
Get With The Guidelines® – Stroke Gold Plus With Target: Stroke Honor Roll Elite and Target Type 2 Diabetes Honor Roll
Montgomery Memorial Hospital
Get With The Guidelines® – Rural Stroke Bronze Type 2 Diabetes Honor Roll


FirstHealth Home Care has been recognized by Strategic Healthcare Programs (SHP) as a “Superior Performer” for achieving an overall patient satisfaction score that ranked in the top 20% of all eligible SHP clients for the 2023 calendar year. The 2023 award recipients were determined by reviewing and ranking the overall satisfaction score for more than 3,200 home health providers.




The dedicated FirstHealth Hospice team has also been acknowledged by Strategic Healthcare Programs as a “Superior Performer” for achieving an overall score that ranked in the top 20% in the SHP national Hospice benchmark and scoring above the SHP national average for each Hospice quality measure as rated from the caregiver’s point of view.

FirstHealth of the Carolinas has earned a distinguished three-star rating from The Society of Thoracic Surgeons (STS) for its patient care and outcomes in isolated coronary artery bypass grafting (CABG) procedures. The three-star rating, which represents the highest category of quality, places FirstHealth’s Cardiovascular & Thoracic Surgery program among the elite for heart bypass surgery in the United States and Canada. The STS star rating system is one of the most sophisticated and highly regarded overall measures of quality in health care, rating the benchmarked outcomes of cardiothoracic surgery programs across the U.S. and Canada. The star rating is calculated using a combination of quality measures for specific procedures performed by an STS Adult Cardiac Surgery Database participant.
John M. Ray Jr., M.D., FAAFP, of Pinnacle Primary Care in Fayetteville, joined FirstHealth of the Carolinas and FirstHealth Physician Group on July 1. Dr. Ray, who is board certified, has served patients in Fayetteville for two decades and said he is thrilled to join FirstHealth.


On September 24, staff from the Moore County Chamber of Commerce and FirstHealth of the Carolinas gathered with community members to open FirstHealth's new convenient care, family medicine practice and 24/7 fitness facility in Whispering Pines, located at 225 Capital Drive, Carthage, in the former Ace Hardware building.
Medical volunteers from throughout FirstHealth played a crucial role in the U.S. Open Championship in Pinehurst, June 8 to 16. Their commitment and expertise ensured the well-being of the thousands of attendees, showcasing the high-quality care our community is fortunate to have. Throughout the championship, these volunteers provided care to approximately 2,500 individuals in need of medical attention within the three medical tents located throughout the course. Matthew Harmody, M.D., and Katherine Newell, M.D., provided outstanding leadership and coordination as co-medical directors for the event.


The Reid Heart Center care team successfully completed its 300th WATCHMAN procedure, marking a significant milestone in efforts to provide cutting-edge care and innovative treatment options for our patients. This milestone is doubly special as
it also signifies the 200th WATCHMAN procedure performed by electrophysiologist Mark Landers, M.D. The WATCHMAN procedure, a minimally invasive alternative to blood-thinning medications for stroke prevention, involves implanting a small, flexible device into the heart. This device, about the size of a quarter, never needs to be replaced and has proven to be highly effective, with a 98.8% procedural success rate.
With more than 150,000 patients worldwide benefiting from the WATCHMAN implant, the program at Reid Heart Center stands out as the fastest growing and largest implanting program in the state.
If you often feel tired or cranky or have trouble concentrating, it could be because you aren’t getting enough good, sound sleep.
Some people function well on as little as six hours of sleep at night, while others require nine or 10 hours. But most people need about eight hours of sleep to stay healthy and be at their best, according to the National Sleep Foundation.
Autumn Grimm, a family nurse practitioner at Sandhills Neurologists, answers questions about frequent sleep issues and what you can do about them.
Q. How many people in the United States deal with sleep issues?
A. Unfortunately, sleep disorders are common among Americans. As many as 50 to 70 million adults deal with chronic sleep issues.
The American Academy of Sleep Medicine recommends adults get seven or more hours of sleep per night, but nearly 40% of Americans sleep six hours or fewer. Putting it bluntly, we are not getting enough sleep.
Q. What are the most common reasons people don’t get good sleep?
A. Sleep problems are caused by a variety of factors, including certain medical conditions, chronic pain and even environmental factors such as your sleep environment. Your room could be too light or hot, and your sleep partner may be keeping you up, as well. Substances like caffeine, alcohol
and nicotine can also have negative effects on our sleep.
Q. How does FirstHealth help with these issues?
A. We offer six sleep testing locations, and our office is growing fast. We offer both in-lab and in-home sleep testing, and our staff is committed to helping people learn about their sleep issues and find solutions. We are passionate about helping our communities sleep better.
To learn more about FirstHealth’s sleep testing or to schedule an appointment, visit FirstHealth.org/Sleep.


Hypertension, more commonly known as high blood pressure, is as simple as it sounds – it’s when your blood pressure is higher than normal. Claire Repine, D.O., a provider who cares for patients at FirstHealth Family Medicine –Chatham, answers some key questions about high blood pressure and what you can do to improve your health.
Q. When is blood pressure considered high?
A. There are two numbers we typically look at when we measure a patient’s blood pressure – the top number is the systolic blood pressure, which measures the pressure of the blood against the blood vessels when the heart beats. The bottom number is the diastolic blood pressure, or the pressure of the blood against the vessels when the heart relaxes between heart beats. We typically like blood pressure to be 120/80 or lower.
Q. Does high blood pressure cause symptoms?
A. Actually, no! The disease typically doesn’t cause symptoms until its later stages, which is why it’s sometimes called “the silent killer.” When symptoms do occur, they often signal developing organ damage. That’s why earlier detection and intervention are important.

Q. How should I address this with my provider?
A. The most important thing you can do is see your health care provider regularly so your blood pressure can be monitored. As primary care providers, we are here to work with our patients, set goals, give guidance and help remove any barriers preventing you from being your healthiest self.
To learn more about scheduling an appointment with a primary care provider, visit FirstHealth .org/PrimaryCare

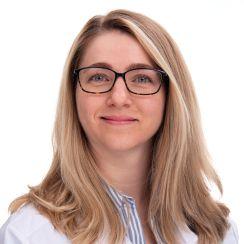
Danielle Benoit, OTR/L, CHT, MEd
It’s easy to take our hands for granted until they hurt, tingle or weaken, or we injure or lose the use of one of them. Fortunately, with more than 25 years in occupational therapy, Danielle Benoit, OTR/L, CHT, MEd, has recently completed an intensive certification in treating hands. She’s ready to help anyone who has had a disruption to the health of their hands, wrists, arms or shoulders.
Q. What does a certified hand therapist do?
A. Certified hand therapists offer exercises and compensatory strategies for conditions that affect the nerves, muscles, ligaments, tendons or bones of the hands, wrists, arms or shoulders. We help people get back to doing the things
that are important to them. We also create splints and dress wounds so that injured extremities have time to heal.
Q. Who needs certified hand therapy?
A. I see everything from repetitive motion injuries to traumatic fractures and digital amputations. Tendonitis or fractures in the wrists or elbows are common, as are compressed nerves and arthritis. If you’re having any kind of pain, tingling, numbness or trouble using your upper extremities that doesn’t go away, certified hand therapy may offer relief.
Q. Why is certified hand therapy so important?
A. Our hands and arms do so much to serve ourselves and others. If function or range of motion is compromised, it can really affect quality of life, even causing feelings of depression or isolation. We may be able to provide something very simple in a couple of sessions that can help someone get back to being their best selves. It’s worth checking out!
To learn more about certified hand therapy at FirstHealth, call (910) 715-1600 or visit FirstHealth.org.

To find a provider closest to you, call (800) 213-3284 or visit FirstHealth.org/Directory.
Clinicians at FirstHealth’s Hospice House can now alleviate patients’ pain, nausea and other symptoms much faster than before, thanks to a stateof-the-art ultrasound device made possible by a group of generous donors.
care to hospice patients, clinicians sometimes use midline intravenous (IV) catheters. These reach larger blood vessels deep in the body, resulting in quicker drug absorption and faster relief. Plus, a midline catheter can stay in the body for up to 30 days, which means fewer painful “sticks” over the course of care.
In the past, FirstHealth’s Hospice House had a handheld ultrasound device for visualizing veins deeper in the body, but it produced cloudy pictures – not ideal for reaching
In a previous role outside FirstHealth, hospice nurse Charlotte Bohn, R.N., CHPN, used the BD PrevueTM II Vascular Access System. Its on-screen tracking allowed her to see the needle as she inserted it, ensuring fast, accurate alignment.
Charlotte and former Hospice House Director Cathy Gentz, CNS,
ACHPN, discussed the system’s
leadership in late 2023 about obtaining one for FirstHealth Hospice House.
was receiving care in the Hospice House. His advanced illness made it
to insert a midline catheter with the old ultrasound technology but couldn’t. He was in a lot of pain, and nurses struggled to keep him comfortable.
Dr. Bodin’s daughter, Heidi Regan, MHA, BSN, R.N., is one of FirstHealth’s quality directors. She saw
At the same time, a PrevueTM II representative was visiting FirstHealth Moore Regional Hospital. The care team arranged for the representative and the vascular access team to come to the Hospice House and try it on Heidi’s father. His midline catheter insertion was easy, and relief was fast.
“I promised my father I would do everything in my power to help control his pain and give him peace when he was no longer able to communicate for himself,” Heidi said.
“The ultrasound was the best thing that could have happened in that moment.”
After her father’s passing, Heidi and her mother asked family and friends to direct gifts in his memory to FirstHealth Hospice Foundation for the purchase of the PrevueTM II, hoping other patients and their families could
The new device arrived at FirstHealth Hospice House in spring 2024, and Bohn said it’s a game changer.
According to fellow hospice nurse Cameron Vestermark, BSN, R.N., “Visualization with the PrevueTM II is so much better than before. We
can help our patients be comfortable in our ability to care for people.”
FirstHealth Hospice House, an 11-bed facility minutes away from FirstHealth Moore Regional Hospital, serves patients who need more medical care than can be provided at home. It is the only facility of its kind in Moore County and most surrounding counties.
The FirstHealth Hospice Foundation, through generous philanthropic support from the community, ensures that Hospice patients are cared for with dignity and respect – regardless of their ability to pay.




In recent years, rural hospitals across challenges, primarily due to aging facilities and shifting health care markets. Montgomery Memorial Hospital found itself at a crossroads. Despite frequent and costly capital improvements, the hospital's age and design began to impose
“As a rural hospital, Montgomery Memorial must adapt to continue serving the people of Montgomery County,” said Mickey W. Foster, MHA, of the Carolinas. “Recognizing the need for transformation, FirstHealth embarked on an ambitious project to reimagine health care in Montgomery County.”
With support from a grant from The Duke Endowment, the Montgomery County Healthcare Reimagining Project was launched, providing a collaborative platform for the community to envision a modernized hospital that would meet their evolving needs.
The new replacement hospital will be a 45,000-square-foot, 10-bed facility equipped to serve the community’s
needs. The design includes 10 emergency department bays, a procedure room, and space to outpatient and observation services.
The new hospital will remain at the same site, in close proximity to on the hospital campus, allowing for future expansion in primary


and specialty care services as the community grows. This thoughtful planning ensures that Montgomery Memorial will not only meet current needs but also be positioned to adapt to future health care demands.
This $40.8 million investment represents more than just a new
building – it symbolizes a renewed dedication to the health and wellbeing of Montgomery County.
With the groundbreaking scheduled for spring 2025, the development of the new Montgomery Memorial Hospital marks the beginning of an exciting new chapter for health care in Montgomery County. By addressing the challenges of an aging facility and creating a space designed for modern health care
its commitment to providing highquality care for the residents of Montgomery County.
“The new hospital will not only meet the current needs of our community but also provide a foundation for future growth and enhanced services,” said Rebecca W. Carter, MSN, R.N., FACHE, president of the western region and administrator of Montgomery Memorial Hospital. “The project is a testament to our dedication to the health and well-being of our residents, ensuring that Montgomery County will continue to have access to exceptional medical care for generations to come.”

For the past 19 years, FirstHealth Moore Regional Hospital has been at the forefront of robotic surgery, providing cutting-edge care to our patients. We are proud to continue this tradition as an SRC-accredited Center of Excellence in Robotic Surgery (COERS). Our accreditation by the Surgical Review Corporation
(SRC) marks a significant achievement in patient care, underscoring our commitment to excellence in health care and patient safety.
SRC, a nonprofit patient safety organization, accredits leading hospitals, outpatient facilities and medical providers worldwide. To earn this prestigious accreditation,
providers must undergo a rigorous, unbiased inspection, demonstrating adherence to nationally and internationally recognized standards of excellence. This thorough evaluation covers treatment pathways, consultative services, equipment, patient education, support groups and surgical experience. Patients can trust SRC’s gold seal as a symbol of
superior patient safety and care. Accreditation requirements have been proven to improve outcomes and reduce hospital stays, offering patients peace of mind and the highest quality care.
Our Robotics Program
FirstHealth’s robotics program offers a revolutionary alternative to traditional open surgery and conventional laparoscopy. By putting a surgeon’s hands at the controls of a state-of-the-art robotic system, we enable unmatched precision, even in the most complex and delicate procedures.
Our skilled surgeons perform a wide range of robotic-assisted procedures, including:
General and Bariatric
• Weight-loss surgery
Gynecologic
• Sacrocolpopexy for treatment of pelvic organ prolapse
• Evaluation and treatment of tubo/ ovarian masses
• Hysterectomy for benign/ early uterine cancer disease (including virtually scarless single-site incision)
• Treatment of endometriosis
• Evaluation of pelvic or abdominal masses
• Pelvic reconstruction
• Removal of uterine fibroids
Gynecologic Oncology
• Evaluation & staging of tubo/ ovarian malignancies
• Uterine malignancies
• Adnexal and pelvic masses
• Diagnosis of lymphadenopathy
• Familial and hereditary cancers including BRCA Syndromes and Lynch 2 Syndromes
• Complex gynecological conditions such as endometriosis and uterine fibroids
Orthopaedic
• Total knee replacement surgery
Solid Organ Surgery
• Bile duct
• Pancreas
• Spleen
• Anti-reflux
• Bowel resection/colorectal surgery
• Adrenal
• Liver
• Gallbladder
• Thoracic
• Lobectomy
Urology
• Prostatectomy
• Nephrectomy
• Pyeloplasty
• Partial nephrectomy
• Adrenalectomy
Robotic surgery is a safe and effective option, offering several advantages over traditional open surgery:
• Minimally invasive techniques mean smaller cuts, leading to quicker healing and less visible scarring.
• Patients experience less postoperative pain and fewer scars, enhancing overall comfort and cosmetic outcomes.
• Shorter hospital stays and quicker return to daily activities are significant benefits of robotic surgery.
• Precision and advanced technology reduce the likelihood of surgical complications.
• Surgeons benefit from better visualization and control, improving surgical outcomes.
With these advancements, robotic surgery at FirstHealth ensures that patients receive the highest standard of care with the most advanced technology available. Trust us to bring you a higher level of surgical care, enhancing your health and well-being with every procedure.
FirstHealth recently introduced robotic knee replacements to our lineup of advanced surgical procedures. This innovative approach combines the precision of robotics with the expertise of highly skilled orthopaedic surgeons, offering patients remarkable benefits:
• Accuracy and precision: Robotic assisted knee replacement ensures precise alignment and placement of the knee implant, improving overall effectiveness.
• Customized approach: Robotic technology allows for personalization to each patient’s anatomy.
• Enhanced recovery and outcomes: Patients typically experience reduced swelling, faster recovery and improved joint stability.
“As the landscape of joint replacement continues to evolve, FirstHealth remains committed to providing patients with the most advanced treatment options available,” said Wayne McFatter, MSN, R.N., CNOR, RNFA, executive director of surgical services for FirstHealth. “The offering of robotic assisted knee replacement surgery is an extension of our continued investment in robotics and technology to enhance care for our patients.”
FirstHealth offers robotic knee replacement surgery at Moore Regional Hospital in Pinehurst and Moore Regional Hospital-Hoke in Raeford.
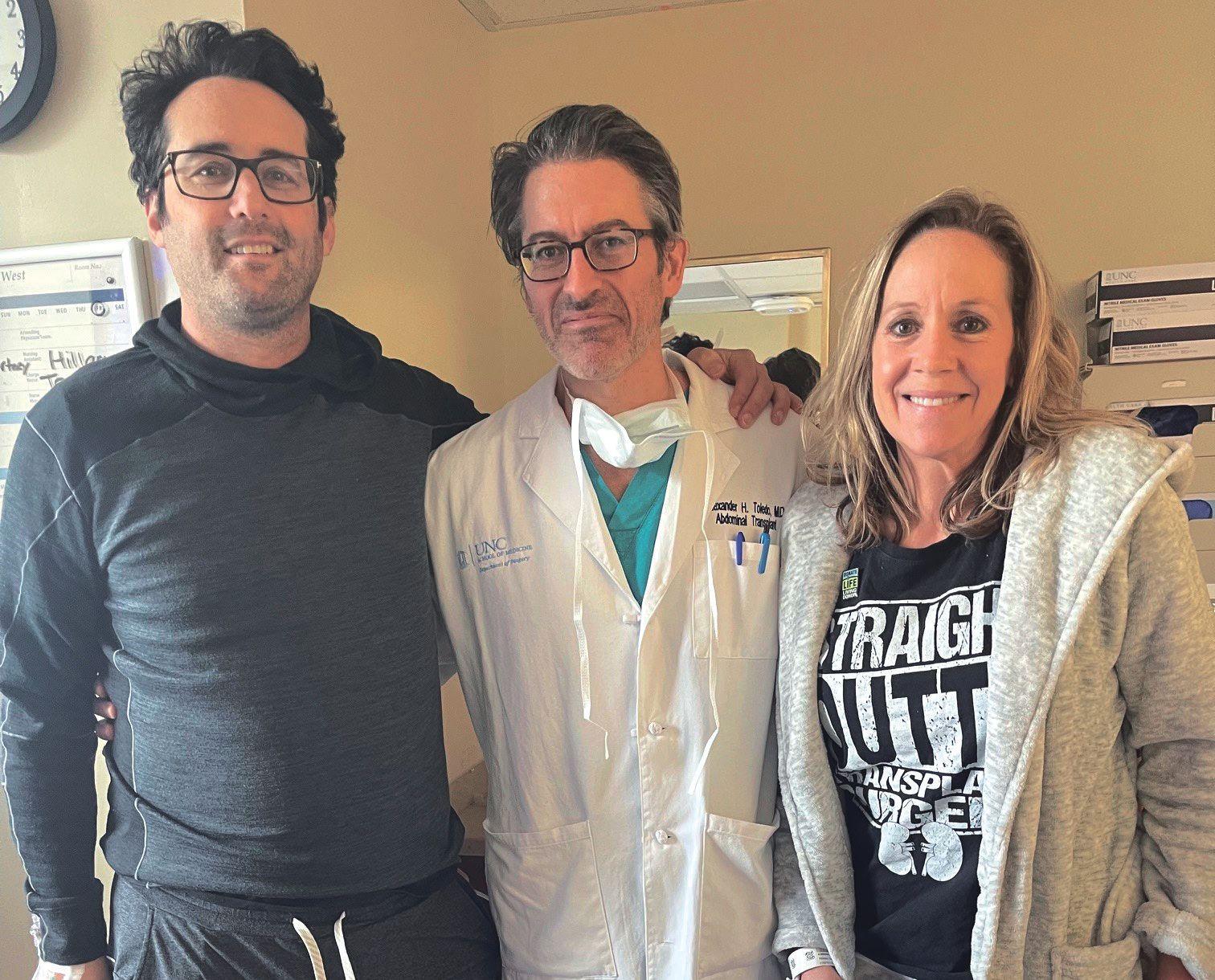
How one special patient became a key cog in her surgeon’s own health care journey
The lifesaving business is one Dr. Peter Ellman knows well. For 15 years now, Ellman, a cardiovascular and thoracic surgeon at FirstHealth’s Reid Heart Center, has changed the lives of thousands of patients and their families.
He has seen everything you can see in an operating room. He’s even saved the lives of other FirstHealth employees. On one occasion, when
Dr. Ellman removed a benign tumor from a coworker’s chest, he had no way of knowing how impactful that procedure would be – both for the patient, Caryn Peterson, and himself.
The surgery, and its impact on Peterson’s life, would become a key cog in Ellman’s own health care journey, one that started early in life and wound its way to the organ transplant unit at UNC Hospital.
Ellman’s path to receiving an organ transplant began with a family tragedy he experienced as a teen.
At 19, Ellman’s mother died after suffering an unexpected brain aneurysm. Ellman said he received the news about his mother’s emergency just as he and his teammates on the Dartmouth
University ski team were preparing to travel to the NCAA Skiing Championships.
“I was diverted from the airport to say goodbye to my mother while she was on life support. At the same time, my father told me her aneurysm was related to polycystic kidney disease (PKD), which they found she had right then and there,” he said. “So, in addition to losing my mother, I was told I had a 50% chance of having this fatal kidney disease.”
Ellman continued with his undergrad education and then went on to medical school, not thinking much about PKD until almost a decade later.
“I was a general surgery resident in my late 20s and, while waiting for a trauma patient to get a CT scan in the middle of the night, ever the optimist, I was thinking maybe I didn’t have it,” he said. “I took an ultrasound probe and checked and saw that my kidneys were full of cysts. This was when I knew I had the disease. It was a little like knowing you have a ticking time bomb in you.”
After completing his education, residency and training, Ellman came to FirstHealth of the Carolinas in 2009. His kidney function was good, and he was ready to begin his career as a CVT surgeon.
“When I started working here my kidney function was normal, but I did get yearly labs. Around 2012 was when the function started to deteriorate, and every year I would hope that perhaps it would not progress, but every year those dreaded labs showed that indeed my function was deteriorating,” he said. “By 2021 my function had deteriorated to the point where I was on the brink of dialysis. That would have meant I was done with my career as a heart surgeon. My hope was that I would potentially be able to get a transplant before that happened.”
Although Ellman’s kidney function continued to decline throughout the 2010s, his impact on patients and families only grew. Around Christmas in 2016, he had his first fateful meeting with Caryn Peterson, who was working as a regional director for FirstHealth clinic in multiple counties.
“Everything was going along fine. I was working, living a perfectly normal life, but I started getting cold-like symptoms and
“I TOOK AN ULTRASOUND PROBE AND CHECKED AND SAW THAT MY KIDNEYS WERE FULL OF CYSTS. IT WAS A LITTLE LIKE HAVING A TICKING TIME BOMB IN YOU.”
— Peter Ellman, M.D.
chest pressure, and I started losing my voice,” Peterson recalled. “It’s getting close to the holidays, and I knew I needed to get checked out. One test led to another, and I ended up seeing a radiologist who was very concerned. He arranged for me to see Dr. Ellman, who pulled me in and showed me a CT scan. He wasn’t 100% sure but told me that I could have a tumor in my chest. It was shocking news.”
Soon after, Ellman and Peterson were discussing surgical options for removing the tumor.
“She was symptomatic from a large tumor about the size of a cantaloupe in the center of her chest. This was compressing her heart and lungs to extent that it was causing her symptoms. We were able to operate the next day and take it out completely. It turned out to be benign, thankfully. She made a quick and complete recovery,” Ellman said.
Peterson said she was “blown away” by the care she received.
“Obviously, he’s a remarkable surgeon. Beforehand he went into a lot of detail and helped explain the best- and worst-case scenarios, so I knew how to prepare mentally. And then he went in and removed it, which is incredible that these surgeons can do these sorts of things day in and day out,” she said. “And on the other end of it, as I’m recovering and regaining my strength, I’m just so grateful for that sort of ability.”
After Peterson’s recovery, a career change led her to the CVT and cardiology clinics, where she became their new director. What seemed like a natural evolution in her career would turn out to be much bigger for Peterson and, more importantly, for the surgeon who had saved her life.
By the end of 2021, as he continued performing surgeries and caring for patients and their families, Ellman’s kidney function had deteriorated to the point that he was referred to the UNC transplantation center. Kidney transplantation can happen with either a living or a deceased donor. Because people can live with only one kidney, it allows a living donor to give life and live the rest of their life with one kidney. Donation is an incredible gift to the recipient, allowing them to avoid going on dialysis and ensuring they can return to a completely normal life, doing what they have always done. Those without a living donor often will go on a deceased donor waiting list, a process that on average means a seven-year wait. During that time, someone with failing kidneys would likely get dialysis three times a week, and they certainly would not be able to do something physically demanding, like heart surgery in Ellman’s case.
“When I went to orientation for transplantation at UNC and learned
about the options, I was hopeful that I would be a candidate for a living donor. Thankfully, my wife Sarah had always told me that she would give me one of her kidneys if I needed it, and she started the work up to be my donor,” Ellman said. “My wife is the toughest person I know. She started the testing to see if she was a match. My kidney specialist here in Pinehurst asked me if I also wanted to go to orientation about dialysis as a backup plan. I told him, ‘No thanks! No plan B!’ He laughed and said, ‘OK, OK!’”
Around this time, as his condition worsened, Ellman began telling those close to him at work about his circumstance.
“I met with Caryn, who was running our clinic, to tell her that in early 2022 I would be out for about two months because I was in kidney failure from polycystic kidney disease. I was just letting her know from a planning standpoint. Certainly, she was surprised because this was not something I had shared with anyone over the years – there was no reason to professionally,” he said.
Dr. Ellman returned to his office and got back to work, and his phone rang five minutes later.
“Caryn called and said she wanted to come down to my office to chat,” he recalled.
It was at that point, only five minutes after learning that he would need a transplant, that Caryn said that she wanted to be Ellman’s donor. Ellman was initially very reluctant about Peterson’s offer, in addition to being amazed with the speed with which Caryn made that decision.
“It is hard to describe what it feels like for someone to come to you and say that they would risk their life for you without hesitation,” he said.
After talking to his wife, Ellman thought it was best to just stick with the original plan of Sarah as the donor.
“I said, ‘OK, I get all that, but I’m going to get tested,’” Peterson said. “I remember going outside and walking around Reid Heart Center’s parking lot, and I felt good. It’s weird to explain it.”
Peterson’s offer to donate led to testing to see if her kidney was a match. And it also led to a heartto-heart conversation with Sarah Ellman at a Christmas party.
“Sarah came up to me, and I remember she held my hand and said that it was beyond amazing that I offered. And she said, ‘We could never let you do that.’”
Peterson recalled. “And I remember looking at her and saying, ‘Sarah, if you both have this surgery, who is going to take care of him? Who is going to take care of you? What about your children?’ And we had this amazing conversation.”
“THIS SOUNDS CRAZY, BUT I KNEW BEFORE THEY CONFIRMED THAT I WAS A MATCH.”
— Caryn Peterson
Peterson said the momentum to donate kept “stirring in her,” and she went down the path, starting with a full round of medical tests, including an extensive review of her entire medical history, including the history of the chest tumor Ellman had removed.
“I contacted UNC and did the initial screening. This sounds crazy, but I knew before they confirmed that I was a match,” she said. “I remember the day UNC called to tell me, and I went over to see Peter. He said, ‘Oh, my gosh.’ And I said we’re going to do this.”
After clearing a few final testing hurdles, there was one choice left for Ellman and Peterson – picking a date for the transplant surgeries. There was only one choice for Ellman.
“We actually did the transplant surgeries in March of 2022, on my mother’s birthday,” Ellman said. “It was a Wednesday, and amazingly enough I had been able to perform a heart surgery on Monday of the same week.”
Two months after the surgery, Ellman was back at work. It would take much longer to start to feel “normal” again, but in 2024 he is exercising again and able to fulfill his passion of taking care of others.
“Right after the surgery you are on a ton of medication, so you feel jittery and not yourself and you are also recovering from the surgery itself,” he said. “I started to feel good after about a year, and now I’ve started running again. Life has gone back to full color. I think one of the hardest things for a human being to deal with is uncertainty. We can deal with bad stuff when we know what it is and what we’ve got to deal with. Now, I no longer have the uncertainty hanging over me. The rain clouds have lifted, so to speak.”
Reflecting on the last eight-plus years, Peterson leans into her faith when explaining what her journey from patient to donor looked and felt like.
“There are moments in life when people have peace about the decisions they make. Maybe you don’t know the why now and maybe you never really know the why, but you have peace,” she said.
“The second part is the impact Dr. Ellman’s had on people and the impact he will continue to have. If heart surgery is what he loves to do and how he can help people, why would we not let him continue to do that? I believe in my core that we are here to serve others, and everybody has different ways of doing it. In that sense, this decision to donate was made for me, and that’s amazing.”
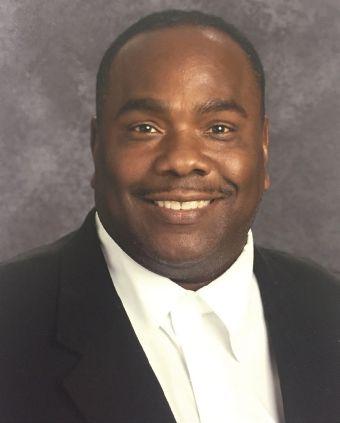


Over the last few years, Glenn Sutton of Hope Mills, North Carolina, experienced a decline in his health due to his increasing weight. Five extra pounds turned into 10, then 20, and soon he felt completely out of control. Diabetes, high cholesterol and high blood pressure became his constant companions.
As a dedicated teacher for 33 years, the turning point came one day while walking the school halls, greeting his students. Glenn found himself extremely tired and winded. He knew then that something had to change.
Glenn started exploring weight-loss options online and came across a patient testimony about weight-loss surgery. He was intrigued and began to research his options. Knowing the excellent reputation of the providers and hospital in Pinehurst, where his wife had recently undergone surgery, Glenn decided to meet with the team at the Metabolic & Weight Management Center.
The Metabolic & Weight Management Center offers both surgical and nonsurgical medical weight management services and a comprehensive approach to weight
loss that is tailored to each patient’s specific goals. A collaborative effort by Pinehurst Surgical Clinic, FirstHealth of the Carolinas and Pinehurst Medical Clinic, the Center is unique to the area and one of the few comprehensive metabolic centers in North Carolina.
From the moment he met general and bariatric surgeon David Grantham, M.D., and the caring team at the Metabolic Center, Glenn felt like he was part of their family.
“I felt like they showed more care and concern for me than I had for myself,” he said. “I know they treat all patients this way, but they made me feel like I was their only patient. That’s how dedicated and passionate they are about what they do.”
On June 18, 2024, Glenn underwent gastric bypass surgery. In less than two months, he lost 46 pounds. His wife, family and church community noticed the change in his physical
appearance almost immediately, but it took Glenn a bit longer to see the new him. One day, he looked in the mirror and barely recognized the person staring back. He was astonished.
The transformation for Glenn has been more than just physical. He now has so much more energy and goes to the gym nearly every day. His blood pressure and cholesterol levels are within normal ranges. He is full of life and happiness, living every day to the fullest. “I really believe this surgery saved my life,” he said.
Glenn is using his experience to encourage and inspire others on their weight-loss journeys. He believes that if there is something out there that can help others take control of their lives and truly live life to the fullest, they should pursue it. For Glenn, that something was weight-loss surgery.
His vibrant personality and cheerful nature shines brighter than ever, proving that with determination and support, a healthy, fulfilling life is within reach.
To learn more about the Metabolic & Weight Management Center, visit WeightLossNC.org or call (910) 725-7966
What is your health story? It began before you were born. From the prenatal care your mother received, to the circumstances of your birth, to your early childhood and adolescence, to your adulthood – all along the way, multiple factors and influences, including genetics, lifestyle and environment, played a role in your current state of health.

For people with unexplained chronic conditions, it often takes time, patience and expertise to find their way back to wellness.
FirstHealth has added a new specialty, functional medicine, which creates a partnership between patients and physicians to delve
into the root causes of illness and restore health.
“The typical functional medicine patient is someone with multisystem, chronic symptoms who has been feeling ill for years and has seen many physicians and health care providers but still lacks a working diagnosis for their illness,” said functional medicine physician Scott Jamison, M.D. Dr. Jamison is an Institute of Functional Medicine Certified Practitioner (I.F.M.C.P.), as well as a board certified internal medicine physician. He is leading the creation of a new functional medicine service line at FirstHealth.
A New Paradigm for Wellness
“The functional medicine model is an individualized, patient-centered, science-based approach that explores genetic, biochemical and lifestyle factors to create a complete picture of a patient’s health status,” Dr. Jamison explained. “We then develop an individualized treatment plan that leads to improved patient outcomes.
“A consultation with a functional medicine physician starts with a simple question: When did you last feel well?” Dr. Jamison said. “For many patients, the answer evokes powerful memories. Then we can
talk about what was going on during that period and whether an accident, illness, surgery or other trauma might have set off a chain of events.
“Ninety percent of patients have experienced some kind of childhood trauma that had an adverse impact on their adult health,” he continued. He gave the example of a 60-year-old patient who recalled moving into an apartment infested with black mold in her teens. She never felt healthy again. For others, the trigger may not be so obvious. For example, many of Dr. Jamison’s patients experienced multiple concussions in their childhood but never connected them with their current health issues.
An initial consultation can take up to two hours, as the patient and physician create a timeline of events and a matrix of health concerns to come to a deep understanding of the patient’s story. This includes thoroughly reviewing all previous medical records and lab results and performing a physical exam.
“Functional medicine physicians never overlook traditional medicine practices; they integrate them into the paradigm,” Dr. Jamison said. “It’s important to look at all previous treatments to see what worked and what failed.”
He noted that in some cases, treatments might

temporarily increase the severity of patients’ symptoms before they gradually improve. By building trusting relationships, functional medicine physicians can help patients stay the course and adhere to a care plan.
Functional medicine physicians can serve as primary care providers, but they can also work closely with specialists.
“We want to build a robust functional medicine program at FirstHealth that is integrated with the primary care program and supports specialty programs, such as rheumatology, cardiology, neurology and oncology,” Dr. Jamison explained. “We can follow patients throughout their care journey, or we can coordinate care with a referring primary care physician.”
Patients can be seen in person or virtually. Dr. Jamison added that, because insurance rarely covers functional medicine, consultations will be priced using an up-front payment model.
“Our first goal is to educate prospective patients and the health care community about what functional medicine is and how we can help patients work through complex medical problems and understand how to take better care of themselves.”
“I’m excited that the forwardthinking leadership at FirstHealth has committed to bringing functional medicine to the network,” Dr. Jamison added. “The most important thing that we can give people is a clear understanding of what has happened to them and a renewed sense of hope that they will find their way back to health.”
For more information, contact FirstHealth Functional Medicine at (910) 684-5499.
1. Stress (physical and psychological)
2. Toxins (biologic, elemental, synthetic) and impaired detoxification
3. Antigens/allergens/food sensitivities (foods, mold, dust, animal products, pollens, chemicals)
4. Inflammations/infections (bacteria, yeast, parasites, prions, other microbes)
5. Nutrition (dietary insufficiencies and excesses)
6. Sleep

From opioid and alcohol addiction to anxiety, depression and other psychological struggles, the demand for mental health services in the United States is at an all-time high. And without enough providers nationwide to help address these issues, many needs go unmet.
FirstHealth of the Carolinas recognizes the importance of caring for the whole person, both body and mind. We designed our Behavioral Health Services to provide the local community greater access to care with specialized services to meet their unique mental health needs.
The FirstHealth Outpatient Behavioral Services Clinic provides mental health services to clients with a variety of concerns – from obsessive-compulsive disorder and post-traumatic stress to early-stage dementia, mood disorders and more. Staffed by a highly collaborative team of nurse practitioners and psychiatrists, including a board-certified child and adolescent psychiatrist, the clinic sees patients of all ages.
Every in-person or online visit is allotted ample time for the provider to give patients their undivided attention. The clinic is able to meet the growing demand for services with the help of an online patient portal. Through the portal, patients can communicate directly with their provider regarding minor questions or concerns. This expedites care and frees up valuable appointments for those who need them.
“Using the online portal has been a game-changer. It allows us to help more patients without compromising our very personalized, high quality of care,” explained Meredith Stanton, M.D., medical director of FirstHealth Outpatient Behavioral Services.
FirstHealth’s 28-bed Inpatient Behavioral Services unit, located at Moore Regional Hospital, is designed for
patients in need of intensive mental health services. The unit helps patients who pose a safety risk to themselves or others. It also offers medically supervised inpatient detoxification for alcohol and is one of the only inpatient units in the state to offer inpatient detoxification for some cases of opioid withdrawal.
Patients often access inpatient mental health services through the emergency department, but FirstHealth also accepts referrals from other health providers.
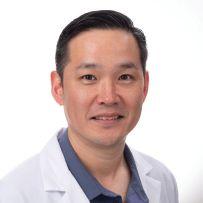
“It’s important to know that inpatient care can be voluntarily, which allows our team to maximize patient autonomy and choice. Our typical length of stay is four to five days,” explained Eugene Kim, M.D., medical director of FirstHealth Inpatient Behavioral Services. “Our role is to help patients work through their acute crisis safely and then refer them for additional care.”
Inpatient services occur on a locked unit to ensure patient safety and include a scheduled routine of psychiatric evaluation, group therapy/classes and recreational therapy. Patients are cared for by psychiatrists, physician assistants, social workers and psychiatric nurses. A number of psychiatrists on staff, including Dr. Kim, have unique qualifications to serve the local community. He is a retired military psychiatrist as well as a specialist in addiction psychiatry.
“Post-traumatic stress disorder and substance use are common struggles in our local military community,” said Dr. Kim. “We work to understand the needs of our patients and are here to assist.”

Cancer survivors shagged the night away to the music of the Sand Band at the Fair Barn in Pinehurst on May 9, 2024.



The FirstHealth family was out in force on September 14, 2024, for the Walk to End Alzheimer’s at Sandhills Community College.

FirstHealth celebrated its annual NICU reunion on September 8, 2024, with a “backyard beach bash” and brought together NICU graduates and their families.

The Strike Out Stroke baseball game with the Sandhills Bogeys was a fantastic opportunity to raise awareness about stroke prevention and care, and it was heartening to see such strong participation from our stroke team and the community. FirstHealth staff were present to provide valuable information and tips about stroke awareness, helping to educate the community on the importance of recognizing stroke symptoms and taking quick action.



FirstHealth Community Health had a Heartto-Heart Conversation with Richmond County community members as part of the Million Hearts initiative.


Behavioral Services
Katie Weinel, M.D.
FirstHealth Outpatient Behavioral Services
Cardiology
Kathy Lewis, AGPCNP
FirstHealth Cardiology – Rockingham

Family Medicine
John M. Ray Jr., M.D

FirstHealth Family Medicine – Pinnacle
Primary Care
Peter Dorton, M.D
FirstHealth Primary Care – Pinehurst

OB/GYN
Julia Malis, M.D.

Cardiology
Amanda Jacobs, FNP
FirstHealth Cardiology – Laurinburg
Functional Medicine
Scott Jamison, M.D.
FirstHealth Concierge & Functional Medicine


Southern Pines Women’s Health Center – a FirstHealth Clinic

Family Medicine
Angie Hounsell, FNP
FirstHealth Family Medicine –Whispering Pines

OB/GYN
Molly Crossman, WHNP
Southern Pines Women’s Health Center, a FirstHealth Clinic – Lee


OB/GYN
Lilliam Schnitzer, DNP
Southern Pines Women’s Health Center –a FirstHealth Clinic
OB/GYN
Tiffany Greco, NP
Pinehurst Surgical Clinic Women’s Center


Primary Care
Patricia Lage, M.D.
FirstHealth Primary Care – Raeford
Primary Care
Anusha Gaddam, M.D.
FirstHealth Primary Care – Lee

Palliative Care
Meagan McLean, DNP
FirstHealth Palliative Care

Primary Care
Jessica Sessoms, FNP
FirstHealth Primary Care – Lee

ANESTHESIA – FIRSTHEALTH
ANESTHESIA
Christine Nagel, CRNA
Maggie Wunder, CRNA
ANESTHESIA – PROVIDENCE
ANESTHESIA ASSOCIATES
William Cox, M.D.
EMERGENCY MEDICINE –SANDHILLS EMERGENCY PHYSICIANS
Steven App, M.D.
Zoe Langseth, PA-C
Lindsey Oberacker, PA-C
Steven Owens, DPA
Kelsey Tunison, M.D.
FIRSTHEALTH CONVENIENT CARE
Havanna Holfert, FNP
America Reece, FNP
Brianna Stone, PA-C
FIRSTHEALTH HOSPITALISTS
Karen Kastler, ACPN
Catherine Kelly, D.O.
FIRSTHEALTH OB HOSPITALISTS
Amanda Kandes, FNP
Tiffany Thompson, CNM
FIRSTHEALTH INTENSIVISTS
John Verrilli, M.D.
GASTROENTEROLOGY –PINEHURST MEDICAL CLINIC
Jenna Cavanaugh, FNP
Lashawnda Campbell, DNP
OPHTHALMOLOGY – PINEHURST SURGICAL OPHTHALMOLOGY
Andrew Coggin, M.D.

PERFUSION
Emily Venneri, CCP
PHYSICAL MEDICINE & REHABILITATION – CAROLINA REHABILITATION & SURGICAL ASSOCIATES
Michelle Huynch, PA-C
Tricia Tie, PA-C
I was recently a patient in three of FirstHealth’s regional facilities: Hoke County (ER only), Richmond County and Montgomery County. I received the absolute best care in all three locations. As an expression of my appreciation to the wonderful staff of the two hospitals in which I was an inpatient (MRH-Richmond and MMH), I would like to provide a full meal to each of them on a date(s)/time(s) most convenient to their hospital’s schedule.
I’ve provided a breakdown of anticipated expenses as provided to me by Brenda Brock, outpatient nurse manager (MMH), just before I was discharged. I think that information was given to Ms. Brock by you, but I've included it just in case.
Although the total cost to provide these meals is listed at $800, I have enclosed a check for $1,000 to cover any unexpected additional charges. If there are little or none, please use the extra money to support any of your foundation’s other projects or events.
Please let the recipients of the meals know who their benefactor is and how grateful I am to each and every one of them. In today's parlance, THEY ROCK! Thank you, in advance, for all your efforts to make this happen ... and for your work to provide the best health care services to our fellow residents of North Carolina.
Sincerely,
Roger J. Dostall, A.A., B.S., M.S.
Reprinted from Nextdoor.com
Do you have a FirstHealth employee you would like to give KUDOS to, or would you like to share your patient experience? If so, visit FirstHealth.org/ CaretoShare and share your exceptional experience with us today.
On Tuesday, February 6, 2024, we admitted my wife, Mariann Benway, for surgical hip replacement by Dr. Dave Casey and the staff of FirstHealth.
From the moment through what I am certain was a dozen and more processes and checkpoints to final discharge, we experienced an unbroken culture of Can Do! and I Care!
From your newly hired cleaning lady who insisted on escorting me to find my wife’s post-surgery room; to the anesthesiologist who tailored his operating room approach based on the factors he researched related to my wife’s childhood polio; to Natalie, our R.N., who made my wife’s first hours out of surgery a cakewalk; to Dave Casey, our surgeon, combination Patton, St. Francis of Assisi and Eddie Shore of the (old) Boston Bruins, who did a superb job in the OR; to the volunteer, a gentleman hailing from Burlington, Vermont, who helped us load Mariann and equipment into the car on discharge; and numerous other pros in between whose names I regret I don’t recall – they all made our stay an entirely warm and professional experience.
We want to thank you and your entire team for your day-to-day pursuit and achievement of excellence.
Most sincerely, Ken and Mariann Benway
Whispering Pines, North Carolina

