Dear colleagues,
If you’ll indulge with some poetic license, a theme for the ages, but particularly 2024, is a tale of two cities: Perspicuity and automaticity. These “cities” aren’t on the map; they are living in our heads. We live mostly automatic lives with routines and heuristics governing most of our actions (automaticity). But what makes us happy humans is when we do purpose-driven actions (perspicuity). In many contemplative traditions, gaining insight through various techniques like asking clarifying questions and questioning automatic routines leads to growth of individuals and organizations. To be perspicuous about metatrends affecting CU PM&R, here are a few to consider:

• We live in the wild, wild west of post-acute care in Colorado, where certificate of need is not necessary and multiple private options exist.
• State and federal legislation will drive more site-neutral payments (reduction of facility fees)
• There will be increased disability with traditional diagnoses as well as long COVID and increasing mental health burden.
• Changing and shifting of health care delivery to involve different disciplines
• Hospital finances and eroding margins affect academic and clinical coverage support
• The value of academics and science needs to be creatively broadcast with societal polarization and media landscape changes.
Last year we bit away at these trends with some major accomplishments:
• Further expansion into the community with bigger clinical footprints in the Denver south suburbs, Colorado Springs, Cherry Creek, Longmont and Boulder
• Received accreditation for the launch of DPT hybrid education
• Cultivating physician and rehabilitation scientists
• Creating new financial models
I hope you perspicaciously enjoy our annual bulletin. As always, we thank you for your support of CU PM&R!
Sincerely,
 Professor and Chair, Department of Physical Medicine & Rehabilitation University of Colorado Anschutz Medical Campus, School of Medicine
Professor and Chair, Department of Physical Medicine & Rehabilitation University of Colorado Anschutz Medical Campus, School of Medicine
HOSPITALS 7
$16.5 MILLION
IN CLINICAL REVENUE
#5
FACULTY RANKED BY BLUE RIDGE NIH RANKINGS, SEE DETAILS ON NEXT PAGE FOR RESEARCHERS.
IN SPONSORED PROJECT FUNDING
$3.9 MILLION FACULTY & STAFF
#12
DOXIMITY REPORT RANKING OF RESIDENCY PROGRAM
293
#13
5280 MAGAZINE
2023 TOP DOCS 11
U.S. NEWS AND WORLD REPORT RANKING OF THE PHYSICAL THERAPY PROGRAM
Don’t forget to vote for rehab and specialty hospital facilities in Colorado: UCHealth University of Colorado Hospital, UCHealth Broomfield Hospital, Children’s Hospital Colorado, Craig Hospital.







University of Colorado $1,724,219
*including CU PM&R researchers erroneously assigned to other departments.
Jennifer Stevens-Lapsley $624,348
Kristin Uhler $385,949
Cory Christiansen $385,090
Michael Bade $201,661
Andrew Smith $127,171
In 2023, CU PM&R was fortunate to welcome seven new members to our faculty!

Alyssa Arms, PT, DPT, OCS is a 2010 graduate of the CU DPT program. She has taught Examination/Evaluation, Foundations of Intervention, and Medical Conditions, and she specifically lectures on all the Integumentary and Wound Care content. Dr. Arms also works at her private practice, Back in Step PT, where she specializes in working with dancers and other performing artists. Dr. Arms is also the 2023 recipient of the CU Physical Therapy Alumni Association Alumni Achievement Award.
Kelli Browning, MSN, RN, CPNP-PC is our newest APP. Kelli works in the Neuromuscular clinic at Children’s Hospital Colorado where she focuses on providing novel treatments, care coordination, and holistic evidence-based care to children and adolescents. Kelli has 7 years of pediatric nursing experience that included care in the CHCO PICU and PACU, Primary Care, and Home Health departments. Kelli’s varied nursing background has given her insight into caring for children with a large range of healthcare needs. She completed her Master of Science in Nursing at the University of Colorado with a focus in Pediatric Primary Care.


EJ Gann, PT, DPT, NCS joined the CU PT faculty and will have strong involvement in the Neuromuscular Conditions track courses. He will be responsible for coordinating Neuromuscular Conditions I, beginning in 2024, and will lecture and assist with lab sessions throughout the rest of the track. He is excited to continue to serve as a facilitator within the two Interprofessional Education courses offered to DPT students which occur in the Spring and Fall and will also serve as a facilitator within the Capstone Course for 3rd year DPT students. In addition, he will be a part-time PT clinician at UCHealth. Dr. Gann joins us from UCSF.
Marc Heronemus, MD is a graduate of the CU PM&R Residency and the CU Primary Care Sports Medicine Fellowship and has joined the CU PM&R faculty as an instructor and attending physician at Denver Health. Dr. Heronemus will be attending to musculoskeletal care, including sports medicine at Denver Health, as well as general physiatry.


Lauren Hinrichs-Kinney, PT, DPT, PhD, OCS has clinical expertise in orthopedics, including over 10 years of clinical experience. Over the past four years, her research has been primarily focused on post-acute care, specifically exploring methods to effectively implement evidence-based rehabilitation practices within skilled nursing facilities. Her role encompasses teaching responsibilities in Foundational, Musculoskeletal, and Applied Exercise Science courses. Additionally, she actively participates in several committees, including the Student Enrichment Committee and the Student Awards Subcommittee. She also makes contributions to the Education Scholarship Group.
Amanda Miller, PA-C joins CU PM&R as one of our newest Pediatric APPs at Children’s Hospital Colorado, serving the pediatric brain injury population. Amanda also serves as a CU CHA/PA (Child Health Associate/Physician Assistant) senior instructor in physiology.


Stephanie Tow, MD, FAAPMR, CAQSM serves as our new pediatric rehabilitation physician focusing on the pediatric chronic pain population as well as pediatric sports medicine in Colorado Springs. Dr. Tow was a CU PM&R fellowship graduate and held previous positions at UT-Southwestern. Dr. Tow has a passion for working with athletes and patients with all types of abilities and is the Head Team Physician for Team USA’s Paralympics Swimming National Team. She also serves as a National Medical Classifier for US Paralympics Swimming.


After 14 years on the CU Physical Therapy and CU Physical Medicine & Rehabilitation faculty, Lisa Dannemiller, PT, DSc, PCS retired from the University of Colorado in February of 2023. Prior to coming to CU, Dr. Dannemiller was a full-time clinician, primarily in pediatrics, for nearly 25 years. She mostly worked in early intervention with families of children from birth to age 3, who had special needs. Dr. Dannemiller completed a Doctor of Science in Pediatric Physical Therapy at Rocky Mountain University of Health Professions from 2000-2005, after which she worked part-time in a county hospital pediatric out-patient clinic and part-time at the University of Findlay in Ohio, as an adjunct faculty member. In 2008, she was chosen as a full-time faculty member at CU, with clinical time at Children’s Hospital Colorado.
During her time at CU, Dr. Dannemiller taught most of the pediatric physical therapy content. She worked with the faculty on integrating this content into appropriate courses and making sure that students were exposed to family-centered care. In addition, Dr. Dannemiller was on the Recruitment and Admissions Committee as a member, and chair of the committee with a major goal of growing the diversity of our cohorts to serve the communities in which they work. This work grew into participation in other School of Medicine and CU PT Diversity, Equity, and Inclusion initiatives over the years. “There is phenomenal work being done in this arena on our campus!” Dr. Dannemiller says.


Dr. Dannemiller describes her time at CU as, “an amazing learning adventure! I so valued the opportunity to gain knowledge and insights from our collaborative faculty and staff who have incredible expertise in a variety of areas that impact the field of physical therapy.” When asked what she will miss most about being on the faculty at CU PT and PM&R, she says,
“
I feel that I will really miss being a part of the formation of future physical therapists who will move this profession ahead in ways I can only begin to imagine. It is all about finding ways to help students maximize their potential through the collaborative work of faculty who are constantly striving to support our students’ passion.
“
In retirement, Dr. Dannemiller and her partner moved to the mountain community of Buena Vista, Colorado. They have spent time hiking, kayaking, and visiting friends and family. They hope they can continue to go outdoors in the winters, but she plans to do more weaving when it is too cold. Dr. Dannemiller will continue to do some pediatric lab instructing at Hawaii Pacific University, some projects with CU PT as an associate faculty member, and volunteer activities with the Academy of Pediatric PT and in her new community. Dr. Dannemiller and her partner have a kayaking and hiking trip planned in Portugal for May 2024. In reflecting on her retirement, she says, “I am so very grateful for this time in my life because I have the gift of time to take care of myself and others in ways that were not feasible when working fulltime. I am thankful for all the students, faculty and staff who have influenced my life in ways they may never know. Every moment is a gift.” CU Physical Therapy and Physical Medicine & Rehabilitation wishes Dr. Dannemiller the very best in this new chapter of her life!


Each year, 5280 Magazine surveys Denver physicians and asks them, specialty by specialty, which metro-area physicians they would trust to treat themselves and their families. The 2023 Top Docs list includes 11 of our esteemed colleagues:

Dr. Jeffrey Berliner
MEDICAL SPECIALTY:
PHYSICAL MEDICINE & REHABILITATION
HOSPITAL AFFILIATION:
Craig Hospital


Dr. Mark Johansen
MEDICAL SPECIALTY:


Dr. Morgan Brubaker
MEDICAL SPECIALTY:
Dr. Rachel Brakke Holman
MEDICAL SPECIALTY:
PHYSICAL MEDICINE & REHABILITATION
HOSPITAL AFFILIATION:
University of Colorado Hospital
PHYSICAL MEDICINE & REHABILITATION
HOSPITAL AFFILIATION:
Craig Hospital
PHYSICAL MEDICINE & REHABILITATION
HOSPITAL AFFILIATION:
Craig Hospital


Dr. Michael Makley
MEDICAL SPECIALTY:
NEUROLOGY
HOSPITAL AFFILIATION:
Craig Hospital


Dr. William Scelza
MEDICAL SPECIALTY:

Dr. Gary Maerz
MEDICAL SPECIALTY:
Dr. Scott Laker
MEDICAL SPECIALTY:
PHYSICAL MEDICINE & REHABILITATION
HOSPITAL AFFILIATION:
University of Colorado Hospital
PHYSICAL MEDICINE & REHABILITATION
HOSPITAL AFFILIATION:
Craig Hospital

Dr. Joseph Rosenthal
MEDICAL SPECIALTY:
PHYSICAL MEDICINE & REHABILITATION
HOSPITAL AFFILIATION:
UCHealth Broomfield Hospital
Dr. Deborah Saint-Phard
MEDICAL SPECIALTY:
SPORTS MEDICINE
HOSPITAL AFFILIATION: University of Colorado Hospital
PHYSICAL MEDICINE & REHABILITATION
HOSPITAL AFFILIATION:
Craig Hospital


Dr. Eric Spier
MEDICAL SPECIALTY:
PHYSICAL MEDICINE & REHABILITATION
HOSPITAL AFFILIATION:
Craig Hospital
Dr. Kristin Uhler is an associate professor in the Department of Physical Medicine & Rehabilitation and audiologist at Children’s Hospital Colorado. Her work has received funding from the NIH National Institute on Deafness and Other Communication Disorders (NIDCD), with her grant lasting through 2028.
In layman’s terms, tell us about the specific research you are doing?
We are researching how babies learn to tell different speech sounds apart, like when they hear “mad” and “sad.” This skill develops in the first year of life and is influenced by the sounds they hear every day. Said a different way, infants go from being universal language learners to nativists around 6-8 months of age. This theoretical construct has been used for more than three decades, and we are applying it to infants who have hearing differences. An infant’s improved ability to differentiate between sounds in their native language has been correlated with better language outcomes. Our goal is to develop benchmarks of auditory development between a group of children with hearing loss and those with typical hearing. If a baby is not meeting these benchmarks, we might change the early intervention strategies.
What are your ultimate goals as it relates to your research projects?
Our long-term goal is to improve speech and language outcomes among children with hearing loss.
Which groups or individuals are you working with for your various investigations?
I work with audiologists and early interventionists across Colorado on this project, as well as Drs. Sharon Hunter, Phillip Gilley, Dan Tollin, Angela Madrid, and Kerry Walker.

What initially drew you to audiology?
I became interested in pediatric audiology around the time that universal newborn hearing screenings began and shortly after the publication of the first seminal paper emphasizing the advantages of early hearing screenings. I am drawn to the physiological and neurological aspects of hearing, and that I have the opportunity to work closely with families and their children, providing support and guidance as they navigate this unexpected journey.
What is your favorite part about being a researcher within the Department of Physical Medicine & Rehabilitation?
I have been incredibly fortunate to find not only a career but also a mentor and a support system within the Department of PM&R and across the CU campuses! The guidance and unwavering support from a solid mentoring team have shaped my journey to become an independent and funded researcher in our department. Next, the supportive nature of the senior researchers in our research community is equally remarkable. Their collective approach to thinking broadly and encouraging young faculty members is an invaluable asset. It goes beyond the transfer of knowledge and embraces the cultivation of new talent, fostering an environment of collaboration and shared learning.
The lifespan approach to research is both intellectually stimulating and profoundly humbling. It emphasizes the continuity and interconnectedness of human development, reinforcing the idea that our work has the potential to impact individuals from the very beginning of life to their golden years. This perspective serves as a constant reminder of the responsibility we carry as researchers to contribute to the well-being and quality of life of people across their entire lifespan.
Has anything surprised you this year as you have embarked on your research endeavors?
This year, I have encountered many surprises that have left a lasting impression on my journey. Most notably, I have been thoroughly impressed by the expertise and dedication of my mentors. Their guidance has been invaluable, not only in terms of honing my research skills but also in shaping my perspective on the field of audiology. Simultaneously, I’ve been humbled by the realization of how much there is to learn. This realization has only ignited my passion further as I eagerly embrace the opportunity to acquire this wealth of knowledge and skills.
The most exciting aspect of this year has been the ability to conduct the line of inquiry that I’m so deeply passionate about. The opportunity to delve into research that not only aligns with my interests but also holds the potential to make a meaningful contribution to the field of audiology has been a source of great enthusiasm.
What advice would you give to aspiring or new researchers in the field?
Work hard, be tenacious, find a good set of mentors, be kind to yourself, if you’re able to build a team, hiring well is crucial; be patient, and take care of yourself!
How can participants who are interested in participating in your trials join them?
https://redcap.ucdenver.edu/surveys/?s=3NKPHX784FM393AK
Any closing thoughts?
I am grateful for Drs. Akuthota and Apkon’s support and commitment to supporting research and the academic growth of our department.

I have been thoroughly impressed by the expertise and dedication of my mentors. Their guidance has been invaluable, not only in terms of honing my research skills but also in shaping my perspective on the field of audiology.
In the field of pediatric rehabilitation medicine, hope is taking center stage as advancements in neuromuscular treatments are changing the lives of children and young adults. The University of Colorado Department of Physical Medicine & Rehabilitation is one of the few academic programs in the country where physiatrists work alongside neurologists in an interdisciplinary team to treat young patients living with these conditions. For the rehabilitation doctors on these teams, ensuring a high quality of life for these patients is central. At Children’s Hospital Colorado, Susan Apkon, MD, professor of Physical Medicine & Rehabilitation, and chief of Pediatric Rehabilitation Medicine at the University of Colorado, and Anne Stratton, MD, associate professor of Physical Medicine & Rehabilitation at CU, are at the forefront of this exciting journey. In a recent interview, they shed light on their groundbreaking work, offering insights into the conditions they treat, promising medical interventions, and their shared vision for the future.
 ANNE STRATTON, MD
ANNE STRATTON, MD
Drs. Apkon and Stratton serve a vast region spanning seven states in the Rocky Mountain Region, treating children and young adults afflicted with an array of neuromuscular conditions, including Spinal Muscular Atrophy (SMA), Duchenne Muscular Dystrophy, Myotonic Dystrophy, and Charcot-Marie-Tooth Disease. Their clinic is a hub of activity for these rare conditions. The common thread linking these conditions is their impact on muscles and nerves, making it a dynamic field of study.
 SUSAN APKON, MD
SUSAN APKON, MD
The advent of groundbreaking treatments is altering the landscape of neuromuscular medicine. Dr. Apkon enthusiastically shared the transformative impact of FDA-approved treatments for SMA. These treatments, such as Nusinersen, Onasemnogene (a gene therapy), and orally administered Risdiplam, have been nothing short of miraculous. What was once a heartbreaking diagnosis with a grim prognosis now has hope. Infants diagnosed with SMA, previously facing a dire future, are now thriving, walking down hallways, and attending school. Dr. Apkon says she can barely contain some of these toddlers during routine examinations!
Dr. Apkon revealed the exciting clinical trials underway at Children’s Colorado, primarily focusing on SMA, Duchenne Muscular Dystrophy (DMD), and Myasthenia Gravis. The trials are instrumental in testing and refining promising treatments. One of the clinical trials includes gene therapy for boys with Duchenne Muscular Dystrophy, providing a one-time infusion of a miniaturized dystrophin gene. Another avenue being explored is antisense oligonucleotide (ASO) exon skipping drugs for specific genetic mutations in DMD patients. The third novel approach involves a cellbased therapy named Capricor, with a goal to improve upper limb function and heart function in older boys with Duchenne Muscular Dystrophy.
While it’s impossible to predict the future with certainty, Dr. Apkon shares her optimism about the direction of neuromuscular medicine. She anticipates a continuation of the trend of increased clinical trials and the potential use of CRISPR technology, albeit with certain limitations. Dr. Stratton believes that precision medicine and more disease modifying treatment options will continue to improve outcomes for these populations. Furthermore, the focus is shifting toward secondary conditions caused by these neuromuscular diseases, which opens new avenues for potential treatments.
What drives Dr. Apkon and Dr. Stratton in their pursuit of better treatments for neuromuscular conditions?
“
Dr. Apkon acknowledged the significant costs associated with gene therapy, noting that the gene therapy for boys with Duchenne Muscular Dystrophy is approximately $3.4million. These expenses are part of the broader challenge in making these groundbreaking treatments accessible to all who need them. Dr. Apkon and Dr. Stratton have both had significant involvement with the national Cure SMA Foundation, Parent Project Muscular Dystrophy, and Muscular Dystrophy Association. Dr. Stratton’s advocacy and dialogue at state and national level plays a pivotal role in addressing these financial hurdles for families of patients with DMD. Dr. Stratton has worked with both the Colorado and the Wyoming Drug Utilization Review Boards to make these treatments available with state Medicaid Funding.
What was once a heartbreaking diagnosis with a grim prognosis now has hope. Infants diagnosed with SMA, previously facing a dire future, are now thriving, walking down hallways, and attending school. Dr. Apkon says she can barely contain these toddlers during routine examinations!
Dr. Stratton pointed to the intricate genetic and pathophysiological aspects of the field. She finds the science side of it fascinating and the possibility to impact the quality of life of these patients profoundly rewarding. Dr. Apkon enjoys being involved in clinical trials to contribute to the design and execution of research, pushing the boundaries of what is possible in the field. She credits her mentor, and former Chair of the Department of Physical Medicine & Rehabilitation, Dr. Dennis Matthews, with allowing her the opportunity to participate in a niche area of medicine usually reserved for neurology trainees during her residency at CU in the 1990’s. Both Drs. Apkon and Stratton view PM&R physicians as critical team members given the expertise in maximizing function and utilizing medical and rehabilitation treatments to meeting patient’s goals.
In November of 2022, Dr. Apkon’s team was awarded a grant in partnership with the Cure SMA registry. Cure SMA came to Children’s Hospital Colorado to celebrate this pivotal partnership.
Drs. Apkon and Stratton’s groundbreaking work in the treatment and research of neuromuscular medicine paints a hopeful picture for children and young adults suffering from these conditions. Their dedication to advancing treatments and their vision for the future reflects the transformative nature of medicine. As they continue to break new ground, children with neuromuscular conditions can look forward to brighter prospects, more smiles, and a life unburdened by the limitations of their diseases.
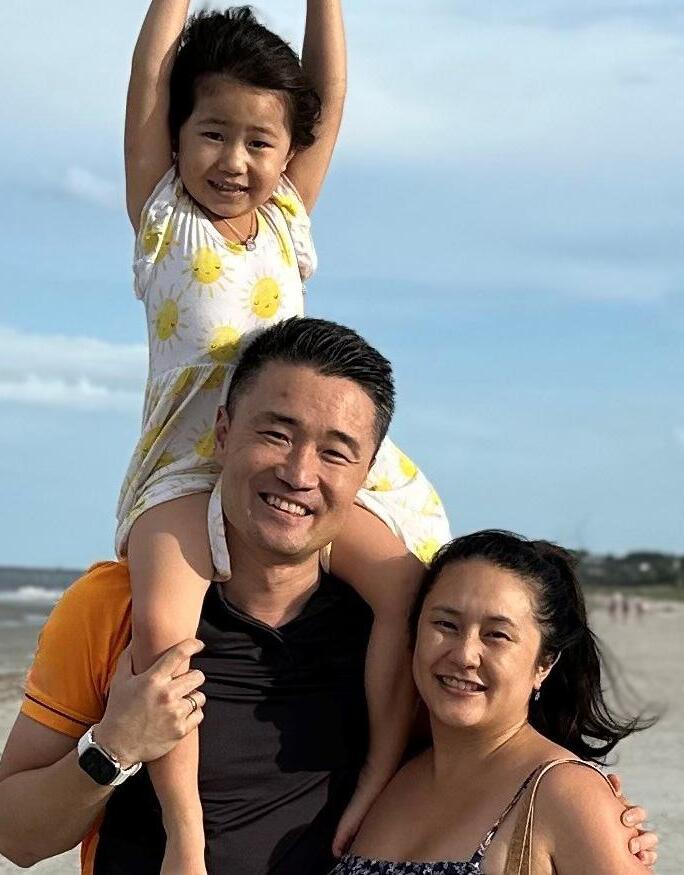
“

CU PM&R alumni Drs. Thomas Xu and Jessica McCabe work together at the Piedmont Physicians Group Sports and Spine Specialists in Atlanta, Georgia. Piedmont Healthcare is one of the oldest healthcare systems in Georgia, established in 1905. It is also one of the biggest healthcare organizations in the state. In its history there was not a physiatry presence and when Dr. Xu joined the organization initially as part of the department of neurosurgery, he proposed the opportunity to establish a physiatry presence to best serve patients and provide a more comprehensive model of care. The practice has now grown to include three physicians, one nurse practitioner, and two EMG technicians and is an entrenched part of the neurosciences program at Piedmont Healthcare. Drs. Xu and McCabe both completed their PM&R residencies at CU in 2016. Prior to residency, Dr. Xu completed his undergraduate degree at the University of Southern California, medical school at the University of Toledo, and internship at Jewish Hospital of Cincinnati. Following residency, he went on to complete an Interventional Spine Fellowship at UCLA, and established his practice in 2017. Dr. McCabe completed her undergraduate degree at the University of Georgia, medical school at Emory University, and internship at Emory University.
Get to know more about Drs. Thomas Xu and Jessica McCabe:
Tell us about the work you are currently doing in Atlanta?
Dr. Xu: I specialize in interventional spine and musculoskeletal medicine. The procedural modalities I perform include cervical, thoracic, lumbar epidural injections, facet injections, radiofrequency ablation, sympathetic nerve blocks, large joint injections, peripheral nerve blocks, spinal cord stimulator trial and implantation.
Dr. McCabe: I specialize in electrodiagnostic studies including polytrauma studies for patients at the Shepherd Spinal Cord Center. I also provide conservative sports and spine care and perform ultrasound guided joint, tendon sheath and muscle trigger point injections. I perform Botox for spasticity and migraine. I also help in the diagnostic work-up for patients with Thoracic Outlet Syndrome including diagnostic anesthetic injections and Botox injections.
Why did you decide to pursue physical medicine and rehabilitation?
Dr. Xu: As a relatively smaller field, not every medical student has the chance to be exposed to PM&R. I was lucky enough to have rotated through the PM&R Department
during medical school which presented itself as a perfect fit for me as the field can be both clinical and procedural. The focus on the improvement of patients’ function is a fulfilling goal to continue to progress toward.
Dr. McCabe: I have always wanted to pursue PM&R because I love the concept of improving a patient’s function and reducing pain so patients can get back to living their life to the fullest.
How did the two of you, both CU trainees, decide to go into practice together?
Dr. McCabe: Dr. Xu and I, and our families, are very close and we spend a lot of personal time doing family activities together. After residency, I moved back to Atlanta to be close to family, and to raise my children. My husband and I both grew up here. A few years later, Dr. Xu finished his fellowship and joined us in Atlanta and started Piedmont Sports and Spine. I left Kaiser Pain Management soon after to join him and help him grow the practice.
How did your training at CU prepare you for your career today?
Dr. Xu: CU provided a very comprehensive program that allowed exposure to all essential parts of PM&R for me. As someone that was interested in interventional spine, I felt the exposure and training during residency prepared me well for fellowship
training and independent practice. Residency not only provided a practical knowledge base but also provided the support and framework to allow me to develop confidence in independent clinical decision making.
Dr. McCabe: CU PM&R training was ideal to prepare me for practice because it was well rounded and comprehensive. The educators were kind and amazing and I will always have fond memories of my time in the program. I am very grateful I was able to be a part of it. The skills and knowledge I learned at the University of Colorado laid the foundation for which I grew my skills and competency for practice. One of the most important skills I learned was how to independently learn and improve on procedural skills, as a physician needs to be a lifelong learner.
What part of your job do you find most rewarding?
Dr. Xu: The best part of the job is following patients through their journey and seeing the progress they make along the way.
Dr. McCabe: My favorite part of the job is helping people find answers to why they have been in pain and then developing a plan to feel better. I love the feeling of mutual trust that develops with a good physician-patient relationship. They trust me to help them find solutions and I trust that they will do the work to feel better.
What career accomplishments are you most proud of?
Dr. Xu: To have built an independent practice under the vision of providing comprehensive care in a system with well-established neurosurgical and orthopedic presence. The ongoing development of the neurosciences service line to best serve the needs of the patients. We are, as a practice, an ongoing work in progress. It’s the progress part that keeps it interesting and drives me daily.
CU PM&R training was ideal to prepare me for practice because it was well rounded and comprehensive. The educators were kind and amazing and I will always have fond memories of my time in the program. I am very grateful I was able to be a part of it. -Dr. Jessica McCabe
Dr. McCabe: It’s a pleasure to have the opportunity to work with a friend and respected colleague. Additionally, I have always wanted to be a physician and a mom. The most important accomplishment to me has been finding the balance between practicing medicine and being at home to support my children. This, of course, will always be a moving target.

Do you have any advice for current residents or fellows?
Dr. Xu: Get to know yourself. Believe in your strengths, build upon your weaknesses. Everyone will have a different approach to practicing medicine. Watch, learn, and take from the mentors that you come across during training as best as you can but don’t replicate them; cultivate your own approach to practicing medicine.
Dr. McCabe: Yes, of course. I think it is so important to develop relationships with your colleagues. Everyone has different strengths and weaknesses, and we can all learn from one another, so we become the best versions of ourselves in our careers. Also, you never know who you might go into practice with!
What do you enjoy doing in your personal time?
Dr. Xu: Spending quality time with my family. Traveling is a passion of mine. I also golf in my free time, snowboard when I can (not much snow in Georgia so we make do with trips to Colorado and Canada), Formula 1 (I try to attend at least 1 race a year), USC football, and cooking for friends and family.
Dr. McCabe: I have a 6, 4, and 1 year old so much of my personal time is spent focusing on the growth and development of my children. I love being a mom. For now, we do a lot of beach trips. I also love running, hiking, biking and really doing anything active with friends and family.
The CU Department of Physical Medicine and Rehabilitation is fortunate to be supported by a phenomenal group of administrative staff, a team which has grown to eleven members over the last couple of years. This team is led by Lauren Collins, MHA, vice chair of finance and administration. Lauren has worked in this role since July of 2017.
Kelly Batory and Amie Taft provide the core administrative support to PM&R Faculty. Kelly Batory, serves as office manager, providing executive support to Lauren Collins and the department chair, Dr. Venu Akuthota in addition to managing many human resources functions in the department such as faculty promotions and leave reporting. Amie Taft serves as administrative assistant, supporting faculty with reimbursements, travel, supply ordering, scheduling, med legal and plans all department events.
Clinical finance and operations is overseen by Rebecca Holmberg, MBA, who is supported by finance coordinator Kevin Hallman, MA. Rebecca and Kevin manage funds flow with hospital partners, revenue cycle, faculty productivity reports, clinical contracts, and budgeting for the department.
Shannon Onken is the manager for research services and is supported by Samina Hamidi and Linh Nguyen. This group assists Principal Investigators (PIs) with administration and management of research grants and contracts, as well as applicable finance and procurement policies and processes. They are primarily responsible for managing all sponsored project activity within PM&R to ensure compliance with all Federal, State, Sponsor and University policies and procedures. Shannon and team work closely with the School of Medicine Pre-Award Shared Services group and CU Office of Grants and Contracts.
Academic services for the PM&R residency and fellowship programs are led by Mallory Pridy, who is supported by Morgan Mestas. Mallory works with residents to provide academic advising and counseling, personnel administration, recruitment and admissions, faculty affairs, library services, and curriculum administration. Morgan provides these services to the Pediatric Rehabilitation Fellowship and serves as back-up to Mallory for residency functions.
Finally, Zachary Noriega, MPA, serves as our communication program manager and provides oversight of PM&R and Physical Therapy internal and external communications, website design and content


Zachary Noriega is an avid road tripper and has transversed the entire lower 48 by car!
Lauren Collins was a Division III collegiate golfer and holds the DePauw Women’s Golf school record for low round - 69!


Kevin Hallman took up wrestling and speed skating in eighth grade and was horrible at both.
Amie Taft loves paddleboarding and golfing. Growing up, she participated in roller blading while doing the limbo and became the winner several times!


Rebecca Holmberg was born and raised in Colorado but didn’t learn to ski until halfway through college!
Samina Hamidi has performed live, and is on an artist’s CD for her poetry and spoken word!


Kelly Batory and her husband won a trip to New York to see Super Bowl XLVIII in 2014 between the Broncos and Seahawks, including transportation to the game. They played at MetLife Stadium in New Jersey, and afterwards, on a private yacht, they got to shake hands with Archie Manning!
Shannon Onken has ridden in a Black Hawk military helicopter from Denver to Trinidad, and back!


Mallory Pridy is a river enthusiast who paddleboards and surfs river waves. She has also completed two self-supported rafting trips down the Grand Canyon!
Linh Nguyen’s family has a birthday bonanza every February. It’s a three-day celebration marathon with birthdays on Feb 3rd, 4th, and 5th. Talk about keeping the cake and candles busy!

Morgan Mestas is a mother of 4 children who are all named after some awesome people (oldest to youngest):
• Alex was named after his father because in our family that’s who you name your 1st born son after. Super special and it’s a great name!

• Logan was named after Wolverine from X-Men because aside from Jean Grey, he’s one of the best X-Men EVER!
• Liam was named after Liam Neeson because not only is it a cool name, but Liam Neeson’s movies and acting skills are nothing short of AMAZING!
• Payton was named after my husband’s favorite football player, Walter Payton (nickname: “Sweetness”). When I was 8 months pregnant, the Broncos signed Peyton Manning, so everyone assumed she was named after him, but nope!
• Not only that, but her and her husband both thought of the same names for each of their children before they even told each other what they were thinking!
On the evening of October 6, 2023, the CU Physical Therapy Program celebrated its 75th Anniversary at the new Anschutz Health and Sciences Building. Over 150 attendees, including faculty, staff, current students, alumni, campus leadership, benefactors, clinical partners, friends of the program, and their guests, were in attendance. The evening started with a cocktail reception in the second-floor atrium, followed by a formal program in the Donald M. Elliman Conference Center.
The programming started with a comedic skit by CU Physical Therapy program director and associate dean of physical therapy education Michael Harris Love, PT, MPT, DSc, FGSA, FAPTA, and co-president of the CU Physical Therapy Alumni Association and Super Bowl 50 Champion David Bruton, PT, DPT ‘21. Following this skit, Joanna Roybal, PT, DPT ‘10, co-president of the CU Physical Therapy Alumni Association, and Margie O’Rourke, alumni relations manager, presented to the alumni in the audience on ways they could get involved with the association.

Retired faculty member of the CU Physical Therapy Program, and president of the CU PT History Committee Sharon Jordan, PT, MA, and communication program manager for the Department of Physical Medicine and Rehabilitation Zachary Noriega, MPA, debuted a 12-minute documentary capturing the history of the CU Physical Therapy Program over the last 75 years. Afterwards, Venu Akuthota, MD, chair of the Department of Physical Medicine and Rehabilitation, and John J. Reilly, Jr., MD, dean of the CU School of Medicine introduced executive vice chancellor for academic and student affairs Roderick Nairn, PhD, who received the Mary S. Lawrence Award, which is given to university employees or other academic partners who have provided sustained, meaningful contributions to the program. Award recipients demonstrate dedication to the program by promoting the CU PT vision, mission, and goals.
After the presentation of the Lawrence Award, current CU Physical Therapy students Angela Delos Santos, Blake Vanderploeg, Aryssara Bryndzia, and Makayla Callender introduced the “Friends of the Program” video. People across the physical therapy community sent in home videos congratulating CU PT on this milestone anniversary. Following this video, Jennifer Stevens-Lapsley, PT, PhD, FAPTA, director of the Rehabilitation Science PhD Program and section director of research and development, gave an update to the audience on research within the program, and Jennifer Rodriguez, PT, DPT, MHS, director of clinical education gave an update on the state of clinical education in the program. Dr. Rodriguez is retiring in 2024 and was surprised by the Clinical Education Team with a special acknowledgement as the longest serving director of clinical education in the country (28 years!)
After Dr. Rodriguez’s special acknowledgement, Andrew Smith, PT, DPT, PhD, associate professor of Physical Medicine and Rehabilitation, and current PhD student and practicing physical therapist at Craig Hospital, Wesley Thornton, PT, DPT, NCS, PhD(c), introduced the keynote speaker, Jandel Allen-Davis, MD, President and CEO of Craig Hospital, who gave a compelling speech to the audience on the importance of compassion in the field of physical therapy, and acknowledging the many CU Physical Therapy graduates who now work at Craig Hospital. Following the keynote address, Travis Leiker, MPA, senior director of development, and Karen Aarestad, PhD, MBA, assistant vice chancellor of Advancement, acknowledged the benefactors in the audience, and introduced the new president of the Philanthropy and Advisory Council, Martha Schram, PT ‘73. Dr. Harris-Love concluded the programming with closing remarks about how his family’s story motivated him to pursue a career in the physical therapy field.

The CU Physical Therapy Program is grateful to everyone who attended the festivities, and everyone who has contributed to making us one of the top physical therapy programs in the country throughout our history. From our humble beginnings in the late1940’s as a small cohort of six students tucked away at the back of the Department of Physical Medicine and Rehabilitation, the program has grown tremendously in the last 75 to include over 220 students, millions of dollars in research funding, partnerships with over 500 clinical sites, expansion to hybrid learning in partnership with UCCS, and a dual DPT-MPH degree with the Colorado School of Public Health. We are proud of all we have built together and look forward to the next 75 years!
The American Academy of Physical Medicine & Rehabilitation (AAPM&R) hosted it’s 2023 Annual Assembly in New Orleans, Louisiana November 15th-19th. The University of Colorado was well represented by our residency alumni, and current faculty and residents. Drs. Rachel Brakke-Holman and Scott Laker both serve on the AAPM&R Board.
The Rehabilitation Services Volunteer Project (RSVP), spearheaded by Drs. William Niehaus, Jeff Berliner, Deanna Claus among others, expanded from Texas into Colorado and Georgia. RSVP is an all-volunteer, non-profit organization that provides rehabilitation services and durable medical equipment to uninsured and underinsured individuals with disabilities that lack access to the services that PM&R provides. The RSVP group received a well-deserved award at AAPM&R.
Our current trainees delivered excellent presentations during the assembly. Dr. Amanda Appel gave a seminar during AAPM&R’s Pediatrics Day Pre-Course on sexual health. People who attended said she was “incredible” and did a great job explaining the role of rehabilitation medicine providers in being intentional with education, communication, and providing anticipatory guidance to patients, families, and support systems about this topic. Dr. Christian Nicolosi presented his study about “Low Back Pain During Pregnancy: Documentation and Referral Patterns at a Tertiary Care Center.” Dr. Zach Abbott presented about “Considering New Diagnostic Criteria: Diffuse Idiopathic Skeletal Hyperostosis.” Drs. Louis Nikolis and Andrea Nikolis presented a case study on “Hemidiaphragm Paralysis Following Interscalene Nerve Block.” Dr. Andrea Nikolis also presented a poster entitled “Prolonged Rehabilitation from COVID-19 Due to Multiple Neurologic Hits: A Case Report” with future resident Dr. Jeff Kepple. Finally, Dr. Megan Machek presented on “Rehabilitation of Severe Traumatic Brain Injury Complicated by Obtained Panhypopituitarism, Stress Dose Steroids Causing Central Diabetes Insipidus.”
The Assembly was concluded by the CU PM&R reception at the Hilton Riverside. Over 30 alumni, residents, faculty members, and current medical students from various institutions interested in our program attended the reception to celebrate the end of a successful conference. We look forward to celebrating next year’s AAPM&R in sunny San Diego, California November 6th-10th, 2024!

Michael Bade, PT, DPT, PhD, OCS, FAAOMPT received a three-year R21 award totaling $400k for his project titled: “Swelling Management after Total Knee Arthroplasty.” He also received the CU PM&R Professionalism Award.
David Baker, PsyD, ABPP-CN was promoted to associate clinical professor of PM&R.
Michael Blei, MD received the Career Service Award from Denver Health.
Lisa Brenner, PhD, ABPP and team published a seminal article on veteran suicide rate. She also became the first female chair and CEO of the International Brain Injury Association. She also led a team on developing community strategies to reduce suicide among veterans in Guam and other US territories. She and her team also published in JAMA on Associations of Military-Related Traumatic Brain Injury With New-Onset Mental Health Conditions and Suicide Risk. She along with Nazanin Bahraini, PhD, Adam Kinney, PhD, and Ryan Holliday, PhD were the recipients of the VA Office of Research & Development – Rehabilitation Research & Development award.
Alison Colbert, PhD was elected President of the American Psychological Association’s Rehabilitation Psychology Division’s Pediatric Section. She also, along with Ann Lantagne, PhD were awarded a community grant through Mindsource.
Bryann DeBeer, PhD received notification of renewed funding for the VA Patient Safety Center of Inquiry-Suicide Prevention Collaborative (through 2026).
Michael Harris Love, PT, MPT, DSc, FGSA, FAPTA delivered a presentation at the UCF Institute of Exercise Physiology and Rehabilitation Sciences, “The Utility of Muscle Texture Analysis to Assess Muscle Health in Older Adults.” He also received the Champion of Allied Health Award from the Mayo Clinic Health Sciences Alumni Association. He was also a panelist for the fourth Lynda D. Woodruff Lecture on Diversity, Equity, and Inclusion in Physical Therapy.
Meghan Hernandez, PT, DPT, PCS was admitted to the 2023 cohort for the APTA Grant Writing & Mentoring in Education Research Workshop.
Claire Hoffmire, PhD served as co-chair for the VA Woman Veteran Suicide Research workgroup.
Holly Ingham, PT, DPT, ATP became a Board-Certified Pediatric Specialist.
Adam Kinney, PhD, along with Nazanin Bahraini, PhD presented at the 14th World Congress on Brain Injury in Dublin, Ireland.
Toby Kinney, PT, DPT, OCS, FAAOMPT, MBA, PhD was promoted to assistant professor. He also completed his PhD program.
Michael Kirkwood, PhD, ABPP-CN received the CU PM&R Professionalism Award.
Wendy Kriekels, PT, DPT, NCS was selected to serve on the Academy of Neurologic Physical Therapy’s Movement System - Balance Diagnoses Knowledge Translation Taskforce.
Susan Ladley, MD garnered a recognition medal by Chancellor Elliman for 25 years of service to the University of Colorado.

Scott Laker, MD was promoted to professor of PM&R.
Amy McDevitt PT, DPT, PhD, OCS, FAAOMPT completed her PhD Program.
Ann Lantagne, PhD won the Children’s Hospital Psychology Mentoring Award.
Daniel Malone, PT, PhD, CCS was named the CU DPT Hybrid Pathway program director.
Adele Meron, MD presented her project for the University of Colorado Academy of Medical Educator’s Teaching Scholars Program (TSP) graduation entitled “A Novel Cultural Competency Curriculum for Physical Medicine and Rehabilitation Residents.”
William Niehaus, MD became the host of the American Congress of Rehabilitation Medicine Rehab Cast podcast. He was also promoted to associate professor of PM&R. He was also invited to address Admiral Rachel L. Levine, MD, assistant secretary for health for the U.S. Department of Health and Human Services on long COVID. He, along with Jeffrey Berliner, DO and Chief Resident Deanna Claus, MD steer the Rehabilitation Services Volunteer Project which received an award at AAPM&R.
Nathan Odom, MD became CU PM&R’s first Director of Quality.
Joyce Oleszek, MD, along with Michael Dichiaro, MD and Aaron Powell, MD were all named top performers at Children’s Hospital Colorado by their patients and their families and received outstanding ratings on the Patient-Family Experience survey for the care they provide patients on the inpatient unit.
Joe Palmer, PT, DPT, PhD was named CU PT director of clinical education upon Jenny Rodrigeuz’s retirement. He also completed his PhD program.
Katherine Payne, MD was promoted to associate professor of clinical PM&R.
Robin Peterson PhD, ABPP won the Journal of Speech, Language, and Hearing Research 2022 Editor’s Award.
Jenny Rodriguez, PT, DPT, MHS received the Award for Leadership in Education - the highest honor given by the APTA Academy of Education. The award recognizes a nationally prominent educator who has exhibited outstanding leadership and contributions to the field. She also received the Cerasoli Award for Outstanding Contributions to Physical Therapy Education and the CU PT Excellence in Teaching Award.
Joseph Rosenthal, MD was promoted to associate professor of PM&R.
Cristina Sarmiento, MD was selected into the Clinical Faculty Scholars Program for 2023-2025 Cohort at the Colorado Clinical and Translational Sciences Institute. She was the first CU PM&R faculty member to be selected into this competitive program. She was also a finalist for two awards at the AACPDM meeting this week in Chicago: Promising Career Award and Best Adult Paper. She, along with Jordan Wyrwa, DO were both accepted into the Training in Grantsmanship for Rehabilitation Research (TIGRR) workshop. She also received a 2023 Cerebral Palsy Research Network Accelerator Award for her project “Priority Setting for Multicenter Research Among Adults with Cerebral Palsy,” and a $250,000 award from the Tai Foundation in support of early career investigators, for her project titled: “Closing the Gap: Developing a Patient- and Family-Centered Transition Process for Young Adults with Cerebral Palsy and Other Neuromuscular Conditions.” She also received the Cerebral Palsy Alliance Research Foundation grant for her project titled: “Screening and Classifying Pain in Adults with Cerebral Palsy Across Centers.”
Tess Simpson, PhD attended the Spina Bifida World Congress, where she gave an oral presentation, presented data at the preconference CDC National Spina Bifida Patient Registry (NSBPR) meeting, moderated a session, and participated in the self-management research working group meeting. She was also promoted to associate professor of PM&R.
Eric Sawyer, PT, DPT, OCS, STC, CFEI© was promoted to assistant professor. He was also named assistant director of clinical education for the Hybrid DPT Pathway at UCCS.
Andrew Smith, PT, DPT, PhD was promoted to associate professor of PM&R.
Jennifer Stevens-Lapsley, PT, PhD, FAPTA was part of the team of APTA thought leaders in the profession of physical therapy who assembled the Research Agenda for Physical Therapy from the American Physical Therapy Association. She was also NIH Grant Awarded for the Training in Grantsmanship for Rehabilitation Research.
Anne Stratton, MD presented 5 talks at the Cure SMA annual meeting.
Maryam Tahmasbi Sohi, MD serves as our Medical Director of the SCI/D ALS program, which was recognized at the ALS Association Mountain States Chapter Gala with the 2023 Excellence in Care Award.

Sarah Tlustos-Carter, PhD, along with Kilby Mann, MD received a grant from the IHQSE Clinical Effectiveness & Patient Safety Grant Program.
Kristin Uhler, PhD was awarded an NIH RO1 grant on “The impact of auditory access on the development of speech perception.” She was also named a top cited article author in Infancy Journal. She also presented at an important international audiology forum in Cologne, Germany.
Pam Wilson, MD was the silver medal winner at World Doubles Wheelchair Curling Championships. She also received the Wheelchair Athlete of the Year Award from USA Curling.
Jordan Wyrwa, DO received the CU PM&R Pilot Grant for his project titled: “Computable Phenotyping of Pediatric Rehabilitation Population.”
Gaffney BMM, Davis-Wilson HC, Christiansen CL, Awad ME, Lev G, Tracy J, Stoneback JW. Osseointegrated prostheses improve balance and balance confidence in individuals with unilateral transfemoral limb loss. Gait Posture. 2023 Feb;100:132-138. doi: 10.1016/j.gaitpost.2022.12.011. Epub 2022 Dec 13. PMID: 36521257.
Peterson AL, Blount TH, Foa EB, Brown LA, McLean CP, Mintz J, Schobitz RP, DeBeer BR, Mignogna J, Fina BA, Evans WR, Synett S, Hall-Clark BN, Rentz TO, Schrader C, Yarvis JS, Dondanville KA, Hansen H, Jacoby VM, Lara-Ruiz J, Straud CL, Hale WJ, Shah D, Koch LM, Gerwell KM, Young-McCaughan S, Litz BT, Meyer EC, Blankenship AE, Williamson DE, Roache JD, Javors MA, Sharrieff AM, Niles BL, Keane TM; Consortium to Alleviate PTSD. Massed vs Intensive Outpatient Prolonged Exposure for Combat-Related Posttraumatic Stress Disorder: A Randomized Clinical Trial. JAMA Netw Open. 2023 Jan 3;6(1):e2249422. doi: 10.1001/jamanetworkopen.2022.49422. PMID: 36602803; PMCID: PMC9856757.

Brenner LA, Forster JE, Walsh CG, Stearns-Yoder KA, Larson MJ, Hostetter TA, Hoffmire CA, Gradus JL, Adams RS. Trends in suicide rates by race and ethnicity among members of the United States Army. PLoS One. 2023 Jan 17;18(1):e0280217. doi: 10.1371/journal.pone.0280217. PMID: 36649302; PMCID: PMC9844903.
Connery AK. Let’s Stop Complaining That Early Childhood Assessments Do Not Predict IQ. JAMA Pediatr. Published online March 13, 2023. doi:10.1001/jamapediatrics.2023.0031
Garbin AJ, Stevens-Lapsley JE, Gritz RM, Tucker CA, Bade MJ. Long-Term Career Earnings in Academia Might Offset the Opportunity Cost of Full-Time PhD and Postdoctoral Education for Physical Therapists Who Hold a Doctor of Physical Therapy Degree. Phys Ther. 2023 Apr 4;103(4):pzad015. doi: 10.1093/ptj/pzad015. PMID: 37128811; PMCID: PMC10152085.
Stevens-Lapsley JE, Derlein D, Churchill L, Falvey JR, Nordon-Craft A, Sullivan WJ, Forster JE, Stutzbach JA, Butera KA, Burke RE, Mangione KK. High-intensity home health physical therapy among older adult Veterans: A randomized controlled trial. J Am Geriatr Soc. 2023 May 24. doi: 10.1111/jgs.18413. Epub ahead of print. PMID: 37224397.
Brenner LA, Forster JE, Gradus JL, Hostetter TA, Hoffmire CA, Walsh CG, Larson MJ, Stearns-Yoder KA, Adams RS. Associations of Military-Related Traumatic Brain Injury With New-Onset Mental Health Conditions and Suicide Risk. JAMA Netw Open. 2023 Jul 3;6(7):e2326296. doi: 10.1001/jamanetworkopen.2023.26296. PMID: 37523186; PMCID: PMC10391302.
Sarmiento CA, Wyrwa JM, Chambliss AV, Stearns-Yoder KA, Hoffberg AS, Appel A, Brenner BO, Brenner LA Developmental Outcomes Following Abusive Head Trauma in Infancy: A Systematic Review. J Head Trauma Rehabil. 2023 Jul-Aug 01;38(4):283-293. doi: 10.1097/HTR.0000000000000808. Epub 2022 Oct 21. PMID: 36730957.
Stevens-Lapsley J, Hicks GE, Zimney K, Slaven EJ, Manal TJ, Jeffries LM. Research Agenda for Physical Therapy from the American Physical Therapy Association. Phys Ther. 2023 Sep 15:pzad126. doi: 10.1093/ptj/pzad126. Epub ahead of print. PMID: 37712887.
Sarmiento CA, Gannotti ME, Gross PH, Thorpe DE, Hurvitz EA, Noritz GH, Horn SD, Msall ME, Chambers HG, Krach LE. Adults with cerebral palsy and chronic pain experience: A cross-sectional analysis of patient-reported outcomes from a novel North American registry. Disabil Health J. 2023 Nov 13:101546. doi: 10.1016/j.dhjo.2023.101546. Epub ahead of print. PMID: 37993325.
Morris, M. A., Sarmiento, C., & Eberle, K. (2023). Documentation of Disability Status and Accommodation Needs in the Electronic Health Record: A Qualitative Study of Health Care Organizations’ Current Practices. The Joint Commission Journal on Quality and Patient Safety. https://www.sciencedirect.com/science/article/abs/pii/ S1553725023002507?via%3Dihub
Judd DL, Cheuy V, Peters A, Graber J, Hinrichs-Kinney L, Forster JE, Christiansen CL, Stevens-Lapsley JE Incorporating Functional Strength Integration Techniques during Total Hip Arthroplasty Rehabilitation: A Randomized Controlled Trial. Phys Ther. 2023 Dec 15:pzad168. doi: 10.1093/ptj/pzad168. Epub ahead of print. PMID: 38102757.
Hoisington AJ, Stamper CE, Stearns-Yoder KA, Haghighi F, Lowry CA, Brenner LA. A cross-sectional study of correlations among blood-based biomarkers for intestinal permeability: A pilot study of United States veterans with posttraumatic stress disorder symptoms. Brain Behav Immun Health. 2023 Nov 10;34:100702. doi: 10.1016/j. bbih.2023.100702. PMID: 38073767; PMCID: PMC10709025.

Claus D, Draganich C, Berliner J, Niehaus W, Berliner J, Magnusson D, Smith AC. Needs of an uninsured equitydeserving minority patient cohort with physical disabilities during the first wave of the COVID-19 pandemic. Front Rehabil Sci. 2023 Feb 17;4:1000838. doi: 10.3389/fresc.2023.1000838. PMID: 36873817; PMCID: PMC9981779.
Draganich C, Park A, Sevigny M, Charlifue S, Coons D, Makley M, Alvarez R, Fenton J, Berliner J. Venous Thromboembolism: Exploring Incidence and Utility of Screening in Individuals With Brain Injury. Arch Phys Med Rehabil. 2023 Feb 1:S0003-9993(23)00087-4. doi: 10.1016/j.apmr.2023.01.012. Epub ahead of print. PMID: 36736807.
Meron A, Barber K, Stokes D, Churchill L, LeDoux C, Akuthota V. Feasibility and acceptability of a telemedicine triage model among Medicaid patients with low back pain referred to a spine center. N Am Spine Soc J. 2023 Feb 10;14:100200. doi: 10.1016/j.xnsj.2023.100200. PMID: 37008515; PMCID: PMC10050782.
Thornton WA, Marzloff G, Ryder S, Best A, Rasheed K, Coons D, Smith AC. The presence or absence of midsagittal tissue bridges and walking: a retrospective cohort study in spinal cord injury. Spinal Cord. 2023 Apr 29. doi: 10.1038/ s41393-023-00890-6. Epub ahead of print. PMID: 37120699.
Brostow DP, Donovan M, Penzenik M, Stamper CE, Spark T, Lowry CA, Ishaq SL, Hoisington AJ, Brenner LA. Food desert residence has limited impact on veteran fecal microbiome composition: a U.S. Veteran Microbiome Project study. mSystems. 2023 Oct 24:e0071723. doi: 10.1128/msystems.00717-23. Epub ahead of print. PMID: 37874170.
Monteith LL, Kittel J, Miller C, Schneider AL, Holliday R, Gaeddert LA, Spark T, Brenner LA, Hoffmire CA. Identifying U.S. regions with the highest suicide rates and examining differences in suicide methods among Asian American, Native Hawaiian, and Pacific Islander Veterans. Asian J Psychiatr. 2023 Nov;89:103797. doi: 10.1016/j.ajp.2023.103797. Epub 2023 Oct 6. PMID: 37847965.
For a full list of our PM&R publications, please use the QR code to visit our website: https://medschool.cuanschutz.edu/physical-medicine-and-rehabilitation/news-and-media/publications