





Produced by The University of Colorado | Department of Orthopedics
Feature writing and editorial design by Tara Bisel
Proofreading by Ellen Rhodes
Data compiled by:
Nicole Aviles
Patrick Carry
Kathy Dwyer-Clonts
Katie Dean
Venkatesh Gaallee
Tommy Hoong
Jennafer Hoyland
Carolyn Jones
Lindsey Renn
Charesa Zahlen
Michael Zuscik
Photography by Photography G where noted
Copyright 2024
Special thanks to:
Josh and Melissa Bryan
Sasha Klepitskaya
Alan Shafner and The Department of Orthopedics Faculty
Additional thanks to all Orthopedics Administrative Staff for their hard work and dedication to the department and the University of Colorado School of Medicine










“
Be present, have compassion, treat your patients with respect and dignity, and be an advocate for the less privileged in this world.
EvalinaBurger,
MD Professor and Chair
Robert D’Ambrosia Endowed Chair of Orthopedics

Greetings,
I am pleased to highlight and celebrate the remarkable achievements of our Orthopedic Department over the past 12 months Despite ongoing challenges impacting the way we practice including changing legislation, our dedication and hard work have led to significant accomplishments that have positively impacted our patients and the healthcare community.
One of the standout achievements of the past year has been our focus on enhancing patient care and outcomes through the implementation of innovative treatment approaches. From adopting minimally invasive surgical techniques to utilizing cutting-edge orthopedic technologies, we have consistently strived to provide the highest quality of care to all our patients
There are too many to name and this annual report will highlight but a few of our new and outstanding programs. Furthermore, our department has played a pivotal role in advancing orthopedic research and education. Our team members have actively participated in research projects, published groundbreaking studies, and shared their expertise through various educational initiatives. These efforts have not only expanded our knowledge base but have also contributed to the advancement of orthopedic practices on a broader scale Many faculty won outstanding research awards and we are ranking #11 on the Blue Ridge Ranking for NIH funding.
Additionally, I must commend our entire team for their unwavering commitment to continuous improvement and excellence. Through ongoing professional development, training programs, and collaborative initiatives, we have fostered a culture of learning and innovation that has propelled our department to new heights.
As we reflect on the achievements of the past year, I am filled with pride and gratitude for each and every member of our orthopedic team. Your dedication, skills, and passion for orthopedic care have been instrumental in our success, and I am confident that together, we will continue to achieve even greater milestones in the future.
Thank you for your outstanding contributions and unwavering commitment to excellence. Your hard work does not go unnoticed, and I look forward to another year of shared successes and accomplishments
Onward in good health,
 Evalina Burger, MD
Evalina Burger, MD
Providing the highest quality patient care, and advancing the field of orthopedics through innovation in research and education

To be the best place for orthopedic care in our community and worldwide, and the most trusted source for musculoskeletal research and education
We set and continually elevate the bar for excellence in patient care, education and research.
We stay sharp to employ new technologies, tackle new challenges in an ever evolving healthcare landscape, and educate the next generation of leaders in orthopedics.
We actively champion a diverse, equitable, and inclusive environmentempowering unique perspectives and cultivating spaces where everyone belongs.
We value the diverse skillsets of our practitioners and staff, encouraging collaboration to ensure superior and holistic patient care, and the highest distinction in education and research.
We foster an environment where new ideas lead to breakthrough changes in healthcare, advancing the science of orthopedics for continuously improving patient care.
We honor the trust our patients and their families bestow to us, and treat them as we would our own loved ones with the best possible care.
We conscientiously and ethically manage all resources entrusted to us.
We hold ourselves accountable to the highest ethical and behavioral standards - committed to integrity, respect, and kindness in our interactions with everyone.
T I E N
P A

238,781
TOTAL OUTPATIENT VISITS

60,064 NEW PATIENT VISITS

20,216 SURGICAL CASES
T I O N
U C A
T C A R E E D
5TH MOST SEARCHED ORTHOPEDIC RESIDENCY PROGRAM
The FREIDA database--the Fellowship and Residency Electronic Interactive Database Access-allows medical students to search through more than 13,000 residency and fellowship programs accredited by the Accreditation Council for Graduate Medical Education.
In 2022, orthopedic surgery residency programs on the platform received over 98,000 views cumulatively, with the University of Colorado ranking fifth in the top ten.

$37M SPONSORED RESEARCH PORTFOLIO #11 in NIH funding
$7M CY2023 GRANT SUPPORTED RESEARCH ACTIVITY
from the Blue Ridge Institute for Medical Research
162
53 PEERREVIEWED PUBLICATONS
151
46 NEW AWARDS FUNDED RESEARCH STUDIES ACTIVE CLINICAL TRIALS
COHORT
1042
ALL LEARNERS
BOARD PASS RATE 5 years running 100%
Our faculty are leaders in their fields in every way. As internationally recognized innovators in research and every sub-specialty of orthopedic clinical care, they have chosen the University of Colorado for its transformative impact on medicine to solve the world’s toughest health challenges. This University is a better place because they did.
We also tackle challenges endemic to the field of orthopedics -- specifically, gender equity. CU Orthopedics leadership strives to recruit the most qualified faculty who represent the department’s diverse patient base, creating an inclusive experience for our patients and clinical trial participants. While we have made great strides in this area, we recognize we still have work to do, and as with every challenge we face we welcome it and we will rise to it. Clinicians. Researchers. Educators. Mentors.

CU Orthopedics exceeds this mark in every faculty category, with 5X the number of female surgeons as the national average.



Catalano,

8 TOP DOCTORS
recognized by their peers for 5280 Magazine





T. Jay Kleeman, MD
Professor Foot & Ankle

CU Orthopedics physicians continue to attract media attention for their world-class care. Our doctors are consistently recognized by patients and peers alike. 2023 was no exception.
Michelle Wolcott, MD Associate Professor Sports Medicine Jason Dragoo, MD Professor Sports Medicine Sumeet Garg, MD Associate Professor Pediatric Orthopedics Louis MD Professor Hand, Wrist & Elbow Sayan De, MD Assistant Professor Pediatric Orthopedics Mark Erickson, MD Professor Pediatric Orthopedics Martin Boublik, MD Professor Sports Medicine AssistantMichael Dayton, MD

Professor
Vice Chair | Education
Jason Dragoo, MD
Professor
Louis Catalano, MD
Han

CJ Kleck, MD
Associate Professor
Section Chief | Spine

Vikas Patel, MD
Professor Executive Vice Chair

Craig Hogan, MD
Vice Chair | Academic Affairs

Fraser Leversedge, MD
Professor
Section Chief | Hand, Wrist & Elbow

Jason Stoneback, MD
Associate Professor
Vice Chair | Clinical Affairs
Section Chief | Trauma & Fracture


Kenneth Hunt, MD
Associate Professor
Section Chief | Adult Reconstruction
Associate Professor
Vice Chair | Quality, Patient Safety and Outcomes
Section Chief | Foot & Ankle

Bennie Lindeque, MD
Professor
Section Chief | Muskuloskeletal Oncology

Klane White, MD
Professor
Vice Chair | Pediatric Orthopedics
Section Chief | Pediatric Orthopedics
Eric McCarty, MD
Professor
Section Chief | Sports Medicine


Michael Zuscik, PhD
Professor Vice Chair | Research


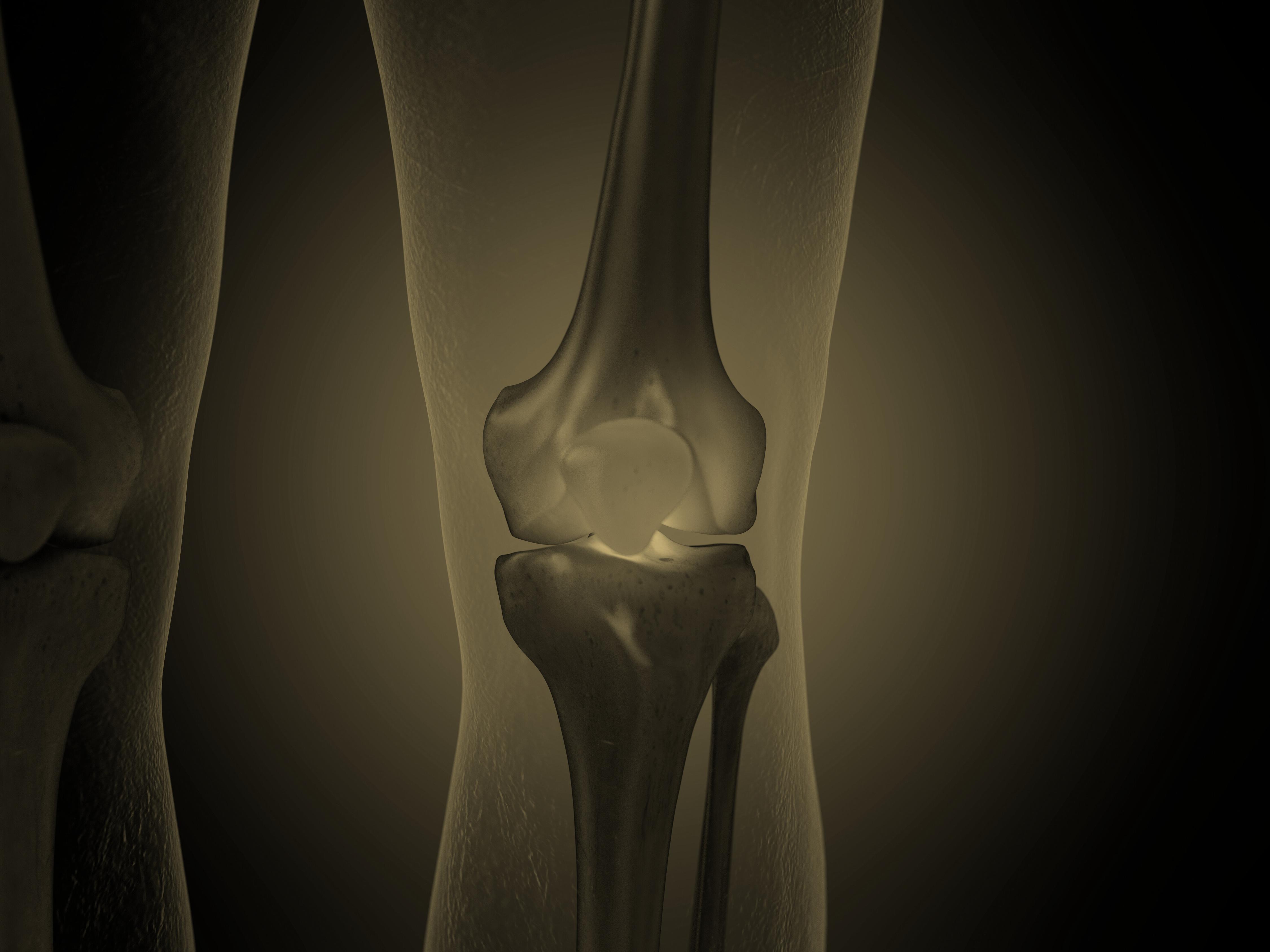
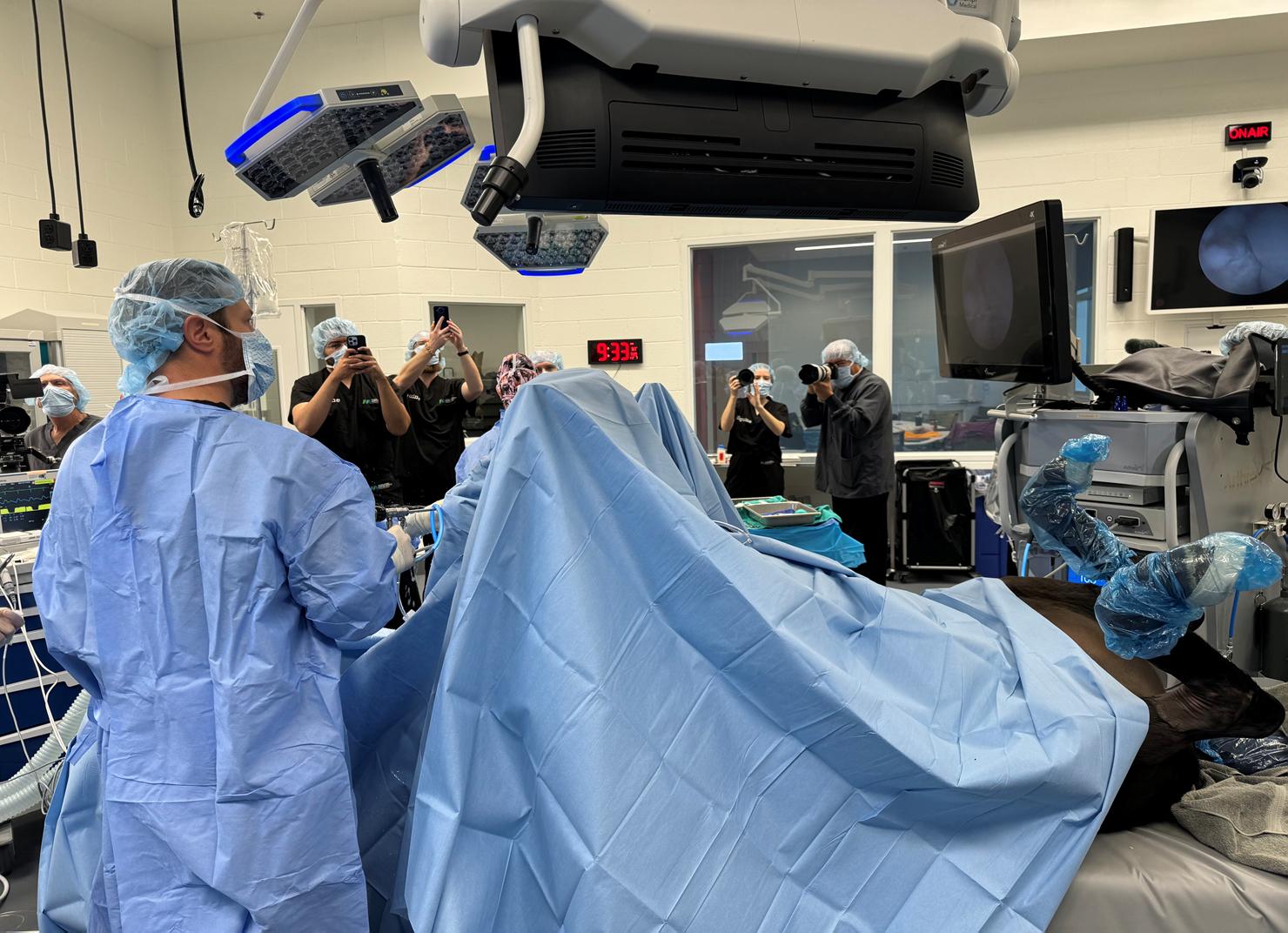
Under the direction of Dr. Ryan Koonce, our Highlands Ranch Hospital has started its robotic assisted surgery program.
Robotic surgery, also known as robot-assisted surgery, is a method of surgery that allows doctors to plan for and perform complex surgical procedures with greater precision, control, and flexibility.
This sophisticated tool is operated entirely by the surgeon, combining technology with long-standing knee replacement principles to achieve a more reproducible knee replacement.

The robotic system works by identifying anatomical landmarks inside the knee joint and tensioning soft tissues at different knee angles. This allows the surgeon to quantify angles and soft tissue tension during surgery to a level that is not available with standard instrumentation.

The system used at Highlands Ranch Hospital does not require a preoperative CT scan or MRI like other knee robotic systems, saving one preoperative task for the patients.
The benefits of robotic knee replacement are currently under investigation, but studies have shown an easier early recovery as well as more precision and accuracy of component placement.
“We are very excited to be offering this technology to patients in the Denver Metro area. We pride ourselves on discussing the benefits and the pros and cons of robotics and how it can be utilized in hip and knee replacement.
Ryan Koonce, MD Assistant Professor
The section of Adult Reconstruction continues to push the advances of hip and knee replacement with minimally invasive surgery and rapid mobilization protocols. The same protocol is used at our four different academic hospital locations with great success.
Over the last year we continue to advance our same day surgery discharge program with now over 50% of our primary hip and knee replacements going home the same day. Of the procedures we have planned for same day discharge, we are at a >90% success rate getting patients home the same day.

Over 50% and knee replacement patients returned home the same day of primary hip
CU Orthopedics new multidisciplinary Periprosthetic Joint Infection (PJI) team oversees a highly specialized center for chronic PJI and annually see over 150 PJI cases, servicing the surrounding 6 states. This unique program provides patients with thorough education, options, and successful surgery.
Our team consists of specialists from multiple fields of medicine including Complex Orthopedic surgery, Orthopedic infectious disease, physical therapy, athletic training, nurse navigation and case management.
150+ from Colorado and PJI cases annually 6 surrounding states
1 million hip and knee replacement surgeries are performed annually in the U.S.
10,000-20,000 patients will develop periprosthetic joint infection (PJI)
We are developing the first of its kind in the nation patient support group for patients with chronic PJI.

2023 was a very productive year for the Section of Foot & Ankle. We are proud to share highlights of our accomplishments in research, education, and clinical care.

46% increase
14 new clinical care faculty
7 Advanced Practice Providers in clinic volume
7 Physicians

2nd year with 2 Foot & Ankle Fellows
We hosted a visiting physician from Egypt for a 3-month Observership as part of our Foot & Ankle International Observership program
11
peer-reviewed publications
17 $256,000 conference abstracts grant support

Sasha Klepitskaya always dreamt of how she would look on her wedding day -- a beautiful white dress, curled hair, and tall high heels on her feet as she elegantly walked down the aisle.
After a terrible accident, she wondered if she would be able to walk again at all.
Working as an English and Drama teacher at a British International School, Sasha called the beautiful and tropical country of Thailand home She lived on the small but lively island of Koh Samui in the south.
“Life in Koh Samui was thrilling - I had a fantastic group of friends with whom I explored the island and went on unforgettable adventures. I lived in a big house with wall-towall windows. I had a spacious porch from which I enjoyed admiring the palm trees and tropical flowers which covered the street in my neighbourhood - pinching myself when realising how lucky I was to live there.”
To prevent flooding during the monsoon season, the house was elevated on stilts fifteen feet in the air. One night, Sasha slipped off the elevated porch and fell fifteen feet to the grass below. As she was falling, Sasha tried to right her position so she would be able to land on her feet. But she didn't quite land evenly and instead hit the ground -- HARD -with the full impact radiating squarely through her right foot.
“I remember hitting my head on the grass and getting the wind knocked out of me. I didn't realise that things were much worse until I tried to stand up and couldn't. I had to crawl all the way around the stilts of my house, up the stairs, and lay down on the porch on my back. I looked at my right foot - it had swelled up like a balloon. I said to myself, ’This isn't good - I need to elevate it.’ Then I lost consciousness.
Fortunately, Sasha’s friends found her soon after and took her to the hospital where her foot was imaged. At first they thought it was a small fracture, until the films were developed. Sasha recalls an audible gasp when the medical team reviewed the images. The injury was severe.
Sasha immediately called her mother. A UCHealth physician at the time, Sasha’s mother called the on-call doctor that night, Dr. Daniel Moon. Dr. Moon offered to connect Sasha with trusted foot and ankle colleagues in Asia, but Sasha decided to fly around the world back to Colorado to be under the care of Dr. Moon. Arrangements were made and Sasha returned to Colorado where she was transported directly from the airport to the hospital to meet him.
Dr. Moon’s diagnosis was fracture dislocations of the 1st 4th and 5th tarsomet metatarsal neck fract shaft fractures.


The next morning, Sasha was in surgery. After eight hours in the operating room, Sasha’s foot was now held together with pins and plates. Dr. Moon used three different orthopedic technique strategies to try to best treat her foot with respect to bony and soft tissue considerations: arthrodesis (fusion) of the unstable 1st TMT, open fixation for the 2nd and 4th metatarsals, and percutaneous pinning for the 3rd metatarsal head & shaft and 5th tarsometatarsal joint.


early postoperative foot with pins, plate fixation, and fusion screws

3 years postoperative healing of foot (AP and lateral views)
Sasha was both shocked and relieved to hear that her injury was among the worst Dr Moon had treated that didn’t end in amputation She knew she had a hard road ahead, but she also knew how fortunate she was. As a very active 26-year old Sasha often felt useless and stuck in her recovery, but she pressed on and got better with each passing week. “Seeing Dr. Moon was probably the highlight of my recovery. He never failed to make me smile, make me feel optimistic and in control, and miraculously, I healed. I went on to run again, even signing up for a half marathon! I was back out doing and coaching gymnastics, hiking in the Philippines, wearing the same shoes as I did before, and some that I had always dreamed of. With my friends and family watching, looking and feeling exactly how I dreamed I would, I walked down the aisle to my husband - white high heels and all.”
“High energy foot trauma can lead to poor results for many patients. I feel fortunate that Sasha was such a motivated patient and has done so well with her foot reconstruction. My surgery helped give her a chance at success, but she deserves the credit for her fantastic functional outcome after a lot of hard work in recovery.
Daniel K. Moon, MD, MS, MBA Assistant Professor
“
Miraculously,
I healed. Dr. Moon gave me a second chance at life as I knew it. He genuinely is the doctor I attribute to saving my foot, to giving me the ability to walk again, and so much more.
Sasha Klepitskaya



For his outstanding work providing foot and ankle care to underserved communities worldwide, Dr. Mark Myerson was presented with the American Academy of Orthopaedic Surgeons (AAOS) 2023
Humanitarian Award by Felix “Buddy” Savoie, III, MD.

“From the very day that I arrived, I felt the need to give back. I was provided with tremendous opportunities here in this country, and very early on, I wanted to give back. As an orthopedic surgeon in this country, many of us are committed to medicine, to good patient care, and to helping others. That's what we do.
Mark Myerson, MDInvolved with humanitarian work since the early 2000's, Dr. Myerson recognized that he felt the most fulfilled professionally on medical mission trips to communities worldwide where access to care is severely limited, if they have care at all. “It is humbling, it is enriching, and it is extraordinarily gratifying,” Myerson says. “When you’re in a situation like that, and you can really change someone's life, you feel blessed as a surgeon. It's an incredible feeling.” With each trip he took, it became apparent to Dr. Myerson that he wanted to do more, and so in 2016, he founded Steps2Walk.
The volunteer organization maintains a dual commitment — to perform life-changing foot and ankle surgeries on individuals in underserved communities around the world— and simultaneously, to educate surgeons in those regions.
Steps2Walk also provides opportunities for residents and fellows at the CU School of Medicine to participate in mission trips with the organization, and to work with Dr. Myerson on research projects on the CU Anschutz Medical Campus.
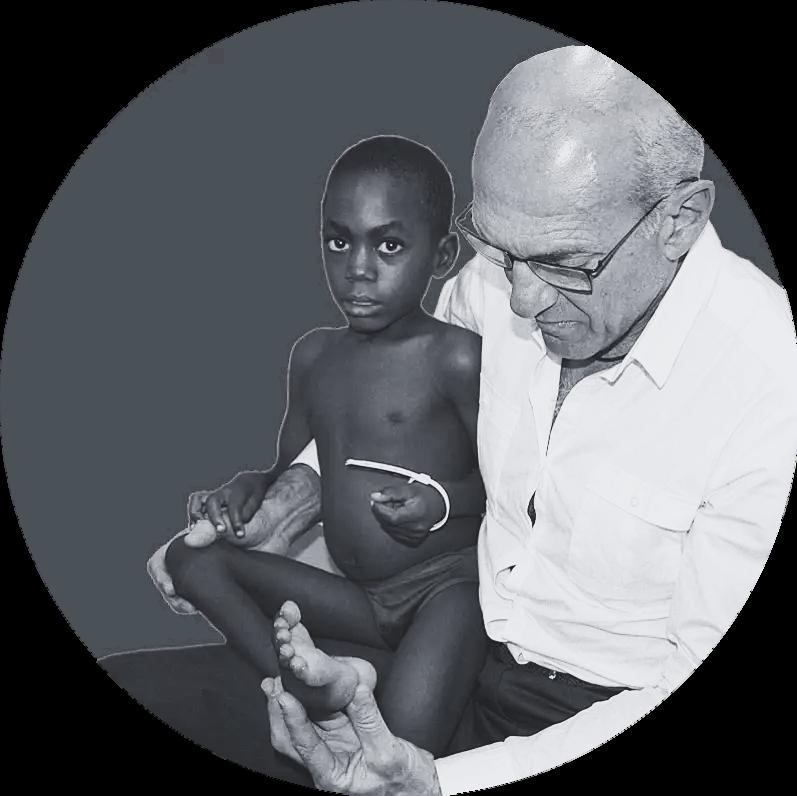
DONATE TO Steps2Walk
To date, Steps2Walk has performed more than 1,400 countries. 24
surgeries in



From exceptional education that extends beyond the department of Orthopedics, to service beyond our borders, the Section of Hand, Wrist & Elbow continues to stand out as a leader in the field of hand and upper extremity surgery.

Regarded as one of the top hand surgery fellowship training programs in the country, our Hand & Upper Extremity Surgery Fellowship program expanded training opportunities in brachial plexus & peripheral nerve injuries, congenital hand surgery, and elbow surgery.
2023 was the first year with 3 fellows. Additionally, we nurtured growth in educational opportunities through a unified core curriculum for hand & upper extremity surgery and integration with Plastic Surgery faculty.
In 2023 we held the 2nd Annual Frank A. Scott, MD Hand Surgery Lectureship. This wellattended event hosts esteemed national leaders in hand and upper extremity surgery. Named for and founded by our Emeritus Program Director, Dr. Frank A. Scott, the event provides invaluable continuing education opportunities for improving patient care, and a chance for meaningful professional connections.


Through their partnership with Touching Hands -- an outreach program of the American Society for Surgery of the Hand (ASSH) -- our faculty have developed opportunities and a formal educational elective to experience and participate in international outreach, supporting two to three week-long trips annually to San Pedro Sula, Honduras.

From children with deformities to adults with chronic pain or victims of unspeakable violence, Touching Hands volunteers work to better the lives of patients who desperately need hand care. Sending teams of hand surgeons, anesthesiologists, nurses and hand therapists to countries that have little access to medical care, their work allows these patients to use their hands again, whether it's to hold their child, return to work, eat a meal, or put on their shoes.
Each brigade evaluates approximately 170 patients in- clinic and performs 50-60 complex surgical cases over the week for both adult and pediatric patients.
This impactful experience includes opportunities to teach local medical students, residents, and surgeons, and to care for patients with limited resources.




4 faculty
3 hand surgery fellows
2 orthopedic surgery residents
1 Physician Assistant
3 resident alumni


Orthopedic Oncology continues to break new ground in research, education, and clinical care.

Our orthopedic oncology unit is one of the few centers in the United States able to customize pelvic implants after major pelvic resections or to customize knee implants after major knee resections to prevent major amputations.

We are the most prominent center in the United States to treat musculoskeletal non-tuberculosis infection in collaboration with the National Jewish Hospital. We are renowned throughout the entire United States as the referral for soft tissue and bone and muscle infections of non-tuberculosis micro bacterium.
Dr. Lindeque has been invited to the World Cancer Conference in Budapest, Hungary in June 2024. As an invited speaker, he will address the conference on biopsy accuracy and types of biopsies and the accuracies thereof in musculoskeletal tumors.
We are on the leading edge of the biomechanical study on suture material and suture knots - testing different materials including micro monocryl nylon and fibral wire to determine the strength of the materials versus the type of knots.
We are also spearheading a study that has never been done to look at the introduction of bacteria into deeper tissue via needlesticks.
We’re looking at spearheading another study -- the extra cellular matrix coverage of wounds as well as deeper layers. We are one of the centers in the world that has the most experience with this material and also with the pathological appearance after implantation.
It is with great enthusiasm that we announce the successful recruitment of Dr. Steven Thorpe. After more than a year of negotiation, Dr. Thorpe will join us on June 1, 2024 as the new Chief of Musculoskeletal Oncology.
Together with Drs. Lindeque and Donaldson, our vision is that the MSK oncology program will become the premier center not only in the region but in the country. The MSK oncology program will be part of the multidisciplinary Cancer Center at UCH and Children’s Hospital Colorado and work side-by-side with their oncology partners.
As we welcome Steve and his wife, Elizabeth, to our Orthopedic faculty, I also want to express my sincere gratitude to Nate and Bennie who have been doing an admirable job through all these years in providing excellent care to orthopedic oncology patients.

 Section Chief | Onco
Section Chief | Onco

“I couldn’t be more excited to join the Department of Orthopedics at CU, partnering with Drs. Lindeque and Donaldson, and the rest of the sarcoma team at both the CU Cancer Center and Children's Hospital Colorado, to become the preferred treatment center in the region and a national leader in delivering care to patients with sarcoma and musculoskeletal tumors.
Steven Thorpe, MD Professor

Children’s Colorado sees more, treats more, and heals more children than any hospital in our seven-state region. 2023 was no exception and was a terrific year for Pediatric Orthopedics at the University of Coloradofull of so many accolades, that this brief highlight cannot begin to do them justice.
Nonetheless, we are excited to share a small snapshot of our education, research, clinical care, and service accomplishments.
The year started out strong, as our sports medicine program hosted the annual Pediatric Research in Sports Medicine Society (PRiSM) meeting in downtown Denver, highlighted by the election of our very own Dr David Howell as president of this distinguished organization.
Dedicated to truly holistic care of the young athlete, PRiSM is a multidisciplinary group of practitioners comprised of athletic trainers, primary care sports medicine physicians, physical therapists, orthopedic surgeons, research scientists, musculoskeletal radiologists, sports nutritionists, nurse practitioners and sports psychologists.
“By creating space to advance the understanding of injuries and pathologies specific to pediatric athletes among clinicians and researchers from many different backgrounds the society is truly special.
David Howell, PhD, ATCWe bookended the year by hosting the annual meeting of the Skeletal Dysplasia Management Consortium (SDMC) here on campus.
The SDMC is a multidisciplinary group of member clinicians who are experts in the field of skeletal dysplasia, and are dedicated to improving the clinical management of skeletal dysplasia.


“The successes of our clinical, educational and research missions are made possible only through the tremendous dedication of the entire pediatric orthopedics group.It is a privilege to be a part of this remarkable team.
Klane White, MD Professor Vice Chair | Pediatric Orthopedics


Research coordinators from the pediatric section of CU Orthopedics are leading the way in an international multicenter study, evaluating the measurement pulmonary function in children with scoliosis - funded by the Scoliosis Research Society.

Point of Care Spirometry – A prospective comparison vs. laboratory spirometry for children with EOS
Scoliosis Research Society Grant Klane White, MD

Early Onset Scoliosis (EOS) results in reduced lung volumes, exercise intolerance, and associated poor health resulting in increased lifelong morbidity.
Spirometry is a lung function testing method that quantitates lung volumes.This test is normally performed in a hospitalbased lab overseen by certified pulmonary function technicians.
For a variety of reasons spine deformity surgeons often fail to capture this critical outcome measure when treating patients with EOS. Point of Care spirometry, performed in the clinic, offers an opportunity for spinal deformity surgeons to obtain pulmonary function data in a timely and convenient fashion.
The goals of this study are to determine the feasibility and reliability of point of care spirometry in pediatric spinal deformity clinics.
Expanding our Understanding of Human KIF7 Mutations Associated with Idiopathic Scoliosis (IS) and Responsiveness to Estrogen
Scoliosis Research Society Grant
Nancy Hadley-Miller, MD
Idiopathic Scoliosis (IS) is the most common pediatric spinal deformity, affecting 2-3% of individuals with ~0.7% resulting in surgical intervention. For unknown reasons, females are more commonly affected with severe curvatures over males at a ratio of ~9:1.
While rooted in childhood, IS has life-long implications. This proposal addresses the urgent need to determine molecular mechanisms underlying IS. For this project we will further our studies related to KIF7, a kinesin protein that plays critical roles in vertebrate development and structure of the primary cilia. Our previous work identified patient specific KIF7 mutations within IS individuals and families The objective of this proposal is to determine the effects of patient-specific KIF7 mutations within fibroblast cells through CRISPR/Cas9 genetic manipulation Additionally, we aim to determine whether the application of 17β-estradiol (E2) to these cells modifies any effects of these mutations. Through the study of patient specific mutations, we will, for the first time be able to identify the mechanistic and functional parameters of human KIF7 variants in vitro and the cellular response to hormonal influences. These studies will afford us critical information for the molecular mechanisms underlying IS human gene variants and their relationship to spinal axial development.
Colorado Clinical Translational Sciences Institute (CCTSI K12 Program) award
Colorado Clinical Translational Sciences Institute
Aubrey Armento, MD
Dr. Armento is developing an innovative, independent research program with a focus on relative energy deficiency in sport (REDs) and the female athlete triad -- the interconnection between nutrition, bone health, and menstrual health in adolescents.
Dr. Armento’s K12 study will examine the relationships of weight-bearing exercise and bone health, including novel bone quality data from high resolution peripheral quantitative computed tomography, in adolescent females with restrictive eating disorders. She also will characterize exercise participation in this population throughout recovery after completion of intensive eating disorder treatment.
Dr. Armento is a true clinician-scientist, solidly grounded with one foot in pediatric clinical care and the other in research. Her work will guide the clinical approach to exercise recommendations and bone health changes in the setting of an eating disorder.
cardiovascular
gastrointestinal
immunological
REDs
bonehealth
metabolic
hematological
endocrine






 3
4
5 6 7
3
4
5 6 7

Learn about more remarkable work our faculty are doing to improve patient care
1

Rectus Femoris Transfer, With or Without Hamstring Lengthening, Does Not Change Hip Kinematics in Children with Cerebral Palsy
2 Hip Dysplasia Treatment and Non-Narcotic Pain Management

3

Less Need for Pavlik Harness for Infants When Accepted Use Criteria Applied to Developmental Hip Dysplasia
4

Predicting Late Developmental dysplasia of the Hip: Using both Ultrasound and Plain Radiographs
5 New Concussion Management Assessment Tools for Youth Sports

6

Twelve-Week Standard of Care
Pavlik Harness Treatment for Infants with IIc Hip Dysplasia
Longer than Median Time to Normalization
7 Current Classification Systems Adequately Assess Severity and Management Patterns of Pediatric Pelvic Fractures


This year we are fortunate to host Dr. Piochih Shen, an international fellow from Taiwan, who has spent the majority of his time with our spine team, but looks to expand his scope to include hip preservation.
On the subject of hip preservation, in April, Dr. Selberg’s team traveled to Switzerland for the renowned Bern Hip Symposium.
This year, we were fortunate to expand the MRC leadership, bringing on Deirdre Rafferty as our MRC manager to oversee this bright and hardworking group of individuals. We also welcomed our first pediatric orthopedic post-doctoral fellow, Dr. Kellen Krajweski, who will be with us for the next two years, supporting our neuromuscular and gait analysis team while pursuing his own line of research. The MRC was host to eight summer research interns, mentored by our faculty and PRA group alike. The most notable products of these efforts were more than 50 peer reviewed articles and 50 abstract presentations in the last academic year.
Under the steady guidance of Dr. Gaia Georgopoulos, our residency program continues to thrive, successfully educating 20 CU Orthopedics residents on the practice of pediatrics annually.
The core of our education program -- our pediatric orthopedic fellowship led by Dr. Erickson -- oversaw the graduation of our two remarkable fellows, Drs. Rado Dimovski and Mariano Garay, and the welcoming of two new pediatric orthopedic fellows Drs. Holt Zalneraitis and Jacob Willen.

or
 Mark Erickson, MD Fellowship Program Director
Mark Erickson, MD Fellowship Program Director
We witnessed the coalescence of all of these educational endeavors in the form of yet another superb Robert E. Eilert Visiting Professorship, honoring Drs. Harry Kim (Texas Scottish Rite Hospital for Children) and Steven Frick (Stanford University), expertly organized by our education coordinator, Caryl Griffith-Abratique.
Beyond these landmark events, our faculty gave countless lectures, courses and presentations at national and international meetings, as well as numerous regional and local venues.



Clinical care continues to be the heart and soul of the pediatric orthopedic division.
Through the efforts of our entire faculty and staff, our dedication yielded a very productive year, once again increasing both outpatient ambulatory and OR volume by 7% and 12% respectively.
More importantly we did so while successfully navigating the restructuring of EPIC and our clinic scheduling process. Our administrative team and clinic staff were instrumental in supporting these changes, working tirelessly to make the transition as seamless as possible.
We welcomed six new providers to our ranks: Dr. Kristina Wilson (Sports Medicine), Dr. Star Nixon (Colorado Springs), and APPs Mariah Miller, Elizabeth Rausch, Elinor “Ryn” Berger, and Blaine Allen --
and our Sports Medicine team rose to new heights in their partnership with the Jefferson County School District, now serving 18 schools.
Learn more about the CHCO and JeffCo Schools partnership


45 states
4,500 surgeries


CU Orthopedics Pediatrics division continues to be a leading provider of choice with both clinic and surgical case volume increases in 2023. Seeing patients from 45 states, we completed over 62,000 outpatient visits and 4,500 surgeries.
We saw significant growth at our network of care locations in Parker and Wheatridge, with surgical volumes increasing by 20%.
>62,000 outpatient visits

Referral volumes increased by 13% in 2023, with our largest referral growth in Northwestern Colorado, and Southern Colorado (south of Colorado Springs)

Colorado Springs Orthopedic Surgeon Brian Shaw, MD, and his wife Lisa Shaw, RN, led a twenty-strong, all volunteer team on their 12th Colorado Pediatric Orthopedic surgical service trip to The Moore Pediatric Surgery Center in Guatemala City, Guatemala.
A true testament to their love for what they do and their dedication to underserved children, the team completed a staggering 44 procedures in 4.5 days.


Typical conditions treated were delayed presentations of developmental dysplasia of the hip DDH (ages 2-6 years), neglected severe club foot deformities in older children – often with skin breakdown and chronic osteomyelitis – and assorted congenital and acquired musculoskeletal conditions.




Brian and Lisa, and 3 additional co-authors, published an 8-year review of their Guatemala work in the March 2023 issue of Journal of Pediatric Orthopaedics




 A patient with neuromuscular club foot with chronic ulcer, and Cast Technician Sam Jones who delights patients with his customized casts.
A patient with neuromuscular club foot with chronic ulcer, and Cast Technician Sam Jones who delights patients with his customized casts.







Last but certainly not least, the pediatrics group banded together to support the Bony Express team in the Courage Classic in memory of our former chair, Dr. Lori Karol.
Founded in 1990, the Courage Classic is a twoday annual bicycle event that brings together riders, volunteers, sponsors, friends and families to support Children’s Hospital Colorado. It is the largest fundraising event for Children’s Colorado. Last year our team raised over $50,000 for this great cause.
Dr. Karol is remembered by her family, friends, colleagues, and patients for her unwavering compassion and generosity. She helped build a foundation for breakthroughs in healthcare that will improve the lives of so many.

1961-2022
DR. LORI A. KAROL,MD
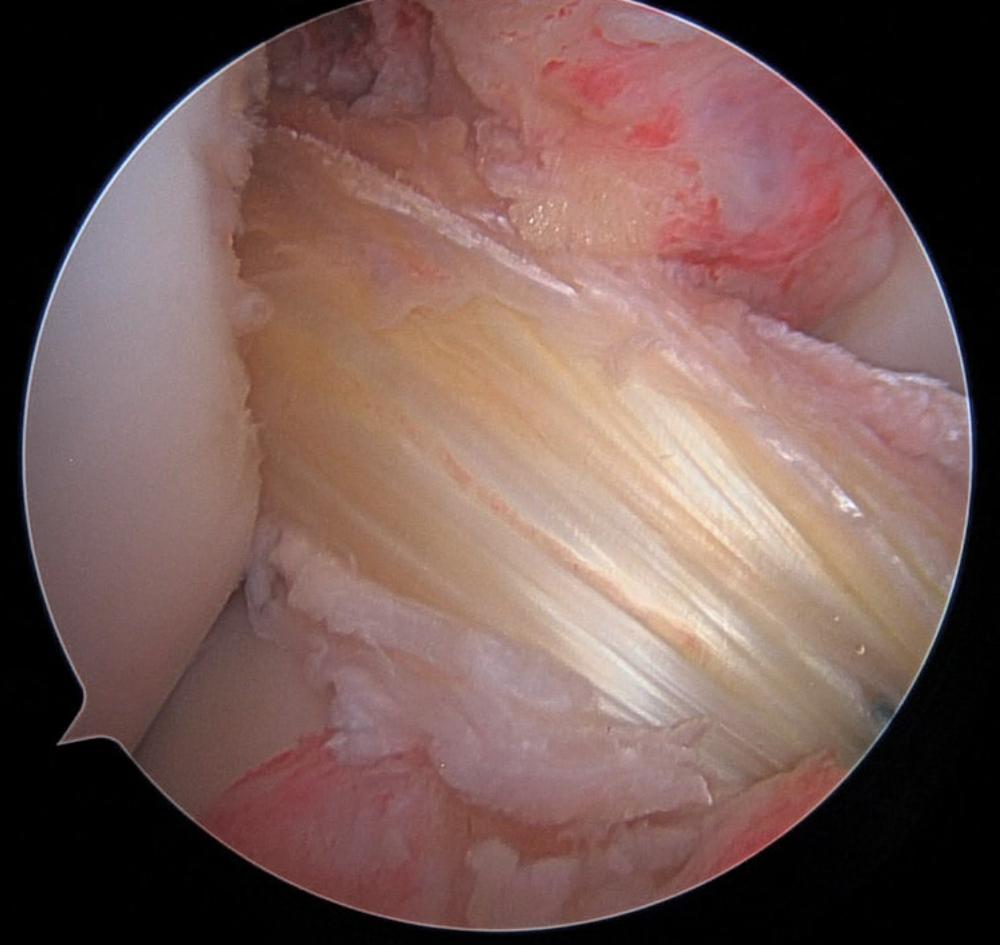
As the spine section continues to flourish, we expand patient safety, care delivery to the highest risk populations, and advancement in the field of orthopedics and spine surgery.

E
Dr. Burger and Dr. Patel have lead the way in Colorado with a novel non-fusion spine implant.
They were both active in the clinical trial, and after FDA clearance, have been at the forefront offering this device to patients
We have created the Spine Infection Multi-disciplinary Infection Board of Advisors (SIMBA) with Infectious Disease, Neurospine, Orthospine and MSK rads for more difficult infections.

We led an Instructional Course Lecture at the Academy on Treatment of Spine Infections.
Patient care also extends beyond the hospital. Guided by our chair, Dr. Evalina Burger, Dr. Nolan Wessell has been a staunch advocate for patients rights, healthcare and wellness. As he works to complete his MBA, he had worked as a board member of the Colorado Orthopedic Society, advocating at all levels of the government. This includes recent testimony to the Colorado legislature. R E S E A R C H
The treatment of spinal infections is not well defined, and a cursory review of the literature can lead to conflicting treatment strategies. To add to the complexity, infections can include primary infection of the spine, infection secondary to another primary source, and postoperative infections including epidural abscesses, discitis, osteomyelitis, paraspinal soft-tissue infections, or any combination. Furthermore, differing opinions often exist within the medical and surgical communities regarding the outcomes and effectiveness of varying treatment strategies. Given the paucity of defined treatment protocols and long-term follow-up, it is important to develop multidisciplinary treatment teams and treatment strategies. This, along with defined protocols for the treatment of varying infections, can provide the data needed for improved treatment of spinal infections.
While the clinical treatment has been an important advance, evaluation of treatments, development of new diagnostic tools, and discovery are also key to this endeavor. Two NIH grants, one spearheaded by Dr. Cheryl Ackert-Bicknell, PhD and the other by Dr. Reed Ayers, PhD are breaking new ground in diagnosis and staging of spine infections and the role of bacteria and metals in the spine. Dr. Ackert-Bicknell, an Associate Professor in the Research Division of Orthopedics, is conducting a study to determine if newly made antibodies by the patient’s immune system can be used not only diagnosis what is causing the infection, but also if they can be used to monitor treatment success with much greater accuracy than is possible now. Dr. Ayers, a Research Assistant Professor, also in the Research Division of Orthopedics, focuses on determining how the metals found in spine orthopedic implants interact with the local tissues, the normal (thought to be harmless) bacteria found patients and with infectious organisms. His work will help redefine what is an infection and how we diagnose and treat spine infections. He is discovering new ways to improve how spine instrumentation integrates into the bone and muscle, reducing patient pain and potential subsequent need for revision.

The Spine Section has continued to expand the frontier of spine infections and tumor treatment.
By taking the novel approach in spine patients - infection treatment mimics tumor necessitating surgical resection and stabilization and local/systemic chemotherapeutics - we have been able to significantly reduce mortality for vertebral osteomyelitis. This was achieved, in part, through the creation of a Spine Infection Multi-disciplinary Board of Advisors (SIMBA).
The group includes orthopedic spine, neurosurgery, infectious disease and musculoskeletal radiology experts who review and make recommendations on complex spine infections.
The treatments follow an algorithmic approach; 1) identification of the organism(s), 2) local disease control with stabilization as necessary, 3) local chemotherapeutics (often with biodegradable antibiotic beads for local delivery), and 4) long-term chemotherapeutic suppression. This approach has led to the successful treatment of a variety of bacterial infections including brucellosis of the spine, non-tubercular and tubercular mycobacteria infections, including the first ever reported case of mycobacterium phlei and a rare case of mycobacterium xenopii, and fungal infections such as aspergillosis.
The University of Colorado has previously reported on the implementation of planning in spine surgery, and this has continued.
Implanting the second pre-planned spine rod, after FDA approval, in 2013, the technology has advanced to include predictive models, artificial intelligence and robotics and navigation technology to improve safety and precision in spine surgery. Dr. Ou-Yang has continued to lead in this area, also leading the way with patient quality and safety. He has solidified his work through IHQSE, developing and improving the complex spine deformity pathway improving patient safety in some of the riskiest surgeries performed by the spine division. This work is now pushing into the intra- and post- operative phases of care. With the continued efforts, the spine division continues its commitment to provide the highest level of care to Colorado’s highest risk patients.
Advancing academic research to transform biomedical discoveries into treatments for patients, SPARK | REACH Colorado provides a funding mechanism through SPARK Awards to CU Anschutz faculty and students developing therapeutics, medical devices, and diagnostics to address unmet medical needs.
Modeled after the Stanford SPARK Program established in 2006 by Dr. Daria Mochly-Rosen as a cost-effective model for this crucial endeavor, the SPARK|REACH Program at CU Anschutz is focused on commercialization with the primary emphasis on product development and technology transfer activities.
To do this, SPARK provides education, access to industry expertise, and fosters a culture of innovation.
Drs. Evalina Burger and Vikas Patel were both presented with SPARK Awards to further their innovations in spinal medicine technology.
This project focuses on reducing subsidence, a complication in spinal fusion surgery where the intervertebral body fusion devices (cages) sink into the endplates of the vertebrae, leading to misalignment and the need for revision surgery. The proposed solution involves developing a patient-specific spinal fusion cage customized to match the stiffness and geometry of the patient's vertebral body endplates, which can be obtained from CT scans The project aims to create a working prototype of the patient-specific cage, develop automated software to determine endplate characteristics, and secure a patent in order to obtain licensing opportunities with existing spinal cage companies.
Collaborators: Ji Ma, PhD, Vikas Patel, MD, Todd Baldini and Andriy Noshchenko

Cervical spine pathology has traditionally been treated with anterior fusion surgery utilizing basic instrumentation. Metal plates stabilize the spine and disc space to provide a controlled environment for bone healing and growth. Standard plate systems come with many limitations: a) difficult sizing, b) difficult positioning, c) adjacent level impingement, poor screw – plate interface /locking, d) need for repeat fluoroscopic x-ray imaging, and e) need for wide exposure. All of this makes the plates "fiddly" to implant. There has not been a significant advancement in cervical plates in many years. Our design provides dramatic improvement on all of these issues. The plating/fixation system improves fixation strength while dramatically easing surgical technique and reducing inventory requirements. The plate has holes which are not full circumference, instead it has about 2/3 of a "hole" and the screws engage the plates with threaded screw heads. The 2/3 hole allows for tremendous ease of implantation by allowing for screws to be placed when sizing the disc space. The plate can then be inserted after the screws have been initially placed in the bone. The screws then lock into the plate with threaded heads. This system keeps the plate far from adjacent levels.


Spondylolisthesis is a displacement of a vertebra in which the bone slides out of its proper position onto the bone below it. Surgery may be necessary to correct the condition if too much movement occurs and the bones begin to press on nerves.
Over the course of four years, Alan Shafner’s calf muscle was inexplicably shrinking. Alan describes it “like a balloon with a slow leak.” As a busy attorney and active Coloradoan with a great golf game, Alan carried on until he started experiencing pain down his right leg. Referred to the CU Department of Orthopedics by his primary care physician, Alan met with Dr. Evalina Burger. “Dr. Burger did an exam like no other I ever had. She was so thorough.”
Explaining treatment options, Dr. Burger discussed a traditional spinal fusion and a new innovative motionpreserving spinal implant for the lumbar spine. Designed to stabilize the lower spine and relieve compressed nerves, the implant would provide lasting mobility and durability.
“Alan had a spondylolisthesis at the L4 – L5 level. This condition causes compression of the nerves and presents both with leg pain and back pain. The back pain is from the instability. This new device allows for a complete decompression of the nerve roots and the general sack while providing stability with motion at that level. This is truly a breakthrough concept as the pain generators in this condition are all addressed through this surgical implant” , Dr. Burger notes.
illustration of spondylolisthesis


“
I can’t say enough good things about Dr. Burger. I am sincerely grateful to her and her team for what they have done for me. I am back to full duty. The
only limitations I have are the limits I put on myself.
Alan Shafner



Championship rings represent greatness and an unwavering commitment to being the best. Imbued with symbolism, brilliant gemstones are set in a design that tells the story of the journey to a championship. But transcending their glinting, radiant exterior, they represent and commemorate a season of hard work, struggles, and ultimately triumph -- the collective effort of a team of individuals working together toward a common goal, forged not in gold, but in a purpose greater than themselves.
Dr. Jason Dragoo knows the same is true of the team of exceptional physicians and advanced practice providers who provide the highest standard of orthopedic care for the athletes. “Just as teamwork is required for players to win a championship, the medical team also requires the same teamwork. The physicians work with team physical therapists, athletic trainers, and performance coaches to collaborate on treatments that not only get the players back on the court and field after injury, but keep them there.”
“We use very sophisticated sensors and tracking software to measure the athletes’ performance and identify weaknesses. This allows the use of cutting-edge treatments that include biologics, blood flow restriction therapy, and other techniques that help the body heal faster.”



While Dr. Dragoo is focused on keeping players on the court, Dr Michelle Wolcott has both eyes on the lacrosse field As a team doctor with the Colorado Mammoth, her role is to coordinate the medical care for the team, evaluate injuries, provide treatment, and assist the athletic trainer in documentation. She performs preseason and exit physicals on all players and provides emergency care at games. “Being a team physician, I watch the games as a fan but also with a sense of purpose to identify injuries as they happen. I am always on the edge of my seat when a player goes down. I watch the athletic trainer as well as the athlete, already trying to figure out what is needed urgently or emergently.”
“I approach my patients as if their regaining function for a job, hobby, or sport is our goal. It is helpful to discuss injuries in athletes as something my patients can relate to and I try to assure them that I treat them the with the same approach. We are all athletes in our own way.
Michelle Wolcott, MD Associate Professor Team Physician | Colorado Mammoth

The physicians’ dedication to the teams - in addition to the uncompromising care they provide to all patients in their full time surgical practices - is remarkable. Team doctors are required to travel with the team for every playoff game. This often means returning from a trip at 3:00 AM and starting surgery at 7:30 that same morning, providing the same exceptional care their professional athletes receive. It takes a commitment by the surgeons to support a championship team, but they love what they do and never lose sight of their greater purpose -- caring for all their athlete-patients, from the professional to the weekend warrior.
At the end of the day, our doctors are always on the most important team: yours.
“When you’re in the OR, you are not only treating the person in front of you, but each surgery allows you an opportunity to learn how to make it better and stimulates new research ideas to try to improve upon what we’re already doing. That really motivated me to want to become an orthopedic surgeon.
Rachel Frank, MD Associate Professor Team Physician | Colorado Rapids Team Physician | US Women’s National Team (USWNT) Dr. Frank with clinicians for the USWNT: Rion Zimmerman, Chiropractor | Juliet Barnes, ATC | Sarah Leslie, ATC | Rachel Frank, MD | Katie Donnelley, ATC | Michael Shirilla, PT
Dr. Frank with clinicians for the USWNT: Rion Zimmerman, Chiropractor | Juliet Barnes, ATC | Sarah Leslie, ATC | Rachel Frank, MD | Katie Donnelley, ATC | Michael Shirilla, PT
Dr. Rachel Frank knows first hand what it’s like to be sidelined form a sport due to injury. A team physician for the Colorado Rapids and the US Women’s National Team (USWNT), Dr. Frank is a also a former NCAA Division I soccer player who underwent seven surgeries on the same knee. “I learned what it means to be on the patient side of things and how challenging that can be.”
It is from this personal place of understanding that she is motivated in her treatment and research of ACL reconstruction and recovery.
Dr. Frank notes that currently, about 60-70% of high level athletes will be able to return to their sport to their pre-injury performance levels. That number is higher for amateur athletes, but still presents a humbling situation, and recovery is often in the range of 8-12 months.
I think if we can marry a biologic repair or reconstruction with a mechanically sound repair or reconstruction, we may have an opportunity to get the ACL healed quicker with excellent reliability.
I think what athletes want is an ability to get back to their sport at the same level quickly. What surgeons want is the exact same thing. We’re just not there yet, but I think there are opportunities to get there.
The anterior cruciate ligament (ACL) is one of the strong bands of tissue in the knee that help connect your thigh bone to your shinbone. ACL injuries most commonly occur while playing sports that involve sudden stops or changes in direction - such as soccer, basketball, football, and downhill skiing. The vast majority of ACL tears require surgery to repair the tissue.
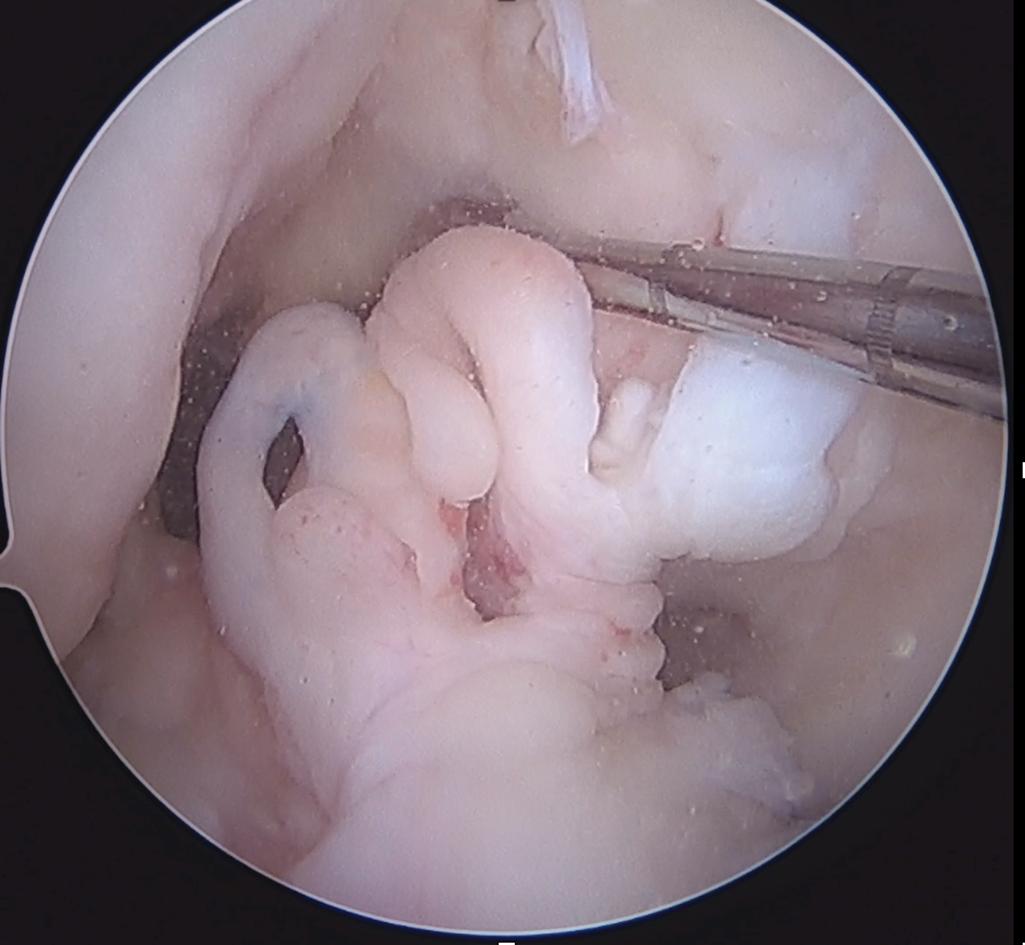

The newest hub for innovative medical technologies, leadingedge minimally invasive procedures, and comprehensive patient care is also one of few centers of its kind in the nation.
Serving patients from across the country, the CU Medicine
Regenerative Medicine, Hand and Spine Center consists of a multi-disciplinary team of board-certified providers specializing in regenerative medicine, hand-wrist-and-elbow conditions, brachial plexus and peripheral nerve injuries, and non-operative spine care.


Located at the Inverness Steadman Hawkins Clinic Denver, physicians provide a team approach with expertise across orthopedic and physical medicine and rehabilitation specialties.
Treatment solutions include minimally invasive arthroscopic and surgical procedures - many without general anesthesia, allowing patients to return home the same day.
Featuring two procedure areas, recovery spaces, and an onsite regenerative medicine laboratory, the CU Medicine Regenerative Medicine, Hand and Spine Center affords patients the opportunity to be seen by a specialist for their joint or nerve ailment or injury, and in many cases receive a minimally invasive procedure the same day.

“We are performing procedures with new technology that allows for minimally invasive arthroscopic treatment with instruments the size of a needle. This trailblazing, integrated approach is a game changer for quality of patient care.
Jason Dragoo, MD Professor
As high school sweethearts, Josh and Melissa Bryan could not have imagined how their lives would reconnect and the extraordinary journey they would travel together.

Eight days into a birthday trip to Thailand, Josh Bryan and his brothers rented scooters to tour the island and experience the beauty of the lush, tropical vistas. Taking a tight turn, Josh lost control of the scooter and found himself pinned under a guardrail with the vehicle still between his legs. He broke both femurs and was in bad shape.
Though she had only recently reconnected with her high school sweetheart, Melissa -- a UCHealth nurse-- knew she had to drop everything and fly to Thailand to be with Josh.
With Melissa by his side, Josh endured months of pain and complications before being cleared to return to the United States.


Back home in Colorado, Josh continued to suffer from infection. The best path forward was amputation, but with very little bone left to be useful afterwards, Dr. Jason Stoneback and team decided to perform a turnplasty. By amputating Josh’s knee joint and ankle, and turning the ankle side of his tibia upside down and connecting it to the remaining portion of his femur, the team was able to effectively give Josh an above-knee amputation.
Soon thereafter, Josh was fitted with a socket prosthesis, but unlike many who have success with such a system, Josh’s experience with it left him mostly immobile, exhausted, and desperate for an alternative.
So much of Josh’s identity had been forged in his ability to be active and physical. He built his own roofing business and now all of that was in jeopardy until he could figure out how to be more mobile. After four years of living with the socket, Josh sought help for a different solution.
Josh returned to Dr. Stoneback to pursue osseointegration (OI) -- an advanced reconstructive surgery technique for amputees that eliminates the need for a traditional prosthesis. Instead, a boneanchored prosthesis is introduced directly into the patient’s skeleton where the bone integrates directly into the implant.


With a history of infection, and his popliteal artery running directly over the bone where the OI implant would go, Josh was not at all a typical candidate for this surgery.
But determined to find a solution, Dr. Stoneback and Dr. Nathan Donaldson collaborated to move Josh’s artery out of the way and set the stage for OI. The surgery was a success beyond Josh’s wildest dreams.
Now, in addition to regaining his mobility and function of his limb, Josh is able to feel through the bone and through the integrated implant -- a phenomeon called osseoperception. For Josh, osseoperception has been a game changer and has given him back his life as he knew it. He can run his roofing company again, he can feel grass versus hard concrete or gravel and can keep himself from falling because he is able to pick up that sensory information through his bone and the leg itself.
 x-ray after turnplasty with abducted limb impacting the side of Josh’s socket prosthesis causing pain with each step
x-ray after osseointegration with normally aligned limbs allowing Josh a more functional gait
x-ray after turnplasty with abducted limb impacting the side of Josh’s socket prosthesis causing pain with each step
x-ray after osseointegration with normally aligned limbs allowing Josh a more functional gait

“This campus and all of the wonderful talented people I have the privilege to work with -- putting our heads together with our individual skillsets to make these sorts of things happen for people who have often been told there’s no hope, there’s no way forward, we have no options for you -- it’s been the best part of my career and that’s why I do what I do.
Jason Stoneback, MD Associate Professor Director | Limb Restoration Program cover portrait and in-clinic photos by Photography G
cover portrait and in-clinic photos by Photography G







“As soon as I started working with the Limb Restoration Program I knew I was in good hands. Up to that point, I was questioning everything and I didn't know what my future would look like. This road has taught me so much humility and has made my life so much better.
Josh Bryan
“
The Limb Restoration Program has been amazing. It has helped us come back into our lives.
Melissa Bryan


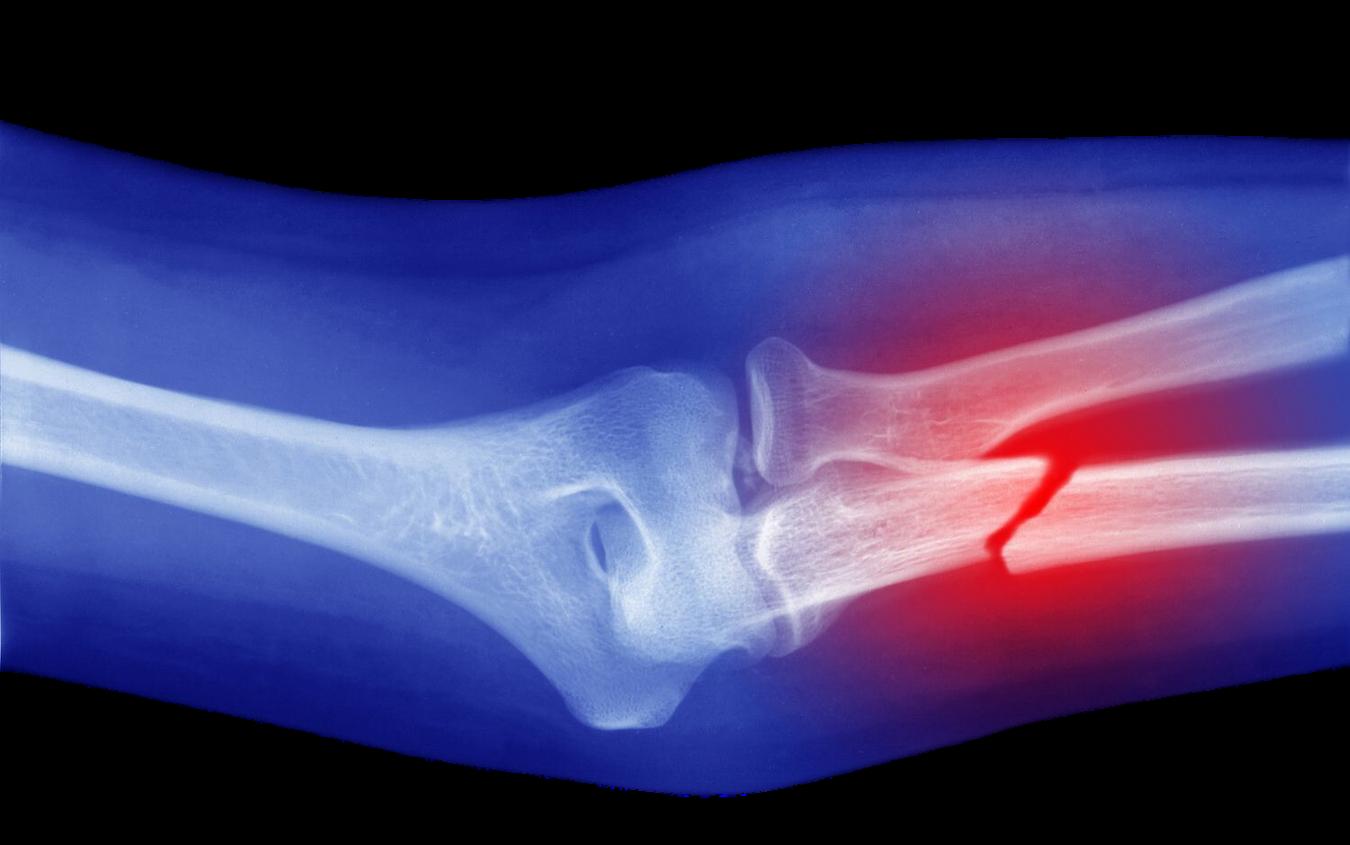
With a grant from the Grayson-Jockey Club Research Foundation and in partnership with the Translational Medicine Institute and Orthopaedic Research Center at Colorado State University, Dr. Jason Stoneback and a multidisciplinary team are using next generation sequencing techniques to study at a single-cell level what’s happening in the joint during arthritis progression.
“It’s an exciting opportunity to look at how does arthritis start, and how does it progress, and are there indicators that we can pick up on early in that progression. Right now we wait until it occurs and typically it results in replacing the joint where we could potentially preserve it. This is absolutely cutting-edge research.
Jason Stoneback, MD Associate Professor Chief | Orthopedic Trauma and Fracture Surgery
Dr. Stoneback and his research team are working with equine veterinarians and researchers to understand the development of post-traumatic arthritis in horses.
The goal is to develop methods for earlier detection and treatment of human post-traumatic arthritis.

People who have experienced trauma to a joint are more likely to develop arthritis in that joint, affecting more than 7x 5 million people every year
 Jason Stoneback, MD
Steve Dow, DVM, PhD
Lynn Pezzanite, DVM, PhD
Laurie Goodrich, DVM, PhD
Jason Stoneback, MD
Steve Dow, DVM, PhD
Lynn Pezzanite, DVM, PhD
Laurie Goodrich, DVM, PhD


2023 was another year of growth for CU Orthopedics in the community, with the January opening of the CU Medicine Orthopedics - Longmont Specialty Care Center. This 14,000 square foot state-of-the-art clinic offers a comprehensive package of orthopedic and spine services in the latest surgical and non-invasive treatment techniques.
We also expanded our clinic at Inverness which includes a clinic-based procedure center.

In addition to our many CU Medicine clinics, our community partnerships continue to flourish in our freestanding hospital based clinics with Boulder Community Health, UCHealth, and Children’s Hospital Colorado.

70% Over
of our faculty have a portion of their practice in the community.

In 2023, our freestanding CU Medicine clinics saw over 100,000 patients
The mission of the Research Division of the Department of Orthopedics is to perform innovative and high-impact basic, translational, and clinical study of the musculoskeletal system, leading to the development of cutting-edge therapies for all orthopedic patients.
We tackle some of the most challenging and complex medical problems facing orthopedics patients -transforming discovery and innovation into solutions that change people’s lives.

We are proud to report that research activity and success in the Department of Orthopedics continued to grow in 2023. The pages that follow highlight just a few of those accomplishments, and our tireless effort to meet our research mission head-on.
We have grown our Clinical Research support infrastructure, which this past year included the addition of a Biostatistics Support Core led by Carson Keeter, and the formation of a Professional Research Assistant Core led in the Adult Sections by Greg Ottenberg and in the Children’s Hospital/Pediatrics section by Deirdre Rafferty.
Augmenting our research-focused faculty group of 10 principle investigators and 51 trainees and staff, we welcomed 4 new research-focused faculty: Dr. David Karasik, Dr. Patrick Carry, Dr. Aubrey Armento, and Dr. Eric Earley. Their incredible work -- which spans from fundamental genetics and molecular biology to clinical impact in orthopedics-- is featured on the pages that follow.
Our community of internationally leading orthopedic and musculoskeletal scientists and trainees has spurned 211 active research studies and 51 clinical trials that are supported by a portfolio of grants exceeding $37M, 15-fold greater than just 5 years ago.
Our national rank among Orthopedics Departments, based on total NIH funding, now sits at #11.


Big data, bioinformatics, and artificial intelligence (AI) approaches can provide new and innovative solutions to complex problems facing orthopedic patients and their surgeons.
Such studies require multidisciplinary teams of people with clinical, biological, mathematical, and statistical expertise. To build collaboration between these disciplines, Orthopedics created the Dyads Pilot Grant Program which pairs researchers from the Colorado Program for Musculoskeletal Research with researchers in the new Department of Biomedical Informatics in the CU Anschutz AI Institute.

The infrastructure created by the Dyads program to bring these two departments together has also launched projects outside of this pilot grant program. We now have teams focused on using AI to better predict surgical complications in spine deformity surgery, identifying the causative genes for idiopathic adolescent scoliosis, and using big data - including genetics - to better predict who is going to need surgery for degenerative disc disease.

The first round of 4 $50,000 will support new high impact projects at the intersection of orthopedics, biomedical informatics and AI awards

Nicholas Dwork, PhD
Julio Carballido-Gamio, PhD
Janani Ravi, PhD
Reed Ayers, PhD
Fan Zhang, PhD
Michael David, PhD
Honey Hendesi, MD, PhD

Investigating how intermittent fasting shifts the gut microbiome and can improve fracture healing in obesity


Biomedical Informatics
Radiology
Biomedical Informatics
Orthopedics
Rheumatology
Orthopedics
Orthopedics
Characterizing post operative infection and how contributing bacteria damage orthopedic hardware, leading to implant failure
Using machine learning approaches to better understand cell behavior changes in the ankle synovium that are associated osteoarthritis progression
Developing deep learning models to help identify fragility fracture risk, which can lead to preventative interventions
Honey Hendesi & Janani Ravi Reed Ayers & Janani Ravi Michael David & Fan Zhang Julio Carballido-Gamio & Nicholas Dwork photo by Photography GDr. David Karasik, PhD, is a new Adjunct Faculty in the Research Division, spending a quarter of his time with our team here in Denver while serving as Professor and Head of the Musculoskeletal Genetics Lab at Bar-Ilan University in Safed, Israel.
Dr. Karasik is a leading expert in the study of the genes that cause complex genetic musculoskeletal diseases including osteoporosis (loss of bone density) and sarcopenia (muscle mass loss).
1 in 3 women and 1 in 5 men the age of fifty will suffer a broken bone due to osteoporosis


“Zebrafish are exceptional allies in our exploration of osteoporosis genetics. Importantly, they are bony fish – resembling other vertebrates, including all higher mammals and even humans. Their genetic similarity to mammals coupled with their transparent embryos during early development offer a window into the process of bone formation in early life and an opportunity to understand how genetics controls bone health as we age. Zebrafish are invaluable partners in unraveling the complexities of osteoporosis, leading our team to uncover new therapeutic strategies to build back bone.
David Karasik, PhD Adjunct Professor
Osteoporosis progresses in four stages, during which the bones become weaker and more prone to fractures and breaking.

Using zebrafish in combination with cutting edge methods such as CRISPR gene editing, Dr. Karasik creates gene mutations that allow him to discover the key mechanisms that underlie disease initiation and progression.

For orthopedic patients and their doctors, the patient experience is tangible and immediate. Research faculty in the laboratory are thinking about that experience, too.
In 2023, Dr. Patrick Carry, PhD established the Carry Musculoskeletal Lab. His lab integrates clinical health records with single and multiomics data to understand the etiology of complex musculoskeletal disease.
The ultimate goal of our work is to ensure research studies are designed to maximize future benefit to the orthopedic patient.
Through partnerships with clinicians, his lab aims to translate these epidemiologic research efforts into effective clinical interventions His lab is actively involved in research projects in the areas of adolescent idiopathic scoliosis, concussion, osteoarthritis, and Type 1 Diabetes. His lab also collaborates with pediatric orthopedic clinical investigators in the Musculoskeletal Research Center (MRC) at Children’s Hospital Colorado.
Dr. Carry’s lab is also interested in the intersection of epidemiology, causal inference, and high dimensional data analysis. His team collaborated with CU Orthopedics Biostatistical Core to develop a novel algorithm to minimize bias during the design of complex, highthroughput experiments. This algorithm, published in the March 2023 issue of BMC Bioinformatics (PMID: 36882691), uses propensity scores to select the optimal methodology for allocating samples across multiple batches.
In 2023, Dr. Carry received a New Investigator Recognition Award from the Orthopaedic Research Society (ORS) based his work entitled When 1 + 1 Does Not Equal 2: Special Considerations are Required for Inclusion of Patients with Bilateral Conditions in Orthopedic Research Studies. This study calls attention to a common source of bias in clinical orthopedic research studies. This work reflects a core priority within his lab, to evaluate and develop new orthopedic clinical research methods.
Effective and appropriate translation of evidence from clinical orthopedic studies into clinical practice requires careful research design and analysis. We are interested in evaluating existing research methods as well as developing new methods.
Patrick Carry, PhD Assistant Professor

In the span of two months, Dr. Aubrey Armento won three high profile scholarships and grants. Of particular note is the Colorado Clinical Translational Sciences Institute (CCTSI K12 Program) award. This prestigious award provides up to three years of funding for clinical translational research.
Dr. Armento is developing an innovative, independent research program with a focus on relative energy deficiency in sport (REDs) and the female athlete triad -the interconnection between nutrition, bone health, and menstrual health in adolescents.
Dr. Armento’s K12 study will examine the relationships of weight-bearing exercise and bone health, including novel bone quality data from high resolution peripheral quantitative computed tomography, in adolescent females with restrictive eating disorders. She also will characterize exercise participation in this population throughout recovery after completion of intensive eating disorder treatment. Her work will guide the clinical approach to exercise recommendations and bone health changes in the setting of an eating disorder.

immunological
gastrointestinal psychlogical growth & development
hematological cardiovascular
REDs
menstrual function
“As
a
sports medicine physicianscientist, I am passionate about promoting the health and well-being of young female athletes, particularly related to nutrition and bone health, through my clinical care and research.
bone health
metabolic
endocrine
Aubrey Armento, MD Assistant Professor Model of Relative Energy Deficiency in Sport (REDs)
Model of Relative Energy Deficiency in Sport (REDs)

Bringing together a multidisciplinary and collaborative team of engineers, scientists, surgeons, clinicians, therapists, and patients to develop novel technologies for prosthetics and rehabilitation, the CU Bone-Anchored Limb Research Group is on the leading edge of prosthetics technology.
Dr. Earley, Assistant Research Professor with the BoneAnchored Limb Research Group, is developing and improving osseointegration technology in a way that can be impactful not only in a laboratory setting, but at home and during daily use.
His research focuses on maximizing patient functionality through improvements to prosthetic control and neurosensory feedback, evaluating quality of life through athome data collection of prosthesis use, and development and validation of new outcome measures.
With the addition of Dr. Earley’s expertise in this groundbreaking research and technology, our team is poised to transform the University of Colorado into a global center for prosthetics and rehabilitation.
Dr. Earley’s groundbreaking work with the Swedish Center for Bionics and Pain Research allows people with amputations above the elbow to achieve an unprecedented level of control over the individual fingers on a bionic hand.
“The most exciting part is the functionality this patient has gained from being involved in the study. After receiving the bone-anchored limb and the implanted sensors, he drastically and very quickly improved his functionality and his independence
Eric J. Earley, PhD Assistant Research Professor

T32s are institutional grants through the NIH that have funding slots for postdocs and/or students. The goal of this T32 program is to train PhD candidates and postdoctoral fellows in diverse areas of musculoskeletal science spanning the bench-to-bedside spectrum from basic science, to translational/preclinical study, to clinical trialing.



To provide comprehensive interdisciplinary training in musculoskeletal science with the aim of developing the next generation of outstanding musculoskeletal investigators

T32 AR080630
Interdisciplinary Training in Musculoskeletal Research
To accomplish this mission, the program provides a series of formalized education elements that will support seated trainees in parallel with a diverse group of unseated trainees spanning from the undergraduate level to clinical residents and fellows, to groups of trainees from our neighboring institutions in Colorado.



The education-specific components of the program include
musculoskeletal science curriculum
Mack Clayton Seminars (preeminent visiting scientists) work-in-progress meetings
journal clubs
Annual Research Symposium and D’Ambrosia Diversity Lectureship weekly interactive Specific Aims Development meetings
In 2023 our program doubled in size from 3 to 6 seated and financially supported trainees, and provided educational content in an ecosystem comprised of 100+ scientists and trainees spanning all 4 CU campuses and 4 outside institutions including Colorado School of Mines, Colorado State University, Denver University, and Steadman Philippon Research Institute in Vail.
MichaelZuscik,
PhD Karin Payne, PhD Program Directors

MUSCULOSKELETAL RESEARCH
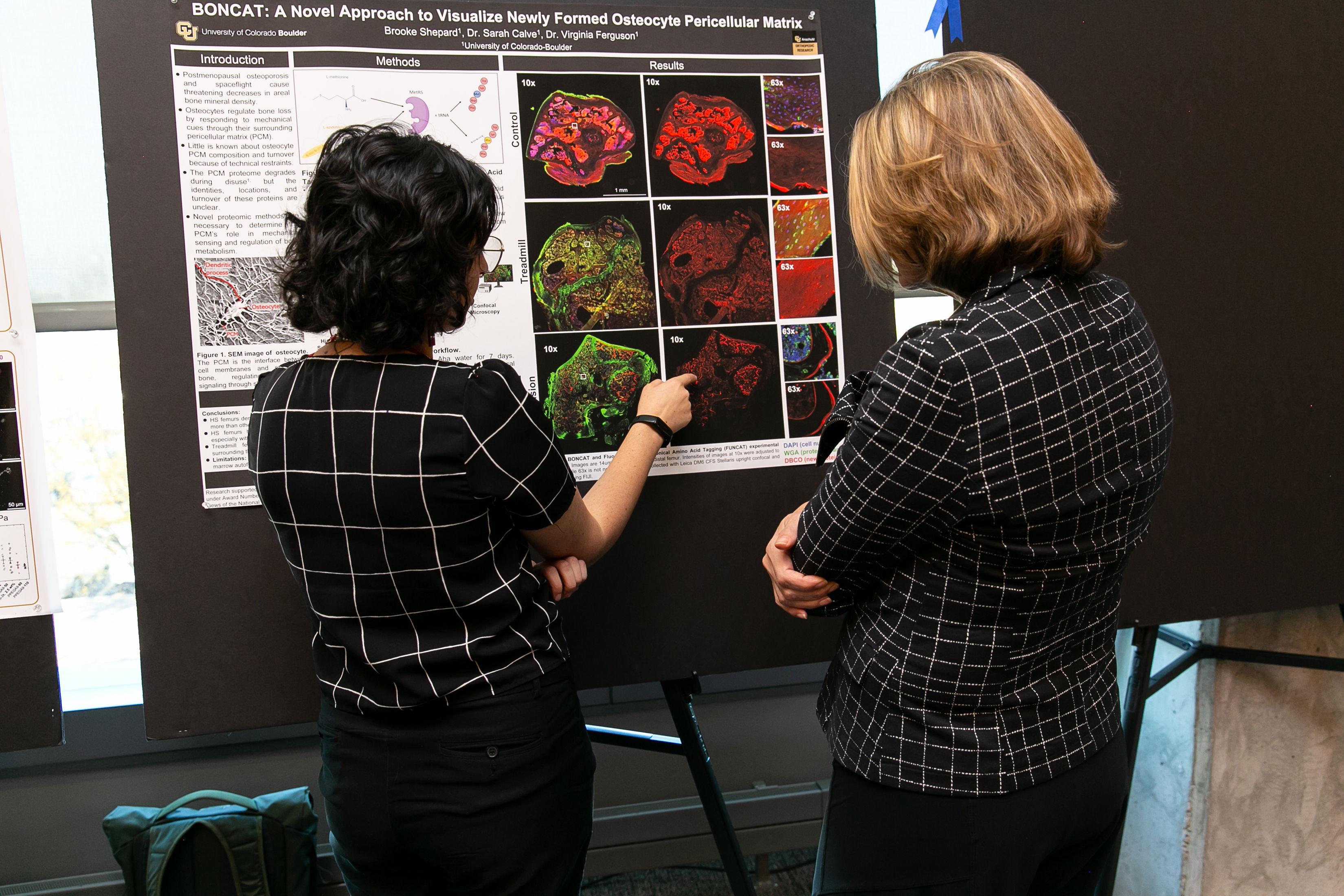
5th Annual Orthopedic Research Symposium & D’Ambrosia Diversity Lectureship


With record breaking participation of more than 300 attendees, 124 poster sessions, and 11 lectures, the Department of Orthopedics and the Colorado Program for Musculoskeletal Research (CPMR) hosted esteemed keynote speakers and scientists representing national and international orthopedic programs. Thanks to expert planning and execution by our Sr. Event Manager, Ellen Rhodes, and the Research team, attendees and keynotes alike raved about the experience.
“Not only were we honored to host our Keynote Speakers Dr. Alliston and Dr. Hogan -- who both taught us so much -- but were also very proud of our faculty and trainee plenary and poster presenters, all of whom did an exceptional job highlighting work taking place across the department and institution over the past year.
Michael Zuscik, PhDProfessor
Vice Chair | Research Director | CPMR
photos by Photography G“As an attendee each year since its inception, this regional symposium is an exceptional format to bring together researchers of all levels for a day of intellectual rapport and comradery. Indeed, the quality of the presentations and interpersonal interactions is unparalleled, allowing the fostering of new connections and collaborations.
Kelly S. Santangelo, DVM, PhD, DACVP
Associate Professor Colorado State University


“I was so honored to be invited as your keynote – and thoroughly enjoyed every part of the trip. It is exciting to see what you are building [at CU Orthopedics]!
Tamara Alliston, PhD Professor, Orthopaedic Surgery Director, UCSF Musculoskeletal Center
University of California San Francisco


















The CU Orthopedics residency program continues to parallel the rising caliber of the department. Over the past five years our graduates have pursued fellowships representing all subspecialties within orthopedics, and have had a 100% Board pass rate. Over a third of our graduates go on to academic careers -- teaching the future generation of orthopedic surgeons.
“I could not be more honored to take on this role and opportunity to give back to a program that has given so much to me. Dr. Dayton has been an incredible role model and I am very fortunate that he continues to mentor me. I believe our program is one of the best places for orthopedic residency training in the world, and I will do my best to continue to build upon this legacy.
Nicholas Alfonso, MD Assistant ProfessorAcross the spectrum of practice models, our graduates serve communities nationwide
In 2023, the baton was passed as Dr. Michael Dayton -Residency Program Director for the past twelve years -- helped recruit a previous graduate from the program to lead it. Dr. Nicholas Alfonso, a graduate of the Class of 2018, assumed the helm of the Residency Program in June.


7 MATCHED 2023
1042 APPLIED
84 INTERVIEWED
matched with 7 residents from:
University of Arkansas
Georgetown University
University of Colorado
Rosalind Franklin
University of Chicago
University of Utah
Wake Forest University

2023 ALL LEARNERS

35
RESIDENTS
17
FELLOWS
PUBLICATIONS & PRESENTATIONS
52
PEER-REVIEWED
66 NON PEER-REVIEWED
290 PRESENTATIONS

Our chief residents began fellowships at renowned programs including Brown, Duke, Stanford, and Washington University.


 Diana Douleh, MD | Class of 2023, with her mentor - Alexander Lauder, MD | Assistant Professor, Denver Health
Diana Douleh, MD | Class of 2023, with her mentor - Alexander Lauder, MD | Assistant Professor, Denver Health
“You only get 5 years to become an outstanding surgeon. When you walk out those doors, there is no "attending" to help make sure you're taking care of things correctly, or preparing for cases the way you need to. Do everything you can to get in every possible surgical case. Prepare like no one else will be there to help you. Use every minute to get better. Time is short, the time to commit to being great is right now.
“
Be mindful of your North Star. Always do the right thing. Keep your indications and your intentions pure. Never settle.
I am proud to be a CU Ortho graduate. I am truly fortunate that I was chosen to train at CU.
Keep perspective, embrace the difficulty and growth, and lean on those next to you. Remember that you are at one of the top orthopedic training programs in the country.
“
Take care of each other. The comradery of the CU Ortho residency is part of what makes it great and pushes you to be the best you can be. Your classmates will challenge you in every way possible but mostly when you are beyond exhaustion, it is being in the trenches together and being a team player that will keep you going.
“Justin Mitchell, MD Class of 2015 Ryan Fader, MD Class of 2016 Amy Harlow, MD Class of 2018 Murray Spruiell, MD Class of 2017

“
The hope is that access to quality healthcare and high-quality education someday becomes a basic human right for all.Regina Richards, PhD, MSW Vice Chancellor Diversity, Equity, Inclusion and Community Engagement
The Department of Orthopedics is committed to actively championing and preserving a diverse, equitable, and inclusive environment that allows us to thrive and serves our patients at the highest levels of compassionate and innovative healthcare.
We believe diverse perspectives empower progress, and we will cultivate spaces where all voices are heard.
Your race, ethnicity, religious practice, sexual orientation, gender identification, and ability are welcome here. You belong here.
A newly appointed Director of Diversity, Equity & Inclusion will be named in 2024.
This position will be instrumental in championing and preserving an inclusive environment in conjunction with the mission, vision and values of the Department of Orthopedics.
$5,237,636.68
2023 total giving to the Department of Orthopedics
We talk a lot about impact.
We have benchmarks of impact by which to measure our own performance, we are inspired by the lifechanging impact our clinicians have on their patients’ lives and, in turn, the impact our patients have made inspiring others we marvel at the extraordinary impact our researchers make discovering new and innovative ways to improve patient care, and we applaud the impact of our faculty educating the next generation of leaders in orthopedics.
But none of this is possible without the gifts of the generous benefactors who believe in our mission and in the far-reaching impact of their philanthropy. For this, our gratitude is immeasurable.

Department of Orthopedics Fund
To provide support for the Department of Orthopedics at the University of Colorado Anschutz Medical Campus
Department of Orthopedics Residents Fund For Professional Excellence
To support the professional development and enrichment of Department of Orthopedics residents at the University of Colorado Anschutz Medical Campus D’Ambrosia Family Endowed Chair in
To provide support for a chair in the Department of Orthopedics at the University of Colorado Anschutz Medical Campus. Support includes research, salaries, supplies and program support for the benefit of the adult (non-pediatric) division

Robert D’Ambrosia, MD Endowed Fund for Diversity in Orthopedics

To provide flexible resources for the greatest diversity initiative needs including but not limited to: lectureships, leadership development and training, student support and other programs in the Department of Orthopedics at the University of Colorado Anschutz Medical Campus
To support the retention and development efforts of the Orthopedic Spine Team in the Department and at UCHealth



To provide support for the Department of Orthopedics in the School of Medicine at the University of Colorado Anschutz Medical Campus. The Fund will provide support for educational programming for residents and fellows within the Department
Limb Restoration Fund
To provide support for the Limb Restoration Program within the Department of Orthopedics at the University of Colorado Anschutz Medical Campus

The following publication list was generated based on the date the citation record was first created in PubMed. Publications created in calendar year 2023 are listed in alphabetical order by first author. Visit the NIH National Library of Medicine for the complete PubMed User Guide.

AAckert-Bicknell CL.
Functional screens refine height GWAS loci
Cell Genom. PMID 37228748
Ackert-Bicknell C, Karasik D.
Proceedings of the Post-Genome Analysis for Musculoskeletal Biology Workshop
Curr Osteoporos Rep. PMID 36869984
Alexeev SO, Buckley SE, Hewitt MA, Hunt KJ.
Publication trends in ligament augmentation techniques: current concepts
J ISAKOS. PMID 37105381
Andras LM, Sanders JS, Goldstein RY, Samora JB.
What's New in Pediatric Orthopaedics
J Bone Joint Surg Am. PMID 36729585
Armento A, Heronemus M, Truong D, Swanson C.
Bone Health in Young Athletes: a Narrative Review of the Recent Literature
Curr Osteoporos Rep. PMID 37289381
Armento A, Keeter C, Gagliardi A, Rossing H, Giachino C, VandenBerg C, Howell D, Albright J.
Association of Grit With Postoperative Knee Outcomes and Physical Function After ACL Reconstruction in Adolescent Athletes Am J Sports Med. PMID 37525482
Armento AM, VanBaak KD, Seehusen CN, Howell DR.
Differences in Training and Health Characteristics Between Trail Ultrarunners and Shorter Distance Runners
Wilderness Environ Med. PMID 36764885
Awad ME, Chung JY, Griffin N, Stoneback JW, Alfonso NA.
Prophylactic Intrawound Antibiotics Significantly Reduce the Risk of Deep Infections in Fracture Fixation: Subgroup Meta-analyses of the Type of Fracture, Antibiotics, and Organism
J Orthop Trauma. PMID 37296086
Bachmaier S, Monaco E, Smith PA, Frank RM, Matzkin EG, Wijdicks CA.
Biomechanical Comparison of 3 Adjustable-Loop Suspensory Devices for All-Inside ACL Reconstruction: A Time-Zero Full-Construct Model Orthop J Sports Med. PMID 37786476
Barnes A, Smulligan K, Wingerson MJ, Little C, Lugade V, Wilson JC, Howell DR.
A Multifaceted Approach to Interpreting Reaction Time Deficits After Adolescent Concussion
J Athl Train. PMID 36701688
Belk JW, Lim JJ, Keeter C, McCulloch PC, Houck DA, McCarty EC, Frank RM, Kraeutler MJ.
Patients With Knee Osteoarthritis Who Receive Platelet-Rich Plasma or Bone Marrow Aspirate Concentrate Injections Have Better Outcomes Than Patients Who Receive Hyaluronic Acid: Systematic Review and Meta-analysis Arthroscopy. PMID 36913992
Belk JW, Littlefield CP, Smith JH, McCulloch PC, McCarty EC, Frank RM, Kraeutler MJ.
Autograft Demonstrates Superior Outcomes for Revision Anterior Cruciate Ligament Reconstruction When Compared With Allograft: A Systematic Review
Am J Sports Med. PMID 36867049
Belk JW, Thon SG, Bravman JT.
Deltoid fascia disruption from the use of a bioinductive collagen scaffold and polyether ether ketone (PEEK) bone staples: a case report
JSES Rev Rep Tech. PMID 37588723
Ben-Zvi I, Karasik D, Ackert-Bicknell CL.
Zebrafish as a Model for Osteoporosis: Functional Validations of Genome-Wide Association Studies
Curr Osteoporos Rep. PMID 37971665
Bookman J, Rocks M, Noh K, Ayalon O, Hacquebord J, Catalano L, Glickel S.
Determining the Optimal Dosage of Corticosteroid Injection in Trigger Finger Hand (N Y). PMID 37191248
Bravman JT.
In Primary RSA, Deltopectoral and Anterosuperior Approaches Differed for Glenosphere Tilt and Beta Angles but Not for Glenosphere Overhang or Prosthesis-Scapular Neck Angle
J Bone Joint Surg Am. PMID 36943928
Buckner T, Johnson RK, Vanderlinden LA, Carry PM, Romero A, Onengut-Gumuscu S, Chen WM, Fiehn O, Frohnert BI, Crume T, Perng W, Kechris K, Rewers M, Norris JM.
An Oxylipin-Related Nutrient Pattern and Risk of Type 1 Diabetes in the Diabetes Autoimmunity Study in the Young (DAISY) Nutrients. PMID 36839302
Buckner T, Johnson RK, Vanderlinden LA, Carry PM, Romero A, Onengut-Gumuscu S, Chen WM, Kim S, Fiehn O, Frohnert BI, Crume T, Perng W, Kechris K, Rewers M, Norris JM.
Genome-wide analysis of oxylipins and oxylipin profiles in a pediatric population Front Nutr. PMID 37057071
Bullock GS, Shanley E, Thigpen CA, Arden NK, Noonan TK, Kissenberth MJ, Wyland DJ, Collins GS. Improving Clinical Utility of Real-World Prediction Models: Updating Through Recalibration
J Strength Cond Res. PMID 36730571
Bullock GS, Thigpen CA, Collins GS, Arden NK, Noonan TJ, Kissenberth MJ, Wyland DJ, Shanley E. Organizational risk profiling and education associated with reduction in professional pitching arm injuries: a natural experiment JSES Rev Rep Tech. PMID 37588509
Burns JD, Upasani VV, Bastrom TP, Baldwin KD, Schoenecker JG, Shore BJ, Brighton BK, Goldstein RY, Heyworth BE, Miller ML, Sanders JS, Truong WH; Childrens ORthopedic Trauma and Infection Consortium for Evidence-Based Study.
Age and CRP Associated With Improved Tissue Pathogen Identification in Children With Blood Culture Negative Osteomyelitis: Results From the CORTICES Multicenter Database
J Pediatr Orthop. PMID 37278086
CCarry PM, Vigers T, Vanderlinden LA, Keeter C, Dong F, Buckner T, Litkowski E, Yang I, Norris JM, Kechris K.
Propensity scores as a novel method to guide sample allocation and minimize batch effects during the design of high throughput experiments BMC Bioinformatics. PMID 36882691
Chang YS, Huang K, Lee JM, Vagts CL, Ascoli C, Amin MR, Ghassemi M, Lora CM, Edafetanure-Ibeh R, Huang Y, Cherian RA, Sarup N, Warpecha SR, Hwang S, Goel R, Turturice BA, Schott C, Hernandez M, Chen Y, Joregensen J, Wang W, Rasic M, Novak RM, Finn PW, Perkins DL. Immune response to the mRNA COVID-19 vaccine in hemodialysis patients: cohort study medRxiv. PMID 36711520
Charchar FJ, Prestes PR, Mills C, Ching SM, Neupane D, Marques FZ, Sharman JE, Vogt L, Burrell LM, Korostovtseva L, Zec M, Patil M, Schultz MG, Wallen MP, Renna NF, Islam SMS, Hiremath S, Gyeltshen T, Chia YC, Gupta A, Schutte AE, Klein B, Borghi C, Browning CJ, Czesnikiewicz-Guzik M, Lee HY, Itoh H, Miura K, Brunström M, Campbell NRC, Akinnibossun OA, Veerabhadrappa P, Wainford RD, Kruger R, Thomas SA, Komori T, Ralapanawa U, Cornelissen VA, Kapil V, Li Y, Zhang Y, Jafar TH, Khan N, Williams B, Stergiou G, Tomaszewski M.
Lifestyle management of hypertension: International Society of Hypertension position paper endorsed by the World Hypertension League and European Society of Hypertension
J Hypertens. PMID 37712135
Chen JS, Paksima N, Rocks MC, Lin CC, Catalano LW 3rd.
Osteolysis Following the Use of Polyetheretherketone Suture Anchors in Hand and Wrist Surgery: A Preliminary Study
J Hand Surg Am. PMID 37542497
Chesler KC, Howell DR, Khodaee M, Pierpoint LA, Comstock RD, Provance AJ.
Are Different Aged Youth Skiers and Snowboarders Experiencing Different Injury Characteristics?
Wilderness Environ Med. PMID 36610917
Cuevas M, Terhune E, Wethey C, James M, Netsanet R, Grofova D, Monley A, Hadley Miller N.
Cytoskeletal Keratins Are Overexpressed in a Zebrafish Model of Idiopathic Scoliosis
Genes (Basel). PMID 37239418
DD'Alessandro A, Earley EJ, Nemkov T, Stephenson D, Dzieciatkowska M, Hansen KC, Minetti G, Champigneulle B, Stauffer E, Pichon A, Furian M, Verges S, Kleinman S, Norris PJ, Busch MP, Page GP, Kaestner L.
Genetic polymorphisms and expression of Rhesus blood group RHCE are associated with 2,3-bisphosphoglycerate in humans at high altitude
Proc Natl Acad Sci U S A. PMID 38147558
Daniels SD, France TJ, Peek KJ, Tucker NJ, Baldini T, Catalano LW, Lauder A.
Posterolateral Rotatory Instability Develops Following the Modified Kocher Approach and Does Not Resolve Following Interval Repair
J Bone Joint Surg Am. PMID 37616381
Davis-Wilson HC, Christiansen CL, Gaffney BMM, Lev G, Enabulele E, Hoyt C, Stoneback JW.
Changes in lower extremity joint moments one-year following osseointegration in individuals with Transfemoral lower-limb amputation: A case series
Clin Biomech (Bristol, Avon). PMID 37043833
Davis-Wilson HC, Christiansen CL, Gaffney BMM, Lev G, Enabulele E, Stoneback JW.
Improvements in disability and function in people with lower-limb amputation one year after prosthesis osseointegration
Prosthet Orthot Int. PMID 36701203
Decilveo AP, Kraeutler MJ, Dhillon J, Harris JD, Fasulo SM, Mei-Dan O, Scillia AJ.
Postless Arthroscopic Hip Preservation Can be Adequately Performed Using Published Techniques
Arthrosc Sports Med Rehabil. PMID 36866293
Dennis DA, Smith GH, Phillips JLH, Ennis HE, Jennings JM, Plaskos C, Pierrepont JW.
Does Individualization of Cup Position Affect Prosthetic or Bone Impingement Following Total Hip Arthroplasty?
J Arthroplasty. PMID 37100096
Dhillon J, Kraeutler MJ, Belk JW, Scillia AJ, McCarty EC, Ansah-Twum JK, McCulloch PC.
Effects of Running on the Development of Knee Osteoarthritis: An Updated Systematic Review at Short-Term Follow-up
Orthop J Sports Med. PMID 36875337
Dhillon J, Kraeutler MJ, Fasulo SM, Belk JW, Mulcahey MK, Scillia AJ, McCulloch PC.
Cartilage Repair of the Tibiofemoral Joint With Versus Without Concomitant Osteotomy: A Systematic Review of Clinical Outcomes
Orthop J Sports Med. PMID 36970318
Dhillon J, Kraeutler MJ, Fasulo SM, Belk JW, Scillia AJ, McCulloch PC.
Isolated Osteotomy Versus Combined Osteotomy and Cartilage Repair for Osteoarthritis or Focal Chondral Defects of the Medial Compartment of the Knee Joint: A Systematic Review
Orthop J Sports Med. PMID 37179710
Dhillon J, Kraeutler MJ, LaPorte DM, Eberson CP, Mulcahey MK.
A Comparison of Match Rates to Orthopaedic Surgery Residency Programs Between First-Time Versus Repeat Applicants: An Analysis of the National Resident Matching Program Data from 2018 to 2022
JB JS Open Access. PMID 37520510
Dhillon J, Orozco E, Keeter C, Scillia AJ, Harris JD, Kraeutler MJ.
Microfracture of Acetabular Chondral Lesions Is Not Superior to Other Cartilage Repair Techniques in Patients With Femoroacetabular Impingement Syndrome: A Systematic Review
Arthroscopy. PMID 37355179
Douleh DG, Baldini T, Carry P, Rogers M, Leversedge FJ, Lauder A.
Ligament-Sparing Volar Radiocarpal Arthrotomy During Distal Radius Fracture Repair: Biomechanical Implications on Wrist Stability in a Cadaveric Model
J Hand Surg Am. PMID 36625632
Dunne LAM, Cole MH, Cormack SJ, Howell DR, Johnston RD.
Validity and Reliability of Methods to Assess Movement Deficiencies Following Concussion: A COSMIN Systematic Review
Sports Med Open. PMID 37578611
Dragoo JL.
Editorial Commentary: Cartilage Restoration Typically Requires Joint Optimization as Well as Local Cartilage Resurfacing to Achieve Best Outcomes: The 30,000 Foot View Arthroscopy. PMID 37716791
Echemendia RJ, Ahmed OH, Bailey CM, Bruce JM, Burma JS, Davis GA, Gioia G, Howell DR, Fuller GW, Master CL, van Ierssel J, Pardini J, Schneider KJ, Walton SR, Zemek R, Patricios JS.
The Concussion Recognition Tool 6 (CRT6)
Br J Sports Med. PMID 37316201
Echemendia RJ, Brett BL, Broglio S, Davis GA, Giza CC, Guskiewicz KM, Harmon KG, Herring S, Howell DR, Master C, McCrea M, Naidu D, Patricios JS, Putukian M, Walton SR, Schneider KJ, Burma JS, Bruce JM.
Sport concussion assessment tool™ - 6 (SCAT6)
Br J Sports Med. PMID 37316203
Echemendia RJ, Brett BL, Broglio S, Davis GA, Giza CC, Guskiewicz KM, Harmon KG, Herring S, Howell DR, Master CL, Valovich McLeod TC, McCrea M, Naidu D, Patricios J, Putukian M, Walton SR, Schneider KJ, Burma JS, Bruce JM.
Introducing the Sport Concussion Assessment Tool 6 (SCAT6)
Br J Sports Med. PMID 37316207
Echemendia RJ, Burma JS, Bruce JM, Davis GA, Giza CC, Guskiewicz KM, Naidu D, Black AM, Broglio S, Kemp S, Patricios JS, Putukian M, Zemek R, Arango-Lasprilla
JC, Bailey CM, Brett BL, Didehbani N, Gioia G, Herring SA, Howell D, Master CL, Valovich McLeod TC, Meehan WP 3rd, Premji Z, Salmon D, van Ierssel J, Bhathela N, Makdissi M, Walton SR, Kissick J, Pardini J, Schneider KJ.
Acute evaluation of sport-related concussion and implications for the Sport Concussion Assessment Tool (SCAT6) for adults, adolescents and children: a systematic review
Br J Sports Med. PMID 37316213
Echemendia RJ, Burma JS, Bruce JM, Davis GA, Giza CC, Guskiewicz KM, Naidu D, Black AM, Broglio S, Kemp S, Patricios JS, Putukian M, Zemek R, Arango-Lasprilla
JC, Bailey CM, Brett BL, Didehbani N, Gioia G, Herring SA, Howell D, Master CL, Valovich McLeod TC, Meehan WP 3rd, Premji Z, Salmon D, van Ierssel J, Bhathela N, Makdissi M, Walton SR, Kissick J, Pardini J, Schneider KJ.
Introducing the Concussion Recognition Tool 6 (CRT6)
Br J Sports Med. PMID 37316214
Elhassan S, Dong F, Buckner T, Johnson RK, Seifert JA, Carry PM, Vanderlinden L, Waugh K, Rewers M, Norris JM.
Investigating iron intake in risk of progression from islet autoimmunity to type 1 diabetes: The diabetes autoimmunity study in the young Front Immunol. PMID 37056761
Ennis HE, Phillips JLH, Jennings JM, Dennis DA.
Patellofemoral Arthroplasty
J Am Acad Orthop Surg. PMID 37364255
Erdogan S, Sakha S, Shanmugaraj A, Prada C, Frank RM, Leroux T, Khan M.
Comparing surgical outcomes of anterior capsular release vs circumferential release for persistent capsular stiffness Shoulder Elbow. PMID 37538519
Foglio AM, McNamara CT, Lindeque BG, Greyson MA.
Technical Strategies for Harvest of the Subtotal Pedicled Fillet of Thigh Flap for Reconstruction of External Hemipelvectomy and Hemicorporectomy Defects
Plast Reconstr Surg Glob Open. PMID 37396841
France T, Lockwood W, Gu S, Tucker N, Baldini T, Lauder A, Catalano LW 3rd.
Radiocapitellar and Ulnotrochlear Pressures Increase in a Radial Head Fracture Model: A Cadaveric Biomechanical Analysis
J Pediatr Orthop. PMID 38147503
Frank RM.
Editorial Commentary: It is Never Wrong to Perform Anterior Cruciate Ligament Revision Reconstruction as a Two-Stage Procedure Arthroscopy. PMID 37543393
Freshman RD, Zhang AL, Benjamin Ma C, Feeley BT, Ortiz S, Patel J, Dunn W, Wolf BR, Hettrich C, Lansdown D; MOON Shoulder Group collaborators; Baumgarten KM, Bishop JY, Bollier MJ, Brophy RH, Bravman JT, Cox CL, Cvetanovich GL, Grant JA, Frank RM, Jones GL, Kuhn JE, Mair SD, Marx RG, McCarty EC, Miller BS, Seidl AJ, Smith MV, Wright RW.
Factors Associated With Humeral Avulsion of Glenohumeral Ligament Lesions in Patients With Anterior Shoulder Instability: An Analysis of the MOON Shoulder Instability Cohort
Orthop J Sports Med. PMID 37900861
Fryar C, Howell DR, Seehusen CN, Tilley D, Casey E, Sweeney EA.
Link Between the Female Athlete Triad and Gymnastics-Related Injury in Retired Collegiate Gymnasts
Clin J Sport Med. PMID 37185819
GGaffney BMM, Davis-Wilson HC, Awad ME, Tracy J, Melton DH, Lev G, Stoneback JW, Christiansen CL.
Daily steps and stepping cadence increase one-year following prosthesis osseointegration in people with lower-limb amputation Disabil Rehabil. PMID 37073780
Gagliardi AG, Walker G, Dahab K, Pearce S, Howell DR, Albright JC.
High healing rate of stable femoral condyle osteochondritis dissecans in young patients placed in a hinged knee brace locked in extension: a retrospective study
J Pediatr Orthop B. PMID 36700964
Geraghty EH, Kraeutler MJ, Clark SC, McCarty EC, Mulcahey MK.
Program and Faculty Reputation Are Valued Most by Applicants to Orthopaedic Sports Medicine Fellowships
Arthrosc Sports Med Rehabil. PMID 36866305
Girardi NG, Kraeutler MJ, Keeter C, Lee JH, Henry K, Mei-Dan O.
During Postless Hip Arthroscopy, Male Patients, High Body Mass Index, Low Beighton Scores, and Limited Range of Motion Require High Traction Force
Arthroscopy. PMID 37634705
HHart E, Howell DR, Brilliant A, O'Brien M, Meehan WP.
Gymnastics and concussions: A retrospective chart review
Brain Inj. 2PMID 37204184
Hassanzadeh H, Baber J, Begier E, Noriega DC, Konishi H, Yato Y, Wang MY, Le Huec JC, Patel V, Varga P, Liljenqvist U, Conly J, Sabharwal C, Munjal I, Cooper D, Radley D, Jaques A, Patton M, Gruber WC, Jansen KU, Anderson AS, Gurtman A; STaphylococcus aureus suRgical Inpatient Vaccine Efficacy Investigator Team. Efficacy of a 4-Antigen Staphylococcus aureus Vaccine in Spinal Surgery: The STaphylococcus aureus suRgical Inpatient Vaccine Efficacy (STRIVE) Randomized Clinical Trial
Clin Infect Dis. PMID 37125490
Hassebrock JD, McCarthy TP, Sylvia SM, Stokes DJ, Shinsako KK, Tokish JM, Frank RM.
Rotator Cuff Repair with Knotless All-Suture Medial Row Anchors and Biceps Autograft Augmentation
Arthrosc Tech. PMID 37654888
Hassebrock JD, Stokes DJ, Cram TR, Frank RM.
Arthroscopic Repair and Reconstruction of Coracoclavicular Ligament
Clin Sports Med. PMID 37716724
Hassebrock JD, Sylvia SM, McCarthy TP, Bravman JT.
Arthroscopic Subscapularis Repair With Preserved Biceps Anatomy
Arthrosc Tech. PMID 37533924
Hassebrock JD, Sylvia SM, McCarthy TP, Stokes DJ, Shinsako KK, Frank RM.
Posterior Labral Repair Using Knotless "All-Suture" Suture Anchors
Arthrosc Tech. PMID 37533896
Hettrich CM, Magnuson JA, Baumgarten KM, Brophy RH, Kattan M; MOON Shoulder Group; Bishop JY, Bollier MJ, Bravman JT, Cvetanovich GL, Dunn WR, Feeley BT, Frank RM, Kuhn JE, Lansdown DA, Benjamin Ma C, Marx RG, McCarty EC, Neviaser AS, Ortiz SF, Seidl AJ, Smith MV, Wright RW, Zhang AL, Cronin KJ, Wolf BR. Predictors of Bone Loss in Anterior Glenohumeral Instability
Am J Sports Med. PMID 36939180
Hohmann E, Bloomfield P, Dvorak J, Echemendia R, Frank RM, Ganda J, Gordon L, Holtzhausen L, Kourie A, Mampane J, Makdissi M, Patricios J, Pieroth E, Putukian M, Janse van Rensburg DC, Viviers P, Williams V, de Wilde J.
Return to Sports Following Sports-Related Concussion in Collision Sports: An Expert Consensus Statement Using the Modified Delphi Technique Arthroscopy. PMID 37414106
Hohmann E, Bloomfield P, Dvorak J, Echemendia R, Frank RM, Ganda J, Gordon L, Holtzhausen L, Kourie A, Mampane J, Makdissi M, Patricios J, Pieroth E, Putukian M, Janse van Rensburg DC, Viviers P, Williams V, de Wilde J.
On-Field and Pitch-Side (Sideline) Assessment of Sports Concussion in Collision Sports: An Expert Consensus Statement Using the Modified Delphi Technique Arthroscopy. PMID 37391103
Holers VM, Frank RM, Clauw A, Seifert J, Zuscik M, Asokan S, Striebich C, Clay MR, Moreland LW, Banda NK.
Potential causal role of synovial complement system activation in the development of post-traumatic osteoarthritis after anterior cruciate ligament injury or meniscus tear Front Immunol. PMID 37207197
Howell DR, Wingerson MJ, Smulligan KL, Magliato S, Simon S, Wilson JC.
Exercising More Than 150 min/wk After Concussion Is Associated With Sleep Quality Improvements
J Head Trauma Rehabil. PMID 38032838
Hunt KJ, Hewitt MA, Buckley SE, Bartolomei J, Myerson MS, Hogan MV, Laf Committee ISAKOS. Ligament augmentation repair is broadly applied across different orthopaedic subspecialities: an ISAKOS international survey of orthopaedic surgeons
J ISAKOS. PMID 37100118
Hurley ET, Sherman SL, Stokes DJ, Rodeo SA, Shapiro SA, Mautner K, Buford DA, Dragoo JL, Mandelbaum BR, Zaslav KR, Cole BJ, Frank RM; Members of the Biologics Association.
Experts Achieve Consensus on a Majority of Statements Regarding Platelet-Rich Plasma Treatments for Treatment of Musculoskeletal Pathology Arthroscopy. PMID 37625660
Hurley ET, Hughes AJ, Savage-Elliott I, Dejour D, Campbell KA, Mulcahey MK, Wittstein JR, Jazrawi LM; Patellar Instability International Consensus Group; Alaia MJ, Arendt EA, Ayeni OR, Bassett AJ, Bonner KF, Camp CL, Carter CW, Chahla J, Ciccotti MG, Cosgarea AJ, Edgar CM, Erickson BJ, Espregueira-Mendes J, Farr J, Farrow LD, Frank RM, Freedman KB, Fulkerson JP, Getgood A, Gomoll AH, Grant JA, Gursoy S, Gwathmey FW, Haddad FS, Hiemstra LA, Hinckel BB, Koh JL, Krych AJ, LaPrade RF, Li ZI, Logan CA, Gonzalez-Lomas G, Mannino BJ, Lind M, Matache BA, Matzkin E, McCarthy TF, Mandelbaum B, Musahl V, Neyret P, Nuelle CW, Oussedik S, Pace JL, Verdonk P, Rodeo SA, Rowan FE, Salzler MJ, Schottel PC, Shannon FJ, Sheean AJ, Sherman SL, Strickland SM, Tanaka MJ, Waterman BR, Zacchilli M, Zaffagnini S.
A modified Delphi consensus statement on patellar instability: part I Bone Joint J. PMID 38037678
Hurley ET, Sherman SL, Chahla J, Gursoy S, Alaia MJ, Tanaka MJ, Pace JL, Jazrawi LM; Patellar Instability International Consensus Group; Hughes AJ, Arendt EA, Ayeni OR, Bassett AJ, Bonner KF, Camp CL, Campbell KA, Carter CW, Ciccotti MG, Cosgarea AJ, Dejour D, Edgar CM, Erickson BJ, Espregueira-Mendes J, Farr J, Farrow LD, Frank RM, Freedman KB, Fulkerson JP, Getgood A, Gomoll AH, Grant JA, Gwathmey FW, Haddad FS, Hiemstra LA, Hinckel BB, Savage-Elliott I, Koh JL, Krych AJ, LaPrade RF, Li ZI, Logan CA, Gonzalez-Lomas G, Mannino BJ, Lind M, Matache BA, Matzkin E, Mandelbaum B, McCarthy TF, Mulcahey M, Musahl V, Neyret P, Nuelle CW, Oussedik S, Verdonk P, Rodeo SA, Rowan FE, Salzler MJ, Schottel PC, Shannon FJ, Sheean AJ, Strickland SM, Waterman BR, Wittstein JR, Zacchilli M, Zaffagnini S.
A modified Delphi consensus statement on patellar instability: part II
Bone Joint J. PMID 38035602
IIgboechi O, Purtell SR, Carry P, Sanders JS.
Pediatric Pelvic and Acetabular Fractures: Discerning Severity by Classification and Clinical Management
J Pediatr Orthop. PMID 37130809
Iyer S, Adams DJ.
Bone and the Unfolded Protein Response: In Sickness and in Health
Calcif Tissue Int. PMID 37243756
JJacobs CA, Ortiz SF; MOON Shoulder Group; Baumgarten KM, Bishop JY, Bollier MJ, Bravman JT, Brophy RH, Cvetanovich GL, Feeley BT, Frank RM, Jones GL, Kuhn JE, Lansdown DA, Ma CB, Mair SD, Marx RG, McCarty EC, Seidl AJ, Wright RW, Zhang AL, Wolf BR, Hettrich CM.
Development and Validation of a Short-Form Version of the Western Ontario Shoulder Instability Scale (Short-WOSI)
Am J Sports Med. PMID 37584514
KKeenan RA, Poddar SK, Ebinger A, McCarty E.
The Collapsed Athlete: General Principles
Clin Sports Med. PMID 37208051
Kelley N, Hubbard J, Belton M.
Cubital tunnel compression neuropathy in the presence of an anomalous venous complex: a case study
JSES Rev Rep Tech. PMID 37588498
Kelley N, Tuttle M, Sylvia SM, Dragoo JL, Khodaee M.
Acromioclavicular Joint Injuries in Sport
Curr Sports Med Rep. PMID 36866952
Khoriati AA, Shahid Z, Fok M, Frank RM, Voss A, D'Hooghe P, Imam MA.
Artificial Intelligence and the orthopaedic surgeon: a review of the literature and potential applications for future practice: current concepts
J ISAKOS. PMID 37949113
Kolaczko JG, Wait T, Stevanovic O, Orahovats A, Griffith E, Genuario JW.
A Modified "Shuttle" Method Technique for Arthroscopic Hip Capsular Reconstruction in Capsular Deficiency Arthrosc Tech. PMID 37780666
Kraeutler MJ, McCulloch PC, Sherman SL, Vidal AF.
The Principles of Knee Joint Preservation: Operative Treatment Strategies
J Bone Joint Surg Am. PMID 37616413
Kraeutler MJ, McCulloch PC, Vidal AF.
The Principles of Knee Joint Preservation Arthroscopy. PMID 37981384
Kwart A, Pacana M, Otsuka N, Piazza B, Armstrong D, Shaw B, S Segal L, Sorenson S, Fortuna K, Abzug J, Hennrikus W.
Developmental dysplasia of the hip and ultrasound reading by pediatric orthopedic surgeons: a pilot study
J Pediatr Orthop B. PMID 36943679
LLaValva SM, Swarup I, Garg S, Yaszay B, Gupta MC, Sucato DJ, Kelly MP, Samdani A, Lenke L, Boachie O, Cahill PJ; Fox Study Group.
Who gets staged surgery in severe pediatric and adolescent spine deformity?
Spine Deform. PMID 38091233
Layne J, Meyer MA, Catalano LW 3rd.
Metacarpal Neck Osteochondroma: An Atypical Cause of "Trigger Finger"
J Hand Surg Glob Online. PMID 37521543
Leversedge FJ, Safa B, Lin WC, Iorio ML, Merced-O'Neill O, Tajdaran K.
Histologic Comparison of the Fascicular Area of Processed Nerve Allograft Versus Cabled Sural Nerve Autograft
Plast Reconstr Surg Glob Open. PMID 37600836
Lindsay A, Seidl A.
A novel supplementary anchor fixation technique for reinforcing fixation in bone grafting procedures for shoulder instability
JSES Rev Rep Tech. PMID 37588292
Liu RKK, Howell DR, Pierpoint LA, Little CC, Spittler J, Khodaee M, Provance A.
SalterHarris fractures in paediatric skiers and snowboarders
Res Sports Med. PMID 37221842
Look N, Mcnulty M, Rodriguez-Fontan F, Fenoglio AK.
Radial-sided wrist pain differentials: presentation, pathoanatomy, diagnosis, and management Medicina (B Aires). PMID 36774602
Lukasiewicz P, McFarland E, Hassebrock JD, McCarthy TP, Sylvia SM, McCarty EC, Weber SC.
Anatomic glenohumeral arthroplasty: State of the art
J ISAKOS. PMID 37207983
MMagliato SN, Wingerson MJ, Seehusen CN, Smulligan KL, Simon SL, Wilson JC, Howell DR.
Sleep Problems After Concussion Are Associated With Poor Balance and Persistent Postconcussion Symptoms
J Child Neurol. PMID 37122172
Maguire JA, Dhillon J, Sarna N, Keeter C, Scillia AJ, McCulloch PC, Kraeutler MJ.
Screw Fixation for the Latarjet Procedure May Reduce Risk of Recurrent Instability but Increases Reoperation Rate Compared to Suture-Button Fixation: A Systematic Review
Arthroscopy. PMID 38040391
Marty E, Genuario J, Aretakis A, Shinsako K, Frank RM.
Left Knee Open Rectus Femoris Repair With Achilles Allograft Augmentation: A Case Report
JBJS Case Connect. PMID 36706196
Martino R, Carry P, Adams J, Brandt A, Sink E, Selberg C.
The Optimal Age for Surgical Management of DDH Differs by Treatment Method
J Pediatr Orthop. PMID 37970702
McCarthy TP, Frank RM, Stokes DJ, McCarty E.
On-Field Sports Emergencies: Preparation and Readiness
Clin Sports Med. PMID 37208050
McCarty E, Poddar SK, Ebinger A.
On-the-Field Emergencies in Athletics: It Takes a Team! Clin Sports Med. PMID 37208065
Medina-Gomez C, Mullin BH, Chesi A, Prijatelj V, Kemp JP, Shochat-Carvalho C, Trajanoska K, Wang C, Joro R, Evans TE, Schraut KE, Li-Gao R, Ahluwalia TS, Zillikens MC, Zhu K, Mook-Kanamori DO, Evans DS, Nethander M, Knol MJ, Thorleifsson G, Prokic I, Zemel B, Broer L, McGuigan FE, van Schoor NM, Reppe S, Pawlak MA, Ralston SH, van der Velde N, Lorentzon M, Stefansson K, Adams HHH, Wilson SG, Ikram MA, Walsh JP, Lakka TA, Gautvik KM, Wilson JF, Orwoll ES, van Duijn CM, Bønnelykke K, Uitterlinden AG, Styrkársdóttir U, Akesson KE, Spector TD, Tobias JH, Ohlsson C, Felix JF, Bisgaard H, Grant SFA, Richards JB, Evans DM, van der Eerden B, van de Peppel J, Ackert-Bicknell C, Karasik D, Kague E, Rivadeneira F.
Bone mineral density loci specific to the skull portray potential pleiotropic effects on craniosynostosis Commun Biol. PMID 37402774
Meyer MA, Leversedge FJ.
Management of Ulnar Styloid Nonunions
Hand Clin. PMID 37979994
Miller BS, Fung EB, White KK, Lund TC, Harmatz P, Orchard PJ, Whitley CB, Polgreen LE.
Persistent bone and joint disease despite current treatments for mucopolysaccharidosis types I, II, and VI: Data from a 10-year prospective study J Inherit Metab Dis. PMID 36840680
Miller SM, Valovich McLeod TC, Zaslow TL, Wilson JC, Master CL, Snedden TR, Halstead ME, Grady MF, Fazekas ML, Santana JA, Coel RA, Howell DR.
Utility of a Clinical Prediction Tool for Persisting Postconcussive Symptoms in a Multicenter Sample of Youth Athletes With Concussion: The Sport Concussion Outcomes in Pediatrics (SCOPE) Study
Am J Sports Med. PMID 37794642
NNemkov T, Stephenson D, Erickson C, Dzieciatkowska M, Key A, Moore A, Earley EJ, Page GP, Lacroix IS, Stone M, Deng X, Raife TJ, Kleinman SH, Zimring JC, Roubinian NH, Hansen KC, Busch MP, Norris PJ, D'Alessandro A.
Regulation of kynurenine metabolism by blood donor genetics and biology impacts red cell hemolysis in vitro and in vivo Blood. PMID 37976448
Norvell MR, Porter M, Ricco MH, Koonce RC, Hogan CA, Basler E, Wong M, Jeffres MN.
Cefazolin vs Second-line Antibiotics for Surgical Site Infection Prevention After Total Joint Arthroplasty Among Patients With a Beta-lactam Allergy Open Forum Infect Dis. PMID 37363051
OO'Neill NP, Mo AZ, Miller PE, Glotzbecker MP, Li Y, Fletcher ND, Upasani VV, Riccio AI, Spence D, Garg S, Krengel W, Birch C, Hedequist DJ.
The Reliability of the AO Spine Upper Cervical Classification System in Children: Results of a Multi-Center Study
J Pediatr Orthop. PMID 36706430
Ou-Yang DC, Kleck CJ, Ackert-Bicknell CL.
Genetics of Intervertebral Disc Degeneration
Curr Osteoporos Rep. PMID 36680730
Orozco E, Dhillon J, Keeter C, Brown TD, Kraeutler MJ.
Rotator Cuff Repair With Patch Augmentation Is Associated With Lower Retear Rates for Large Tears: A Systematic Review of Randomized Controlled Trials Arthroscopy. PMID 37734446
Ortiz-Catalan M, Zbinden J, Millenaar J, D'Accolti D, Controzzi M, Clemente F, Cappello L, Earley EJ, Mastinu E, Kolankowska J, Munoz-Novoa M, Jönsson S, Cipriani C, Sassu P, Brånemark R.
A highly integrated bionic hand with neural control and feedback for use in daily life Sci Robot. PMID 37820004
PPasic N, Bradsell HL, Barandiaran A, Robinson AS, Cole BJ, Vidal AF, Frank RM.
Rate of Conversion to Matrix-Induced Autologous Chondrocyte Implantation After a Biopsy: A Multisurgeon Study
Orthop J Sports Med. PMID 37188223
Pasic N, Storaci H, Guzman R, Debaun M, Maruyama M, Hall K, Salazar BP, Dragoo JL.
A Biomechanical Comparison of All-Inside Versus Transtibial Meniscus Root Repair Techniques
Am J Sports Med. PMID 37358235
Patsimas T, Howell DR, Hovater W, Drexelius K, Selberg C, Armento A, Mayer S.
Recovery in Hip Range of Motion in Young Flexibility Athletes 1 Year After Periacetabular Osteotomy
J Dance Med Sci. PMID 37864457
Paulson AE, Clement RC, Holt JB, Sanders JS, Louer CR Jr.
Orthopaedic Surgery Subspecialty Podcast Effectively Disseminates Peer-reviewed Articles Relative to Traditional Online Publishing
J Pediatr Orthop. PMID 38131346
Phillips JLH, Ennis HE, Jennings JM, Dennis DA.
Screening and Management of Malnutrition in Total Joint Arthroplasty
J Am Acad Orthop Surg. PMID 36812414
Potyk AG, Belk JW, Bravman JT, Seidl AJ, Frank RM, McCarty EC.
Immobilization in External Rotation Versus Arthroscopic Stabilization After Primary Anterior Shoulder Dislocation: A Systematic Review of Level 1 and 2 Studies
Am J Sports Med. PMID 36867050
Purtell SR, Thornhill D, Loi M, Lockwood J, Kim JS, MacBrayne CE, DeVine MN, Sanders J, Searns J.
Risk Factors for Venous Thromboembolic Events in Children With Acute Musculoskeletal Infections
J Pediatr Orthop. PMID 36922007
RRademacher JG, Wingerson MJ, Smulligan KL, Little CC, Wilson JC, Howell DR.
Early Moderate to Vigorous Physical Activity After Concussion Is Associated With Faster Symptom Resolution Time
J Sport Rehabil.PMID 37295788
Ratto AB, Bascom J, daVanport S, Strang JF, Anthony LG, Verbalis A, Pugliese C, Nadwodny N, Brown LXZ, Cruz M, Hector BL, Kapp SK, Giwa Onaiwu M, Raymaker
DM, Robison JE, Stewart C, Stone R, Whetsell E, Pelphrey K, Kenworthy L.
Centering the Inner Experience of Autism: Development of the Self-Assessment of Autistic Traits
Autism Adulthood. PMID 36941856
Richman EH, Richman OT, Lee MS, Qubain L, Heylmun L, Awad ME, Alfonso N.
Social Media and Digital Footprints in Orthopaedic Trauma: An Analysis of 1465 Orthopaedic Trauma Association Members
J Orthop Trauma. PMID 37559214
Rilk S, Saithna A, Achtnich A, Ferretti A, Sonnery-Cottet B, Kösters C, Bottoni CR, Monaco E, Cavaignac E, Ahlbaeumer G, Brandl G, Mackay GM, Vermeijden HD, Dallo I, Pace JL, van der List JP, Moggia JR, Chahla J, Batista JP, Frosch KH, Schneider KN, Smith PA, Frank RM, Hoogeslag RAG, Eggli S, Douoguih WA, Petersen W, DiFelice GS.
The modern-day ACL surgeon's armamentarium should include multiple surgical approaches including primary repair, augmentation, and reconstruction: A letter to the Editor
J ISAKOS. PMID 37023928
Roda GF, Awad ME, Melton DH, Christiansen CL, Stoneback JW, Gaffney BMM.
The Amputated Limb Gluteus Medius is Biomechanically Disadvantaged in Patients with Unilateral Transfemoral Amputation
Ann Biomed Eng. PMID 37946055
Rodriguez Fontan F, Douleh D, Federer A, Lindeque B.
Giant Cell Tumor of the Wrist After Fracture Osteosynthesis: A Case Report Cureus. PMID 36843756
Rodriguez-Fontan F, Tucker NJ, Pflug EM, Leversedge FJ, Catalano LW, Lauder A.
Proximal Hamate Reconstruction of Proximal Pole Scaphoid Nonunion: A Case Series and Analysis of Clinical Outcomes Hand (N Y). PMID 37161279
Rohde MS, Shea KG, Dawson T 2nd, Heyworth BE, Milewski MD, Edmonds EW, Adsit E, Wilson PL; SCORE Group; Albright J, Algan S, Beck J, Bowen R, Brey J, Cardelia M, Clark C, Crepeau A, Edmonds EW, Ellington M, Ellis HB, Fabricant P, Frank J, Ganley T, Green D, Gupta A, Heyworth BE, Latz K, Mansour A, Mayer S, McKay S, Milewski M, Niu E, Pacicca D, Parikh S, Rhodes J, Saper M, Schmale G, Schmitz M, Shea K, Storer S, Wilson PL, Ellis HB.
Age, Sex, and BMI Differences Related to Repairable Meniscal Tears in Pediatric and Adolescent Patients
Am J Sports Med. PMID 36629442
Rosenthal RM, Featherall J, Parkes CW, Khalil AZ, Genuario JW, Maak TG, Aoki SK.
Acetabular Labral Reconstruction: Review of Techniques and Outcomes
Curr Rev Musculoskelet Med. PMID 37493964
SSalton RL, Carry PM, Hadley-Miller N, Murphy-Zane MS, Brazell C, Novais E, Georgopoulos G. Prediction of Late Dysplasia Based on Ultrasound and Plain X-Ray at 6 Months. J Pediatr Orthop. PMID 36607921
Schutz J, Lalka A, Williams MA, Sibbel SE, Sinclair MK.
Establishing the Role of Inflammatory Markers in the Diagnosis and Treatment of Acute Hand Infections in the Pediatric Population J Pediatr Orthop. PMID 37678156
Seehusen CN, Howell DR, Potter MN, Walker GA, Provance AJ.
Athlete Burnout Is Associated With Perceived Likelihood of Future Injury Among Healthy Adolescent Athletes Clin Pediatr (Phila). PMID 36908104
Shapiro LM, Chang J, Fox PM, Kozin S, Chung KC, Dyer GSM, Fufa D, Leversedge F, Katarincic J, Kamal R.
The Development and Validation of Data Elements and Process Steps for an Electronic Health Record for Hand Surgery Outreach Trips
J Hand Microsurg. PMID 38152677
Shapiro LM, Welch J, Leversedge C, Katarincic JA, Leversedge FJ, Dyer GSM, Kozin SH, Fox PM, McCullough M, Agins B, Kamal RN. Capacity Assessment Tool to Promote Capacity Building in Global Orthopaedic Surgical Outreach
J Bone Joint Surg Am. PMID 37319177
Shah VN, Qui S, Stoneback J, Qamar L, Ferguson VL, Kohrt WM, Snell-Bergeon JK, Rao SD. Bone Structure and Turnover in Postmenopausal Women With Long-Standing Type 1 Diabetes JBMR Plus. PMID 38025041
MOON Knee Group: Sheean AJ, Jin Y, Huston LJ, Brophy RH, Cox CL, Flanigan DC, Jones MH, Kaeding CC, Magnussen RA, Marx RG, Matava MJ, McCarty EC, Parker RD, Wolcott ML, Wolf BR, Wright RW, Spindler KP.
Predictors of Return to Activity at 2 Years After Anterior Cruciate Ligament Reconstruction Among Patients With High Preinjury Marx Activity Scores: A MOON Prospective Cohort Study
Am J Sports Med. PMID 37724692
Silverstein RS, McKay SD, Coello P, Pupa L, Latz K, Craig Kemper W, Adsit E, Wilson PL; Members of the SCORE Quality Improvement Registry; Albright J, Algan S, Beck J, Bowen RE, Brey J, Marc Cardelia J, Clark C, Crepeau A, Edmonds E, Ellington M, Fabricant PD, Frank JS, Ganley TJ, Green DW, Gupta A, Heyworth B, Mansour A, Mayer S, Milewski MD, Niu E, Pacicca DM, Parikh SN, Rhodes J, Saper M, Schmale GA, Schmitz M, Shea K, Storer S, Ellis HB Jr.
Relationship Between Age and Pathology With Treatment of Pediatric and Adolescent Discoid Lateral Meniscus: A Report From the SCORE Multicenter Database
Am J Sports Med. PMID 37899536
Skedros JG, Dayton MR, Bloebaum RD, Bachus KN, Cronin JT.
Strain-mode-specific mechanical testing and the interpretation of bone adaptation in the deer calcaneus
J Anat. PMID 37953064
Skedros JG, Cronin JT, Dayton MR, Bloebaum RD, Bachus KN. Exploration of the synergistic role of cortical thickness asymmetry ("Trabecular Eccentricity" concept) in reducing fracture risk in the human femoral neck and a control bone (Artiodactyl Calcaneus)
J Theor Biol. PMID 37068584
Smulligan KL, Wingerson MJ, Little CC, Wilson JC, Howell DR.
Early physical activity after concussion is associated with sleep quality but not dizziness among adolescent athletes
J Sci Med Sport. PMID 36804710
Sorrentino R, Carlson KJ, Orr CM, Pietrobelli A, Figus C, Li S, Conconi M, Sancisi N, Belvedere C, Zhu M, Fiorenza L, Hublin JJ, Jashashvili T, Novak M, Patel BA, Prang TC, Williams SA, Saers JPP, Stock JT, Ryan T, Myerson M, Leardini A, DeSilva J, Marchi D, Belcastro MG, Benazzi S.
Morphological and evolutionary insights into the keystone element of the human foot's medial longitudinal arch
Commun Biol. PMID 37857853
Stokes DJ, McCarthy TP, Frank RM.
Physical Therapy for the Treatment of Shoulder Instability
Phys Med Rehabil Clin N Am. PMID 37003660
Sumalde AAM, Scholes MA, Kalmanson OA, Terhune EA, Frejo L, Wethey CI, Roman-Naranjo P, Carry PM, Gubbels SP, Lopez-Escamez JA, Hadley-Miller N, SantosCortez RLP.
Rare Coding Variants in Patients with Non-Syndromic Vestibular Dysfunction
Genes (Basel). PMID 37107589
Sylvia SM, Stokes DJ, McCarthy TP, Hassebrock JD, Shinsako KK, Frank RM.
Low-Profile Cartilage Repair With Knotless All-Suture Anchors: Surgical Technique Arthrosc Tech. PMID 37533926
TTaylor ZR, Hamblin RW, Shaw BA, Navas-Solares JC, Shaw LF.
Special Report: The Moore Pediatric Surgery Center: An Evolving Model for Pediatric Orthopaedic Surgical Care in a Limited Resource Environment
J Pediatr Orthop. PMID 36649473
Tetreault TA, Garg S.
Return to play following spine surgery
Front Pediatr. PMID 37138567
Tabbaa SM, Pace JL, Frank RM, Grammens J, Verdonk P.
Meniscus Size Differs Between Patient and Donor Populations for Meniscus Allograft Transplantation Arthrosc Sports Med Rehabil. PMID 37388864
Terhune E, Heyn P, Piper C, Wethey C, Monley A, Cuevas M, Hadley Miller N.
Association between genetic polymorphisms and risk of adolescent idiopathic scoliosis in case-control studies: a systematic review
J Med Genet. PMID 37696603
Tepavcevic S, Romic S, Zec M, Culafic T, Stojiljkovic M, Ivkovic T, Pantelic M, Kostic M, Stanisic J, Koricanac G. Effects of Walnut-Rich Diet on Cation-Handling Proteins in the Heart of Healthy and Metabolically Compromised Male Rats
J Med Food. PMID 37889606
Tanguilig G, Kraeutler MJ, Mulcahey MK.
Virtual Interviews Are Not Adequate Replacements for In-Person Interviews for Orthopaedic Sports Medicine Fellowship Program Directors and Applicants
Arthrosc Sports Med Rehabil. PMID 38155814
Valovich McLeod TC, Snedden T, Halstead M, Wilson J, Master C, Grady M, Fazekas M, Santana J, Zaslow T, Miller S, Coel R, Howell DR; PRiSM Concussion Research Interest Group.
Influence of Personal and Injury-Related Factors Predicting Deficits in Quality of Life Domains Among Pediatric Athletes: Findings From the Sport Concussion Outcomes in Pediatrics Study
Clin J Sport Med. PMID 36858431
Vandenberg NW, Stoneback JW, Davis-Wilson H, Christiansen CL, Awad ME, Melton DH, Gaffney BMM.
Unilateral transfemoral osseointegrated prostheses improve joint loading during walking
J Biomech. PMID 37276681
WWagner KJ 3rd, Beck JJ, Carsen S, Crepeau AE, Cruz AI Jr, Ellis HB Jr, Mayer SW, Niu E, Pennock AT, Stinson ZS, VandenBerg C, Ellington MD.
Variability in Pain Management Practices for Pediatric Anterior Cruciate Ligament Reconstruction
J Pediatr Orthop. PMID 36728478
Wait TJ, Kolaczko JG, Stevanovic O, Orahovats A, Boublik M, Mayer SW, Genuario JW.
Lateral Extra-articular Tenodesis: The Onlay Technique
Arthrosc Tech. PMID 37654867
Weinstein MA, Beaumont A, Campbell P, Hassanzadeh H, Patel V, Vokshoor A, Wind J, Radcliff K, Aleem I, Coric D.
Pulsed Electromagnetic Field Stimulation in Lumbar Spine Fusion for Patients With Risk Factors for Pseudarthrosis
Int J Spine Surg. PMID 37884337
Welton KL, Kraeutler MJ, Garabekyan T, Mei-Dan O.
Radiographic Parameters of Adult Hip Dysplasia
Orthop J Sports Med. PMID 36874050
Whang PG, Patel V, Duhon B, Sturesson B, Cher D, Carlton Reckling W, Capobianco R, Polly D.
Minimally Invasive SI Joint Fusion Procedures for Chronic SI Joint Pain: Systematic Review and Meta-Analysis of Safety and Efficacy
Int J Spine Surg PMID 37798076
Willwerth SB, Lempke LB, Lugade V, Meehan WP, Howell DR, DeJong Lempke AF.
Ankle Sprain History Does Not Significantly Alter Single- and Dual-Task Spatiotemporal Gait Mechanics
J Sport Rehabil. PMID 37758257
Wingerson MJ, Baugh CM, Provance AJ, Armento A, Walker GA, Howell DR.
Changes in Quality of Life, Sleep, and Physical Activity During COVID-19: A Longitudinal Study of Adolescent Athletes
J Athl Train. PMID 36827615
Wingerson MJ, Magliato SN, Smulligan KL, Wilson JC, Little CC, Howell DR.
Predicting Time to Evaluation After Pediatric Concussion: Factors Affecting Specialty Concussion Care
Orthop J Sports Med. PMID 37655238
MARS Group: Wright RW, Huston LJ, Haas AK, Pennings JS, Allen CR, Cooper DE, DeBerardino TM, Dunn WR, Lantz BBA, Spindler KP, Stuart MJ, Albright JP, Amendola AN, Andrish JT, Annunziata CC, Arciero RA, Bach BR Jr, Baker CL 3rd, Bartolozzi AR, Baumgarten KM, Bechler JR, Berg JH, Bernas GA, Brockmeier SF, Brophy RH, Bush-Joseph CA, Butler JB 5th, Campbell JD, Carey JL, Carpenter JE, Cole BJ, Cooper JM, Cox CL, Creighton RA, Dahm DL, David TS, Flanigan DC, Frederick RW, Ganley TJ, Garofoli EA, Gatt CJ Jr, Gecha SR, Giffin JR, Hame SL, Hannafin JA, Harner CD, Harris NL Jr, Hechtman KS, Hershman EB, Hoellrich RG, Johnson DC, Johnson TS, Jones MH, Kaeding CC, Kamath GV, Klootwyk TE, Levy BA, Ma CB, Maiers GP 2nd, Marx RG, Matava MJ, Mathien GM, McAllister DR, McCarty EC, McCormack RG, Miller BS, Nissen CW, O'Neill DF, Owens BD, Parker RD, Purnell ML, Ramappa AJ, Rauh MA, Rettig AC, Sekiya JK, Shea KG, Sherman OH, Slauterbeck JR, Smith MV, Spang JT, Svoboda LSJ, Taft TN, Tenuta JJ, Tingstad EM, Vidal AF, Viskontas DG, White RA, Williams JS Jr, Wolcott ML, Wolf BR, York JJ. Meniscal and Articular Cartilage Predictors of Outcome After Revision ACL Reconstruction: A 6-Year Follow-up Cohort Study
Am J Sports Med. PMID 36734487
Wu EY, Singh NP, Choi K, Zakeri M, Vincent M, Churchill GA, Ackert-Bicknell CL, Patro R, Love MI.
SEESAW: detecting isoform-level allelic imbalance accounting for inferential uncertainty
Genome Biol. PMID 37438847
YYamamoto N, Szymski D, Voss A, Ishikawa H, Muraki T, Cunha RA, Ejnisman B, Noack J, McCarty E, Mulcahey MK, Itoi E. Non-operative management of shoulder osteoarthritis: Current concepts
J ISAKOS. PMID 37321293
Yamamura MK, Carry PM, Gibly RF, Holmes K, Ogilvie B, Phillips A, Georgopoulos G, Miller NH, Payne KA. Epidemiology of Physeal Fractures and Clinically Significant Growth Disturbances Affecting the Distal Tibia, Proximal Tibia, and Distal Femur: A Retrospective Cohort Study
J Am Acad Orthop Surg. PMID 37054395
Yankey KP, Owusu DN, Sackeyfio A, Wulff I, Duah HO, Gross LF, Lenke LG, Sponseller P, Shah S, Erickson MA, Sides B, Newton P, Bumpass D, Gupta M, Ravinsky R, Boachie-Adjei O; Fox Pediatric Spinal Deformity Study; FOCOS Research Group. Medical complications and health-related quality of life in complex pediatric spine deformities exceeding 100 degrees or treated by 3CO Spine Deform. PMID 36826693
Young-Xu Y, Epstein L, Marconi VC, Davey V, Korves C, Zwain G, Smith J, Cunningham F, Bonomo RA, Ginde AA.
Tixagevimab/cilgavimab for preventing COVID-19 during the Omicron surge: retrospective analysis of National Veterans Health Administration electronic data mBio. PMID 37535398
ZZbinden J, Sassu P, Mastinu E, Earley EJ, Munoz-Novoa M, Brånemark R, Ortiz-Catalan M.
Improved control of a prosthetic limb by surgically creating electro-neuromuscular constructs with implanted electrodes
Sci Transl Med. PMID 37437016
Zhou Y, Guglielmi G, Garg S, Hankinson TC.
Delayed Diagnosis of Cervical Epidural Hematoma in a 3-Year-Old Boy: A Case Report
JBJS Case Connect. PMID 37651573

QR code for digital format of this report