82 Gifts
Publishing research that propels orthopedic science forward, our faculty exemplify "The Brightest Minds, The Boldest Ideas".
Their diverse array of studies spans cutting-edge techniques, innovative treatments, and patient-centered care improvements. Each publication highlights our commitment to addressing pressing challenges and fostering collaboration to shape the future of orthopedics.
These contributions not only enhance global medical knowledge, but they reaffirm our department’s leadership position in advancing research, education, and clinical care on a transformative scale.
This index of publications was generated based on the date the citation record was first created in PubMed Peer reviewed publications created in calendar year 2024 are listed in alphabetical order by first author Visit the NIH National Library of Medicine for the complete PubMed User Guide
AAdhikari B, Stager MA, Collins EG, Fischenich KM, Olusoji J, Ruble AF, Payne KA, Krebs MD. Sustained release of MAPK14-targeting siRNA from polyelectrolyte complex hydrogels mitigates MSC osteogenesis in vitro with potential application in growth plate injury
J Biomed Mater Res A. PMID 39145460
Alexeev SO, Trikha R, Short S, Hunt KJ
The Antigravity Treadmill as a Postoperative and Injury Rehabilitation Tool: Reduction in Contact Forces and Muscle Activity With Reduced Weight Running Clin J Sport Med PMID 39133106
Ammons DT, Chow L, Goodrich L, Bass L, Larson B, Williams ZJ, Stoneback JW, Dow S, Pezzanite LM
Characterization of the single cell landscape in normal and osteoarthritic equine joints
Ann Transl Med PMID 39507442
Aretakis AC, Farrell JP, Ou-Yang DC, Kleck CJ
Intraoperative fat embolism syndrome associated with implantation of titanium sacroiliac joint fusion implants: a report of two cases
J Spine Surg PMID 38567009
Armento AM, Brna M, Seehusen C, McCarthy A, VanBaak KD, Howell DR
Examination of Sex Differences in Energy Availability, Disordered Eating, and Compulsive Exercise Among Male and Female Adolescent Athletes Clin J Sport Med PMID 39570011
Awad ME, Griffin NA, Epperson AB, Alfonso NA, Ou-Yang D
Extended Postoperative Antibiotic Prophylaxis Is Associated with No Clinical Value and Higher Projected Cost Following Adult Spinal Surgery: A Stratified Meta-Analysis and Probability-Based Cost Projections JBJS Rev PMID 39226392
Awad ME, Melton D, Shaw KG, Lev G, Gaffney BMM, Christiansen CL, Stoneback JW. How Comprehensive and Efficient Are Patient-Reported Outcome Measures for Individuals with Lower Extremity Amputation Undergoing Implantation of Osseointegrated Bone Anchored Limbs?
JBJS Rev PMID 38489397
BBarthold JE, Cai L, McCreery KP, Fischenich KM, Eckstein KN, Ferguson VL, Emery NC, Breur G, Neu CP. Integrative cartilage repair using acellular allografts for engineered structure and surface lubrication in vivo NPJ Regen Med. PMID 39341829
Bedi A, Smith BL, Mitchell JJ, Frank RM, Hauck OL, Wijdicks CA. Effect of Quadriceps Tendon Autograft Preparation and Fixation on Graft Laxity During Suspensory Anterior Cruciate Ligament Reconstruction: A Biomechanical Analysis Orthop J Sports Med PMID 39391073
Bermudez B, Brown KC, Vahidi G, Ferreira Ruble AC, Heveran CM, Ackert-Bicknell CL, Sherk VD
Sex-specific effects of Fat-1 transgene on bone material properties, size, and shape in mice JBMR Plus. PMID 38523667
Bourgeau M, Marshall CB, Schowinsky JT, Lindeque B, Clay MR.
Synthetic Electrospun Fiber Matrix May Resemble Fungal Hyphae Over the Course of Tissue Regeneration: A Retrospective Review
Int J Surg Pathol. PMID 39471849
Bradsell H, Frank RM.
Anterior cruciate ligament injury prevention Ann Jt. PMID 38529144
Bullock GS, Thigpen CA, Zhao H, Devaney L, Kline D, Noonan TJ, Kissenberth MJ, Shanley E. Neck range of motion prognostic factors in association with shoulder and elbow injuries in professional baseball pitchers J Shoulder Elbow Surg. PMID 39396612
Burger E, Ghanayem A, Mulcahey MK.
AOA Critical Issues: Promoting Leadership Development Among Orthopaedic Faculty J Bone Joint Surg Am. PMID 38557798
CCarry PM, Vanderlinden LA, Johnson RK, Buckner T, Steck AK, Kechris K, Yang IV, Fingerlin TE, Fiehn O, Rewers M, Norris JM.
Longitudinal changes in DNA methylation during the onset of islet autoimmunity differentiate between reversion versus progression of islet autoimmunity
Front Immunol PMID 38915393
Chin G, Kraeutler MJ, Batiste A, McCarty C, McCarty EC
Management of the In-Season Athlete with an Anterior Shoulder Dislocation
J Shoulder Elbow Surg PMID 39094761
Churchill L, John Bade M, Koonce RC, Stevens-Lapsley JE, Bandholm T.
The past and future of peri-operative interventions to reduce arthrogenic quadriceps muscle inhibition after total knee arthroplasty: A narrative review
Osteoarthr Cartil Open. PMID 38304413
CreveCoeur TS, Iyer RR, Goldstein HE, Delgardo MW, Hankinson TC, Erickson MA, Garg S, Skaggs DL, Andras L, Kennedy BC, Cahill PJ, Lenke LG, Angevine PD, Roye BD, Vitale MG, Mendiratta A, Anderson RCE
Timing of intraoperative neurophysiological monitoring (IONM) recovery and clinical recovery after termination of pediatric spinal deformity surgery due to loss of IONM signals
Spine J PMID 38614157
Cronin KJ, Calcei JG, Port J, Wright MA, Hll BW, Reynolds AW, Sabasen VJ, Abboud JA, Bushnell BD, Franke MA, American Shoulder Elbow Surgeons Political Advocacy Committee, Schlegel TF
American Shoulder & Elbow Surgeons Perspectives on Political Advocacy
J Shoulder Elbow Surg PMID 39009181
DDaley MM, Howell DR, Lanois CJ, Berkner PD, Mannix RC, Oldham JR, Meehan WP 3rd. Concussion Symptoms and Neurocognitive Performance of Children and Adolescents on Antidepressants Med Sci Sports Exerc PMID 38233981
Desai VM, Bowen M, Anari JB, Flynn JM, Brooks JT, Snyder B, Ramo B, Li Y, Andras LM, Truong WH, Fitzgerald R, El-Hawary R, Roye B, Yaszay B, Kwan KYH, McIntosh A, Nelson S, Gupta P, Erickson M, Garg S, Cahill PJ, Pediatric Spine Study Group. Rib-on-Pelvis Deformity and Reported Pain in Neuromuscular Early-Onset Scoliosis J Pediatr Orthop PMID 38987900
Dhillon J, Keeter C, Kraeutler MJ. Does Calculation of the MCID Make Sense? Ways to Improve Arthroscopy PMID 38206251
Dhillon J, Kraeutler MJ.
Spin and Statistical Fragility: What Are They and How to Avoid Them Arthroscopy PMID 38296428
Dhillon J, Tanguilig G, Keeter C, Borque KA, Heard WM, Kraeutler MJ
Insufficient Evidence for Anterior Cruciate Ligament Reconstruction Utilizing Suture Tape Augmentation: A Systematic Review of Clinical Outcomes at Minimum 1-Year Follow-up Arthroscopy PMID 38309447
Dhillon J, Tanguilig G, Kraeutler MJ
Virtual and Augmented Reality Simulators Show Intraoperative, Surgical Training, and Athletic Training Applications: A Scoping Review Arthroscopy PMID 38387769
Donaka R, Zheng H, Ackert-Bicknell CL, Karasik D. Early life lipid overload in Native American Myopathy is phenocopied by stac3 knockout in zebrafish Gene PMID 39592070
Dragoo JL, Hirpara A, Constantine E, Williams KG, Fry SA, Kandil R.
Intraosseous Treatment of Bone Marrow Lesions in the Knee: Surgical Technique
Arthrosc Tech PMID 39036410
Dragoo JL, Hirpara A, Sylvia S, McCarthy T, Constantine E, Pappas G.
Arthroscopic Lateral Retinacular-Lengthening Procedure
Arthrosc Tech PMID 39036392
Drossopoulos PN, Sharma A, Ononogbu-Uche FC, Tabarestani TQ, Bartlett AM, Wang TY, Huie D, Gottfried O, Blitz J, Erickson M, Lad SP, Bullock WM, Shaffrey CI, Abd-El-Barr MM.
Pushing the Limits of Minimally Invasive Spine Surgery-From Preoperative to Intraoperative to Postoperative Management
J Clin Med PMID 38673683
EEarley EJ, Zbinden J, Munoz-Novoa M, Just F, Vasan C, Holtz AS, Emadeldin M, Kolankowska J, Davidsson B, Thesleff A, Millenaar J, Jonsson S, Cipriani C, Granberg H, Sassu P, Branemark R, OrtizCatalan M
Cutting Edge Bionics in Highly Impaired Individuals: A Case of Challenges and Opportunities
IEEE Trans Neural Syst Rehabil Eng. PMID 38363669
Eckhardt SC, Richardson CM, White KK, Parikh SR, Bonilla-Velez J, Dahl JP
Rates of tracheostomy in patients with complex skeletal dysplasia: A 32-year institutional experience
Int J Pediatr Otorhinolaryngol. PMID 39405659
Epperson AB, Awad ME, Gorman M, Loker K, Alfonso NA, Stoneback JW. Clinical practice guidelines for antimicrobial-loaded cements and beads in orthopedic trauma and arthroplasty Eur J Orthop Surg Traumatol. PMID 39585403
FFelan NA, Garcia-Creighton E, Hirpara A, Narváez I, Miller A, Batiste AJ, Stokes DJ, Tseng R, Santiago A, Smyth A, Pulciano NR, Wharton BR, McCarty EC, Muffly TM.
Navigating the Orthopaedic Maze as a New Patient: A National Mystery Caller Study on Medicaid Coverage and Access to Specialized Surgeons
J Am Acad Orthop Surg PMID 39637372
Foessl I, Ackert-Bicknell CL, Kague E, Laskou F, Jakob F, Karasik D, Obermayer-Pietsch B, Coauthors, Alonso N, Bjørnerem Å, Brandi ML, Busse B, Calado Â, Cebi AH, Christou M, Curran KM, Hald JD, Semeraro MD, Douni E, Duncan EL, Duran I, Formosa MM, Gabet Y, Ghatan S, Gkitakou A, Hassler EM, Högler W, Heino TJ, Hendrickx G, Khashayar P, Kiel DP, Koromani F, Langdahl B, Lopes P, Mäkitie O, Maurizi A, Medina-Gomez C, Ntzani E, Ohlsson C, Prijatelj V, Rabionet R, Reppe S, Rivadeneira F, Roshchupkin G, Sharma N, Søe K, Styrkarsdottir U, Szulc P, Teti A, Tobias J, Valjevac A, van de Peppel J, van der Eerden B, van Rietbergen B, Zekic T, Zillikens MC.
A perspective on muscle phenotyping in musculoskeletal research
Trends Endocrinol Metab PMID 38553405
Ford E, Frank R, Pontes M, McMillan S
Improved Network Integrity and Patient Follow-up After In-Office Needle Arthroscopy Compared to Outpatient Advanced Diagnostic Imaging for Intra-articular Pathology
Arthrosc Sports Med Rehabil PMID 38379598
Fratus A, Nirunsuk P, Feng X, Mauffrey C
A survey on the perspective and benefits of being an international Visiting Surgeon at a leading Level I Trauma centre
Int Orthop PMID 39556265
GGaffney BMM, Thomsen PB, Leijendekkers RA, Christiansen CL, Stoneback JW. Lumbopelvic movement coordination during walking improves with transfemoral bone anchored limbs: Implications for low back pain
Gait Posture. PMID 38432038
Garg S, Heffernan M, Feddema T, Luhmann S, Sturm P, Vitale M, Andras L, White K, Carry P; Pediatric Spine Study Group.
Actuator Size of Magnetic Controlled Growth Rod (7 cm vs. 9 cm) is Not Predictive of Unplanned Return to the Operating Room: A Retrospective Multicenter Comparative Cohort Study J Pediatr Orthop PMID 39466293
Georgiadis AG, Davids JR, Goodbody CM, Howard JJ, Karamitopoulos MS, Payares-Lizano M, Pierz KA, Rhodes JT, Shore BJ, Shrader MW, Tabaie SA, Thompson RM, Torres-Izquierdo B, Wimberly RL, Hosseinzadeh P, Research in Neuromuscular Orthopaedics (RINO) Study Group
Reliability of a Photo-Based Modified Foot Posture Index (MFPI) in Quantifying Severity of Foot Deformity in Children With Cerebral Palsy J Pediatr Orthop PMID 39256907
Gilley SP, Ta A, Pryor W, Ropper B, Erickson M, Fenton LZ, Tchou MJ, Cotter JM, Moore JM. What Do We C in Children With Scurvy? A Case Series Focused on Musculoskeletal Symptoms Hosp Pediatr PMID 38234212
Gilligan C, Volschenk W, Russo M, Green M, Gilmore C, Mehta V, Deckers K, De Smedt K, Latif U, Sayed D, Georgius P, Gentile J, Mitchell B, Langhorst M, Huygen F, Baranidharan G, Patel V, Mironer E, Ross E, Carayannopoulos A, Hayek S, Gulve A, Van Buyten JP, Tohmeh A, Fischgrund J, Lad S, Ahadian F, Deer T, Klemme W, Rauck R, Rathmell J, Maislin G, Heemels JP, Eldabe S.
Five-Year Longitudinal Follow-Up of Restorative Neurostimulation Shows Durability of Effectiveness in Patients With Refractory Chronic Low Back Pain Associated With Multifidus Muscle Dysfunction PMID 38483366
Girardi NG, Kraeutler MJ, Jesse MK, Lee JH, Genuario JW, Mei-Dan O The Windshield Wiper Sign Is an Instability-Related Osteochondral Defect of the Anterolateral Femoral Head Arthroscopy
PMID 38697329
Girardi NG, Kraeutler MJ, Lee JH, Merkle AN, Mei-Dan O. Arthroscopic Femoral Head Allograft With Proximal Femoral/Periacetabular Osteotomies for Sequelae of Perthes: A Case Report
JBJS Case Connect. PMID 38635784
Girardi NG, Lee JH, Genuario JW, Vogel LA, Kraeutler MJ, Keeter C, Mei-Dan O The Everted Acetabular Labrum: Outcomes of Surgical Management Am J Sports Med PMID 38544383
Girardi NG, Malin S, Zielenski C, Lee JH, Henry K, Kraeutler MJ, Mei-Dan O.
Association Between Low-Dose Ketamine After Periacetabular and/or Femoral Osteotomy and Postoperative Opioid Requirements Orthop J Sports Med PMID 39131097
Goltz DE, Khan AZ, Cronin KJ, Williams GR, Romeo AA, Schlegel TF, Frankle MA, Abboud JA Protecting patients and ourselves: conversations with our leaders on advocacy J Shoulder Elbow Surg. PMID 39326659
HHarris C, Mauffrey C, Junior C.
Enhancing orthopaedic surgery research: developing manuscripts using systematic checklists Int Orthop. PMID 39305315
Hassebrock JD, McCarty EC.
Evaluating the Athlete with Instability from on the Field to in the Clinic Clin Sports Med PMID 39232566
Healy KM, Ritter J, Barr E, Churchill JL, Trasolini NA, Waterman BR, Reynolds AW Osteoporosis Management for Shoulder Surgeons
Curr Rev Musculoskelet Med. PMID 39276194
Herrero C, Wasterlain A, Bloom DA, Pham H, Weinberg M, Dragoo JL, Strauss EJ. Leukocyte-Poor Platelet-Rich Plasma as a Treatment for Patellar Tendinopathy A Multicenter, Randomized Controlled Trial
Bull Hosp Jt Dis (2013) PMID 39259953
Herzberg SD, Zhao Z, Freeman TH, Prakash R, Baumgarten KM, Bishop JY, Carey JL, Jones GL, McCarty EC, Spencer EE, Vidal AF, Jain NB, Giri A, Kuhn JE, Khazzam MS, Matzkin EG, Brophy RH, Dunn WR, Ma CB, Marx RG, Poddar SK, Smith MV, Wolf BR, Wright RW. Obesity is associated with muscle atrophy in rotator cuff tear
BMJ Open Sport Exerc Med PMID 38974096
Hipp J, Grieco T, Newman P, Patel V, Reitman C.
Reference Data for Diagnosis of Spondylolisthesis and Disc Space Narrowing Based on NHANES-II X-rays Bioengineering (Basel) PMID 338671782
Hipp JA, Mikhael MM, Reitman CA, Buser Z, Patel VV, Chaput CD, Ghiselli G, DeVine J, Berven S, Nunley P, Grieco TF
Diagnosis of spine pseudoarthrosis based on the biomechanical properties of bone Spine J. PMID 39154949
Hirpara A, Carpenter M, Dayton M, Hogan C.
Antiphospholipid Syndrome Increases Postoperative Complications After Total Hip and Knee Arthroplasty
Orthopedics PMID 38935847
Hirpara A, Koshak C, Marty E, Gallus C, Kleck C
Outcomes and Spinopelvic Changes After Anterior Lumbar Interbody Fusion With a Novel Interbody Fusion Device: A Retrospective Study
Int J Spine Surg PMID 39079745
Hoffman CJ, France T, Cram T, Bodmer JL, Sanders JS.
Pediatric Multidrug-Resistant Disseminated Tuberculosis Presenting as Small Finger Tuberculous Osteomyelitis: A Case Report
JBJS Case Connect. PMID 38306445
Hohmann E, Keough N, Frank RM, Rodeo S
Micro-Fragmented Adipose Tissue Demonstrates Comparable Clinical Efficacy to Other Orthobiologic Injections in Treating Symptomatic Knee Osteoarthritis: A Systematic Review of Level I to IV Clinical Studies
Arthroscopy PMID 38467171
Holers VM, Frank RM, Zuscik M, Keeter C, Scheinman RI, Striebich C, Simberg D, Clay MR, Moreland LW, Banda NK.
Decay-Accelerating Factor Differentially Associates With Complement-Mediated Damage in Synovium After Meniscus Tear as Compared to Anterior Cruciate Ligament Injury
Immune Netw. PMID 38725672
Hop JC, Belk JW, Mayer BK, Frank RM, Seidl AJ, McCarty EC, Bravman JT
Outcomes of Total Shoulder Arthroplasty With and Without Prior Rotator Cuff Repair: A Systematic Review Orthop J Sports Med. PMID 39221043
Hosseinzadeh P, Torres-Izquierdo B, Tippabhatla A, Denning J, Vidyadhar U, Sanders J, Goldstein R, Baldwin K.
Operative Versus Nonoperative Treatment of Displaced Proximal Humerus Fractures in Adolescents: Results of a Prospective Multicenter Study
J Pediatr Orthop PMID 38912592
Hunt KJ, Ross D, Fontan F.
Clinical Outcomes and Registry Data in Total Ankle Arthroplasty
Foot Ankle Clin PMID 38309795
Hunt KJ.
Nitinol Staples in Foot and Ankle Surgery: Panacea or the Next Bubble? Foot Ankle Int PMID 38850060
JJohnson AJ, Wharton BR, Geraghty EH, Bradsell H, Ishikawa A, McCarty EC, Bravman JT, Frank RM
Patient Perception of Social Media Use by Orthopaedic Surgeons: A Pilot Study. Orthop J Sports Med PMID 38465258
Johnson RK, Ireton AJ, Carry PM, Vanderlinden LA, Dong F, Romero A, Johnson DR, Ghosh D, Yang F, Frohnert B, Yang IV, Kechris K, Rewers M, Norris JM.
DNA Methylation Near DLGAP2 May Mediate the Relationship between Family History of Type 1 Diabetes and Type 1 Diabetes Risk
Pediatr Diabetes PMID 38765731
KKahan R, Higinbotham S, Garoosi K, Lauder A.
Electric Scooter-related Injuries Are Becoming More Frequent and Costly in Denver, CO Clin Orthop Relat Res. PMID 339136941
Keogh RA, Huyvaert S, Moore GD, Horswill AR, Doran KS
Virulence characteristics of Gram-positive bacteria isolated from diabetic foot ulcers FEMS Microbes PMID 38783991
Kim YJ, Retrouvey H, Lauder A, Pesante BD, Parry JA.
Urinary bladder matrix versus dermal regeneration template for lower extremity wound coverage
Eur J Orthop Surg Traumatol PMID 38488935
Klingebiel FK, Sawauchi K, Mittlmeier A, Kalbas Y, Berk T, Halvachizadeh S, Teuben M, Neuhaus V, Mauffrey C, Pape HC, Pfeifer R.
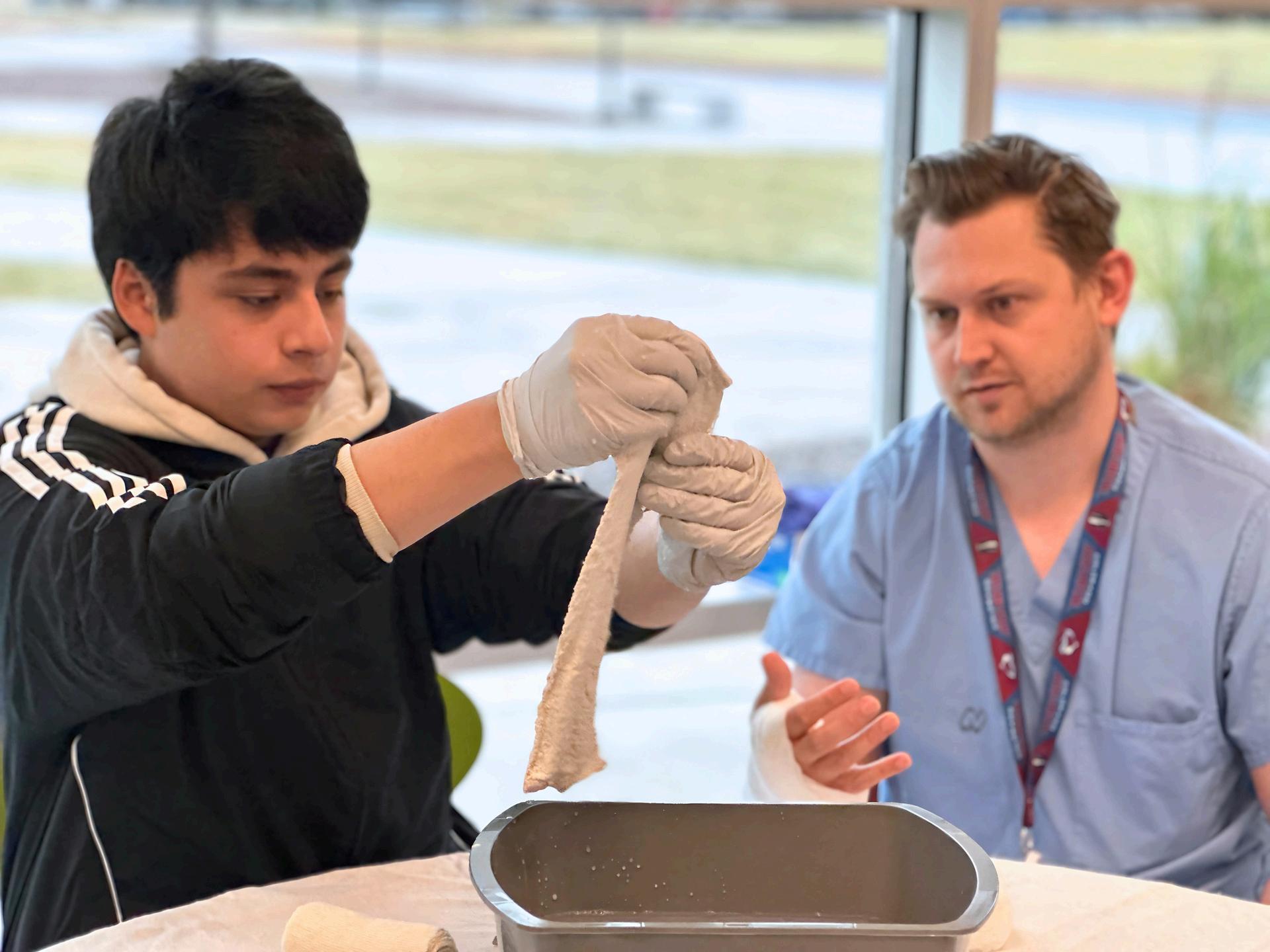
Improving surgical technical skills for emergency fixation of unstable pelvic ring fractures: an experimental study using a pelvic ring fracture simulator Patient Saf Surg. PMID 39334252
Kon E, Anzillotti G, Conte P, Ruosi L, Cole B, Dragoo J, Zaslav K, Frank R, De Girolamo L, Mandelbaum B, Rodeo S, Marcacci M, Filardo G, Di Matteo B.
The chimera of reaching a universal consensus on platelet-rich plasma treatment for knee osteoarthritis: a review of recent consensus statements and expert opinion
Expert Opin Biol Ther PMID 39073848
Kostyun RO, Nguyen JC, Chhabra B, Todd R Lawrence J, Polousky JD, Saper M, Uquillas C, Nissen CW, Members of the ROCKET Group, Kostyun RO, Albright J, Bae D, Bohn D, Chan C, Crepeau A, Edmonds E, Fabricant P, Ganley T, Little K, Lee Pace J, Pacicca D, Pennock A, Saluan P, Shea K, Wall E, Wilson P, Nissen CW.
MRI Features That Contribute to Decision-Making for Treatment of Capitellar OCD Lesions: An Expert Consensus Using the Delphi Method
Orthop J Sports Med PMID 338845610
Kraeutler MJ, Garabekyan T, Mei-Dan O.
We Need Better Classification of Patients With Borderline Hip Dysplasia: Shifting the Focus From Dysplasia to Instability
Arthroscopy. PMID 338206250
Kraeutler MJ, Hernandez E, Samuelsson K, Mei-Dan O
The Principles of Hip Joint Preservation
Arthroscopy PMID 38960506
Kraeutler MJ, Marder RS, Fasulo SM, Dávila Castrodad IM, Mei-Dan O, Scillia AJ.
Patients Undergoing Postless Hip Arthroscopy Demonstrate Significantly Better Patient-Reported Outcomes and Clinically Significant Outcomes Compared to Conventional Post-Assisted Hip Arthroscopy at Short-Term Follow-Up
Arthroscopy PMID 38599534
Kraeutler MJ, Terle PM, Malempati M, Dhillon J, Samuelsson K, Mei-Dan O
Risk Factors for Failure of Hip Arthroscopy in Patients With Borderline Dysplasia Include a Tönnis Angle 15°, Age 40 to 42 Years, Female Sex, Anterior Wall Index <0 35, Labral Debridement, and Preexisting Hip Osteoarthritis: A Systematic Review
Arthroscopy PMID 39490543
Krajewski KT, Coomer W, Gerk A, Miller SC, Kwok C, Pan Z, Oleszek JL, Stratton AT, Chang F, De S. Hip Instability in Children With Spinal Muscular Atrophy: A Retrospective Study
J Pediatr Orthop. PMID 39282710
Krajewski KT, Miller S, Dimovski R, Rhodes J, De S.
Retrograde Insertion Approach for Anterior Distal Femoral Hemiepiphysiodesis Procedure: A Case Report JBJS Case Connect PMID 39208151
Krieg B, Dayton M, Alfonso N.
Re-revision Extensor Mechanism Reconstruction Because of Nonunion and Tendon Failure After Total Knee Arthroplasty
Orthopedics. PMID 39163604
Kuhn JE, Dunn WR, Sanders R, Baumgarten KM, Bishop JY, Brophy RH, Carey JL, Holloway BG, Jones GL, Ma CB, Marx RG, McCarty EC, Poddar SK, Smith MV, Spencer EE, Vidal AF, Wolf BR, Wright RW, Multicenter Orthopaedic Outcomes Network (MOON) Shoulder Group. 2024 Kappa Delta Ann Doner Vaughan Award: Nonsurgical Treatment of Symptomatic, Atraumatic FullThickness Rotator Cuff Tears-a Prospective Multicenter Cohort Study With 10-Year Follow-Up
J Am Acad Orthop Surg. PMID 39325825
Kuhn JE, Dunn WR, Sanders R, Baumgarten KM, Bishop JY, Brophy RH, Carey JL, Holloway BG, Jones GL, Ma CB, Marx RG, McCarty EC, Poddar SK, Smith MV, Spencer EE, Vidal AF, Wolf BR, Wright RW.
The Predictors of Surgery for Symptomatic, Atraumatic Full-Thickness Rotator Cuff Tears Change Over Time: Ten-Year Outcomes of the MOON Shoulder Prospective Cohort
J Bone Joint Surg Am. PMID 38980920
LLalonde RL, Wells HH, Kemmler CL, Nieuwenhuize S, Lerma R, Burger A, Mosimann C. pIGLET: Safe harbor landing sites for reproducible and efficient transgenesis in zebrafish Sci Adv. PMID 38838146
Lauder A, Rodriguez-Fontan F, Pflug EM.
Revision Thumb Metacarpophalangeal Joint Ulnar Collateral Ligament Reconstruction With Autograft and Button Suspension: Correspondence Tech Hand Up Extrem Surg. PMID 39298542
Laynes RA, Aravindan S, Wharton B, Layne JE, Kleck CJ, Patel VV. Injury to the Superior Gluteal Artery During Minimally Invasive Sacroiliac Joint Fusion: A Case Series JBJS Case Connect PMID 39270041
Laynes RA, Kleck CJ. Patient-specific implants and spinal alignment outcomes N Am Spine Soc J PMID 39524185
Lee JH, Girardi NG, Kraeutler MJ, Keeter C, Genuario JW, Garabekyan T, Mei-Dan O.
Staged Hip Arthroscopy and Periacetabular Osteotomy in Active Patients 45 Years and Older Produces Comparable Improvements in Outcome Scores to Younger Patients Arthroscopy PMID 39521385
Lee N, Fisher MH, McNamara CT, Greyson MA, Hogan CA, Iorio ML.
A Systematic Review of Clinical Outcomes of Pedicled Flap Repairs of the Knee Extensor Mechanism J Reconstr Microsurg PMID 38936419
Lendaro E, Van der Sluis CK, Hermansson L, Bunketorp-Käll L, Burger H, Keesom E, Widehammar C, Munoz-Novoa M, McGuire BE, O'Reilly P, Earley EJ, Iqbal S, Kristoffersen MB, Stockselius A, Gudmundson L, Hill W, Diers M, Turner KL, Weiss T, Ortiz-Catalan M. Extended reality used in the treatment of phantom limb pain: a multicenter, double-blind, randomized controlled trial Pain. PMID 39250328
Lim JJ, Belk JW, Wharton BR, McCarthy TP, McCarty EC, Dragoo JL, Frank RM. Most Orthopaedic Platelet-Rich Plasma Investigations Don't Report Protocols and Composition: An Updated Systematic Review Arthroscopy. PMID 38522650
Lindeque B, Moon D.
Wound healing outcomes following treatment with synthetic hybrid-scale fiber matrix after resection of soft tissue tumors or infections Wounds. PMID 38479428
Low Wang CC, Chong T, Moore G, Echalier B, Haakonsen N, Carter JE Jr, Mathes D, Hsia J, Phan TT, Lim IJ, Freed BM.
Results of the Phase 1 Open-Label Safety Study of Umbilical Cord Lining Mesenchymal Stromal/Stem Cells (Corlicyte(®)) to Heal Chronic Diabetic Foot Ulcers Biomedicines PMID 38927582
MMagliato SN, Wingerson MJ, Smulligan KL, Little CC, Lugade V, Wilson JC, Howell DR. Virtual Neuromuscular Training Among Physically Active Young Adults: A Feasibility Study J Sport Rehabil PMID 39374925
Maguire JA, Dhillon J, Scillia AJ, Kraeutler MJ
Rotator Cuff Repair With or Without Acromioplasty: A Systematic Review of Randomized Controlled Trials With Outcomes Based on Acromial Type Am J Sports Med PMID 38312081
MARS Group, Vasavada K, Vasavada V, Moran J, Devana S, Lee C, Hame SL, Jazrawi LM, Sherman OH, Huston LJ, Haas AK, Allen CR, Cooper DE, DeBerardino TM, Spindler KP, Stuart MJ, Ned Amendola A, Annunziata CC, Arciero RA, Bach BR Jr, Baker CL 3rd, Bartolozzi AR, Baumgarten KM, Berg JH, Bernas GA, Brockmeier SF, Brophy RH, Bush-Joseph CA, Butler V JB, Carey JL, Carpenter JE, Cole BJ, Cooper JM, Cox CL, Creighton RA, David TS, Dunn WR, Flanigan DC, Frederick RW, Ganley TJ, Gatt CJ Jr, Gecha SR, Giffin JR, Hannafin JA, Lindsay Harris N Jr, Hechtman KS, Hershman EB, Hoellrich RG, Johnson DC, Johnson TS, Jones MH, Kaeding CC, Kamath GV, Klootwyk TE, Levy BA, Ma CB, Maiers GP 2nd, Marx RG, Matava MJ, Mathien GM, McAllister DR, McCarty EC, McCormack RG, Miller BS, Nissen CW, O'Neill DF, Owens BD, Parker RD, Purnell ML, Ramappa AJ, Rauh MA, Rettig AC, Sekiya JK, Shea KG, Slauterbeck JR, Smith MV, Spang JT, Svoboda SJ, Taft TN, Tenuta JJ, Tingstad EM, Vidal AF, Viskontas DG, White RA, Williams JS Jr, Wolcott ML, Wolf BR, Wright RW, York JJ. A Novel Machine Learning Model to Predict Revision ACL Reconstruction Failure in the MARS Cohort Orthop J Sports Med. PMID 39555321
MARS Group, Wright RW, Huston LJ, Haas AK, Pennings JS, Allen CR, Cooper DE, DeBerardino TM, Dunn WR, Lantz BBA, Spindler KP, Stuart MJ, Amendola AN, Annunziata CC, Arciero RA, Bach BR Jr, Baker CL 3rd, Bartolozzi AR, Baumgarten KM, Berg JH, Bernas GA, Brockmeier SF, Brophy RH, BushJoseph CA, Butler JB 5th, Carey JL, Carpenter JE, Cole BJ, Cooper JM, Cox CL, Creighton RA, David TS, Flanigan DC, Frederick RW, Ganley TJ, Gatt CJ Jr, Gecha SR, Giffin JR, Hame SL, Hannafin JA, Harner CD, Harris NL Jr, Hechtman KS, Hershman EB, Hoellrich RG, Johnson DC, Johnson TS, Jones MH, Kaeding CC, Kamath GV, Klootwyk TE, Levy BA, Ma CB, Maiers GP 2nd, Marx RG, Matava MJ, Mathien GM, McAllister DR, McCarty EC, McCormack RG, Miller BS, Nissen CW, O'Neill DF, Owens BD, Parker RD, Purnell ML, Ramappa AJ, Rauh MA, Rettig AC, Sekiya JK, Shea KG, Sherman OH, Slauterbeck JR, Smith MV, Spang JT, Svoboda SJ, Taft TN, Tenuta JJ, Tingstad EM, Vidal AF, Viskontas DG, White RA, Williams JS Jr, Wolcott ML, Wolf BR, York JJ.
Surgical Predictors of Clinical Outcome 6 Years After Revision ACL Reconstruction Am J Sports Med PMID 39503722
Martino R, Carry P, Stickel J, Samara O, Lee S, Selberg C.
Use of the flat panel detector fluoroscope reduces radiation exposure during periacetabular osteotomy Sci Rep. PMID 38658572
Marty E, Keeter C, Henry K, Kraeutler MJ, Lee JH, Mei-Dan O. Midterm Outcomes After Simultaneous Hip Arthroscopic Surgery for Bilateral Femoroacetabular Impingement Am J Sports Med PMID 39097759
Mason CE, Green J, Adamopoulos KI, Afshin EE, Baechle JJ, Basner M, Bailey SM, Bielski L, Borg J, Borg J, Broddrick JT, Burke M, Caicedo A, Castañeda V, Chatterjee S, Chin CR, Church G, Costes SV, De Vlaminck I, Desai RI, Dhir R, Diaz JE, Etlin SM, Feinstein Z, Furman D, Garcia-Medina JS, GarrettBakelman F, Giacomello S, Gupta A, Hassanin A, Houerbi N, Irby I, Javorsky E, Jirak P, Jones CW, Kamal KY, Kangas BD, Karouia F, Kim J, Kim JH, Kleinman AS, Lam T, Lawler JM, Lee JA, Limoli CL, Lucaci A, MacKay M, McDonald JT, Melnick AM, Meydan C, Mieczkowski J, Muratani M, Najjar D, Othman MA, Overbey EG, Paar V, Park J, Paul AM, Perdyan A, Proszynski J, Reynolds RJ, Ronca AE, Rubins K, Ryon KA, Sanders LM, Glowe PS, Shevde Y, Schmidt MA, Scott RT, Shirah B, Sienkiewicz K, Sierra MA, Siew K, Theriot CA, Tierney BT, Venkateswaran K, Hirschberg JW, Walsh SB, Walter C, Winer DA, Yu M, Zea L, Mateus J, Beheshti A.
A second space age spanning omics, platforms and medicine across orbits Nature PMID 38862027
McDevitt A, Cleland J, Hiefield P, Bravman J, Snodgrass S. Physical Therapy Utilization Prior to Biceps Tenodesis or Tenotomy for Biceps Tendinopathy Int J Sports Phys Ther PMID 39502549
McDonald LS, Hynes KK, Parry JA, Stephens BF, Schwab JH. The 2024 American Orthopaedic Association-Japanese Orthopaedic Association Traveling Fellowship J Bone Joint Surg Am PMID 39602503
Mehta JS, Pahys JM, Saad A, Sponseller P, Andras L, Marks D, Poon S, Klineberg E, White KK, Helenius I, Welborn M, Redding G. Paediatric syndromic scoliosis: proceedings of the half-day course at the 57th annual meeting of the Scoliosis Research Society Spine Deform PMID 38366266
Meyer MA, Leversedge FJ, Catalano LW 3rd, Lauder A. Complex Elbow Fracture-Dislocations: An Algorithmic Approach to Treatment J Am Acad Orthop Surg PMID 38709855
Milewski MD, Miller PE, Gossman EC, Coene RP, Tompkins MA, Anderson CN, Bauer K, Busch MT, Carey JL, Carsen S, Chambers HG, Coene RP, Edmonds EW, Ellermann J, Ellis HB Jr, Erickson J, Fabricant PD, Ganley TJ, Gossman EC, Green DW, Heyworth BE, Hoi Po Hui J, Kocher MS, Krych AJ, Latz K, Lyon RM, Mayer S, Milewski MD, Miller PE, Nelson BJ, Nepple JJ, Nguyen JC, Nissen CW, Lee Pace J, Paterno MV, Pennock AT, Perkins C, Polousky JD, Saluan P, Shea KG, Tompkins MA, Wall EJ, Weiss JM, Willimon C, Wilson P, Wright RW, Zbojniewicz A, Myer GD. A Simple Clinical Predictive Model for Arthroscopic Mobility of Osteochondritis Dissecans Lesions of the Knee Am J Sports Med PMID 39584729
Myerson MS, Fernández-Rojas E, Rosa MM, Araya-Bonilla V, Barra-Dinamarca E, Elgueta-Grillo J. Talocalcaneal coalition classifications: A critical analysis review and suggested new classification system with implications for treatment Foot Ankle Surg PMID 38584062
NNguyen TB, Weitzel N, Hogan C, Kacmar RM, Williamson KM, Pattee J, Jevtovic-Todorovic V, Simmons CG, Faruki AA.
Comparing Anesthesia and Surgery Controlled Time for Primary Total Knee and Hip Arthroplasty Between an Academic Medical Center and a Community Hospital: Retrospective Cohort Study JMIR Perioper Med. PMID 38407957
OOkamoto F, Chitre AS, Missfeldt Sanches T, Chen D, Munro D, Aron AT, Beeson A, Bimschleger HV, Eid M, Garcia Martinez AG, Han W, Holl K, Jackson T, Johnson BB, King CP, Kuhn BN, Lamparelli AC, Netzley AH, Nguyen KH, Peng BF, Tripi JA, Wang T, Ziegler KS, Adams DJ, Baud A, Carrette LLG, Chen H, de Guglielmo G, Dorrestein P, George O, Ishiwari K, Jablonski MM, Jhou TC, Kallupi M, Knight R, Meyer PJ, Solberg Woods LC, Polesskaya O, Palmer AA
Y and mitochondrial chromosomes in the heterogeneous stock rat population G3 (Bethesda). PMID 339250761
Oldham JR, Howell DR, Lanois CJ, Berkner PD, Iverson GL, Mannix RC, Meehan WP 3rd
Baseline Symptoms and Neurocognitive Performance across Collision, Contact, and Noncontact Female High School Athletes
Med Sci Sports Exerc PMID 39140797
PParry JA, Patterson JT, O'Hara NN.
What outcomes do patients value after orthopaedic trauma: A best-worst scaling choice experiment Injury PMID 38878386
Parry JA, Salimi M, Stacey SC, Mauffrey C
There is no correlation between differences in adverse events and differences in patient-reported outcome measures in orthopaedic trauma randomized controlled trials: A systematic review Injury PMID 39332228
Parry JA, Working ZM.
Special edition: updates in pelvic and acetabular surgery
Eur J Orthop Surg Traumatol PMID 38367187
Patel V, Meyer SC, Kovalsky D, Lockstadt H, Farris J, Limoni R, Chowdhary A, Yuan P, Langel C, Kranenburg A, Tender G.
Prospective Trial of Sacroiliac Joint Fusion Using 3D-Printed Triangular Titanium Implants: 5-Year Follow-Up Spine (Phila Pa 1976) PMID 39344079
Patel V, Wind JJ, Aleem I, Lansford T, Weinstein MA, Vokshoor A, Campbell PG, Beaumont A, Hassanzadeh H, Radcliff K, Matheus V, Coric D.
Adjunctive Use of Bone Growth Stimulation Increases Cervical Spine Fusion Rates in Patients at Risk for Pseudarthrosis Clin Spine Surg PMID 38650075
Patterson JT, Parry JA, Working ZM, McKibben NA, Baca J, Duong A, Senior J, Kim A, Marchand LS, O'Hara N.
Patient Preferences for Operative Versus Nonoperative Treatment of LC1 Pelvis Fracture: A Discrete Choice Experiment J Orthop Trauma. PMID 38442188
Patterson JT, Parry JA.
Lateral Compression Fragility Fractures of the Pelvis: Diagnosis, Classifications, and Modern Management Curr Osteoporos Rep. PMID 39313717
Peebles LA, Blackwood NO, Verma A, O'Brien MJ, Lintner DM, Kraeutler MJ.
Medial Ulnar Collateral Ligament Reconstruction With Allograft Provides Excellent Clinical Outcomes, High Rates of Return to Play, and a Low Incidence of Postoperative Complications: A Systematic Review Arthroscopy. PMID 38593928
Pesante BD, Mauffrey C, Parry JA.
Rise of the Machines: The Prevalence and Disclosure of Artificial Intelligence-Generated Text in High-Impact Orthopaedic Journals
J Am Acad Orthop Surg. PMID 38941622
Pesante BD, Moore EE, Pieracci FM, Kim YJ, Mauffrey C, Parry JA.
Increasing the Threshold to Perform Preperitoneal Pelvic Packing Decreases Morbidity Without Affecting Mortality
J Orthop Trauma. PMID 39007658
Pesante BD, Parry JA.
The Effect of Vancomycin and Tobramycin Local Antibiotic Powder on Surgical Site Infections After Open Treatment of Fracture: A Retrospective Propensity-Matched Analysis
J Orthop Trauma PMID 38176854
Pesante BD, Salimi M, Miller WL, Young HL, Jenkins TC, Parry JA
Associations with unplanned repeat irrigation and debridement of native septic arthritis
Eur J Orthop Surg Traumatol PMID 38573381
Pesante BD, Salimi M, Miller WL, Young HL, Jenkins TC, Parry JA.
The Effect of Crystal Arthropathy on the Diagnostic Criteria of Native Septic Arthritis
J Am Acad Orthop Surg PMID 38652879
Pesante BD, Ward BA, Stacey SC, Parry JA.
A Retrospective Comparison of Headless Versus Standard Interlocking Screw Fixation of Tibia Intramedullary Nails
J Am Acad Orthop Surg PMID 39602625
Pflug EM, Rodriguez-Fontan F, Lauder A
Revision Thumb Metacarpophalangeal Joint Ulnar Collateral Ligament Reconstruction With Autograft and Button Suspension
Tech Hand Up Extrem Surg PMID 38916579
Pollard TG, DeLeon JC, Parry JA, Stacey SC, Heare A, Richard RD, Mauffrey C.
Tips and tricks for the reduction and fixation of sacroiliac joint fracture-dislocations
J Clin Orthop Trauma PMID 38223901
Prato TA, Lynall RC, Howell DR, Lugade V.
Validity and Reliability of an Integrated Smartphone Measurement Approach for Balance
J Sport Rehabil PMID 39557038
QQu F, Ji L, Sun C, Zhu M, Myerson MS, Li S, Zhang M.
Arthroscopic Anterior Talofibular Ligament Repair Combined With All-Inside Suture Tape Augmentation for Treatment of Chronic Lateral Ankle Instability With Generalized Joint Laxity
Foot Ankle Int. PMID 39212116
RRamirez N, Deliz-Jimenez D, Torres-Lugo N, Olivella G, Cahill P, Gupta P, Garg S, Pahys J, Mac-Thiong JM.
Clinical Relevance of Painful Congenital Early-onset Scoliosis: A Magnetic Resonance Image-based Study J Pediatr Orthop PMID 38269603
Reeves B, Roper B, Salton R, Baumann A, Dimovski R, Hadley-Miller N, Albright J
Outcomes of Simultaneous Lengthening and ACL Reconstruction in Fibular Hemimelia: A Retrospective Case Series
Iowa Orthop J PMID 38919371
Retrouvey H, Harmange C, Saggaf M, DeSanto K, Leversedge FJ, Lauder A.
Low-Velocity Ballistic Trauma-Related Upper Extremity Nerve Injury: A Systematic Review and Meta-Analysis
J Am Acad Orthop Surg. PMID 39467287
Retrouvey H, Meyer MA, Ipaktchi K, Maertens A, Folchert M, Lauder A. Management of Xylazine-Induced Soft-Tissue Necrosis: A Review of 20 Cases
J Am Acad Orthop Surg PMID 39197079
Richard RD, Pesante BD, Parry JA, Mauffrey C
The Effect of Adverse Events on Orthopaedic Surgeons: A Review
J Am Acad Orthop Surg PMID 39019003
Richman EH, Brinkman JC, Paul BR, Griffin N, Alfonso N. Trends in Medicare Utilization and Reimbursement for Intertrochanteric Femur Fractures: A 21-Year Review Eur J Orthop Surg Traumatol. PMID 39567377
Roberts J, Wilson JC, Halstead ME, Miller SM, Santana JA, Valovich McLeod TC, Zaslow TL, Master CL, Grady MF, Snedden TR, Fazekas ML, Coel RA, Howell DR.
Variables associated with days of school missed following concussion: results from the Sport Concussion Outcomes in PEdiatrics (SCOPE) study Phys Sportsmed. PMID 38648009
Rodriguez Fontan F, Hunt KJ.
Talus Idiopathic Versus Stress-Injury-Related Osteonecrosis and Its Resolution: A Case Report Cureus PMID 38213383
Rogers ND, Trizno AA, Joyce CD, Roberts JL, Soep JB, Donaldson NJ.
Spine Involvement and Vertebral Deformity in Patients Diagnosed with Chronic Recurrent Multifocal Osteomyelitis
J Pediatr Orthop. PMID 38881233
Roper B, Purtell SR, De S, McLaughlin D, Truong WH, Miller ML, Swarup I, Ramalingam W, Sanders JS, Children’s Orthopaedic Trauma and Infection Consortium for Evidence-Based Studies (CORTICES)
Practice Patterns Vary Widely in the Care of Pediatric and Adolescent Pelvic and Acetabular Fractures: A CORTICES Survey
J Pediatr Orthop PMID 39428588
Ross LK, Lalka A, Keeter C, Hamati MC, Robell K, Howell DR, Zona NE, Hunt KJ.
Playing surface and sport contact status modulate time to lower extremity musculoskeletal injury at a greater level than concussion history among collegiate student-athletes
J ISAKOS PMID 38925353
SSaarinen AJ, Sponseller P, Thompson GH, White KK, Emans J, Cahill PJ, Hwang S, Pediatric Spine Study Group, Helenius I.
Outcomes after completing growth-friendly surgical treatment for early-onset scoliosis in patients with skeletal dysplasia
Bone Joint J. PMID 38821501
Salimi M, Pesante BD, Junior CW, Mauffrey C
Validation of a novel system to quantify authorship diversity in orthopaedic surgery literature Int Orthop PMID 39289181
Sayan D, Skinner A, Tagawa A, Coomer W, Koerner J, Silveira L, Carollo J, Rhodes J
Effect of split posterior tibialis tendon transfer on foot progression angle in children with cerebral palsy Foot (Edinb) PMID 38569253
Schönberg NKT, Poppel J, Howell D, Wagner J, Höfinger M, Fabri N, Bonke EM, Rojczyk P, Hösl M, Kiwull L, Schröder SA, Blaschek A, Vill K, Koerte IK, Huppert D, Heinen F, Bonfert MV.
Instrumented Balance Error Scoring System in Children and Adolescents-A Cross Sectional Study Diagnostics (Basel) PMID 38472985
Schutz J, Korrell H, Look N, Lalka A, Hild J, Cleary G, Sinclair MK, Sibbel SE. Outcomes of Pediatric Proximal Phalanx Base Fractures
J Am Acad Orthop Surg PMID 38489764
Seidl AJ, Ahmed AF, Woods D, Abboud JA, Bravman JT. Strategies to Mitigate Bleeding in Shoulder Arthroplasty in the Setting of an Arteriovenous Fistula: A Report of 3 Cases
JBJS Case Connect PMID 38306442
Seidl AJ, Daniels SD. Instability and the Anatomic Total Shoulder Arthroplasty
J Am Acad Orthop Surg PMID 39254950
Sinkler MA, Benedick A, Kavanagh M, Alfonso N, Vallier HA. Complications and Outcomes After Fixation of Lisfranc Injuries at an Urban Level 1 Trauma Center
J Orthop Trauma PMID 38294227
Skedros JG, Dayton MR, Cronin JT, Mears CS, Bloebaum RD, Wang X, Bachus KN. Roles of collagen cross-links and osteon collagen/lamellar morphotypes in equine third metacarpals in tension and compression tests
J Exp Biol. PMID 39045755
Slatnick LR, Cost C, Garrington T, Donaldson N, Macy ME
Central Nervous System Metastases in Pediatric Patients With Ewing Sarcoma J Pediatr Hematol Oncol. PMID 38316140
Smulligan KL, Carry P, Smith AC, Esopenko C, Baugh CM, Wilson JC, Howell DR. Cervical spine proprioception and vestibular/oculomotor function: An observational study comparing young adults with and without a concussion history Phys Ther Sport PMID 39013262
Smulligan KL, Magliato SN, Keeter CL, Wingerson MJ, Smith AC, Wilson JC, Howell DR. The Diagnostic Utility of Cervical Spine Proprioception for Adolescent Concussion Clin J Sport Med PMID 38953712
Smulligan KL, Wingerson MJ, Magliato SN, Rademacher JG, Wilson JC, Howell DR. Post-Concussion Moderate to Vigorous Physical Activity Predicts Anxiety Severity Among Adolescent Athletes Med Sci Sports Exerc. PMID 38181208
Sparks CA, Fasulo SM, Windsor JT, Bankauskas V, Contrada EV, Kraeutler MJ, Scillia AJ ChatGPT Is Moderately Accurate in Providing a General Overview of Orthopaedic Conditions JB JS Open Access. PMID 38912370
Sparks CA, Kraeutler MJ, Chester GA, Contrada EV, Zhu E, Fasulo SM, Scillia AJ.
Inadequate Performance of ChatGPT on Orthopedic Board-Style Written Exams Cureus PMID 39036109
Stokes DJ, Cram TR, Laynes RA, Peszek A, Shinsako KK, Frank RM.
Posterior Meniscus Root Repair Using a Retensionable Knotless All-Suture Anchor Arthrosc Tech PMID 39100261
Stokes DJ, Elrick BP, Carpenter ML, Raji Y, McQuivey KS, Sherman SL, Frank RM Tibial Tubercle Osteotomy: Indications, Outcomes, and Complications
Curr Rev Musculoskelet Med. PMID 39102076
Stokes DJ, Frank RM.
Editorial Commentary: Meniscus Repair Technique Must Be Determined on a Tear-by-Tear Basis: Hybrid Techniques Plus Biologics Are Optimal Arthroscopy. PMID 38479636
Stokes DJ, Sanchez RA, Williams BT, Strassman AK, Shinsako KK, DiFelice GS, Frank RM. Tibial Spine Avulsion Fracture Fixation Using a Re-tensionable All-Suture Construct Arthrosc Tech PMID 39100271
Strassman AK, Stokes DJ, Sanchez RA, Shinsako KK, Smith PA, DiFelice GS, Frank RM
Anterior Cruciate Ligament Repair Using a Re-tensionable All-Suture Construct
Arthrosc Tech. PMID 38584624
TTakagi T, Nguyen PD, Leversedge FJ
Ten Steps for a Successful Hand Surgery Mission Trip - Experiences from Supporting Paediatric Hand in Vietnam and Honduras
J Hand Surg Asian Pac Vol PMID 39544038
Tanguilig G, Dhillon J, Kraeutler MJ.
Platelet-Rich Plasma for Knee and Hip Osteoarthritis Pain: A Scoping Review
Curr Rev Musculoskelet Med PMID 39002073
Tanguilig G, Dhillon J, Scillia AJ, Heard WMR, Kraeutler MJ.
The Addition of a Pericapsular Nerve Group Block for Postoperative Pain Control Does Not Result in Less Narcotic Use After Hip Arthroscopy: A Systematic Review
Arthrosc Sports Med Rehabil PMID 38379602
Tepavčević S, Zec M, Stojiljković M, Bošković M, Ćulafić T, Stanković A, Romić S, Živković M, Korićanac G.
Unlocking the Cardiovascular Benefits of Walnuts: Insights on Molecular Mechanism From Animal Studies
Nutr Rev. PMID 39565929
Terle PM, Peebles LA, Verma A, Kraeutler MJ.
Minimal Clinically Important Difference (MCID), Substantial Clinical Benefit (SCB), and Patient Acceptable Symptom State (PASS) Values Following Hip Arthroscopy for Femoroacetabular Impingement Are Highly Dependent on Their Study Population and Calculation Methods: A Systematic Review Arthroscopy PMID 39147078
Thomsen PB, Gaffney BMM, Tracy JB, Vandenberg NW, Awad ME, Christiansen CL, Stoneback JW
Cumulative loading increases and loading asymmetries persist during walking for people with a transfemoral bone-anchored limb
Gait Posture PMID 38843706
Thorne A, Moss A, Sanders JS, Stein J, Searns JB.
Clinical Utility of Repeat Magnetic Resonance Imaging Studies Among Children With Acute Hematogenous Osteomyelitis
J Pediatr Orthop PMID 38477331
Tippabhatla A, Torres-Izquierdo B, Pereira DE, Goldstein R, Sanders J, Neal K, Bellaire L, Denning J, Hosseinzadeh P.
Risk Factors for Stiffness After Surgical Treatment of Pediatric Humeral Lateral Condyle Fractures: Results of a Multicenter Study
J Pediatr Orthop PMID 38282478
Tracy JB, Gaffney BMM, Thomsen PB, Awad ME, Melton DH, Christiansen CL, Stoneback JW.
Dynamic gait stability and stability symmetry for people with transfemoral amputation: A case-series of 19 individuals with bone-anchored limbs
J Biomech. PMID 38941842
Trask M, Yamaguchi JT, Redding G, Yaszay B, Browd S, White KK.
Posterior Column Release and Lengthening with a Magnetic Growing Rod Construct in Severe Congenital Thoracic Fusion: A Report of 2 Cases
JBJS Case Connect PMID 39446981
Tucker NJ, Stacey S, Kim YJ, DeLeon J, Richard R, Heare A, Mauffrey C, Parry JA.
Variables Associated With Loss of Fixation of Retrograde Rami Screws in Minimally Displaced Lateral Compression Type 1 Pelvic Ring Injuries
J Orthop Trauma PMID 38176888
VVandenberg NW, Wheatley BB, Carpenter RD, Christiansen CL, Stoneback JW, Gaffney BMM. Feasibility of predicting changes in gait biomechanics following muscle strength perturbations using optimal control in patients with transfemoral amputation Comput Methods Biomech Biomed Engin PMID 39256913
Vinson AL, Vandenberg NW, Awad ME, Christiansen CL, Stoneback JW, M M Gaffney B. The biomechanical influence of transtibial Bone-Anchored limbs during walking J Biomech. PMID 38636112
WWang C, Jiang W, Leitz J, Yang K, Esquivies L, Wang X, Shen X, Held RG, Adams DJ, Basta T, Hampton L, Jian R, Jiang L, Stowell MHB, Baumeister W, Guo Q, Brunger AT Structure and topography of the synaptic V-ATPase-synaptophysin complex Nature PMID 38838737
Wessell NM, Krieg B, Damioli L, Kleck CJ. Atypical Mycobacterial Infections of the Spine: Evaluation and Management Orthopedics PMID 38285551
Widmann RF, Wisch JL, Tracey OC, Zucker CP, Feddema T, Miller F, Linden GS, Erickson M, Heyer JH. Analysis of 5,070 consecutive pedicle screws placed utilizing robotically assisted surgical navigation in 334 patients by experienced pediatric spine deformity surgeons: surgical safety and early perioperative complications in pediatric posterior spinal fusion Spine Deform. PMID 38556583
Williams BT, Hunt KJ. Hallux Rigidus: Anatomy and Pathology Foot Ankle Clin. PMID 39068015
Wingerson MJ, Schmitz B, Smulligan KL, Walker GA, Magliato S, Wilson JC, Howell DR. Concussion symptom presentation and clinical recovery among pediatric athletes: comparing concussions sustained during school and summer months Brain Inj. PMID 38511887
Wininger AE, Kraeutler MJ, Goble H, Cho J, Mei-Dan O, Harris JD.
The Physics of Postless Hip Arthroscopy
Arthrosc Tech PMID 39479047
Woods D, Illing D, Cao J, Bolson RM, Lauder A, Ipaktchi K.
Hand Surgical Operating Room Size Allocation: A Comparative Space Utilisation Study
J Hand Surg Asian Pac Vol PMID 39397277
Wyatt M, Choudhury A, Von Dohlen G, Heileson JL, Forsse JS, Rajakaruna S, Zec M, Tfaily MM, Greathouse L.
Randomized control trial of moderate dose vitamin D alters microbiota stability and metabolite networks in healthy adults
Microbiol Spectr PMID 39189761
YYendluri A, Gallate ZS, Chari RR, Locke AR, Obana KK, Trofa DP, Frank RM, Parisien RL.
Between 2008 and 2022, Lower-Extremity Injuries Declined in Male Rugby Players, Whereas Noncontact Knee Injuries Showed No Decline in Female Rugby Players
Arthrosc Sports Med Rehabil. PMID 39534036
Yoon YC, Parry JA, Mauffrey C.
Comparative study on anterior pelvic plating and pubic ramus screw fixation for straddle fracture: a matchedpair outcome analysis
Int Orthop. PMID 39340641
Yoon YC, Tucker NJ, Kim YJ, Pollard TG, Mauffrey C, Parry JA.
Surgical complications after fixation of minimally displaced lateral compression type 1 pelvic ring injuries
Eur J Orthop Surg Traumatol PMID 38573380
ZZbinden J, Earley EJ, Ortiz-Catalan M.
Intuitive control of additional prosthetic joints via electro-neuromuscular constructs improves functional and disability outcomes during home use-a case study
J Neural Eng PMID 38489845
Zeitlinger L, Chavez GM, Darrow M, Canter RJ, Randall RL, Thorpe SW.
Musculoskeletal Tumor Society Member Survey: Intra-Operative Peripheral Margins in Soft Tissue Sarcoma
J Surg Oncol PMID 39523920
Zeitlinger L, Chavez GM, Wilson MD, Darrow M, Canter RJ, Lor Randall R, Thorpe SW
Intraoperative Peripheral Frozen Margin Assessment in Soft Tissue Sarcoma
J Surg Oncol PMID 39523913
Zhao L, Uchtman M, Aretakis A, Selberg C, McCarthy JJ, Whitlock PW
Maintenance of acetabular correction following PAO: a multicenter study comparing stainless-steel and titanium screws
J Hip Preserv Surg PMID 39070209
Zhu M, Gu W, Wang C, Sun S, Sempson S, Zhang M, Hunt KJ, Myerson MS, Li S
Different Positions of Weightbearing CT Images Can Influence the Hindfoot Alignment Evaluation Using 2Dimensional Methodology
Foot Ankle Int PMID 39460595
Zuleger TM, Slutsky-Ganesh AB, Grooms DR, Yuan W, Barber Foss KD, Howell DR, Myer GD, Diekfuss JA.
High magnitude exposure to repetitive head impacts alters female adolescent brain activity for lower extremity motor control
Brain Res PMID 38272157
CU Orthopedics is a magical place. We believe we can find cures for many of the diseases that are truly crippling, and we also believe that we have an obligation to train the doctors of tomorrow That leads you to push the ceiling and think, “What can I do better?” Translating that to clinical care affords our patients the best care—cutting-edge care We are delivering personalized care to everyone who enters our doors.
Evalina Burger, MD
Professor Chair | Department of Orthopedics
Opening Doors—an art installation by Christopher Weed—features three 19-foot-tall, 3,000-pound doors standing as sentinels between two main science buildings at the University of Colorado Anschutz. These vibrant and visually striking doors symbolize the new opportunities and discoveries that education and science provide.