2025 Number 55
Clinical Effectiveness Bulletin
Clinical Governance Directorate of the British Orthodontic Society




FREE Core CPD Online courses
FREE Core CPD Online Courses


Free registration with ProDental CPD in mandatory topics is a BOS members benefit. ProDental CPD includes courses in a range of GDC recommended topics including:
Free registration with ProDental CPD in mandatory topics is a BOS member benefit. ProDental CPD includes courses in a range of GDC recommended topics including:
Medical Emergencies
Medical Emergencies
Radiography/Radiation Protection
Radiography/Radiation Protection
Decontamination/Disinfection
Decontamination/Disinfection
To register, please email executivesec@bos.org.uk and enter BOS CPD in the subject line. Please provide your name and GDC number and you will be sent an invitation to access the FREE core CPD available to BOS members It really is that easy!
To register, please email ann.wright@bos.org.uk and enter BOS CPD in the subject line. Please provide your name and GDC number and you will be sent an invitation to access the FREE core CPD available to BOS members.
It really is that easy!
Thank you for the opportunity to update the Society on the work of the Governance team in this latest issue of the Clinical Effectiveness Bulletin (CEB). As I enter my last year as Chair of Governance and the advert for my successor has been published, it does seem an opportunity to reflect. I would like to thank Robert for his fantastic stewardship of the CEB. Robert has published an excellent series of Bulletins and has organised their contents so that all the Bulletins are searchable via the BOS website. This was an enormous task that has proved very successful and will be a lasting legacy. I would like to thank Robert on behalf of the Governance team and the BOS. The Bulletin remains an effective way for audits and service evaluations to be shared by members of the BOS and is a resource developed by our members for our members.
We continue to offer the opportunity to ask members of the Society their views on a wide range of topics through Dr Mariyah Nazir, Chair of Audit. These surveys can be very powerful and often form part of the research component of training for our specialist trainees or come directly from the Society in order to ensure our executive keeps in touch with the views of the membership. Either way, I would encourage everyone to make the effort to have your voice heard. I know we all face a daily blizzard of email requests for our attention and our opinions, but your views are crucial for the successful running of our Society, or represent the research aspirations of one of our young colleagues. They need your help so please do complete these surveys do not let them down.
Dr Sameer Patel, Chair of Publications has continued to publish and update our written information for patients and our advice sheets.
These advice sheets are not prescriptive or restrictive but represent the research and opinions of their authors who have often faced the challenges which the advice sheets might help you to avoid. I am very grateful to Sameer who has pioneered the regular publication of a selection of these documents, as too often our members would only read the advice sheet after problems had occurred. As a Society we are very fortunate we have so many members who are willing to give up their time and publish their opinions in this format and I know many members have found the information, useful and well-constructed.

I am sure we have all seen the scope of practice guidance from the General Dental Council. Our Chair of Ethics, Dr Nicky Stanford, has worked with the regulator to produce the orthodontic aspect of this scope of practice guidance. I would like to take this opportunity to thank Nicky for his dedication and steadfast support.
Finally, I would like to thank all our British Orthodontic Society team, now based at the Royal College of Surgeons of England, for their help for me as Chair of Governance. I am grateful for their patience, their wisdom and their dedication to our wonderful specialty.
Stephen Chadwick Director of Clinical Governance of the British Orthodontic Society
Aims and Scope
The British Orthodontic Society Clinical Effectivness Bulletin is an official bi-annual publication of the British Orthodontic Society Clinical Governance Directorate. The primary focus of articles in the Bulletin is the reporting of the quality of orthodontic care and ways to improve it via both clinical audit and effectiveness. The British Orthodontic Society Clinical Effectiveness Bulletin welcomes submissions reporting both these aspects of clinical governance. Clinical audits (in particular multi-cycle audits) and service evaluations would be considered for publication.
All submitted articles undergo peer-review. Acceptance of articles will be based on the recommendations of the reviewers with the final decision made by the Editor. In addition, submissions will be judged against the following criteria:
1. Does this article add anything new to the existing literature?
2. Does the subject content reflect any relevant national topics?
3. Have the authors implemented a change in clinical practice and assessed the effects? i.e. re-audits
submitted to the Editor
Articles sent to regional Sub-editors
Articles sent to peer -reviewers (Post-CSST trainees) via Sub-editors
Peer-reviewed articles returned to Editor from Sub-editors with comments/decisions Final decision made by Editor
Provisional article acceptance
Articles returned to authors including:
• Amended article
• Peer-reviewers checklist with comments/ feedback
Amended articles returned to Editor with 8 weeks for final editorial changes
Final acceptance email sent to authors prior to publication
Article rejected
Articles returned to authors including:
• Amended article
• Peer-reviewers checklist with comments/ feedback
Editor's Remarks
Welcome to the Autumn edition of the Clinical Effectiveness Bulletin.
As I come to the end of my three-year tenure as Editor of the British Orthodontic Society Clinical Effectiveness Bulletin, I’ve taken a moment to reflect on my time in the role. It has been a privilege to help shape the direction of the Bulletin and to work alongside such a dedicated editorial team, contributors, and readers.
One of the highlights of this period was overseeing the publication of our 50th issue — a significant milestone that speaks to the enduring relevance and quality of the Bulletin. Reaching this landmark was not just a celebration of longevity, but a testament to the collective efforts of all those who have contributed over the years.
Another achievement I’m particularly proud of is the development of a searchable digital archive of past articles, available on the Society’s website. This resource opens up decades of insight, discussion and scholarship to a wider audience, and I hope it will continue to support both clinical practice and academic inquiry for years to come.
Adverse Incident Reports
Since the last edition report (Spring 2025) there have been 2 incidents reported to the Society through our confidential reporting system.
A transpalatal arch fractured at the solder point whilst a patient was eating, and was subsequently swallowed. The patient was referred to A&E, following radiographic examination they were advised to allow the appliance to pass, no surgical treatment was required. Subsequent to which, a review of materials of the laboratory as well as the addition of a warning on the statement of conformity regarding safe use of intra-oral devices and risk of fracture. It was thought the appliance fatigued over time.
Congratulations to the CEB Prize winners who were announced at the conference, Ailidh Carney, Sean Daley and Joseph Bell – very well done. The quality of submissions remains high for the Bulletin, which really does make choosing the winners difficult for the Editorial team!
Throughout my time as Editor, I’ve been continually inspired by the breadth of perspectives and the spirit of collaboration that defines our community. Thank you to all who have submitted articles, offered feedback, and supported the Bulletin in countless ways. I would like to extend specific thanks to Dr Stephen Chadwick, Mr Chris Baker and the team for their support in producing this issue of the Bulletin. Finally, I would like to wish Dr Madeleine Storey all the best as she takes on the role of Editor. I leave the role with a deep sense of gratitude and confidence in the future of the publication.
Robert Smyth Editor, BOS Clinical Effectiveness Bulletin
Following the fitting of fixed anterior bite turbos on the upper central incisors, external resorption on palatal aspect of UL1 was noticed. The bite turbo was subsequently removed and the patient referred for investigation regarding root canal treatment. The bite turbo was constructed chairside using a mould and filled composite. Possible increase in occlusal forces may have contributed to the resorption.
Farooq Ahmed
Adverse Incidents Officer British Orthodontic Society
Assessment of orthodontic case complexity for NHS hospital treatment: A multicentre audit.
V Ravindra, L Cockerham, K Patel, L Davenport-Jones, R Stephens, G Mack
Are we checking orthodontic new patients for oral cancer abnormalities? A local two-cycle audit at the Queen Victoria Hospital.
L Brooks, L Rennie
A two-cycle audit assessing the orthodontic attendances at the Royal Surrey Hospital.
J Watt, S K Kassam, N Taylor, G Minhas
A service evaluation of virtual orthodontic education clinics at the Birmingham Dental Hospital.
N Caratela, A Bains, S Higgins, S Kotecha
A multi-centre two-cycle audit into the use of Cone-Beam Computed Tomography (CBCT) for investigation of ectopic canines.
B Gill, F Jones, C Casey
A two-cycle audit to assess orthodontic treatment outcomes at Liverpool University Dental Hospital.
YM Lin, S Turner, J Harrison
Patient experience of digital scans in the orthodontic department at King’s Dental Institute: A service evaluation.
B McGuckin, J Watt, M Shahid Noorani
Managing the gap: a local service evaluation of the multidisciplinary management of hypodontia.
SL Tan, M Aldihani, R Jennings, H Moseley, FS Ryan
Ectopic maxillary canine referrals: A two-cycle audit.
A Carter, R O’Brien
An assessment of patient understanding of the risks of orthodontic treatment at The Royal London Hospital.
E Johnson, P Jauhar
Complexity of hospital orthodontic new patient referrals accepted for treatment: A two-cycle audit.
MB Javed, R McDowall
Canine assessment at the optimal age: A three-centre retrospective audit.
O Thompson, E O’Sullivan
Assessment of orthodontic case complexity for NHS hospital treatment: a multicentre audit
Vinya Ravindra (ST), Laura Cockerham (Orthodontic Therapist), Kishan Patel (Post CCST), Lucy Davenport-Jones (Consultant), Rachel Stephens (Consultant) and Gavin Mack (Consultant) King's College Hospital NHS Foundation Trust, London, UK
Background/Rationale NHS England produced guides for commissioning dental specialities in 2015 and subsequently produced the clinical standard for orthodontics in 2023 to reflect the need and complexity of patient care and clinician competency required to undertake treatment1,2. The framework describes the patient journey from primary care to specialist care and aims to generate consistency at a national level, ensuring effective utilisation of NHS resources by rationing service commissioning in orthodontics. The guide categorises the provision of treatment based on tier complexity levels (level 1, 2, 3a and 3b) with referrals to secondary care for consultant specialist services fulfilling level 3b criteria based on treatment complexity, multidisciplinary (MDT) input, medical and/or social history.
Specialty registrars (StRs) and specialists undertaking higher training after their Certificate of Completion of Specialist Training (post-CCST) should have an adequate case mix (level 3a and/or 3b respectively) to fulfil training requirements stated in the Orthodontics Specialty Training Curriculum produced by the Special Advisory Committee (SAC) and quality assured by the General Dental Council (GDC)3,⁴. Patients accepted for treatment must demonstrate excellent oral hygiene, absence or stabilisation of oral disease and commitment to the overall treatment, including their willingness to attend frequent appointments and motivation towards wearing appliances.
Aims and Objectives
This multicentre audit aims to assess the complexity of orthodontic referrals received and case acceptance to demonstrate compliance with the NHS England commissioning guide as well as the ability to fulfil postgraduate training requirements for training orthodontic specialists and post-CCST.
The objectives were to assess the complexity of orthodontic referrals by means of the complexity descriptors defined in the NHS England commissioning guide and assess the criteria for case acceptance for orthodontic treatment based on complexity, training provision and dental health status at 3 postgraduate orthodontic training units in South London - King’s College Hospital (KCH), St George’s Hospital (SGH) and Queen Mary's Hospital (QMH).
Standards/guidelines/evidence base
The regionally agreed standards between the units were based on previously published audits⁵,⁶. The first standard was that 80% cases accepted for orthodontic treatment should be IOTN 4/5 and/or complexity level 3b1,3,⁴. The second standard was 100% of accepted cases should be deemed
suitable for orthodontic treatment (i.e. excellent oral hygiene and no active dental disease)2.
Standards for this project were adopted as follows: 100% of referrals for ectopic canines should be received for orthodontic assessment between the ages of 10-12 years of age. 100% of referrals for ectopic canines should have the appropriate accompanying radiographs of good diagnostic quality.
Sample and data source
All patients who attended new patient clinics over a 4 consecutive week period (8th January 2024 – 2nd February 2024) at all 3 sites were included in this audit cycle. Patients were identified through electronic case note review using the relevant consultant-led new patient clinic codes with consultant-led triaging of the referrals to populate the face-to-face assessments. All patients who attended the new patient clinics were included in the sample with no restriction on age and gender.
Audit type
Retrospective
Methodology
A data collection tool was developed and piloted amongst all relevant orthodontic departments to ensure homogenous data collection. The data collection forms were completed using the electronic clinical notes from the new patient assessments and then collated onto a Microsoft Excel spreadsheet. Cases were excluded in the presence of insufficient data.
Patient demographics were captured, and each patient allocated a local audit patient identification number. Medical and social history was also noted to justify case acceptance owing to patient management in secondary care. The referring practitioner and details about the presenting malocclusion including IOTN and tier
complexity were included as well as MDT requirements and clinic outcome.
Findings
Within the 4-week period, 76 patients were identified at KCH, 35 patients at SGH and 43 patients at QMH. At KCH, 27 (36%) patients were accepted for treatment, 9 (26%) at SGH and 35 (81%) at QMH. 11 (15%) patients were planned for consultant-led review and 2 for other treatment including debond and retainers only at KCH. 1 patient was referred to another specialty at SGH and 1 patient planned for consultant-led review at QMH (Figure 1). Table 1 describes the IOTN, tier complexity levels, dental health status, clinic outcome and reasons for discharge across all units.
Table 1 IOTN, tier complexity level, outcome and dental health status of accepted and discharged patients
Table : IOTN, tier complexity level, outcome and dental health status of accepted and discharged patients
1: Outcome of new patient clinic assessment
The results from this audit cycle show that the set standard of 80% for cases accepted with IOTN 4 or 5 and/or tier complexity level 3b was only met at SGH with 100% IOTN 4/5 and 90% complexity 3b. At KCH and QMH, 85% and 89% were IOTN 4/5 respectively, however, 74% complexity 3b at both sites. Furthermore, the set standard of ‘100% cases accepted for treatment should be dentally fit’ was not met at any of the sites with 11% accepted patients deemed not dentally fit at KCH and QMH. 22% accepted patients at SGH were not dentally fit.
Primary reasons for discharge were patients not meeting the criteria for hospital orthodontic treatment, cases suitable for treatment in specialist practice and being deemed too early for treatment.
Figure 2 summarises the main reasons for discharge collectively.
Observations
This audit demonstrated that the included orthodontic units were not appropriately accepting cases for orthodontic treatment with regards to tier complexity, case mix and dental health status.
This may be attributed to a shortage of patients for trainees at KCH with the absence of an active waiting list to allocate from during the set audit period. Thus, the threshold for case acceptance is likely to have been lower to ensure training requirements are met and trainees have an adequate number of patients to treat with a varied case mix. KCH and QMH are also part of the same trust and accommodate more trainees in comparison to SGH resulting in a greater demand for training cases.
Figure 2: Primary reason for discharge following new patient clinic assessment
Dental trauma and development defects (e.g. amelogenesis imperfecta) may also justify case acceptance below the level 3b complexity tier.
Although several patients were accepted with inadequate dental health (poor oral hygiene and/or active caries), they were appropriately informed that orthodontic treatment would only commence on establishment of a dentally fit status with demonstration of excellent oral hygiene. Furthermore, a significant number of patients were referred to a multidisciplinary clinic of which the outcome is unknown and not within the remit of this audit. Patients with active dental disease may have been referred to the clinic for extraction based treatment only and therefore it is unclear whether these patients were accepted for orthodontic treatment following the multidisciplinary assessment.
A previous similar audit undertaken by Sedgwick et al. (2021) used the same standard for case complexity, which was successfully met in their audit6. In this audit, only IOTN was used as a measure of treatment need but the Index of Functional Treatment Need (IOFTN) should have also been included in the audit standards for patients referred for orthognathic surgery, similar to the previous audit. This may have resulted in case acceptance with a lower IOTN for orthognathic patients with a greater functional treatment need, thus deviating from the set standard.
The limitations of the audit include insufficient documentation and subsequent bias as data was collected retrospectively.
Recommendations
1. Findings will be disseminated to the wider team as well as referring practitioners to encourage more referrals to the department of dentally fit patients.
2. Electronic new patient clinic documentation templates to be amended to include all data required in this audit to minimise bias in a 2nd audit cycle when data can be collected prospectively ensuring that appropriate measures including IOFTN can be included.
3. Assessment of incoming referrals during the triaging stage to evaluate the appropriateness of orthodontic referrals to secondary care at the point of acceptance for face-to-face assessment.
4. Distribution of the complexity of allocated cases can be assessed using individual trainee logbooks.
5. Establishing clear referral guidelines with consistency at a national level would facilitate meeting the agreed standards and ensure effective utilisation of NHS resources as well as optimising the quality of clinical care that can be provided.
Project involvement
Dr Vinya Ravindra (Project lead)
Ms Laura Cockerham (Data collection assistant)
Dr Kishan Patel (Reviewer)
Miss Lucy Davenport-Jones (Supervisor)
Miss Rachel Stephens (Supervisor)
Mr Gavin Mack (Supervisor)
References
1. NHS England (2015b) Guides for commissioning dental specialties: orthodontics. Available at: https://www.england. nhs.uk/commissioning/wp-content/uploads/ sites/12/2015/09/guid-comms-orthodontics.pdf
2. NHS England. (2023). Clinical standard to dental specialties – orthodontics. Available at: https://www.england.nhs.uk/ publication/clinical-standards-for-dentalspecialties-orthodontics/
3. The Joint Committee for Postgraduate Training in Dentistry and The Specialist Advisory Committee in Orthodontics. Curriculum and Specialist Training Programme in Orthodontics. 2010. Available at https://www.gdc-uk.org/docs/ default-source/specialist-lists/ orthodonticcurriculum.pdf?sfvrsn=76eecfed_2
4. Joint Committee for Postgraduate Training in Dentistry (2012) Guidelines for UK post-CCST training appointments in orthodontics. Available at: https://www.rcseng.ac.uk/-/media/files/rcs/ fds/careers/jcptd/guidelines-for-postccsttraining-Orthodontics-july-2012.pdf
5. Giles, E., Rizvi, Z., Gray, J. A., Barker, C. S., & Spencer, R. J. (2019). To accept, or not to accept? A service evaluation to appraise complexity assessment of orthodontic patients referred into a secondary care setting. British dental journal, 226(12), 963–966. https://doi.org/10.1038/s41415-019-0384-6
6. Sedgwick, M., Nirmal, H. and Bhamrah, G. (2021) ‘Assessment of referral complexity and case acceptance for NHS Hospital Orthodontic Treatment’, Faculty Dental Journal, 12(3), pp. 138–143. doi:10.1308/rcsfdj.2021.33.
Are we checking orthodontic new patients for oral cancer abnormalities? A local two-cycle audit at the Queen Victoria Hospital
Laura Brooks (ST) and Lisa Rennie (Consultant)
Orthodontic Department, Queen Victoria Hospital NHS Foundation Trust, East Grinstead, UK
Background/Rationale An extra and intra-oral examination to screen for soft and hard tissue abnormalities is an essential part of orthodontic and dental care, along with asking patients about their smoking/vaping status and alcohol intake1. The incidence of oral cancer has increased in the UK by 34% in the last decade, with a significant increase of 19% and 22% in overall cancer rates in patients aged 0-24 and 25-49 years respectively2. The majority of secondary care orthodontic patients are in this age group, therefore a thorough history and examination is essential to detect any abnormalities. Risk factors for oral cancer include: smoking and alcohol (synergistic effect), chewing tobacco/betal nut, poor diet with <5 portions of fruit and vegetable/day, HPV (human papillomavirus) and social deprivation3, ⁴. Screening is important as early detection can boost the chances of survival from 50-90%3. In the orthodontic clinical notes, a full extra-oral and soft tissue examination was not often documented and few clinicians recorded patient’s smoking/vaping status and alcohol intake. This audit was essential to improve record keeping and standards of care delivered to patients.
Aims and Objectives
This audit aimed to assess the documentation of extra-oral and intra-oral soft tissue assessment of all new patients in the orthodontic department along with the smoking/vaping and alcohol status of adult patients. The audit also aimed to raise awareness of the importance of screening for oral abnormalities and to make recommendations to improve record keeping.
Standards/guidelines/evidence base
100% of new patient clinical notes to document the following details as part of a new patient assessment as stated by the Faculty of General Dental Practice 2016 Good Practice Guidelines - Clinical Examination and Record Keeping1.
Criteria: (1) An extra-oral examination including the TMJ, lymph nodes and asymmetries. (2) An intra-oral soft tissue examination. (3) Smoking status, vaping status and alcohol intake in patients over 18 years of age as this is the legal age to smoke/vape and drink alcohol in the UK⁵-⁷. Although 40% of 11-15 year olds have had an alcoholic drink and 9% are e-cigarette users, 43% were secret smokers and their family did not know⁸. It was felt as the vast majority of under 18 year olds are accompanied by their parents/legal
guardian to their appointment, they would not be entirely truthful regarding their smoking/vaping and alcohol status when asked in front of caregivers.
Sample and data source
Data was collected from the clinical notes of 50 consecutive new patients attending orthodontic new-patient clinics at the Queen Victoria Hospital, in October 2023 (cycle 1) and May 2024 (cycle 2). All patients were included regardless of age or if they were referred for orthodontic treatment or a mandibular advancement splint for obstructive sleep apnoea. No exclusion criteria was used. The clinical notes were accessed via the Trust electronic notes system.
Audit type
Retrospective.
Methodology
Data was collected from new patient notes and entered into a proforma. The following data was collected: age of the patient, date of the new patient clinic, type of patient (<18 yrs, >18 yrs or referred for a mandibular advancement splint), grade of the clinician that examined the patient, extra-oral examination: asymmetry, lymph nodes, TMJ; intra-oral soft tissue examination; smoking/ vaping and alcohol status.
Patients attending the new patient clinic ranged from 7 to 66 years old. The majority (60%) were under 18 years of age, 22% were over 18 and a further 18% were referred for the construction of mandibular advancement splints for managing obstructive sleep apnoea (OSA) (Figure 1: Types of patients in new patient clinic). Most patients were examined by a consultant (72%), 18% by a post CCST, 6% by an associate specialist and 4% by a specialist registrar. There was no difference
between the level of documentation and the grade of the clinician. Clinical entries correctly recording the required information in the 1st cycle (October 2023) were as follows: TMJ 52%, asymmetry 52%, lymph nodes 2%, soft tissues 14%, smoking/ vaping status 10% and alcohol status 25% (Figure 2: Documentation results-extra-oral and intra-oral assessment, Figure 3: Documentation results- alcohol and smoking/vaping status). None of the clinical entries recorded all three parts of the extra-oral examination required, which included the TMJ, the presence of asymmetry and examination of the lymph nodes.
Types of patients in new patient clinic
2: Documentation results - extra-oral and intra-oral assessment
status
Intervention
The results were presented at the Orthodontic Department Audit Meeting in March 2024 to raise clinicians’ awareness of the importance of recording a full extra-oral and soft tissue examination along with the alcohol and smoking/vaping status of patients. Clinicians were also encouraged to update their new patient proformas. A teaching session was given to the orthodontic department on oral cancer including trends, signs and symptoms and risk factors and a re-audit was planned for May 2024.
Cycle 2
In cycle 2 (May 2024), the patients seen ranged from 9-75 years old. Most (84%) were under 18 years old, 8% were over 18 and 8% were referred for mandibular advancement splints to manage obstructive sleep apnoea. (Figure 1: Types of patients in new patient clinic). The majority of patients in this cycle were also examined by a consultant (66%), 2% post CCST, 18% by an associate specialist and 14% by a specialist registrar. Again in cycle 2, there was no difference between the level of documentation and the grade of the clinician. The percentage of clinical entries correctly recording the required information had each increased as follows: TMJ 78%, asymmetry 92%, lymph nodes 70%, soft tissues 78%,
smoking/vaping status 43% and alcohol status 43% (Figure 3: Documentation results - alcohol and smoking/vaping status). In 56% of patients all three aspects of the extra-oral examination were recorded (Figure 2: Documentation results-extra-oral and intra-oral assessment).
Observations
The gold standard was not met in either cycle but significant improvements were made after changes were implemented, which included presenting the audit results to the Orthodontic Department Audit Meeting, changing new patient clinic proformas and providing an oral cancer teaching session. Examination of the lymph nodes increased by 68% (cycle 1: 2%, cycle 2: 70%) and the soft tissues by 64% (cycle 1: 14%, cycle 2: 78%). These two aspects of a full patient examination are particularly important in detecting oral cancer, however, they were less commonly recorded possibly because they do not influence orthodontic treatment planning and are therefore more easily forgotten. Although less relevant in detecting oral cancer, the examination of the TMJ increased by 26% (cycle 1: 52%, cycle 2: 78%) and asymmetry increased by 40% (cycle 1: 52%, cycle 2: 92%). They were recorded more in both cycles than other factors as they are more relevant to treatment planning.
The alcohol and smoking/vaping status of patients were less commonly recorded and the results from cycle two showed that this was only noted in 43% of adults. It was observed that the department’s medical history form does not include a section where smoking/vaping and alcohol status can be documented, most likely because the vast majority of our patients are under 18 years of age. Importantly, age does not preclude those patients from smoking/vaping and drinking and it is important to know a patient’s smoking/vaping status as it can increase the risk of infection following dentoalveolar or orthognathic surgery⁹. If patients are smoking/vaping and drinking heavily, it is our duty of care as clinicians to signpost them to smoking/vaping cessation and alcohol support services for their general health and well being. Following cycle 2, the department has approved a new medical history form that includes smoking/vaping and alcohol status.
The OSA patients seen in the department are generally of an older age cohort than the orthodontic patients (age 56-75 years). These patients are referred by the secondary care respiratory sleep services, rather than primary care, and during the audit it was observed that a significant number of the OSA patients had not accessed dental care for many years. Patients reported that difficulties accessing a NHS dentist, especially since COVID-19, have increased this trend. This patient cohort is therefore potentially at a higher risk of undetected hard and soft tissue abnormalities due to their age, especially as OSA and oral cancer patients can share common risk factors10. It is essential that a thorough extra and intraoral examination is carried out and clinicians should be mindful that some groups of patients may not have regular screening with a GDP.
Recommendations
1. Update the department’s medical history form to include smoking, vaping and alcohol status. This was introduced in December 2024.
2. Present the results of both cycles at the next Orthododontic Department Audit Meeting.
3. Ensure all clinician new patient proformas include the required information to ensure 100% compliance in the re-audit.
4. Re-audit in 12 months and as an improvement of the audit to ask patients under 18 years old their alcohol and smoking/vaping status, as previously mentioned NHS England surveys show young people in this age group regularly drink and smoke/vape.
Project involvement
Laura Brooks (Project lead, project design, data collection, analysis, presentation, manuscript preparation).
Lisa Rennie (Project supervision, project design and manuscript review).
References
1. Hadden AM. Clinical Examination and Record Keeping: Good Practice Guidelines. 3rd ed. London: Faculty of General Dental Practice (UK); 2016.
2. Cancer Rearch UK. Cancer incidence by age [Internet]. London: Cancer Research UK; 2024 [Accessed 23rd April 2025]. Available from: https://www.cancerresearchuk.org/healthprofessional/cancer-statistics/incidence/age#heading-Three.
3. Oral Health Foundation. The State of Mouth Cancer UK Report 2024 [Internet]. Rugby: Oral Health Foundation; 2024 [Accessed 23rd April 2025]. Available from: https://www.dentalhealth. org/thestateofmouthcancer.
4. Ravaghi V, Durkan C, Jones K, Girdler R, Mair-Jenkins J, Davies G, et al. Area-level deprivation and oral cancer in England 2012–2016. Cancer epidemiology. 2020;69:101840.
5. GOV.UK. Alcohol and young people [Internet]. UK: GOV.UK; 2025 [Accessed 24th April 2025]. Available from: https://www.gov.uk/ alcohol-young-people-law#:~:text=If%20 you're%20under%2018%2C%20it's%20 against%20the%20law%3A,to%20buy%20 alcohol%20for%20you.
6. GOV.UK. Youth Vaping: call for evidence. [Internet]. UK: Office for Health Improvement and Disparities; 2023 [Accessed 24th April 2025]. Available from: https://www.gov.uk/government/ calls-for-evidence/youth-vaping-call-forevidence/youth-vaping-call-for-evidence#:~: text=call%2Dfor%2Devidence-,Introduction, substantially%20less%20harmful%20than%20 smoking.
7. Legislation.GOV.UK. Children and Families Act 2014: Tobacco, nicotine products and smoking [Internet]. UK: legistation.gov.uk; 2021[Accessed 24th April 2025].
Available from: https://www.legislation.gov.uk/ ukpga/2014/6/part/5/crossheading/tobacconicotine-products-and-smoking#:~:text=92 Prohibition%20of%20sale%20of,to%20 persons%20aged%20under%2018.
8. NHS England. Smoking, Drinking and Drug Use among Young People in England, 2021 [Internet]. England: NHS England; 2022 [Accessed 24th April 2025]. Available from: https://digital.nhs.uk/ data-and-information/publications/statistical/ smoking-drinking-and-drug-use-among-youngpeople-in-england/2021/part-5-alcohol-drinking-prevalence-and-consumption#pupils-whohad-an-alcoholic-drink-in-the-last-week.
9. Kuhlefelt M, Laine P, Suominen AL, Lindqvist C, Thorén H. Smoking as a significant risk factor for infections after orthognathic surgery. Journal of Oral and Maxillofacial Surgery. 2012;70(7):1643-7.
10. Mitra AK, Bhuiyan AR, Jones EA. Association and Risk Factors for Obstructive Sleep Apnea and Cardiovascular Diseases: A Systematic Review. Diseases. 2021;9(4):88.
A two-cycle audit assessing the orthodontic attendances at the Royal Surrey Hospital
John Watt (ST), Shaira Karim Kassam (Post CCST), Nigel Taylor (Consultant Orthodontist) and Gursharan Minhas (Consultant Orthodontist)
Royal Surrey County Hospital, Surrey, London, UK
Background/Rationale
Unsupervised orthodontic treatment following missed appointments can be detrimental to patients’ dental health, compromise treatment outcomes and have financial impacts on limited NHS resources creating further pressures on waiting lists. Many orthodontic patients are dependent on their parents/guardians to attend appointments, therefore the ‘was not brought’ (WNB) initiative was developed to recognise that children (0-17 year-olds) are not responsible for their missed appointments¹. Non attendance for this cohort of patients should be recorded in the clinical notes as ‘WNB’, instead of ‘Did not Attend’ (DNA). To ensure appropriate outcomes regarding missed appointments, both WNB and DNA should be documented and followed-up. Correct documentation allows clinical staff to monitor potential safeguarding concerns and to identify when to discharge patients with poor attendance to improve best use of resources.
Aims and Objectives
The aims of this audit include:
i) Reviewing attendance (WNB and DNA) of all orthodontic appointments, including new patient clinics, treatment clinics and multidisciplinary clinics specifically in line with the set standard.
ii) Developing a new departmental protocol to ensure appropriate follow up and management occur, following missed appointments.
The objective is to ensure all missed appointments are appropriately recorded, including the safeguarding management for 0–17 year-old vulnerable patients at the Royal Surrey Hospital.
Standards/guidelines/evidence base
All WNB appointments must be followed-up; either discharged with letter sharing information to General Dental practitioners/General Medical practitioners (GDP/GMP), or a further appointment arranged as per WNB guidance1.
Sample and data source
The data sample included all orthodontic patients attending orthodontic appointments at Royal Surrey Hospital, including new patient assessments and attendance on multidisciplinary clinics with
allied specialities. Period of data collection included between October 2023-January 2024 (n= 2877) and after allowing for a period of change, May 2024 – July 2024 (n=1297). Data was collected from trust computer systems and confirmed from paper clinical diary logbooks to assess patient attendance and outcomes when patients failed to attend. Data was separated between 0-17 years old (WNB) and those 18 and over (DNA).
Audit type
Retrospective audit for the first cycle and prospective audit for second cycle, following the action plan and implementation of the protocol.
Methodology
Electronic patient records (Cerner) and clinical paper logbooks within the orthodontic department at the Royal Surrey Hospital were reviewed during select dates for each cycle of this audit. The first cycle was retrospective to align with the start date of new orthodontic trainees within the department (October 2023). The second cycle was prospective following local and regional presentation of results. Data collection included all orthodontic appointments including multidisciplinary clinics with allied specialities, new patient clinics and all clinicians’ treatment sessions within the orthodontic department. Orthodontic clinicians within the department included three
orthodontic consultants, one speciality doctor, five orthodontist registrars and one orthodontic therapist. Specific information collected for analysis included patient attendance at appointment, patients age at appointment, type of clinic (i.e. treatment, new patient, multidisciplinary), type of treatment if applicable (i.e. fixed adjust, retainer review etc.), day of the week, documentation of DNA/WNB evidenced in clinical notes, and outcome if the patient missed the appointment (i.e. appointment rescheduled, patient discharged, telephone follow-up etc.).
Results from the initial audit cycle were discussed at a local audit meeting with implementation of a new protocol (diagram 1), followed by a regional orthodontic audit discussion. The second cycle of data collection used the same method and commenced after a 3-month period, to allow change. There was no exclusion of patients who repeatedly failed to attend their appointments.
Findings
Between the first and second cycles, there was an overall improvement in attendance rate, record keeping and appropriate follow up (Table 1).

Table 1: Summary of results ducation Delivered
From this audit, orthodontic missed appointment rate decreased from 5.67% (163/2877) to 3.79% (49/1294). Documentation in clinical notes, recording appropriately whether a patient failed to attend their appointment, dramatically improved between cycles from 36.81% (60/163) to 75.51% (37/49).
Appropriate follow up for WNB appointments had improved from 58/60 (96.67%) to 14/14 (100%), meeting our standard that all patients 0-17 years of age, who miss their appointment should be appropriately followed up. The rate of WNB missed appointments had decreased between cycles from 60/163 (36.81%) in the first cycle to 14/49 (28.57%) in the second cycle.
From types of appointments missed in the first cycle, 123/163 (75.46%) of appointments were treatment sessions vs 40/163 (24.54%) joint clinic assessments. The second cycle is 37/49 (75.51%) vs 12/49 (24.49%) joint clinics. The significance is that MDT appointments may have greater financial implications to the trust or greater impact on overall to treatment if the patients are mid-treatment and have to be placed on a waiting list to be seen again.
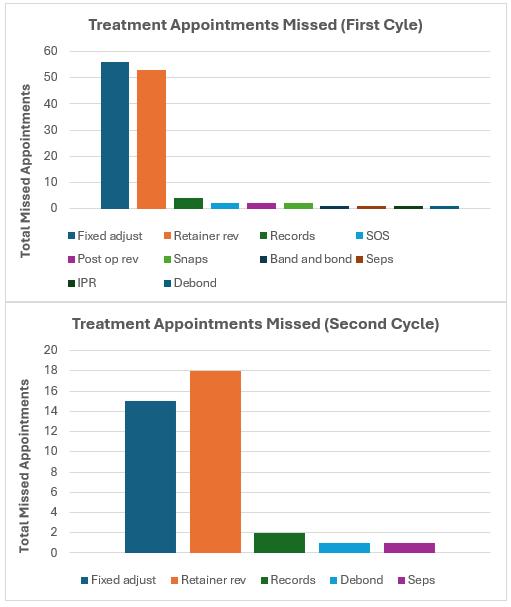
Table 2: Comparison of missed treatment appointments, between cycles
The majority were unsurprisingly fixed adjust appointments 56/123 (45.53%) followed by retainer reviews 53/123 (43.09%). Both of these make up large portions of appointment types in orthodontic patients. Other missed appointments included records 4/123 (3.25%), emergency ‘SOS’ appointments/post operative reviews and snap reviews which has 2/123 patients missing their appointment for each category (1.63%). Placement of separators, interproximal reduction (IPR), band and bond and debond each made up 1/123 (0.81%) patient for each category.
In the second cycle there was less variation in the type of appointments which were missed, likely due to smaller sample size. Retainer reviews and fixed adjust appointments made up the majority of missed appointments 18/37 (48.65%) and 15/37 (40.54%) retrospectively. Other missed appointments included orthodontic records 2/37 (5.41%) and a single patient missed an appointment for placement for separators and a debond 1/37 (2.70%)
Observations
The first cycle failed to achieve the standard criteria with 96% of WNB patients appropriately followed up. However, the standard criteria of 100% was met in the second cycle. A local protocol was developed to minimise missed appointments and to ensure appropriate safeguarding outcomes were followed. The protocol, based on the published BDA flowchart 2 was shared with all staff and suggests patients are contacted within 72 hours of not attending, with different stages of outcomes depending on treatment type (Diagram 1).
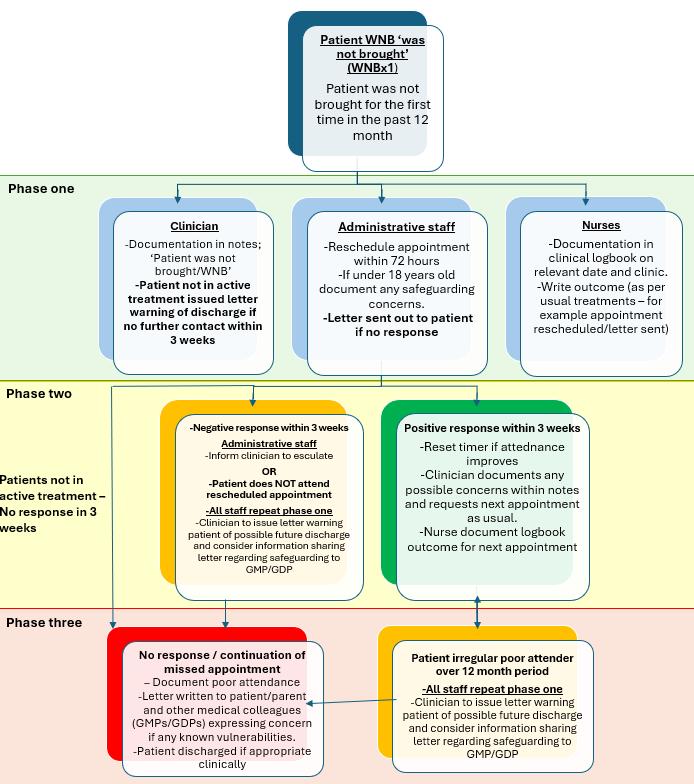
Despite most patients being appropriately followed up, there was a lack of documentation of patients missing appointments within the Trust’s electronic paper record (EPR) system. Failure of documentation makes it difficult for staff to identify trends in poor attendance and potential safeguarding concerns. Following the implementation of the protocol (Diagram 1) there was a dramatic increase in documentation of missed appointments within the EPR (36.81% vs 75.51%).
Between cycles, there is a decrease in the department's missed appointments rate from 5.67% to 3.79%. This is lower than the national average of all NHS specialities of 6.43% from the 2022/23 publication3. The overall percentage of 0-17 year-olds not attending their appointments had decreased, potentially due to an increase in letters warning of safeguarding concerns (36.81% vs 28.57%).
The majority of appointments patients failed to attend in both cycles were ‘active treatment sessions’ (75.46% and 75.51%) (figure 2). Both cycles had similar representation of ‘fixed adjust’ and ‘retention’ appointments which were missed, that made up most of the overall missed appointments.
In the first audit cycle, fixed adjust accounted for 56/123 (45.53%) of missed appointments, followed by retention reviews 52/123 (43.09%). In the second cycle fixed adjust represented 15/37 (40.54%) of missed appointments, followed by retainer reviews 18/37 (48.65%) (table 2).
Friday was the least likely day for patients to miss appointments making up 14% vs 10% in the first and second audit cycle, respectively. Whereas missed appointments appear to most likely occur on a Wednesday (first cycle – 34%) or Tuesday (second cycle – 26%). This would correlate with the two days of the week where new patient clinics were scheduled. Further explanation would require further analysis, which is outside the scope of this audit.
In conclusion, to ensure continuation and improvement of results, all new staff will be informed about the missed appointment and WNB
safeguarding protocol. Copies of the protocol have been distributed in folders on clinic for reference. Similar audits have been undertaken at other institutions i.e. Eastman Dental Hospital⁴. Population demographics do vary, and additional Trust information could be useful for a general database for the NHS for orthodontics. This audit demonstrates how it is possible to improve DNA/ WNB rate by putting a protocol in place.
Recommendations
1. All staff need to be aware of the DNA/WNB protocol, including existing clinical and administrative staff and new staff and document on EPR as this indicates to clinician previous WNB and DNA.
2. Protocol can be disseminated to other departments wishing to improve attendance rate and safeguarding measures.
3. Re-audit in 12 months.
Project involvement
John Watt (Audit and protocol design, data collection, audit lead, presenter)
Shaira Karim Kassam (Audit design, data collection)
Nigel Taylor (Audit and protocol design, audit supervisor)
Gursharan Minhas( Protocol design)
References
1. Kirby J, Harris J C. Development and evaluation of a 'was not brought' pathway: a team approach to managing children's missed dental appointments. Br Dent J 2019; 227: 291-297.
2. British Dental Association (BDA). Implementation ‘Was Not Brought’ In your practice, 5 (2000). Available from: wnb-implementation-guide-2024_v3.pdf (Accessed: 04/11/2024).
3. NHS Digital. Summary Report – Attendances. September 2023 cited July 2024. Available from https://digital.nhs.uk. (Accessed: 04/11/2024).
4. Murphy, I, Johnson, A, Sheriteh, Z. Was Not Brought: A three cycle audit of missed children’s appointments in the orthodontic department. BOS Clinical Effectiveness Bulletin. 2023; 50: 44-47
A Service Evaluation of Virtual Orthodontic Education Clinics at the Birmingham Dental Hospital
Nabeela Caratela (DCT), Amandeep Bains (ST) and Shane Higgins (Consultant Orthodontist) and Sheena Kotecha (Consultant
Orthodontist) Birmingham Dental Hospital, UK
Background/Rationale Patients on the orthodontic treatment waiting list at Birmingham Dental Hospital are invited to attend a 45-minute virtual education clinic with an oral health education trained orthodontic nurse. This takes place prior to their initial orthodontic records appointment. The consultation includes a PowerPoint presentation and discussion focussing on:
1. The risks of orthodontic treatment including dental caries and decalcification.
2. Tailored oral hygiene (OH) and dietary advice. Patients are given plaque disclosing tablets and are asked to use them 10-15 minutes before the session to demonstrate their tooth brushing technique.
3. The standard of compliance required for successful orthodontic treatment and details of the hospital attendance policy.
4. What to expect at their first clinical appointment and throughout their treatment journey.
The remote consultation clinics have been operational within the department since the COVID-19 pandemic. Lockdown measures during the pandemic forced healthcare systems to reduce face-to-face clinical contact. To minimise aerosol generating procedures (AGPs), it was no longer deemed acceptable for patients to brush their teeth on clinic. Whilst the virtual delivery of oral health education poses some challenges, it confers many benefits regarding opportunities to enhance and update the delivery of patient education1, 2 .
Aims and Objectives
• To assess patient experience of the remote consultations, including suitability for intended purpose, accessibility, clinical value and effectiveness.
• To explore the limitations of online remote consultation clinics for patients.
• To ensure continuous evaluation of remote clinic provision to facilitate improvements for patients using this service.
Standards/guidelines/evidence base
This was a service evaluation with no published guidelines.
Locally set standards were agreed by the department:
• 100% of patients should rate their understanding of the orthodontic treatment process and oral health level expected as “well understood or very well understood” following the remote consultation.
• 100% of patients should agree that safety and confidentiality is not compromised by the remote consultation process.
• 100% of patients should report no technical issues/concerns.
Sample and data source
All patients who completed the virtual clinic were invited to complete a survey directly following the remote consultation. The ‘Smart Survey’ platform was used for the questionnaire. There were no exclusion criteria.
In cycle 1 (October 2022 - June 2023), 36 responses were obtained, and for cycle 2 (July 2023 – January 2024), there were 31 responses.
Audit type
Prospective patient questionnaire-based service evaluation.
Methodology
The service evaluation was registered and approved by the Birmingham Community Healthcare NHS Foundation Trust Clinical Governance Team. The questionnaire was developed within the orthodontic department at the Birmingham Dental Hospital and was piloted with 5 patients via a face-to-face consultation. The final questionnaire was agreed with the Orthodontic Department Lead and Clinical Governance Team.
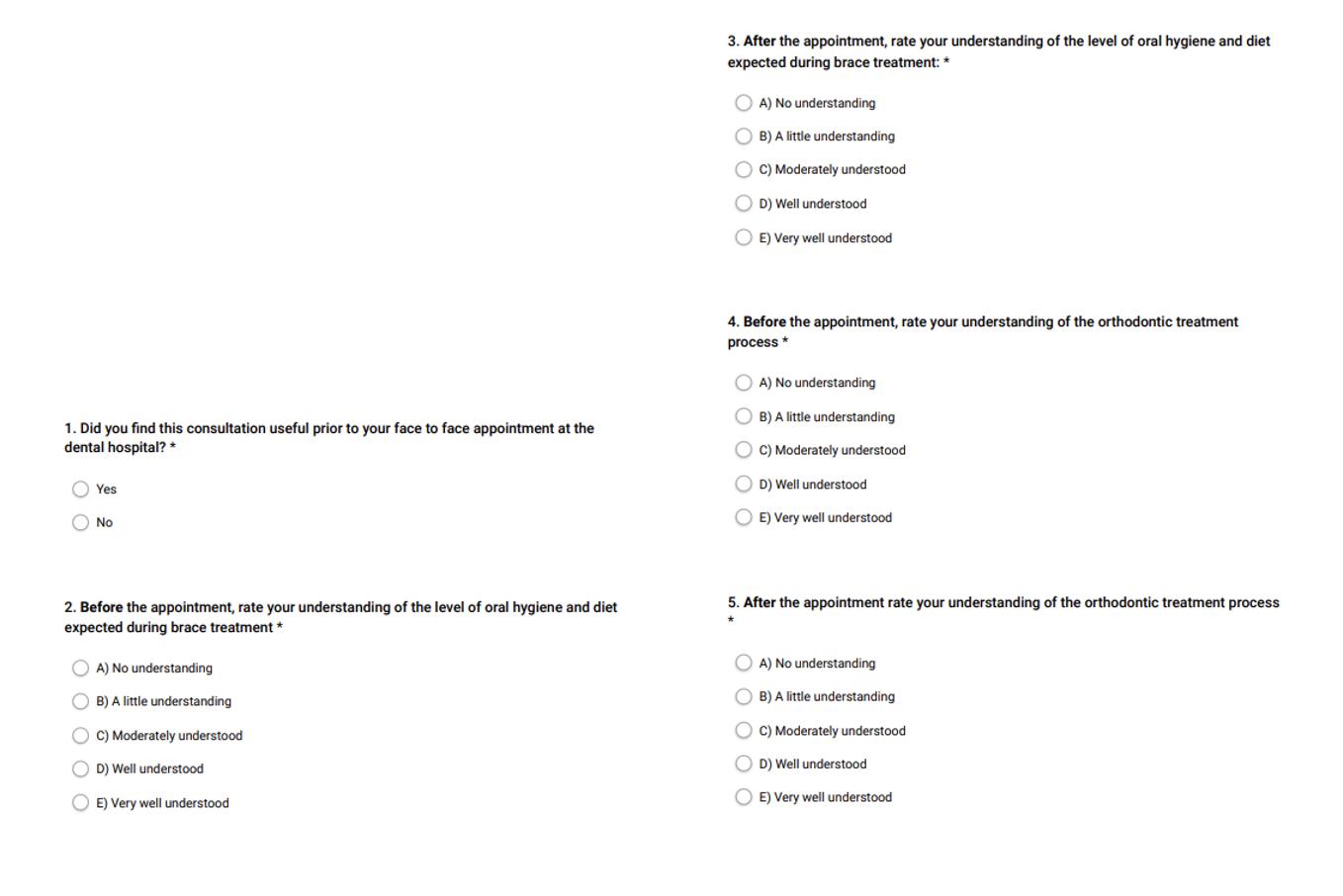
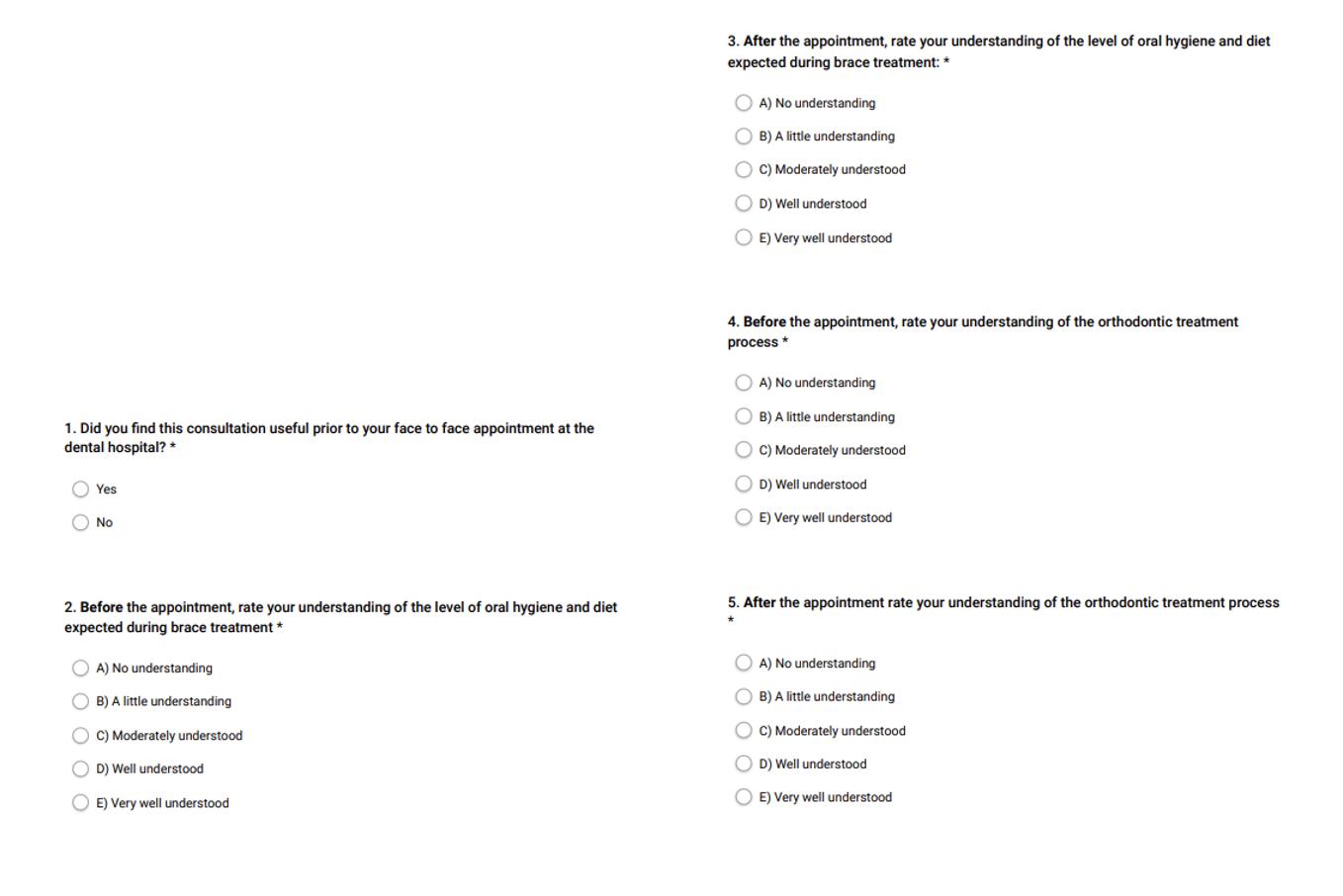
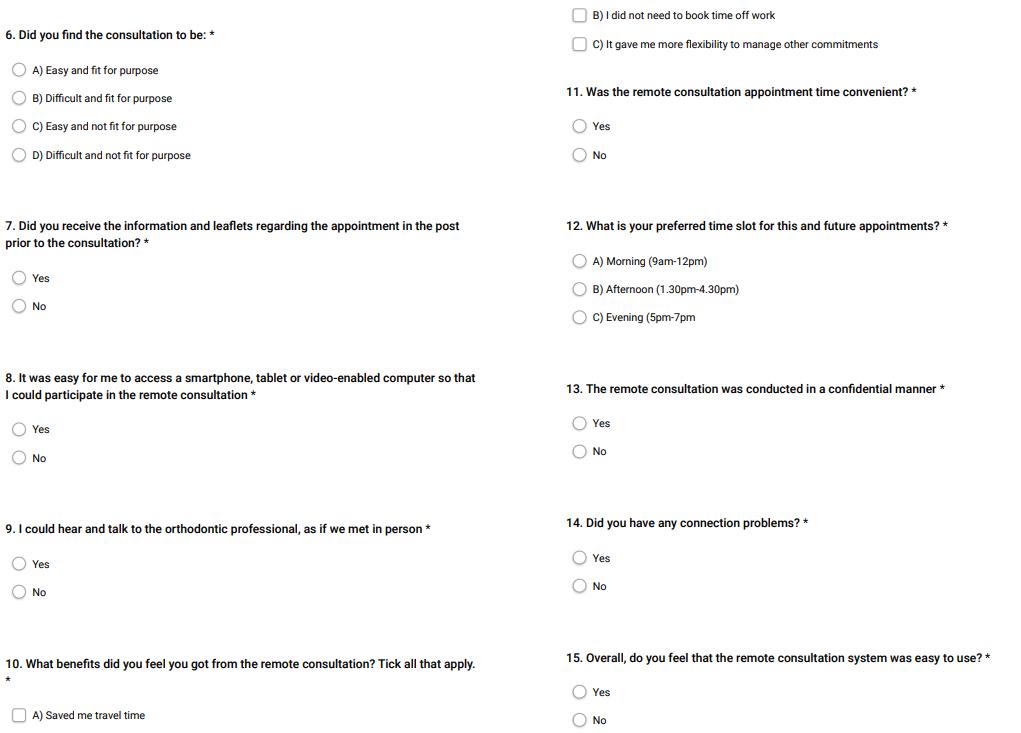
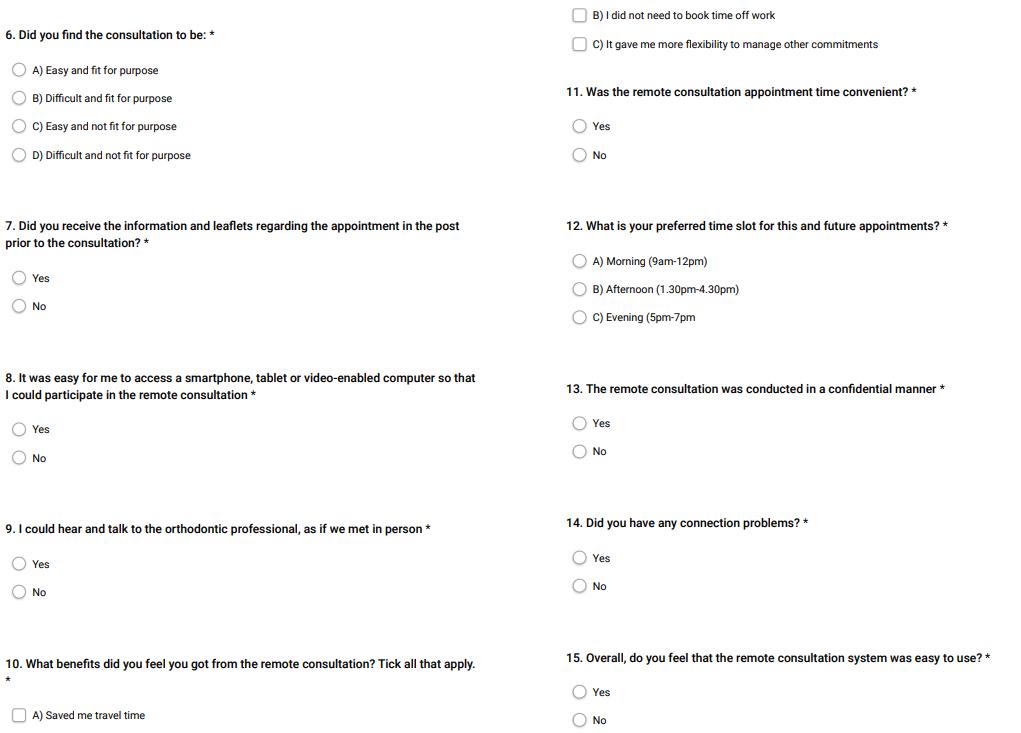
The questionnaire consisted of 15 questions developed to assess patients’ understanding of the orthodontic treatment process, the level of compliance required, ease of access to remote consultations, technical issues encountered and overall patient opinions on the remote clinics.
Anonymous questionnaires were distributed to patients via the online ‘Smart Survey’ platform
(Figure 1) following the virtual clinic for both cycles. For children, the survey was completed by their parents or individual with parental responsibility.
Baseline data were collected in cycle 1 (June 2023). The action plan following this cycle consisted of a revision of the PowerPoint presentation to improve the explanation of patients’ journey throughout
Cycle 2 (January 2024) assessed the impact of this change to the remote clinics.
The data from the questionnaires were analysed using Microsoft® Excel™.
Findings
Across cycles 1 and 2, 100% of participants agreed that their confidentiality was maintained, 100% understood the level of OH expected during treatment and 100% of respondents found the consultation easy to navigate, fit for purpose and useful prior to the face-to-face appointment.
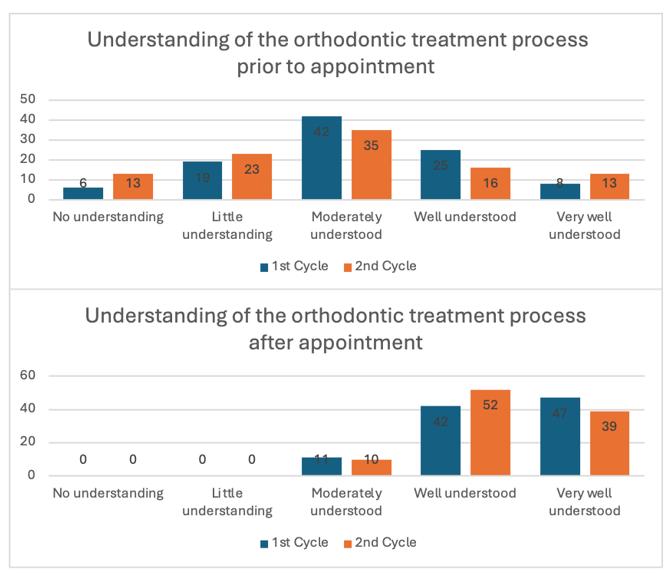
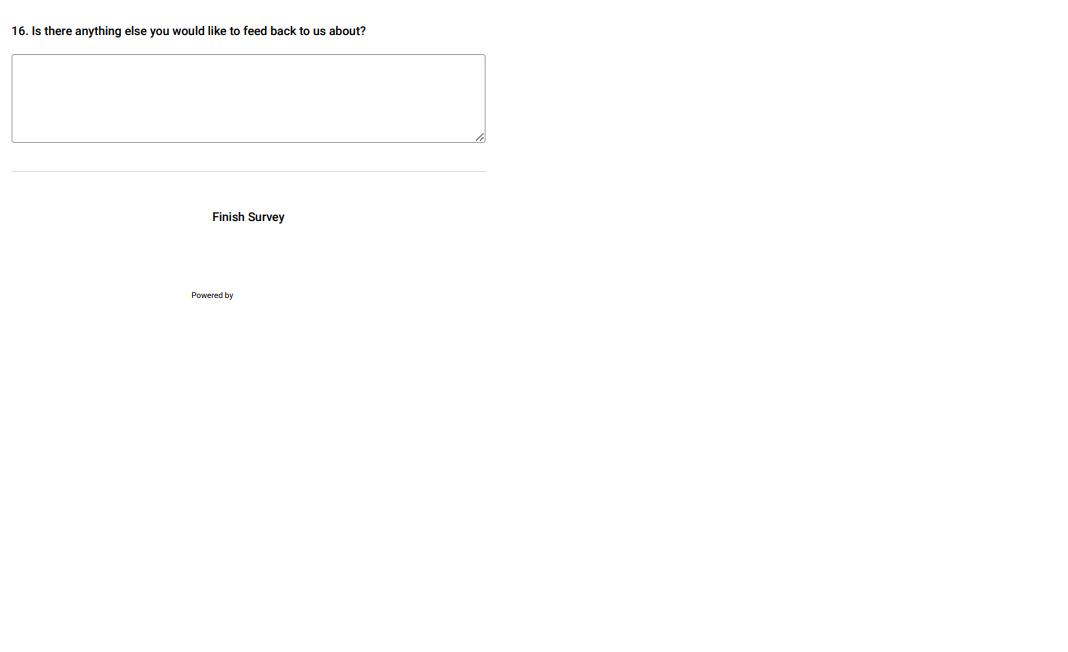
Figure 2: Cycle 1 and 2 results for levels of understanding of the orthodontic treatment process pre and post remote consultation.
The findings in cycle 1 showed that 89% understood the treatment process at the level of ‘well understood or very well understood’ and the remaining 11% reported a ‘moderate’ understanding of process. In cycle 2, 91% understood the treatment process at level of ‘well understood or very well understood’ and the remaining 9% reported a ‘moderate’ understanding post consultation.
Figure 3: Cycle 1 and 2 results for levels of understanding of compliance required for orthodontic treatment pre and post remote consultation.
During cycle 1, 100% reported it was easy to access a smartphone, tablet or computer for the consultation, but this reduced to 93% in cycle 2. In cycle 1, 100% reported they could hear and talk to the nurses as if they were in person and in cycle 2 this was 97%. Fourteen percent of participants reported connection issues in cycle 1, and this increased to 17% in cycle 2. In cycle 1, 94% agreed the consultation was booked at a convenient time for them, however this reduced to 84% in cycle 2.
There were 3 additional comments left by the respondents in cycle 2 stating “very helpful”, “easy to talk to” and “easy to access”.
Observations
Suitability
In both cycles, 100% of patients found the remote consultations suitable for the intended purpose and all patients felt their confidentiality was maintained throughout, encouraging patients’ confidence in the system. All patients are given an anonymised identification number according to their IP address, therefore patient identifiable information is not shared.
Accessibility
Overall, the remote consultations were accessible for patients. However, accessibility was reduced in
the second cycle due to issues with access to devices and internet connection problems. This could likely be due to the optimisation of internet connection and access to devices immediately following the COVID-19 pandemic which could be reflected in cycle 1 findings. Whilst the gradual return to face-to-face work and education activities over time could have resulted in difficulties in accessing the appointments in cycle 2.
Furthermore, 6% of patients reported not receiving the pre-consultation information letter; this could be explained by the postal industrial action during the cycle 2 data collection period. The preferred appointment times in cycle 1 were afternoon and evening, however in cycle 2 the preferred timing of appointments was the morning. Timing preferences vary between patients; differences in appointment time preferences could be due to work/education commitments and appointments corresponding with school holidays. Flexibility with appointment times would help address the differences in patient preference.
Clinical value
All respondents reported the appointment was useful and found it increased their understanding of the standard of oral hygiene and diet required during treatment. The respondents’ understanding of the orthodontic treatment process, sequence of appointments and attendance requirements was also improved. This highlights the benefit of the virtual clinic in making patients aware of their responsibilities in terms of oral hygiene, diet and attendance during their orthodontic treatment.
Benefits to patients
Most patients found the remote clinic saved them travel time. In cycle 2, 84% found the allocated time convenient. Approximately one third of respondents did not need to take leave from work to attend the appointments.
The potential limitations identified in this project were the small sample size and the short length of time between cycles. Additionally, in cases where the patients were children, responses provided by parents may not fully reflect the child’s own understanding or perspective.
Overall, patient attendance at a virtual orthodontic education clinic prior to commencement of orthodontic treatment appeared to be an effective
intervention. Clinicians feel that the levels of understanding regarding treatment and compliance have shown improvement due to the remote clinics. Patient confidentiality is being maintained in the process. Challenges highlighted in this service evaluation include connectivity issues and suitability of appointment times.
Recommendations
1. To review the appointment timing allocation to facilitate patient flexibility and reduce the need to take leave from work for appointments.
2. To consider the implementation of virtual clinics in other areas of orthodontic treatment, for example, retainer review clinics.
3. To complete a further service evaluation to measure the impact of the interventions in 12 months.
4. Aim to increase the response rate of the questionnaire to ensure accuracy of results for the next cycle of the service evaluation.
Project involvement
Nabeela Caratela (Manuscript and project write-up) Amandeep Bains (Project lead, data collection and analysis, presentation of results)
Shane Higgins (Project Supervisor) Sheena Kotecha (Project Supervisor)
Acknowledgements
Thank you to Ms. Sheena Kotecha and Mr. Shane Higgins for supervising this project, and the Orthodontic Nursing Team at the Birmingham Dental Hospital for operating the remote clinics and supporting the data collection for this project.
References
1. Monaghesh E, Hajizadeh A. The role of telehealth during COVID-19 outbreak: a systematic review based on current evidence. BMC public health. 2020 Dec;20:1-9.
2. British Orthodontic Society. Guidance on teledentistry and remote interactions in orthodontic care [Internet]. London: BOS; 2022. Available from: https://www.bos.org.uk/ wp-content/uploads/2022/02/BritishOrthodontic-Society-Guidance-onteledentistry-and-remote-interactions-inorthodontic-careFinal-v5awamended.pdf (Accessed: 01 October 2024).
A multi-centre two-cycle audit into the use of Cone-Beam Computed Tomography (CBCT) for investigation of ectopic canines
Balraj Gill (ST), Francine Jones (Post-CCST) and Christine Casey (Consultant)
The Royal London Dental Hospital, London, UK
Background/Rationale CBCT investigations have many uses within orthodontics and are commonly used for localised examination of the anterior maxillary region to assess the position of ectopic unerupted canine teeth and to exclude root resorption of adjacent incisors1. Plain film radiographs are still considered sufficient for diagnosis in most ectopic canine cases and can be supplemented with use of parallax. CBCT imaging needs to be sufficiently justified to ensure there is ‘net benefit’ to the patient. The principle of optimisation should be taken into account given the effective dose for CBCT is greater than that of conventional radiographic techniques2. Generally, the effective dose of panoramic radiographs falls within 2.7−38 μSv and 0.3−21.6 μSv for periapical radiographs3. This can vary widely for CBCT imaging with a range of 11 - 674 μSv for dentoalveolar CBCTs, with exposure settings even more pertinent since our cohort of patients are predominantly children and young adults. With this in mind, an audit into justification and referral criteria for CBCTs within a large secondary care orthodontic service at The Royal London Dental Hospital and Whipps Cross Hospital was performed.
Aims and Objectives
The primary aims were to measure compliance of orthodontic CBCT justification and referral criteria against nationally published guidelines and compare results against a previous local CBCT clinical audit completed in 2022-3. Furthermore, a concurrent service evaluation was performed to investigate CBCT use, looking at factors including patient demographics, number and type of plain films taken and wait times for CBCT.
Standards/guidelines/evidence base
Currently, there are no published guidelines which can be used as a gold standard for CBCT justification and referral criteria in orthodontics. Local standards were set, based upon European guidelines from SEDENTEXCT1, orthodontic radiograph guidelines from the British Orthodontic Society (BOS)2 and guidelines from the Royal College of Surgeons (RCS) in 20224. The aims were agreed upon following discussion and consensus decision within a departmental meeting with Senior Consultants. This led to creation of four clinical standards in relation to CBCT requests, as illustrated in Table 1.

Table 1: Agreed local standards and target compliance
For standard 4, there should be no CBCT canine cases where sufficient information had already been obtained through plain film imaging. This was developed specific to ectopic canines as it was derived from selection criteria published by RCS ‘Management of the palatally ectopic maxillary canine’ and BOS ‘Orthodontic Radiographs Guidelines’ (pg. 22)2, ⁴. Additionally, a previous local service evaluation in 2022 highlighted that the majority of CBCT requests were related to ectopic canines and so by developing this local standard it would be more representative of the department.
Sample and data source
The sample comprised of 256 child and adult orthodontic CBCT requests in total. In the second cycle, this included additional requests (n = 34) from Whipps Cross Hospital. CBCT cases were identified by the local clinical effectiveness unit from a radiographic logbook and relevant
electronic case notes were analysed for the following data sets: Patient age and gender; number and type of plain film imaging prior to CBCT requests (only imaging relating to the tooth/teeth in question on CBCT request were included); CBCT justification given by clinician and date from CBCT referral to exposure.
Exclusion criteria included any requests that were made by another specialty because the primary aim of this audit related to orthodontic CBCT requests. Further, any duplicates, specifically patients that had CBCT of maxilla and mandible (n=43) were counted as one request as it was not the number of requests being evaluated through this audit, but the justification given.
Audit type
A two cycle, multi-centre audit undertaken between July-December 2023 and July-December 2024. The first cycle single-centre and retrospective, the second cycle multi-centre and prospective).
Methodology
The project arose from a previous audit carried out between February 2022 – June 2023, which sampled 60 patients attending a joint canine MDT clinic and underwent subsequent CBCT. This formed the basis to expand further to include all cases referred for CBCT regardless of which clinic they attended. The project was registered with the local clinical effectiveness unit (ID: 13826 and reaudit 14369). Data was collected during two separate timepoints: Cycle 1 July-December 2023 and Cycle 2 July-December 2024.
Records were analysed according to the data sets as described above and collated into a Microsoft Excel spreadsheet. Specifically, electronic casenotes were reviewed to determine the justifications given by clinicians when requesting CBCT and compared against the agreed standards. Standards 1-3 were carried over from the previous audit, whilst standard four was added for this current two-cycle audit following review at a departmental meeting. Both cycles were presented locally, with overall recommendations discussed in January 2025. Figure 1 highlights the timeline of events.
Figure 1: Audit timeline
Findings
There was an almost equal proportion of male:female patients that underwent CBCT examinations between 2023-24, with a mean age of 16-years-old and age range from 11-58 years old. For standard 1, 2 and 3, the compliance rate was maintained at 100% between cycles. In over half of the cases referred for CBCT, it related to ectopic canines (n=78), which was then followed by impacted teeth (excluding canines – predominantly second molars and premolars) and supernumerary teeth (see figure 2). All cases had some form of plain imaging taken prior to CBCT, with the vast majority being DPT (n=92%) whereas peri-apical and upper standard occlusal radiographs were not taken as frequently (n=35).
CBCT Justification Canine
Supernumerary
Impacted tooth (other than canine)
Odontome
Surgical planning
Cystic changes
Pulp canal anatomy
Cleft planning
Resorption
For standard 4, The first cycle data revealed one canine case in which plain imaging confirmed severe resorption of adjacent teeth and correct localisation of the tooth, which would typically be sufficient for treatment planning purposes. However, a subsequent CBCT was requested with the same reasoning given as plain film imaging and there was no change in the clinicians’ treatment plan pre-or-post CBCT. This highlights how plain films were likely to be sufficient for orthodontic purposes for this specific case. Following the second cycle, there was improvement in compliance to 100% as all cases were referred for CBCT because there was insufficient information provided by plain imaging.
Observations
A total of 256 CBCT cases have been analysed as part of this two-cycle audit, which has demonstrated that ectopic canines remain the most common justification for CBCT requests within orthodontics, which has also been found in similar audit projects⁵. However, the concurrent service evaluation revealed variation between cases in terms of plain imaging taken prior to CBCT, as evidenced in a drop of 25% in the number of canine cases that have parallax done prior to CBCT, highlighting the need for national standards. Wider agreement in the orthodontic community on what is deemed insufficient information obtained from plain films would aid in planning. Although CBCT has been shown to be more accurate than conventional radiographs in localisation of ectopic canines⁶, clinicians should avoid requesting CBCT for every case due radiographic exposure risk. It is also important to note that standards cannot be entirely prescriptive and there should be a balance with clinical findings informing decision-making.
Comparing first and second cycle data, there has been a drop of roughly 40% in the number of canine cases that have parallax done (vertical or horizontal) prior to CBCT and mean wait times for CBCT from request increased from 35 to 59 days. Further exploration would be required to definitively determine reasoning for both of these points and if this trend continues with a subsequent audit cycle planned in 12 months’ time.
Recommendations
1. To re-audit in 12-months to assess if compliance continues with sufficient justification prior to CBCT requests. Local standards should be based on BOS, SEDENTEXCT and RCS Guidelines in terms of CBCT requests1,2, ⁴.
2. To disseminate specific guidance to the orthodontic team from the RCS on management of ectopic canines, which highlight the need for CBCT if plain film imaging is not sufficient for treatment planning purposes. Whether clinicians opt to carry out CBCT should take these guidelines into consideration in order to avoid unnecessary radiographic exposures.
3. Future local CBCT audits should always ensure a sufficient sample size, as opposed to the previous audit carried out in 2022-2023, considering over 300 orthodontic requests for CBCT are typically carried out per year.
4. These recommendations will be shared with staff during clinical governance meetings and through email. The audit will be repeated in 18 months using the updated data collection form.
Project involvement
Balraj Gill (Project lead, project design, data collection and analysi)
Francine Jones (Project design, project supervision, manuscript revision)
Christine Casey (Project design, project supervision, manuscript revision)
Acknowledgements
Mr Edward Spirling and Mr Nicholas Ogunlaga, Clinical Effectiveness Unit, Barts Health NHS Trust, for compiling relevant CBCT requests from electronic casenotes.
References
1. SEDENTEXCT. Radiation protection 172. Cone beam CT for dental and maxillofacial radiology: Evidence based guidelines. Luxembourg: European Commission; 2012.
2. Isaacson K, Thom A, et al. Guidelines for the use of radiographs in clinical orthodontics. 4th ed. British Orthodontic Society; 2015.
3. Horner K, Eaton KA. Selection Criteria for Dental Radiography 3rd edn. Faculty of General Dental Practice (UK), 2013.
4. Hussain J, Burden D, McSherry P, Hania M.
Management of the palatally ectopic maxillary canine. The Royal College of Surgeons of England, Faculty of Dental Surgery Clinical Guidelines, 2022.
5. Lin Y, Hamilton S. Cone Beam Computed Tomography (CBCT): Are we scanning appropriately? A service evaluation. Clinical Effectiveness Bulletin, British Orthodontic Society, May 2023.
6. Serrant, P.S, McIntyre, G.T., & Thomson, D. J.
Localization of ectopic maxillary canines – is CBCT more accurate than conventional horizontal or vertical parallax? Journal of Orthodontics. (2014). 41(1):13-18
A two-cycle audit to assess orthodontic treatment outcomes at Liverpool University Dental Hospital
Yen Ming Lin (ST), Sarah Turner (Consultant Orthodontist) and Jayne Harrison (Consultant Orthodontist)
Liverpool University Dental Hospital, Liverpool, UK
Background/Rationale The Orthodontic Commissioning Guide (2015) offers direction to specialist dental services to promote consistent, high-quality care1. All primary care orthodontic providers in England and Wales are contractually obliged to submit PAR score changes as one of five key performance indicators of annual activity. All cases must be scored if the contractor completes <20 cases/year however, if completing >20 cases/year, then 20 cases plus 10% of the remaining cases, need to be scored. The PAR index is a form of outcome measure, although overall outcome measures should also include PROMs and PREMs.
To provide good care for patients and to ensure efficient use of NHS resources, we aim to provide treatment in a timely manner in line with locally recommended treatment times2. This is important for patient compliance and informed consent, as patients should be aware of realistic timescales involved before commencing treatment, as some may find it difficult to commit to the duration of orthodontic treatment 3 .
Assessment of treatment outcomes at Liverpool University Dental Hospital (LUDH) has not been undertaken since 1993, so this audit was long overdue.
Aims and Objectives
Primary Aim: To determine whether orthodontic PAR score outcomes at LUDH fell within NHS Commissioning guidelines.
Secondary Aims: To assess compliance with locally set standards that for 80% of patients: treatment was carried out within ≤30 months, patients were treated by ≤2 clinicians for continuity of care and PAR scores were recorded at debond.
Standards/guidelines/evidence base
Standard 1 and 2: As outlined by NHS England (2015) in ‘Guides for Commissioning Dental Specialities – Orthodontics’1: ≥75% of completed cases should exhibit a reduction in PAR score of ≥70% and ≤3% of completed cases should have a PAR score reduction of <30%.
Standard 3: The NHS advises that orthodontic treatment usually lasts from 12 months to 2 and a half years so we set the standard that ≥80% of patients should have a treatment time of ≤30 months.
Standard 4: There is evidence to suggest that transfer of care to other clinicians increases treatment time⁴ so we set a standard that ≥80% of patients should be treated by ≤2 clinicians
Standard 5: To ensure that we have a representative sum of cases, we set a standard that ≥80% of pre- and post-treatment PAR scores should be recorded at debond.
Sample and data source
A retrospective convenience sample of 50 patients who attended for orthodontic debonding of their fixed appliance, starting from 30th September 2023 for cycle 1 and 31st January 2025 for cycle 2 was identified. Cases were identified using the departmental debond diary. Clinical case notes and letters from Medical Records were retrieved and reviewed.
One of the two dental technicians, trained and calibrated in PAR scoring study models, should have scored plaster study models, taken at initial record collection and at debond and recorded the PAR scores in the Laboratory database as per the department protocol.
Exclusion criteria were patients with cleft and/or craniofacial deformities, moderate or severe hypodontia, receiving orthognathic treatment, treatment with limited objectives, removable appliance treatment only or who discontinued treatment.
Any cases with missing pre- or post-treatment study models or incomplete medical records were recorded and excluded. Only patients treated by orthodontic therapists, ST1-ST5 trainees and postgraduate students at any point throughout their course of treatment, were included. Patients treated by consultants were excluded as their caseload was comprised of predominantly patients with moderate/severe hypodontia and/or receiving orthognathic treatment.
Audit type
Local retrospective cross-sectional audit.
Methodology
Data were collected retrospectively for 50 patients per audit cycle between March and September 2023 for cycle 1 and September 2024 and January 2025 for cycle 2. Information was extracted from patient notes including dates of bond-up and debond to determine treatment duration and the number of clinicians who had treated the patient over their course of orthodontic treatment.
Study models (SMs) were expected to have been scored in both cycles. This had not occurred prior to cycle 1, so the SMs were retrieved and scored by one of two dental technicians. To facilitate SM scoring, time was identified for the technicians for PAR scoring to be completed, and a new lab card was designed and implemented prior to cycle 2.
Findings
PAR Score
Standard 1: >75% have PAR reduction of >70% (Figure 1)
Cycle 1: 86% of cases had a PAR score reduction ≥70% whereas the remaining 14% had a PAR score reduction between 30–69%.
Cycle 2: 78% of cases had a PAR score reduction of ≥70%, 16% of cases had a PAR score reduction between 30-69%.
The standard was met in both cycles.
Standard 2: ≤3% have PAR reduction <30% (Figure 1)
Cycle 1: No cases had a PAR reduction of <30%. Standard met.
Cycle 2: 6% of cases had a PAR score reduction of <30%. Standard not met.
Standard 3: ≥80% have treatment time of ≤30 months (Figure 2)
Figure 2: Comparison of LUDH treatment duration in cycle 1 (2024) versus cycle 2 (2025)
Cycle 1: 56% of cases had a treatment time of ≤30 months.
Cycle 2: 60% of cases had a treatment time of ≤30 months.
Mean treatment time was 33 months (95%CI=29-37 months) in cycle 1 compared to 30 months (95%CI=26-35) in cycle 2. The standard was not met in both cycles.
Standard 4: Continuity of Care – ≥80% treated by ≤2 clinicians (Figure 3)
Figure 3: Comparison of LUDH number of clinicians in cycle 1 (2024) versus cycle 2 (2025)
Cycle 1: 84% of cases were treated by ≤2 clinicians.
Cycle 2: 90% of cases were treated by ≤2 clinicians.
The mode number of clinicians per patient was 1 in both cycles. The standard was met in both cycles.
Standard 5: ≥80% of PAR scores done
Cycle 1: None of the cases had PAR scores completed by technicians, at the start of data collection. Standard not met.
Cycle 2: 98% of cases had been PAR scored at the start of data collection. Standard met.
Observations
This audit demonstrated that PAR score changes complied with the agreed standards in cycle 1 but not cycle 2 with 6% of patients having <30% reduction in PAR score. Despite this, they still objectively show that the standard of treatment was high.
The same technician did not PAR score all cases, however both technicians were trained and calibrated, therefore scores should be reliable⁵. However, the audit could have been improved by assessing the inter-rater reliability. All treatment was planned and supervised by a Consultant Orthodontist and the overall results suggests this system works well⁶. This enables trainees to treat complex cases with an IOTN of 4 and 5, under supervision of a Consultant Orthodontist, to obtain good treatment outcomes⁷.
Patients with moderate or severe hypodontia were not included in the audit as changes in tooth position and occlusion when opening or closing space are reflected poorly by PAR, despite the increased complexity and greater technical skill required⁸. Orthognathic cases were not included as PAR only assesses dental occlusion and has no quantitative measure for skeletal changes⁹. PAR should not be used in isolation to determine treatment complexity and the Index of Complexity Outcome and Need (ICON) has been developed for this purpose. Treatment results should be viewed together with other performance indicators such as qualitative patient satisfaction questionnaires⁶,10
Unmet Standards
Treatment time for 44% and 40% of cases was >30 months in Cycles 1 and 2 respectively. The wide variation in treatment times is potentially due to a combination of biological variation, treatment complexity, patient compliance, operator type and skill 2. As this audit was undertaken in a teachinghospital, increased treatment time may be attributed to levels of operator experience as most patientwere treated by clinicians in training. Change of operators has also been linked to increased treatment duration⁴ therefore, the number of operators should be limited to reduce the likelihood of extended treatment duration. In this audit most patients were treated by 1 clinician.
It was disappointing that none of the cases had PAR scores completed prior to cycle 1. This was fed back to the Laboratory team who acknowledged that PAR scoring models at debond had not become embedded into their routine. In addition, key information regarding e.g. impactions, missing or extracted teeth was rarely supplied by clinicians on the lab card at debond. Following implementation of the new lab debond card, 98% of cases were PAR scored prior to cycle 2.
This audit was performed retrospectively which may have limitations due to its reliance on cases having been entered correctly in the departmental debond diary. Two technicians carried out the PAR scoring and this could have potentially affected the inter-rater reliability of the scores
Recommendations
1. Continue using the new debond laboratory card (available at https://archive.bos.org.uk/ Portals/0/Public/docs/Research%20and%20 Audit/PARSCORINGSHEET.pdf) to facilitate recording of PAR scores by technicians as this improved PAR scoring significantly by cycle 2.
2. Provide opportunities for training and recalibration of laboratory technicians to provide consistently accurate PAR scores.
3. Implement locally agreed departmental policy regarding transfer cases to ensure that each course of treatment is provided by a maximum of 2 clinicians, unless unavoidable, to improve continuity of care and reduce treatment times.
4. Re-audit in 12 months to reassess the impact of the transfer of care policy.
5. Extend audit regionally to allow comparison of outcomes and share good practice between units.
Acknowledgements
The authors would like to thank the dental technicians for all their help in PAR scoring the study models.
Project involvement
Yen Ming Lin (Project lead, project design, data collection and analysis, manuscript drafting and submission)
Sarah Turner (Project supervision, project design, manuscript editing and approval)
Jayne Harrison (Project supervision, project design, manuscript editing and approval)
References
1. NHS England and NHS Improvement. Guide for Commissioning Orthodontics. 2015.
2. Soneji B, Kane G. An audit to evaluate orthodontic treatment times in secondary care across the East Midlands region. Clinical Effectiveness Bulletin. 2019;43:15-7.
3. Wilson V, Fox N. An audit to assess orthodontic treatment duration and DNA rates in specialist practice. Clinical Effectiveness Bulletin. 2017;39:1-3.
4. McGuinness NJ, McDonald JP. The influence of operator changes on orthodontic treatment times and results in a postgraduate teaching environment. European journal of orthodontics. 1998;20(2):159-67.
5. Farmahan S, Campbell C. Outcome of orthognathic cases using PAR: A retrospective regional audit. Clinical Effectiveness Bulletin. 2017;39:20-1.
6. Crawford E, Fahey T, Brown A. Audit on quality of treatment outcomes using the PAR index at the Royal Gwent Hospital. Clinical Effectiveness Bulletin. 2015;35:36-7.
7. Hand D, Khalaf K, Mattick C. Assessment of orthodontic treatment outcome using PAR score for patients treated at an orthodontic teaching hospital. Clinical Effectiveness Bulletin. 2010;24:12-4.
8. Patel Y, Mangnall L, Juggins K. Three sides to every story, even in orthodontics: PROM, PAR and IOTN. Clinical Effectiveness Bulletin. 2021;46:13-6.
9. Hitchens G, Prado N, Miller C, Caldwell S, Doumpiotis D. Patient reported satisfaction and Peer Assessment Rating (PAR) outcome of combined Orthodontic/Orthognathic treatment; a multi-centre audit. Clinical Effectiveness Bulletin. 2019;43:42-4.
10. Khan Z, Barry G. A PAR score audit to assess treatment outcome of combined orthognathic treatment at Arrowe Park Hospital. Clinical Effectiveness Bulletin. 2017;39:33-4.
Patient experience of digital scans in the orthodontic department at King’s Dental Institute: A service evaluation
Bronagh McGuckin (ST), John Watt (ST) and Mariam Shahid Noorani (Consultant Orthodontist) King’s Dental Institute, London, UK
Background/Rationale
Digital intraoral scanning has become increasingly prevalent in orthodontics, offering an alternative to conventional impression techniques. These scanners capture three-dimensional images of the dentition and oral tissues, potentially improving patient comfort, efficiency, and accuracy1. While studies have demonstrated the clinical validity of digital scans, less research has focused on patients' subjective experiences of the scanning process. Patient perception and acceptance are crucial factors in successfully implementing new healthcare technologies. Previous studies in restorative dentistry suggest that patients generally prefer digital scans to conventional impressions2. However, the orthodontic context presents unique considerations, including a predominantly adolescent patient population.
As digital scanning becomes more widely adopted in orthodontic practice, evaluating patients' experiences is essential to ensure this technology enhances rather than detracts from the quality of care. Patient-Reported Experience Measures (PREMs) have become increasingly important in healthcare quality assessment, particularly within the NHS3. These questionnaires capture patients' perceptions of their healthcare experiences, providing valuable insights that complement clinical outcomes and other quality indicators. This service evaluation at King's Dental Institute sought to assess patient perceptions of digital intraoral scanning in an orthodontic setting, providing valuable insights to inform clinical practice and future research directions.
Aims and Objectives
This project aims to evaluate the service provided by the Orthodontic Department in implementing digital scanning technologies, with a specific focus on patient experience. We aim to explore these aspects by analysing patient feedback which will be gained through a devised questionnaire.
Our objectives are to evaluate patient satisfaction, comfort, and acceptability of digital scanning technology in comparison to traditional methods, to assess the effectiveness of communication and patient understanding of the digital scanning process, and to analyse patient feedback in order to identify areas for service improvement and staff training in digital scanning procedures.
Standards/guidelines/evidence base
While formal standards are not typically established for service evaluations, we can draw upon findings from a recent systematic review to provide context for our results which concludes that studies consistently show that "patient perception and comfort are better with intraoral scanners" compared to conventional methods⁴. This qualitative evidence serves as a contextual
framework rather than definitive standards, allowing us to maintain the exploratory nature of our service evaluation while still having a basis for interpreting our findings.
Sample and data source
Data were collected prospectively from patients undergoing digital intraoral scanning in the Orthodontic Department at King's Dental Institute. Each cycle comprised 50 consecutive patients, with the first cycle running from February 2024 and the second from January 2025, each concluding once 50 questionnaires were completed. All patients, aged 11 and above, attending new patient, multidisciplinary, or records clinics for digital scans during these periods were eligible unless they were unable to complete the questionnaire independently or could not understand English. Questionnaires were administered immediately after the procedure to minimise recall bias and ensure accurate feedback.
Audit type
This is a service evaluation with two cycles, collecting prospective data.
Methodology
A patient questionnaire was piloted, refined for clarity, and approved by the PPI team at King’s College Hospital NHS Foundation Trust. Clinicians distributed the final questionnaire to patients immediately after their digital scan, and completed forms were collected and securely stored by the nursing team to maintain confidentiality. Data were collated weekly in Microsoft Excel. To ensure accuracy, a second clinician randomly checked 10 entries against the original questionnaires for validation.
Several changes were implemented following the first cycle including: continued staff training for both dentists and nursing staff of utilising the digital scanning equipment and software, phasing out the use of alginate impressions in the Department and increased utilisation of digital scanning technology and a dedicated bay for scanning to improve efficiency. Additionally, a patient information page was made available for patients to read before the digital scan.
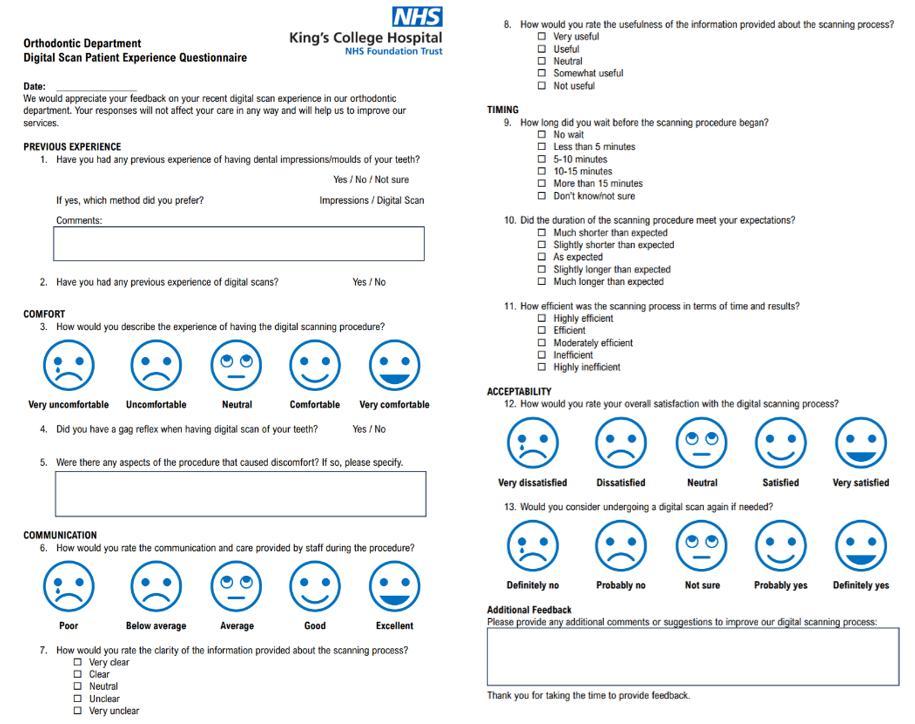
Findings
Patient experiences with digital scanning were measured across two cycles with 50 patients in each. In Cycle 1, 68% of participants had no prior experience with dental impressions, while 24% reported previous alginate impressions and 10% had undergone digital scans. Among those with alginate experience, 92% preferred digital scanning, rising to 100% in Cycle 2 after workflow optimisations. The transition to digital methods proved particularly impactful for patients with prior alginate exposure, aligning with findings that digital impressions reduce discomfort compared to conventional methods.
Comfort ratings improved significantly between cycles (shown in Figure 2): 70% initially rated scans as "comfortable" or "very comfortable," increasing to 86% in Cycle 2. Reports of gag reflex decreased from 8% to 4%. Discomfort sources in Cycle 1 included scanner pressure (42% of discomfort reports) and jaw positioning requirements (33%), which were mitigated in Cycle 2 through improved operator training and patient preparation protocols.
to patients. Waiting times showed marked progress, with 66% reporting no wait in Cycle 2 versus 56% initially. The proportion perceiving scans as longer than expected halved from 8% to 4%, reflecting both technical refinements and better patient education about procedure duration.
Patient feedback highlighted strong preferences for digital scanning's cleanliness (78% positive comments) and real-time visualisation capabilities (65% of respondents). While 12% of Cycle 1 participants requested "more technical explanations" of the scanning process, this concern decreased to 6% in Cycle 2 after introducing pre-procedure informational materials. A selection of representative patient feedback comments, illustrating both positive experiences and suggestions for further improvement, is presented in Figure 3. The overall satisfaction with the digital scanning process remained high throughout both cycles, and nearly all patients indicated they would be willing to undergo a digital scan again if needed.
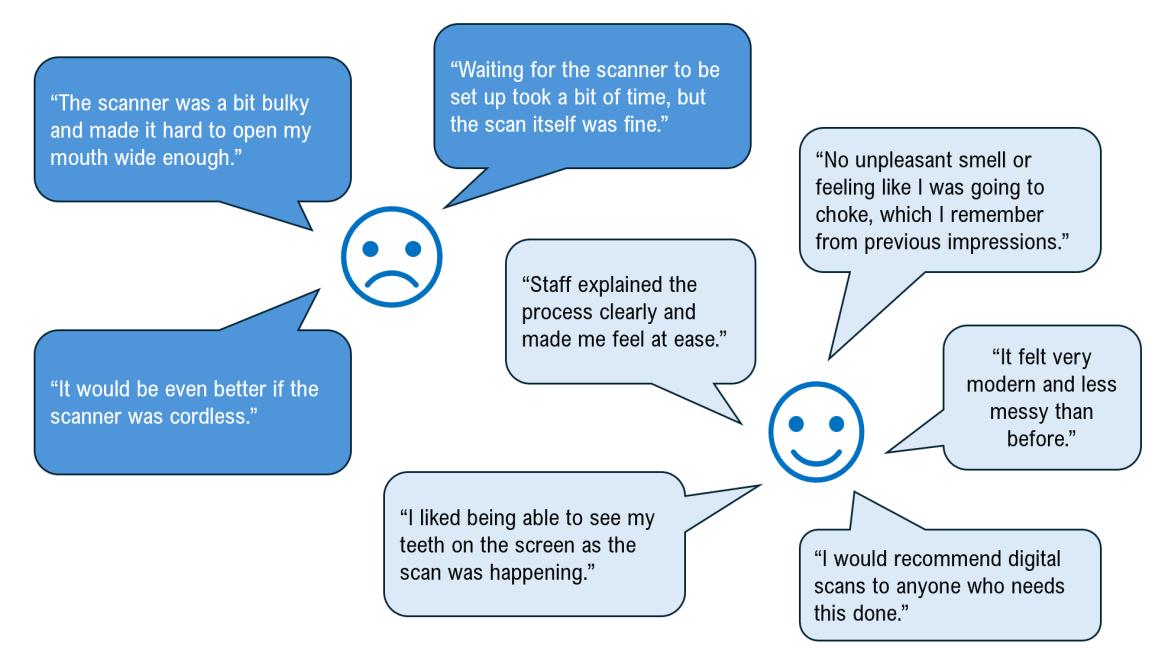
Observations
Communication quality improved from 86% rating it "excellent" in Cycle 1 to 94% in Cycle 2 following enhanced staff training. Specifically, the percentage of patients finding the information 'clear' or 'very clear' rose from 72% to 96% between the cycles, while ratings for the usefulness of information increased from 88% to 100%, demonstrating that staff training and the patient information leaflet have improved the quality of information provided
The observations from this service evaluation reinforce and expand upon a growing body of evidence supporting the use of digital intraoral scanning in orthodontic settings. Across both cycles, patients consistently expressed a strong preference for digital scanning over alginate impressions, a finding echoed in the literature. Mangano (2018) demonstrated that digital impressions are significantly more accepted and comfortable for orthodontic patients than conventional techniques, with participants in their study universally preferring the digital method⁵.
This aligns with our own results, where nearly all patients with prior experience of both methods indicated a clear preference for digital scanning.
Patient comfort emerged as a central theme, with most rating the digital scanning experience as comfortable or very comfortable, and this proportion increased following service improvements between cycles. A recent network meta-analysis supports these findings, concluding that intraoral scanners are associated with significantly greater patient comfort than conventional impressions, largely due to the elimination of impression trays and materials that can provoke gag reflex or discomfort2. Our data reflected this, with a low and decreasing incidence of gag reflex reported by patients, consistent with the controlled breathing, absence of unpleasant taste or smell, and reduced anxiety documented in the literature⁶.
Efficiency and workflow improvements were also evident. Although some studies have noted that digital scanning can take longer than traditional impressions, patient perception in our evaluation was that the process was efficient and, with improved staff training and workflow adjustments, fewer patients reported the procedure taking longer than expected in the second cycle⁶. This suggests the learning curve and initial technical barriers associated with digital scanning can be effectively mitigated through targeted staff development, as the literature indicates that operator familiarity and confidence with scanning technology are key to maximising its benefits⁶.
Communication and patient engagement were highlighted as areas of strength following intervention. Patients appreciated the clarity and usefulness of the information provided, with satisfaction ratings for communication increasing notably after the introduction of enhanced patient information materials. This is supported by research showing that the visual and interactive nature of digital scanning enables clinicians to better educate and involve patients in their care, fostering improved understanding and satisfaction⁵.
Patients with no prior experience of dental impressions adapted quickly and positively to digital scanning, suggesting that the advantages of this technology are not limited to those with negative prior experiences of traditional methods. The findings from this evaluation, in conjunction with recent systematic reviews and clinical trials, strongly support the continued integration of digital scanning technology in orthodontic practice, provided that ongoing staff training and patient communication remain priorities. Ultimately, digital scanning offers a more comfortable, engaging, and patient-centred approach to orthodontic care, consistent with the direction of contemporary dental practice.
Recommendations
The following recommendations were implemented following the results of the second evaluation:
1. Continued staff training for both dentists and nursing staff of utilising the digital scanning equipment and software
2. Inclusion of digital scanning training to all new staff member induction programmes
3. Establishing a relationship with an external lab who could manage digital workflow
4. An additional IT personnel member was trained to support intra-oral scanner updates
We aim to assess the effectiveness of these recommendations by carrying out a third cycle of this service evaluation in 2026.
Acknowledgements
We would like to express our sincere gratitude to all members of staff in the Orthodontic Department at King's Dental Institute for their invaluable support in facilitating this service evaluation.
Project
involvement
Bronagh McGuckin
John Watt
Mariam Shahid Noorani
1. Zarbakhsh A, Jalalian E, Samiei N, Mahgoli MH, Kaseb Ghane H. Accuracy of Digital Impression Taking Using Intraoral Scanner versus the Conventional Technique. Front Dent. 2021;18(6).
2. Sivaramakrishnan G, Alsobaiei M, Sridharan K. Patient preference and operating time for digital versus conventional impressions: a network meta‐analysis. Aust Dent J. 2019;64(4):354-363.
3. Kingsley C, Patel S. Patient-reported outcome measures and patient-reported experience measures. BJA Educ. 2017;17(4):137-144.
4. Serrano-Velasco A, Martín-Vacas A, Paz-Cortés M, Giovannini G, Cintora-López M, Aragoneses J. Intraoral scanners in children: evaluation of the patient perception, reliability and reproducibility, and chairside time-A systematic review. Front Pediatr. 2023;11:1213072.
5. Mangano A, Beretta M, Luongo G, Mangano C, Mangano F. Conventional Vs Digital Impressions: Acceptability, Treatment Comfort and Stress Among Young Orthodontic Patients. Open Dent J. 2018;12:118-124.
6. Gruenheid T, McCarthy S, Larson B. Clinical use of a direct chairside oral scanner: An assessment of accuracy, time, and patient acceptance. Am J Orthod Dentofacial Orthop. 2014;146:673-682.
Managing the gap: a local service evaluation of the multidisciplinary management of hypodontia
Siew Leng Tan (ST), Modhi Aldihani (ST), Rosalind Jennings (Post CCST)
Howard Moseley (Consultant Orthodontist) Fiona Ryan (Consultant Orthodontist)
Orthodontic Department, Eastman Dental Hospital, University College London Hospitals NHS Trust, London, UK
Background/Rationale Hypodontia, defined as the developmental absence of one or more teeth, affects approximately 4.6% to 6.3% of the European Caucasian population, with a higher prevalence observed in females1. It can lead to significant aesthetic, functional, and psychosocial concerns. Management often requires a multidisciplinary approach, typically involving orthodontic space preparation followed by restorative replacement of missing teeth. However, a frequent challenge is the delay between completion of orthodontic treatment and initiation of restorative care. Reasons for this delay include biological factors such as periodontal reorganisation, as well as systemic or administrative issues2,3. During this waiting period, patients may experience retainer failure, relapse, or be lost to follow-up3. Relapse may compromise the restorative space(s), ultimately affecting clinical outcomes and patient satisfaction⁴. To address these concerns, previous research has called for improved, streamlined pathways that better coordinate orthodontic and restorative care⁵. This service evaluation, framed within a Quality Improvement Project (QIP), represents a Plan–Do–Study–Act (PDSA) model aimed at improving the orthodontic–restorative transition for hypodontia patients in a tertiary care setting.
Aims and Objectives
The aim of this multidisciplinary service evaluation was to assess the orthodontic/restorative pathway and determine the time taken for hypodontia patients to receive restorative treatment following orthodontic debond in a tertiary care setting. The objectives were to identify areas for improvement in the orthodontic/restorative care pathway, to inform future patients of likely waiting times, and to support improved communication between clinicians, patients, and general dental practitioners (GDPs), facilitating smoother transitions to the restorative phase.
Standards/guidelines/evidence base
There is currently no published standard for waiting times between debond and restorative treatment completion in hypodontia cases. Literature suggests that periodontal fibres take at least 232 days to reorganise following orthodontic movement, making one year a reasonable benchmark before initiating definitive restorations2. Other sources recommend beginning restorative care approximately six to nine months post-debond 3. In consultation with clinical leads from the hypodontia team and based on existing literature, two standards were defined. For patients receiving resin bonded bridges, 100% should complete treatment within 12 months of orthodontic debond. For patients receiving implant-supported restorations, 100% should
complete treatment within 12 months of debond or within 12 months after turning 18 years old, if debond occurred prior to that age. For this service evaluation, treatment completion was defined as placement of the definitive restoration
Sample and data source
Eligible patients were identified by screening laboratory records of those who had retainers with pontics issued between August 2021 and January 2023. Two researchers independently reviewed electronic clinical records to identify patients meeting the inclusion criteria: hypodontia patients who had completed both orthodontic and restorative treatment at the Eastman Dental Hospital. Exclusion criteria comprised patients whose restorative care was carried out externally, those with tooth loss not due to hypodontia, e.g. trauma, and patients whose missing teeth were managed through orthodontic space closure rather than prosthetic replacement. Of the 289 patient records reviewed, 80 were identified as being on the orthodontic–restorative pathway. Only 21 met the inclusion criteria (Figure 1), as 18 patients were awaiting restorative assessment and 41 patients were still undergoing restorative treatment. Depending on the patient’s age at debond, restorative care was provided by either the Adult Prosthodontics orPaediatric Dentistry departments.

Audit type
This was a retrospective, multidisciplinary service evaluation conducted as part of a Quality Improvement Project, using the a PDSA framework.
Methodology
A data collection spreadsheet (MS Excel) was used to record and analyse retrospective data extracted from the hospital’s EPIC electronic records system. Key data points included patient age, number and type of missing teeth, date of orthodontic appliance removal, restorative treatment provider, dates of restorative assessment and completion, type of restorative treatment provided, and number of missed restorative appointments.
Findings
Among the 21 patients included, 17 received treatment in the Restorative Dentistry Department and four in Paediatric Dentistry. The mean age at
debond was 19.6 years, with a range of 13 to 36. The number of missing teeth (excluding missing third molars) ranged from one to 21 (Figure 2), with a median of two. The most commonly missing teeth were the upper lateral incisors. Nearly half the patients (47%) had one to two missing teeth. The Index of Orthodontic Treatment Need (IOTN) classification was 4h in 43% and 5h in 57% of patients. The number of prosthetic units ranged from one to eleven per patient, with an average of three. Most patients received resin bonded bridges, while four were provided with implant-supported restorations. The average time from debond to restorative assessment was 7.2 months for patients receiving bridges and 10.5 months for those receiving implants (Table 1). The average time to final restoration was 16.6 months for bridges and 43.3 months for implants.
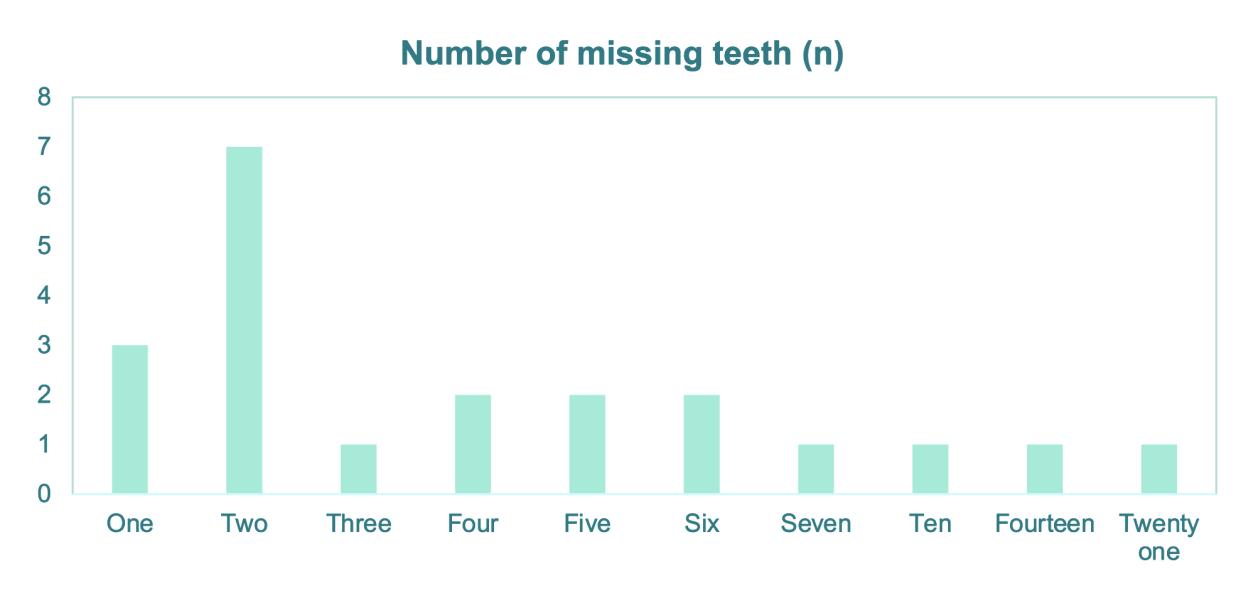
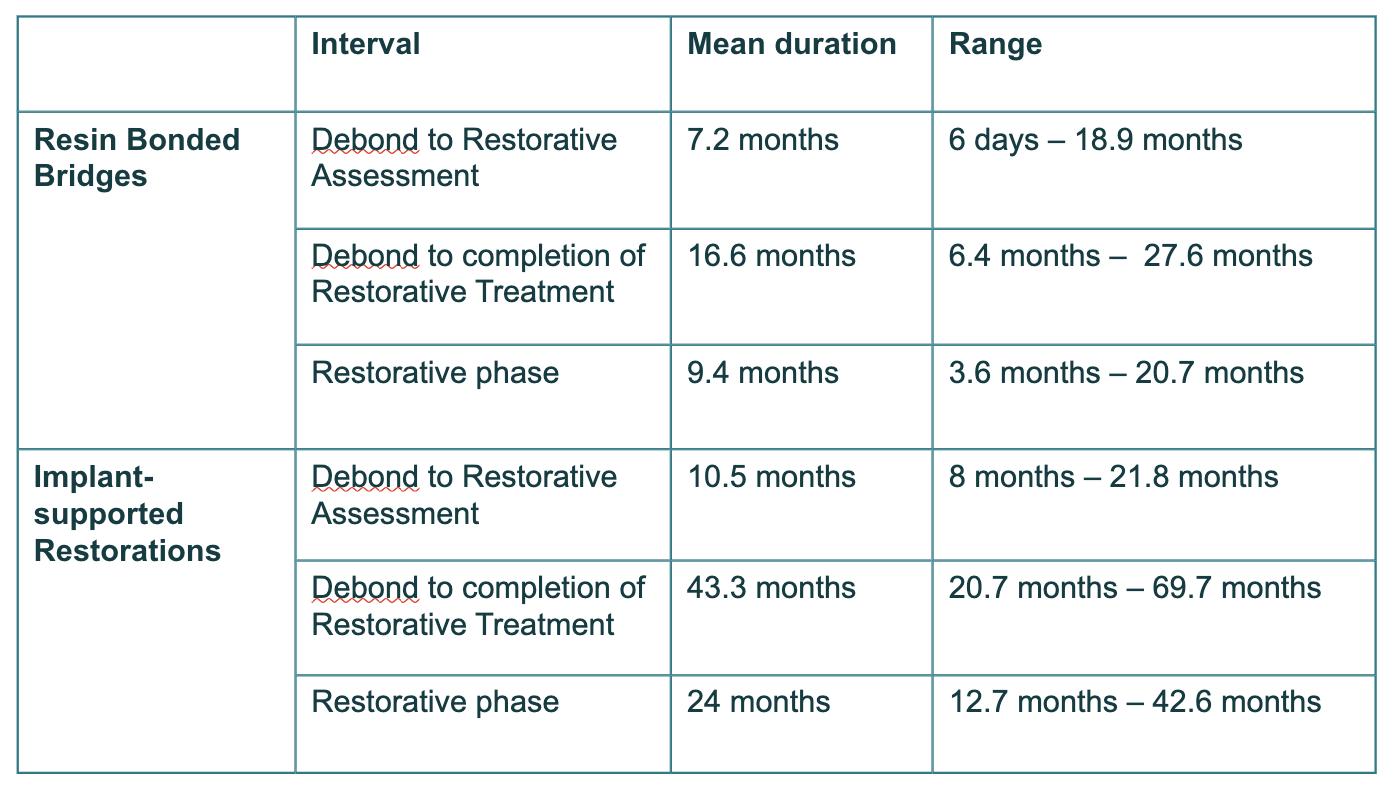
Table 1: Average time interval between stages of treatment
The gold standards were not met. Only 35% of patients receiving bridges completed treatment within 12 months of debond. None of the implant patients met the standard of completion within 12 months of debond or within 12 months of turning 18. The shortest time between debond and restorative assessment was six days in a case where referral was made at pre-debond stage. The longest time was 21.8 months in a patient who was lost to follow-up. The shortest time to treatment completion was 6.4 months for a single-unit bridge. The longest was 5.8 years, in a case where the patient was debonded at 18 and completed implant-supported restoration at age 24. Approximately one third of patients failed to attend at least one restorative appointment, contributing to delays. In some instances, restorations had to be remade as restorative spaces had changed due to tooth movement. Other sources of delay included missed or unsatisfactory lab work, pontic shade issues, or restorative treatment was put on hold during the changeover of clinicians.
Observations
This service evaluation highlighted both patient-related and systemic contributors to delayed restorative care. Patient non-attendance, poor oral hygiene, and failure to wear retainers were some of the issues identified. Short-term tooth movement due to retainer failure often necessitated additional orthodontic intervention or remaking of prostheses. Systemic issues observed were patients not being referred by the clinicians for restorative treatment after debond and administrative errors such as failure to book follow-up appointments. In some cases, delays were exacerbated by laboratory-related issues or changes in treating clinicians over extended treatment periods. The finding that 47% of patients had only one or two missing teeth raised questions about whether these cases could have been managed in primary care. While this study focused on patients treated in a tertiary setting, the potential for managing simpler cases outside of hospital should be further explored.
A multidisciplinary team approach is required to facilitate an efficient transition to the restorative phase after completion of orthodontic treatment and minimise complications. The results of this service evaluation were presented to the Restorative and Paediatric Dentistry Department
leads involved in the management of hypodontia patients to identify areas of good practice and recommendations to improve waiting times. Clinicians should aim to confirm the intended restorative provider early and document this during the consent process. Patients should be informed about expected waiting times and the importance of retention compliance. Optimal retainer design should be planned to protect restorative space during the waiting period.
This evaluation represents the "Study" phase in a Quality Improvement Project. As part of the "Act" phase, several interventions have been introduced. These include referring patients for restorative treatment at the pre-debond appointment and exploring the role of a treatment coordinator to track patients between departments and ensure continuity of care. These changes aim to reduce waiting times, prevent loss to follow-up, and improve patient outcomes. A second cycle of data collection is planned no sooner than 18 months after implementation, allowing time for sufficient numbers of patients to complete both orthodontic treatment and restorative treatment within a tertiary care setting. Future work should assess the outcomes of patients whose restorative treatment is provided in primary care following hospital-based orthodontics. This will help clarify the most appropriate care setting for various presentations of hypodontia and provide further insights into access and quality of care across primary and secondary care.
Recommendations
1. IOTN 4h, especially those with single units and simple restorative work to be treated in primary care, where appropriate.
2. Clinicians to confirm restorative treatment provider at consent stage to manage patients’ expectations, where possible.
3. Add patients to restorative waiting list at the pre-debond review.
4. 4. Reinforce patient's compliance in wearing retainers as relapse could adversely affect restorative space.
5. Treatment or administrative coordinator to follow up hypodontia patients between stages of treatment to prevent patients from being lost to follow up.
Project involvement
Siew Leng Tan (Project lead, project design, data collection, data analysis, presentation and preparation of manuscript)
Modhi Aldihani (Project design, data collection)
Rosalind Jennings (Project design)
Howard Moseley (Project design)
Fiona Ryan (Preparation and approval of manuscript)
References
1. Polder BJ, Van’t Hof MA, Van der Linden FP, Kuijpers‐Jagtman AM. A meta‐analysis of the prevalence of dental agenesis of permanent teeth. Community Dent Oral Epidemiol. 2004;32(3):217–26.
2. Reitan K. Clinical and histologic observations on tooth movement during and after orthodontic treatment. Am J Orthod. 1967;53:721–45.
3. Stevenson B, Patel D, Ricketts D, Cord A. The orthodontic-restorative interface in patients with hypodontia: the patient's journey. Dent Update. 2013;40(5):354–60.
4. Pace-Balzan A, Chatzipantelis A, Dunn KJ, Charan G, Ashley MP. Restorative dentistry clinical decision-making for hypodontia: complex cases. Br Dent J. 2023;235(7):489–95. doi:10.1038/s41415-023-6324-5
5. Meaney S, Anweigi L, Ziada H, Allen F. The impact of hypodontia: a qualitative study on the experiences of patients. Eur J Orthod. 2012;34(5):547–52. doi:10.1093/ejo/cjr061
Ectopic maxillary canine referrals: A two-cycle audit
Annabelle Carter (ST) and Rachel O’Brien (Consultant)
Kingston and Richmond NHS Foundation Trust, Kingston upon Thames, UK
Background/Rationale Ectopic Maxillary canines affect approximately 2% of the population1. Early diagnosis and appropriate management is important to reduce complications, such as root resorption and ankylosis, optimise treatment success and reduce delays in care. The Dental Getting It Right First Time (GIRFT) Report published in 2021 discussed the importance of reviewing waiting times for oral surgery procedures such as canine exposures, after orthodontic treatment has begun2 If the wait time for surgery is longer than three months, a plan should be put in place to reduce the waiting times.
Aims and Objectives
The aims of the audit were as follows:
1. Evaluate the referral process and management protocols for impacted maxillary canines at Kingston Hospital.
2. Assess the average age of patients being referred for impacted maxillary canines.
3. Assess time lapses and waiting times between referral, new patient consultant assessment, and surgery.
Standards/guidelines/evidence base
Standard 1: All patients (100%) with suspected impacted canines should be referred to Kingston Hospital by 12 years of age.
Standard 2: Surgery should be conducted within 18 weeks following commencement of orthodontic treatment, as per GIRFT recommendations.
Standard 1 was a standard set in keeping with previous audits completed within the region, and on the Royal College of Surgeons Guidelines1,3, ⁴. Standard 2 was based on the 2021 GIRFT report, advising waiting times for surgical procedures should be no longer than 18 weeks once orthodontic treatment has commenced, which is classified as when fixed or removable appliances have been placed 2 .
Sample and data source
Data was collected from the electronic patient records (CRS) for 50 new patients who had attended a new patient appointment in the orthodontic department at Kingston Hospital for impacted maxillary canines that required surgical
intervention, between February 2023– June 2023 (first cycle). The inclusion criteria were any new orthodontic patient referred with maxillary impacted/ectopic canines requiring surgical exposure or removal from February 2023 until 50 patients were identified. Exclusion criteria were impacted mandibular canines and patients not accepted for treatment or refused active treatment
Audit type
A two-cycle retrospective audit was carried out.
Methodology
Approval was granted from the Clinical Audit and Effectiveness Team and the audit was registered (Audit Number 178). The data was collected retrospectively via the electronic patient records for 50 new patients seen for impacted maxillary canines. The data was collected and analysed on an excel spreadsheet. The information collected included: Age at referral, referral source, gender, wait times from referral to consultant assessment, wait times from assessment to surgery, treatment completed.
Following cycle one, an action plan was completed. This included a presentation of results and education and awareness of standards to the local team, a targeted webinar to the local primary care referrers, collaboration with the administrative team to improve waiting list times, construction of a proforma to help prioritise surgery bookings, and a planned re-audit. The re-audit (cycle 2) was completed from January – March 2024.
Findings
The results of the audit cycles are summarised in Figure 1. Figure 2 summarises the age of patients at referral. Figure 3 illustrates waiting times and treatment pathway for patients.
1: Summary of Results of Audit Cycles
Figure 2: Summary of patient ages at referral for impacted canines
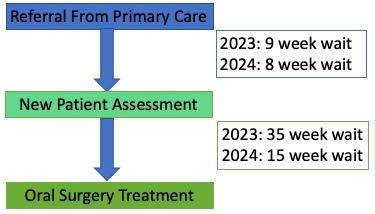
Figure 3: Infographic of treatment pathway and average waiting times
Cycle 1 Findings
The results show only 22% of patients were referred by 12 years old, with an average (mean) age of 13.6 years (range 11-17 years). Two patients of the fifty cases that were analysed had fixed appliances placed prior to surgery, and all of these had their surgery before 18 weeks following the start of this orthodontic treatment, meeting the GIRFT standard. Average waiting time from referral
in primary care to new patient assessment was 9 weeks, then from new patient assessment to surgical treatment of the impacted canines was high, 35 weeks.
Cycle 2 Findings
Following the interventions of the action plan, the results show improvements in waiting times for surgery, with a reduction in average waiting time for surgical treatment from 35 to 15 weeks. However, there has been no improvement in age of referral for impacted canines, with only 22% referred by 12 years old, with an average (mean) age of 14 years (range 11-17 years).
Observations
The gold standard set for age of referral was not met for any cycles, reflecting ongoing challenges related to primary care referrals. 78% of referrals were made after the age of 12 in both cycles, which did not meet the standard, despite targeted education to primary care in the local area. Interestingly, similar results were found in another retrospective audit at the Royal Surrey Hospital in 2016, which found 76% patients were being referred after 12 years old3. Following discussions at local departmental audit meetings and at the Regional South West Thames Audit meeting, we concluded there may be factors out of our control which could explain late presentation, such as COVID having a long-lasting impact on patients’ ability to access primary care. We do not know if it is lack of primary care access causing delays or lack of understanding of the importance of assessing the developing dentition. There is no way to retrospectively know when the patient initially presented to their General Dental Practitioner which is worth considering as a metric in future audits.
This audit highlighted the need for further interventions and education in primary care to ensure earlier identification and referral of impacted canines. A letter to the BDJ has been published to raise awareness amongst colleagues of the importance of assessment of canines and timely referral⁵. The audit showed significant improvements in waiting list times for surgical treatment, which reflect successful changes in internal processes following the action plan
implemented. These included collaboration with the administration team to prioritise surgical procedure bookings for patients undergoing orthodontic treatment, discussion of possible solutions with the administrative team during departmental meetings to engage them, a new proforma sheet for surgical bookings, and improved communication regarding recommended waiting times for each patient when added to the waiting list e.g. ‘to be offered surgical date within 8-12 weeks due to root resorption’ written on surgical day case referrals.
This audit was of benefit to the department as it illustrated care pathways for this cohort of patients and identified where improvements were required. This facilitated useful interdisciplinary team discussion, across different teams within the hospital (the orthodontic, oral surgery and administrative teams), to allow successful implementation of an action plan, which has yielded positive improvements for the benefit of both clinicians and patients within the department. This was a very worthwhile audit which we feel should be carried out on an ongoing basis, over a suitable timeframe.
Recommendations
Points 1 and 2 have been completed following the 1st cycle of the audit, point 3 was completed following the second cycle of the audit, with point 4 to be completed in the future.
1. Presentation of audit results at clinical governance meeting, and circulation via email to all clinicians and administrative teams.
2. Targeted education of Primary Care Referrers including a Webinar and Question & Answer Session on the importance of timings of referrals.
3. Publication of a letter in the British Dental Journal for national education and to raise awareness amongst dental colleagues⁵.
4. Complete a further re-audit in 12 months.
Project Involvement
Annabelle Carter (Lead, data collection, presentation, write up)
Rachel O’Brien (Supervisor, design)
References
1. Husain J, Burden D, McSherry P. (2016). Management of the Palatally Ectopic Maxillary Canine. Royal College of Surgeons England.
2. Jones, L (2021). National Getting it Right First Time: Hospital Dentistry GIRFT National Specialty Report.
3. Patel D, Taylor NG. (2016). Are patients with impacted canines referred too late? Br Dent J. Nov 4;221(9):561-564. doi: 10.1038/ sj.bdj.2016.816
4. Hassan T, Nute S J. An audit of referral practice for patients with impacted palatal canines and the impact of referral guidelines. Br Dent J 2006; 200: 493–496.
5. Carter A, O’Brien. (2025). A simple check, a big difference: canine assessments. British Dental Journal. 238, 367 (2025). https://doi.org/10.1038/s41415-025-8571-0
A two - cycle audit: An assessment of patient understanding of the risks of orthodontic treatment at The Royal London Hospital
Ellen Johnson (ST) and Preeti Jauhar (Consultant Orthodontist)
The Royal London Dental Hospital, London, UK
Background/Rationale Obtaining valid, informed consent is an ethical and legal prerequisite to orthodontic treatment. The General Dental Council (GDC) Standards for the Dental Team1 state that all relevant options and risks must be explained to patients before treatment commences. Furthermore, national guidance from the British Orthodontic Society (BOS)2 outlines specific risks that should be routinely discussed during the consent process. The department sought to review the consent process and assess patients’ understanding of all orthodontic risks outlined in the national guidance, prompting this audit.
Aims and Objectives
The aim of this project was to evaluate and improve patient understanding of the risks of orthodontic treatment provided in NHS secondary care at the Royal London Hospital. The first objective was to quantify patient understanding of key risks, as defined by the British Orthodontic Society (BOS), using a 0–10 visual analogue scale (VAS) in Cycle 1. The second objectives were to implement a standardised PowerPoint consent aid and then to re-measure patients’ understanding.
Standards/guidelines/evidence base
Standard 1 (GDC, 2013): Valid consent must be obtained before any treatment; all relevant options and risks should be explained. Standard 2 (BOS, 2023): 100% of patients should be informed of the main risks of orthodontic treatment as outlined in BOS guidelines. Audit criterion: A locally agreed patient VAS score ≥8/10 for each of the risk domains is taken as evidence that the risk was adequately understood.
Sample and data source
The inclusion criteria for both audit cycles were patients attending consent or bond-up appointments with ST1-3 orthodontic trainees. Patients were excluded if they were already in active treatment or not yet ready for bond-up. The sample for this project was drawn from patients attending orthodontic appointments at the Royal London Hospital.
Cycle 1 was conducted over five weeks, from 14 October to 18 November 2024, and included 13 eligible patients. Data were collected using a paper questionnaire completed after the consent discussion and before fixed appliances were placed.
Cycle 2 took place over four weeks, from 24 February to 24 March 2025, and included 14 eligible patients. Data were collected using the same questionnaire completed after the consent process, which was supported by a standardised PowerPoint consent aid.
Audit type Prospective.
Methodology
A five-page draft questionnaire was initially piloted with local orthodontic consultants to assess its clarity, relevance, and usability. Feedback from the pilot highlighted areas for improvement, including concerns about the overall length and the potential for respondent fatigue. As a result, the questionnaire was refined and reduced to three pages by having one VAS at the top of the questionnaire instead of a VAS on every risk. Additionally, the demographic section was revised to align with UK Office for National Statistics categories, enhancing data comparability and ensuring inclusivity. Following these refinements, the final version of the questionnaire was administered prospectively to patients and can be seen in Figure 1. This contained demographics, 20 orthodontic risk statements scored on a 0-10 scale (10 = complete understanding, 0 = no understanding), and a free-text section invited suggestions. The same questionnaire was used in both cycles. Data were entered into Microsoft Excel and analysed. Mean VAS scores and the proportion of patients scoring ≥8 was calculated for each risk domain.
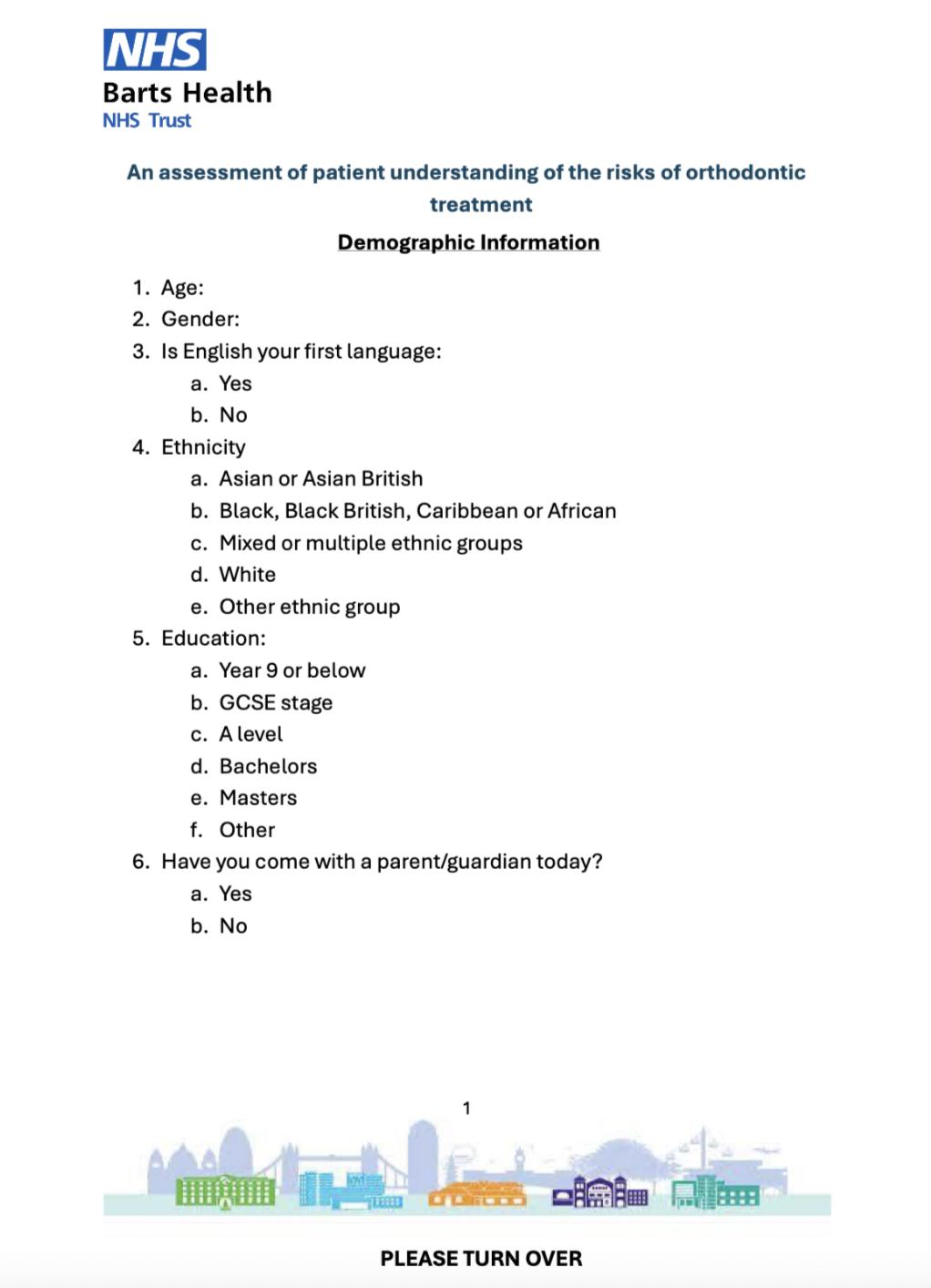
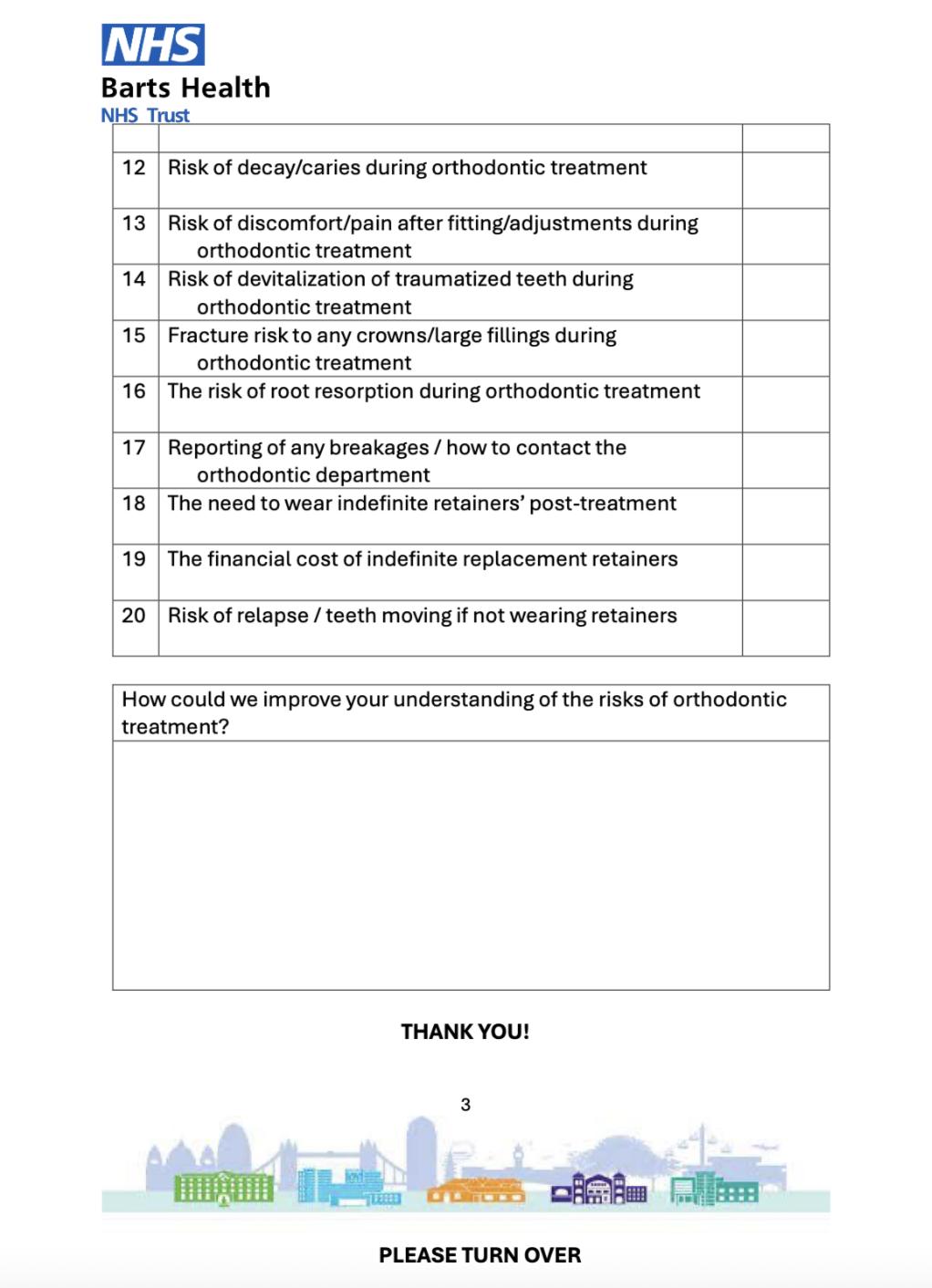
1 : Post-pilot questionnaire used
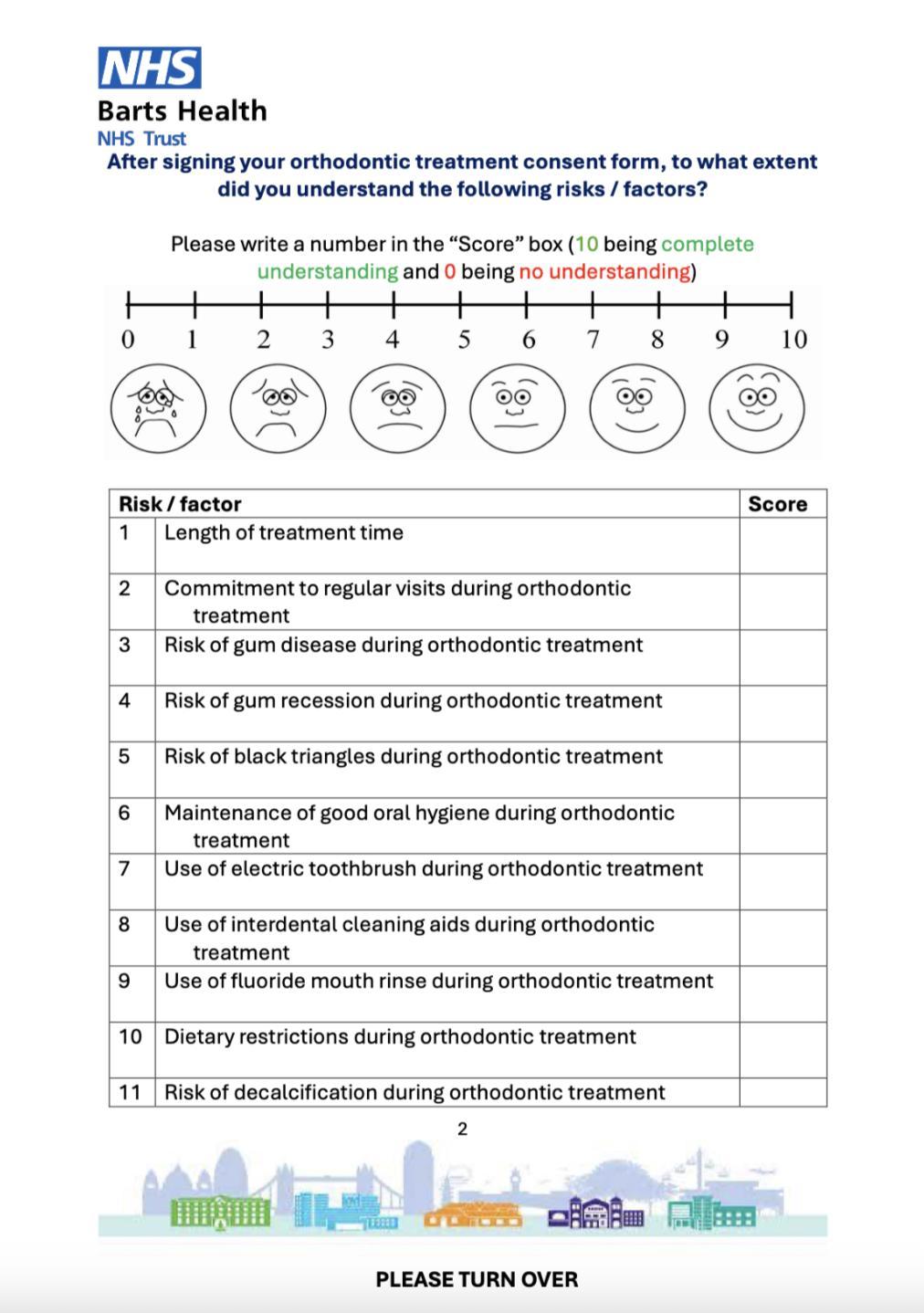
The risks mentioned in the questionnaire are listed here:
1. Length of treatment time
2. Commitment to regular visits during orthodontic treatment
3. Risk of gum disease during orthodontic treatment
4. Risk of gum recession during orthodontic treatment
5. Risk of black triangles during orthodontic treatment
6. Maintenance of good oral hygiene during orthodontic treatment
7. Use of electric toothbrush during orthodontic treatment
8. Use of interdental cleaning aids during orthodontic treatment
9. Use of fluoride mouth rinse during orthodontic treatment
10. Dietary restrictions during orthodontic treatment
11. Risk of decalcification during orthodontic treatment
12. Risk of decay/caries during orthodontic treatment
13. Risk of discomfort/pain after fitting/adjustments during orthodontic treatment
14. Risk of devitalisation of traumatised teeth during orthodontic treatment
15. Fracture risk to any crowns/large fillings during orthodontic treatment
16. Risk of root resorption during orthodontic treatment
17. Reporting of any breakages / how to contact the orthodontic department
18. The need to wear indefinite retainers post-treatment
19. The financial cost of indefinite replacement retainers
20. Risk of relapse / teeth moving if not wearing retainers
Findings
For both Cycle 1 and Cycle 2, 20 orthodontic risks were assessed. In Cycle 1, 16 out of 20 orthodontic risks had a mean patient understanding score below 8/10, demonstrating that many patients were not adequately informed about main orthodontic risks. Thus, the audit standard was not being met. The wide variation in scores also
indicated inconsistent communication among clinicians. The lowest scoring areas were the risk of root resorption, devitalisation of traumatised teeth, and the cost of indefinite retainers, highlighting limited patient understanding in these domains. After using a PowerPoint presentation explaining the risks of orthodontic treatment, Cycle 2 demonstrated substantial improvement. All 20 risks achieved average scores above 8/10. Notable increases were seen in the understanding of root resorption (from 5 to 9) and the cost of indefinite retainers (from 4 to 9). Score variability also decreased, suggesting more consistent and effective communication across the team (Figure 2).

Figure 2: Average results comparing cycle 1 to cycle 2. The y-axis shows average score 0 to 10. The x-axis shows the questionnaire risks labelled 1 to 20. Blue – cycle 1 results. Orange – cycle 2 results.
Observations
Cycle 1 confirmed wide variation in patient understanding, reflecting inconsistent consent delivery across trainees. The use of visual aids and structured explanations has been shown to significantly enhance patient understanding during orthodontic consent discussions. Standardising the discussion with a visual, image -rich PowerPoint dramatically improved comprehension across all domains and reduced inter- clinician variability. As a result, the PowerPoint presentation should continue to be used as a standard adjunct in all consent appointments. However, it should be noted that a sample size of 13 and 14 participants is small and could be a limitation to this audit.
To further improve patient comprehension, a patient-friendly video aligned with current BOS guidance2 is recommended. However, the existing
BOS video3 does not comprehensively represent all relevant risks. We encourage collaboration from readers with experience in video production or connections to the BOS to help develop an updated, standardised video resource. Our long-term aim is to work with the BOS to revise the “Orthodontic Risks” video, ensuring it reflects current practice and evidence-based information.
Recommendations
1. Embed the PowerPoint consent aid as mandatory for all consent appointments; review annually for content accuracy.
2. Develop a short patient-facing video in partnership with the British Orthodontic Society to deliver the same risk information digitally (the BOS risks video is currently outdated). Colleagues with multimedia expertise are invited to collaborate.
3. Re -audit annually, aiming for 100 % of risk domains achieving mean VAS ≥ 8 and ≥ 100 % of patients scoring ≥ 8/10 across all domains.
Project involvement
Ellen Johnson (Project lead)
Preeti Jauhar
Acknowledgements
Thanks to the RLH orthodontic nursing team for distributing questionnaires.
References
1. Council GD. Standards for the dental team. London: General Dental Council [Internet]. 2013
2. British Orthodontic Society. Risks of orthodontic treatment: Advice sheet [Internet]. 2023 [cited 2025 Jul 26].
Available from: https://bos.org.uk/wp-content/ uploads/2023/05/RisksOfOrthodonticTreatmentAdviceSheet-2023.pdf
3. British Orthodontic Society. Orthodontic risks explained [Internet]. YouTube; 2017 [cited 2025 Jul 26].
Available from: https://www.youtube.com/ watch?v=oiYKCxElc3E
Complexity of hospital orthodontic new patient referrals accepted for treatment: A two-cycle audit
Muhammad Bilal Javed (SHO) and Ross McDowall (Consultant Orthodontist)
Queen Alexandra Hospital, Portsmouth, UK
Background/Rationale The Orthodontic Department at Queen Alexandra Hospital (QAH) is currently facing significant challenges due to a recent surge in referral numbers. This increase is largely attributed to the closure and reduction of neighbouring secondary care orthodontic services, which has led to an overwhelming demand for treatment at QAH. According to the “Guide for Commissioning Orthodontics,” hospitals are mandated to accept only cases of high complexity, classified as level 3b1. This guideline aims to ensure that hospital-based orthodontic services are reserved for the most complex cases that cannot be managed in primary care settings. Equally, there is an aspiration, articulated in the Introductory guide to commissioning dental specialties, 2 that as much care as possible should take place in primary care because of the perceived improvement in value for money, as well as offering care ‘closer to home’.
Aims and Objectives
To assess the compliance of orthodontic case acceptance at QAH with national guidelines for case complexity. Ultimately aiming to ensure that hospital resources and clinical capacity are appropriately being used, to safeguard a sustainable service.
Standards/guidelines/evidence base
Based on NHS England guidelines for complexity of accepted cases1, and a study published by Giles Et al. in 20193 .
1. 80% or more of accepted cases to be level 3b
2. 20% or less of accepted cases to be level 3a or lower, allowing for training cases
Sample and data source
The audit sample consisted of orthodontic new patients examined at QAH during two specific time periods. For cycle 1, retrospective data collection was conducted for all new patients seen in March and April 2023 (n=115). In cycle 2, data were collected prospectively for all new patients assessed in March 2024 (n=110). The sample sizes for both cycles were agreed upon by the clinical audit team, ensuring an adequate representation of new patients for comparison purposes across both time frames.
Patients were identified through clinic codes assigned to the Orthodontic Consultants. In cycle 1, four Orthodontic Consultants and their
Specialist Registrars evaluated the patients, while in cycle 2, five Orthodontic Consultants, including two newly appointed Consultants, conducted the evaluations.
The data utilised for the clinical audit were drawn from multiple sources, including electronic health records and handwritten clinical notes.
Exclusion Criteria
Patients of appropriate complexity with suboptimal oral hygiene were rejected for the treatment
Audit type
2-cycle audit. Cycle 1, retrospective data collection. Cycle 2, prospective data collection.
Methodology
A Microsoft Excel (MS Excel) spreadsheet was developed to systematically collect and organise the new patient data. The following variables were extracted for each new patient: demographic details (age and gender), waiting time for initial consultation, the source of referral (general dental practitioner, primary care orthodontist, or secondary care Consultant), treatment complexity, Index of Orthodontic Treatment Need (IOTN) score, and the outcome of the first appointment (accepted for treatment or discharged).
Once data collection was complete for each audit cycle, the MS Excel spreadsheet was used for data analysis.
Findings
The results of the audit, comparing both cycles, are shown in Figures 1 and 2
Figure 1: Comparison of demographics between audit cycles
Cycle 1:
115 new patient referrals were included. Of the 92 patients accepted for treatment, 54% had a 3b treatment complexity and 44% where at 3a or less falling short of the audit standards.
Changes Implemented:
Following cycle 1, there was an Orthodontic Consultant's meeting to discuss the audit results. A document was produced and disseminated, outlining the commissioners' 3a, 3b, and 2 acceptance criteria. In this meeting, it was collectively agreed upon that stricter measures will be implemented when accepting cases.
Cycle 2:
110 new patient referrals were included. Of the 74 patients accepted for treatment, 60% had a 3b treatment complexity and 40% where at 3a or less. Again, the audit standards were not achieved, with only a 6% improvement in level 3b case acceptance between cycles 1 and 2.
Figure 1 highlights IOTN 5i cases specifically, as they represented the majority of all referrals during both audit cycles. This subcategory was reported separately to reflect its clinical predominance and to enable focused analysis. Other IOTN subcategories were excluded due to their low frequency and limited impact on overall trends, to maintain clarity in data presentation.
Figure 2: Comparison of compliance with audit standards between audit cycles
Observations
Identified Good Practice
Audit findings demonstrate partial progress toward aligning case acceptance with commissioning guidelines. In both cycles, Level 3b complexity cases were accepted more frequently than Level 3a cases, though not to the extent required to meet audit standards. Incremental improvements were observed in the appropriate redirection of 3a cases and increased acceptance of 3b cases, suggesting a gradual shift in clinical practice toward prioritising higher-complexity patients.
Figure 3: Comparison of cases accepted at level 3b between Consultants
Furthermore, a significant majority of referrals—71% in cycle 1 and 78% in cycle 2— originated from primary care orthodontists. This indicates that referral pathways are functioning effectively and that patients are largely being routed through appropriate channels.
Areas for Improvement and Clinical Significance Despite observed improvements, audit standards were not met in either cycle. This is clinically
significant as it suggests that a substantial number of patients with Level 3a complexity— whose treatment could be managed within primary care—continue to be accepted into secondary care services. This practice directly contributes to increased demand on hospital resources and limits access for patients with more complex needs (Level 3b), who are the intended recipients of specialist care under current commissioning guidance.
The implications of this are already evident: average waiting times from referral to initial assessment increased markedly from 38 weeks in cycle 1 to 54 weeks in cycle 2. This trend reflects growing systemic pressure, exacerbated by reduced capacity in neighbouring secondary care units and a consequent rise in referrals to QAH. Delays of this magnitude risk compromising timely care for high-need patients and may negatively impact treatment outcomes.
Additionally, the audit highlighted a disproportionate number of 3a referrals originating from primary care. While this indicates engagement with the referral system, it also signals a need for improved communication and reinforcement of acceptance criteria to referring clinicians. However, tightening acceptance thresholds may inadvertently shift demand back to primary care, underscoring the need for system-wide coordination and potential investment in primary care capacity.
Notably, the acceptance pattern in cycle 2 was influenced by the appointment of two new consultants, both of whom demonstrated a higher rate of 3a case acceptance. This variability underscores the importance of consistent application of case selection criteria across the team. Standardising consultant induction and implementing regular peer review or calibration sessions may help ensure uniformity in clinical decision-making and support sustainable service delivery.
Recommendations
1. Audit results are to be disseminated to all Orthodontic Consultants, highlighting our downfall and the need to adhere strictly to the commissioning guidelines.
2. Newly appointed Consultants to be made aware of the Department’s acceptance criteria.
3. Primary care orthodontists are to be informed via the Managed Clinical Network (MCN) of our strict acceptance criteria.
4. Primary care orthodontists to be supported in referring patients directly to Oral Surgery for cases requiring specific interventions, such as canine exposures or the extraction of impacted teeth.
5. Audit results are to be shared with local commissioners to support the expansion of primary and secondary care services to meet regional demands.
6. Repeat data collection for a third audit cycle, following the implementation of these recommendations.
Project involvement
Muhammad Bilal Javed (Project lead, design, data collection, data analysis, presentation, development of action plan)
Ross McDowall (Design, data collection, data analysis, presentation, development of action plan)
Acknowledgements
We would like to thank all the staff who contributed to this audit, as well as the support of the Audit Department at Queen Alexandra Hospital, Portsmouth.
References
1. Chief Dental Officer team. Guides for commissioning dental specialities: orthodontics. London: NHS England, 2015. Available at https://www.england.nhs. uk/commissioning/wp-content/uploads/ sites/12/2015/09/guid-comms-orthodontics.pdf
2. Introductory Guide for Commissioning Dental Specialties: NHS England, 2015. Available at https://www.england.nhs.uk/commissioning/ wp-content/uploads/sites/12/2015/09/ intro-guide-comms-dent-specl.pdf
Canine assessment at the optimal age: a three-centre retrospective audit
Olivia Thompson (DCT) and Elizabeth O’Sullivan (Consultant) Highlands Paediatric Dental Services Hull (PDS), Hull - City Health Care Dental Services (GDS1)
and Beverley - City Health Care Dental Services (GDS2).
Background/Rationale The maxillary canine is a commonly impacted tooth, with an incidence of approximately 1-2%. Of these impactions, around 85% occur palatally1. Canine impaction is associated with significant complications, including root resorption of adjacent teeth and cystic change, which highlights the importance of timely detection2. Palpation of the maxillary canines at around age 9 is recognised as a critical screening step for the early identification of positional abnormalities. As a simple and non-invasive clinical assessment, palpation enables practitioners to detect ectopic eruption patterns during the mixed dentition stage. Current guidelines indicate that failure to detect a palpable canine bulge by age 10–11 should be considered a warning sign and may warrant further investigation or referral3. This audit was undertaken to evaluate current practice against evidence-based standards, comparing specialist paediatric dental services with general dental practice, in order to assess adherence and inform strategies for optimising patient outcomes.
Aims and Objectives
The aim of this audit was to determine whether canine palpation was performed and documented as part of orthodontic screening during examination appointments.
Standards/guidelines/evidence base
The British Orthodontic Society3,⁴ and Royal College of Surgeons3 advises annual palpation of the canine region from age 8-9 years. Any deviations from normal eruption must be documented. The Faculty of General Dental Practice⁵ indicate that General Dental Practitioners (GDPs) should include orthodontic screening in routine examinations and be competent in recognising and recording deviations. Likewise, the British Dental Journal1 highlights the key role of GDPs in monitoring dentition, stressing that early detection reduces the need for complex treatment and helps mitigate medico-legal risks. A standard was agreed that canine palpation must be undertaken and documented in 100% of cases.
Sample and data source
This two-cycle audit was undertaken across three sites in Hull, UK: Specialist Paediatric Dental Services (PDS) and two General Dental Practices (GDS 1 and GDS 2). The audit population included patients aged 9-10.5 years attending routine examination appointments who were sufficiently compliant to undergo assessment in the dental chair with a dental mirror. This age range was selected to capture the critical period for early detection of ectopic maxillary canines. By 10-11
years, the maxillary canine should be clinically palpable in the buccal sulcus⁴, with average eruption occurring betwen 11 and 12 years⁶. Guidelines recommend routine palpation from age 8-9 years to identify displacement early3,⁴. The lower limit was set at 9 years, as palpation before this age is less reliable for identifying true displacement. The upper limit was set at 10.5 years to ensure patients remained within the pre-eruptive phase, where detection of abnormalities is most clinically relevant. Exclusion criteria included patients outside the specified age range, those unable to tolerate examination, those with partially or fully erupted maxillary canines, and those for whom canine palpation had already been recorded at a previous visit.
For cycle one, data was collected retrospectively from day lists between August and October 2024, and for cycle two between March and May 2025. Eligible patients were identified through clinical day lists, with 164 patients reviewed in cycle one and 150 in cycle two. The sample size was determined pragmatically, including all eligible patients attending within the defined periods. This provided a representative audit cohort. Corresponding electronic health records were then accessed, and clinical notes analysed to establish whether canine palpation had been performed and appropriately documented.
Audit type
Retrospective, three-centre, two-cycle audit.
Methodology
Data analysis was conducted retrospectively using the R4 patient database system. For each participating clinic, patient day lists were reviewed over the designated three-month periods: August-October 2024 for cycle one, and March-May 2025 for cycle two. Each patient record was initially screened for basic demographic information, and those aged between 9 and 10.5 years attending for an examination appointment were considered for inclusion. Records were then examined in greater detail to confirm sufficient compliance, defined as documented ability to sit in the dental chair and undergo examination with a dental mirror. Eligible records were subsequently analysed to determine whether canine palpation had been performed and documented. Compliance with this standard was recorded in a spreadsheet for each site, providing a basis for comparison across the three sites.
Findings
Cycle 1:
The audit standard was not achieved at any of the participating sites. At PDS, canine palpation was documented in 38% of patients. This site was staffed by nine clinicians, including dental core trainees, dental officers, speciality registrars, specialists, and consultants. At GDS 1, documentation was recorded in 0% of cases, with two GDPs providing care at this site. At GDS 2, compliance was 43%, with one GDP undertaking the examinations. These results highlight variation in practice that may be influenced by clinician numbers, professional roles, and service pressures. The findings were disseminated to clinicians across all sites. Teaching was given to educate and reinforce the importance of identifying ectopic canines and the potential consequences of missed diagnoses. The introduction of an electronic documentation template was recommended to standardise recording practices. A second audit cycle was planned to assess the impact of these interventions.
Cycle 2:
In cycle two, improvements were observed across all three centres. At PDS, compliance increased substantially, with near-complete adherence to the standard at 92%. GDS 1 demonstrated a small increase to 9%, although performance remained significantly below the recommended level. GDS 2 showed a marked improvement, with documentation of canine palpation recorded in 67% of patients, however the agreed standard was still not met. A summary of the results is presented in figure 1.
Figure 1: a graph to summarise audit results.
Observations
Improvements were observed across both audit cycles, with PDS demonstrating strong engagement and notable progress. As a training site, higher compliance may be expected due to broader staffing, greater clinical experience, and access to supervision. The educational environment also supports a culture of clinical governance and standardised use of the electronic template. However, the high staff turnover inherent to a training centre highlights the need for a clear induction process to maintain standards.
In primary care, challenges remain. Limited appointment time was reported as a barrier. However, canine palpation requires minimal time and documentation can be streamlined via the electronic proforma. At GDS 1, template uptake was low and clinical notes were often brief, contributing to reduced compliance. Inconsistent documentation risks compromising patient safety, continuity of care, and medico-legal protection. Strengthening compliance will require targeted use of digital tools, alongside focused training and ongoing staff support.
This audit reinforces that best practice involves routine palpation from age 8–9 years, with accurate, timely documentation ideally facilitated through an electronic template. In summary, meaningful progress has been achieved across cycles, but further improvement is required to meet clinical standards fully. A third audit cycle is recommended to consolidate progress, strengthen adherence, and embed best practice consistently across all sites.
Recommendations
1. Present findings from both audit cycles at all three sites during local clinical governance meetings.
2. Provide tailored teaching for staff on ectopic canine detection and documentation requirements in line with GDC standards.
3. Incorporate canine palpation and documentation training into staff induction to address turnover and maintain standards.
4. Re-audit in December 2025, aiming to achieve full compliance with the audit standard.
Project involvement
Olivia Thompson (Audit lead)
Elizabeth O’Sullivan (Audit Supervisor)
References
1. Husain J, Burden D, McSherry P, et al. National clinical guidelines for management of the palatally ectopic maxillary canine. Br Dent J. 2012;213(4):171-6. doi:10.1038/sj.bdj.2012.726
2. Patel D, Taylor N. Are patients with impacted canines referred too late? Br Dent J. 2016;221(10):561-4. doi:10.1038/sj.bdj.2016.816
3. British Orthodontic Society, Royal College of Surgeons (Eng). Management of the palatally ectopic maxillary canines. Revised ed. London: British Orthodontic Society; 2023 [cited 2025 Sept 30].
Available from: https://www.rcseng.ac.uk/-/
4. British Orthodontic Society. Managing the Developing Dentition. 1st ed. London: British Orthodontic Society; 2023.
Available from: https://bos.org.uk/wpcontent/uploads/2023/05/Managing-theDeveloping-dentition-2023-1.pdf
5. Faculty of General Dental Practitioners (FGDP). Clinical Examination & Record-Keeping Good Practice Guidelines: Clinical Examination and Record Keeping. London: Faculty of General Dental Practice (UK), The Royal College of Surgeons of England; 2021.
6. Thilander B, Bjerklin K, Bondemark L. Essential Orthodontics. 1st ed. Hoboken, NJ: Wiley-Blackwell; 2018.

LearnfromtheUK'slargest groupofOrthodontic Nurses,Therapists, PracticeManagersand TreatmentCo-ordinators.

Jointodayandenjoy...
•arangeofexclusive benefits,includingaccess tocontinuingeducation opportunities
•discountedratesfor eventsandconferences
•connectingwithyour peers,andexchanging experiencesandnews
•stayingup-to-datewith thelatestindustry developments
Becomeamemberat orthodontic-ong.org