
















At ChristianaCare, Clinical Effectiveness is foundational to improving the health and well-being of our communities. Every day, across every area of care, our caregivers strive to deliver the highest standard of service, ensuring that all patients receive safe, effective and compassionate care with love and excellence.
The framework of our Clinical Effectiveness Structure is built upon six pillars Zero Harm, Patient Experience, Quality, Patient Flow, Health Equity and Population Health that support the delivery of safe, high-quality and effective clinical care and are the driving force behind our success. The structure is designed to ensure care that delivery is evidence-based and patient-centered. Its pillars utilize key components to execute on annual goals that include evidence-based practice, quality improvement initiatives, multidisciplinary teams, patient safety programs, education and training, and patient and family engagement.
A significant goal for Clinical Effectiveness is to be among the top 25 comprehensive academic medical centers in the nation for Quality and Safety by 2025. This commitment is propelled by rigorous benchmarking standards, including the Vizient Quality and Accountability Performance Scorecard (see page 42), which evaluates more than 100 academic medical centers across six key domains: mortality, efficiency, effectiveness, patient-centeredness, safety and equity. In 2020, we ranked 83rd among our peers, at which point we set the goal of becoming one of the top 25 by 2025. We have made significant progress thanks to the extraordinary dedication of our Clinical Effectiveness committee, councils, caregivers and targeted initiatives across our three campuses, ambulatory practices and HomeHealth.
“Our
North Star is the journey to the top 25 by 2025. It shapes every Quality and Safety initiative, innovation and improvement. Whether we reach our goal this year or in the future, ChristianaCare’s unwavering pursuit of excellence continues transforming care for our patients and communities.

This report celebrates and shares our teams’ tremendous efforts and ongoing work to achieve quality and safety goals.”
Varadarajan Subbiah, M.D., MBA, FACP, CHCQM, chief clinical effectiveness officer


Fiscal Year 2025

Delaware is No. 1 in the nation for hospital quality, according to the latest U.S. News & World Report “Best States” rankings, a measure of hospital success in performing or treating various procedures and conditions, such as cancer surgeries, organ failure, joint replacement and more. Right: Stephanie Caterson, M.D., and John Przybylski Jr., PA-C, are sought-after experts in breast reconstruction and microsurgical techniques after cancer surgery.
“The Transitional Medical Unit team is passionate about striving for excellence in Quality and Safety through the collaborative work of our Unit Performance Teams, which are closely integrated with our Unit Practice Council.
Achieve year-over-year improvement in clinical excellence through a high-reliability approach, a culture of safety and a commitment to the identification, prevention and elimination of patient and caregiver harm.

This structure leads the way in fostering caregiver engagement, leadership development and mentorship, ultimately resulting in a ‘compound influence effect.’
The phenomenon has allowed me to add value and cultivate other leaders who then add value and cultivate more leaders, producing a culture of shared decision making, peer-topeer accountability and endless opportunities for growth and development. Consequently, we have driven exceptional patient outcomes and an overall improvement in caregiver wellbeing and that is why I’m here!”
Tim Heckman, MSN, RN - BC, nurse manager, 3D Transitional Medical Unit


The Preventable Harm Rate is a key patient safety measure at ChristianaCare. We measure 19 indicators across our three hospital campuses and ambulatory practices. Among them are health care-associated infections, Agency for Healthcare Research and Quality patient safety indicators (PSI), acute care falls with major injury, and falls in ambulatory settings.
Most measures are required for reporting to the Centers for Medicare and Medicaid Services (CMS) and tied to payfor-performance programs (see page 45). Progress in the indicators helps strengthen our core Clinical Effectiveness
Structure goal of getting to and maintaining a standing among our academic medical center cohort peers in the Vizient Quality and Accountability Performance Scorecard’s Top 25 performers (see page 42).
Preventable Harm Rate



Jul-20Sep-20Nov-20Jan-21Mar-21May-21Jul-21Sep-21Nov-21Jan-22Mar-22May-22Jul-22Sep-22Nov-22Jan-23Mar-23May-23Jul-23Sep-23Nov-23Jan-24Mar-24May-24Jul-24Sep-24Nov-24Jan-25Mar-25
Through March, the FY 25 Preventable Harm Rate is 0.77, below the Annual Operating Plan stretch goal of 0.87. The rate has decreased 5.4% from FY 24; the number of patients harmed decreased by 3%, to 252 from 261.

Our Zero Harm Council is accountable for driving progress. Teams responsible for developing, implementing and measuring zero harm include Infection Prevention and our HAPI systemwide committee; PSI-90 steer; Falls Committee and Ambulatory Safety Committee. All report to the Zero Harm Council.
To advance patient safety and harm reduction, the Council identified several priority areas for FY 25 :
• PSI 3: Hospital-acquired pressure injuries (HAPI)
• PSI 11: Postoperative respiratory failure
• Colon surgical site infections (SSI)
• Central line-associated bloodstream infections (CLABSI)
• Catheter-associated urinary tract infections (CAUTI)
• Falls (acute and ambulatory) and Falls with major injury
Preventable Harm Rate by Campus


Two of our three campuses have improved their preventable harm rate and are better than stretch goals; Wilmington has seen a small increase.

ChristianaCare tracks 11 Agency for Healthcare Research and Quality (AHRQ) PSIs as part of our commitment to zero harm.
The PSI 90 is a weighted combination of 10 specific PSI measures, primarily related to postsurgical complications.
CMS incorporates PSI 90 into its pay-for-performance initiatives and star rating system. National hospital rating organizations like Leapfrog use this measure to assess and compare hospital performance.
ChristianaCare’s PSI 90 Steer, under our surgical service line, creates and oversees review teams for every PSI. Each team includes a physician, an advanced practice clinician and a nurse. They review cases related to their PSI and share observations and opportunities at collective PSI 90 group meetings.
Learn how our caregivers are advancing safety in Guideline to Reduce Postoperative Acute Kidney Injury in Surgical Patients on page 69.


The PSI-90 composite score has improved yearly, to 0.93 in FY 25 from 1.27 in FY 21, a 27% reduction. The risk-adjusted score has been better than the national in ten of the past 13 months.

In FY 25, ChristianaCare has made significant strides in patient safety, improving our PSI 90 rates overall and bringing our AHRQ Patient Safety Composite Score below target. Our commitment to excellence continues to set us apart, as we outperform other academic medical centers in 9 of 11 patient safety indicators.
With consistently lower risk-adjusted PSI rates compared to our peers, we remain strong in key areas, including PSI 12 (see sidebar), and have identified opportunities for further improvement in PSI 3 (see page 12), PSI 10 (see sidebar) and PSI 11 (see page 14).

Targeted interventions by the Venous thromboembolism (VTE) Steer reduced rates for PSI 12 Perioperative Pulmonary Embolism or Deep Vein Thrombosis by 50%.
We continue to perform better overall, with lower observed to expected rates in most PSIs than other academic medical centers.
Key FY 25 steer-led enhancements include a revised risk assessment tool prioritizing high-risk patients, updated prophylaxis dosing for morbid obesity, renal impairment, and trauma patients and mandatory VTE risk reassessments at designated intervals. Additionally, 100 new pneumatic compression boot machines were purchased, nursing education on equipment return was enhanced, and a comprehensive VTE Prophylaxis Care Guideline was developed. These systemwide improvements ensure consistency, optimize patient care and strengthen postoperative VTE prevention, demonstrating our commitment to reducing preventable complications and enhancing outcomes.

After several years of improvement, we experienced an overall increase in PSI 3 rates across all three campuses in FY 25. At the same time, our HomeHealth agency remained below the national home health benchmark.
To address the campus increases, our systemwide HAPI committee implemented several interventions, including developing unit-level action plans, creating a patient mobilization job aid, assessing positioning product availability and restructuring the HAPI Triad to expand learning across the system. The team also established a process for concurrent PSI 3 event review.
Additional actions underway included the development of acute skin failure criteria for PSI 3 validation while maintaining preventative measures, piloting an enhanced skin assessment for patients with dark skin tones (see next page), revising our Accountability Toolkit, exploring new technology and prevention devices and collaborating with select units to enhance risk identification and care planning.
HomeHealth continues its multidisciplinary prevention strategy, promoting customized care plans, risk-specific interventions, and education on weight-shifting and pressure relief devices to prevent injury at home.
ChristianaCare HAPI Rate


After successfully driving down the HAPI rate to 0.43 in FY 22 from 3.65 in 2019 and maintaining a low rate for more than a year, ChristianaCare’s rate began to increase, reaching 0.76 in FY 25.


Although the percent of patients with new or evolving stage 2 or higher pressure injuries increased to 0.29% in FY 25 from 0.20% in FY 24, HomeHealth pressure injuries remain below the 0.35% SHP national home health benchmark.

To identify areas for HAPI rate improvement, our Evidence-Based Practice Fellowship team conducted a comprehensive review of current practices against the latest research. A critical gap was identified in the assessment of darker skin tones.
Data shows that patients with darker skin tones experience pressure injuries at rates two to three times higher than those with lighter skin. This disparity leads to increased morbidity rates and imposes a significant financial burden, with treatment costs exceeding $70,000 per patient due to prolonged hospital stays.
The National Pressure Injury Advisory Panel emphasizes the need for enhanced assessment techniques, including skin moistening, improved lighting, palpation and objective skin tone identification. Using standardized tools such as the Fitzpatrick Scale or the Munsell System of Color Notation an unbiased benchmark for skin color helps avoid making race-based assumptions in assessment.
The HAPI team created an action plan that includes targeted interventions, such as:
• Updating the Skin Integrity Case Mix Group, a system for categorizing patients into groups based on similar clinical characteristics, to include enhanced assessment guidelines for darker skin tones.
• Integrating enhanced skin assessment protocols into Integumentary iView documentation.
• Conducting enhanced skin assessments upon admission and every eight hours.
• Implementing comprehensive nursing education on identifying pressure injuries in darker skin tones.
A pilot of the plan began in March 2025 on select units across our three campuses.

The incidence of HAPI among patients with darker skin tones is 2 to 3 times higher compared to those with lighter skin tones — about 0.12% (12 in 10,000) Black/African American and Asian patients compared to 0.4% (4 in 10,000) of White patients.

In response to rising PSI 11 rates, a postoperative Respiratory Failure Subcommittee formed in October 2024 to improve outcomes and reduce reintubations. Key interventions have included:
• Requiring documentation of extubation criteria and increasing use of Sugammadex.
• Mandating the use of TwitchView an objective neuromuscular monitor to help reduce residual paralysis by guiding precise dosing and reversal of paralytics.
• Creating a new Rapid Response Team (RRT) Dashboard to highlight trends in location, case type and anesthesia details for surgical patients. Critically reviewing outcomes for patients triggering a rapid response within an eight-hour window and 24 hours of surgery allows the opportunity to improve postoperative plans of care and surgical management of complex patients.
• Developing a Reintubation Dashboard that tracks timing, surgical specialty and case classification for all unplanned reintubations, helping teams spot patterns and address care standards.
• Establishing PACU Anesthesiologist Evaluation Criteria for structured bedside assessments of transfer readiness, enhancing triage of hemodynamics, airway and mental status.

Postoperative Respiratory Failure Rates have increased 23% since FY 24 and are higher than our academic medical center peers

Health care-associated infections contribute to increased mortality, morbidity and health care costs, making prevention a key priority in ChristianaCare’s commitment to zero harm.
Based on our performance in FY 24, three priority areas were identified for FY 25: CAUTI, CLABSI and Colon SSI. Notable improvements were seen in both CAUTI and Colon SSI rates over the past year. However, while they remain below expected, C. difficile rates increased during FY 24 and have now been designated as a new priority for the upcoming fiscal year.
Health Care-Associated Infections

Both CAUTI and Colon SSI improved compared to FY 24. Small increases were seen in CLABSI and MRSA. C. difficile has the greatest opportunity, with a rate increase of 46%.
Both CAUTI and Colon SSI improved compared to FY 24. Small increases were seen in CLABSI and MRSA. C. difficile has the greatest opportunity with a rate increase of 46%.

After seeing increased CAUTI rates from 2022 to 2024, the rate decreased in FY 25. The observed-to-expected Standardized Infection Ratio (SIR) improved significantly, dropping from 1.03 at the end of 2022 to 0.45 less than half the number of expected cases, and outperforming the Vizient median. A key driver of this improvement was the focused effort on timely removal of Foley catheters, which led to a decrease in the Standardized Utilization Ratio (SUR) from 0.51 to 0.35, indicating that we’re now using about one-third of expected catheters.
In FY 25, the systemwide CAUTI Steer:
• Worked with catheter kit vendor to perform our annual assessment, finding our Foley utilization rate continues to decrease since 2017 and the duration of Foley insertion has increased for the first time this year.
• Planned a review of current products and equipment to standardize and update supplies across all three campuses.
• Updated Foley bag labels with date of insertion to standardize nursing processes.
• Investigated the use of impregnated Foley catheters for patients who are long admissions or who require extended duration of catheterization.
Quality and Safety Impact
Learn how our caregivers are preventing CAUTI. See Be Aware of Perfect Care on page 68.

The observed versus expected standardized infection ratio improved to 0.45 in FY 24 from 1.03 in FY 22. The focus on timely removal of Foley catheters led to a reduction in the observed versus expected standardized utilization ratio to 0.35 from 0.51 during the same period.

Surgical site infections are among the most common preventable surgeryrelated complications, particularly with colorectal procedures. A Colon SSI can increase a patient’s length of stay and overall risk of readmissions and death. Reducing SSIs is critical to improving patient outcomes and surgical success.
After an increase in Colon SSI rates from FY 23 to FY 24, we’ve seen a decline in FY 25, thanks to our Colorectal Pathway Team’s focused work to further reduce infection rates. The team meets monthly. Among its recent activities are:
• Streamlining Performance Improvement case review using our Report2Learn (R2L) platform, including engagement with operating surgeons.
• Developing department-wide education on documentation and adherence to the Colon Bundle.
• Monitoring compliance with evidence-based infection prevention protocols.
• Implementing operating room improvements, including wound class reconciliation and enhanced closure protocols.
Site Infections - Colon Procedures


Following the Colon SSI team focus on standardized review and bundle processes, the SSI rate decreased 58%, to 2.94 from 6.94 infections per 100 procedures.

Although CLABSI rates improved in the beginning of Q1 of FY 25, we saw a slight increase as of March. Our systemwide CLABSI Steer focused on the following initiatives to reduce CLABSI rates further:
• Sharing lessons learned during CLABSI Triad case reviews (and CAUTI and C. difficile) with Nursing in monthly newsletter, The Metric.
• Launching New Central Line (CL) PowerPlans specific for Newly Inserted or Present on Admission CLs in PowerChart, allowing for timely and accurate order entry and documentation.
• Standardizing care for patients with venous sheaths.
• Investigating use of sterile end caps (SwabTip) at Christiana and Wilmington Hospitals to align with Union Hospital.
• Developed scripting for caregivers when patients refuse CHG bathing/Nasal PI and instructions for escalation to managers if patients continue to decline care.
• Developing an algorithm for CL dressing management.
Line-Associated Bloodstream Infections



Although CLABSI incidence has improved substantially since FY 23, there has been a small increase this fiscal year. The number of CLABSI increased 33% FY 25 to-date through March to 36 from 33. The rate increased 13%, to 0.77 from 0.68 cases per 1,000 line days. During the same period, central line utilization improved slightly, to 1.4 from 1.5 lines per 10 patient days.

From 2023 to 2024, C. difficile rates saw a consistent decline across the health system. While most cases occur at Christiana Hospital, occasional cases are also seen at Wilmington and Union Hospitals.
At the same time, in FY 25, there has been a gradual increase in hospital-onset cases, prompting intensified efforts from the C. difficile Steer to curb infections. After an intensive case review, the team found most hospital-onset cases appeared to be true infections rather than colonization. Among several interventions set up in FY 25 were:
• Introducing a patient-friendly Bristol Stool Scale for Nursing discussions with patients to better document diarrhea and prompt earlier testing.
• Clarifying for providers that the Enteric Pathogens panel at ChristianaCare does not contain C. difficile testing.
• Revising the C. difficile Risk Calculator, Smart Zone Alert and Test PowerPlan to improve infection identification.
• Targeting IP observations of C. difficile isolation rooms to focus on soap and water hand hygiene and proper use of personal protective equipment.
• Continuing work with Environmental Services and Capacity Management to maximize thorough room cleaning while maintaining efficient room turnaround.
• Piloting a commode liner to help prevent transmission of C. difficile in the patient care environment.

After declining incidence in FY 24, cases of C. difficile have increased in FY 25, particularly during the high-census winter months. At 0.37, the SIR remains below the national level of 1.0 and Vizient academic medical center 50th percentile of 0.4.

ChristianaCare’s Hand Hygiene Steer works with unit leaders to improve caregiver hand hygiene practices through education, data analysis and targeted interventions. To monitor HH protocol compliance, Leapfrog recommends performing at least 200 hand hygiene observations per unit each month.
In FY 25, ChristianaCare units and our Infection Prevention (IP) team conducted 175,336 evaluations, with most inpatient units consistently meeting Leapfrog observation goals. They found most units and departments monitoring hand hygiene met or exceeded the minimum required observations.
Key improvement efforts included focusing IP observations in C. difficile isolation rooms, starting new rewards and recognition programs for both individual and unit hand hygiene observation volumes and compliance, and completing an IP/unit ”buddy" system to assess the accuracy of unit-based observations. Improving adherence to hand hygiene particularly before patient contact remains a top priority for reducing health care-associated infections.



More than 90% of the 60 patient care units and departments that monitor hand hygiene met or exceeded the minimum required observations. Hand hygiene practice adherence, measured as hand hygiene before entering or upon leaving a patient's room, was 92%. (Infection Prevention, which completes independent monitoring to validate hand hygiene practice and provide real-time education, found that compliance was only 59% systemwide. The gap between unit-based and IP validation monitors was significantly smaller at Union Hospital.) Use of appropriate personal protective equipment was 97%, and compliance with equipment cleaning was 98%.

Acute inpatient fall rates across our three campuses have significantly improved since FY 22, remaining below the National Database of Nursing Quality Indicators (NDNQI) Magnet® benchmark.
In FY 25, our multidisciplinary, systemwide Fall Prevention and Mobility team implemented proactive fall prevention strategies to further reduce inpatient fall rates. These included standardizing fall reviews, revising documentation, enhancing communication, updating the Perfect Care Bundle with questions about mobility, targeting education for caregivers, expanding mobility initiatives and more.

Falls with Major Injury have decreased 29% since FY 22, to 0.24 from 0.34 per 10,000 patient days. The number of falls with major injury is on track to decrease 33% in FY 25.
Proactive prevention cut fall rates at Union Hospital Union Hospital reduced patient falls by 61% in FY 25’s first two quarters. Key initiatives driving this decrease include implementing weekly fall review meetings, automated EMR interventions and the Johns Hopkins Mobility Program. Now, all patients receive fall prevention measures, reinforcing Union Hospital’s commitment to patient safety and continuous improvement.

Acute inpatient fall rates remain below the NDNQI Magnet© Benchmark, improving by almost 50% for the Wilmington and Cecil County campuses since FY 22. Newark rates declined 21%. Since FY 22, there have been over 230 fewer falls across the three campuses.

Since FY 21, ChristianaCare HomeHealth has had fewer Falls with Major Injury than state and national benchmarks.
The agency continues to take a multidisciplinary approach to fall prevention. Its ongoing efforts to reduce falls include:
• Using a multifactor tool to assess a patient’s risk for falling.
• Implementing individualized interventions to improve safety, such as recommending home modifications and equipment.
• Providing individualized home exercise programs for strengthening and balance.Collaborating during team case conferences to identify challenges and opportunities.
In FY 25, HomeHealth maintained its standing below state and national benchmarks.


The incidence of HomeHealth Falls with Major Injury decreased to 0.40% in FY 25 from 0.53% in FY 24.

The Ambulatory Falls Subcommittee implemented multiple interventions to address ambulatory-specific risks for patient falls.
Among the strategies were:
• Disseminating Huddle Tips on Falls Best Practices to reinforce awareness in clinical settings.
• Implementing a fall risk screening tool before rooming patients, allowing for early intervention.
• Assigning Web-Ed training in Learning Space, with an 80%+ completion rate among caregivers.
• Establishing an audit tool to monitor compliance with best practices and ensure sustained improvement.
• Enhancing processes to support high fall-risk patients with cognitive impairment, ensuring they receive additional assistance.

Following a gap analysis and a 2022 Medical Office Culture of Safety Survey, our ambulatory practices launched a novel, multifaceted and replicable Ambulatory Safety Program (ASP). The data-driven approach aims to increase event reporting and strengthen the culture of safety among caregivers. One key ASP enhancement was creating the "Quick Submit" form a shorter, more intuitive event reporting tool within R2L. This led to a 65% increase in ambulatory event reporting and a 23% increase in Good Catch submissions. Additionally, Culture of Safety Survey responses related to ASP interventions improved by 2%.
Falls in the medical group office practices have decreased 47% in FY 25, to 36 from 68. The fall rate decreased to 0.54 from 1.13 falls per 10,000 office visits.
The ASP team received the 2025 RLDatix Patient Commitment Award for its work. The national award celebrates initiatives that are transforming the future of health care.

Annually, nearly 10,000 patients nationwide die each year, and more than one million experience adverse events due to medication errors. According to the National Center for Biotechnology Information, the U.S. spends more than $40 billion per year on patients affected by medication errors. Documenting a patient’s medication history sets the foundation for safe and effective treatment decisions in health care.
The current standard of care is to have a dedicated resource who documents an accurate medication history when patients are admitted to the hospital. To advance our medication safety program, ChristianaCare has hired two pharmacy technicians to focus exclusively on obtaining accurate medication histories for patients admitted through the Wilmington Hospital ED.
This improves quality of care and efficiency for our other frontline caregivers, including physicians, advanced practice clinicians, pharmacists and nurses. Based on positive results and feedback, we aim to expand this program across all three campuses, prioritizing patients at highest risk for medication errors and adverse events.
to Medication History Completion



Pharmacy technicians completed 1,127 medication histories over a 12-month period in the Wilmington ED. Average time from admission to completion for the more than 500 high-priority patients was 6.9 hours versus 15.2 hours for histories completed by other clinicians.

For 10 years, ChristianaCare has implemented the Communication and Optimal Resolution (CANDOR) program, a structured approach to addressing unexpected patient harm with transparency and support. As an early adopter of communication and resolution programs (CRP), ChristianaCare fosters open discussions with patients and families while strengthening a culture of safety and learning.
This approach aligns with new CMS regulations requiring CRPs in hospital patient safety programs by 2026. The Accreditation Council for Graduate Medical Education also mandates CRP education for medical trainees, reinforcing ChristianaCare’s leadership in this area.
Since 2015, CANDOR has reviewed nearly 650 cases 66% of which were unexpected deaths, 33% of which were permanent harm to patients. This has led to 500 system improvements, improved caregiver support and timely case resolutions without litigation.
Through collaboration with other CRPs as part of the national PACT Collaborative (Pathway to Accountability, Compassion, and Transparency), ChristianaCare has introduced recent improvements to CANDOR, including developing patient education brochures and communication tools to enhance caregiver understanding and patient engagement.
See how learnings from CANDOR can drive change in Decannulate and Defend: Tracheostomy Rounding to Optimize Outcomes on page 68.

Since its inception, the CANDOR program has evaluated almost 650 cases. Volumes in recent years are similar to prepandemic years.

96% of debrief participants from September 2023 to January 2025 strongly agreed or agreed that other participants assumed good intentions, a principle of CANDOR, during incident debrief meetings — all felt the debrief leader assumed good intentions.

ChristianaCare assesses its progress toward high reliability and a strong safety culture every two years through the Hospital Survey on Patient Safety Culture and the Medical Office Survey on Patient Safety Culture. Both surveys are validated by the Agency for Healthcare Research and Quality, a national leader in healthcare safety and quality. The most recent survey, conducted in late 2024, revealed notable improvements in key areas compared to 2022.
To address areas identified for improvement in the Hospital Survey — particularly Staffing and Management Support for Patient Safety — ChristianaCare is taking the following actions:
• Enhancing transparency in staff recruitment and retention with a strategic, multifaceted approach.
• Engaging frontline caregivers to address concerns, develop solutions and ensure follow-through.
• Enhancing education to support a culture of safety and high reliability.
• Boosting Good Catch reporting visibility with Zero Hero Awards and Bravo recognition.
• Simplifying Report2Learn (R2L) with a Quick Submit form for streamlined, efficient event reporting.
To drive improvement in medical offices, specifically around Work Pace and Pressure, we are:
• Creating and implementing tools to assist with office scheduling and managing patient follow-up.
• Enhancing communication and coordination with centralized departments.
• Developing strategies to address workplace violence.
Culture of Safety Survey - Hospital
2024 COS 2022 COS SOPS Benchmark

Scores in 11 of the 13 domains improved from 2022 survey results. The largest increase was seen in two areas with the greatest opportunity Staffing and Work Pace, and Hospital Management Support for Patient Safety. Rating of Teamwork exceeds the national benchmark.
Culture of Patient Safety - Medical Office


Scores in 11 of 14 domains improved or remained stable compared to 2022 results. Strongest performing domains include Teamwork and Patient Care Tracking/Follow-up. The greatest improvement was in Communication Openness. Opportunities include Work Pressure & Pace and Leadership Support for Patient Safety

For a decade, ChristianaCare’s Care for the Caregiver (C4C) program has provided essential emotional support to caregivers experiencing distress. This evidence-based approach helps to decrease acute and chronic stress reactions for caregivers, which is essential to patient safety.
In FY 25, the program saw its highest-ever number of referrals: 508. Of these, 79% were accepted for support, leading to 384 peer support encounters. In addition to individual support, C4C expanded group support, hosting 25 sessions up from 20 in 2023 with an average of 12 caregivers per session, ultimately reaching 300 additional caregivers. Our 70 trained peer supporters make this possible.
Additionally, after rolling out our Psychological First Aid (PFA) training program in 2023, we noticed a steady increase in leaders and supervisors referring their teams, colleagues and peers to C4C. PFA is an intervention designed to help those in highrisk professions like health care recognize and respond to signs of emotional distress in the wake of traumatizing events.
As in past years, workplace violence remains one of the top reasons for C4C referrals, second only to patient death or coding events. This continues a four-year trend (2021–2024), highlighting the need for ongoing peer support as violence against caregivers remains a nationwide crisis.
Supervisor Self Colleague Other

Over 500 requests for C4C were made in 2024. The percentage of referral requests from supervisors has increased to 57% in 2024 from 32% in 2021.
Referrals for workplace violence have increased in recent years, accounting for more than 30% of requests in 2024.
*Staff concern can be either a work-related concern or personal concern and refers to issues such as anxiety, depression, and burnout.

Ensuring caregiver safety is a critical priority, as outlined by OSHA’s standards for workplace safety in healthcare. Among ChristianaCare’s OSHA reportable events, we saw no significant changes in needlestick/sharps injuries between FY 24 and FY 25. Patient handling injuries also decreased slightly, from 31 in FY 24 to 30 in FY 25.
Nursing accounts for approximately 44% of these incidents.
To address this, we've implemented initiatives such as a sharps safety workshop during our Nursing Onboarding: Strengthening the Core with Excellence program. Additional prevention initiatives include sharps safety rounds, systemwide safety communications, device review and focused education.
Additionally, the Patient, Environment, Equipment, Posture, Safety (PEEPS) safe patient handling team developed a new Web-Ed module for inpatient acute care teams in our Newark and Wilmington campuses, complementing existing training for outpatient and ancillary staff. PEEPS has also partnered with organizational excellence to reduce sling losses and associated costs. Additionally, PEEPS. launched a SharePoint site for caregivers with enhanced educational tools, including instructional videos, informational resources and reference pages.
The Occupational Safety team has been working with several Support Services departments (e.g., environmental services, food and nutrition, and textiles) to enhance Personal Protective Equipment and train teams on body mechanics to address injuries from physical demands and material handling. Several initiatives are also underway in our contractor safety program, including the development of a new training video, as well as updates to the Pre-Construction Risk Assessment Policy and Safe Work Permit revisions.
Cut-Puncture Needlestick/Sharp Number
Slips, Trips, Falls
Struck By-Caught Between
Patient Handling
Physical Demands
Patient Assault
Lift-Move Material
Cut-Puncture-Industrial
Accident

Needlestick/Sharps account for the majority of recordable injuries and increased just slightly in FY 25. The greatest increases were seen for Struck by-Caught Between injuries, which rose 31%, to 34 from 26 and Slips, Trips and Falls, which increased 16%, to 51 from 44.

The OSHA Recordable and Lost Time Injury Rates have not changed in FY 2025 to date through January compared to the same period in FY 2024.

ChristianaCare is taking bold steps to combat workplace violence (WPV) and ensure a safer environment for caregivers. While systemwide data indicates increased physical assaults, positive trends in the Culture of Safety data highlight improvements in our workplace aggression composite, reporting, policies and training.
As part of our FY 25 Annual Operating Plan, the health system has expanded existing initiatives and launched new ones to cultivate a safe workplace. Led by the Systemwide Interprofessional Workplace Civility Steer, activities to improve workplace civility include implementing:
• Strategies to improve interprofessional collaboration in care planning or risk mitigation included creating a clinical safety clinical coordinator role to partner with the patient’s care team in specialized care planning and coordination for aggressive or violent patients.
• An EMR Violence Alert to communicate patient or visitor risk.
• An ED aggression risk assessment to identify patient risk.
• A Patient and Visitor Code of Conduct.
• A comprehensive event review process for analysis and clinical management optimization, including developing a Delirium Management Implementation Guide to assist with the management of delirious patients who are violent and/or aggressive.

Workplace Aggression
I report workplace violence events
Problem with patients/visitors being physically or verbally aggressive toward caregivers
There are effective policies and procedures to keep caregivers safe
Caregivers are trained on how to deescalate aggressive behavior
Problem with cargivers being physical, verbally aggressive or threatening toward other caregivers Percent Positive Responsives
Significant positive change Significant negative change
Systemwide Culture of Safety responses improved significantly for the overall score and three other questions. Responses for "In this practice area, there is a problem with patients or visitors being physically and/or verbally aggressive toward caregivers" had a significant negative change.
Additionally, we increased the number of caregivers trained in de-escalation training by 22%; created a new Administrative Provider Discharge Order for “Administrative” use in discharging patients in accordance with the revised Patient /Visitor Disruptive Patient Policy; launched an aggression/violence risk intervention safety plan for the ED; and implemented a revised Behavioral Health Emergency Response process at Wilmington Hospital inclusive of the Emergency Department that’s planned to expand to the other campuses.

ChristianaCare’s Zero Harm Awards recognize hospital patient care units, HomeHealth teams across Delaware, Perioperative Services departments and Ambulatory Practices that have maintained zero cases of preventable harm in one of nine harm categories for at least 12 months. From July 2024 through March 2025, 128 awards were given, including four awards for 11 years (132 months) with zero harm. Since January 2017, 1,351 awards have been earned.
NEWARK CAMPUS
CLABSI
84 months TSU
60 months TNU
24 months 6B, 5B, C6MS, Hospital at Home
12 months 3C, 4B, SCCC, 5N, TMU, CEAD, 2C
CAUTI
120 months BMT
72 months TNU
60 months CEAD
24 months 3C, 5D, 5E, 3A, Hospital at Home
12 months 2C, 4C, TMU, 4D, 6B, MICU, SCCC, NCCU
MRSA
96 months TNU
72 months BMT
60 months CEAD
48 months 6A, C6MS
24 months 7E, 5A, 4E, 5C, 6A, SCCC
12 months 4C, 4D, 2C
C. difficile
72 months TSU
60 months CEAD
36 months C6MS
24 months 4B, Hospital at Home
12 months MICU, 6B
All Falls
12 months TNU, LBR, NICU
Antenatal Steroids
36 months OB Triage
CAMPUS
CLABSI
60 months Rehab (6W)
48 months WCCU
12 months WICU, 5N
CAUTI
132 months 7S
120 months 4N/5W
96 months 6S
72 months WICU, Rehab (6W)
48 months WCCU
MRSA
132 months 7S
48 months 5N, WCCU
36 months 6S
24 months WICU, 4N/5W, 8S
C. difficile
132 months 7S
60 months 7N
48 months WCCU
36 months 4W, 6S
24 months WICU
All Falls
12 months WICU


CECIL COUNTY CAMPUS
CLABSI
36 months PCU
12 months MSU
CAUTI
72 months ICU
36 months SSU, MSU
MRSA
72 months SSU
36 months ICU
C. difficile
48 months CDU
12 months PSU, SSU, ICU, MSU
All Falls
12 months SSU
HOMEHEALTH
CLABSI
72 months NC Team 6
12 months CD Team 1
CAUTI
12 months NC Team 4, NC Team 5
AMBULATORY PRACTICES
Hypertension Admissions
(primary care & cardiology practices)
36 months PC Kirkwood
24 months CHF CHR 1070, PC at Home
12 months PC Northeast, PC Kennett, PC
Riverfront, PC Smyrna, PC Lantana, PC Greenville, PC Whitehall, Cardiology Consultants-NJ
Short - Term Complications of Diabetes Admissions
(primary care & endocrinology)
36 months PC Whitehall
12 months PC Linden Hill, CP Gateway,
PC Jennersville, PC West Grove, PC Kennett, Ctr Special Healthcare Needs, PC Smyrna
PERIOPERATIVE SERVICES
48 months GI Lab-WH, PACU-WH
36 months Christiana Surgery Center
24 months Endoscopy-Union, Interventional Radiology-Union, Wound Center-Union, OR-Union, PACU-CH, Wound Care Center
12 months GI Lab-CH, OR-CH, HVIS, OR-WH


At ChristianaCare, safety is a team effort. Our Zero Hero Awards program honors caregivers who make “good catches” by identifying and correcting safety risks before they cause harm. A good catch could be an unsafe condition that increases risk or a near miss where an issue is resolved before reaching a patient.
Every month, a Zero Hero awardee is selected from the nominees. Clinical Effectiveness leaders in the System Support & Resolution Huddle recognize the awardees for contributing to essential system improvements, and they’re highlighted throughout internal platforms. Monthly winners are eligible for the annual Zero Hero Award, which is presented at the ChristianaCare Way Awards ceremony.
January 2024
Angelina Marie Stevens, RN, 3D Transitional Medical Unit
Good catch: A medication amount was listed in mL instead of mg in the system because the PCA banner requests mg and the iView documentation is in mL.
As a result: Nurses were educated to document the medication volume infused in the nursing task, which then lists the volume in mg in iView. Educational materials were shared to inform nurses.
February 2024
Amanda Williams, NP, 3A
Good catch: Although a patient was given medication once, the Medication Administration Record showed they were given it twice, 10 minutes apart.
As a result: The Information Technology (IT) department continues to investigate with Cerner/Oracle the root cause of this incorrect documentation.
March 2024
Kari Matthews, RN, Cardiovascular Critical Care Complex
Good catch: An intra-aortic balloon pump (IABP) was malfunctioning and measuring a patient’s heart rate in the 180s when it was actually in the 80s, causing hypotension.
As a result: The IABP has since been repaired and adjusted, with help from the Clinical Engineering department and the IABP’s manufacturer.
April 2024 (Tie)
Alexis Martin, RN, Emergency Department
Good catch: Hours after an Emergency Department (ED) patient was sent to an intensive care unit (ICU), the nursing coordinator was told that no beds were available for the patient.
As a result: New processes were developed so that when an ICU is at capacity, other ICUs can take on the overflow patients.

April 2024 (Tie)
Shannan Shelton, Clinical Pharmacy Specialist, Pharmacy
Good catch: Because the PowerChart dosage calculator couldn’t differentiate between elemental and total iron, a patient’s weight-based ferrous sulfate prescription would have been underdosed.
As a result: New language is being developed for weight-based orders relating to the amount of elemental iron that should be prescribed to patients.
May 2024
Judi Smith, Ambulatory Operations Manager
Good catch: Lynx Messenger was deployed in the PMRI Lab in 2023. During the deployment of the remaining practices and services in PMRI, Public Safety tested one of the workstations in the lab to ensure that it had been moved to the correct group and identified that Lynx Messenger was no longer on that desktop. After speaking with the lab caregivers, it was determined that the desktop had been refreshed since the original deployment in 2023. The keyboard was still marked with the panic stickers, but no alert would have been sent if the keys were pressed. The Lab caregivers indicated they were not aware that the new desktop did not have Lynx Messenger on it.
As a result: Ambulatory Workplace Safety & Civility leadership is working with IT and Security to resolve this issue.
June 2024
Maeve Scully, Phlebotomy Supervisor
Good catch: When a phlebotomist was activating the in-vein safety feature of our Smith Medical 23g butterfly, she engaged the safety and attempted to retract the needle. The wings of the butterfly broke.
As a result: The materials team was notified of the defective lot. The team removed all defective lots and sent them back to the warehouse. A safety alert was created and sent out to staff. The recall coordinator filed a complaint with the manufacturer.
July 2024
Vaneisha Neal, RN, Helen F. Graham Cancer Center & Research Institute Infusion Suite
Good catch: A patient was scheduled for outpatient chemotherapy when their son inquired about administering Ruxience, noting the patient had recently received it during an inpatient admission. The staff was initially unaware, but a nurse consulted the clinician and confirmed that the medication should not be given again.
As a result: The Helen F. Graham Cancer Center & Research Institute has created workgroups tasked with revising processes for inpatient and outpatient chemotherapy to improve communication and avoid such issues.
August 2024
Alexis Shields, RN, C4C
Good catch: While retrieving IV Ondansetron from the AcuDose, an RN discovered 10 vials of hydralazine incorrectly placed in pocket 7 alongside ondansetron. The RN adjusted the medication count accordingly. Due to limited space in the designated hydralazine pocket, the misplaced vials were placed in the pharmacy return drawer.
As a result: Pharmacy now mandates a double-check process with two staff signatures for restocking stock-out items from satellite pharmacies. While the exact root cause remains undetermined, the inpatient pharmacy has implemented a policy requiring all ADC stock-outs to undergo a double-check procedure to prevent similar occurrences.

September 2024
Heather Bracken, RN, C4D
Good catch: A patient was discharged to a rehabilitation facility after a 46-day hospital stay.
The Virtual RN paged the discharging provider and bedside RN to clarify the insulin medication orders in the patient’s Discharge Medication Reconciliation. The Virtual RN identified a discrepancy between the patient’s hospital insulin regimen and the discharge medication orders. The hospital regimen had effectively controlled the patient’s blood sugar.
As a result: The provider adjusted the insulin discharge medication orders. The Virtual RN notified the bedside RN that the updated paperwork, including the Discharge Workflow, Meducation and Extended Care Facility Medication Reconciliation, had been printed. In collaboration with key leaders, an intensive review will be conducted. ECRI/ISMP was engaged to analyze and enhance medication history and reconciliation processes.
October 2024
Elizabeth Redman, Registered Dietitian
Good catch: A patient with a documented shellfish allergy was prescribed a specific type of lipid, SMOF. Fortunately, this error was caught before the patient received the lipid.
As a result: The pharmacy clinical team contacted the lipid manufacturer, who confirmed that the risk of an allergic reaction was low. This case will be reported, likely leading to a revision of the lipid Care Management Guidelines, as the current guidelines do not address this issue.
November 2024
Mai Lam, Resident
Good catch: Vocera messages were not reaching a provider’s phone or the phones of several other providers. Vocera pages from nursing staff and other providers regarding patient care, as well as MICU alerts from the ED, were not received.
As a result: The issue was escalated, and it was determined that the network had experienced unplanned downtime. IT identified the root cause. The matter was further escalated to the appropriate IT leadership for resolution.
2024
Ashley Barron, Respiratory Therapist
Good catch: A patient required intubation. The Respiratory Care team retrieved a sealed Medline airway box (Lot #24EDA505) from the Rapid Response Team cart. Upon inspection, the team discovered both the 7.5 and 8.0 endotracheal tubes were missing.
As a result: A Value Analysis analyst met with the Medline vendor representative, the respiratory care manager, the value analysis manager and the materials supervisor to assess other airway boxes in the materials supply. They confirmed that all other boxes were sealed and fully stocked. Previously, boxes had been opened for storage due to space constraints in the code carts. Next steps include meeting with senior leadership to evaluate all code carts for proper stocking and re-locking procedures.

Engage all caregivers to serve our patients with love and excellence, providing an ideal experience across the continuum of care.

“Every encounter I have with our caregivers reminds me that patients are truly at the heart of everything we do.
I see it daily — whether it's at the front of the hospital or at the bedside —
caregivers take the time to connect with patients, to listen closely, and to ensure they’re understood. When I watch them asking patients to repeat instructions back, I know it’s not just about accuracy; it’s about making patients feel seen, heard, and genuinely cared for.”
LeRoi S. Hicks, M.D., MPH, FACP. Campus President - Wilmington


In FY 25, ChristianaCare reimagined our Patient Experience (PX) framework with the launch of THE WAY We Care unifying approach to putting people at the heart of every interaction.
Rooted in the health system’s values of love and excellence, new service standards were created, introducing a memorable acronym THE WAY (Take the time, Help with heart, Explain what to expect, Welcome warmly, Accept responsibility, You make a difference) that reflects actionable and observable behaviors. Caregivers across the system designed the service standards.
THE WAY We Care aligns ChristianaCare’s mission and values. It connects to initiatives like THE WAY We Lead and THE WAY We Thrive by helping teams support each other as caregivers and deliver exceptional, personalized care.
The new brand was unveiled at a systemwide Leader Showcase attended by more than 400 caregivers representing 250 departments, 150 nurse leaders, 50 Medical Staff leaders and 4,000 years of collective experience.
Central to the new framework are PX Champions, caregivers who serve as role models and communicators within their departments, ensuring the values of patient-centered care are integrated into daily practices. In January, a PX Champion showcase event presented the framework’s new service standards, which the champions developed.
Fully launched for all caregivers in April, THE WAY underscores our systemwide commitment to consistently elevating every experience for every person, every time.


Every experience. Every time.

The HCAHPS survey offers critical insight into how patients perceive our care and their experience with us. It measures across eight domains: care transitions, cleanliness, communication about medication, communication with doctors, communication with nurses, discharge information, overall rating and would recommend.
Our Patient Experience Improvement team drives efforts to improve patient experience through several subcommittees: Doctor Communication, Nursing Communication, Discharge and Care Transitions, Teach-back, Caregiver Engagement and Service Standards, and Clean and Restful Environment.

In FY 23, ChristianaCare's Nursing team implemented an evidence-based practice bundle across all caregiver roles to enhance patient safety and experience (PX) after ambulatory metrics were well below the overall targets for PX.
Initially launched in the Women and Children’s (W&C) and cancer service lines, the bundle improved NRC Health survey metrics for Courtesy and Respect, Teach-back Would Recommend. Comparison of FY 23 and FY 24 qualitative data shows a decrease in the percentage of negative comments in three thematic areas for W&C and four thematic areas for the cancer service line. Team collaboration and structured workflows proved essential, offering a scalable model for improving ambulatory care nationwide.
Seven domains improved FY 25 to date compared to the same period in FY 24, with the greatest improvement in Cleanliness. Discharge Information, which remained flat, and Care Transitions exceeded the CMS 50th percentile benchmark.

The Doctor Communication subcommittee made strides in improving provider-patient interaction. By analyzing communication barriers, developing a priority matrix and sharing a provider communication board, the team focused on empathy and the Teach-back method. A new road map and toolkit reinforced the commitment to clear, compassionate care. These efforts led to improvements across doctor communication scores.
The Nursing Communication subcommittee drove improvements in patient interactions by revising standards of practice, securing dedicated time for nurse leader rounding and updating bedside shift report procedures. These changes strengthened patient trust and satisfaction. Nurse communication scores improved measurably.


Explained Things Understandably


By focusing on empathy and Teach-back, all three doctor communication scores improved. “Explained things understandably” exceeds the HCAHPS benchmark.
After implementing new standards for Bedside Shift Report, nurse communication scores improved. Nurses “explained things understandably” improved to 74.5% from 73.1% and exceeds the national benchmark.

The Discharge and Care Transitions subcommittee focused on refining posthospitalization care. The team supported more seamless transitions by improving patient instructions, piloting Twistle for post-discharge communication and optimizing how patients interpret survey questions. These efforts increased patient understanding scores.
The Teach-back subcommittee prioritized improving how providers and nurses communicate medication information. Training expanded to inpatient nurses, hospitalists, psychiatry staff and resident groups, reinforcing the use of Teach-back for clarity. The integration of Meducation enhanced discharge medication instructions, resulting in measurable gains in patient comprehension and significantly improved HCAHPS scores in communication about medications.




Revision of discharge instructions and other efforts contributed to a 4% increase in questions related to patient understanding; both exceed the benchmark.
Jul-23Aug-23Sep-23Oct-23Nov-23Dec-23Jan-24Feb-24Mar-24Apr-24May-24Jun-24Jul-24Aug-24Sep-24Oct-24Nov-24Dec-2425-Jan25-Feb25-Mar
Scores related to medication communication decreased slightly in FY 25 but remain at the CMS 50th percentile benchmark.

The Clean and Restful Environment subcommittee focused on room cleanliness and nighttime quietness. Innovations included pyramid cards with quiet slogans, an environmental services reward program and a new cubicle curtain initiative. Despite staffing challenges, cleanliness scores significantly improved statistically, reinforcing our commitment to patient comfort and healing.
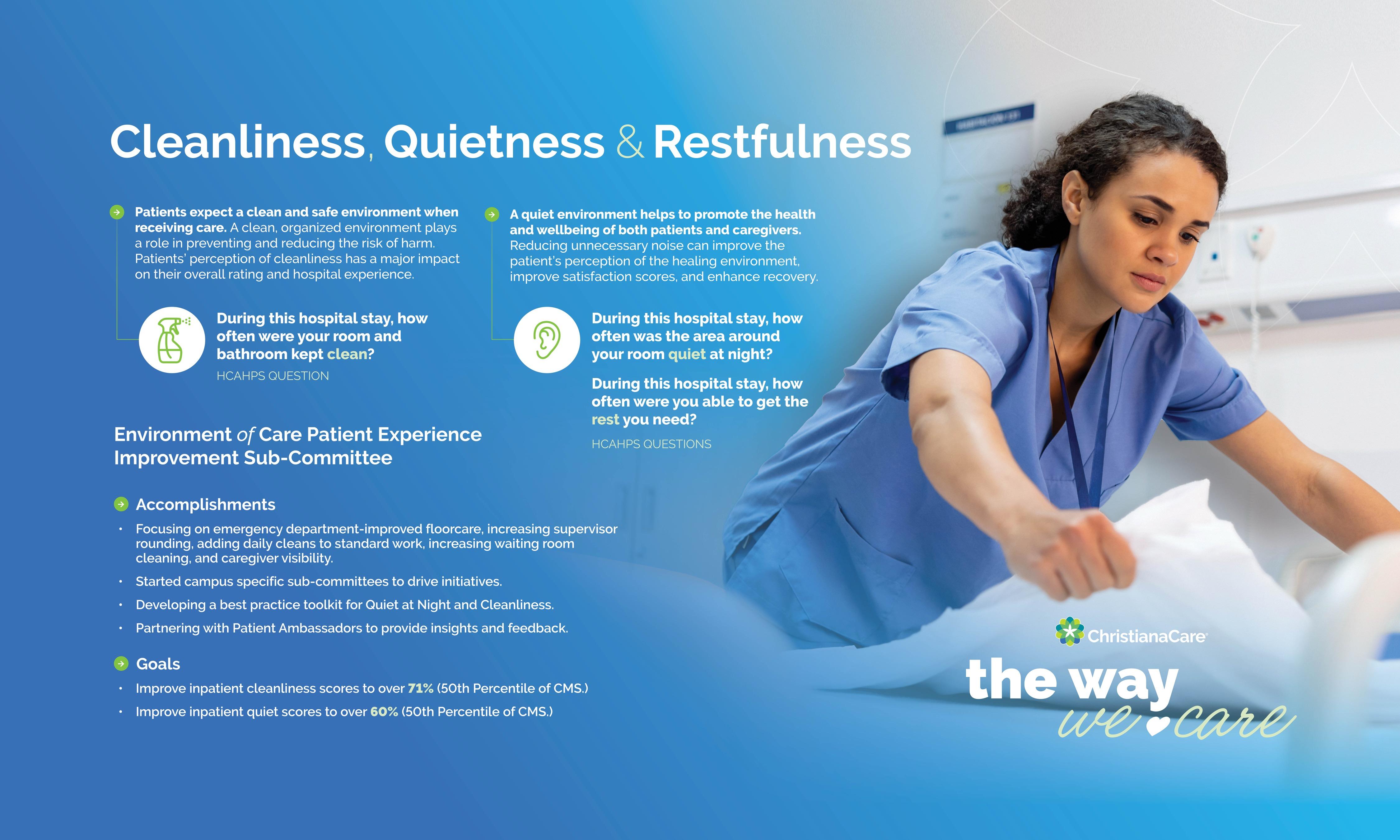
Clean and Restful Environment




Drive health outcomes as a national leader in clinical excellence through continuous improvement in effectiveness, timeliness and efficiency of care provision.

“In health care, we always hope to make an impact, even when we’re not on the front lines with patients. I’m so grateful we have this Quality space and support from the health system to create Quality and Safety drives and initiatives that become a standard for how care is delivered and how we improve patient outcomes.”
Jennifer Brettler, DO, FACP, CHCQM-PHYADV


ChristianaCare made significant progress in the 2025 year-todate Vizient Quality and Accountability Scorecard, improving from 83rd (2020) out of 100 hospitals to 50th out of 118.
The scorecard is an annual performance report measuring the quality of inpatient care across six domains: Mortality, Efficiency (length of stay and cost), Safety, Effectiveness (readmissions and excess hospital days), and Patient-centeredness and Equity. Our improved ranking reflects the health system’s commitment to delivering high-quality care that our neighbors value. It also brings us closer to our goal, set in 2020, to rank among the top 25 academic medical centers by the end of 2025.
ChristianaCare’s Union Hospital, which only recently began participating in Vizient, is embarking on its journey and assessing opportunities compared to its peer community hospitals.


ChristianaCare's ranking against our academic medical center peers improved to 50 out of 118 hospitals from 83 out of 100 hospitals.

In Vizient’s report for the first half of 2025 (July-December 2024), ChristianaCare exceeded the peer median for the overall score and in two key areas: mortality and safety. The safety domain, which includes HAIs and PSIs, improved to a rank of 9 from 72 in 2020 due to efforts led by the Zero Harm Council (see page 43). The mortality domain tracks risk-adjusted mortality by service line and improved to a rank of 9 from a low of 72 in 2022.
Our greatest opportunities for improvement compared to peer performance is patient-centeredness and effectiveness. The patient experience rebranding and extensive efforts of the Patient Experience subcommittees are having a positive impact on HCAHPS scoring and will drive improved ranking (see page 37).
Overall Score 54.8%
Rank 50

Our 2025 year-to-date domain weighted scores improved in two dimensions — mortality and safety — and rankings now exceed the 50th percentile. Our greatest opportunities are effectiveness (readmissions/excess days) and patient-centeredness.

One of ChristianaCare’s most notable achievements is our ranking of 9 in the Mortality domain. After receiving a ranking of 72 in 2022, with a mortality index of 0.99, an interdisciplinary team led by Clinical Documentation convened to improve our outcomes.
Efforts included conducting a standardized review of all mortality cases, ensuring clinical documentation integrity to assure appropriate and complete coding for accurate risk adjustment that reflects the true acuity of our patients and establishing a process to identify trends in mortality with direct feedback to service lines for possible care delivery opportunities.
Clinical improvement in populations such as sepsis led to a decrease in mortality rates since 2022. During the same period, risk-adjusted expected rates increased, resulting in a decrease in the mortality index.
Mortality Index

The observed to riskadjusted expected mortality index decreased more than 41% since 2022, to 0.58 from 0.99.
Jan-22Mar-22May-22Jul-22Sep-22Nov-22Jan-23Mar-23May-23Jul-23Sep-23Nov-23Jan-24Mar-24May-24Jul-24Sep-24Nov-24


The inpatient mortality rate has improved 30% since 2022, to 1.5% from 2.1%. During the same period, the expected mortality increased 19%. Observed mortality is significantly below expected (p < 0.01).
Jan-22Mar-22May-22Jul-22Sep-22Nov-22Jan-23Mar-23May-23Jul-23Sep-23Nov-23Jan-24Mar-24May-24Jul-24Sep-24Nov-24

The CMS Overall Hospital Quality Star Rating evaluates hospital performance across five key domains: mortality, safety of care, readmission, patient experience and timely and effective care. ChristianaCare’s Christiana and Wilmington hospitals have maintained a strong 4-star rating, while Union Hospital holds a 3-star rating.
CMS also operates three value-based (pay-for-performance) programs the Hospital Readmission Reduction Program (HRRP), which reduces payments for excessive readmissions; the Hospital-Acquired Conditions Reduction (HAC) program, which penalizes hospitals with high rates of preventable infections and safety events; and Value-Based Purchasing (VBP), which rewards hospitals for quality and efficiency. (Maryland has its own program and is exempt from these three see page 47.)
This year, ChristianaCare avoided an HRRP penalty and remained penaltyfree under HAC for the fifth consecutive year. A minor (<1%) penalty was assessed under VBP.
In FY 25, ChristianaCare launched three key initiatives across all three campuses to improve care coordination and reduce readmissions:
• Meds to Beds (December 2024) delivers prescriptions bedside before discharge more than 1,700 patients have received medication this way since implementation.
• Simplified Discharge Instructions (November 2024 for hospitalists’ patients) make discharge guidance clearer for caregivers and patients.
• Twistle Post-Discharge Outreach (January 2025 in five patient units) uses text-based follow-ups to identify and address patient concerns.




ChristianaCare's Delaware hospitals' readmission rates were better than expected across all five populations.
ChristianaCare's performance was better than the national mean in three of the six measures. The very low scores for the PSI 90 composite and C.difficile drove the overall score well below the threshold for a penalty.

In FY 24, ChristianaCare’s Union Hospital on the Cecil County campus incurred a penalty from the Maryland Health Services Cost Review Commission (HSCRC) due to excess readmissions in calendar year 2023. An additional penalty was issued under the Maryland Hospital-acquired Conditions (MHAC) program for a high incidence of preventable complications. In response, the hospital implemented measures that reduced readmissions and complications in calendar year 2024, positioning it for a potential FY 25 reward.
Key readmission improvements included forming a campus workgroup to identify opportunities and solutions and launching the Acute Care Connector program to address challenges with high-risk patients e.g. scheduling follow-ups before discharge, coordinating transportation, initiating a Meds-to-Beds program (see page 45) and deploying at-home services through primary care nurse practitioners. The workgroup also leveraged community resources, such as mobile health vans, to support underserved areas.
To improve the MHAC score, the campus aligned case review with the system, increased provider engagement, educated staff on the program and added Union Hospital to the clinical documentation integrity dashboard to track campuswide queries.
As a result, Union Hospital reduced its in-state readmission rate below target in calendar year 2024 and improved its MHAC score to 85%. For the first time in years, the hospital is positioned to earn a financial reward rather than a penalty.


Union Hospital reduced in-state readmissions to 10.56% in 2024 from 11.07% in 2023 and is below target for the performance period, qualifying for a financial reward instead of a penalty under HSCRC.

By reducing potentially preventable complications in 2024, Union Hospital increased the HAC score to 80% from 35%, exceeding the goal for the performance period and qualifying for a financial reward.

Sepsis continues to be the leading cause of death in U.S. hospitals. Early recognition and treatment are paramount to decrease mortality.
In FY 25, ChristianaCare continued our “Get Ahead of Sepsis” initiative, educating inpatient clinicians on recognizing, documenting and treating patients with suspected sepsis. Our sepsis capture rates have remained strong and exceed those of other top academic medical centers.
Additionally, a multidisciplinary team, including leadership from Clinical Documentation Integrity and Health Information Management Services, was established in FY 25 to ensure clinical validation of sepsis cases.
The Severe Sepsis and Septic Shock Early Management Bundle, or SEP-1, is a complex CMS composite quality measure that promotes severe sepsis and septic shock treatment guidelines. The percent of patients with sepsis meeting all aspects of the SEP-1 increased 21%, to 44.7% from 36.8%



The percent of adult inpatients appropriately diagnosed with sepsis doubled to 5.1% in 2024 Q4 from 2.4% in 2022 Q1, and now exceeds the capture rate of topperforming academic medical centers.

In FY 25, increased sepsis education and chart review feedback were provided to ED caregivers to help promote early identification and standardize sepsis treatment.
A sepsis alert pilot was also implemented at our Newark and Wilmington campuses’ EDs. As a result, our Delaware campuses’ SEP-1 compliance increased by 8% for calendar year 2024.


“Safety doesn’t happen by accident. It’s the result of thoughtful work behind the scenes. Every improvement is about protecting people before harm has a chance to happen. To me, safety is a shared responsibility, a mindset we all carry, because even the smallest miss can change someone’s life.”
Juliana Rahmer , AGACNP-BC, FNP-BC, CHCQM, CEN, Sepsis program coordinator

Sepsis mortality decreased 60% in the three-year period from 2022 Q1 to 2024 Q4, to 8.9% from 22.0%. During the same period, the mortality observed to riskadjusted expected index improved to 0.7 from 1.5.

In 2023, ChristianaCare was performing below the 10th percentile in malnutrition capture, negatively impacting patient care, reimbursement and value-based quality and safety ratings. Given the many contributing factors, a systemwide team recognized the need for a systemwide intervention, starting with improved screening.
To address this, the team implemented a validated Malnutrition Screening Tool (MST) across inpatient units as a required Nursing task at admission to identify at-risk patients. As of February 2024, patients who screened positive on the MST automatically triggered a referral in PowerChart to a registered dietitian for further evaluation.
Along with implementing the MST, the team developed a SmartZone in Cerner to automatically add malnutrition to the Diagnosis List for caregivers to select when malnutrition is identified, ensuring accurate documentation for coding.
As a result of this initiative, malnutrition capture rates increased, surpassing the 50th percentile among our academic medical center cohort. Malnutrition Detection


Apr-23May-23Jun-23Jul-23Aug-23Sep-23Oct-23Nov-23Dec-23Jan-24Feb-24Mar-24Apr-24May-24Jun-24Jul-24Aug-24Sep-24Oct-24Nov-24
The percent of adult inpatients appropriately coded with malnutrition increased to 11.4% from 5.5%, impacting almost 2,000 patients. Our ranking of appropriate capture among our academic medical center peers improved from 7 to 55.

Retinal eye exams are critical for detecting diabetic retinopathy, a leading cause of blindness. For years, compliance with retinal eye exams, one of our Standards of Care domains for diabetes, was relatively low across ChristianaCare ambulatory practices. Providers had limited ability to perform tests in offices, faced challenges obtaining documentation from outside ophthalmologists and struggled with patients not following up on recommended testing.
In response, several practices adopted IRIS, a software screening tool that integrates exams into routine visits. Even with IRIS, retinal screening rates were at 34% in June 2024, short of the 45% target.
Based on continued low performance, primary care leadership took strategic actions to improve rates, including reassigning cameras to higher-utilization sites and evaluating usage every six months in a "use it or lose it" approach; hosting a usage practice-wide contest to encourage participation and prioritizing retinal screenings by scheduling them on ancillary schedules, ensuring efficient resource use. Additionally, IRIS reports were integrated into EPIC, streamlining documentation and tracking.
These efforts paid off, with compliance rising to levels surpassing the target.



Use of IRIS cameras has increased significantly since inception, reaching almost 2,000 screenings in 2024. From June 2024 to January 2025, practices with IRIS cameras increased compliance 13%, to 46.9% from 41.5%, exceeding the 45% target.

Streamline the flow of patients across our health care system through improved organizational efficiencies, elimination of waste and coordination of transitions of care.

My why
“Flow is essential to delivering safe, high-quality care. When patients move smoothly through
our system,
it means
timely treatment, less stress and better outcomes.
For caregivers, it means fewer barriers and more time to focus on what matters caring for our neighbors. Quality and safety live in these everyday moments. I’m driven to improve flow because it creates a safer and more efficient and compassionate experience for everyone who walks through our doors.”
Valerie Dechant , MD, MBA, FACP, chief medical officer, Newark Campus


Observation care involves treatment, assessment and reassessment to determine whether a patient can be safely discharged from the hospital. Typically, OBS patients stay in the hospital for less than 48 hours. In FY 25, we set a goal to reduce OBS LOS by at least 3% on at least two of our three campuses. Key initiatives include the following for each campus:
• Wilmington launched a cohort pilot on 4West to enhance patient management and streamline OBS care. It also implemented provider workload adjustments to improve efficiency and patient throughput.
• Newark’s Medical Observation Units (MOUs) developed a dizziness pathway, implemented concurrent utilization management reviews for ED boarders and modified the evening huddle script to improve communication. The campus also improved OBS cohorting in the Cardiac Short Stay Unit (CSSU) to enhance patient monitoring and care coordination. It introduced multidisciplinary rounds and assigned a dedicated case manager to oversee patient transitions. And the Newark campus also launched a Services and Diagnostics Escalation Process.
• Cecil County optimized the cohorting of OBS patients in the Clinical Decision Unit to improve efficiency and patient outcomes. It implemented a 2 a.m. huddle to enhance nighttime communication and facilitate decision making.
As of December 2024, our Wilmington and Newark campuses successfully met the target for OBS LOS.



Our Newark and Wilmington campuses have reduced length of stay for observation patients by at least 3%, meeting the AOP target.

ChristianaCare’s focus on efficiency and patient-centered care has improved hospital LOS and care transitions over the past year.
The LOS Index for post-acute placement decreased in FY 25, and overall hospital LOS reduced by roughly half a day. We saw the most dramatic improvement in discharges to skilled nursing facilities (SNFs).
These gains result from enhanced multidisciplinary rounds (MDRs), stronger partnerships with post-acute providers and improved care coordination workflows. A refined complex discharge management process and expanded Hospital Care at Home services further accelerated transitions, ensuring timely discharges. Additionally, optimized diagnostic turnaround times particularly for echocardiograms and MRIs contributed to reduced LOS, especially for OBS patients.


Although the LOS Index exceeded targets this winter due to high census, all three campuses have met the AOP goal for the year-todate improvement.

The Length of Stay observed to risk-adjusted expected LOS Index for post-acute placement decreased an average of 25% in FY 25 to-date compared to FY 24. Hospital length of stay decreased by almost 1/2 day, with the greatest improvement in discharges to skilled nursing facilities, which dropped 6%. In total, 4,217 patient days have been saved.

Optimizing service and diagnostic TAT is a key priority in delivering timely and effective patient care. In FY 25, ChristianaCare implemented a three-tiered time standard for EDs, OBS units and inpatient settings, ensuring faster diagnostics and streamlined care.
An OBS TAT pilot launched in December 2024 focuses on critical diagnostics TATs, such as MRI and echocardiograms (ECHO). In late summer and early fall, ECHO turnaround time significantly improved, driven by optimized staffing models and enhanced recruitment and training partnerships. Additionally, a new escalation process for diagnostic delays ensures real-time interventions, further enhancing efficiency in patient care delivery.
ChristianaCare also saw notable improvements in operational turnaround across all three campuses. In FY 25, Inpatient Patient Escort TAT improved by 4%, with the most significant gains in reducing the time from Request to Scheduled. Environmental Services also saw a 6% improvement in cleaning TAT for inpatient and observation rooms following discharge, including a 9% decrease in the time from Scheduled to Start.
Echocardiogram Turnaround Time



The total TAT for Newark Hospital OBS patients’ echocardiograms decreased 30%
FY 25, to 19.7 average hours from 28.4 hours, and has been better than the 19hour target since December 2024. The biggest improvement was in the time from order to exam start, which improved by eight hours.

Multidisciplinary rounds are the backbone of coordinated inpatient care, ensuring that care teams align on patient needs, barriers and discharge processes. The year saw enhancements to MDRs that included standardizing Nursing report sheets to streamline communication, modifying rounding start times to improve engagement and efficiency and refining our escalation process for addressing delays in real-time.
As a result, in FY 25, ChristianaCare saw strong adherence to structured MDRs. Most teams effectively escalated barriers to discharge, and a significant portion of those issues received follow-up and resolution.



In FY 25, ChristianaCare achieved a 91% adherence to structured MDRs. Overall, 84% of teams successfully escalated barriers to discharge, with a 40% follow-up resolution on escalated issues.

In health care, complex care refers to patients with intensive medical, behavioral and social needs requiring coordinated, multidisciplinary care. Complex care patients often experience prolonged hospitalizations due to discharge barriers such as lack of insurance, guardianship delays, psychiatric issues or limited placement options. Challenges also include frequent readmissions, repatriation needs or uncooperative legal guardians.
Across the health system, delays in identifying complex care patients, inconsistent cohorting and variable rounding contribute to excess resource use and staff strain.
ChristianaCare also saw an opportunity to refine the definition and standard management of complex and prolonged acute hospitalizations.
We are redesigning patient care coordination across the continuum acute, ambulatory, population health, virtual care, home health, and community-based services. Expected outcomes include a standard definition for complex cases, reduced LOS and cost and improved efficiency for providers, nurses and case managers.
To address these challenges, in FY 25, ChristianaCare made some changes to flow management for complex care patients, including adding a PowerChart flag to highlight patients medically ready for discharge and establishing a bimonthly review of complex cases on our Newark Campus.
% of Inpatient Discharges
Long Stay Patient Discharges
Percent of Discharges with LOS 15 Days or More



Week Ending
From the end of October 2024 through March 2025, more than 2,200 patients — approximately 9% of all adult discharges across the three campuses — had a length of stay of 15 days or more.
The median length of stay for these patients was about 20 days; the maximum was 848 days.

Leading the nation in population health outcomes by ensuring every person receives the best care in the right setting while reducing the total cost of care by 5%.

“Community health impact is at the heart of how we care at ChristianaCare. Basic social needs – like housing, food and transportation – profoundly impact people’s health and wellbeing and the communities in which they live.
That’s why we work to connect people with resources and remove obstacles to care. I do this work because all communities deserve fairness, dignity and lasting change. Advancing improvements in health outcomes means working every day to build healthier communities for everyone.”
Jacqueline Ortiz, M.Phil, chief community health impact officer


Delivering high-quality health care for everyone involves more than knowing a patient’s symptoms; it includes understanding their lived experiences. In FY 25, ChristianaCare’s Office of Community Health Impact led the expansion of our SDoH screening, which asks patients about food insecurity, interpersonal safety, housing insecurity, transportation insecurity and utilities. This approach helps to advance improvements in outcomes for everyone across our campuses and ambulatory care practices.
Patients in acute care settings who indicate social challenges receive a complete health needs assessment from our Acute Care Connectors. Then, connectors provide referrals to Unite Delaware, ensuring a closed-loop follow-up when services are received. The model expanded in FY 25 to include acute psychiatric units.
Social Needs Practices with High Positive Screen Rate

Seven practices, including four Complex Care practices and three Maryland practices, had more than 30% of patients with positive SDOH screens. Overall, the top opportunities were Financial Insecurity, Food Insecurity and Medical Literacy.

In response HHS’s SOGI Action Plan and Joint Commission’s guidelines on demographic data collection, in FY 24 ChristianaCare launched the “We Ask Because We Care” campaign to improve the collection of patient-reported SOGI and REL information.
In FY 24 Community Health Impact launched the “We Ask Because We Care” campaign to improve the collection of patient-reported SOGI and race, ethnicity and language (REL) data. Accurate demographic data is critical to delivering high-quality care to every individual, helping to ensure that care is respectful and consistent.
Since launching, the campaign has maintained a steady collection rate, marking an important step towards consistent and valid demographic data for all patients. ChristianaCare has also prioritized caregiver education, with more than 1,800 caregivers completing training to support respectful, informed interactions.
The initiative will expand into our Emergency Departments, primary care sites and surgical centers, with posters, wall clings and digital displays reinforcing patient awareness.





The End Disparities SAWs are dedicated to eliminating disparities in access, experience, care delivery and health outcomes. Four strategic aspirations guide the group’s work, each with a five-year goal and targeted interventions for improving health outcomes in:
Aiming to reduce disparities in latestage diagnosis of breast cancer by 10%, efforts including deploying community health workers and launching a Cancer IQ/risk assessment pilot. Funding from the Cancer Consortium supports outreach to women who have a higher risk for breast cancer and reside in Wilmington’s Riverside neighborhood.
Targeting a goal of increasing the rate of hypertension control to 70% for all patients served in the Complex Care Primary Care practices, the SAW has selected an intervention to provide individualized support for 100 patients in partnership with Story Health. Advanced data analytics are underway in partnership with Health Catalyst and NCQA. A home-based blood pressure monitoring program has also been implemented to improve outcomes for all patients.
A cultural navigation pilot has increased the number of patients with limited English proficiency who are able to have bariatric surgery. A partnership with the University of Pennsylvania’s Center for Surgical Health is also underway. It will deploy personal patient navigators to support improved surgical outcomes for patients undergoing joint replacement surgery.
Seeking a 20% reduction in the disparity in preeclampsia at 37 weeks, the SAW developed interventions to increase connection to prenatal care, visits to the Early Pregnancy Center and adherence to low-dose aspirin therapy during pregnancy.


Bariatric surgery is complex, multi-step process requiring consistent and accessible patient information and education. In 2021, Spanish-speaking patients with limited English proficiency were under-represented among patients undergoing bariatric surgery, comprising just 7.8% of patients compared to 10.5% of Delaware’s overall population (according to the Delaware Census).
At the time, the Bariatric Surgery team reviewed its program and identified the lack of formal protocols for Spanish-speaking patients. To bridge the gap, the program implemented targeted interventions, including collaboration with the Community Health Impact team, expansion of interpreter services and development of Spanish-language patient education. These efforts expanded in 2024 to bilingual navigation of patients through the pre-surgical and surgical process with the creation of a group of interpreternavigators to support Spanish speaking patients.
By December 2024, Hispanic-Latino patient representation grew to surpass the team’s goal.
Bariatric Surgery Program: Percent Spanish-speaking



The percentage of Spanish-speaking patients in the Bariatric Surgery program increased 59% in the three-year post-intervention period (2021-2023), to 12.5% from 7.8%. The improvement continued in 2024, reaching 13.6% and exceeding the Delaware 2020 Census percentage of 10.5%.

Leading the nation in population health
outcomes by ensuring every person receives the best care in the right setting while reducing the total cost of care by 5%.

“As a primary care physician, one of the things I love about our work is the focus on prevention. We’re not just reacting; we’re proactively helping patients stay well.
Population health allows us to rethink how we care for people, not just when they’re sick, but long before. Population health is about prevention, connection and truly meeting people where they are. For example, when we invest in wellness and maternity care, we’re investing in the long-term health of our communities. And when our patients feel supported, when they know someone is walking alongside them, that’s when real change happens.”
Rose Kakoza , M.D., MPH, senior clinical network director for Population Health and medical director for ChristianaCare’s Delaware Medicaid Quality Partners


Since 2016, eBrightHealth ACO has been at the forefront of valuebased care, bringing together a network of health care providers across Delaware and the surrounding region to improve care coordination and lower costs. The physician-led ChristianaCare Clinical Alliance supports the ACO, and the program uses CareVio, our subsidiary organization, for case management.
eBrightHealth ACO coordinates care for behavioral, social and chronic health conditions, helping to reduce emergency visits and hospitalizations and promote patient well-being.
For nearly 10 years, eBrightHealth ACO has been a dedicated participant in Medicare’s Shared Savings Program. This means when the ACO succeeds in delivering high-quality care and spending health care dollars more wisely, it may be eligible to share in the savings it achieves for the Medicare program.
Today, 31,600 beneficiaries benefit from the ACO’s patient-centered approach, with 19,600 people attributed to ChristianaCare. Since 2016, eBrightHealth ACO has seen seven consecutive years of cost savings and three of sharing savings.


Since 2016, eBrightHealth ACO beneficiaries had a 41% increase in annual wellness visits and a 13% improvement in primary care physician visits. The average Quality score was 89%.

ChristianaCare’s Delaware Medicaid Quality Partners ACO has set the standard for innovative, high-quality care at lower cost for Delaware’s Medicaid population.
According to the most recent data, the ACO reduced health care spending by $6.2 million in 2023 while improving care for nearly 30,000 Medicaid beneficiaries in Delaware, including approximately 8,000 children.
With a network of more than 1,900 primary and specialty care clinicians, the ACO ensures that patients receive essential screenings and treatments.
Since the COVID-19 pandemic, the ACO has seen a shift in its patient population: lower-cost, lower-acuity members have exited Medicaid, leaving behind a sicker, higher-risk population that requires more intensive care.
Primarily located in Wilmington, these high-risk patients represent 20% of beneficiaries but account for 80% of costs, making strategic care management essential for primary care providers. In FY 25, ChristianaCare’s Clinical Alliance is exploring how we shift resources and workflow to better support these members’ needs.



Since our Medicaid ACO launched in 2021, maintenance of healthy blood sugar levels for patients with diabetes improved by 7%, asthma medication management improved by 21% for patients aged 12-18 years, and by 15% for patients aged 5-11 years; breast cancer screening increased 4%.


2024 President’s Award
Scrub-a-Dub-Dub, Line and the Hub: An Interdisciplinary Approach to Reducing CLABSI
The Transitional Medical Unit (TMU) CLABSI Comprehensive Unit-based Safety Program (CUSP) team detected an increase in CLABSI rates from July through December 2023, totaling three CLABSIs. During the first half of FY 24, the team recognized an opportunity to increase the quality and quantity of CLABSI perfect care bundle rounding. They developed a weekly rounding strategy that included caregiver feedback and education. CLABSI rounding increased from 53 to 291 rounds within six months and perfect care bundle compliance improved from 49% to 78%. From January to August 2024, the TMU had 0 CLABSI, for an estimated cost savings of $138,000.
Value & People's Choice Award
How Many Urines Had We Been Culturing? Way Too Many….
A multidisciplinary team including caregivers from the Departments of Pathology & Laboratory Medicine, Emergency Medicine and Medicine, as well as Infection Prevention, The Institute for Research on Equity and Community Health, Pharmacy Services, Information Services and Nursing Quality and Safety collaborated to implement new evidence-based reflex criteria for urine cultures and make necessary changes to the lab’s urinalysis standard operating procedures. The criteria change had statistically significant results, including a 37% decrease in the urinalyses that reflexed to culture, a 26% increase in the culture-positive rate, and a cost savings of $65,000.
Transformation Award
Suspect Sepsis, Say Sepsis. A Systemwide Approach to Improving Sepsis
Clinical Documentation Integrity recognized that ChristianaCare was under-capturing sepsis Diagnosis-Related Groups compared to other academic medical centers nationwide and had a higher mortality index than the benchmark hospitals. A multidisciplinary team implemented systemwide criteria to help clinicians identify sepsis and revised screening and clinical decision support tools to help guide clinicians in the workup and treatment for sepsis. Sepsis capture improved to the 70th percentile among academic medical centers from the 6th, the mortality index improved 36% and revenue increased by $11 million.
Strengthen the Core: Safety Gold Award
ALL for NONE: NICU CLABSI Prevention Perfect Care Bundle
CLABSIs are a major concern in Neonatal Intensive Care Units, leading to increased morbidity, mortality and health care costs. The NICU identified CLABSI prevention best practices and collaborated with Infection Prevention to standardize workflows and reduce variability via a “ring of things” bedside compilation of checklists and job aids targeting all elements of line insertion and maintenance. Incidence of CLABSI decreased 60% in FY 24, with an estimated savings of 57 patient days and more than $150,000.

Strengthen the Core: Safety Silver Award
Decannulate and Defend: Tracheostomy Rounding to Optimize Outcomes
From 2021 to 2023, 8.1% of tracheostomy patients on our Newark campus experienced unplanned decannulation, with 84% of cases associated with documented patient agitation/confusion. In March 2024, a tracheostomy rounding team of Respiratory Therapy, Speech Therapy and Nursing began rounding weekly on tracheostomy tube patients to assess patient readiness for a planned decannulation, discuss interventions for patient safety and provide education on tracheostomy care and emergency situations. The rounding team decreased unplanned decannulations by 59%. The unplanned decannulation rate per 1,000 tracheostomy days decreased from 4.64 to 2.85.
Strengthen the Core: Safety Bronze Award
Be Aware of Perfect Care
In early 2023, ChristianaCare saw a rise in CLABSI and CAUTI, prompting Infection Prevention to act. The team implemented rou nding on patient care units aligned with Nursing’s Perfect Care Bundles. The rounds incorporated evidence-based best practices, indications for central lines or Foleys and real-time education for care teams. Use of Cipher for rounds increased transparency and allowed validation of results against Nursing perfect care rounds. From August 2023 through May 2024, more than 1,400 rounds were completed. CAUTI rates decreased 31% and CLABSI rates declined 29%.
Strengthen the Core: Safety Honorable Mention Award
Deep Dive to Increase Infusion Pump Compliance with Dose Error Reduction Systems
Smart infusion pumps with dose error reduction systems (DERS) combine computer technology and drug libraries to limit the potential for dosing errors. In June 2022, DERS compliance was 91.7% versus best practice of 95% or better. An interdisciplinary team identified patient care units or departments with low compliance rates. They also investigated the barriers to employing DERS. To remove barriers and improve DERS compliance, the team’s interventions included adding medications, modifying profiles, educating caregivers, simplifying reporting of issues through R2 and increasing data transparency. DERS compliance improved to 93.5% by June 2024, translating to more than 25,800 additional infusions run on DERS annually and potentially averting 1548 IV infusion therapy administration errors.
Strengthen the Core: Quality Gold Award
Stop the Bleeding! A Multidisciplinary Planning Approach for Severe GI Hemorrhage
Root cause analysis of patients with severe gastrointestinal (GI) hemorrhage revealed delays in definitive care due to fragmented communication among multiple specialties. To address this, a Gastrointestinal Response Team (GIRT) alert system was implemented to facilitate real-time coordination among emergency room clinicians, gastroenterology, vascular interventional radiology, surgery, and intensivists. The goal was to enhance timely decision-making and establish clear plans of care for GI bleed patients. Between March and July 2024, 29 GIRT alerts were activated across three campuses, with an average of five clinicians responding per case. Notably, 90% of alerts resulted in a documented care plan and mortality among patients with severe GI hemorrhage decreased by 90%.

Strengthen the Core: Quality Silver Award
A Guideline to Reduce Postoperative Acute Kidney Injury in Surgical Patients
Postoperative acute kidney injury (AKI) is an AHRQ patient safety indicator (PSI-10) and a potentially avoidable safety event. In Q3 of 2021, our observed-to-expected ratio of AKI was 4.32, significantly higher than other academic medical centers. The multidisciplinary PSI-10 task force implemented a comprehensive guideline and validated risk assessment tool to identify patients at risk for AKI or dialysis after elective surgical procedures. Post-implementation, patients had significantly shorter hospital lengths of stay, ICU lengths of stay, and ventilator days compared to a similar preimplementation patient cohort. The need for dialysis decreased 42%, and the percentage of patients with post-op AKI decreased to less than 10%.
Strengthen the Core: Patient Experience Award
Courtesy and Respect: Impacting Patient Experience in the Ambulatory Care Setting
In FY 23, the patient experience scores for ambulatory practices were below the National Research Corporation 50 th percentile in almost all categories, with the lowest score for “staff members courtesy and respect.” A bundle of best practices, including AIDET, HEAT and Teach-back was implemented across ambulatory primary and specialty practices through web-based training of all caregivers, along with an observation tool for real-time feedback. The bundle was piloted in Women & Children’s and Cancer service lines in the first half of FY 24. On average, 84% of caregivers completed the required training, and 195 observations were conducted. Percentile ranks for “staff courtesy and respect” and “explain things back” improved by an average of more than 13 points.
Strengthen the Core: Flow Award
Timely Consult Calls: Not a Delusion
An Achieving Competency Today (ACT) team identified an opportunity to reduce consult-related delays. Specifically, the team aimed to decrease the time from consult order to receipt by the consulting ChristianaCare Psychiatric Group provider, which had a baseline of 194 minutes. The team discovered that consult order tasks were appearing under the “PRN/Continuous” tab instead of the “Scheduled” tab in PowerChart, leading to delays. To address this, the team developed educational materials for Nursing staff and patient care technicians on the correct location of the consult task. During the twoweek ACT team implementation period, consult time decreased by 27%, lowering the average to 142 minutes. The consult task has since been moved to the “Scheduled” tab, and ongoing collaboration with key stakeholders continues to further reduce consult times.
End Disparities Gold Award
Improving Access to Bariatric Surgery Care for Spanish-Speaking Patients
Hispanic adults accounted for only 7.8% of the Bariatric Surgery Program patient population in 2021 versus 10.5% of the Delaware census. Access was limited due to a lack of translated materials or communication methods for Spanish-speaking patients. The Bariatric Surgery Program team recognized there was no formal protocol for Spanish-speaking patients and there were only limited translated materials and communication methods, both of which potentially limited access to bariatric care. The team worked with our Health Equity team on interventions such as translating materials into Spanish and creating formal protocols. Data from the Bariatric Surgery Program (January 2021–December 2023) showed a 59.25% increase in Hispanic patient enrollment, rising from 7.83% to 12.47%, surpassing the team’s goal.

End Disparities Silver Award
Addressing the Other 80% of Health Care
Medical care accounts for only 10-20% of modifiable factors affecting health outcomes, while 80-90% are driven by Social Drivers of Health (SDoH) such as food insecurity, housing instability and lack of transportation. ChristianaCare expanded SDoH screening and resource connections by enhancing PowerChart tools for automated referrals, implementing Tonic for self-screening in ambulatory settings, establishing the Social Care Connection Center and integrating screenings into acute care to address discharge barriers. From January 2023 to June 2024, more than 30,000 patients were screened, with nearly 9,000 identifying at least one social need most commonly financial insecurity (23%), food insecurity (20%) and housing (16%).
Enable Every Caregiver to Thrive Gold Award
Promoting Safety: A Workplace Violence Mitigation Strategy
Per the U.S. Bureau of Labor Statistics, health care and social service workers accounted for 76% of all nonfatal workplace injuries and illnesses due to violence. ChristianaCare’s 2022 Culture of Patient Safety Survey found an opportunity in caregiver perception of workplace aggression and de -escalation tools/training. The Workplace Violence subcommittee on Practice and Policy developed an Aggression Interdisciplinary Plan of Care, implemented the Dynamic Appraisal of Situational Aggression (DASA) to screen patients at risk for aggression, created aggression risk door signage to alert caregivers and visitors and implemented an aggression SmartZone Alert. Six months post-implementation, the DASA identified 782 patients as high risk for aggression, and the percent of patients with an aggression IPOC created more than doubled
Enable Every Caregiver to Thrive Silver Award
Unlocking Safety: The Parking Perception Puzzle
The Achieving Competency Today team discovered a common issue among caregivers: Feeling unsafe in the Newark campus’ parking lots and not knowing ChristianaCare Public Safety’s contact information. The team created a flyer with parking lot safety tips and a QR code that enables any caregiver to scan and save the Newark Campus Public Safety’s contact to their phone. They shared the flyer with more than 700 caregivers. The team also coordinated with Public Safety to order 80 Public Safety Contact Info signs for the employee parking areas. Post-intervention, 70% of surveyed caregivers reported feeling safer.
Radically Simplify Access Award
Need for Speed: Improving the Infusion Prior Authorization Process for Rheumatology
Specialty Pharmacy reallocated an access coordinator for a three-month pilot to obtain prior authorization (PA) approvals for infusions referred by rheumatologists and to notify infusion center staff to schedule patient infusion appointment. Median time to PA approval decreased to three from 32 workdays and time from referral to first infusion decreased to 17.5 days. Provider satisfaction of the referral process improved to “outstanding.”

Healthy at Home Award
PIP PIP Hooray! Pressure Injury Prevention, Performance Improvement Project
To improve Braden Risk Assessment accuracy, HomeHealth implemented several activities, including an interactive Braden Risk scoring education for caregivers and standardized score-based interventions. The team also developed a Pressure Injury Prevention Protocol, or PIPP, that involved a wound care virtual visit for high-risk patients. Braden scoring accuracy improved 37% and 23 virtual visits were completed. And the FY 24 pressure injury rate decreased by 39%.
Operational Improvement Gold Award
Lines, Tubes and Drains, Oh My! Tracking Device Utilization for Infection Prevention
Infection Prevention expanded use of the Lines, Tubes and Drains (LTD) report to patient care units through an automated dail y PowerChart report for use during daily rounds to assess the necessity of the devices. The mean monthly central line day count decreased by 9%; urinary catheter day counts decreased by 16%. Additionally, 88% of surveyed caregivers said the LTD reports made their jobs easier, saved time and are more efficient; 73% said the reports helped them remove devices sooner.
Operational Improvement Silver Award
We Can't Fix It If We Don't Know About It: Increasing Reporting in Patient Safety
The ambulatory safety team created a QuickSubmit form in R2L by reducing redundant fields, using natural language prompts and creating a single point of reporting. This led to a more intuitive and time-saving workflow for caregivers entering events. The time to enter an event report decreased significantly by more than six minutes. The average number of monthly event submissions increased by 50%.
Operational Improvement Bronze Award
Patient Safety is Patient Care: Bringing an EBM Patient Safety Program to Ambulatory
Patient safety has traditionally focused on inpatient care, with less emphasis on ambulatory settings due to perceived inpatient control. To address this, multiple EBP interventions were implemented, including defining metrics, identifying caregivers for report analysis, simplifying forms, leadership rounding and communicating safety metrics consistently. Additionally, a shortened event report form was piloted in six primary care practices and expanded enterprise-wide in November 2023. Post-intervention, the average number of event reports increased almost 12% to 124 per month

Operational Improvement Honorable Mention Award
NutriCatch: Enhancing Malnutrition Detection in Hospitalized Patients
The Systemwide Malnutrition Workgroup implemented a validated malnutrition screening tool that electronically refers high-risk patients to registered dieticians for a nutritional assessment. Malnutrition coding increased to more than 10% and the CMS Global Malnutrition Composite measure was met.
Resident's Award
Guardians of Safety: Linking Residents to Interprofessional Learning Networks
In 2014, ChristianaCare’s Department of Academic Affairs formed the Resident Quality and Safety Council to provide a forum fo r integrating patient safety best practices across clinical departments and enhance communication between hospital committees and residency programs. Resident event reporting increased 167% and now averages 35 reports monthly. Resident presentations included the medication reconciliation process, availability of emergency equipment and handoffs.
Magnet Structural Empowerment
Nurse Driven Ultrasound Guided Peripheral IV Course Reduces Device Utilization Rate
Central line utilization ratio in Surgical Critical Care Complex (SCCC) and Transitional Surgical Unit (TSU) was 0.47. Patients with a central line are more than 200% more likely to develop a CLABSI compared with patients with only peripheral vascular access. The SCCC and TSU developed the first nursing specific ultrasound guided peripheral IV course. After launching the ultrasound-guided peripheral IV course in January 2020, the ratio dropped to 0.30 (a 19% decrease) from 2020 to 2023. Since then, SCCC and TSU have placed 1,291 peripheral IVs, leading to an estimated $321,361.44 in potential savings based on 2017 hospital-acquired CLABSI costs.
Magnet Exemplary Professional Practice Award
Take a Second Look: Two-Nurse Verification to Reduce Lab Errors
To help address preventable errors that may cause delays in care, potential harm and increased costs, the MICU implemented two-nurse verification for all lab specimens. The process requires a second look for correct patient, sample, specimen and/or medium. The team educated staff on the process and repeated education when errors occurred. Leadership also debriefed events with involved staff in person and via email. Signs posted at the tube station and huddle board served as visual reminders. The intervention led to a 27% decrease in lab specimen errors and a 17% decrease in preventable errors.

Magnet Transformational Leadership Award
The “WE CARED” Program: It’s Not Just a Card, It’s an Experience
Facing challenges in patient communication and a decline in Teach-back scores, the Newark Campus’s 4B leadership team launched the "WE CARED" initiative in September 2023. Designed to enhance patient education, align with systemwide fall prevention strategies and improve patient experience, the program leveraged virtual nursing and structured Teach-back pauses. As a result, the unit achieved 131 fall-free days, a 9% increase in patient portal enrollment, a 25% improvement in Teach-back scores and an increase in the number of DAISY nominations. Discharge lounge utilization also exceeded goals at 62%.
Magnet New Knowledge, Innovations & Improvements
Decreasing ED Lab Hemolysis: An Evidence-Based Practice Change
In the Newark campus emergency department (ED), there has been an increase in laboratory specimen hemolysis. Hemolysis is the breaking down of red blood cells caused by the mishandling of blood samples during blood specimen collection. The blood test is unable to run when hemolysis occurs. This can lead to increased ED patient length of stay, delay in patient diagnosis and treatment, decreased patient and caregiver satisfaction and increased costs. ED nurses made an evidence-based practice change to utilize straight steel phlebotomy for ED lab specimens, leading to a decrease in the hemolysis rate from 8.9% to 4.7%.




Headquartered in Wilmington, Delaware, ChristianaCare is one of the country’s most dynamic health care organizations, centered on improving health outcomes, and innovating to make high-quality care more accessible, equitable and affordable. ChristianaCare includes an extensive network of primary care and outpatient services, home health care, urgent care centers, three hospitals (1,430 beds), a freestanding emergency department, a Level I trauma center and a Level III neonatal intensive care unit, a comprehensive stroke center and regional centers of excellence in heart and vascular care, cancer care and women’s health. It also includes the pioneering Gene Editing Institute. ChristianaCare is nationally recognized as a great place to work. ChristianaCare is rated by Newsweek as one of the World’s Best Hospitals and is continually ranked among the best in the U.S. in national quality and safety ratings. ChristianaCare is a nonprofit teaching health system with more than 260 residents and fellows. With its groundbreaking Center for Virtual Health and a focus on population health and value-based care, ChristianaCare is shaping the future of health care.


