CAMPBELL ORTHOPAEDIC JOURNAL 2024























Go where no surgeon has gone before. Explore the latest in minimally invasive surgery with a high-resolution, 1.9 mm diameter, single-use NanoNeedle camera, medical-grade console, and 2.8 mm diameter NanoResection devices. The full portfolio of NanoNeedle Scopes—available in three lengths—includes a variety of sheaths and cannulas to meet your unique needs.


Learn more about Nano arthroscopy at: RevolutionizingArthroscopy.arthrex.com

Available Lengths:
125 mm — Knee, Shoulder, Hand and Wrist, and Foot and Ankle
180 mm — Hip, Larger Joint Spaces, and NanoScopic Carpal Tunnel Release
250 mm — Endoscopic Spine and Multispecialty

The Center for Orthotics & Prosthetics is a full service orthotic and prosthetic facility providing orthotic and prosthetic services for newborns to geriatrics. Below is an abbreviated list of patient needs serviced by COPI:
The Center for Orthotics & Prosthetics is a full service orthotic and prosthetic facility providing orthotic and prosthetic services for newborns to geriatrics. Below is an abbreviated list of patient needs serviced by COPI:
The Center for Orthotics & Prosthetics is a full service orthotic and prosthetic facility providing orthotic and prosthetic services for newborns to geriatrics. Below is an abbreviated list of patient needs serviced by COPI:
Cerebral Palsy
Cerebral Palsy

Cerebral Palsy
Muscular Dystrophy
Muscular Dystrophy
Spina Bifida
Spina Bifida
Osteoporosis
Osteoporosis
Scoliosis
Scoliosis
• Diabetes
• Diabetes
Muscular Dystrophy
• Diabetes
• Ankle/Foot Deformity
• Ankle/Foot Deformity
Spina Bifida
• CVA (Stroke)
• CVA (Stroke)
Osteoporosis
• Clubfoot Deformity
• Clubfoot Deformity
Scoliosis
• Amputees
• Amputees
• Ankle/Foot Deformity
• CVA (Stroke)
• Clubfoot Deformity
• Amputees
For consultation and referrals, contact us at: 6655 Quince Road #124, Memphis, TN 38119 Office: 901. 757.5461 | Fax: 901.757 0909
For consultation and referrals, contact us at:
For consultation and referrals, contact us at:
6655 Quince Road #124, Memphis, TN 38119
6655 Quince Road #124, Memphis, TN 38119
Office: 901. 757.5461 | Fax: 901.757.0909
Office: 901. 757.5461 | Fax: 901.757 0909
38 N. Pauline, Memphis, TN 38105 Office: 901.531.1980 | Fax: 901.531.1984
38 N. Pauline, Memphis, TN 38105
38 N. Pauline, Memphis, TN 38105
Office: 901.531.1980 | Fax: 901.531.1984
Office: 901.531.1980 | Fax: 901.531.1984
2321 5th Street N, Columbus, MS 39705 Office: 662.243.7435 | Fax: 662.240.4126
2321 5th Street N, Columbus, MS 39705
2321 5th Street N, Columbus, MS 39705
Office: 662.243.7435 | Fax: 662.240.4126
Office: 662.243.7435 | Fax: 662.240.4126
email: copi@thecenterforoandp.com
email: copi@thecenterforoandp.com
email: copi@thecenterforoandp.com
Practitioners:
Practitioners:
• Jack Steele, CO, LO, FAAOP
• Jack Steele, CO, LO, FAAOP
Practitioners:
• Jack Steele, CO, LO, FAAOP
• Jim Huddleston, CO, LO
• Jim Huddleston, CO, LO
• Thomas Baker, CP/LP, COA
• Thomas Baker, CP/LP, COA
• Jim Huddleston, CO, LO
• Wendy Sandlin, CO
• Wendy Sandlin, CO
• Thomas Baker, CP/LP, COA
• Cathie Baker, CPO/LPO
• Cathie Baker, CPO/LPO
• Cathie Baker, CPO/LPO
• Wendy Sandlin, CO
• Bradley Carver, CPO/LPO
• Bradley Carver, CPO/LPO
*Accepting new patients. Accepting most insurance.
• Bradley Carver, CPO/LPO ”Focus on You”
”Focus on You”
”Focus on You”


First device to quantify joint laxity prior to bony resections, with a robotic 1,2




First robotic-assisted system indicated for Revision Knee Arthroplasty






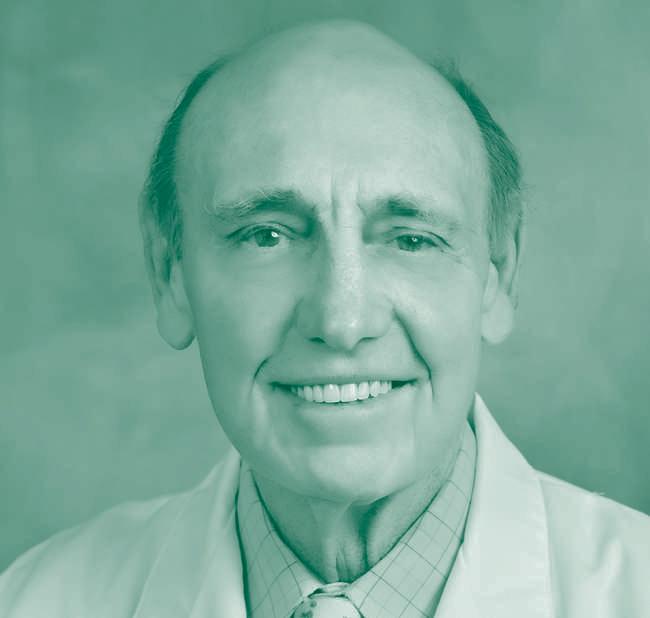
Frederick M. Azar, MD
Chief of Staff, Campbell Clinic Orthopaedics
Professor, University of Tennessee Health Science Center
Department of Orthopaedic Surgery and Biomedical Engineering; Sports Medicine Fellowship Director
Campbell Clinic Foundation Family and Friends,
This past year will be remembered as the most challenging in our history
The tragic loss of our brother, Dr. Ben Mauck, still seems surreal. He was not only a masterful physician, but a mentor and teacher, shaping the careers of aspiring medical professionals. His infl uence at Campbell Clinic and within our medical community will serve as a positive model for excellence and compassionate care for generations to come. Please continue to pray for Rhiannon, their children, and for the divine strength and comfort that only God can provide to them. We also lost Dr. Terry Canale who was an iconic leader at Campbell Clinic and to our entire profession. It is because of his vision that this journal exists.
In2023wewelcomedarecordnumberofnewproviders,includingthosewho specialize in adult reconstruction, spine, pediatrics, hand, sports medicine orthopaedics, and primary care. We also onboarded an orthopaedic hospitalist, an internal medicine physician, and numerous physician assistants. They are all superb individuals, dedicated to compassionate patient care and to education and research. To improve patient access and care, we also added another satellite offi ce in Oxford, Mississippi, and now serve 11 locations in the Mid-South and across Tennessee.
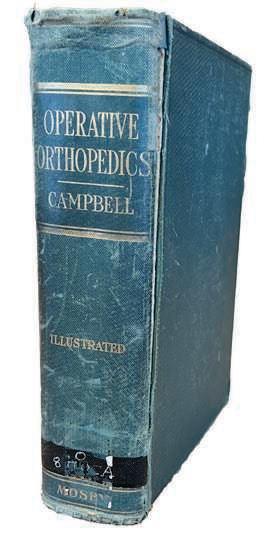
The Campbell Clinic Foundation has experienced tremendous growth as well. We have expanded our clinical trials initiative, producing more than 200 presentations, publications, and posters to share the results of our research with the orthopaedic community. The second edition of Campbell’s Core Orthopaedic Procedures was published, and we are well into the work on the 15th edition of Campbell’s Operative Orthopaedics.
These achievements serve to remind us that we are making great strides in advancing our mission, which is unsurpassed orthopaedic patient care, an objective we strive to accomplish through our research and education programs. The ongoing support of our patients, alumni, industry partners, staff, and donors from around the world has allowed us to continue working toward this goal as we carry on into the next 100 years. We are humbly indebted to all of you for your generosity and passion.
We are pleased to introduce our 2024 Graduating Class of Residents and Fellows, all exceptional surgeons who will continue to provide excellent care to their patients and contribute to our profession. Included in this issue are abstracts of the research they completed during residency. Also included are the top research and review articles by our staff physicians.
This year marks the 100th anniversary of our residency program. Campbell Clinic remains committed to education and to our mission of excellent patient care, a standard set by our founder, Willis C. Campbell, MD, more than a century ago. We continue to be guided by our Core Values of Excellence, Integrity, Compassion, Innovation, Commitment, Legacy, and Unity. And we remain committed to our priorities of faith, family, and patient care. We look forward to being together for our combined Triennial and Alvin J. Ingram Lectureship in April of 2024.
Thank you for all that you do for our patients and our profession.
Together, we are Moving Lives.
Best regards and God Bless,
Frederick M. Azar, MD Campbell Clinic Chief of Staff
The mission of the Campbell Clinic is to provide unsurpassed patient care while being recognized as a leader in teaching and research in the profession of orthopaedic surgery.
Another century of world-class orthopaedic care restoring function and quality of life.
We aim to exceed expectations by providing an exceptional patient experience through accessible & efficient quality care, a comfortable and safe environment, and effective communication.
We embrace, expect, and exhibit honesty, accountability and professionalism toward patients, each other, and outside partners.
We commit to cultivating an environment of compassion for each patient and family member through sensitivity, sincerity, and empathy.
We commit to delivering innovative technologies, products, and services through our rich orthopaedic heritage and a strong research foundation.
We commit to each other, to excellent patient care, to education, to innovation and research, to community service, and to orthopaedic leadership.
We will do what is right for the Campbell Clinic, our patients, and our employees.
Everything we do, we do together.

The region’s top orthopaedic specialists are available near you when you need them most.
• Break, sprain, and injury care
• Outpatient hip, shoulder, ankle, and knee surgery
• Physical therapy
• Entire family musculoskeletal care














































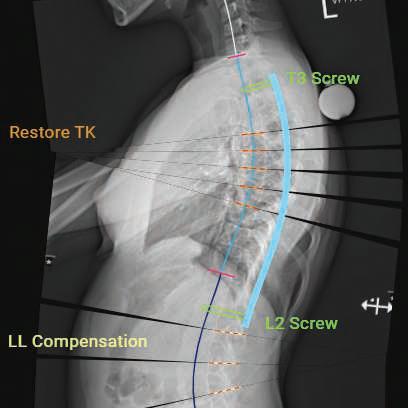
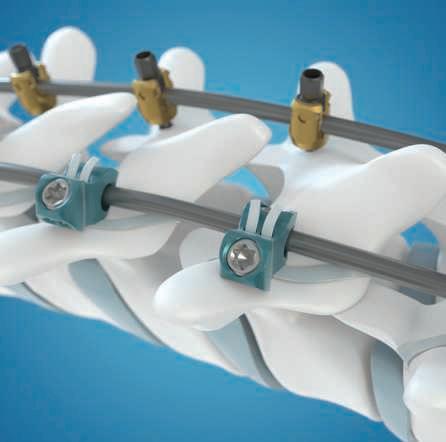

UNiD™ ASI leverages predictive models for pediatric deformity to provide compensatory measurements of lumbar lordosis and pelvic tilt aiding in pre-operative planning, intra-operative alignment execution, and longitudinal data collection for patients.
LigaPASS™ 2.0 system is designed to help achieve a wellbalanced spine in both coronal and sagittal planes when screws, hooks, or wires cannot be placed and axial derotation and reduction are both desired.
Mazor ™ robotic guidance platform is a powerful minimally invasive solution featuring planning tools that enable 3-D construct design and robotic surgical execution for a seamless OR experience.
Josephine™ the giraffe is our ambassador for education to children with early onset scoliosis and their families.
For instruments and implant-specific indications, contraindications, warnings, precautions, and other important medical information, please see the package inserts for the respective product(s). An electronic version of the package insert may be found at www.medtronic.com/manuals. www.Medtronic.com/UNiD

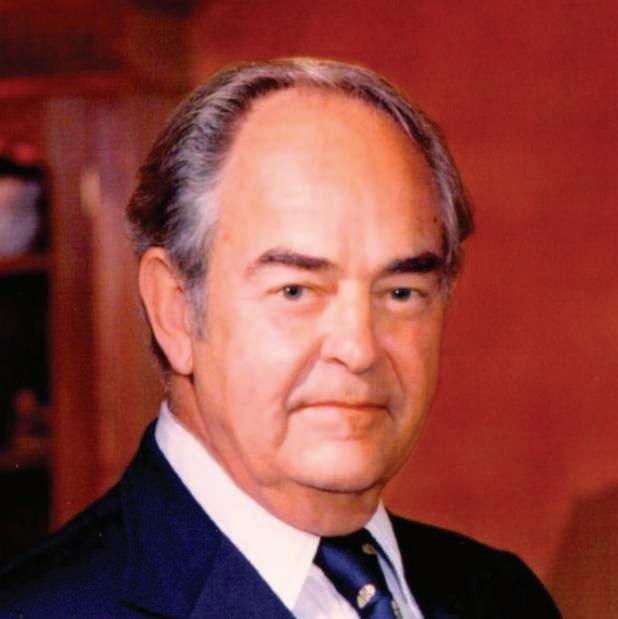
The Campbell Clinic Foundation remembers and celebrates the life of our cherished leader and Editor-in-Chief Emeritus, Dr. S. Terry Canale, who passed away in August of 2023 at the age of 83 in Memphis, Tennessee.
If visionary is a word used to describe leaders, Dr. Canale was the actual embodiment of that concept, as he was a person who fully embraced progress. The ideas he introduced and implemented during his time ultimately took our organization to new heights. He had a profound understanding that innovation and calculated risk were not only necessary for growth but they also had to be driven with intent, a role that he assumed with ease. Dr. Canale never wavered from what he believed was the right path, and this was true in not only his professional but personal life as well. The two mingled comfortably, and he pursued and juggled both with equal positivity and zeal, accomplishing more in one day than most people in a month, always moving things forward no matter the obstacles and always willing to battle complacency and stagnation.
Having graduated from the University of Virginia and the University of Tennessee Medical College, Dr. Canale joined the Campbell Clinic staff in 1974, eventually becoming the Chief-of-Staff, Editor of Campbell’s Operative Orthopaedics, and Professor and Chairman of the Department of Orthopaedic Surgery
of the University of Tennessee Health Science Center. Among his many national leadership positions, he served as President of the Pediatric Orthopaedic Society of North America, President of the Council of Musculoskeletal Specialty Societies, Chairman of the Board of Directors of the Orthopaedic Research and Education Foundation, and President of the American Academy of Orthopaedic Surgeons. His contribution to orthopaedics was substantial, not only because of his leadership and service but because of his willingness to mentor and foster a new generation of orthopaedic surgeons, something that was close to his heart. Dr. Canale inspired others to serve and take leadership roles to advance the orthopaedic profession.
Throughout his career, he was a staunch supporter of the Campbell Clinic Foundation and the pillars upon which we were founded: education, research, publication, and outreach. With enthusiasm and optimism, he guided us through the uncharted waters of progress to where we are now. There was never a dull moment when he was around, and one could count on anything but being bored. It is with fondness that we remember Dr. Terry Canale.


On Tuesday, July 11, 2023, an unimaginable tragedy struck our Campbell Clinic family when our friend and colleague, Dr. Benjamin Mauck, was taken from us. Ben was a graduate of our residency program and a member of the Campbell Clinic staff. He was a compassionate and gifted hand surgeon who worked tirelessly to provide the best care for patients with difficult hand, wrist, and elbow problems. He became the expert in congenital hand deformities and served as the director of the Congenital Hand Deformities Clinic at Le Bonheur Children’s Hospital, helping scores of young children with hand anomalies. He was highly regarded by his patients and their families for his kind bedside manner and the ability to help them feel cared for. He never sought tributes and only wanted to provide the best care for patients who put their trust in him. Ben took the same care in his role as educator and has been described by our residents and fellows as being an easygoing mentor and a superb and patient teacher. His passion for our profession and his commitment to excellence in patient care and education were clearly evident in all things he touched.
Ben was born on April 11, 1980, in Covington, Virginia, to Ann and Gregory Mauck. He attended high school in Savannah, Tennessee where he also played basketball. In 1998 he joined the TSSAA All-Star Basketball team and earned a basketball scholarship to Western Kentucky University. Ben went on to graduate from Lambuth University and received his MD at the University of Tennessee Health Science Center (UTHSC). He then completed his orthopaedic residency at the UTHSC Campbell Clinic Department of Orthopaedic Surgery. Before joining our staff, he completed a fellowship in hand surgery at the University of Texas Health Science Center of San Antonio.
In addition to being an outstanding orthopaedic surgeon and Campbell Clinic partner, Ben was a devoted family man. He and his wife, Rhiannon, met in college and married on May 12, 2007. They had two children, a son and a daughter. He was immensely proud of his family and sought out every opportunity to spend quality time with them. Ben also loved the outdoors and often shared his affinity for fishing and hunting with family and his friends. Ever giving of his time and energy, he will be remembered as a kind, generous, and compassionate individual, with a true doctor’s heart. We are better for having known him.

Much has been written about the early years of Campbell Clinic and the Campbell Clinic Foundation, but what about the last two decades? This article, informed by the leaders and clinicians who have led practice, education and research, highlights the exciting growth and changes that have defi ned our 21st century thus far.
Campbell Clinic’s first century has been marked by an explosion of growth, with new locations, operating hours, surgeons and nonoperative physicians being added to help expand access to the highest quality of orthopaedic care in the Mid-South. Both joint-replacement and outpatient surgeries also have boomed thanks to expanded facilities and staff, substantial research, and changes in healthcare policy.
And while the clinic has expanded, physicians have continued training future orthopaedic surgeons and performing clinical research. Faith, family, and patient care remain the priorities.
“We continue to bring in high character, high quality physicians,” said Dr. Frederick Azar, Chief of Staff of Campbell Clinic. “We are dedicated to excellence in patient care, education, and research. These priorities allow us to seek innovative ways to improve the quality of life for our patients.”
Though now headquartered in Germantown, Campbell Clinic in 2001 resumed its Midtown clinic hours and physical therapy at a leased site at 1211 Union Ave. In 2019, the Clinic added to its Germantown footprint by opening a $49 Million, four-story facility at 7887 Wolf River Blvd., adjacent to the 1400 S. Germantown Rd. location. The 120,000 square-foot Wolf River building includes an ambulatory surgical center with eight operating rooms, outpatient clinical space, and a leading-edge physical therapy and sports performance center named after the late former chief of staff Dr. S. Terry Canale.
The year 2022 brought a merger with Tier 1 Orthopaedic and Neurosurgical Institute in Cookeville, TN and its 11 physicians. That move extended the clinic’s reach to East Tennessee. Campbell Clinic also opened new branches in East Memphis, Arlington, Olive Branch, MS and, in 2023, Oxford, MS. And, in 2024, the clinic will open a 30,000 square-foot facility in suburban Collierville to replace a leased site.
Improved access to orthopaedic care also has come in the form of “after hours” service, which caters to urgent, acute injuries, and “walk in” hours. The goal of all of this expansion has been to serve more orthopaedic patients. At the turn of the 21st Century, Campbell Clinic was treating almost 44,000 people annually. In 2023, 224,000 patients were treated.
“When I joined the group 40 years ago, in 1982, I was the 13th person,” said Dr. James H. Beaty, former Chief of Staff. “By early 2024, we’re going to be approaching 60 doctors.”
Besides the addition of orthopaedic surgeons, Campbell Clinic has hired physiatrists (nonoperative musculospinal physicians) and family-medicine physicians who have been fellowship-trained in sports medicine and offer nonoperative orthopaedic care. Almost 20 Advanced Practice Providers, including nurse practitioners and physician assistants, have joined the clinic ranks, giving the clinic an approximate grand total of 860 employees. At the helm is the Chief of Staff, who was Dr. Canale from 1994 to 2001. Dr. Beaty replaced him until 2010, at which time Dr. Azar assumed the reins.
Excellence in orthopaedic research, advancement of surgeon education and community outreach are the three pillars on which the Campbell Clinic Foundation(CCF) was built. Founded in 1946, the Foundation has grown during the 21st Century largely due to the direction of Jack Blair, now retired after serving as Smith + Nephew President of North America and Japan. As chairman of CCF’s Board of Trustees from 2000 to 2021, Blair guided its expansion to include prominent business leaders, who helped strengthen the foundation’s financial position, expand community outreach, and raise its public profile.
He also played a major role in establishing the Center of Excellence for Cerebral Palsy(CP) Care and Research in partnership with Le Bonheur Children’s Hospital, the only comprehensive center of its kind within 300 miles of Memphis. The CP Center, opened in 2018, offers a broad range of services and individualized, multi-disciplinary treatment.
Throughout the last decade, more and more prominent orthopaedic surgeons and scholars have served as Campbell Clinic Foundation visiting professors. Since 2022, the Alvin J. Ingram Memorial Lecture has become the "Who's Who" of the orthopaedic world, featuring top society presidents and innovating leaders. In addition, the Sports Medicine and Shoulder Annual Visiting Professor Lecture, the James H. Beaty MD Visiting Professor in Pediatric Orthopaedic Surgery Lecture, and the James Harkess MD Total Joint Visiting Professor Lecture are all programs that have both enhanced the teaching experience and brought new knowledge to Campbell residents, staff, and alumni.
A challenging time for Campbell Clinic—and the world—came when the COVID-19 pandemic struck in early 2020. The clinic never closed, but it operated during fewer hours, and with fewer physicians and staff, from March to June 2020. To ensure a high level of safety, additional cleaning procedures were instituted, handshaking was discontinued, and all people, patients and employees alike, were screened for the contagious deadly virus. Telehealth appointments were offered and some staff, such as CCF employees, began working from home.
“Like so many other industries, we had to move much of our formal teaching and research online,” said Residency Program Director Derek M. Kelly, MD. “We also facilitated an entirely virtual resident recruitment and selection process for three consecutive years.”
As clinical and educational programs continued, the Foundation's staff and Clinic physicians embarked on the 15th edition of Campbell's Operative Orthopaedics and added Campbell's Core Procedures to its family of publications.
With leadership from Dr. Terry Canale, the Campbell Orthopaedic Journal was introduced in 2015 to showcase the Campbell Clinic Foundation's breadth and depth of research. This annual publication also highlights residents' research, program milestones, and new insights and findings for orthopaedic care and practice.
Community outreach has remained a priority during the 21st Century:
• In 2007, Memphis became one of the first new locations for expansion of Pittsburgh’s Our Hearts to Your Soles project. Dr. David Richardson continues to lead this annual tradition, where Campbell Clinic foot and ankle sub-specialty physicians and residents provide Memphis Union Mission clients with new shoes, socks, and foot care.
• In 2012, the International Service Elective was established to let one senior resident teach and work alongside healthcare professionals in an under-served, developing country. The Molly Shumate Community Service Scholarship and international elective program continue to be beneficiaries of the Campbell Clinic Foundation's annual Campbell Celebrates gala fundraiser.
• Each spring, young athletes who attend 13 area high schools receive annual free, comprehensive physical exams administered by the clinic’s physicians, residents, fellows, and athletic training staff, usually at the Germantown Road location.
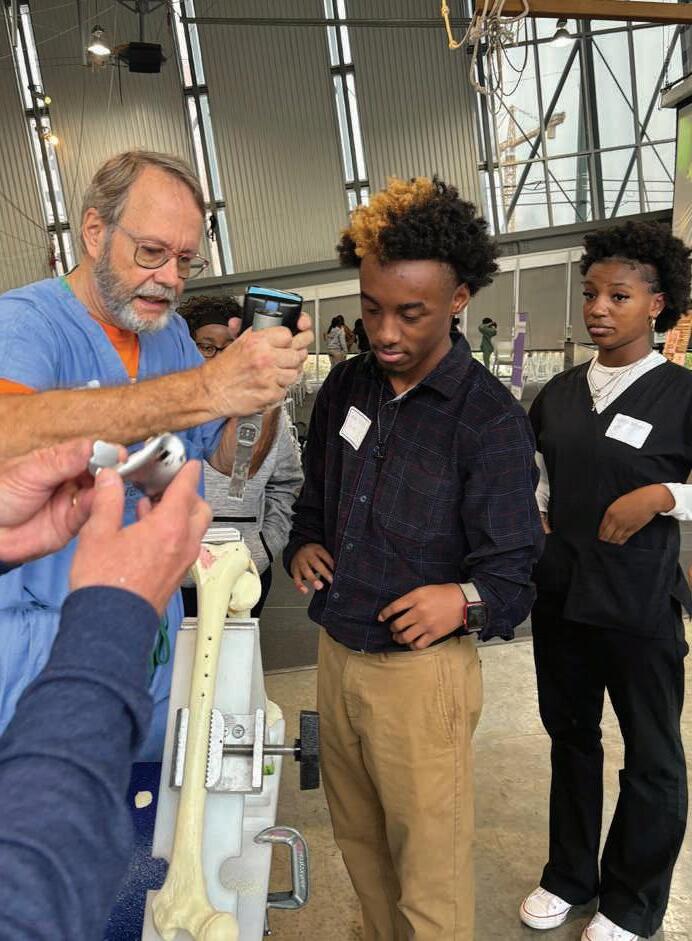
• Since 2022, the Campbell Clinic Foundation has partnered with Nth Dimensions to host a summer medical student scholar to learn alongside Campbell faculty. In 2023, the Foundation introduced Moving Community to focus effort and investment on developing the future orthopaedic workforce. This included participation in the Junior Achievement INSPIRE Career Fair and hosting an Nth Dimensions BioSkills Workshop for 80 Memphis-Shelby County High School students. Each event gives middle- and high school students hands-on exposure to orthopaedic tools and mentorship with healthcare professionals and physicians.
To support Moving Community or get involved, contact Amy Farris, Development Officer, Campbell Clinic Foundation at 901.759.5588
or apfarris@campbell-foundation.org

Small device foot print; 58”x73”; Point-of-Care; Ready to incorporate into small office setting.

Radiation dose is significantly lower than standard MDCT protocols1.

35% improved fracture detection and 2-fold improved identification of complex fracture over X-Ray2.
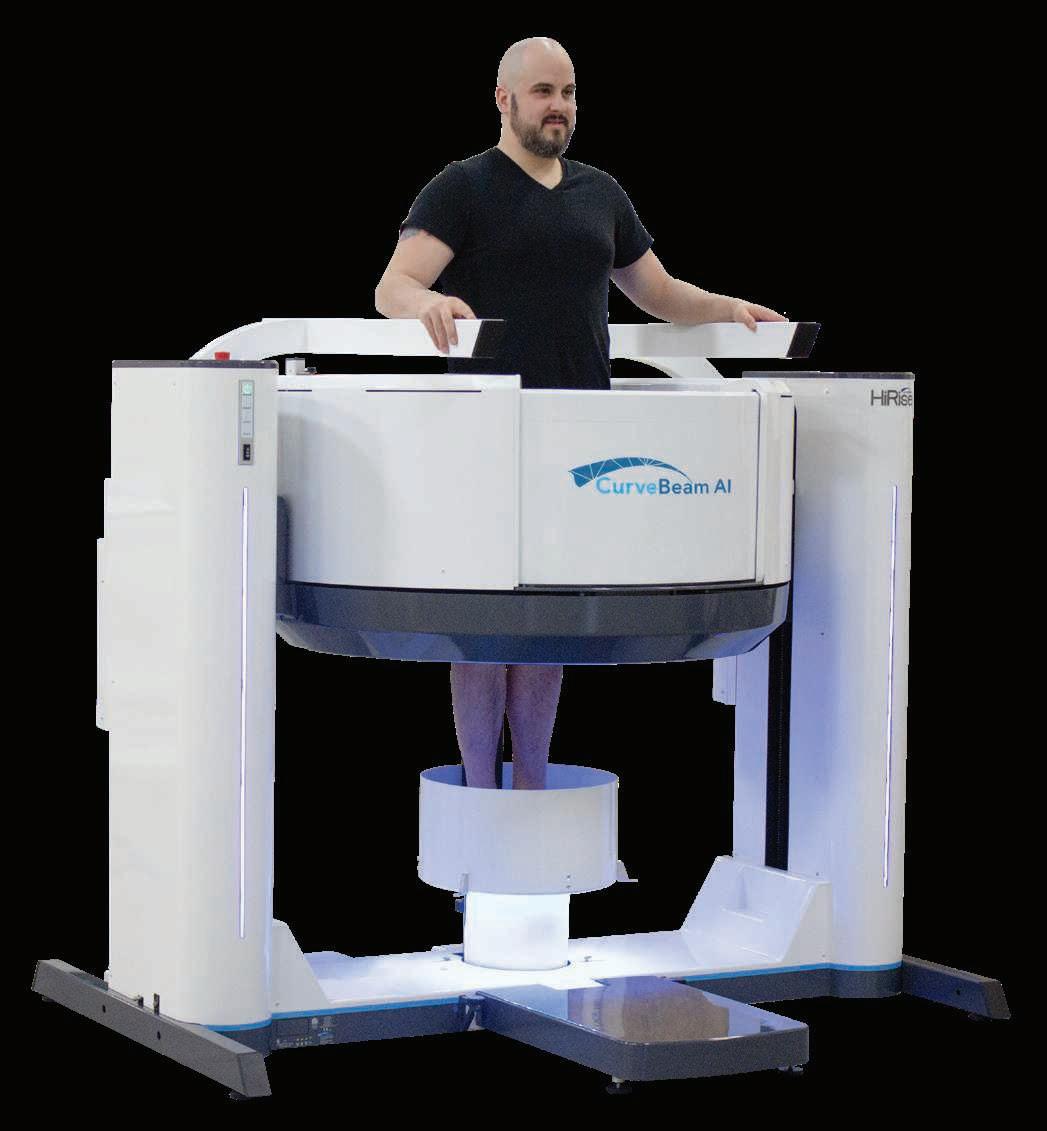


Self-shielded; Runs off standard 230V/30A outlet; 33-55 seconds per orbit.

Assess total leg alignment with 0.3mm slices.



Vendor approved protocols for joint replacement planning.
Decrease operative time and increase rates of implant survival.3
(1) Jaydev Dave, PhD. Effective Dose Associated With Weight-Bearing Cone Beam Computed Tomography Imaging of the Hip and Extremities. Poster presented at: IUPESM World Congress on Medical Physics and Biomedical Engineering; June 12 - 17, 2022; Singapore.
(2) Diagnostic Value of Cone Beam Computed Tomography (CBCT) in Occult Scaphoid and Wrist Fractures Christophe Borel et al, https://pubmed.ncbi.nlm.nih.gov/29153368/.
(3) Zeitlin J, Henry J, Ellis S. Preoperative Guidance With Weight-Bearing Computed Tomography and Patient-Specific Instrumentation in Foot and Ankle Surgery. HSS Journal®. 2021;17(3):326-332.
1920 Dr. Willis C. Campbell, who had established the Campbell Clinic in 1909, realizes more orthopaedic surgeons are needed in Memphis. He recruits Dr. James S. Speed, a graduate of Johns Hopkins Medical School, who, in spite of having no orthopaedic training, was attracted to the position because Dr. Campbell “assured him that, after one year, he’d be a well-trained orthopaedic surgeon, and that proved to be true.”

1924 Dr. Willis Campbell establishes an orthopaedic surgery residency program in Memphis, Tennessee. This program trains physicians to be orthopaedic surgeons and deliver much-needed bone and joint care to the Memphis and Mid-South region.
1933 The American Academy of Orthopaedic Surgeons is established by Dr. Campbell and other orthopaedic surgeons as a way to support the emerging field and share challenges, solutions and innovations to improve patient care.
1939 Dr. Campbell made yet another game-changing contribution to the orthopaedic field with his Textbook on Orthopaedic Surgery. This book was later renamed Campbell’s Operative Orthopaedics. While edited throughout the following years, this textbook is in use today, with the 15th edition scheduled to publish in 2026.
1946 The Campbell Foundation is formed as an education trust by Dr. Campbell’s partners to assist in the teaching and training of physicians. The Foundation would provide funds and support to further the field of orthopaedic surgery, including the expansion of residency and fellowship programs.
1960 The residency program was met with much success and, as a result, the number of residents is increased from four to eight per year.
1967 After much consideration, the Campbell Foundation and Campbell Clinic implements post-residency fellowships. The addition of fellows would foster more innovation and learning opportunities for all of the staff.
1983 The Elvis Presley Trauma Center at Regional One Health is established with a dedicated orthopaedic surgery trauma sub-specialty team. Today, “The Med” is one of the busiest Level 1 Trauma Centers in the nation and the only one in a 150-mile radius of Memphis. Orthopaedic Surgery residents spend nearly half their training learning trauma care. This Center is crucial to public health and safety in Tennessee, Missouri, Arkansas and Mississippi.
1986 The Russell-Taylor Nail is developed and introduced by two Campbell Clinic residents. It would become the number one intramedullary device used across the world in a decade. The same principles developed by those residents are still used to make nails today.
1990 The Campbell Foundation formally unites with the University of Tennessee Department of Orthopaedics to manage the residency program after a long-standing informal partnership. The
University of Tennessee Health Science CenterCampbell Clinic Orthopaedic Residency Program is an accredited, five-year orthopaedic residency program for 40 full-time orthopaedic residents.
1992 Campbell Clinic moves from its original home at 869 Madison Avenue in Memphis to its current home in Germantown, Tennessee. In what was once seen as a risky decision by Campbell Clinic, the move turned into an immense growing opportunity for the clinic and for the city of Germantown. Today, it lies in the center of what is now known as the Wolf River Medical Corridor.

1998 Campbell Clinic begins providing orthopaedic care for the Memphis Redbirds, Triple A baseball team, in what would be a successful relationship that has carried on to this day. Residents and fellows on sports medicine rotations support athlete care and events.
1999 Campbell Clinic opens its Collierville, Tennessee location, extending resident and fellow clinical and operative training to suburban clinic locations.
2000 The University of Tennessee Medical Center is renamed to the University of Tennessee Health Science Center (UTHSC). With six colleges under its umbrella (Dentistry, Graduate Health Services, Health Professions, Medicine, Nursing and Pharmacy), UTHSC has greatly affected the healthcare field by delivering extensive research, training, and successful healthcare professionals in diverse fields and specialties.
2001 The Campbell Foundation Board of Trustees expands to include business and community leaders to guide Foundation governance and growth. Jack Blair, a Smith + Nephew executive, is elected Chairman.
2001 When the Grizzlies NBA team moves from Vancouver, BC, Canada to Memphis, Tennessee, Campbell Clinic becomes the official sports medicine provider to the team and events.
2001 Campbell Clinic opens its Southaven, Mississippi location at Baptist Memorial Health Care DeSoto Hospital.
2002 As demand for outpatient surgery grows, the Campbell Clinic opens its first ambulatory surgery center (ASC) on Brierbrook Road in Germantown, Tennessee, with four operating rooms, expanding patient care as well as operative experience and training for residents.
2007 Cranbeary, a polar bear at the Memphis Zoo, falls 14 feet from her enclosure causing a serious break in her leg. Two steel plates and 26 screws later, Cranbeary’s leg was successfully treated by Campbell Clinic physician, Dr. Edward Perez, allowing her to heal and eventually regain full mobility.
2010 Clinical research gains momentum, with more projects led by staff physicians. Over the past 9 years, Campbell Clinic researchers have published 777 manuscripts and have presented 610 podiums and 279 posters.
2012 The UTHSC-Campbell Clinic Department of Orthopaedic Surgery expands to the UTHSCCampbell Clinic Department of Orthopaedic Surgery and Biomedical Engineering with William M. Mihalko, MD, PhD as the J.R. Hyde Professor, Combined Graduate Program Chair in Biomedical Engineering and Campbell Clinic Department of Orthopaedic Surgery and Biomedical Engineering.
2012 To honor his wife, Molly, and to provide residents unique learning opportunities, Daniel Shumate, Chief Financial Officer for Campbell Clinic, establishes the Molly Shumate International Elective Scholarship, allowing residents to make annual medical mission trips to developing countries, including Haiti, Honduras, and Nicaragua, to work and learn alongside healthcare professionals.
2014 The annual Alvin J. Ingram, MD Memorial Lecture, established by the family of beloved former Chief of Staff and Department Chair, Dr. Alvin J. Ingram

to honor his drive for education, expands under the leadership of Dr. Derek Kelly. It now draws an esteemed visiting professor and industry support. This prestigious signature lecture program includes early career to veteran surgeons and healthcare professionals and fosters collaboration across the industry.
2015 Drs. S. Terry Canale, James H. Beaty and Frederick M. Azar bolster the Canale Presidential Research Fund, with proceeds from their honoraria earned while leading the American Academy of Orthopaedic Surgeons.
2018 The Campbell Clinic Foundation leads the creation of the Center of Excellence for Cerebral Palsy Care and Research at Le Bonheur Children’s Hospital, becoming the only one-stop shop for comprehensive, multi-specialty care for children with cerebral palsy in the Mid-South with the support of a generous $1 Million seed gift from the Children’s Foundation of Memphis. Drs. David Spence and William C. Warner, Jr. serve as co-directors.

2019 Campbell Clinic’s exponential growth leads to the opening of the flagship Wolf River facility. This facility coincides with the increased support for outpatient surgery and the demand for orthopaedic care in the Mid-South region.
2020 Due to the COVID-19 pandemic, the Campbell Clinic residency implements virtual Monday Night Meetings to continue didactic training. Hybrid (virtual and in-person) meetings resumed in 2021 and have been maintained since to allow for
greater participation among residents and faculty, as well as allow for long-distance lectures. In addition, Visiting Rotations are created for 4th year medical students outside of UTHSC to experience Campbell Clinic training and learning experiences.
2021 The Campbell Foundation becomes the Campbell Clinic Foundation (dba). In honor of the Foundation’s 75th anniversary, the Diamond Fund is created to augment residency training and research, with alumni contributing nearly $500,000 to ensure the continued growth and success of the program.
2022 The Campbell Clinic opens three new satellite clinic locations in Arlington, TN, East Memphis, and Olive Branch, MS. In addition, Campbell Clinic acquires Tier 1 Orthopedic and Neurosurgical Institute in Cookeville, TN.
2022 The Campbell Clinic Foundation hosts the 25th Triennial Celebration, combined with the annual Alvin J. Ingram Memorial Lecture, drawing more than 300 participants, 26 industry supporters, and visiting faculty from Hospital for Special Surgery and Stanford University School of Medicine.
2022 During the 25th Campbell Club Triennial weekend, six alumni are presented with Campbell Awards and honored for their achievements, leadership, and contributions to orthopaedic medicine.
2023 The Campbell Clinic Foundation and Campbell Clinic collaborate with Nth Dimensions to host the first BioSkills Workshop in Memphis, TN, to introduce high school students to careers in orthopaedic surgery. Three fellows and five residents are among the volunteers. In addition, Campbell Clinic opens a facility in Oxford, MS.





















With 20 years of clinical use, the Equinoxe system offers the most complete shoulder solutions, proven through data generated by the largest single prosthesis database.
Gary Stavrum Chairman
Granite Forge
Frederick M. Azar, MD Chief Staff Officer
Campbell Clinic Orthopaedics
Kelly Luttrell Finance Chair
Vital Records Control
G. Andrew Murphy, MD Development Chair
Campbell Clinic Orthopaedics
James H. Beaty, MD President
UTHSC Department of Orthopaedics
Peg Murphy Branyan Retired, International Paper
Derek M. Kelly, MD
Campbell Clinic Orthopaedics
David G. LaVelle, MD Retired, Campbell Clinic Orthopaedics
Santos F. Martinez, MD
Campbell Clinic Orthopaedics
William M. Mihalko, MD, PhD
Campbell Clinic Orthopaedics
Frank T. Navarra Retired, Smith+Nephew Orthopaedics
Jack R. Blair
S. Terry Canale, MD*
Daniel H. Shumate Chief Executive Officer
Campbell Clinic
Buzzy Hussey
Joseph Orgill, III*
David Popwell First Horizon Bank
Jeffrey R. Sawyer, MD
Campbell Clinic Orthopaedics
Norfleet B. Thompson, MD
Campbell Clinic Orthopaedics
Thomas W. Throckmorton, MD
Campbell Clinic Orthopaedics
Barbara Williamson
Gary K. Wunderlich, Jr. Live Oak Merchant Partners
*Deceased EMERITUS
Larry W. Papasan*
Joseph C. Weller*
Jenny Koltnow Executive Director
Campbell Clinic Foundation

The only hip brace that integrates cold and control into your hip protocol. The EXCYABIR™ Hip Brace* combines the latest in DonJoy™ technology with a patented strapping system, easy range of motion settings, and a comfortable wrap-around design. EXCYABIR helps to provide protected range of motion following minimally invasive hip procedures, total hip arthroplasty, labral repair/FAI, unilateral mild-to-moderate hip osteoarthritis (OA), and preventively when there is risk of hip dislocation or as a conventional treatment after dislocation/reduction.

The low-profile, DonJoy® VersaROM® Hip helps deliver effective, functional ROM restriction in 15° increments.
Easy-to-use abduction/adduction push buttons and malleable hip and thigh shells help provide an individualized fit for increased patient comfort and compliance. The adjustable compression belt with easy-grip pull tabs anchors the hip joint, and the padded thigh cuff increases optimal alignment.
With a universal fit, one brace fits right or left hip up to a 54” waist circumference.

*WARNING: This device can be cold enough to cause serious injury. Serious adverse reactions & safety hazards may occur when using this device. Read and understand all warnings and Instructions Use, including contraindications, before using this device. Additional warnings appear in the Instructions for Use. DO NOT use this device without a prescription from a physician. Your prescription must state how long and how often the device should be used and the length of breaks between uses.
We are committed to lifelong bone and joint health for all through community outreach. Moving Community fosters health and well-being by applying the Campbell Clinic Foundation’s core strengths –education, research, outreach – to make orthopaedic care accessible today and tomorrow. We have cared for generations of families, often at the same time.
The Foundation plays a fundamental role in cultivating, inspiring, and preparing the next generation of orthopaedic surgeons and healthcare professionals equipped to serve their patients, their field, and their communities.
The Foundation also identifies, studies, and delivers care to meet the complex and unique needs of
patients with debilitating musculoskeletal conditions. From diagnosis to treatment to rehabilitation, we are there for you.
This comprehensive program strategy includes the Orthopaedic Workforce of Tomorrow. This is a new initiative driven to attract young people to the vast careers in orthopaedic healthcare. This includes partnerships with Memphis-based youth development programs and strategic alignment with national initiatives to give underrepresented minorities and women access and mentorship to pursue careers in medicine.
The CCF is eager to help build the orthopaedic workforce of tomorrow and foster a more diverse, inclusive, and equitable environment for individuals to learn, work, and thrive.
We have been fortunate to partner with Nth Dimensions, a national organization dedicated to eliminating healthcare disparities in all communities by diversifying the physician workforce. To accomplish this mission, they develop and implement pipeline initiatives that provide resources, including scholarships, expertise, mentorship, and hands-on experience for women and underrepresented minorities.

As part of our partnership with Nth Dimensions, we host a summer internship with Campbell Clinic for medical students. This opportunity provides an immersion in orthopaedics with opportunities to scrub into surgery, participate in research, and meet a diverse network of talented physicians and healthcare professionals.
Eddie Minaya, a rising M2 at Georgetown University, was our 2023 Nth Dimensions Summer Scholar. He had an interest in working with his hands and solving complex medical problems. He is motivated by the
In November, we hosted the inaugural Campbell Clinic-Nth Dimensions BioSkills Workshop for Memphis high school students. Led by the idea, “Teach me, show me, let me,” this was a handson opportunity to get exposure to the orthopaedic field, careers, industry, and equipment. This skills training event was hosted in collaboration with Nth Dimensions, Bridges, and Memphis-Shelby County Schools. Our sincere thanks to Zimmer Biomet for providing instrumentation for eight hands-on stations used by 80 students, to the Junior League of Memphis and QC Medical for funding, and to the Campbell Clinic physicians, residents and fellows, UTHSC medical students, and Foundation team members who volunteered their time.

idea of restoring patient function and ambulation as well as working with a broad population, from young patients with acute injuries to elderly patients with chronic ailments.
He was looking forward to building upon the mentoring relationship with Nth Dimensions and with his Campbell Clinic connections as he returned to his second year of Medical School at Georgetown as well as making new connections and adding to his orthopaedic research experiences.



During this half-day program, students had the opportunity to hear from physicians, rotate through skill stations, and network with diverse healthcare

professionals to learn careers in orthopaedics. We look forward to building on these new partnerships with more hands-on events in 2024.

Our Hearts to Your Soles returned to the Memphis Union Mission shelter. Campbell Clinic foot and ankle physicians and residents provided foot care and new shoes to community members experiencing homelessness or housing insecurity. We recognize that proper foot health is an essential part of everyday life, and it is important to an overall health maintenance program.
Vital support was provided by the Campbell Clinic Foundation and its orthopaedic surgery staff, fellows, residents, research nurses, physician assistants and employees, as well as Stryker representatives and UTHSC medical students. Footwear was donated by Red Wing Shoes. Socks, toiletries, and snacks were donated by generous Campbell Clinic employees.
Dr. David Richardson, foot and ankle sub-specialist, has led this for 16 years, and Angel Agus has been his

right hand, baking cookies, collecting supplies, and making sure we continue to provide great care to the Memphis Union Mission clients. Thank you to all who make this community event possible each year!


Since January 2018, the Campbell Clinic Foundation has led a comprehensive, multidisciplinary outpatient clinic focused on children with cerebral palsy in partnership with Le Bonheur Children’s Hospital, thanks to a transformational $1,000,000 commemorative grant from the Children’s Foundation of Memphis. The Center serves more than 425 patients and their families per year. Collaboration is underway with three other specialties at Le Bonheur (Pediatric Endocrinologists, Pediatric Pulmonologists, and Developmental Pediatricians) to research and develop clinical practice guidelines to serve the whole patient.



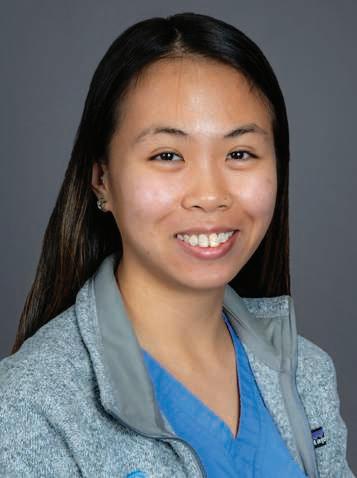
Under the talented, compassionate leadership of Campbell Clinic pediatric orthopaedic surgeons, Drs. William Warner, David Spence, and Stephanie Chen, a dedicated team of nurses, therapists, and subspecialty physicians strives to meet the unique needs of each patient. As the last five years have passed, the clinic reaches more patients, delivers more resources and identifies better ways to serve children and families seeking care at all functional levels.
We are incredibly grateful for generous support of individuals, families, and allies in children’s health, including Orthopediatrics, Center for Orthotics and Prosthetics, the Plough Foundation and Shelby County Board of Commissioners.


Your contributions to the CP Center ensure more patients will receive care and families will receive support. If you are interested in helping children with CP, contact Jenny Koltnow, Executive Director, Campbell Clinic Foundation at 901.759.3233 or jkoltnow@campbell-foundation.org.
A fundamental part of the UTSHC-Campbell Clinic Orthopaedic Surgery Residency training is service at Regional One Health. This Level 1 trauma center is a fast-paced, high-intensity environment in which the residents are exposed to vast orthopaedic injuries and conditions and quickly learn to work both autonomously and as a team.
Regional One has a constant deluge of high-energy complex trauma that is seen in few other places in the country. Dr. Chris Cosgrove explained that most trauma centers that consistently have this volume of work typically have a large number of orthopaedic

trauma fellows. “With only one fellow in our program, our residents are expected to achieve a high degree of surgical prowess. Nearly a quarter of their residency is spent at Regional One,” Cosgrove explains, adding that this comprehensive aspect is unique to the Campbell Clinic program. During each rotation, the residents are gradually exposed to various surgical techniques and, as they gain more experience, earn more autonomy.
Dr. David Cooper, Chief Resident, credits learning to perform surgery to the hands-on experience at Regional One. “It has made me a capable and competent surgeon. If you’ve not had this experience, when you get out (of residency) and are starting to practice, it could be a big adjustment,” Cooper said. “But I’m already very comfortable performing surgery.”
The challenging experience teaches skills and fundamentals that are applicable to any subspecialty. Residents perform early rounds with inpatients, develop

surgical plans, attend morning conferences, and perform surgery.
On-call residents typically work a 24- to 28hour shift, while those not on call usually spend 12 to 14 hours a day at Regional One.
Campbell Clinic residents encounter many different trauma situations daily including gunshot and knife wounds, high energy
car and motorcycle accidents, and industrial accidents. The large volume of patients forces the residents to stay organized and coordinate closely with other physicians. Dr. Clayton Wing, another PGY-5 resident adds, “this experience has helped me learn how to make clinical and operative decisions in stressful situations.”
The trauma program began in 1983, when Campbell Clinic under the leadership of Dr. Toney Russell (class of 1980) helped launch the Elvis Presley Trauma Center within Regional One. The center was modeled after the ground-breaking Shock-Trauma program at the University of Maryland Medical Center in Baltimore
“This was the first time that complex trauma could be referred to and treated by specialist surgeons who were trained, ready to go, and able to offer patients the best chance of survival and recovery,” Russell said.
Both uninsured and underinsured patients are served, many of whom have minimal access to health care and might have chronic illnesses as well.
Nancy Antone, 72, is one of our grateful Campbell Clinic trauma patients. She was working in her yard when she fell in late 2022, breaking the top of her right femur. During the next year, she underwent five surgeries—once to implant a metal rod, once to address an E.coli infection, a third operation to replace the incorrectly situated rod with an antibiotic one, a fourth operation to implant an all-new metal rod, then finally a knee replacement. After her original operation at Baptist-Desoto, Ms. Antone consulted with Dr. Marc Mihalko, then was under the care of Drs. Cosgrove and Gregory Dabov.
“It was a rough year,” said Ms. Antone, who was wheelchair bound and caught COVID during the ordeal. “I could have lost my leg. I could have lost my life if Dr. Mihalko had not seen the problem. I am so thankful to be walking.”

Five visiting fellows from the American Orthopaedic Foot and Ankle Society (AOFAS)
Traveling Fellowship Program visited Campbell Clinic in September to take part in a multi-day tour of the clinic and Memphis. The fellows represented five countries: Chile, United Kingdom, South Korea, Argentina, and Canada.
The fellows observed operating rooms and learned new surgical techniques alongside accomplished surgeons. In addition to giving fellows the opportunity to present their own research and clinical experiences, this collaboration promoted the exchange of ideas and new ways of thinking about research and clinical care topics.
After these orthopaedic sessions, the group explored
Memphis and enjoyed the many sights, sounds, and tastes of the city! Stops on the itinerary included a visit to St. Jude Children’s Research Hospital, the National Civil Rights Museum, and Central BBQ.

On October 13 and 14, the Campbell Clinic Foundation hosted the Inaugural Kinematic Knee Alignment Course in Memphis, directed by Program Chair Michael D. Hellman, MD and Course Chair, Campbell Clinic’s Marcus C. Ford, MD. Led by a star-studded faculty, the course featured didactic sessions, robust discussion, and cadaver labs with robot-assisted and nonrobot-assisted procedures.
Randomized controlled trials have shown superior clinical outcomes for kinematic alignment (KA) when compared to traditional mechanical alignment (MA) TKA. Now with reported excellent mid and longterm survivorship, KA is becoming a mainstream treatment option. Special thanks to our participants, faculty, generous supporters – especially presenters
Medacta and Zimmer Biomet – and meeting partner Broadwater.

The 2nd Annual KA Course will take place September 20-21, 2024, in Memphis, TN. Register early to receive early-bird discounts. Open to orthopaedic generalists, sports medicine, and lower extremity (LE) adult reconstruction subspecialists!
Sept. 20–21, 2024


COURSE CO-CHAIRS
Marcus C. Ford, MD
Michael D. Hellman, MD
PROGRAM CHAIR
Nicholas Brown, MD
ASST. PROGRAM CHAIR
Christopher T. Holland, MD
Registration and Meeting information: www.broad-water.com



The month-long American Shoulder and Elbow Surgeons (ASES) Asian Exchange Fellowship Program included stops at Cleveland Clinic, University of California San Francisco, the ASES Annual Meeting

After being delayed for three years, we were thrilled to finally host the 2020 SLAOTI Fellows Dr. Ana Laura Loyola Munhoz da Cunha from Curitiba, Brazil, and Dr. Gonzalo Chobadjian of Santiago, Chile. Our team facilitated two days in Memphis packed with meetings and demonstrations with residents and staff, tours through our beautiful community, and collaboration among new friends.
in Scottsdale, and Campbell Clinic! We were thrilled to welcome the fellows from South Korea, Jung Han Kim, MD and Sung-il Wang, MD.
“This prestigious fellowship brings two surgeons from Korea to visit selected shoulder and elbow centers in the U.S. every two years. Drs. Kim and Wang brought a wealth of knowledge, and we had a terrific exchange of ideas,” explains Thomas (Quin) Throckmorton, MD.
Tyler Brolin, MD, added, “A traveling fellowship such as this is invaluable, as this facilitates the sharing of thoughts and ideas from different institutions across the globe. We are humbled in their interest in visiting Campbell Clinic and allowing us to share our practice and thoughts on shoulder and elbow surgery."

We were honored to attend the POSNA Annual Meeting in Nashville in April. These meetings offered opportunities to connect with international orthopaedic leaders, reconnect with Campbell Residency and Fellowship alumni (some who traveled from as far as Alaska!) and stay apprised of the insights and innovations driving patient care.
Please join us in congratulating Campbell Pediatric Orthopaedic Surgeon Dr. Jeffrey Sawyer,
who concluded his term as the 39th president of the organization in April 2023. Dr. Sawyer was the third Campbell physician to serve in this esteemed role, following in the footsteps of Drs. Terry Canale and Jim Beaty. During this year's event, POSNA also honored Dr. Beaty as the Presidential Guest Speaker. Plus, Drs. Derek Kelly, Ben Sheffer, David Spence, Jeffrey Sawyer, and William Warner, Jr. presented their work on various pediatric conditions, treatments, and insights.
Backfilling with bone graft

and up to 8mm expansion

Hyperlordotic profiles up to 22°
3D printed endplates
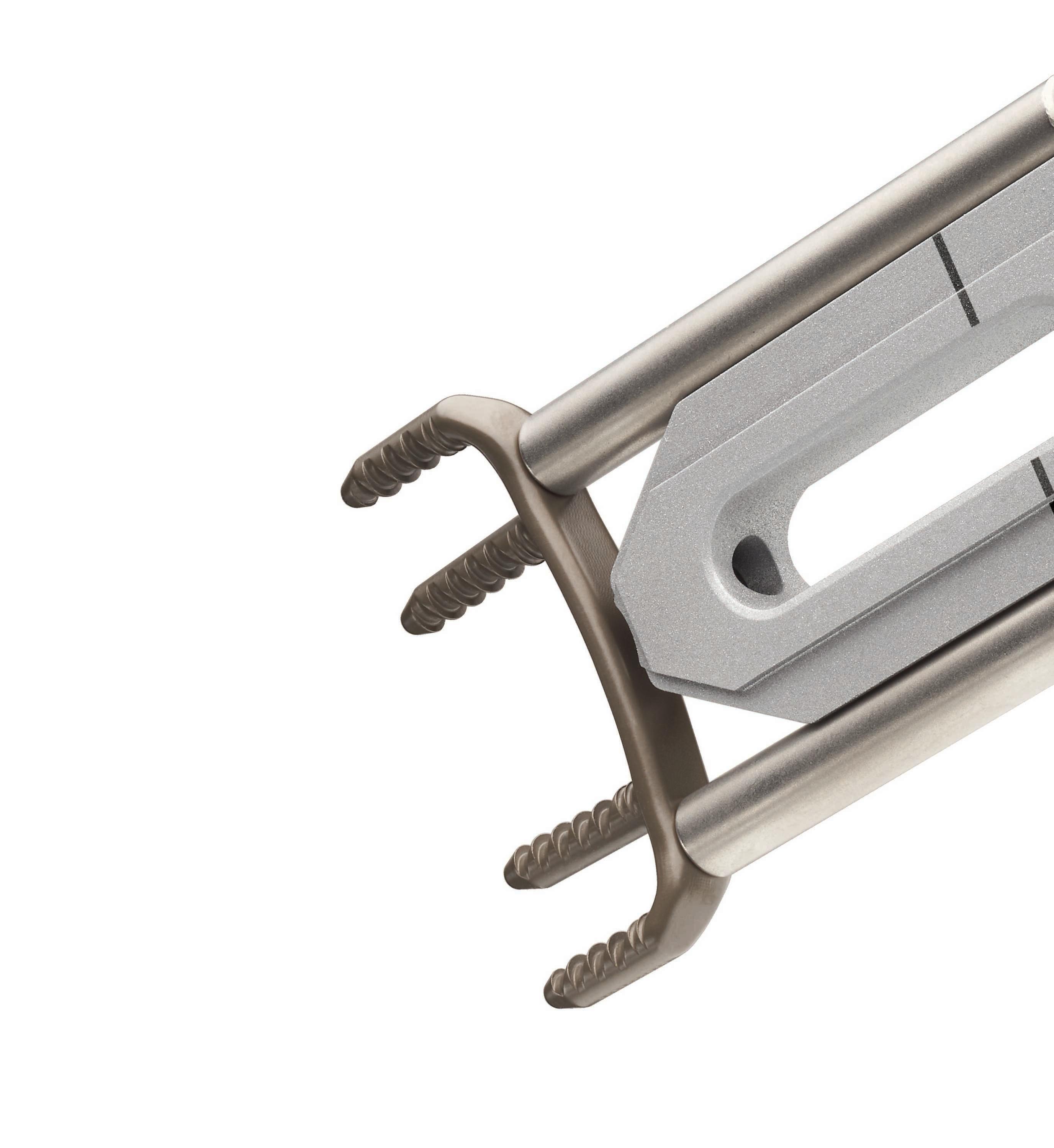
The innovative SABLE® Spacer is designed to enable sagittal correction without compromising a low starting height. Implant heights may be adjusted for each patient by expanding to fit their unique anatomy. SABLE® also features 3D printed titanium endplates and post-expansion bone graft packing to help promote fusion.


The study “Muscle Activation Patterns during Active External Rotation after Reverse Total Shoulder

During the 2023 American Association of Hip and Knee Surgeons (AAHKS) Annual Meeting, Campbell Clinic’s Marcus C. Ford, MD and William Mihalko, MD, PhD, were awarded the AAHKS Clinical Research Award for investigating the safety and clinical efficacy of extended postoperative tranexamic acid (TXA) use in total knee arthroplasty (TKA). Other contributors in this study were Mateo Kirwan, MD; Zachary R. Diltz, MD; Derek T. Dixon, BS; Carlos A. Rivera-Peraza, BS; Christal J. Gammage, PhD; James Harkess, MD; James Guyton, MD; and John Crockarell, MD.
Arthroplasty: An Electrophysiological Study of the Teres Minor and Associated Musculature was a study honored with the prestigious Charles S. Neer Award in March 2023. Campbell Clinic contributors include Thomas Throckmorton, MD; Tyler Brolin, MD; William Mihalko, MD, PhD; David Bernholt, MD; Frederick Azar, MD; former Sports Medicine Fellow William Polio, MD; and research manager, Margaret Knack. UTHSC contributors include Blake Hajek; Kunal Singhal, PhD; Shannon Hughes, PhD; Alexis Nelson; Chi-Yang Chiu, PhD; and Tristan Hayes. The Neer Award was presented during the American Shoulder & Elbow Surgeons Specialty Day during the American Academy of Orthopaedic Surgeons Annual Meeting.



Elevating mobility. Enriching lives. Your partner in extremity solutions.





Robert T. Trousdale, MD
Consultant, Department of Orthopedic Surgery, Mayo Clinic College of Medicine
Professor of Orthopedics, Mayo Clinic College of Medicine
Master’s Faculty Privileges in Orthopedic Surgery, Mayo Clinic Graduate School of Biomedical Sciences, Mayo Clinic College of Medicine and Science

Dr. Robert T. Trousdale of Mayo Clinic College of Medicine was the second annual Visiting Professor to be sponsored by the James W. Harkess, MD Total Joint Education Fund.
Dr. Trousdale spoke last June to surgeons, residents and medical students. Case discussions took place in the afternoon, followed by dinner and lecture. The Harkess Fund honors the lifetime contributions made by Campbell Clinic’s Dr. James W. Harkess, who specializes in total joint replacement.
Dr. Trousdale has taught at Mayo Clinic College of Medicine since 1992. A University of Notre Dame
graduate, he received his medical degree from St. Louis University School of Medicine, interned at the Mayo Graduate School of Medicine, then completed fellowships in adult reconstruction at Mayo Graduate School of Medicine and M.E. Müller Foundation in Bern, Switzerland.
His honors include two Mark B. Coventry Clinical Research Awards and a Frank Stinchfield Award from the Hip Society. He is a former president of the Knee Society.
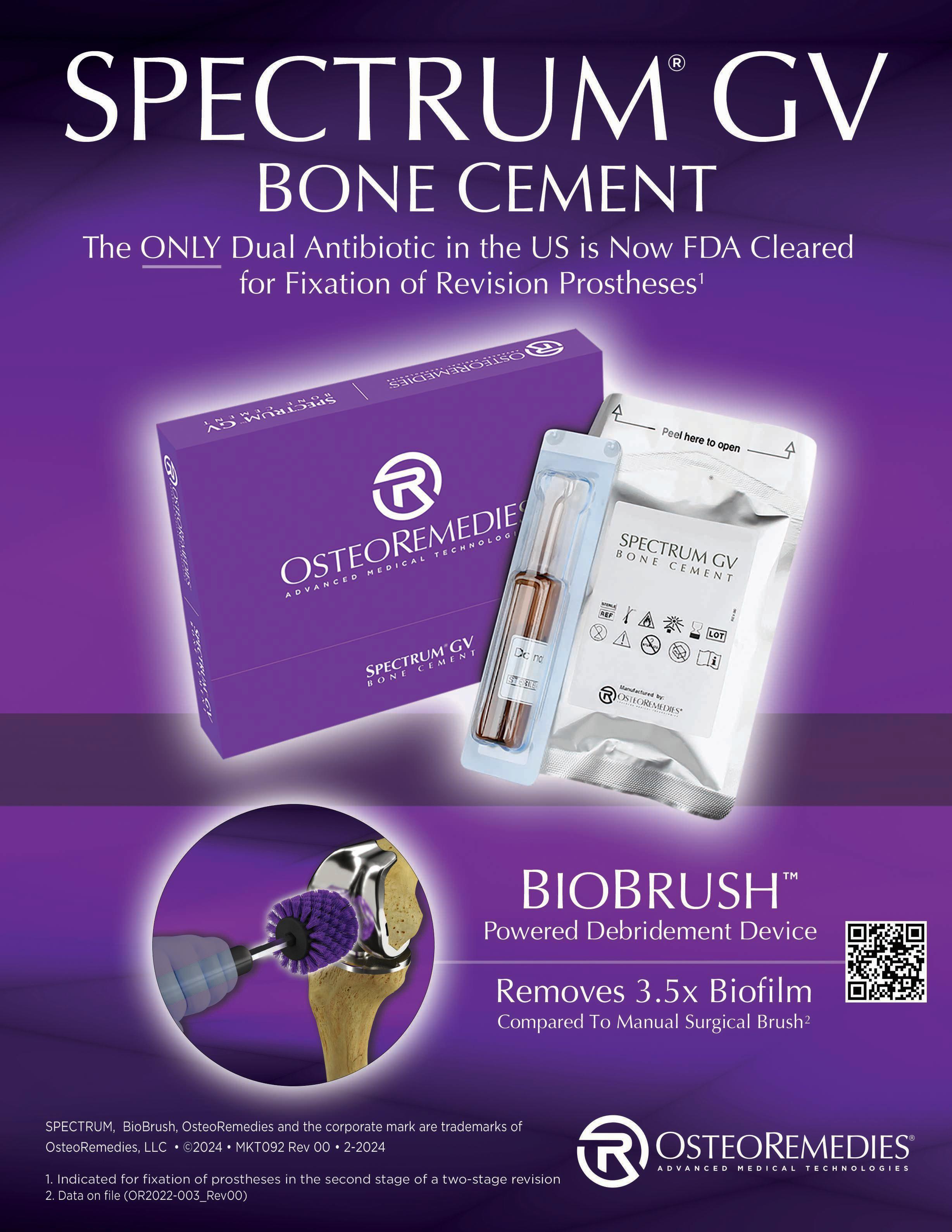
Thank you to Dr. Marcus Ford, who has led the Harkess Fund initiative; Dr. Jim Guyton, who helped facilitate last year’s program; and our generous partners, including OsteoRemedies and Stryker.
Daniel J. Sucato, MD, MS
Chief of Sta , Scottish Rite for Children
Professor of Orthopaedic Surgery, The University of Texas Southwestern Medical Center

Dr. Daniel J. Sucato was featured on Feb. 8 as the James H. Beaty MD Pediatric Orthopaedics Visiting Professor.
After graduating magna cum laude from Canisius College, Dr. Sucato received his medical degree
and a master’s degree in biophysics from the State University of New York School of Medicine at Buffalo. He finished his general surgery internship, orthopaedic residency and basic science research fellowship at the SUNY School of Medicine, then completed the Dorothy and Bryant Edwards Fellowship in Pediatric Orthopaedics and Scoliosis at Scottish Rite for Chil-
dren and the Hip-Preservation Fellowship at the University of Bern, Switzerland. He stayed on at Scottish Rite as a staff orthopaedic surgeon in 1998. In 2003, he was selected as one of three International Traveling Fellows for the Scoliosis Research Society (SRS) traveling throughout Europe for three weeks.
Dr. Sucato’s clinical practice focuses primarily on spinal deformity and hip conditions, with an emphasis on complex cases and reconstructions. He has presented and written extensively on a number of these techniques. His research focuses on clinical studies primarily but also those involving improved operative techniques. Dr. Sucato has published over 220 scientific peer-reviewed articles and 50 book chapters, and
has given over 300 presentations at national/international meetings and 45 visiting professorships.
He has been awarded the Angelo S.M. Kuo Memorial Award, the Best Clinical Paper Award through POSNA and both the Russell I. Hibbs and Louis A. Goldstein Award at the SRS meetings. He is a member of several research study groups including ANCHOR (Academic Network of Conservational Hip Outcomes Research), and the Fox and Harms Study Groups. He chaired the Pediatric Section of the Spine Deformity Study Group (SDSG) during its last 3 years.
Dr. Sucato currently is the President of the Pediatric Orthopaedic Society of North America.
Anthony Miniaci, MD
Deputy Chief Medical Executive, Baptist Health Orthopedic Care
A liate Professor Orthopedic Surgery, Florida Atlantic University Schmidt College of Medicine

Anthony Miniaci, MD served as our 2024 esteemed Visiting Professor on March 8. He is an orthopaedic surgeon specializing in sports medicine and shoulder and knee surgery with Baptist Health, and the deputy chief medical executive of Baptist Health Orthopedic Care. As the son of Italian immigrants to Canada, Dr. Miniaci is fluent in English and Italian. He has produced many internationally recognized scientific papers, patents, and presentations with a vast career in orthopedic research and development. Dr. Miniaci’s patented technology offers patients a less invasive shoulder surgery using industry-leading hardware uniquely designed for the complex shoulder joint.
At Baptist Health, he leads a growth and integration of a team of surgeons actively involved in clinical and basic science research to improve patient outcomes worldwide. From 2003-22, Dr. Miniaci worked for Cleveland Clinic’s Center for Sports Health in
Cleveland, OH and Cleveland Clinic’s Sports Medicine Clinic in Toronto, Canada. He was also an orthopaedic surgery professor at the University of Toronto and Case Western Reserve University. Dr. Miniaci has treated high-profile Olympic and professional athletes, including players from the National Hockey League, National Football League, and Major League Baseball. He has been the head team physician for the Cleveland Browns and an orthopaedic consultant to the Toronto Blue Jays.
Dr. Miniaci has received many awards, including the 2022 Alumni of Distinction award from the University of Western Ontario, where he received his medical degree. After completing his residency there, Dr. Miniaci served a fellowship at Kerlan-Jobe Orthopaedic Clinic. As chairperson of the American Shoulder and Elbow Surgeons Foundation, Dr. Miniaci led the creation of the National Shoulder and Elbow Health Week. He is Vice President of the American Shoulder and Elbow Surgeons, and will be its President in 2025-2026.
The Campbell Clinic Foundation offers exceptional training and experience to newly minted orthopaedic surgeons through five distinct 12-month subspecialty fellowships each year: Foot and Ankle (two Fellows); Hand; Trauma; Pediatric Orthopaedics; and Shoulder and Sports Medicine. The Foundation and Campbell Clinic also partner with the University of Tennessee Health Science Center to offer a Primary Care Sports Medicine Fellowship program.
Fellows have specific clinical, hospital, and surgical duties and are introduced to the latest techniques and innovations within their subspecialty. Each fellow gets significant operative and clinical experience, thanks to considerable time spent with subspecialty faculty members and both junior and senior residents throughout the year. Sub-specialty courses and cadaveric labs augment the hands-on and didactic experience.
Fellows are encouraged to pursue research during their training year with support from the Campbell Clinic Foundation, including research scholars, clinical research coordinators, a full-time librarian, a statistician, and editorial support. This allows fellows to
study important aspects of orthopaedic research and collaborate with sites locally and nationally. From retrospective record reviews to prospective, randomized clinical trials, Fellows engage in myriad musculoskeletal studies and innovations.
The Campbell Clinic Foundation Fellowship programs receive funding from the OMeGA Medical Grants Association, Arthrex, Smith + Nephew, Skeletal Dynamics, Arthroscopy Association of North America, and the American Orthopaedic Foot and Ankle Society, in addition to generous local partners, which support Fellows training and academic activity. We are very grateful for this support. To learn more, check out https://campbell-foundation.org/surgeon-education.
Clayton C. Bettin, MD, Assistant Professor, Director of Foot and Ankle Fellowship
Two fellows spend 5 days each week with the Foot and Ankle staff, gaining exposure to acute and reconstructive surgery of the foot and ankle and advanced knowledge about clinical nonsurgical problems. The fellowship is focused on education (as opposed to routine clinical tasks), with ample time for reading and research. Fellows perform all procedures, and the training locations include Baptist Memorial Health Care, Methodist Le Bonheur Healthcare, Regional One Health, and Campbell Clinic Surgery Centers.

Hometown: El Dorado, AR
Undergraduate Institution:
University of Arkansas-Fayetteville
Medical School: University of Arkansas for Medical Sciences
Orthopaedic Residency: University of Arkansas for Medical Sciences
Personal: Dr. Henry met his wife
Jordan in high school. They have two sons: Wyatt Hayes, 2; and Brooks Anthony, 6 months. Hobbies: Grilling/smoking, hunting, working on cars, spending time with family/friends
Asked why he chose medicine as a career: “It’s a perfect blend of science and humanity. Medicine appealed to my interest in how things work and lets me work with people daily.”
And why he chose orthopaedics as a specialty: “I enjoy the challenge and variety of surgery. The instant gratification from preoperative and postoperative X-rays plays to my need to see the effects of my work.”
Favorite memory of fellowship: “I love the camaraderie with my co-fellows and staff. It really feels like a team approach to patient care and learning.”
Research activities: Exploring radiation exposure of surgeons with mini-c versus large c-arm Plans after Campbell: Dr. Henry is going to join OrthoArkansas in Little Rock.
Dr. Henry adds: “I have had a great time. Thank you to the staff for the excellent operative experience and training. Thanks to the residents for their help, which has helped me focus on operating. And thanks to my co-fellow for being a great partner and another resource during training.”
Hometown: Liberty, MO
Undergraduate Institution: University of Kansas
Medical School: University of Kansas
Orthopaedic Residency: Loyola University-Chicago
Personal: His father is a general/ trauma surgeon in Kansas City. Dr. McGregor met his wife Liz through a mutual friend during their junior year in high school; they have three children: Lola, 5; Max 3; and Meryl, 9 months.
Hobbies: “Cooking, using kettlebells, watching KC Chiefs football and Kansas Jayhawks sports, chasing my kids around.”
Asked why he chose medicine as a career: “I saw the tangible effect that good medicine can have on people’s lives by watching my Dad and his patients, and knew that it would be a meaningful profession.”
And why he chose orthopaedics as a specialty: “It’s a unique combination of hammering things and science.”
Favorite memory of fellowship: Working with the “awesome” foot-and-ankle staff.
Research activities: Investigating outcomes in Charcot reconstruction Plans after Campbell: Dr. McGregor will be joining OrthoKansas in Lawrence, KS
Dr. McGregor adds: “Thank you to the foot-and-ankle staff for their invaluable knowledge and to the Campbell Clinic residents for all of their hard work.”
Norfleet B. Thompson, MD, Assistant Professor, Hand Program Director
This fellowship focuses on hand surgery and hand conditions, with extensive exposure to surgical management of acute and reconstructive upper-extremity procedures as well as education about clinical nonsurgical problems. Hospital and surgical experiences span various facilities, including Baptist Memorial Health Care, Methodist Le Bonheur Healthcare, Regional One Health, and Campbell Clinic Surgery Centers.
JARED BELL, MD
Hometown: Lucas, TX
Undergraduate Institution:
University of Texas at Austin
Medical School: Texas Tech
University – Paul L. Foster School of Medicine
Orthopaedic Residency: University of Florida Health - Jacksonville
Personal: Dr. Bell met his wife
Lindsey when they were microbiology lab partners in undergraduate school. She is a Certified Registered Nurse Anesthetist.
Hobbies: Hiking, golf, horseback riding, playing lacrosse
Asked why he chose medicine as a career: “While growing up, I was always the curious one, fascinated with the intricacies of biology. This innate curiosity, combined with the desire to help others, led me to choose medicine – a field where every day is an opportunity to learn, evolve, and positively impact someone’s life.”
And why he chose orthopaedics as a specialty: “I chose orthopaedic surgery because of its rewarding ability to restore function and autonomy to a person’s life. Additionally, I was drawn to the intricate anatomy of
the musculoskeletal system. The precision required to navigate bones, tendons, ligaments, and neurovasculature appealed to my meticulous nature. This combination of making a direct impact on someone’s life and the continual exploration of our body’s mechanics makes every day in this profession rewarding.”
Favorite memory of fellowship: “The camaraderie I shared with the residents and faculty. Their friendship, support and genuine interest in teaching the next generation of surgeons has had a lasting impact on me.”
Research activities: “I co-authored articles entitled, ‘Pitfalls of Difficult Distal Radius Fractures and Provisional Reduction,’ ‘Surgical Considerations for Osteoporosis, Osteopenia, and Vitamin D Deficiency in Upper Extremity Surgery,’ and ‘Maintaining Professionalism in the Difficult Patient Interaction.’ ” Also conducted a cadaveric study outlining the anatomy and feasibility of hand-denervation procedures.
Plans after Campbell: “I’m going to serve active duty in the U.S. Air Force.”
Dr. Bell adds: “I am grateful to the Campbell Clinic faculty, staff and residents for their mentorship, patience, and countless shared moments.”
Derek M. Kelly, MD, Professor, Director of Pediatric Orthopaedic Fellowship
This ACGME- and POSNA-accredited fellowship program combines clinical training and research, preparing surgeons for a career in both private practice and academic settings. The fellowship offers extensive exposure to trauma, scoliosis, clubfoot, hip diseases, limb deformities, tumors, hand and upper-extremity conditions, sports orthopaedics, metabolic and genetic conditions, neuromuscular disorders, cerebral palsy, myelomeningocele, degenerative diseases, congenital conditions, and other conditions that affect the spine, hip, foot and ankle, and hand. Training locations include Le Bonheur Children’s Hospital and Campbell Clinic.

Hometown: Venezuela, Portuguesa
Undergraduate Institution: None
Medical School: Occidental University Center Lisandro Alvarado, Venezuela
Orthopaedic Residency: Hospital Central Maracay, Venezuela
Personal: Dr. Pargas is the first doctor in his family. He met his wife, Carolina Zuluaga, at a Christmas Party in 2013. She works in business administration at Capital One. They have two children: Amanda, 5; and Alan, 2.
Hobbies: Playing team sports such as basketball and baseball, traveling
Asked why he chose medicine as a career: “It’s an appropriate way to help others, and a prestigious
profession with much room for practice globally.”
And why he chose orthopaedics as a specialty: “The musculoskeletal system plays a major role in every activity in our lives, especially sports.”
Favorite memory of fellowship: “The awesome teamwork and chemistry between everyone. Working with residents always is a fantastic experience as they grow to become young attendings.”
Research activities: Supra-patellar Approach Experience on Tibial Shaft Fractures Treated with Intramedullary Rigid Nail in Patients with Open Physis
Plans after Campbell: Dr. Pargas plans to practice at an academic institution in the United States.
Dr. Pargas adds: “Keep working as a unit. Fellows, take advantage of the multiple cases and staff’s wide medical knowledge and experience.”
Frederick M. Azar, MD, Professor, Director of Sports Medicine Fellowship
Tyler J. Brolin, MD, Assistant Professor, Associate Program Director
The Sports Medicine and Shoulder Surgery Fellowship combines 6 months of Sports Medicine education with 6 months of Shoulder and Elbow training. This hybrid program exposes each fellow to a breadth of pathology of the knee, shoulder, and elbow and focuses on all aspects of arthroscopic shoulder, knee, and elbow surgery with special emphasis on shoulder arthroplasty, open shoulder instability, multi-ligamentous knee reconstruction, as well as complex patellofemoral reconstruction. Fellows also gain training in hip arthroscopy, hip preservation, pediatric sports medicine, and are exposed to all aspects of practice management including formal training in billing and coding. A major part of the fellowship is the opportunity to participate in clinics, team, and event coverage for the Memphis 901 FC (US Soccer League), Memphis Showboats (US Football League), Memphis Redbirds (AAA baseball), Division I, II, and III collegiate teams as well as high school teams.

ROBERT AMADI ACHILIKE, MD
Hometown: Dallas, TX
Undergraduate Institution:
Washington University
Medical School: UT Southwestern
Medical Center
Orthopaedic Residency: University of Arkansas for Medical Sciences
Personal: Dr. Achilike’s oldest sister is a staff anesthesiologist.
Hobbies: Basketball, weightlifting, beach volleyball, singing, salsa dancing
Asked why he chose medicine as a career: “It seemed like the best way to combine my love for science and desire to help people.”
And why he chose orthopaedics as a specialty: “As a recreational athlete, I’ve torn my Achilles tendon. I want to be able to help people return to active lives.”
Favorite memory of fellowship: Helping the University of Memphis Tigers on the sidelines during football games.
Plans after Campbell: Working for a private group in Texas Dr. Achilike adds: “I’m thankful to all the faculty and OR staff for teaching me so much over a short period of time.”
John C. Weinlein, MD, Associate Professor, Director of Trauma Fellowship
The trauma fellow receives comprehensive experience at a high-volume Level 1 trauma center that serves as a referral facility for Tennessee, Arkansas, Mississippi, Missouri, and Kentucky, with four orthopaedic traumatologists on staff. This program is primarily focused on the operative and nonoperative management of complex polytrauma, including pelvic, acetabular, and periarticular fractures; reconstructive fracture management, including nonunions, malunions, and deformity correction; and clinical investigation and research, which provides extensive operative exposure of complex fractures with an emphasis on pelvic and acetabular injuries. Interaction with two orthopaedic trauma teams includes daily morning report/fracture conferences, after which the fellow has first choice of operative cases in a minimum of three orthopaedic trauma rooms. The fellow has opportunities to pursue additional areas of interest, including total joint replacement for fracture, advanced soft tissue coverage procedures, and deformity correction.

Hometown: Flagstaff, AZ
Undergraduate Institution: University of Arizona
Medical School: Indiana University
Orthopaedic Residency: Indiana University
Personal: Dr. Wallentin-Flores’ father is a family practitioner. He and his wife Emily were friends in high school and started dating during undergraduate school. She is a speech-language pathologist. They have two children: Jack, 6; and Eliza, 4.
Hobbies: Enjoying the outdoors
Asked why he chose medicine as a career: “To use my opportunities, knowledge and skill to help and comfort people during some of the most trying moments of their lives.”
And why he chose orthopaedics as a specialty: “There’s nothing better. I get to work with my hands and help people regain function and return to their lives.”
Favorite memory of fellowship: “Getting to know all of the residents and working with great faculty.”
Plans after Campbell: "We will be moving back to Flagstaff, AZ."
Dr. Wallentin-Flores adds: “Thanks to all of the residents and staff for being so welcoming and enjoyable. Special thanks to all my interns for helping me get through the craziness.”
John C. Hyden, MD, Assistant Professor of Family Medicine, Director, Primary Sports Medicine Fellowship
The Campbell Clinic/UTHSC Primary Care Sports Medicine Fellowship’s mission is to train physicians from primary specialties in the art and science of musculoskeletal and sports medicine, encompassing the science and clinical application of exercise physiology, kinesiology, nonoperative orthopaedics, cardiology, and general medicine applied to the care of the active person. It also trains physician specialists who understand, advance, and apply evidence-based medicine in the psychosocial, environmental, and physiologic milieu of athletic training and competition from the pediatric to the elite.

Hometown: Smithtown, NY
Undergraduate Institution: Florida State University
Medical School: St. George’s University
Family Medicine Residency: University of Tennessee Health Science Center (St. Francis)
Personal: Dr. Chaloupecky met his significant other, Ashley, at church. She is a graphic designer.
Hobbies: Bonsai, travel, baseball
Asked why he chose medicine as a career: “I wanted to help people.”
And why he chose orthopaedics as a specialty: “I played sports growing up and wanted to make a career out of helping athletes and people with similar injuries.”
Favorite memory of fellowship: Covering various sporting events around Memphis
Research activities: Frozen Shoulder study with Dr. Beard and Dr. Lamplot.
Plans after Campbell: Will be practicing Primary Care Sports Medicine in Jacksonville, Florida.
Dr. Chaloupecky adds: “Thank you to Campbell Clinic and Drs. Azar, Hyden, Beard, Owen, Gilbert, Mancell, Brandon, and Quirolgico for accepting me as one of their own and helping me grow as a physician.”


What if we had a confidential partner to help us manage pain points and support peak performance?
Whether addressing challenges or achieving goals, working with a coach that really gets us shouldn’t just be for high-performance athletes and c-suite executives.

The annual Alvin J. Ingram, MD Memorial Lecture was begun to honor the memory of a former Campbell Clinic Chief of Staff and department chairman who had a larger-than-life presence among his colleagues.
“Alvin Ingram was a thoughtful and very well-respected man,” said Dr. James H. Beaty, who worked under the Jackson, TN native as an orthopaedic resident and during Ingram’s last two years at Campbell Clinic. “He was my mentor, role model, and the reason I went into pediatric orthopaedics.”
Beaty described Ingram as a great leader who was President of everything from the Memphis and Shelby County Medical Society to the American Orthopaedic Association, Pediatric Orthopaedic Society of North America, American Academy for Cerebral Palsy, American Orthopaedic Association, and American Board of Orthopaedic Surgery.
“Dr. Ingram was the kind of person who, when he spoke, people listened,” Beaty said. “He was a consensus builder, but he could make a decision when it needed to be made. He was a wonderful leader in every way.”
Dr. Ingram attended Union University before receiving a bachelor of science degree from the University of Tennessee-Knoxville, then proceeding to UT-Memphis for his medical degree. A graduate of the University of Tennessee-Campbell Clinic’s residency program, Ingram was medical director of the Crippled Children’s Hospital and a world authority on polio treatment. He died in 1999 at age 85.
The lecture in Ingram’s honor highlights achievements in surgeon education and features a distinguished visiting professor and presentations from the Campbell Clinic Foundation graduating residents. Since 2014, under the guidance of Course Director Derek M. Kelly, MD, the lecture has expanded to include talks by a distinguished professor, faculty, and an expert panel.
Two renowned Philadelphia orthopaedic surgeons are the keynote speakers for the Ingram Memorial Lecture this year.

Kelly IV
Dr. John D. Kelly IV is director of Shoulder Surgery, Sports Medicine at the University of Pennsylvania, co-director of the university’s Sports Medicine Fellowship Program, coordinator of its medical school’s Musculoskeletal Exam Module, and an orthopaedic surgery instructor at Temple University Hospital. In addition, Dr. Kelly is an attending surgeon at Philadelphia Veterans Affairs Medical Center and a consultant to Shriners Hospital for Children, Philadelphia.
His numerous honors include being named a Top Doctor by U.S. News and World Report, Main Line Today, Philadelphia Life/Suburban Life, Philadelphia Magazine, and Castle Connolly; receiving a Torg Award from Philadelphia Sports Congress, and an AAOS Achievement Award. Dr. Kelly is the Second Vice President of the Arthroscopy Association of North America (AANA).
After graduating from Columbia College, Dr. Kelly attended University of Cincinnati College of Medicine, then served his residency at the Hospital of University of Pennsylvania and completed a sports medicine fellowship at Temple University Hospital. Dr. Kelly has been a contributing writer to orthopaedic textbooks published by McGraw Hill, AAOS, Thieme Publishers, Boston Med Publishing, W.B. Saunders, Lippincott Williams and Wilkins, Springer, and Wolters Kluwer. He also has been a Food and Drug Administration consultant, columnist for New Jersey Golf Magazine, editor of Arthroscopy Association of North America’s Newsletter, and a stand-up comedian who has appeared on Oprah Radio and Dr. Oz.

Dr. Javad Parvizi MS, FRCS
Dr. Javad Parvizi MS, FRCS is the James Edwards Professor in Orthopedic Surgery at Jefferson Medical College, Thomas Jefferson University in Philadelphia, where he is also Vice Chairman of Clinical Research. He specializes in pelvis, hip, and knee reconstruction, with a special interest in hip pain in young adults and joint preservation procedures.
Dr. Parvizi graduated from the University of Sheffield, then performed a fellowship at Royal College of Surgeons of England. He completed his surgical training at Mayo Clinic in Rochester, MN and fellowship training in Bern, Switzerland. He is president of the American Association of Hip and Knee Surgeons and former president of the Eastern Orthopaedic Association and Musculoskeletal Infection Society. Dr. Parvizi, who has lectured internationally, holds 10 patents for orthopaedic treatments.
His many honors include a Clinical Research Award from the American Association of Hip and Knee Surgeons, Researcher of the Year from the Arthritis Foundation, and a Mark Coventry Award for Excellence in Clinical Research.
We are proud that the Ingram legacy includes the following list of esteemed leaders in the orthopaedic community who have served as Distiguished Professor:
TERRANCE PEABODY, MD
Edwin W. Ryerson Professor & Chairman
Northwestern University Feinberg School of Medicine
2015
J. LAWRENCE MARSH, MD
Chairman, Professor
Residency Director, Carroll B. Larson Chair
Department of Orthopaedic Surgery
University of Iowa Hospitals & Clinics
2016
WILLIAM J. MALONEY, MD
Elsbach-Richards Professor in Surgery
Chair, Stanford University School of MedicineOrthopaedic Surgery
2017
DAVID A. HALSEY, MD
Medical Director, Adult Reconstructive Surgery
Professor, University of Vermont College of Medicine
2018
KRISTY L. WEBER, MD
Chief, Orthopaedic Oncology
Department of Orthopaedic Surgery
Perelman School of Medicine
University of Pennsylvania
2019
JOSEPH A. BOSCO, III, MD
Professor & Vice Chair
Department of Orthopaedic Surgery
NYU Langone Health


DANIEL K. GUY, MD, FAAOS
Emory Southern Orthopedics
Medical Director, Emory Surgery Center at LaGrange
2021
FELIX "BUDDY" SAVOIE, MD
Ray J. Haddad Professor of Clinical Orthopaedics
Chief of the Division of Sports Medicine
Tulane School of Medicine
Director, Tulane Institute of Sports Medicine
2022
AMY L. LADD, MD, FAOA, FAAOS
Elsbach-Richards Professor of Surgery, Stanford University School of Medicine; Vice-Chair of Academic Affairs, Department of Orthopaedics; Chief, Chase Hand & Upper Limb Center; Assistant Dean for Medical Student Advising
MICHAEL L. PARKS, MD
Associate Professor of Clinical Orthopaedic Surgery at Weill Cornell College of Medicine; Associate Attending at the Hospital for Special Surgery
ANNUNZIATO (NED) AMENDOLA, MD, FRCS(C), DABOS
Virginia Baker-Flowers Distinguished Professor & Vice Chair of Department of Orthopaedic Surgery, Duke University; Division Chief of Sports Medicine; Director of Urbaniak Sports Sciences Institute; Chief Medical Officer of Duke Athletics
In support of improving patient care, this activity has been planned and implemented by Medical Education Resources (MER) and Campbell Clinic Foundation. MER is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Thank you to the partners who support the Alvin J. Ingram Memorial Lecture in its commitment to provide continuing education to physicians and health professionals dedicated to excellence in orthopaedics.














University of Tennessee Health Science Center-Campbell Clinic
Department of Orthopaedic Surgery and Biomedical Engineering Residency Program
The year 2024 marks the 100-year anniversary of the Campbell Clinic Orthopaedic Surgery Residency. From the brace-and-buckle days through world wars through the advent of outpatient surgery, Campbell Clinic-trained orthopaedic surgeons have been pioneers, leaders and role models in our field. The contributions of both faculty and alumni—too numerous to list here—include international medical society presidencies, globally-recognized publications and, most importantly, exceptional patient care. At the heart of this century of success is commitment to education and lifelong learning.
As we celebrate the accomplishments and milestones, we also look forward to exciting developments underway to continue achieving excellence in resident education.
This year marked the return to in-person residency program interviews. After three years of virtual interviews due to the COVID pandemic, in-person interviews allowed us to showcase our greatest assets: our residents, attending surgeons, administrators, research team, and facilities. The updated interview experience included an orientation and BBQ dinner on Thursday evening followed by a social at Bosco’s with our residents to learn about Memphis and the Campbell Clinic. Friday interviews consisted of five separate small groups interviews,
followed by a tour of the Campbell Clinic Wolf River and Germantown campus. The experience concluded with a bus tour to see where residents work, live, and socialize. Through this entire process, applicants gained a better perspective of and appreciation for the Campbell residency.
Recently, the educational programs have expanded to include more simulated surgery and cadaveric
dissections. Each year in July, staff and senior residents facilitate a casting and splinting workshop for junior residents. All first-year residents complete a series of modules on arthroscopy simulators for shoulder, knee, and hip at the UTHSC CHIPs simulation laboratory.
Thanks to industry partners aligned with our mission, we have expanded laboratory experiences for residents. In October, OrthoPediatrics hosted a pediatric orthopaedic sawbones and supracondylar humeral fracture laboratory at Le Bonheur Children’s Hospital. Arthrex and Gentleman Orthopedic Solutions hosted residents for upper extremity cadaver surgical dissection led by Drs. Jake Weller and Tyler Brolin for shoulder and elbow arthroscopy and approaches for arm, forearm, wrist, and hand fracture care. Medacta and the MORE institute hosted residents at the Medical Education and Research Institute (MERI) to study approaches to the spine with Dr. Chad Campion. And in November, Smith + Nephew hosted residents with Drs. Chris Cosgrove, David Bernholt, Michael Beebe, and Matthew Rudloff to study lower-extremity surgical approaches.
The Campbell Clinic Foundation introduced the Residency Resource Network (RRN) to help attract and recruit diverse medical students interested in orthopaedic residency and foster relationships among prospective residents, current residents, and alumni. All candidates invited to interview with the Campbell Clinic program were encouraged to participate in the RRN to be matched with residents or alumni based similar interests. Through this effort, we paired applicants with those who have walked through our residency with similar experiences and backgrounds, from military service to ethnicity. More than 75 alumni volunteered to help, which is a remarkable testament to the mentorship model that has distinguished Campbell Clinic for a century!
The Campbell Clinic Foundation is also committed to offering residents more educational travel experiences. With the generous support of the Willis C. Campbell Club alumni board, residents attend
various hands-on sub-specialty courses, medical board prep programs, and leadership development symposia, all which augment surgical skills and clinical competencies.
Thanks to the generosity of Baptist Memorial Health Care, all PGY-5 residents receive full scholarships to attend the Miller Board Review Course each May. This intensive five-day course prepares senior residents for their board exams which take place immediately after graduation and before their fellowship year begins. Since 2022, the Campbell Clinic Foundation has provided scholarships for all PGY-1 residents to attend the Orthopaedic Trauma Association Fracture Basics course. This 3-day program includes rapid-fire series of mini-lectures, an extensive open case-based discussion, video demonstrations of techniques, and hands-on skills lab exercises that collectively equip interns with critical skills and perspective as they enter their second year of residency.
Chief Resident, Dr. Cole Skinner, shared after the American Academy of Orthopaedic Surgeons Annual Meeting, “The AAOS 2024 meeting was an incredible experience for continued learning and networking. The ICLs, paper sessions, and sponsored events were thought-provoking and informative. I enjoyed the opportunity to visit with old friends and mentors as well as meet new orthopaedic colleagues from across the country. I would like to thank the Campbell Clinic, the Campbell Clinic Foundation, and our sponsors and donors for supporting my participation!”
A huge thank you to our Campbell Clinic Education Committee, Residency Director, Dr. Derek Kelly and Assistant Residency Director, Dr. Clayton Bettin, for their leadership, vision and commitment to continued growth and excellence.
If you are interested in supporting resident education, either through hands-on experiences or by providing travel scholarships, contact Jenny Koltnow, Executive Director, Campbell Clinic Foundation at jkoltnow@campbell-foundation.org or 901.759.3233 to learn more!

Andrew J. Couture, MD
Undergraduate: University of Central Arkansas
University of Arkansas for Medical Sciences College of Medicine

Matthew R. Colatruglio, MD
Undergraduate: The Ohio State University Medical: Ohio State University College of Medicine

Stanley C. Eboh, MD
Undergraduate: Texas Tech University Medical: Texas Tech University Health Sciences Center

Stefan J. Hanish, MD
Undergraduate: University of CaliforniaLos Angeles Medical: University of Missouri-Columbia School of Medicine

Nolan D. Farrell, MD
Undergraduate: The Ohio State University
Ohio State University College of Medicine

Lauren A. Foropoulos, MD
Undergraduate: University of Mississippi Medical: University of Tennessee Health Science Center College of Medicine

Thomas J. Iorio, MD
Undergraduate: University of Tennessee Medical: University of Tennessee Health Science Center

Joshua C. Hutchinson, MD
Undergraduate: Clemson University Medical: Medical University of South Carolina College of Medicine

Andrew D. Gailey, MD
Undergraduate: Tulane University
University of North Carolina at Chapel Hill School of Medicine

Paul T. Greenfield, MD
Undergraduate: Rice University Medical: Emory University School of Medicine

Dylan S. Koolmees, MD
Undergraduate: University of California Medical: Wayne State University School of Medicine

Joseph R. Johnson, MD
Undergraduate: Brown University Medical: Stanford University School of Medicine

Brenton R. Jennewine, MD
Undergraduate: Case Western
University
University of Virginia School of Medicine

Evan P. Johnson, MD
Undergraduate: University of South Florida Medical: University of Central Florida College of Medicine

Kailey L. Mansour, MD
Undergraduate: University of Florida Medical: University of Miami Leonard M. Miller School of Medicine

Brent V. Scheckel, MD
Undergraduate: Lindenwood University Medical: University of Tennessee Health Science Center

Andrew D. Nahr, MD
Undergraduate: Newman University Medical: University of Kansas School of Medicine

Mateo J. Kirwan, MD
Undergraduate: University of Kansas Medical: University of Kansas School of Medicine

William G. Murphy, MD
Undergraduate: Rhodes College Medical: University of Tennessee Health Science Center

Lena N. Sifen, MD
Undergraduate: Florida State University Medical: Wake Forest University School of Medicine

Evan R. Porter, MD
Undergraduate: Drury University Medical: Geisinger Commonwealth School of Medicine

Elliot N. Konrade, MD
Undergraduate: Washburn University Medical: University of Kansas School of Medicine

Robert T. Neel, MD
Undergraduate: University of Tennessee Medical: University of Tennessee Health Science Center

Matthew D. Smith, MD
Undergraduate: University of Georgia Medical: Vanderbilt University School of Medicine

Eric J. West, MD
Undergraduate: Lafayette College Medical: The Brody School of Medicine at East Carolina University

Tanner R. Poppe, MD
Undergraduate: University of Kansas Medical: University of Kansas School of Medicine – Wichita

Kristin Sheaffer, MD
Undergraduate: University of Georgia Medical: Mercer University School of Medicine

Patrick S. Sullivan, MD
Undergraduate: Texas State University Medical: University of Texas Medical Branch

Jacob T. Zalewski, MD
Undergraduate: Sewanee: The University of the South Medical: East Tennessee State University James H. Quillen College of Medicine

Ryan G. Rogero, MD
Undergraduate: University of California Medical: Lewis Katz School of Medicine at Temple

Matthew D. Wideman, MD
Undergraduate: University of Alabama Medical: University of Tennessee Health Science Center

Nikhil Yedulla, MD
Undergraduate: Wayne State University Medical: Wayne State University School of Medicine
Tyler E. Calkins, MD1
Devon D. Goetz, MD2
Jacob T. Zalewski, MD1
Caleb A. Jones, MD1
Peyton R. Gaumer, BS3
Marcus C. Ford, MD1
Patrick C. Toy, MD1
John R. Crockarell, MD1
James W. Harkess, MD1
William M. Mihalko, MD, PhD1
James L. Guyton, MD1
1 Department of Orthopaedic Surgery and Biomedical Engineering, University of Tennessee Health Science CenterCampbell Clinic, Memphis, Tennessee
2 DMOS Orthopaedic Centers, Des Moines, Iowa
3 Des Moines University School of Medicine, Des Moines, Iowa
Background
Periprosthetic femoral fractures (PFFs) in total hip arthroplasty (THA), especially those in contact with the diaphyseal stem, carry high morbidity. This study evaluated how stem design influences the risk of early Vancouver B PFF or other PFF requiring operative intervention after THA.
A multicenter, retrospective study of 3,433 primary cementless THAs performed from 2014 to 2021 included 2,302 single-taper (micro M/L [n ¼ 1,169]; M/L [n ¼ 1,133]) and 1,131 double taper (fit-and-fill [n = 420]; compaction-collared [n = 711]) stems. Mean follow-up was 2.2 years (range, 0.3 to 6.5 years). Primary outcomes were Vancouver B and surgically treated postoperative PFFs among differing femoral stems. Secondary outcomes included rates of intraoperative and postoperative Vancouver A and C PFFs.
Reprinted with permission from: J Arthroplasty. 2023;38:849-854.
Institutional review board approval was obtained from the University of Tennessee Health Science Center (21-08322-FB).
Forty five postoperative PFFs (1.3%) occurred within 8.8 weeks (median), 25 of which were Vancouver B (0.7%) and 20 total PFFs that required operative intervention (0.6%). Compaction-collared stems had a decreased risk of Vancouver B (hazard ratio 0.18, 95% confidence interval: 0.030.97 P = .044) and any surgically treated PFF (hazard ratio 0.10, 95% confidence interval: 0.01-0.95; P = .037). Intraoperative PFFs were most common with fit-and-fill stems (3.6%, P < .001) and Vancouver A with compaction-collared stems (1.8%, P < .001). The cohort with PFF had a higher Charlson comorbidity index (P = .004), more women (P = .001), more Dorr A or C femora (P = .013), and more posterior or lateral surgical approaches compared to those without PFF (P < .001).
Corresponding Author:
James L. Guyton, MD
1211 Union Avenue, Suite 510 Memphis, Tennessee 38104
jguyton@campbellclinic.com
After controlling for confounding variables, compaction-collared stems had a significantly lower risk of postoperative Vancouver B and PFF requiring operative treatment than single-taper and double-taper stems.
Hometown: Parkersburg, West Virginia
Undergraduate Institution: West Virginia University
Medical School: West Virginia University
Personal: Dr. Calkins is the first physician in his family.

Hobbies: Dr. Calkins enjoys any form of outdoor recreation, live music, and hanging out with friends and family.
Asked why he chose medicine as a career: I enjoyed science throughout school and wanted to help people live better and healthier lives.
And why he chose orthopaedics as a specialty: I like the hands-on nature, making immediate tangible improvements in patients’ lives, and the personalities within orthopaedics.
Favorite memory of residency: Hanging out after Monday night meetings, finishing a long day at the Med with the team, camping out at WHJC, and the Jobe golf tournaments.
Plans after Campbell: Total Joint Fellowship at New England Baptist Hospital in Boston.
Dr. Calkins adds: Thank you to the staff at the Med and Le Bonheur for the operative autonomy. Thanks to Dr. Cal for keeping his residency traditions strong. Thanks to the adult reconstruction staff for their support in my career as an arthroplasty surgeon. Thanks to my co-residents for a great 5 years.
David W. Cooper, MD1
Benjamin M. Mauck, MD1
Norfleet B. Thompson, MD1
William J. Weller, MD1
1 Department of Orthopaedic Surgery and Biomedical Engineering, University of Tennessee Health Science Center-Campbell Clinic, Memphis, Tennessee
Institutional review board approval was obtained from the University of Tennessee Health Science Center (21-08332-FB).
Distal radius fractures are common orthopaedic injuries and approximately 85,000 are treated with open reduction internal fixation annually in the United States. Opioid medications have historically been a staple of postoperative pain control regimens. Recently, the opioid epidemic has been a center of focus for healthcare providers and governmental agencies due to rising rates of opioid abuse, opioid-related fatalities, and overall economic burden of treating the opioid epidemic. Orthopaedic surgeons account for nearly 8% of all dispensed opioid prescriptions within the United States, and surgeons have investigated multimodal pain management strategies to assess effectiveness in controlling postoperative pain as well as limiting opioid use and opioid-related complications. We hypothesized that a postoperative opioid-sparing multimodal pain medication regimen would yield superior patient-reported postoperative pain scores compared with a traditional opioid-based regimen.
Corresponding Author:
William J. Weller, MD
1211 Union Avenue, Suite 510 Memphis, TN 38104
wjweller@campbellclinic.com
We conducted a prospective, randomized, controlled trial at one institution between December 2021 and December 2023. Patients presenting to our institution with closed distal radius fractures meeting criteria for open reduction internal fixation with a volar locking plate were invited to participate in the study and were randomized to either a traditional opioid-based or opioid-sparing postoperative pain control regimen. Patients completed a home diary documenting postoperative visual analog scale (VAS) pain scores and quantity of opioids consumed daily. Patients were evaluated at regular intervals through the 12-week postoperative visit with VAS and patient satisfaction recorded at each appointment. The primary outcome measure was oral morphine equivalent (OME) differences between the two groups. Secondary outcomes were VAS pain scores and patient satisfaction.
Seventy-two patients were randomized to the opioid-sparing (n=36) and opioid-based (n=36) postoperative pain control groups after agreeing to
take part in the study. All patients had distal radius fractures fixed through a standard volar approach with a locking plate construct by one of three fellowship-trained hand surgeons. The two groups did not differ significantly with respect to demographic characteristics. There were no significant differences between the two groups with regard to postoperative VAS scores or patient satisfaction. The opioid-based group had a significantly higher OME consumption compared with the opioid-sparing group (P<0.05).
Distal radius fractures are a common orthopaedic injury, and when treated operatively, require adequate pain control regimens in the postoperative period. Recently, both providers and patients have become increasingly concerned about the use of opioid medications for pain control. Our study demonstrates pain can be adequately controlled in the postoperative period using a multi-modal opioid-sparing medication regimen without a decrease in patient satisfaction.
Hometown: Greeneville, Tennessee
Undergraduate Institution: Tusculum University
Medical School: East Tennessee State University Quillen College of Medicine

Personal: Dr. Cooper is the first physician in his family. He is married to Abby Cooper. They met in Johnson City, Tennessee while they were both in school. She is a child counselor at Youth Villages.
Hobbies: Dr. Cooper’s hobbies are distance running, road cycling, hiking, and watching the Tennessee Volunteers’ sporting events.
When asked why he chose medicine as a career: I chose to pursue a career in medicine after enjoying basic science classes in college while also wanting a career where I could apply that material while working with people. One of my college professors, a retired pathologist, encouraged me to apply to medical school during my sophomore year of college while I was trying to decide on a career path. She fostered my early interest in the field of medicine and played a huge part in my choice to become a physician.
And why he chose orthopaedics as a specialty: I chose to pursue orthopaedics for a variety of reasons. It was the specialty I saw during medical school where the physicians seemed happiest in their day-to-day work lives, and their patients often seemed very appreciative after receiving care. The fast-paced clinics and operations appealed to me, and I also liked the ability to identify and fix specific mechanical problems. The work is grounded in an understanding of mechanics while it also offers opportunities to be creative and variable from one case to the next. Orthopaedics also seemed unique in the diverse patient population seen, both in terms of the diversity of pathology encountered and the varied age of patients treated.
Favorite memory of residency: The memory that stands out from residency comes from Dr. Cal’s annual Wilderness Hand Journal Club event, an overnight camping adventure at his farm in Hickory Valley, Tennessee that combines time with good friends, a diverse wild game dinner menu, a huge bonfire, and special hand-made commemorative medallions. Plans after Campbell: Hand and Upper Extremity Fellowship at the Indiana Hand to Shoulder Center, Indianapolis, Indiana. After fellowship, David and Abby will be returning to East Tennessee where David will join Knoxville Orthopaedic Clinic as a hand surgeon.
Dr. Cooper adds: I just want to say thank you to my seven co-residents. I couldn’t have asked for a better group of people to spend five years with in Memphis. It’s been great working with all of you, but it’s been even better hanging out as friends outside of work, and I look forward to staying in touch and seeing where we all land. I also look forward to continuing our group text thread for the foreseeable future.
Zachary R. Diltz, MD
Zachary A. Mosher, MD
Andrew D. Gailey, MD
William M. Mihalko, MD, PhD
Marcus C. Ford, MD
Department of Orthopaedic Surgery and Biomedical Engineering, University of Tennessee Health Science CenterCampbell Clinic, Memphis, Tennessee
Introduction
Total joint arthroplasty (TJA) is increasingly performed in the outpatient setting, with equivalent safety and satisfaction compared to inpatient procedures. Obesity is a major risk factor for osteoarthritis, and obese patients have increased complication rates in TJA. Our study aimed to evaluate the safety of TJA performed at an ambulatory surgery center (ASC) with planned same day discharge (SDD) in patients with a body mass index (BMI) ≥35.
Institutional review board approval was obtained from the University of Tennessee Health Science Center (21-08139-XP).
Corresponding Author:
Marcus C. Ford, MD
1211 Union Avenue, Suite 510 Memphis, TN 38104
mford@campbellclinic.com
This study is a retrospective review of all body mass index (BMI) ≥ 35 patients who underwent total hip arthroplasty (THA) or total knee arthroplasty (TKA) at 2 free-standing ASCs from June 2013 through December 2020. The medical records were queried to collect pre-operative, as well as dayof-surgery data and post-operative complications. The primary outcome was successful SDD. Secondary outcomes included 90-day unplanned emergency department (ED) visits, readmissions, and re-operations.
A total of 645 patients were included, 443 underwent TKA and 202 underwent THA. The average age and BMI for the included patients were 57.5 years and 38.7, respectively. The most common medical comorbidities were hypertension (68.4%), obstructive sleep apnea (27.0%), and diabetes mellitus (21.7%). 2 patients (0.3%) were kept overnight the day of surgery for a next-day discharge (NDD). All others underwent SDD. There were 9 unplanned ED visits, 14 readmissions, 25 re-operations, and 43 post-operative complications.
Carefully selected patients with a BMI ≥35 may undergo TJA in an ASC with reliable SDD and similar or lower re-admission, surgical site infection, and overall complication rates compared with inpatient TJA.
Hometown: Lima, Ohio
Undergraduate Institution: University of Alabama
Medical School: The Ohio State University

Personal: Dr. Diltz’s twin brother Garrett is a hematology/oncology fellow at Georgetown. Dr. Diltz met his wife in Memphis. She is an optometrist.
Hobbies: Dr. Diltz’s hobbies are running, reading, and watching television shows and movies.
When asked why he chose a career in medicine: I’ve had an interest in medicine and surgery since high school that continued through college, and I applied to medical school.
And why he chose orthopaedics as a specialty: I really enjoyed my medical school rotation in orthopaedic surgery, and I found the field very interesting.
Favorite memory of residency: The yearly roasts to commemorate each year have been my favorite memories.
Plans after Campbell: Spine fellowship at Houston Methodist.
Dr. Diltz adds: Thank you to all my fellow residents and staff.
Ilya M. Gutman, MD
Robert Neel, MD
David L. Bernholt, MD
Frederick M. Azar, MD
Tyler J. Brolin, MD
Thomas W. Throckmorton, MD
Department of Orthopaedic Surgery and Biomedical Engineering, University of Tennessee Health Science CenterCampbell Clinic, Memphis, Tennessee
International review board approval was obtained from the University of Tennessee Health Science Center (20-07235-XP)
Presented as poster 173, 2023 American Orthopaedic Society for Sports Medicine (AOSSM) Annual Meeting. Abstract published in the AOSSM Annual Meeting Supplement of Orthopaedic Journal of Sports Medicine, 2023 Jul; 11 (7 suppl3):2325967123S00159.
Diagnosis of subscapularis tears via Magnetic Resonance Imaging (MRI) has been reported to have variable accuracy, with prior studies indicating sensitivity of MRI ranging from 30.0-83.0%. In the current literature, studies utilizing 3.0T MRI scans have generally shown higher sensitivity compared to studies utilizing 1.5T MRI scans; however, there has not been direct comparison of differences in accuracy of 1.5 vs. 3.0T for diagnosis of subscapularis tear. The aim of this study is to investigate this difference. We hypothesize that 3.0T MRI scans will show higher sensitivity for the detection of subscapularis tears compared to 1.5T MRI scans.
A single institution data set was queried to identify patients undergoing rotator cuff repair between January 2015 and January 2020. Patients were separated based on 1.5T and 3.0T MRI strength and these cohorts were analyzed based on intraoperative findings of subscapularis tears and interpretation of these MRI reports. Likewise, demographic information of the cohorts was analyzed including BMI, age, and sex. Univariate analysis, multivariate analysis, and Pearson’s χ2 test, Mann-Whitney U test were used when appropriate.
Corresponding Author:
Thomas W. Throckmorton, MD
1211 Union Avenue, Suite 510 Memphis, TN 38104 tthrockmorton@campbellclinic.com
In a total 756 of patients, 151 were identified as having rotator cuff surgery with preoperative MRI that met our inclusion criteria. A total of 50 (33.1%) patients were identified as having intraoperative findings of subscapularis tears that were not appreciable on MRI. A statistically significant difference was found when comparing the sensitivity of 3.0T MRI for identifying subscapularis tears when compared to 1.5T MRI. 3.0T MRI had a sensitivity of 72.9% compared to 56.4% respectively (P < 0.05). Both groups had a PPV of 100% given no false positive results. 3.0T MRI had a NPV of 92.5% while 1.5T had a NPV of 92.2%.
When a subscapularis tear is clinically suspected, surgeons should be critical over the choice of 1.5T vs 3.0T MRI imaging and understand their sensitivity to guide recommendations for intervention, preoperative planning, and overall patient satisfaction.
Hometown: Birmingham, Alabama
Undergraduate Institution: University of Alabama

Personal: Dr. Gutman is married to Jessica Gutman, who is a pediatrician. They have a golden retriever named Sailor.
Hobbies: Dr. Gutman’s hobbies are traveling, skiing, live music, college football, fishing, kayaking, and boating.
When asked why he chose a career in medicine: The opportunity to help others when they need it the most.
And why he chose orthopaedics as a specialty: The depth and breadth of surgical cases.
Favorite memory of residency: Meeting my co-residents for the first time.
Plans after Campbell: Spine Fellowship, Indiana Spine Group.
Dr. Gutman adds: Thank you all for the opportunity to learn from you and walk in the footsteps of giants.
Claire E. Hays, MD1
Zachary K. Pharr, MD2
Patricia J. Goedecke, MS3
Qi Zhao, MS, PhD3
Tyler J. Brolin, MD1
Frederick M. Azar, MD1
Thomas W. Throckmorton, MD1
1 Department of Orthopaedic Surgery and Biomedical Engineering, University of Tennessee Health Science Center-Campbell Clinic, Memphis, Tennessee
2 Mid-Tennessee Bone & Joint Clinic, Columbia, Tennessee
3 The Biostats, Epidemiology, and Research Design (BERD) Clinic at University of Tennessee Health Science Center, Memphis, Tennessee
A potential risk of reverse total shoulder arthroplasty (RTSA) is the need for blood transfusion because of blood loss and the large associated dead space in a rotator cuff deficient shoulder. The aim of this study was to determine which indications for RTSA are predictive of an increased likelihood of the need for transfusion. We hypothesized that patients with traumatic and post-traumatic indications would require more blood transfusions than patients with non-traumatic indications.
Reprinted with permission from Seminars in Arthroplasty: JSES. 2023:33(1):1-7.
Institutional review board approval was obtained from University of Tennessee Health Science Center (19-07081-XP).
Retrospective review identified 1083 patients with RTSA. After exclusion of revision and tumor cases, 783 patients were divided into three groups: traumatic (acute fractures, fracture-dislocations), post-traumatic (nonunions, malunions, chronic dislocations), or non-traumatic (chronic rotator cuff insufficiency, glenohumeral arthritis with advanced glenoid wear). Demographics, operative indications, preoperative hematocrit, postoperative hematocrit, change in hematocrit, estimated blood loss, operative time, and blood transfusion rates were compared. We constructed a logistic regression model to determine the risk factors predicting blood transfusion.
Corresponding Author:
Thomas W. Throckmorton, MD
1211 Union Avenue, Suite 510 Memphis, TN 38104
tthrockmorton@campbellclinic.com
Indications were acute trauma in 83 patients, post-traumatic sequelae in 65, and non-traumatic conditions in 635. There were no statistically significant differences regarding body mass index (BMI) (P = .5) or American Society of Anesthesiologists (ASA) score (P = .11) between the groups.. There were more females in the traumatic and post-traumatic cohorts than in the non-traumatic cohort (P < .001). Surgical age was younger in the post-traumatic cases (P = .002). The overall frequency of blood transfusion was 4.6% (36/783): traumatic, 19% (16/83); post-traumatic, 17% (11/65); and non-traumatic, 1.4% (9/635). Both the traumatic and post-traumatic groups had significantly higher rates of blood transfusion than non-traumatic cases (P < .001). Preoperative hematocrit was lower in the traumatic group and estimated blood loss was higher in the traumatic and post-traumatic groups (P = .001). Post-traumatic patients experienced the greatest drop in postoperative hematocrit from preoperative levels.
The multivariate logistic regression model showed that traumatic and post-traumatic indications for surgery were each an independent risk factor for blood transfusion, as was change in hematocrit, BMI, surgical age, estimated blood loss, and preoperative hematocrit.
Conclusion
Our results suggest that acute trauma as the indication for RTSA is the strongest independent risk factor for blood transfusion followed by post-traumatic sequelae. Surgeons should be aware of the markedly increased risk of transfusion based purely on these two surgical indications especially when in combination with other predictors of transfusion.
Hometown: Lake Charles, Louisiana
Undergraduate Institution: Louisiana State University
Medical School: Louisiana State University Health Sciences Center, Shreveport

Personal: Dr. Hays is the first physician in her family. She met her fiancé, Zac Lange, in Memphis while here in residency. He works in business valuation at Mercer Capital.
Hobbies: Dr. Hays’ hobbies include running, going on walks with Zac and their dog Topo, snow skiing, fishing, and cooking.
When asked why she choose a career in medicine: I wanted a fulfilling career that would allow me to work with others and make a difference.
And why she chose orthopaedics as a specialty: I wanted to pursue a specialty that would allow me to help people in a challenging and hands-on way.
Favorite memory of residency: Wilderness Hand Journal Club at Dr. Calandruccio's cabin.
Plans after Campbell: Shoulder and Elbow Surgery Fellowship, Cleveland Clinic, Cleveland, Ohio.
Dr. Hays adds: I want to thank Drs. Brolin and Throckmorton for being outstanding mentors and guiding me to choose shoulder and elbow surgery as my specialty. I also want to thank the trauma staff: Drs. Beebe, Cosgrove, Rudloff, and Weinlein for both the challenging lessons learned and fun times had at the Med. Lastly, a special shoutout to Dr. Cal for teaching us all the quintessential bedside manner.
William C. Skinner, MD
Naveen Pattisapu, MD
Clayton C. Bettin, MD
Department of Orthopaedic Surgery and Biomedical Engineering, University of Tennessee Health Science CenterCampbell Clinic, Memphis, Tennessee
Charcot neuroarthropathy (CN) is a complex disease process with progressive degeneration of normal bone architecture. Treatment options for CN include both conservative measures and operative management with the goal of achieving or maintaining a plantigrade ulcer-free foot. Operative treatment of CN varies widely with regards to timing and type of interventions. Surgical interventions include debridement, exostectomy, and complex reconstructions. The technique of intramedullary beaming with supplemental medial locking plate (referred to here as a Midfoot Nail Plate Construct [MNPC]) utilizes large diameter intramedullary screws linked to a medial locked plate for midfoot stabilization, which is the focus of this study.
Institutional review board approval was obtained from the University of Tennessee Health Science Center (16-04974-XP).
Corresponding Author:
Clayton C. Bettin, MD
1211 Union Avenue, Suite 510 Memphis, TN 38104
cbettin@campbellclinic.com
Eighteen patients (19 limbs) with midfoot CN treated at our institution by a single surgeon from January 2017 through December 2021 met inclusion criteria and were included in our MNPC cohort. Retrospective chart review was performed to obtain demographic data, comorbidities, previous treatment data, ambulation status pre/post intervention, radiographic (Brodsky) classification, time to intervention, number of operations, and outcomes after operative management with MNPCs with a descriptive statistical analysis. Furthermore, post-intervention outcomes (rates of post-operative ulceration, post-operative infection, and amputation) were compared with our previously reported institutional baseline data of postsurgical complications of CN in 58 patients treated between 2005-2016 with limited and reconstructive techniques without MNPCs.
The mean age of the MNPC cohort was 55.6 (range 37 – 73 years), mean body mass index was 39.3, and 77.8% (14/18) of patients had diabetes (mean A1c 7.0, A1c range 5.8 to 10.4). 47.3% (9/19) had undergone previous non-operative management and 21.1% (4/19) received prior operative treatment. Mean follow-up was 19.4 months (range 3 – 47 months, median 17 months). Average time from presentation to intervention was 10.4 months (range 1 – 32 months, median 6 months). Post-intervention rates of ulceration, infection, and amputation for the MNPC cohort were 31.6% (6/19), 26.3% (5/19), and 15.8% (3/19), respectively. Compared with our institutional baseline data of complications after limited and reconstructive surgical techniques without MNPCs from 2005-2017, MNPC had a lower rate of ulceration and amputation. Ulceration rate
after limited, reconstructive, and MNPC were 34.4% (11/32), 42.3% (11/26), and 31.6% (6/19) respectively. Infection rates were 25% (8/32), 42.3% (11/26), and 26.3%, with amputation rates of 21.9% (7/32), 23.1% (6/26), and 15.8% (3/19), respectively.
Despite continued innovation in surgical management of CN of the foot, post-intervention complication rates remain high. This study provides patient and outcome data for Midfoot Nail Plate Constructs as a treatment for CN in a large cohort with midterm follow-up. Compared with our own institutional historical data prior to adoption of this technique, MNPCs have an equivalent infection rate and lower rate of ulceration and amputation at an average of 19.4 months follow-up.
Hometown: Savannah, Georgia
Undergraduate Institution: University of Georgia
Medical School: Medical College of Georgia

Personal: Dr. Skinner’s uncle and maternal grandfather were physicians. He is married to Sarah Byrd Skinner, who is an obstetrics/gynecology resident physician.
Hobbies: Dr. Skinner enjoys gardening, travel, college football, being outdoors, and National Parks.
When asked why he chose medicine as a profession: I was inspired by my grandfather initially to pursue a career where I could help others.
And when asked why he chose orthopaedics as a specialty: Orthopaedic surgeons have the unique ability to keep people active and maintain and improve their quality of life.
Favorite memory of residency: Time spent with co-residents at the Med and outside of work (golf tournament, roasts, etc.)
Plans after Campbell: Foot and Ankle Fellowship, Baylor, Scott & White, Dallas, TX.
Dr. Skinner adds: Thank you to all the Campbell Clinic physicians, staff, and my co-residents for a great five years.
Carson J. Smith, MD1
Braden J. Boyer, MD2
Clayton C. Bettin, MD1
1 Department of Orthopaedic Surgery and Biomedical Engineering, University of Tennessee Health Science Center-Campbell Clinic, Memphis, Tennessee
2 OrthoArizona, Phoenix, Arizona
This abstract was presented at the MidAmerica Orthopaedic Assoication (MAOA) meeting in 2023 and as an e-poster at the American Orthopaedic Foot & Ankle Society (AOFAS) annual meeting in 2023.
Institutional review board approval was obtained from the University of Tennessee Health Science Center (22-09067-XP).
Tibiotalocalcaneal (TTC) arthrodesis is a treatment option for several pathologies of the hindfoot and ankle. Traditional fixation options include intramedullary nailing (IMN) or plate-screw constructs. In certain complex patients, such as those with deformity, bone loss, or difficulty complying with post-operative restrictions, more robust fixation may be desired. New trauma literature shows hybrid plate-nail constructs (PNCs) may permit early weight-bearing in osteoporotic distal femur fractures. We report early results of TTC arthrodesis using PNCs in patients with complex deformities of the ankle and hindfoot.
Patients undergoing TTC arthrodesis via IMN plus plating by a single surgeon from September 2020 to May 2023 were included in our study. Indications included Charcot neuroarthropathy (CN), posttraumatic deformities, and advanced arthritis. Age, comorbidities, ulceration, operative details, and postoperative complications were retrospectively recorded.
Corresponding Author:
Clayton C. Bettin, MD
1211 Union Avenue, Suite 510 Memphis, TN 38104
cbettin@campbellclinic.com
Fifteen patients (16 feet) met inclusion criteria. Most cases were performed for CN or post-traumatic complications. Average age was 54.7 years. Most (11) patients were treated with a lateral TTC locking plate, though other plates were used for select indications. All patients received a TTC arthrodesis nail. In all cases, cellular bone matrix was used; in fourteen cases, autograft was also used. Average follow-up was 42 weeks (min. 12). Three patients ultimately underwent below-knee amputation, two for infection and the other for hardware failure. Three others required reoperation but ultimately achieved union. In 13 of 16 cases, patients achieved a stable, plantigrade, non-infected, ulcer-free foot at latest follow-up.
TTC arthrodesis with PNCs is an attractive limb-salvage option in cases of complex ankle and hindfoot pathology. This technique should particularly be considered when patients present difficult challenges such as deformity, bone loss, and impaired ability to comply with postoperative restrictions. We reported an 81% favorable outcome rate in our series, with major complications mostly confined to patients with significant medical comorbidities.
Hometown: Memphis, TN
Undergraduate Institution: University of Miami
Medical School: University of South Florida

Personal: Dr. Smith's wife, Elizabeth, is a physical therapist, and they met on a medical mission trip to Panama. His cousin is a cardiologist in Little Rock, Arkansas, but he is the first orthopaedist in his family.
Hobbies: Dr. Smith enjoys weightlifting, running, sports, and outdoor activities including snowboarding and going to the beach.
Asked why he chose medicine as a career: The human body was always fascinating to me, and my undergraduate major in exercise physiology reinforced that interest. I owe my interests in both science and helping other people to my father, who was my single largest influence to pursue medicine.
And why he chose orthopaedics as a specialty: My father was a dentist as well as a very skilled handyman around the house, so he passed on to me the love for working with my hands. This combined with my interest in the musculoskeletal system led naturally to orthopaedics. I love being able to use my hands to fix problems and thus restore essential functions to patients’ lives.
Favorite memory of residency: My time spent at the Med will certainly be the most memorable. Not only do we learn so much about the basics of orthopaedic surgery there, but we also go through so many trials and tribulations which are made much more bearable (and hilarious) by having 10 or so other residents around to commiserate with. My best friends from residency are those that I have spent at least one stint at the Med with. As a Memphian, I am proud to have spent time training there.
Plans after Campbell: Foot and Ankle Fellowship, University of California, Davis, Sacramento, CA and Reno Orthopaedic Center, Reno, Nevada. Dr. Smith hopes to practice in the Tampa Bay Area.
Dr. Smith adds: There are so many co-residents and staff who have been vital in shaping my time here. I would particularly like to thank the Foot & Ankle and Trauma staff for teaching me so much, serving as excellent mentors and career role models, and helping me achieve my career goals. I have had many amazing co-residents over the years, many of whom I look up to and have served as examples of how to be a great resident and surgeon. I would particularly like to thank Dr. Carson Rider, who (as a 4th-year resident) was a big part of why I ended up at the Campbell Clinic, and as my chief resident and now attending has always served as an excellent example of a great surgeon and colleague.
Tyler E. Calkins, MD
Clayton C. Wing, MD
Zachary R. Diltz, MD
William M. Mihalko, MD, PhD
Patrick C. Toy, MD
Department of Orthopaedic Surgery and Biomedical Engineering, University of Tennessee Health Science CenterCampbell Clinic, Memphis, Tennessee
Introduction
This study evaluated the effect of bupivacaine versus mepivacaine spinal anesthesia and preoperative adductor canal block (ACB) on recovery, length of stay, pain, and complications of same-day discharge total knee arthroplasty (TKA) at a free-standing ambulatory surgery center.
Reprinted with permission from J Am Acad Orthop Surg 2023; 31(5):e256-e263.
Institutional review board approval was obtained from the University of Tennessee Health Science Center (17-05344-XP).
Corresponding Author:
William M. Mihalko, MD, PhD
1211 Union Avenue, Suite 510 Memphis, TN 38104
wmihalko@campbellclinic.com
We performed a retrospective review of patients who underwent TKA between March 2018 and September 2019. The patients were grouped based on the neuraxial anesthetic regimen: bupivacaine with ACB, bupivacaine without ACB, and mepivacaine without ACB. Preoperative ACBs were discontinued in December 2018, and use of mepivacaine spinal anesthesia was initiated in March 2019. Length of stay in the postanesthesia care unit (PACU), time to controlled void and ambulation, postoperative pain, morphine milligram equivalents (MME), and transient neurologic symptoms were compared.
Ninety consecutive patients who underwent TKA were identified. Fifty patients received bupivacaine with ACB, 20 received bupivacaine without ACB, and 20 received mepivacaine without ACB. Mepivacaine spinal anesthesia led to a 93-minute shorter PACU stay (P < 0.001), 115-minute quicker time to void (P < 0.001), 60-minute earlier ambulation (P = 0.024), and 109-minute shorter total facility time (P = 0.003) but increased total MME (P = 0.049) despite nonsignificant difference in pain at discharge (P = 0.908) compared with bupivacaine. Patients receiving bupivacaine with and without ACB had a nonsignificant difference in pain scores at discharge, time to ambulation, and time to discharge (P ≥ 0.1). No transient neurologic symptoms or overnight stays were observed.
Mepivacaine spinal anesthesia for TKA safely facilitated more rapid sameday discharge through decreased times to controlled void and ambulation but with a slight increase in MME requirements. Discontinuing preoperative ACBs did not negatively affect PACU outcomes.
Hometown: Watkinsville, Georgia
Undergraduate Institution: University of Georgia
Medical School: Medical College of Georgia

Personal: Dr. Wing is the first physician in his family. He met his wife Casey in high school. She is a school counselor. They have a son Cooper (2 yrs) and a daughter Charley (8 months).
Hobbies: Dr. Wing enjoys hunting, fishing, golf, watching sports, and cooking.
When asked why he chose a career in medicine: Patient care.
And when asked about orthopaedics as a specialty: The surgeries are fun and engaging. The community is great as well.
Favorite memory of residency: Rotations with residency classmates.
Plans after Campbell: Joint Fellowship, Mayo Clinic, Jacksonville, Florida
Dr. Wing adds: Thank you for patiently teaching clinical and operative skills. Also special thanks to Dr. Spence, Dr. Ford, and Dr. Brolin for taking me on as a patient and helping me regain physical activity.
Clinical orthopaedic research by Campbell Clinic physicians and residents enables our doctors to deliver superior, evidence-based orthopaedic care to patients.
“Research and innovation drive patient outcomes. Simply thinking that something seems like a good idea and trying it just isn’t enough,” Dr. Derek M. Kelly explains. “Better healthcare requires physicians, healthcare systems, and industry to be thoughtful in their approach to developing great ideas and research questions, conducting well-designed research studies, and reporting both good and bad results so that all can benefit.”
Throughout the last 15 years, a concerted effort to step up staff-driven research efforts has yielded more than 150 studies each year. Extensive support for the Campbell Clinic researchers includes a research manager, five clinical research coordinators, three research scholars, a full-time librarian, and an editorial team to prepare studies for peer-reviewed publications and presentations.
Through this research, new orthopaedic techniques and treatments are found to better serve patients, thus reducing pain, enhancing mobility and improving their quality of life. It also helps Campbell Clinic maintain a global reputation for orthopaedic excellence. “There’s
so much information out there that you can’t keep up with everything,” said Dr. James H. Beaty, Chairman, UTHSC-Campbell Clinic Department of Orthopaedic Surgery and Biomedical Engineering. “You want (Campbell Clinic) to be seen as a thought leader so that when our physicians publish their research, people will want to read it. These findings are going to ultimately translate into better patient care.”
Campbell Clinic Research teams have been nationally recognized for their research endeavors. During the March 2023 Annual meeting of the American Academy of Orthopaedic Surgeons (AAOS) Annual Meeting, the study, led by Tyler Brolin, MD and Quin Throckmorton, MD, "Muscle Activation Patterns during Active External Rotation after Reverse Total Shoulder Arthroplasty: An Electrophysiological Study of the Teres Minor and Associated Musculature" was honored with the prestigious 2023 Charles S. Neer Award. And during the 2023 American Association of Hip and Knee Surgeons (AAHKS) meeting, Marcus Ford, MD and William Mihalko, MD were awarded the AAHKS Clinical Research Award for investigating the safety and clinical efficacy of extended postoperative oral tranexamic acid use in total knee arthroplasty.
Last year, six of the most significant Campbell Clinic research contributions were published in Spine Deformity and the Journals of Arthroplasty, Foot and Ankle Surgery, Pediatric Orthopaedics, and Journal of Shoulder and Elbow Surgery. Those findings included:
• Administration of a perioperative injection is effective and should be considered in the perioperative protocol in patients undergoing posterior spinal fusion (PSF) for adolescent
idiopathic scoliosis (AIS). In 2019, Dr. Kelly and his team began using a perioperative injection administered during PSF surgery with AIS to control postoperative pain. The perioperative injection was
composed of ropivacaine, epinephrine, ketorolac, and morphine. Patients who were given the perioperative injection were compared with those who had surgery before the perioperative injection was introduced. Results showed a significant decrease in PRN (postoperative as need) use of opioids and a significantly higher rate of ambulation on postoperative day one.
• A shoulder injection that includes a corticosteroid will decrease shoulder pain. Methylprednisolone acetate (MPA) and triamcinolone acetonide (TA) are the standard of care medications commonly administered along with numbing medications. Dr. Tyler Brolin observed that patients receiving MPA in the shoulder injection called back shortly after the injection complaining of an increase in shoulder pain while other patients receiving TA did not. Patients were enrolled in the prospective, parallel study design with pain scores collected at 12 time points from the day of injection to one year later. The first cohort received 2 milliliters (ml) of lidocaine, 2 ml of bupivacaine, and 80 milligrams (mg) of MPA, while a second cohort received 2 ml of lidocaine, 2 ml of bupivacaine and 80 mg of TA. Shoulder injections with TA resulted in an over five-fold reduction of steroid flare reactions with a statistically superior 6-month efficacy rates compared with MPA injection.
• Patient education is needed to improve the safety of patients who use wheeled knee walkers (WKW). The question of safety and differences between WKW designs prompted an observational and descriptive study led by Dr. Drew Murphy. Eighty foot-and-ankle patients completed the survey, which found that 43% had fallen, 64% of whom had multiple falls. Yet 85% of those surveyed were satisfied with use of the WKW. This was the first study reporting on WKW in a clinical population; it resulted in a patient education program to improve safety.
• Preoperative cryoneurolysis in patients with knee osteoarthritis can reduce opioid consumption and improve functional outcomes after total knee arthroplasty (TKA). Dr. William Mihalko led a prospective randomized controlled trial to determine if preoperative treatment with cryoneurolysis of the superficial genicular nerves
before patients’ TKA would decrease postoperative opioid use as compared with standard of care treatment (SOC). Patients receiving cryoneurolysis before their TKA procedure (n=62) were compared with patients receiving SOC (n=62) out to 12 weeks postoperative. There were no differences in medications or treatments administered between the two cohorts. Analysis of the per-protocol data revealed a significant decrease in oral morphine equivalent (cryoneurolysis = 4.1 vs SOC = 5.9; P = 0.0186). Compared with the SOC group, the cryoneurolysis group had improved functional scores and numerical improvements in pain scores across all follow-up assessments.
• Pediatric surgery appears to be safer and result in fewer complications when conducted in ambulatory surgical centers (ASC) rather than in hospitals. Dr. Jeffrey Sawyer and researchers conducted a retrospective record review over nine years to assess the safety of surgical procedures in a free-standing ASC. The 3,780 pediatric subjects included 9 (0.24%) intraoperative complications, 2 (0.08%) urgent hospital transfers, 114 (3%) complications, and 16 (0.42%) readmissions. The rate of an emergency hospital transfer, surgical complications and 30-day readmission, even by the stringent criteria, were lower than those reported for outpatient procedures performed in hospitals.
• A postoperative opioid-sparing (OS) regimen after shoulder arthroplasty (SA) results in a nearly fourfold reduction in opioid pain pill consumption and a higher rate of satisfaction with pain management. Since no clear consensus exists on ideal pain-management strategies after SA and most protocols are opioid-driven, Dr. Brolin sought to determine if SA patients not taking opioids after surgery would have equivalent pain scores and satisfaction as patients using a traditional opioidbased (OB) regimen. Patients were prospectively enrolled and randomized into either the OS or OB cohort and followed until completion of their 12week visit. There were no differences in pain scores in any time point between the cohorts. The OS regimen demonstrated a nearly 4-fold reduction in opioid consumption and earlier cessation of opioids as compared to the OB regimen.

Nathaniel B. Alexander, MD1
Shumaila Sarfani, MD2
Carson D. Strickland, MD3
David R. Richardson, MD1
G. Andrew Murphy, MD1
Benjamin J. Grear, MD1
Clayton C. Bettin, MD1
1 Department of Orthopaedic Surgery and Biomedical Engineering, University of Tennessee Health Science CenterCampbell Clinic, Memphis, Tennessee
2 Ortho San Antonio, San Antonio, Texas
3 Mid Tennessee Bone and Joint, Columbia, Tennessee
Weightbearing computed tomography (WBCT) is becoming a valuable tool in the evaluation of foot and ankle pathology. Currently, cost analyses of WBCT scanners in private practice are lacking in the literature. This study evaluated the costs of acquisition, utilization, and reimbursements for a WBCT at a tertiary referral center, information of particular interest to practices considering obtaining such equipment.
All WBCT scans performed at a tertiary referral center over the 55-month period (August 2016 to February 2021) were retrospectively evaluated. Patient demographics, pathology location, etiology, subspecialty of the ordering provider, and whether the study was unilateral or bilateral were collected. Reimbursement was calculated based on payor source as a percentage of Medicare reimbursement for lower extremity CT. The number of total scans performed per month was evaluated to determine revenue generated per month.
Reprinted with permission from: Foot Ankle Orthop. 2023:8(1):1-6.
Over the study period, 1903 scans were performed. An average of 34.6 scans were performed each month. Forty-one providers ordered WBCT scans over the study period. Foot and ankle fellowship-trained orthopaedic surgeons ordered 75.5% of all scans. The most common location of pathology was the ankle, and the most common etiology was trauma. The device was cost neutral at 44.2 months, assuming reimbursement for each study was commensurate with Medicare rates. The device became cost neutral at approximately 29.9 months when calculating reimbursement according to mixed-payor source.
Corresponding Author:
Clayton C. Bettin, MD
1211 Union Avenue, Suite 510 Memphis, Tennessee 38104
cbettin@campbellclinic.com
As WBCT scan becomes more widely used for evaluation of foot and ankle pathology, practices may be interested in understanding the financial implications of such an investment. To the authors’ knowledge, this study is the only cost-effectiveness analysis of WBCT based in the United States. We found that in a large, multispecialty orthopaedic group, WBCT can be a financially viable asset and a valuable diagnostic tool for a variety of pathologies.
Aaron M. Baessler, MD1
Jessica Buchman, M. DO2
Dexter A. Witte, MD3
David D. Spence, MD4
Thomas W. Throckmorton, MD4
Tyler J. Brolin, MD4
Frederick M. Azar, MD4
David L. Bernholt, MD4
1 AHNI Orthopedics, Carmel, Indiana
2 Mercy Hospital, Washington, Missouri
3 Midsouth Imaging and Therapeutics, Memphis, Tennessee
4 University of Tennessee Health Science Center- Campbell Clinic Department of Orthopaedic Surgery and Biomedical Engineering, Memphis, Tennessee
Skeletally Immature Patients With Classic Anterior Cruciate Ligament Bone Bruise Patterns Have a Higher Likelihood of Having an Intact Anterior Cruciate Ligament Compared With Skeletally Mature Patients
Background
The incidence of anterior cruciate ligament (ACL) tears in skeletally immature patients with an ACL bone contusion pattern has been sparsely investigated. The purpose of this study is to investigate whether physeal status has an influence on the likelihood of sustaining an ACL tear when classic bipolar ACL bone bruising pattern is present.
Reprinted with Permission:
J Pediatr Orthop 2023; 43(1)
Corresponding Author:
David L. Bernholt, MD
1211 Union Avenue, Suite 510 Memphis, Tennessee 38104 dbernholt@campbellclinic.com
Magnetic resonance imaging reports were queried for “contusion” on all patients between 6 and 22 years between 2015 and 2019. Images were reviewed to denote all intra-articular pathology and the physeal status of the femur and tibia. The primary outcome was the incidence of ACL tears in patients with the presence of bipolar bone contusions. Fischer exact testing was used to determine associations.
Of 499 patients included, 269 of those had bipolar bone contusions. Patients with bipolar bone contusions and ACL tears had a shorter duration between injury and imaging date compared with patients with ACL tears without bipolar bone contusions (6.9 vs. 38.6 d, P=0.05). Patients with an open femoral physis had a higher likelihood of having an intact ACL despite the presence of bipolar bone contusions than patients with a closed femoral physis (10.8% vs. 1.0%, P<0.001). Of patients with bipolar bone contusions, those with an intact ACL were younger than patients with an ACL tear (14.6 vs. 16.4, P=0.017).
Although bipolar bone contusions of the central lateral femoral condyle and posterior lateral tibial plateau are typically found after ACL injury, these bipolar contusions can be found concomitantly with an intact ACL and were more often found in relatively younger patients. Patients who have an open femoral physis have a higher likelihood to have an intact ACL despite the presence of bipolar bone contusions compared with patients who have a closed femoral physis.
Although bipolar bone contusions of the central lateral femoral condyle and posterior lateral tibial plateau are typically found after ACL injury, these bipolar contusions can be found concomitantly with an intact ACL and were more often found in relatively younger patients. Patients who have an open femoral physis have a higher likelihood to have an intact ACL despite the presence of bipolar bone contusions compared with patients who have a closed femoral physis.
Nahum M. Beard, MD, CAQSM1
Luke Beggs, PhD, MD1
William G. Murphy, MD1
Margaret Knack, RN, BSN, MS, CCRP2
Owen Golden, MS, ATC1
William Ross, MD3
1 Department of Orthopaedic Surgery and Biomedical Engineering, University of Tennessee Health Science CenterCampbell Clinic, Memphis, Tennessee
2 Campbell Clinic Foundation, Germantown, Tennessee
3 University of Tennessee Health Science Center, College of Medicine, Memphis, Tennessee
Fluoroscopic injection through the rotator cuff interval (RCI) is a common technique for diagnostic arthrography and therapeutic intervention. Ultrasound approaches through the RCI have been less commonly studied, but there is a growing body of literature.
The purpose of this study was to present a standardized technique of ultrasound-guided injection into the glenohumeral joint utilizing the RCI in magnetic resonance imaging (MRI) arthrography (MRA) and to report one medical group’s experience with the technique.
Reprinted with permission from:
J Osteopath Med. 2023; 123(12):571-576.
Corresponding Author:
Nahum M. Beard, MD
1211 Union Avenue, Suite 510 Memphis, Tennessee 38104
nbeard@campbellclinic.com
A retrospective chart review of all ultrasound-guided injections into the glenohumeral joint utilizing the RCI was performed from July 1, 2014 through June 1, 2021. Data were compiled for age, gender, body mass index (BMI), and prior surgery on the shoulder. The primary endpoint was successful administration of intra-articular dilute gadolinium contrast adequate for radiologic interpretation. A total of 487 injections into the glenohumeral joint via the RCI were performed. One hundred and fiftyfive patients had previous shoulder surgery, with the remainder naive to intervention.
The success rate of injections into the glenohumeral joint was 99.4%, with only three injections considered unsuccessful. The three unsuccessful injections did not succeed because of a lack of intra-articular contrast media present. This success rate is impressive and promising, particularly when considering that 155 of the patients had previous surgery, which could potentially cause complications, and because these injections were performed over a long period of 7 years.
Accessing the RCI under ultrasound guidance is a very successful technique for injection within the glenohumeral joint.
Tyler E. Calkins, MD1
Evan P. Johnson, MD1
Robert R. Eason2
William M. Mihalko, MD, PhD1
Marcus C. Ford, MD1
1 Department of Orthopaedic Surgery and Biomedical Engineering, University of Tennessee Health Science Center-Campbell Clinic, Memphis, Tennessee
2 University of Tennessee Health Science Center College of Medicine, Memphis, Tennessee
Spinal anesthesia is the predominant regimen in outpatient total joint arthroplasty (TJA), but induction often is unsuccessful, unobtainable, or against patient preference. We compared outcomes of same-day discharge (SDD) TJA with spinal versus general anesthesia in a free-standing ambulatory surgery center (ASC).
Reprinted with permission from: J Arthroplasty. 2023: S0883-5403(23)01212-3.
Corresponding Author:
William M. Mihalko, MD, PhD
1211 Union Avenue, Suite 510 Memphis, Tennessee 38104
wmihalko@campbellclinic.com
We took 105 general anesthesia TJA and one-to-one nearest-neighbor matched them to 105 spinal anesthesia TJA over 7 years at 1 ASC. The rate of successful SDD, minutes to discharge, postoperative pain and nausea, and 90-day complications were compared. Postanesthesia care unit outcomes were additionally stratified by spinal anesthetic (mepivacaine versus bupivacaine).
All spinal anesthetic patients underwent SDD compared with 103 (98%) general anesthetic patients (P = .498). Mepivacaine spinal anesthesia patients spent the fewest minutes in postanesthesia care unit prior to discharge from the facility (206), followed by general anesthesia (227), and bupivacaine spinal anesthesia (291; P < .001). General anesthesia patients had the highest levels of pain at 1 hour (5.2 versus 1.5 versus 1.5) and 2 hours (3.2 versus 2.0 versus 1.3) postoperatively, and rates of nausea (48 versus 22 versus 28%) compared with mepivacaine and bupivacaine spinal anesthesia, respectively. The 90-day complications (6 versus 7), admissions (1 versus 3), and reoperations (5 versus 2) were similar among spinal and general anesthesia, respectively (P ≥ .445).
Both spinal and general anesthesia led to reliable SDD with similar 90-day complication rates. General anesthesia facilitated faster discharge from the ASC compared with bupivacaine spinal anesthesia but led to higher levels of pain and incidence of nausea postoperatively.
Stephanie N. Chen, MD1
Tyler D. Ragsdale, MD2
Leslie N. Rhodes, DNP, PPCNP-BC3,4
Lindsey L. Locke, MSN, CPNP-PC4
Alice Moisan, BSN, RN5
Derek M. Kelly, MD1
1 Department of Orthopaedic Surgery and Biomedical Engineering, University of Tennessee Health Science CenterCampbell Clinic, Memphis, Tennessee
2 St. Louis University, St. Louis, Missouri
3 University of Tennessee Health Science Center, College of Nursing, Memphis, Tennessee
4 Le Bonheur Children’s Hospital, Memphis, Tennessee
5 ICON PLC, Brentwood, Tennessee
Clubfoot is a common congenital foot deformity in children. The Ponseti method of serial casting has become the standard of care in clubfoot treatment. Clubfoot casting is performed in many centers by both orthopaedic surgeons and physical therapists (PTs); however, direct comparison of outcomes and complications of this treatment between these providers is limited. This study prospectively compared the outcomes of patients with clubfoot treated by these 2 groups of specialists.
Between January 2010 and December 2014, all patients under the age of 12 months with a diagnosis of clubfoot were included. Patients were randomized to an orthopaedic surgeon (MD) group or a PT group for weekly serial casting. Main outcome measures included the number of casts required to achieve correction, clinical recurrence of the deformity, and the need for additional surgical intervention.
Reprinted with permission from:
J Pediatr Orthop. 2023:43(2):e93-e99.
Corresponding Author:
Derek M. Kelly, MD
1211 Union Avenue, Suite 510 Memphis, Tennessee 38104
dkelly@campbellclinic.com
One hundred twenty-six infants were included in the study. Patient demographics and characteristics (sex, race, family history of clubfoot, laterality, and severity of deformity) were similar between treatment groups, with the only significant difference being the mean age of entry into the study (5.2 weeks in the MD group and 9.2 weeks in the PT group, P=0.01). Mean length of follow-up was 2.6 years. The number of casts required trended to a lower number in the MD group. There was no significant difference in the rates of clinical recurrence or additional surgical intervention between groups.
Ponseti casting for treatment of clubfoot performed by orthopaedic surgeons and PTs results in equivalent outcomes without any difference in complications. Although the number of casts required trended to a lower number in the MD group, this likely did not result in any clinical significance, as the difference in cast number equaled < 1 week’s difference in the overall duration of serial casting.
Robert R. Eason, MS1
Myles R. Joyce, BS1
Thomas W. Throckmorton, MD1
Frederick M. Azar, MD1
David L. Bernholt, MD1
Abu Mohd Naser, PhD, MBBS2
Tyler J. Brolin, MD1
1 Department of Orthopaedic Surgery and Biomedical Engineering, University of Tennessee Health Science CenterCampbell Clinic, Memphis, Tennessee
2 Division of Epidemiology, Biostatistics, and Environmental Health, School of Public Health, University of Memphis, Memphis, Tennessee
A corticosteroid fl are reaction is a well-described phenomenon that causes signifi cant pain and dysfunction. The paucity of literature impedes decision making regarding which corticosteroid to use for shoulder injection. The purpose of this study was to compare methylprednisolone acetate (MPA) and triamcinolone acetonide (TA) injections in the glenohumeral joint and/or subacromial space in terms of effi cacy and the incidence of steroid fl are reactions.
Reprinted with permission from J Shoulder Elbow Surg. 2023; 32:2214-2221.
Corresponding Author:
Tyler J. Brolin, MD
1211 Union Avenue, Suite 510 Memphis, Tennessee 38104
tbrolin@campbellclinic.com
In this prospective, interrupted time series, parallel study, patients received injections in the glenohumeral joint and/or subacromial space. MPA and TA were used during 2 discrete 3-month periods. The injections consisted of 2 mL of lidocaine, 2 mL of bupivacaine, and 80 mg of either MPA or TA. Visual analog scale (VAS) pain scores were recorded immediately before injection; 1-7 days after injection; and 3, 6, and 12 months after injection. The primary outcome was the incidence of a steroid flare reaction, defined as a post-injection increase in the VAS score by 2 points. The secondary outcome was injection failure, defined as a postinjection VAS score greater than the baseline score or the need for another intervention. We used linear mixed models with a patient-level random intercept to identify the mean VAS score change for TA injections in the first week after injection.
MPA or TA shoulder injections were administered in 421 patients; of these patients, 15 received bilateral-joint injections whereas 406 received a single-joint injection, for a total of 436 injections (209 MPA and 227 TA injections). Pain scores in the first week after injection were available for 193 MPA and 199 TA injections. Significantly more patients in the MPA cohort reported flare reactions compared with the TA cohort (22.8% vs. 4.0%, P < .001) during the first week after injection. In the first week after injection, the mean VAS score of patients receiving TA injections was 1.05 (95% confidence interval, 0.47-1.63) lower
than that of patients receiving MPA injections when adjusted for age, sex, race, pain type, surgeon type, and injection site. At 3 months, surveys for 169 MPA and 172 TA injections were completed, with no significant difference in the rate of injection failure for MPA vs. TA (42.6% vs. 36.1%, P = .224). Treatment failure rates were significantly higher for MPA than for TA at 6 months (78.44% vs. 62.5%, P < .001) but not at 12 months (81.18% vs. 81.42%, P = .531).
TA injections resulted in a > 5-fold reduction in steroid flare reactions, with statistically superior 6-month efficacy rates, compared with MPA injections. This study supports TA as a more viable corticosteroid option for shoulder injection.
Nolan Farrell, MD1
Paul T. Greenfield, MD1
Paul T. Rutkowski, MD1
William Jacob Weller, MD1
1 University of Tennessee Health Science Center – Campbell Clinic Department of Orthopaedic Surgery and Biomedical Engineering, Memphis, TN
Distal radius fractures have a high incidence among both young and elderly patients, and in many instances require operative intervention. When operative intervention is employed, adequate pain management is essential to decrease postoperative complications, such as chronic pain and disability, while minimizing the risk of prolonged opioid use and dependence. Strategies to optimize pain management include regional anesthesia, preoperative dosing of medication, multimodal regimens, long-acting selective opioids at the time of surgery, corticosteroids, and non-pharmacologic therapies.
Key points
• Combination perioperative analgesic drugs decrease opioid utilization and improve pain control.
• Regional anesthesia is a useful adjunct to pain control in the acute postoperative setting.
Reprinted with permission from: Orthop Clin North Am. 2023; 54(4):463-470.
Corresponding Author:
William J. Weller, MD
1211 Union Avenue, Suite 510 Memphis, Tennessee 38104 wjweller@campbellclinic.com
• Preoperative assessment is imperative to tailor the patient's paincontrol plan.
• Further data are needed to determine medication dosages, duration, and explore opioid-sparing regimens.
Catherine R. Olinger, MD1
Alex Coffman1
Chad E. Campion, MD2
Kirk M. Thompson, MD2
Raymond J. Gardocki, MD3
1 Department of Orthopedics and Rehabilitation, University of Iowa, Iowa City, Iowa
2 Department of Orthopaedic Surgery and Biomedical Engineering, University of Tennessee Health Science CenterCampbell Clinic, Memphis, Tennessee
3 Department of Orthopaedic Surgery, Vanderbilt University Medical Center, Nashville, Tennessee
The purpose was to investigate the learning curve for elective endoscopic discectomy performed by a single surgeon who made a complete switch to uniportal endoscopic surgery for lumbar disc herniations in an ambulatory surgery center and determine the minimum case number required to safely overcome the initial learning curve.
Electronic medical records (EMR) of the first 90 patients receiving endoscopic discectomy by the senior author in an ambulatory surgery center were reviewed. Cases were divided by approach, transforaminal (46) versus interlaminar (44). Patient-reported outcome measures (visualanalog-score (VAS) and the Oswestry disability index [ODI]) were recorded preoperatively and at 2-week, 6-week, 3-month, and 6-month appointments. Operative times, complications, time to discharge from PACU, postoperative narcotic use, return to work, and reoperations were compiled.
Reprinted with permission from: Eur Spine J. 2023;32:2694-2699.
Corresponding Author:
Raymond J. Gardocki, MD
Department of Orthopaedic Surgery
Vanderbilt University Medical Center Nashville, TN
raymond.gardocki@vumc.com
Median operative time decreased approximately 50% for the first 50 patients then plateaued for both approaches (mean: 65 min). No difference in reoperation rate was observed during the learning curve. Mean time to reoperation was 10 weeks, with 7(7.8%) reoperations. The interlaminar and transforaminal median operative times were 52 versus 73 min, respectively (p = 0.03). Median time to discharge from PACU was 80 min for interlaminar approaches and 60 min for transforaminal (p < 0.001). Mean VAS and ODI scores 6 weeks and 6 months postoperatively were statistically and clinically improved from preoperatively. The duration of postoperative narcotic use and narcotics need significantly decreased during the learning curve as the senior author realized that narcotics were not needed. No differences were apparent between groups in other metrics.
Endoscopic discectomy was shown to be safe and effective for symptomatic disc herniations in an ambulatory setting. Median operative time decreases by half over the first 50 patients in our learning curve, while reoperation rates remained similar without the need for hospital transfer or conversion to an open procedure in an ambulatory setting.
William P. Polio, MD1
Blake Hajek, BS, MS2
Tyler J. Brolin, MD1
William M. Mihalko, MD, PhD1
Kunal Singhal, PT, PhD3
Shannon Hughes, PT, DPT, EdD, OCS, MTC4
Alexis Nelson, BS, MS5
Tristan Hayes, MS3,6
Chi-Yang Chiu, PhD6
David L. Bernholt, MD1
Frederick M. Azar, MD1
Thomas W. Throckmorton, MD1
1 Department of Orthopaedic Surgery and Biomedical Engineering, University of Tennessee Health Science CenterCampbell Clinic, Memphis, Tennessee
2 College of Medicine, University of Tennessee Health Science Center, Memphis, Tennessee
3 Department of Physical Therapy, College of Rehabilitation Sciences, University of St. Augustine for Health Sciences, Austin, Texas
4 Department of Physical Therapy, University of Tennessee Health Science Center, Memphis, Tennessee
5 College of Graduate Health Sciences in the Biomedical Sciences Program, University of Tennessee Health Science Center, Memphis, Tennessee
6 Biostats, Epidemiology, and Research Design (BERD) Clinic, University of Tennessee Health Science Center, Memphis, Tennessee
Reprinted with permission from:
J Shoulder Elbow Surg. 2023:S10582746(23)0078-5.
Corresponding Author:
Thomas W. Throckmorton, MD
1211 Union Avenue, Suite 510 Memphis, Tennessee 38104 tthrockmorton@campbellclinic.com
Preoperative teres minor insufficiency has been identified as a risk factor for poor restoration of external rotation (ER) after reverse total shoulder arthroplasty (RTSA). However, there has been little investigation regarding muscle activation patterns generating ER. This prospective study sought to determine the timing and activation levels of the shoulder girdle musculature during ER in well-functioning RTSAs with an intact teres minor using a lateralized design.
Patients who underwent RTSA > 1 year previously with functional ER, an American Shoulder and Elbow Surgeons (ASES) score > 70, superior rotator cuff deficiency, and an intact teres minor were identified. Electrophysiological and kinematic analyses were performed during ER in the modified neutral position (arm at side with 90° of elbow flexion) and in abduction (AB) (shoulder abducted 90° with 90° of elbow flexion). Dynamometer-recorded torque and position were pattern matched to electromyography during ER. The root-mean-square and integrated electromyography (in microvolts x milliseconds with standard deviation [SD]), as well as median frequency (MF) (in hertz with SD), were calculated to determine muscle recruitment. Pair-wise t test analysis compared muscle activation (P < .05 indicated significance).
After an a priori power analysis, 16 patients were recruited. The average ASES score, visual analog scale pain score, and ASES subscore for ER in AB (‘‘comb hair’’) were 87.7, 0.5, and 2.75 of 3, respectively. In AB, muscle activation began with the upper trapezius, middle trapezius, and latissimus dorsi, followed by the anterior deltoid activating to neutral. With ER beyond neutral, the teres major (9.6 mV x ms; SD, 9.2 mV x ms) initiated ER, followed by the teres minor (14.1 mV x ms; SD, 18.2 mV x ms) and posterior deltoid (11.1 mV x ms; SD, 9.3 mV x ms). MF analysis indicated equal contributions of the teres major (1.1 Hz; SD, 0.5 Hz), teres minor (1.2 Hz; SD, 0.4 Hz), and posterior deltoid (1.1 Hz; SD, 0.4 Hz) in ER beyond neutral. In the modified neutral position, the upper trapezius and middle trapezius were not recruited to the same level as in
AB. For ER beyond neutral, the teres major (9.5 mV x ms [SD, 9 mV x ms]; MF, 1.1 Hz [SD, 0.5 Hz]), teres minor (11.4 mV x ms [SD, 15.1 mV x ms]; MF, 1.1 Hz [SD, 0.5 Hz]), and posterior deltoid (8.5 mV x ms [SD, 8 mV x ms]; MF, 1.2 Hz [SD, 0.3 Hz]) were activated in similar sequence and intensity as AB. No differences in muscle activation duration or intensity were noted among the teres major, teres minor, and posterior deltoid (P > .05).
Conclusion
Active ER after RTSA is complex and is not governed by a single muscle-tendon unit. This study establishes a sequence, duration, and intensity of muscle activation for ER in well-functioning RTSAs. In both tested positions, the teres major, teres minor, and posterior deltoid function equally and sequentially to power ER.
Austin Sturdivant, BS1
Christian Roberts, BS, MBA1
Andrew Nahr, MD2
Kayla G. Bryan, MD3
Benjamin W. Sheffer, MD2
David D. Spence, MD2
Jeffrey R. Sawyer, MD2
Derek M. Kelly, MD2
1 University of Tennessee Health Science Center, Memphis, Tennessee
2 Department of Orthopaedic Surgery and Biomedical Engineering, University of Tennessee Health Science CenterCampbell Clinic, Memphis, Tennessee
3 Department of Anesthesiology and Neurosurgery, University of Tennessee Health Science Center, Memphis, Tennessee
The American Society of Anesthesiologists (ASA) recommends fasting before surgery: clear liquids (2 hrs), breast milk (4 hrs), light meal (6 hrs), and fried foods/fatty foods/meat (> 8 hrs). In emergencies, guidelines are bypassed for timely surgical intervention. Pediatric post anesthesia complications caused by violating fasting guidelines remain controversial. The aim of this study was to compare the risk of postanesthetic complications in patients who met and did not meet ASA fasting guidelines for pediatric orthopaedic emergency procedures.
Reprinted with Permission:
J Pediatr Orthop N Amer. 2023:5(4)
Corresponding Author:
Derek M. Kelly, MD
1211 Union Avenue, Suite 510 Memphis, Tennessee 38104
dkelly@campbellclinic.com
Patients were retrospectively identified who had emergent procedures at a level 1 pediatric trauma center from 2010 to 2020. Patients were divided into two groups: those meeting current ASA fasting criteria of fasting and those who did not. Charts were reviewed for complications of gastric content aspiration during or following anesthesia.
There were 321 patients who met inclusion criteria for emergency orthopaedic surgeries. Of these, 264 (82%) met fasting guidelines, and 57 (18%) did not. One patient who met preoperative fasting status needed postoperative supplemental oxygen and met criteria to be reported as an adverse event. Of the 57 patients not meeting fasting guidelines, there were no anesthesia-reported adverse events.
No increased risk was found with anesthesia in nonfasted patients with orthopaedic emergencies undergoing general anesthesia during the perioperative period in this underpowered, pilot study. No respiratory complications (pulmonary aspiration, intraoperative or postoperative emesis, or postoperative respiratory support) were reported in patients who did not meet fasting guidelines. The authors believe this is a valuable starting point for further research into fasting criteria in pediatric trauma patients.
Nathan R Mulroy, MD1
Rumana Siddique, PhD2
Benjamin W. Sheffer, MD3
John C. Hyden, MD3
Jonathan K. Rowland, BS4
Derek M. Kelly, MD3
1 University of Tennessee Health Science Center, Memphis, Tennessee
2 Children’s Foundation Research Institute, Le Bonheur Children’s Hospital, Memphis, Tennessee
3 University of Tennessee Health Science Center -Campbell Clinic Department of Orthopaedic Surgery and Biomedical Engineering, Memphis, Tennessee
4 Le Bonheur Children’s Hospital, Memphis, Tennessee
Contact sports concussions have been linked to long-term sequelae such as chronic traumatic encephalopathy. Safety protocols were implemented over the past 15 years to reduce American tackle football concussions.
We hypothesized concussion rates among youth (5-19 years) tackle football participants would decline over the study period.
A stratified probability sample of patients (5-19 years) from 2012-2019 was obtained from the National Electronic Injury Surveillance System of U.S. Hospitals. Concussion and lower-extremity injury codes were two injury subsets. The control group included lower-extremity injuries, which remained relatively stable during a previous study interval. A Z-test compared variable and year estimates. P values less than 0.05 were considered statistically significant. Participation statistics from the National Federation of State High School Associations were obtained for high school football players from 2012 to 2018 (2019 unavailable at time of study).
Institutional review board approval was obtained from the University of Tennessee Health Science Center (# 20-07695-XR).
Corresponding Author:
Derek M. Kelly, MD
1211 Union Avenue, Suite 510 Memphis, Tennessee 38104
dkelly@campbellclinic.com
Football-related concussions statistically significantly declined from 2012-2019 (P<0.001); the mean number of concussions of the percent of estimated sample decreased yearly by 1.018 (95% CI, 1.01, 1.02). Lowerextremity injuries statistically significantly reduced during the study period (P<0.001); the mean number of lower-extremity injuries of the percent of estimated sample decreased yearly by 1.047 (95% CI, 1.045, 1.048). Percentages of football-related injuries for both groups remained relatively stable during this time. Participation declined steadily at the high school level from 2012 to 2018.
Falling rates of concussion and lower-extremity trauma could be caused by declining participation rates or implemented safety measures. Rising concussion rates among youth athletes after safety and rule changes at professional and college levels have tapered off with more consistent diagnosis and awareness of concussions. It is unclear if falling concussion rates among youth football players over the past decade have outpaced decline in participation.
Concussions in contact sports are an ever-increasing area of focus in both the public and sports medicine due to recent links made between concussions and development of long-term, and at times even life-long, sequalae such as post-traumatic headache, post-traumatic epilepsy, post-traumatic vertigo and dizziness, and most notably chronic traumatic encephalopathy (CTE), which has been linked to increased rates of cognitive impairment, behavior changes, personality changes, depression, suicidality, parkinsonism, and speech and gait abnormalities.4,14 The publicity around prominent athletes who have suffered the sequelae of concussions and the growing medical literature on these issues have raised public awareness and led to the need for sports leagues, from youth to the highest levels of professional sports, to implement rule changes to limit traumatic brain injuries, establish concussion detection protocols, and improve safety equipment over the past 15 years.10
Concussion rates have increased over time, possibly due to improved recognition and awareness.7 Although concussion rates are the highest among men, particularly in football, wrestling, ice hockey, and lacrosse where collisions and contact are inherent to the sports, girls' and women's soccer rates are also high.13 There appears to be a correlation between playing experience and concussion rates and severity, with less experienced players having greater concussion risks and more severe injuries.1 The concussion rate for men’s sports (1.0; 95% CI, 0.97-1.03) was higher than that for women’s sports (0.91; 95% CI, 0.87-0.95); however, in four of the five sports in which both women and men participated, women had a higher rate of concussion injury.2 In football, practice duration and more intense contact practice sessions increase the risk of a player sustaining a concussion more than the number of practices held by a team.18 With increased recognition of a possible association between repetitive head impact exposure and concussion, efforts at reducing concussion incidence in contact sports should include a reduction in overall head impact exposure.11,17
Studies evaluating the effectiveness of interventions and regulations on reducing head impact exposures or head injuries have shown mixed results. Some regulations may be more effective than others, but meth-
odological design and risk of bias pose limitations to generalize effects.12 Thus far, even at the highest level of professional competition such as the National Football League, well-intentioned rules adopted every season by the NFL have been proven to be too weak to make the game safer. Broad-based management of brain and orthopaedic injuries and adoption of preventative measures to reduce the number of players injured and the seriousness of their injuries are required in the modern NFL.16
This study focused on concussion incidence in tackle football at the youth level as participants in these age groups make up approximately 70% of all tackle football participants.19 The objective of this study was to determine whether the changes that have been made to tackling techniques, safety protocols, and safety equipment at the middle school and high school levels have led to a reduction in the incidence of concussions in tackle football in the United States (US) over the past decade. We hypothesized that concussion rates among youth participants in tackle football would decline over the study period.
This study examined the estimated number of emergency department visits in the United States associated with football for victims ages 5 to 19 years who were treated for football-related concussions and lower-extremity injuries from 2012 to 2019. Study data were obtained from the National Electronic Injury Surveillance System (NEISS) which is a freely available, de-identified nationwide database operated by the US Consumer Product Safety Commission; it gathers data from approximately 100 hospitals selected as a probability sample. The probability sample was obtained by dividing the entire population into different subgroups or strata, then randomly selecting the final subjects proportionally from the different strata of all 6,100 US hospitals that have a minimum of 6 beds with a 24-hour emergency department and extrapolating or estimating national numbers for the entire United States.3,15 A stratified probability sample was obtained from the NEISS of US hospitals for the years 2012 through 2019. The study did not examine data beyond 2019 due to concerns that coronavirus disease 2019 (COVID-19) would have affected sports participation during 2020 and 2021. The authors ob-
tained data on football-related concussions and lower-extremity injuries in children 5 to 19 years of age treated in emergency departments for the years 2012 through 2019. Lower-extremity injuries were used as a control because a previous study with similar design had shown that incidence of lower-extremity injury had remained stable over time.8 No specific inclusion or exclusion criteria were needed because the information was obtained by running codes for ages 5 to 19 years. All estimates were included. Variables studied were emergency department visits related to football injury, football-related concussions, football-related lower-extremity injuries, age, sex, and location (school place of recreational sports, other or unknown). Participation data were obtained for participation rates in 11-player football from the National Federation of State High School Associations (NFHS) for high school football players from 2012 to 2018 as the data from 2019 had not yet published at the time of this study.9
Trend analysis was used for observing the trend of the estimates of football-related concussion and football-related lower-extremity injury over the study interval with a 95% confidence interval and statistical significance of P-value less than 0.05. The trend of the number of participants in football was also observed using the trend analysis with a 95% confidence interval and statistical significance of P-value less than 0.05. All analyses were done using SAS 9.4 (SAS Corporation, Cary, NC).
There was a statistically significant reduction in the overall number of football-related concussions from 2012 to 2019 (P < 0.001). Every year, the mean number of concussions of the percent of estimated sample decreased yearly by 1.018 (95% CI, 1.01, 1.02) (Table 1).
The data also showed that there was a statistically significant reduction from 2012 to 2019 in the number of lower-extremity injuries related to football as well (P < 0.001). The mean number of lower-extremity injuries of the percent of the estimated sample decreased yearly by 1.047 (95% CI, 1.045, 1.048) (Table 2)
The data were plotted alongside each other as a function of time to further illustrate this point (Figure 1)
of the short-term and long-term sequelae discussed previously. Emphasis on safer tackling techniques, heavier in-game penalties for dangerous contact, and improvements in helmet design have been implemented over the past 15 years with the intention of reducing the incidence in concussions related to American tackle football. The aim of this study was to determine whether these changes have led to a meaningful reduction in the number of concussions sustained by youth athletes participating in this sport over the past decade. We hypothesized that concussion rates among youth participants in tackle football would decline over the study period.
While there was a statistically significant reduction in both concussion and lower-extremity injury rates during the study interval, the percentage of football-related injuries for both concussion and lower-extremity stayed relatively stable over the designated study interval. This raised the question of whether the lack of change in the percentage of all concussions and lower-extremity injuries relative to the declining overall incidence of each injury might be attributed to
The percentage of football-related injuries for both concussion and lower-extremity stayed relatively stable over the designated study interval (Table 3)
Data obtained from the NFHS found that national participation rates at the high school level declined from 2012 through 2018 (Figure 2).
Concussions in American tackle football continue to be an area of focus in sports medicine because
declining participation numbers nationally. This could be due in part to falling participation rates; however, NEISS data uses estimated values,6 whereas NFHS data provides the exact number. This does not give a reliable estimate of association between the datasets. The possibility also remains that safety measures have an effect; however, this is difficult to measure or quantify which is a limitation to this study. The results of this study do indicate a fall in the rate of concussion diagnosis among youth participants in American tackle football over the 2010s, but it remains unclear to what this decline can be attributed. It is possible that rule changes and safety measures have played a key role, but declining participation numbers over the same time period cloud the issue and make it difficult to determine the true benefit of safety improvements. Another factor that may be contributing to a lower incidence of concussions presenting to the emergen-
1. Bayram JM, Hamilton DF, Saunders DH. Epidemiology of American football injuries at universities in the United Kingdom. Orthop J Sports Med. 2020;8(10): 2325967120960206. PMID: 33195720
2. Chun BJ, Furutani T, Oshiro R, et al. Concussion epidemiology in youth sports: sports study of a statewide high school sports program. Sports Health. 2021;13(1):18-24. PMID: 32716762
3. Consumer Product Safety Commission. The National Electronic Injury Surveillance System: A Tool for Researchers. http://www.cpsc.gov/en/ Research--Statistics/NEISS-Injury-Data/. Published 2000. Accessed January 17, 2023.
4. Evans RW, Furman JM. Sequelae of mild traumatic brain injury. UpToDate web site. https://www.uptodate.com/contents/sequelae-ofmild-traumatic-brain-injury. Accessed March 21, 2021.
5. Guerriero RM, Proctor MR, Mannix R, et al. Epidemiology, trends, assessment and management of sport-related concussion in United States high schools. Curr Opin Pediatr. 2012;24(6): 696-701. PMID: 23042252
6. Kessler, E. and T. Schroeder. NEISS Sample (Design and Implementation), Washington, DC: U.S. Consumer Product Safety Commission. October 1999.
7. Lincoln AE, Caswell SV, Almquist JL, et al. Trends in concussion incidence in high school sports: a prospective 11-year study. Am J Sports Med. 2011;39(5):958-63. PMID: 21278427
8. Naranje SM, Erali RA, Sawyer JR et al. Football-related concussion and lower extremity injuries: have changes in the NFL/NCAA had any effect on younger participants? Campbell Orthop J. 2017;3:72-76.
9. National Federation of State High School Associations. Participation Statistics. NFHS web site. Available at: https://members.nfhs.org/ participation_statistics. Published 2000. Accessed April 2022.
10. National Football League. The National Football League Player Healthy and Safety Guidelines. National Football League web site. https://operations.nfl.com/inside-football-ops/players-legends/playerhealth-safety/. Accessed October 2022.
cy department is the increasing number of providers who treat concussion outside of the emergency department. It is becoming more common in the United States to have athletic trainers, primary care providers, and primary care sports medicine physicians manage concussion outside of the emergency room, and this study does not account for this possibility.5
It does appear that the initial phase of rising concussion rates has gradually tapered off now that the diagnosis is being made consistently due to the heightened awareness and emphasis on identifying players who may have sustained a concussion. However, without exact numbers, it remained unclear if the falling concussion rates among youth football players over the past decade is outpacing the overall decline in participation.
11. Pfaller AY, Brooks MA, Hetzel S, et al. Effect of a new rule limiting full contact practice on the incidence of sport-related concussion in high school football players. Am J Sports Med. 2019;47(10):2294-2299. PMID: 31306587
12. Phillips N, Crisco JJ. The effectiveness of regulations and behavioral interventions on head impacts and concussions in youth, high-school, and collegiate football: a systematized review. Ann Biomed Eng. 2020 Nov;48(11):2508-2530. PMID: 33051744
13. Pierpoint LA, Collins C. Epidemiology of sport-related concussion. Clin Sports Med. 2021;40(1):1-18. PMID: 33187601
14. Ryan LM, Warden DL. Post concussion syndrome. Int Rev Psychiatry. 2003;15(4):310-306. PMID: 15276952
15. Schroeder T, Ault K. The NEISS Sample Design and implementation 1997 to present. Bethesda MD: US Consumer Product Safety Commission Division of Hazard and Injury Data Systems; 2021.
16. Sheth SB, Anandayuvaraj D, Patel SS, Sheth BR. Orthopaedic and brain injuries over last 10 seasons in the National Football League (NFL): number and effect on missed playing time. BMJ Open Sport Exerc Med. 2020 Apr 5;6(1):e000684. PMID: 32341797
17. Stemper BD, Shah AS, Harezlak J, et al. Repetitive head impact exposure in college football following an NCAA rule change to eliminate two-a-day preseason practices: a study from the NCAA-DoD CARE Consortium. Ann Biomed Eng. 2019;47(10):2073-2085. PMID: 31388849
18. Stemper BD, Shah AS, Mihalik JP, et al. Head impact exposure in college football after a reduction in preseason practices. Med Sci Sports Exerc. 2020;52(7):1629-1638. PMID: 32541378
19. Wong AH, Wong AK, Balles JE. Frequency magnitude, and distribution of head impacts in Pop Warner football: the cumulative burden. Clin Neurol Neurosurg. 2014; 118:1-4. PMID: 24529219
Bhanu Shukla, PhD1
Lisa Lucks Mendel, PhD1
Monique Pousson, MS1
Hailey Wilson, BS1
Kara Sander, BA1
Jonathan K. Rowland, BS2
Jeffrey R. Sawyer, MD3
1 School of Communication Sciences and Disorders, University of Memphis, Memphis, Tennessee
2 Le Bonheur Children’s Hospital, Memphis, Tennessee
3 University of Tennessee Health Science Center-Campbell Clinic Department of Orthopaedic Surgery and Biomedical Engineering, Memphis, Tennessee
Appreciation is expressed to Cheryl Perkins, RN for assistance with operating room protocol during data collection.
Portions of this work were funded by a microgrant from the Pediatric Orthopaedic Society of North America (POSNA).
Institutional review board approval was obtained from the University of Tennessee Health Science Center (20-7662-XP).
Chronic exposure to damaging noise levels has been linked to negative health outcomes among staff members and reductions in the quality of patient care. In addition, the presence of background noise in operating rooms (OR) can interfere with effective communication. The purpose of this study was to investigate the impact of noise levels on surgical team members during posterior spinal fusion (PSF) for the treatment of adolescent scoliosis.
Surgical team members completed an initial hearing screening and answered pre- and post-surgery questionnaires regarding their perceptions of the background noise in the operating room. Sound level measurements were recorded for 10 PSF surgeries in locations within the OR.
Noise levels averaged 66.20 decibels (dBA) across the 10 PSF surgeries. The average peak level was 85.16 dBA; however, levels as high as 107 dBA were measured at times.
Although average sound levels across all procedures did not reach levels considered to be potentially damaging to hearing, those closest to the patient (i.e., surgeon, orthopaedic fellow) recorded negative effects of background noise on their ability to hear and communicate, and all members of the surgical team experienced some level of impaired communication during PSF.
Corresponding Author:
Jeffrey R. Sawyer, MD
1211 Union Avenue, Suite 510 Memphis, Tennessee 38104 jsawyer@campbellclinic.com
Effective communication among healthcare staff members is integral to optimal efficiency and patient safety.1 However, the pervasive presence of noise, commonly defined as “unwanted sound,” remains a barrier to successful spoken communication. A high level of noise is a significant risk factor in the development of noise-induced hearing loss and has been associated with stress and fatigue among hospital staff,2-4 reduced job productivity,5 and even employee burnout.6 Noise exposure has been empirically proven to negatively impact patient well-being as well,7-12 which
can result in increased healthcare burden as evidenced by a higher risk of re-hospitalization13 and extended hospital stays.14 Reducing the negative effects of noise exposure may improve communication between healthcare workers as well as between patients and staff, subsequently leading to fewer patient complications.15,16
Concerns regarding increasing noise levels in hospitals have led to the creation of targeted guidelines from the World Health Organization (WHO) and the Occupational Safety and Health Administration.17,18 WHO identified occupational noise exposure as a primary work-related risk factor, second only to workplace injuries, but, fortunately, exposure to damaging noise levels is preventable.17 Noise is a prevalent issue in hospitals, with average noise levels steadily increasing 20 to 40 dB since the 1960s19 and continuing to rise. Further, noise levels within operating rooms (ORs) range from 58 to 67 decibels (dBA),20,21 which is considerably above international standards.22 PSF surgeries, which typically last 5 to 6 hours, are complex procedures requiring efficient communication among multiple team members in the OR (a high-noise environment) to avoid complications such as irreversible spinal cord injury or even death.
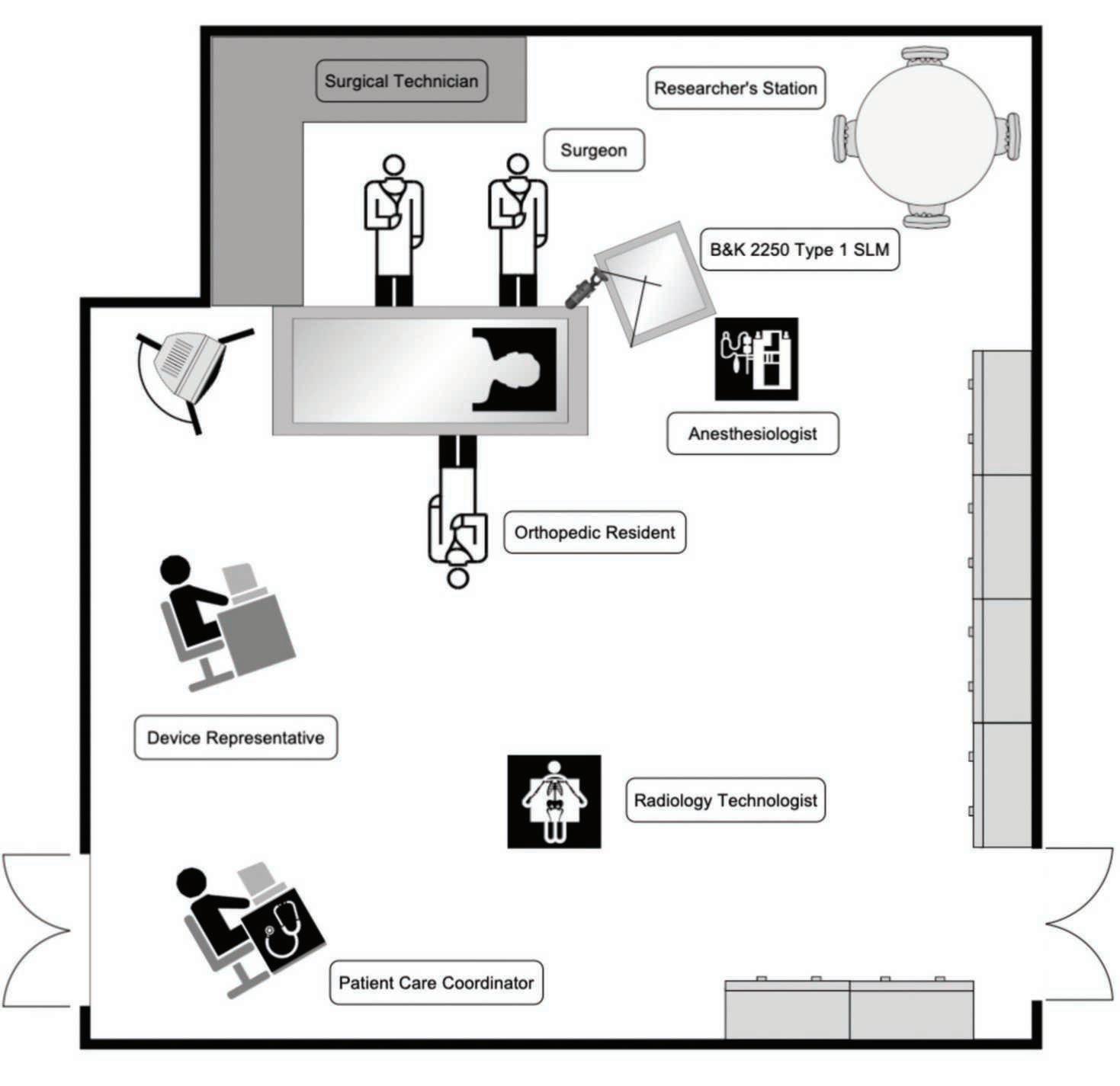
Previous research has focused primarily on the effects of noise on specific healthcare workers in concentrated work environments23 and less on the effects of fluctuating noise during ongoing procedures.24 The focus of this study was to determine the consequences of noise levels on surgical team members working in different locations within the OR during PSF surgery. The purposes were: (1) to document noise levels in the OR during PSF and (2) to determine the impact on hearing, communication, and job performance of surgical team members. This knowledge can be used in the development of noise regulation strategies within ORs to increase patient safety.
This study was approved by the institutional review board (Approval # 20-7662-XP). Surgical team members were recruited to participate in this study. Although the institution has dedicated spinal surgery personnel, the team members present for each specific procedure varied. Team members were categorized as surgeon, surgical assistant, surgical technician, anesthesiologist/CRNA, circulator, neurophysiologist, radiology technician, and device representative. A single attending spine surgeon was present for all 10 PSF surgeries.
Two questionnaires were developed by the researchers: one completed by the participant before the surgery began, and the other after the surgery ended. The pre-surgery questionnaire included demographic and hearing-related questions, inquiring about any
daily hearing difficulties, frequent exposures to loud sounds, and use of hearing aids or hearing protection (Appendix A). The post-surgery questionnaire requested information related to participants’ perception of noise in the OR and its potential effect on them. In addition, participants were asked to rate their perception of the loudest parts of the surgery and the overall procedure and whether they thought the noise impeded communication or the ability to concentrate and perform or if they perceived any vocal strain ranked on a scale of 0 (no effect) to 7 (greatest effect) (Appendix B)
After signing the informed consent, each participant underwent an otoscopic examination and hearing screening at 25 dB HL at 500, 1000, 2000, and 4000 Hz in both ears. The participants were then asked to complete the pre-surgery questionnaire. At the conclusion of each surgery each participant was asked to complete the post-surgery questionnaire within 24 hours.
Sound level meter (SLM) measurements were taken during 10 PSF surgeries spanning a 6-month period. The surgical procedure was divided into six phases, each lasting about 1 hour: baseline, opening (room set up), spine exposure, pedicle screw placement, curve correction, and closure. A minimum of 5 hours of SLM measurements were taken during each surgery. SLM measurements were recorded using a Type 1 Brüel & Kjær 2250 SLM (B&K; Nærum, Denmark) with a ½ inch Type 4189 microphone for the duration of each surgery. In addition, measurements were recorded at five different locations in the OR using a Reed R8080 handheld Type 2 SLM (Reed Instruments, Wilmington, NC). Figure 1 displays the locations in the OR where measurements were taken, including anesthesia, surgeon, radiology technician, orthopaedic fellow/ resident, surgical technician, neurophysiologist, and the circulating nurse locations.
Before each PSF, the microphone of the B&K 2250 Type 1 SLM was calibrated and secured approximately 24 inches above the left ear of the primary surgeon’s position at the OR table (Figure 2) and baseline noise measurements recorded. Noise levels were measured for 30 seconds at 10-minute intervals until

the surgery was completed. A fast, A-weighting setting was used to obtain the average sound level (LAF) along with minimum and maximum levels (LAFmin and LAFmax). In addition, LAeq (Equivalent Continuous Sound Pressure Levels) and peak levels with ‘C’ weighting (LCpeak) were measured. A dBA filter was used because the dBA measurement scale is most suited to human perception of noise intensity. Every hour during the surgery, noise measurements were also recorded for 1 minute using a Reed 8080 Type 2 SLM at each of five additional locations in the OR. Fast, A-weighting was used to obtain LAF, LAFmin, and LAFmax measurements.
Sound measurements were recorded for 10 PSF procedures in 8 patients with adolescent idiopathic scoliosis and 2 with neuromuscular scoliosis (4 males, 6 females; mean age 14.1 years). The mean surgical time and number of levels fused was 334 minutes and 14.5 levels, respectively. There were no perioperative complications during the study period.
Twenty-nine adult (15 women, 14 males; ages 22-60 years [mean 37 years]) spine-specific surgical team members who were assigned to a study room participated in the study. Of the 29 who participated, 90% passed the hearing screening test in both ears. Three participants (10%) had some baseline hearing loss, with one (3%) having elevated hearing thresholds of 30 and 40 dB at 4000 Hz in both ears and two (6%)
Table 1: Noise levels of common everyday equipment for comparison
levels (LAFmax) for a typical case, highlighting sound peaks associated with pneumatic burr use.
having 30 dB thresholds at 250 Hz in one ear. A total of 53 (76%) survey responses from 29 unique team members were reviewed.
The mean baseline OR sound level was 60 to 70 dBA, depending on the specific location in the room, with the highest baseline level being in the anesthesiologist’s position. The mean sound level (LAF) for each procedure was 66.2 dBA (range, 60.7-74.7 dBA, max 107 dBA). The average sound level with peak weighting (LC peak) was 85.2 dBA. For comparison, Table 1 shows average noise levels produced by common everyday equipment.
Levels recorded at the typical distance an individual would be from the noise. (Information derived from the Noise Pollution Clearinghouse, Montpelier, VT. https://www. nonoise.org/library/household/index.htm Accessed December 22, 2022.)
The mean time-weighted average sound level (LAEq) was 64.3 dBA as shown in Figure 3. Peak sound levels were noted during pedicle screw placement, which was related to the use of the pneumatic burr for pedicle screw starting holes (>100 dBA). The mean sound levels by surgical phase and location were reproducible across procedures and did not exceed 70 dBA, (Figure 4). Figure 5 shows average (LAF) and maximum sound
Sound levels had the greatest effect on the surgeon during the self-reported loudest portions of the procedure compared with any other team member in terms of ability to communicate, job performance, and vocal strain. When considering the procedures in their entirety, however, the surgeon was not the most affected compared with the other team members. In terms of effect on team communication, noise levels affected all members of the team both at subjective peak levels (mean rating 3.9: scale 0-7m) and during the entire procedure (mean rating 2.8). Most impacted by peak noise levels were the surgeon (5.6/1.4x mean) and the radiology technician (4.6/1.2x mean) (Figure 6). Regarding vocal strain, the mean level of noise impact was 3.2 (scale 0-7). All team members experienced vocal strain, but those with the most vocal strain during the loudest portions of the procedure were the surgeon (5.6/1.8x mean) and anesthesiologist 3.8/1.2x mean). When considering the entirety of procedures, most team members experienced similar levels of vocal strain (Figure 7).
With regard to job performance (mean 3.1: scale 0-7), the surgeon experienced the greatest impairment during the loudest portions of the procedure (5.3/1.7x
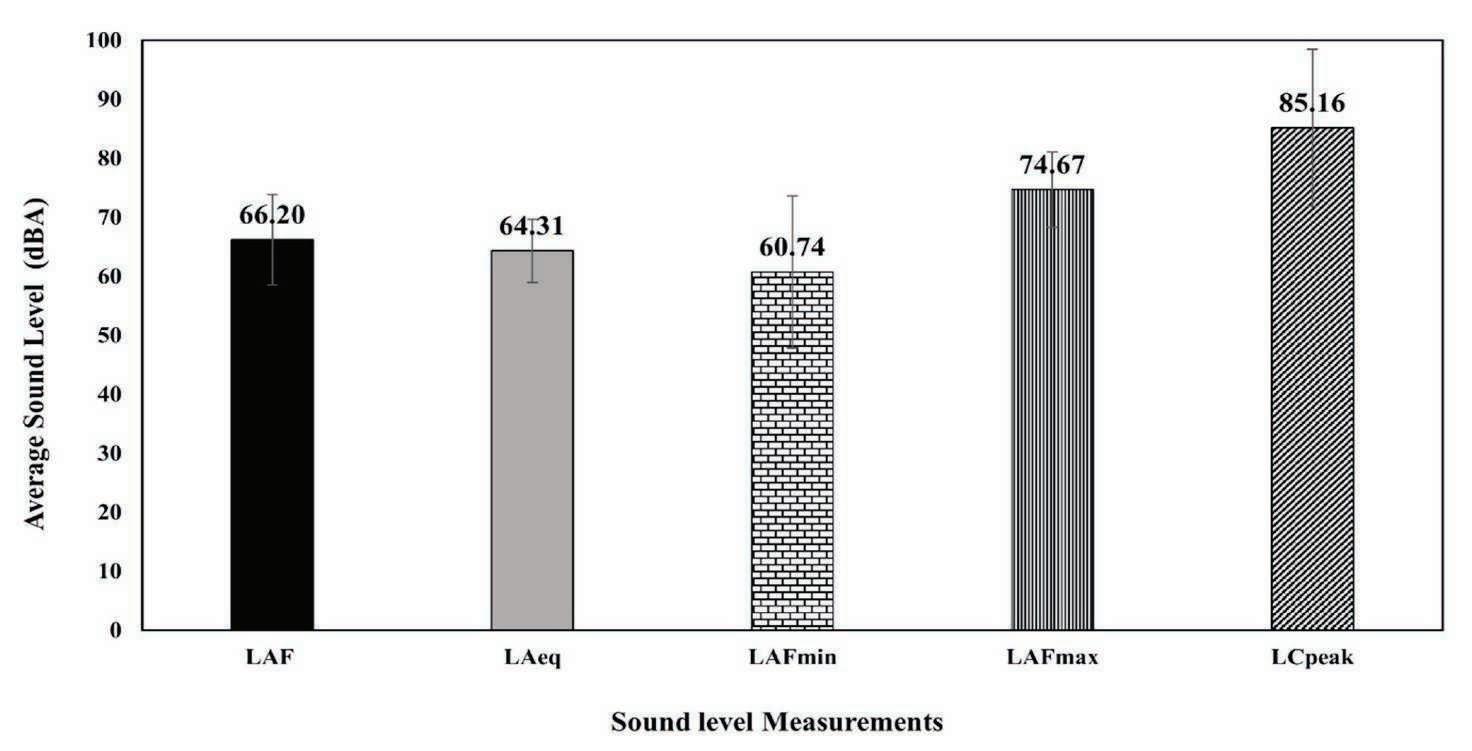
Figure 3:
level;
equivalent continuous sound pressure level
a measure that represents a varying sound over a period of time. LC peak= peak levels with C weighting. Frequency weightings are used to ensure that the sound level meter is accurately measuring what is actually being heard by an individual. The “A” weighting cuts off the lower and higher frequencies that humans usually cannot hear, and the “C” weighting is used for peak measurements (100 dB and above).
mean) followed by the circulating nurse (3.8/1.2x mean) and radiology technician (3.8/1.2x mean). Interestingly, the circulating nurses and the surgical assistants experienced higher levels of job impairment during the entire procedure than the surgeon (Figure 8)
To our knowledge this study is the first to document noise levels measured in the OR during PSF surgery for adolescent idiopathic scoliosis (AIS). The sound levels measured were similar to previous studies that found levels in the OR to range between 58 and 67 dBA.20,21 Overall, the measurements of sound level taken during these procedures were consistent and predictable for each procedure in the study period. Fortunately, they were below levels that could damage hearing for the OR team and the patient.18
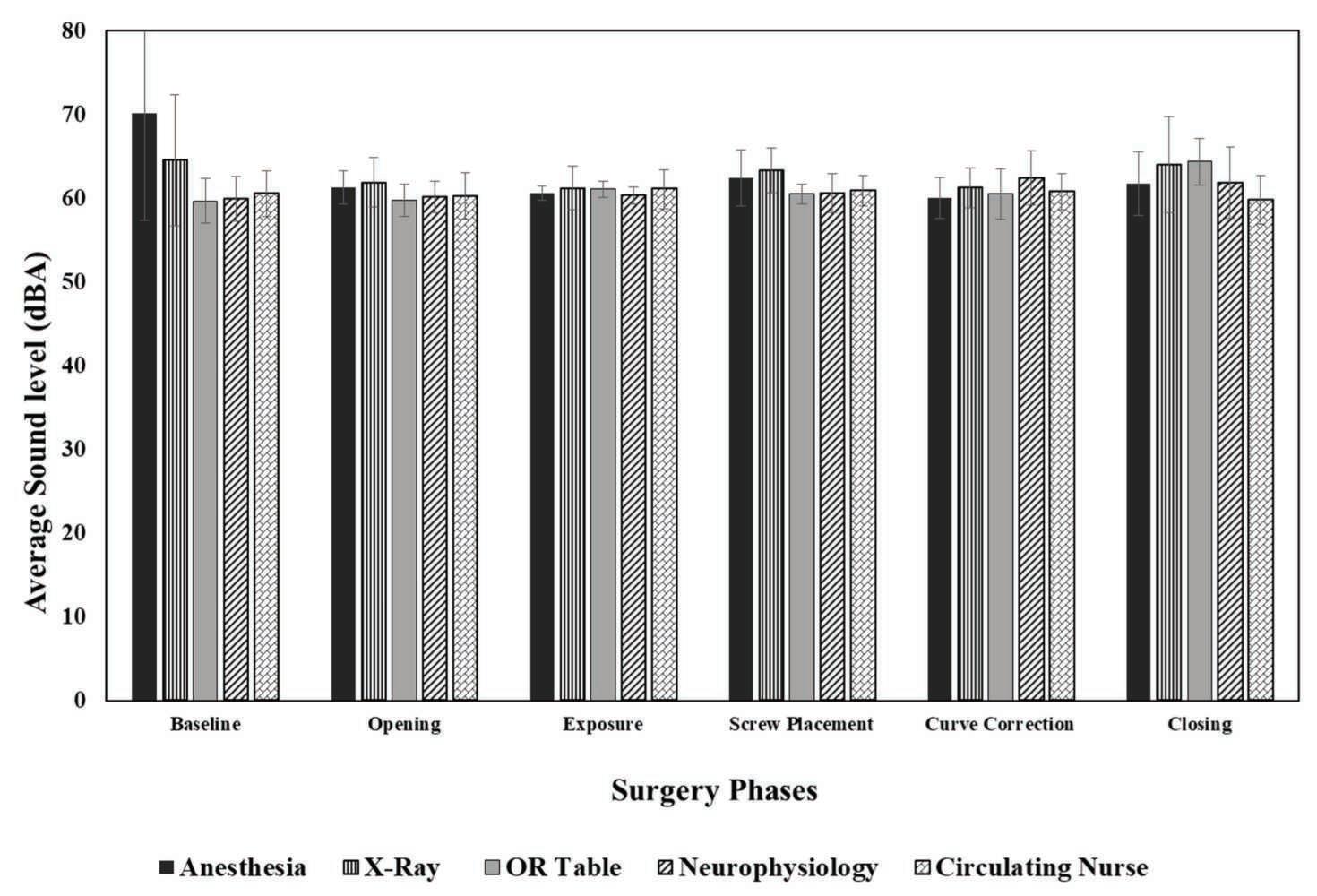
Despite the fact that the noise levels were not loud enough to cause hearing damage, responses to the post-surgery questionnaire provided insight into the potential impact on communication, job performance, and vocal strain of surgical team members. The surgical team members differed considerably in their

Figure 5:
PSF procedure (Case 10). LAeq = equivalent continuous sound pressure level is a measure that represents a varying sound over a period of time. LC peak= peak levels with C weighting. Frequency weightings are used to ensure that the sound level meter is accurately measuring what is actually being heard by an individual. The “A” weighting cuts off the lower and higher frequencies that humans usually cannot hear, and the “C” weighting is used for peak measurements (100 dB and above).
perceptions of the noise, which is not surprising given the varying distances from the noise-generating equipment as well as the variability in the need to verbally communicate with the team based on their role. Some roles may not require as high a level of communication for effective job performance. Interestingly, the surgeon was most affected during peak noise levels across all three metrics including communication, vocal strain, and job performance but was not the most affected when considering the entirety of the procedures compared with other team members. Although the surgeon is the leader of the surgical team and must communicate with all members, each within a unique noise environment, important information is continuously being relayed among other team members independent of the surgeon. Background noise can impair communication among staff members, decreasing their job efficiency and ultimately compromising patient care. In fact, the Joint Commission noted that 70% of medical errors in emergency departments were the result of “communication short-
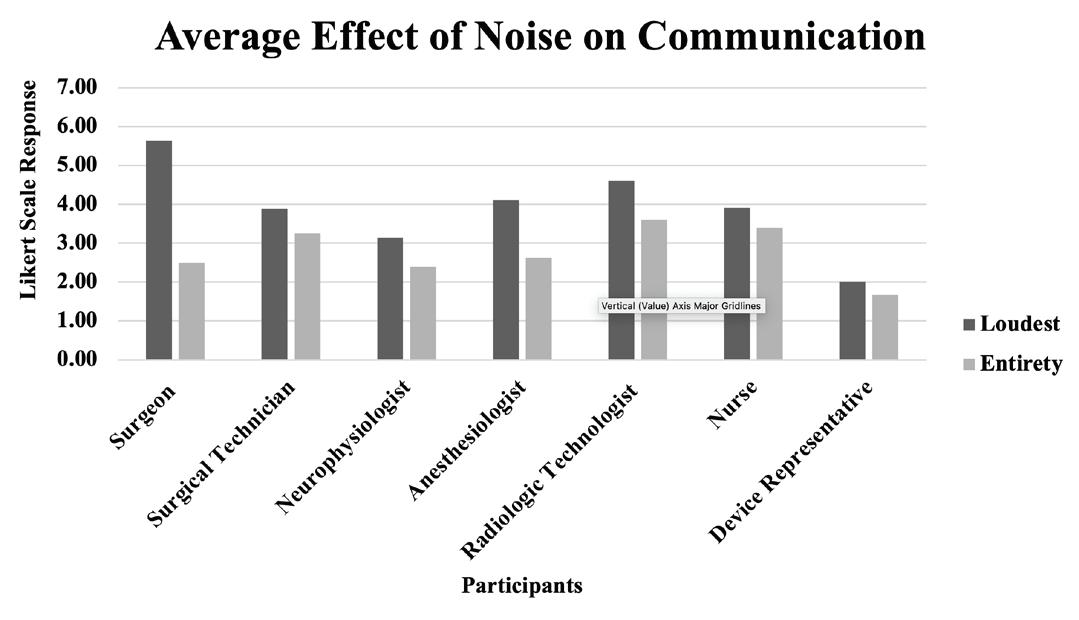
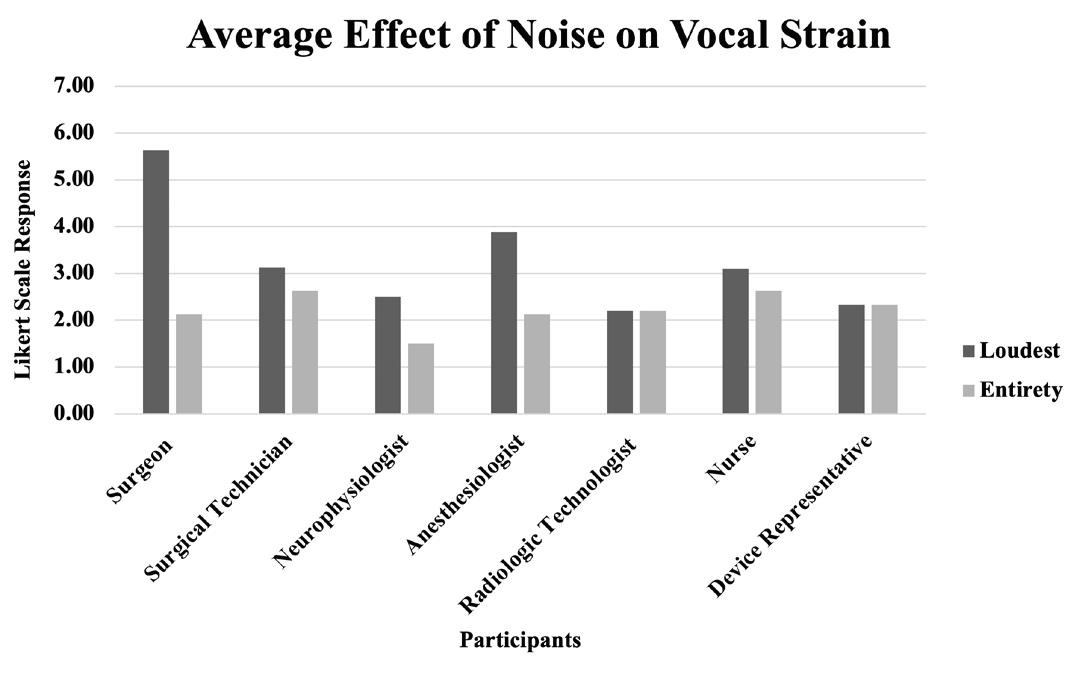
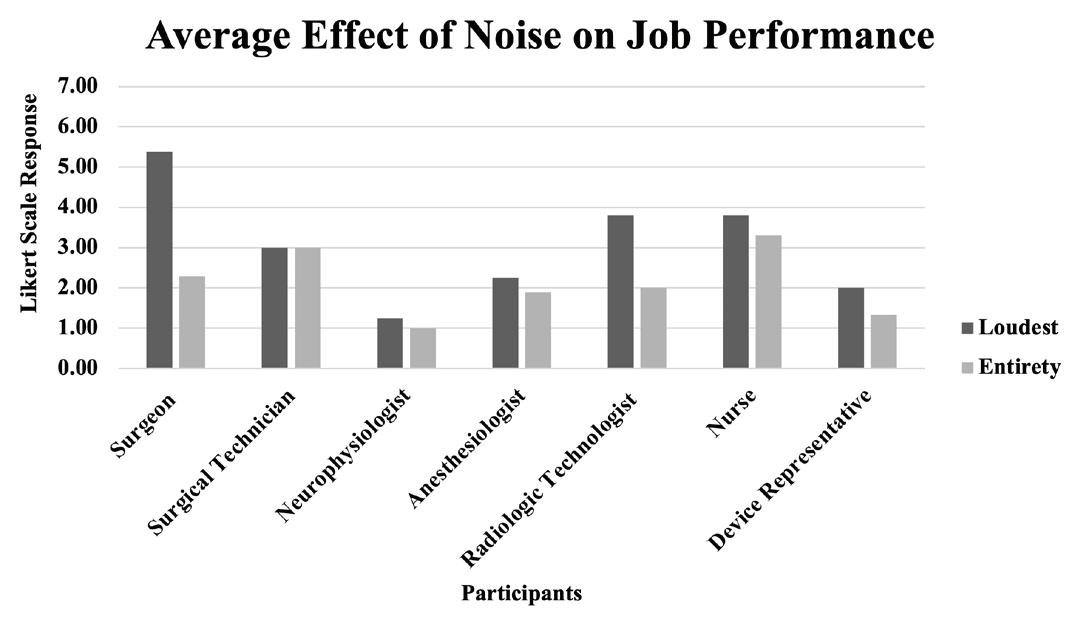
been shown to be an occupational hazard to personnel29 and to impair communication and cognition.30 In addition, certain noises, such as conversation, even at lower levels, can result in distraction during complex thought processes.31 The findings of this study highlight the complex nature of sound measurements and their effects on communication and performance.
This study has several limitations. Team members may have altered their behaviors, or their perceptions may have changed based on the nature of the questionnaire before surgery or by having sound-measuring equipment and an observer in the OR (Hawthorne effect). However, although each surgery had a different team, intraoperative measurements remained highly consistent. Nevertheless, one must consider that this consistency may have been related to the fact that the noise-generating equipment is set-up in standardized locations within the OR for this particular procedure. Another limitation is that even though the sophisticated equipment used in this study to measure true sound levels is extremely accurate, the effect of noise levels on any given individual is entirely subjective, and some participants may even have had difficulty providing accurate and/or complete responses on the questionnaire. We expected that similar sound levels would be perceived as more distracting by inexperienced team members who were less proficient in a given skill, but the exact opposite was demonstrated. The surgeon, having performed approximately 500 PSF surgeries and being the most experienced team member in the room, also experienced the highest levels of impairment in terms of communication, vocal strain, and job performance during peak noise levels. Last, this is a single-surgeon, single-center experience, so these results can be expected to vary between centers in terms of equipment, placement of equipment, experience level of the surgical team, and the way in which team members communicate (e.g., verbally or nonverbally).
comings,” which included multitasking and interruptions.25 Common and significant sources of OR noise include music, monitor alarms, forced-air warming devices, computer fans, and other OR equipment.26-28
With technological advancements, such as high-airflow operating rooms and other equipment, background noise levels continue to increase and have
Despite these limitations, this study highlights that OR noise levels during PSF for AIS are high, but below the level that can cause hearing damage. However, certain noise levels during the procedure, such as when using the pneumatic burr, can be potentially hazardous for the surgical team as well as the patient and should be considered for noise-reduction interventions. Noise levels differ by location in the OR,
and the effects they have on different team members are variable. This study demonstrates that increased noise levels adversely affect communication and job
performance during PSF surgery, and further study is necessary to develop noise-reducing strategies for all members of the team.
AAOS Now. Distractions in the Operating Room Threaten Patient Safety
https://www.aaos.org/aaosnow/2012/may/clinical/clinical5/
OSHA: Occupational Noise Exposure.
https://www.osha.gov/noise
Gouvernement du Québec: Noise Measurement
https://www.quebec.ca/en/health/advice-and-prevention/health-and-environment/the-effects-of-environmentalnoise-on-health/noise-measurement
SoundEar: Decibel Scale
https://soundear.com/decibel-scale/
1. Woloshynowych M, Davis R, Brown R, et al. Communication patterns in a UK emergency department. Ann Em Med. 2007; 50(4):407-413.
2. Topf M. Noise-induced occupational stress and health in critical care nurses. Hospital Topics. 1988; 66(1):30-34.
3. Morrison WE, Haas EC, Shaffner DH, et al.. Noise, stress, and annoyance in a pediatric intensive care unit. Crit Care Med. 2003; 31(1):113-119
4. Basner M, Babisch W, Davis A, et al. Auditory and non-auditory effects of noise on health. The Lancet. 2014; 383(9925): 1325-1332.
5. Gurses AP, Carayon P. Performance obstacles of intensive care nurses. Nursing Res. 2007; 56(3):185-194.
6. Topf M, Dillon E. Noise-induced stress as a predictor of burnout in critical care nurses. Heart Lung. 2007; 56(3):185-194.
7. Errett J, Bowden EE, Choiniere M, et al. Effects of noise on productivity: does performance decrease over time? Faculty Publications in Architectural Engineering. DigitalCommons@University of Nebraska - Lincoln. 2006; 13: 1-9. https://digitalcommons.unl.edu/ archengfacpub/13 . Accessed January 5, 2023.
8. Freedman NS, Gazendam J, Levan L, et al. Abnormal sleep/ wake cycles and the effect of environmental noise on sleep disruption in the intensive care unit. Am J Resp Crit Care Med. 2001; 163(2):451-457.
9. Gabor JY, Cooper AB, Crombach SA, et al. Contribution of the intensive care unit environment to sleep disruption in mechanically ventilated patients and healthy subjects. Am J Resp Crit Care Med. 2003; 167(5):708-715.
10. Bevan R, Grantham-Hill S, Bowen R, et al. Sleep quality and noise: comparisons between hospital and home settings. Arch Dis Childhood. 2018; 104(2):147-151.
11. Astin F, Stephenson J, Wakefield J, et al. Night-time noise levels and patients’ sleep experiences in a medical assessment unit in Northern England. Open Nurse J. 2020; 14(1):80-91.
12. Johansson L, Bergbom I, Waye KP, et al. The sound environment in an ICU patient room – a content analysis of sound levels and patient experiences. Intensive Crit Care Nurs. 2012; 28(5):269-279.
13. Hagerman I, Rasmanis G, Blomkvist V, et al. Influence of intensive coronary care acoustics on the quality of care and physiologics state of patients. Int J Cardiol. 2005; 98(2):267-270.
14. Fife D, Rappaport E. Noise and hospital stay. Am J Pub Health. 1976; 66(7):680-681.
15. Mazzocco K, Petitti DB, Fong KT, et al. Surgical team behaviors and patient outcomes. Am J Surg. 2009; 197(5):678-685.
16. Tschan F, Seelandt JC, Leller S, et al. Impact of communication within the surgical team on surgical site infections. Br J. Surg. 2015; 102(13):8.
17. World Health Organization. Regional Office for Europe. Environmental noise guidelines for the European Region. World Health Organization. Regional Office for Europe. https://apps.who.int/iris/ handle/10665/279952. Accessed
18. Occupational Safety and Health Administration. Occupational safety and health standards: Occupational health and environmental control (Standard No. 1910.95). https://222.osha.gov/laws-regs/regulations/ standardnumber/1910/1910.95. Accessed
19. Busch-Vishniac IJ, West JE, Barnhill C, et al. Noise levels in Johns Hopkins Hospital. J Acoust Soc Am. 2005; 118(6):3629-3645.
20. Kracht J, Busch-Vishniac IJ, West JE. Operating room noise at Johns Hopkins Hospital. J Acoust Soc Am. 2006; 119(5): 3385-3385.
21. Healey AN, Sevdalis N, Vincent CA. Measuring intra-operative interference from distraction and interruption observed in the operating theatre. Ergonomics. 2006; 49(5-6):589-604.
22. Shankar N, Malhotra KL, Ahuja S, et al. Noise pollution: a study of noise levels in the operation theatres of a general hospital during various surgical procedures. J Ind Med Assoc. 2001; 99(5):244, 246247.
23. Kurmann A, Peter M, Tschan F, et al. Adverse effect of noise in the operating theatre on surgical-site infection. Br J Surg. 2011; 98(7):1021-1025.
24. Keller S, Tschan F, Beldi , et al. Noise peaks influence communication in the operating room. An observational study. Ergonomics. 2016; 59(12):1541-1552.
25. The Joint Commission. Advancing Effective Communication. Cultural Competence, and Patient- and Family-Centered Care: A Roadmap for Hospitals. 2010. Outbrook Terrace IL.
26. Katz JD. Noise in the operating room. Anesthesiology. 2014; 121(4):894-898.
27. Carillo L, Devic A, Soulié M, et al. Assessment of the sound level in the operating room during urological surgery. Progress Urology. 2019; 29(1):45-49.
28. Fritsch MH, Chacko CE, Patterson EB. Operating room sound level hazards for patients and physicians. Otol Neurotol. 2010; 31(5):715-721.
29. Willett KM. Noise-induced hearing loss in orthopaedic staff. J Bone Joint Surg Br. 1991; 73(1);113-115.
30. Murthy VS, Malhotra SK, Bala I, et al. Detrimental effects of noise on anaesthetists. Can J Anaesth. 1995; 42(7):608-611.
31. Stevenson RA, Schlesinger JJ, Wallace MT. Effects of divided attention and operating room noise on perception of pulse oximeter pitch changes: a laboratory study. Anesthesiology. 2013; 118(2):376381.
Q1. What is your job title?
Q2. What is your age?
Q3. What is your occupation? Circle one.
Surgeon (4)
Assistant Surgeon/Fellow/Resident (5)
Scrub Technician (6)
Circulator (7)
Anesthesiologist (8)
CRNA (9)
Radiology Technician (10)
Other (11)
Q4. How long have you been working in the orthopedic OR?
Q5. Do you have any difficulties hearing in your everyday environments? If so, how long have you noted this difficulty? In what environments do you perceive this difficulty?
Q6. Are you exposed to any other loud noises in your daily life? (Music, power tools, gunfire, etc.). If so, do you wear hearing protection during these activities?
Q7. Do you have any pre-existing conditions or anything in your medical history that you think affects your hearing?
Q8. Have you had a hearing test before? If so, do you know the results of that hearing test? If not, do you think you have a hearing loss?
Q9 Have you ever worn hearing aids? Please specify for which ear(s).
Q10 Please enter your Participant Number
Q11 Please enter today's date.
Post-Surgery Questionnaire (Please complete within 24 hours after the surgery.)
Q1. What is your job title?
Q2. Please rate the following on a scale from 1-7, with 1 being "Entirely Disagree" and 7 being "Entirely Agree."
Q3. Please indicate along the spectrum how you would rate the loudest parts of the surgery.
Q4. Please indicate along the spectrum how you would rate the entirety of the surgery.
Q5. Would you be open to wearing hearing protection in the OR in the future?
Q6. What concerns would you have about hearing protection?
Q7. Please enter your participant number
Q8. Please enter today's date
Jointly provided by Medical Education Resources (MER) and the Campbell Clinic Foundation
Target Audience: This activity has been designed to meet the educational needs of orthopaedic surgeons, residents, fellows, and allied health providers involved in the care of patients with shoulder pain.
Statement of Need/Program Overview: This activity enables providers to differentiate between presentations of cervical and shoulder pathology and more effectively route patients to the appropriate treatment pathway.
Educational Objectives: After completing this activity, the participant should be better able to differentiate patients presenting with shoulder pain as either shoulder or cervical in origin.
Faculty
Andrew Nahr, MD1; Savannah Lee, MS2; Thomas W. Throckmorton, MD1; Tyler J. Brolin, MD1; Jim Y. Wan, PhD3; David L. Bernholt, MD1; Frederick M. Azar, MD1; Adam Smith, MD4
1 University of Tennessee Health Science Center – Campbell Clinic Department of Orthopaedic Surgery and Biomedical Engineering, Memphis, Tennessee
2 University of Tennessee Health Science Center, College of Medicine, Memphis, Tennessee
3 University of Tennessee Health Science Center, Department of Preventative Medicine, Memphis, Tennessee
4 West Tennessee Bone and Joint Clinic, Jackson, Tennessee

In support of improving patient care, this activity has been planned and implemented by Medical Education Resources (MER) and Campbell Clinic Foundation. MER is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team
Physician Credit: Medical Education Resources designates this enduring material for a maximum of .5__ AMA PRA Category 1 Credits™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing Credit: Medical Education Resources designates this enduring material for a maximum of_.5 ANCC nursing contact hours.
Medical Education Resources is a provider of continuing nursing education by the California Board of Registered Nursing, Provider #CEP 12299, for .5 contact hours.

Physician Assistant Credit: Medical Education Resources has been authorized by the American Academy of Physician Assistants (AAPA) to award AAPA Category 1 CME credit for activities planned in accordance with AAPA CME Criteria. This activity is designated for _.5_AAPA Category 1 CME Credits. Physician Assistants should only claim credit commensurate with the extent of their participation.
Disclosure of Relevant Financial Relationships: Medical Education Resources ensures balance, independence, objectivity, and scientific rigor in all our educational activities. In accordance with this policy, MER identifies relevant financial relationships with its instructors, content managers, and other individuals who are in a position to control the content of an activity. Reported relevant financial relationships are mitigated by MER to ensure that all scientific research referred to, reported, or used in a CE activity conforms to the generally accepted standards of experimental design, data collection, and analysis. MER is committed to providing learners with high-quality CE activities that promote improvements or quality in health care and not the business interest of an ineligible company.
The authors reported the following financial relationships with ineligible companies whose products or services may be mentioned in this activity:
Andrew Nahr, MD No relevant financial disclosures
Savannah Lee, MS No relevant financial disclosures
Thomas W. Throckmorton, MD No relevant financial disclosures
Tyler J. Brolin, MD No relevant financial disclosures
Jim Y. Wan PhD No relevant financial disclosures
David L. Bernholt, MD No relevant financial disclosures
Frederick M. Azar, MD No relevant financial disclosures
Adam Smith, MD No relevant financial disclosures
The content managers reported the following financial relationships with ineligible companies whose products or services may be mentioned in this activity:
The Campbell Clinic Foundation
No financial relationships to disclose.
Planners at Medical Education Resources
No financial relationships to disclose.
Disclaimer: The content and views presented in this educational activity are those of the authors and do not necessarily reflect those of Medical Education Resources, and the Campbell Clinic Foundation. The authors have disclosed if there is any discussion of published and/or investigational uses of agents that are not indicated by the FDA in their presentations. Before prescribing any medicine, primary references and full prescribing information should be consulted. Any procedures, medications, or other courses of diagnosis or treatment discussed or suggested in this activity should not be used by clinicians without evaluation of their patient’s conditions and possible contraindications on dangers in use, review of any applicable manufacturer’s product information, and comparison with recommendations of other authorities. The information presented in this activity is not meant to serve as a guideline for patient management.
Method of Participation: There are no fees for participating and receiving credit for this activity. During the period from April 2024 to October 2024, participants must 1) read the learning objectives and faculty disclosures, 2) study the learning objectives and faculty disclosures, and 3) complete the evaluation form. Place the following link in a browser, complete the evaluation survey, click the words "Click Here" on the last page of the evaluation survey, and download the certificate. https://merpcc.formstack.com/forms/1article2024
This link will be inactive on November 1, 2024.
MER Privacy Policy: http://cmepartner.org/privacy
Medical Education Resources and the Campbell Clinic Foundation maintain high standards for the protection of privacy over the Internet. The purpose of this statement is to explain what information we obtain, how it is used, and how visitors can restrict its use or disclosure.
The only information MER obtains is information supplied voluntarily by the visitor.
We do not sell or disclose individually identifiable information obtained online unless it is required by law or disclosure is necessary to protect the safety of customers, employees, or property.
We use the information to grade your posttest and to issue a certificate of completion of the activity. If we use a third-party company to grade your posttest and issue certificates of completion, we will give the information to that company for that purpose only.
For each activity that you take, you must complete an evaluation questionnaire. That questionnaire may ask if you are willing to participate in a follow-up survey. If you answer yes, we will use your name and contact information to send you the survey.
We may use the information to invite you to participate in other activities that we may offer.
In accordance with the ACCME Standards for Integrity and Independence in Accredited Continuing Education, MER will not share the names or contact information of learners with any ineligible company or its agents without the explicit consent of the individual learner.
Medical Education Resources is committed to safeguarding customer privacy, and we require our employees to protect the privacy of information about our customers. Should you wish to delete your information from our files or discuss our privacy policy, please contact us at https://cmepartner.org/contact/
Andrew Nahr, MD1
Savannah Lee, MS2
Thomas W. Throckmorton, MD1
Tyler J. Brolin, MD1
Jim Y. Wan, PhD3
David L. Bernholt, MD1
Frederick M. Azar, MD1
Adam Smith, MD4
1 University of Tennessee Health Science Center – Campbell Clinic Department of Orthopaedic Surgery and Biomedical Engineering, Memphis, Tennessee
2 University of Tennessee Health Science Center, College of Medicine, Memphis, Tennessee
3 University of Tennessee Health Science Center, Department of Preventative Medicine, Memphis, Tennessee
4 West Tennessee Bone and Joint Clinic, Jackson, Tennessee
Objective
The authors hypothesized that a simple questionnaire given to patients who presented with the chief complaint of shoulder pain could be administered to differentiate patients with cervical, shoulder, or mixed shoulder and cervical pathology.
Patients who presented from 2019 to 2020 were given a 22-item questionnaire prior to being evaluated for a new complaint of shoulder pain. The questionnaire items included basic demographics, primary complaint, and symptom-specific inquiries.
A total of 350 patients responded to the questionnaire: 28 (8%) patients were found to have cervical pathology, 288 (83%) patients had shoulder pathology, and 32(9%) patients had both cervical and shoulder disease. Of the 22 questions on the instrument, four yielded significant (P < 0.05) relationships with the final diagnostic category.
The results of this study suggested that the questionnaire is a reliable tool for predicting patients presenting with cervical pathology with the chief complaint of shoulder pain.
Institutional review board approval was obtained from the University of Tennessee Health Science Center (approval #2108553-NHSR).
Corresponding Author:
Thomas W. Throckmorton, MD
1211 Union Avenue, Suite 510 Memphis, Tennessee 38104
tthrockmorton@campbellclinic.com
The overlapping pain pathways between the cervical spine and shoulder continue to create diagnostic challenges, creating difficulties for these patients to obtain accurate diagnoses and gain access to effective treatments. Causation for cervical pathology manifesting as shoulder pain and vice versa is multifactorial and has been the subject of numerous previous works. To the authors’ knowledge, cervical nerve root irritation was first shown to manifest as shoulder pain in 1954 when Feinstein, et al.1 injected saline into the cervical facet joints of his subjects at different vertebral levels to evaluate their dermatomal distributions. Subjects reported pain at least partially localized to the shoulder in all cervical nerve roots distal to C3.1 Regarding shoulder pathology, a similar study was performed by Gerber et al.2 in 1998 with 25 volunteers receiving acromioclavicular (AC) joint injections with hypertonic saline to study pain referral patterns. Vol-
unteers reported experiencing pain in multiple areas, including the AC joint, anterolateral neck, trapezius, and supraspinatus.2
As orthopaedic care continues to evolve and become more specialized, patients presenting with shoulder pain ideally would be triaged by symptomatology to the appropriate spine or shoulder provider and receive the proper imaging, work-up, and treatment. Unfortunately, it is not uncommon for patients with cervical pathology to present for initial evaluation with isolated shoulder pain, which challenges that concept. In 2015, Roberson et al.3 published a series of 1169 patients presenting primarily with shoulder pain; of those patients, 4% (60) were found to have the primary diagnosis of cervical radiculitis and had excellent results with targeted therapies (injections, physical therapy [PT], anterior cervical discectomy and fusion [ACDF]).3 Inability to screen and differentiate shoulder and cervical-generated shoulder pain may lead to delays in treatment and unneeded costly studies or work-up for the patient, as well as lost productivity and inefficiency for the shoulder subspecialist. Little is known about potential tools to optimize patient routing and maximize surgeon efficiency. The authors hypothesized that a simple questionnaire given to patients presenting with the chief complaint of shoulder pain could be administered to differentiate patients presenting with cervical, shoulder, or mixed shoulder and cervical pathology.
After obtaining institutional review board approval, patients were included who presented to the practice of the senior author, a subspecialty shoulder surgeon, with a new complaint of shoulder pain from 2019 to 2020. Patients with known shoulder girdle fractures were excluded from study. A questionnaire was administered to patients prior to being evaluated and included 22 questions including basic demographics, primary complaint, and symptom-specific inquiries (Figure 1). The questionnaire also included routine questions historically believed to be beneficial in differentiating patients with cervical and shoulder pathology (e.g., shoulder blade pain, burning/numbness in arm, pain at nighttime).4-6
Patients were then evaluated by a physician after the survey, and given a diagnosis after the appropriate
history, physical examination, and imaging were obtained. Data regarding diagnosis were collected from the clinical record and placed into four categories: shoulder, cervical, shoulder and cervical, and other. Patients tended to respond to all questionnaire items; however, some patients did not respond to all questions on the instrument. If patients skipped a question, they were eliminated only from the analysis that focused on the question they skipped. The evaluating surgeon was blinded to the results of the questionnaire prior to clinical evaluation.
A power analysis was used to identify questions that were significant in differentiating between the four diagnostic categories (cervical, shoulder, cervical and shoulder, other). Statistical tests found the following questions in the instrument to be powered at 0.80 or above using chi-squared analysis: “Do you have neck
/ cervical pain?” (power = 1.00; p < 0.0001); “Do you have shoulder blade pain?” (power = 1.00; p < 0.0001); “Do you have burning, stabbing, numbness or tingling in your affected shoulder blade, hand, or arm(s)?” (power = 0.89; p = 0.0024); and “Mechanism of injury” (power = 1.00; p < 0.0001). “Does your shoulder hurt at night / wake you up from sleep?” was found to have a p value = 0.058 and was included in some analysis due to historical significance. We then developed confusion matrices for each questionnaire item, estimating sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) for three pathologies: cervical, shoulder, and cervical/shoulder. For each of the four most effective yes or no questions, we used cross-tabulation to estimate sensitivity, specificity, PPV, and NPV for these three pathologies, including standard error (SE) and confidence interval (CI) of estimates. For all possible combinations of these four responses, we also used cross-tabulation to estimate sensitivity, specificity, PPV, and NPV for the three pathologies, including standard error and confidence interval of estimates. Analyses were performed using R v4.2.0 and SAS v9.4; a significant alpha of 0.05 was applied throughout.
A total of 350 patients responded to the questionnaire. Twenty-eight (8%) patients were found to have cervical pathology, 288 (83%) patients had shoulder pathology, and 32(9%) patients had both cervical and shoulder disease (Table 1).
Of the 22 questions on the instrument, a total of four questions yielded significant (p < 0.05) relationships with the final diagnostic category. Two questions relat-
Table 1: Frequency distribution of diagnosis category.
ed to location of pain, one to characterization of pain, and one to mechanism of injury. The significant questions were: (1) “Do you have neck / cervical pain?”, (2) "Do you have shoulder blade pain?”, (3) “Do you have burning, stabbing, numbness or tingling in your affected shoulder blade, hand, or arm(s)?”, and (4) “Mechanism of the injury." The question “Does your shoulder hurt at night / wake you up from sleep?” narrowly missed the significance cut-off (p = 0.058); however, it was included in the confusion matrix analysis due to the classical association of night-time shoulder pain and shoulder pathology.
When patients were asked if they had neck or cervical pain, the patients who responded “yes” (25 of 28 patients with cervical pathology) were significantly (p < 0.05) more likely to have a diagnosis category of cervical or mixed shoulder/cervical pathology. The patients who responded “no” were significantly more likely to have a diagnosis category of shoulder-generated pain. The same result can be seen for the question “Do you have shoulder blade pain?” with a significant correlation between a “yes” answer and the final diagnosis of cervical pathology. One survey item asked if the patient was experiencing “burning, stabbing, numbness or tingling in their affected shoulder blade, hand, or arm(s).” The question then included follow-up responses related to the frequency of the pain. Patients who responded “yes” to the initial question were significantly more likely to have a diagnosis category of cervical or shoulder/cervical (p < 0.05).
In regard to the question “Does your shoulder hurt at night?”, a total of 344 responses were recorded. Twenty-four out of 27 total patients with a cervical diagnosis answered positively to this question, along with 28 out of the 32 mixed pathologies, and 299 out of the 344 patients in the pure shoulder diagnosis category. Utilizing chi-squared analysis this fell just under the cutoff for significance (p = 0.058) in diagnostic utility.
For analysis of clinical utility, the sensitivity, specifi city, positive predictive value (PPV), and negative predictive value (NPV) for each question was analyzed regarding a cervical, shoulder, and mixed diagnosis. Questions were then combined into confusion matrices to analyze diagnostic value when combined. See Tables 2 and 3 for a complete breakdown of results.
Table 2: Diagnostic results of statistically significant questions individually
Table 3: Confusion matrix results for specificity and sensitivity given various combinations of answers (responses per diagnosis).
Q, question *Responses to these questions in order
1. Do you have neck/cervical pain?
2. Do you have shoulder/shoulder blade pain?
3. Do you have burning/stabbing pain in your shoulder or arm?
4. Does your shoulder hurt at night/wake you up from sleep?
Finally, mechanism of injury was also evaluated as part of the survey instrument. For simplicity, patients who responded with multiple mechanisms of injury were restricted to only one mechanism. For this reason, the total of 281 responses was restricted to those of only 266 patients, and patients were restricted to only one mechanism of injury response. A chi-square analysis was then conducted with mechanism of injury as one variable and diagnostic category as the other variable. Results indicated significant relationships between mechanism of injury and diagnostic category [X2(10,266) = 18.752, p = 0.044]. Participants who identified a fall as their mechanism of injury were more likely to have a diagnostic category of shoulder. Those patients who identified a mechanism of injury as exercise were more likely to have a diagnostic category of shoulder. However, patients who reported no injury were less likely to have a diagnostic category of shoulder.
Orthopaedic complaints are some of the most common reasons for patients to seek medical treatment.7 Epidemiologic studies analyzing the prevalence of musculoskeletal disease quote the spine being the most common area of symptoms followed by the knee, and then shoulder.8,9 With increasing lifespans and improved access to care among all groups, the number of patients seeking specialized orthopaedic care is set to increase. The benefit of being able to screen and allocate patients presenting with shoulder pain to the appropriate provider will allow efficient clinics to avoid unnecessary testing, delays in patient care, and inappropriate utilization of provider resources.9
Traditionally, surgeons have relied upon careful history taking and physical examination skills to differentiate shoulder and cervical pathologies, which has been well described in past work.4-6 Briefly, the characteristic pain of shoulder pathology is classically stated to be “dull or sharp” versus the burning, lightning like pain seen in cervical disease.5 Pain that is worsened with use of the affected shoulder, or pain that interferes with sleep is thought to be an indicator of a shoulder origin.6 Another useful clue is the location of pain: pain radiating from the neck to medial scapula, or pain extending past the elbow is indicative of cervical pathology, while shoulder-oriented pain tends to be localized
to the lateral deltoid and upper arm.6 Examination maneuvers such as the shoulder abduction sign can be useful as cervical pain tends to improve with abduction of the shoulder as nerve root tension decreases, while shoulder pathology tends to worsen.5,10 Finally, specific tests for nerve root impingement such as Lhermitte’s or Spuring’s test can be used to help elucidate origin.5 Regarding patient history, atraumatic, insidious, onset of symptoms tends to point to a cervical origin in contrast to rotator cuff pathology, in which an inciting event is common (only 14.8% of cervical radiculopathy is associated with trauma).11
It is not surprising that cervical disease can be mistaken for shoulder pathology. In one of the largest epidemiologic studies on cervical radiculopathy in Rochester, MN out of 561 patients with isolated cervical pathology, all but 14 (97.5%) patients presented with pain in the neck and shoulder.11 This poses a huge diagnostic dilemma to support staff, nurses, providers, and physicians who are tasked to differentiate between shoulder pain and cervical-generated shoulder girdle pain in an accurate and timely manner. Historically, when looking at patients with the primary complaint of shoulder pain, around 4% will have isolated cervical pathology.3 In our cohort, we found this number to be even higher with 9% (35 out of 383) of patients presenting with shoulder pain being diagnosed with isolated cervical disease. Unfortunately, it is all too common for a patient to see an inappropriate subspecialist and receive unnecessary imaging before the correct diagnosis has been made. Our questionnaire given at the time of presentation to patients presenting with the primary complaint of shoulder pain had encouraging results in being able to differentiate patients presenting with primary shoulder and cervical disease. We believe this has the potential to be invaluable in the future in regard to streamlining patients to the correct specialist, increasing practice efficiency, and improving the quality of patient care.
Three yes-or-no style questions were found to be adequately powered in relation to making a diagnosis of cervical pathology utilized both individually and in combination: (1) “Do you have neck/cervical pain?”, (2) “Do you have shoulder blade pain?”, (3) “Do you have burning, stabbing, numbness, or tingling in your affected shoulder blade, hand, or arm(s)?” Sensitivity in the study population for each of the questions alone
was high at 0.91, 0.83, and 0.89, respectively. In combination, we see the clinical characteristics change and function with much higher specificity (0.92). The data trends indicate each additional question with a “yes” response increases the specificity (Figure 2). Unlike a screening test for cervical etiologies capturing all patients with cervical pathology and some without (high sensitivity), this combination of questions functions more to identify those with true cervical disease (high specificity). This allows us to identify a separate subset of patients with obvious, true cervical pathology from all patients presenting with shoulder/upper-extremity pain and direct them to the appropriate provider. Unlike a screening test, however, there will undoubtably be some patients who fall somewhere in between diagnoses with an indeterminate diagnosis based on questionnaire responses who require a trained physician to appropriately elucidate the true cause of the symptomatology.
For the sake of analysis, although significant in differentiating cervical from shoulder-based pain, mechanism of injury was not included in more advanced calculation. In this patient population, in agreement with past work, patients with no mechanism were more likely to be diagnosed with cervical pathology vs shoulder.12,13 Further studies with standardized mechanism of injury evaluations, acute vs chronic, may prove useful to improve the accuracy of the questionnaire.
Traditionally, nighttime shoulder pain has been strongly associated with rotator cuff symptomatology.6 One of the goals during statistical analysis of this study was to examine if nighttime pain does indeed prove useful and unique in its association with shoulder pathology. Somewhat surprisingly, the question “Does your shoulder hurt at night” in these responses seemed to be relatively high in sensitivity for cervical pathology (sensitivity = 0.87), with 24 of the 27 patients who presented with pure cervical pathology admitting to night-time pain, while being relatively low in sensitivity (sensitivity = 0.11) for pure shoulder pathology. This correlation reverses when specificity is calculated (0.13 and 0.87, respectively). However, as a screening test for shoulder pathology, night-time pain in this series was less reliable. While undoubtably an aspect of the patient’s history that should be investigated, this data would suggest that night-time pain as a screening mechanism for shoulder pathology may need to be reconsidered.
Figure 2: Cervical Specificity by responses to questions 1 through 4 by no (n) or yes (y) answers showing increased specificity with positive responses. Questions: 1) Do you have neck/cervical pain? 2) Do you have shoulder/ shoulder blade pain? 3) Do you have burning/stabbing pain in your shoulder or arm? 4) Does your shoulder hurt at night / wake you up from sleep?
This study has limitations. First, patients presenting to subspecialty shoulder or sports surgeons with shoulder pain may have experienced some contact with other providers previously and therefore may have been triaged before the questionnaire was administered. Future work in this area with patients presenting in other clinical settings may prove useful. Also, while our cohort of 350 patients did prove to be statistically significant, a larger cohort may work to further characterize testing characteristics (sensitivity, specificity, etc.). Finally, this questionnaire evaluated only a single fellowship trained shoulder surgeon’s practice and may benefit from larger scale, multi-institutional validation.
The results of this study suggested that the questionnaire is a reliable tool for predicting patients presenting with cervical pathology with the chief complaint of shoulder pain. The questionnaire demonstrated high levels of specificity in predicting cervical pathology, with an overall rate of 0.91 when combining the
three questions: (1) ‘Do you have neck/cervical pain?”, (2) “Do you have shoulder blade pain?”, (3) “Do you have burning, stabbing, numbness or tingling in your affected shoulder blade, hand, or arm(s)?”. These findings have important clinical implications, as early and accurate diagnosis of cervical and shoulder pathology can lead to more effective treatment and better outcomes for patients. The questionnaire may serve clinicians in primary care settings to help differentiate between patients with shoulder pain and pain referred
1. Feinstein B, Langton JN, Jameson RM, Schiller F. Experiments on pain referred from deep somatic tissues. J Bone Joint Surg Am. 1954;36A(5):981-997.
2. Gerber C, Galantay RV, Hersche O. The pattern of pain produced by irritation of the acromioclavicular joint and the subacromial space. J Shoulder Elbow Surg. 1998;7(4):352-355.
3. Roberson TA, Nicholas B, Azar F, et al. Cervical radiculitis presenting as shoulder pain: frequency and results of multidisciplinary care. Curr Orthop Pract. 2015;26(5):521-525.
4. Katsuura Y, Bruce J, Taylor S, Gullota L, Kim HJ. Overlapping, masquerading, and causative cervical spine and shoulder pathology: a systematic review. Global Spine J. 2020;10(2):195-208.
5. Bokshan SL, DePasse JM, Eltorai AE, et al. An evidence-based approach to differentiating the cause of shoulder and cervical spine pain. Am J Med. 2016;129(9):913-918.
6. Throckmorton TQ, Kraemer P, Kuhn JE, Sasso RC. Differentiating cervical spine and shoulder pathology: common disorders and key points of evaluation and treatment. Instr Course Lect. 2014;63:401408.
7. Margham T. Musculoskeletal disorders: time for joint action in primary care. Br J Gen Pract. 2011;61(592):657-8.
from the cervical spine to the shoulder girdle. It may also be used by shoulder subspecialty providers prior to patient evaluation as a screening tool to steer patients to the correct subspecialty provider. Future research should be conducted to validate the questionnaire in a larger, more diverse patient population. Overall, the questionnaire has the potential to be a valuable tool for the diagnosis and management of patients with cervical and shoulder pathology.
8. Mansfield M, Smith T, Spahr N, Thacker M. Cervical spine radiculopathy epidemiology: A systematic review. Musculoskeletal Care. 2020;18(4):555-567.
9. Urwin M, Symmons D, Allison T, et al. Estimating the burden of musculoskeletal disorders in the community: the comparative prevalence of symptoms at different anatomical sites, and the relation to social deprivation. Ann Rheum Dis. 1998;57(11):649-55.
10. Fast A, Parikh S, Marin EL. The shoulder abduction relief sign in cervical radiculopathy. Arch Phys Med Rehabil. 1989;70(5):402-3.
11. Radhakrishnan K, Litchy WJ, O'Fallon WM, Kurland LT. Epidemiology of cervical radiculopathy. A population-based study from Rochester, Minnesota, 1976 through 1990. Brain. 1994;117 (Pt 2):325-335.
12. Varacallo M, El Bitar Y, Mair SD. Comprehensive shoulder evaluation strategies. [Updated September 4, 2022]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538309/ Accessed March 6, 2023
13. Caridi JM, Pumberger M, Hughes AP. Cervical radiculopathy: a review. HSS J. 2011; 7(3):265-72.
Jointly provided by Medical Education Resources (MER) and the Campbell Clinic Foundation
Target Audience: This activity has been designed to meet the educational needs of orthopaedic surgeons, residents, fellows, and allied health providers involved in the care of patients who undergo perioperative nerve blocks with dexmedetomidine.
Statement of Need/Program Overview: This activity enables providers to identify patients with complications and have informed discussions with patients regarding peripheral nerve blocks with dexmedetomidine and understand the risk of chronic neuropathic symptoms.
Educational Objectives: After completing this activity, the participant should be better able to have an informed discussion regarding peripheral nerve block with dexmedetomidine with their patients and understand the risk of chronic neuropathic symptoms.
Nolan Farrell, MD1; Derek Dixon, BS2; Brent Scheckel, MD1; Thomas W. Throckmorton, MD1; Tyler J. Brolin, MD1
1 University of Tennessee Health Science Center – Campbell Clinic Department of Orthopaedic Surgery and Biomedical Engineering, Memphis, TN
2 Campbell Clinic Foundation, Germantown, TN

Accreditation Statement
In support of improving patient care, this activity has been planned and implemented by Medical Education Resources (MER) and Campbell Clinic Foundation. MER is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC) to provide continuing education for the healthcare team
Physician Credit: Medical Education Resources designates this enduring material for a maximum of .5 AMA PRA Category 1 Credits™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing Credit: Medical Education Resources designates this enduring material for a maximum of .5 ANCC nursing contact hours.
Medical Education Resources is a provider of continuing nursing education by the California Board of Registered Nursing, Provider #CEP 12299, for .5 contact hours.

Physician Assistant Credit: Medical Education Resources has been authorized by the American Academy of Physician Assistants (AAPA) to award AAPA Category 1 CME credit for activities planned in accordance with AAPA CME Criteria. This activity is designated for .5 AAPA Category 1 CME Credits. Physician Assistants should only claim credit commensurate with the extent of their participation.
Disclosure of Relevant Financial Relationships: Medical Education Resources ensures balance, independence, objectivity, and scientific rigor in all our educational activities. In accordance with this policy, MER identifies relevant financial relationships with its instructors, content managers, and other individuals who are in a position to control the content of an activity. Reported relevant financial relationships are mitigated by MER to ensure that all scientific research referred to, reported, or used in a CE activity conforms to the generally accepted standards of experimental design, data collection, and analysis. MER is committed to providing learners with high-quality CE activities that promote improvements or quality in health care and not the business interest of an ineligible company.
The authors reported the following financial relationships with ineligible companies whose products or services may be mentioned in this activity:
Nolan Farrell, MD No relevant financial disclosures
Derek Dixon, MD No relevant financial disclosures
Brent Scheckel, MD No relevant financial disclosures
Thomas W. Throckmorton, MD No relevant financial disclosures
Tyler J. Brolin, MD No relevant financial disclosures
The content managers reported the following financial relationships with ineligible companies whose products or services may be mentioned in this activity:
The Campbell Clinic Foundation
No financial relationships to disclose.
Planners at Medical Education Resources
No financial relationships to disclose.
Disclaimer: The content and views presented in this educational activity are those of the authors and do not necessarily reflect those of Medical Education Resources, and the Campbell Clinic Foundation. The authors have disclosed if there is any discussion of published and/or investigational uses of agents that are not indicated by the FDA in their presentations. Before prescribing any medicine, primary references and full prescribing information should be consulted. Any procedures, medications, or other courses of diagnosis or treatment discussed or suggested in this activity should not be used by clinicians without evaluation of their patient’s conditions and possible contraindications on dangers in use, review of any applicable manufacturer’s product information, and comparison with recommendations of other authorities. The information presented in this activity is not meant to serve as a guideline for patient management.
Method of Participation: There are no fees for participating and receiving credit for this activity. During the period from April 2024 to October 2024, participants must 1) read the learning objectives and faculty disclosures, 2) study the learning objectives and faculty disclosures, and 3) complete the evaluation form. Place the following link in a browser, complete the evaluation survey, click the words "Click Here" on the last page of the evaluation survey, and download the certificate. https://merpcc.formstack.com/forms/2article2024
This link will be inactive on November 1, 2024.
MER Privacy Policy: http://cmepartner.org/privacy
Medical Education Resources and the Campbell Clinic Foundation maintain high standards for the protection of privacy over the Internet. The purpose of this statement is to explain what information we obtain, how it is used, and how visitors can restrict its use or disclosure.
The only information MER obtains is information supplied voluntarily by the visitor.
We do not sell or disclose individually identifiable information obtained online unless it is required by law or disclosure is necessary to protect the safety of customers, employees, or property.
We use the information to grade your posttest and to issue a certificate of completion of the activity. If we use a third-party company to grade your posttest and issue certificates of completion, we will give the information to that company for that purpose only.
For each activity that you take, you must complete an evaluation questionnaire. That questionnaire may ask if you are willing to participate in a follow-up survey. If you answer yes, we will use your name and contact information to send you the survey. We may use the information to invite you to participate in other activities that we may offer.
In accordance with the ACCME Standards for Integrity and Independence in Accredited Continuing Education, MER will not share the names or contact information of learners with any ineligible company or its agents without the explicit consent of the individual learner.
Medical Education Resources is committed to safeguarding customer privacy, and we require our employees to protect the privacy of information about our customers. Should you wish to delete your information from our files or discuss our privacy policy, please contact us at https://cmepartner.org/contact/
Nolan Farrell, MD1
Derek Dixon, BS2
Brent Scheckel, MD1
Thomas W. Throckmorton, MD1
Tyler J. Brolin, MD1
1 University of Tennessee Health Science Center – Campbell Clinic Department of Orthopaedic Surgery and Biomedical Engineering, Memphis, TN
2 Campbell Clinic Foundation, Germantown, TN
Perioperative pain management is an important factor in the management of the orthopaedic patient. Recently, dexmedetomidine (DEX) has been added to perioperative nerve blocks (PNB) to prolong anesthetic effect and pain control. When juxtaposed against data showing PNB are associated with an approximate 1% risk of long-term neurological complaints, we aimed to define the incidence of neurologic sequelae after perineural DEX.
A retrospective study of 460 patients who underwent PNB during 1 year at one institution’s ambulatory surgery centers included patients 15 to 70 years of age, 64.6% of whom were male. PNBs were completed by staff anesthesiologists using ultrasound guidance. Patients with persistent neurologic sequelae had subjective or physical examination findings of persistent numbness, tingling, neuropathic pain, dysesthesia, paresthesia, or muscular weakness lasting greater than 72 hours that was not explained by the surgical procedure. Frequency distribution, variability, and central tendency of incidence of neurologic complications were measured.
Institutional review board approval was obtained from the University of Tennessee Health Science Center (approval #22-08644-XP).
We identified 21 patients with persistent neurologic sequelae at the 2-week follow-up or later, demonstrating greater than 72 hours of symptoms after the PNB was given. The most common finding was persistent numbness in 16 patients. The leading comorbidities in patients with neurological complications were hypertension (39.1%), diabetes (13.0%), and history of deep vein thrombosis (DVT) (4.3%). Of the 21 patients with persistent neurologic sequelae, 18 had resolution of their symptoms at an average duration of 106 (+/- 77) days postoperatively. The total complication rate of long-term persistent neurological symptoms after PNB with DEX was 4.5%.
Corresponding Author:
Tyler J. Brolin, MD
1211 Union Avenue, Suite 510 Memphis, Tennessee 38104
tbrolin@campbellclinic.com
This study showed persistent symptoms in a larger percentage of patients than previously described in the literature. A prospective study evaluating neurological complications due to PNB with DEX would provide a better scope of knowledge for continued use for perioperative pain control.
Perioperative pain management remains an important factor in the management of the orthopaedic patient. Adequate postoperative pain control has consistently proven to yield better outcomes functionally, increase participation in physical therapy, and decrease hospital utilization.1-3 Modern pain-control measures for outpatient orthopaedic surgery includes multimodal therapy with preoperative oral medications, regional anesthesia, and postoperative protocols to minimize opioid usage and maximize pain control.3 Recently, dexmedetomidine (DEX) has been added to perioperative nerve blocks in an attempt to prolong anesthetic effect and pain control.4-7 DEX is a selective alpha-2 receptor agonist, primarily inhibiting the release of nociceptive transmitters, such as glutamate and substance P.8 By inhibiting nociceptive release, DEX has shown to increase the duration of regional anesthesia, improve recovery from general anesthesia, and decrease the use of postoperative opioids.4
Side effects of DEX include hypotension, bradycardia, atrial fibrillation, and hypoxia.9 While these are rare side effects and occur at higher systemic doses, DEX has not been found to have prolonged neuropathic symptoms. A meta-analysis of randomized controlled trials (RCT) of DEX reported no findings of neurologic sequelae in 1,026 patients.6 RCTs utilizing DEX in regional blocks for orthopaedic surgery have shown no neurologic sequelae and full recovery of patients.10,11 When juxtaposed against data showing peripheral nerve blocks (PNB) are associated with an approximate 1% risk of long-term
neurological complaints,12 we suspected some rate of neurologic sequelae after perineural DEX when compared with standard PNB. Thus, we aimed to define the incidence of prolonged neurologic sequelae after administration of perineural DEX in the setting of PNB for perioperative pain control.
After institutional review board approval, all patients who underwent peripheral nerve block during 1 year at one institution’s ambulatory surgery centers were reviewed retrospectively. Patients without a dictated follow-up note at 2 weeks or greater and those with blocks not performed with DEX were excluded. PNBs were completed by staff anesthesiologists using ultrasound guidance. DEX-ropivacaine PNB dosages were determined by the staff anesthesiologist. During the study period, we identified patients who received a block that included DEX and had persistent neurologic sequelae as those with dictated subjective or physical examination findings of persistent numbness, tingling, neuropathic pain, dysesthesia, paresthesia, or muscular weakness lasting greater than 72 hours that was not explained by the surgical procedure. Chart review included patient demographics, surgical procedure, location of PNB, duration of neurologic complication, treatment for complication, dosage of DEX, and if there was unknown, complete, incomplete, or no resolution of symptoms. American Society of Anesthesiologists (ASA) score was not consistently recorded, thus was not included. Descriptive statistics were performed to determine incidence of neurologic complications as a percentage. Frequency distribution, variability, and central tendency of incidence of neurologic complications were measured. Comparative statistics were not performed.
During the 12-month study period, 460 patients underwent PNB with DEX. (Table 1) The cohort included patients 15 to 70 years old, 64.6% of whom were male (Table 2). We identified 21 patients with persistent neurologic sequelae at the 2-week follow-up or later who demonstrated greater than 72 hours of symptoms after the PNB was given. The most common finding was persistent numbness in 16 patients. Persistent tingling was found in eight patients and
Mean Age
Asian:
Hispanic:
Other:
Mean
Gender Male:
persistent weakness was found in five patients. The most common comorbidities in patients with neurological complications were hypertension (39.1%), diabetes (13.0%), and history of deep vein thrombosis (DVT) (4.3%). Of the 21 patients with persistent neurologic sequelae, 18 had resolution of their symptoms at an average duration of 106 (+/- 77) days postoperatively. The total complication rate of long-term persistent neurological symptoms after PNB with DEX was 4.5%. (Table 3)
well documented. Peripheral nerve injury, described as persistent neurologic sequelae, after regional anesthesia for upper-extremity surgery is between 0.5% to 1.3% in a systematic review of 50 studies.17
Experiencing neurologic complications from a PNB is rare, which is why it is difficult to find quality data on the long-term complications postoperatively. Most studies have focused on short-term complications, which are mostly non-neurological complications including hypotension, nausea, and vomiting.7-9 Fritsch et al.11 in a prospective study of 59 patients who underwent PNB with and without DEX found no statistical difference in persistent neurologic sequelae in the two groups after 28 days of follow-up. This study was likely underpowered given the low incidence of neurologic sequelae after PNB to detect a significant difference. We found persistent symptoms lasted an average of 106 days postoperatively. Our study showed persistent symptoms in a larger percentage of patients than previously described in the literature. While we cannot make direct comparisons, this shows the need for further study of the inclusion of DEX in PNB. Of the 21 patients with persistent symptoms, 10 required additional testing or follow-up with other providers for evaluation and treatment of their persistent symptoms, in addition to the standard therapy and medications postoperatively. This resulted in an added cost to the patient and healthcare system.
This study demonstrated a rate of persistent neurologic sequelae in a large cohort of 4.5% after PNB with DEX. Orthopaedic surgeons are focused on maximizing pain control after surgery while limiting perioperative narcotic use. DEX, when included in regional or local anesthesia, has shown to decrease opioid usage, decrease onset time of block, and prolong block duration.13-16 However, the surgeon must balance postoperative pain control with adverse events from PNBs. Although the reported short-term complications of DEX are well described in the literature,4 the longterm neurologic complications of DEX in PNB are not
Postoperative pain control is an important factor in the recovery after orthopaedic surgery and current multimodal pain regiments lead to adequate pain control with improved outcomes.2,3,18 Currently, multimodal pain-control regiments exist, including opioid-sparing protocols that do not include PNB as part of their protocol, with equivalent results.18-20 The availability and effectiveness of these multimodal regimens, when weighed with the potentially long-term complications from DEX, show the need for further evaluation of DEX when used in conjunction with PNB. Persistent neurologic symptoms have the potential to slow recovery for the patient as well as have a negative effect on patient satisfaction for an otherwise-uneventful operation. Surgeons must weigh the balance of pain control in the postoperative period since evidence has supported both pericapsular or periarticular injections and standard PNB without use of DEX, with the potential avoidance of rebound pain in those who receive pericapsular injections.21
This study was limited by its retrospective nature. Because neurologic sequelae after PNB occur rarely, it is difficult to compare this study population with those who did not have neurologic sequelae. This study relies on the surgeon documenting the ongoing neurologic complaints, and its likely etiology, which may lead to underreporting or overreporting of the incidences as some neurologic symptoms could be procedurally related. There was inherent bias by the surgeons reporting the symptoms because neuropathic sequelae cannot be definitively determined to be as a direct result of the PNB; only a high likelihood can be assumed. The benefit of the study’s retrospective
1. Morrison SR, Magaziner J, McLaughlin MA, et al. The impact of post-operative pain on outcomes following hip fracture. Pain. 2003;103(3):303-311.
2. Lavernia C, Cardona D, Rossi MD, Lee D. Multimodal pain management and arthrofibrosis. J Arthroplasty. 2008;23 (6 Suppl 1):74-9.
3. Chunduri A, Aggarwal AK. Multimodal pain management in orthopedics. J Clin Med. 2022;11(21):6386.
4. Dai W, Tang M, He K. The effect and safety of dexmedetomidine added to ropivacaine in brachial plexus block: A meta-analysis of randomized controlled trials. Medicine (Baltimore). 2018;97(41):e12573.
5. Tang R, Liu YQ, Zhong HL, et al. Evidence basis for using dexmedetomidine to enhance the quality of paravertebral block: A systematic review and meta-analysis of randomized controlled trials. Front Pharmacol. 2022;13:952441.
6. Vorobeichik L, Brull R, Abdallah FW. Evidence basis for using perineural dexmedetomidine to enhance the quality of brachial plexus nerve blocks: a systematic review and meta-analysis of randomized controlled trials. Br J Anaesth. 2017;118(2):167-181.
7. Abdallah FW, Dwyer T, Chan VW, et al. IV and perineural dexmedetomidine similarly prolong the duration of analgesia after interscalene brachial plexus block: a randomized, three-arm, triplemasked, placebo-controlled trial. Anesthesiology. 2016;124(3):683-95.
8. Bajwa S, Kulshrestha A. Dexmedetomidine: an adjuvant making large inroads into clinical practice. Ann Med Health Sci Res. 2013;3(4):475-83.
9. Gertler R, Brown HC, Mitchell DH, Silvius EN. Dexmedetomidine: a novel sedative-analgesic agent. Proc (Bayl Univ Med Cent). 2001;14(1):13-21.
10. Ammar AS, Mahmoud KM. Ultrasound-guided single injection infraclavicular brachial plexus block using bupivacaine alone or combined with dexmedetomidine for pain control in upper limb surgery: A prospective randomized controlled trial. Saudi J Anaesth. 2012;6(2):109-14.
11. Fritsch G, Danninger T, Allerberger K, et al. Dexmedetomidine added to ropivacaine extends the duration of interscalene brachial plexus blocks for elective shoulder surgery when compared with ropivacaine alone: a single-center, prospective, triple-blind, randomized controlled trial. Reg Anesth Pain Med. 2014;39(1):37-47.
12. Watts SA, Sharma DJ. Long-term neurological complications associated with surgery and peripheral nerve blockade: outcomes after 1065 consecutive blocks. Anaesth Intensive Care. 2007;35(1):24-31.
nature is that it relied on dictated symptoms and the sequelae were significant enough to be documented. This study also avoided recall bias among patients.
Although the results of this study differed from the literature, with a complication rate of 4.5% versus the 0.5% to 1% historical control, the long-term complications of DEX should be studied. A prospective study evaluating neurological complications due to PNB with DEX would provide a better scope of knowledge for continued use for perioperative pain control.
13. Keniya VM, Ladi S, Naphade R. Dexmedetomidine attenuates sympathoadrenal response to tracheal intubation and reduces perioperative anaesthetic requirement. Indian J Anaesth. 2011;55(4):352-7.
14. Packiasabapathy SK, Kashyap L, Arora MK, et al. Effect of dexmedetomidine as an adjuvant to bupivacaine in femoral nerve block for perioperative analgesia in patients undergoing total knee replacement arthroplasty: A dose-response study. Saudi J Anaesth. 2017;11(3):293-298.
15. Kassim DY, Mahmoud HE, Fakhry DM, Mansour MA. Comparative study of dexmedetomidine versus fentanyl as adjuvants to bupivacaine in ultrasound-guided transversus abdominis plane block in patients undergoing radical cystectomy: a prospective randomised study. BMC Anesthesiol. 2022;22(1):340.
16. Donatiello V, Alfieri A, Napolitano A, et al. Opioid sparing effect of intravenous dexmedetomidine in orthopaedic surgery: a retrospective analysis. J Anesth Analg Crit Care. 2022;2(1):49.
17. Silverstein ML, Tevlin R, Higgins KE, Pedreira R, Curtin C. Peripheral nerve injury after upper-extremity surgery performed under regional anesthesia: a systematic review. J Hand Surg Glob Online. 2022;4(4):201-207.
18. Jones CA, Throckmorton TW, Murphy J, et al. Opioid-sparing pain management protocol after shoulder arthroplasty results in less opioid consumption and higher satisfaction: a prospective, randomized controlled trial. J Shoulder Elbow Surg. 2022;31(10):2057-2065.
19. Pires Sousa I, Leite da Silva Peixoto CI, Fernandes Coimbra LA, da Costa Rodrigues FM. Comparison of pericapsular nerve group (PENG) block and epidural analgesia following total hip arthroplasty: A retrospective analysis. Rev Esp Anestesiol Reanim (Engl Ed). 2022;69(10):632-639.
20. Jimenez-Almonte JH, Wyles CC, Wyles SP, et al. Is local infiltration analgesia superior to peripheral nerve blockade for pain management after THA: a network meta-analysis. Clin Orthop Relat Res. 2016;474(2):495-516.
21. Dada O, Gonzalez Zacarias A, Ongaigui C, et al. Does rebound pain after peripheral nerve block for orthopedic surgery impact postoperative analgesia and opioid consumption? A narrative review. Int J Environ Res Public Health. 2019;16(18):3257.
Calkins CE, Wing C, Diltz Z, Toy PC, Mihalko WM. Changes in Neuraxial Anesthesia Protocols Lead to Improved Efficiency of Same Day Discharge Total Knee Arthroplasty in an Ambulatory Surgery Center: A Retrospective Cohort Study. JAAOS. 2023 Mar 1;31(5):e256-e263. doi: 10.5435/JAAOS-D-22-00754. PMID: 36821081
Calkins TE, Ford MC, Mihalko WM. Spinal versus General Anesthesia for Outpatient Total Hip and Knee Arthroplasty in the Ambulatory Surgery Center: A Matched-Cohort Study. J Arthroplasty. 2023 Dec 14:S0883-5403(23)01212-3. doi: 10.1016/j.arth.2023.12.020. Online ahead of print. PMID: 38103803
Calkins TE, Goetz DD, Zalewski JT, Jones CA, Gaumer PR, Ford MC, Toy PC, Crockarell JR, Harkess JW, Mihalko WM, Guyton JL. Hip Arthroplasty Femoral Stem Designs and Their Association With Early Postoperative Periprosthetic Femoral Fractures. J Arthroplasty. 2023 May;38(5):849-854. doi: 10.1016/j. arth.2022.12.020. Epub 2022 Dec 16. PMID: 36535442
Calkins TW, Jove M, Jove N, Mihalko WM. United States Experience with a Femoral Neck Retaining Total Hip Arthroplasty Stem: Retrospective Study with Control Comparison from the Literature. J Arthroplasty. 2023 Aug 26:S0883-5403(23)00883-5. doi: 10.1016/j.arth.2023.08.074. Online ahead of print. PMID: 37640246
Eason T, Mihalko WM, Toy PC. Robotic-Assisted Total Knee Arthroplasty is Safe in the Ambulatory Surgery Center Setting. Orthop Clin North Am . 2023 Apr;54(2):153-159. doi: 10.1016/j. ocl.2022.11.001. PMID: 36894288
Jennewine B, Mihalko WM. Body Habitus Impact on Success of Cryoneurolysis for Postoperative Total Knee Arthroplasty Pain Control: A Retrospective Study. Arthroplasty Today. 2023 Jul 24;22:101164. doi: 10.1016/j.artd.2023.101164. eCollection 2023 Aug. PMID: 37521741
Mihalko WM, Johnson KC, Neiberg RH, Bahnson JL, Singhal K, Richey PA; Look AHEAD Research Group. The Association of Total Knee Arthroplasty With Weight Loss in the Look AHEAD (Action for Health in Diabetes) Clinical Trial. J Arthroplasty. 2023 Jun;38(6S):S81-S87.e2. doi: 10.1016/j.arth.2023.03.023. Epub
2023 Mar 16. PMID: 36933679
Nelson A, Fong H, Carnall AM, Puppa MJ, Beeler D, Stickley C, Mihalko WM, Powell D. Increasing Trunk Mass Evokes Lower Extremity Biomechanical Plasticity during Stair Descent. Int J Exerc Sci. 2023 Aug 1;16(1):942-953. eCollection 2023. PMID; 37649868
Russell TA, Klima ML. History and Evolution of Hip Design to Decrease Failure. J Orthop Trauma. 2023 Oct 1;37(10S):S49-S54. doi: 10.1097/BOT.0000000000002668. PMID: 37710375
Alexander NB, Sarfani S, Strickland CD, Richardson DR, Murphy GA, Grear BJ, Bettin CC. Cost Analysis and Reimbursement of Weightbearing Computed Tomography. 2023 Mar 27;8(1):24730114231164143. doi: 10.1177/24730114231164143. eCollection 2023 Jan. PMID: 37009418
Doty J, Murphy GA, Friscia DA, Bohay D, Strasser N, Newton W, Gross C. Two Year Survivorship and Patient Reported Outcomes of Prospectively-Enrolled Cohort of INFINITY Total Ankle Arthroplasties. Foot Ankle Int. 2023 Dec 22:10711007231212484. doi: 10.1177/10711007231212484. Online ahead of print. PMID: 38140701
Harrison HR, Murphy GA, Bettin CC, Richardson DR, Grear BJ. The Chevron Bunionectomy for Moderate to Severe Hallux Valgus Deformity: Effects of Procedural Factors on Hallux Valgus Correction. Foot Ankle Surg. 2023 Jun;29(4):373-379. doi: 10.1016/j.fas.2023.03.002. Epub 2023 Mar 17. PMID: 37024363
Smith CJ, Skinner WC, Bettin CC. Tibiotalocalcaneal Arthrodesis Using Hybrid Plate-Nail Constructs: A Novel Technique for Treatment of Unstable Ankle and Hindfoot Deformities. J Orthop Trauma. 2023 Aug 1;37(8S):S11-S12. doi: 10.1097/BOT.0000000000002636. PMID: 37443438
Wishman MD, Henry J, Rider CM, Sofka C, Yoon E, Elliott A. Osteoid Osteomas of the Talus: A Case Report of Four Patients. Cureus. 2023 Jun 22;15(6):e40798. doi: 10.7759/cureus.40798. eCollection 2023 Jun. PMID: 37485164
Gailey AD, Ostrum RF. The Use of Liposomal Bupivacaine in Fracture Surgery: A Review. J Orthop Surg Res . 2023 Apr 1;18(1):267. doi: 10.1186/s13018-023-03583-1. PMID: 37005638
Azar FM. Managing Comorbidities. Orthop Clin North Am. 2023 Jul;54(3):xvii-xviii. doi: 10.1016/j.ocl.2023.05.001. PMID: 37271565
Azar FM. Perioperative Pain Management. Orthop Clin North Am. 2023 Oct;54(4):xv-xvi. doi: 10.1016/j.ocl.2023.06.008. Epub 2023 Jul 21. PMID: 37718089
Azar FM. Preface. Orthop Clin North Am. 2023 Apr;54(2):xv. doi: 10.1016/j.ocl.2023.01.001. PMID: 36894296
Azar FM. Preface. Orthop Clin North Am. 2023 Jan;54(1):xi-xii. doi: 10.1016/j.ocl.2022.10.001. PMID: 36402515
Holbrook HS, Greenberg JA, Weller WJ. Application of Tendon With Z-Lengthening Technique. 2023 Jul;48(7):740.e1-740. e11. doi: 10.1016/j.jhsa.2022.12.016. Epub 2023 Mar 4. PMID: 36878756. Review
Holbrook HS, Calandruccio JH. Management of Gout in the Hand and Wrist. Orthop Clin North Am . 2023 Jul;54(3):299-308. doi: 10.1016/j.ocl.2023.02.003. PMID: 37271558
Farrell N, Greenfield PT, Rutkowski PT, Weller WJ. Perioperative Pain Management for Distal Radius Fractures. Orthop Clin North Am. 2023 Oct;54(4):463-470. doi: 10.1016/j. ocl.2023.05.006. Epub 2023 Jun 26. PMID: 37718085
Chen AN, Ragsdale TD, Rhodes LN, Lock LL, Moisan A, Kelly DM. Prospective, Randomized Ponseti Treatment for Clubfoot: Orthopaedic Surgeons Versus Physical Therapists. J Pediat Orthop. 2023 Feb; 43(2):e93-e99. doi: 10.1097/ BPO.0000000000002291, Epub 2022 Nov. 4. PMID: 36607913. Clinical Trial
Cope SR, Wideman M, Sheffer BW, Sawyer JR, Beaty, JH, Warner, WC, Spence DD, Kelly DM. Early Failure of Locking Compression Plates in Pediatric Proximal Femoral Fracture. JPOSNA Vol 5(3) Aug 2023. https://doi.org/10.55275/ JPOSNA-2023-436
Farrell ND, Dooley JH, Sheffer BW, Sawyer JR. Kelly DM. Radiation Exposure in Multiple Hereditary Exostoses: A Retrospective Review. J Orthop. 2023 May 5;40:87-90. doi: 10.1016/j.jor.2023.05.004. eCollection 2023 Jun. PMID: 37234093
O'Neill NP, Mo ZA, Miller PE, Glotzbecker MP, Li Y, Fletcher ND, Upsasani VV, Riccio AI, Spence DD, Garg S, Krengel W,
Birch C, Hedquist DJ. The Reliability of the AO Spine Upper Cervical Classification System in Children: Results of a MultiCenter Study. J Pediatr Orthop. 2023 Apr 1;43(4):273-277. doi: 10.1097/BPO.0000000000002363. Epub 2023 Jan 30. PMID: 36706430
Padgett AM, Kapoor S, Rhodes LN, Keen K, Cao X, Locke LL, Warner WC, Sawyer JR, Sheffer BW, Spence DD, Kelly DM. Perioperative Multimodal Analgesic Injection for Patients with Adolescent Idiopathic Scoliosis Undergoing Posterior Spinal Fusion Surgery. Spine Deform. 2023 Jul;11(4):977-984. doi: 10.1007/s43390-023-00670-5. Epub 2023 Apr 6. PMID: 37022606
Penncok AT, Bastrom TP, Boutelle KE, Carroll AN, Edmonds EW, Nepple JJ, Polinsky SG, Spence DD, Heyworth BE, Perkins C, Willimon SC. FACTS Study Group. Bony
Remodeling of Adolescent Displaced Clavicle Fractures: A FACTS Study. Am J Sports Med. 2023 Mar;51(4):871-876. doi: 10.1177/03635465231152884. Epub 2023 Feb 20. PMID: 36802767
Quan T, Matsumoto H, Bonsignore-Opp L, Ramo B, Murphy RJ, Brooks JR, Wellborn MC, Emans JB, Anari JB, Johnnston CE, Akbarnia BA, McCarthy R, Flynn J, Sawyer JR, Vitale MG, Roye BD, Pediatric Spine Study Group. Definition of Tweener: Consensus Among Experts in Treating Early-onset Scoliosis. J Pediatr Orthop. 2023 Mar 1;43(3):e215-3222. doi: 10.1097/ BPO.0000000000002321. Epub 2022 Dec 12. PMID: 36729774
Rambo AJ, Sheffer BW, Hajek B, Almatari A, Suit P, Rhodes LN, Cao X, Warner WC, Sawyer JR, Kelly DM, Spence DD. Asymptomatic Lumbar Spondylolysis in the Pediatric Population: A Retrospective CT Review with Radiology Review. Accepted to JAAOS-11/17/23
Spence DD (FACTS Study Group). Five Year Radiographic and Functional Outcomes of Non-operative Treatment of Completely Displaced Midshaft Clavicle Fractures in Teenagers. Accepted to AJSM-12/11/23
Spence DD, Hefti F. Online Video Resources Pertaining to Cerebral Palsy: A YouTube-Based Quality-Control Study. Accepted to J of Children's Orthopaedics-12/9/23
Sturdivant A, Roberts C, Nahr A, Bryan K, Sheffer BW, Spence DD, Sawyer JR. Fasted or Not: Anesthesia-Related Pulmonary Complication in Pediatric Orthopedic Emergencies. JPOSNA: 5(4):1-8. November 2023
Swarup I, Pearce R, Sanborn BS, Spence DD (CORTICES). Variations in the Management of Closed Salter-Harris II Distal Tibia Fractures. J Pediatr Orthop . 2023 Oct 1;43(9):e742-e746. doi: 10.1097/BPO.0000000000002488. Epub 2023 Aug 22. PMID: 37606098
Diltz ZD, Sheffer BJ. Intraoperative Navigation and Robotics in Pediatric Spinal Deformity. Orthop Clin North Am . 2023 Apr;54(2):201-207. doi: 10.1016/j.ocl.2022.11.005. PMID: 36894292
Locke LL, Rhodes LN, Sheffer BW. Accelerated Protocols in Adolescent Idiopathic Scoliosis Surgery. Orthop Clin North Am. 2023 Oct;54(4):427-433. doi: 10.1016/j.ocl.2023.04.003. Epub 2023 Jun 26. PMID: 37718082












Beard NM, Beggs L, Murphy WG, Knack MC, Golden O, Ross W. Ultrasound-Guided Injection Through the Rotator Cuff Interval: A Clinical Perspective of One Institution's Results and Description of Technique. J Osteopath Med. 2023 Aug 18. doi: 10.1515/jom-2023-0129. Online ahead of print. PMID: 37589664
Martinez SF. A Fresh Review of Common Shoulder Conditions. Phys Med Rehabil Clin N Am. 2023 May;34(2):xiii-xiv. doi: 10.1016/j.pmr.2023.02.001. Epub 2023 Mar 3. PMID: 37003667
Martinez SF. Insights with Friends. Phys Med Rehabil Clin N Am. 2023 Feb;34(1):xiii. doi: 10.1016/j.pmr.2022.09.002. Epub 2022 Oct 18. PMID: 36410894
Allen C, Kumar V, Elwell J, Overman S, Schoch B, Aibinder W, Parsons M, Watling J, Ko JK, Gobbato B, Throckmorton TW, Routman H, Roche CP. Evaluating the Fairness and Accuracy of Machine Learning Based Predictions of clinical Outcomes after Anatomic and Reverse Total Shoulder Arthroplasty. J Shoulder Elbow Surg. 2023 Sep 12:S1058-2746(23)00651-1. doi: 10.1016/j.jse.2023.08.005. Online ahead of print. PMID: 37703989
Amini MH, Patel M, Stone GP, Roberson TA, Brolin TJ, Sykes JB. Acute, Traumatic Rotator Cuff Tears Have Smaller Critical Shoulder Angles Than Degenerative Tears. Arthroscopy. 2023 Feb;39(2):225-231. doi: 10.1016/j.arthro.2022.08.042. Epub 2022 Oct 5. PMID: 36208709
Eason RR, Joyce MR, Throckmorton TW, Azar FM, Bernholt DL, Naser AM, Brolin TJ. Comparison of Triamcinolone and Methylprednisolone Efficacy and Steroid Flare Reaction Rates in Shoulder Corticosteroid Injection: A Prospective Interrupted Time Series Study. J Shoulder Elbow Surg. 2023 Nov;32(11):22142221. doi: 10.1016/j.jse.2023.05.023. Epub 2023 Jun 20. PMID: 37348782
Flurin PH, Abadie P, Lavignac P, Laumonerie P, Throckmorton TW. Outpatient vs Inpatient Total Shoulder Arthroplasty: Complication Rates, Clinical Outcomes and Eligibility Parameters. JSES International. 22 August 2023. https://doi. org/10.1016/j.jseint.2023.06.029
Holbrook H, Azar FM, Throckmorton TW, Brolin TJ. Determining the Follow-up Rates for Shoulder Arthroplasty: A Retrospective Review of a Multicenter Study of 4700 Shoulders. Seminars in Arthroplasty: JSES. 2 Dec 2023. https://doi. org/10.1053/j.sart.2023.10.004
James N, Jennewine B, Polio W, Naser AM, Nieboer M, Schoch B, Throckmorton TW, Bernholt DL, Azar FM, Brolin TJ. Superior Humeral Head Osteophytes Are Associated with Rotator Cuff Insufficiency in Glenohumeral Osteoarthritis: a Retrospective Analysis. Eur J Orthop Surg Traumatol. 2023 Sep 28. doi: 10.1007/s00590-023-03727-3. Online ahead of print. PMID: 37770594
Jawa A, (RSA Multicenter Research Group), Konrade E, Knack MC, Brolin TJ, Throckmorton TW. Predictors of Dislocations After Reverse Shoulder Arthroplasty: A Study by the ASES Complications of RSA Multicenter Research Group. J Shoulder Elbow Surg. 2023 Jun 26:S1058-2746(23)00484-6. doi: 10.1016/j.jse.2023.05.028. Online ahead of print. PMID: 37379964
Jawa A, (RSA Multicenter Research Group), Konrade E, Knack MC, Brolin TJ, Throckmorton TW. Risk Factors of Acromial and Scapular Spine Stress Fractures Differ by Indication: A study by the ASES Complications of Reverse Shoulder Arthroplasty Multicenter Research Group. J Shoulder Elbow Surg . 2023 Dec;32(12):2483-2492. doi: 10.1016/j.jse.2023.05.015. Epub 2023 Jun 15. PMID: 37330167
Jennewine B, Pierce AS, Miller AH, Azar AT, Sharp CD, Azar FM, Bernholt DL, Throckmorton TW, Brolin TJ. PatientSelection Algorithm for Outpatient Shoulder Arthroplasty in Ambulatory Surgery Center: A Retrospective Update. J Shoulder Elbow Surg. 2023 Aug 23:S1058-2746(23)00601-8. doi: 10.1016/j.jse.2023.07.018. Online ahead of print. PMID: 37625693
Marois A, Brolin TJ, Bernholt DL, Azar FM, Throckmorton TW. Teres Minor Deficiency Does Not Predict Clinically Inferior External Rotation After Reverse Total Shoulder Arthroplasty: A 2-year Matched Cohort Study. Accepted to Seminars in Arthroplasty: JSES-11/30/23
Murphy A, Azar FM, Brolin TJ, Throckmorton TW. Accuracy of MRI to Detect Lateral Ulnar Collateral Ligament Tears. Accepted to JSOA-8/1/23
Neel R, Bernholt DL, Azar FM, Brolin TJ, Throckmorton TW, Gutman I. Comparison of Sensitivity of Diagnosis of Subscapularis Tear on 1.5 Tesla versus 3.0 Tesla Magnetic Resonance Imaging. Orthop J Sports Med. 2023 Jul; 11(7 suppl3): 2325967123S00159. PMC10392414.
Polio WP, Hajek, Brolin TJ, Mihalko WM, Singhal K, Hughes S, Nelson A, Hayes T, Chiu CY, Bernholt DL, Azar FM, Throckmorton TW. Muscle Activation Patterns during Active External Rotation after Reverse Total Shoulder Arthroplasty: An Electrophysiological Study of the Teres Minor and Associated Musculature. J Shoulder Elbow Surg. 2023 Sep 29:S10582746(23)00708-5. doi: 10.1016/j.jse.2023.08.031. Online ahead of print. PMID: 37778657
Simmons C, DeGrasse J, Polakovic S, Aibinder W, Throckmorton T, Noerdlinger M, Papandrea R, Trenhaile S, Schoch B, Gobbato B, Routman H, Parsons M, Roche CP. Initial Clinical Experience with a Predictive Clinical Decision Support Tool for Anatomic and Reverse Total Shoulder Arthroplasty. Eur J Orthop Surg Traumatol. 2023 Dec 14. doi: 10.1007/s00590-02303796-4. Online ahead of print. PMID: 38095688
Jennewine BR, Brolin TJ. Emerging Technologies in Shoulder Arthroplasty: Navigation, Mixed Reality, and Preoperative Planning. Orthop Clin North Am. 2023 Apr;54(2):209-225. doi: 10.1016/j.ocl.2022.11.006. Epub 2023 Jan 31. PMID: 36894293
Polio W, Brolin TJ. Postoperative Rehabilitation After Shoulder Arthroplasty. Phys Med Rehabil Clin N Am. 2023 May;34(2):469479. doi: 10.1016/j.pmr.2022.12.010. Epub 2023 Feb 26. PMID: 37003664
Throckmorton TW. Rehabilitation of Operative and Nonoperative Shoulder Pathologies. Phys Med Rehabil Clin N Am. 2023 May;34(2):xv-xvi. doi: 10.1016/j.pmr.2023.02.002. PMID: 37003668)
Chambers JS, Kropp RG, Gardocki RJ. Reoperation Rates and Patient-reported Outcomes of a Single and Two-level Anterior Cervical Discectomy and Fusion. Arch Orthop Trauma Surg. 2023 Jan; 143(1):265-268. doi: 10.1007/s00402-021-04056-y. PMID: 34244874
Olinger C, Coffman A, Campion CE, Thompson KM, Gardocki RJ. Initial Learning Curve After Switching to Uniportal Endoscoppic Discectomy for Lumbar Disc Herniations. Eur Spine J. 2023 Aug;32(8):2694-2699. doi: 10.1007/s00586-02307583-x. Epub 2023 Feb 22. PMID: 36811652
Romero A, Lunch D, Johnson E, Zhu X, Kirkpatrick J. MRI Order Appropriateness for Chronic Neck Pain: Comparison of Ordering Practices and Treatment Outcomes for Primary Care Physicians and Specialists. J Orthop Res. 2023 Jul 31. doi: 10.1002/jor.25669. Online ahead of print. PMID: 37525551
Diltz ZR, West EJ, Colatruglio MR, Kirwan MJ, Konrade EN, Thompson KM. Perioperative Management of Comorbidities in Spine Surgery. Orthop Clin North Am. 2023 Jul;54(3):349358. doi: 10.1016/j.ocl.2023.02.007. Epub 2023 Apr 7. PMID; 37271563
Azar FM (NBA sports group), Mack CD. Epidemiology of Injuries among National Basketball Association Players: 2013-14 through 2018-19. Accepted to Sports Health-11/25/23
Azar FM, Brolin TJ, Throckmorton TW, Witte D, Bernholt DL. The Incidence of Posterolateral Tibial Plateau and Central Lateral Femoral Condylar Impaction Fractures in a Pediatric and Young Adult Population after ACL Injury. J Pediatr Orthop. 2023 Jan 1;43(1):18-23. doi: 10.1097/BPO.0000000000002270. Epub 2022 Sep 21. PMID: 36129359
Baessler AM, Buchman JM, Witte DA, Spence DD, Throckmorton TW, Brolin TJ, Azar FM, Bernholt DL. Skeletally Immature Patients with ACL Bone Bruise Patterns Have a Higher Chance of Having an Intact ACL Than Skeletally Mature Patients. J Pediatr Orthop. 2023 Jan 1;43(1):13-17. doi: 10.1097/ BPO.0000000000002268. Epub 2022 Sep 21. PMID: 36129350
Bernholt DL, Skinner WC, Holt AM, Azar FM. Knee Arthroscopy After Prior Total Knee Arthroplasty; Narrative Review. J Am Acad Orthop Surg. 2023 Jan 15;31(2):57-63. doi: 10.5435/JAAOS-D-21-01094. PMID: 36580044
Lamplot JD, Smith BL, Slone HS, Hauck OL, Wijdicks CA. Tape-reinforced Graft Suturing and Retensioning of Adjustableloop Cortical Buttons Improve Quadriceps Tendon Autograft Biomechanics in Anterior Cruciate Ligament Reconstruction: A Cadaveric Study. Arthroscopy. 2023 Jun 22:S07498063(23)00473-5. doi: 10.1016/j.arthro.2023.06.021. Online ahead of print. PMID: 37355187
Marois AJ, Achecar A, Azar FM, Bernholt DL, Brolin TJ, Throckmorton TW. Grit Score Predictive of Increased Risk for Opioid Prescription Refill Following Primary Arthroscopic Rotator Cuff Repair. J Surg Orthop Adv. 2023 Fall; 32 (3): 177-181. PMID: 38252605.
Petit CB, Diekfuss JA, Warren SM, Barber Foss KD, Valencia M, Thomas SM, Petushek EJ, Karas SG, Hammond KE, Pombo MW, Labib SA, Maughon TS, Whitfield BJ, Myer GD, Xerogenanes JW, Lamplot JD. Allograft Anterior Cruciate Ligament Reconstruction Fails a Greater Rate in Patients Younger Than 34 Years. Arthrosc Sports Med Rehabil. 2023 Jun 10;5(4):100741. doi: 10.1016/j.asmr.2023.04.024. eCollection 2023 Aug. PMID: 37645392
Schick A, Cantrell CK, Young B, Mosher Z, Ewing M, Elphingstone JW, Brabston E, Ponce BA, Momaya. The Mechanism of Anterior Cruciate Ligament Injuries in the National Football League: A Systematic Video Review. Cureus. 2023 Jan 27;15(1):e34291. doi: 10.7759/cureus.34291. eCollection 2023 Jan. PMID: 36860227
Wallace GJ, Thompson JD, Diekfuss JA, Champagne AA, Myer GD, Kaiser J, Lamplot JD. Suture Augmentation of a Four-Strand Semitendinosus Graft Improves Time-Zero Biomechanical Properties. Arthroscopy. 2023 Jun 22:S0749-8063(23)00472-3. doi: 10.1016/j.arthro.2023.06.020. Online ahead of print. PMID: 37355190
Guo S, Chen J, Hu P, Li C, Wang X, Chen N, Sun J, Wang Y, Wang J, Gu W, Wu S. The Value of Circulating Tumor Cells and Tumor Markers Detection in Lung Cancer Diagnosis. Technol Cancer Res Treat. 2023 Jan-Dec;22:15330338231166754. doi: 10.1177/15330338231166754. PMID: 37093867
Seo JW, Jo SH, Kim SH, Choi BH, Cho H, Yoo JJ, Park SH. Application of Cartilage Extracellular Matrix to Enhance Therapeutic Efficacy of Methotrexate. Tissue Eng Regen Med . 2023 Oct 14. doi: 10.1007/s13770-023-00587-0. Online ahead of print. PMID: 37837499
Yao L, Chemaitelly H, Goldman E, Gudina EK, Khalil A, Ahmed R, James AB, Roca A, Fallah MP, Macnab A, Cho WC, Eikelboom J, Qamar FN, Kremsner P, Oliu-Barton M, Sisa I, Tadesse BT, Marks F, Wang L, Kim JH, Meng X, Wang Y, Fly AD, Wang CY, Day SW, Howard SC, Graff JC, Maida M, Ray K, Franco-Paredes C, Mashe T, Ngongo N, Kaseya J, Ndembi N, Hu Y, Bottazzi ME, Hotez PJ, Ishii KJ, Wang G, Sun D, Aleya L, Gu W. Time to Establish an International Vaccine Candidate Pool for Potential Highly Infectious Respiratory Disease: A Community's View. EClinicalMedicine . 2023 Sep 26:64:102222. doi: 10.1016/j.eclinm.2023.102222. eCollection 2023 Oct. PMID: 37811488
Zhang C, Yao J, Liu C, Yang K, Zhang W, Sun D, Gu W. The Role of Thyroid Hormone Synthesis Gene-related miRNAs Profiling in Structural and Functional Changes of the Thyroid Gland Induced by Excess Iodine. Biol Trace Elem Res. 2023 May 27. doi: 10.1007/s12011-023-03691-3. Online ahead of print. PMID: 37243879
Zhu C, Gu W, Sun D, Wei W. The Mechanism Underlying Fluoride-induced Low-renin Hypertension is Related to an Imbalance in the Circulatory and Local Renin-angiotensin Systems. Toxicol Lett. 2023 May 15;381:36-47. doi: 10.1016/j. toxlet.2023.04.010. Epub 2023 Apr 25. PMID: 37105417
Dunbar RP, Egol KA, Jones CB, Ertl JP, Mullis B, Perez E, Collinge CA, Ostrum R, Humphrey C, Gardner MJ, Ricci WM, Phieffer LS, Teague D, Ertl W, Born CT, Zonno A, Siegel J, Sagi HC, Pollak A, Schmidt AH, Templeman D, Sems A, Friess DM, Pape HC, Krieg JC, Tornetta P 3rd. Locked Lateral Plating vs Retrograde Nailing for Distal Femur Fractures: A Prospective Multicenter Randomized Trial. J Orthop Trauma. 2023 Feb 1;37(2):70-76. doi: 10.1097/BOT. 0000000000002482. PMID: 36026544
Dunbar RP, Egol KA, Jones CB, Ostrum RF, Humphrey CA, Ricci WM, Phieffer LS, Teague DC, Sagi HC, Pollak AN, Schmidt AH, Sems A, Pape HC, Morshed S, Perez EA, Tornetta P 3rd. Locked Plating versus Nailing for Proximal Tibial Fractures: A Multicenter RCT. J Orthop Trauma. 2023 Apr 1;37(4):155-160. doi: 10.1097/BOT.000000000000253. PMID: 36729919. Clinical Trial
Tobey D, Wing C, Calkins T, Heck RK. The Use of Proximal Femur Replacement for the Management of Oncologic Lesions in the Proximal Femur: A Review. Orthop Clin North Am . 2023 Jan;54(1):23-35. doi: 10.1016/j.ocl.2022.08.006. Epub 2022 Oct 23. PMID: 36402508
Garner S, Zhao J, Murphy GA, Rider CM. Graft Reconstruction for Treatment of Chronic Achilles Tendon Ruptures. Master Techniques in Orthopaedic Surgery: The Foot and Ankleaccepted per Dr. Zhao-11/29/23
Kelly DM, Sawyer JR. Lateral Condylar and Capitellar Fractures of the Distal Humerus, in Waters PM, Skaggs DL, Flynn JM (editors): Rockwood and Wilkins Fractures in Children, in production
McClatchy SG, Throckmorton TW. Outpatient Total Joint Arthroplasty, in AAOS, Value-Based Health Care, In production
Rambo AJ, Sawyer JR. Open Reduction and Internal Fixation of Tibial Tubercle Fracture, in Oetgen and Fletcher (editors): Pediatric Orthopaedic Surgery, in production

As president of the Willis C. Campbell Club, I’ve had the benefit of speaking with many of our dedicated alumni. What sets our group apart is that we are truly a family. As we say around here, at Campbell, you can always come home.
This year marks the 26th WCC Triennial, the 2024 Alvin J. Ingram Lecture, and the celebration of the Campbell Residency Centennial!
It’s an honor to support this great legacy and serve you, our fellow alumni. Throughout the last year, we’ve seen hundreds of you attend Campbell alumni gatherings at orthopaedic conferences and subspecialty meetings. The new online WCC Alumni Directory is now a resource for you all. Many of you have signed up to serve as mentors to current and future orthopaedic surgery residents.
I’d like to welcome John Priddy, MD, Class of 2002, as the incoming WCC alumni president. As a graduate of the Campbell Clinic Foot and Ankle fellowship, Dr. Priddy practices in Tyler, Texas at Azalea Orthopaedics and Sports Medicine. Said Dr. Priddy, “As alumni donors and mentors, you help residents prepare for an increasingly complex and sub-specialized world for medicine. Your gift results in more cadaveric labs, education travel, and hands-on experiences so they can be prepared for anything.”
We all feel pride in the exceptional orthopaedic surgery training that has distinguished our Campbell experience and prepared us to be surgeons and leaders.
None of this would be possible without you: the donors, partners, and friends who support this work. Your gifts are the secret sauce to excelling in education, orthopaedic research, and community outreach – and moving lives each and every day.
Thank you for your generosity,
Christopher (Chris) Ihle, MD, Class of 1985 Willis C. Campbell Club Alumni PresidentFrederick M. Azar, MD Class of 1994
Memphis, TN
James H. Beaty, MD Class of 1981
Memphis, TN
Gregory M. Behm, MD Class of 1999
Hamilton, MT
W. Kenneth Bell, MD Class of 1981
Maryville, TN
Bradford L. Boone, MD Class of 1990
Tulsa, OK
Douglas N. Calhoun, MD Class of 2004
Knoxville, TN
James L. Chappuis, MD Class of 1985
Atlanta, GA
Michael S. Clarke, MD Class of 1974
Springfield, MO
Scott S. Cooper, MD Class of 1996
Bentonville, AR
Stephen B. Cope, MD Class of 1989
Mobile, AL
Randall L. Davidson, Jr., MD Class of 1990
Columbia, TN
Robert H. Haralson, III, MD Class of 1969
Knoxville, TN
David Heinsch, MD
Class of 2015
Newnan, GA
Philip G. Hunt, MD Class of 1988
Paducah, KY
Christopher L. Ihle, MD, President Class of 1985
Omaha, NE
A. Alex Jahangir, MD Class of 2008
Nashville, TN
Scott W. McCall, MD Class of 2006
Franklin, TN
Hassan Mir, MD Class of 2008
Tampa, FL
Kenneth L. Moore, MD Class of 1975
Franklin, TN
Catherine Olinger, MD Class of 2020
Iowa City, IA
Brian Perkinson, MD Class of 2012
Nashville, TN
John F. Priddy, MD Class of 2002
Tyler, TX
Walter R. Shelton, MD Class of 1979
Madison, MS
Jeffrey M. Smith, MD Class of 1995
San Diego, CA
Simplified access with preferred status for EUFLEXXA on any plans #1 #1

REFERENCES: 1. Rolling 12-month average of IQVIA claims data based on unique patients (through October 2020). 2. MMIT medical benefits data (October 2020); preferred status for commercial, Medicare Advantage, and managed Medicaid plans.
EUFLEXXA® is a registered trademark of Ferring B.V. ©2021 Ferring B.V. All rights reserved. 01/21 US-EU-2000134 Contact
Alfons Altenberg, MD
Lewis D. Anderson, MD
Robin Arena, MD
Borden Bachynski, MD
Troy Bagwell, MD
James Barnett, MD
Robert Basist, MD
Henry Beck, MD
Reginald V. Bennett, MD
Dan R. Bigelow, MD
Thomas H. Blake, Sr., MD
W. Griffin Bland, MD
Michael Bluhm, MD
Joseph C. Boals, III, MD
Harrison O. Bourkard, MD
Robert L. Bourland, MD
William J. Bourland, MD
Harold B. Boyd, MD
David M. Bratton, MD
Hanes H. Brindley, Sr., MD
Robert G. Brashear, MD
Charles E. Brighton, MD
Louis P. Britt, MD
Joseph C. Burd, MD
John G. Caden, MD
Rocco A. Calandruccio, MD
Willis C. Campbell, MD
S. Terry Canale, MD
Dan Carlisle, MD
Peter G. Carnesale, MD
Charles O. Carothers, MD
Charles A. Carraway, MD
Paul A. Caviale, MD
Tom Phillip Coker, MD
Romulo E. Colindres, MD
Harry Collins, MD
Francis V. Costello, MD
John M. Crates, MD
P. Thurman Crawford, MD
A. Hoyt Crenshaw, Sr., MD
Henry I. Cross, MD
Jere M. Disney, MD
Daniel B. Eck, MD
Thomas S. Eddleman, MD
Allen S. Edmonson, MD
Richard L. Ennis, MD
J. Kendall Ethridge, MD
E.W. Ewart, MD
W. McDaniel Ewing, MD
Edward L. Farrar, MD
M. Craig Ferrell, MD
Bryan Fleming, MD
Dale E. Fox, MD
Kermit W. Fox, MD
Isaac L. George, MD
Marvin M. Gibson, MD
E.R. ‘Rickey’ Innis, MD
Otis E. James, Jr., MD
Leland H. Johnson, Jr., MD
David S. Johnston, MD
Orville N. Jones, MD
Dan Klinar, MD
Robert A. Knight, MD
Timothy H. Krahn, M.D
F. E. Linder, MD
Stanley Lipinski, MD
Wayne B. Lockwood, MD
John F. Lovejoy, MD
William L. Lovett, MD
Harry A. Luscher, MD
Athey R. Lutz, MD
Arthur Osborne, MD
W. Martin Payne, MD
Samuel B. Prevo, MD
George D. Purvis, MD
R. Beverly Ray, MD
Thomas A. Richardson, MD
S. L. Robbins, MD
R. C. Robertson, MD
Gary Giles, MD
A. Lee Gordon, III, MD
Harry R. Gossling, MD
John T. Gray, MD
Basil Griffin, MD
Herbert Alfred Hamel, MD
Joe Frank Hamilton, Jr., MD
Joe Frank Hamilton, Sr., MD
Richard M. Harkness, MD
Benjamin L. Hawkins, MD
David N. Hawkins, MD
Harold M. Hawkins, MD
C. Leon Hay, MD
Don Henard, MD
Edward D. Henderson, MD
Michael Lynch, MD
H. B. Macey, MD
Thomas W. Marks, MD
Paul H. Martin, MD
Benjamin M. Mauck, MD
George S. Mauerman, MD
Juan A. Mayne, MD
James M. McBride, MD
Frank O. McGhee, MD
C. C. McReynolds, MD
I. S. McReynolds, MD
Malcolm E. Heppenstall, MD
George B. Higley, Sr., MD
Kenneth C. Hill, MD
Royce Hobby, MD
John T. Hocker, MD
Frank C. Hodges, MD
James D. Hodnett, MD
Louis Horn, III, MD
John M. Hundley, MD
Wiley C. Hutchins, MD
Alvin J. Ingram, MD
Walter C. Metz, MD
Lee W. Milford, MD
T. Rothrock Miller, MD
Alfred F. Miller, MD
Andrew H. Miller, MD
William L. Minear, MD
J. M. Mitchell, MD
Joseph Mitchell, MD
J. M. Mitchner, MD
Wayne S. Montgomery, MD
James D. Moore, MD
Larry B. Morrison, MD
James S. Mulhollan, MD
John T. Murphy, MD
Vernon Nickel, MD
R. C. Rountree, MD
Fred P. Sage, MD
Fred M. Sandifer, III, MD
Stanley Schwartz, MD
T. David Sisk, MD
W. H. Sisler, MD
Donald Slocum, MD
Hugh Smith, MD
J. Spencer Speed, MD
William B. Stanton, MD
Marcus J. Stewart, MD
Bruce Stivers, MD
Mario M. Stone, MD
Henry Thomas Stratton, MD
Ernest J. Tarnow, MD
Ethan O. Todd, MD
Robert E. Tooms, MD
Phillip C. Trout, MD
Thomas C. Turner MD
Fredrico Van Domselaar, MD
Keith D. VandenBrink, MD
Isaac L. Van Zandt, MD
John A. Vann, MD
R. H. Walker, Jr., MD
Thomas L. Waring, MD
Robert E. Wells, MD
Gilbert G. Whitmer, MD
James H. Wiley, MD
Harold Williamson, MD
Frank D. Wilson, MD
Frederick C. Workmon, MD
B. T. Wright, MD

Since 1946, the Campbell Clinic Foundation has trained the physicians and facilitated the research that has helped people in our community –and around the world – keep moving toward their best lives.
We work every day to take that legendary orthopaedic leadership to the next level, to make life better for those of us who have bone and joint injuries. To make life better for all of us.
We educate top-tier physicians who are committed to unsurpassed patient care through the UTHSC-Campbell Clinic Department of Orthopaedic Surgery and Biomedical Engineering Residency and Fellowship programs and unique sub-specialty medical education programs.


We conduct pioneering research into the causes, cures, and treatments of musculoskeletal diseases and disorders, and we educate the healthcare community as a leading provider of scholarly publications.


Through diverse programs and physician involvement, we provide orthopaedic resources and education programs to children and adults across the Mid-South and around the world.


Movement is a gift, and when you support the Campbell Clinic Foundation, you invest in leading-edge medical education, life-changing research, and high quality, compassionate orthopaedic care to move lives in our local communities and across the globe.
At the core of our work is a mission of care, service to the orthopaedic profession, and service to a greater community. Our growth, success, and impact are only possible because of you – our donors, partners, and colleagues. Whether you attend Foundation events, share our mission and our story, or contribute funds to our programs, you make a difference. You can change the world for a runner. A child with a disability. A caregiver with chronic pain. A parent. A family.
At the core of our work is a mission of care, service to the orthopaedic profession, and service to a greater community. Our growth, success, and impact are only possible because of you – our donors, partners, colleagues. Whether you attend Foundation events, share our mission and our story, or contribute funds to our programs, you make a difference. You can change the world for a runner. A child with a disability. A caregiver with chronic pain. A parent. A family.
$155,036 Individual Support
$481,053 Events
$59,484 Miscellaneous
$662,635 Industry Grants
$106,200 Editorial Services
$348,706 Research Revenue

$138,653 Alumni




$1,090,305 MD Contributions
Make a tribute gift in memory or in honor of someone who has moved your life – a physician, support staff or a loved one.
Become a member of the Campbell Clinic Foundation Legacy Society. By naming the Foundation in your will, your commitment to MOVING LIVES lasts for generations.
Sign up to receive communication from us – stay informed and be involved! Learn about educational events, research breakthroughs, community outreach programs and more.