Journal of Trauma and


Volume 10 | Issue 04 | December 2022 | The Journal of the British Orthopaedic Association | boa.ac.uk
Immersive VR for surgical training p22 Hand partnerships around the world p52 Teaching surgery: Out of Africa, into the future p34
Par tnerships
Orthopaedics
Hand
OrthoFoam Knee Wedges Nailing, nailed.
Simplify patient positioning for tibial or retrograde femoral nailing procedures with our range of trauma triangles. The knee remains in the correct position throughout the procedure with our durable foam providing the perfect balance of cushioning and stability.
Product Code:
OL.OF.KWS Ortholove Knee Wedge Small
OL.OF.KWM Ortholove Knee Wedge Medium






OL.OF.KWL Ortholove Knee Wedge Large
OrthoFoam Adult Ramp Elevator
Surgery, sorted.
Indicated for all surgical cases where elevation is necessary without offloading the heel. Frequently used in trauma cases to enable easy x-ray control. The ergonomic design, with slight concavity, ensures stable support of the limb without too much pressure on the calf.
Product Code: OL.OF.ARE
OrthoFoam SRE Swelling no more.
Indicated following foot and ankle surgical cases for application in theatre or recovery or even preoperatively for trauma cases to ensure reduction of swelling. The ergonomic design ensures patient comfort, with stable elevation at heart level and without strain on the knee or hip. A home use version of the SRE allows patients’ seamless recovery after leaving hospital to the comfort of their home.
Product Code: OL.OF.SRE
01480 457222 / info@ortholove.com / www.ortholove.com Distributed in the UK by LEDA Orthopaedics Other shapes and sizes available. Call or email for more info
22
30
34

38
42
26
44
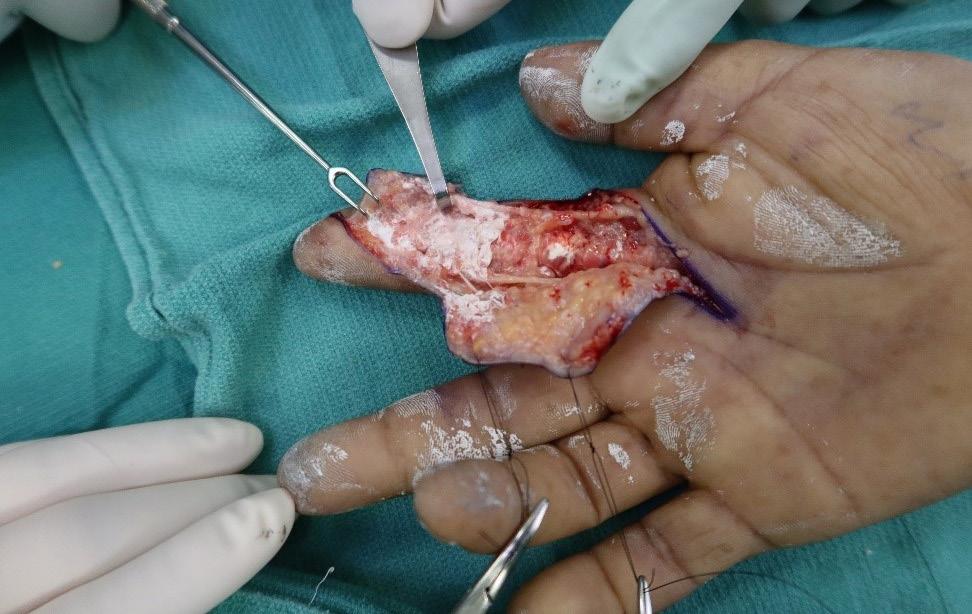
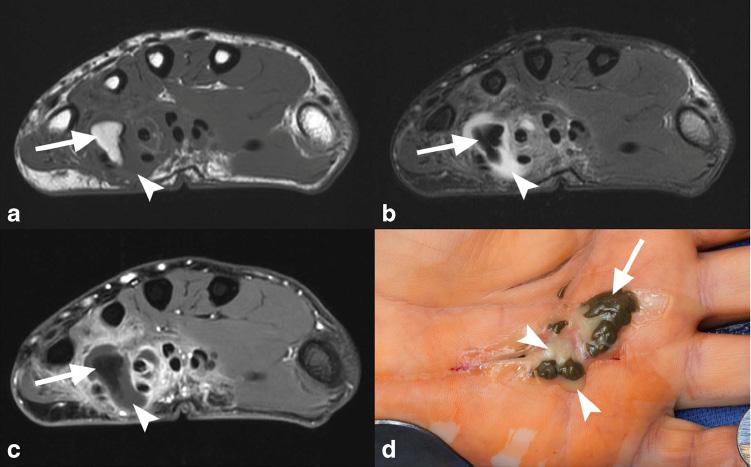
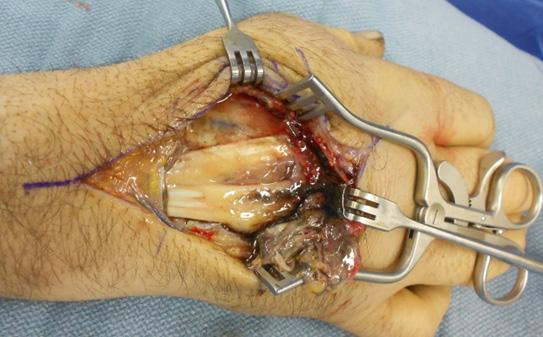
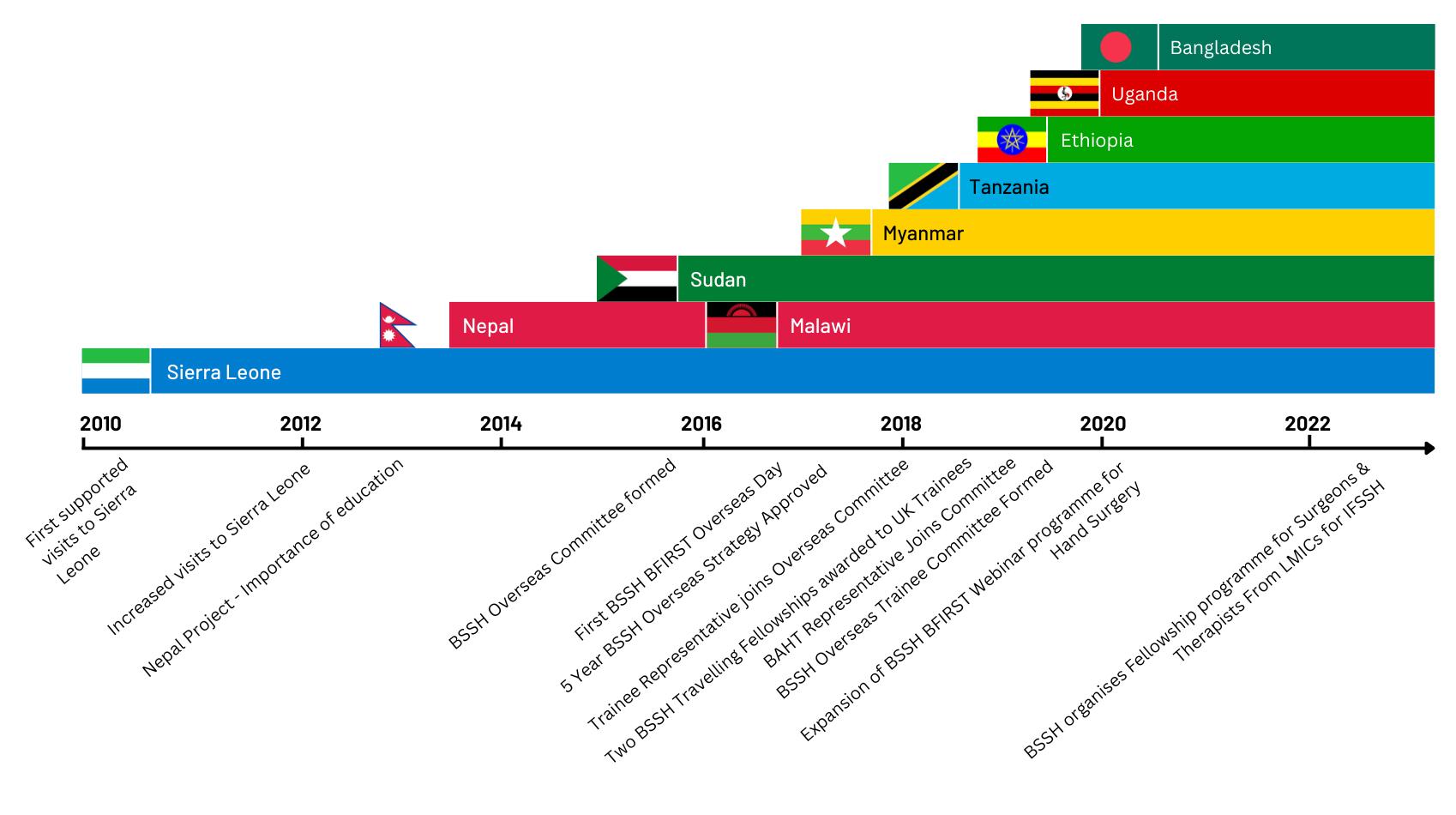
48 Subspecialty: Management of high-pressure injection injuries Guang Yim, Jens Roesner, Warren Hammert, Adeline Clement, Patrick Gillespie and Oliver Stone 52 Subspecialty: Hand partnerships around the world Jonathan Jones, Stephen Hodgson, Rowa Taha and Wee Lam 56 In Memoriam: Gwyn Amman Evans Obituary by Nigel Kiely


Download the App The Journal of







We are




JTO | Volume 10 | Issue 04 | December 2022 | boa.ac.uk | 01 3 From the Executive Editor Simon
5 From
6-7
Latest News 14
18
20
Trauma and Orthopaedics (JTO) is the official publication of the
only publication that reaches T&O surgeons throughout the UK and every BOA member worldwide. The journal is
available to everyone around the world via the
App.
the
function to
access
content.
Did you know that as well as advertising in our Journal publication, we can offer footer banner
on the JTO App! For more information please contact Wendy Parker Email: Wendy@ob-mc.co.uk |
200 7820
Hodkinson this issue... Contents Amputation the context T Orthopaedics T Orthopaedics A Surgical Day Begins Volume 08 Issue 02 Volume 08 Issue 01 Volume 08 Issue 04 Journal of the British Orthopaedic Association The Journal of Trauma and Orthopaedics (JTO) has a dedicated news section, a features section containing interesting articles on various themes, a subspeciality section and a medico-legal section.
the President Deborah Eastwood
BOA
News: 2022 BOA Congress Review
News: New BOA Trustees
News:
Joint Action update
Features: Immersive virtual reality for surgical training in trauma and orthopaedic surgery Thomas Lewis, Mark Bowditch, Wathik El-Alami, Diane Back and Adil Ajuied
Features: Introducing the British Orthopaedic Medical Students Association (BOMSA) Sulaiman Uppal
Features: How do we ensure that the NJR holds high quality data? Chris Boulton, Derek Pegg, Tim Wilton and Mark Wilkinson, on behalf of the NJR
International: Teaching surgery: Out of Africa, into the future Ad Gandhe
Medico-legal: Getting started as an orthopaedic expert witness Sameer Singh
Subspecialty: Partnerships in hand surgery Jonathan Hobby
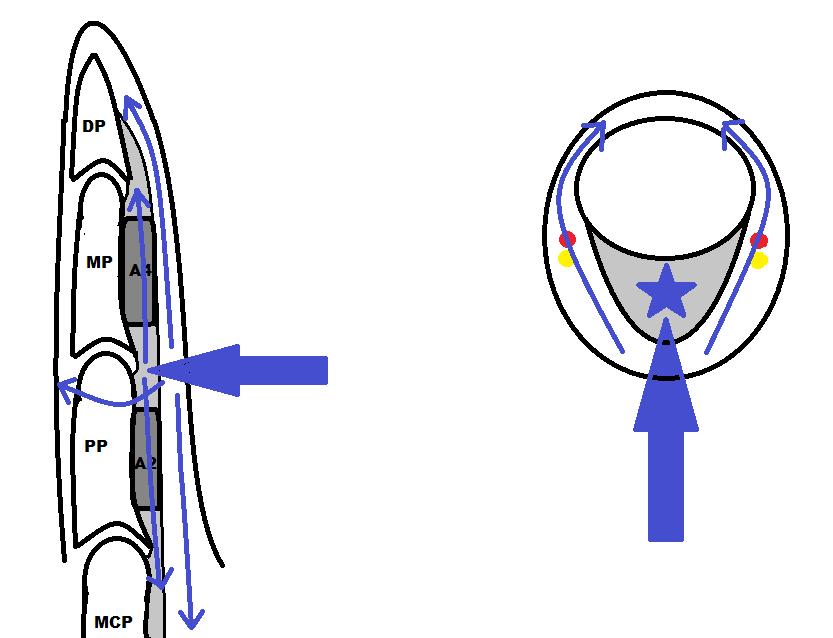
Subspecialty: Management of closed extensor tendon injuries Sarah Turner, Nick Gape and Jonathan Hobby
British Orthopaedic Association (BOA). It is the
also now
JTO
Read
latest issue and past issues on the go, with an advanced search
enable easy
to all
Available at the Apple App Store and GooglePlay – search for JTO @ BOA
advertising
Telephone: +44 (0)121
In
committed to sustainable forest management and
Buxton Press
are
only with 100% vegetable based inks
uses alcohol free printing solutions, eliminating volatile
compounds
well as ozone damaging emissions. Open Box Media & Communications are proud to be corporate sponsors of Heart Research UK (Midlands) 26
Journal of Trauma and Orthopaedics
this publication is printed by
who
certified to ISO14001:2015 Standards (Environmental Management System). Buxton prints
and
organic
as

MOVING
the preparation of implant-like spacers with an articulating bearing S pacer adaptable to the individual patient Mobilisation of the patient during the spacer interval possible In 2-stage revision Simple. Practical. Individual. NO NEED TO STAND STILL www.heraeus-medical.com 11361 EN Medical
KEEP
For
JTO Editorial Team
l Simon Hodkinson (Executive Editor)
l Hiro Tanaka (Editor)
l Simon Britten (Medico-legal Editor)
l Oliver Adebayo (Trainee Editor)
l Jonathan Hobby (Guest Editor)
BOA Executive
l Deborah Eastwood (President)
l John Skinner (Immediate Past President)
l Simon Hodkinson (Vice President)
l Mark Bowditch (Vice President Elect)
l Fergal Monsell (Honorary Secretary)
l Ian McNab (Honorary Treasurer)
l Bob Handley (Appointed Trustee)

BOA

BOA Staff
Executive Office
Chief Operating Officer - Justine Clarke
Personal Assistant to the Executive - Celia Jones
Education Advisor - Lisa Hadfield-Law
Policy and Programmes
Head of Policy and Public Affairs - Gary Robjent
Head of Education and Programmes - Alice Coburn
Programme and Committees Officer - Eliza Heng
Educational Programmes Assistant - Lina Mirghani
Elected Trustees
l Deborah Eastwood (President)
l John Skinner (Immediate Past President)
l Simon Hodkinson (Vice President)
l Mark Bowditch (Vice President Elect)
l Fergal Monsell (Honorary Secretary)
l Ian McNab (Honorary Treasurer)
l Colin Esler
l Anthony Hui
l Andrew Manktelow
l Ian McNab
l Fares Haddad
l Amar Rangan
l Sarah Stapley
l Hiro Tanaka
l Cheryl Baldwick
l Deepa Bose
l Caroline Hing
l Andrew Price
Communications and Operations
Director of Communications and Operations - Annette Heninger
Marketing and Communications Officer - Pujarini Nadaf
Membership and Governance Officer - Natasha Wainwright
Interim Membership and Governance Officer - Vicky McGuinness
Publications and Web Officer - Nick Dunwell
Finance
Director of Finance - Liz Fry
Finance Assistant - Hayley Ly
Events and Specialist Societies
Head of Events - Charlie Silva
Events Coordinator - Venease Morgan Exhibition and Events Coordinator - Anna Prunty
UKSSB Executive Assistant - Henry Dodds
Copyright
Copyright© 2022 by the BOA. Unless stated otherwise, copyright rests with the BOA. Published on behalf of the British Orthopaedic Association by: Open Box M&C
Advertising
All advertisements are subject to approval by the BOA Executive Board. If you’d like to advertise in future issues of the JTO, please contact the following for more information:
Wendy Parker - Media Manager
Email: Wendy@ob-mc.co.uk | Telephone: +44 (0)121 200 7820 Open Box M&C, Premier House, 13 St Paul’s Square, Birmingham B3 1RB
Disclaimer
The articles and advertisements in this publication are the responsibility of the contributor or advertiser concerned. The publishers and editor and their respective employees, officers and agents accept no liability whatsoever for the consequences of any inaccurate or misleading data, opinions or statement or of any action taken as a result of any article in this publication.
BOA contact details
The British Orthopaedic Association, 38-43 Lincoln’s Inn Fields, London WC2A 3PE Telephone: 020 7405 6507
From the Executive Editor
Simon Hodkinson A
s ever it is a pleasure to welcome you all to the December edition of the JTO. In my first editorial Flaming June was a damp squib but three months later we were begging for rain! Now we have it in biblical proportions! Let’s hope we are not emulating Siberia for the next edition.
It been a tumultuous last few months politically, financially and of course in the Health Service with ever increasing winter pressures, elective waiting lists and trauma numbers.
In this edition of the Journal, we open with an article on virtual reality (VR) in surgical training by Thomas Lewis et al. (page 22). Not a new subject by any means but a subject of increasing importance as our young colleague’s grapple with the effects of the pandemic and the loss of over a year’s worth of elective practice. The article covers the considerable advantages of such training but also the current constraints in increased use. We have some way to go in emulating Mr Zuckerberg’s recent TV advert!
The next article introduces a new and very important society in the world of T&O, ‘BOMSA’ the British Orthopaedic Medical Student’s Association (page 26). This new association is the culmination of some very hard work by enlightened young colleagues who have succeeded in bringing together many separate medical school associations under the umbrella of a national body. Medical students are a vital group to T&O as the grass roots of the future work force and the BOA has for a while been focusing on this group primarily to support students with an interest in T&O and to dismiss some of the more archaic impressions students have of the profession. We have a way to go but BOMSA is a great start.
We have our second article this year from the NJR (page 30), highlighting the importance of high quality data in the Registry and as we look to the introduction of an implant registry this article is undoubtedly timely.
Ad Gandhe’s article from Rwanda (page 34) records his latest chapter in his continued passion for, as he puts it, ‘democratising medical education’. A thought provoking article all the way from rusty nails to high tech drone delivery of blood products.
Sameer Singh writes on how to get started as a medico-legal expert continuing the series of articles from the Medico-legal Committee (page 38).
Finally, our subspeciality section looks at hand surgery. Jonathan Hobby, BSSH President, introduces the specialist section (page 42) and is co-author on the first of three articles covering the management of extensor injuries (page 44). This is followed by the management of high pressure injection injuries to the hand (page 48) and then a different perspective on the subject when Jonathan Jones and colleagues discuss the development of hand partnerships around the world (page 52).
Hopefully something for everyone and may I take this opportunity to wish all readers in these difficult times, a happy and at least at some stage, a restful festive season. n
JTO | Volume 10 | Issue 04 | December 2022 | boa.ac.uk | 03
Credits


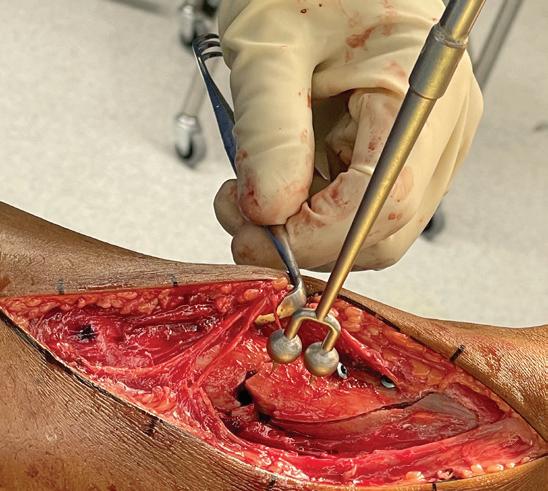

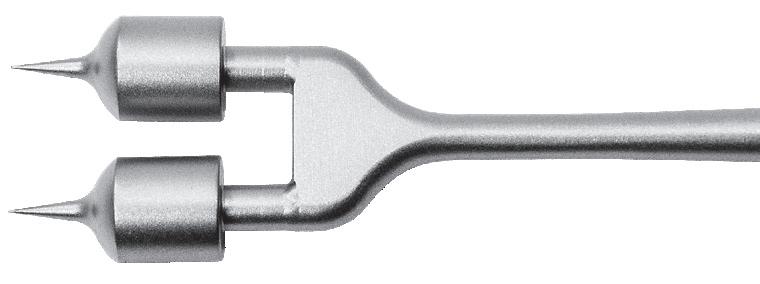
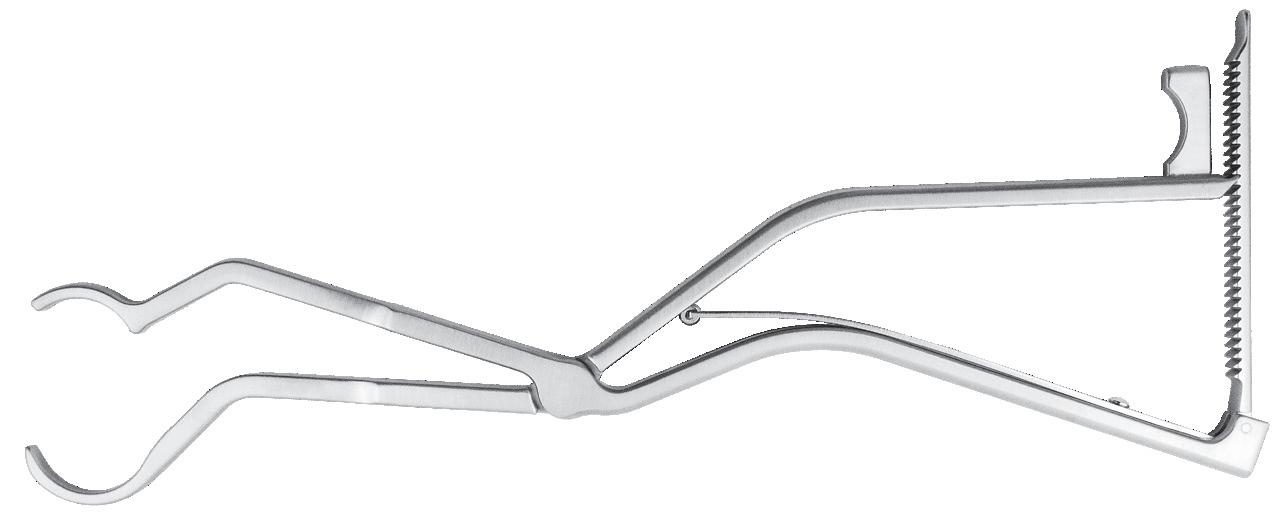










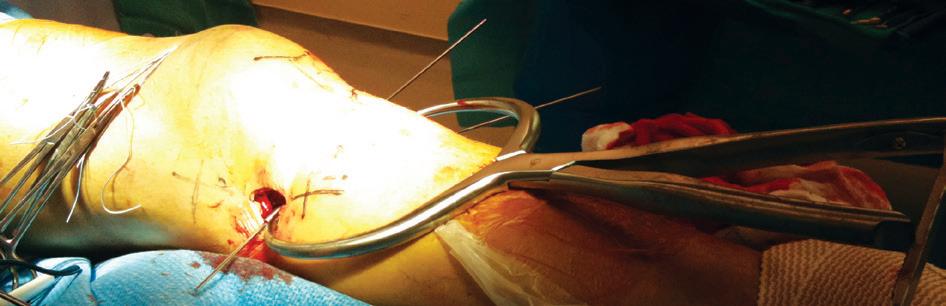





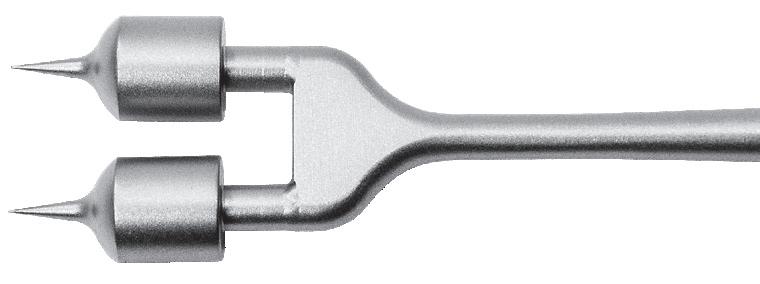
Chandran Double Ball Spike Designed to help rotate and control a butterfly bone fragment for fixation Designed by Rama E. Chandran, MD Designed with a unique contour, the clamp helps with subtrochanteric and femoral shaft fractures treated with current generation femoral IM rodding systems using external aiming arms/targeting devices PRODUCT NO: 3850 Subtrochanteric Femur Fracture Reduction Clamp Designed by David Beard, MD Designed to help provide quick grasp-and-release of an IM guide wire for positioning and advancement along the length of the guide wire Beard IM Nail Guide Wire Clamp Designed by David Beard, MD PRODUCT NO’S: 3019 [Clamp with Ratchet] 3019-01 [Clamp without Ratchet] Available with or without ratchet Designed by Bruce D. Browner, MD Browner MIS Bone Clamp Designed to help hold a bone or bone plate for fixation, the clamp is inserted anterior to the bone, rotated to wrap around the bone, then screwed into the desired position 1379 Designed by Caleb Vosburg, MD Vosburg Cannulated Periarticular Clamp Cannulated clamp tips allow passage of k-wires MADE EXCLUSIVELY FOR INNOMED IN GERMANY PRODUCT NO: 1864 Periarticular Reduction Forceps PRODUCT NO’S: 1856-01 [Small] 1856 [Medium] 1857 [Large] Designed for reduction of intraarticular and periarticular fractures Large Pin Distractor and Compressor Larger 1/8" (3,2 mm) pin hole size for extra sturdy distraction or compression PRODUCT NO’S: 4233 [Large Pin Distractor] 4234 [Large Pin Compressor] COMPRESSOR DISTRACTOR Universal extractor designed to accommodate a large range of screws and screw heads Screw Extractor with Speed Lock Designed by Khaled Sarraf, MD & Konstantinos Doudoulakis, MD PRODUCT NO: 2021 Can also be used to help with removal of other devices that may require a twisting universal locking gripper. FREE TRIAL ON MOST INSTRUMENTS 1.800.548.2362 103 Estus Drive, Savannah, GA 31404 www.innomed.net info@innomed.net 912.236.0000 Phone 912.236.7766 Fax Innomed-Europe Tel. +41 41 740 67 74 Fax +41 41 740 67 71 © 2022 Innomed, Inc. Innomed Europe Alte Steinhauserstrasse 19 CH 6330 Cham Switzerland Tel: +41 (0) 41 740 67 74 www innomed europe com UK Distributor: Hospital Innovations Ltd. Concept House Talbot Green Business Park Pontyclun UK CF72 9FG Tel: +44 1443 719 555 www hospitalinnovations co uk ISO 13485:2016
Reasons to be cheerful?
Deborah Eastwood
If it’s not one thing, it’s another – life keeps us on our toes and balls keep flying in from left field which I am not sure I can blame on the variety of World Cups be it rugby, football or cricket that have tried to distract us recently. Whilst juggling the ‘early’ winter pressures, staff and bed shortages, waiting lists, supply chain issues and the whims of the MHRA it can be difficult to feel optimistic but, in the words of Ian Dury there are ‘reasons to be cheerful’.
On your behalf I have congratulated Professor Tim Briggs on his appointment as NHS England’s National Director for Clinical Improvement and Elective Recovery – it will certainly be a boost to our colleagues and our patients to have an orthopaedic voice so close to the heart of government. He is asking us to think differently in how we deliver care and the BOA is looking to support innovative practice and ideas that will deliver sustainable system changes. Details of the Presidents’ Prize for Sustainable Change will be announced in the new year.
Congratulations too to Deepa Bose who is succeeding Rob Gregory as Chairman of the SAC – big shoes to fill but we have no doubt she will do so.
They say good things come in threes. Hot off the press we are delighted to congratulate John McFall on his selection as the world’s first person with a disability to undergo astronaut training. We really hope he makes it through to take orthopaedics into space! John featured in our June JTO, if you missed it I heartily recommend catching up, it’s a fantastic read.
Since Congress, the executive and I have been engaged in meeting as many of you as possible to ensure that we understand any local problems and we learn from the solutions you have found. On your behalf, we have also put our case to the new Secretary of State for Health and the Chief Executive of the NHS. We need to be proactive in lobbying for our patients and for ourselves: delivery of the elective recovery seems a near impossible ask when we know that there are non-ambulatory trauma admissions, the walking wounded waiting at home for surgical management of their fractures, medical patients with the full gamut of acute illnesses and then our deserving patients who need their life changing orthopaedic care. We have asked that they involve us in developing sustainable change in health care delivery for our MSK patients.
Our BOTA/BOA culture and diversity champions have been working hard designing and delivering projects to bring about sustainable culture change too. I was delighted to see that whilst women still represent only 7.8% of our consultant body, 19% of consultant appointments in 2021 went to women – change is happening.

The STEP (Scottish T&O Equality Project) had a 70% response rate and the analysis will be presented at the SCOT meeting next month. The LOST (Leaving Orthopaedic Surgical Training) Study has begun interviewing trainees who have left our profession to try and understand why. We are working closely with BOMSA (British Orthopaedic Medical Students Association) and BOTA to improve the perception of trauma and orthopaedics as a career option.
We are developing work streams on assessing and combating differential attainment and are very aware of the inequities in our examination systems for both conventional and non-conventional trainees: this needs to be addressed. We need to support our IMG and our SAS colleagues.
On the back of COP27, the BOA is keen to play its part in supporting the Green Surgery agenda and ensuring our systems are kind to the planet –another aspect that could be explored in projects for the President’s Prize for sustainable system change.
As 2022 draws to a close, I am looking forward to spending time with a bright and sparkly Xmas tree, family and friends. On behalf of all of us at the BOA I wish you all a merry Christmas and rest and relaxation over the festive season.
From the President
BOA Educational Courses

The BOA runs a wide range of courses under the Education Committee. These cater for the educational needs of a wide range of members (and non-members in some cases) at all stages of their careers.
These are in addition to the BOA Annual Congress, which is our largest learning opportunity, attracting around 2,000 delegates each year.
Courses includes SAS Professional Development Programme, Training Orthopaedic Trainers Course (V-TOTs) & Training Orthopaedic Educational Supervisors (V-TOES) Course & Law for Orthopaedic Surgeons.
Full details of all our courses can be found at www.boa.ac.uk/courses
Work on Registries
We are all aware of the benefits of registries and that good data, analysed by clinicians, supports the best patient care. Trauma and Orthopaedics has for many years led the way in the design and implementation of such registries.
The National Joint Registry is the largest orthopaedic registry in the world and a global exemplar with over 3.7 million procedure records recorded, and in trauma National Hip Fracture Database (NHFD) and Trauma Audit and Research Network (TARN) are widely accepted leaders. Over the past 10 years a further seven registries have been developed across the wider T&O specialty. The British Spine Registry, the National Ligament Registry (NLR), the UK Knee Osteotomy Registry (UKKOR), the Non-Arthroplasty Hip Register (NAHR), the Bone and Joint Infection Registry and audits led by BSSH and BOFAS.
In 2020, the Cumberlege Inquiry report, made strong recommendations on the importance of medical device information systems and how implants could be monitored and tracked across all surgical specialties. NHSE have since been working on the implementation of these recommendations and in particular a system where registry collection of implant data will be mandated by Government policy.
The BOA has been lobbying, alongside the NJR, to be ensure that clinicians remain at the heart of the development of any new systems. We have met with key stakeholders, and at the BOA Congress in September, Scott Pryde (NHSE) and Tim Briggs participated in a session to discuss these proposals and to consult with representatives from T&O registries.
We are awaiting (at the time of writing) further announcements from the Government with regards to the exact details of medical device level registry data collection, how data collection will be mandated and the governance structures overseeing it, but data collection will cover both trauma and elective. We have been assured that any new systems will build on the experience of the NJR and other exemplar registries as well as existing, scalable registry technology platforms.
We will keep you updated with developments via newsmails and member communications.
NICE Guideline on Osteoarthritis: Care and Management (Update)
The final guideline on Osteoarthritis: Care and Management (Update) has now been published on the NICE website, of which the BOA contributed to through stakeholder comments. You can read the full final guideline at www.nice.org.uk/guidance/ng226
BOA Archive
We are pleased to say that we have been working in partnership with the Borthwick Institute in York who are now host to the BOA archive, where it will be kept safe for future generations. Access to a list of archive contents can be found here: https://borthcat. york.ac.uk/index.php/boa and physical access can be arranged directly via the Borthwick Institute. We will be adding to BOA archive and hope to further develop it by digitising some content. We would like to thank Ian Stephen, Honorary BOA Archivist for all his hard work and support, and we hope that it will prove a useful research resource for all for years to come.
2022 BOA Medical Student Essay Prize
The BOA are pleased to announce the Medical Student Essay Prize title for 2023 will be ‘With the changing demographics and working practices within T&O, how can we sustain the work force and standards of care currently provided within the NHS?’
Submissions will open on 1st February 2023. Further information on the BOA Medical Student Essay Prize can be found www.boa.ac.uk/medical-student-essay The winning 2022 Medical Student Essay from Jan Drmota is featured on page 08.
The National Joint Registry 19th Annual Report

This is the formal public report of the registry for the period of 1st April 2021 to 31st March 2022. Registry data for the surgery that has taken place this past year, have again been analysed by expert statisticians and the results published with the continued aim of enhancing safety and improving clinical outcomes for the benefit of patients and the whole orthopaedic health care sector.
The report summarises our work and shares the analysis of data for the past year, visually in tables and graphs, for procedures across each of the joints, as well as implant and hospital outcomes and is downloadable from the NJR’s dedicated Annual Report website: https://reports.njrcentre.org.uk.
06 | JTO | Volume 10 | Issue 04 | December 2022 | boa.ac.uk
Latest News
BOA ORUK Research Fellows
The BOA and Orthopaedic Research UK are delighted to announce the second cycle of BOA ORUK joint Research Fellowships will be open for expressions of interest from 1st January 2023, closing 28th February. Two fellowships of up to £65k will be available for a project in any area of orthopaedics. Funding will be available for salary (maximum £60k) or as a stipend at UKRI levels. BOA Members at any trainee grade and SAS surgeons are invited to apply. To support diversity and inclusion within trauma and orthopaedics, we encourage applications from individuals that wish to undertake their research flexibly or less than full-time (minimum 0.5 FTE). For more information go to www.boa.ac.uk/researchfellowships.html
BOA Virtual Ortho Update 2023
Saturday 7th January, 8:30am - 5:00pm, Manchester
The Ortho Update brings together trauma and orthopaedic trainees at all stages of their postgraduate training, to prepare for their FRCS examination. The new face-to-face course format is a course of two halves. We are continuing with the popular critical condition CBDs, which this year will cover neurovascular injuries, compartment syndrome and physiological response to trauma. There will also be a new quick-fire trauma meeting called ‘The Good, the Bad and the Ugly’ which will look at basic science of trauma, biomechanics and complications.
The other half of the course will be practical simulation sessions. Each candidate will participate in a trauma moulage to fulfil the trauma resuscitation CEX. There will also be spinal trauma assessments that can be counted towards the ‘initial assessment and referral of spinal trauma’ critical condition.
To view the updated programme and book your place visit www.boa.ac.uk/OrthoUpdate for more information and how to register.
UK and Ireland In-Training Examination (UKITE)
More than 800 trainees from across the UK and Ireland are expected to take the UKITE Exam online between the 9th and 16th December. Since its inception in 2007, UKITE has helped trainees prepare for section 1 of the FRCS Tr and Orth with questions covering the full spectrum of sub-specialties, contributed by our volunteers. We would like to thank our tireless team of over 30 editors and subspecialty leads, and Ajay Malviya our clinical lead, for their tireless work. For any queries, or to get involved, please contact ukite@boa.ac.uk and further information on UKITE is available on the BOA website: www.boa.ac.uk/ukite
BOA Annual Congress 2023
- Save the Date!
Thank you to everyone for attending the BOA Annual Congress this September, we have received great feedback from our delegates, speaker and exhibitors.
Our next Annual Congress for 2023 is taking place in Liverpool on 19th – 22nd September, the programme will be created around the theme of ‘Sustainable Systems’. Keep a look out in the next few months for more information including abstract submissions on our website at www.boa.ac.uk/Congress
Thank you to all our exhibitors and sponsors for supporting the 2022 Annual Congress. For information regarding exhibiting and sponsorship at the 2023 Annual Congress, download the new Exhibitor and Sponsorship brochure at www.boa.ac.uk/sponsorship-brochure.
AGM Update
We were delighted to see so many of you at the AGM in Birmingham to hear updates on the BOA activities, finances for the previous year and to vote on key governance changes. We are pleased to report that the BOA remains in good financial health and that all resolutions for updating the Articles of Association and Rules were passed by a majority vote. These changes will allow the Association to properly function from a governance perspective and to facilitate more effective administration, we can also take better advantage of electronic meetings and voting so that we can enable members to engage with us in ways that make best use of time and resources.
JTO | Volume 10 | Issue 04 | December 2022 | boa.ac.uk | 07
Latest News
2022 BOA Medical Student Essay Prize Winner
Congratulations to Jan Drmota, winner of the 2022 Medical Student Essay prize for his essay on ‘How can we make Trauma & Orthopaedics in the UK more Eco-friendly?’.

Jan Drmota is a final year medical student at Imperial College London, originally from the Czech Republic. During his studies he has developed an interest in T&O and medical management consulting, particularly the application of technology in solving surgical and clinical challenges and in streamlining workflows. His winning essay is titled “EcoWolff’s law”: Identitybased Sustainable Adaptation of Trauma & Orthopaedics. Jan hopes his essay helps in adopting eco-friendly practices and further aids in developing frameworks for positive personal development and he would like to thank the BOA for receiving this award.
Essay Summary
The net zero NHS Carbon Footprint by 2040 pledge is a pressing challenge for Trauma and Orthopaedics, a key surgical specialty. Achieving any change on a personal level is extremely difficult: we find comfort in familiarity and the external environment always seems better suited for our status quo. Change becomes exponentially harder on a specialty-wide
level, particularly with sustainability as it requires overhauling everything from supply chains to operating room practices.
Inspired by self-help books and approaches of management consultancies, I propose an eco-friendly identity framework that can be applied across individual, hospital and national levels to better enable sustainability. By adopting eco-friendliness as a core pillar in T&O’s identity, sustainable practices will become second nature. In contrast to simply tracking performance indicators of managerial decisions, I believe the identity-based approach will be more meaningful to all T&O personnel and thus much more productive. The specialty will remodel by adapting to external pressures from policy-makers and contribute significantly to the national efforts.
You can read Jan’s winning essay on Orthopaedics Online at www.boa.ac.uk/O2 where we will be featuring the highest ranked essays throughout December.
BMA Pensions Information

The BMA have recently provided some advice to its members on recent government announcements that will impact on your pension. They are continuing to call for a tax unregistered scheme and an amendment to the Finance Act so that doctors and surgeons no longer pay a punitive rate of tax on their pensions savings. Some of the new government policies announced include: Correcting pension rules regarding inflation, encouraging NHS trusts to explore local solutions such as pension recycling, and implementing measures to allow experienced staff to return to service or stay in service longer. You can read their response to the new policies on their website at the following links:
BMA Response to the Government Announcements: http://bit.ly/3hQenZq
Further information from the BMA: http://bit.ly/3ECmK3K

08 | JTO | Volume 10 | Issue 04 | December 2022 | boa.ac.uk News
Jan Drmota receiving his award at 2022 Annual Congress









































































































British Orthopaedic Research Society (BORS) update
Andrew Phillips, BORS President
Following the online success of the 2020 and 2021 BORS (British Orthopaedic Research Society) annual meetings, 2022 saw a welcome return to in-person meetings, with BORS hosting the World Congress of Orthopaedic Research at the University of Edinburgh, on behalf of ICORS (the International Combined Orthopaedic Research Societies) in conjunction with EORS (the European Orthopaedic Research Society) and the AO Foundation. The combined meeting of orthopaedic research societies was launched in 1992 and has taken place every three years since then, with the eleventh meeting in Edinburgh being the first to be hosted by the British Orthopaedic Research Society. The meeting was held on 7th – 9th September 2022, with McEwan Hall providing an impressive backdrop for the plenary sessions. With six parallel sessions and almost 500 attendees, the conference provided ample opportunities for the diverse membership of BORS, and other orthopaedic research societies to catch-up with friends and colleagues as well as broadening their knowledge through attending sessions in unfamiliar research fields. Thanks go to the organising committees, and the Conference Chair, Professor Hamish Simpson.
As one of the host organisations, BORS organised several workshops, highlighting the diversity of their membership, which includes surgeons, scientists, engineers, veterinarians, and other allied health care professionals. The workshops included ‘How does joint loading influence pain and degeneration?’ with presentations from the past three BORS Presidents (Professors Mark Wilkinson (Sheffield), Richie Gill (Bath), and Debbie Mason (Cardiff)), chaired by the current BORS President (Dr Andrew Phillips); ‘Prevention of traumatic osteoarthritis’ featuring a keynote talk from Dr Fiona Watt (Imperial); and ‘Finite element modelling in orthopaedic research’, led by Professor Ruth Wilcox (Leeds). Clinical bridge sessions were also held by BORS in conjunction with the British Hip Society and the British Orthopaedic Foot & Ankle Society.
A separate online event is being arranged for the BORS 2022 awards. Dates and details for BORS 2023 will be available soon, while ICORS 2025 will be held in Adelaide, Australia, on 20th – 24th October 2025. Readers interested in joining the British Orthopaedic Research Society can apply on the website: www.borsoc.org.uk n

British Association for Surgery of the Knee (BASK) update
Murray, BASK Honorary Secretary
During 2022 BASK resumed a more normal service after the COVID lockdown years. The spring meeting for 2022 was in May at the ICC in Newport under the Presidency of Andrew Porteous. This was the first face-to-face meeting for many people as evidenced by the highest attendance at a BASK Spring Conference to date; there were instructional lectures, free papers, very popular industry sessions and of course the pre-BASK golf and for the first time crazy golf!
The BASK working groups have continued to work hard on behalf of the membership and for the whole UK knee community – with the patient at the forefront. BOASTs have been released from the BOA, following output from the relevant BASK working groups for the management of ACLs and patella dislocation, following the lead on the investigation and management of problematic and infected knee arthroplasty previously released. The Primary Knee Arthroplasty Working Groups and the Injury Prevention Groups are well on the way to their respective outputs. There is no doubt that we are living
and working in extra-ordinary times and the current pressure on both the trauma and planned care sectors is enormous. During this year the Major Revision networks went live – there are still some areas to iron out but the early feedback is very positive. This represents a new partnership with NHSE&I on low volume high complexity funding and organisation which is very likely to expand into other areas.
In September during the BOA Annual Congress at the ICC in Birmingham, the BASK specialty day saw the hand-over of presidency from Andrew Porteous to Professor Leela Biant – Professor Biant had also just delivered her King James VI Lecture – a great achievement indeed and

also becoming the first female President of BASK.
There is a undoubtedly a significant amount of development in biological knee surgery and this was well supported by Professors Elizaveta Kon (Humanitas University Milan) giving the Lorden Trickey Lecture in Newport and Tom Minas (Emeritus Professor Harvard and now the Paley Institute Florida) delivering the Adrian Henry in Birmingham. Our thanks go out to both of them for making the time to travel and for excellent lectures.
2023 will see a number of upcoming BASK executive posts, so please look out for the adverts through BASK membership email and apply if you want to get involved – if you are not a BASK member then why not consider joining? The BASK Annual Conference is free with your membership and in 2023 will be in London at Central Hall Westminster from 16th – 17th May. n
10 | JTO | Volume 10 | Issue 04 | December 2022 | boa.ac.uk
News
James
Professor Leela Biant receiving her King James VI Lecture award



































Imperial College London THE GREAT DEBATE CPD POINTS APPLIED FOR DAY ONE: KNEE DAY TWO: HIP FEE: £50 REGISTER NOW! WEDNESDAY 8TH & THURSDAY 9TH FEB 2023 1 WIMPOLE STREET, LONDON INTRODUCING A NEW CLASS OF INJECTABLE THERAPY TO TREAT KNEE OA iPAAG — SAFE AND SUSTAINED PAIN RELIEF WITH A SINGLE INJECTION2 www. Arthrosamid .com @ConturaLtd Contura-Orthopaedics-Ltd Contura Orthopaedics Ltd For more information, read the IFU for full details about Warnings and Precautions. The IFU is also available from https://www.arthrosamid.com or info@arthrosamid.com. References: 1 Bliddal H, Beier J, Hartkopp A, Conaghan PG, et
A
of Polyacrylamide Hydrogel Injection for Knee
2.
Hydrogel Injection for
Scan to see the new data that shows statistically significant reduction in pain maintained at 2 years.1 Reduces pain and increases mobility
www.mediuk.co.uk Tel: 01432 373 500 medi soft OA light knee brace osteoarthritis off-loading knee brace now available on prescription. Intended purpose: medi soft OA light is a knee brace for load relief.
al. (2022)
Prospective Study
Osteoarthritis: Results From 2 Years After Treatment. Poster presented at OARSI 2022;
Bliddal H, Overgaard A, Hartkopp A, Beier J, Conaghan PG, et al. (2021) Polyacrylamide
Knee Osteoarthritis: A 6 Months Prospective Study. J Orthop Res Ther 6: 1188. OUS/ARTHRO/NOV2022/116
medi. I feel better.
UK Prosthetic Joint Infection meeting – Glasgow April 1st 2022
The Grand Central Hotel in Glasgow welcomed orthopaedic surgeons, microbiologists and scientists to the fourth UK PJI meeting. This year we were joined by our trauma specialists for break-out sessions on fracture related infections, while a parallel session on arthroplasty infection was held.

Delegates had the opportunity to review the draft BOASTs for ‘managing native joint infection’ and ‘managing PJI for on call surgeons’ developed in collaboration with the BOA, BASK, BHS, BOFAS and BESS, and presented by Andrew Toms. Rhidian Morgan-Jones was able to provide us with insight into ‘what is required to be an infection revision surgeon’, and Ley Jeys explained how dual operating for complex cases is now standard practice at ROH.
Exeter’s Amy Cudmore, Revision Knee Nurse Specialist discussed how to manage the ‘leaky wound’. Thank you very much to Bilal Jamal, Dominic Meek and David Shields for organising a great meeting. The next UKPJI meeting is being planned to be held at Sandy Park in Exeter, Devon from 15th – 16th June, 2023. For further meeting information please contact Clockwork Medical at: david@clockwork-uk.com At the 2023 meeting, we will be encouraging our colleagues outside from the hip and knee world to join us to learn together how to manage complex infection cases. Our keynote lecture will be on the future of phage therapy to treat infection, a technology that could become a game-changer in infection management.
We hope to see you all in Devon in June 2023. n
BOA and Postgraduate Orthopaedics sponsored travelling fellowship
to Hôpital de la Tour, Geneva and ICR Locomoteur & Sport Clinic, Nice
Figure 1:
Iam indebted to the BOA and Postgraduate Orthopaedics for awarding me this travelling fellowship which allowed me the opportunity to work with two highly-respected consultants in the field of shoulder and elbow surgery.
I started the fellowship by visiting Dr Alexandre Lädermann, who I met at the London Shoulder Meeting earlier this year, at Hôpital de la Tour in Geneva where his practice is impressively geared towards research with patients completing multiple outcome scores and being enrolled into various studies. Perhaps the most striking evidence of his aggressive post-operative rehabilitation was seeing patients who were six weeks following open Latarjet doing full push ups in clinic.
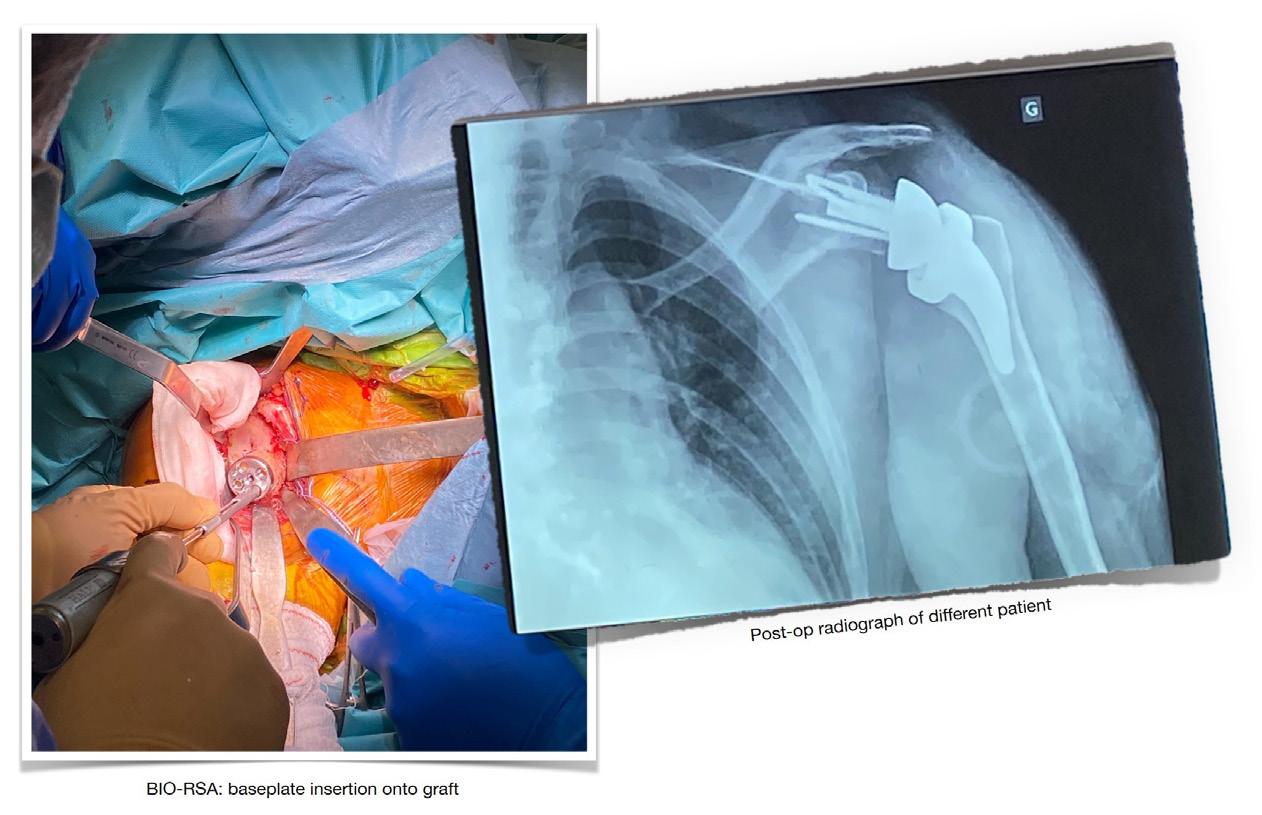
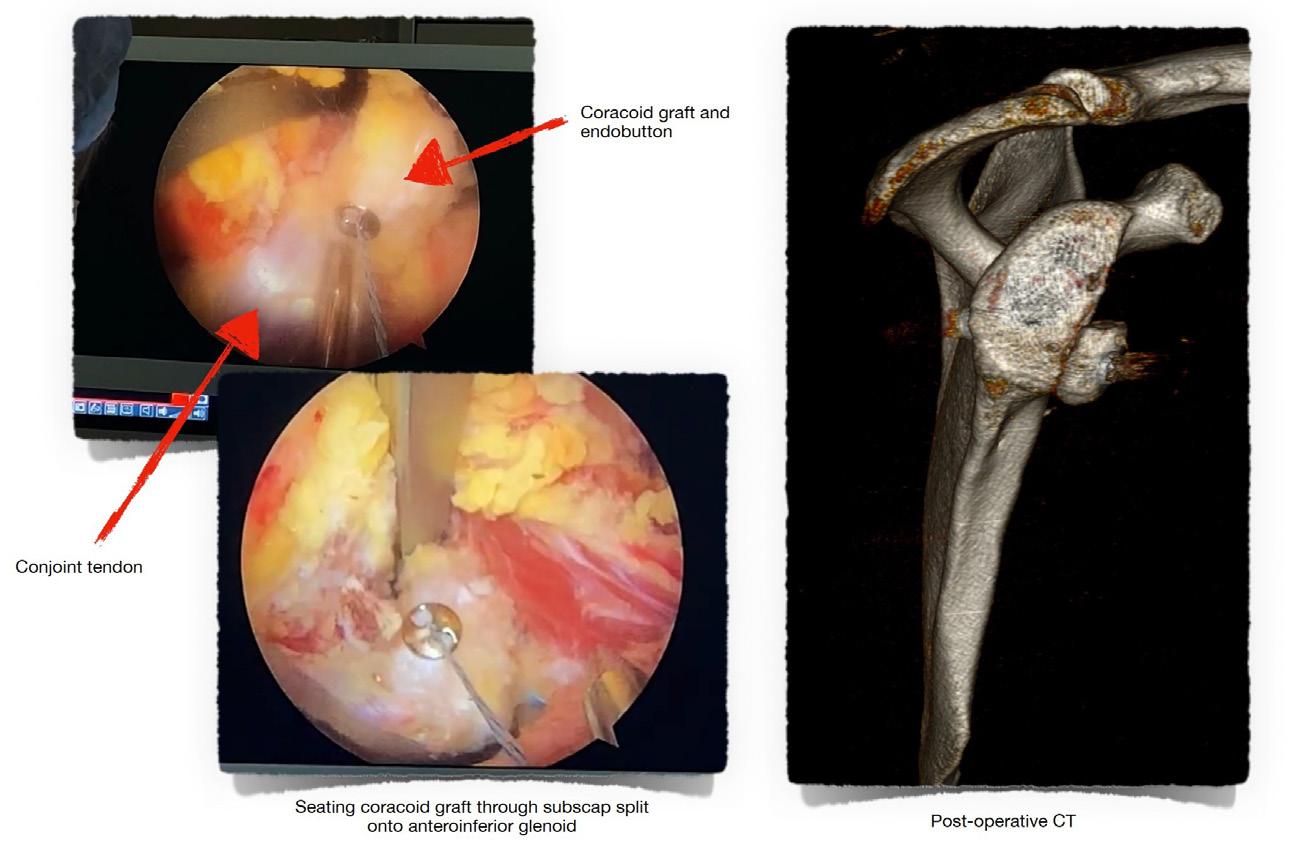
I then travelled to Nice, where I worked with the world-renowned Professor Pascal Boileau at the Institut de Chirurgie Réparatrice (ICR) Locomoteur & Sport Clinic. He was previously the Head of Trauma and Orthopaedic Surgery in Nice, and has been at the forefront of innovation in shoulder surgery. To witness arthroscopic Latarjet (Figure 1) being performed by one of its pioneers was a brilliant experience. I was also able to observe a bony increased-offset reverse shoulder arthroplasty (BIO-RSA) (Figure 2), a technique which Professor Boileau pioneered.
I have learned a great deal from observing and assisting these highly-skilled surgeons in both the clinic and theatre environments, and the tips and techniques, philosophies and analogies discussed, will no doubt be invaluable to my future practice as an upper limb surgeon.
I had a thoroughly enjoyable and rewarding time undertaking this fellowship and would like to express my gratitude to both the BOA and Postgraduate Orthopaedics for this unique opportunity. n
Figure 2:
12 | JTO | Volume 10 | Issue 04 | December 2022 | boa.ac.uk News
Delukshan Srikantharajah
Jon Phillips
Grand Central Hotel, Glasgow










TITANIC CENTRE BELFAST 23 & 24 MARCH 2023 CPD POINTS APPLIED FOR BOOKINGS NOW OPEN EARLY BIRD RATE UNTIL THE 11TH FEBRUARY 2023 Contact us today sales@aneticaid com +44 (0)1943 878647 aneticaid.com The one-device approach to transport, treatment and recovery. Affordable private diagnostic imaging Why refer to Oryon Imaging? MRI from £250 Ultrasound from £265 X-ray from £55 DEXA from £95 Contact us: 020 7042 1888 imaging@oryon.co.uk Located in central London Scan me to find out more Same day appointments Open 7 days a week Results in one day 96% perfect imaging quality achieved CQC inspection rating good IEP and Connect immediate access to results Oryon_190x130mm_BOA_final.indd 1 07/11/2022 10:15
2022 BOA Congress Review
Fergal Monsell, BOA Honorary Secretary
Iwrite with delight and relief in approximately equal measure to report that the 2022 BOA Congress was an unqualified success. Whilst the long tail of the pandemic continues to affect us all on a daily basis, we had sufficient manoeuvrability to deliver an ‘old style’ event. We are still collating the feedback but prima facie, this has been universally complimentary and is due to the herculean efforts of Charlie Silva, Venease Morgan, Anna Prunty and the wider team. Our partners in industry have also been accommodating and flexible and with a little bit of imagination, we were able to be sufficiently nimble to deliver all aspects of a traditional BOA Congress. The behind-the-scenes work, which is required for an event of this size is colossal and I am grateful to Simon Hodkinson for completing a large part of it, and the organisation was already at an advanced stage
when I became involved in January.
We were returning to a familiar venue at the International Convention Centre in Birmingham with excellent transportation links, accessibility and a city centre location, which accommodated a wide variety of extracurricular activities. The timing coincided with a major urban face lift that had been undertaken for the recent Commonwealth Games and the most visible mascot of this event, a large metal bull, remained in residence until the last day of our Congress.
There were approximately 2,000 delegates for the main section of the Congress, which was punctuated with excellent scientific content. The theme was ‘Technology, data and recovery’ with a Presidential guest lecture delivered by Professor Berry considering the introduction

of new technology with lessons from joint arthroplasty and relevance to the coming digital instrumentation revolution. Plenary sessions included ‘The vision, the opportunity and the reality’ and ‘The Big Studies 2022’, with both sessions attracting more than 800 delegates. There was a slight reduction in the number of free papers, which may be a legacy effect of COVID but nevertheless, we were able to combine where necessary and deliver sessions with top quality educational content.

Our engagement with industry is fundamentally important to the success of this event and 81 companies exhibited, occupying 20% more exhibition space than the previous event in Aberdeen. Industry feedback has also been very positive, with 80% describing this year’s Congress as either an excellent or good event and 85% have already expressed a wish to attend next year.

For those that were unable to attend in person or who faced the dilemma of choosing between simultaneous sessions, all content is available on the BOA website and can be viewed at leisure. Delegates have exclusive access to this material for a period of three months and following this, it will be made more widely available on a number of digital media outlets.
After a short break, we are already planning for the 2023 Congress with a theme of ‘Sustainable Systems’ and hope that you will be able to join us 19th – 22nd September at the ACC, Liverpool. n

14 | JTO | Volume 10 | Issue 04 | December 2022 | boa.ac.uk
News












CPD POINTS APPLIED FOR PatelloFemoral Masterclass POWER OF THE PAST FORCE OF THE FUTURE SAVE THE DATE! THURSDAY 27TH & FRIDAY 28TH APRIL 2023 EDGBASTON PARK HOTEL BIRMINGHAM
Awards and Medals
Congratulations to our Congress prize winners! It was wonderful to be able to celebrate the fantastic achievements of our members with our Awards and Medals session at Congress in Birmingham.
The Best of the Best Certificate went to Alistair Mayne representing the Northern Ireland region – for their talk on “The feasibility of achieving Elective Care Framework targets for Total Hip Arthroplasty (THA) and Total Knee Arthroplasty (TKA) in Northern Ireland”.

The Medical Student Podium Prize winner was Sophie Heppenstall for their presentation “Exploring the association between DXA-derived hip geometric measures and hip osteoarthritis: findings from 40,000 individuals”.
Karola Pawloy was the winner of the Best Poster Prize with “No difference in risk for revision due to deep infection between clindamycin and cephalosporins in cemented primary total knee replacements. A report from The Norwegian Arthroplasty Register 2005-2019”.


We extend our congratulations to Kalpesh Vaghela, winner of the Robert Jones essay prize and medal; and Jan Drmota, winner of the medical students’ essay prize.
Thank you to all our exhibitors who supported us to help make Congress happen. The winner of the Exhibitors Cup for Best Large Stand was Stryker UK and the Exhibitors Plaque for Best Compact Stand went to JRI Orthopaedics n
16 | JTO | Volume 10 | Issue 04 | December 2022 | boa.ac.uk
News
Karola Pawloy
41st Annual Meeting of the European Bone and Joint Infection Society EBJIS2023 #EBJIS2023 www.ebjis2023.org Submit your abstract now! Save the date 12 -14 October 2023 · Basel · Switzerland Important dates Abstract submission deadline: 12 April 2023 Early registration deadline: 1 July 2023
Alistair Mayne

















surgical education: From the
to the
and beyond... The world’s most detailed and accurate 3D reconstruction of human anatomy Visit primalpictures.com to learn more about our catalogue of interactive learning tools, created from real body scans and imaging data – bringing the Primado2 NSK SURGICAL FEEL THE DIFFERENCE nsksurgical @NSK_Surgical nsk.surgical Call us on 0800 6341909 or visit nsk-surgery.co.uk BASK 2 23 16-17 MAY CENTRAL HALL WESTMINSTER LONDON WWW.BASKMEETING.COM COMBINED WITH COKS
Supporting
hand
wrist
New BOA Trustees ( 2023 – 2025)
Paul Banaszkiewicz
Paul graduated from Glasgow University, completing his basic SHO surgical training in the Merseyside Deanery and then undertook specialist registrar training on the North East of Scotland training programme. He was appointed as Hip and Knee arthroplasty surgeon at Queen Elizabeth hospital Gateshead in 2004.

He is passionate about training and medical education being a fellow of Higher Education Academy, fellow Academy of Medical Educators and has a Master’s degree in Medical Education.
He is an RCSEng member for the appointments accreditation committee (AAC) and RCSEng quality assurance and accreditation assessor for courses seeking RCSEng course accreditation.
Paul is visiting professor at Northumbria University this role acts as an interface between the academic roles Northumbria University provides and his own clinical oriented background that provides a practical focus for research.
He has been a strong supporter of the BOA Futures Leadership Programme and the BOA annual Travelling Fellowships. He is a keen supporter of BOTA being regularly involved with their annual instructional course and sponsor of BOTA travelling fellowships.
Paul is the main editor and author for three FRCS (Tr&Orth) related exam books that are international best sellers and have won several BMA book awards. He co-ordinates an annual six-day intensive FRCS (Tr&Orth) revision course at Newcastle. In recent years Paul has run its international equivalent for overseas trainees with courses taking place in Dubai, India, Singapore and Jordan.
For many years Paul was involved in humanitarian work in Northern Iraq regularly visiting the region to undertake neglected hip and knee arthroplasty surgery. This gave him a greater appreciation and understanding of our own health care system. Many patients would have continued to struggle due to a lack of local expertise and resources to pay for expensive surgery.
Through the contacts he has made overseas Paul is keen to develop the international profile of the BOA.
In his spare time, Paul is a keen runner, skier, gardener and Burnley FC fan. n
Andrew Manktelow
Andrew trained at the Royal Free and RNOH before moving to Nottingham in 1999. As part of a busy trauma group for many years, his practice is now based around hip surgery. His clinical interest in hip and hip revision surgery started in London and developed during a year in Boston, at MGH. The scope of his unit provides an understanding of the issues that confront all orthopaedic practice. Andrew has been Head of Service for Elective Orthopaedics at NUH since 2019.
Andrew’s clinical work provides research opportunities and forms the basis of his educational activities. He travels widely to demonstrate and discuss his practice. Andrew set up the Nottingham Revision Course in 2007. Recently, work with the East Midlands Specialist Orthopaedic Network (EMSON) has received attention nationally and internationally.
Andrew was President of the British Hip Society between 2018 – 2019, and was elected a Trustee on the BOA Council in 2019. Sitting on the Orthopaedic Committee and reporting on PHIN and FIPO, he has really enjoyed his role. Andrew is delighted to have been re-elected to Council this year and is very keen to further his contribution, specifically to review how the BOA can support colleagues on issues relevant within the Independent Sector.
Married to Claire, a GP and with four beautiful and tolerant daughters, Andrew has little time to spare away from my work. When quiet, he enjoys travelling, music, gardening, (watching) sport and planning future revisions. Encouraged to submit a less formal picture, Andrew chose a ‘stylish’ image taken while wandering around Petra in Jordan, a place he hugely recommends to offset the stress of a busy orthopaedic life. n
18 | JTO | Volume 10 | Issue 04 | December 2022 | boa.ac.uk News
Andrea Sott
Andrea Sott is working as a Trauma and Orthopaedic Consultant at Epsom & St Helier NHS Trust and the South West London Elective Orthopaedic Centre SWLEOC since 2004.
Andrea leads her Trust’s large planned Care division as Medical Director and is Surgical Director at SWLEOC. In all her roles she strongly promotes excellent surgical care and senior clinical leadership to continuously improve services for our patients.
As a leader Andrea has been instrumental in achieving national top performance in hip fracture care, MSK elective recovery and patient waiting times providing mutual aid to more challenged UK regions.
Andrea maintains a GMC portfolio as an active and enthusiastic Trainer. She is Senior Examiner for the JCIE, past Surgical Tutor and current AAC panel member for the Royal College of Surgeons of England, continuously inspiring students, trainees and colleagues to take up professional and leadership roles in Trauma and Orthopaedic Surgery. Andrea is host to a well-established BOA Future Leaders Programme CCT F&A fellowship and has been invited as director/faculty to several BOFAS and BOA courses and meetings.
She has published many papers in her field. As member of the SWL executive R&D committee, she oversees several NIHR studies some as PI, advocating evidence-based surgery at all times.
Married to Simon with three children, Andrea enjoys a busy family life, running, paddle boarding, boating and baking with their own chicken’s eggs.
As the only female surgeon at SWLEOC she is keen demonstrate that a flourishing orthopaedic career, senior leadership positions and happy fulfilling family life are indeed achievable to all.
Grateful to the voting members Andrea wants to bring to the BOA Council her considerable surgical, professional and leadership experience, and strong work ethics to which ever position is allocated to her, promoting diversity and sustainability in surgery. n
New Honorary Treasurer
Ian McNab
Ian McNab trained at the London Hospital Medical College and then as an SHO in London, Sussex and Oxford. His higher orthopaedic surgical training was on the Pott rotation, based on St Bartholomew’s and the Royal London Hospitals. It spanned the transition into SpR training and he was ‘the last SR’! He undertook hand and upper limb fellowship training in Oxford and then during a year in Melbourne.
He was appointed in 2000 as a Consultant Hand Surgeon at the Oxford University Hospitals Trust. He works in an excellent integrated team of thirteen T&O and Plastics hand consultants and closely with other T&O colleagues.
He has a keen interest in teaching, as an Honorary Senior Clinical Lecturer in the University of Oxford, and as Head of the Oxford Hand Fellowship Programme. He has served on the Training Interface Group for Hand Surgery, on the UK Hand Diploma Committee, as a Diploma examiner and as past chair of the AOUK Hand & Wrist Courses. In 2007 he was awarded and undertook the prestigious BSSH Stack Travelling Fellowship in New Zealand, Australia, Singapore and USA.

Ian has also served on: the BOA Board of Specialist Societies, Professional Practice, Education, Trauma and Research Committees; BOA Council (2014-25) and as BOA Honorary Treasurer (2022-25); as RCS/BOA Regional Specialty Professional Adviser (proposing the motions at the 2014 RCS EGM on Health & Social Care Act); the BSSH Research & Audit, Diploma, Instructional Course and Trauma Committees, BSSH Council (2009-12 & 2017-25), BSSH Honorary Secretary (2020-25); as BMA LNC Chair, Regional & National Consultant Committees, Chair BMA Orthopaedic Sub-Committee and as BMA T&O Subspecialty Lead (2019-24).
Ian’s wife Frances is a consultant anaesthetist – with an interest in acute pain (management)! Previously he enjoyed rowing and mountaineering but now usually undertakes more gentle travel, navigational car rallies and hill-walking.
He believes the BOA must continue to develop strong leadership, with pro-active policies and actions, and to work collaboratively with other bodies, to improve T&O services and training amongst the maelstrom of NHS changes and challenges – he will focus his energies and experience on helping the BOA to deliver. n
JTO | Volume 10 | Issue 04 | December 2022 | boa.ac.uk | 19 News
Joint Action Update


TCS London Marathon 2022


Congratulations to our fabulous London Marathon runners! On Sunday 2nd October, Imran Ahmed, Alex Chipperfield, Tim Davies, Robert Gregory, William Paton, Richard Secular and Ben Skinner completed the 26.2 mile challenge around the iconic London Marathon course. Their amazing efforts have raised £13,000 for Joint Action to support vital research on orthopaedics. If you would like to show your support for their fantastic achievement please donate by selecting either of the donation links on our page at www.boa.ac.uk/London-marathon


All our runners had a fantastic day and have shared some great photos of their experience. Hopefully these will inspire you to think about setting yourself a challenge and raising funds for Joint Action. The BOA’s London Marathon places for 2023 have already been filled but if you have set yourself a challenge or have your own place for the marathon in 2023, please consider running for Joint Action.

You can contact us at jointaction@boa.ac.uk

2023 RideLondon - Essex

The BOA do not have any charity places available this year for the 2023 RideLondon-Essex but you can still get involved. If you have been lucky enough to secure your own place through the ballot, we would love for you to ride and raise money and awareness for Joint Action. You will receive the same support as a charity place participant but there is no fundraising target, we simply ask that you raise as much as you can. All funds raised will support research into musculoskeletal disorders and any and all support is most welcome.
Please contact us at jointaction@boa.ac.uk for further information.
20 | JTO | Volume 10 | Issue 04 | December 2022 | boa.ac.uk
News
Alex Chipperfield
q Ben Skinner with a 6 foot high model of the tree on Andry which he carried on his back!
p Tim Davies and Richard Secular
t William Paton
Robert Gregory
Conference Listing 2023:
BHS (British Hip Society) www.britishhipsociety.com 08-10 March 2023, Edinburgh
BOFAS (The British Orthopaedic Foot and Ankle Society) www.bofas.org.uk 08-10 March 2023, Liverpool
BSCOS (British Society for Children’s Orthopaedic Surgery) www.bscos.org.uk 09-10 March 2023, Southampton
BLRS (British Limb Reconstruction Society) www.blrs.org.uk 23-24 March 2023, Belfast
BRITSPINE 2023 Scottish Event Campus (SEC) Centre, Glasgow 18-20 April 2023

p BRITSPINE 2023 www.BritSpine.com

18-20 April 2023, Glasgow
BASK (British Association for Surgery of the Knee) www.baskonline.com 16-17 May 2023, London
OTS (Orthopaedic Trauma Society) www.orthopaedictrauma.org.uk 25-26 May 2023, Edinburgh
BESS (British Elbow and Shoulder Society) www.bess.ac.uk 27-30 June 2023, Newport
UKPJI (UK Prosthetic Joint Infection) www.ukpji.com 15-16 June 2023, Exeter
BIOS (British Indian Orthopaedic Society) www.britishindianorthopaedicsociety.org.uk 07-08 July 2023, Windsor
BOA (British Orthopaedic Association) www.boa.ac.uk 19-22 September 2023, Liverpool
BOSTAA (British Orthopaedic Sports Trauma and Arthroscopy Association) www.bostaa.ac.uk 09 November 2023, London
JTO | Volume 10 | Issue 04 | December 2022 | boa.ac.uk | 21
BSSH (The British Society for Surgery of the Hand) www.bssh.ac.uk 22-24 November 2023, Glasgow News
Immersive virtual reality for surgical training in trauma and orthopaedic surgery
Thomas Lewis, Mark Bowditch, Wathik El-Alami, Diane Back and Adil Ajuied
Thomas Lewis is an ST7 trainee from South East Thames. He has a strong research background with peer reviewed publications, international and national presentations spanning research projects in surgery, anatomy, surgical education and mobile health. He is the regional virtual reality lead for the South East Thames Deanery.
Surgical training is widely acknowledged to be vitally important to maintain the surgical workforce of the future. Delivering surgical training in the modern NHS is technically challenging due to numerous factors including access to training opportunities, balancing service commitments, theatre pressures, all of which have been exacerbated by the COVID pandemic1-3. Simulation, technical instructional courses offer trauma and orthopaedic surgery trainees the opportunity to develop their technical and non-technical surgical skills4-9
What is surgical simulation?

Surgical simulation comes in multiple modalities ranging from simple low fidelity simulation such as sawbones tutorials, through detailed procedures specific computerised simulators, all the way to cadaveric laboratory-based simulation. A more recent development is that of procedure specific virtual reality surgical simulation, allowing a more immersive experience. Recent studies have suggested that the use of virtual reality (VR) during the training of orthopaedic surgery residents improves surgical performance4-6,10-11
Virtual reality in surgical training
Integrating VR into surgical training has a number of advantages as shown in Table 1. Trainees have the opportunity to review and practice the procedural steps of an operation prior to attending a real world operating theatre. The most important aspect of VR in surgical simulation is that trainees can learn the ordered steps of a surgical procedure (the work-flow), in a safe and self-directed fashion. Trainees can also gain familiarity with the theatre environment setup, instruments and develop their situational awareness and non-technical skills managing a procedure all without placing patients at risk12
At present, most surgical VR modules are quite didactic in their workflow structure, but as they evolve and become more sophisticated, alterative surgical techniques and strategies will become options within individual modules, as will intra-operative complications and their management.

Mark Bowditch is a Consultant and Divisional Clinical Director for MSK & surgical specialties at the East Suffolk and North Essex NHS Foundation Trust. Mark’s specialist interests are in surgery of the knee and all levels of surgical education and he is currently the Head of School of Surgery in the East of England.
What exactly is VR? VR utilises readily available hardware, this consists of three main components; firstly a headset, which incorporates stereoscopic visualisation, microphones, accelerometers, speakers and enables users to experience a 3-dimensional computer-generated multisensory environment which responds to their head and body movements. The second component are two handsets which contain accelerometers and control buttons and joysticks. These are used to interact and manipulate with the virtual world. Lastly, the third component is that of a very intricate and sophisticated software package that describes the VR environment, and how you will interact with it.
For many years surgical institutions and Surgeons, have been compared to pilots and the wider aviation industry respectively. We have sought and adopted within surgery insights and best practice from aviation around safety, and standardisation of processes. Examples of this include the WHO checklist, the no-blame culture, and the right to speak up. VR surgical simulation, allows us to draw another parallel with the aviation industry, where all commercial and much civil aviation transitions from the class room through flight-simulators, before getting to real world flight. Indeed, commercial pilots, frequently return to the flight-simulator for re-licencing assessments, upskilling, and to train others.
VR will never replace the real world haptic feedback of actual tissue handling as it cannot
Features
22 | JTO | Volume 10 | Issue 04 | December 2022 | boa.ac.uk
Wathik El-Alami is a Consultant Trauma and Orthopaedic surgeon at Guy’s and St Thomas’ NHS Foundation Trust. He is the Director of Medical Education and has a keen interest in utilising technology and simulation for improving medical education.


Diane Back is a Consultant Trauma and Orthopaedic surgeon at Guy’s and St Thomas’ NHS Foundation Trust. She is the Training Programme Director of South East Thames and is passionate about improving training.
Advantages
Can perform procedures in risk-free environment
Accessibility and availability of virtual theatre environment not limited regardless of external factors e.g. geography or time
Opportunity for trainees to focus on operative competence and skills in a consistent manner
Simulate and develop non-technical human factors skills through interaction with other multi-disciplinary team members
Develop knowledge of technical procedural skills for an operation prior to theatre
Regular assessment and feedback on technical performance Scenarios can be adjusted for different skill levels
Improved accessibility to regional training opportunities as can join virtual lecture theatres and breakout rooms independent of geography (for both trainees and trainers)
Immersive simulated environment compared to other simulation techniques
Disadvantages
Lack of tissue handling and haptic feedback
Limited modules currently available
Cost of hardware and ongoing software licences
Hardware and software limitations e.g. resolution, model freedom, instrumentation
Adil Ajuied has worked as a Consultant at Guy’s and St Thomas’ Hospitals since 2009 and specialises in all aspects of knee surgery. He completed a postgraduate Masters’ degree, and has been appointed a Senior Honorary Clinical Lecturer in Trauma and Orthopaedics as well as Director of Education for South London Orthopaedics. He has served as an executive board member of BASK, and Associate Editor of the Knee Journal, as well as convening scores of educational and instructional courses. He has a strong interest in how new technologies and innovations can be leveraged to enhance training and ultimately patient outcomes.
recreate the muscle memory that comes from handling and operating on actual tissue, however we believe it can improve the efficiency of surgical education and maximise the learning opportunity that can be gained from that ever-dwindling training resource, time in theatre13
There are also advantages to integrating VR into medical training unrelated to the development of technical and non-technical skills. There are no geographical restrictions so trainees and trainers can collaborate in the same VR physical environment, while being geographically remote.


Putting VR to the test
At the beginning of August 2022, we held a virtual reality surgical education day for trainees across south London in order to explore the utility of virtual reality for surgical training. The day consisted of lectures delivered within a VR lecture theatre to a large auditorium of delegates, before each entering their own individual operating theatre to perform two different surgical procedures. Each trainee performed a therapeutic hip arthroscopy for femora-acetabular impingement and an anterior cruciate ligament reconstruction (Figure 1 & 2). >>
Features
Table 1: Advantages and disadvantages of virtual reality in trauma and orthopaedic surgery surgical training.
JTO | Volume 10 | Issue 04 | December 2022 | boa.ac.uk | 23
Figure 1 & 2: Photograph of delegate using virtual reality headset and controllers to perform simulated procedures in a virtual operating theatre environment.
Each trainee had 1:1 consultant supervision in their individual theatre (Figure 3) and were able to receive targeted feedback and teaching regarding each step of the procedure.
The feedback from the trainees was universally positive as demonstrated in Figure 4. Trainees reported that the simulated theatres felt ‘realistic’ and offered the opportunity to take time to understand the steps of a procedure prior to theatre. Multiple trainees reported that the structured work-flow within the simulation module aided them in understanding the critical steps of the procedure’s set up and execution, that become intuitive for the experienced trainer and hence may often be skimmed over or purely taught.
VR allowed trainees access to information and training opportunities that they would otherwise never have the opportunity to see, such as to explant a him with femoral acetabular impingement before, mid and post cam resection, assessing the bony architecture of the pathology and it’s real time response to surgical intervention.
Other benefits reported by the trainees included, feeling that they would require less real world training cases to gain competence in a particular procedure (flattening the learning curve), the opportunity to ‘familiarise with operations that are done rarely’ and and ‘improve understanding of surgical instrumentation’. The virtual reality modules recorded technical data which provided each trainee with immediate feedback on their progress and helped them identify areas of development for future cases. 94% of attendees felt that virtual reality training should be incorporated into their current surgical training programme.
“[Virtual reality] would allow for much greater exposure to the routine of surgical procedures. Significantly limited opportunities at the moment therefore this would be a vital way to bridge the gap. Feels like undoubtedly the future of training.”

Is VR training effective?
The evidence base for VR simulation in trauma and orthopaedic surgery is relatively limited with VR yet to be broadly incorporated into surgical training. A number of recent systematic reviews of VR surgical simulation
in orthopaedics have found VR simulators are excellent tools for improving surgical training and skills acquisition4-8,14. Metrics for surgical skill that were studied included mean time and accuracy to perform an operation, instrument handling, implant placement, knowledge of procedural steps and efficiency of movement. There are a number of randomised control trials, across a number of orthopaedic subspecialties, which demonstrated that VR can improve surgical skills acquisition, especially in comparison to non-VR training simulation methods. Although the results and potential applications of VR are encouraging there are a number of important limitations. The most important of these is the lack of methodologically robust high quality, large-scale studies with long follow-up periods.
A number of studies assessing trainee attitudes to virtual reality for surgical education have found encouraging results in terms of enjoyment, utility and efficacy, when compared to more traditional teaching methods. Trainees reported they saw a role for VR in surgical training, particularly during the early phases of training where operative opportunities were increasingly limited. There is emerging evidence of construct validity and transferability of VR acquired skills to the real world operating theatre environment4-7,14-15 however further research is certainly needed in this area. Virtual reality simulation is potentially more effective than traditional simulation methods and may help mitigate surgical skill decay by providing additional opportunities to refresh knowledge prior to attending theatre16. Skill acquisition and retention is particularly important in surgical

Features
Figure 3: Screenshot demonstrating an operating surgeon teaching other surgeons in a virtual reality operating theatre.
24 | JTO | Volume 10 | Issue 04 | December 2022 | boa.ac.uk
Figure 4: Participant responses following virtual reality surgical training day (0 (worst response) - 10 (best response).
training as the nature of rotational sub-speciality-based placements mean that it is possible to deskill without regular refreshment of cognitive and manual skills. Complex cognitive and technical skills decay rapidly compared to simple tasks with interval task iteration shown to be an effective means of maintaining competence. VR may have a valuable role to play in allowing safe and convenient skill updating, alongside objective VR procedure specific metrics.
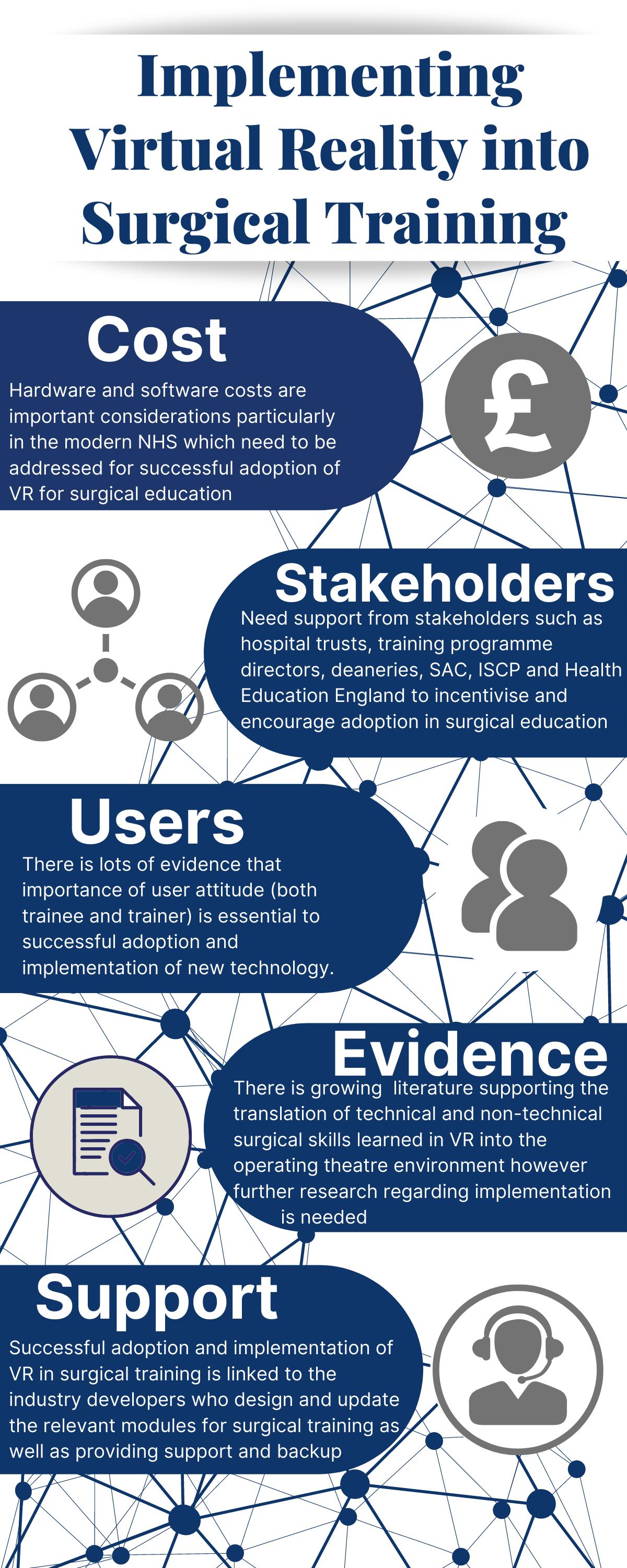
Constraints to implementation
There are current barriers to implementation of virtual reality of which the greatest is cost and accessibility of hardware and associated software (Figure 5)17. However, given the current pressures on surgical training, alternative strategies to enhance training and education such as virtual reality may play an integral role in training. General challenges to adoption of virtual reality technology include reduced face-to-face communications, cost limitations (in terms of hardware and ongoing software licences), educational, and users’ attitude. There are also specific challenges that need to be addressed for successful implementation. These include ensuring support from relevant stakeholders such as Health Education England, SAC, JCST, ISCP, local TPD’s, deaneries and hospital trusts. Given the limited time available for surgical training, integrating VR into training may come at the expense of other training opportunities such as regional teaching days so this needs to be considered. One major barrier is the limited evidence base to support the transferability of technical and non-technical skills from VR training to real-life hospital environments. Finally, as with any new technology, additional support in terms of hardware and availability of software modules will be seen as key to implementation.
The potential for virtual reality extends beyond surgical training to the wider theatre team. We have piloted a proof of concept MDT collaborative simulation by virtually performing a case with an anaesthetist, scrub nurses, circulating staff and other theatre members all in one theatre. This has many future applications to focus on non-technical skills such as human factors and communication in theatre as well as simulation of critical scenarios without placing patients at risk or using real world resources18
Conclusion
In summary, immersive virtual reality has great potential to positively improve surgical training by allowing trainees to develop their technical and non-technical skills in a range of scenarios without placing patients at risk and improving the efficiency of learning when physically in theatre. There are a number of barriers to implementation that may limit the adoption of virtual reality into surgical training and future research should focus on evaluating the transferability of technical and non-technical skills developed in VR to the real operating theatre environment. n References
References can be found online at: www.boa.ac.uk/publications/JTO
Figure 5: Key themes identified related to implementation of virtual reality into surgical training
Features JTO | Volume 10 | Issue 04 | December 2022 | boa.ac.uk | 25
“VR can improve the efficiency of surgical education and maximise the learning opportunity that can be gained from that ever-dwindling training resource... time in theatre.”
Introducing the British Orthopaedic Medical Students Association (BOMSA)
 Sulaiman Uppal
Sulaiman Uppal
Sulaiman Uppal is a medical school student at Oxford University. Sully has been Medical Student Representative on the BOA Education and Careers Committee and the BOA Representative on the BOMSA Executive Committee.

Comprising more than 95% of UK medical schools and overseen by a national body of students and junior doctors, BOMSA aims to enhance medical students’ exposure to Trauma and Orthopaedic (T&O) surgery from a grassroots level.
The society stands alongside BOA and BOTA to support aspiring orthopaedic surgeons. The Committee itself is made up of two local representatives from each medical school. Each of the regions are headed by a regional lead, with oversight from a National Committee that works hand-in-hand with BOA, BOTA and its subsidiaries to disseminate the aims and objectives of these organisations to the medical student audience.

Despite the significant amount of musculoskeletal conditions accounting for A&E and primary care attendances, we’re all aware of the small amount of undergraduate teaching that is dedicated to T&O. Instead, a lot of exposure comes from the fantastic initiatives ran by orthopaedic and surgical societies all over the UK. BOMSA aims to centralise and orchestrate such endeavours to provide greater learning, mentorship and research opportunities to aspiring orthopaedic surgeons over the UK than ever before.
Our core values of diversity, equality and inclusivity have been at the heart of our organisational process and we are proud to champion these at the grassroots level.
Features
The BOA Annual Congress marks the end of the first tenure for the newly founded British Orthopaedic Medical Students Association (BOMSA).
26 | JTO | Volume 10 | Issue 04 | December 2022 | boa.ac.uk
BOMSA Committee.
The BOMSA network has been working tirelessly over this past year, supporting our regions to develop and deliver valuable events across the UK. In total, over 50 virtual teaching sessions were delivered across the BOMSA regions, with over 800 medical students tuning in. BOMSA South West and South East both delivered popular orthopaedic teaching series that attracted nearly 250 students between them. We are particularly proud of our BOMSA London division, who teamed up with the Royal National Orthopaedic Hospital to enrol 50 medical students in a successful mentorship scheme that matched them each with their own specialty registrar contact. This gave them the opportunity to not only gain valuable career advice, but to also participate in research projects. BOMSA East has helped medical students build their portfolios as well as their writing skills by hosting an essay competition, in which the top prize included a publication in a PubMed indexed journal.
BOMSA Scotland and North West ran a series of popular webinars that provided useful guidance
on portfolio-building. We know that our audience value these kind of relevant and practical methods to build towards their ambitions, and as an organisation we take pride in widening access to and facilitating these opportunities.
Furthermore, in just under a year, BOMSA’s main and regional social media accounts have accumulated just under 5.5k followers. Our student podcast, ‘Oh Snap!’, has also gained a growing following on Spotify, so tune in for the inside scoop on life in T&O!
With the return of in-person events, our BOMSA divisions have also been able to organise conferences covering a wide range of T&O-related topics. BOMSA London hosted
an Undergraduate Orthopaedic Symposium that attracted 60 delegates from four different continents. In Leicester, BOMSA Midlands sponsored a free-of-charge international T&O conference centred around women in orthopaedics and promoting diversity. Students were given the opportunity to present abstracts, and talks covering the ins-and-outs of a career in orthopaedics and the future of the field were also given. Apart from interesting talks, these events provide the valuable opportunity for medical students to network with each other, as well as professionals working in T&O. It is our firm belief that for the field to flourish, we must continue to encourage and nurture this spirit of community.
No event in the calendar encapsulates BOMSA’s aims of connecting aspiring orthopaedic surgeons like the BOA Annual Congress. Students are given the opportunity to present papers on the Thursday of main Congress, of which one will be selected as the winner. On Friday, the Medical Student Day >>

Features
JTO | Volume 10 | Issue 04 | December 2022 | boa.ac.uk | 27
“Comprising more than 95% of UK medical schools and overseen by a national body of students and junior doctors, BOMSA aims to enhance medical students’ exposure to Trauma and Orthopaedic (T&O) surgery from a grassroots level.”
puts aspiring orthopods and BOMSA in the spotlight with a variety of talks and practical sessions. The talks cover the journey through a career in T&O, addressing topics such as training applications, work-life balance and subspeciality choice. There is also the chance for students to meet and speak with T&O consultants and take part in a question-andanswer session to get a deeper insight into the field. A firm favourite of past attendees also made a reappearance this year, which is the opportunity to get some hands-on experience with some fantastic orthopaedics kit, courtesy of our sponsors. Many students struggle to find adequate time in theatres, especially with T&O placements being so notoriously short, making opportunities like these all the more valuable.

Going forward, BOMSA hopes to continue organising and supporting all of these fantastic events that inspire T&O-minded medical students across the country. This year’s inaugural Committee have built BOMSA to stand on its core pillars of being active, sustainable and providing incentivisation.

By being active, we aim to increase T&O exposure nationwide; by being sustainable, we endeavour to strengthen BOMSA yearon-year by passing on our culture and processes to successive Committees; and by providing incentivisation, we aim to reward our Committees selfless work in return for personal and professional development opportunities. We’re also thrilled to have announced our new National Committee for the academic year 20222023 at the BOA Congress, and we hope to see them take BOMSA to even greater heights!
Want to get involved as a student?
BOMSA recruits two local representatives from each medical school every year - typically one T&O and one surgical society president. Any positions declined are opened up to Committee members of the same societies. Local representatives may apply to be regional leads and our National Committee is recruited every August. If your university does not have a surgical or T&O society and you are thinking of setting one up, please also get in touch so we can get you on board.
We are also always looking for registrars and consultants who are interested in teaching and helping medical students climb the professional ladder. If this sounds like you, please scan the QR code below to register your interest.
For further information, please visit www.bomsa.org.uk or follow any of our social media pages. n

Features
28 | JTO | Volume 10 | Issue 04 | December 2022 | boa.ac.uk
“We are particularly proud of our BOMSA London division, who teamed up with the Royal National Orthopaedic Hospital to enrol 50 medical students in a successful mentorship scheme that matched them each with their own specialty registrar contact.”
JBJS | Miller Review Course I
The JBJS | Miller Review Course is a current, comprehensive review of orthopaedics unlike any other course. Taught by renowned surgeons across all subspecialties, the Miller Review Course I provides an in-depth analysis of key orthopaedic concepts to help you build knowledge and prepare for your future.
• Engage in five days of exciting live lectures from top faculty with on-demand versions available for 2 months of studying.
• Focus your learning through an intense and immersive comprehensive review of orthopaedics.
• Receive free one-year access to JBJS Clinical Classroom — an adaptive learning platform with over 4500 questions that builds knowledge by targeting areas that need strengthening.
And so much more!
You can attend the 2023 course in person or virtually from the comfort of your preferred location. As a participant you will: Learn more and register at millerreview.org
24 28 May 2023
How do we ensure that the NJR holds high quality data?
Derek Pegg is a Consultant Trauma and Orthopaedic Surgeon in Mid Cheshire Hospitals Foundation Trust, Leighton Hospital, Crewe. He is Chair of both NJR Regional Clinical Coordinators Committee and NJR Data Quality Committee.


Data of high quality is critical to meaningful interpretation of registry information. The National Joint Registry (NJR) currently has a compliance accuracy of 97.9% and continues auditing year-on-year to maintain and improve this degree of correctness. The NJR was established in 2002 in response to an unexpectedly high failure rate of a cemented total hip replacement.
Here, we briefly describe the effect of the implementation of the NJR’s formal data quality audit (DQA) programme on data compliance.
Where did we start on the data quality pathway?
Tim Wilton is a Consultant Orthopaedic Surgeon at Department of Orthopaedics, Royal Derby Hospital, Derby, with specialist interests in knee and hip replacement surgery. He is Past President of the BOA and BASK and is Medical Director of the NJR.

In this short article we describe the establishment of a formal data quality audit process within the NJR that enables bi-directional validation of every NJR entry and retrospective correction of any identified errors. This process has led to an increase in overall baseline compliance from 92.6% in 2014/2015 to 97.9% in 2018/19 period, with 91.5% of units ultimately achieving >95% compliance as of October 2022. We also briefly outline the further automation of the process that was initiated in 2018, to reduce hospital administrative burden and to integrate the data quality process into routine workflows. Our quality improvement results demonstrate that the process may be implemented successfully at national level, whilst minimising the burden on hospitals.
Why is good quality data important?
Good clinical audit requires good quality data. In the setting of joint replacement registries, key quality metrics include: compliance –the proportion of procedures performed that are entered onto the registry and measured against independently-collected administrative data; consent – the proportion of patients undergoing those procedures who have consented for their personal identifiers to be used by the registry; and linkability to outcomes events – the presence of a valid set of identifiers that can be used to match the record to revision and mortality events1
In the early years of the NJR our funding model was based on a levy system in which orthopaedic implant manufacturers collected a fee for each construct they sold and this was passed on to the NJR. Comparison of sales numbers with the corresponding records in the NJR gave a rough estimate of the registry completeness, but was unable to distinguish within year rates of compliance nor differentiate between primary and revision procedures. An alternative comparator was therefore needed. The Hospital Episode Statistics (HES) dataset, maintained by NHS Digital, has been used for this purpose for English NHS organisations since 2006. This comparison of data entry between the NJR and HES data gave a clear indication of incomplete data, but did not establish a mechanism for missed cases to be retrieved. It was also unable to provide the data for the examination of independently funded procedures. For this reason, a formal audit cycle capable of reconciling the two sources of data and allowing their correction was set up. Here, the NJR dataset is compared directly with each NHS organisation’s Patient Administration System (PAS) and each independent sector organisation’s business administration system, and vice versa.
How did we put the strategy into practice?
A Data Quality Committee (DQC) was established to determine and oversee the strategy, with the support of NHS England, patient representatives, and other key stakeholders. All organisations contributing data to the NJR were sent an annual statement showing cases found on the registry but missing from that unit’s PAS data, along with a similar list
Features
Chris Boulton is the Deputy Director of Operations of the National Joint Registry.
Chris Boulton, Derek Pegg, Tim Wilton and Mark Wilkinson, on behalf of the NJR
30 | JTO | Volume 10 | Issue 04 | December 2022 | boa.ac.uk
of those cases found in the PAS data but not in the NJR data. Data entry managers at each organisation were asked to check the individual unit records and upload the correct data to the NJR. Each unit worked with the NJR to share data and identify areas for improvement. An overview of the process is shown in Figure 1.

Process and procedure documents were agreed for each step of the audit process undertaken by the NJR team and the unit-nominated Data Quality (DQ) lead. The audit tool was finalised as a means to 1) semi-automate the process of validating returned audit data, and 2) provide a mechanism to track progress metrics against individual unit records. This enabled clear audit status reporting back to the NJR DQC. A compliance audit report was developed and sent to the Chief Executive Officer (CEO) and Clinical Lead for each organisation containing the key findings, recommendations and additional learning points from the audit process. Thus, the report provided each organisation with their own key learning points to act upon.
Has the DQA process improved baseline data completeness?

The baseline level of compliance does not represent the final compliance achieved
in each year since the audit cycle was introduced. Our final compliance accuracy for the 2018/19 period is 97.9%. The baseline completeness in 2014 prior to any missed cases being entered demonstrated an average organisation-level compliance of 92.6%, but there remained over 7,000 cases where a record was present in the provider data without a corresponding record in the NJR. There was a higher percentage of revision cases that were missed, with 9.7% of revision hips missing versus 5.6% of primaries and 9.8% revision knees versus 5.1% of primaries. From 2015, the audit was conducted at individual unit level and included the independent sector. This demonstrated an average baseline unit level compliance rate of 91.8% in 2015/16, increasing to 92.6% in 2016/17 and to 94.1% in 2017/18. Baseline performance of data completeness shows a year-on-year improvement across all units. For the 2018/19 audit year, the first year of automation, 61.5% of units achieved 95% or higher compliance upon first run of the audit (Figure 2). This increased to 76.4% of units for the 2019/20 period. As of October 2022, 91.5% of units have now achieved >95% compliance for 2018/19 and 88.5% of units for 2019/20. These audits remain open and units continue to work to improve these figures towards 100%. >>
Features
Mark Wilkinson is Professor of Orthopaedics at the University of Sheffield and an Honorary Consultant Orthopaedic Surgeon at Sheffield Teaching Hospitals. He is Chair of the Research Committee at the NJR.
JTO | Volume 10 | Issue 04 | December 2022 | boa.ac.uk | 31
Figure 1: Overview of NJR data quality strategy.
The NJR oversaw a national roll out of a semi-automated audit process in 2020/21. An automated secure data quality platform was developed to allow the upload of PAS data direct to the NJR data entry system (Figure 3). This enables users to upload PAS data at their convenience and to produce real-time reports of compliance against NJR submissions. Following processing, an updated compliance percentage is displayed, providing motivation for users to correct all missing or incorrect entries. Automation greatly reduces the number of potential missing cases that have to be checked each time the audit is run and also allows units to qualify for and receive their NJR Quality Data Provider certificates closer to real time. A new reporting

suite also supports the programme by providing comprehensive information on the status of each unit in the audit cycle and exception reports flag any areas of concern for the NJR compliance team. This system also allows units to take responsibility locally to ensure target compliance is achieved and maintained.
What still needs fixing?
The NJR’s Annual Report now reports on a ‘whole construct’ basis, meaning that an incomplete set of components entered for a case would be classed as ‘unconfirmed’, and excluded from some analyses. Work to examine these unconfirmed components has commenced across key areas, including elbow surgery, reverse shoulder replacement, dual mobility hip replacement and multiple-unicompartmental knee replacement.
This ongoing work is led by the NJR DQC and the relevant specialist societies, and involves both validation of component classification with industry and examination of individual cases by units. For elbow surgery, a nationwide DQA led by the British Elbow and Shoulder Society (BESS) with support from the BOA and RCS, has recruited BOTA surgical trainees to examine the operative notes of cases that are either absent from the registry (but present in administrative data) or with unconfirmed constructs. As a result of these efforts by the BESS team and the trainees, completeness of the elbow dataset has improved from 61% to 84% and accuracy from 93% to 98% (2022 NJR Annual Report https://reports.njrcentre.org.uk/downloads).
Take-home messages
Implementation of the DQA programme has had a substantial effect on ensuring the high quality of data in the NJR. Completeness is now routinely above 95% at baseline, increasing to 97% nationally post-audit, with many units capturing 100% of cases within each cycle. For NHS organisations, this has also resulted in gains in best practice tariff through increased recorded procedure volumes.
Establishment of the data quality audit as ‘business-as-usual’ has meant that the NJR has been able to increasingly focus on a more targeted examination of areas of data quality concern relating to implants.
Other registries looking to implement similar data audit processes would be encouraged to consider the following points:
• A data quality committee should be established to set the strategic aims and oversee and monitor the process.
• Clear and regular communication should be targeted to named data quality leads at each unit involved with the registry.
• Registry staff should be appropriately resourced to support units with engaging with the process. Particularly in the early years of implementation.
• Where possible, technological solutions should be implemented to reduce the burden on units and help establish these processes as part of routine work stream registry participation. n
Explanatory note
For full details of the DQA audit development and implementation, please see our companion piece in BJO2
References
1. Burgess R. New Principles of Best Practice in Clinical Audit. 1st ed: CRC Press; 2011 20 Jan 2011.
2. Boulton C, Harrison C, Wilton T, Armstrong R, Young E, Pegg D, et al. Implementing large-scale data quality validation in a national arthroplasty registry to improve compliance: the National Joint Registry data quality audit programme. Bone Jt Open. 2022;3(9):716-25.
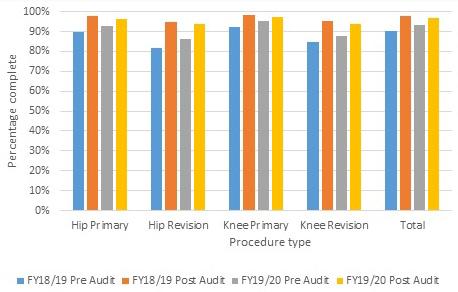
Features
Can we incorporate the DQA into ‘business-as-usual’ workflows for hospitals?
Figure 2: Effect of the data quality audit on completeness for 2018/19 and 2019/20.
32 | JTO | Volume 10 | Issue 04 | December 2022 | boa.ac.uk
Figure 3: Process flow diagram of secure file transfer protocol (SFTP) for automated data quality audit.



 An AK MEDICAL Company
Category Manager Rebecca Green: rebeccca.green@jri-ltd.co.uk
Innovative Custom Orthopaedic Solutions (ICOS) by JRI Designed and fabricated bespoke implants that help patients return to anatomical wellness.
An AK MEDICAL Company
Category Manager Rebecca Green: rebeccca.green@jri-ltd.co.uk
Innovative Custom Orthopaedic Solutions (ICOS) by JRI Designed and fabricated bespoke implants that help patients return to anatomical wellness.
Because we are all different.
Teaching surgery: Out of Africa, into the future
 Ad Gandhe
Ad Gandhe
Ad Gandhe is a Trauma & Orthopaedic Surgeon at Portsmouth Hospitals University Trust, UK, where he is also an Honorary Senior Lecturer. He is the faculty of various national and international educational groups, including the AO Foundation and AO UK&I. He is also an ambassador for The Primary Trauma Care Foundation.

He invented Touch Surgery which is an award-winning app and hence founded the company, Digital Surgery Ltd. This pioneering technology led the way to remote surgical training. He is the CEO and founder of Amodisc Ltd, which develops innovating technologies to help individuals and institutions deliver accessible, high quality surgical and medical education across the world.
On the 26th April 2022, I found myself sitting on a hotel balcony in Kigali, Rwanda, contemplating the road ahead. All my passion and love for combining education with technology had led me to this moment. My goal to democratise medical education was within reach. Here was my opportunity to take it further and what a place to start: Africa, the continent where we all originated from.
So, what led to this point? The short answer is that my experience in building technological solutions for surgical education led me to founding a new company, Amodisc, with exactly that vision. My contacts with Operation Smile, notably Wg Cdr Ankur Pandya of Operation
Smile UK, introduced me to the international Operation Smile Team in late 2019. They were keen to enter the Global Surgical Training Challenge competition with a multimodal and cost-effective solution that remotely teaches specialist skills to surgeons around the globe. The listed benefits of remote surgical teaching are long. They include, greater reach, reduced carbon-footprint and cost-effective training. This was made more acute by the COVID-19 pandemic. Our visions were aligned and so the Amodisc - Operation Smile collaboration began. An international team of clinical and technological experts from South Africa, Rwanda, USA, Bolivia, Malta and the UK, led by a US plastic surgical resident, Zach Collier, met every Thursday on Zoom.
Together we designed and developed a low cost simulation model made from local materials and an accompanying app which interactively teaches the skills required to perform surgical procedures. We deliberately chose procedures that are not widely available in subSaharan Africa owing to the paucity of available specialist training programmes.
Working with this team has been one of the most challenging and enjoyable experiences I have ever had. Every member brought solutions to the ‘virtual table’ with a strong desire to succeed at our project. The competition host, NESTA threw curve-balls at us left, right and centre, but nothing was too big a challenge. In fact it gave us an opportunity
Features
“If there is one thing COVID-19 has proven, it is the interconnectedness of different actors of society, the underlying resilience to disruption, the ability to transform challenge into opportunity, and agility to respond to crises adaptively.”
Kenichi Yokoyama, Director General, South Asia Department, Asian Development Bank
34 | JTO | Volume 10 | Issue 04 | December 2022 | boa.ac.uk
Zach, Arsen and myself (right to left) in front of Kibungo General Hospital.
to make our product better. The remarkable thing is that, despite never meeting one another in person for 18 months, we still completed our prototype and made it to the competition final round. The next phase had begun.

Making a prototype app and low-cost simulator is one thing, but designing it to work in an unfamiliar environment is a different matter. I had never been to sub-Saharan Africa before and had no idea what to expect. Would the trainees want to adopt it? Do they have the same technology and infrastructure as us? Will they feel patronised by us? These were all questions racing through my mind… as I sat there on the hotel balcony in Kigali.
Zach soon joined me along with our team’s Rwandan plastic surgery representative, Arsen Muhumuza. Arsen dedicated a week towards hosting us along with his two compatriots: Benjamin Ngarambe (Operation Smile Country Coordinator) and Andrew Karima (Operation Smile Country Manager). We visited three main institutions and their chiefs: Professor Ntirenganya Faustin, Plastic Surgeon at University Teaching Hospital of Kigali, Professor Julien Gashegu, Professor of Anatomy, at University of Rwanda, Butare and Dr Gahima John, Director General of Kibungo Provincial Hospital. This was a good mix of city hospital, district general hospital, and university. Our intention was primarily to meet our collaborators in Rwanda, build trust and discover the differences between our countries so that we can design our platform more effectively. However, what struck me were the similarities we share despite the resource restrictions they have. The poverty is evident, but how they overcome these limitations was impressive.
There are no short cuts to providing healthcare. The WHO checklists, team briefs and preoperative meetings are conducted as per usual. The theatres have computers in them and everyone has a smartphone: essential components of today’s data-driven healthcare. No arm table attachments for the operating table? No problem. They just use the patient bedside tables as they are height-adjustable. Theatre discipline is paramount (something we could all learn from) and of course, the residents have a jolly good knees-up at their end of year presentations. >>

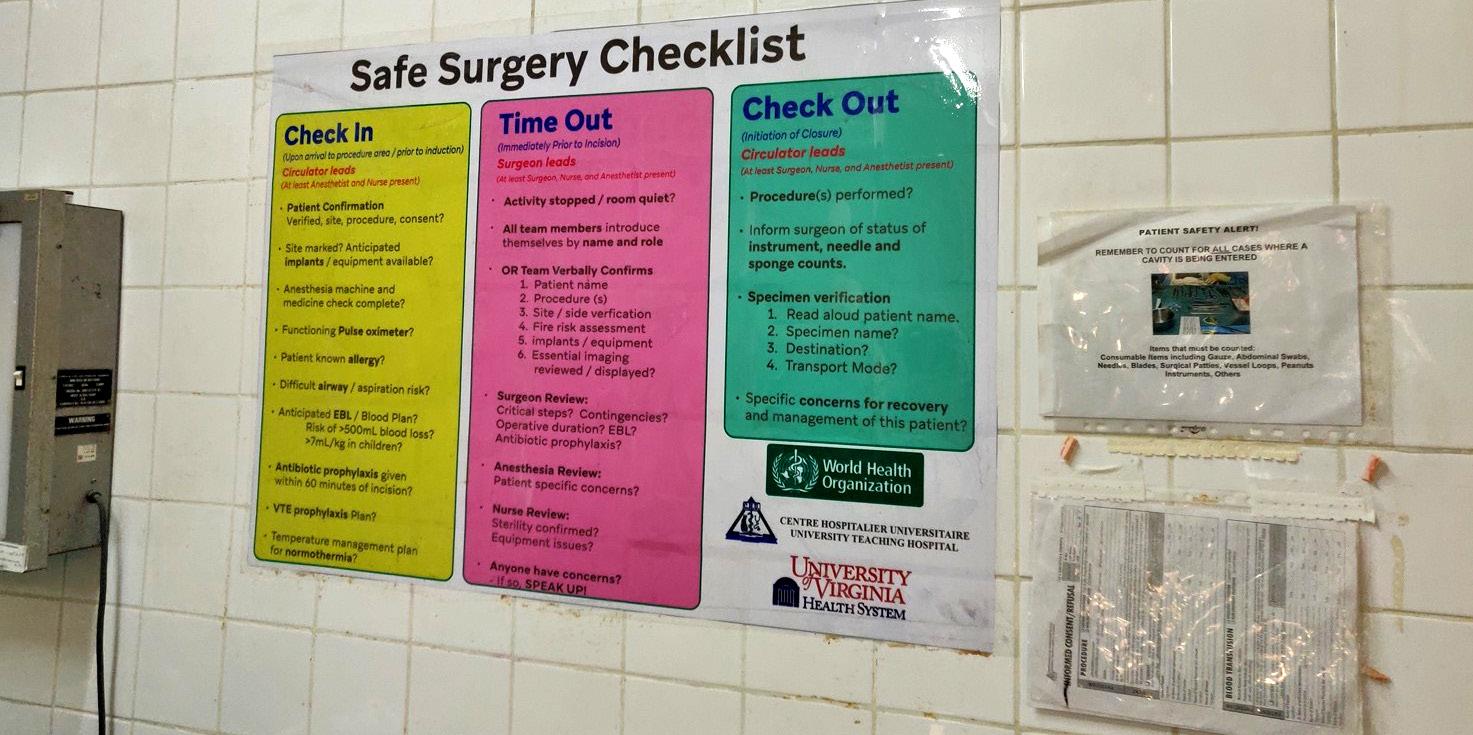

Features
in
WHO checklist in theatre.
Computers
theatre.
Sourcing raw materials for the low-cost physical simulator in Kigali marketplace.
JTO | Volume 10 | Issue 04 | December 2022 | boa.ac.uk | 35
Operating theatre in Kigali University Hospital (with some equipment donated by Operation Smile).
“Working with this team has been one of the most challenging and enjoyable experiences I have ever had. Every member brought solutions to the ‘virtual table’ with a strong desire to succeed at our project.”
Where there are challenges, there are opportunities. As I walked into the Kibungo Hospital, I heard a ‘thud’ behind me. Somewhat startled, I asked what this package was that had dropped out of the sky. In Rwanda, not all the hospitals have blood banks. The solution is a centrally run system whereby the path-lab calls an operator, who promptly dispatches the type-matched blood to the requesting hospital by drone. Blood is delivered within five minutes of the request. I felt this was a good example of where the resources are tight, innovations overcome. In the West, we have traditionally invested in cumbersome and antiquated systems, making the change to new technologies difficult to justify financially. Conversely, in Rwanda, they are not bound by these investments. They can use new disruptive technologies to bypass such systems, providing more cost-effective and efficient solutions.
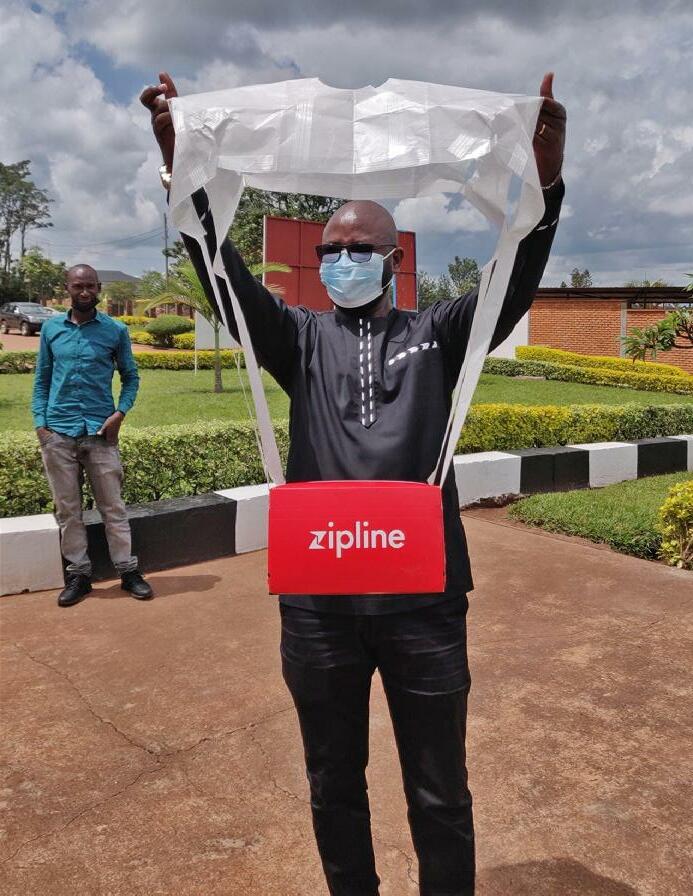
There was a refreshing willingness to solve many of the issues caused by the restricted resources. Professor Faustin had a vision of expanding the reach of plastic surgical education between the Rwandan institutions, giving all residents access to learning specialist procedures and thus providing better quality surgery. He viewed our platform as a potential solution for this. Professor Gashegu explained to me that cadaver supplies are limited in Rwanda for social and cultural reasons.
We explored building augmented reality and smart technologies to deliver detailed anatomical teaching to his students remotely. Dr Gahima John demonstrated how the resilience and flexibility they used to pivot resources in order to overcome the issues caused by the pandemic, can be used in the same way to rebuild better data connectivity between their institutions. Remote access could therefore still be achieved where the infrastructure is lacking. I have the deepest respect for these individuals who understand the future is best mapped out through collaborative working.
Having met such positive people, I left Rwanda, feeling more energised than ever. There is clearly a need to deliver surgical teaching more effectively. Access to this training is far from universal, but the need persists. Technology can break down financial and geographical barriers so that we can deliver it remotely. As surgeons, we are best suited to find the most innovative ways to deliver this training, albeit through videos, interactive animations, augmented reality or whatever technology delivers us. Through collaboration, we have the greatest chance of achieving this goal. The road ahead will have its challenges in delivering the training remotely, but with this genuine solidarity and willingness to succeed, I feel we are moving into a future of the greatest possibilities n



Features
Trainees constructing their low-cost simulator.
Zach, myself and the trainees outside the newly constructed Plastic Surgery Department at Kigali University Hospital.
AMOSMILE accompanying simulator app.
36 | JTO | Volume 10 | Issue 04 | December 2022 | boa.ac.uk
Blood products that have just been air-dropped by drone outside Kibungo Hospital.
Jig-guided hip revisions
For the first time, Gomina has developed an extraction set that allows a hip revision to be done with minimal bone loss. Thanks to innovative production technologies, it is possible to manufacture dimensionally rigid chisels with different radii. The precision ground, sharp cutting edges of the chisels are the result of Gomina’s many decades of expertise.

The bespoke crafted jigs manufactured by Gomina ensure the application of a precise separation of bone and prosthesis. This innovative pioneering extraction set from Gomina makes surgeon’s work far easier, leading to shorter operating times. Entirely for the patient’s benefit.

Official Distributor for the UK
Judd Medical Unity House, Buntsford Park Road, Bromsgrove, Worcestershire B60 3DX Tel. +44 (0)15 27 55 90 10, sales@judd-medical.co.uk, www. judd-medical.co.uk
www.gomina.ch
swiss quality

Getting started as an orthopaedic expert witness
Sameer Singh
Sameer Singh is Consultant Orthopaedic Surgeon at Bedfordshire Hospital NHS Trust and member of BOA Medico-legal Committee.

An expert witness is a person whose level of specialist knowledge or skill in a particular field qualifies them to present their opinion about the facts of a case during legal proceedings. Medical experts provide a fundamental role within the judicial system to provide opinions to assist the court to reach decisions. While you may be instructed and paid by a solicitor, your overall duty is to the court. It is important act within your defined area of expertise and remain impartial. Present your opinion on the evidence provided by examination and medical records.
Personal attributes required
• Probity
• Commitment to CPD
• Impartiality
• Declaration of interests
• Define scope of practice and act within limits of expertise
• Time management
Advantages of expert witness work
Working as an expert witness can be financially rewarding and intellectually stimulating. It can improve one’s own clinical practice and documentation by analysis of the medical records of many cases from different hospitals. Working as an expert witness will provide greater insight into long-term outcomes of the injured. The work can be challenging but also fun and allows interaction with solicitors who have a different perspective on the long-term outcome of trauma and orthopaedic conditions. Whilst examination of the client will be required, a lot of the work can be performed at home.
Disadvantages of expert witness work
Expert witnesses can have their credibility, integrity and qualifications challenged by opposing parties hence an expert witness should be thick skinned.
The Supreme Court in the case of Jones v Kaney [2011] overturned 400 years of practice and has held that a party can sue its own expert witness for negligence in litigation. Hence acting within limits of expertise and producing reports which are for the court (and not being influenced by the instructing party) are critical.
Expert witness work is also deadline driven and you must be comfortable working to strict deadlines. Travel may be required for conference with Counsel and court attendance. A time commitment is required and this may involve evening work to complete reports. Payment for work is often delayed. Clinical duties can be interrupted with attendance at court, however employing organisations should be prepared to release staff if they are acting as an expert witness. Having said that court attendance is rare and settlement is often reached before a proposed court date.
What does an expert witness actually do?
• Review documents
• Take a history and perform a physical examination
• Search the literature for relevant papers
• Formulate an opinion
• Draft reports
• Attend conference with Counsel, solicitors and claimants
• Attend court
The majority of expert witness work is personal injury, through the civil courts. Some work involves cases of clinical negligence. Various bodies advise that surgeons should have been in consultant practice for several years before taking on clinical negligence work – professional reputations can hang on such work, and it may be fiercely contested.
Most cases are settled out of court, and hence court attendance is often not required. While attending court may seem daunting with the opposing party critically analysing your report;
Medico-legal
38 | JTO | Volume 10 | Issue 04 | December 2022 | boa.ac.uk
if your opinion is fair, balanced and unbiased then court attendance should proceed relatively smoothly.
What is needed to get started in expert witness work?
It is important to receive appropriate training prior to commencing expert witness work. This is endorsed by the Academy of Medical Royal Colleges. Various organisations provide training in aspects of expert witness work, including but not limited to the British Medical Association, the Expert Witness Institute, Bond Solon, Inspire MediLaw, the Academy of Experts etc. The British Orthopaedic Association does not endorse any specific provider of such courses over any other.
Training allows an understanding of Practice Direction 35 also known as CPR Part 35. When acting as an expert witness, doctors must be familiar with the duties required and the courts will expect these to be understood and followed.
Part 35 of the Civil Procedure Rules governs the use of evidence from experts and assessors in civil proceedings [www.justice.gov.uk/courts/ procedure-rules/civil/rules/part35].
Appropriate indemnity needs to be in place. It is unusual for an expert witness to face litigation but there have been cases where an expert witness has been required to pay back the costs of the case. This is extremely rare and as long as

you stick to what you know, don’t advocate for either side and follow the relevant guidance – this should not occur. For reference the following are notable cases where experts have found themselves in hot water.
• Jones v Kaney [2001] https://en.wikipedia. org/wiki/Jones_v_Kaney
• Samantha Thimmaya v Lancashire Teaching Hospitals NHS Foundation Trust [2020] www.hempsons.co.uk/app/uploads/2020/ 02/Thimmaya-v-Lancashire-NHS-TrustFoundation-v-Mr-Jamil-ApprovedJudgment.pdf
• Bux v The General Medical Council [2021] www.mpts-uk.org/-/media/mptsdocuments/a06-21-bux-v-gmc-2021-ewhc762---circular_pdf-86085196.pdf
Like many areas of medicine regular CPD is required to demonstrate that your practice is updated and develop areas of practice in both the clinical and legal arena. It is important to perform CPD and expert witness work should be declared on annual appraisal
Text books
Books are available to assist with report writing. Having access to these is a useful guide in the preparation of medico-legal reports. This will help guide your opinion based on published research:
Medicolegal Reporting in Orthopaedic Trauma
Authors: Michael Foy, Phillip Fagg
Writing Medico-Legal Reports in Civil Claims –an Essential Guide (2nd Edition) (2015)
Authors: Giles Eyre and Lynden Alexander
Clinical practice and the law – a legal primer for clinicians (2018)
Author: Giles Eyre
Other considerations
A CV should be drafted which outlines your qualifications, experience, training and area of expertise.
It is extremely important to act within your area of expertise as this may be challenged in the future. If there is any conflict of interest this should be declared and work declined if there is conflict of interest. If there is any doubt about a specific matter you should ask the instructing party for guidance. It is important to address these issues at the time of instruction prior to preparation of reports or Court attendance.
The CV should include a corresponding address, email address, consulting addresses for appointments, relevant training, professional qualifications, education, languages spoken, turn-around time for production of a report, Claimant to Defendant ratio of reports written, and any positions of responsibility held at local or national level. >>
Medico-legal
JTO | Volume 10 | Issue 04 | December 2022 | boa.ac.uk | 39
A separate document outlining terms and conditions needs to be prepared. This should outline the fee for report, hourly rate, fees for conference with Counsel and Court attendance. Payment terms need to be included in terms and conditions. Most instructing parties like payment to be made on conclusion of the case, however, this may be many months or years after you produce a report. Working with agencies there is some negotiation with payment terms. It should be stated on the terms and conditions if there is a DNA fee for missing appointments and a cancellation of Court attendance. Registration with ICO will be required. Compliance with GDPR should also be stated on the terms and conditions. All medical information provided and stored should follow the same guidelines of confidently as NHS and Private patients. Sharing of information with instructing party and solicitors must be secure.
A redacted report is sometimes asked for particularly when starting with a new firm. This is difficult if it is your first report but after a while you will have many to choose from.
The administration can be onerous when acting as an expert witness especially as the work-load increases. Appropriate secretarial and admin support must be available for arranging appointments, preparation of reports and chasing payment. Your skill is writing reports and treating patients so delegate the other tasks.
You will need to allow time within your weekly working schedule. A daily time commitment will be required to respond to instructions from instructing parties, deal with amendments of reports, and reviewing reports once dictated. This does require a daily commitment between 30-60 minutes to respond to queries. A time commitment per week is required to prepare and review reports and letters. Expert witness work is deadline driven and the instructing parties are under pressure from Court deadlines. If you are unable to meet these tight deadlines then you should inform the instructing party so they can arrange Court extension.
Guidelines
• General Medical Council: www.gmc-uk. org/ethical-guidance/ethical-guidance-fordoctors/acting-as-a-witness/acting-as-awitness-in-legal-proceedings
• Royal College of Surgeons of England: www.rcseng.ac.uk/standards-and-research/ standards-and-guidance/good-practiceguides/expert-witness
• Academy of Medical Royal Colleges: www.aomrc.org.uk/news-and-views/ acting-as-a-professional-or-expert-witnessguidance-published
Marketing
Once you have a CV, terms and conditions, indemnity and training you will need to market yourself for expert witness work. There are a number of avenues for this.
There are expert witness directories, this will involve paying a fee and the directories will advertise for instructing parties. When an instructing party is looking for a particular expert they will search the directory looking for appropriate witness in the location required. Some will require a short biography and artwork.
Instructing parties’ solicitors often subscribe to law magazines, and adverts can be placed in these advertising the services you offer. These can be full page, or a banner and provide a link to contact details.
Some expert witness work is performed via agencies. The advantage of working with agencies is that they will promote you to instructing parties, provide you with all the relevant documents and there will be a steady stream of instructions. The disadvantages of working via agencies are that the reports are often fixed fees and for complex cases a greater time commitment will be required. The remuneration from working with agencies will be less than working directly with solicitors. However, it is certainly an excellent starting point and there will be less chasing of outstanding payments.
MedCo was established to facilitate the operational changes required under the Ministry of Justice pre action protocol for low value personal injury claims in road traffic accidents. Most agencies like their experts to be MedCo registered.
A personal website can be used and it is important to include key words to optimise search engines.
LinkedIn and social media can be helpful in advertising your skills as an expert witness. LinkedIn is particularly useful as many solicitors are listed here.
Solicitors can be approached directly with a CV and terms and conditions outlining the services you provide and your particular area of expertise. Providing presentations and training for solicitors is a good way to promote yourself. They are interested to hear from Orthopaedic Surgeons and the surgery we perform.
When starting expert witness work it is useful to be seen on all types of platforms for advertising as instructing parties will have different preferences on how they search for experts. Once they have gained confidence in you producing accurate reports within timescales they will tend to use you again. Your last report is the best advert!
To be MedCo registered involves registering with their website and agreeing to their terms and conditions. An annual fee is required. If working as an indirect medical expert (i.e. via agencies for MedCo work) the fee is £200/ yr. If working as a direct medical expert (solicitors, claimant representative, insurers will contact directly) the fee is £500/yr. To be MedCo registered you will have to complete online training and multiple choice questions which will ensure that your training is up to date and this CPD will need to be maintained on a regular basis. Hence being MedCo registered is useful as the training and CPD requirements will be met. The fee for a trauma and orthopaedic report via MedCo is £420 if working as a direct medical expert. If working as an indirect medical expert (via agency) then the fee will be less as the agency will take a percentage of the fee.
The best advertisement for your work would be unbiased reports which are produced for solicitors with clear explanation and prognosis. In broad terms if instructing parties are happy with your work, they will instruct you for future cases.
To summarise, expert witness work can be financially rewarding and stimulating. It will improve your own clinical practice as reviewing documents from other institutions will help assist with your own clinical practice. The work is deadline driven and it is important to set time in your daily and weekly schedule to deal with the matters that arise.
Medico-legal
n
40 | JTO | Volume 10 | Issue 04 | December 2022 | boa.ac.uk
“The best advertisement for your work would be unbiased reports which are produced for solicitors with clear explanation and prognosis. In broad terms if instructing parties are happy with your work, they will instruct you for future cases.”
Don’t leave fusion to chance Prioritise Bone Graft

Safe
Demonstrated to be as safe as autograft in a Level 1 human clinical study
E ective
Achieved a fusion rate of 97.3% at 24 months in a Level 1 human clinical study
Proven
A powerful cell attachment factor backed by Level 1 human clinical evidence

Spine


1 ACDF – 319 patients (IDE RCT) “i-FACTOR subjects demonstrated higher overall success rate than control (autograft) subjects (68.75% and 56.95% respectively, p = 0.0382)”
2 PLF – 98 patients (RCT) “This RCT indicates i-Factor being signi cantly superior to allografted bone in enhancing intertransverse fusion (p = 0.000)”
3 ALIF – 110 patients “…high fusion rate and clinical improvements comparable to the published results for ALIF using autograft or BMP”
4 PLIF – 40 patients “i-FACTOR is associated with faster formation of bridging bone when compared to autologous bone in patients undergoing PLIF”
Orthopaedics
5 Long bone non-union and delayed union 22 patients – 90% bone consolidation “P-15 appears to o er a safe, economical, and clinically useful alternative to autograft in the repair of ununited fractures”


6 Foot and ankle – 170 patients i-FACTOR yields 92% fusion at 12 months post-op across fore-, mid- and hindfoot joints
7 Foot and ankle – 16 patients 100% fusion at 12 months in hindfoot and ankle fusion revision procedures

8 Peri-acetabular osteotomy – 51 patients Patients treated with i-FACTOR were 3x more likely to attain a partial or complete fusion at 6 months post-op compared to allograft

Internal Unpublished Data Level 1 Prospective Study Published Case Series
Partnerships in hand surgery
 Jonathan Hobby
Jonathan Hobby
Hand Surgery is an interface speciality comprising both plastic and orthopaedic surgeons. Since the formation of our society in 1952, the two specialities have worked together. We created the first interface fellowships in 1991 and all of our activities rely on a partnership between our two parent specialities.
Jonathan Hobby is a Consultant Orthopaedic and Hand Surgeon at the Hampshire Hospitals, and is the current President of the British Society for Surgery of the Hand.

In my own training I spent a year as an interface fellow in an advanced training post in hand surgery with the majority of my time spent at the St Andrew’s Centre for Plastic Surgery in Chelmsford. One of our recent initiatives is the ‘Hand in hand with Ukraine’ webinar series, which started in March a few weeks after the Russian invasion. The series is held in partnership with FESSH (the Federation of European Society for Surgery of the Hand) and the Ukrainian Hand Society. Surgeons from the UK and Europe with experience of surgery in conflicts deliver instructional lectures and discuss current cases with Ukrainian surgeons.
It is therefore fitting that the three articles in this subspeciality section all involve partnerships.
The management of closed extensor tendon injuries is increasingly delivered in partnership with our hand therapy colleagues, with considerable recent advances in splinting and the evidence base for non-operative management.
The BSSH has launched an initiative in partnership with industry to raise awareness of high-pressure injection injuries. These may initially seem innocuous and are often neglected both by the patient and first contact clinicians. However, they have serious consequences with swelling, compartment syndrome and secondary infection, which all too often leads to tissue loss and amputation. Outcomes are significantly improved if the severity of the injury is recognised early, and surgical decompression and debridement is performed urgently.
The final article reviews the Society’s work to develop global partnerships over the last decade. This has particularly focused on support and training for our orthopaedic and plastic surgery colleagues from countries with less resources than our own. A highlight of these efforts was the recent triennial International Hand Surgery Federation meeting (IFSSH) held in London in June of this year; the first time the meeting has been held in the UK. As a truly international meeting, speakers were invited from our project countries and were sponsored to contribute to sessions including the management of infection, burns contractures, neglected trauma and congenital surgery. There was also a virtual complex case discussion with surgeons joining virtually from around the world. There was a fellowship program with 30 of the brightest young surgeons from high and lowincome countries around the world visiting 18 UK hand surgery centres. In addition to seeing new techniques, this group have formed lasting friendships with daily case discussions on their WhatsApp group. n
Subspecialty
The International Fellows and Invited LMIC Speakers at a teaching day at the Royal College of Surgeons of England before the IFSSH, IFSHT and FESSH combined congress in June 2022
42 | JTO | Volume 10 | Issue 04 | December 2022 | boa.ac.uk
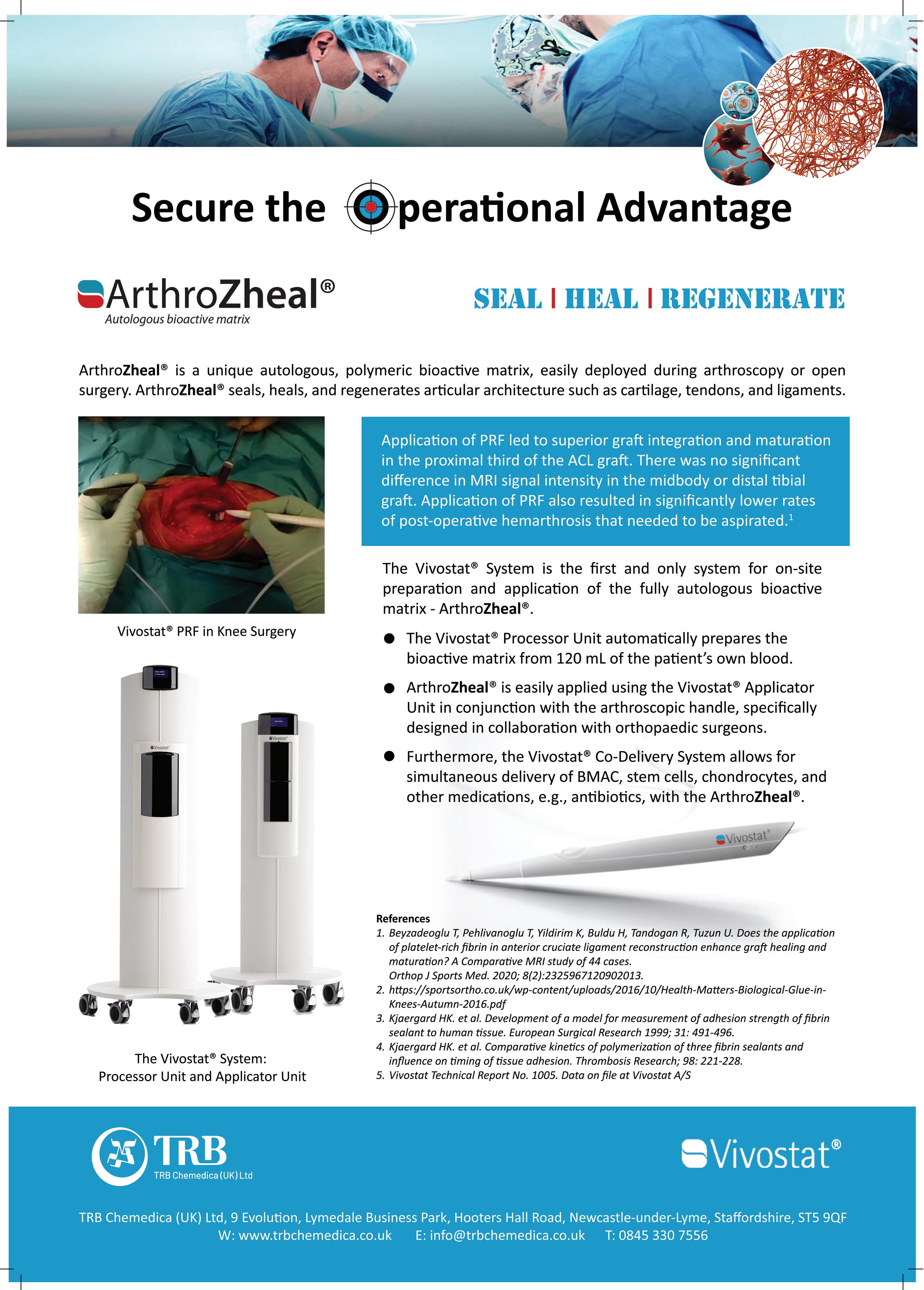
Sarah Turner has worked at Manchester Foundation Trust for over 20 years as a clinical specialist physiotherapist in hand therapy and has a particular interest in the management of hand trauma.

Management of closed extensor tendon injuries
Injuries to the extensor tendons of the hand and digits are a frequent presentation to the acute hospital setting. They are the most frequent tendon injury (54%)1, and are predominantly seen in men between the ages of 15 and 59. The majority are closed injuries.
Nick Gape is an occupational therapist and accredited hand therapist who works at the Cardiff and Vale University Health Board with a special interest in hand trauma.

Open injury usually requires further exploration with possible tendon repair but the majority of closed injuries, especially affecting the fingers, can be managed successfully with conservative treatment with the use of splinting and appropriate exercise therapy. The focus of this paper is to update on the management of the most common conditions in extensor zones 1 to 5: mallet finger, closed boutonniere and sagittal band injuries.
Mallet finger
Jonathan Hobby is a Consultant Orthopaedic and Hand Surgeon at the Hampshire Hospitals, and is the current President of the British Society for Surgery of the Hand.

Injury to the terminal extensor tendon in zone 1 is one of the most common hand conditions presenting to Emergency Departments making up almost 6% of all hand injuries. Closed mallets are caused by a sudden flexion (or extension) force to the distal interphalangeal joint (DIPJ), resulting in an extensor lag which is passively, but not actively, correctable. X-rays should always be taken to confirm if the injury involves an avulsion (or impaction2) fracture of the dorsal base of the distal phalanx. Patients may present with a chronic mallet deformity some time after injury.
The vast majority of closed injuries can be treated conservatively, however, surgical exploration is always indicated for the less common open mallet injury where the terminal extensor tendon is divided. It may also considered for closed bony mallets where > 3040% of the DIPJ surface is affected and if there
is subluxation of the distal phalanx, a lateral view x-ray taken in extension is essential to confirm the presence of irreducible subluxation. An attempt to treat these injuries with a splint in slight flexion, with reduction confirmed by x-ray, should be made in the first instance2. Even in the presence of persistent subluxation the joint can remodel with satisfactory functional outcomes2
Management of closed mallet injuries are through application of a splint to maintain DIPJ extension. Various types of splint have been described and include ‘off the shelf’ Stack splints or ones fabricated for a custom fit e.g. moulded foam aluminium (Zimmer splint), or thermoplastic splints made by a specialist hand therapist. There is however no clear evidence for the superiority of one splint type over another2. The proximal interphalangeal joint (PIPJ) should be left free to mobilise to full range to prevent stiffness although a longer splint can be fabricated to hold it in a flexed position should a swan neck deformity tendency be present.
There is no consensus of the duration of splint application but the authors advocate it be worn full time for six weeks for avulsion fractures and up to eight weeks for soft tissue mallets; a further two weeks of ‘weaning’ via night splintage is advised. Should the extensor lag recur, a return to full time splintage should be considered for a further 2-3 weeks then the active extension re-assessed.
The outcome of conservative management for acute closed mallets has been reported as less favourable for tendinous injuries, whilst a higher age at time of injury is also associated with poorer outcome3. Patients should be always be advised that the result of
Subspecialty
Sarah Turner, Nick Gape and Jonathan Hobby
44 | JTO | Volume 10 | Issue 04 | December 2022 | boa.ac.uk
treatment may not restore full range of DIPJ extension with a small residual lag not being uncommon. There is also usually a dorsal prominence which may be tender and ache in cold weather, although these symptoms improve with time.
A failure of the injury to respond to conservative management should be evaluated as to the effect on the affected digit: persistent DIPJ extensor lags may result in a swan neck deformity in some individuals, especially those with hypermobile PIPJs, which can be functionally debilitating. In the absence of swan-necking, reported pain and the patient’s desire for further intervention should be taken into consideration and the benefits and risks of surgery explained. Surgery may involve a simple trans-articular k-wiring of the DIPJ in extension for six weeks followed by a further four weeks of splintage, or for chronic mallets options include terminal extensor tendon reconstruction and DIPJ arthrodesis. There are a range of more complex surgical techniques described for acute injuries, but there is little robust evidence that these lead to better outcomes and complication rates are higher2
Boutonnière injury
The extensor tendon mechanism of the finger is an intricate interplay between the extrinsic and intrinsic muscles. Distal to the metacarpophalangeal joint (MCPJ), the extensor tendon divides in to the central slip, which inserts into the base of the middle phalanx, whilst radial and ulnar lateral bands converge along with the intrinsic muscles to become the terminal tendon that inserts in the distal phalanx.
The term boutonnière (buttonhole) aptly describes the mechanism of this injury of the extensor mechanism at the PIPJ. In the closed injury, the PIPJ is forcefully flexed or dislocated volarly causing the central slip to either avulse from its insertion, or to rupture just proximal to this point in the manner of a mallet injury. The central slip, however, is not the only extensor of the middle phalanx; extension is also possible through the lateral bands, providing their
stabilising structures (the triangular ligament and the transverse retinacular ligament) remain intact. If the integrity of these structures is also compromised, then the lateral bands sublux volarly acting instead as a flexor of the PIPJ whilst at the same time hyperextending the DIPJ.
Whilst this typical boutonnière posture may not be present initially, careful assessment using Elson’s or modified Elson’s tests have a high sensitivity in establishing the integrity of the central slip. When the classic deformity is present then Boyes’ test may prove more useful. Early diagnosis and treatment will likely favour a better outcome.
As with mallet injuries, non-surgical management is the mainstay of treatment in this zone of injury. Several treatment approaches have been described but there is little evidence to suggest the superiority of one over another.
Immobilisation of the PIPJ in full extension for a number of weeks is perhaps the most common approach. Various manufactured and custom-made splints/casts will fulfil this role but whichever is utilised, it is essential that the DIPJ is allowed to mobilise intermittently
(Figure 1). This allows the lateral bands to glide, discouraging their volar subluxation, and preventing the tightening of the retinacular ligament, a situation that can quickly become established. Immobilisation for six weeks is suggested 4 in the presence of a purely tendinous injury, although earlier protected mobilisation may be permitted with bony avulsions due to the quicker healing time of bone. Other authors do not differentiate and allow protected movement with a spring-wire Capener splint 5 or within a restricted range6 . Either will require the supervision and guidance of a hand therapist and progression of mobilisation should be pragmatic, as outcomes, whilst usually favourable, are not always predictable in this zone 4
More recently the use of relative motion has been advocated in the treatment of tendon injuries7. In this zone, the injured digit is placed in 15-20° relative flexion. This increases the laxity of the flexor digitorum profundus tendon and relaxes lumbrical tension, which in turn decreases the tension on the extensor hood. There may need to be some restriction of the flexion arc initially and potentially a night extension splint. Suitability for this approach requires the patient to pass the pencil test (Figure 2) by actively extending the PIPJ in this relatively flexed position. The central slip cannot realistically heal at the appropriate length with this regimen but this need not matter if the remainder of the mechanism is intact and the potentially deforming forces controlled. The patient is allowed to use their hand almost normally in the Relative Motion Flexion Splint (RMFS) (Figure 3). Reported outcomes in a series of cases studies are encouraging although as with other approaches, there is a paucity of evidence.
Closed injuries that do not respond to a splinting regimen will require referral to a hand surgeon with a view to extensor tendon reconstruction. Particular attention should be directed to extensor injuries associated with volar or lateral dislocation of the PIP joint. These injuries are uncommon, but may be associated with buttonholing of the condyle through the >>


Subspecialty
Figure 1: Dorsal based extension splint (distal strap removed to allow DIPJ flexion exercises).
JTO | Volume 10 | Issue 04 | December 2022 | boa.ac.uk | 45
From: Boyce, Giddens, Shewring, Tendon Disorders of the Hand & Wrist, Thieme Publishers 2022.
interval between the central slip and lateral band. This will lead to difficulty in achieving a stable congruent reduction. Early surgical exploration is indicated with open reduction and repair of the injured structures. These injuries are difficult to treat if neglected. Tendon lacerations in this zone, where the central slip and/or lateral bands are involved, will require primary repair. Similar rehabilitation regimens are utilised, although mobilisation is usually initiated at an earlier stage.
Sagittal band injury
Presentation of sagittal band injury may be either acute, with localised pain, swelling and tenderness, or chronic attrition. Acute injuries, frequently the result of either a direct blow including a punch mechanism (so called Boxer’s Knuckle), or a sudden hyperflexion force to the MCPJ, most often affect the radial sided band and the middle finger due to its local anatomical idiosyncrasy. Diagnosis is usually by clinical examination, x-rays may be taken to exclude localised fractures, further investigations are not routinely required but an ultrasound scan can confirm the diagnosis.
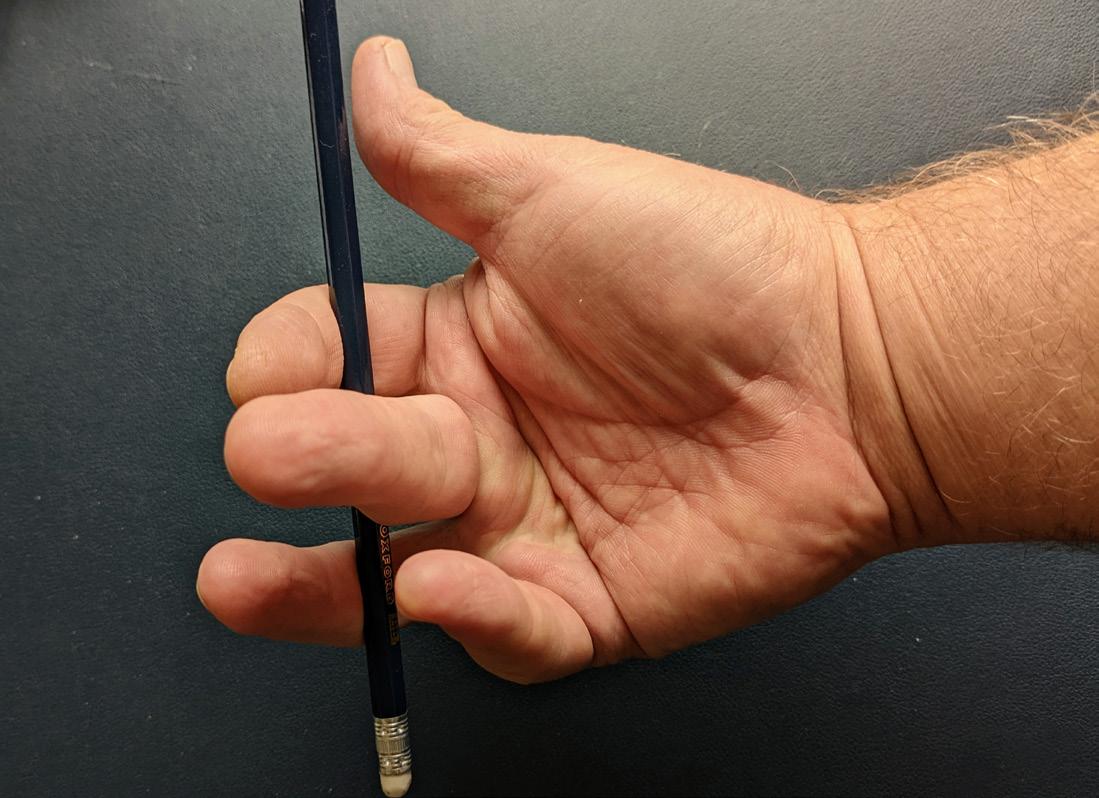
Classification by Rayan and Murray8 is according to the pathological severity; Grade 1 being a contusion or partial tear with no tendon instability; Grade 2 presents with a subluxing central tendon, usually in an ulnar direction off the metacarpal head during MCPJ flexion, relocating centrally when the joint extends. Grade 3 presents with full dislocation of the extensor tendon into the unaffected side intermetacarpal sulcus, the ability to actively extend the joint may be limited or impossible.
Management of the condition varies according to both severity and the time since injury. Evidence is variable about how late conservative management can be effective for patients with complete tendon dislocation9, injuries of up to three weeks duration are
generally accepted to respond better to conservative methods. Outcomes for conservative management are reduced with age, manual labour occupations, and for grade 3 injuries9. Chronic presentations, or where tendon dislocation is constant and occurs without pain, swelling or other inflammatory manifestations8, and also those acute injuries that have failed to respond to less invasive procedures, are likely to require surgical intervention.
Grade 1 sagittal band injuries can be treated adequately in full time neighbour strapping for up to four weeks duration. Grades 2 and 3 require splint application. There is no definitive consensus on which splint is most appropriate with a variety of hand based splints described whose function is to hold the affected MCPJ in a neutral to extended position. The authors favour use of the Relative Motion regime applying the Relative Motion Extension Splint (RMES) to position the affected digit in 15-20° hyperextension relative to the uninjured fingers, so relieving the tension on the extensor complex of said digit via the quadriga effect (Figure 4). There is again no consensus on the splint wear duration but six weeks full time wear and a further two weeks during activity has been advocated.
Light use and finger mobilisation is permitted whilst wearing the splint, recent publications indicate it is well tolerated due to its low profile.


Surgery involves open direct repair of the extensor hood for acute injuries whilst chronic presentations may require reconstruction using tendon grafts to reconstruct the sagittal bands. There are many techniques which create a check rein to centralise the extensor tendon10. Post-operative management involves application of the RMES as above. n
References
References can be found online at www.boa.ac.uk/publications/JTO
Subspecialty
Figure 4: Relative motion extension splint (RMES). From: Boyce, Giddens, Shewring, Tendon Disorders of the Hand & Wrist, Thieme Publishers 2022.
Figure 3: Relative motion flexion splint (RMFS). From: Boyce, Giddens, Shewring, Tendon Disorders of the Hand & Wrist, Thieme Publishers 2022.
46 | JTO | Volume 10 | Issue 04 | December 2022 | boa.ac.uk
Figure 2: Pencil Test.
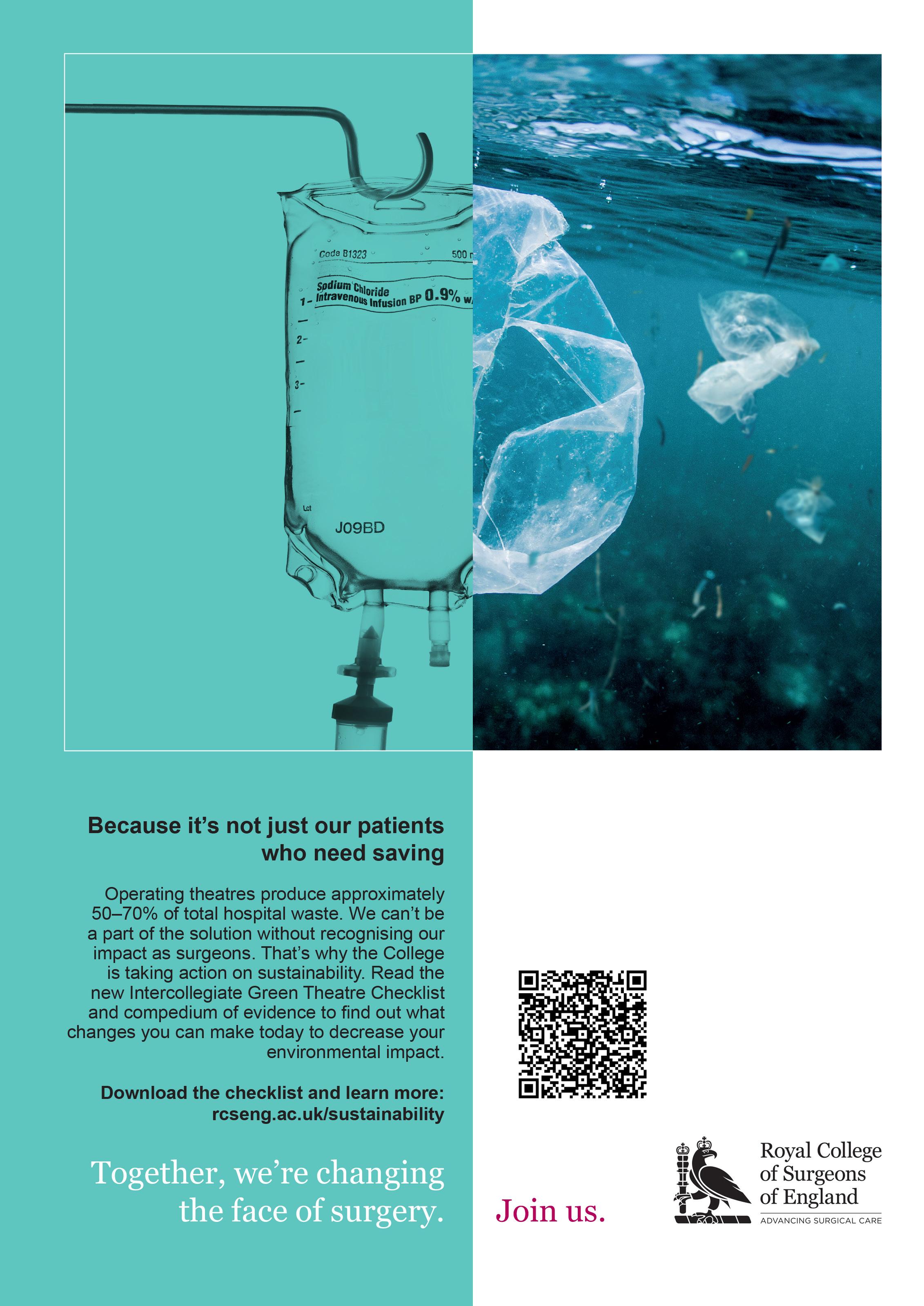
Major Guang Yim is a Plastic Surgeon currently based in South Wales working as the Major Trauma and Limb Reconstructive Microsurgery Fellow. He has trained in the West Midlands at the prestigious Queen Elizabeth Hospital Birmingham and then undertaken his Speciality Training in the South West of England.

Management of high-pressure injection injuries
 Guang Yim, Jens Roesner, Warren Hammert, Adeline Clement, Patrick Gillespie and Oliver Stone
Guang Yim, Jens Roesner, Warren Hammert, Adeline Clement, Patrick Gillespie and Oliver Stone
High pressure injection injuries are defined as puncturing of the dermis by a jet of fluid or air under pressure. When a leak or accidental activation occurs, a pressure of only 100 pounds per square inch (psi) is enough to puncture human dermis. Whilst uncommon, a hand centre in the United Kingdom (UK) is expected to see one to four cases presented per year1. If untreated or inadequately treated, the consequences of these injuries are devastating. In this article we provide an overview for clinicians to understand why high-pressure injuries are so damaging and under-recognised. We then provide an outline of how these limb threatening injuries should be managed as surgical emergencies.
Background
High pressure injection injuries are a relatively new phenomena that have emerged since industrialisation. The first case report of a highpressure injection injury was less than a hundred years ago. Within the English literature, the first report was by Rees in 1937 that involved the high-pressure injection of diesel from an engine injector to the right middle finger2
Many of us unknowingly have tools capable of causing significant harm within our own households such as a pressure washer that operate between 1,500 to 4,000 pounds per square inch (psi). Within commercial and industrial settings, paint guns, grease guns and hydraulic hoses are common sources of injury. The pressures that are present within these systems can range from 100 psi for a grease gun to 10,000 psi in hydraulic systems. Some spray guns can deliver 100 litres per minute; this means that even 0.5 seconds of injection can deliver 833 ml of fluid into tissue.
Physics
Fluid is used within hydraulic equipment to multiply the applied force to exert a greater output force through Pascal’s principle.
The ability of high-pressure equipment to inject fluid through skin is a function of:
1. Pressure – Higher pressures increase the ability of the fluid to puncture the skin.
2. Proximity to skin – The further away the aperture is from skin, the greater the air resistance the fluid has to overcome.
3. Aperture size – Smaller aperture sizes lead to higher velocities of fluid as it exits the aperture.
Pathophysiology and mechanism of tissue injury
High pressure injection injuries cause damage and morbidity through three different mechanisms.
1. Direct compressive effects from the presence of large volume of, uncompressible, fluid within small anatomical spaces with little to no room for expansion. This leads to effects analogous to compartment syndrome; ischaemia, venous occlusion and thrombosis due to the presence of foreign material.

2. Chemical toxicity from the noxious chemicals contained within the injected fluid.
3. Secondary infection from fluid that is non-sterile and also the inoculation of environmental organisms into deep tissue.
In the 1970s Kaufman demonstrated that the position of the hand at the point of high-pressure injection influenced the pattern of injuries encountered. Cadaveric Injection of wax at
Subspecialty
Warren Hammert is Professor of Orthopaedic and Plastic Surgery at Duke University, Durham, NC, USA.
Adeline Clement is a Consultant Orthopaedic Hand and Wrist Surgeon at The Department of Trauma & Orthopaedics, Raigmore Hospital (NHS Highland), Inverness.
48 | JTO | Volume 10 | Issue 04 | December 2022 | boa.ac.uk
Oliver Stone is a Consultant Orthopaedic Hand Surgeon and Clinical Lead for Orthopaedic Hand Surgery in the Exeter Hand Unit at the Royal Devon and Exeter Hospital, Exeter.


750psi in the midline over the flexor tendon second and fourth annular pulleys would spread wax in the subcutaneous tissues to completely encircle the digit and the neurovascular structures; due to the thickness of the pulleys. This is shown in Figure 1.

If injection occurred in the midline at the level of the joints, where the thin cruciate pulleys lie, then the wax would spread into the flexor tendon sheath in addition to encirclement of the digit (Figure 2).

If higher pressures are applied at the level of the joints, intra-articular spread could also occur as shown in Figure 3.
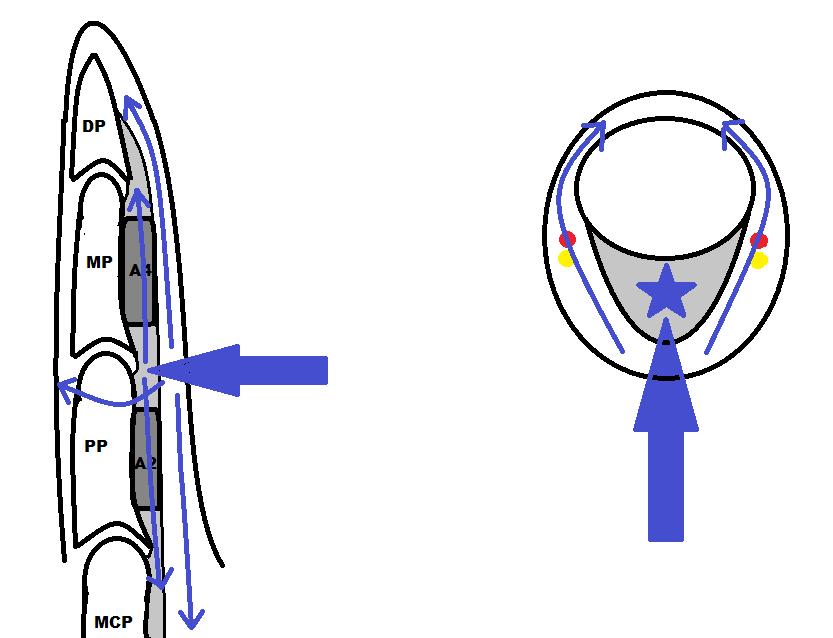
If para-midline injection occurred, the fluid would also spread to the dorsum and along the dorsal spaces of the finger and hand. If the thumb or little finger tendon sheaths
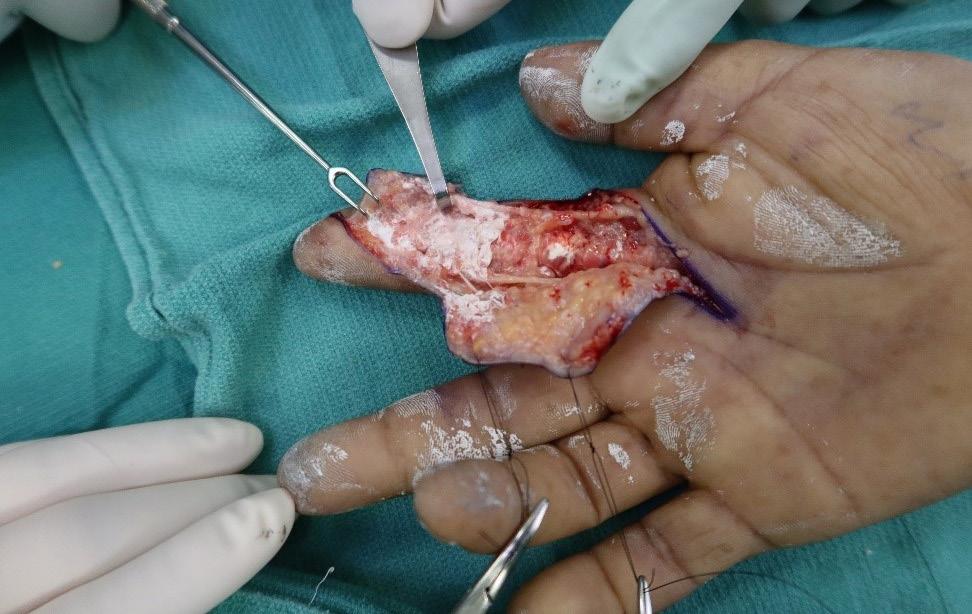
were breeched, the radial and ulnar bursae were respectively contaminated. Injection of the volar palm would lead to contamination of the interosseus muscle spaces, the palmar arch, common digital nerves and also extension to the dorsal spaces of the hand; this is exemplified in Figure 4.
The composition of the injected material significantly influences the morbidity of these injuries. Table 1 (below) correlates expected amputation rates for the different compositions of material injected. >>

Subspecialty
Patrick Gillespie is a Consultant Hand Surgeon in the Exeter Hand Unit and Department of Plastic Surgery at the Royal Devon and Exeter Hospital, Exeter.
Injected material Amputation rate Solvent based Paint 80% Oil-based Paint, hydrocarbons 70% Grease 20% Water <20%
Figure 2: Injection at the level of the joints leads to fluid spreading into the flexor sheath as well as the subcutaneous plane circumferentially around the digit and neurovascular bundles.
Figure 3: Very high-pressure injection at the level of the joints can lead to fluid spreading into the joint as well as the flexor sheath, the subcutaneous plane circumferentially around the digit and neurovascular bundles.
Figure 4: An X ray demonstrating the contamination of the interosseus muscle spaces, the palmar arch, common digital nerves and also extension to the dorsal spaces of the hand after volar injection of into the palm6
Reproduced from High-pressure chemical injection injury to the hand: usually underestimated injury with major consequences.
BMJ Case Rep. 2019;12(9):e231112. With permission from BMJ Publishing group Ltd.]
Table 1: The reported amputation rates according to the type of material injection.
JTO | Volume 10 | Issue 04 | December 2022 | boa.ac.uk | 49
Figure 1: Injection at the level of the annular pulleys leads to fluid spreading in a subcutaneous plane circumferentially around the digit and neurovascular bundles.
Even water alone is still associated with significant morbidity due to flexor tenosynovitis, compartment syndrome and even amputation.
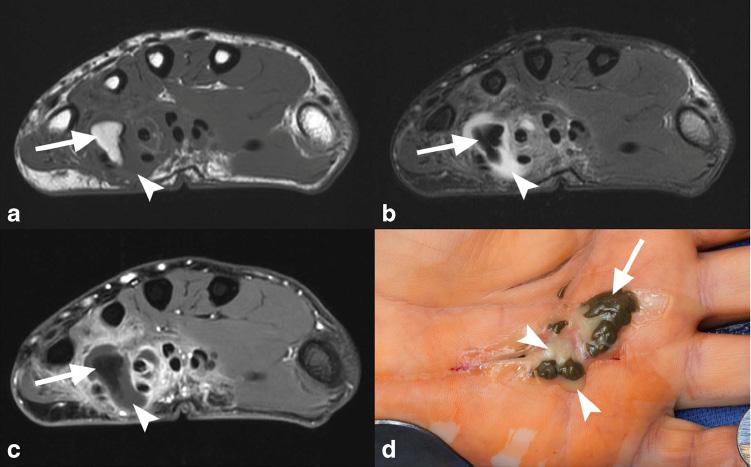
Consequences if untreated or inadequately treated
Common themes in literature through the past century are non-recognition of the severity of the injury by both patients and clinicians. This leads to delayed presentation of patients who do not understand the significance of the injury, when compartment pressures may have been raised for hours. Attending clinicians may lack experience or education in treating such injuries which can lead to a sense of non-urgency in management. This leads to delays in surgical decompression and washout; further compounding the toxic effects of the injected material, increased pressure at the injections site which results in tissue necrosis and longterm morbidity.
If untreated or inadequately treated, the affected areas remain intensely painful as the tissue undergoes necrosis, which often will be complicated by secondary infection. Delays in treatment lead to substantially worse outcomes.
As a result of ischaemia there may be a substantial loss of soft tissues, including amputation if digits are involved. Extensive fibrosis and scarring may lead to contracture limiting the function of the affected limb or digit. If the injected fluid remains in the tissue granulomas of varying sizes will likely form and drainage through sinuses may occur weeks to months after injury as can be seen in Figure 5.
Amputation rates
High pressures are associated with a greater likelihood of amputation. Table 2 shows the reported rates of amputation with increasing injection pressures. When patients presented with altered perfusion at the time of initial assessment, it was associated with amputation 4
Presentation
The ‘typical’ presentation is a male in their 30s who has an isolated injury of their non-dominant upper limb and this is usually of the index finger. This reflects the manual nature of work associated with the use of the equipment that utilises liquids held in high pressures. However, other more unusual anatomical areas have been reported to have had high pressure injection injuries. These include the face, neck, spinal cord, thorax and even the perineum.
The main circumstances leading to highpressure injection injuries are inattention, misuse and material failure and this has consistently been reflected across the literature.
The patients feel a sharp sting at the point of injury with immediate swelling. However, as the wounds are pin-point and innocuous little attention is paid to the injury unless they have had prior education. This often leads to delay in presentation of hours to days and is usually due to pain that develops at that time.
Initial assessment and management
Recognition of the injury severity is critical. High-pressure injection injuries should be placed in the same category of urgency as compartment syndrome as lower rates of amputation were seen with decompression and wide debridement <6hrs after injury5
A full history of the mechanism, hand position, type of fluid injected, equipment pressure, distance and nozzle type help define the pattern of injury. Occupation, hand dominance, past medical history, allergies, medication status, smoking history and last meal are all relevant to treatment of patients. Patients should be starved for emergency surgery.
The initial clinical examination should start with neurovascular status of the digits and hand before moving onto tendon function. X-rays should be undertaken to assess for joint involvement and the spread of fluid to aid surgical planning. Figure 4 shows the intercompartmental and dorsal spread. Figure 6 shows the clinical appearances.
Blood tests for, FBC, U&Es, CRP should be undertaken with broad-spectrum intravenous antibiotics started to cover skin organisms and environmental contaminants. Infections are usually poly-microbial and will involve a range of organisms from skin flora to gram-negative bacteria and, if fresh or brackish water is injected, organisms such as Aeromonas or Vibrio may be encountered. It is very important to send samples for microbiology at initial debridement as this is the best guidance for subsequent therapy.
If the fluid injected is toxic, the National Poisons Information Service (Toxbase) advice should be sought to manage systemic effects.
Subspecialty
Injection pressure Amputation rate <1,000 psi 19% 1,000 – 7,000 psi 43% >7,000 psi 95-100%
Table 2: The reported amputation rates with increasing injection pressures. 50 | JTO | Volume 10 | Issue 04 | December 2022 | boa.ac.uk
Figure 5: Late MRI findings and clinical appearance of discharging sinuses within the hand after injection of grease into the palm3 Reprinted by permission from Skeletal Radiology, High-pressure injection injury of the hand: peculiar MRI features and treatment implications. Skeletal Radiol. 2019;48(2):295-9.
Immediate emergency referral to the relevant surgical specialty (usually a Hand or Upper limb surgeon) should be undertaken to attain surgical decompression less than six hours from injury. The management of these injuries are complex and challenging even for experienced hand surgeons with generally poor outcomes and therefore urgent treatment ideally in a dedicated hand unit may give the best chance of optimal outcome.

Surgical management
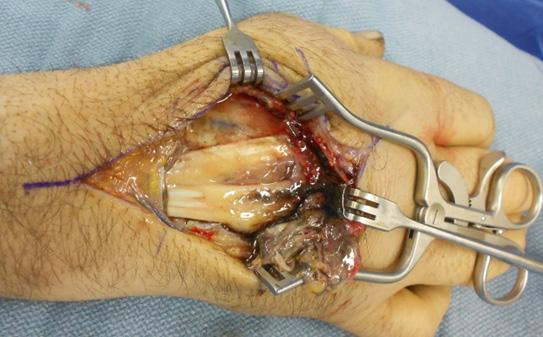
The patient should undergo surgery under general anaesthesia +/- Axillary block (by a competent block anaesthetist) with tourniquet control.
The release of the high-pressure injection injuries should be designed along fasciotomy incisions that will be sufficient to ensure full decompression of all neurovascular structures and all muscle compartments. The debridement and washout should aim to remove as much foreign body as possible; balanced against the morbidity of tissue damage. Figure 6 below demonstrates the extent of tissue release relative to the initial injury.
The addition of Povidone-Iodine 10%, in cadaveric studies, showed greater removal of latex and oil-based paints compared to saline alone7. However there is controversy around its effect on infection rates when compared to saline. In the event of latex or oil-based contaminants which are adherent to tissues it would be reasonable to consider PovidoneIodine 10% at the initial debridement to aid removal of the contaminant followed by low pressure high volume saline to dilute and remove microbes.
48 hours after the initial decompression and debridement, a second look is required to undertake further debridement and washout of any further non-viable tissue before deciding on the suitability of closure.
Post-operative completion of antibiotics with close supervision of wound care and hand therapy are essential to minimising morbidity and maximising the outcome of patients.
Conclusion
High-pressure fluid injection injuries can be devastating and require prompt diagnosis and treatment or they can result in notable morbidity and loss of function. Lack of recognition from patients and inexperienced clinicians compounds the damage. High injection pressures >7,000psi and oil-based paint are associated with an increased risk of amputation.
If one learning point is to be taken away from this article then it should be that these injuries are surgical emergencies and are often underestimated by patients as well as clinicians. Decompression within six hours from point of injury is associated with a reduction in morbidity. n
References
1. Neal NC, Burke FD. High-pressure injection injuries. Injury. 1991;22(6):467-70.
2. Rees C. Penetration of tissue by fuel oil under high pressure from a diesel engine. JAMA . 1937;109:886-7.
3. Collins M, McGauvran A, Elhassan B. Highpressure injection injury of the hand: peculiar MRI features and treatment implications. Skeletal Radiol. 2019;48(2):295-9.
4. Lewis HG, Clarke P, Kneafsey B, Brennen MD. A 10-year review of high-pressure injection injuries to the hand. J Hand Surg Edinb Scotl. 1998;23(4):479-81.
5. Hogan CJ, Ruland RT. High-pressure injection injuries to the upper extremity: a review of the literature. J Orthop Trauma 2006;20(7):503-11.
6. Sharma R, John JR, Sharma RK. Highpressure chemical injection injury to the hand: usually underestimated injury with major consequences. BMJ Case Rep 2019;12(9):e231112.
7. Bascone CM, Sheber B, Dave D, Firriolo JM, Pereira C. Optimal Irrigant in High Pressure Paint Injection Injuries of the Hand. Plast Reconstr Surg Glob Open. 2022;10(1):e4064.
Subspecialty
JTO | Volume 10 | Issue 04 | December 2022 | boa.ac.uk | 51
Figure 6: The clinical appearances of dorsal spread after volar injection of grease into a hand.
Hand partnerships around the world
Jonathan Jones is a Hand and Orthopaedic Surgeon in Peterborough and formerly a medical officer in the Royal Air Force. He has led surgical educational visits to Uganda, Malawi and Sierra Leone and is the current chair of the BSSH Overseas Committee.

For the last 12 years the British Society for the Surgery of the Hand (BSSH) has been supporting and coordinating the development of hand surgery services and education in low income countries (LIC’s). The success of our work was recognised by the global hand surgery community at the recent International Federation of Societies of Surgery of the Hand (IFSSH) Congress held in London 2022. A key component of that success has been working with a variety of groups at home and abroad to create long-term partnerships.
Surgery”. We knew that BSSH members had the skills, knowledge and commitment to make a real and tangible difference in LIC’s. The challenge was to mobilise our resources and members to work together towards this worthwhile cause.
Development 2010 – 2019
Stephen Hodgson has been an Orthopaedic Hand Surgeon in Bolton for 30 years. He is proud to have helped develop the BSSH work in low income countries. Personal involvement has been in Sierra Leone, Sudan, Bangladesh, Tanzania and with the West African College of Surgeons.

Rowa Taha is an Orthopaedic trainee with an avid interest in global surgery. She is chair of the BSSH Overseas Trainees Committee, trainee lead for the BSSH-LION project and past member of IFSSH Young Surgeons Committee.

Why offer education in Low Income Countries (LICs)?
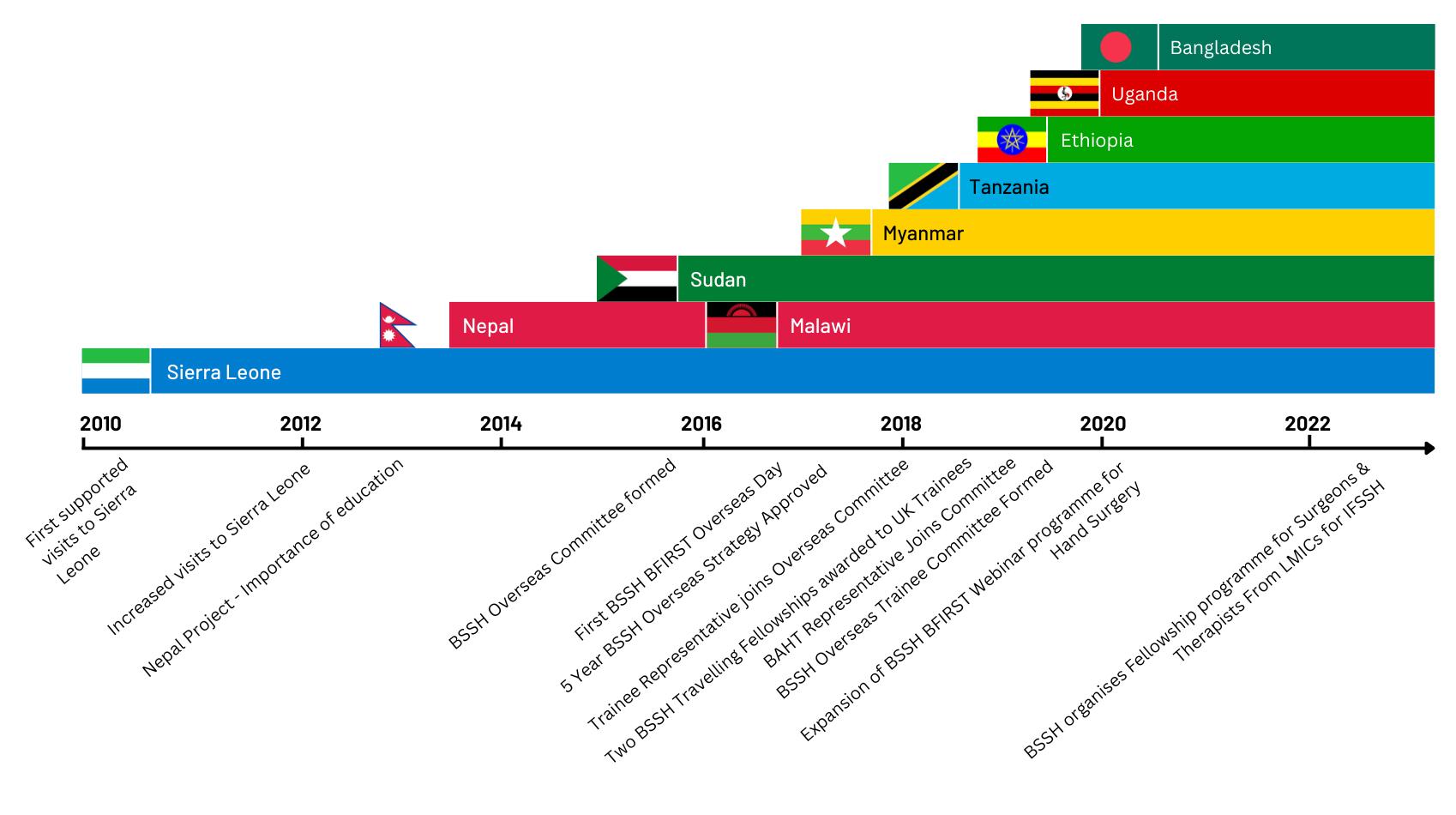
With over five billion people in LIC’s lacking access to safe, affordable surgery1 BSSH saw the need to use its resources globally. The burden of trauma care in LICs is growing including a significant proportion of hand injuries2. The objectives of our society are “to promote the development of Hand Surgery and to foster and coordinate education, study and research in Hand
In 2010 the BSSH Council provided funding to support the first BSSH overseas project to Sierra Leone in 2011. There was considerable interest from BSSH members with many volunteering their free time to get involved. This dedication and the commitment of Council to annual funding of overseas work led to the initiation of educational projects in other LIC’s. As the number of projects gradually increased so did the need to coordinate and share learning. This was met by the formation of the BSSH Overseas Committee in 2016.
By the time overseas visits were suspended in 2020 due to COVID-19, there had been 37 educational visits to ten different LIC’s with participation from 68 BSSH members2. The gradual expansion of our work is indicated by the fact that in 2019 we visited eight different LIC’s, providing face-to-face training to over 475 LIC surgeons and their teams by 23 BSSH members.
Subspecialty
“If you want to go fast go alone, if you want to go far go together” – African proverb
Figure 1: BSSH Overseas Activity Chart 2014 – 2022.
52 | JTO | Volume 10 | Issue 04 | December 2022 | boa.ac.uk
Jonathan Jones, Stephen Hodgson, Rowa Taha and Wee Lam
Wee Lam is a Plastic and Hand Surgeon. He was on the BSSH Overseas Committee and the immediate past chair of the British Foundation of International Reconstructive Surgery and Training (BFIRST), the official outreach arm of BAPRAS. Wee was delighted to lead the partnerships between BSSH and BFIRST which had resulted in several fruitful collaborations and raising of standards for overseas work.

BSSH Partnerships
1) Overseas partners
The BSSH currently has partnerships with surgeons in eight project countries. The Sierra Leone partnership was initiated by Resurge Africa with the goal of establishing a Reconstructive Surgery Unit at the Holy Spirit Hospital (HSH) in Makeni; the first such unit in the country and second in West Africa. BSSH surgical teams made regular visits, delivering surgical treatment and training for theatre, ward and therapy staff. The project was not without its challenges, which included the Ebola and SARS – Cov-2 pandemics, an absence of statefunded healthcare, and a devastating fuel tanker
explosion which led to the redeployment of HSH staff. Despite this, the reconstructive unit remains operational with a functioning Reconstructive service since 2020.
“Learning is a two way process and everyone who visited the HSH in Makeni benefited with regard to their own personal development in addition to supporting the unit”
During the COVID-19 pandemic, BSSH began regular online MDT meetings with the Makeni team and a visit by surgeons and therapists is planned for later this year. After 12 years, this project, against all the odds, has come to fruition and the partnership continues. The
BSSH has also forged a partnership with the West African College of Surgeons (WACS) and with that a programme of online training modules in Hand Surgery.
“It became evident that there was good engagement from the membership and a palpable desire to make a real difference in healthcare in LICs globally”
Partnering with other organisations remains key to our efforts. Other than Sierra Leone, several milestones were also achieved in Malawi. The BSSH was invited by World Orthopaedic Concern (WOC) to deliver a Hand Trauma course for the Orthopaedic Clinical Officers (OCOs) at the Malawian Orthopaedic Association Conference in 2015. The BSSH has since partnered with AO Alliance to run a further course in 2017. In 2019 BSSH and Harvard Global Orthopaedic Collaborative (HGOC) partnered to run combined courses in hand trauma and ankle fracture fixation. The BSSH Malawi project has expanded to offer Hand Surgery courses to Surgical Trainees at the QECH in Blantyre, in partnership with the College of Surgeons Eastern, Central and Southern Africa (COSECSA).

The BSSH has also established projects in Bangladesh, Ethiopia, Myanmar, Sri Lanka, Sudan and Uganda. Educational courses and workshops are strictly needs led, at the invitation of the local surgical unit and fully evaluated. In 2015 the BSSH helped to form the Sudanese Society for the Surgery of the Hand (SSSH). In Uganda, the BSSH partners with the Church of Uganda Hospital Kisiizi and has delivered teaching for trainees and OCOs, and supported paediatric surgical camps. >>

Subspecialty
Figure 2: BSSH Surgical Team visit to Holy Spirit Hospital in Makeni 2011.
Figure 3: BSSH / Interburns Teaching at Connaught University in Sierra Leone 2018.
JTO | Volume 10 | Issue 04 | December 2022 | boa.ac.uk | 53
Other than surgical teaching, we recognise the importance of research. In March 2022, the BSSH delivered an interactive online research methodology course in partnership with the North West Alliance for Africa (NOTAA) and HGOC to Ethiopian trainees, and this will be rolled out to other countries.

The BSSH-BFIRST Webinar series started in 2019 has expanded to offer high quality teaching on the virtual platform. These monthly webinars are delivered in partnership with a LIC and have reached 1,320 delegates in 92 countries. This has led surgeons in Bangladesh to start their own Hand Surgery Webinar Series, offering teaching to surgeons in Bhutan and Nepal.

2) Core partnerships in the UK
The BSSH partners with The British Foundation of Reconstructive Surgery and Training (BFIRST) which is the overseas group of BAPRAS. This alliance has led to joint visits to Tanzania, Myanmar, Sudan and Ethiopia. BSSH surgeons offer Hand Surgery and Orthopaedics of the Upper Limb, whereas BFIRST surgeons offer general plastics, reconstructive surgery, burns, congenital hand and brachial plexus surgery. This synergistic approach between the two organisations has been extremely beneficial in covering the entirety of hand surgery cases encountered.
Other than experienced consultant volunteers, the BSSH has a separate Overseas Trainee Committee which is extremely active and utilises links with other UK trainee organisations such as Global Anaesthesia, Surgery and Obstetric Collaboration (GASOC), the British Orthopaedic Trainees Association (BOTA), NOTAA and the BFIRST Trainees Committee to forge partnerships with trainee organisations around the world. This has improved the connectivity with surgeons in training globally and enhanced the productivity of our overseas work especially via the BSSH-BFIRST webinar series. The BSSH
also works closely with the British Association of Hand Therapy (BAHT), and the hand therapists are an integral part of the visiting teams and educational webinars. The role of therapy in the conservative management of hand injuries is crucial as is their involvement in facilitating post-operative rehabilitation.
3) Collaborative partnerships, home and abroad
Since the establishment of the Overseas Committee, the BSSH has enjoyed a good rapport with a number of well-known organisations involved in education and training globally, including WOC (Malawi), NOTAA (Ethiopia), HGOC (Ethiopia and Malawi), AO Alliance (Malawi), Resurge Africa (Sierra Leone and West Africa), COSECSA (Uganda and Malawi) and Interburns (Sierra Leone).
In Malawi the BSSH now partners with the Lilongwe Institute of Neurosurgery and Orthopaedics (LION) to create an Orthoplastic Hand Unit. During this ambitious five-year programme, UK staff will help provide hand surgery services and training for COSECSA surgeons, forming an integral part of the wider BSSH Malawi Project.

Benefits of collaborative working
The value of partnership and team-working is not a new concept to anyone working in healthcare and it is vital in enabling the delivery of surgical training and care. So it is no surprise that it is the crucial component in supporting healthcare training initiatives globally. There is shared learning from the outset and the enthusiasm for teaching is infectious and stimulating. Welling4 emphasised the improved outcomes achieved in humanitarian missions when multiple organisations are present on the ground.
“Trainees who have been on educational visits to project countries have gained in their confidence, personal growth and team-working skills.”
Taking part in global outreach work is highly rewarding for all involved, with trainees reporting improved confidence, personal growth and team-working skills following overseas visits.
Subspecialty
Figure 4: BSSH AO Alliance Hand Trauma Workshop for Orthopaedic Clinical Officers in Malawi 2017.
Figure 5: The Inaugural Meeting of the Sudanese Society for Surgery of the Hand 2017.
54 | JTO | Volume 10 | Issue 04 | December 2022 | boa.ac.uk
Figure 6: A BSSH BFIRST Webinar Course Poster 2021.
Challenges and solutions in partnership working
Working in partnerships is not without its challenges and some partnerships do not progress or deliver maximum potential. In our view successfully addressing the challenges as they occur has been one of the most rewarding aspects of our overseas work. It is essential to long-term success and provides mutual learning for all parties. Examples of some of the challenges we have encountered are:
1. Differing agendas – as surgeons we tend to have strong opinions and are used to a lead role. Partnership working requires alignment of agendas and agreeing a shared opinion requires shared decision-making and mutual objectives. Agreeing that the primary aim of a project is supporting the local surgeons to meet the needs of their population has been helpful.
2. Logistics – planning, scheduling and resource use is undoubtedly more complex with a larger multidisciplinary team. We aim to include an Orthopaedic Surgeon, a Plastic Surgeon, a surgical trainee and a hand therapist on all visits. It is important that surgeons are prepared to be flexible, empower the local surgeons to take a lead role in visit planning and are aware of the potential negative impact of the visit on the host unit in terms of disruption of routine services and financial costs.
3. Competing egos (both individual and organisational) – for us this is about who gets the credit for the success of a project and may determine the success of future funding bids. Key solutions are to focus on a successful outcome and ensure that credit is shared.
4. Cultural challenges – members of a partnership can come from a variety of professional and national cultures leading to differing approaches. Fortunately, hand surgery has a long track record of harnessing the differences between orthopaedics, plastic surgery and hand therapists.


Summary and conclusion
Team working is crucial to the success of global surgical work, whether it be running a webinar or skills workshop, or delivering surgical treatment. The BSSH endeavours to achieve this and has been flexible to multiple partnerships to find the optimal way to achieve differing tasks. As a diverse orthoplastic society, BSSH members are used to collaborative working. All learn differing skills, knowledge and effective team-working. The emphasis is on synergistic, mutual learning and shared goals and outcomes.
After 12 years, the BSSH Overseas continues to offer training and collaboration with its global partners. In the aftermath of the SARS – CoV-2 pandemic, the BSSH now delivers this using a combination of virtual medium and ‘in country’ visits. Time, energy and commitment is needed to engage in this type of work. There is an old Zambian Proverb which says “you can’t paddle a canoe with one foot on the bank”. In the context of global healthcare, any person or organisation has to engage fully with this type of work otherwise potentially transformative partnerships will neither develop, sustain nor make any significant difference in local healthcare systems.
For further information about the BSSH overseas work please visit www.bssh.ac.uk/ overseas or email secretariat@bssh.ac.uk
Key messages
• To be aware of existing overlapping nongovernmental organisation work streams in global healthcare.
• To understand the importance of assessing the local need in order to target resources appropriately.
• To be realistic about what can be achieved and be flexible to respond to opportunities at short notice.
• To appreciate that partnership challenges can be overcome and that collaborative working is more likely to make a sustained difference in the long-term.
• Global partnership in healthcare is a two-way process. n
References
1. Meara JG, Leather AJ, Hagander L, et al. Global Surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet 2015;386(9993):569-624.
2. Crowe CS, Massenburg BB, Morrison SD, et al. Global trends of hand and wrist trauma: a systematic analysis of fracture and digit amputation using the Global Burden of Disease 2017 Study. Inj Prev 2020;26 (Supp 1):i115-i124.
3. Hodgson SP, Abdelrahman M, Jeme B, et al. Cultural challenges facing UK surgeons providing education in low and middle income countries: How can we use cultural theory to maximise the success of courses overseas? RCSEng Bulletin 2022;104(4):196-200.
4. Welling DR, Ryan JM, Burris DG. Seven sins of humanitarian medicine. World J Surg 2010;34(3):466-70.

Subspecialty
Figure 7: Global engagement - BSSH BFIRST Webinar Series 2019 – 2022 (1,320 delegates in 92 countries).
JTO | Volume 10 | Issue 04 | December 2022 | boa.ac.uk | 55
Figure 8: Therapy Splinting Photos in Malawi and Uganda.
For anyone who met Gwyn Evans, the lasting memory will be of his kindness, modesty, good humour and humanity. For anyone that worked with him, the memory will also include his surgical skill, knowledge and diligent teaching. There are innumerable children, now adults, who owe him a debt of gratitude.
Gwyn was born the son of a minister in North Wales, with the family then moving to Swansea. His religious conviction stayed with him throughout life. Gwyn studied medicine at St Bartholomew’s in London, qualifying in 1967. He impressed the dean of the medical school and became his surgical house officer. Training posts followed in Birmingham, London, Cardiff and then onto the Oswestry rotation in 1974. A fellowship in Newington Children’s Hospital, Connecticut, USA, completed his training. Upon his return to Oswestry, he was ushered into post as a children’s orthopaedic surgeon. This commenced in 1980, along with sessions in the Wrexham Maelor Hospital where he treated adults.
In 1984, he was awarded the ABC travelling fellowship. He held clinics in Bangor, north Wales, and as a proud Welshman was able to ‘siarad Cymraeg’ to his patients.
Gwyn then retired in 2004, but worked part time for another five years.
During his career, he established a progressive children’s unit, introducing the skills and knowledge from his training. He inspired many generations of surgeons with his knowledge and teaching, emphasising the importance of principles when managing complex problems. He became recognised for his abilities and lectured across the world.
Gwyn Amman Evans
24 March 1944 – 20 July 2022
Obituary by Nigel Kiely

Gwyn was fearless in his convictions, and closed a children’s ward upon commencing his consultant post, as long term traction for various conditions was abandoned and the children were liberated!
His commitment to teaching and training was exemplified by posts as royal college tutor, regional speciality advisor, postgraduate clinical tutor for the West Midlands, EPOS council and BOA Council member. However, in the clinic, ward or theatre, he would happily teach doctors, nurses, physiotherapists and anyone who would listen!
None of these extensive achievements would have been possible without the support of his wife Mary, a nurse, horse enthusiast and farmer. Gwyn knew that at work he may be a hero, but at home he was a farm hand!
Retirement did not lead to a quiet life. From 2004 onwards he worked at the Gordon Roberts Hospital in Shillong,

India and the Beit Cure Hospital, Blantyre, Malawi. Mary accompanied him for these trips, and they raised funds for a generator and an intensive care unit. Later, Gwyn used his skills as a volunteer for the local Citizens Advice bureau.
He was diagnosed with pancreatic cancer four years ago, but remarkably maintained good health until a few months before his death. His mind was as sharp as ever to the end.
The British Society for Children’s Orthopaedic Surgery (BSCOS) have announced a travelling fellowship, and the Welsh Orthopaedic Society will have a lecture named after Gwyn.
Gwyn will be remembered in our hearts, and the knowledge he has imparted will forever endure.
Our condolences to Mary; their three children, Alys, Sian, and Owen; and grandchildren. n
56 | JTO | Volume 10 | Issue 04 | December 2022 | boa.ac.uk In Memoriam
Products, Courses and Events
MSK MRI Interpretation Courses
We’re
and
major trauma patients Whenever and wherever you need us
We provide national support and can help with:
• Emergency funding so money is one less thing to worry about.
• Peer support from someone who has been through a similar situation.
• 24hr counselling to provide a confidential space to talk.
15th Trauma & Orthopaedics Update
Val d’Isere, 23-26 January 2023 www.doctorsupdates.com info@doctorsupdates.com +44 (0) 208 7151924
Doctorsupdates 2023, in their 34th year will feature 15th Trauma and Orthopaedics Update. This meeting is unique as it provides interaction between a number of
Find out more about how we can help:
Visit dayonetrauma.org/supporting-you Call 0300 303 5648

Email dayone@dayonetrauma.org Follow @dayonetrauma
Together, we will provide #MoreTraumaSupport
Charity number 1194227
different specialities: orthopaedics, anaesthetics, critical care and pain, emergency medicine, radiology, plastic surgery, dermatology and general practice. We also invite speakers from other specialties like haematology, neurology, rheumatology to contribute to our education.
The programme is suitable for consultants and senior trainees. The format is informal and sessions
Forthcoming courses via Zoom:
MSK MRI for Beginners Course Covers: MRI of knee, shoulder and lumbar spine Date: 28th January 2023

Further MSK MRI for Beginners Course Covers: MRI of hip, elbow, ankle and cervical spine Date: 25th March 2023
include trauma and elective surgery, multidisciplinary sessions and a free paper competition for trainees.
Each day concludes with a lecture of general interest by an eminent guest speaker.
We have an excellent orthopaedic faculty lined up and the programme, when confirmed, will be available at www.doctorsupdates.com

For details please visit: www.mskbeginner.com
For a registration form please email: admin@mskbeginner.com
Web: https://uk.unitedorthopedic.com Email: uk.service@unitedorthopedic.com Telephone: +44 (0) 1827 214773

For over 25 years, United Orthopedic has been a leading international designer, manufacturer, and distributor of versatile orthopaedic solutions that deliver world-class orthopaedic joint replacement implants which have made life better for hundreds of thousands of patients needing hip and knee replacements. Find out more about our USTAR II Primary and & Revision Hinge Knee and Limb Salvage System which is part of the United Orthopedic portfolio of arthroplasty and limb salvage products.
• Platform-based approach - consistent design philosophy allows a platformbased approach to provide surgeons flexibility for a wide range of procedures
• Demand-matching - includes a wide range of product options for demandmatching to optimise solutions based on patient needs

• Advanced surgical technologies - builds on proven design philosophies with advanced surgical technologies to help deliver reproducible clinical outcomes and a streamlined procedure
We specialise in casing and packaging solutions for orthopaedic implants, medical equipment and have supplied many of the world’s leading medical organisations.
We specialise in casing and packaging solutions for orthopaedic implants, medical equipment and have supplied many of the world’s leading medical organisations.
Our flight cases are made in our 70,000 sq ft factory in the UK using the highest quality materials to ensure that your vital
Our flight cases are made in our 70,000 sq ft factory in the UK using the highest quality materials to ensure that your vital equipment is fully protected in transit.

equipment is fully protected in transit. We design and manufacture cases to your exact specification. A range of pull-out drawers, shelves, lift-out trays, doors and shutters can be integrated into the case. With an in-house design team and advanced computer aided design and CNC routing facilities, we can produce custom foam interiors to




house implant samples, instruments and any other equipment.

Trifibre Ltd 17 Boston Rpad Gorse Hill Industrial Estate Leicester LE4 1AW
Telephone: 0116 232 3166 Email us: info@trifibre.co.uk Web: www.trifibre.co.uk
We design and manufacture cases to your exact specification. A range of pull-out drawers, shelves, lift-out trays, doors and shutters can be integrated into the case. With an in-house design team and advanced computer aided design and CNC routing facilities, we can produce custom foam interiors to house implant samples, instruments and any other equipment.
Trifibre Ltd 17 Boston Rpad
Gorse Hill Industrial Estate Leicester LE4 1AW
Telephone: 0116 232 3166 Email us: info@trifibre.co.uk Web: www.trifibre.co.uk

JTO | Volume 10 | Issue 04 | December 2022 | boa.ac.uk | 57
here for you
your
Step-by-step | Interactive | Case based
Who’s looking out for you?
Protection that fights your corner
Outstanding careers deserve uncompromising support. That’s what we’ve always believed. Membership gives you the right to request indemnity for cases arising in a range of different situations. And with the largest medicolegal team of any medical defence organisation, we’re always ready to fight for your reputation.

For just £549 can feel safe in the support membership brings. We also offer competitive, tailored prices for consultants working in Private Practice.
See how we’r
The Medical Protection Society Limited (“MPS”) is a company limited by guarantee registered in England with company number 00036142 at Level 19, The Shard, 32 London Bridge Street, London, SE1 9SG. MPS is not an insurance company. All the benefits of membership of MPS are discretionary as set out in the Memorandum and Articles of Association. MPS® and Medical Protection® are registered trademarks.
2111122727: 02/22
























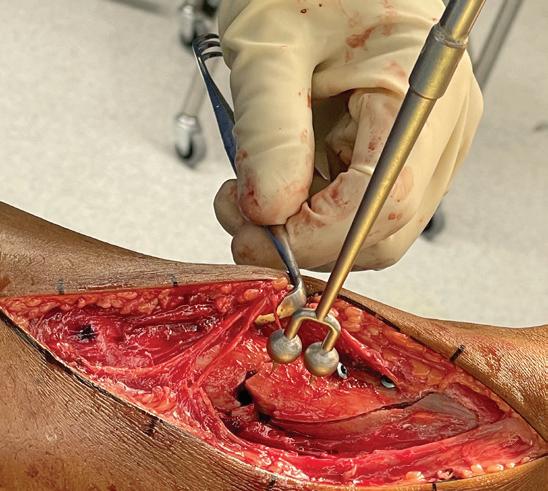

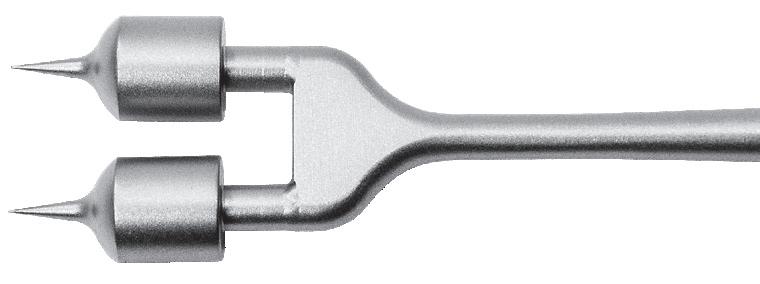
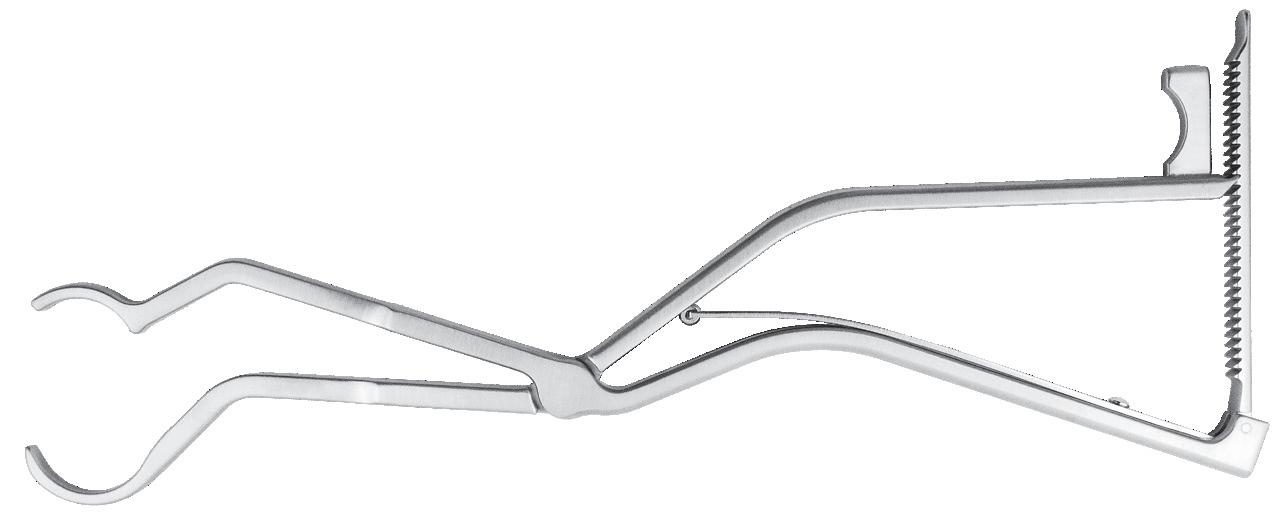










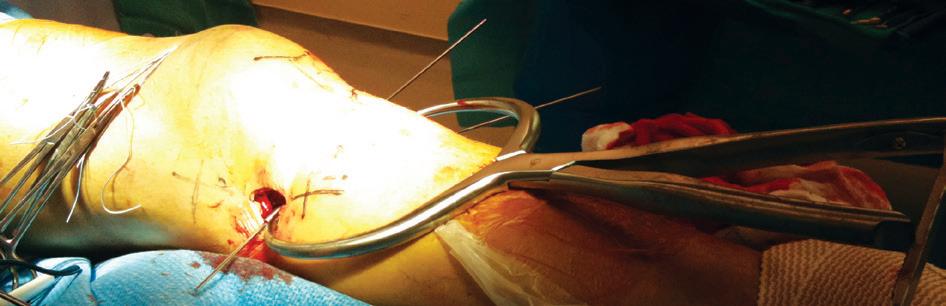

































































































































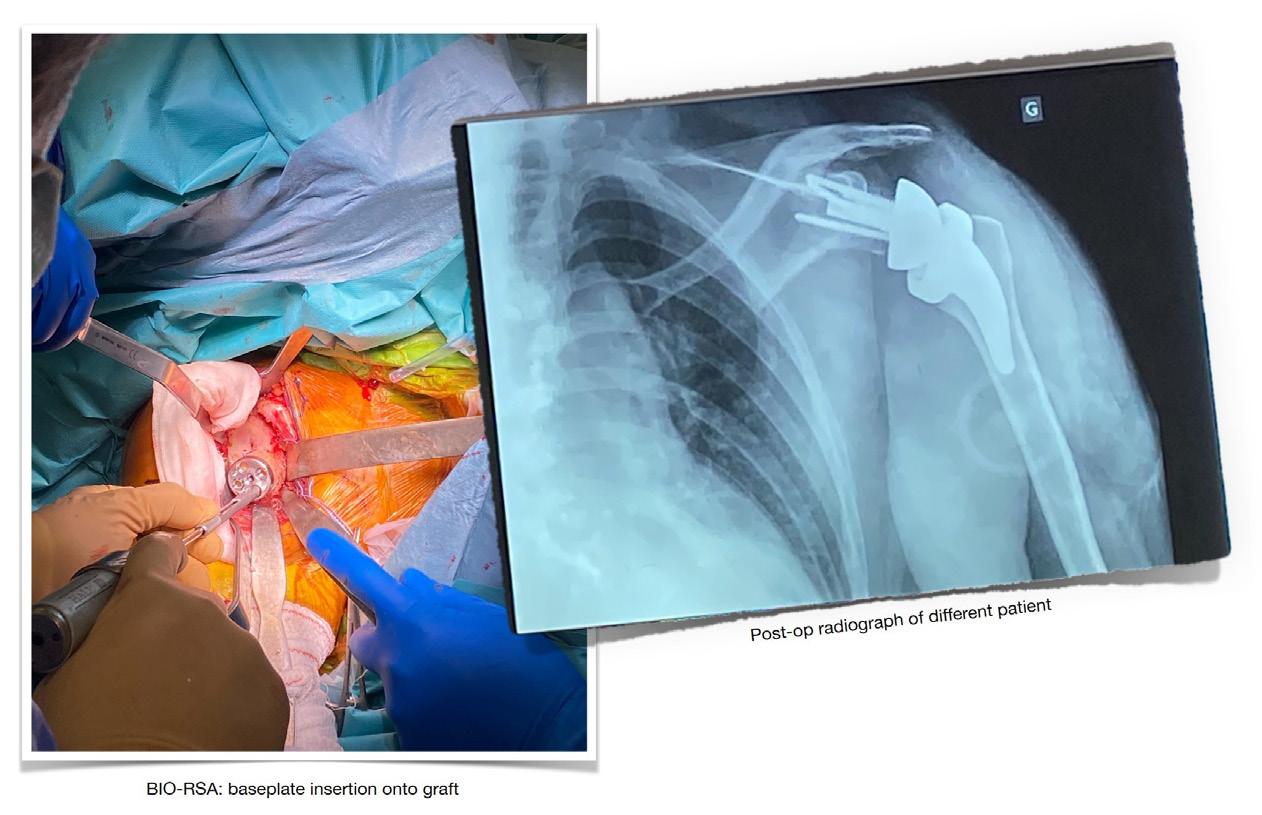
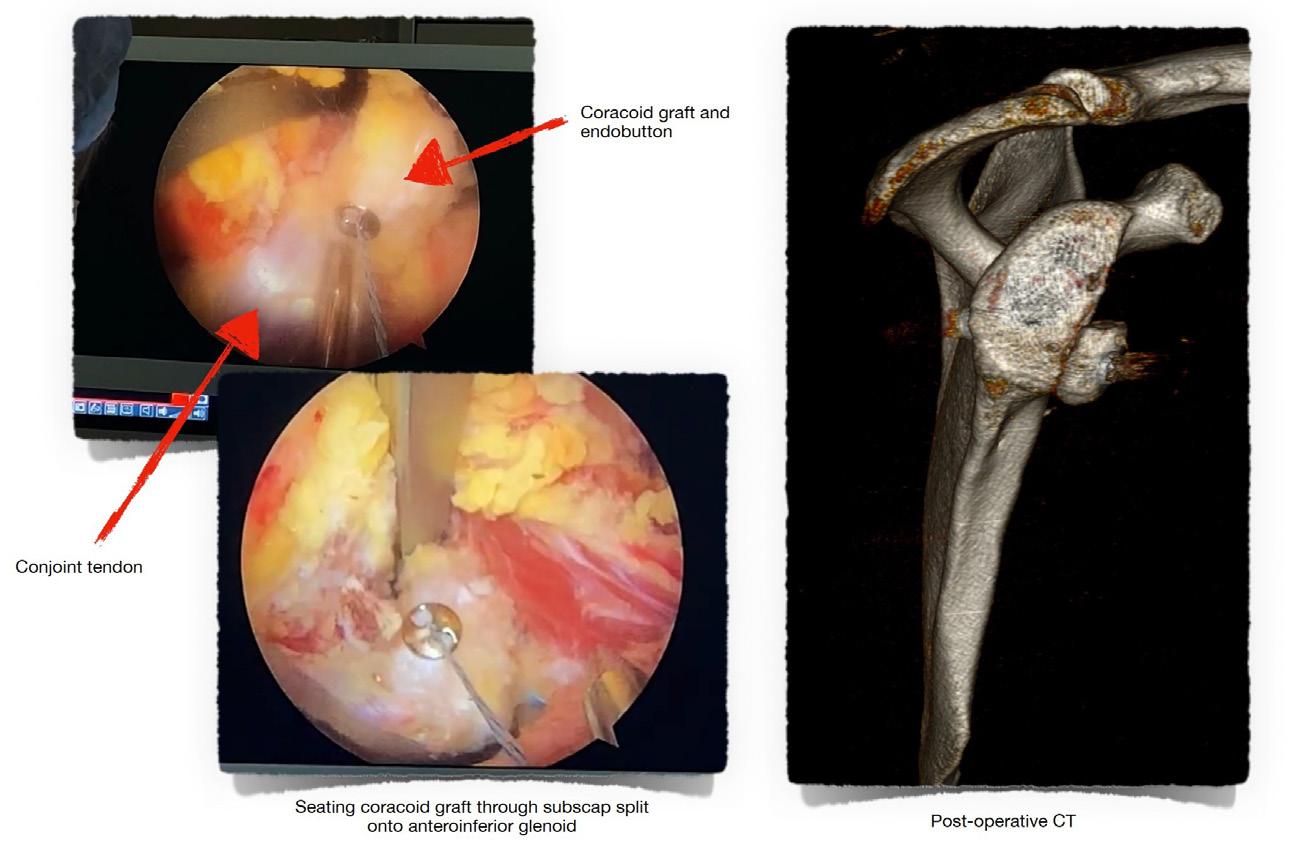













































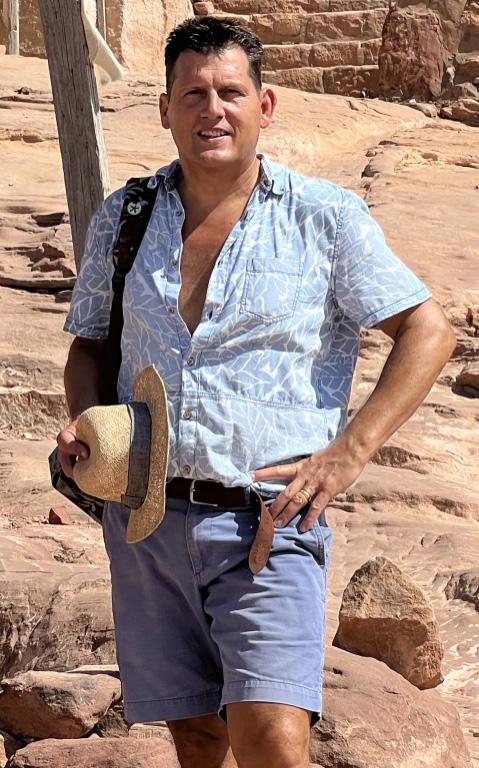




















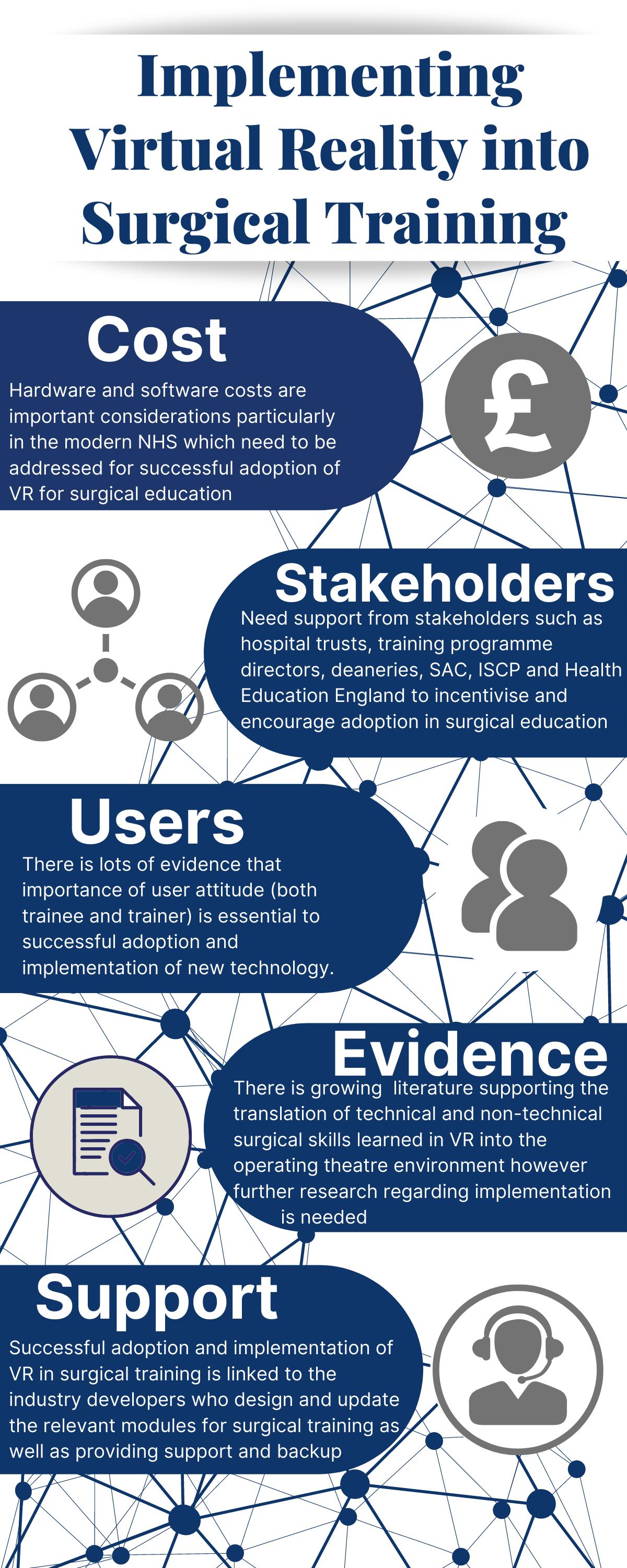
 Sulaiman Uppal
Sulaiman Uppal












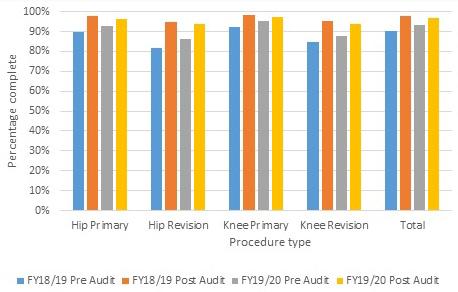



 An AK MEDICAL Company
Category Manager Rebecca Green: rebeccca.green@jri-ltd.co.uk
Innovative Custom Orthopaedic Solutions (ICOS) by JRI Designed and fabricated bespoke implants that help patients return to anatomical wellness.
An AK MEDICAL Company
Category Manager Rebecca Green: rebeccca.green@jri-ltd.co.uk
Innovative Custom Orthopaedic Solutions (ICOS) by JRI Designed and fabricated bespoke implants that help patients return to anatomical wellness.
 Ad Gandhe
Ad Gandhe



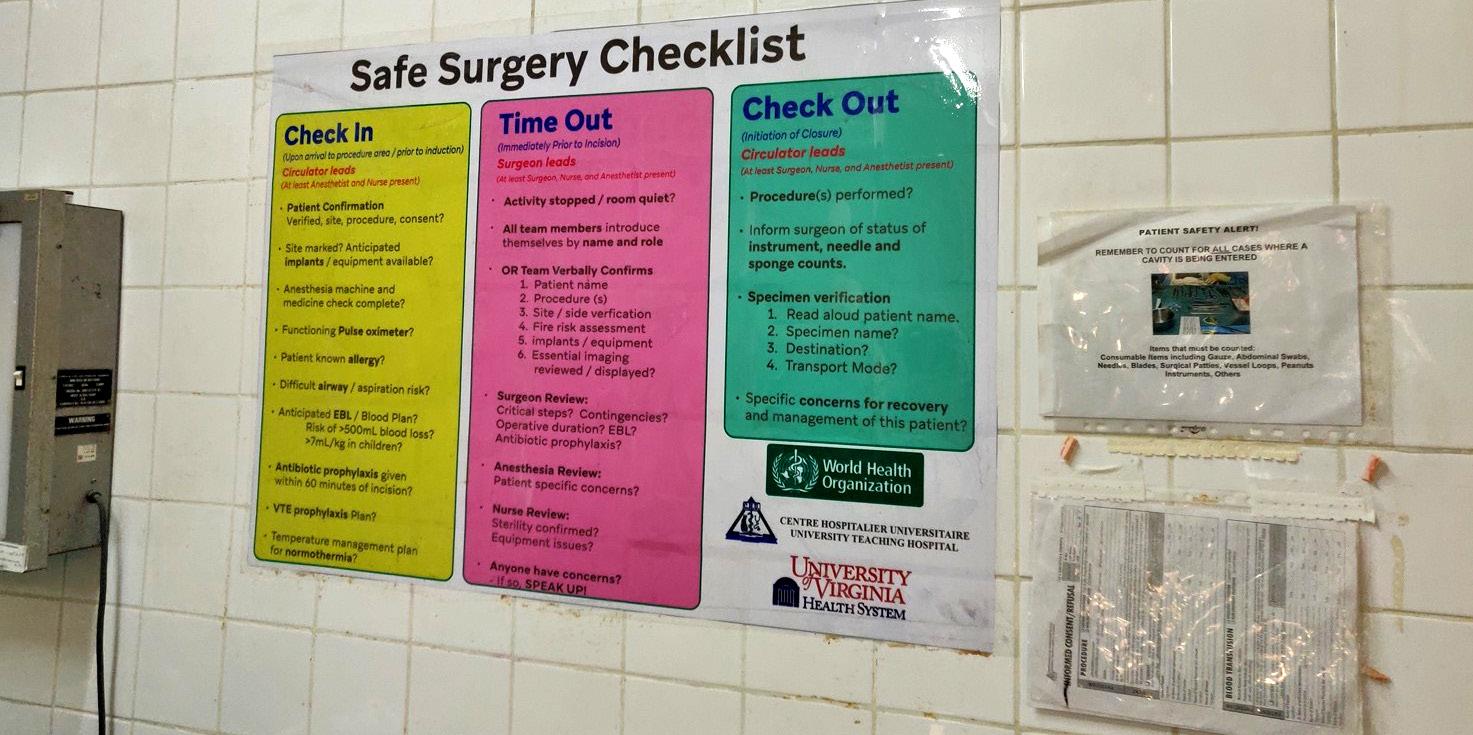

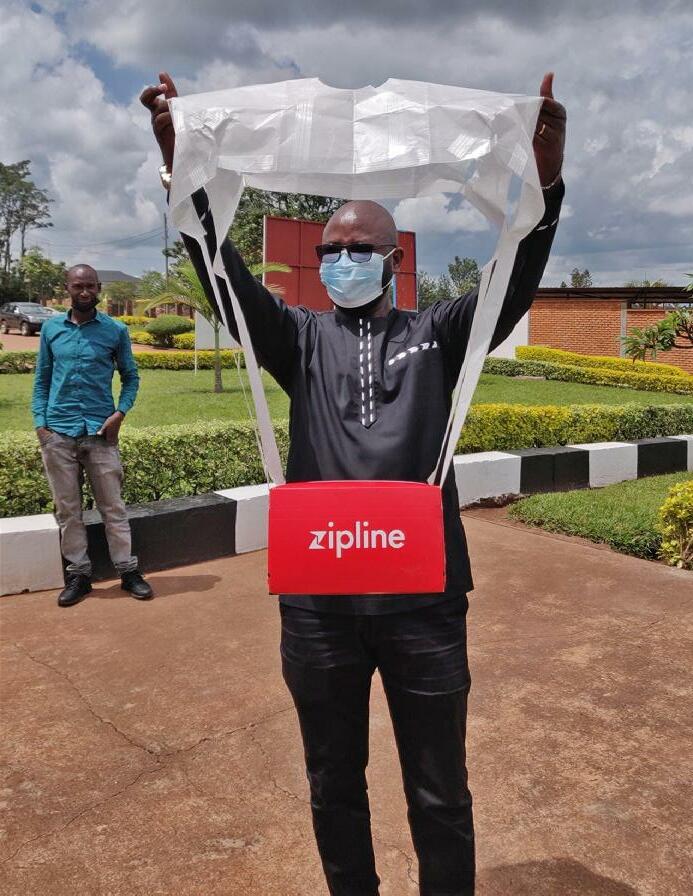
















 Jonathan Hobby
Jonathan Hobby









 Guang Yim, Jens Roesner, Warren Hammert, Adeline Clement, Patrick Gillespie and Oliver Stone
Guang Yim, Jens Roesner, Warren Hammert, Adeline Clement, Patrick Gillespie and Oliver Stone