

Matters of the Heart
Why getting the details right in cardiovascular care – from BP cuffs to ECG leads – makes all the difference in patient outcomes.

Matters of the Heart
Clarity at the Heart of Care
Cutting Down on Repeat ECGs in Primary Care
Getting Blood Pressure Right
` PHYSICIAN OFFICE LAB
PAMA is Your Friend National reimbursement, CMS innovation, and the three elements of value guiding lab sales forward.
DISTRIBUTION
A Start-Up With Old-School Values Inside the launch of HSS Medical Supply. ` LEADERSHIP

` TRENDS 32 An Unsustainable Equation
Flat reimbursement, rising wages and persistent turnover are forcing physician practices to rethink how they staff, support and sustain their workforce.
` INFECTION PREVENTION
Heroes of Infection Prevention
Infection preventionist shares her career journey and what led her to be recognized nationally for her clinical accomplishments.
` POST-ACUTE 46 Advancements in Patient Nutrition
Exploring the nutritional delivery space in recognition of Feeding Tube Awareness Week in February.
` TRENDS
50 Eliminating Barriers to Medical Supplies
MedWish Medworks merges healthcare access, sustainability, and volunteerism into one mission – ensuring every person has the chance to live a healthier life. ` IDN INSIGHTS
Clinicians and Supply Chain – Turning Dodgeball into Volleyball
Conversation, collaboration works with sportsmanlike conduct.
Cardiac Rehabilitation Week 2026 highlights the importance of ongoing care and support after a cardiac event.
Medical supply chain issues to watch in 2026.
Relationships Still Drive Medical Distribution
In an industry transformed by technology, trust between distributors and manufacturers remains the most powerful driver of long-term success.

While many people associate February with chocolates, cards and reservations made weeks in advance, it is also a perfect time to reflect on the relationships that truly matter in our professional lives. In medical distribution, few relationships are more important than the ones we share with our manufacturing partners.
This industry was built on relationships, real ones. Long before dashboards, CRMs and digital ordering platforms, success was driven by trust, credibility and a firm handshake. While technology has made our jobs faster and more efficient, it has not changed the core truth of how business is won and retained. People still buy from people. And more importantly, people still buy from people they trust.
In fact, study after study continues to show that the number one reason someone makes a purchasing decision today is because a product or solution was recommended by a friend, family member or trusted advisor. That holds true whether the purchase is made through a distributor, directly from a manufacturer or even online through Amazon or other digital outlets. The channel may evolve, but the human element remains constant.
For distribution sales representatives, teaming up with manufacturing counterparts in the field is no longer optional, it is essential. When those relationships are strong, aligned, and intentional, everyone wins. Manufacturers gain better visibility and execution. Distributors gain stronger support, deeper product knowledge and greater credibility with customers. Most importantly, the end user receives better solutions, better service, and better patient outcomes.
Strong partnerships are not built overnight. They are built through shared goals, open communication, mutual respect, and a genuine interest in helping one another succeed. That means planning calls together, understanding each other’s priorities, and showing up consistently not just when a deal is on the line, but throughout the year.
My challenge to you for 2026 is to find ways to utilize one another every month, whether that is a ride-day together, or a lunch and learn, or just simply brainstorming on ways to grow your sales.
Success in this industry has never been a solo effort. It is, and always will be, a team sport. This February, let’s show a little extra appreciation for the partners who help us reach our goals and remember that strong relationships remain the most powerful tool we have.
Dedicated to the industry for the past 30 years,
R. Scott Adams Publisher
editorial staff
editor Graham Garrison ggarrison@sharemovingmedia.com
editor-in-chief, Dail-eNews Jenna Hughes jhughes@sharemovingmedia.com
content creator Pete Mercer pmercer@sharemovingmedia.com
art director Brent Cashman bcashman@sharemovingmedia.com
circulation Laura Gantert lgantert@sharemovingmedia.com
sales executive Aili Casey acasey@sharemovingmedia.com (404) 625-9156
publisher Scott Adams sadams@sharemovingmedia.com (800) 536.5312 x5256
founder Brian Taylor btaylor@sharemovingmedia.com
Subscriptions www.repertoiremag.com/subscribe or (800) 536-5312 x5259
Repertoire is published monthly by Share Moving Media 350 Town Center Ave, Ste 201 Suwanee, GA 30024-6914 Phone: (800) 536-5312, FAX: (770) 709-5432; e-mail: info@sharemovingmedia.com; www.sharemovingmedia.com

Act fast this flu season
Explore our rapid solutions
Act fast this flu season
Navigate this respiratory season with SOFIA™ 2
Explore our rapid solutions
Delivering accurate, objective and automated results in as few as 3 to 15 minutes.
Revolutionizing rapid diagnostics
Navigate this respiratory season with SOFIA™ 2
SOFIA 2 Assays
RSV
Influenza A+B
Delivering accurate, objective and automated results in as few as 3 to 15 minutes.
• Flu + SARS Antigen
SARS Antigen
• SARS Antigen+
Strep A+
Revolutionizing rapid diagnostics

SOFIA 2 Assays
RSV
• Influenza A+B
Flu + SARS Antigen
• SARS Antigen
SARS Antigen+
• Strep A+
For more information on QuidelOrtho’s rapid flu solutions, scan the QR code or contact your QuidelOrtho representative.
For more information on QuidelOrtho’s rapid flu solutions, scan the QR code or contact your QuidelOrtho representative.
PAMA is Your Friend
National reimbursement, CMS innovation, and the three elements of value guiding lab sales forward.
 It’s February, and there are a few things you can count on during February each year: Groundhog Day, Valentine’s Day and my annual column on the Protecting Access to Medicare Act (PAMA). After last year’s column suggesting that PAMA was at a dead end, you might have assumed there would be no further news on PAMA. I did. But it turns out that since PAMA has not been repealed by an act of Congress, it will still be around in one fashion or another.
While decreases in reimbursement under the Clinical Lab Fee Schedule (CLFS) managed by the Centers for Medicare and Medicaid Services and mandated by PAMA have been on hold since 2020, Congress has avoided passing the SALSA (Saving Access to Lab Services) Act which would have made meaningful changes to
PAMA. These modifications to PAMA would have assured that data collection truly represented the types of labs eligible to report payment data (reference labs, hospital outreach labs and physician office labs) more equitably. The best available data indicates that while private reference labs represent only about 50% of all

By Jim Poggi
lab tests performed in the U.S., PAMA calculations weighted their reimbursement at 90% of the data they collected to determine the baseline of private lab reimbursement. It was this highly skewed baseline against which cuts in CLFS reimbursement were to be measured, with the goal of closing the gap between the CLFS

reimbursement and private insurance. In addition to making the data collection more equitable by weighting different types of labs more accurately, the SALSA Act would also have increased the reporting cycle for reimbursement by labs from every three years to every four years, reducing the burden on labs reporting payment information. It also proposed to create “guardrails” against payment increases or decreases to avoid dramatic impacts on laboratories, ensuring more stable and equitable reimbursement. However, rather than pass the SALSA Act, Congress has created an annual patchwork of legislative work arounds, including the Lab Access to Beneficiaries Act (LAB) in 2019, the CARES Act (Coronavirus Aid, Relief, and Economic Security Act) in 2020 and various “add on” legislative addenda to annual budget bills since then. As of this writing, PAMA was again on hold through the end of January, 2026 pending a longer term federal budget which was pending at that time. As you read this column in February, I anticipate that Congress will once again have added a temporary fix to PAMA within the new federal budget rather than enact the SALSA Act. In the event SALSA is passed, I will alert you in a future column and present the changes in the CLFS that would result from this more comprehensive action. So, then, where does this leave us? There is no question that the improvements anticipated under the SALSA Act would result in a distinct and more permanent solution than the annual “kick the can down the road” legislative patchwork
we have experienced, but delays in further PAMA cuts to the CLFS are welcome nonetheless. Moreover, when we look at CLFS reimbursement compared to private insurance and do our work as valued consultants to identify and communicate the economic value of lab testing, it turns out that PAMA and the CLFS truly is our friend. Follow along with me while I provide my data and logic for this conclusion. I am willing to bet you will find a few surprises, and information you can share as high value consultants to your customers.
profit they make. Then your solution and your reputation with this customer and others they may influence is on the line. Take it from me and hundreds of other successful distributor account managers who have abandoned selling lab on profit: use this technique at your peril and do not be surprised if the results end up with unhappy customers and lots of your time spent justifying their results. Stick to the three elements of value (more on this later) and avoid the inherent dangers in selling on profit. You will be glad you did.
From patient encounter to the request for lab tests, to performing them, counseling the patient and reporting results into EMR, the shortest time frame with the most direct path to having the data available wins every time.
Before we dive into the specifics of why PAMA and the CLFS is our friend, I need to provide a note of caution on selling on profit. While this selling technique was popular and largely successful from the 1980s through the early days of the current century, it is fraught with danger in today’s market. Courting customers mainly motivated by profit leads inevitably to the customer question, “Why am I not making the amount of money you said I would?” And discussions veer away from the true total benefits of in-office testing to analysis and review of customer financial data. It is a rare customer who is primarily motivated by profit that will be satisfied with the results, no matter how much
The CLFS value story:
Most CLFS reimbursement is now standardized nationally
This may not sound like a big deal for newer distribution account managers who joined their company after the CLFS instituted national reimbursement for most tests, but, for those of us who were around when there were more than 50 CLFS carriers and a crazy quilt of reimbursement rates for the same test, this is a welcome and meaningful change.
Just to make the point, I pulled up my copy of the 2015 CLFS CPT payment schedule. There were 57 different carriers with individual CPT payment rates! In my research, I
looked up influenza, CPT code 87804(QW). In 2015, the payment rates peaked at $16.32, but they ranged from $12.63 all the way up to $16.32 with multiple carriers below the high value of $16.32. At that time, manufacturers and distributors needed to alert their field sales teams that reimbursement for influenza varied and to be careful to check with local carriers if the distributor account manager chose to let the customer know the approximate reimbursement they could expect. Many other tests followed this same pattern, and it caused confusion at the manufacturer, distributor account manager and customer level. Fast forward to the current CLFS reimbursement schedule, and influenza CPT code 87304(QW) is national (no variation by carrier) and reimbursed at $17.00.
The extent to which CPT code reimbursement has become national is significant. Of the current 2,149 lab CPT codes, 2,032 of them or nearly 95% are standardized nationally. What an improvement! In contrast, there are only 117 local CPT codes and most of them are for CLIA high complexity molecular assays. Bucking the trend toward standardization of CPT code reimbursement, CMS went backwards in my opinion when they once again began initiating local coverage for new CPT codes following the COVID pandemic. While disappointing, the only local coverage determination CPT code that should impact us to any extent is G0567(QW), screening test for hepatitis C. So, for the most part, the tests we usually sell are reimbursed on a national scale.

While many private carriers classify new molecular tests covered by CLFS as “experimental” and do not cover them, the CMS has adopted a different approach and adds new tests frequently.
In contrast, lab CPT code reimbursement from private carriers is as complex and difficult to understand as ever. Reimbursement within the same carrier for any CPT code varies by geography, and reimbursement among carriers for the same CPT code varies widely. There has been no improvement on the private payer side to standardize reimbursement, and I do not see current market forces that will change this.
The CMS value story: Coverage for new molecular
assays
Our portfolio of molecular tests began with respiratory assays and continues to grow. CMS covering a broader range of molecular tests is a benefit to the lab market overall. This trend points to the fact that CMS understands and fosters innovation in the lab business and rewards it with new CPT codes. As a result, CMS is far ahead of private payers in rewarding innovative new



lab tests and I expect this trend to continue. From an overall value to the healthcare system perspective, I believe this is a healthy approach. While many private carriers classify new molecular tests covered by CLFS as “experimental” and do not cover them, the CMS has adopted a different approach and adds new tests frequently. There are many good examples, but a couple of specifics will make the point. CPT code 0497U is an assay to determine the risk of prostate cancer, the most common cancer in men and number two behind breast cancer for all cancers. It is reimbursed at $3,873 nationally in the CLFS. Why does this matter and what does the future hold? It matters since it is consistent with the latest trends in technology, specifically including the advent of data mining tools including AI. Overall, creating reimbursement for these new tests acknowledges innovation and stimulates manufacturers to continue meaningful innovation. Remember when we were talking about “big data” just a few years ago and the buzz about AI now? Well, the data bases are getting larger and new data mining techniques are making it easier to use lab tests in two novel ways. First, there are new tests to estimate “predisposition” to develop a specific cancer, typically performed when a patient has a family history of prostate, breast or colorectal or other cancer. These tests can help as part of a strategy to determine which patients need to be followed more closely for specific cancers if they show the same genotype as family members who have experienced specific cancers. This is a new way to provide even earlier surveillance of patients and prevent disease. Secondly, there

Private insurance has led the way to reductions in reimbursement for lab tests. Do you know the proportion of your customers’ patients covered on Medicare, Medicaid and private insurance? You should.
are tests that compare the genotype of a patient’s tumor with vast data bases of other patients with similar cancers. The outcome here is to attempt to estimate whether the progression of this patient’s cancer will be slow or rapid and to understand which therapies will be most successful. These two uses of molecular data in combination with utilization of massive data bases has the possibility to initiate cancer diagnosis earlier and make treatment more precise and effective. CMS’ decision to add these new tests early once reasonable proof of their usefulness has been established is a meaningful new way to harness innovation to improve patient health. Private insurance companies are lagging well behind the federal government.
The CMS Story: Recognizing the value of new molecular assays
It’s not just the breadth of new molecular assays where CMS is leading the pack. They are also assigning significant reimbursement to these assays. There are now 186 lab CPT codes that reimburse more than $1,000. Most of them will not soon be available in the physician office market, but they point to advances in lab technology that will benefit the healthcare system, improve patient health and reduce healthcare costs. As usually happens, I expect at least some of these tests to migrate to the physician office. At the same time, I predict that private data base companies will begin
offering analytical services to the physician office market (some already have) based on a panel of molecular tests. There is already a panel of prostate assays using a combination of three different tests to predict whether a patient has prostate cancer or just a more benign condition. There is every reason to believe the combination of new tests and new ways to interpret them will lead the way in cancer diagnosis and treatment in the future. I am confident an increasing number of these assays and services will be coming to the physician office lab.
At this point, you are probably wondering: OK, what does this mean to me?
Key takeaways: CMS/CLFS/ PAMA: expect temporary halts in implementation of PAMA to continue. Be sure to check in with the Clinical Lab Fee Schedule from time to time, discuss the information with your colleagues and trusted lab manufacturers and become familiar with it. This, alone, will set you apart
from others: cms.gov/medicare/ payment/fee-schedules/clinicallaboratory-fee-schedule-clfs. This is a tremendous resource for you and your customers.
My view of the future is a continuing merger of data mining tools and lab tests with predictive measures becoming more common. Keep an eye on this trend.
The three elements of value will continue to be our “north star” now and in the future, no matter what direction new assays and data base mining methods take.
Clinical Value: Clinical value remains the greatest single reason to perform lab tests in any setting, but most particularly, in the physician office and point of care. The most appropriate reason to perform any lab test is to provide data “to initiate or modify a patient treatment program.”
Workflow Value: From patient encounter to the request for lab tests, to performing them, counseling the patient and reporting
results into EMR, the shortest time frame with the most direct path to having the data available wins every time.
Economic Value: PAMA certainly adds challenges here, even with reductions in CLFS rates postponed yet again. But, is PAMA the biggest economic risk? Probably not. Private insurance has led the way to reductions in reimbursement for lab tests. Do you know the proportion of your customers’ patients covered on Medicare, Medicaid and private insurance? You should.
The three elements of value will all point you and your customers in the direction of the most meaningful tests for them and their patients. Are you using the three elements of value in your daily customer consultation? If you are not, beware. Your competition may be. Get ahead of the pack and become familiar with the three elements of value and use them as your guidepost to successful lab sales!
A Start-Up With Old-School Values
Inside the launch of HSS Medical Supply.
 For Pete McCann and Patrick Kiss, the spark that ignited HSS Medical Supply didn’t come during a strategy retreat or a market analysis session. It arrived on “a simple phone call on a random November afternoon.”
At the time, McCann and Kiss were wrapping up the buildout of an orthopedic MSO. Then the unexpected happened. “A former employee of mine called and explained that he and many other people were displaced from their organization,” McCann said. “A team of talented, resolute sales and operations people who gave 25+ years to the industry were now looking for a new home.” For most startups, assembling a proven salesforce is a multi-year challenge – a prerequisite to scaling that often slows progress before it begins. That day, McCann explained, “I had the key to success handed to me. Now the hard work of building an operational structure to support them, something I have done several times before, was my new mission.”



Re-igniting a family culture
For McCann, the mission was bigger than logistics and process design. His vision for HSS Medical Supply is rooted in something more personal, a sense of belonging he felt early in his life.
“The family culture starts with a feeling, the feeling I had when I went to work with my dad in his company,” he said. “You feel welcomed, excited, and part of something that could be forever in your heart.” Many in distribution, he added, grew up with that same sense of purpose and pride. Reestablishing that spirit became central to the new company’s identity. “For many of our employees we
Pete McCann
Patrick Kiss


do not need to re-create it, we just need to re-ignite it – the feeling never leaves, it is why so many of us stay in this profession.”
And for McCann, it’s come full circle. “Giving my teenage son the same opportunity I had, sweeping floors and picking orders, is a full-circle cultural experience that has been the fabric of this industry,” he said. “The next generation is out there and ready to carry that cultural torch, if given the opportunity.”
A financial mindset meets a relationship-driven business Kiss, whose career began in finance and accounting, brings the structure and discipline that help turn vision into sustainable growth. “My foundational knowledge of finance and accounting, coupled with having built an Orthopedic MSO, gave me a perspective of how to build and scale the operation,” he said.
Startups face a delicate balance between investment and stability – especially in distribution, where inventory demands can drain cash quickly. Kiss embraced the challenge. “The challenge in this was to balance the start-up expenses and the inventory turns to create a pathway for positive cash flow to support the start of the company,” he said. “We spent months using data from Pete’s former companies to chart a logical growth plan to utilize cash effectively.”
With that structure in place, the founders focused on the gap they believed had widened across the industry. “The main gap has been the shift away from relationships with the customers and the sales team,” they explained. In their view, the industry’s historic strength – personal relationships – had been diluted. “Re-creating that relationship, coupled with the new investor-backed large groups create a unique pathway that other
companies in the space seem to be moving away from.”
Learning from the big players – and doing it differently
Both founders credit their experiences at large organizations with shaping their philosophy – in some cases by contrast.
“Large organizations give a perspective that is needed to contrast the founder/family owned business,” they said. Those lessons created “a checklist of what worked well and what needs improvement.” They are quick to point out the advantages of major distributors: “scaled operations, cash, established systems and proven logistics that work extremely well.”
But the HSS model isn’t built to rely on those systems. “The large organization’s model creates an environment where ‘any-body’ can take an order and hit send to deliver products,” they said. At
HSS Medical Supply, they have something different in mind. “We are not looking for ‘any-body’, we only employ experienced industry professionals that enable us to handle the logistics challenges with the lifetime of experience.
from some of the legends in this industry; Henry and Ester Schein, Doug Harper, Stanley Bergman, Pat Kelly, Pete McCann, Sr. –we are here to build something together,” McCann said. The mission they emphasized is twofold:

“ We complement each other’s strengths and weaknesses. When a visionary meets a grounded, data driven operator, the two can develop a plan to realize the vision –that’s why our partnership works.”
That experience is the differentiator – supported, they believe, by a culture of trust, transparency, and service. “True customer relationships are the key, sales professionals who know their customers and the industry,” they said. Their goal is simple: “Developing a standard of service that starts and ends with people.”
Guiding principles for a new generation
The company’s values draw from industry legends and mentors. “My guiding principles come
service to customers and service to employees. “Every new person that walks into the building needs to share that belief, we need to lead a life of service to others.”
That philosophy comes alive each week around what has already become a company tradition. “We sit every Monday at a large table, located in the warehouse and discuss every issue and success we faced the prior week,” they said. “The conversation always revolves around how to best serve the customers while maintaining the employee spirit
of ‘getting it done’.” Internally, they refer to it as the kitchen table meeting. The motto? “WE can figure it out.”
Complementary strengths
McCann and Kiss first worked together at Growth Orthopedics, where they learned how seamlessly their styles aligned. “We complement each other’s strengths and weaknesses,” they said. “When a visionary meets a grounded, data driven operator, the two can develop a plan to realize the vision – that’s why our partnership works.”
In year one, their eyes are on fundamentals. “The life of any start-up in the first year has to be focused on three main objectives; building a solid customer base, delivering on our commitment to service and maintaining a positive spirit through the growing pains that are inevitable.”
From there, the roadmap becomes more ambitious. “To start and build logically to ensure stable success,” they said. “From there we will scale into new regions and continue to add experienced sales professionals each year.” Within three to five years, the founders envision “a national, multi-specialty business that has succeeded by creating a positive experience for our employees and customers.”
But the true measure of success is something far more personal – something that ties back to McCann’s earliest memories in his family’s business. “When my son walks into the building and feels that connection to the company that I felt as a teenager – this isn’t a company, it’s a family.”
And that, they say, is when they’ll know: “We did it right.”

respiratory diagnostics designed to perform across point-of-care, OTC and clinical settings.
PHASE Scientific Americas delivers a respiratory testing portfolio that supports clinical decision-making across point-of-care, OTC and laboratory settings. From COVID-19 and Influenza A/B to combination assays and advanced respiratory solutions, our diagnostics are designed to perform when patient volumes rise and turnaround time matters.

Servant Leadership
Embracing the journey over the destination.
By Pete Mercer
 Dick Bowley isn’t doing good – he’s doing great. That’s at least what he says when he’s asked, often catching people off guard with his initial answer. It’s a bit of light playfulness that is a brief snapshot into Bowley’s personality, showing how he can seemingly build bridges with everyone he meets.
As a retired sales professional, Bowley fills his time wearing a few different hats: serving on the prayer team at his church, taking his grandchildren on golf cart rides in his hometown, and acting as a corporate leadership coach for individuals who are looking to improve themselves. For Bowley, that desire to improve themselves is the most important component of the coaching relationship. Repertoire Magazine recently spoke with Bowley about his role as a leadership coach and how servant leadership has helped him to find his life’s purpose.
What is servant leadership?
In many ways, servant leadership is exactly what it sounds like – a leadership approach where the leader’s primary goal is to serve their team and community, prioritizing the growth, well-being, and empowerment of others before their own needs.
“To me, it’s helping people to be the best that they can be and to help them see what they cannot see. Servant leadership is not based on doing things for people but leading them out of what’s holding them back,” Bowley said.
Bowley uses wisdom from John Maxwell, renowned author

and pastor, to help him shape his approach. Maxwell has an idea called The Law of the Lid, where he argues that we all have a lid that keeps us from realizing our true potential. With servant leadership, you can help people release their lids.
Another one of Maxwell’s ideas, that Bowley references frequently, is that leadership is influence. True leadership doesn’t
come from a position of authority – it’s all about your ability to positively impact others to reach a shared, common goal together.
“In my early days, I thought leadership was based on your title. When I wasn’t doing well in my early stages, I heard people talking about servant leadership. I started studying it to see exactly what they were talking about – it came at a time when it was all
Dick Bowley
about management, not leadership. Management is all about getting something done, where leadership is more about helping that person get it done to the best of their ability.”
The role of a coach
If we look at the role of a coach through this lens of encouragement, we can better understand how this coaching dynamic can positively impact the people that they work with. For Bowley, coaching is about helping people to see and achieve their full potential, whether it’s in their personal or professional lives.
Coaching is also very situational, meaning that what you do with one person may not fit the needs of another. An effective coach gets to know the person that they’re working with to better understand their needs and where they want to improve.
There’s a big opportunity with coaching, where the coaching dynamic can be a different relationship than the person has with a manager or a boss. Bowley likens this dynamic to that of a fun uncle. He said, “To me, an uncle is like a dad without an agenda. He’s family, someone you respect, but he doesn’t yell at you or tell you what to do. When I coach someone, especially in the corporate space, I’m not their boss or their manager. I try to set that expectation early – I’m not your boss, so you can talk to me differently. Just like you would talk to your uncle differently than you would your dad.”
Living out your purpose
Bowley became a leadership coach shortly after taking a StrengthsFinder assessment, where he found his purpose in life. He said,
“The key to everything, the key to life is knowing your purpose.” Once he discovered his purpose, which is to build people up, he was able to then channel that energy into coaching.
Bowley’s key strength is Maximizer, which is an encourager. This theme in the StrengthsFinder assessment identifies individuals naturally talented at turning something strong into something superb, focusing on excellence by nurturing existing strengths rather than fixing weaknesses. “One of the characteristics of Maximizer is that you want to encourage – you want to take people from good to great.”
there’s almost always something we can be grateful for. Whether it’s something like another day with our loved ones or it’s something bigger like a new opportunity, gratitude is a deep well that we have to choose to pull from. It’s not always an easy choice to make, but it is a good choice to make.
Bowley had a successful career in sales, but these days he is deeply grateful for this opportunity to pivot into something that is meaningful for him and helps to impact the lives of others. His lived experience is now a tool that he uses to coach and mentor his clients, leading with a servant’s
I try to set that expectation early – I’m not your boss, so you can talk to me differently.
With this new charge, Bowley thought he would pursue an opportunity as a counselor. As an encourager, would this not be a perfect fit for his newfound purpose in life? After a year of training to be a lay counselor, Bowley found that counseling was decidedly not the right fit for him.
From there, he decided to pursue coaching, where the people that he’s working with are actively trying to learn and improve themselves. In these sessions, he will often challenge people to consider their own life’s purpose because he knows how important it is to their success. “Seeing someone go from good to great is the ultimate reward –that’s my pay,” Bowley said.
The power of gratitude
Gratitude is an emotion that isn’t always easy to tap into, but
heart and an attitude of joy and gratitude to build connections with them.
With gratitude and service as his lens for his coaching and leadership style, he is able to offer a unique and invaluable perspective to the people that he works with. Whether he’s leading a small group at church or working with current and future business leaders, he does it all with a joyful, grateful heart.
“A phrase that I’ve been using for years that we use at church quite a bit is ‘I don’t have to, I get to,’” Bowley said. “When I get to work with managers and leaders who are having trouble with their employees getting stuff done, it always comes back to this ‘I have to get this done’ mentality. Just changing that attitude makes a huge difference – I don’t have to, I get to.”
The Deal Wasn’t Lost –You Just Let It Drift
Most sales losses don’t come from competitors or pricing. They come from silence, hesitation and a failure to lead the process.
By Brian Sullivan

 The deal didn’t blow up.
No angry email.
No competitor swooping in with a miracle discount.
No dramatic “we’ve decided to go in another direction” call. It just … faded.
The emails got shorter.
The response time got longer.
The calendar invite stayed tentative.
And eventually, the deal joined the largest graveyard in sales: “Still working it.”
If you’ve been in sales longer than five minutes, you know exactly what I’m talking about.
Most deals don’t die in a fire. They die quietly – starved by indecision, politeness and a lack of pressure everyone pretends isn’t there.
Here’s the uncomfortable truth: The deal wasn’t lost. You let it drift.
Drift is the silent killer
Drift happens when momentum slows and no one takes responsibility for restarting it.
It sounds harmless:
` “I didn’t want to push.”
` “They said timing was tough.”
` “I’m giving them space.”
` “I’ll follow up next week.”
Drift feels professional.
Drift feels respectful.
Drift feels safe.
And drift absolutely murders pipeline.
The best reps don’t wait for clarity to appear. They create it. They understand that momentum isn’t rude – it’s leadership.
When deals drift, it’s rarely because the buyer lost interest. It’s because the rep lost control of the process.
The lie we tell ourselves
Here’s the lie reps tell themselves to sleep at night: “If they’re interested, they’ll get back to me.”
That’s not how buying works.
Buyers are busy.
They’re distracted.
They’re juggling priorities you’ll never see.
Interest without structure doesn’t move.
Interest without next steps evaporates.
Interest without urgency defaults to “later.”
And “later” is where deals go to quietly die.
Momentum is a choice
Elite reps treat momentum like oxygen. If it drops, they don’t panic, but they don’t ignore it either.
They notice:
` When meetings don’t end with a clear next step
` When follow-ups become vague
` When timelines turn into “we’ll see”
` When enthusiasm softens into politeness
And instead of backing off, they lean in.
Not aggressively. Not awkwardly. But intentionally. Momentum isn’t about pressure. It’s about direction.
Where drift usually begins
Drift almost always starts in one of three places:
No. 1: Weak endings
Meetings that end with:
` “This was great.”
` “Let’s touch base.”
` “We’ll reconnect.”
That’s not a next step. That’s a hope. Strong reps end meetings with clarity:
` “Here’s what we agreed happens next.”
` “Here’s who needs to be involved.”
` “Here’s when we’ll reconnect –and why.”
If the meeting ends fuzzy, the deal will drift.
No. 2: Polite follow-up
The fastest way to kill momentum is the classic:“Just checking in.” Checking in checks the deal out. Great reps follow up with purpose, not politeness: New insight
A clarifying question
A decision that needs to be made
A reminder of impact or urgency
If your follow-up doesn’t move something forward, it’s just noise.
No. 3: Fear of tension
This is the big one.
Reps let deals drift because they’re afraid to create tension:
` “I don’t want to be pushy.”
` “I don’t want to bother them.”
` “I don’t want to hear ‘no.’”
But tension is not the enemy.
Uncertainty is.
Great reps are willing to risk a clear “no” to avoid a slow, painful “maybe.”
How great reps stop the drift
Elite reps do a few things differently – and none of them require magic scripts or Jedi mind tricks.
They say things like:
` “Help me understand what’s changed.”
` “It feels like momentum has slowed – am I reading that right?”
` “What would need to happen for this to move forward?”
` “Should we put this on pause, or is there a real path ahead?”
Those questions feel uncomfortable because they are honest. And honesty accelerates decisions.
Control without control freak energy
Stopping drift doesn’t mean controlling the buyer. It means owning the process.
The best reps:
` Set expectations early
` Define what progress looks like
` Reconfirm timelines
` Name hesitation when they sense it
They don’t hover. They don’t disappear. They lead.
Buyers don’t resent leadership
– they crave it.
Drift is a skill problem, not a market problem
If deals are stalling, it’s tempting to blame:
` The economy
` The industry
` The competition
` The pricing
Sometimes those matter.
Most of the time, they don’t. More often than not, deals stall because no one is brave enough to say: “Let’s decide what we’re doing here.”
That’s not pressure. That’s professionalism.
The year you stop letting deals fade
The reps who win consistently aren’t luckier.
They’re not louder. They’re not pushier.
They’re clearer.
They refuse to let good conversations dissolve into vague intentions.
They don’t confuse activity with progress.
They don’t confuse politeness with professionalism.
So the next time a deal starts to drift, don’t wait it out.
Don’t send another hollow follow-up.
Don’t hope momentum magically returns.
Step in.
Name it.
Lead it.
Because most deals aren’t lost to competitors.
They’re lost to silence. And silence only wins when you let it.
Brian Sullivan, CSP, Founder of PRECISE Selling, founder of The PRECISE Selling and PRECISE Performers, helping companies train, coach, and outsource top-tier sales talent. Learn more at www.preciseselling.com

Matters of the Heart
Why getting the details right in cardiovascular care – from BP cuffs to ECG leads – makes all the difference in patient outcomes.
In cardiovascular care, precision is everything. From the first beat to advanced imaging, small differences in how clinicians measure, interpret, and act on cardiac data can have outsized effects on patient outcomes, clinical efficiency, and healthcare costs. In this issue of Repertoire, our heart health series explores the ways that accuracy, technology, and workflow improvements are reshaping how heart disease is detected, monitored, and managed.


Clarity at the Heart of Care
From early disease detection to workflow relief, echocardiography’s evolution is giving clinicians sharper insight – and patients clearer answers.
Over the past decade, echocardiology has quietly transformed diagnostic confidence in cardiovascular care – often in ways clinicians may not fully recognize. As Jacob Dewees, Clinical Luminary Leader, Cardiovascular Ultrasound at GE Healthcare, explained, “the very first line of visual interpretation of the heart” comes through echo, long before other modalities can reveal how the heart is actually functioning.
That accessibility has helped fuel rapid innovation. “The one beautiful thing about echo is that it’s really easily accessible,” Dewees said, noting that ultrasound systems can be brought directly to the patient, wherever care is being delivered. Over the past decade, advancements such as speckle tracking strain technology have improved clinicians’ ability to understand myocardial motion, detect disease earlier,

and better differentiate cardiac conditions. Echo has also become essential in structural heart interventions, with transesophageal probes guiding complex procedures, while pediatric cardiology has benefited from increasingly smaller, high-performing 4D probes.
“The thread that holds all of that together is image quality,” Dewees said. Improvements in software beamforming and adaptive imaging technologies have enabled clinicians to see smaller structures and capture more detailed information across a wider range of patients. Ultimately, clearer images have enhanced not only measurement accuracy, but clinicians’ confidence in interpreting data and making the best possible decisions for their patients.
Spotting the subtle
Advances in echocardiography are allowing clinicians to detect cardiac changes that were once too subtle to see – sometimes years earlier than was previously possible. According to Dewees, many of these changes occur long before symptoms emerge and are “really invisible to the naked eye.” Improvements in image quality and advanced quantification tools are now bringing those early signals into focus.
Dewees, who began working in echocardiography in 2002, has witnessed this evolution
firsthand. “Back then seeing chordal structures and valvular information and the valve apparatus in the detail that we can see now would’ve been impossible,” he said.
Today, sonographers can visualize valve anatomy and blood flow with far greater precision, including “the origination of those jets,” allowing clinicians to better understand pathology and optimize procedural planning. In structural heart interventions, this level of detail helps teams determine exactly where devices should be placed to achieve the best patient outcomes.
The impact extends across a wide range of disease states, including hypertrophic cardiomyopathy, diastolic dysfunction, and even the effects of blood pressure on the heart muscle. Clinicians can now expand these assessments to the atria and right ventricle, improving evaluation of pulmonary hypertension and gaining a more comprehensive view of cardiac function.
“There are a ton of subtle changes from the atrium to how blood flows to valvular tissue that now we can see, we can analyze, we can quantify and then do something with it,” Dewees noted.
Diagnostic confidence also plays a critical role for cardiologists facing growing patient volumes. As the number of cardiac patients increases, clinicians are being asked to read more studies with fewer resources.
Beyond anatomy, newer technologies are revealing functional changes within the myocardium itself. Using Automated Functional Imaging (AFI)-based speckle tracking strain, clinicians can follow how the heart muscle moves –insights that have expanded into what Dewees describes as myocardial work, “literally being able to measure how much work the heart can do.” These tools act, he said, “like a bionic eye,” uncovering early indicators of ischemic heart disease, identifying regions most affected by coronary blockages, and detecting complex conditions such as amyloidosis, which presents with distinctive strain patterns that would otherwise be impossible to visualize.
Underlying all this progress is image quality. “The better the image quality we get, the better we can interpret that information,” he said, calling image quality “the backbone of echocardiography.” Clearer images improve measurement accuracy, enable more reliable AI-assisted analysis, and support faster, more confident decision-making – ultimately helping patients move more quickly onto the right care pathway.
Relieving healthcare workforce pressures
As healthcare systems continue to grapple with staffing shortages, time pressure, and rising patient complexity, diagnostic confidence has taken on new
urgency. According to Dewees, more accurate and efficient echocardiography can help relieve several of these pressures at once – particularly in the wake of the COVID-19 pandemic.
“Post COVID, this really hit medicine significantly,” Dewees said, pointing to ongoing shortages of both sonographers and cardiologists. While artificial intelligence is often discussed in terms of speed and automation, Dewees emphasizes its less visible – but equally important – ergonomic impact on sonographers. Performing echocardiographic exams requires repetitive motions and sustained physical strain, and “there was a study done that said 80% to 90% of sonographers are in pain while they do their job,” he noted. By automating common measurements and reducing the number of clicks, traces, and manual inputs required, AI can shorten scan times and reduce the physical toll of each exam.
Less time performing repetitive measurements also means less probe-on-patient time. Dewees said that this can help sonographers scan with less pain and potentially avoid the musculoskeletal injuries that often force them out of a profession they otherwise love. In that sense, AI doesn’t just improve efficiency – it may help address workforce shortages by keeping experienced clinicians in the field longer.
Diagnostic confidence also plays a critical role for cardiologists facing growing patient volumes. As the number of cardiac patients increases, clinicians are being asked to read more studies with fewer resources. AI-assisted reporting can streamline workflows, allowing
cardiologists to edit and finalize reports rather than build them from scratch. That time savings can be redirected toward patient care, clinical decision-making, and complex interventions.
Finally, improved image quality underpins all these advances. From obesity to congenital heart disease, clearer images help clinicians navigate increasing patient complexity with greater confidence, making echocardiography faster and more sustainable in today’s constrained healthcare environment.
Better decisions, sooner
Looking ahead, Dewees is most excited by how rapidly echocardiography continues to advance – and what that means for both
clinical decision-making and patient experience. “We can make better decisions sooner because that’s our first line of imaging,” he said, pointing to echo’s central role in evaluating cardiac patients. As image quality improves, clinicians are gaining clearer, more actionable information earlier in the diagnostic process, allowing care teams to move faster and with greater confidence.
Dewees is particularly optimistic about the future of echoguided interventional procedures. Technologies supporting transcatheter aortic valve replacements (TAVRs), mitral valve clips, and valve replacements have already transformed care that once required open-heart surgery and lengthy recovery times. In the
As image quality improves, clinicians are gaining clearer, more actionable information earlier in the diagnostic process, allowing care teams to move faster and with greater confidence.
AI’s role in echocardiography
Artificial intelligence is reshaping echocardiography by improving efficiency while reducing variability. One of AI’s most impactful contributions is automating measurements, eliminating the need for clinicians to repeatedly trace borders and push the same buttons. In doing so, AI brings greater accuracy and reproducibility, ensuring that measurements are consistent regardless of whether they are performed by a sonographer, cardiologist, or surgeon. Tasks once subject to wide variability, such as manually measuring ejection fraction, can now deliver the same reliable results across users and care settings. AI is also enhancing image acquisition, with tools that guide probe placement and positioning to help clinicians capture better images.
years ahead, he anticipates these procedures becoming even less invasive – potentially evolving into same-day surgeries. “This is why we kind of go into healthcare,” he noted, emphasizing the ability of better imaging to help clinicians deliver safer, faster solutions that meaningfully improve patients’ lives.
Yet significant challenges remain. Chief among them is the need for true multi-modality interpretation. An echocardiogram alone can generate thousands of data points – from strain and myocardial function to hemodynamics and valvular flow. When additional imaging such as CT, PET, or stress testing is added, the volume of data multiplies. Dewees sees an opportunity and a necessity to better connect these datasets. Patterns that may appear subtle or insignificant in one modality could become clinically meaningful when viewed alongside another.
Solving this puzzle, he believes, will require advanced AI. “There’s so much data, it’s almost impossible for someone to filter all of that information in their own head,” he said. AI-driven multi-modality interpretation could help clinicians identify complex or early-stage disease states more reliably and sooner.
Ultimately, Dewees hopes future progress translates into faster, more accurate diagnoses and clearer care pathways. For patients and families, he said, the hardest part is often uncertainty – “not knowing what’s wrong, not knowing how bad it is and what needs to be done to fix it.” If imaging can reduce that uncertainty, he believes the field will have taken a meaningful step forward.

Put Heart Care in Focus Vivid
The Vivid portfolio combines renowned image quality with AI-enabled workflow to help teams see more and act faster, delivering the clarity clinicians expect and the efficiency teams need.




Complete por tfolio, f lexible pathways. Of fer customers options from premium (Vivid Pioneer, Vivid S70N with Dimension) to value (Vivid T9 and Vivid iq), plus education, ser vice, and upgrades that keep f leets current .
Connect with your GE HealthCare CVUS representative to learn more today.
Cutting Down on Repeat ECGs in Primary Care
Simple workflow improvements — and technology designed to help reduce unnecessary repeats — may save time, resources and patient frustration.
Electrocardiograms are among the most frequently performed diagnostic tests in primary care, but they are also repeated far more often than many realize. In a Baxter (formerly Hillrom) study with 101 respondents, the prevalence of repeat ECGs in the primary-care setting is approximately 11%.1
In many clinics, issues such as artifact, poor data quality, or improper lead placement result in ECGs being redone before the physician even reviews them. Baxter’s study found that physicians
encountered poor-quality or artifact-laden ECGs about 19% of the time, and more than half of those problematic tracings required a repeat.1 In addition, roughly a quarter of end-users chose to repeat the ECG before submitting it, often out of concern that the initial tracing would not be usable.1 These repeat exams may seem like an acceptable inconvenience, but they collectively create meaningful clinical and operational burdens. Every repeated ECG consumes staff
time, equipment availability, and appointment minutes that could otherwise serve other patients. They can delay diagnostic decision-making, particularly when the ECG is needed to evaluate arrhythmias, ischemia, or other time-sensitive conditions. Patients may also become frustrated when asked to wait longer or return for another test. At scale, repeat ECGs contribute to workflow inefficiencies and can undermine both productivity and revenue for primary-care practices.

The causes behind repeat ECGs are typically preventable. Baxter identifies several contributors, including patient movement that introduces motion artifact, degraded or expired electrodes, worn adapter clips or lead wires, and electrical interference from environmental sources.1 In many cases, the issue originates with inconsistent training or infrequent practice, as primary-care staff may not perform ECGs often enough to maintain confidence in lead placement and preparation. Even small missteps – skin not fully prepped, leads placed slightly off-position, or equipment not inspected regularly – can lead to distorted signals that render the tracing unusable.
Why quality matters
Reducing repeat ECGs begins with strengthening the first-pass quality of the exam. High-quality ECG devices equipped with data-quality algorithms can automatically select the cleanest segment of data, minimizing the effect of motion or intermittent interference. Baxter’s portfolio of ELI ECG devices, for example, use extended-data recording that captures multiple seconds of ECG tracings and extracts the best 10-second segment for interpretation.2 Clinics can further reduce repeat exams by reinforcing consistent patient-prep protocols – ensuring clean, dry skin; removing lotions or oils; addressing hair at electrode sites; and maintaining a calm, low-interference environment during the test.
References:
Why ECGs are essential
Early detection of cardiac conditions: ECGs help identify heart rhythm abnormalities (arrhythmias), ischemia, or previous heart attacks, enabling clinicians to detect cardiovascular issues early –often before symptoms become severe.
Guiding treatment decisions: ECG findings inform medication choices, referrals to cardiology, or urgent interventions. In primary care, this allows providers to manage chronic conditions like hypertension or heart disease more safely and effectively.
Baseline and monitoring tool: ECGs provide a baseline for a patient’s heart function, allowing longitudinal comparison over time. Regular ECGs help monitor the effects of medications, disease progression, or postprocedure recovery, supporting proactive rather than reactive care.
Regular equipment checks — verifying the condition of electrodes, wires, and clips — also prevent quality issues that accumulate slowly over time.
Equally important is standardizing workflow and training. Routine refreshers on lead placement, equipment handling, and troubleshooting common issues help ensure that every staff member has the confidence and skills to obtain a high-quality tracing on the first attempt. Regular equipment checks – verifying the condition of electrodes, wires, and clips – also may prevent quality issues that accumulate slowly over time.
ECG-to-EMR connectivity plays a role as well. Seamless digital transfer can help reduce uncertainty about whether a test
1 Baxter. Best 10 Research—Repeat ECGs. Clinical Study. Retrieved August, 2022.
2 Baxter Internal Data on File.
has been completed or documented, preventing unnecessary repeats triggered by missing or misplaced results.
Taken together, improving ECG quality at the point of capture can reduce the number of repeat exams. For busy primarycare practices, addressing this challenge leads to streamlined workflow, improved patient satisfaction, reliable clinical data and a reduction in wasted time and resources. With more than 100 million ECGs performed annually in the U.S., even small gains in quality can have an impact across healthcare settings.1
Rx Only. For safe and proper use of the products mentioned herein, please refer to the Operator’s Manual or Instructions for Use. US-FLC64-260001 (v1.0) 01/26
Getting Blood Pressure Right
Why accuracy in BP measurements has never mattered more.

When Dr. Thomas Schwieterman talks about blood pressure, he’s really talking about the future of healthcare. As Vice President of Clinical Affairs and Chief Medical Officer at Midmark Corporation, he has seen the impact that a single, seemingly simple measurement can have on the trajectory of chronic disease, provider performance, and even national health economics.
And yet, blood pressure (BP) – the vital sign that influences more diagnoses and
treatment decisions than almost any other – is among the most commonly mismeasured.
“Errors in BP measurement, unfortunately, are too common,” Dr. Schwieterman said. In clinics across the country, clinicians rush through the reading with patients “with feet dangling from a tall table, over a shirt sleeve and immediately upon entry into the room.” These shortcuts, long regarded as harmless, have turned out to be anything but.
What’s at stake is not just accuracy. It’s whether tens of millions of patients are treated appropriately – or treated unnecessarily.
The ripple effect of the SPRINT study
The turning point, Dr. Schwieterman explains, came nearly a decade ago with the landmark SPRINT study. “Since the SPRINT study was published, there has been a consistent flow of clinical science that affirms the importance
of both accurate BP acquisition and proper hypertension management,” he said.
SPRINT revealed that lowering systolic blood pressure by just 10 mmHg dramatically reduced the risk of heart disease, heart attacks, and strokes. “If a patient’s BP is maintained below 130/80, about 25% of adverse cardiovascular events could be avoided,” he noted.
But this discovery came with a paradox. By lowering the threshold for what qualifies as hypertension, “nearly 40 million more Americans would be classified as having high BP.” Overnight, more than half the U.S. population could be considered hypertensive.
With so many more patients now flagged as potentially at risk, the margin for error shrank. False high readings suddenly meant tens of millions of people might be put on costly, unnecessary medication – all because of improper chair height, unsupported limbs, crossed legs, a full bladder, or conversation during the test.
“To avoid patients getting unnecessary medication with false positive high numbers, it became even more important for providers to capture this routine measurement exactly to protocol,” he said.
Old habits, new science
Blood pressure has long been viewed as a quick, routine task –one of the first skills healthcare workers learn. But that familiarity is part of the problem.
“Taking a BP is often one of the first things clinicians of all levels learn in their training, and it has the reputation of being trivial in nature,” he explained. Asking seasoned professionals to
change their technique is “similar to asking a professional golfer to relearn how to complete a 2-foot putt or an NBA star how to shoot a free throw.”
Yet the science is conclusive: proper technique matters.
And slowly, Dr. Schwieterman says, the clinical community is adapting. “I am witnessing the medical profession doing just that – relearning how to capture a proper BP reading. This is a good thing to avoid overprescribing medicine for normotensive individuals.”
To quantify just how much technique influences results, Midmark commissioned the CORRECT BP Study in 2021 – a multi-site investigation conducted by a principal investigator, a clinical data scientist, and an independent Clinical Research Organization.
improper technique resulted in a 7 mm systolic and 4.5 mm diastolic error on the HIGH side,” he said.
Those numbers may appear small at first glance. But at scale?
“This level of error would result in about 40 million patients being wrongly diagnosed,” he said. That’s “more people than in the entire state of Texas.”
The consequences ripple far beyond incorrect prescriptions. When clinics must report their hypertension control rates to payors, faulty readings can hurt their reimbursement. “With a 7/4.5 drop in their numbers,” he explains, many providers would suddenly meet performance thresholds – “without changing anything in their therapeutic programs.”
In other words, better technique can improve both population health and financial outcomes.
“ There are so many things that need to be done at every encounter and often not enough time to do them. So, it is essential that the setup and equipment make the job as efficient as possible.”
The study took blood pressure readings at The Ohio State University in three scenarios:
1. Traditional technique on a high table without proper support
2. Correct technique, following all SPRINT guidelines
3. The original, incorrect position repeated, with order randomized
The results were eye-opening.
“The CORRECT BP study investigators found, with extremely high confidence, that
Matching the rigor of other diagnostic tests
Why does BP accuracy lag behind other clinical measurements? The discrepancy puzzles Dr. Schwieterman.
“Most of your readers are likely familiar with the need to fast before a blood test or prep in some way for a procedure,” he said. These protocols exist for a reason: they ensure the results reflect reality.
Blood pressure should be no different.
“Patients need to avoid recent caffeine, empty their bladder, skip the cigarettes and avoid talking during the testing,” he said. Combined with proper positioning and a quiet rest period, these steps create a consistent and reliable baseline.
When half the population has high blood pressure and half does not, “the only way to know which is which, is to capture as accurate as possible measurements.”
Anything less risks overtreatment, expense, inconvenience –or dangerous undertreatment.
Exam room setup: The foundation of accuracy
Better BP measurement doesn’t fall solely on clinicians. The environment itself must support the right behaviors.
“There are so many things that need to be done at every encounter and often not enough time to do them,” he said. “So, it is essential that the setup and equipment make the job as efficient as possible.”
That means exam chairs that allow patients to rest their feet flat on the floor. Armrests positioned at heart level. Support behind the back. Equipment that prompts standardization instead of shortcuts.
“Setup and equipment” must make doing things the right way the easiest way.
Why BP is front and center in chronic disease prevention
The broader push for chronic disease management – including diabetes, kidney disease, cardiac
Midmark’s Better BP ® Program began with a simple but transformative realization: improving blood pressure accuracy required a fully integrated clinical process. The initiative is built on three pillars proven to reduce variation in blood pressure measurement: proper patient positioning, standardized automated BP capture, and seamless EMR connectivity. Together, these elements create a point-of-care ecosystem designed to generate more reliable readings, enhance workflow efficiency, and support better clinical outcomes.
According to Dr. Thomas Schwieterman, Vice President of Clinical Affairs and Chief Medical Officer at Midmark, the spark for the program came during a 2015–2016 product planning meeting. At the time, the SPRINT trial had just been published in The New England Journal of Medicine, offering clear evidence on how to achieve a true resting blood pressure. The study emphasized two critical factors: averaging multiple readings and positioning patients correctly. Midmark had just developed a new exam chair with support rails that aligned perfectly with all recommended positioning requirements.
When the team recognized they could also embed validated averaging protocols into their vital signs device, the vision crystallized. As COO at the time, Mike Walker put it, Midmark wasn’t just delivering equipment – “we’re providing accurate blood pressure.”
health, and even cognitive function – has made BP accuracy even more essential.
“Even cognitive disorders have been found to be accelerated by elevated BP,” he said. Blood pressure’s influence touches nearly every system in the body.
“One reason BP is so prevalent as a quality measure among payors and quality supervisors is this one attribute of human physiology can significantly impact so many heavy hitting chronic conditions,” he added, including “heart attacks, strokes, diabetes, cognitive disorders, kidney function and peripheral vascular issues.”
Put simply: getting BP right helps prevent or delay a long list of complications.
“It is a blessing that blood pressure is both easy to measure and easy to treat, in most cases.”
A call to distributors and providers
For Dr. Schwieterman, the message to Repertoire’s audience of healthcare distributors and frontline providers is clear.
“There aren’t many aspects to patient care where one test can positively impact so many disorders,” he said. Treating osteoporosis strengthens bones. Treating thyroid disorders affects specific organs. But with blood pressure, “proper treatment positively impacts dozens of problematic disorders.”
This is why the stakes are so high – and why the opportunity is so great.
“That’s why proper blood pressure measurement is so essential when trying to achieve holistic and long-term outcomes,” he said.
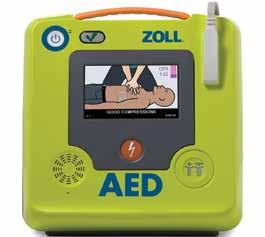
Seconds Save Lives
Why early CPR, accessible AEDs, and bystander confidence are critical in sudden cardiac arrest.
It can happen in an instant. A person collapses – the victim of sudden cardiac arrest (SCA) – and the clock starts ticking in the race to restore a normal rhythm to the heart.
A rescuer armed with an Automated External Defibrillator (AED) and performing CPR is the victim’s best chance for survival until medical personnel arrive.
Indeed, research shows that the probability of survival goes up dramatically when CPR is performed and when an AED is applied before an ambulance arrives.1
“Sudden cardiac arrest (SCA) is one of the leading causes of death in the U.S.,” said Jonathan Bowman, Senior Director of Sales, Acute Care Technologies – ZOLL. “The only effective treatment is a shock from an AED combined with high-quality CPR administered as soon as possible after a victim collapses. This ensures the most favorable outcome.”
An AED will only recommend a shock 50% of the time on the first analysis. A cardiac arrest victim will require high-quality CPR all the time. For the 50% of cases where no shock is advised, high-quality CPR increases the flow of oxygenated blood to the heart, brain, and other vital organs. With CPR, a victim’s chance of survival increases significantly. Even when a shock is advised, a struggling heart needs high-quality CPR to provide it

with oxygenated blood to return it to a normal rhythm.
Awareness, education and access
Even with the availability of this technology, barriers to lifesaving action can happen well before emergency responders arrive.
One of the most persistent challenges is fear. “People are afraid to cause more harm, not understanding that you are protected by the Good Samaritan laws, and when someone is not breathing and unresponsive, bystander help is critical to their chances of survival,” Bowman said. Compounding that fear is a widespread misconception that AEDs are only for medical professionals. In reality, Bowman noted, “An AED is designed to be used by anyone for helping someone who is suffering from cardiac arrest.”
Recognition is another hurdle. Many people have never witnessed cardiac arrest and may
1 Weisfeldt ML, et al. J Am Coll Cardiol. 2010;55(16):1713–20
struggle to identify its signs. Bowman pointed to the importance of broader education efforts, explaining that increased public awareness campaigns and workplace CPR training can help close that gap and empower people to act decisively in emergencies.
Over the past two decades, access to technology has dramatically changed cardiac arrest care. Bowman highlighted the growing availability of AEDs in public spaces and a deeper understanding of CPR effectiveness. “The realization that not all CPR is great, and that monitoring of the quality of CPR can make a huge difference in patient outcomes,” has reshaped resuscitation practices across public, EMS, and hospital settings, Bowman said. This evolution is reflected in the American Heart Association’s ongoing updates to CPR and AED guidelines, including the newly released 2025 recommendations.
Looking ahead, Bowman sees education and accessibility as the next frontier. Continued CPR and AED instruction for students of all ages, mandatory training for coaches and teachers, and better visibility of AED locations are essential. Bowman also pointed to innovation that connects personal technology with AED registries, helping bystanders quickly locate lifesaving devices when seconds matter most.







An Unsustainable Equation
Flat reimbursement, rising wages and persistent turnover are forcing physician practices to rethink how they staff, support and sustain their workforce.
 In today’s marketplace, staffing in medical groups is like walking a tightrope for practice owners and managers, said Andy Swanson, chief revenue officer, Medical Group Management Association (MGMA). “Recruiting is challenging, particularly for hard-to-find clinical roles, niche specialties, and specialized technical positions such as anesthesiology assistants or nurse specialists. Retention is an even greater concern today than ever before.”
Non-clinical staff face their own pressures, grappling with outdated technology, inefficient processes, and systems that are not patient-friendly. Balancing old ways of working with new expectations from clinicians and patients has become increasingly unsustainable.
Indeed, physician practices and medical groups are facing a staffing environment that leaders describe as increasingly unsustainable. Flat or declining reimbursement, rising operating costs, and persistent turnover in key roles are combining to create some of the toughest workforce pressures the sector has seen in years, according to leaders from the American Medical Group Association (AMGA).
At a high level, the core issue is simple math, says Mike Coppola, MBA, former chief operating officer at AMGA. “Reimbursement is flat to declining and expenses are increasing, so it’s a financial model that’s not
compensation scale, experience some of the highest turnover in medical groups. Competing with retail or big-box employers has become increasingly difficult when those settings offer comparable pay with less stress and fewer administrative burdens.
RNs fare slightly better on the pay scale but face similar challenges. “Those are the two areas where we see some of the biggest challenges,” Coppola said – roles that are essential to maintaining clinic flow, supporting providers, and keeping patient access open.
Matthew Wells, Ph.D., senior director of consulting at AMGA, points out that while reimbursement stagnates, provider salaries continue to rise – up 27% since 2017 for physicians in medical specialties. “They’re not going to go down anytime soon,” he noted. With operating expenses already squeezed, medical groups are being forced to pursue efficiency wherever possible.
In many environments, there isn’t “new money” flowing into physician practices to offset increased labor costs, so sustainability comes down to how well practices operate.
sustainable,” he explained. Wage inflation – especially acute over the last several years – has placed even more strain on medical groups already operating with tight margins. And unlike other expense categories, wages rarely move downward.
The impact shows up most clearly in recruiting and retaining medical assistants (MAs) and front-desk staff. These positions, which sit on the lower end of the
What the numbers tell us
The Association for Advancing Physician and Provider Recruitment’s (AAPPR) 2025 Benchmarking Report revealed the median organization conducted 96 provider searches in 2024, highlighting sustained demand that often exceeds internal recruiting capacity. “When leaders don’t have the time or resources to focus on sourcing, interviewing, and onboarding,
searches take longer and candidate experience suffers,” said AAPPR CEO Carey Goryl.
Difficulty varies by location and specialty, but practices commonly struggle across both clinical and non-clinical roles, including medical assistants, front-office staff, advanced practice providers, and physicians. “From an AAPPR perspective, extended recruiting timelines – including a 121 days-to-fill the typical physician search when using an in-house recruiter – reflect ongoing supply constraints, workforce age trends in certain specialties, competition, and changing expectations around workload and work-life balance all play a role,” Goryl said.
MGMA tracks medical practice costs through the association’s financial operations data, and the latest numbers tell an interesting story, said the MGMA’s Swanson. “Overall, practices are still managing to keep margins sustainable, but it’s getting harder.” Before the pandemic, many private groups boosted their support staff, including advanced practice providers (APP), to about 3.8–4.7 staff per physician, depending on specialty. The idea was simple: let doctors focus on high-level care while the rest of the team handled everything else.
Fast forward to 2024, and those staffing levels have dropped by roughly two full-time positions across the board. “Why? Rising labor costs and shrinking reimbursement rates make it nearly impossible to maintain those extra hands,” Swanson said. Now, physicians are back to doing tasks that should fall to support staff, which only adds to frustration and burnout. “Unless practices invest in technology to
fill the gap, which comes with its own price tag, the burden will stay on physicians.”
Vacancy rates depend on the market, Swanson said. In some areas – mainly suburban communities and other “desirable” locations – staffing has stabilized, and supply generally meets demand. But in many parts of the country, especially rural regions, staffing remains a full-blown crisis.
“Take a two-doctor clinic in rural Tennessee as an example: if one physician retires unexpectedly due to health issues and the other is just two years from retirement, the entire practice, and the community it serves, faces an immediate emergency,” he said. “That clinic has been trying to recruit one or two replacements for three years without success. How likely is it they’ll find a qualified specialist in time, let alone prepare for the second retirement?”
category – salaries and benefits for staff and providers – represents roughly 80% of a medical group’s operating expense. “It’s a people industry,” Coppola said. With limited room to cut elsewhere, practices are left with few levers: reduce staff, restructure roles, or invest in technology that automates certain tasks.
Access is already feeling the effects. Many groups report longer wait times as shortages limit how many patients a clinic can move through each day. Some organizations are considering consolidation – reducing the number of standalone sites or bringing small practices together under one roof to create economies of scale. While these moves may improve efficiency, they can also reduce geographic access for patients, creating another trade-off for leadership to manage.
Retention bonuses may offer a temporary boost but rarely deliver lasting impact. Instead, successful practices focus on engagement – regular rounding with staff, early check-ins with new hires, and consistent recognition.
Unfortunately, Swanson noted this scenario is common across wide swaths of the country. When practices can’t fill these gaps, they’re forced to cut services, leaving patients and families to either go without care or travel long distances to get it.
Tradeoffs that physician groups don’t want to make
Workforce pressure is driving difficult decisions among physician groups. The staff support
Inside practices, the burden is increasingly shifting to those who remain. Wells notes that responsibilities that once belonged to multiple roles are now being combined out of necessity. “If they say, ‘We can’t get a medical assistant,’ they’re just expecting the RN to cover that and do their RN duties as well,” Coppola said. The result: employees stretched thin, dissatisfaction rising, and turnover accelerating as staff choose less demanding work elsewhere.
Leaders are being pushed to meet higher expectations with fewer people and at a higher cost, said Goryl. In many environments, there isn’t “new money” flowing into physician practices to offset increased labor costs, so sustainability comes down to how well practices operate.
That reality is driving tradeoffs that include delaying hires, redistributing work, redesigning roles, cross-training and leaning more heavily on operational efficiency. “The practices that are adapting best are those that treat workforce challenges as a systems issue, not just a hiring issue, by improving workflows, reducing friction, strengthening onboarding and building healthy workplace cultures that support retention,” Goryl said. “Simply asking fewer people to do more is not a longterm solution; it increases burnout and turnover, which ultimately costs more.”
Why staff are leaving
As staffing shortages continue to strain physician practices, leaders say the reasons employees are walking out the door are both practical and cultural.
“We are not hearing new or different challenges than in recent years,” Swanson said. Wage inflation in other industries continues to put pressure on healthcare, where revenues remain flat or even decline. Recent Medicare reimbursement cuts, with private payers likely to follow, make this problem unique: no other industry faces such limited ability to increase revenue while costs rise.
Staff wages have kept pace with inflation, but physician and APP salaries have not. This creates short-term staffing
TWO TRUSTED PRODUCTS. ONE CONVENIENT WAY TO ORDER AND SAVE.
Influenza and COVID-19 share overlapping symptoms and seasonal trends, making preparedness essential. Order both tests under one SKU to simplify ordering and enjoy built-in cost savings.
COST SAVINGS
Enjoy cost advantages when purchasing both products via the Test Pack
a trusted molecular solution for fast and reliable results.
FLEXIBLE ORDERING
Select the Test Pack or individual kits to align with customers’ operational strategies
AVAILABLE YEAR-ROUND
Access the Test Pack throughout the year for savings, regardless of the season

adjustments, but the long-term outlook is a systemic concern that medical groups cannot ignore. “We need government partners to revisit reimbursement cuts and take a holistic view of the industry’s viability. If revenues keep shrinking while costs climb, the situation will become unsustainable.”
According to AMGA experts, one of the most common frustrations is being asked to perform work outside an employee’s training or licensure – often because vacancies elsewhere in the practice leave gaps that must be filled.
For example, registered nurses frequently find themselves completing tasks that fall squarely within a medical assistant’s role. “That’s not the best use of their license and their training,” said Coppola. Faced with spending their day on duties that don’t match their skill level, many RNs choose to seek work environments where they can practice to the full extent of their training.
Front desk positions, already among the lowest paid in physician practices, are prone to even faster turnover. Staff often leave
Meeting patient demand a “persistent challenge”
Physician practices aren’t closing their doors to patients, but access remains strained. “We’re not hearing about groups reducing hours or closing panels to new patients, but longer wait times, especially in underserved communities and certain specialties, remain a persistent challenge,” said Swanson.
Missed appointments are a major factor. In 2024, single-specialty practices reported that 20% of patients canceled appointments, and fewer than one-third rescheduled within 30 days. Each open slot represents both a lost opportunity for patients seeking care and lost revenue for providers.
To address the issue, many practices are adopting smarter scheduling strategies, including rapid rescheduling technologies that help refill openings quickly. As healthcare becomes more consumer-driven, these tools are emerging as a practical way to improve access, reduce wait times, and keep schedules – and care delivery – on track.
AAPPR members and recruitment leaders consistently connect staffing delays to access delays, said Goryl. “When it takes months to fill roles and a meaningful share of offers are declined, the impact shows up in longer waits and communities going underserved.”
In many markets, leaders also report downstream effects such as service line reductions, deferred growth plans, or shifts in coverage models when hiring timelines extend.
“This is why AAPPR increasingly emphasizes ‘days-to-fill’ as a missing metric in workforce conversations: it translates hiring friction into real access constraints,” he said.
for an increase as small as 50 cents to a dollar per hour – especially when retail and big-box employers offer similar pay with less pressure. “The pay isn’t commensurate with what the ask is,” Coppola said, noting the heavy administrative load and constant patient interaction required at check-in.
Workplace culture plays a significant role as well. Staff may tire of challenging physician personalities or feel they are no longer part of a missiondriven environment. “Do they really feel like they’re providing healthcare?” asked Dr. Wells. “When they don’t, we really see turnover increase.”
As for retention, both leaders stressed that money alone won’t solve the problem. Retention bonuses may offer a temporary boost but rarely deliver lasting impact. Instead, successful practices focus on engagement –regular rounding with staff, early check-ins with new hires, and consistent recognition. “Because the cost to recruit and replace is so high, doubling down on retention is critically important,” Coppola said.
Focal points
So, what can be done? Goryl said the most successful retention strategies are practical and repeatable:
` Build a healthy workplace culture on purpose: consistent communication, visible leadership, clear expectations and recognition.
` Give frontline staff influence over the decisions that shape their day (scheduling templates, patient flow, rooming standards, handoffs).
` Protect staffing levels so roles stay humane. Chronic

There when you need it
Gone when completed

Terumo’s innovative SurTract™ safety syringes and needles provide a passive safety system*, while minimizing patient discomfort during injection.
Once the plunger is fully depressed, you’ll hear a “click” followed by automatic needle retraction into the plunger body – reducing the risk of needlestick injuries.*
Call your Terumo representative at: 1.800.888.3786 or visit www.TerumoTMP.com
understaffing becomes a retention killer because it guarantees burnout.
` Offer schedule flexibility where possible, because flexibility is now a major differentiator for candidates and current staff.
` Invest in tools and processes that reduce friction (documentation workflows, better recruiting and onboarding systems). AAPPR’s 2025 Report shows many organizations rate their recruiting tech as “average” or below, which is an opportunity area.
` Address toxic behavior quickly: retaining high performers often requires helping misaligned employees exit.
“The throughline: practices retain talent when they make it easier for staff to do great work for patients, with the support and resources that prevent constant ‘catch-up mode,’” Goryl said.
MGMA members consistently tell the association that when practices have the resources to invest, they focus on technology that speeds up workflows, reduces reliance on hard-to-fill roles, and lightens the load on clinical staff. “Every tech investment is scrutinized, and the ones that succeed share two traits,” Swanson said. One, they’re easy to implement. And two, they deliver a clear return on investment, which is better than sticking with the status quo or absorbing rising labor costs.
But when budgets are tight, practices turn to culture. “I say ‘best place to work’ in quotes because the most successful groups define what that means for them, not for the practice down the street,” Swanson said. A surgical group might

As workforce shortages continue to challenge physician practices, AMGA leaders say medical groups must rethink how they recruit, develop, and support their staff if they want long-term stability.
prize autonomy, efficiency, and high standards, so they recruit people who value those things. A pediatrics practice, on the other hand, might emphasize relationship-building, hands-on care, and a “can-do” attitude. Both approaches work because they align with the group’s core values.
“Culture doesn’t cost money, but it does take time and intentional effort. And when done well, it not only improves retention but also keeps staff engaged and focused on delivering better patient care.”
Swanson recommends physician practice leaders focus on the environment inside the practice. This is entirely controllable and within each location’s purview. “Agreeing on cultural
norms for handling operational hurdles, challenging patients, and stress is essential, and every group approaches these issues differently,” he said. With aligned expectations, all staff, clinical and non-clinical, can feel a part of the team and critical to their sense of contribution to the important work of the practice. This will serve groups well as they take on new cost pressures, rising reliance on technology as a partner in their work, and staff outages as they experience those as well.
Building a stronger workforce pipeline
Over the next decade, the U.S. is projected to face a shortage of 86,000 physicians. “As more baby
boomers require care, demand will rise for doctors, nurses, physician assistants, and other clinical roles,” Swanson said. Clinical “extenders” will be especially important in areas with significant provider shortages, helping triage and deliver care where physicians are scarce.
Operational roles will also remain essential, Swanson continued, though the expectations are shifting. Success now requires stronger skills in process optimization, technology integration, culture building, and team leadership, alongside the foundational practice-management expertise needed to run
specialized medical groups on increasingly thin margins.
As workforce shortages continue to challenge physician practices, AMGA leaders say medical groups must rethink how they recruit, develop, and support their staff if they want long-term stability. While there is no single solution, several strategies are emerging as best practices across high-performing organizations.
One of the clearest opportunities lies in diversifying talent pipelines. Dr. Wells emphasized that practices can no longer rely solely on traditional recruitment sources for medical assistants
Data points to continued strain
AAPPR’s 2025 Physician and Provider Recruitment Benchmarking findings point to continued strain rather than meaningful relief:
` Recruitment demand remains high (typical organization conducted 96 searches in 2024) and with organizations with less than 200 providers, they typically conducted 16 searches in 2024
` Days-to-fill remains elevated, especially in specialty and surgical searches (physicians median 121 days; oncology median 332 days).
` In 2024, physicians accepted 71% of offers, consistent with 2023, while advanced practice providers accepted 80%, down from 83% the previous year.
` Turnover persists: median turnover rates 7.3% physicians and 7.9% APPs, still above pre-pandemic levels.
` A separate pressure point is the “infrastructure of recruiting” itself: organizations that under-resource recruitment capacity and tools make the problem worse.
On wage pressures and decision drivers, recruiters report that compensation expectations are evolving, but candidates are also increasingly prioritizing schedule control and slower decision timelines.
“Data suggests that staffing conditions have stabilized at a high-pressure level, with persistent challenges in specialty roles and competitive markets,” Goryl said. “While there are pockets of improvement, the overall environment continues to require intentional recruiting strategies, operational efficiency and retention focus rather than a return to pre-pandemic norms.”
(MAs) and other frontline roles. “Groups need to diversify where they’re looking for talent,” he said. Internships, externships, and partnerships with local schools can help build a more reliable flow of candidates. Several AMGA members are also investing in in-house education programs to upskill staff and create clearer development pathways.
Engagement remains another essential component. Instead of treating MA teams as separate or subordinate, Wells said practices need to foster a sense of shared mission and teamwork. When staff feel supported by providers and leadership, they are more likely to stay and grow within the organization.
Career development is especially important for front-desk employees – one of the hardest groups to retain. Coppola noted that healthcare historically has not provided robust advancement tracks for these roles. Creating structured career paths, with defined skills and expectations, can help reduce turnover while strengthening internal leadership. Dr. Wells and Coppola also stressed the importance of understanding the day-to-day pressures staff face. Being mindful of when and how employees are approached – whether by vendors or other departments – can reduce overwhelm and contribute to a healthier work environment.
Ultimately, strengthening the workforce pipeline requires new recruitment strategies, intentional development, and a supportive practice culture. As Coppola reminded, “Just being aware of some of the things that are happening in a practice … it can be a little overwhelming.”
Heroes of Infection Prevention
Infection preventionist shares her career journey and what led her to be recognized nationally for her clinical accomplishments.
By Jenna Hughes
 Each day, approximately one in 31 U.S. patients and 1 in 43 nursing home residents contracts at least one infection in association with their healthcare, according to the Centers for Disease Control and Prevention (CDC); highlighting the need for improvements in patient care practices across facilities.

Infection prevention (IP) is a crucial step in the healthcare delivery continuum which aims to break the chain of infection within facilities through coordinated clinical activities, and is designed to stop healthcareassociated infections (HAIs) from spreading.
IP is especially important in long-term and post-acute care settings to ensure resident safety, quality of life and emotional wellbeing. As a result, many long-term and post-acute care facilities have begun implementing infection prevention protocols to reduce the risk of HAIs and protect their residents and staff.
At the forefront of these efforts is Clinical Nurse Manager and Infection Preventionist Jane Owino, RN, BSN, MPH-CIC, of Parker Health Group in New Jersey. Owino was recognized for having successfully reduced infection risk for patients across her clinical practice.
Owino was a recipient of the 2025 Association for Professionals in Infection Control and
Epidemiology’s (APIC) Heroes of Infection Prevention Award in the Infection Prevention and Control (IPC) Quality Improvement Category. Each year, APIC recognizes two members and/or their IPC teams for their IP efforts.
“Infection preventionists have many responsibilities within the clinical setting,” said Owino. “In my role, I work among other clinical managers to participate in the entire clinical operation of my facility’s healthcare community,” she said.
Owino serves on the clinical leadership team in her long-term care (LTC) community while also emphasizing a core focus on IPC. In her dual role, Owino oversees daily IPC clinical operations and ensures that infection prevention practices are implemented effectively across all care settings – while at the same time collaborating closely with interdisciplinary healthcare teams to promote resident safety, staff education, compliance with regulatory standards and continuous quality improvement.
“An individualized, holistic patient care approach is often linked to successful infection prevention,” said Owino. “If a resident falls, this type of incident should not exclude the input of the infection preventionist, because it is possible that the cause of the fall is an infection that may be beginning to crop in, for example. We as IPs must look at clinical problem solving collectively to come up with the best solutions for the resident.”
Implementing infection prevention and control
A key milestone for Owino’s journey to the Heroes of
Infection Prevention Award was Parker Health Group’s adoption of the Minnesota Antimicrobial Stewardship Data Collection Tool in 2022, which enabled consistent month-by-month microbe data tracking and reporting across the health system’s stewardship committees.
“Since 2021, our community teams have been building a strong foundation for antimicrobial stewardship. With organizational leadership support, we’ve strengthened all seven elements outlined in the CDC’s core elements for antimicrobial stewardship in nursing homes,” said Owino. “This data-driven approach has improved transparency, accountability and informed our clinical decisions for better resident outcomes.”
had the privilege to collaborate with NGOs, CBOs, government agencies and international partners, fostering strong public health networks.”
Owino also had the opportunity to co-chair the South Sudan Health NGO Network in 2006 through GOAL- Ireland, an international humanitarian response agency, in partnership with World Relief, Tearfund and UNICEF; supported the meningitis outbreak response in the Bahr el Ghazal region (South Sudan, 2005) under The United Nations Development Program (UNDP); and lead the development of the first Indoor Residual Spraying Training Manual for malaria control at Research Triangle Institute International (RTI) in 2010, which was later adopted across 14 African countries.
Infection prevention protocol is especially critical in long-term care settings because residents often have multiple comorbidities and weakened immune systems, making them more vulnerable to potential infections.
Owino’s personal interest in IP began in 2002, when she transitioned from a nurse manager role in a medical-surgical unit in Kenya to a position in public health working for humanitarian organizations in South Sudan.
“From 2002 to 2010, I held several leadership positions –ranging from health program manager to program specialist – working with in-country teams to develop proposals and secure funding for HIV, tuberculosis and malaria prevention programs across Kenya and South Sudan,” said Owino. “During this time, I
“Supporting the meningitis response in South Sudan was my first hands-on experience in outbreak management, which solidified my passion for infection control in resource-limited settings,” said Owino. “Meningitis can spread very quickly in a short period of time, and so many patients contracted the disease during the 2005 outbreak that we had to rapidly train local healthcare personnel to be able to provide immunizations quickly and effectively. When the vaccines arrived, these same healthcare personnel had
to then reach out to each village’s population, because we had to perform a mass immunization of thousands of villages to combat the outbreak.”
Owino calls on her former experience in international public health and infection prevention each day as she continues her nursing and IP career in the U.S.
“These experiences deepened my commitment to infection prevention and control and shaped my professional journey when I later relocated to New Jersey,” said Owino. “What I learned early in my career journey provided the backbone to my knowledge and passion for IP and has been fueled into the roles I carry now.”
of life, safety and dignity,” said Owino. “It not only applies scientific problem-solving: IPC involves identifying patterns, investigating outbreaks and implementing evidence-based interventions, but also enhances patient quality of life by preventing infections to help residents remain healthy and engaged.”
Infection prevention in longterm care can vary significantly in comparison to acute-care settings due to differing patient populations, resources and facility types.
“In long-term care, infection prevention is primarily nurse-led –with the nurses serving as the cornerstone of IPC activities,” said Owino. “Unlike hospitals, LTC
“ Staff engagement in IPC programs begin with education, ownership and recognition. We foster a culture where every team member – clinical and non-clinical – understands their role in protecting residents.”
IP in long-term care
Long-term care residents, like patients in acute-care hospitals, are at an elevated risk of acquiring healthcare-associated infections once admitted to a facility.
Infection prevention protocol is especially critical in long-term care settings because residents often have multiple comorbidities and weakened immune systems, making them more vulnerable to potential infections. Residents also often live in close quarters in LTC facilities, making disease transmission of increased concern.
“Strong IPC strategies directly impact residents’ quality
settings are both healthcare facilities and a home for its residents, requiring a more personalized and continuous approach.”
Examples of nurse-driven IPC responsibilities, said Owino, include patient admission and immunization management, ongoing clinical surveillance, daily IPC enforcement, environmental oversight, shift ‘huddles’ where nurses conduct meetings for educational moments and micro-learning and ensuring that IPC principles are integrated into a facility’s daily routines (and not as separate initiatives.)
“We use ongoing education and microlearning sessions to
keep IPC practices top-of-mind for staff and encourage accountability,” said Owino. “Recognizing staff for their contributions publicly also helps sustain enthusiasm and reinforces the idea that infection prevention is everyone on the team’s responsibility.”
“Staff engagement in IPC programs begin with education, ownership and recognition. We foster a culture where every team member – clinical and non-clinical – understands their role in protecting residents,” said Owino. “Ongoing feedback, visibility of infection data and celebrating team successes have been key motivators to maintaining IP protocol.”
Overcoming
obstacles to IP IP and outbreak management is an ongoing, evolving practice within long-term care facilities, requiring staff and patient education and the constant re-evaluation of current practices to be executed properly.
There can be, however, numerous obstacles to implementing infection prevention in long-term care, and challenges include staffing shortages and role overlap, limited diagnostic stewardship, time constraints and competing clinical priorities.
“Limited diagnostic stewardship is an ongoing issue for many staff members in longterm care,” said Owino. “For example, if a doctor assumes that a certain patient may have a urinary tract infection (UTI), we as IPs have had to put in place certain steps to ensure that we are arriving at that potential diagnosis (or that we are ruling out other diagnoses) using evidence-based care.”


Instead of a healthcare professional assuming that a patient has a UTI and diagnosing it without further testing, diagnostic stewardship makes sure doctors are thorough with their diagnoses – such as ordering testing like a white blood count (WBC) for a suspected bladder infection to find out if a resident has elevated WBCs or not before they are administered antibiotics.
“We must make sure as infection preventionists that we go further – running blood work, following up with an assessment and performing proper follow-up care with each and every patient,” said Owino. “We as long-term care staff
must continually ask ourselves, are we really treating what we need to treat? Or are we just treating?”
Despite inherent challenges to IP protocol, Owino and her team have demonstrated exceptional leadership and innovation, overcoming many obstacles to prevent HAIs in long-term care on the journey to becoming a recipient of the APIC Award.
To provide expert patient care, infection preventionists must focus on treating patients in a constantly changing clinical environment, which requires a more comprehensive look at each patient’s specific condition, comorbidities and personal needs.
To address this, Parker Health Group has integrated a culture of transformation for long-term care residents into its facilities based on Eden Philosophy, which approaches each patient as an individual and considers each resident beyond their clinical needs.
Eden Philosophy aims to view patients holistically, considering their emotional and physical wellbeing as inherently linked by addressing loneliness, boredom and other challenges in the transition to long-term care.
“In long-term care, a patient might be losing cognitive and functional ability due to Alzheimer’s and dementia, but who they

were before they entered LTC does not disappear once they are going through an illness,” said Owino. “As a Certified Eden Trainer, I teach my staff that Eden Philosophy recognizes the identity of an individual before they were diagnosed with a disease, and that we all must treat all residents with that in mind – maintaining their natural routines and an inherent respect for each resident’s identity.”
Eden Philosophy aims to address some of the inherent challenges in long-term healthcare by promoting person-directed care in terms of meaning and patient choice.
Becoming an IP hero
While infection prevention achievements are often highlighted in acute-care and hospital settings, long-term care facilities play an equally important role in the prevention of HAIs and deserve equal support and recognition, said Owino.
“Professionally, APIC’s recognition has fueled my passion to continue advancing IPC initiatives,” said Owino. “It reaffirmed that with dedication and collaboration, LTC nurses can make significant contributions to infection prevention at both the local and national levels.”
For Owino, being awarded the Heroes of Infection Prevention Award is affirmation that long-term care nurses, too, can excel in the clinical setting by elevating infection prevention for the enhancement of LTC resident safety.
“This recognition came to me as a surprise, because at the time, I had been trying to find grounding in what I do for my career,” said Owino. “I was motivated to
apply for the Heroes of Infection Control as I was reading through the awards that other nurse preventionists had received. I realized then that there was so much that we had done at our own facility as a team in long-term care for antimicrobial stewardship.”
career to my children is deeply fulfilling as a mother.”
Building on these achievements going forward, Owino recognizes that some of the biggest opportunities for change toward better infection prevention in postacute care overall are empowering
“Professionally, APIC’s recognition has fueled my passion to continue advancing IPC initiatives. It reaffirmed that with dedication and collaboration, LTC nurses can make significant contributions to infection prevention at both the local and national levels.”
Owino encourages all nurses and clinical staff to apply for awards like APIC’s, and to speak up at their own practice when they accomplish something in order to gain more recognition for hardworking providers across the post-acute sector.
“We as clinical staff must encourage and empower LTC nurses in our workplaces and create a space for them to have a voice and speak up for IP,” said Owino.
Fueling personal drive and future growth
Owino has also gained meaningful personal validation and a deeper appreciation for her career in the process of applying for and receiving the Heroes of Infection Prevention Award.
“Being given opportunities such as this one to write about my professional journey is profoundly rewarding and fuels personal drive into what I do,” said Owino. “It is also a living example for my two daughters and my son. One of my children once said, ‘If Mommy can do it, we can do it,’ so being a role model in my
staff through education and habit-building to sustain infection control practices, strengthening diagnostic stewardship through collaboration with prescribers and leveraging technology and data for surveillance and feedback to drive continuous improvement.
“My guidance for other organizations looking to implement infection prevention protocols is to start by building a strong foundation of education and culture,” said Owino. “It is important to engage all levels of staff early, establish clear communication channels and ensure leadership commitment. Then, begin to develop policies aligned with CDC and Centers for Medicare and Medicaid Services (CMS) guidelines and implement consistent surveillance tools and track measurable outcomes.”
“Most importantly,” said Owino, “Celebrate small wins in IP with your clinical team to build momentum – because infection prevention is not just a program; it’s a continuous journey of improvement and shared accountability.”
Advancements in Patient Nutrition
Exploring the nutritional delivery space in recognition of Feeding Tube Awareness Week in February.
By Jenna Hughes
 Proper nutrition plays a critical role in patients’ wellness, healing and recovery. Those receiving care in post-acute, long-term and at-home facilities may require nutrition via a feeding tube if unable to consume food orally.
Consequently, it is becoming increasingly important that postacute hospital and healthcare facility staff and caregivers are trained on the innovative solutions in nutritional delivery to support adult and pediatric enteral feeding needs from the hospital to the home.
Feeding Tube Awareness Week is recognized this year during the week of February 8 through the 14 by the Oley Foundation, an organization enriching the lives of those living with tube feeding, to normalize the reality of receiving


nutrition in different ways and to provide support for patients who rely on feeding tubes.
Enteral
feeding and nutrition
Advancements in clinical nutrition delivery have transformed care by enhancing patient diets, streamlining clinical workflows and leveraging new automated technology.
“Enteral feeding, also referred to as ‘tube feeding,’ is a way of providing nutrition directly into the gastrointestinal (GI) tract through an access device, or a
feeding tube,” said Emily Miller, BSN, RN, medical advisor for nutritional delivery, Cardinal Health. Miller spent 11 years as a hospital bedside nurse, working directly with patients receiving enteral nutrition.
Enteral feeding is designed for patients who are physically unable to eat and swallow (dysphagia) or for those unable to obtain sufficient nutrition through eating and swallowing.
“Enteral nutrition can either be delivered through a short-term
device that is placed through the nose or a long-term device that is surgically implanted into the stomach or small intestine,” said Miller.
Patients of all ages from infants to adults may have a feeding tube while in acute, post-acute and long-term care settings, and patients can live on a feeding tube for as long as needed.
“Related conditions include, but are not limited to cancer, critical illness, GI disease, or non-GI diseases such as stroke, kidney disease or lung disease,” said Miller.
Infants may also require enteral feeding if they cannot sufficiently suck or swallow during bottle or breast feeding, said Miller. This can happen if a baby is born prematurely or lacks the strength or skills to feed orally.
Sometimes, tube feeding is used for a short time, then decreased or stopped when the patient begins to eat enough by mouth, according to the Oley Foundation. Other patients receive tube feeding in long-term facilities or via at-home care their entire lives.
Advancements in enteral nutrition
In general, enteral nutrition can be administered by three different methods: manually with a syringe, using a gravity bag or via an enteral feeding pump.
“Gravity bags, typically hung above the patient on an IV pole or hook, provide enteral feeds using gravity without an electronic pump,” said Miller. “Both syringe and gravity feeds deliver food relatively fast, which can cause intolerance symptoms like nausea or vomiting in certain patients.”
Enteral feeding pumps, on the other hand, provide a
portable nutrition option delivered at a controlled flow rate with the use of electronics, providing a customized and fully automated feeding experience, said Miller.
Despite the need for a medical prescription for enteral feeding to ensure adequate nutrition, some patients in both hospital and at-home settings remain at risk for malnutrition due to feeding intolerance and delivery challenges.
“Feeding intolerance can result from several factors, including poor gastroenteric access (from issues such as incorrect tube size or placement), partial bowel obstructions, medication side effects, hyperglycemia and electrolyte imbalances,” said Miller. “These issues can prevent patients from receiving the full volume of prescribed nutrition, leading to inadequate caloric intake and poor weight gain.”
Increasingly, patients receiving nutrition at home are shifting toward blenderized whole-food options to avoid these common feeding challenges. The term blenderized tube feeds (BTFs) refers to commercially available products and homemade blends made from real food ingredients, blended into a consistency that can be fed through a feeding tube, according to the Oley Foundation.
“Prepared or homemade blenderized foods differ from traditional, ready-to-feed formulas in that they are comprised of real, whole foods that are blended to a smooth consistency so they can be delivered through an enteral access device or feeding tube,” said Miller.
Most patients will also need water periodically delivered through the tube, called a “flush,” as the formulas do not
“ BTF allows patients and caregivers to incorporate familiar foods and individualized nutrition into enteral feeding, creating a more natural and inclusive experience.”
Another significant contributor to feeding intolerance, said Miller, is the potential intolerance to standard commercial formulas.
Adult patients have traditionally been fed largely on commercially manufactured and readyto-feed formulas. These can be liquids or powdered, concentrated formulas that are mixed with water. Some patients have demonstrated a lower tolerance for these standard, ready-to-feed formulas. This may result in gastrointestinal symptoms and reduced adherence to feeding.
provide enough water for their needs. Enteral feeding pumps that automatically feed and flush, like the Cardinal Health Kangaroo OMNITM Enteral Feeding Pump, can help promote hydration.
“With automatic flushing, this also helps reduce the burden on caregivers compared to manual flushing,” said Miller.
Organic, whole-food diets
According to Miller, one of the most significant changes in enteral nutrition is the shift toward whole-food, prepared blenderized
diets – also referred to as BTFs. These types of diets are becoming increasingly popular. A recent global study indicated as many as 40% to 55% of adult patients receiving home enteral nutrition used BTF, she said.
“Studies have shown that when patients receive real-food blenderized tube feedings, they tend to experience fewer GI symptoms, ultimately lowering the risk of malnutrition,” said Miller. “Transitioning to BTFs has also been linked to higher patient and caregiver satisfaction, as well as relief from certain persistent GI symptoms that can occur with traditional, standard commercial formulas.”
These blends can retain more of the natural components of food including pulp and skins, which can make them thicker than standard commercial formulas, said Miller.
The International Dysphagia Diet Standardization Initiative (IDDSI) standardizes naming and descriptions for texture-modified foods and thickened liquids for people with dysphagia.
The IDDSI Framework, supported by the American Society for Parenteral and Enteral Nutrition (ASPEN), consists of a continuum of eight levels designating thickness, ranging from thin liquids to regular foods.
“Because BTF retains the integrity of real food including fiber and complex carbohydrates, it naturally falls into the thicker range of liquids on the IDDSI framework. This higher viscosity is one of the reasons specialized feeding sets and pumps are essential for delivering blenderized diets safely and accurately,” said Miller.
“The Cardinal Health Kangaroo OMNITM Enteral Feeding Pump is the first attitude-independent feeding pump in the U.S. designed to deliver thick formula*.”
Standard feeding pumps and sets are not typically designed to handle thick formulas, which can lead to under-delivery of up to 22.5% of food compared to programmed volumes. This discrepancy can significantly impact nutritional status, especially in medically complex patients.
Personalized nourishment
BTF not only provides an alternative to standard formulas but also has the potential to improve the patient experience through personalized nutrition and natural nourishment.
“BTF allows patients and caregivers to incorporate familiar foods and individualized nutrition into enteral feeding, creating a more natural and inclusive experience,” said Miller. “It is also reported that BTF allows the patient to feel
Notes:
*Thick formula can be defined as enteral fluids of smooth consistency that are categorized as Level 2, 3 or 4 Drinks within the International Dysphagia Diet Standardization Initiative (IDDSI) Framework.
more included in family meals and social gatherings – ultimately improving quality of life.”
New commercially prepared BTF formulas are also increasingly becoming available, made with whole food-based ingredients and limited processing, said Miller.
“According to the Oley Foundation, when starting on BTF, it is best to start slowly and transition over a few days. Additionally, the Foundation recommends patients work with a healthcare provider and a registered dietitian/nutritionist to ensure that a diet is appropriate for the individual’s specific nutrition needs,” said Miller. “A nutritionist can evaluate food and fluid choices and monitor a person’s nutritional progress.”
BTF and commercial feeding products can be combined, according to the Oley Foundation. Caregivers can learn to prepare BTF at home by working with a registered nutritionist. When blending formula, it is best to use a high-powered blender and strain any bits and pieces that may clog a tube. Anyone who prepares BTF for a patient at home should be sure to practice proper food safety habits.
In both long-term care and at-home settings, nutritionists supporting enteral feeding should work closely with clinical care staff to ensure timely and appropriate enteral nutrition – while supporting this essential component of patient-centered, quality care.
“By enabling safe delivery of thick, whole-food blends, enteral feeding is moving away from a one-size-fits-all model toward an approach that offers patients a choice in enteral formula selection,” said Miller.
Better Health Better Future





Eliminating Barriers to Medical Supplies
MedWish Medworks merges healthcare access, sustainability, and volunteerism into one mission – ensuring every person has the chance to live a healthier life.
 In Northeast Ohio, a unique humanitarian nonprofit is redefining the way healthcare resources are distributed, both locally and globally. MedWish Medworks (MW2) is committed to advancing health equity and environmental sustainability by providing essential care, redistributing surplus medical supplies, and connecting medically underserved communities with vital resources. Its vision is ambitious: a world free from healthcare disparities, where everyone has access to highquality care and essential resources.

“At MedWish Medworks, we harness the power of volunteerism and partnerships to eliminate barriers to medical supplies, referrals, and care,” the organization explains. “We empower individuals to live healthier lives.” This mission drives every aspect of MW2’s work, from local clinics to international brigades, and underpins its innovative approach to addressing healthcare inequities.
Providing essential care
Central to MW2’s mission is the delivery of essential care. Each year, the organization hosts six to eight medical clinics at locations selected specifically for their accessibility to neighborhoods with the highest needs – areas marked by poverty, high rates of uninsured residents, and other social determinants of health. Whenever possible, MW2 clinics include a wide range of medical specialties, ensuring comprehensive care for participants.
Beyond domestic clinics, MW2 organizes volunteer mission trips to impoverished countries, staffing brigades with healthcare professionals – including doctors and nurses – and lay volunteers who assist with translation, clinic coordination, and other critical roles. In 2025, these brigades served communities in Honduras and the Dominican Republic, continuing a longstanding tradition of global outreach that includes El Salvador, Nicaragua, Guatemala, Peru, and Kenya.
Redistributing surplus medical supplies
MedWish Medworks leverages its extensive network and inventory to ensure that surplus medical supplies and equipment reach those who need them most.


Internationally, the organization partners with healthcare facilities and medical missions in developing areas, providing items that range from essentials like wheelchairs or ventilators to full restocks of clinics and hospitals. Recipients span Asia, Africa, Eastern Europe, the Middle East, and Central and South America, including clinics operating in conflict zones or responding to natural disasters.
Domestically, MW2 collaborates with more than 300 social service agencies and nonprofits in Northeast Ohio to distribute free medical supplies and equipment.


Recipient organizations submit wish lists, which MW2 fulfills from its inventory. Items provided include everything from walkers and home health beds to diapers and hygiene supplies. This thoughtful redistribution maximizes the impact of donations, ensuring that medical resources are efficiently directed to those who need them most.
Connecting communities with vital resources
MW2’s work extends beyond providing supplies and care to navigating complex healthcare systems. At every clinic, a Navigation Team
assists patients with health insurance questions, Medicaid and SNAP applications, and connections to primary medical homes and other social resources. By building long-term, trusting relationships, the team supports follow-up care, improves access to services, and enhances overall well-being in medically underserved communities.
This holistic approach positions MW2 not merely as a supplier of resources but as a partner in health equity, ensuring that patients have the guidance and tools they need to maintain their health over time.
Ensuring quality and compliance
Maintaining high-quality, usable medical supplies is critical to MW2’s operations. With a volunteer force exceeding 3,500 annually, donated items are sorted, counted, and packed for redistribution. Volunteers remove expired, broken, or soiled items, while retired biomedical engineers test and vet more technical equipment.
The sorting process is meticulous. Initially, volunteers conduct “gross sorting,” reviewing donations for expiration and quality and categorizing items into 22 medical areas, such as cardiac, orthopedics, wound care, and OBGYN. During “fine sorting,” items within each category are separated, inspected, and prepared for bulk packaging with detailed labeling, including count, weight, and expiration date. This rigorous process ensures that each donation meets strict standards before leaving the warehouse.
Selecting recipient organizations
Not every clinic or organization qualifies to receive MW2’s


supplies. Each potential recipient completes an application detailing their operations, population served, and capacity to handle donations. For international shipments, a U.S.-based nonprofit must sponsor the request, and additional vetting is required for disaster zones. Domestic recipients, likewise, must be nonprofit or social service organizations that serve specific populations, from stocking backpacks for backto-school events to providing
equipment for patients who cannot afford it. Applications are carefully reviewed by MW2 staff before supplies are delivered. Internationally, MW2 ensures compliance with country-specific regulations. Recipient organizations coordinate shipping and often engage customs agents to facilitate entry. All recipients sign agreements affirming that supplies will not be distributed to restricted entities, will not be sold, and will be used solely for humanitarian aid.
Measuring impact
MedWish Medworks employs a combination of quantitative and qualitative measures to assess the effectiveness of its programs. Metrics include orders fulfilled, pounds of equipment shipped, number of recipients served, and geographic reach. Whenever possible, the organization tracks the number of individuals impacted by shipments, though many international clinics operate in underresourced locations with limited data collection capacity.
Qualitative feedback – including stories, photographs, and testimonials from recipients— provides invaluable context for evaluating long-term outcomes. Domestically, MW2 tracks shipments, items distributed, and estimated numbers of people served, while clinic teams collect data on patient demographics, services offered, and follow-up care. This multifaceted approach ensures that the organization continually evaluates its operations, benchmarks success, and identifies areas for improvement.
MW2 is currently expanding its reach and capabilities. Following the merger of MedWish International and Medworks last year, the organization has unified all programming under one roof. Its immediate priorities include deepening existing programs, improving operational systems, and meeting the growing demand for services.
Looking forward, MW2 plans to increase its budget and expand its pool of volunteers, supplies, and equipment, enabling the organization to help more people in more profound ways. The goal is not just to meet immediate needs but to create sustainable, lasting
impact on health equity and environmental sustainability.
Opportunities for partnership
MedWish Medworks offers multiple avenues for individuals and organizations to support its mission:
1. Be an ambassador – Spread the word in your community and network, and share MW2’s initiatives on social media.
2. Donate surplus medical supplies and equipment –Medical professionals and manufacturers can redirect unused inventory, reducing landfill waste and providing critical support to underserved communities. MW2 provides tax documentation and, in some cases, direct feedback on the impact of donations.
3. Conduct a supply drive – Collect items from home, workplace, or community, or contribute through MW2’s Amazon wishlist to support clinics and nonprofit partners.
4. Make a financial donation –Funding is essential to MW2’s operations, and every contribution helps sustain and expand programs.
These partnerships extend MW2’s reach and amplify its impact, ensuring that more patients receive the care and resources they need.
A vision for the future
MedWish Medworks exemplifies the power of combining healthcare, volunteerism, and sustainability to create meaningful change. By redistributing surplus medical supplies, facilitating access to care, and providing navigation support to underserved communities, the organization
addresses both immediate and systemic healthcare inequities. Its model demonstrates that healthcare access is not solely about financial investment but also about resourcefulness, collaboration, and a commitment to serving those most in need. Through a combination of strategic planning, meticulous operations, and volunteer engagement, MW2 has built a scalable framework that reaches across neighborhoods in Northeast Ohio and extends to the most resource-limited regions of the world.
The organization’s rigorous approach to measuring impact, paired with a qualitative understanding of community needs, ensures that its work remains both accountable and responsive. By emphasizing partnerships and community involvement, MW2 encourages individuals and organizations alike to contribute to its mission, magnifying the effects of its programs and fostering a culture of shared responsibility.
As healthcare disparities persist and the demand for medical resources grows globally, MedWish Medworks continues to lead by example – demonstrating that one nonprofit can drive meaningful change while maintaining sustainability, efficiency, and compassion at the heart of every initiative. Through its clinics, brigades, and supply redistribution efforts, MW2 is not just providing care – it is empowering communities, saving resources, and building a healthier, more equitable world.
For more information, visit www.medwish.org, or call (216) 692-1685.
Clinicians and Supply Chain – Turning Dodgeball into Volleyball
Conversation,
By R. Dana Barlow
collaboration works with sportsmanlike conduct.
 If healthcare supply chain executives and leaders were asked to identify the two most challenging conversations that they experience on a daily basis they likely would place themselves between two bookends – contract negotiations with suppliers and service companies on one side and product and service discussions with clinicians (e.g., nurses, physicians and surgeons, etc.) on the other.

Bridging the gap between the two can have its positives and negatives, expectations and nuances. It can leave supply chain feeling like Crayola’s Silly Putty.
Working with external suppliers and service companies, supply chain strives to be the hero of its own story, representing the product and service needs and demands of its internal customers based on their clinical preferences and quality issues while trying to appease the fiscal constraints of its organizational employers.
Working with internal clinical customers, supply chain strives for credibility and respect, representing the cost pressures inflicted by
its organizational employers while trying to explicitly understand as well as advocate for the product and service needs and demands of nurses, physicians and surgeons.
Supply chain nurtures the delicate balance between the provider organization on one hand and the clinical community on the other as it weaves between the art and science of conversations and negotiations with suppliers.
Supply chain experts generally agree that successful business relationships and transactions occur when they are fortified with clinical input and intelligence before sitting at the negotiation table with supplier and service company executives.

They also acknowledge that those clinical conversations straddle the line between art and science with clear recommendations on what to say, how to say it and what to avoid saying.
What supply chain should never say to a clinician
If there’s a common denominator for ticking off nurses, physicians and surgeons, supply chain experts agree on this: Ignore them, followed closely by talking down to them.
Joe Colonna, chief supply chain and project management officer, Piedmont Health, warns against tacitly excluding them from the product selection process, by “assuming that they don’t care about cost or imply anything that questions their clinical expertise,” he indicated. Colonna further lists two more red flags: “Your [insert product or procedure here] is costing too much money.” “Why do you have to have this?”
Don’t even think about dissing a clinician or a supplier, according to Mark Dozier, CPA, associate vice president, supply chain services, strategic sourcing and engagement, HonorHealth. “Never use unprofessional language when discussing a product request or the behavior of a specific supplier,” he told The Journal of Healthcare Contracting
Dozier also dismissed the notion of supply chain acting like a boss with “You should clinically be able to use the product.”
Tom Lubotsky, vice president and chief supply chain officer, Allina Health, pooh-poohs the idea of playing the cost card right from the start.
“Don’t go with ‘I need you to consider this product because it is so far less expensive,’” he said. “Don’t lead with that. You’re going to shut off the conversation. Instead, you should lead with ‘I’d like for you to consider this because it sounds like it might offer the same or similar clinical benefit at a lower cost.”
What clinicians hate to hear from supply chain
Aside from budgetary and economic complaints, clinicians really don’t like to hear about limits on product and supplier choices, particularly if an agreed-upon formulary isn’t in place, according to Allina’s Lubotsky. “‘I want to be innovative. I want us to be innovative. I want us to be at the bleeding edge of providing the best of care, so don’t tell me what I can’t use,’” he added.
Piedmont’s Colonna points to accessibility with three statements that lack any explanation:
` “Your device is on backorder or is in some other way unavailable.”
` “You can no longer use your preferred vendor/product [no reasons given].”
` “Your new product request has been denied [no reason given].”
Passive-aggressive behavioral modification doesn’t work either, he added: “Your peers can change so why can’t you?”
HonorHealth’s Dozier also cites the backorder revelation, adding insult to injury by applying it to the clinician’s next case.
Further, clinicians don’t appreciate hearing that “the supplier rep who services you recently had a blatant violation of hospital policy and has been suspended from our campuses for the next 30 days” and “no additional suppliers can

be added to this modality at this time,” he said.
Dozier also notes that clinicians tend to frown “when they are shown data that their procedures are not profitable for the healthcare organization.”
What clinicians prefer to hear from supply chain
Short of “you can have everything you want,” Dozier offers two distinct responses clinicians want to hear from supply chain: “Your new product request has been promptly considered and approved,” and the more succinct, “Yes.”
Colonna and Lubotsky center around collaboration and relationship management.
Colonna lists four statements that clinicians want to hear from supply chain that invite cooperation:
` “Can you help us to better understand your request and are you open to other options?”
` “Can we discuss both the clinical and financial aspects of the products you use?”
` “Would you join us in the value analysis process?”
` “What information and data would help you be more comfortable with our request for a product change?”
Lubotsky highlights the giveand-take of mutual compromise and concession.
“They would prefer to hear we are open to considering all suppliers that bring innovation and improvement in our care,” he told JHC. “We’re willing to do so, but I need your help in understanding what percent of our spend can accommodate innovation. We might pick two vendors that may represent 80% of the market share or spend in that category. That leaves 20% to allow innovation and other players in the door that they can continue to work with.
“What they prefer to hear is us saying is we are open to inviting all suppliers that you are interested in using. But then I need your help in figuring out how do we offer that choice,” he added.
What clinicians should never say to supply chain
Supply chain may say the darndest things to clinicians that irk
them to no end, but then clinicians can reciprocate with questionable replies and retorts, too, that can be abrasive and petulant. And that can happen before they pull rank and approach the C-suite as a last resort.
Colonna and Dozier both hint at geographical leverage and the proverbial threat to relocate.
Dozier shares the nebulous: “Either give me what I want by approving my new product request, or I’m taking my patients and volume elsewhere.”
Colonna emphasizes proximity: “I want to use what I want to use, and if you don’t let me have it, I am going across the street.”
Then Colonna migrates to the dismissive with two more examples: “You only care about the money.” “I am not interested in hearing from you.”
Dozier moves to the intimate and intricate: “I want to move to this new vendor because the rep I depend on is now employed by them.” “I don’t care if I use the cheaper product at the ASC; I’m not going to use it at the hospital.”
Lubotsky winces when hearing, “I have to use this” or “I have to use that” without any background evidence because this really doesn’t invite supply chain’s expertise to help with any decision. “Show evidence on what you call best and let’s look at it critically,” he advised. “Part of it is the style or manner on how physicians approach us. It is always better if we talk about what are the clinical criteria [supporting] why you need it? What is the evidence behind it?
“We prefer to hear, ‘I’d like you to consider this product because I believe this has applications to a select set of patients
and would like to have that be considered as part of the portfolio of offerings for our clinical patients,’” he added.
What supply chain hates to hear from clinicians
One of the challenges supply chain faces when working with clinicians is their employment status. Nurses tend to be employed staff; physicians and surgeons can be employed staff, depending on the provider organization, or they may simply have privileges to practice at the facility. The former grants the hospital more authority and control over decisions than the latter, which may require handling with kid gloves.
Lubotsky acknowledges that physicians and surgeons are suspicious that “we may seem to be interested in spending money on innovative products,” he indicated. “I’d rather they say, ‘I know you guys care about innovation and I found this product area of focus here that I like and I need some help in exploring it further. Can we look at this together?’”
Still, Lubotsky admits one familiar comment can be really upsetting to supply chain: “‘My patients are different. What I do is different.’ There may be clear instances of complex morbidity that require a different approach and therapeutic regimen to take care of a patient. I get that. But
Supply chain experts concur that their team must demonstrate an openness and willingness to understand clinical desires to provide the best, if not optimal, care with the appropriate products, services and technology available.
Colonna lists four potential statements that call for further discussion about procedures and processes:
` “The device you made me use is causing patient harm.”
` “The information you provided is old or incorrect.”
` “I already made this change, so why are you still asking? Do you actually know what is going on in the hospital?”
` “I feel like this change is being forced on me without my concerns be addressed.”
A blatant rejection of cooperation turns off Dozier: “I’m not willing to participate in a trial of your recommended contracted product.”
unequivocally saying, ‘my patients are different so I can’t use these products’ does not foster engagement with Supply Chain.”
Lubotsky also recognizes when residents come in and prefer to use products and technology they trained on in medical school, but the organization may have standardized to a set of branded product already or it may not have any of that on hand and isn’t likely going to invest in it.
“It’s kind of an acceptable reality,” he added.
What supply chain prefers to hear from clinicians
Collaboration and cooperation toward the common goal of
providing quality care for patients while keeping the facility’s doors open should be shared goals and responsibilities of administrators and clinicians alike.
Supply chain experts concur that their team must demonstrate an openness and willingness to understand clinical desires to provide the best, if not optimal, care with the appropriate products, services and technology available. Meanwhile, clinicians need to recognize and understand the motivations and reasons around fiscal constraints and restraint to act as economic stewards.
the patient and the organization.”
` “I may need help in getting comfortable with these new devices so can we discuss what I will need to help me change?”
` “Here are my concerns. If we can address them, I may be able to make this change.”
` “What can I do to support this initiative?”
` “Thank you. I feel included and heard in this process.”
Dozier adds two more:
`
“I’m open to trialing a product that is recommended by the value analysis process or
“ The key is always to listen to the purpose around why physicians want to do what they want to do. Their style or manner may not be what you like, but at the end of the day, they’re doing this because they care about their patients.”
Lubotsky would like to hear something along the lines of “‘I know that things are tough in terms of being careful about managing our costs. I have a product or a service that I really would like to use. I need your help to examine it. Let’s evaluate it together and see if this is something that we could work towards bringing on board,’” he said. “I just think that’s a much better approach in terms of cooperation and the sensitivity and understanding around the financial hardships.”
Colonna give five clinician statements that make supply chain smile and offer value:
`
“I am open to change if it makes clinical and financial sense for
awarded a contract by your GPO aggregation model.”
` “What the hospital has on product formulary is fine with me and will meet my needs.”
Lessons learned
Clinicians and supply chain working together with shared goals and successful outcomes can be turbulent and unnerving, but ultimately necessary for the organization and the healthcare system to continue operating.
Much of this is rooted in simply listening, according to supply chain experts.
“I think among the most important [lesson] was to listen to the concerns and ideas,” Colonna noted. “There is more than one way to achieve the outcome
you desire. Instead of coming to a clinician with a savings goal and a predetermined strategy or solution, just come with the goal and work out the strategy with the impacted clinicians. Then agree to move forward, together, with a commitment to the success of the strategy and to achieving the goal.”
Lubotsky concurs. “The key is always to listen to the purpose around why physicians want to do what they want to do,” he said. “Their style or manner may not be what you like, but at the end of the day, they’re doing this because they care about their patients. Get a deeper understanding about the reasons why they want to use or buy a certain instrument or device. You must listen to the purpose and the why and then help them create the business point, the business position around doing just that, but it may not always be attractive because it could be just too costly. The lesson here is don’t get contentious. Don’t say we can’t afford it. Listen to their purpose and the why and then go from there.”
Dozier shares four additional relevant tips. “In-person conversations can sometimes be helpful as opposed to email,” he recommended. “Never ever share data with a clinician unless you are absolutely sure it is correct. If you find out later that the data wasn’t correct, the clinician will never forget it. It’s important and beneficial to get clinicians involved early in the process of a product decision, evaluation, conversion, etc. And it’s better to have clinicians trial a new product first to see if the technology walks the talk before approving it and adding it to contract.”
EXPLORE THE PATH OF LEAST RESISTANCE
POINT-OF-CARE LIPID TESTING CAN HELP PROVIDERS GUIDE PATIENTS TO BETTER OUTCOMES


Healing the Heart: Cardiac Rehabilitation
Cardiac Rehabilitation Week 2026 highlights the importance of ongoing care and support after a cardiac event.

 Every year, more than 1 million Americans have a coronary event or undergo a cardiac-related procedure, according to the American Association of Cardiovascular and Pulmonary Rehabilitation (AACVPR). And nearly 18 million adults in the U.S. are currently living with some form of heart disease, according to the National Library of Medicine study “Cardiac Rehabilitation in the Modern Era.” Returning to daily life and regular habits after a diagnosis or cardiac event is therefore a critical part of ongoing clinical care and recovery for patients.
Cardiac rehabilitation (CR), a medically supervised program designed to improve cardiovascular health, is a form of secondary prevention for cardiovascular disease, according to the National Library of Medicine study. Participation in CR offers benefits across mortality, reduced hospital readmissions and quality of life for patients.
The primary goal of CR is to provide ongoing medical support after a cardiac event while enabling patients to achieve their optimal physical, psychological and social functioning through exercise, training and lifestyle change.
Cardiac Rehabilitation Week takes place this year in 2026 from February 9 through the 15,
according to AACVPR, to draw attention to the role that cardiac rehabilitation plays in reducing the potentially devastating effects of heart disease.
Moving forward one step at a time
In the clinical setting, CR is prescribed by a cardiologist and delivered by a multidisciplinary
team that includes nurses, exercise physiologists, dietitians, behavioral health specialists, and in some cases, pharmacists and social workers.
Programs are generally structured around 36 sessions over 12 weeks, with duration and intensity adapted to patient needs.
CR is typically delivered in an outpatient, hospital-based setting in the U.S., but can also be delivered in facility-based, home-based, virtual or hybrid models, allowing for flexibility in program access.
Patients with a history of heart attack, coronary artery bypass graft surgery (CABG), heart valve repair or replacement, heart or heart-lung transplant, heart failure, and those with ventricular assist devices, coronary artery disease equivalents such as diabetes or peripheral artery disease and more may benefit from a prescription for cardiac rehabilitation, according to AACVPR.
Exercise for heart health
Beginning or returning to exercise is an important component of recovery for patients who have heart disease or have had a cardiac event.
In fact, at least 150 minutes per week of moderate-intensity physical activity can help lower blood pressure and cholesterol, according to the American Heart Association. It can also help patients keep their weight at a healthy level.
Cardiac rehabilitation offers a clinical setting in which patients can safely exercise, noted Cleveland Clinic, and provides patients with an individualized plan for returning to movement.
Cardiac rehabilitation allows patients to lessen their chances of another heart attack, control heart disease symptoms such as chest pain and shortness of breath, stop or reverse damage to the blood vessels in the heart, lessen the physical and emotional effects of heart disease and improve stamina and strength.
In addition to providing patients with prescribed exercise to improve cardiovascular fitness without exceeding safe limits, cardiac rehab also educates patients about their health journey and guides them on ways to stabilize or reverse heart disease.
beyond extending patient lifespan and into improving patients’ quality of life and long-term wellbeing, according to the National Library of Medicine.
Cardiac rehabilitation now not only encourages a gradual return to a patient’s physical movement and activity level but also provides them with lifestyle counseling to promote increased physical activity, healthy habits and medication adherence; nutrition counseling and weight management; and psychosocial support including depression screening and stress management.
Beyond its physical benefits, a multidimensional approach to CR
Cardiac rehabilitation offers a clinical setting in which patients can safely exercise, noted Cleveland Clinic, and provides patients with an individualized plan for returning to movement.
Long-term lifestyle changes such as reducing or eliminating smoking, lowering cholesterol, controlling high blood pressure, eating a healthier diet, weight loss/control, improving or managing diabetes, increasing physical activity and improving psychological wellbeing may address certain risk factors for heart disease, according to the American Heart Association.
Addressing long-term well-being
As advances in medical and interventional therapy continue to prolong patient survival, more people are living longer lives with cardiovascular disease.
As a result, the focus of CR programs has recently refocused
also provides patients with both psychological and social support, according to AACVPR, including coping skills, stress reduction, group support, community building and family engagement.
In fact, AACVPR data demonstrated that participation in early outpatient cardiac rehab results in improved adherence to preventative medications, function and exercise capacity, quality of life and modifiable risk factors.
For Cardiac Rehabilitation week this year, AACVPR is raising awareness for the numerous benefits of cardiac rehabilitation, highlighting the impact CR has in improving quality of life, and encouraging physicians and cardiologists to educate their patients about CR.
The Year Ahead In Washington
Medical supply chain issues to watch in 2026.
 Legislative progress tends to slow down in midterm election years, as both parties prepare to make their case to the voters. Nevertheless, the policy signals emerging from such legislative debates matter for healthcare distributors. Federal decisions and unresolved proposals influence long-term planning around sourcing strategies, inventory management, and the ability to deliver critical products to providers and patients.
Trade: Strengthening access through trusted partnerships
Outside of the complex trade landscape, the House and Senate have introduced legislation that would impact global medical supply chains. Trade policy remains a key lever for improving supply-chain resilience, particularly for medical products dependent on global manufacturing networks. The Medical Supply Chain Resiliency Act (S. 998 / H.R. 2213) reflects growing bipartisan interest in improving access through smarter trade relationships. The legislation authorizes the President to negotiate “trusted trade partner” agreements that would offer favorable tariff treatment for medical goods and devices.
As policymakers seek to balance domestic manufacturing goals with global supply realities, distributors will play a central role in operationalizing these policies while maintaining continuity of supply.
Transportation: Building resilience across sectors
Transportation and logistics challenges exposed during recent disruptions continue to shape congressional action. The Promoting
Resilient Supply Chains Act of 2025 (S. 257 / H.R. 2444) directs the U.S. Department of Commerce to establish a Supply Chain Resilience Working Group to assess critical supply chains, identify vulnerabilities, and coordinate with international partners. Distributors should expect increased federal attention on how products move from manufacturing to last-mile delivery.
Preparedness:
Building stockpiles and enhancing
readiness
Preparedness remains a defining issue for the medical supply chain. A long-standing HIDA priority is reauthorization of the Pandemic and All-Hazards Preparedness and Response Act (PAHPA), which expired in 2023. PAHPA would strengthen the Administration for Strategic Preparedness and Response (ASPR), modernize the Strategic National Stockpile, and support medical countermeasure development and distribution.
For distributors, PAHPA reauthorization affects federal procurement practices, stockpile turnover, readiness expectations,

By Wyeth Ruthven, Director of Congressional and Public Relations, Health Industry Distributors Association
and compliance obligations –each with direct implications for inventory management and contract opportunities.
Medicaid Payments: Coverage Shifts and Rural Impact
Medicaid policy will remain an indirect but powerful driver of supply chain dynamics. The “One Big Beautiful Bill Act,” passed in July 2025, reduces federal Medicaid funding by an estimated $911 billion over ten years, increasing pressure on providers with large Medicaid patient populations. While these changes are phased in, their impact will be felt most acutely by community and rural providers. Initiatives such as the Rural Health Transformation Program aim to help providers adapt, but uneven impacts are likely.
Taken together, these legislative efforts signal a continued focus on resilience, coordination, and preparedness. As 2026 kicks off, HIDA will continue to engage policymakers to advance solutions that protect patient access and recognize the indispensable role distributors play in sustaining healthcare delivery nationwide.


Industry News
Owens & Minor announces corporate name change to Accendra Health, Inc.
Owens & Minor, Inc. announced that it will change its name to Accendra Health, Inc. with an anticipated effective date of Dec. 31, 2025. The name change affects only the name of the parent corporation and is intended to better reflect the company’s strategic direction and future organizational focus as a leader in the home-based care market. The company will continue to use
and operate under the Apria and Byram Healthcare brands.
“The renaming of our organization is another milestone in the strategic transformation of our company as a leading, pure play home-based care business that puts the patient first while consistently delivering long-term profitable growth. Our commitment to providing the highestquality offerings to patients throughout the country remains unchanged. By becoming Accendra Health, we mark the next
Midmark enhances global healthcare through collaboration with World Vision
Midmark Corp. announced a new equipment donation to World Vision, continuing its longstanding philanthropic partnership with the global humanitarian organization dedicated to improving the well-being of children, families and communities in nearly 100 countries.
As part of this effort, in 2025 alone, Midmark Medical is donating nearly 600 sterilizers and exam tables to support healthcare delivery to communities in need. Since Midmark’s partnership with World Vision began in 2005, Midmark has leveraged its trade-in promotions to donate thousands of exam tables and other essential medical equipment to underserved regions around the world, enabling better care for communities that lack essential healthcare infrastructure.
“At Midmark, we believe that all patients deserve accessible, quality healthcare,” said Tracy Timmerman, EDAC, director of marketing at Midmark. “Through our unique trade-in program and our longstanding relationship with World Vision, Midmark is helping provide better care and improve medical services that impact lives globally.”
exciting chapter in our evolution as a company,” said Edward A. Pesicka, the company’s president and chief executive officer.
In connection with the name change, the company will change its ticker symbol to “ACH”. The company’s common stock is expected to begin trading on the New York Stock Exchange under the new name and ticker symbol on Jan. 2, 2026. Also on Jan. 2, the company launched its new website, www.accendrahealth.com. All company stock trading, filings, and market related information will be reported under the new symbol “ACH”. The company’s CUSIP number will remain unchanged, and no action is required from shareholders.
CMS creates Office of Rural Health Transformation
The Centers for Medicare & Medicaid Services recently announced the creation of the Office of Rural Health Transformation. The office will oversee management of the Rural Health Transformation Program and includes a Division of State Rural Engagement that will provide policy and operational guidance to states and other stakeholders. The office will monitor states’ implementation of the program’s initiatives to ensure compliance.
Improving Patient Health Better BP®
Heart disease is the leading cause of death for Americans today and hypertension is a contributing and modifiable risk factor for heart disease and stroke. 1 Proper patient positioning alone can lower resting blood pressure (BP) measurements by 7 mmHg systolic and 4.5 mmHg diastolic. 2 That’s why, Midmark designed the first and only fully integrated point of care ecosystem that has been clinically validated to achieve improved accuracy for a resting BP.
01 Low-height exam chair helps patients keep their back supported and feet flat on the floor
Articulating arm rail supports the patient’s arm and cuff at heart height
02 Automated vital signs promote consistency and data accuracy
03 EMR connectivity improves workflow efficiency and reduces errors
February is American Heart Month. Learn more about the 3 key considerations of Better BP and their impact on heart health. midmark.com/betterbpin3

Scan to explore the latest study reporting the cumulative effect of poor positioning that occurs when BP is taken with the patient sitting on a typical clinical exam room table.
1 https://www.cdc.gov/nchs/fastats/leading-causes-of-death.htm
2 https://www.thelancet.com/journals/eclinm/article/PIIS2589-5370(23)00396-6/fulltext
© 2026 Midmark Corporation, Versailles, Ohio USA
1
2
3





















































































