The project is being implemented with the support of UNICEF Ukraine and with financial support from the Government of Norway.
Implemented by: Partner:





The project is being implemented with the support of UNICEF Ukraine and with financial support from the Government of Norway.
Implemented by: Partner:





Dott. Paolo Tavassi
UDGEE Santa Marinella - Department of Neurorehabilitation - Bambino Ges˘ Children's Hospital
- Outcomes of periventricular leukomalacia
- Diagnosis: SPASTIC DIPLEGIA as a result of Cerebral Palsy, with increased tone in distal areas

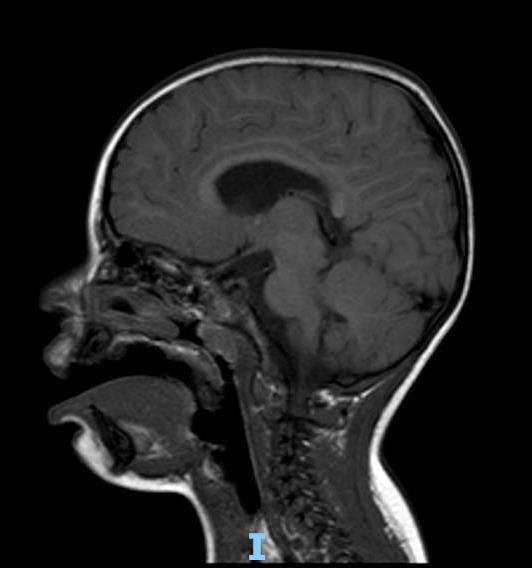
• Neuromotor profile consistent with spastic diplegia
• Passive mobilization shows joint limitation at the tibiotarsal level
• All floor posture transitions are autonomously achievable
• The child is able to reach sitting and standing positions independently; the latter is achieved with upper limb support
• Independent ambulation is possible, characterized by: anterior trunk displacement, bilateral pelvic anteversion, lower limbs in triple flexion with internal rotation, and bilateral forefoot weight-bearing
• Tibiotarsal dorsiflexion poorly reducible to 90 , with initial retractions
Included in a rehabilitation program
Good family compliance.
AFO orthoses in use
Periodic botulinum toxin injections


..and than?
Shared assessments
Physiatrists, neurosurgeons,
therapists, technicians, surgical team
Post-surgical perspectives
Comprehensive 360-degree view of the patient.
Surgical approach
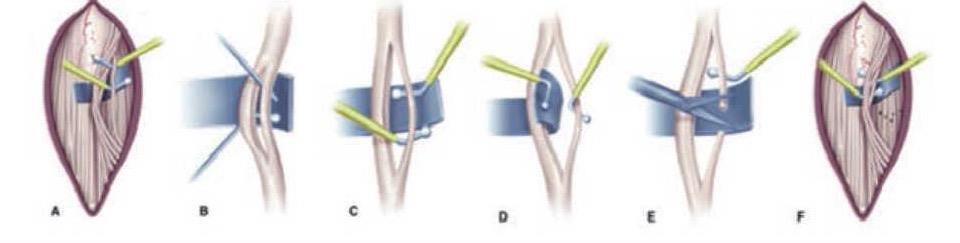
Selective Dorsal Rhizotomy (SDR) procedure
´In general anesthesia, patient prone, neurophysiological monitoring (EMG-triggered stimulation parameters: THR 0.2 ms, 1 Hz; TETANIC 0.1 ms, 50 Hz for 1 sec. Recording muscles: adductor longus, vastus lateralis, tibialis anterior, peroneus longus, gastrocnemius, abductor hallucis, anal sphincter bilaterally, iliopsoas). Midline skin incision from L1 to L3, median fascia incision, skeletonization of L2 lamina and partial of L1 and L3; L2 laminotomy; median dural incision and suspension; opening of the arachnoid; identification of midline (filum terminale and conus medullaris); rhizotomy performed as follows:
TOTAL section: left 50.6%; right 56.8%.
Hemostasis, watertight dural suture (verified with Valsalva maneuver), replacement of L2 lamina fixed with silk-0; muscular, fascial, subcutaneous and skin closure.ª
Days 1–5:
• Rest
• Guidelines and precautions
• Family education
• Gentle mobilization
• Antigravity postural transitions
• Initiation of sitting position

- Stretching
- Selective activation
- Sitting position
- Positioning orthoses

- Sitting and balance training
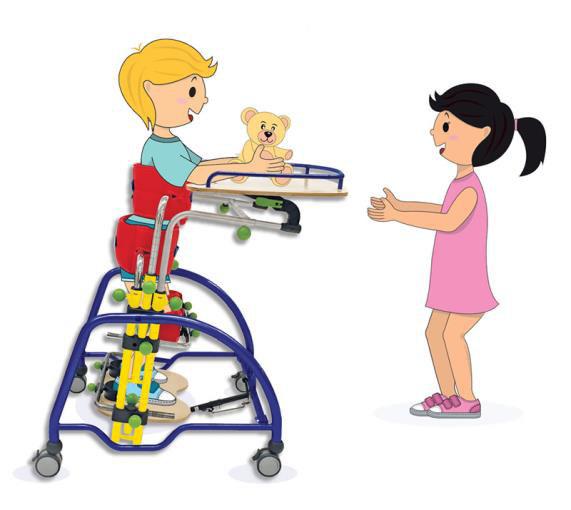
- Assisted standing with standing frame
- Transfers
- Selective activations


- Stabilization of upright posture
- Gradual resumption of gait
- Search for suitable assistive devices
- Work on rhythm and cadence




Recovery of physiological joint range of motion at hip, knee, and tibiotarsal joints
Active recruitment of lower limb muscles
Postural balance in sitting and functional use of upper limbs
Consolidation of autonomous postural transitions on horizontal and vertical planes
Promote acquisition of positive support reaction and trunk balance over lower limbs in upright position with orthoses
Gait training with orthoses and quad canes as needed
Facilitate selective flexion-extension of hip, knee, and ankle joints and reduce pathological synergy during gait
Active recruitment of lower limb muscles and gait training

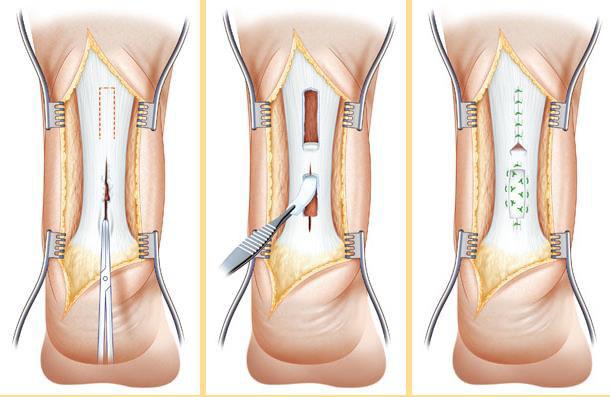
´Following orthopedic specialist visit, surgical correction of bilateral equinus foot was indicated



´
Fibrotomy-based Achilles tendon lengthening performed, achieving correction of equinus
deformity and full ankle dorsiflexionª
• Maintains orthoses
• Dressings clean and dry, to be changed as needed
• Orthoses can be removed for 3 hours in the morning and 3 hours in the afternoon
• Begin gentle mobilization of both ankles
• No weight-bearing for 15 days
Goal: Recovery of joint range of motion
Stretching
Orthotic positioning
Maintenance of joint length

Goal: Recovery of active ankle dorsiflexion •Ball exercises •Activation exercises •Muscle strengthening

Goal: Recovery of verticalization
Standing table • Sit-to-stand transitions • Maintenance of upright position

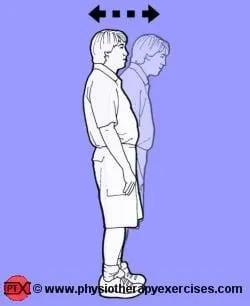
Goal: Balance and postural control •Standing perturbation exercises
Reaching tasks
Balance board

Goal: Load distribution and alternation
• Balance board with increasing difficulty
• Single-leg support exercises
• Play-based squatting to encourage posterior load shift


Goal: Recovery of correct gait pattern and ambulation
•Initial gait with double support
•Gait with pelvic support
•Exercises to vary lateralization
Recovery of functional gait with the most correct pattern possible
How do we achieve it? Working toward gradual Objectives!
• Bilateral selective segmental recruitment of the tibiotarsal joint
• Postural transitions, maintenance and control of achieved postures (correcting compensations)
• Focus on movement selectivity and trunk-limb coordination, using the pelvis as a pivot to minimize compensations and improve load transfer between sides
• Maintain optimal musculoskeletal conditions to minimize stiffness
• Sit-to-stand training without upper limb involvement
• Play-based squatting to promote posterior weight shift, guided from the pelvis
• Standing training with/without balance board for better posture and weight distribution
• Enhance single-leg control with weight-shifting exercises
• Gait pattern improvement with scapular guidance to promote dissociation of shoulder and pelvic girdles; include multidirectional walking (forward, backward, lateral)
• Elastic bands used during therapy to reduce femoral internal rotation and enhance proprioceptive input for external rotation
• Need for intensive gait training → LOKOMAT • Improved gait stability → CHANGE OF ORTHOSES
• Improved hindfoot control
• Better proximal stability
• Transition from AFO to NH T2


Importance of clinical assessments
Collaboration with the family and communitybased services
Ongoing communication with the medical team
Proposal of targeted therapeutic exercises
Interdisciplinary teamwork
Goaloriented therapeutic planning
This document was prepared in 30 slides by the Bambino Ges˘ Children’s Hospital on June 18, 2025. The contents are strictly confidential; reproduction or disclosure, even partial, is prohibited without the prior written consent of the Bambino Ges˘ Children’s Hospital