The project is being implemented with the support of UNICEF Ukraine and with financial support from the Government of Norway.
Implemented by: Partner:





The project is being implemented with the support of UNICEF Ukraine and with financial support from the Government of Norway.
Implemented by: Partner:




Pre/Post-operative evaluation, rehabilitation, and 2-year follow-up

UDGEE Santa Marinella - Neurorehabilitation
Department - Bambino Ges˘ Pediatric Hospital
F.M. b. 14/5/2017
- Preterm infant from twin pregnancy (30+5 weeks of gestational age), conceived via IVF - Neurological outcomes due to perinatal hypoxicischemic encephalopathy
- Imaging: Periventricular leukomalacia, thinning of the corpus callosum


- Diagnosis: Spastic diplegia secondary to cerebral palsy RM 1/10/2019
Followed at OPBG for outpatient visits
Physiatric consultation – 28/01/2020:
"Paralysis assessment provided; parents informed about potential treatment with botulinum toxin under NORA protocol. Rehabilitation project to include orthoses as support to therapeutic exercises."

Rx 14/10/2020
1st Botulinum Toxin Injections: 05/03/2020
Medial and lateral gastrocnemius, bilaterally
Physiatric Evaluation
14.10.2020
“Child is a good candidate for SDR, but currently not eligible due to immature motor skills and significant attention deficit, which could hinder the post-operative rehabilitation process."
3rd Botulinum Toxin Injections 10.2021
Medial and lateral gastrocnemius, soleus bilaterally
2nd Botulinum Toxin Injections: 14/04/2021
Medial and lateral gastrocnemius, bilateral posterior tibial muscles.
Neuromotor Assessment:
- Able to perform all postural transitions in the horizontal plane
- Requires upper limb support for vertical transitions
- Upright posture maintained briefly with bilateral upper limb support
- Ambulates independently with walker: trunk anteversion, narrow base of support, proximal adduction fixation, reduced swing phase
- Forefoot contact predominates, with internal rotation (worse on the right side)
- Alternates between active participation and passivity in rehabilitation setting. Low personal
Gillette Functional Assessment Questionnaire: 9
10 Meter Walking Test (10MTW): 14,5 sec (using AFO and walker) GMCS: III
Six-Minute Walk Test (6MWT): 122m, 7 stops (using AFO and walker)
Qualitative analysis shows a communication development profile where structural aspects of speech are a strength, while coherence, stereotyped language, and linguistic interests represent weaknesses.
NEUROPSYCHOLOGICAL ASSESSMENT:
Normal cognitive level. Deficits in executive function prerequisites (response inhibition, attention).
- F. is usually assisted in primary ADLs, although generally cooperative.
- Difficulties observed in dressing/undressing upper and lower body, and minor challenges with feeding and personal hygiene tasks.
- Architectural barriers: mother reports absence of a suitable shower chair.

Wee Fim II: 71/102 → 69,6%
AbilhandKids: 17/42 (13/21)
Care and Comfort

GMCS III
Satisfactory cognitive abilities
Positive response to botulinum toxin

Strong family and local network support
Good adherence to treatment
18/11/21 DH
Multidisciplinary Evaluation
surgical plan (SDR) discussed with family,
including risks and benefits.
01/22 NHC Admission for Preoperative Assessment
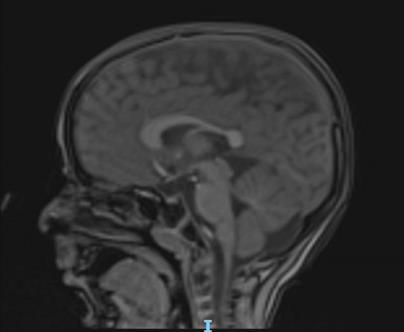
Brain and spinal cord MRI under general anesthesia
Post-void bladder ultrasound: minimal residual (~20 cc)
Neurological evaluation confirms surgical indication
Physical therapy assessment: lower limb ROM measured for pre-rhizotomy baseline
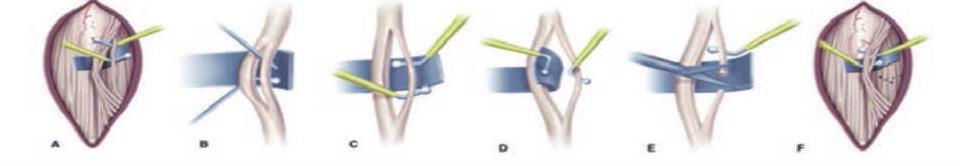
o ´Patient in prone position under general anesthesia
o Neurophysiological monitoring: tcMEP, tibial nerve SEP, BCR, free-run EMG
o EMG-triggered mapping:
THR 0.2 ms @ 1 Hz and TETANIC 0.1 ms @ 50 Hz for 1 sec
o Muscles monitored: adductor longus, vastus lateralis, tibialis anterior, peroneus longus, gastrocnemius, adductor hallucis, anal sphincter, iliopsoas (bilaterally)
o Midline incision (L1–L3), partial laminectomy at L1 and L3, full at L2
o Exposure and sectioning of dorsal roots L2–S1 bilaterally
o Left Side: L2–S1 (53.3% section)
o Right Side: L2–S1 (46.7% section)
o Dura closed watertight, lamina repositioned, standard layered closure
o No significant intraoperative neurophysiological changes
Days 1–5
- Rest
- Family education and precautions
- Gentle mobilization
- Anti-gravity postural transitions
- Begin sitting training
22/02/2022
✔ Good pain tolerance
✔ Positioning showers provided
✔ Stretching exercises
✔ Self-propelled wheelchair provided
✔ Sitting posture achieved
✔ Selective activation exercises for the lower limbs
✔ Consolidation of postural control and response to perturbations in sitting position
✔ Consolidation of autonomy in postural transitions
✔ Standing position achieved using assistive devices (static)
✔ Standing posture with external suppor
✔ Improvement in balance control
✔ Ambulation between parallel bars
✔ Use of walker
✔ Gait training to improve stepping pattern and quadripod walking training
Video Analysis:
Video Analysis:
Ashworth:
Discharge and Coordination with Local Services
• Passive/active mobilization and stretching of the lower limbs
• Reinforce sit-to-stand transitions with upper limb support
• Consolidate upright standing with hand support, progressively reducing assistance
• Correct postural compensations and promote balance between hemibodies (including with wobble board)
• Single-leg support training, with proposals for load transfer and alternation
• Step training using visual-spatial cues to achieve target step length
• Bilateral support ambulation (parallel bars)
• Ambulation using personal walker
• Initiation of bilateral quadripod training

6-Month Follow-Up – S. Paolo Clinic (14/05/2022)
Multidisciplinary Evaluation:
• Continuation of community-based therapy and intensive training in Santa Marinella
• Orthoses renewed
• Re-evaluation scheduled for September hospitalization at Santa Marinella
• Clinical team remains available for follow-up

6-Months Follow-Up
Four-week inpatient stay at UDGEE S. Marinella for intensive rehabilitation
Functional Evaluation
- Clinical presentation of spastic diplegia significantly improved post-surgery
- Increased tone during activation of adductors and internal rotators; limited plantar flexor activation
Independent and functional supine-to-stand transitions, with supervision only
Stable bench sitting posture without upper limb support; functional reaching achieved
Autonomous sit-to-stand using bimanual anterior traction
Upright posture maintained with unilateral support; mild reduction in adductor tone
Gait with bilateral quadripods: reduced step length/width, minimal hip lift during swing, full-foot contact, incomplete knee extension
Improved gait fluency and rhythm post quadripod training
Passive mobilization: increased but reducible tone in all regions

21 sessions
- Duration: 30–40 minutes for a session
- Progressive reduction of body weight support
- Progressive reduction in robotic guidance force
Active stretching Improvement in stiffness
Intensive activation of the lower limbs Endurance during gait and muscular strength
Modulation of selective activation of the lower limbs Step length optimization; focus on the swing and stance phases of gait"

Pre: FollowUp:
Pre: FollowUp:

Six-Minute Walk Test (6MWT): 75m 10 Meter Walking Test (10MTW): 43,4s
Gillette Functional Assessment Questionnaire: 5
Discharge and Coordination with Local Services
- Consolidate ambulation using quad canes, proposing training with a single quad cane exclusively during supervised therapy sessions.
Introduce walking paths and activities involving starts and stops, changes of direction, and obstacle negotiation.
- Continue to enhance performance in Activities of Daily Living (ADLs) as addressed during Occupational Therapy sessions.

Upright stance more stable
Gait performed with quadripods
4 weeks
Assessment + Intensive Treatment + Lokomat Training"
Discharge and sharing of goals with local services:
• Consolidate ambulation using a quadruped walker as a stable support.
• In standing position, promote proper balance between the hemibodies, including the use of oscillating platforms, by proposing single-leg stance exercises and transfer activities with weight shifting.
• Implement walking courses and activities involving stopping and restarting gait, changes in direction, and obstacle negotiation to improve real-life gait management.
• Propose exercises aimed at enhancing the main components of the gait pattern.
• Continue to strengthen activities of daily living (ADLs) introduced during Occupational Therapy treatment.

Functional Assessment
Independent ambulation is achieved using forearm crutches with brachial support. Mild trunk oscillations are observed in both the frontal and sagittal planes, which are used as a motor strategy to facilitate step progression.
4 weeks
Assessment + Intensive Treatment + Lokomat Training
• Consolidate ambulation with Canadian crutches
• Reduce postural compensations during gait
• Increase core stability
• Continue to strengthen ADLs through Occupational Therapy

Functional Evaluation
• Upright posture further stabilized
• Gait performed using Canadian crutches
4 weeks Assessment + Intensive Treatment + Lokomat Training
Notable development and stabilization of gross motor skills 2 years post-op
Ashworth:

Significant and stable reduction in spasticity of targeted muscle groups
Questionnaire:
Aspetti Occupazionali – Autonomie:
CS MOT COGN
The SDR intervention significantly improved the child’s daily function and autonomy
Family cooperation and consistent therapy in the community helped maintain these results
Selective dorsal rhizotomy for spasticity of genetic etiology Apr 16, 2020 L. Lohkamp, I. Coulter, G. Ibrahim Child's Nervous System
Evaluation of selective dorsal rhizotomy for the reduction of spasticity in cerebral palsy: a randomized controlled trial Apr 1, 1998 F. V. Wright, Elizabeth M H Sheil, J. Drake+2 more Developmental Medicine & Child Neurology
Pre- and Postoperative Gait Analysis and Video for Selective Dorsal Rhizotomy in Spastic Diplegia: 2-Dimensional Operative Video. Dec 27, 2018 J. Archer, A. Yaacoub, Francisco Angulo-Parker+7 more
Short- and long-term effects of selective dorsal rhizotomy on gross motor function in ambulatory children with spastic diplegia. Apr 29, 2011 P. V. van Schie, M. Schothorst, A. Dallmeijer+4 more Journal of neurosurgery. Pediatrics
Factors Associated With Long-Term Improvement of Gait After Selective Dorsal Rhizotomy. Mar 1, 2019 L. Oudenhoven, M. M. van der Krogt, M. Romei+5 more Archives of physical medicine and rehabilitation
Multidimensional Outcomes of Selective Dorsal Rhizotomy for Children With Spastic Cerebral Palsy: Single-Level Laminectomy vs Multiple-Level Laminotomy Techniques Jun 13, 2022 Zhexi He, Sui-To Wong, H. Law+4 more Neurosurgery
Selective dorsal rhizotomy in Hong Kong: multidimensional outcome measures. Jul 1, 2008 S. Chan, K. Yam, Beverley Pui-Heung YiuLau+5 more Pediatric neurology
Long term outcome of Selective Dorsal Rhizotomy for the management of childhood spasticity—functional improvement and complications Jun 23, 2020 A. Tu, P. Steinbok Child's Nervous System
Selective dorsal rhizotomy for spasticity of genetic etiology Published Apr 16, 2020 L. Lohkamp, I. Coulter, G. IbrahimChild's Nervous System
This document was prepared in 61 slides by the Bambino Ges˘ Children’s Hospital on June 18, 2025. The contents are strictly confidential; reproduction or disclosure, even partial, is prohibited without the prior written consent of the Bambino Ges˘ Children’s Hospital.