The project is being implemented with the support of UNICEF Ukraine and with financial support from the Government of Norway.

Implemented by: Partner:





The project is being implemented with the support of UNICEF Ukraine and with financial support from the Government of Norway.

Implemented by: Partner:




September 2024 – February 2025

OT MSc. Sara Gentili
sara.gentili@opbg.net
Palidoro - Neurorehabilitation
First interview
•Semi-structured occupational interview;
•Wee-Fim administration;
•Objectives selection.
First evaluation (T0)
•Occupational performance observation;
•PQRS (T0).
Treatment proposal
•Grooming;
•Dressing;
•School ADL (sharpening a pencil, writing, cutting…);
•Free time ADL (playing, drawing, playing piano/flauto);
•Hand rehabilitation;
•Use of wheelchair;
•Environmental adaptations.


Client-centred objectives
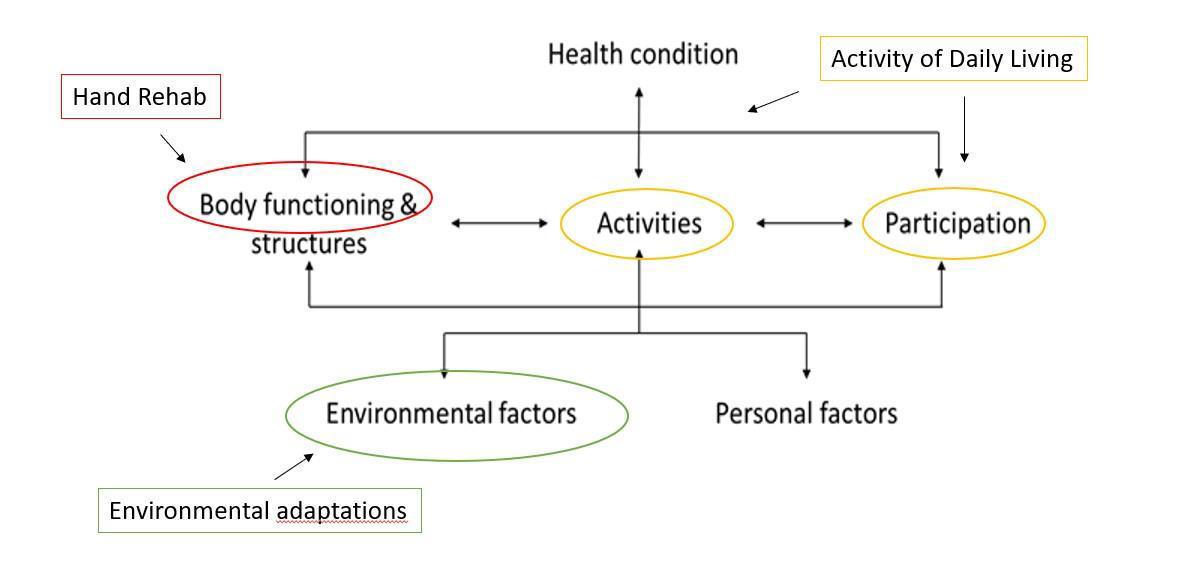
Motivating and useful occupations for Chiara’s functioning (ICF)
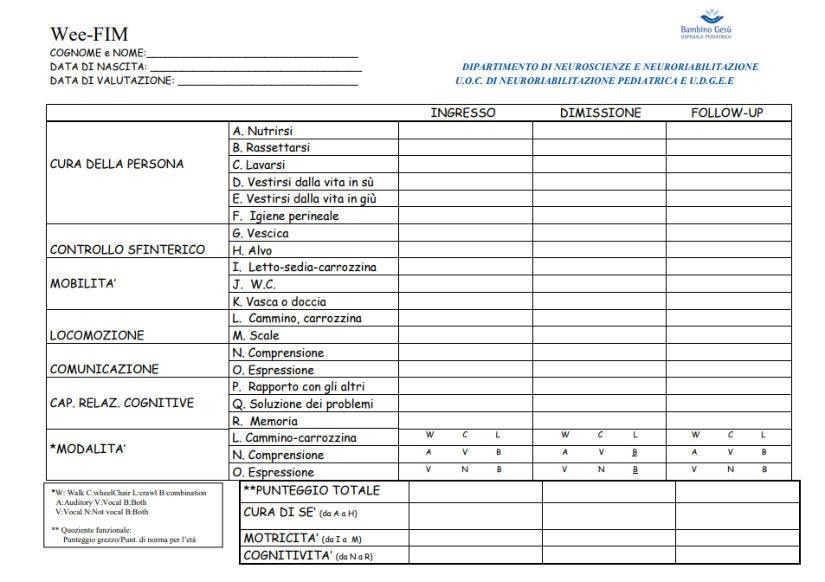
WeeFIM is an 18-item, 7-level ordinal scale instrument that measures a child's consistent performance in essential daily functional skills.
Three main domains (self-care, mobility, and cognition) are assessed by interviewing or by observing a child's performance of a task to criterion standards.
PQRS is an observational measure of performance quality of client-selected, personally meaningful activities.
It is useful to qualify the child’s overall performance in terms of quality and completeness.
It is categorized into 2 main functional streams: "Dependent" (ie, requires helper: scores 1-5) and "Independent" (ie, requires no helper: scores 6-7).
1 (total assistance); 2 (maximal assistance); 3 (moderate assistance); 4 (minimal contact assistance); 5 (supervision or set-up); 6 (modified independence); 7 (complete independence).




Functional quadriparesis with a greater involvement of the lower limbs.
Upper limbs: possible activation of proximal joint districts.
Sensibility: altered: C. outlines persistent pain, specifically at dorsal level.

At T0, C. prospects many difficulties in I/ADL, such as self hygiene, dressing, school ADL and free time ADL.
In 2025 C. is going to finish her middle school cycle. She would like to become a psychologist, that is why she is going to attend social pedagogy and social psychology high school.
Lastly, in her spare time, C. is a proud scout and a volleyball player.

She lives with her family in an indipendent barrier-free house.
For what concerns school architectural barriers, at the moment there are no accessible toilets.
Wheelchair user: at T0 C. is not able to manage a wheelchair herself, that is why she comes with a multi-functional wheelchair.

C. is a 12 years old girl who had a SCI (level C6) in summer 2024.
She is socially active: full-time student, she goes to church every Sunday.
In her spare time she also like to go out with her friends.
• The functional hand, when in absence of an active muscle capacity, must be able to make light and functional grips.
• C6 level is characterized by the presence of the active functional hand: the grip function is achieved with the active extension of the wrist, resulting in closing the fingers and bending the thumb until it touches the index.

It is important to assess the presence of the extensors that prevent the shortening of the finger flexors:
Presence of the extensors
Promotion of the retraction of flexors

Presence of both flexors and extensors
Strenghtening exercices and ADL training will be carried out


Passive and active mobilization
Forearm, wrist and finger extension – flexion
Finger curl (thumb opposition)
Hand supination – pronation
Grip – release – rolling movements
Dexterity and fine motor skills
Hand-eye coordination
Robotic rehabilitation treatment was also suggested in order to practice the following activities:
Forearm extension/flexion;
Pointing activities in peri-personal space;
Strenght measurement activities.







After the initial interview with clients, in order to build the client-centered performance context and to gather relevant information and identify the clients’ goals, a topdown approach is used to evaluate the situation with considerations of the clients’ diagnosed conditions.
Identifying strengths and problems of the patient is the further step for the therapists to implement the clients’ performance analyses.
After the performance analysis is obtained, the therapists can identify the actions that the clients do not perform well and clarify the possible cause, such as physical environments, social environments or societal constraints.
Based on the performance analysis result, the therapists choose suitable intervention approaches or plan adaptive strategies in order to compensate the clients’ ineffective actions.
Grooming
•Restorative model

T0 Wee-Fim
Self care: 23,21%
Mobility: 14,28%
Cognition: 100,00%
Total: 42,06%
Dressing (higher part)
•Restorative model
Dressing (lower part)
• Compensatory model
• Restorative model
• Compensatory model
• Restorative model
Use of wheelchair
• Compensatory model
• Educational model
Grooming/self hygiene
PQRS T0: 2 PQRS T1: 6
Dressing (higher part)
PQRS T0: 2 PQRS T1: 9
Dressing (lower part)
PQRS T0: 1 PQRS T1: 4
School ADL (sharpening a pencil, writing, cutting…)
PQRS T0: 2
PQRS T1: 6
Free time ADL (playing, drawing, playing piano/flauto)
PQRS T0: 2
PQRS T1: 7
Use of wheelchair
PQRS T0: 1 PQRS T1: 8





Many people with a C6 injury are able to use a manual wheelchair for some mobility. Limited function of your arm muscles can mean this is very tiring, takes a long time and might cause shoulder pain. They will need help to negotiate slopes, gutters and soft terrain like grass.

Some people use motorised wheels on their manual chair to be able to push their chair independently in more situations. The wheels, called “power assist technology”, magnify the force of pushing, making it easier to push with weak muscles.

It is as well important to encourage exercise and sports participation to promote health and well-being among people living with SCI.
Most people with an injury level below C6 can propel a manual chair and some individuals with a C6 level can as well.
While manual wheelchair propulsion can be a form of exercise, it can also lead to arm injuries from repetitive use.
This risk makes it critical to get the right chair, to set it up correctly and to learn how to effectively propel.
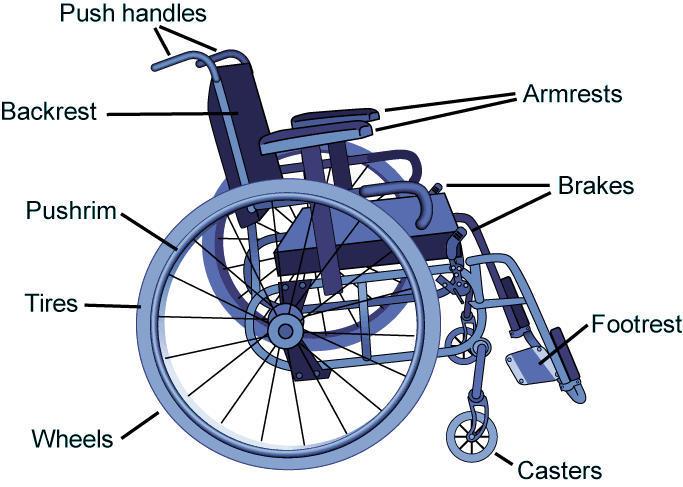
•They can be fixed, folding or swing-away and come in many different styles (better “fixed” in this case).
•They can be wraparound, full-length or desk-length; fixed or height-adjustable; removable or flip-back. Fit is important because armrest position can alter the way you propel your wheelchair.
• Many individuals choose not to have armrests because they get in the way of propulsion. Other people, as C., prefer to have them in order to complete in a more secure way her bed-to-chair transfers.
•They may be push-to-lock or pull-to-lock, positioned low or high on the wheelchair, and retractable or not, depending on what the user finds easier. Wheel locks can get in the way during propulsion and add weight to the wheelchair.
Choosing the Right Manual Wheelchair for SCI | MSKTC
C6 Complete - SpinalHub
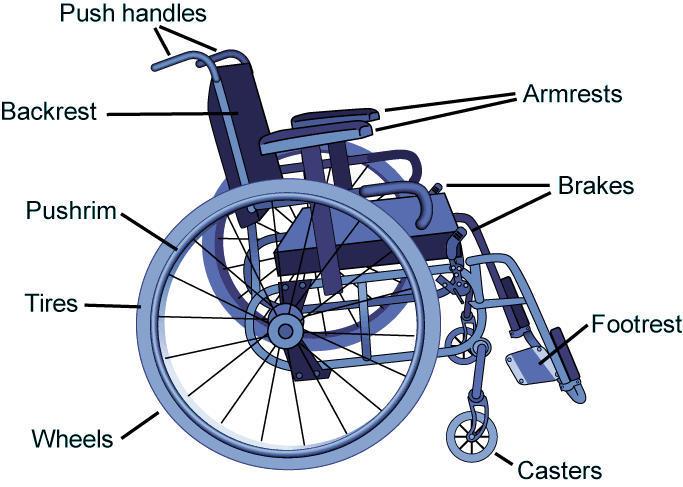
• Sling backrests are the most common, but provide little postural support. Adjustable tension backrests can provide more support and can be adjusted over time. Rigid backrests provide the best support, but may make it more difficult to collapse the chair.
• The weight and height of the backrest are important. In general, the lighter the better, with carbon fiber backrests being a nice option. If support is not needed, a lower backrest is better as it does not get in the way of pushing.
• Come in a huge and ever-changing array of different types and materials and comprise a major topic unto itself. While pressure relief is an important consideration when selecting a cushion, it is also necessary to keep in mind that it is better to provide a firm base and a light-weight cushion.
• A firm base refers to feeling stable, not sliding on the cushion when reaching for an object or propelling your chair.
• There are a variety of pushrims with different friction coatings and shapes that may assist with propulsion and reduce the risk of injury to the hand.
•It is the angle of the wheel with respect to the chair. A little camber is a good thing as it will protect your hands and increase your base of support. Too much camber will make it hard to fit through doorways.
•Including anti-tippers, wheels and caster wheels of various styles, push handles and grade-aids, which keep the chair from rolling backward.
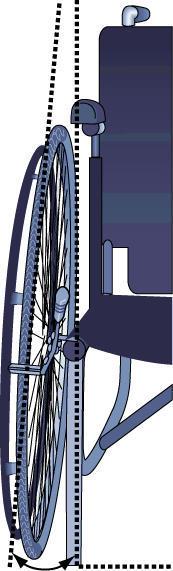
At T0, C. was not able to use her upper limbs, that is why she needed complete assistence.

A manual test drive has been provided in order to let C. experience a greater autonomy and freedom. She is at T1 able to use it, for a limited time, inside the hospital. She is as well working on slopes and soft terrains.

The patient’s desires should definitely be considered. It is very important to actively involve your patient in the evaluation process and have an open discussion / interview regarding their mobility goals.
• Many patients prefer to have a manual chair, if possible, because of the stigma associated with power — greater disability — and because of the convenience of transport in a manual chair. So why not recommend ultralight chairs for these clients?
• On the other side, a significant detail in this decision is propulsion pattern. If the patient must utilize significant compensations to create a push stroke, such as shoulder abduction, which maintains the shoulder in misalignment throughout each stroke, it is recommended power over manual. A poor propulsion pattern puts a patient at very high risk for overuse injury.
Some people are able to get themselves and their wheelchair in the car independently although there are also many people who need moderate assistance. Many of them perform a lift transfer into the car and many other people need to use a slide board. Try new
Training patients with SCI on the use of a bladder management method is essential for the independence in self-care. Intermittent self-catheterization (ISC) decreases the presence urinary tract lesions. There have been good results in patients with a C6 motor level, despite upper-limb impairment.
Il presente documento Ë stato elaborato in n.xx slide da Ospedale Pediatrico Bambino Ges˘ il xxxxxx.
I contenuti sono strettamente riservati; Ë vietata la riproduzione e la divulgazione, anche solo parziale, senza il benestare scritto di Ospedale Pediatrico Bambino Ges˘.