The project is being implemented with the support of UNICEF Ukraine and with financial support from the Government of Norway.

Implemented by: Partner:





The project is being implemented with the support of UNICEF Ukraine and with financial support from the Government of Norway.

Implemented by: Partner:




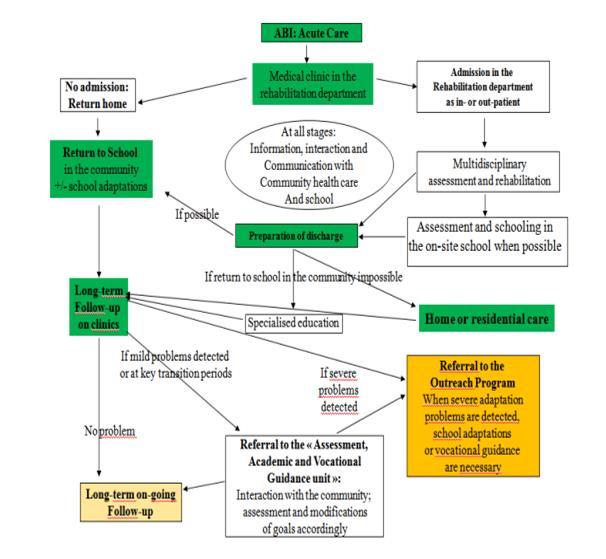
U.D.G.E.E. Neurorehabilitation



From Chevignard et al. 2009 Child: care, health and development, 36, 1, 31–43.

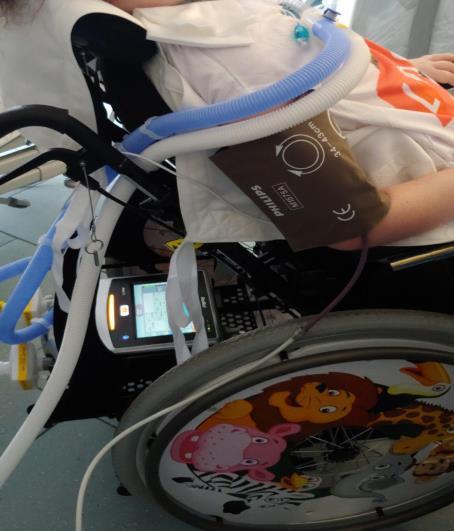
- Last decade literature shows the importance of early mobilization in ICU (Choong et al 2021; Needham et al. 2012; Kayambu et al 2013; Stiller at al. 2013)
- As shown prompt and targeted rehabilitation, together with minimize sedation and facilitating spontaneous breathing, can bring outstanding results
- A continuous exchange of information between therapists and doctors is crucial for a safe and effective work
- Partnership with families in both motor and respiratory physiotherapy can accelerate and improve the efficiency of treatment.
- However, a critical issue arises: in most Intensive Care Units, parents are allowed to enter for only a few hours, and their emotional state is often highly fragile.
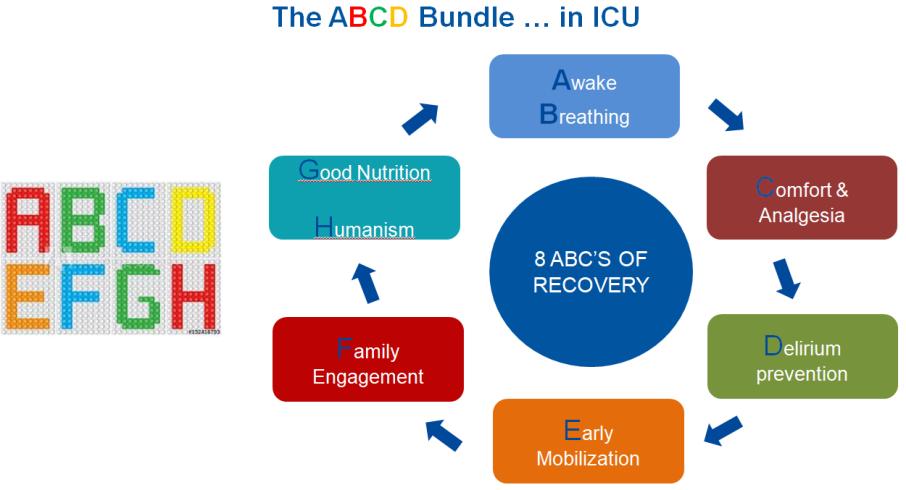

LiberAction (2021) is the latest project that highlights the necessity of an early mobilization, made thanks to cooperation between Bambino Gesù Pediatric Hospital and McMaster Children Hospital.

Ottobre 2019 Hamilton, Ontario, Canada



Evaluating the patient in the intensive care unit (ICU) with a rehabilitative perspective is essential to optimizing recovery and preventing complications.
In this way it will be possible to define more precisely: 1. Level of assistance
Objectives 3. Initial contraindications 4. The Red Flags that may arise during therapy 5. The orthoses or assistive devices the patient may need
1 MAXIMUM Total or almost total assistance by caregiver during his activities (75-100% assistance)
Patients who are sedated, non cooperative, unable to move or minimally able to participate to passive mobilization
NB: Necessary precautions
2 MODERATE Patient requires moderate to significant amount of help during his activities (25-75% of assistance)
He can partially actively participate
NB: Necessary precautions

3 MINIMUM
Patient can actively participate, but he needs some assistance (<25% assistance) and/or supervision
∙ Passive mobilization
∙ Manual therapy
∙ Passive change of decubitus
∙ Transfers to the wheelchair, manually or with lift
∙ Standing position with the Standing
∙ Semi-active/active mobilization
∙ Manual therapy
∙ Semi-active/active exercise on the bed
∙ Semi-active/active change of decubitus
∙ Sit to stand and back
∙ Transfers from bed to wheelchair and back
∙ Degait
∙ Activities of daily living
∙ Age-related skills development
∙ Increasing time of all the previous activity
∙ Acquiring or increasing social skills

SOME CONTROINDICATIONS
Only change of decubitus
Not mobilization
Orthopaedical
•Unstable fracture
•Uncontrolled bleeding
•Large gaping wounds
Neurological
•Unstable craniotomy (excessive cranial depression)
•Seizure in progress
•Confusion/delirium
•Highly invasive NIV
•High level of O2
Respiratory
Emo-cardiac
•Airways reconstructive surgery
•Hypotension
•Bradycardia
•Arrhythmia
CARDIO-RESPIRATORY
INSTABILITY

. Desaturation or respiratory distress
. Variation of heart rate (at rest),blood pressure or respiratory frequency
. Onset of arrhythmias
. Increased need of ventilator or conflict with it
NEUROLOGICAL INSTABILITY . Variation of intracranial pressure
. Agitation, depression, seizure, fainting
. Inconsolable crying
WOUNDS and SKIN
. Bleeding wounds or decubitus
. Pain
. Reddening of the skin

Inform doctors
DEVICE
ORTHOPEDIC
. Risks for devices
. Malfunctioning
. Falling
. Swelling of a joint
. Muscular pain
State of consciousness

Family
Residual functions
Side effects management (medicaltherapeuticsnursing)
Assistive devices/Orthoses
Pre-existing abilities
PHYSIATRIST
NEUROPSYCHIATRIST
NURSE

ORTHOPTIST
PSYCHOLOGIST
OCCUPATIONAL THERAPIST
DYSPHAGIA THERAPIST
PHYSIOTHERAPIST
DEVELOPMENT AL NEUROPSYCHOMOTOR THERAPIST (TNPEE)
SPEECH THERAPIST

On the basis of:
• Initial Glasgow Coma Scale (GCS)
• Duration of loss of consciousness (LOC)
• Duration of post-traumatic amnesia (PTA)

Consciousness is a multifaceted concept that has two major components:
1. Awareness of environment and of self (ie the content of consciousness)
2. Wakefulness (ie the level of arousal).
You need to be awake to be aware (REM sleep being a notable exception).
There are situations in which wakefulness and awareness are dissociated.
The most tragic example is the vegetative state.


GLASGOW OUTCOME
SCALE
SCALE
COMA RECOVERY SCALE – REVISED
• Administered within the first week of admission
• To be repeated once a month
• Self-sufficiency
• Ability to follow instructions
• Communication skills
• Social interaction
• 5 Senses
• Response to commands
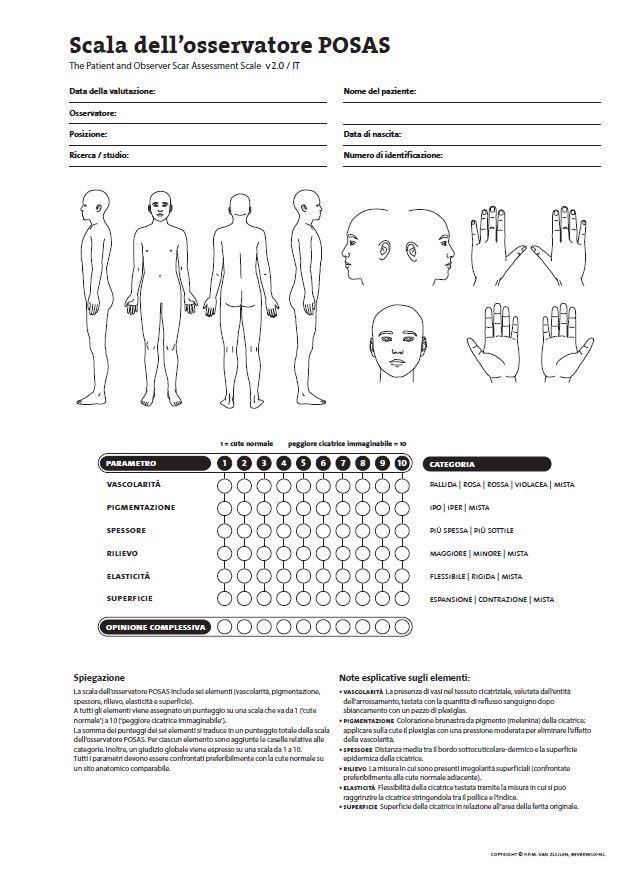
• Pain
• Vocalization

• Auditory/visual function
• Communication
• Oral function
• Alertness
• Motor skills

Therapist in conjunction with the psychologist
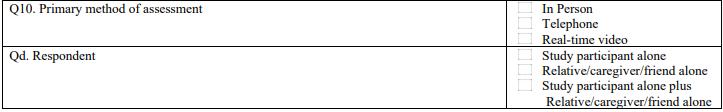
To make the assessment more aligned with the patient's present condition, the following would be advisable:
- Conduct the assessment together with the patient's treating therapist
- Choose the appropriate time of day
- Ensure that the clinical conditions are optimal
- As with any scale, it is necessary to choose the most appropriate setting, free from distracting and anxiety-provoking stimuli.

- Position and posture should be appropriate for the patient and should facilitate it (Postural system or bed).
- For standardized assessment administration, it is recommended to use tools/targets unfamiliar to the patient, or at least not routinely used in therapy, to avoid potential learning bias.
- They are administered approximately once a month, before starting the activating drug (or making a large dosage variation) or when the patient's clinical conditions change

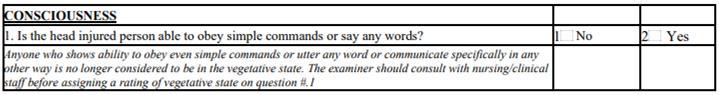
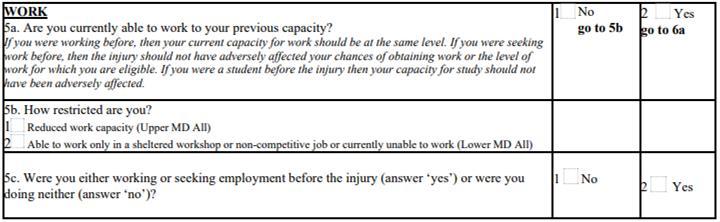
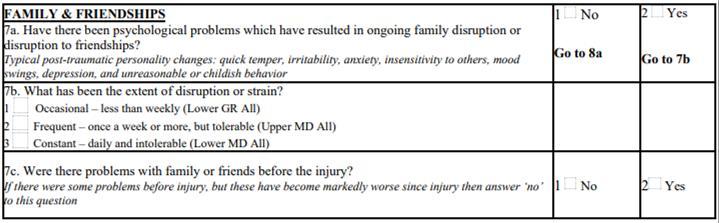
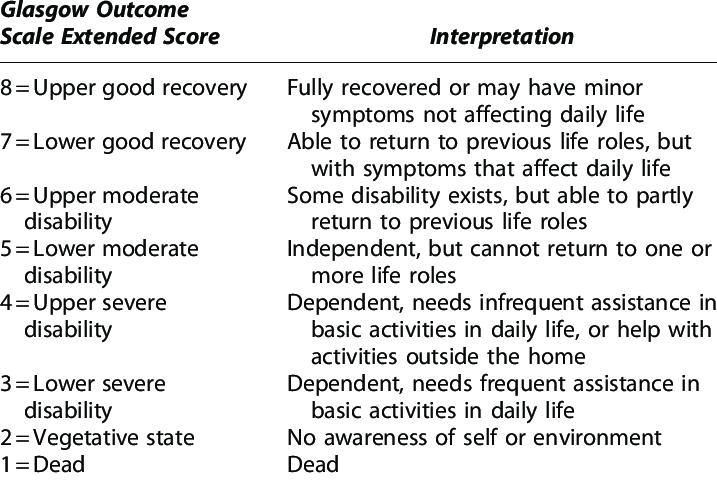
- Structured Assessment Overview
- Divided into multiple investigative areas.
- Binary response system (yes/no).
- Each area of investigation, except the first and last, includes questions about both the current situation and the pre-trauma condition.
https://siren.network/sites/default/files/gose_worksheet_hobit_12_8_21.pdf
https://reference.medscape.com/calculator/721/glasgow-outcome-scale-extended-gos-e#
- Demographic Data & Functional Status
- Consciousness (ability to follow simple commands).
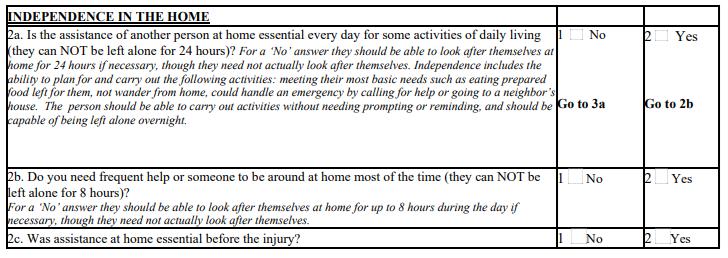
- Complete independence at home.

- Independence for less than 8 hours
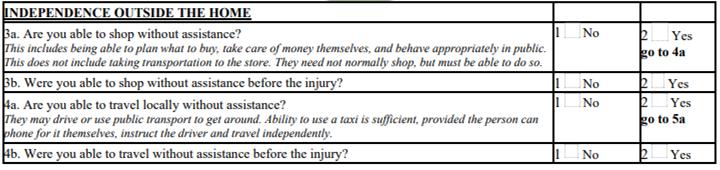
-Independence outside the home (social interactions and financial management).

- Autonomous mobility (public transport or taxi with instructions).
- Work capacity compared to pre-injury (employment, jobseeking, student).
- Potential limitations (reduced abilities, protected category, non-competitive, unemployed).
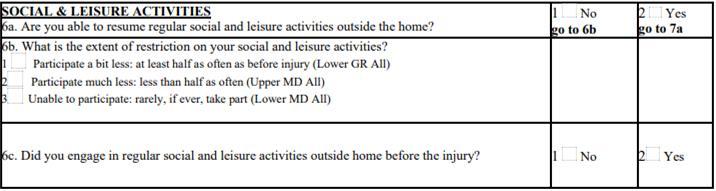
- Recreational activity (discontinuation of most activities or lack of general interest).
- Limitations in participation in social and leisure activities.
- Family and social situation (conflicts, mood or behavioral disorders).
- Frequency of conflicts or tensions.
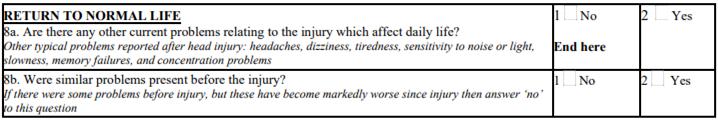
- Return to daily life (physical, cognitive, or neuro-sensory symptoms).


- Epilepsy & Neurological Outcomes (Seizure risk awareness and communication)
- Impact on outcome (neurological effects of trauma and/or other peripheral injuries).

- Score correlations.
- Sensory & Pain Perception Assessment

- Considers all sensory aspects of the patient, pain perception, and vocalization ability.
- Briefly describes the stimulus used, number of administrations, expected response, scoring system, and how to assign scores.
- Scoring:
0 → The patient fully completes the task.
2 → Partial completion.
4 → No or minimal response.
https://www.tbims.org/cnc/cncform.pdf
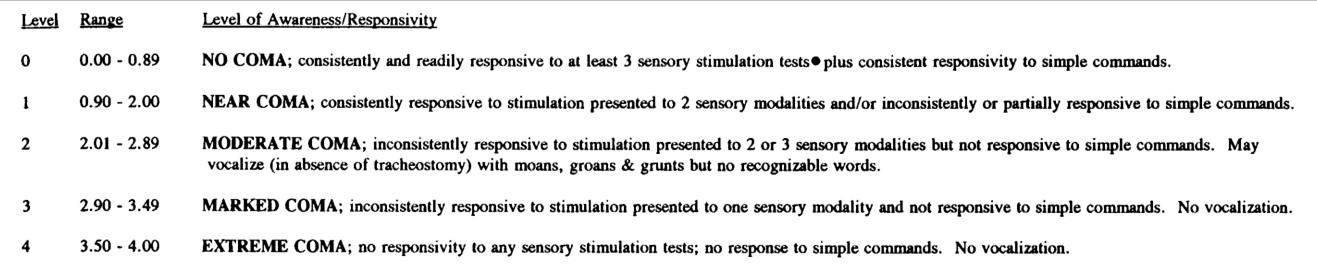


- Scores and levels of consciousness - Assessment dates & Results
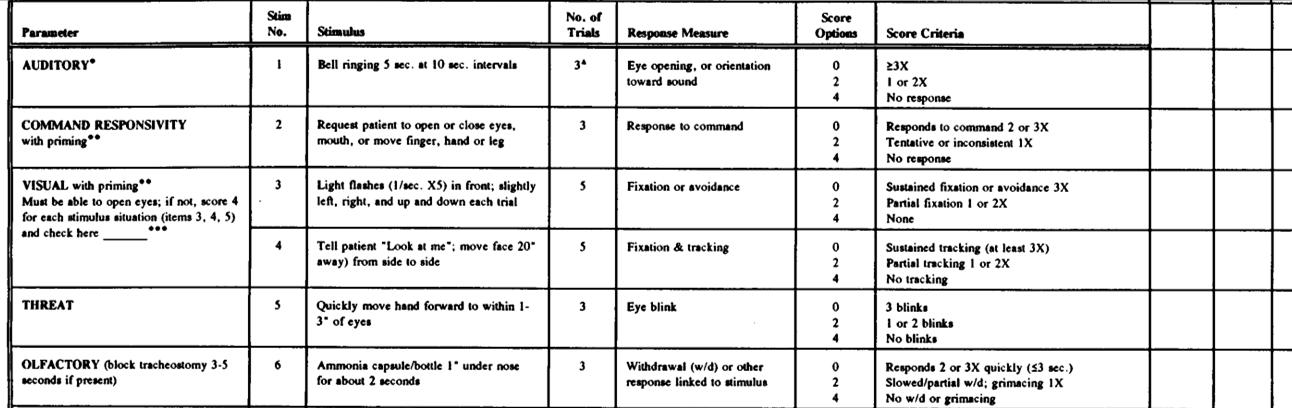
- Hearing (eye opening/orientation to bell sound).
-Command response (e.g., opening mouth, moving a body part).

-Vision (fixation and tracking of light points).
-Vision (fixation/tracking of a face).
-Threat response (blinking).
- Olfaction (reaction to unpleasant odors).
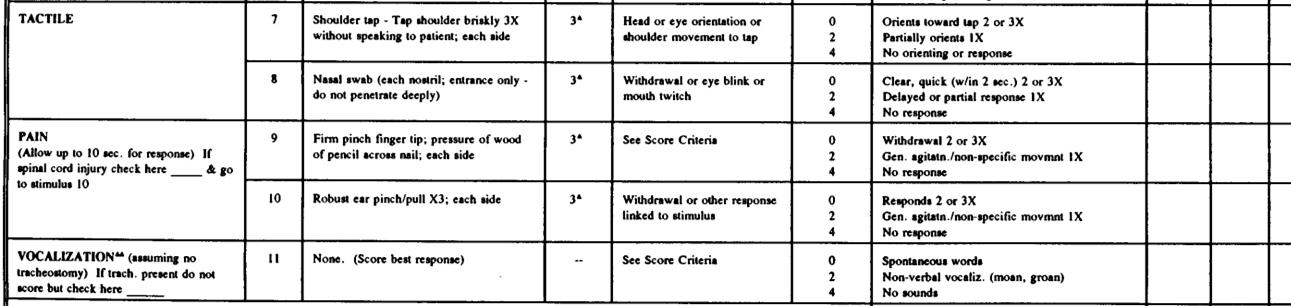
- Touch (orientation towards touch).

- Touch (withdrawal from nasal swab).
- Pain (response to pinprick pain).
- Pain (response to pressure pain).
- Vocalization.

- Evaluates broader patient functions, including auditory and visual abilities, motor functions (manual and oral), communication, and alertness
- Includes a medically relevant section on brainstem reflexes.
- Scoring is provided alongside responses, allowing for immediate identification of consciousness state (marked with an asterisk () or cross (+) depending on the patient's state or level of emergence*).
- Compared to previous two scales, this assessment is less intuitive in stimulus administration and requires greater manual consultation.
https://www.tbims.org/combi/crs/CRS%20Syllabus.pdf
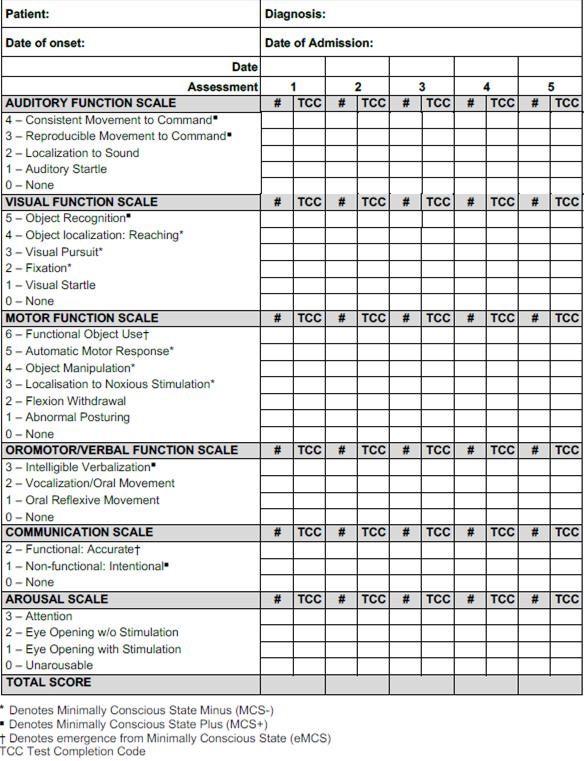
- Anagraphic data

- Auditory function (startle, localization, movements).
- Visual function (startle, fixation, tracking, localization/reaching, recognition).
- Motor function (posture, pain withdrawal/localization, manipulation/reflexive or voluntary object use).
- Oral/verbal function (reflex movements, reflexive/intelligible vocalizations).
- Communication (none, intentional but non-functional, appropriate).
- Alertness (unresponsive, eye opening with/without stimulation, attention).
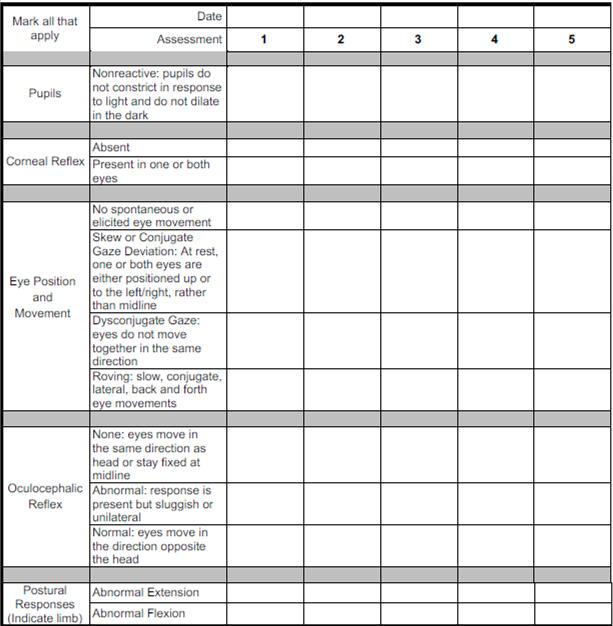
-Pupils.

-Corneal reflex.
-Spontaneous eye movements
-Oculocephalic reflex.
- Postural responses.

Assessment scales provide a snapshot of the patient's condition at the time of administration, and therefore may not fully reflect their typical daily functioning as observed by the therapist.
It is essential to supplement scale-based assessments with descriptive evaluations from each rehabilitation professional to achieve a comprehensive and patient-centered assessment.
State of consciousness

Family
Residual functions
Side effects management (medicaltherapeuticsnursing)
Assistive devices/Orthoses
Pre-existing abilities

- The residual functions outlined below are primarily related to neuromotor function
- Accurate assessment requires an interdisciplinary evaluation
- Each member of the interdisciplinary team, according to their area of expertise, investigates the patient's residual abilities
- The final rehabilitation program is developed through the integration of multiple multidisciplinary objectives
Musculoskeletal


- Muscle tone quality (Hypertonia or hypotonia)
- Muscle trophism and weakness (Complex Regional Pain Syndrome, Phlebitis)
- Joint range of motion (Calcifications)
- Fractures or dislocations (with possible involvement of the peripheral nervous system)
Evaluation tools
Modified Ashworth Scale (MAS)
Medical Research Council scale (MRC)
Range of Motion (ROM)


- Paresthesia
- Sensory impairments
- Tactile and pressure sensitivity
- Scars
- Burns
Evaluation tools
Visual Analog Scale (VAS)
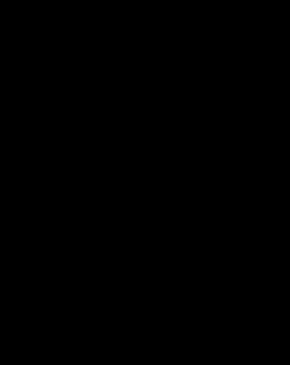
Patient and Observer Scar Assessment Scale (POSAS)
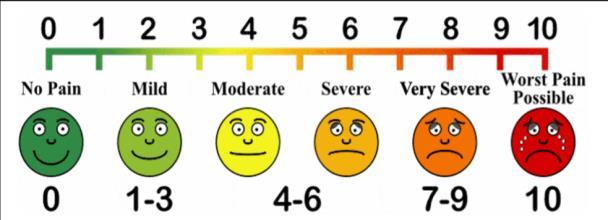

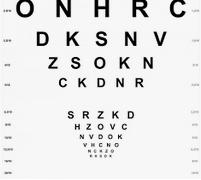
- Fixation/pursuit/saccades deficit
- Strabismus
- Nystagmus
- Diplopia
- Amblyopia
- Reduction of visual acuity
- Reduction in contrast sensitivity
- Reduction of visual field



Visuo-spatial and visuo-motor integration disorders (occipito-parietal pathway involvement)
Visual recognition disorder (occipito-temporal pathway involvement)
- Head and trunk control
- Standing position
- Gait
- Postural transitions
- Balance
- Parachute reactions
- Involuntary movements

Evaluation tools
Gross Motor Function Measure (GMFM-88 e GMFM-66)
Scale for the Assessment and Rating of Ataxia (SARA)
ABC Movement-2
Observational Gait Scale (OGS)
10 Meters and 6 Minutes Walking



- Manipulation
- Eye-hand coordination
- Bilateral coordination
- Transitive praxis (Exploration and Object use)
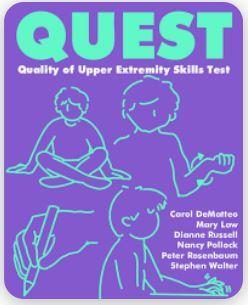
- Intransitive praxis (Expressive gestures or representational gestures)
Evaluation tools

Evaluation tools
Functional Independence Measure for Children (WeeFIM)
Pediatric Evaluation of Disability Inventory (PEDI) ADL’s
Self-care

Cognitive and social abilities
Mobility
Communication

Evaluated to prevent unexpected complications during therapy
- Secretion management (suctioning, oxygen saturation)
- Respiratory function (automatic or semi-assisted ventilator, cough effectiveness, need for manual ventilation with AMBU)
- Feeding function (PEG feeding schedules)
State of consciousness

Family
Residual functions
Side effects management (medicaltherapeuticsnursing)
Assistive devices/Orthoses
Pre-existing abilities
They assess the patient's pre-trauma status.
They allow us to:
- Set appropriate goals that are not beyond the patient’s capabilities.
- Communicate effectively with the family.
- Broaden our understanding of the context in which the patient lived and to which they will return.

Achieved developmental milestones and typical development
Under 2 years old developmental milestones are physiologically not reached
TBI on pre-existing pathology
State of consciousness

Family
Residual functions
Side effects management (medical-therapynursing)
Assistive devices/Orthoses
Pre-existing abilities
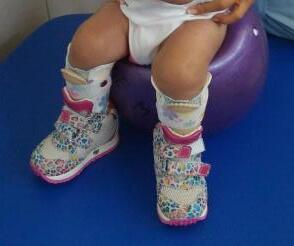



AFO
STANDING/ KAFO
BRACE


UPPER LIMB ORTHOSES
WHEELCHEAR/ POSTURAL SYSTEM
WALKER


State of consciousness

Family
Residual functions
Side effects management (medicaltherapeuticsnursing)
Assistive devices/Orthoses
Pre-existing abilities

- Significant cranial depression in the absence of an operculum.
- Vital parameter instability (vagal crises, trophic alterations).
- Pelvic and/or vertebral fracture without a containment brace.
- High-contagion infectious isolation.
- Pressure ulcers.
- Severe motor agitation.


- Consists of prolonged and fluctuating wakefulness, characterized by aggressiveness towards oneself or others, motor agitation, and oppositional behavior.
- Usually transient and short-lived
- Signals a phase of increased awakening.
- Can be dangerous for the patient due to self- or hetero-aggression or the risk of falling from the bed/postural system.
- It’s crucial to inform and reassure family members.
- The patient may be able to communicate simply and recognize objects or presented targets.
- Can be more effectively managed in therapy with two therapists or with the help of a parent.
State of consciousness

Family
Residual functions
Side effects management (medical-therapynursing)
Assistive devices/Orthoses
Pre-existing abilities
- Recognition of the impacts of pABI on the whole family
- Individualized information about diagnosis and prognosis for child’s survival and recovery
- Acknowledge of current and future plan of care
- Involvement in child's care

- Sharing information with clinician
