The project is being implemented with the support of UNICEF Ukraine and with financial support from the Government of Norway.
Implemented by: Partner:





The project is being implemented with the support of UNICEF Ukraine and with financial support from the Government of Norway.
Implemented by: Partner:





Andrea Sancesario MD PhD
andrea.sancesario@opbg.net
Neuroriabilitazione UDGEE Degenze
What is a traumatic brain injury?
A traumatic brain injury (TBI) refers to a brain injury that is caused by an outside force. TBI can be caused by a forceful bump, blow, or jolt to the head or body, or from an object entering the brain.
Not all blows or jolts to the head result in TBI.


Some types of TBI can cause temporary or short-term problems with brain function, including problems with how a person thinks, understands, moves, communicates, and acts.
More serious TBI can lead to severe and permanent disability, and even death.




Some injuries are considered primary, meaning the damage is immediate. Others can be secondary, meaning they can occur gradually over the course of hours, days, or weeks after injury. These secondary brain injuries are the result of reactive processes that occur after the initial head trauma.

There are two broad types of head injuries: Penetrating and non-penetrating.
Penetrating TBI (also known as open TBI) happens when an object pierces the skull (e.g., a bullet, shrapnel, bone fragment, etc.) and enters the brain tissue.
Penetrating TBI typically damages only part of the brain.
Non-penetrating TBI (also known as closed head injury or blunt TBI) is caused by an external force strong enough to move the brain within the skull. Causes include falls, motor vehicle crashes, sports injuries, blast injury, or being struck by an object.
Some accidents or trauma can cause both penetrating and non-penetrating TBI in the same person.
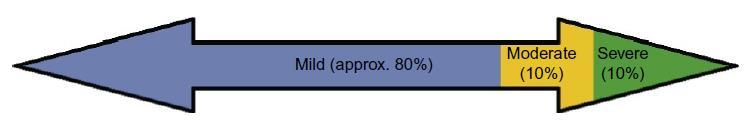
GREATER ELASTICITY FOR MILD TRAUMA
GREATER SUSCEPTIBILITY TO MILD TRAUMA
INCREASED POST-TRAUMATIC VASCULAR REACTIVITY

• Headache
• Convulsions or seizures
• Blurred or double vision
• Unequal eye pupil size or dilation
• Clear fluids draining from the nose or ears
• Nausea and vomiting

• New neurological problems, such as slurred speech, weakness of arms, legs, or face, or loss of balance


• Loss of or change in consciousness from a few seconds to a few hours
• Decreased level of consciousness (e.g., hard to awaken)
• Confusion or disorientation
• Problems remembering, concentrating, or making decision
• Changes in sleep patterns (e.g., sleeping more, difficulty falling or staying asleep, inability to wake)
• Frustration and irritability



Perception and sensation symptoms of TBI
• Light-headedness, dizziness, vertigo, or loss of balance or coordination
• Hearing problems, such as ringing in the ears
• Unexplained bad taste in the mouth
• Sensitivity to light or sound
• Mood changes or swings, agitation, combativeness, or other unusual behavior
• Feeling anxious or depressed
• Fatigue or drowsiness; a lack of energy or motivation
Children might be unable to let their caregivers know that they feel different following a blow to the head.
It is important for adults to pay attention to a child’s behavior and ask about possible symptoms following a head injury.
A child with a TBI may display the following signs or symptoms:
• Changes in eating or nursing habits
• Persistent crying, irritability, or crankiness; inability to be consoled
• Changes in ability to pay attention
• Lack of interest in a favorite toy or activity
• Sadness
• Loss of a skill, such as toilet training


TBI-related damage can be confined to one area of the brain, known as a focal injury, or it can occur over a more widespread area, known as a diffuse injury.
The type of injury also affects how the brain is damaged. The types of damage usually seen in the brain from a TBI include bleeding, swelling, and tearing that injures nerve fibers. This damage can cause inflammation, swelling, and metabolic changes.
Primary injuries occur at the time of the injury as a direct result of traumatic impact, resulting in epidural or subdural hematomas, microvascular injuries, cortical contusions, and axonal shearing.
Secondary injuries occur over hours and days, and generally result from a complex biochemical cascade of events often manifesting as cerebral edema and elevated intracranial pressure. Secondary injuries include the nonmechanical damage that may result from complex metabolic cascades set off by cell membrane disruption



• Diffuse axonal injury (DAI)
• Concussion
• Hematomas
• Contusions
• Skull fractures
• Chronic traumatic encephalopathy (CTE)
• Post-traumatic dementia (PTD)
One of the most common types of brain injuries, refers to widespread damage to the brain's white matter. DAI commonly occurs in car accidents, falls, or sports injuries. It can disrupt and break down communication among nerve cells in the brain. It also leads to the release of brain chemicals that can cause further damage.
Brain damage may be temporary or permanent and recovery can take a long time.








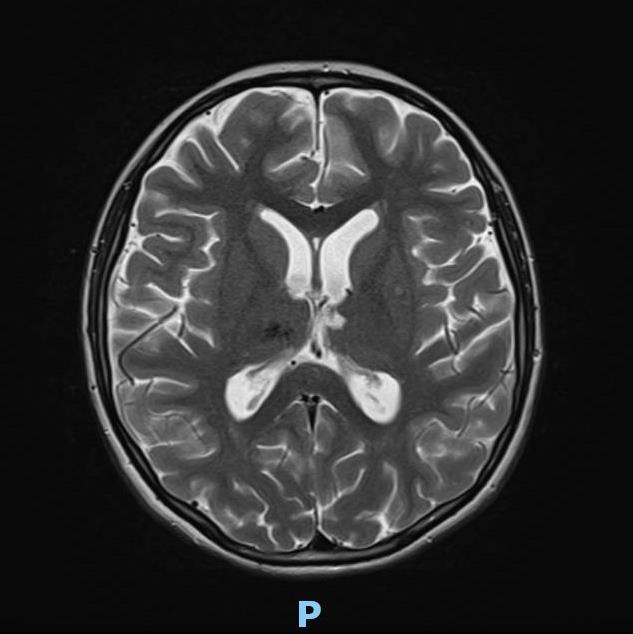





On the MRI, the diffuse axonal damage in this child is evident in the brainstem, isthmus, and splenium of the corpus callosum, the thalami, the subcortical and deep white matter in the frontoparietal regions of both hemispheres, and in the white matter of the right cerebellar hemisphere.




1. Mechanical movement of the brain tissue causes massive depolarization of neurons. The indiscriminate release of neurotransmitters opens postsynaptic receptors and intermembrane ion concentrations are disrupted as ions flow down their concentration gradients. Na+ and Ca++ accumulates in the cells. Energy demanding ATPase pumps are activated to return ionic homeostasis.
2. Calcium accumulation is managed by calcium binding proteins and sequestration into mitochondria after TBI.
3. Changes in mitochondrial electron transport enzyme activities after TBI contribute to acute decrease ATP production and increase in reactive oxygen species production. The slower maturing antioxidant systems contribute to younger age vulnerabilities.
4. Metabolism induced oxygen free radicals form along the electron transport chain. Maturational lower levels of mitochondrial superoxide dismutase (SOD) and antioxidant enzyme glutathione peroxidase (GPx) along with the younger brain’s lessened upregulation after TBI limit their capacity for reactive oxygen species management. This contributes to the oxidative stress of the cells.
5. After TBI, neurons release damage-associated molecular patterns (DAMPs), which induce morphological changes in astrocytes and microglia. In their activated states, microglia release cytokines and chemokines and astrocytes can inhibit microglial signaling and generate glial scarring that then contribute to the inflammatory cascades post injury.





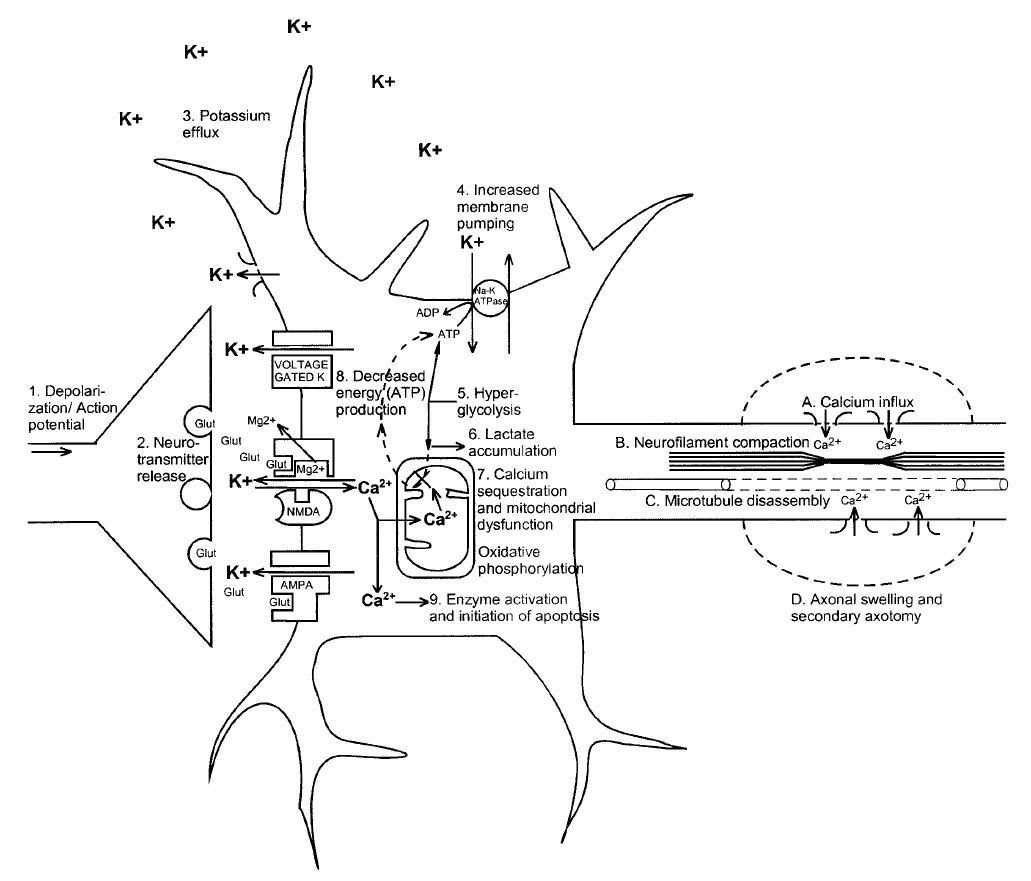
(1) Nonspecific depolarization and initiation of action potentials.
(2) Release of excitatory neurotransmitters.
(3) Massive efflux of potassium.
(4) Increased activity of membrane ionic pumps to restore homeostasis.
(5) Hyperglycolysis to generate more adenosine triphosphate (ATP).
(6) Lactate accumulation.
(7) Calcium influx and sequestration in mitochondria leading to impaired oxidative metabolism.
(8) Decreased energy (ATP) production.
(9) Calpain activation and initiation of apoptosis.
A, Axolemmal disruption and Ca2+ influx.
B, Neurofilament compaction via phosphorylation or sidearm cleavage.
C, Microtubule disassembly and accumulation of axonally transported organelles.
D, Axonal swelling and eventual axotomy.
K+, potassium; Na+, sodium; Glut, glutamate; Mg2+, magnesium; Ca2+, calcium; NMDA, N-methyl-D-aspartate; AMPA, d-amino-3-hydroxy-5-methyl-4-isoxazole-propionic acid.
Is a mild TBI that may be considered a temporary injury to the brain but could take minutes to several months to heal. Concussion may be caused by a blow to the head, a sports injury or fall, a motor vehicle accident, or a rapid movement of the brain within the skull, as can happen when a person is violently shaken. The individual with concussion either suddenly loses consciousness or their state of conscious or awareness changes suddenly.
A second concussion closely following the first one (“second hit” phenomenon) and can lead to permanent damage or even death in some instances. Post-concussion syndrome involves symptoms that last for weeks or longer.
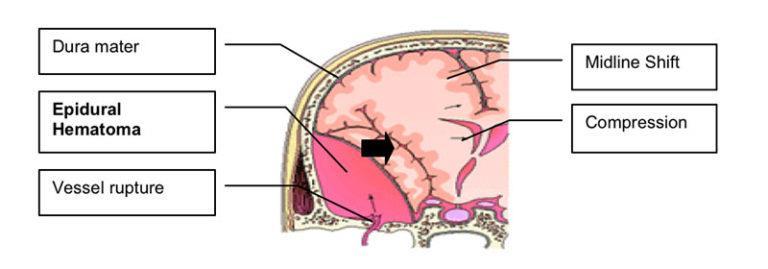
Are bleeding in and around the brain caused by a burst blood vessel. Different types of hematomas form depending on where the blood collects in the protective membranes surrounding the brain, which include the dura mater, arachnoid and pia mater
• Epidural hematomas
• Subdural hematomas
• Subarachnoid hemorrhage
• Intracerebral hematoma
- Epidural hematomas involve bleeding into the area between the skull and the dura mater. These can occur within minutes to hours after injury and are particularly dangerous - Subdural hematomas involve bleeding between the dura and the arachnoid mater, and, like epidural hematomas, exert pressure on the outside of the brain (common in older adults after a fall)

- Subarachnoid hemorrhage is bleeding between the arachnoid mater and the pia mater.
- Intracerebral hematoma involves bleeding into the brain itself and damages the surrounding tissue.


Are a bruising or swelling of the brain that occurs when very small blood vessels bleed into brain tissue. Contusions can occur directly under the impact site (coup injury) or, more often, on the opposite side of the brain from the impact (contrecoup injury). They can appear after a delay of hours to a day. These generally occur when the head abruptly decelerates, which causes the brain to bounce back and forth within the skull (such as in a high-speed car crash or in shaken baby syndrome).


Are breaks or cracks in one or more of the bones that form the skull. They are a result of blunt force trauma and can cause damage to the membranes, blood vessels, and brain under the fracture.
Helmets can help prevent skull fractures.
Bone Fractures
Subgaleal Hematoma
Epidural hematomas

Subarachnoid
Hemorrhage
Progressive neurological disorder with symptoms that may include problems with thinking, understanding, and communicating; movement disorders; problems with impulse control and depression; confusion and irritability.
While it was originally identified only at autopsy, research to date suggests CTE may be caused in part by repeated TBIs. It develops over years and can take years to show symptoms.
Studies of retired boxers have shown that repeated blows to the head can cause issues including memory problems, tremors, lack of coordination, and dementia.
Recent studies have demonstrated cases of CTE in other sports with repetitive mild head impacts (e.g., soccer, wrestling, football, and rugby).

Can arise after a single, severe TBI. PTD may be progressive and share some features with CTE.
Studies assessing patterns among large populations of people with TBI indicate that moderate or severe TBI in early or mid-life may be associated with increased risk of dementia later in life.
The initial damage to the brain described above can itself cause secondary damage. Secondary damage refers to the changes occur over a period of hours to days after the primary brain injury. Examples of secondary damage include:
• Hemorrhagic progression of a contusion (HPC)
• A breakdown in the blood-brain barrier
• Increased intracranial pressure
• Other secondary damage can be caused by infections to the brain, low blood pressure or oxygen flow as a result of the injury, hydrocephalus, and seizures.
Are injuries that occur when a contusion continues to bleed in and around the brain and expand over time.
This creates a new or larger lesion and leads to swelling and further brain cell loss.
A breakdown in the blood-brain barrier refers to the disruption of the network that controls the movement of cells and molecules between the blood and fluid that surrounds the brain's nerve cells.
Once the blood-brain barrier is disrupted, blood, plasma proteins, and other foreign substances leak into the space between neurons in the brain and trigger a chain reaction that causes brain swelling. It also causes inflammatory responses which can be harmful to the body if they continue for an extended period of time and the inappropriate release of neurotransmitters, which can damage or kill nerve cells.
Is usually caused by brain swelling inside the skull as a result of the injury. This pressure can damage brain tissue and prevent blood flow to the brain, depriving it of the oxygen it needs to function.


At its least, normal human consciousness consists of a serially time-ordered, organized, restricted and reflective awareness of self and the environment. Moreover, it is an experience of graded complexity and quantity.
William James - 1894


Consciousness is a multifaceted concept that has two major components: awareness of environment and of self (i.e. the content of consciousness) and wakefulness (i.e. the level of consciousness). You need to be awake to be aware (REM-sleep being a notable exception). There are situations in which wakefulness and awareness are dissociated. The most tragic example is the vegetative state.
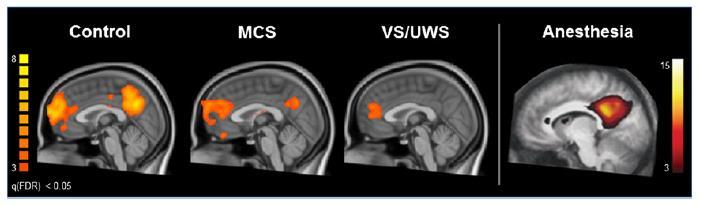
A TBI can cause problems with consciousness, awareness, alertness, and responsiveness. Generally, there are four abnormal states that can result from a severe TBI:
Coma is a specific neurobehavioral diagnostic term that denotes unarousability, with absence of sleep/wake cycles on electroencephalogram (EEG) and loss of the capacity for environmental interaction.
The neuropathologic substrate typically consists of severe, diffuse bihemispheric lesions and/or brain stem injury. When injury is localized to the brain stem (eg, hemorrhage), coma results from disruption of the reticular activating system usually involving the upper two thirds of the brain stem.
1. The patient does not open their eyes either spontaneously or in response to external stimuli 2. They do not follow any commands 3. They do not emit any intelligible words 4. They do not show any intentional movement 5. They are unable to sustain eye tracking movements within a 45° arc in any direction, even when their eyes are manually kept open 6. The above description is not secondary to the use of paralytic drugs
Vegetative State/Unresponsive wakefulness syndrome (UWS)
A result of widespread damage to the brain, people with UWS are unconscious and unaware of their surroundings.
However, they can have periods of unresponsive alertness and may groan, move, or show reflex responses.
VS is a specific neurobehavioral diagnostic term that indicates complete loss of the ability to interact with the environment despite the capacity for spontaneous or stimulus-induced arousal.
American Congress of Rehabilitation Medicine - Arch Phys Med Rehabil. 1995 76(2):205-9.
American Academy of Neurology - Arch Phys Med Rehabil. 2018 99:1710-9

Vegetative State/Unresponsive wakefulness syndrome (UWS)
• Behavioral responses consist of reflexive reactions only.
• Sleep/wake cycles may be present on EEG, and subcortical reflexes are partially or fully preserved.
• Vegetative (ie, autonomic) functions may no longer require artificial support.
• No specific neuropathological correlates exist; however, the VS is frequently observed in patients who manifest severe bi-hemispheric pathology with relative preservation of brain stem structures.
American Congress of Rehabilitation Medicine - Arch Phys Med Rehabil. 1995 76(2):205-9.
American Academy of Neurology - Arch Phys Med Rehabil. 2018 99:1710-9
Vegetative State/Unresponsive wakefulness syndrome (UWS)
1. The patient opens their eyes spontaneously or after external stimulus.
2. Criteria 2, 3, 4, 5, and 6 for the diagnosis of coma are met.
The definition of permanent vegetative state (beyond 12 months) has been changed in chronic vegetative state. Based on an expert review of the epidemiology and biology of the permanent vegetative state, the authors believe that 20 percent of patients thought to be permanently vegetative could regain consciousness.
American Congress of Rehabilitation Medicine - Arch Phys Med Rehabil. 1995 76(2):205-9.
American Academy of Neurology - Arch Phys Med Rehabil. 2018 99:1710-9
This term should be reserved for use with those patients whose responses are inconsistent but indicative of meaningful interaction with the environment.
The capacity for environmental interaction is evident on observation or is elicitable through testing.
Meaningful responses are characteristically inconsistent and often dependent on external stimulation.
American Congress of Rehabilitation Medicine - Arch Phys Med Rehabil. 1995 76(2):205-9.
American Academy of Neurology - Arch Phys Med Rehabil. 2018 99:1710-9
Any instance of comprehensible verbalization, even in the absence of any other meaningful responses, would qualify the patient as Min-R.
The characteristic neuropathologic substrate is probably similar to that found in VS (ie, bilateral, diffuse cortical damage).
American Congress of Rehabilitation Medicine - Arch Phys Med Rehabil. 1995 76(2):205-9.
American Academy of Neurology - Arch Phys Med Rehabil. 2018 99:1710-9
It applies only when there is clear evidence of:
A significant and certain behavioral response following a specific order, question, or environmental stimulus; or
In the presence of an ambiguous response, there is still evidence of a significant reduction in the response in the absence of the order, question, or stimulus to which it is associated;
The response observed at least once during a formal observation period (regular, structured, or standardized procedure).
American Congress of Rehabilitation Medicine - Arch Phys Med Rehabil. 1995 76(2):205-9.
American Academy of Neurology - Arch Phys Med Rehabil. 2018 99:1710-9
MINIMALLY CONSCIOUSS STATEfull arousal level and inconsistent but reproducible evidence of awareness
MINIMALLY CONSCIOUSS STATE +
evidence of command-following, intelligible verbalization, or intentional communication
The lack of measurable brain function and activity after an extended period of time is called brain death and can be confirmed by tests that show blood is not flowing to the brain.


Joseph T. Giacino, Joseph J. Fins, Steven Laureys and Nicholas D. Schiff. Disorders of consciousness after acquired brain injury: the state of the science. Nat. Rev. Neurol. 10, 99–114 (2014)


VEGETATIVE STATE/UNRESPONSIVE WAKEFULNESS SYNDROME
higher level of arousal without awareness of self or environment



Il presente documento è stato elaborato in n.xx slide da Ospedale Pediatrico Bambino Gesù il xxxxxx.
I contenuti sono strettamente riservati; è vietata la riproduzione e la divulgazione, anche solo parziale, senza il benestare scritto di Ospedale Pediatrico Bambino Gesù.

• The Glasgow Coma Score (GCS)
• The Glasgow Outcome Scale (GOS and GOSE)
• The Rancho Los Amigos Scale
• Coma Recovery Scale (CRS)
Most commonly used measure of primary injury in the pre-hospital and acute care setting for grading TBI severity. The resulting score reflects the primary event of direct brain injury to the parenchyma.
1. Eye opening 15-point scale with three dimensions: 2. Best verbal response
3. Best motor response

Has been used to define neurologic outcomes after TBI. The GOS score ranges from 1 (death), 2 (vegetative), 3 (severely disabled) to the more positive outcomes of 4 (moderately disabled) and 5 (good recovery).

The scale evaluates the patient's interaction with environmental stimulation as an indication of the stage of recovery from injury.
Many of the responses are associated with executive functioning, such as judgment, reasoning, attention and focus, memory, orientation to environment, and appropriateness of verbalizations and actions.
Level I No Response: No response to external stimuli Total Assistance
Level II Generalized Response: Responds inconsistently and non-purposefully to external stimuli Total Assistance
Level III
Localized Response: Responds inconsistently and specifically to external stimuli; directly related to the stimulus, patient withdraws or vocalizes to painful stimuli; more to familiar people (friends and family) versus strangers
Level IV Confused/Agitated: hyperactive state with bizarre and non-purposeful behavior; demonstrates agitated behavior that originates more from internal confusion than the external environment; Absent short-term memory
Level V Confused, Inappropriate Non-Agitated: Shows increase in consistency with following and responding to simple commands; Responses are non-purposeful and random to more complex commands; Behavior and verbalization is often inappropriate, and individual appears confused and often confabulates
Level VI Confused, Appropriate: Able to follow simple commands consistently; Able to retain learning for familiar tasks they performed pre-injury (brushing teeth, washing face) however unable to retain learning for new tasks
Level VII Automatic, Appropriate: Oriented in familiar settings; Able to perform daily routine automatically with minimal to absent confusion; Unsafe and Impulsive; Decrease social awareness; Can cary an intelligent conversation with minimum confusion
Level VIII Purposeful, Appropriate: Consistently oriented to person, place and time; Decrease tolerance to stress; some reasoning skills; Retains new tasks learned with assistance
Level IX Purposeful, Appropriate Able to shift between different tasks and complete them independently; With assistance able to think about consequences of actions and decisions; Acknowledges the emotional needs of others with stand by-assistance; Continues to demonstrate depression and low frustration threshold
Level X Purposeful, Appropriate: Able to multitask in many different environments with extra time or devices to assist; Able to create own methods and tools for memory retention;Independently anticipates obstacles that may occur as a result of impairments and take corrective actions; Able to appropriately interact with others in social situations
Minimal Assistance for Daily Living Skills
Stand By Assistance
Stand By Assistance on Request
Modified Independent









Measurement Characteristics and Diagnostic Utility. Arch Phys Med Rehabil 2004;85:2020-9
• Age at trauma < 4 years = worse prognosis
• GCS Score
• Location and extent of brain injuries
• Hypoxemia, hypotension
• Intracranial hypertension
• Severity of extracranial injuries
• Altered SEP (Somatosensory Evoked Potentials)
• Socio-economic-cultural characteristics of the family



The first acute injury management goal is to promote neuroprotection and cerebral perfusion.
Stabilization of vital parameters, weaning from support systems and drugs
Improvement of consciousness using sensorial and motor rehabilitation, the affective relationship with family members, talking to the child
Treatment of muscular spasticity and dystonic/dyskinetic disorders
Prevention of damages related to immobility, supply of orthoses and postural systems
Training for dysphagia (at least for oral secretions)
Recovery of pressure control and of lower limbs circulation using standing bed
Training of family members and psychological support and counselling
• Craniectomy
• Dysautonomia symptoms
• Seizures
• Dysphagia
• Drooling or Sialorrhea
• Deep vein thrombosis
• Spasticity
When intracranial pressure is refractory to medical management surgical intervention by a decompressive craniectomy may be required
The resected bone segment is cultured and placed in sterile frozen storage for a future cranioplasty.
When the brain edema is resolved as indicated by computerized tomography, the harvested bone segment is surgically replaced (about 6 to 12 weeks), based on the neurosurgeon's assessment.
If the autologous bone flap is unable to be used, alternative implant materials may be used (Beauchamp et al., 2010; Suarez et al., 2011)
Bone flap replacement is preferred as soon as deemed possible by the neurosurgical and rehabilitative team.
The wearing of protective head gear until replacement is based on physician preference and patient safety needs.



Prior to cranioplasty, the site of absent bone flap must be monitored for fluctuations in fluid levels, which may indicate complications as previously listed.



Dysautonomia affect 1/3 of patients after moderate to severe TBI in the first few weeks after brain injury
• Tachycardia
• Hyperthermia
• Diaphoresis
• Muscle over-reactivity


• Increased respiratory effort or rate
• Hypertension
• Pupillary dilatation

The incidence of a triad of symptoms, like hypertension, dystonia, and diaphoresis, has been studied and found to be associated with poorer outcomes, possibly from secondary brain injury from the hypermetabolic state or elevated sympathetic tone.
Compared with injured children who do not have dysautonomia, children with dysautonomia required longer rehabilitation and had less improvement in motor skills scores
In addition to strategies such as environmental controls to reduce noxious stimuli, pharmacologic management includes the use of benzodiazepines, opioid antagonists, beta-blockers, central dopamine agonists, dopamine antagonists and alpha-agonists.





After TBI, children are at increased risk for post-traumatic Seizures. Early post-traumatic seizures may occur in the first 7 days, whereas late seizures occur after 1 week.
Prophylaxis antiepileptic drug (AED) therapy is often prescribed for a minimum of 7 days.
Coordination between four stages of swallowing (oral preparatory, oral, pharyngeal, and esophageal) permit the transition of bolus from the anterior to the posterior oropharynx and esophagus; and prevent airway aspiration. Aspiration may be silent or chronic, resulting in pulmonary issues such as pneumonia or wheezing with respiratory compromise.
Swallow training is required
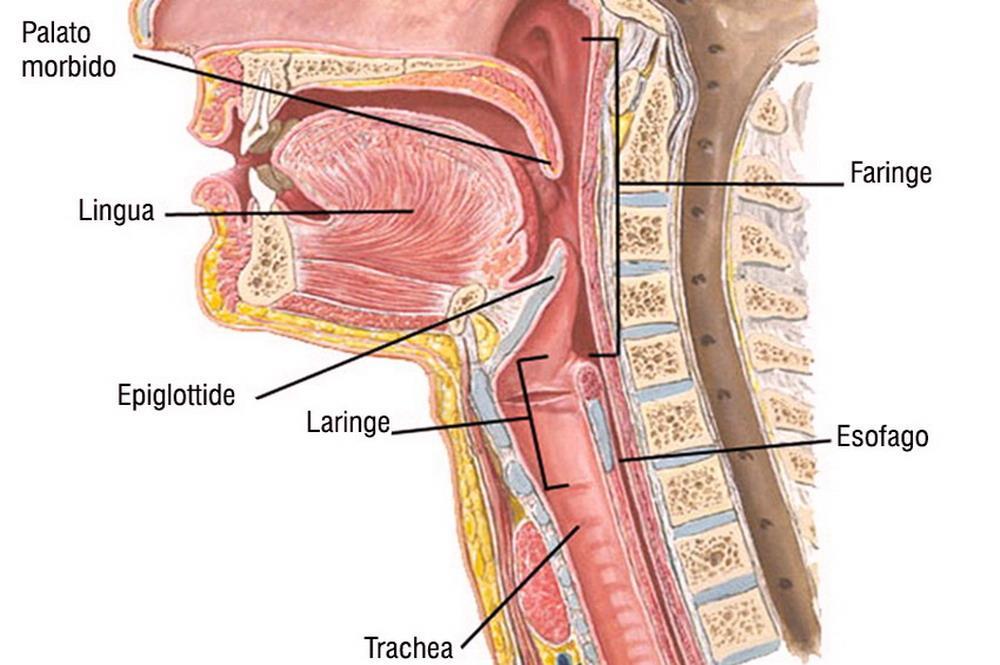
Compensatory strategies are often utilized, such as texture modification of thick liquids or solids.
Oral motor integrity plays an integral part in the ability to manage oral secretions as well.

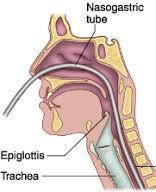
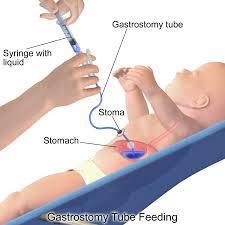
Until adequate oral nutrition is provided, alternative tube feeding options, such as nasogastric, nasojejunal, or gastrostomy feeding, are maintained to meet nutritional and caloric requirements and provide daily maintenance of fluid volumes.
Drooling is the unintentional loss of saliva from the mouth, due to and insufficient swallowing of drool or, more rarely, excess saliva production. Anterior drooling (over the lip causing visible drooling) can cause skin irritation and breakdown and may cause social embarrassment, which adversely affects a child’s social integration and quality of life.

Posterior drooling (into the hypopharynx causing coughing and aspiration) increases the risk of serious medical problems including choking, aspiration, and associated pneumonia.
Drugs commonly used are anticholinergics
- Scopolamine
- Glycopyrrolate
- Botulinum toxin injections to salivary glands blocks acetylcholine release, inhibiting secretion of saliva.





Avoid the systemic adverse effects caused by oral medications
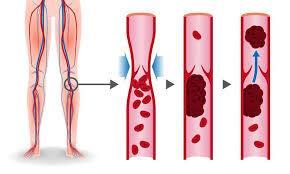
Risk increases for multi-trauma patients, who are more likely to have hemodynamic instability resulting in vascular stasis, coagulopathic states, infections, and the use of invasive hemodynamic monitoring catheters such as central venous access.
Comorbidities of extremity fractures and prolonged immobilization also contribute to such events.
Initiation of therapeutic anticoagulants as soon as the patient is considered not to be at risk for intracranial bleeding.

Early Mobilization
Anti-embolism stockings
Spasticity and elevated muscle tone commonly evolve after brain injury because of dysfunction of sensorimotor control in the upper motor neurons
Although a child requires a degree of tone for postural control during sitting and transfers, increased flexor tone and spasticity can become disabling and interfere with function.
Spastic dystonia leads to discomfort, contractures, or joint deformities, such as talipes equinovarus or scoliosis

It is important for the rehabilitation team members to monitor the spasticity for a short interval, such as 2 weeks, for natural improvement, while maximizing physical therapy with therapeutic stretching exercises and medications.
Evaluation of pain and spasticity is assessed daily by the rehabilitation team in relation to interference with functional gains, as well as caregiver tasks such as personal hygiene. This information is used to guide medication management by the medical staff.
Spasms may interfere with bowel and bladder function and result in alterations in skin integrity from vulnerable tissue pressure or sheering injury.
Medications to manage tone are started at “low and slow” doses.
- Baclofen (GABA-agonist), is most widely used initially and is titrated to tolerance and effect. Starting dose at 0,3 mg/kg per day in 2-4 somministration. Associated fatigue, in the beginning, may require a larger dose to be given initially at night. Over time the child should accommodate to the medication with fewer signs of fatigue symptoms.
- Clonidine (central alpha agonist), is also frequently used and may be transitioned from every-8-hour dosing to transdermal delivery with a 24-hour enteral bridge until the patch is effective. This method permits a more even distribution and medication effect without variability in blood pressure levels.
- Gabapentin, a modulator of excitatory neurotransmitter release, may be useful as well with additional benefit of pain relief.
- Tizanidine (alpha-2 receptor agonist), acts as a central muscle relaxant as well; however, tizanidine requires monitoring of liver enzymes for risk of acute hepatitis, which may limit its use in children.
- Benzodiazepines may be used, but sedative effects may interfere in daytime use, yielding undesired fatigue and a decreased level of alertness.
The goal of single or combined medications is to optimize spasm relief and minimize adverse effects, which impede neurocognitive recovery.
- Botulinum toxin reversible blocks pre-synaptic acetylcholine release
Indicated for focal treatment targets a specific skeletal muscle
Reduce spastic hypertonia
Improve posture
Enhance voluntary movement or overall limb functionality
Improve nursing care in patients with no voluntary activity in that segment



• Clinico-neurophysiological identification of the muscle groups to be treated: - Biomechanical and Postural assessment - Cost/benefit evaluation
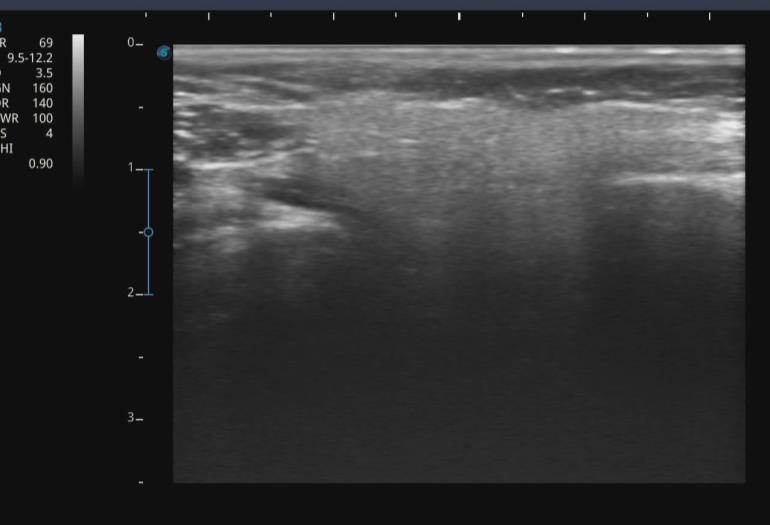
• Ultrasound-guided intramuscolar injection
• Improved diffusion through muscle activation (mobilization, stretching, bandaging)
• The effects are evident within 2 weeks and may last up to 3 months.
• Serial casting or splinting may be implemented in addition to ongoing therapy to maximize the beneficial effect of the botulinum toxin injections
Prevention of muscle-tendon contractures and joint deformities
Maintaining autonomy participation in postural transitions
Promoting hygiene care
Reducing caregiver burden

If focal treatment is ineffective and more general relief is indicated, insertion of a baclofen pump may be instituted for continuous intrathecal medication infusion.
Surgical interventions such as selective rhizotomy, tenotomy, or myotomy are reserved for failure of pharmacologic and physiotherapy management to achieve patient goals.

A direct relationship has been documented between the post-traumatic patient's outcome and the quality of rehabilitative and caregiving interventions provided during the acute phase
In the acute phase, it is essential to treat associated pathologies, prevent secondary impairments due to immobility, facilitate weaning from vital function support systems, stimulate recovery of environmental contact and consciousness.
Enhancing mechanisms of neural plasticity, even with the use of medication
In children, these aspects are even more critical considering their physical, sensory, motor, cognitive, and psycho-relational development process
Rehabilitation intervention is complicated by the instability of the clinical picture, the presence of vital sign monitoring devices, devices for supporting vital functions, intracranial pressure monitoring, infusion therapy, etc.
Alteration of consciousness due to the lesion or pharmacological therapy
Loss of vital functions (breathing, feeding, movement, vegetative crises, sphincter control, etc.)
Posture in a decorticate or decerebrate pattern, sometimes asymmetrical
Reflex motor activity
Increased muscle tone
Epilepsy, vegetative crises
Surgical issues
Internal medicine complications
Skin wounds, bone fractures
Endocrinological disorders
Presence of monitoring systems or invasive device



Treatment of respiratory and internal medicine issues







weaning from ETT, NG-tube



Prevention of immobilizationrelated pathologies
assistance with coughing
sialorrhea and dysphagia
vegetative system disturbances
of recovery

thrombophlebitis, pressure sores



postural care mobilization, orthotics
control of muscle hypertonia, dyskinesia, and dystonia

Sensory, cognitive, linguistic, AAC development



Motor, walking, upper limb
Psychological support
Dysphagia, independence in ADLs
Prevention of immobilization-related pathologies
Treatment of muscle hypertonia, dystonia, and dyskinesia (postural care, pharmacological therapy)
Stretching of hypertonic muscles and joint mobilization
Prevention of soft tissue constriction (tendons, muscles, capsules)
Timely use of botulinum toxin
Use of splints and positioning devices
Use of pressure-relieving mattresses
Early mobilization
Progressive loading with a static table


Allows for a posture different from being bedridden
Reduces muscle tone
Facilitates the recovery of the physiological length of certain muscle groups (hamstrings, triceps surae)
Opposes osteoporosis due to lack of load and activity
Allows recovery of peripheral circulatory control (orthostatic hypotension)
Stimulates environmental exploration with eyes and head, encourages control
Improves bowel regularity

The decision should be shared by:
PMR
Physiotherapist
Occupational therapist
Speech therapist
Dysphagia specialist
Family

Posture-motor pattern definition (Tetraparesis, Hemiparesis, Diparesis, Paraparesis)
Tone abnormalities (Hypotonia, Spasticity, Dystonia, Dyskinesia, Ataxia)
Functional status (Axial control, head and trunk; Upper limb functionality, visual ability)
Joint deformities (Hip dislocation, Scoliosis, Kyphosis, Pelvic obliquity, Muscle-tendon retraction, Muscle contractures)
Sensory deficits, sphincter management, skin integrity, pain




Dynamic seating system


Il presente documento è stato elaborato in n.xx slide da Ospedale Pediatrico Bambino Gesù il xxxxxx.
I contenuti sono strettamente riservati; è vietata la riproduzione e la divulgazione, anche solo parziale, senza il benestare scritto di Ospedale Pediatrico Bambino Gesù.