The project is being implemented with the support of UNICEF Ukraine and with financial support from the Government of Norway.
Implemented by: Partner:





The project is being implemented with the support of UNICEF Ukraine and with financial support from the Government of Norway.
Implemented by: Partner:





giulia.pini@opbg.net
Neuroriabilitazione UDGEE Degenza
PULMONARY REHABILITATION (PR) IS ONE OF THE CORE COMPONENTS IN THE MANAGEMENT OF PATIENTS WITH TRAUMATIC INJURIES OF NERVOUS SYSTEM AND NEUROLOGICAL DISEASES

CHILDREN WITH MEDICAL COMPLEXITY (CMC) ARE AFFECTED BY VARIOUS CHRONIC
HEALTH ISSUES THAT IMPACT MULTIPLE ORGANS AND RESULT IN SIGNIFICANT
FUNCTIONAL LIMITATIONS.
- BRAIN AND SPINAL CORD MALFORMATIONS
- METABOLIC DISORDERS
- CARDIAC OR RESPIRATORY MALFORMATIONS
- CEREBRAL PALSY AND RELATED NEUROLOGICAL SYNDROMES
- NEUROMUSCULAR DISORDERS
- TRAUMATIC BRAIN INJURY (TBI)
- ENCEPHALOPATHIES
THESE CHILDREN OFTEN EXPERIENCE RESPIRATORY ISSUES, WHICH PLAY A MAJOR
ROLE IN THEIR QUALITY OF LIFE AND ESPECIALLY IN THEIR LIFE EXPECTANCY.

• UNDERLYING CONDITION INDICATIONS vs CONTRAINDICATIONS OF PR
• BRONCHIAL SECRETIONS (quantity, quality etc)
• THORAX EVALUATION
• HEART AND RESPIRATORY RATE
• BODY TEMPERATURE, BLOOD PRESSURE
• COUGH
• LUNG AUSCULTATION
• OXYGEN SATURATION
• OXYGEN THERAPY
• NIV
• TRACHEOSTOMY
• IMAGING METHODS (X RAYS/TC etc.)

AFTER ASSESSMENT, THE PATIENT
CAN’T BE TREATED DUE TO CLINICAL CONDITIONS (ES. POST SURGERY)
AFTER ASSESSMENT, THE PATIENT STARTS THE TREATMENT
IT’S IMPORTANT TO COORDINATE THE MEDICAL AND NON MEDICAL TEAM AND SHARE THE REHABILITATION OBJECTIVES.
VARIETY OF TECHNIQUES, DEPENDING ON THE PATIENTS’ CONDITION AND NEEDS
PERFORMED BY PHYSIOTHERAPISTS THAT AIM TO PROMOTE THE MOBILIZATION AND EXPECTORATION OF SECRETIONS AND MITIGATE THE COMPLICATIONS ASSOCIATED WITH THEIR ACCUMULATION.
• COUGHING
•POSITIONING (TO ENSURE FULL PULMONARY VENTILATION)
• MANUAL AND MECHANICAL DRAINAGE TECHNIQUES
•POSITIVE EXPIRATORY PRESSURE
• AMBU
• ROLE OF PARENT/CAREGIVER
• PARENTS OF CHILDREN WITH COMPLEX MEDICAL NEEDS, REPORT TAKING ON ADDITIONAL ROLES, SUCH AS THAT OF A HEALTH CARE PROVIDER, CASE MANAGER, STUDENT, TEACHER, AND ADVOCATE (WOODGATE ET AL., 2015)
• DURING THE HOSPITALIZATION, WE EMPHASIZE THIS EDUCATIONAL PART. WE LET THE PARENTS/CAREGIVERS IN WHILE WE SET THE TREATMENT SO THEY CAN SEE HOW TO DO IT. WE THEN WAIT UNTIL THEY BECOME CONFIDENT AND START TO TRY AND DO BY THEIRSELVES.
• CONSTANTLY GUIDE AND SUPPORT.
A REFLEX COUGH HAS FOUR PHASES—IRRITATION, INSPIRATION, COMPRESSION, AND EXPULSION—BUT A VOLUNTARY COUGH DOES NOT REQUIRE THE FIRST PHASE. TO BE EFFECTIVE, COUGH MUST GENERATE ENOUGH FORCE TO CLEAR SECRETIONS FROM THE AIRWAYS, WHICH USUALLY INCLUDE THE FIRST FIVE OR SIX GENERATIONS OF BRONCHI.
THE PHYSICAL THERAPIST IMPROVES A COUGH BY INSTRUCTING THE PATIENT IN PROPER COUGH TECHNIQUE.
- POSITIONING - HUFFING - TRACHEAL STIMULATION

IF THESE TECHNIQUES FAIL TO CLEAR THE AIRWAY, OR WE HAVE UNCOOPERATIVE PATIENTS , WE USE THE MECHANICAL INSUFFLATOR–EXSUFFLATOR.
A MECHANICAL INSUFFLATOR/EXSUFFLATOR USES POSITIVE PRESSURE VIA A FACEMASK OR MOUTHPIECE TO DELIVER A MAXIMAL LUNG INSPIRATORY VOLUME, FOLLOWED BY AN ABRUPT SWITCH TO NEGATIVE PRESSURE TO THE AIRWAY FOR FORCED EXPIRATION, WHICH SHOULD TRANSPORT MUCUS TO THE CENTRAL AIRWAYS AND OUT OF THE PATIENT.
THE RAPID CHANGE FROM POSITIVE TO NEGATIVE PRESSURE SIMULATES AIRFLOW CHANGES EXPERIENCED DURING A NORMAL COUGH MANOEUVER WITH THE HIGH EXPIRATORY AIRFLOW CARRYING MUCUS UPSTREAM.
• INSUFFLATION AND EXSUFFLATION PRESSURES AND TIMING ARE AGREED BY THE MEDICAL TEAM
• PRESSURE STARTING POINT TIPICALLY AROUND +/- 30CM H2O AND GRADUALLY INCREASES
• TIMING TIPICALLY FROM 1 TO 3 SEC
CONTRAINDICATIONS:
• PNEUMOTHORAX
• CARDIOVASCOLAR COLLAPSE
• UNCONTROLLED ARYTHMIAS
• FACIAL TRAUMAS

TREATMENT CONSISTS OF 4/5 CYCLES OF INSUFFLATION AND EXSUFFLATION, ALTERNATED WITH 30/60 SECONDS OF PAUSE BETWEEN EACH CYCLE.
X 4
THE NUMBER OF DAILY SESSIONS DEPENDS ON THE DEGREE OF OBSTRUCTION AND FATIGUE OF THE PATIENT

PAY ATTENTION TO THE PATIENT'S FATIGUE AND/OR HYPERVENTILATION
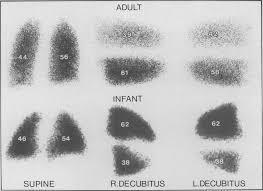
POSITIONING TO DRAIN A PARTICULAR SEGMENT OR LOBE
REQUIRES THAT THE AREA TO BE DRAINED SHOULD BE UPPERMOST, WITH THE BRONCHUS FROM THE AREA IN AS CLOSE TO A VERTICAL POSITION AS IS POSSIBLE OR REASONABLE.
• IN THE SUPINE POSITION, VENTILATION IS GREATER IN THE POSTERIOR PART OF THE LUNG (WHICH, IN THIS POSITION, IS THE LOWEST PART), COMPARED TO THE ANTERIOR PART (WHICH, IN THIS POSITION, IS THE HIGHEST PART).
• IN LATERAL POSITION, VENTILATION IS GREATER IN THE LOWER PART (I.E., IN THE LUNG ON THE SIDE THE PERSON IS LYING ON). IN INFANTS IS THE OPPOSITE.
THIS GROUP OF TECHNIQUES REPRESENTS THE CLASSIC AND TRADITIONAL APPROACH TO AIRWAY CLEARANCE.
PERCUSSION AND VIBRATION OF THE THORAX ARE FREQUENTLY PERFORMED AS A MEANS OF LOOSENING ACCUMULATED SECRETIONS TO ENHANCE THEIR MOVEMENT
TO THE MORE PROXIMAL AIRWAYS ASSOCIATED WITH POSITIONING FOR GRAVITYASSISTED POSTURAL DRAINAGE.
THESE TECHNIQUES ARE USUALLY PERFORMED IN AN AREA OF THE THORAX CORRESPONDING TO THE LUNG SEGMENT BEING DRAINED WHILE THE PATIENT IS SPECIFICALLY POSITIONED.


POSITIVE EXPIRATORY PRESSURE (PEP) BREATHING IS ANOTHER MECHANICAL DEVICE
EMPLOYED FOR AIRWAY CLEARANCE DYSFUNCTION.
PEP MASK WAS DEVELOPED IN ATTEMPT TO MAINTAIN AIRWAY PATENCY WITH THE USE OF EXPIRATORY AIRFLOW TO DISLODGE AND MOVE SECRETIONS PROXIMALLY IN THE RESPIRATORY TRACT.
PEP CAN BE USED WITH ANESTHESIA FACE MASK, MOUTHPIECE OR CATETER MOUNT FOR TRACHEOSTOMY USE.
AS THE PATIENT EXPIRES, THE PEP VALVE PROVIDES A POSITIVE PRESSURE OF 10 TO 20 CM H2O WITHIN THE AIRWAYS. THIS POSITIVE PRESSURE STABILIZES THE SMALL AIRWAYS, THEREBY PREVENTING THEIR COLLAPSE
PATIENTS TIPICALLY EXECUTE 2 SESSIONS PER DAY, EVERY DAY.
EACH SESSION CONSTITUTED BY 10 CYCLES (1 MINUTE OF BREATHING INTO THE MASK/TRACHEOSTOMY, 30 SEC/1 MINUTE OF REST).




CONTRAINDICATIONS:
• UNTREATED PNEUMOTHORAX
• ACUTE ASTHMA
• ACUTE RESPIRATORY DISTRESS SYNDROME
• POST-SURGICAL PERIOD
• PATIENTS WITH NEUROMUSCULAR DISEASES
• HEART DISEASES AND RELATED CONDITIONS (AFTER MEDICAL OPINION)
• BRONCHOSPASM
• CONDITIONS PREDISPOSING TO INCREASED INTRACRANIAL PRESSURE.
• A TECHNIQUE AIMED AT MODIFYING AIRFLOW WITHIN THE AIRWAYS IN ORDER TO EXPAND THE CHEST AND FACILITATE THE UPWARD MOVEMENT AND REMOVAL OF SECRETIONS.
• IT ALLOWS FOR GREATER INDEPENDENCE FROM THE VENTILATOR, ESPECIALLY DURING DAYTIME HOURS.
• TIPICALLY, INSUFFLATIONS ARE PERFORMED IN SUPINE AND LATERAL POSITION, THREE CYCLES OF 10 INSUFFLATIONS IN EACH POSITION.

SIGNS AND SYMPTOMS OF HYPERVENTILATION


AIR STACKING (AS) EXERCISE INCREASES THE CAPACITY TO STACK AIR WITH DEEP
INSUFFLATIONS AND CAN IMPROVE COUGH EFFECTIVENESS
1. CLOSE THE NOSE WITH A CLIP AND INSERT THE MAK/MOUTHPIECE
2. ASK THE PATIENT TO TAKE A DEEP INSUFFLATION WHILE THE THERAPIST
SQUEEZES THE RESUSCITATOR BAG
3. REMOVE THE MOUTHPIECE AND ASK THE PATIENT TO RAPIDLY EXSUFFLATE.
THERAPIST CAN PERFORM AN ABDOMINAL THRUST


THE INCENTIVE SPIROMETER IS A DEVICE THAT MEASURES THE VOLUME OF THE AIR INHALED INTO THE LUNGS DURING INSPIRATION.
WHEN BREATHING IN THROUGH AN INCENTIVE SPIROMETER, A PISTON RISES
INSIDE THE DEVICE AND MEASURES THE VOLUME OF THE INSPIRED AIR
THE INCENTIVE SPIROMETER USES VISUAL FEEDBACK TO ASSESS A PATIENT'S INSPIRATORY EFFORT BY MEASURING THE INHALATION VOLUME
INSPIRATORY MUSCLE TRAINING IS A VITAL
FACTOR IN REDUCING OR PREVENTING
POSTOPERATIVE PULMONARY COMPLICATIONS.
USING AN INCENTIVE SPIROMETER FOLLOWING
SURGERY CAN HELP PRESERVE THE LUNGS' INTEGRITY AND KEEP THE LUNGS CLEAR.
DEEP BREATHING SUPPORTS THE MOVEMENT OF SECRETIONS AND ASSISTS IN OPENING LUNG SPACES THAT MAY HAVE BECOME COLLAPSED


Il presente documento è stato elaborato in n.xx slide da Ospedale Pediatrico Bambino Gesù il xxxxxx.
I contenuti sono strettamente riservati; è vietata la riproduzione e la divulgazione, anche solo parziale, senza il benestare scritto di Ospedale Pediatrico Bambino Gesù.