Epidemiologic and clinical characteristics of pediatric SARS-CoV2 infection

Dr. Mary H Lombardi – Dr. Andrea Campana

Lazio regional pediatric COVID center

Pediatric Multispecialty Unit
Emergency and General Pediatrics Department
Bambino Gesù Children’s Hospital, IRCCS, Rome, Italy
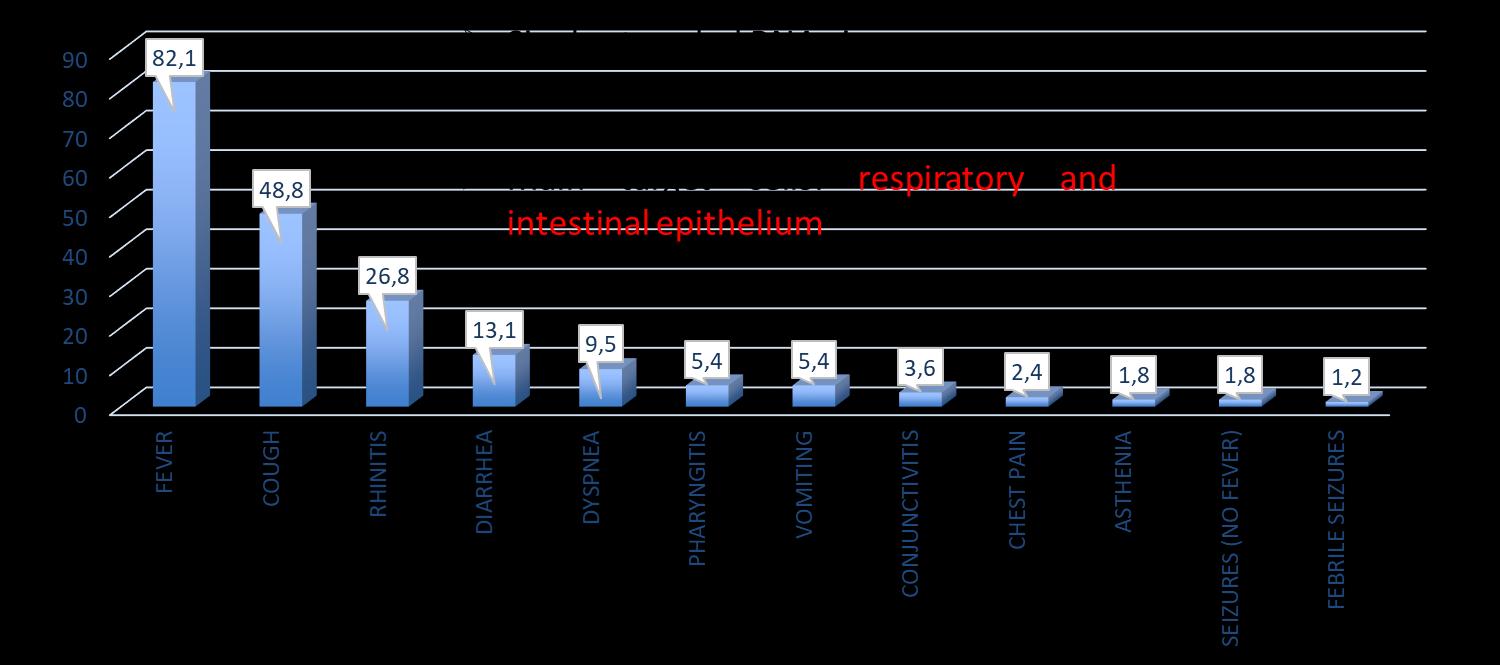
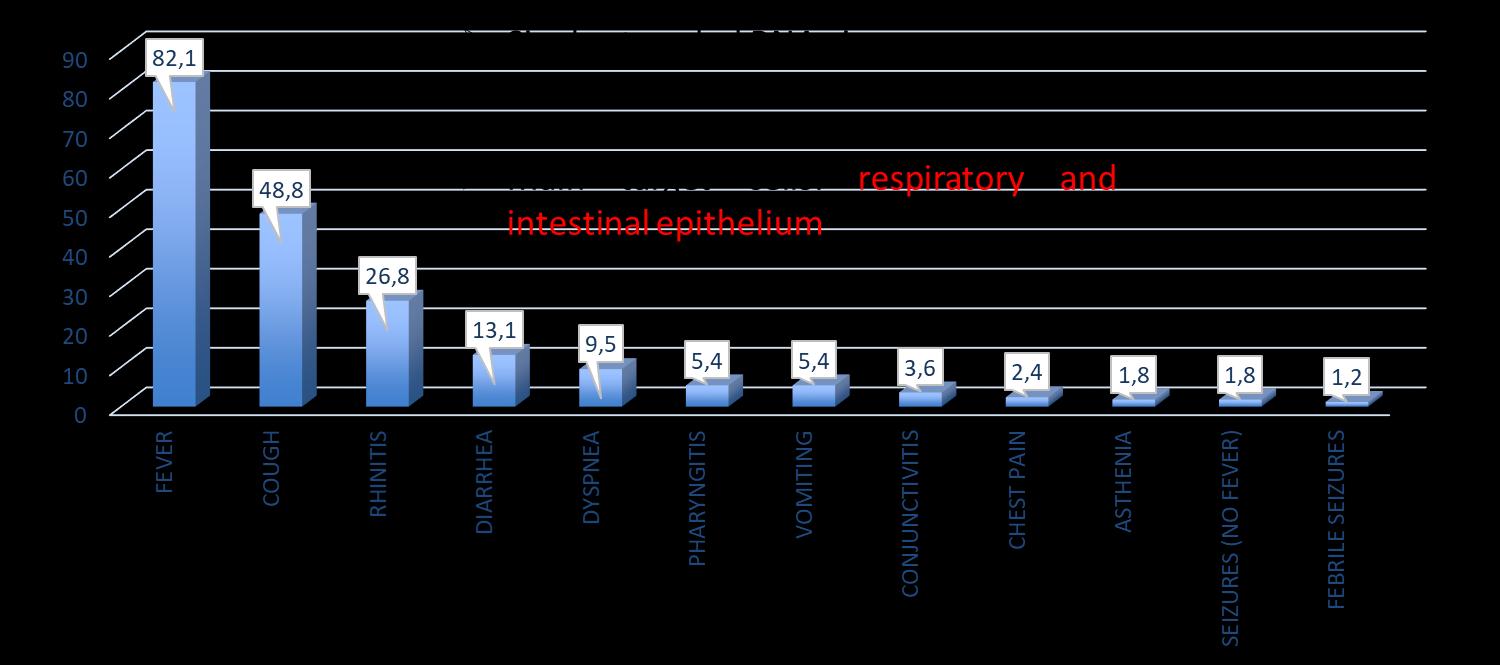
COVID-19 SYMPTOMS IN CHILDREN

(Garazzino et al. Multicentre Italian study of SARS-CoV-2 infection in children and adolescents, preliminary data as at 10 April 2020. Euro Surveill. 2020;25(18):pii=2000600. https://doi.org/10.2807/1560-7917.ES.2020.25.18.2000600)

and clinical characteristics of pediatric SARS-CoV2 infection

2
Epidemiologic
COVID-19 SYMPTOMS IN CHILDREN

(Garazzino et al. Multicentre Italian study of SARS-CoV-2 infection in children and adolescents, preliminary data as at 10 April 2020. Euro Surveill. 2020;25(18):pii=2000600. https://doi.org/10.2807/1560-7917.ES.2020.25.18.2000600)

and clinical characteristics of pediatric SARS-CoV2 infection

Epidemiologic
3
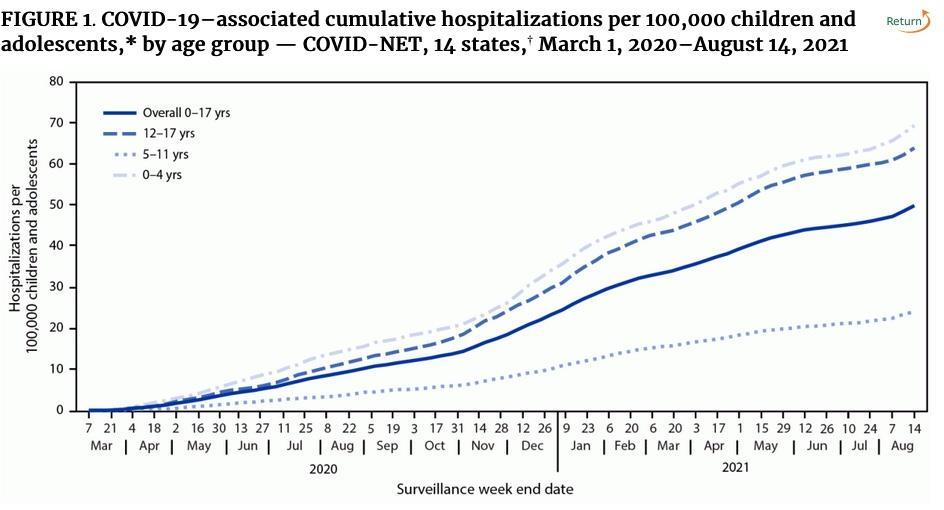
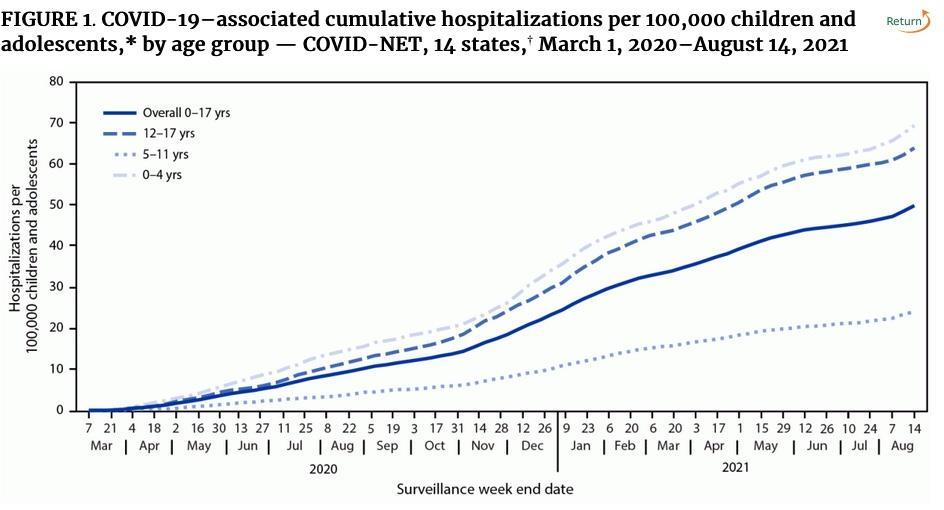
CHILDREN HOSPITALIZED WITH COVID

The majority of children (65.1%) were hospitalized
Hospital admission was inversely related to age (p < 0.01; Fisher exact test);

Children and COVID-19: State-Level Data Report (Sept 2021)



Epidemiologic and clinical characteristics
4
of pediatric SARS-CoV2 infection
CHILDREN HOSPITALAZED WITH COVID
However, some kids still do get admitted
…
Our experience:
OPBG – PALIDORO
Lazio Regional Pediatric COVID center

(16 march 2020 – 18 sept 2021)


Total confirmed admitted pediatric cases 678

M/F = 1.18/1
Mean age 6,3 years (median 3,7)
Lazio -- Population 6 million Population < 20years --- 1 million

characteristics of pediatric SARS-CoV2 infection
Epidemiologic and
5
clinical
CHILDREN HOSPITALAZED WITH COVID
MMWR --- Delahoy MJ, Ujamaa D, Whitaker M, et al. Hospitalizations Associated with COVID-19 Among Children and Adolescents — COVID-NET, 14 States, March 1, 2020–August 14, 2021. MMWR Morb Mortal Wkly Rep 2021;70:1255–1260. DOI: http://dx.doi.org/10.15585/mmwr.mm7036e2



and clinical characteristics of pediatric SARS-CoV2 infection

Epidemiologic
6
CHILDREN HOSPITALAZED WITH COVID








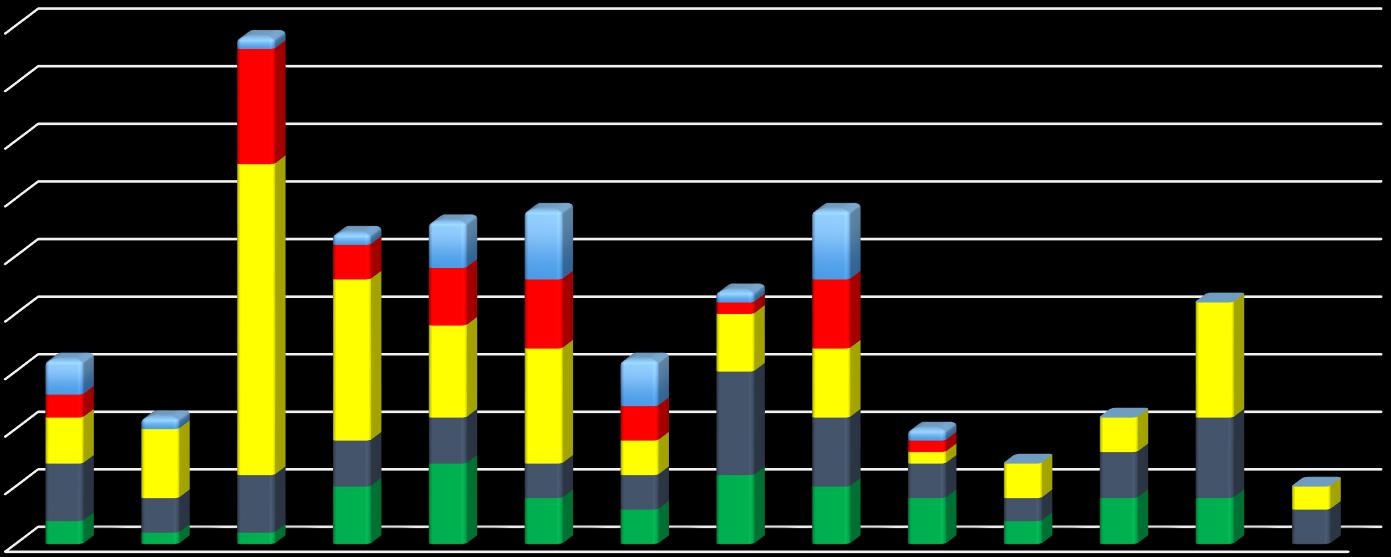
Epidemiologic and clinical characteristics of pediatric SARS-CoV2 infection 7 0 5 10 15 20 25 30 35 40 45 GI PNEUMONIA NEUTROPENIA MIO-PERICARDITIS MIS-C 31 PZ TOT: PICU 8: SURGICAL PROC. 14: SEIZURES 2: MONOCLONAL AB 6: REMDESEVIR
CHILDREN HOSPITALAZED WITH COVID



Epidemiologic and clinical characteristics of pediatric SARS-CoV2 infection 8 Age N° PTS COMPLICATIONS NO COMPL MINOR COMPL GI PULM MIS-C MYO-PERICARDITIS 0-1 216 126 80 1 5 2 6 2-6 175 115 30 8 14 6 6 7-10 75 49 7 12 6 6 6 11-14 88 45 11 14 10 12 16 >14 124 67 13 14 26 3 5 TOTAL 678 402 (59%) 141 49 61 29 39
CHILDREN HOSPITALAZED WITH COVID

Therapy
= Supportive
Monitor vital signs, urine output, weight

Fever control
IV fluids
Oxygen if needed
Antibiotics only if you suspect an overinfection
Anticoagulation only if risk factors

Epidemiologic and clinical characteristics of pediatric SARS-CoV2 infection 9
CHILDREN HOSPITALAZED WITH COVID



Epidemiologic and clinical characteristics of pediatric SARS-CoV2 infection 10 Age N° PTS COMPLICATIONS NO COMPL MINOR COMPL GI PULM MIS-C MYO-PERICARDITIS 0-1 216 126 80 1 5 2 6 2-6 175 115 30 8 14 6 6 7-10 75 49 7 12 6 6 6 11-14 88 45 11 14 10 12 16 >14 124 67 13 14 26 3 5 678 402 (59%) 141 49 61 29 39
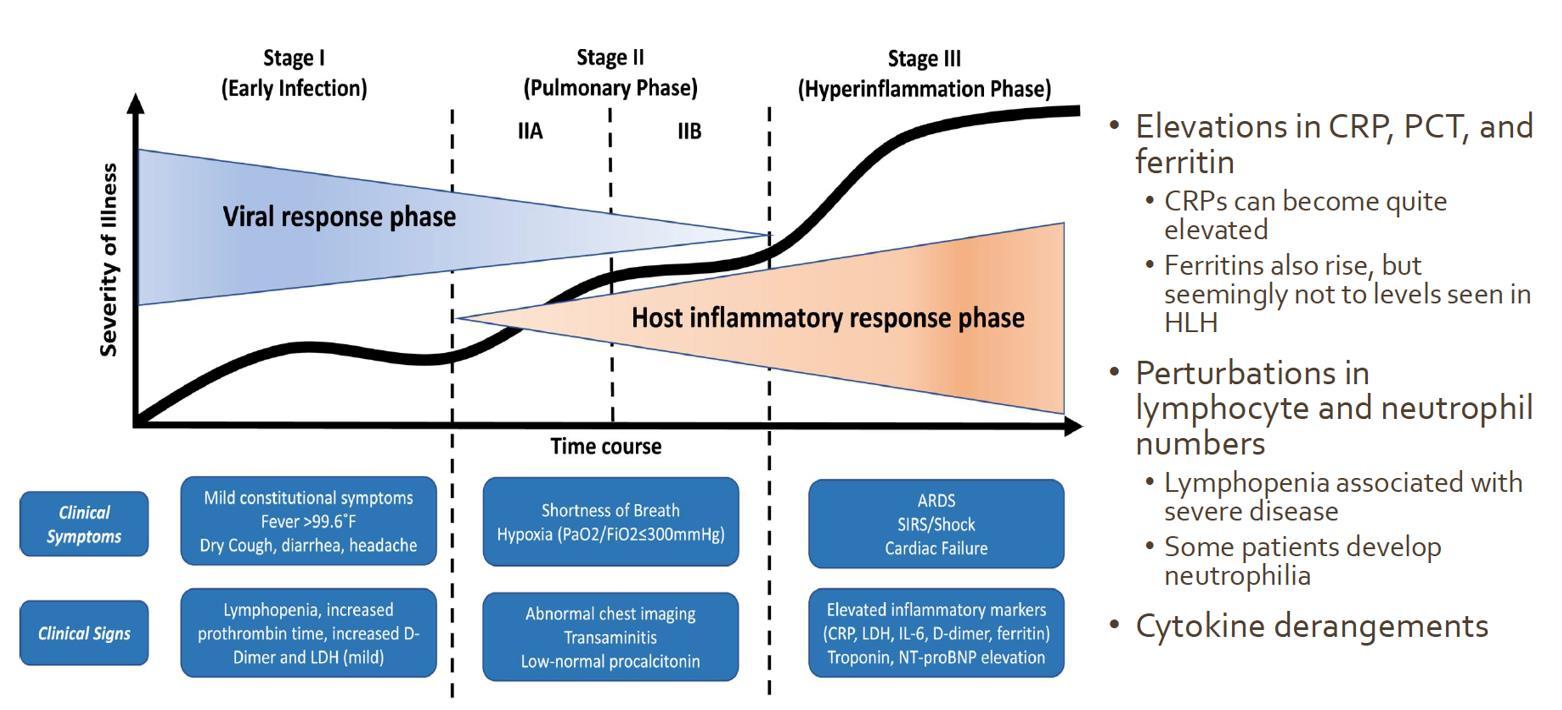
MIS-C (Multisystem Inflammatory Syndrome in Children)
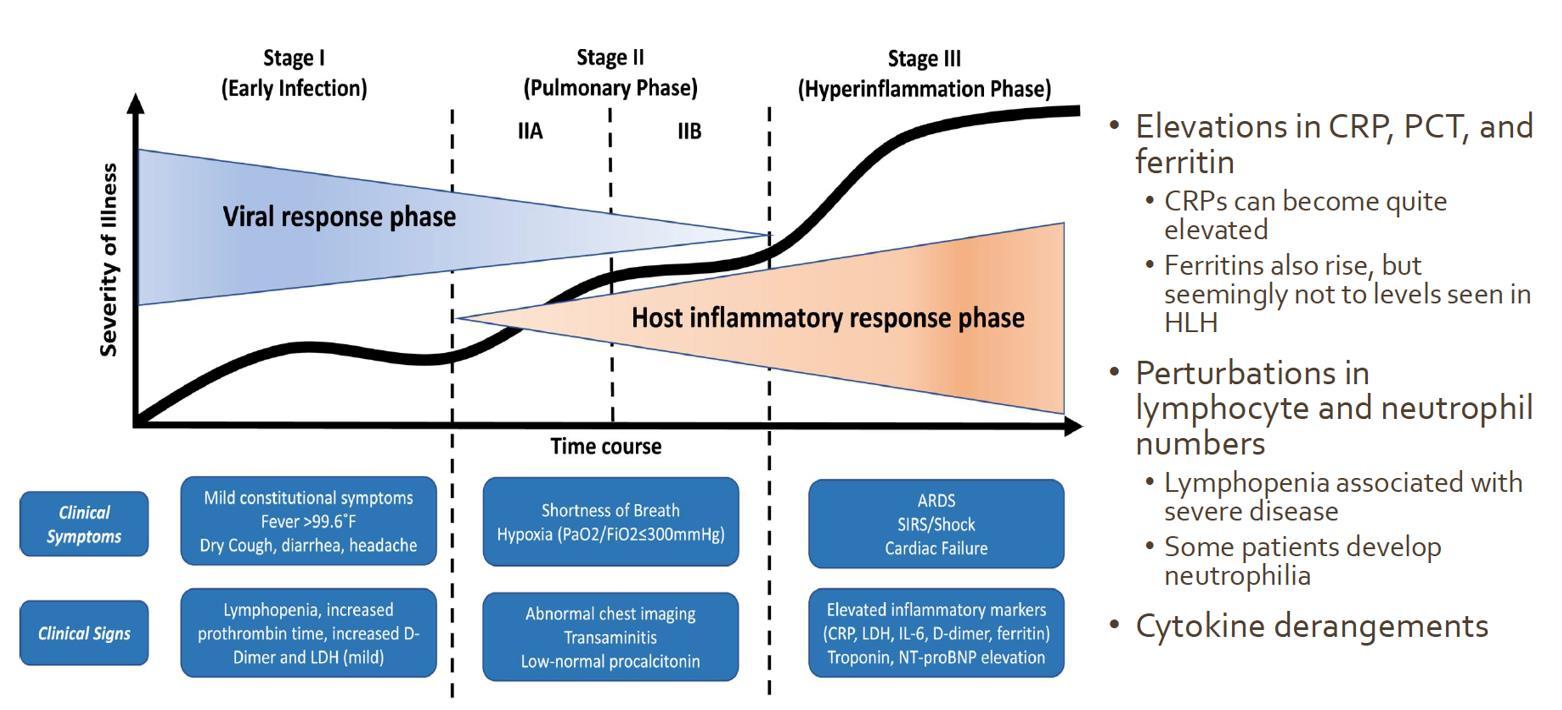


Kids also get a hyper-inflammatory syndrome (MIS-C versus MIS-A)


Epidemiologic and clinical characteristics of pediatric SARS-CoV2 infection 11
MIS-C (Multisystem Inflammatory Syndrome in Children)


Signs and Symptoms
- Unremitting fever
- Epidemiologic link to SARS-CoV-2(*)

- >/=2 of the following symptoms:
Rash
GI symptoms
Peripheral edema
Mucosal changes
Conjunctivitis
Lymphadenopathy
Neurologic symptoms
NB: not necessarily positive swab
CRP > 5mg/dl
Lymphopenia (<1.000)


Thrombocytopenia (<150.000/mcL)
Neutrophilia
Epidemiologic and clinical characteristics of pediatric SARS-CoV2 infection 12
↑ Ferritin ↑ BNP/TPN, ↑ D-Dimers, ↑ LDH, ↑ triglycerides, ECG alterations
Positive
↓ Sodium ↓ Albumin
+/-
serology

MIS-C (Multisystem Inflammatory Syndrome in Children)

0-19 years (0-21 years)
fever >3days (>24 hrs)
Involvement of multiple systems (more systems)

lab Inflammatory markers (defined)
Other microbiologic causes excluded
Evidence of SARS-CoV-2 infection (current or recent)

Epidemiologic and clinical characteristics of pediatric SARS-CoV2 infection 13
MIS-C (Multisystem Inflammatory Syndrome in Children)
Kids also get a hyper-inflammatory syndrome (MIS-C versus MIS-A)


Pulmonary involvement is MILD in children

Some degree of cardiac and/or intestinal involvement is almost always present

Lab markers which correlate with the disease and severity (lymphopenia, ↑ CRP, ↓ albumin, ↑ D-dimer, ↑ Troponin and BNP)
Important to quickly recognize the “cytokine storm” for a prompt diagnosis
Treatment is most effective when started early

Epidemiologic and clinical characteristics of pediatric SARS-CoV2 infection 14
MIS-C (Multisystem Inflammatory Syndrome in Children)

Treatment - 1

IVIG: 2 g/kg in 12 h (or slower/divided doses if pump failure or electrolyte issues)
Methylprednisolone: 2mg/kg/day
In 2 divided doses OR

Methylprednisolone: 30 mg/kg (Max 1g) QD for 1-


3 days, then Methylprednisolone/Prednisone OR
If CNS involvement, consider Dexamethasone (10mg/m2/die)
IF PERSISTENCE, THEN CONSIDER
Anakinra ev: 2 mg/kg (max 100 mg) Q.I.D. or continuous IV (12 mg/kg die) (max 400mg/day)

Epidemiologic and clinical characteristics of pediatric SARS-CoV2 infection 15
+
MIS-C (Multisystem Inflammatory Syndrome in Children)



Treatment - 2

+ supportive treatment
• Anticoagulation (prophylactic dosage)
• IV hydration / NPO

• Inotropes as needed
• Albumin / Furosemide as needed

• Electrolyte and fluid homeostasis
• (Antibiotics only if suspect superinfection)
Epidemiologic and clinical characteristics of pediatric SARS-CoV2 infection 16
MIS-C (Multisystem Inflammatory Syndrome in Children)
Outcomes

45 children admitted for MIS-C, followed up for 4-9 months
76% required intensive care / 64% required vasopressors and/or inotropes.

80% had some form of echocardiographic abnormalities (44% moderate-severe)
FOLLOW UP:
By 1 to 4 weeks most inflammatory markers normalized, 32% persistent lymphocytosis
By 1 to 4 weeks, only 18% had mild echocardiographic findings; all had normal coronaries.

At 4 to 9 months, only 1 child had persistent mild dysfunction.
The majority of children with MIS-C present critically ill, but most inflammatory and cardiac manifestations go on to resolve within a few months.

17 Titolo Presentazione
MIS-C (Multisystem Inflammatory Syndrome in Children)

Why not so common in Asia?
Different prevalence rates and different case fatality rates in different geographical areas
Different ethnic or genetic background (HLA subtypes?)

In New York Compared with White children:
higher incidence of MIS-C among Black (IRR, 3.2; 95% CI, 2.04.9) and Hispanic (IRR, 1.7; 95% CI, 1.1-2.7) children

no difference among Asian or Pacific Islander children (IRR, 0.9; 95% CI, 0.4-1.7)
Also higher rate of admission for COVID
Different SARS-CoV-2 subtypes

Epidemiologic and clinical characteristics of pediatric SARS-CoV2 infection 18
MIS-C (Multisystem Inflammatory Syndrome in Children)




Epidemiologic and clinical characteristics of pediatric SARS-CoV2 infection 19
PERIOD TOT PTS ADMITT ED MEAN AGE MEDIA N AGE M/F MEA NLEN GTH OF STAY MEDIAN LENGTH OF STAY NEGATIVE ON D/C (N, %) COMPLICATIONS TOT PZ GI NEUTR OPENI PULM MIS-C MYOPERICARD 01/0331/05 53/56 7.56 7.02 31/22 10.2 7 31 (55.4%) 15 2 4 5 3 2 01/0631/08 40/42 4.91 2.22 17/23 6.7 4 11 (26.2%) 8 1 6 3 1 0 01/0931/10 110/116 4.78 1.38 66/44 5.6 4 23 (19.8%) 50 1 27 5 1 10 01/1130/11 58/61 5.47 1.53 35/23 5.02 4 9 (14.7%) 26 5 14 4 1 3 01/1231/12 48/56 6 5 26/22 6.2 4 25 (44.6%) 22 7 8 4 4 5 01/0131/01 57/63 7.95 8.36 26/31 6.1 4 19 (34.5%) 27 4 10 3 6 6 01/0228/02 35/49 6.33 4.55 14/21 5.74 4 11 (31.4%) 15 3 3 3 4 3 01/0331/03 64/72 8,09 8,07 34/30 5,55 3,5 15 (23,4%) 26 6 5 9 (3) 2 1 01/0430/04 61/71 6,04 3,53 30/31 3,5 3 19 (32,2%) 26 5 6 6 (1) 6 6 01/0531/05 33/37 5,59 3,59 16/17 3,94 3 16 (48,5%) 9 4 1 3 (1) 1 1 01/0630/06 19/26 6,6 3,25 10/9 6,05 6 7 (36,8%) 9 2 3 2 (0) 0 0 01/0731/07 33/40 6,66 3,91 18/15 5 3 14 (42,4%) 10 4 3 4 (0) 0 0 01/0831/08 48/58 5,6 2,58 30/18 4,04 3 11 (22,9%) 21 4 10 7 (1) 0 0 01/0918/09 19/24 6,75 4,41 3,47 3 4 (23,5%) 10 0 2 3 (0) 0 0
MIS-C (Multisystem Inflammatory Syndrome in Children)

Why not so common in Asia?
- Different prevalence rates and different case fatality rates in different geographical areas
- Different ethnic or genetic background (HLA subtypes?)

- Compared with White children

- higher incidence of MIS-C among Black (IRR, 3.2; 95% CI, 2.0-4.9) and Hispanic (IRR, 1.7; 95% CI, 1.1-2.7) children

- no difference among Asian or Pacific Islander children (IRR, 0.9; 95% CI, 0.4-1.7)
- Also higher rate of admission for COVID
- Different SARS-CoV-2 subtypes
Epidemiologic and clinical characteristics of pediatric SARS-CoV2 infection 20
Long-COVID IN CHILDREN


1355 children in schools in Switzerland
SCV2 seroprevalence + questionnaire
- 3% fatigue

- 2% difficulty concentrating
- 2% increased sleep
Overall 4% of the serology positive children had some symptoms above background rate lasting > 12 weeks (3 months)
*** 1 in 25 kids ***
11-17 year olds Cohort study of 3.000 positive kids and age/sex/geography matched controls
questionnaire
At 3 months post positive test 30% of kids had 3+ symptoms (versus 16% in controls)
Preprint ResSquare Sept 2021--- Stephenson

T, et al. Long COVID – the physical and mental health of children and nonhospitalised young people 3 months after SARS-CoV-2 infection; a national matched cohort study (The CLoCk study).
and clinical characteristics of pediatric SARS-CoV2 infection
Epidemiologic
21
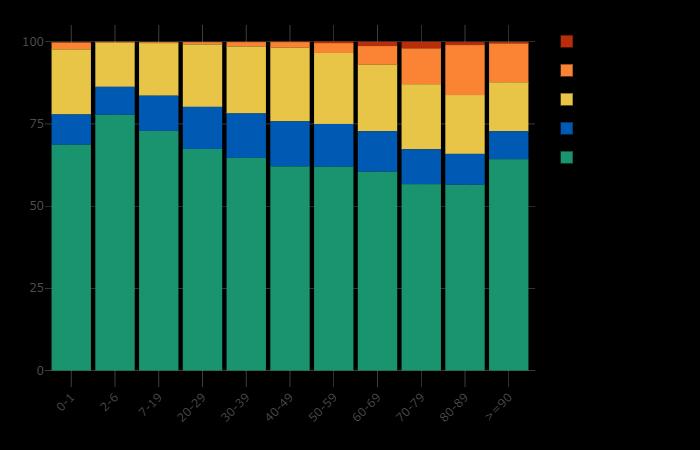
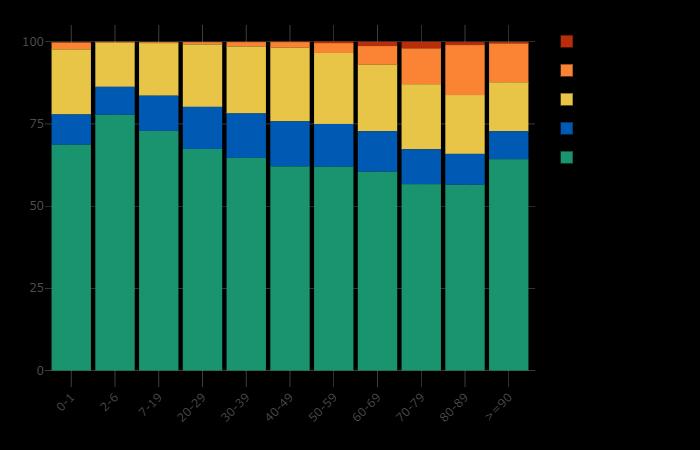
COVID-19 MORTALITY N CHILDREN

Mortality (45 states, NYC, PR and GU reported)*


Among states reporting, children were 0.00%-0.25% of all COVID-19 deaths, and 7 states reported zero child deaths
In states reporting, 0.00%-0.03% of all child COVID-19 cases resulted in death

Children and COVID-19: State-Level Data Report (Sept 2021)

Epidemiologic and clinical characteristics of pediatric SARS-CoV2 infection 22
THE SITUATION IN ITALY
(Source: EPICENTRO.ISS.IT The Italian Health Institute Epidemiology Center)



Epidemiologic and clinical characteristics of pediatric SARS-CoV2 infection 23
EPIDEMIOLOGY IN KIDS V. ADULTS
Why do kids get less sick than adults?
What is the mechanism?
Does infection determine persistent immunity in children? More so or less so than in adults?
Various hypotheses

Different amount of expression of the 2 receptors (ACE and renin-angiotensin) in the upper airways (primary site of infection)
Lower levels of IL-6, IL-10, myeloperoxidase, and P-selectine






Possible protective role of pulmonary resident lymphocytes which interact between respiratory system and immune system
Two studies found high titers of RSV- and mycoplasma IgG which might offer cross-protection towards SARS-CoV-2
Possible cross-protection by routine childhood vaccines
Why COVID-19 is less frequent and severe in children: a narrative review; Reza Sinaei, Sara Pezeshki, Saeedeh Parvaresh, Roya Sinaei; Received: 19 May 2020 / Accepted: 8 September 2020 © Children’s Hospital, Zhejiang University School of Medicine 2020 World Journal of Pediatrics

characteristics of pediatric SARS-CoV2 infection

Epidemiologic
clinical
24
and
EPIDEMIOLOGY IN KIDS V. ADULTS
OPBG PALIDORO
(16 march 2020 – 18 sept 2021)


• Total confirmed admitted cases 678


• M/F = 1.18/1
• Total 771 admission
• Mean age 6,3 years (median 3,7)
• Contacts: 530 (78,2%) history of contact with at least one known positive or suspected case (78,2%)
• Deaths in family or contacts: 14 (13 cases)
Epidemiologic and clinical characteristics of pediatric SARS-CoV2 infection 25
EPIDEMOLOGY TRANSMISSION

Attack rate of covid19 among close contacts
- Population based cohort study of contact tracing
- 730 index patients jan – july 2020


- 8852 close contacts

- Timeline
Highest risk is 2 days prior and 3 days after onset of symptoms
Mild/Mod symptomatic index case: 4.3 RR of infection compared to asymptomatic index case
Epidemiologic and clinical characteristics of pediatric SARS-CoV2 infection 26
EPIDEMIOLOGY TRANSMISSION IN CHILDREN

Children play a large role in community transmission of multiple infectious pathogens. Interacting with children: inherent exposure to and risk of infectious diseases (parents, grandparents, daycare workers, teachers).,

Household transmission dynamics: only 3.8% had a pediatric index case

Secondary infection rates of pediatric household contacts lower than adult
Transmission in schools typically follows trends in community transmission, rather than preceding or augmenting them

Increased risk of COVID-19 in kids attending school in person is lessened by layered prevention measures
Epidemiologic and clinical characteristics of pediatric SARS-CoV2 infection 27
EPIDEMIOLOGY TRANSMISSION IN CHILDREN

TRANSMISSION DEPENDS ON
Do kids infect adults or do adults infect kids?
Are kids a reservoir for infection now that adults are vaccinated?
Exposure (duration, location, timing)
Virus type/variant


Donor Symptoms (type, severity, duration)
Donor Viral load
Donor Host factors (susceptibility and immune responses / vaccination status)
Receiver Host factors
What will happen with schools reopening ?
KIDS vs ADULTS
more often asymptomatic,
fewer symptoms, shorter duration

Less symptomatic likely lower viral load
Epidemiologic and clinical characteristics of pediatric SARS-CoV2 infection 28
EPIDEMIOLOGY TRANSMISSION in



kids household contact
Cohort study of Children and transmission


6280 households with a pediatric index case
27.3% experienced secondary transmission
Frequency of transmission was age-dependent
Age 0-3 -- (OR 1.43) versus reference 14-17 year-olds
Age 4-8 (OR 1.4)


Age 9-13 (OR 1.15)
Younger children = higher odds of transmission
Epidemiologic and clinical characteristics of pediatric SARS-CoV2 infection 29
EPIDEMIOLOGY TRANSMISSION

Can we open schools safely?
Yes we can!
Maximize vaccination levels among the adults in the school and parents particularly those in contact with young children


Keep community transmission under control

Layered prevention measures within the school and public transport
Vaccinate children when possible
Epidemiologic and clinical characteristics of pediatric SARS-CoV2 infection 30