The project is being implemented with the support of UNICEF Ukraine and with financial support from the Government of Norway.
Implemented by: Partner:





The project is being implemented with the support of UNICEF Ukraine and with financial support from the Government of Norway.
Implemented by: Partner:





Dott.ssa Sarah Bompard
Dott.ssa Alessandra Lacopo
Sarah.bompard@opbg.net
Alessandra.lacopo@opbg.net
Unit of Neurorehabilitation, Bambino Ges˘ Children’s Hospital
Cerebral palsy is a group of permanent disorders affecting the development of movement and posture, causing activity limitations, attributed to non-progressive disturbances occurring in the developing fetal or infant brain. (Bax,1964)




Paul S et al. A Review on Recent Advances of Cerebral Palsy. Oxidative Medicine and Cellular Longevity 2022 Jul

AND POSSIBLE!!!
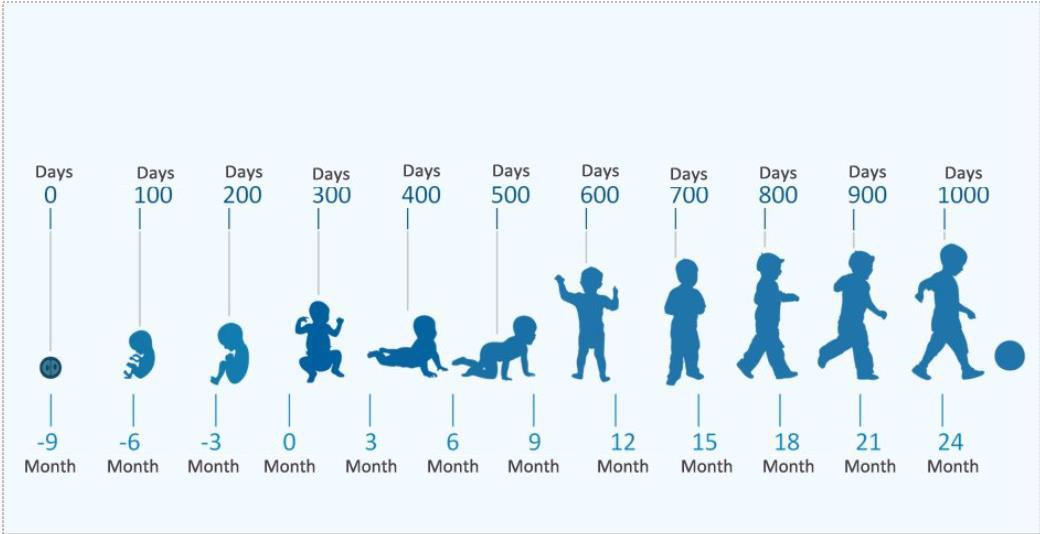

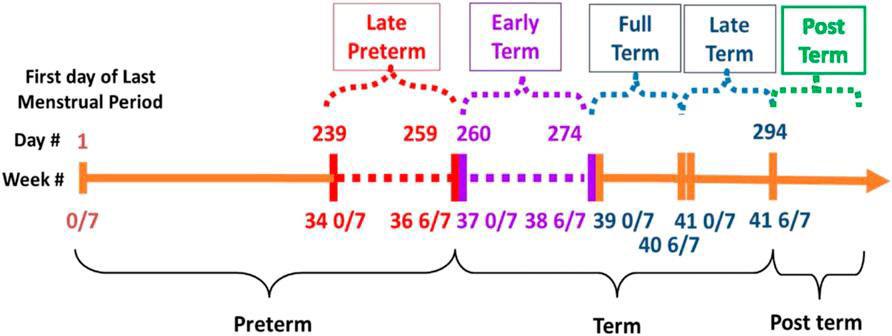
Upto24months,the milestonesof psychomotor developmentshould beassessed consideringthe correctedage (chronologicalage minustheperiodof prematurity).

Pretermbirthisoneof themostsignificant riskfactorsforthe developmentof cerebralpalsy.
Inthefirstmonths,itisessentialtopromptlyidentifymajordisabilities.
- ModeratetosevereCerebralPalsy(CP)withGrossMotorFunction ClassificationSystem(GMFCS)≥2. - Cognitivescorebelow70ontheBayleyScaleseGMFCS≥2 - Bilateralvisionimpairmentwithvisualacuitylessthan1/10
- Hearingimpairmentlimitingcommunicationdespitehearingaidsor cochlearimplant
Preconceptional Risk Factors:
•Previousspontaneousabortions
•Medicallyassistedreproduction
•Lowsocioeconomicstatus
•Parentscarryingchromosomal abnormalities

Surveillance of Cerebral Palsy Europe and Australian Cerebral Palsy Register inclusion criteria
Risk Factors During Pregnancy:
•Genetic defects
•Complications during delivery
•Multiple pregnancy (twinning)
•Male sex
•Maternal thyroid dysfunction
•Pre-eclampsia
•Infections
•Intrauterine growth restriction (IUGR)
•Prematurity
•Substance abuse

Perinatal Risk Factors:
•Acute intrapartum hypoxia
•Seizures
•Hypoglycemia
•Infections

Surveillance of Cerebral Palsy Europe and Australian Cerebral Palsy Register inclusion criteria
Postnatal Risk Factors:
•Stroke
•Neurological damage
•Infections

Surveillance of Cerebral Palsy Europe and Australian Cerebral Palsy Register inclusion criteria


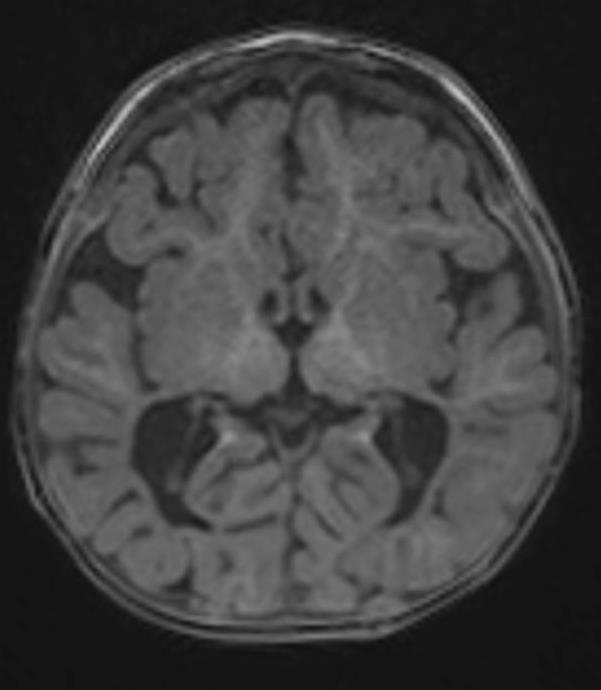
Before 5 months of corrected age:
Abnormal brain MRI, absent fidgety movements on General Movements
Assessment (GMA), and an abnormal Hammersmith Infant Neurological Examination (HINE) demonstrate a sensitivity of 97.86% and specificity of 99.22% for diagnosing CP.
After 5 months of corrected age:
Abnormal brain MRI and a Hammersmith
Infant Neurological Examination (HINE) score below 73 predict CP in 90% of cases.

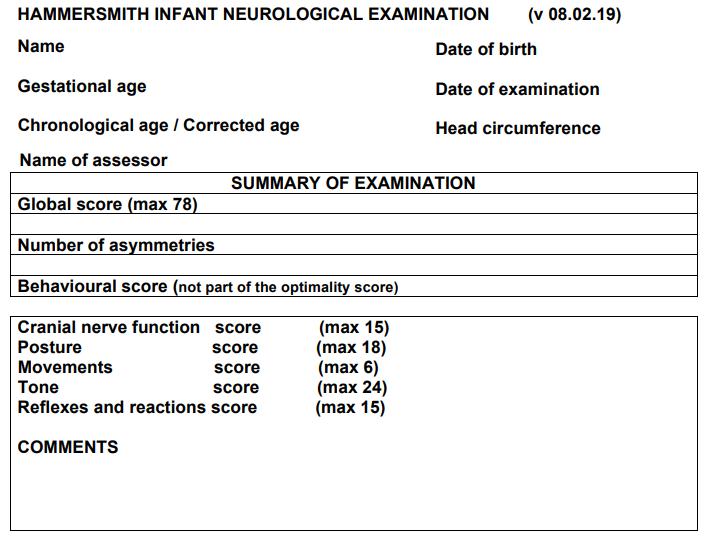
HINEisastandardized neurologicalassessment tooldesignedtoevaluate motorandneurological functionininfantsaged2to 24months.Itassesses cranialnervefunction, posture,movements,tone, andreflexes,providinga scorethathelpsinearly detectionofneurological impairments,including cerebralpalsy.
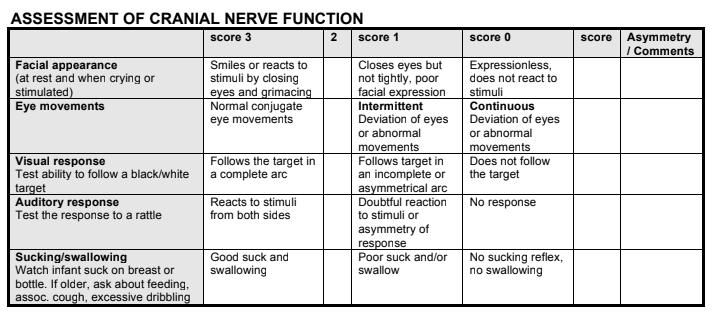
Abnormal movementsof theeyes
Doubtfulreaction tostimuli
Followstargetin anincomplete arc
Noswallowing, enteralfeeding
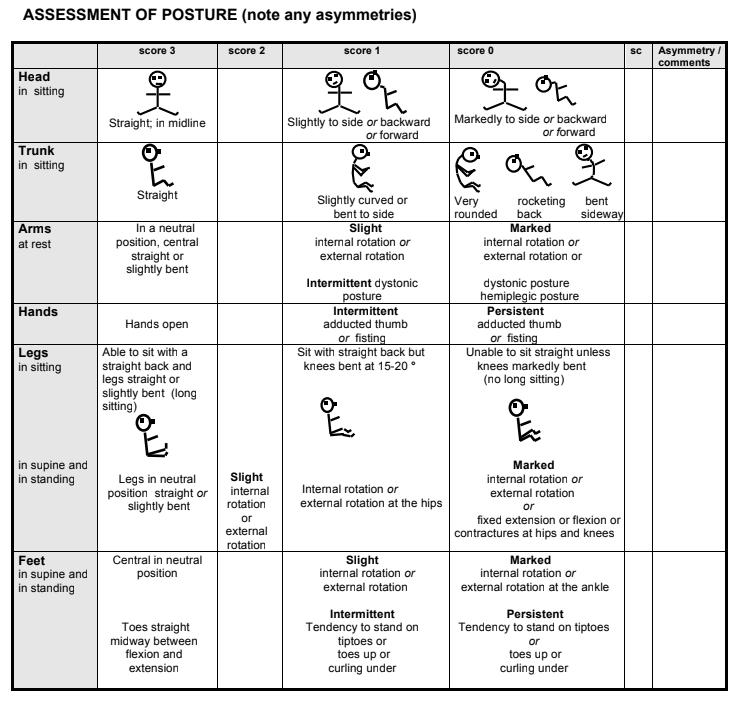
Handswith persistent adductedthumb
Trunkinsitting veryrounded
Feetwith tendencyto standontiptoes

Minimal Tremulous Distonicposture
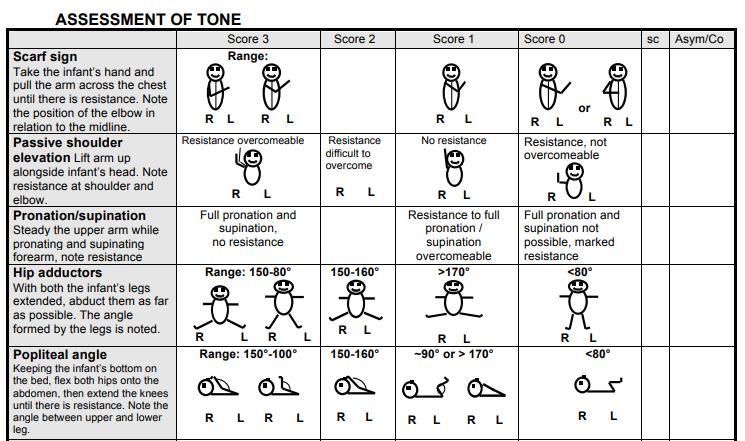
Increasedmuscle tonethatlimited alltherangeof movements
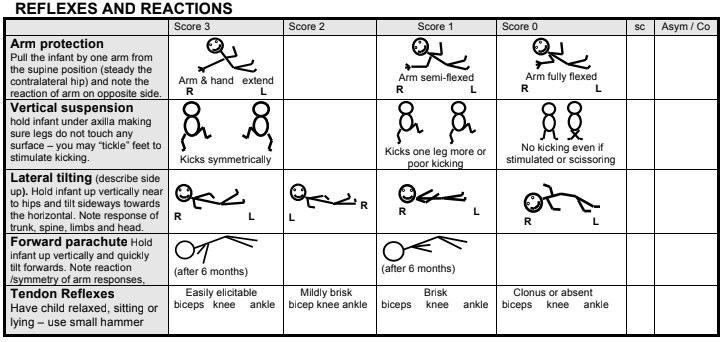
Armprotectionabsent
Tendonreflexbrisk

Refer to spontaneous, complex, and variable movements involving the whole body, observed in fetuses and young infants. These movements are characterized by their fluency, variability, and complexity and are an important indicator of the integrity of the developing nervous system.
Writhing Movements: frompretermageuntilabout 6–9weekspost-term.
Fidgety Movements: 9weekspost-termuntil20 weekspost-term
-poorrepertoire:monotonous movements
-crampedsynchronized:infant’s limbsandtrunkmusclescontract andrelaxalmostsimultaneously, producingstiffandrigidmovements withalackofsmoothness
-chaotic:movementsarelarge, abrupt,andlacksmooth coordination.
-abnormal
-absent
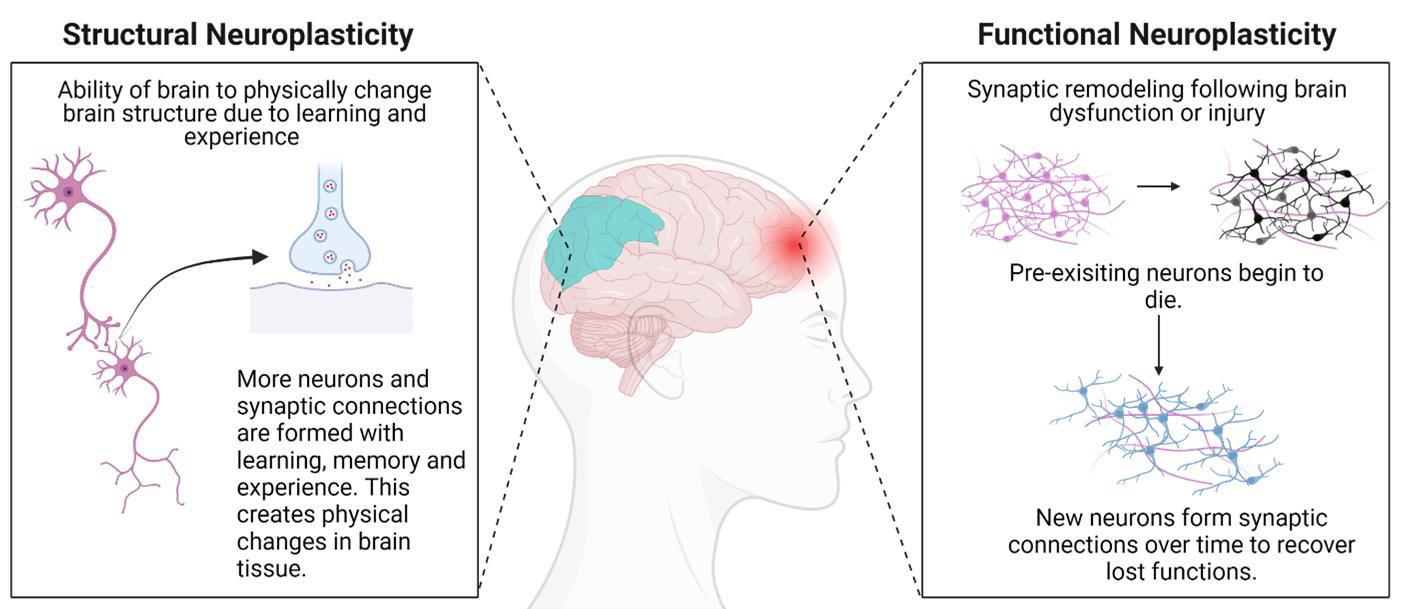
"is the brain's ability to reorganize and form new neural connections in response to learning, experience, or injury. It allows the brain to adapt, recover from damage, and optimize function.".



Earlyrehabilitationprevents secondarycomplications:
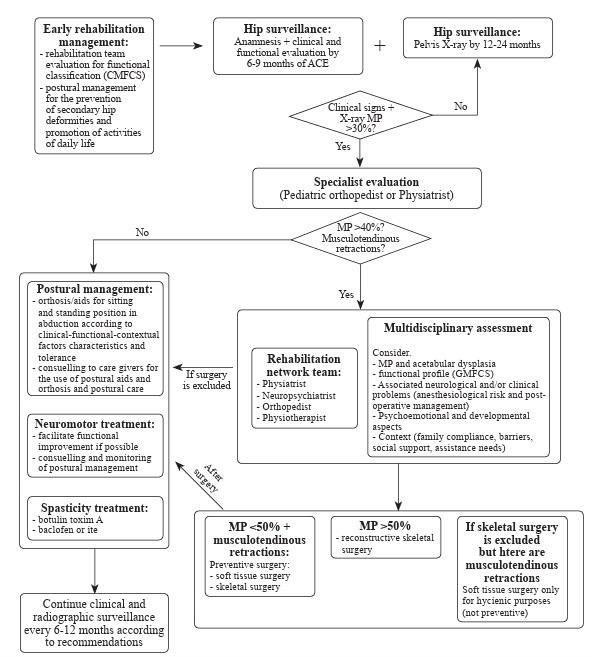
Hipdislocation
Jointcontractures
Scoliosis









•High Prevalence & Risk Factors
Scoliosisoccursin20–25%ofCPpatients;riskincreaseswithseverity ofmotorimpairmentandreducedambulation.
•Functional Impact
Trunkimbalanceandpelvicobliquityaffectsitting,standing,and walking;severecurvescancauserespiratoryandskincomplications.
•Curve Progression Patterns
Curvesworsenrapidlyduringadolescenceandcontinuepost-skeletal maturityif>50 ,especiallyinnon-ambulatorypatients.
•Curve Types
Group1:ambulatory,idiopathic-likecurves.
Group2:non-ambulatory,longcollapsingcurveswithpelvicobliquity.
•Conservative Management
Includesseatingadaptationsandspinalbracestoimprovepostureand delaysurgery,thoughtheydon’thaltprogression.
•Surgical Indications & Outcomes
Indicatedforcurves>45–50 ,rapidprogression,orfunctionaldecline.
Goal:stable,balancedspinetoenhancequalityoflife.

•Spasticity and dystonia often coexist inCPbutrequiredistinct treatment approaches; spasticity may respond to baclofen, while dystoniamayneeddeepbrainstimulation.
•Children with CP have shorter, weaker muscles with reduced fibre diameter, contributing to decreased strength and motor function.
•Physiotherapy should be goal-oriented and engaging, focusing on task-specific training and individualized strengthening,ratherthanpassiveorgeneralizedapproaches.
•Contractures develop progressively as muscles fail to keep pacewithbonegrowth;earlydynamiccontracturesmayrespond tocastingorBoNT-A,butfixedonesmayrequiresurgery.
•Preventive strategies like orthoses, bracing, and positioning arecommonlyused,thoughevidenceislimited;long-termfollowupandgaitanalysisareessentialforoptimizingoutcomes.














•Head–trunk–pelvis axis alignment
•Pelvic positioning and stability
•Lower limb positioning
•Upper limb freedom to support tabletop activities
•Proper posture during feeding

Greater pelvic containment with abducted sitting and asymmetry
Possibility of tilt-in-space and lumbar support
Reclining backrest with lateral supports
Straps with customized fastenings
Headrest integration
Height-adjustable footrest
High customization options for headrest selection

Greater pelvic containment
Reclining backrest with curved supports (pelottes)
Custom belts with specialized fasteners
Adjustable headrest
Elevating footplate
Rigid shell for support and tilt function
More stability and comfort than semi-postural and commercial strollers

•A multiposition system that allows continuous transition from supine to prone position without any adjustment or change in configuration.




Standing frames support upright posture and promote weight-bearing in children with cerebral palsy.
Some models include adjustable hip abduction to accommodate hip subluxation.
Optional trays enable children to participate in play and therapeutic activities while standing.






•Provide postural support and promote upright mobility.
•Encourage independent movement and improve gait patterns.
•Can be anterior or posterior based on child’s needs and control.
•Aid in functional mobility, participation, and physical development.




• Orthosis made of elastic material
• Support and stabilization of the trunk and proximal segments in all three planes of space
• Freedom of movement for the limbs

ELASTO-COMPRESSIVE SUIT


• Properly designed and customized orthoses can realign and stabilize the body.
• They help correct or limit the worsening of mild dysmorphisms and paramorphisms.
• Their effectiveness relies on dynamic elastic actions of deflection and detorsion.

•Mainly made of elastic material
•Wrist and finger extension
•Wrist stabilization
•Thumb opposition/abduction
•Forearm supination/pronation
•Elbow extension/flexion
•Shoulder elevation/external rotation
•Stabilization of the scapulohumeral girdle





Carbon Orthosis


•Supports the ankle and foot, enhancing gait and preventing deformities
•Hybrid carbon orthosis: Lightweight, energyefficient, and preferred by children with cerebral palsy for improved gait and mobility
There is no evidence supporting a change in the Gross Motor Function Classification System (GMFCS)level,BUTearlyinterventionallowsto:
Developfunctionalskills(e.g.,CIMT,containmentofmaladaptivepostures,AAC)
Preventsecondarydeformities
Improvequalityoflife.
Patients with cerebral palsy (CP) who receive Goals-Activity-Motor Enrichment (GAME), an early and intensive motor intervention combined with parent education and environmental enrichment, demonstrate better motor and cognitive abilities at 1 year compared to those receivingusualcare.

InfantswithhemiparesiswhoreceiveearlyConstraint-InducedMovement
Therapy(CIMT)showintheshorttermimprovedhandfunctioncompared tocontrols.

Earlyinterventionoptimizesthemotorandcognitiveplasticityof theinfant,preventssecondarycomplications,andimproves caregiverwell-being.

Regular follow-up, including pelvic Xrays from an early age, and early rehabilitative treatment are essential to prevent hip dislocation in children withseverecerebralpalsy.



Adapted Physical Activity leads to an improvement in PHYSICAL and MENTAL FUNCTIONING.
• Improvement in pain
Rehabilitation + Adapted Physical Activity:
Improvement in physical functioning
• Improvement in motivation
• Improvement in self-sufficiency
• BENEFITS OF PARTICIPATING IN APA
Increased well-being
Greater integration into the community
Improved muscle strength
Enhanced fundamental movement skills
• BARRIERS TO APA PARTICIPATION
Misconception: No programs available for this population
Misconception: Participation is unsafe or too risky
Misconception: Sports rules are too difficult to learn or cannot be adapted to include children with disabilities (CWD)
• FACILITATORS TO APA PARTICIPATION
Preliminary assessments to maximize safety with appropriate settings
Organizing sports focused on fun rather than competition
Healthcare professionals, PE teachers, and coaches who prescribe/suggest physical activity practices while recognizing individual needs
Adaptations such as longer rest periods, closer coach-to-athlete ratios, frequent positive feedback, and careful monitoring of fatigue or injury symptoms





Il presente documento Ë stato elaborato da Ospedale Pediatrico Bambino Ges˘.
I contenuti sono strettamente riservati; Ë vietata la riproduzione e la divulgazione, anche solo parziale, senza il benestare scritto di Ospedale Pediatrico Bambino Ges˘.