

STRENGTH IN NUMBERS


WE BELIEVE
a healthy team makes a healthier Arkansas.
Scott Provencher
Scott Provencher is a healthcare lawyer who assists clients in matters related to compliance with HIPAA and HITECH, the Physician Self-Referral (Stark) Law, Anti-Kickback and EKRA Statutes, and EMTALA. He also counsels hospitals, physicians, pharmacists and other healthcare providers regarding contracts, proceedings before state licensing boards, and issues related to credentialing and peer review.
Jennifer L. Smith, JD, RN, CEN
Jennifer rejoins WLJ after working in house at the state’s only academic health sciences university, and she previously practiced as a registered nurse. With 18 years of health law experience, Jennifer provides a wealth of knowledge to guide clients through regulatory, administrative and compliance concerns.
STRENGTH IN NUMBERS

ARKANSAS HOSPITALS
Arkansas
Natural Resources Drive | Little Rock, AR 72205
To advertise, please contact Brooke Wallace magazine@arkhospitals.org
Becca Bona, Editor in Chief
Katie Hassell, Graphic Designer
Roland R. Gladden, Advertising Traffic Manager
BOARD OF DIRECTORS
Larry Shackelford, Fayetteville / Chairman
Greg Crain, Little Rock / Chairman-Elect
Michelle Krause, MD, Little Rock / Treasurer
Ron Peterson, Mountain Home / Past-Chairman
Ryan Gehrig, Fort Smith
Crystal Bohannan, Hot Summers
Connie Castleberry, Camden
Sammie Cribbs Roberson, Harrison
David Deaton, Clinton
Phil Gilmore, Crossett
Michael Givens, Jonesboro
Tommy Hobbs, Clarksville
Charlotte Jackson, Searcy
Eric Pianalto, Rogers
Brian Thomas, Pine Bluff
Matt Troup, Conway
Cody Walker, North Little Rock
EXECUTIVE TEAM

Robert “Bo” Ryall / President and CEO
Jodiane Tritt / Executive Vice President
Tina Creel / President of AHA Services, Inc.
Pam Brown / Vice President of Quality and Patient Safety
Lyndsey Dumas / Vice President of Education
Debbie Love / CFO

Last Training: August 11–22 in Springdale, AR
FREE hybrid training | $500 monthly stipend
FREE lodging for in-person classes


This FREE 1-year program is for individuals who are employed full-time with 3 years or less of experience in the field and includes:
•$500 monthly stipend
•160 hours of training
•7 college credit hours
•Mentorship + career support
•Lodging for out-of-town participants
Spots are limited. Apply today!

Strength in Action
Ongoing legislative discussions and policy proposals in the federal arena are transforming the health care landscape. Hospitals across the state continue to demonstrate remarkable resilience, steadily adapting to serve their communities. At the Arkansas Hospital Association (AHA), we’re realistic about the challenges — notably, the financial pressures hospitals face, especially with proposals for substantial cuts to Medicaid and the potential for millions to lose coverage. This reality prompts us to ask: How do hospitals continue to maintain, enhance, and provide essential services with less?
Financial strains, coupled with workforce shortages and complex regulatory environments, make the path forward feel daunting. Even so, it’s precisely in these times that the adage, “a rising tide lifts all boats,” comes to mind. The collective strength of Arkansas’s health care ecosystem has never been more vital. This year’s Hospital Statistics insert provides a valuable starting point for conversations with lawmakers, regulators, and other stakeholders, highlighting the financial viability of our hospitals and outlining the necessary steps to ensure care for all Arkansas patients. Data and insights from our dedicated analytics and policy team offer essential guidance, empowering hospitals to gain greater control over their operational future.
We continue to tell the Arkansas hospital story in our advocacy efforts.
With the closing of the recent 95th General Assembly legislative session, we celebrate wins: Medicaid expansion and momentum surrounding maternal health, to name a couple. We also continue to advocate in the national arena. We recently undertook a highly productive delegation to Washington, D.C., where we engaged with congressional members and their staff to underscore hospitals’ already-strained finances, particularly concerning proposed federal cuts to Medicaid. A key highlight was our impactful meetings on Capitol Hill with Senators John Boozman and Tom Cotton, as well as Representatives Steve Womack and French Hill, along with dedicated staff from Representatives Rick Crawford’s and Bruce Westerman’s office. These direct engagements with lawmakers are vital as we advocate for the needs of Arkansas hospitals and the health of their communities.

We remain committed to our member hospitals by leveraging their combined strength through tangible resources and collaborative platforms. We at the AHA provide a forum for so many within the health care sector, including our vital network of affiliated groups, offering an avenue to track regulatory changes, network with peers across the state, and access ongoing education. We also seek ways to provide new educational opportunities, including our recent Certification in Infection Control (CIC®) Prep Course. Through a federal grant, we were able to host this comprehensive course for 50 hospital Infection Preventionists (IPs) at no cost, increasing the number of certified IPs in Arkansas and enhancing the quality of health care across our state. Knowledge is power, but the strength found in peer-to-peer networks, mentorship, and connecting with others facing similar circumstances is invaluable.
In challenging times, the path forward isn’t always clear. Even so, by harnessing the collective power of shared knowledge, unified advocacy, and unwavering commitment to excellence, Arkansas hospitals can forge a path forward, together. The AHA is proud to support each of our member hospitals, providing connections, data, and resources that help make the health care network in Arkansas robust. Arkansas hospitals are not just adapting to change; they are actively shaping a stronger, healthier tomorrow for every Arkansan.

Bo Ryall President and CEO

HOSPITALIZATION
NOTIFICATION SERVICES


SHARE's Daily Hospitalization Reports are given directly to SHARE-connected providers and care teams, to assist with care coordination and patient follow-up.
Real-time notification of hospital visits (admissions, discharges, or ED transfers) for practices' active patients
Allows providers to proactively coordinate their patients' care and schedule any necessary follow-up treatments or visits
Assists in meeting value-based contract arrangements
All Together Now
This morning, I walked out onto my patio and plucked a perfectly poised cucumber from a wily vine. In a few weeks, it’ll probably be packed into a mason jar, seasoned and sealed, ready to share with my family, neighbors, and co-workers in pickle form. This time of year, I spend a lot of time in my garden, talking to my plants. Sometimes I even sing to them, depending on the day, either the Beatles or the Stones.
When I was younger, I spent a lot of time with my Dad in his garden. He showed me how to maintain the plot while explaining the science behind it in a fun, hands-on kind of way. Technically, my Dad can be classified as a plant pathologist (among other things), so he went into immense detail about photosynthesis, gene crossings, soil pH, and more. I remember my ten-year-old brain struggled to keep up with the knowledge he wielded upon me.
The most interesting thing about the photosynthesis part was learning about

how plants and humans create their own ecosystems. And then, more than 20 years later, the profound epiphany hit me on my own garden-oasis-patio: nothing exists in a vacuum. These thoughts come flooding over me on a bright, sunny June morning, while I’m holding a cup of coffee and a cucumber, with the news murmuring in the background.
In the face of potential Medicaid cuts and other fiscal pressures, I’m thinking about the delicate fabric needed to keep our hospitals and health care system thriving. Any action taken — whether it’s reducing funding or altering regulations — has a ripple effect that can cause a significant impact somewhere else down the line. It’s not a far cry from that human-plant symbiotic relationship — plants supply oxygen for human breathing, and in return, humans supply carbon dioxide for plant photosynthesis. Of course, it’s way oversimplified in this example, but imagine you’re ten years old with me, in the side yard asking Dad about banana peppers.
Similarly, hospitals are part of an intricate ecosystem that relies on so many moving parts. This concept of interconnectedness, of strength in numbers, was powerfully evident during the recent legislative session. Your voice mattered at the Capitol. In this issue, you’ll find a comprehensive legislative recap detailing the key wins, challenges, and ongoing efforts from the recent session. It’s a testament to what we can accomplish when we stand united at the state level, but remember,
the fight for favorable health care policy continues, requiring persistent advocacy at the federal level, as well.
In the meantime, as hospitals navigate complex financial landscapes, we continue to provide resources for all our members. Every hospital, regardless of size or location, contributes uniquely to the overall health and prosperity of Arkansas. You’ll also find our annual Hospital Statistics guide in this issue. The numbers don’t lie – hospitals across the state are a boon to the economy, creating jobs, driving innovation, and serving as a cornerstone for community well-being. It’s a powerful quantitative illustration of the immense, undeniable value hospitals bring to Arkansas, highlighting why their sustained health is crucial for everyone. We’re better when we’re connected. The AHA actively fosters this by collaborating with our affiliated groups to offer peer-to-peer networking and continuing education tailored to various hospital niches. The value of sharing insights, challenges, and best practices with colleagues who understand your unique struggles is immense. As we continue to come together, our foundation grows ever stronger. Ultimately, the success of Arkansas hospitals, much like the delicate balance observed in my garden, hinges on thorough understanding of these intricate, interconnected relationships. We are all integral parts of the same ecosystem, united by the common goal of ensuring every Arkansan has access to quality care.

Becca Bona Incoming Editor in Chief
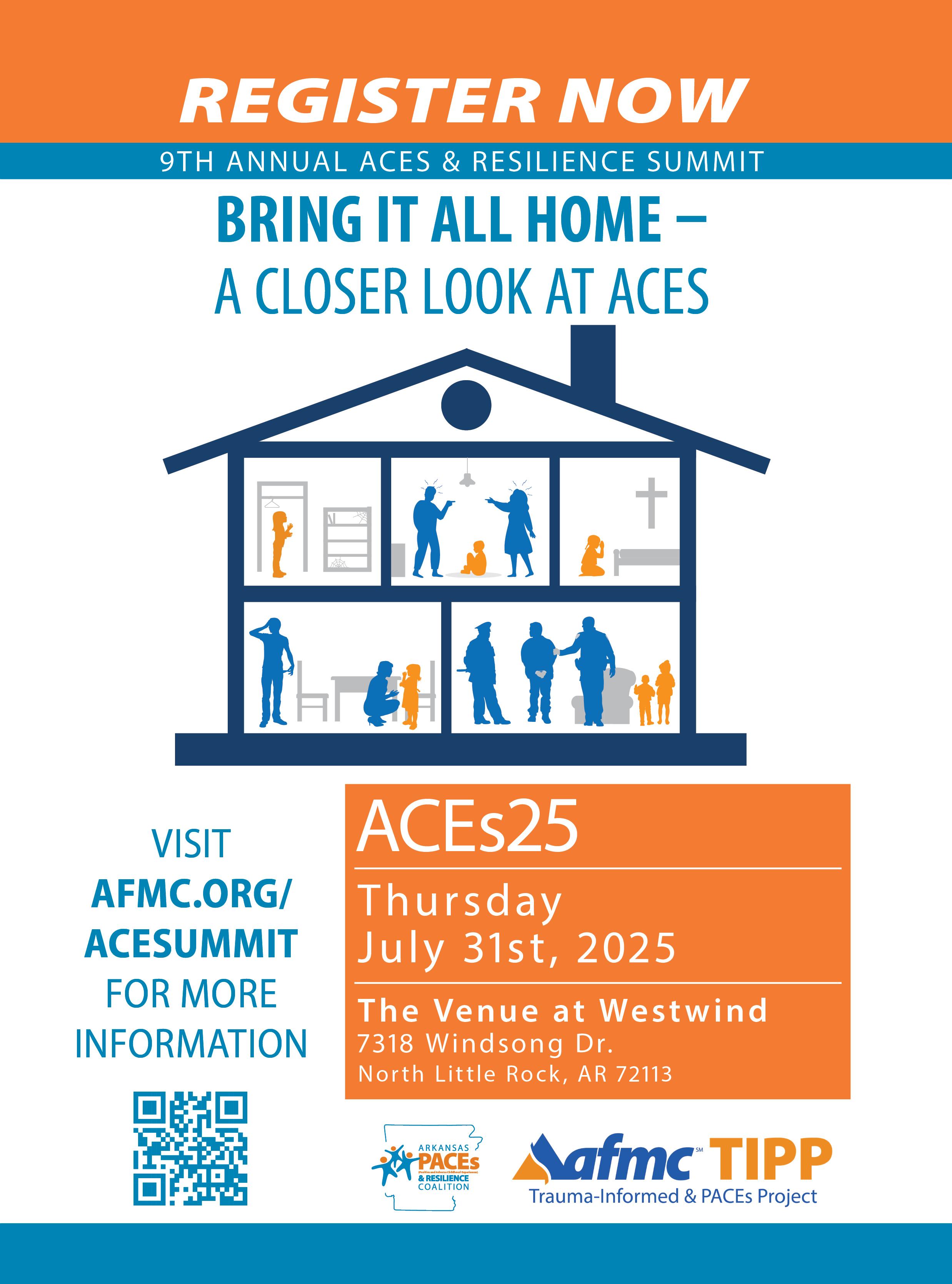
2025 Summer Calendar

JULY
July 16
Do No Harm: Advancing Health Care Sustainability Hosted by Vizient AHASI Webinar
July 31
Arkansas Society for Healthcare Marketing and Public Relations (ASHMPR) Summer Conference White River Health, Batesville
AUGUST
August 20-22
2025 Mid-South CAH & Rural Hospital Conference The Seelbach Hilton Louisville
SEPTEMBER
September 18-19
Arkansas Healthcare Human Resources Association (AHHRA) 2025 Fall Conference Wyndham Riverfront, North Little Rock
September 19
Arkansas Association for Healthcare Engineering (AAHE) Fall Conference Mercy Northwest, Rogers
Register for AHA Events Online!
Employees of AHA member hospitals can now log in to www.arkhospitals.org and register for events online.

Save the Date! OCTOBER 15-16
Arkansas Hospital Association 2025 Annual Meeting
UPDATED OPENING SPEAKER:
Command Sergeant Major Gretchen Evans
The Game-Changing Power of Your Rope Team
Little Rock Marriott
As one of the most highly decorated women in the U.S. Army, Gretchen Evans had finally achieved her dream. Overseeing 30,000 troops as a Command Sergeant Major, she was on top of the world. But all of that changed in an instant during a rocket attack in Afghanistan when she suffered catastrophic injuries and became deaf. Gretchen's presentation will take you on a journey from her finding her purpose in the military as a young woman, to her devastating injury, to her decision to reclaim her life with the support of her Rope Team. With her Rope Team of friends, supporters, and service dogs by her side, Gretchen not only re-discovered the will to live, but she dedicated her life to serving others by founding Team UNBROKEN, a mixed-ability athletic team. Between her stories, Gretchen will offer her wisdom on the topics of grit, hope, and overcoming any barrier. With a heartfelt message and a touch of humor, Gretchen provides a keynote that inspires all of us to believe 'what's within us is stronger than anything in our way'.
CLOSING SPEAKER: RaDonda Vaught
This closing keynote will feature RaDonda Vaught, whose case made headlines in March 2022 when a jury found her guilty of criminally negligent homicide and gross neglect of an impaired adult in the death of a patient to whom she accidentally gave the wrong medication. Her presentation will be followed by a reaction panel focused on how we, as leaders, can cultivate a culture of safety in our hospitals.
The Annual Meeting will kick off with the Leadership Workshop on Wednesday and feature hot topics focused on leadership and patient safety on Thursday morning.
Stay tuned for updates on our site: www.arkhospitals.org

Command Sergeant Major Gretchen Evans

RaDonda Vaught
HOSPITAL NEWSMAKERS


Mercy Fort Smith celebrated the opening of its $186 million ER and ICU expansion in May. The facility announced the expansion project in 2021 with the goal of improving emergency and critical care for patients. The expansion will enable the ER to serve an additional 25,000 patients annually, growing its capacity from 29 to 50 rooms. The ICU’s capacity increased from 38 to 64 beds, allowing the facility to double the rooms capable of supporting ventilators. The hospital’s former ICU space will be converted into a 22-bed observation unit. The ICU and ER upgrades are supported by a state-of-the-art automation system that allows entire floors or pods to be converted into isolation areas when needed. Mercy expects to hire about 200 more caregivers in the next few years to help expand patient care in the new departments. To support the increased patient volume, Mercy Fort Smith is adding 400 parking spaces near the new ER entrance and plans to expand visitor services with a gift shop and meeting room space, expected to be complete in the fall.
Mercy Fort Smith celebrated the opening of its $186 million ER and ICU expansion with a ribboncutting ceremony in May. The project adds 21 ER rooms and 26 ICU beds, aiming to serve 25,000 more patients annually. (Photos provided)
Arkansas Hospice Family of Care will rebrand to Life Touch Health in October. Life Touch Health will bring a continuum of services including hospice and palliative care, plus primary care to patients with limited mobility and transportation who live in independent or assisted living facilities, and personal care services. While the team remains the same, Arkansas Hospice expects to release a rebranded website on Oct. 1 equipped with new email addresses. Their phone numbers and physical locations will remain the same.
Ouachita Behavioral Health and Wellness is partnering with CHI St. Vincent to provide a new mental health program. The Ouachita Regional Counseling and Mental Health Center will place two mental health professionals in the emergency room at CHI St. Vincent to assist with patients in a behavioral health crisis, ensuring a seamless handoff from discharge to their follow-up appointment with a mental health professional.
CHI St. Vincent reached a new multiyear agreement with UnitedHealthcare, effective April 9, 2025. The renewal agreement will allow patients to maintain in-network access to all CHI St. Vincent services across existing contracted products, including UnitedHealthcare and Medicare Advantage. CHI St. Vincent sought to work with UnitedHealthcare to reach an agreement, with the end goal to ensure that it could continue to meet the needs of Arkansas patients today and in the future.
Washington Regional Medical Center has been redesignated for a fourth time as an Antimicrobial Stewardship Center of Excellence by the Infectious Diseases Society of America (IDSA).
The Arkansas Department of Health has recognized Saline Memorial Hospital , North Arkansas Regional Medical Center and Mena Regional Health System as Arkansas Stroke Ready Hospitals (ArSRH). Hospitals with the ArSRH designation partner with local EMS to improve outcomes by helping ensure stroke patients are rapidly transported to the most appropriate hospital. EMS providers screen patients with standardized protocols to effectively recognize stroke and ensure patients receive the right kind of care. Arkansas’s stroke systems of care consist of Det Norske Veritas and The Joint Commission Certified Comprehensive Stroke Centers, Primary Stroke Centers, Acute Stroke Ready Facilities and ADH-designated ArSRHs. ArSRHs can provide time-critical care for stroke patients, including initial emergency evaluation with real-time stroke assessment and treatment through telemedicine.
The University of Arkansas for Medical Sciences and Washington Regional Medical Center have received initial accreditation for new neurology and emergency medicine residency programs in Northwest Arkansas, marking the region’s first non-primary care residencies. These programs, which can begin recruiting residents this fall for a July 2026 start, will eventually host a total of eight neurology residents and 18 emergency medicine residents. This expansion, supported by $4.5 million in state funds, addresses the growing demand for specialized medical care in Northwest Arkansas, aiming to reduce wait times and improve access for patients. Washington Regional will serve as the primary clinical site for both programs, with rotations also occurring at Arkansas Children’s Northwest and other facilities. The neurology program is led by Dr. Jay Hinkle and Dr. Margaret Tremwel, while Dr. Joel “Cam” Mosley and Dr. Ryan Mantooth lead the emergency medicine program. These additions are part of a broader effort by the UAMS/Washington Regional Graduate Medical Education Program, established in 2021, to expand physician numbers and enhance health care access in the rapidly growing region.
Baxter Health officially opens its new facility at 100 Town Center Drive in Harrison with a ribbon-cutting ceremony June 16. The location houses Baxter Health Ambulatory Surgery Center and Baxter Health Imaging at Harrison, plus Arkansas Orthopedics and Sports Medicine, expanding local access to outpatient surgical care and imaging services.
The University of Arkansas for Medical Sciences Medical Center has been recertified as a Comprehensive Stroke Center by DNV Healthcare USA Inc.
Ronald McDonald House Charities of Memphis announced its expansion into Jonesboro, Arkansas, in partnership with St. Bernards Healthcare, Hunt Properties, and Hyatt Place Hotels. This collaboration will bring much-needed support to families with critically ill children receiving medical care in the region. While specific details about the expansion, including the location and construction timeline, are still being developed, RMHCMemphis is dedicated to creating a space where families can find the respite and resources they need. As plans progress, updates will be shared with the Jonesboro community.
Investing in Safety: AHA Program Drives Infection Control Certification Success
By Nikki Wallace, MS, BSN, RN, CIC
Infection preventionists (IPs) play a crucial role in their health care organizations in preventing transmission of infections. This is accomplished through surveillance, implementation of evidence-based practices and protocols, epidemiologic investigations, educational program development, compliance with regulatory and reporting requirements, performance improvement, occupational health, advocacy, and much more. IPs constantly collaborate with team members within their organizations as well as key stakeholders outside of their organizations such as public health officials, product vendors, and community health partners. Adapting to changing regulations and best practices requires IPs to continuously learn and increase their skills. One way to measure current knowledge is through Certification in Infection Control (CIC®) which is a comprehensive exam designed by the Certification Board in Infection Control & Epidemiology (CBIC).
The Arkansas Hospital Association, through funding from the U.S. Department of Health and Human Services, Assistant Secretary for Preparedness and Response (ASPR) Hospital Association COVID-19 Preparedness and Response Activities grant, was able to host a CIC Prep Course for 50 hospital IPs. The course included a full-day, in-person intensive overview followed by eight virtual sessions that provided a deep dive into each chapter of the Association of Professionals in Infection Control and Epidemiology (APIC) Certification Guide. Participants benefited from a comprehensive package provided at no cost, which included: a study guide, a prep course, the APIC Text, nursing contact hours, peer networking, exam fee reimbursement upon passing, and access to a national infection prevention expert. Certification is valuable to both the IP and the health care organization. The course’s monetary value is estimated at $124,500; however, the impact goes far beyond the estimate with evidence suggesting that hospitals with certified IPs have lower infection rates. The course was very successful, with 20 participants taking and passing the Certification in Infection Control (CIC®) exam, significantly increasing the number of certified IPs in Arkansas.
PARTICIPANT FEEDBACK:
“Thank you to the Arkansas Hospital Association in helping me achieve my goal of becoming Certified in Infection Control.”
Hilda Lauhon (since 2009), Infection Preventionist- Chicot
PARTICIPANT FEEDBACK:
“I am appreciative of our team at AHA and their support of Arkansas hospitals. My passion is to see others grow in their chosen roles. This group of IPs represent such dedication and passion to ensure our patients, their families, our health care teams and the communities they serve receive the best care. Having been an IP in a hospital, I know how difficult the demands of this role can be. I am so proud of this group and know they will do great things! I encourage others to become certified. I wish I had not waited 20 years, but thankful to be part of the “Class of 2025” with an amazing team of IPs.”
Nikki Wallace, Arkansas Hospital Association, Quality Specialist
This accomplishment shows the commitment of these individuals to the profession of infection prevention, their hospitals and the quality of care to the patients they serve in Arkansas. The following individuals earned their certification through this course:
Patricia Braun — Baptist Health- Fort Smith/Van Buren
Madison Chiolino — Saint Mary’s Regional Medical Center
Kenda Clopton — Ozarks Community Hospital
Roxanne Farmer — Ashley County Medical Center
Elisabeth “Beth” Felty — Saline Memorial Hospital
Matthew Helms — Baptist Health- Fort Smith
Bianca Johns — Washington Regional Medical Center
Alicia Knight — Izard Regional Hospital
Cayce Ladyman — Northwest Medical Center- Springdale
Hilda Lauhon — Chicot Memorial Medical Center
Margo Leavitt — Washington Regional Medical Center
Hazel Liverett — UAMS Medical Center
Hayley Montoya — CHI St. Vincent Infirmary
Melissa Reny — Stone County Medical Center
Allison Scroggins — CHI St. Vincent Sherwood Rehab Hospital
Michelle Sepulvado — South Arkansas Regional Hospital
Nikki Wallace — Arkansas Hospital Association
Cissy Ward — CHRISTUS St. Michael Health System
Joy Watts — Baptist Health- Drew County
Salena Wright-Brown — Central Arkansas Veterans Healthcare System

It was an honor to coach and support such a highly motivated and energized group of Infection Preventionists in Arkansas. I am passionate about supporting the next generation of Infection Preventionists as our work and contributions to safer health care communities is so vital.
Barbara DeBaun, Independent Consultant/Improvement Advisor
PARTICIPANT FEEDBACK:
“I am so very thankful for the opportunity that AHA afforded to all Arkansas IPs to increase our knowledge and grow the profession in Arkansas. It was so satisfying to recognize that I could stretch my brain and continue to learn and be a valuable partner in providing care to our “friends and families” in the community I serve. The AHA has shown a great commitment to healthcare professionals by supporting them with excellent educational and networking opportunities.”
Elisabeth Felty, Infection Preventionist (since 2022), Saline Memorial Hospital

The Capitol Report: 2025 Legislative Summary
By Jodiane Tritt, Executive Vice President, Arkansas Hospital Association
On Jan. 13, 2025, Representative Brian Evans of Cabot was formally elected as the Speaker of the House of Representatives, and Senator Bart Hester began another term as the President pro tempore of the Senate. Each of the 100 members of the House represents about 30,000 Arkansans, and each of the 35 Senators represents about 83,000 Arkansans. Of the 81 Republicans and 19 Democrats elected to the House, 12 served their first term. Of the 29 Republicans and six Democrats elected in the Senate, only one was a new member.
Of the 1,959 bills of all types filed, 1,026 (about 52%) became law. Six hundred two regular House bills became Acts (about 60% of the 1,005 filed), and 424 regular Senate bills that did the same (about 66% of the 647 filed).
For hospitals, the session highlights include Medicaid expansion, maternal health, pharmacy, and commercial insurance relationships.
M EDICAID EXPANSION
Since its inception in 2013, authorizing and funding the Medicaid expansion program has been politically challenging. Originally known as the Arkansas Private Option, the program has undergone changes in each legislative session to ensure that 75% of both the House (75/100) and Senate (27/35) approve the appropriation that funds not only
Cheri
the expansion program but also the majority of Medicaid spending within the Department of Human Services (DHS) Division of Medical Services.
The current program is known as Arkansas Health and Opportunities for Me (ARHOME). The waiver to allow the program expires in December of 2026, so this session was the most efficient time to make any changes to ensure that DHS has the ability to negotiate terms and conditions with the federal government to maintain the state-federal funding mechanism that allows 19- to 64-yearold Arkansans under 138% of the federal poverty level to be covered by insurance on the health insurance marketplace.
Medicaid expansion has been a lifeline for Arkansas hospitals. Every person can seek care in a hospital emergency department, regardless of their ability to pay. When patients have insurance, Medicaid, or Medicare, the hospital can recover at least a portion of the cost of providing that care. When patients have no insurance and no financial ability to pay for the care they receive, the hospital is forced to absorb significant uncompensated care expenses. When costs exceed revenues, hospitals are left with no choice but to cut personnel or services. Hospitals that are already operating at a loss and have already made cuts could face closure, leaving Arkansans with decreased access to health care.
This session, Senator Missy Irvin filed SB 527 (Act 774). Senator Irvin also led the charge to reauthorize the Medicaid expansion and modified the program to add (1) a work requirement for enrollees and (2) a medical loss ratio requirement intended to ensure that a higher percentage of the premiums paid to insurers is paid to providers or to invest in quality
improvement activities benefiting patients. In addition, SB 33 (Act 887) exceeded the 75% threshold for the Medicaid appropriation.
MATERNAL HEALTH
Arkansas has one of the highest maternal mortality rates in the United States and only 33 Arkansas hospitals have a labor and delivery department. Fifty-one of our 75 counties are without delivery services. Because Arkansas Medicaid covers pregnant women up to 214% of the federal poverty level, about 60% of births are paid for by Medicaid (whether through fee-for-service or Medicaid expansion).
Governor Sarah Huckabee Sanders held a press conference on Thursday, Feb. 6, 2025, to announce an investment of more than $45 million for maternal health and for substantive legislation — HB 1427 and SB 213 (Act 140) — to expressly:
• require Medicaid to reimburse providers for depression screenings of pregnant women;
• require Medicaid to reimburse providers for prenatal, delivery, and postpartum services separately (no longer in a bundled payment);
• add “presumptive eligibility” (temporary Medicaid coverage while the full Medicaid application is being processed) for pregnant women;
• require Medicaid to cover blood pressure monitoring services for pregnant women;
• require Medicaid to cover medically necessary remote ultrasound procedures; and
• add Medicaid reimbursement opportunities for community health workers and doulas related to prenatal and postpartum care.
Other Acts aimed at improving maternal health include:
• HB 1181 (Act 138), which allows certified nurse midwives admitting and vital statistics privileges if approved by hospital medical staff.
• HB 1610 (Act 387), which clarifies a medical emergency under the Arkansas Human Life Protection Act and the Arkansas Unborn Child Protection Act.
• HB 1826 (Act 866), which mandates coverage for delivery of a newborn in a licensed birthing center.
• HB 1252 (Act 965), which creates certification and reimbursement for doulas.
• HB 1258 (Act 435), which creates certification and reimbursement for Community Health Workers.
• HB 1296 (Act 556), which allows for reimbursement for health care services provided in mobile units.
• HB 1333 (Act 627), which allows for reimbursement for breastfeeding and lactation consultant services.
• HB 1826 (Act 866), which allows for reimbursement for delivery of a newborn in a licensed birthing center.
PHARMACY
Since 1975, with the exception of a few grandfathered-in hospital pharmacies, Arkansas nonprofit and governmental hospitals have been prohibited from having a retail pharmacy permit. SB 58 (Act 52), led by Senator Jonathan Dismang and Representative Jon Eubanks, removes that prohibition, which will allow hospitals opportunities to provide better pharmacy access to patients. Act 52 was not the pharmacy bill with the most attention this session, though. The Arkansas Pharmacists Association legislation — HB 1150
(Act 624) — was the pharmacy showstopper. In a press conference on Jan. 16, 2025, Representative Jeremiah Moore and Senator Kim Hammer, alongside independent pharmacists, pharmacy advocates, Attorney General Tim Griffin, and Lieutenant Governor Leslie Rutledge, touted the bill’s intent to eliminate anticompetitive business practices by pharmacy benefit managers (PBMs). That Act is the first of its kind in the nation and prohibits PBMs from owning or operating pharmacies in the state. Both CVS and ExpressScripts have filed lawsuits in the United States District Court for the Eastern District of Arkansas.
COMMERCIAL INSURANCE RELATIONSHIPS
In the previous legislative session, Representative Lee Johnson and Senator Missy Irvin did an incredible job of passing negotiated legislation intended to reduce the administrative burdens that insurance companies impose on health care providers through the prior authorization process. Unfortunately, many insurance companies created even bigger roadblocks for efficient patient care between the last session and this one, necessitating more changes to Arkansas’s Prior Authorization Transparency Act.
HB 1300 (Act 510) establishes a trust fund for the Arkansas Insurance Department to collect penalties and fees from health care insurers for noncompliance with the Prior Authorization Transparency laws. HB 1301 (Act 511) better defines the “Gold Card” program that requires a health care insurer to authorize exemptions from a health care insurer’s or pharmacy benefits manager’s prior authorization requirements.
In addition to prior authorization process changes, HB 1288 (Act 423) now requires health care insurers to retroactively reimburse providers awaiting in-networking credentials for the work that the provider does back to the date that the medical board submits a completed packet to the insurance company and HB 1788 (Act 571) requires that a health care insurer make a determination of in-

Scan this code to visit the list of bills impacting health care.
network participation of a provider (who is not a physician) within 90 calendar days from the date of submission of a completed application.
The bill that received the most attention from the health insurance industry, though, is HB 1930, which, if passed, would have required that, by Jan. 1, 2030, minimum hospital and physician (and certain other health care providers) reimbursement from commercial insurance plans would be set at 100% of the average commercial rate of Louisiana, Mississippi, Missouri, Oklahoma, Tennessee, and Texas. Representative Jeff Wardlaw stood firm against insurance companies and ushered the bill out of the House Insurance and Commerce Committee, despite loud opposition from employers and insurance companies alike.
While the bill fell just short of the necessary 51 House floor votes, the conversation around poor hospital reimbursement, increasing employee insurance premium costs, and insurance profits was important and places the topic of hospital and health care financing high on the priority agenda for upcoming sessions.
NEXT STEPS
The 95th General Assembly adjourned sine die on May 5, 2025. Thankfully, the soft drink tax remains in place, which funds the discretionary portion of the Medicaid Trust Fund. The Arkansas Nurses Association led the charge for SB 435 (Act 753) to improve upon the definition of a “health care worker” regarding enhanced penalties of assault and battery upon a health care worker. SB 601 (Act 971) establishes a pathway for graduates of foreign medical schools to be licensed in Arkansas under certain conditions. And there is more.
For a more comprehensive list of bills impacting health care this session, please visit our website at arkhospitals.org/Online/Advocacy/2025_Session.aspx.
In the meantime, please continue to advocate for patients and hospitals between sessions. Successful sessions are not earned during the legislative session alone. Everything hospitals do in the interim is important, too.
Jodiane Tritt, JD, serves as Executive Vice President of the Arkansas Hospital Association.

Peer Power: AHA Affiliated Groups – Unlocking Collective Strength for Arkansas Health Care
The need for hospital services often arises without warning, yet accessible health care remains a universal necessity. A community’s well-being is closely tied to readily available medical support, especially when individuals are managing chronic illnesses or facing sudden health crises where timely access to providers and care can truly determine outcomes.
For many in Arkansas, a predominantly rural state, timely access to local care is vital. Whether for a new parent, an older individual managing a longterm condition, or someone experiencing a medical emergency, by the time a hospital is truly needed, it’s too late to consider the consequences if one isn’t nearby — or worse, if a familiar facility is no longer available.
Providers and health systems are navigating increasingly complex financial landscapes. Unlike many other sectors, hospitals often rely on reimbursement structures that limit their ability to adjust rates to keep pace with rising operational costs. This, combined with economic shifts, presents significant challenges.
Those entrenched in health care understand the difficulty of long-term planning today. From supply chain disruptions to evolving regulations and policy changes, there’s a constant stream of factors to monitor and manage.
One of the most effective ways to optimize resources and navigate these challenges is to embrace the philosophy that a rising tide lifts all boats. The Arkansas Hospital Association supports a variety of affiliated groups designed to foster collaboration and shared progress. These groups offer specialized areas within hospitals an avenue to track regulatory changes, network with peers across the state, and access ongoing education. Knowledge is certainly power, but the strength found in peer-to-peer networks, mentorship, and connecting with others facing similar circumstances brings a lasting impact.
The following pages highlight the vital work of a handful of affiliated groups connected with the Arkansas Hospital Association. For a complete list of affiliated groups, to learn more about each, and to find out how to join, please visit our website: arkhospitals.org/Online/ About_AHA/Affiliated_Groups.aspx.
Scan this code to to learn more about our affiliated groups.

ACHE of Arkansas: Fostering the Health Care Leaders of Tomorrow
By Becca Bona
Just as effective leaders navigate numerous challenges, exceptional health care leaders guide their organizations through uncertainty and complex regulatory burdens with grace. For health care professionals in Arkansas, there are ample opportunities to sharpen leadership skills, including staying active with the Arkansas Chapter of the American College of Healthcare Executives (ACHE of Arkansas).
ACHE of Arkansas is the local chapter of the American College of Healthcare Executives and serves as a forum for professional development for health care executives in the state. Since its inception, the association has expanded its membership to include all those involved in care-related professions, including consultants, informaticists, accountants, and students in health care management programs. The ACHE of Arkansas membership connects health care professionals from diverse settings who face similar challenges, empowering them to focus on professional growth and enhance health care management.
Vice President of St. Bernards Medical Center Connie Hill has served in various capacities with ACHE of Arkansas. A former president, presidentelect, and committee member, she’s currently a member and fellow within the organization. For Hill, the state chapter is integral for staying informed about both federal and state issues. “The purpose of the local or the state ACHE is to promote the goals of the national organization at a local level,” Hill said. “And I think one of the most impactful things about ACHE of Arkansas, is that it keeps us
informed about not only what is happening at the state level but also educates us regarding federal activities that can impact us at the state and local level.” This knowledge is crucial for hospitals to strategically allocate resources and adapt to changing regulations.
ACHE of Arkansas also provides a learning network, in which members can collaborate, identify issues, and share best practices. “The networking is really a big piece for me, because health care happens locally, and while there are things that are decided at the federal level, things transpire in your state at your local level,” she explained. “Being able to interact with each other at a local level and to network with each other across the state has been extremely vital to our organization and to my personal leadership success.”
During the height of the COVID-19 pandemic, Hill noted that ACHE of Arkansas was “vital” for knowledge sharing in a continually changing landscape. She also highlighted the benefit of ACHE of Arkansas’s affiliation with the Arkansas Hospital Association, noting that members stay wellinformed and connected. A robust knowledge sharing environment ensures that resources are maximized and services not duplicated. There is also a dedication to mentoring within the Arkansas chapter.
“Our Arkansas board really focuses on mentorship and supports students majoring in health care administration” Hill said. “That includes students who are getting their master’s in health care administration or MBAs, with an interest in health care. We have two programs that we work

with to provide them with free membership into ACHE at the state level for the purpose of providing mentorship. We have also provided financial support for attending ACHE Congress in the past.”
At St. Bernards, Hill applies ACHE’s mentorship principles directly into her own workflow. “Sometimes you need another person to be a sounding board,” she explained. “Asking them, am I really looking at all the options that are available? I think mentorship is the key to longevity of our program at both the national and the state level.”
ACHE of Arkansas offers various engagement opportunities, including in-person and virtual learning. Hill emphasized the importance of leadership endorsement within health care organizations to underscore the value of ACHE membership and its contribution to organizational capacity. “In our leadership classes at St. Bernards, ACHE is mentioned as a resource that is endorsed by administration and is found to be valuable,” she explained. “It’s used as a stepping stone and helps foster growth during one’s professional development.”
ACHE facilitates valuable networking opportunities that extend beyond the state’s border allowing members to learn from and adapt best practices. Hill shared an example involving fact-gathering when she

Leaders gathered at the recent ACHE of Arkansas and Arkansas Association of Hospital Trustees panel discussion in May, “The Healthcare Organization's Role in Public Policy,” to explore crucial policy engagement for health care organizations. (Photos by Lyndsey Dumas)


Stronger Hospitals, Smarter Solutions.
with
Chris Newkirk Area Vice President chris_newkirk@ajg.com (501) 485-3082
© 2025 Arthur J. Gallagher & Co. | GBSUS104196
Bill Birch Senior Area Vice President bill_birch@ajg.com (501) 614-1170



became involved in a new line of service at St. Bernards. “I was able to evaluate who was already providing the service at a very high level and then reach out to that person for more information,” she said. Her first contact happened to be an ACHE of Arkansas member she knew professionally. Likewise, St. Bernards frequently hosts site visits for other organizations that are starting new programs, who desire to network and learn about processes and successes.
“When we connect with groups through ACHE, they’ll come visit, bring their team, and participate in the daily activities of the given department,” she further explained. “Then typically we host a round table discussion to ensure we answer all of their questions.”
According to Hill, the site visits that St. Bernards have hosted and attended whether in person or virtually, have all evolved from ACHE of Arkansas networking opportunities. “We have worked with Washington Regional, Baptist Health-Little Rock, Conway Regional Medical Center and White River Medical Center, just to name a few,” she said. Regionally, St. Benards has hosted and visited with ACHE partners at Vanderbilt, Centennial, Mayo, and Cleveland Clinic.
“These relationships were very valuable to us as we pushed our Emergency Department to improve throughput, quality, and decrease Left Without Being Seen percentages,” she said. “We again utilized our ACHE partners when the ED adopted Pulsara for all incoming EMS transfers and Mass Casualty.” Hill reiterated that without leadership backing, St. Benards would not likely see benefits from ACHE. “Michael Givens is our COO at St. Bernards, and he is incredibly supportive of ACHE and often facilitates sharing of information across our organizations where we have developed ACHE ties,” she said.
By fostering leadership development, promoting collaboration, and facilitating the sharing of best practices, ACHE of Arkansas directly contributes to building capacity within Arkansas hospitals, enabling them to navigate financial challenges and continue providing highquality care.

BOWEN HEFLEY N. LITTLE ROCK

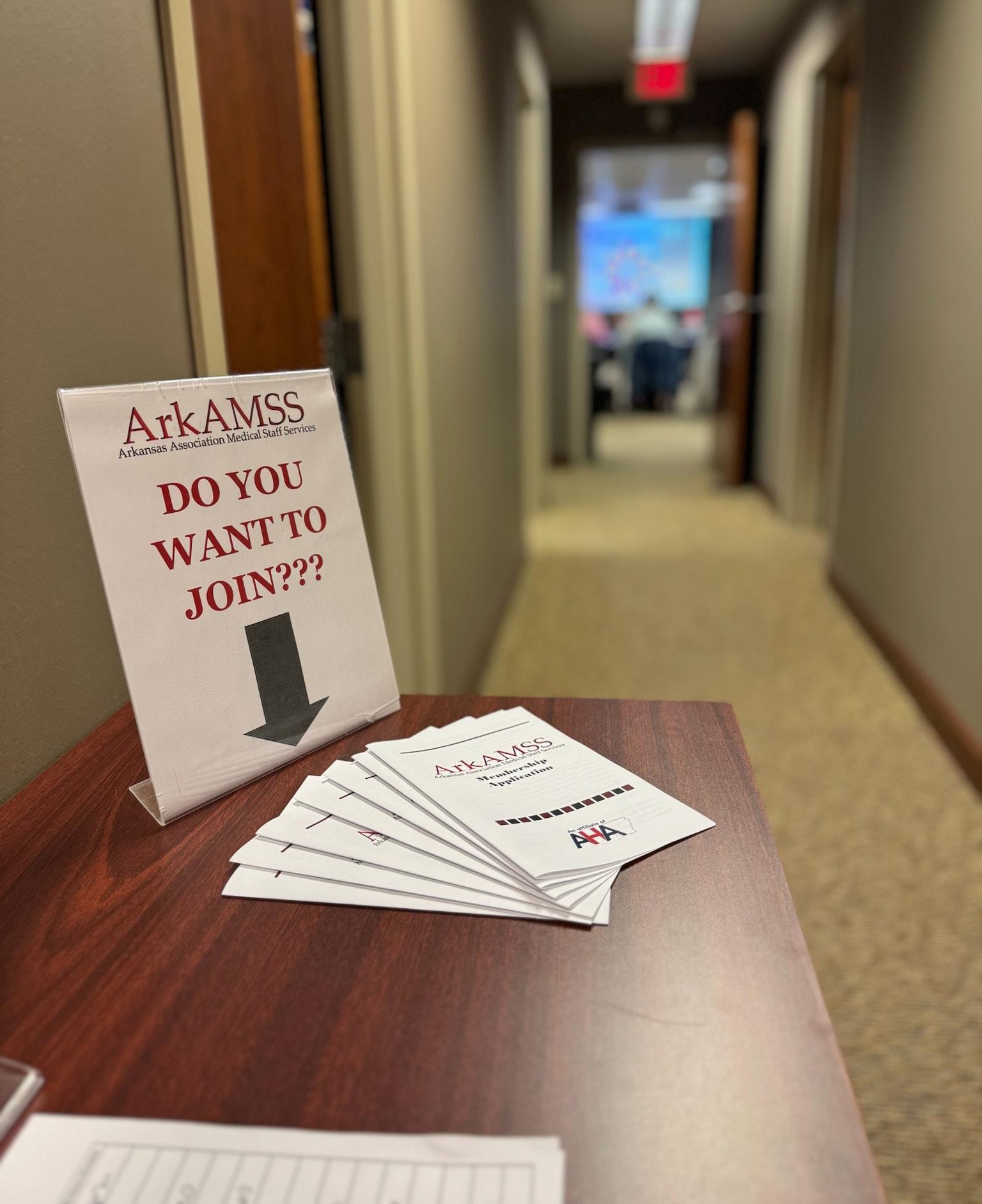
Behind the Scenes: ArkAMSS Connects Medical Staff Services, Elevates Standards
By Becca Bona
In the complex world of health care administration, ensuring the competency and credibility of medical professionals usually happens behind the scenes. As an affiliate of the Arkansas Hospital Association, the Arkansas Association of Medical Staff Services (ArkAMSS) connects professionals statewide to foster a knowledge-sharing network and uphold the highest standards of patient care.
Medical staff services professionals manage the intricate credentialing and privileging processes, verifying the training, experience, and licensure of physicians and other health care practitioners. Their work ensures patients can trust the qualifications of those providing their care. Beyond initial verification, medical staff services professionals are also responsible for managing accredited continuing medical education programs, ensuring that practitioners stay up to date with the latest advancements and best practices.
Expanding its reach, ArkAMSS hosted its first hybrid conference in April, ensuring medical staff services professionals from all corners of Arkansas could access essential knowledge and peer support.
(Photo by Tiffany Hawkins)
Credentialing Manager for the UAMS Professional Staff Office Tiffany Hawkins, this year’s president of ArkAMSS, emphasizes the importance of open knowledge-sharing within the association, either via the group’s listserv or networking. “We try to focus on the fact that there’s no such thing as a dumb question,” she said. “Even if someone’s not comfortable communicating and writing in that group, they can pick up the phone, and they can ask whatever they need to ask, and we’re happy to share that information.”
Members can connect with peers through regular meetings, workshops, and conferences, exchange best practices, and stay informed about the latest regulatory changes and industry trends. This collaborative environment is particularly valuable in a state like
Arkansas, where professionals may be the sole experts in their field within their respective institutions. Director of Medical Staff Services at North Arkansas Regional Medical Center Christy Gray, ArkAMSS past president and board member, underscores the importance of this peer network. “In my opinion, ArkAMSS is a group of medical staff professionals that can count on each other and bounce ideas off each other,” she said.
Both Hawkins and Gray remember their early days in the field. As an office of one, Hawkins relied heavily on her predecessor’s meticulous documentation but found ArkAMSS early on. “This is an ‘Each One, Teach One,’ environment and it is important for us to make sure that organizations know exactly what we represent and
why we are of value, because many of us stumble into this field. Sometimes we don’t have someone in our office to teach us,” she said.
Gray made the move from marketing to medical staff servicing, and remembered how overwhelming it was, as she also served in an office of one. “I didn’t really have a lot of guidance, and ArkAMSS was instrumental in leading the way,” she said. Gray has been involved in the board and ArkAMSS in some capacity for the past 10 years.
ArkAMSS strives to host one or two conferences a year, and under Hawkins’ leadership, is focusing on carving out board member roles and duties. “Part of my goal list that I’ve created for myself as the president this term is to try to identify who can take up that charge for the various committees on our board so that we can focus on education initiatives and membership engagement,” she said. “I want to make sure that not only are we getting new faces involved, but that we also are thriving and meeting all of the needs for not just the metro here in Little Rock, but all of our regional and rural areas that are underrepresented.”
ArkAMSS is made up of geographical districts across the state, with elected district representatives at the helm. Gray and Hawkins feel that more interaction between district representatives and some of the harderto-reach hospitals within their districts would be invaluable for improving rural outreach. “Whether it’s a huge hospital
Photo by Cassandra Van Tassel
with 300 providers, or a small hospital with 10, we all have the same rules, regulations, and guidelines to follow,” Gray said. “We all credential the same.”
COVID-19 affected member engagement, but the ArkAMSS board tackled that issue head-on this year by embarking on a phone campaign to reach all hospitals across the state and their various medical staff services. “There were plenty of people who hadn’t heard of us,” Gray said. “We invited them to become members because we want to grow.” In yet another effort to reach those who might not be able to travel, ArkAMSS recently conducted its first hybrid conference in April. “Being able to host a virtual conference will allow us to reach those who might not be able to travel to those in-person conferences,” Hawkins said.
ArkAMSS works to keep education at the forefront for all aspects of the evolving scope of the profession. “It’s not that we’re only dealing with making sure that someone is who they say they are so they can be privileged,” Hawkins said. “It’s also being able to maintain that competency, which translates to wellness.”
As ArkAMSS continues to evolve under the guidance of dedicated leaders like Hawkins and with the enduring support of members like Gray, its commitment to connection, education, and outreach remains steadfast. By embracing innovation and actively seeking to engage every medical staff services professional across Arkansas, ArkAMSS is poised to further elevate standards and strengthen the very foundation upon which exceptional patient care is built.


DREAM BIGGER
.

Progress starts with our team’s healthcare finance solutions.

Shared Insights, Stronger HR: Maximizing Capacity Through AHHRA’s Network
By Becca Bona
In today’s financial landscape, health care leaders seek ways to maximize resources and achieve optimal efficiency without sacrificing care delivery. Now more than ever, knowledge sharing can be a beacon for hospitals of all sizes, especially in a small, rural state like Arkansas.
One Arkansas Hospital Association affiliated group — The Arkansas Healthcare Human Resources Association (AHHRA) — provides its members with a robust knowledgesharing forum and has done so for over 50 years. Richard Tyler — Chief Human Resources Officer with Conway Regional Health System, has been involved with AHHRA for nearly 20 years, serving as president in the past, and currently serving as vice president. Tyler noted that at its core, AHHRA was formed to provide continuing education: “Historically, that’s been the primary focus in our bylaws, to educate our membership.”
AHHRA generally represents between 40 and 50 Arkansas hospitals; membership typically hovers around 65 individuals and is open to practitioners within the HR
field in a health care setting in Arkansas who pay an annual membership fee. AHHRA typically organizes and offers two conferences each year to serve its mission.
Layton Anderson, Vice President and Chief Human Resources Officer for Jefferson Regional Medical Center and current AHHRA Executive Vice President, explained how AHHRA strives to meet its membership where they are.
“This last year, we didn’t charge our members to attend our conferences due to the financial pressures that health care is under these days,” Anderson said. He explained that the board can leverage valuable partnerships with sponsorships to keep prices down.
The conferences offer an opportunity for those from smaller hospitals to access fundamental HR continuing education, and for members to do a deep dive into regulatory overhauls. Tyler cited the introduction of Obamacare as an example. “We brought in a lot of great national speakers as well as local speakers to make sure that our membership could handle that transition to Obamacare,”

he said. Over the years, topics have included everything from regulatory updates to employee retention. Current AHHRA President, Sally Cassell, Employee Services Specialist at Ozark Health Medical Center, noted the next focus will be on benefits and retirement regulations. “I feel like that’s going to bring a lot of interest to our group, as well,” she added.
Beyond providing education, AHHRA also includes networking opportunities, which Tyler noted is incredibly valuable to HR professionals, whether seasoned in their career or just starting in the profession. Conference attendees can share knowledge in real time at the much-anticipated HR roundtable, which takes place during each event. “I think our membership gets a lot out of that, because there are things that will come up that several of us may not be aware of,” he explained. “I think that is what a lot of our members value, is building those relationships with each other.”
At the recent AHHRA Spring Conference in early April members gained essential knowledge and forged valuable connections. This annual event is a cornerstone of AHHRA's mission to enhance HR capacity across Arkansas hospitals through shared insights and collective expertise. (Photos by Cassandra Van Tassel)
Arkansas Senior Health Insurance Information Program

Arkansas Senior Health Insurance Information Program (AR SHIIP)









Tyler, Cassell, and Anderson all represent different organizations, and their work environments alone illustrate AHHRA’s goal to include everyone. “Some of the smaller hospitals in Arkansas don’t have access to legal counsel and other educational resources,” Anderson said. “We find when we get together and start having open discussions with them, they’re seeking to get some of that general knowledge, things that we may take for granted in our organizations.”
Cassell, who works for a critical access facility, agreed. “We have around 400-plus employees, so the funds that we do have are not available for this type of education. If I wasn’t in this group, we would be very limited here in terms of the knowledge we have,” she said. As the leadership of AHHRA monitors members’ needs, they employ a dynamic approach with educational opportunities, including

providing more education opportunities in different formats. “Some people can’t travel to the conferences,” Anderson noted, “so we are examining how we can provide those resources to them digitally.”
As an association vested in the future of health care in Arkansas, AHHRA is also now involved in educational pathways. Tyler noted that the Arkansas Economic Development Commission recently reached out to AHHRA asking what training needs in health care currently look like. “Our board members compiled a list of the hard-to-fill jobs in health care. We will have further discussions with the state,

because we want the state to devote resources to more RN schools, LPN schools, surgical scrub techs, respiratory therapists, and med techs.” While these jobs may be easier to fill in a larger metropolitan area in the state, they remain difficult to fill in more rural areas. “That’s what we’re trying to do, is help facilitate that discussion so that the state will devote more resources to help fill this gap in employment that we all are experiencing,” Tyler added.
Moving forward, AHHRA is working to ensure that membership from all areas of the state is well-represented within the organization, especially Northwest Arkansas which currently is not heavily represented. Ultimately, the benefits of AHHRA go back to that knowledge sharing and networking.
“The relationship aspect — to just be able to call on somebody, but also to build those long-term career relationships — is beneficial in being a part of this organization,” Tyler said. Cassell echoed that sentiment, noting that the membership is what sets AHHRA apart. “At AHHRA, members come first. Here’s the truth about membership — we tell it like it is, provide practical tools, and connect you with a powerhouse network of health care HR leaders. If your purpose is to grow, lead, and drive meaningful change in your organization, AHHRA is where you belong.”



Arkansas Society for Directors of Volunteer Services: Empowering Volunteer Leaders
By Becca Bona
The Arkansas Society of Directors of Volunteer Services (ASDVS) plays a vital role in supporting leaders of volunteer programs across the state. As an affiliate of the Arkansas Hospital Association, ASDVS provides networking, educational opportunities, and a platform for collaboration among directors of volunteer services in Arkansas member hospitals.
Current president Kristi King, Ozark Health DVS, said that one of the most significant benefits of membership is becoming a part of a network that strives to engage and empower. “We help to build camaraderie among volunteer leadership,” she said. “And we take back ideas to our hospitals so that we can help our volunteer programs be the best that they can be.”
ASDVS holds educational conferences two to three times a year, featuring a wide range of topics relevant to volunteer management, ensuring members stay
informed about best practices, emerging trends, and regulatory updates. King believes that having that inperson networking opportunity is incredibly valuable. “[Members] can usually break away from their groups for a little bit, and they really like the opportunity to network and have that time together,” she said.
For many members, this knowledge sharing directly impacts their own best practices. ASDVS member Becky Rose, Director of Volunteer Services at Baxter Health Auxiliary said: “Through discussions, it was shared that Modern Woodmen had a matching grant for fundraising efforts of non-profit organizations, and we held a March Gladness Sale at our Bargain Box Thrift Shop and we were able to receive a $2500 gift from Modern Woodmen.”
King and the ASDVS leadership recognize the value of connecting professionals who share common goals and challenges. “Having a resource to reach out to when you are needing guidance on volunteer management is a valuable tool,” Rose said. “Managing paid staff is different from managing volunteer staff, so having a seasoned volunteer manager willing to share how they have handled a challenging volunteer interaction can be a lifeline and ultimately help someone salvage a volunteer relationship.”
Beyond knowledge-sharing, membership offers a range of benefits, including reduced rates for workshops, active networking opportunities, and communication with peers. Members also receive membership in the Arkansas Hospital Association, further integrating them into the broader health care community. The organization also facilitates communication through a listserv and provides a membership directory.
COVID-19 significantly impacted ASDVS, as many volunteer service positions either disappeared, transitioned, or pivoted. “The number of ASDVS members dropped, but also the number of volunteers across the state dropped significantly, too,” King said.
“We are in a rebuilding phase right now, and we have been for the last couple of years, but I see that not only in hospital volunteers but also with other volunteer programs within my community, as well.”
Looking to the future, ASDVS aims to continue to evolve to meet the needs of its members. Right now, King said that means focusing on providing education on fraud, abuse, and artificial intelligence. “Those are the big things that are trending for us, and we talk about it quite a bit among ourselves,” she said. “Volunteers [...] want to see and believe so much of the good in the world that it’s hard for them to recognize these things.”
Additionally, to serve a largely rural state like Arkansas, ASDVS continually navigates the needs of critical access hospitals with smaller budgets while also supporting larger regional systems that comprise the diverse membership across the state. While members serve a variety of different hospital environments, most are quick to agree that the education, learning, and networking experienced from ASDVS is second to none.
Stephanie Hunter, Manager of Volunteer and Guest Services at CHI Hot Springs, is relatively new to ASDVS. She immediately felt the value of membership: “Networking with the ASDVS community provides practical guidance, resources, as well as inspiration to improve our programs.” She was also able to implement changes even after attending one meeting. For Hunter, ASDVS serves as an advocate for volunteer services in the broader health care conversation: “This ensures that volunteer contributions are valued and protected.”
Rose echoes this sentiment. “Hospital leadership should be recognizing the value the local hospital volunteers and hospital auxiliaries — what those folks bring to their organization — from assisting staff, patients, and their families to understanding that volunteers turn into donors once they see the high quality of care that is provided at each of our hospitals by our staff as they volunteer each day,” she said.


Arkansas Hospital Auxiliary Association: Serving Arkansas with Heart and Hands
By Becca Bona
Since 1955, the Arkansas Hospital Auxiliary Association (AHAA) has supported health care in the state. The organization’s mission, as stated in its bylaws, is “to improve patient care in Arkansas hospitals by assisting in the organization of local hospital auxiliaries, by promoting the development of existing hospital auxiliaries, by providing services and acting as a coordinating body for its members, and by supporting the Arkansas Hospital Association and the American Hospital Association.”
Founded by hospital administrators, AHAA provides a network for auxiliaries and their volunteers who offer essential services to hospitals and communities across
Arkansas. AHAA’s work is carried out through district meetings, state conventions, and various initiatives to support hospitals and enhance patient care. These gatherings provide guidelines, foster collaboration, and celebrate the contributions of volunteers.
AHAA’s structure includes district chairs who help coordinate activities and communication across the state. The organization is governed by a board of directors, with various committees overseeing key functions including the annual convention, bylaws, finance, and membership. Through regular board meetings and the yearly convention, AHAA provides opportunities for members to connect, learn, and celebrate their shared commitment to service.
This year, Charlotte Jackson serves as AHAA’s president, and her chosen theme is modeled after Mother Teresa’s motto: “Do Small Things with Great Love.” For Jackson, the theme emphasizes the importance of every contribution, no matter how small. When she became president, Jackson sent out blank stationery cards to everyone, asking them to mail back examples of how they carried out this motto via their service.
“I’ve heard from many across the state,” she said. “For instance, some work in their cancer center, and the patients might be too weak to open a bottle of water. An act as simple as opening a bottle of water for these patients is huge.” From surgery to the children’s floor and everywhere in between, auxilians across the state are setting out to employ small acts of kindness. These contributions go beyond small moments of grace. Volunteers collectively contributed over $3 million back to hospitals in the past year, demonstrating a significant monetary impact, as well.
Beyond small acts of kindness and fundraising, volunteer activities include advocacy and offering scholarships to future health care workers. However, at the core of their mission is to bring human connection to the forefront. “Coming into the hospital can be scary for the patient, for the visitors, they’re uncertain what they’re going to see or be exposed to,” Jackson said. “Our volunteers are [...] there to help alleviate their fears.”
At the start of 2025, Jackson began visiting member hospitals across the state to listen and learn about their needs and successes. From these meetings, she has developed a major concern regarding the gradual decline in AHAA membership. “I think that volunteers could be utilized more, but what we’re seeing a lot of right now is that hospitals aren’t doing very well. People are having to take on extra roles to keep their jobs,” she said. As volunteer coordinators take on more roles, they don’t have as much time to devote to the volunteers. “The local hospitals are losing [volunteer] membership because they don’t have time to devote to that meaningful experience,” she elaborated.
COVID-19, of course, is primarily to blame for the decline of volunteers across the board, but Jackson sees a changing culture emerging from the aftermath. “Some of the volunteers have grandchildren or great-grandchildren that move back in, and they’re taking care of,” Jackson said. “People in my generation are also having to work.”
For Jackson and many members of the AHAA, this is a question to pose to leadership. “Administrators need to decide — do we want this free labor?” she said. Volunteers can be a method to offer a small glimmer of hope, make a difference, and even provide a financial impact through auxiliary giving. Despite the challenges facing health care and volunteerism, AHAA and its dedicated members continue to play a vital role in supporting Arkansas hospitals and the well-being of their communities.



Whether dressed in costume at a lively AHAA conference or providing direct patient assistance, Arkansas hospital auxilians volunteer their time and efforts to support hospitals across the state. (Photos provided)


HOSPITAL STATISTICS 2025
ARKANSAS HOSPITAL ASSOCIATION 2024 HOSPITAL STATISTICS
35 Arkansas Hospitals 2025 by the Numbers
36 Impact of Medicare Advantage Plans in Arkansas
37 Financial Impact of MA Plans on Arkansas Hospitals
39 AHA Members by City, Type, Size, and Services
42 AHA Members by Control and System Affiliation
44 Arkansas Hospitals Receiving Local Tax Support, 2025
45 AHA Member Organizations by Congressional District
46 Economic Impact of Arkansas Hospitals, 2024
47 Key Financial Indicators: Arkansas and Surrounding States, 2023
48 Statewide Hospital Financial and Utilization Indicators, 2019-2023
49 Comparative Financial Indicators: U.S. Community Hospitals
50 Inpatient and Emergency Department Discharges by Payer, 2023
XX Uninsured Inpatient Admissions and Costs, 2011-2023
51 Hospital Uncompensated Care Costs, 2019-2023
XX Top 20 Inpatient DRGs, 2023
52 Hospital Access by County, 2025
53 Arkansas Hospitals, 2025
Prepared by
Donald McCormick, MSHI, AHA Director of Analytics and Financial Policy
Hart Black, UAMS Graduate Assistant for AHA
Hospital Statistics uses the latest data available. This edition includes utilization and financial data reflecting the periods during and following the public health emergency declaration for the COVID-19 pandemic. When comparing data from 2022-2024 to previous years, it is important to remember that hospitals experienced massive disruptions in 2020-21. Reductions in revenue due to deferred and delayed care, expenditures related to pandemic preparedness and response, supply chain issues, staffing shortages, and several major surges associated with COVID-19 during previous years can bias trends seen in post-emergency data. Financial and utilization measures included are reported based on hospital fiscal year, and not all 2023 data reflect the same 12-month period for each hospital.
ARKANSAS HOSPITALS 2025
BY THE NUMBERS
Newborns were delivered in Arkansas hospitals in 2024. Over 60% of those births were covered by Medicaid. 116
Hospitals of all types are located in cities, towns, and communities throughout Arkansas.
Hospitals and other health care organizations are members of the Arkansas Hospital Association.
Community hospitals have fewer than 100 acute care beds.
Hospitals are designated by the federal government as critical access hospitals, having no more than 25 acute care beds.
Counties are served by a single hospital. Twenty-one of those counties are served by a single critical access hospital and two counties are served by a single rural emergency hospital.
Is contributed by hospitals toward Arkansas’s economy, through the impacts of well-paid, consistent employment, purchases of goods and services, and construction and capital spending.
Of Arkansas workers are employed by hospitals or other health care organizations.
Arkansas counties and cities believe their hospitals to be important enough that people in those areas have voted to provide local tax support for the hospital.
Arkansas counties — more than 25% of all counties in the state – do not have a local community hospital.
Of AHA member organizations are charitable, not-for-profit organizations, while 25% are operated by private, for-profit companies, and 11% are public hospitals owned and operated by a city, county, state, or federal government.
Hospitals offer labor and delivery services for birthing mothers in Arkansas.
Arkansans sought inpatient or outpatient care from the state’s hospitals each day in 2023, on average, for illnesses, injuries, and other conditions that require medical attention.
IMPACT OF MEDICARE ADVANTAGE PLANS IN ARKANSAS
At the end of 2024, roughly 305,000 Arkansans — about 45% of all Medicare beneficiaries in the state — were enrolled in Medicare Advantage plans. Enrollment in these plans has climbed steadily over the last decade, with year-over-year gains first accelerating in 2019 and peaking in 2023 with a 5.5 percentage-point jump over the prior year. As more patients shift into MA plans, Arkansas hospitals have felt the financial squeeze of these plan’s reimbursement practices more acutely.
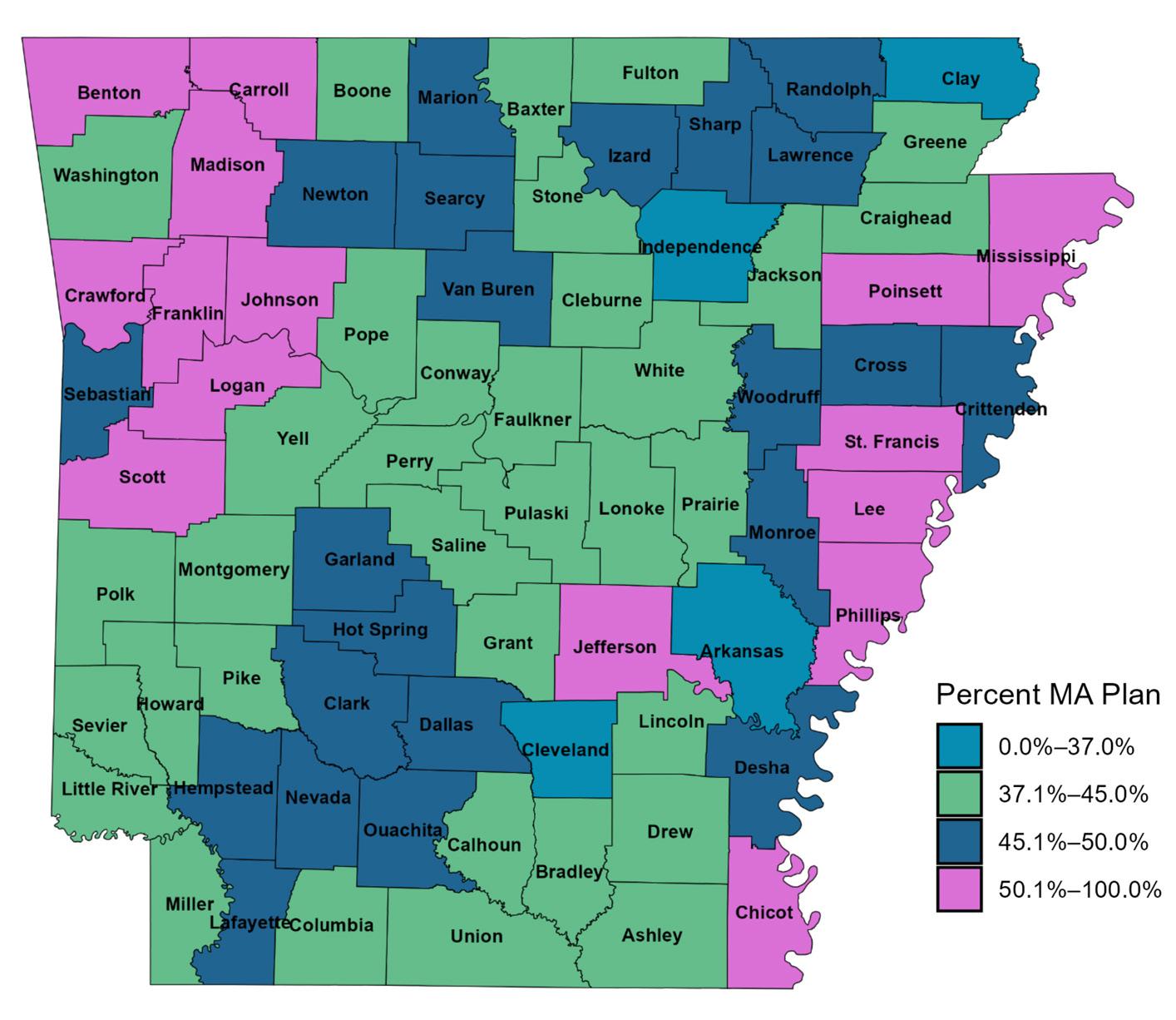
Nationally, hospitals report widespread struggles with inappropriate denials. In 2022, the Kaiser Family Foundation found that more than 83.2% of MA prior- authorization denials were overturned on appeal. Locally, MA plans deny services at twice the rate of traditional Medicare and downcode over 3,500 claims annually compared to fee - for- service Medicare. Even when denials are “cured” on appeal, MA plans take an average of over 70 days to pay — versus roughly 44 days under traditional Medicare.
For many Arkansas hospitals, these delays translate directly into a working - capital gap of 25-40 days. Considering this, a mid-sized community hospital with $10 million in monthly patient revenue suddenly carries an extra $1.3-$1.7 million in receivables on its balance sheet. To bridge this gap, institutions frequently draw on short - term lines of credit — and at current interest rates around 5.5%, holding a $2 million balance for an extra month can tack on more than $9,000 in interest expense alone. Those borrowing costs chip away at already razor- thin operating margins and force hospitals to postpone staffing hires, defer critical equipment purchases, and delay IT and quality - improvement initiatives — ultimately impacting both financial health and patient care.
THE FINANCIAL IMPACT OF MA PLANS ON ARKANSAS HOSPITALS
As Medicare Advantage (MA) enrollment continues to rise, Arkansas hospitals are experiencing measurable financial impacts compared to serving patients with Traditional Medicare. Data from the Vitality Index, which includes 40 participating hospitals over a 12-month period in Arkansas, reveals distinct differences in reimbursement levels, payment timeliness, denial trends, and other financial indicators. The following sections highlight these impacts in detail.
IMPACT TO REIMBURSEMENT
MA plans reimburse Arkansas hospitals 20.2% less than Traditional Medicare for the same services. For patients enrolled in these plans, the patient responsibility is also 36.7% lower. Based on current enrollment patterns, if MA plans reimbursed hospitals at the same rate as Traditional Medicare, the 40 hospitals participating in the Vitality Index would collectively receive an estimated $187 million more in payments each year. This disparity in reimbursement represents a significant loss of funding that directly impacts operational and care delivery opportunities across the state.
“One
of the largest MA plans in our market pays about
82% of Medicare.”
“Financially, MA reimburses us about 6 to 9 percent less than [Traditional] Medicare.”
IMPACT TO PAYMENT TIMELINES
When it comes to clean claims – those processed the first time without error or denial – MA and Traditional Medicare have similar payment timelines. However, the differences become evident when claims require reprocessing after an initial denial. Traditional Medicare typically issues payment within 55 days following resubmission, while MA plans take, on average, 25 days longer.
For hospitals that have already rendered care, these delays impose unnecessary financial strain, particularly when claims remain unpaid for an average of three months due to avoidable denials and administrative burdens.
“…account receivable [for claims] over 120 days are nearly three times higher with MA plans”
“…MA payers have forced us to allocate three full-time staff members to manage denials.”
“MA PLANS DENY SERVICES AT A FAR HIGHER RATE THAN COMMERCIAL PLANS.”
“WHEN WE DO APPEAL, MORE OFTEN THAN NOT, WE PREVAIL.
The MA plan is going to tout [this] as a ‘success’…. What no MA plan wants to acknowledge is that appeals take a lot of time and are very expensive for hospitals. Hospitals rely on physicians and nurses to fight for a service that never should have been denied in the first place.”
IMPACT TO DENIALS
Claims submitted to Medicare Advantage plans are denied at twice the rate of those submitted to Traditional Medicare. In some specialties, denial rates under MA plans are up to six times higher, creating a disproportionate administrative burden on hospital billing departments. Among our hospitals, no medical specialty shows a higher denial rate for Traditional Medicare compared to MA plans. Furthermore, although cured denials (denials reversed upon resubmission) are only 10% more frequent under MA plans, the financial value of these cured denials is twice as high.
“the denial itself can be for any number of reasons (some quite trivial) and always AFTER the service has been provided.”
“While MA plans are only 27% of our overall volume, they create 71% of our claims denials.”
IMPACT TO OTHER FINANCIAL INDICATORS
One significant concern is the practice of downcoding, where insurers alter a claim to reflect a lower level of care than was provided. Over a 12-month period, Medicare Advantage plans downcoded claims 475 times more often than Traditional Medicare. This aggressive cost containment tactic further reduces reimbursement, regardless of the actual acuity of care delivered. Additionally, patients covered by MA plans are more likely to be discharged earlier and less likely to be admitted for inpatient care, even for identical conditions. These patterns suggest care access restrictions driven not by clinical need, but by insurance practices.
While these tactics lower immediate costs for the insurer, they may compromise long-term patient outcomes leading to readmissions that place a downward pressure on hospital finances, ultimately reducing accessibility and quality of care across communities.
“We serve a large population of seniors, and Medicare Advantage (MA) plans have not provided them with the same level of consistent coverage as Original [Traditional] Medicare.”
“We routinely see MA plans challenging and delaying our physicians’ clinical decisions, including downcoding instances as well as 80 percent of reclassifications to observations status versus necessary inpatient care.”
“We spend approximately $200K PER YEAR with a vendor to fight downcoding claims – and that’s after considerable expense to get it right in the first place. Unfortunately, it is necessary as without the ability to fight downcoding, WE WOULD LOSE MUCH MORE THAN THAT.”
This pattern reflects not just added administrative cost but also delayed revenue recovery, compounding the burden on hospitals. Source:
“Traditional Medicare includes additional payments for things like Graduate Medical Education. This additional Medicare payment supports the training of physicians. As MA plans increase, funding for Physician Residents decrease making these programs more and more of a burden.”
SPRINGDALE
AHA MEMBERS BY CITY, TYPE, SIZE, AND SERVICES
General Medical-Surgical Hospitals (43)
AHA MEMBERS BY CITY, TYPE, SIZE, AND SERVICES
Critical Access Hospitals (27)
Inpatient Psych Hospitals (12)
Veterans Affairs Hospitals (2)
AHA MEMBERS BY CITY, TYPE, SIZE, AND SERVICES
Inpatient Rehab Hospitals (7)
Rural Emergency Hospitals (5)
Special Focus Hospitals (4)
Long Term Care Hospitals (3)
Non-Hospital Facilities (3)
Out-of-State,
19TH MEDICAL GROUP
AHA MEMBERS BY CONTROL AND SYSTEM AFFILIATION
ADVANCED CARE HOSPITAL OF WHITE COUNTY
ARKANSAS CHILDREN'S HOSPITAL
ARKANSAS CHILDREN'S NORTHWEST
ARKANSAS HOSPICE
ARKANSAS METHODIST MEDICAL CENTER
ARKANSAS STATE HOSPITAL
ASHLEY COUNTY MEDICAL CENTER
BAPTIST HEALTH EXTENDED CARE HOSPITAL
BAPTIST HEALTH MEDICAL CENTER - ARKADELPHIA
BAPTIST HEALTH MEDICAL CENTER - HEBER SPRINGS
BAPTIST HEALTH MEDICAL CENTER-CONWAY
BAPTIST HEALTH MEDICAL CENTER-DREW COUNTY
BAPTIST HEALTH MEDICAL CENTER-HOT SPRING COUNTY
BAPTIST HEALTH MEDICAL CENTER-LITTLE ROCK
BAPTIST HEALTH MEDICAL CENTER-NORTH LITTLE ROCK
BAPTIST HEALTH MEDICAL CENTER-STUTTGART
BAPTIST HEALTH REHABILITATION INSTITUTE
BAPTIST HEALTH-FORT SMITH
BAPTIST HEALTH-VAN BUREN
BAPTIST MEMORIAL HOSPITAL-CRITTENDEN
BAXTER HEALTH
BAXTER HEALTH FULTON COUNTY HOSPITAL
BRADLEY COUNTY MEDICAL CENTER
CARTI
CENTRAL ARKANSAS VETERANS HEALTHCARE SYSTEM
CHAMBERS MEMORIAL HOSPITAL
CHI ST. VINCENT - INFIRMARY
CHI ST. VINCENT - MORRILTON
CHI ST. VINCENT - NORTH
CHI ST. VINCENT HOSPITAL HOT SPRINGS
CHI ST. VINCENT HOT SPRINGS REHABILITATION HOSPITAL
CHI ST. VINCENT SHERWOOD REHABILITATION HOSPITAL
CHICOT MEMORIAL MEDICAL CENTER
CHRISTUS ST. MICHAEL HEALTH SYSTEM
CONWAY BEHAVIORAL HEALTH
CONWAY REGIONAL HEALTH SYSTEM
CONWAY REGIONAL REHABILITATION HOSPITAL
CORNERSTONE SPECIALTY HOSPITALS - LITTLE ROCK
CROSSRIDGE COMMUNITY HOSPITAL
DALLAS COUNTY MEDICAL CENTER
DARDANELLE REGIONAL MEDICAL CENTER
DELTA MEMORIAL HOSPITAL
DEWITT HOSPITAL AND NURSING HOME
ENCOMPASS HEALTH REHABILITATION HOSPITAL, A PARTNER OF WASHINGTON REGIONAL
EUREKA SPRINGS HOSPITAL
FORREST CITY MEDICAL CENTER
GREAT RIVER MEDICAL CENTER
HELENA REGIONAL MEDICAL CENTER
HOWARD MEMORIAL HOSPITAL
IZARD REGIONAL HOSPITAL
JEFFERSON REGIONAL
JEFFERSON REGIONAL SPECIALTY HOSPITAL
LTCH
CHILDREN'S
CHILDREN'S
INPATIENT HOSPICE
RURAL/RRC
URBAN
RURAL/SCH
RURAL/MDH
URBAN
URBAN
RURAL/MDH
IRF
URBAN
URBAN
URBAN
RURAL/SCH/RRC
CAH
CAH
VETERANS AFFAIRS
RURAL/SCH
URBAN
CAH
URBAN
URBAN/RRC IRF IRF CAH
URBAN (TX) IP PSYCH
URBAN
RURAL/SCH/RRC REH CAH CAH
URBAN/SCH
U.S. DEPARTMENT OF DEFENSE
UNITY HEALTH
ARKANSAS CHILDREN'S
ARKANSAS CHILDREN'S
LOCAL BOARD
LOCAL BOARD
STATE
LOCAL BOARD
BAPTIST HEALTH
BAPTIST HEALTH
BAPTIST HEALTH
BAPTIST HEALTH
BAPTIST HEALTH
BAPTIST HEALTH
BAPTIST HEALTH
BAPTIST HEALTH
BAPTIST HEALTH
BAPTIST HEALTH
BAPTIST HEALTH
BAPTIST HEALTH
BAPTIST MEMORIAL HEALTHCARE CORP.
BAXTER HEALTH SYSTEM
BAXTER HEALTH SYSTEM
LOCAL BOARD
LOCAL BOARD
U.S. DEPARTMENT OF VETERANS AFFAIRS
LOCAL BOARD
COMMONSPIRIT HEALTH
COMMONSPIRIT HEALTH
COMMONSPIRIT HEALTH
COMMONSPIRIT HEALTH
ENCOMPASS HEALTH
ENCOMPASS HEALTH
LOCAL BOARD
CHRISTUS HEALTH
ACADIA HEALTHCARE
CONWAY REGIONAL HEALTH SYSTEM
CONWAY REGIONAL HEALTH SYSTEM
SCIONHEALTH
ST. BERNARDS HEALTHCARE COUNTY
CONWAY REGIONAL HEALTH SYSTEM
LOCAL BOARD
LOCAL BOARD
ENCOMPASS HEALTH
EUREKA SPRINGS HOSPITAL COMMISSION
QUORUM HEALTH
COUNTY
LOCAL BOARD
LOCAL BOARD
BOA VIDA HEALTHCARE
LOCAL BOARD
JEFFERSON REGIONAL
SEARCY
LITTLE ROCK
LITTLE ROCK
NORTH LITTLE ROCK
LITTLE ROCK
LITTLE ROCK
LITTLE ROCK
LITTLE ROCK
LITTLE ROCK
LITTLE ROCK
LITTLE ROCK
LITTLE ROCK
LITTLE ROCK
LITTLE ROCK
LITTLE ROCK
LITTLE ROCK
MEMPHIS, TN
MOUNTAIN HOME
MOUNTAIN HOME
LITTLE ROCK
LITTLE ROCK/NLR
CHICAGO, IL
CHICAGO, IL
CHICAGO, IL
CHICAGO, IL
BIRMINGHAM, AL
BIRMINGHAM, AL
IRVING, TX
FRANKLIN, TN
CONWAY
CONWAY
LOUISVILLE, KY
JONESBORO N/A
CONWAY
BIRMINGHAM, AL
EUREKA SPRINGS FRANKLIN, TN
CROWN POINT, IN
PINE BLUFF
JOHNSON REGIONAL MEDICAL CENTER
LAWRENCE MEMORIAL HOSPITAL
LEVI HOSPITAL
LITTLE RIVER MEDICAL CENTER
MAGNOLIA REGIONAL MEDICAL CENTER
MCGEHEE HOSPITAL
MENA REGIONAL MEDICAL CENTER
MERCY HOSPITAL BERRYVILLE
MERCY HOSPITAL BOONEVILLE
MERCY HOSPITAL FORT SMITH
MERCY HOSPITAL NORTHWEST ARKANSAS
MERCY HOSPITAL OZARK
MERCY HOSPITAL PARIS
MERCY HOSPITAL WALDRON
MERCY REHABILITATION HOSPITAL FORT SMITH
MERCY REHABILITATION SERVICES - NORTHWEST AR
METHODIST CHILDREN'S BEHAVIORAL HOSPITALJONESBORO
METHODIST CHILDREN'S BEHAVIORAL HOSPITALMAUMELLE
NATIONAL PARK MEDICAL CENTER
NEA BAPTIST MEMORIAL HOSPITAL
NORTH ARKANSAS REGIONAL MEDICAL CENTER
NORTHWEST HEALTH PHYSICIANS' SPECIALTY HOSPITAL
NORTHWEST MEDICAL CENTER - BENTONVILLE
NORTHWEST MEDICAL CENTER - SPRINGDALE
OUACHITA COUNTY MEDICAL CENTER
OZARK HEALTH
OZARKS COMMUNITY HOSPITAL
PERIMETER BEHAVIORAL HOSPITAL OF WEST MEMPHIS
PIGGOTT HEALTH SYSTEM
PINNACLE POINTE BEHAVIORAL HEALTHCARE SYSTEM
REGIONAL ONE HEALTH
RIVENDELL BEHAVIORAL HEALTH SERVICES
RIVERVIEW BEHAVIORAL HEALTH
SAINT MARY'S REGIONAL MEDICAL CENTER
SALINE MEMORIAL HOSPITAL
SEVIER COUNTY MEDICAL CENTER
SILOAM SPRINGS REGIONAL HOSPITAL
SOUTH ARKANSAS REGIONAL HOSPITAL
SOUTH MISSISSIPPI COUNTY REGIONAL MEDICAL CENTER
SOUTHWEST ARKANSAS REGIONAL MEDICAL CENTER
SPRINGWOODS BEHAVIORAL HEALTH HOSPITAL
ST. BERNARDS MEDICAL CENTER
ST. BERNARDS MEDICAL CENTER - FIVE RIVERS
ST. JUDE CHILDREN'S RESEARCH HOSPITAL
STONE COUNTY MEDICAL CENTER
THE BRIDGEWAY
UAMS MEDICAL CENTER
UNITY HEALTH - JACKSONVILLE
UNITY HEALTH - NEWPORT
UNITY HEALTH - SEARCY
VALLEY BEHAVIORAL HEALTH SYSTEM
VANTAGE POINT OF NWA
VETERANS HEALTH CARE SYSTEM OF THE OZARKS
WASHINGTON REGIONAL MEDICAL SYSTEM
WHITE RIVER HEALTH SYSTEM
WILLOW CREEK WOMEN'S HOSPITAL
RURAL/MDH
CAH
URBAN
CAH
RURAL/SCH
CAH
CAH
CAH
CAH
URBAN
URBAN
CAH
CAH
CAH
IRF
IRF
IP PSYCH
IP PSYCH
URBAN/RRC
RRC
RURAL/SCH/RRC
URBAN
URBAN
URBAN
RURAL/SCH
CAH
CAH
IP PSYCH
CAH
IP PSYCH
URBAN (TN)
IP PSYCH
IP PSYCH
RURAL/RRC
URBAN
RURAL
URBAN
RURAL/SCH
REH
RURAL
IP PSYCH
URBAN/RRC REH
CHILDREN'S
CAH
IP PSYCH
URBAN
URBAN
CAH
RURAL/SCH/RRC
IP PSYCH
IP PSYCH
VETERANS AFFAIRS
RURAL
RURAL/SCH/RRC
URBAN
LOCAL BOARD
ST. BERNARDS HEALTHCARE
LOCAL BOARD
LOCAL BOARD
LOCAL BOARD
LOCAL BOARD
CITY
MERCY
MERCY
MERCY
MERCY
MERCY
MERCY
MERCY
LIFEPOINT HEALTH
LIFEPOINT HEALTH
METHODIST FAMILY HEALTH
METHODIST FAMILY HEALTH
LIFEPOINT HEALTH
BAPTIST MEMORIAL HEALTHCARE CORP.
LOCAL BOARD
COMMUNITY HEALTH SYSTEMS
COMMUNITY HEALTH SYSTEMS
COMMUNITY HEALTH SYSTEMS
LOCAL BOARD
LOCAL BOARD
LOCAL BOARD
WOODRIDGE BEHAVIORAL CARE
CITY
UNIVERSAL HEALTH SERVICES
REGIONAL ONE HEALTH
UNIVERSAL HEALTH SERVICES
ACADIA HEALTHCARE
LIFEPOINT HEALTH
LIFEPOINT HEALTH
LOCAL BOARD
COMMUNITY HEALTH SYSTEMS
LOCAL BOARD
COUNTY
PAFFORD MEDICAL SERVICES
UNIVERSAL HEALTH SERVICES
ST. BERNARDS HEALTHCARE
ST. BERNARDS HEALTHCARE
WHITE RIVER HEALTH SYSTEM
UNIVERSAL HEALTH SERVICES
STATE
UNITY HEALTH
UNITY HEALTH
UNITY HEALTH
ACADIA HEALTHCARE
ACADIA HEALTHCARE
U.S. DEPARTMENT OF VETERANS AFFAIRS
LOCAL BOARD
WHITE RIVER HEALTH SYSTEM
COMMUNITY HEALTH SYSTEMS
JONESBORO
CHESTERFIELD, MO
CHESTERFIELD, MO
CHESTERFIELD, MO
CHESTERFIELD, MO
CHESTERFIELD, MO
CHESTERFIELD, MO
CHESTERFIELD, MO
BRENTWOOD, TN
BRENTWOOD, TN
LITTLE ROCK
LITTLE ROCK
BRENTWOOD, TN MEMPHIS, TN
FRANKLIN, TN
FRANKLIN, TN
FRANKLIN, TN
JACKSON, TN
KING OF PRUSSIA, PA MEMPHIS, TN
KING OF PRUSSIA, PA
FRANKLIN, TN
BRENTWOOD, TN
BRENTWOOD, TN
FRANKLIN, TN
HOPE
KING OF PRUSSIA, PA
JONESBORO
JONESBORO
BATESVILLE
KING OF PRUSSIA, PA
SEARCY
SEARCY
SEARCY
FRANKLIN, TN
FRANKLIN, TN
BATESVILLE
FRANKLIN, TN
ARKANSAS HOSPITALS
RECEIVING LOCAL TAX SUPPORT, 2025
INDICATOR
ASHLEY COUNTY MEDICAL CENTER
BAPTIST HEALTH MEDICAL CENTER-DREW COUNTY
BAPTIST HEALTH MEDICAL CENTER-HOT SPRING COUNTY
BAPTIST HEALTH MEDICAL CENTER-STUTTGART
BAXTER HEALTH FULTON COUNTY HOSPITAL
BRADLEY COUNTY MEDICAL CENTER
CHI ST. VINCENT - MORRILTON
CHICOT MEMORIAL MEDICAL CENTER
CROSSRIDGE COMMUNITY HOSPITAL
DALLAS COUNTY MEDICAL CENTER
DELTA MEMORIAL HOSPITAL
DEWITT HOSPITAL AND NURSING HOME
GREAT RIVER MEDICAL CENTER
JOHNSON REGIONAL MEDICAL CENTER
LAWRENCE
LITTLE
HOSPITAL
MERCY HOSPITAL BOONEVILLE
MERCY HOSPITAL OZARK
MERCY HOSPITAL PARIS
OUACHITA
OZARK
N/A=Information not available
Source: Self-reported information provided to the Arkansas Hospital Association
$649,000 $670,000 $1,600,000 $2,300,000 $600,000 $1,200,000 $1,000,000 $1,100,000 $2,500,000 $840,000 $1,000,000 $850,000 $2,439,800 $65,000 $1,900,000 $834,000 $2,600,000 $540,000 $600,000 $360,000 $350,000 N/A N/A $150,000 $500,000 $829,300 $800,000
AHA MEMBER ORGANIZATIONS
BY CONGRESSIONAL
1st Congressional District
Arkansas Methodist Medical Center
Baptist Health Medical Center-Stuttgart
Baptist Memorial Hospital-Crittenden
Baxter Health
Baxter Health Fulton County Hospital
Chicot Memorial Medical Center
CrossRidge Community Hospital
Delta Memorial Hospital
DeWitt Hospital & Nursing Home
Forrest City Medical Center
Great River Medical Center
Helena Regional Medical Center
Izard Regional Hospital
Lawrence Memorial Hospital
Methodist Children’s Behavioral Hospital-Jonesboro
McGehee Hospital
NEA Baptist Memorial Hospital
North Arkansas Regional Medical Center
Perimeter Behavioral Health of West Memphis
Piggott Community Hospital
SMC Regional Medical Center
St. Bernards Five Rivers
St. Bernards Medical Center
Stone County Medical Center
Unity Health – Newport
White River Health System
Total = 26
2nd Congressional District
19th Medical Group
Advanced Care Hospital of White County
Arkansas Children’s Hospital
Arkansas Hospice
Arkansas State Hospital
Baptist Health Extended Care Hospital
Baptist Health Medical Center-Conway
Baptist Health Medical Center-Heber Springs
Baptist Health Medical Center-Little Rock
Baptist Health Medical Center-North Little Rock
Baptist Health Rehabilitation Institute
CARTI
Central Arkansas Veterans Healthcare System
CHI St. Vincent Infirmary
CHI St. Vincent Morrilton
CHI St. Vincent North
CHI St. Vincent Sherwood Rehabilitation Hospital, A Partner of Encompass Health
Conway Behavioral Health
Conway Regional Health System
Conway Regional Rehabilitation Hospital
Cornerstone Specialty Hospitals Little Rock
Methodist Children’s Behavioral Hospital-Maumelle
Ozark Health Medical Center
Pinnacle Pointe Behavioral Healthcare System
Rivendell Behavioral Health Services
Saline Memorial Hospital
The BridgeWay
UAMS Medical Center
Unity Health – Jacksonville
Unity Health – Searcy
Total = 30
3
DISTRICT

1
2
4
3rd Congressional District
Arkansas Children’s Northwest
Baptist Health-Fort Smith
Baptist Health-Van Buren
Encompass Health Rehabilitation Hospital, A Partner of Washington Regional
Eureka Springs Hospital
Mercy Hospital Berryville
Mercy Hospital Fort Smith
Mercy Hospital Northwest Arkansas
Mercy Rehabilitation Hospital Fort Smith
Mercy Rehabilitation Services-Northwest Arkansas
Northwest Health Physicians’ Specialty Hospital
Northwest Medical Center Bentonville
Northwest Medical Center Springdale
Ozarks Community Hospital
Siloam Springs Regional Hospital
Springwoods Behavioral Health Hospital
Valley Behavioral Health System
Vantage Point of NWA
Veterans Health Care System of the Ozarks
Washington Regional Medical System
Willow Creek Women’s Hospital
Total = 21
Additional AHA Member
Hospitals Include:
CHRISTUS St. Michael Health System, Texarkana, TX
Regional One Health, Memphis, TN
St. Judes Children’s Research Hospital, Memphis, TN
4th Congressional District
Ashley County Medical Center
Baptist Health Medical Center-Arkadelphia
Baptist Health Medical Center-Drew County
Baptist Health Medical Center-Hot Spring County
Bradley County Medical Center
Chambers Memorial Hospital
CHI St. Vincent Hot Springs
CHI St. Vincent Hot Springs Rehab Hospital, A Partner of Encompass Health
Dallas County Medical Center
Dardanelle Regional Medical Center
Howard Memorial Hospital
Jefferson Regional
Jefferson Regional Specialty Hospital
Johnson Regional Medical Center
Levi Hospital
Little River Medical Center
Magnolia Regional Medical Center
Mena Regional Health System
Mercy Hospital Booneville
Mercy Hospital Ozark
Mercy Hospital Paris
Mercy Hospital Waldron
National Park Medical Center
Ouachita County Medical Center
Riverview Behavioral Health
Saint Mary’s Regional Medical Center
Sevier County Medical Center
South Arkansas Regional Hospital
Southwest Arkansas Regional Medical Center
Total = 29
ECONOMIC IMPACT OF ARKANSAS HOSPITALS, 2024
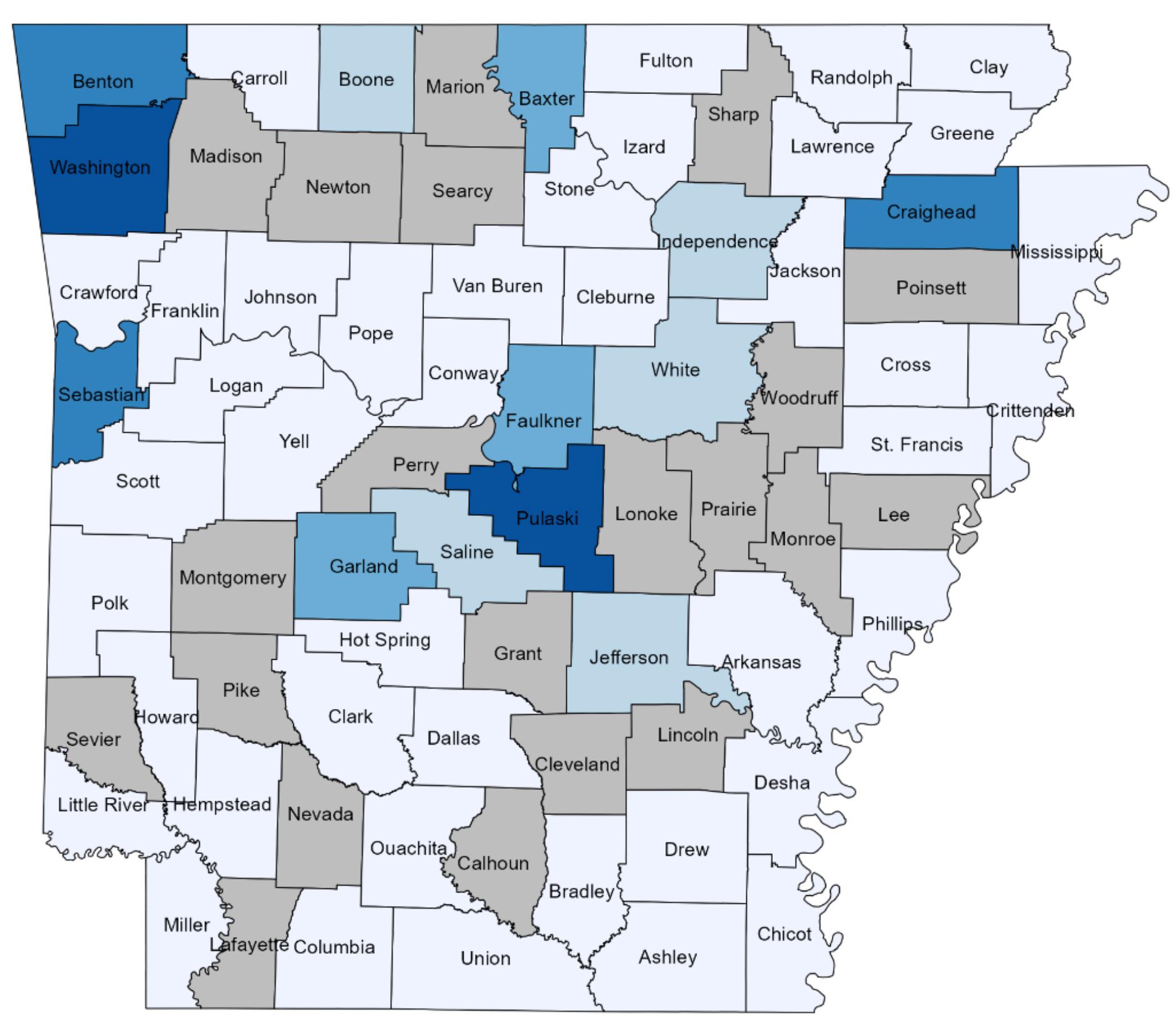
Arkansas hospitals are economic powerhouses for our state. In 2022, hospitals directly employed 48,200 individuals with a total payroll of $4,335,511,000. Those payroll dollars, when spent on groceries, housing, and other goods and services, generated an additional $8,086,595,000 in economic activity and supported 46,200 more jobs across Arkansas. Hospitals also purchased $4,968,149,000 worth of supplies, utilities, and services, which rippled out to generate another $9,266,591,000 in the wider economy. Capital investments — $371,201,000 in building and equipment — created roughly $692,363,000 of economic impact. Altogether, Arkansas hospitals supported or created 94,400 jobs and delivered a total economic impact of $18,045,549,000.
Beyond their economic footprint, hospitals deliver lifesaving and lifeenhancing services around the clock. In 2023 alone, they cared for over 350,000 admitted patients and managed more than 6.5 million outpatient visits including 1.4 million visits to emergency departments. Surgeons in Arkansas hospitals performed over 300,000 inpatient and outpatient procedures, and 31,629 babies were welcomed into the world by our hospital staff. More than $690 million in charity care ensured that no one was turned away for inability to pay — all while hospitals provided high quality, efficient care, served as safe harbors in emergencies, offered end-of-life comfort, educated communities on disease prevention, and fought to retain critical health services in their regions.
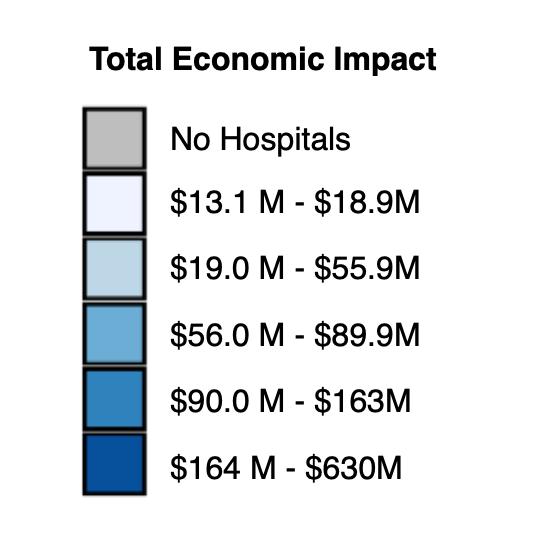
In times of crisis, hospitals stand ready as pillars of community resilience. During the COVID-19 public health emergency, they provided care to tens of thousands of Arkansans, established comprehensive testing, treatment, and vaccination infrastructure, rolled out novel telemedicine programs, and expanded ICU capacity with negativepressure beds. In March 2023, when tornadoes tore through Little Rock’s Rodney Parham corridor, hospital teams and first responders treated at least 40 storm-injured patients. And through the statewide trauma system — now comprising 57 designated trauma centers (six of them Level I) — Arkansans in critical condition are expertly triaged and transported, cutting preventable deaths by nearly half and saving more than $180 million each year.
Source:
KEY FINANCIAL
ARKANSAS AND SURROUNDING STATES, 2023
$5,536,649,596,244
Texas
Tennessee
$532,708,572,869
$113,145,100,826
$4,206,366,870,821.00 $1,330,282,725,423.00 $1,381,871,477,674.00 441,222,967 ($51,588,752,251) ($116.92) -3.88%
$429,748,121,299
$88,509,896,991
$102,960,451,570 $99,642,335,774
$121,935,995,590 $70,347,243,339 4.84% $35,821,470,147 $106,168,713,486 7.13%
Louisiana
Arkansas
$107,589,227,887 $78,498,893,662 $29,090,334,225 $30,289,195,038 10,805,929 ($1,198,860,813) ($110.94) -4.12% $2,183,310,797 $984,449,984 3.15%
$79,265,681,270
$36,948,799,383
$59,755,593,190 $19,510,088,080
$27,269,530,971 $9,679,268,412 $10,180,413,147 4,415,436 ($501,144,735) ($113.50)
Hospitals charged this amount for the inpatient and outpatient care they provided in 2023: But patients and payer groups didn't pay the full amount of billed charges for various reasons. Government programs like Medicare and Medicaid, workers' comp programs, and others never pay the full hospital bill. Managed care plans and other insurers typically pay discounted amounts only, and individual patients often can't afford to pay some or any of the out-of-pocket costs related to their hospital bills. For those reasons, hospitals had to forfeit this much of their billed charges:
As a result, actual payments to hospitals were:
At the same time, hospitals spent this much providing patient care services… …to patients needing care for this many adjusted patient days while being served. So the revenue excess (loss) was: In other words, hospitals made (or lost) this much on each of the equivalent days of care they provided to intpatients and outpatients: Yielding a "patient service" margin of:
In addition, hospitals also received revenues from normal, day-today operations from services other than health care provided to patients, such as space rental, cafeteria and gift shop sales, and operating gains:
Which raised total operating income to:
As a result, the "operating margin" rose to:
Hospitals also collected other types of revenue from sources including contributions, tax appropriations, and investments. Those amounted to: That resulted in total funds available to reinvest in new equipment, update facilities, expand programs and repay debt equaling: For a return on investment totaling
Source: American Hospital Association, Hospital Statistics 2023
STATEWIDE HOSPITAL
AND UTILIZATION INDICATORS, 2019 - 2023
INDICATOR
BEDS AVAILABLE
ADMISSIONS
PATIENT DAYS
AVERAGE LENGTH OF STAY
NON-EMERGENCY OP VISITS
OUTPATIENT VISITS
NON-EMERGENCY AS A % OF TOTAL OP VISITS
ADJUSTED PATIENT DAYS
OCCUPANCY RATE
INPATIENT SURGERIES
OUTPATIENT SURGERIES
TOTAL SURGERIES
OUTPATIENT AS % OF TOTAL SURGERIES
TOTAL FULL-TIME EQUIVALENT EMPLOYEES
FULL-TIME EQUIVALENT EMPLOYEES PER ADJUSTED
OCCUPIED BED
GROSS REVENUE, INPATIENT
GROSS REVENUE, OUTPATIENT
GROSS PATIENT REVENUE
BAD DEBTS
CHARITY
MEDICARE, MEDICAID, & OTHER PAYER WRITEOFFS
TOTAL DEDUCTIONS
NET PATIENT REVENUE
OTHER OPERATING REVENUE
NONOPERATING REVENUE
TOTAL NET REVENUE
PAYROLL EXPENSE
TOTAL EXPENSE
PATIENT REVENUE MARGIN
TOTAL MARGIN
CHARGE PER ADJUSTED INPATIENT DAY
PAYMENT PER ADJUSTED INPATIENT DAY
EXPENSE PER ADJUSTED INPATIENT DAY
PAYROLL PER ADJUSTED INPATIENT DAY
PAYROLL AS % OF TOTAL EXPENSE
BAD DEBT AND CHARITY AS % OF TOTAL CHARGE
TOTAL DEDUCTIONS AS % OF TOTAL CHARGE
OUTPATIENT REVENUE AS % TOTAL PATIENT REVENUE
ADMISSIONS PER BED
PATIENT DAYS PER 1,000 POPULATION
ADMISSIONS PER 1,000 POPULATION
POPULATION (000'S)
$14,814,502,613
$17,025,641,576
$31,840,144,189
$509,174,368
$442,315,671
$22,702,507,161
$23,653,997,200
$8,186,146,989
$433,117,737
$145,788,360
$8,765,053,086
$3,040,326,208
$8,049,927,966
$7,445.97
$1,914.37
$1,882.51
$14,965,703,755
$16,733,703,930
$31,699,407,685
$503,958,456
$499,580,152
$22,706,699,474
$23,710,238,082
$7,989,169,603
$760,697,334
$164,859,866
$8,914,726,803
$3,122,035,492
$8,206,104,259 -2.72%
$7,519.32
$1,895.09
$1,946.54
$17,185,062,486
$18,570,833,303
$35,755,895,789
$512,576,407
$574,072,837
$25,738,880,672
$26,825,529,916
$8,930,365,873
$919,369,130
$246,467,868
$10,096,202,871
$3,542,564,965
$9,161,715,585 -2.59% 9.26% $8,160.14 $2,038.07
$16,766,340,537 $19,010,965,594 $35,777,306,131 $468,830,369 $466,432,386 $25,758,657,460 $26,693,920,215 $9,083,385,916 $1,143,477,147 ($5,690,890) $10,221,172,173 3,844,177,083 $10,093,617,469 -11.12% 1.25% $8,033.36 $2,039.56 $2,266.40 $863.16
6,519,716 78.05%
$17,441,647,083 $19,507,152,300 $36,948,799,383 $520,657,399 $693,849,202 $26,055,024,370 $27,269,530,971 $9,679,268,412 $791,778,997 $230,969,958 $10,702,017,367 $3,689,381,915 $10,180,413,147
COMPARATIVE FINANCIAL INDICATORS: U.S. COMMUNITY HOSPITALS
DISTRICT
CALIFORNIA ALASKA
FLORIDA
NEVADA NEW
DISTRICT
SOUTH
ALABAMA
HAWAII
LOUISIANA
MAINE
WASHINGTON
COLORADO
IDAHO
MINNESOTA
DELAWARE
NORTH DAKOTA
NEBRASKA
OREGON
HAWAII
MARYLAND
NEW
MASSACHUSETTS INDIANA
CONNECTICUT
NEW YORK
MAINE
CALIFORNIA
WASHINGTON
MASSACHUSETTS
MINNESOTA
IDAHO
OREGON
NORTH DAKOTA
DELAWARE
COLORADO
MARYLAND
UTAH
NEBRASKA
HAWAII
CONNECTICUT
NEW HAMPSHIRE
NEW JERSEY
MONTANA
PENNSYLVANIA
VERMONT
OHIO
SOUTH DAKOTA
U.S.
VIRGINIA
WYOMING
NEW MEXICO
WISCONSIN
TEXAS
NORTH CAROLINA
ILLINOIS
MISSOURI
MICHIGAN
ARIZONA
GEORGIA
RHODE
WEST
KENTUCKY
WSC
TENNESSEE
LOUISIANA
IOWA
FLORIDA
NEVADA
SOUTH
OKLAHOMA
DISTRICT
VIRGINIA
ALABAMA
MISSISSIPPI
NORTH CAROLINA
GEORGIA
SOUTH CAROLINA
OKLAHOMA
NEBRASKA
WISCONSIN
WYOMING
NEW JERSEY
DELAWARE
VERMONT
ILLINOIS
LOUISIANA
IDAHO
NORTH DAKOTA
CALIFORNIA
SOUTH DAKOTA
MONTANA
NEW HAMPSHIRE
RHODE ISLAND
MISSOURI
MASSACHUSETTS
ARKANSAS
KANSAS
WEST VIRGINIA
IOWA
PENNSYLVANIA
ALASKA
NEW MEXICO
WASHINGTON
NEW YORK
HAWAII
MARYLAND
CONNECTICUT
MICHIGAN
MINNESOTA
OREGON
MAINE
TENNESSEE
PROGRAMS
COSTS,
Source: Arkansas Department of Health, Hospital Discharge Program, 2023
HOSPITAL UNCOMPENSATED CARE COSTS, 2019-2023
REVENUES (BILLED
$31,840,144,189
$31,699,407,685
$35,755,895,789
$35,777,306,131
$36,948,799,383 16.04%
UNCOLLECTED AMOUNTS DUE
$23,653,997,200
$23,710,238,082
$26,825,529,916
$26,693,920,215
$27,269,530,971
REVENUES (AMOUNT COLLECTED)
$8,186,146,989
$7,989,169,603
$8,930,365,873
$9,083,385,916
$ 9,679,268,412
$433,117,737
$760,697,334
$919,369,130
$1,143,477,147
$ 791,778,997
$32,273,261,926
$32,460,105,019
$36,675,264,919
$36,920,783,278
$37,971,548,338
$8,049,927,966
$8,206,104,259
$9,161,715,585
$10,093,617,469
$ 10,180,413,147 26.47%
$509,174,368
$503,958,456
$512,576,407
$468,830,369
$520,657,3992.26%
$442,315,671
$499,580,152
$574,072,837
$466,432,386
$693,849,202
$951,490,039
$1,003,538,608
$1,086,649,244
$935,262,755
$1,214,506,601 27.64% TOTAL OPERATING COSTS
$222,318,771
$238,120,014
$256,264,830.53
$243,811,319.81 $334,630,060 50.52%
Source: American Hospital Association, Hospital Statistics 2022
TOP 20 INPATIENT DRGS, 2023
DIAGNOSIS-RELATED GROUP
885 - PSYCHOSES
871 - SEPTICEMIA W/O MV 96+ HOURS W MCC
795 - NORMAL NEWBORN
807 - VAGINAL DELIVERY WITHOUT STERILIZATION OR D&C W/O CC/MCC
794 - NEONATE W OTHER SIGNIFICANT PROBLEMS
291 - HEART FAILURE & SHOCK W MCC
189 - PULMONARY EDEMA & RESPIRATORY FAILURE
788 - CESAREAN SECTION W/O STERILIZATION W/O CC/MCC
193 - SIMPLE PNEUMONIA & PLEURISY W MCC
897 - ALCOHOL/DRUG ABUSE/DEPENDENCE W/O REHABILITATION THERAPY W/O MCC
177 - RESPIRATORY INFECTIONS & INFLAMMATIONS W MCC
872 - SEPTICEMIA W/O MV 96+ HOURS W/O MCC
392 - ESOPHAGITIS, GASTROENT & MISC DIGEST DISORDERS W/O MCC
057 - DEGENERATIVE NERVOUS SYSTEM DISORDERS W/O MCC
806 - VAGINAL DELIVERY WITHOUT STERILIZATION OR D&C W CC
641 - NUTRITIONAL & MISC METABOLIC DISORDERS W/O MCC
690 - KIDNEY & URINARY TRACT INFECTIONS W/O MCC
683 - RENAL FAILURE W CC
881 - DEPRESSIVE NEUROSES
682 - RENAL FAILURE W MCC
CHARGES
$758,896,646.34
$960,189,031.84
$113,820,083.66
$264,820,333.76
$102,242,505.41
$311,998,574.75
$239,047,152.90
$141,088,591.82
$195,790,717.14
$89,202,423.33
$212,271,590.30
$132,070,121.21
$94,096,693.01
$161,500,948.04
$61,508,448.18
$67,652,433.87
$73,722,108.95
$83,659,778.96
$59,375,728.70
$125,477,737.37
$21,587.16
$55,886.68
HOSPITAL ACCESS BY COUNTY
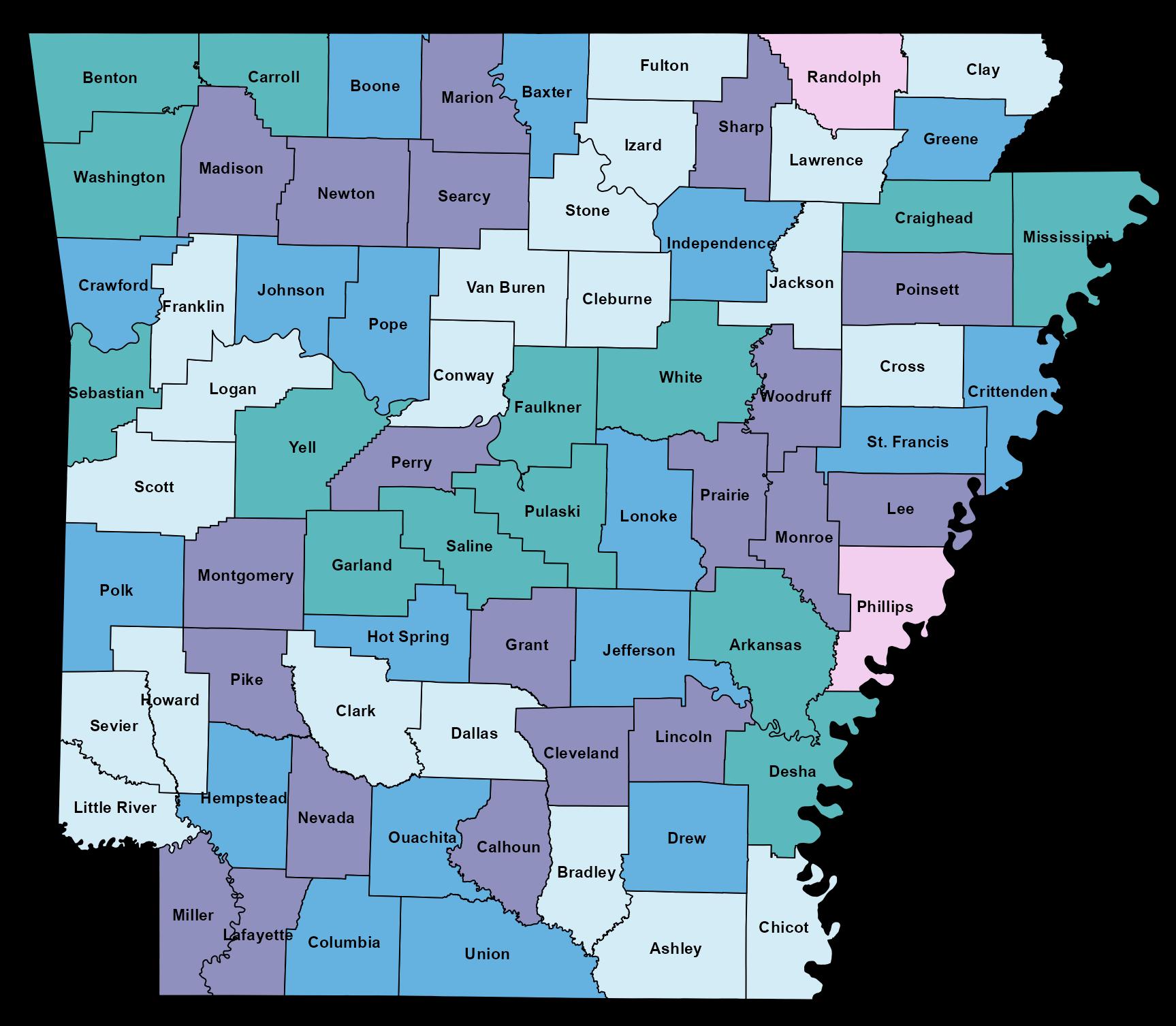
HOSPITAL TYPE
Multiple
Single Acute Only
Single CAH Only
None
Single REH Only
Arkansas Hospitals, 2025
The Power of Community:
Unity Health’s LaDonna Johnston Leads with a Servant’s Heart
By Becca Bona

While the saying goes, “Home is where the heart is,” for Unity Health President and CEO LaDonna Johnston, home is more than a hometown. Her roots are deep in the small town of Bald Knob in White County, where she was raised. Home is also Unity Health, where she has served for more than 35 years. “I believe it is very important to take care of those around you and provide quality health care in the communities we serve,” said Johnston.
FOLLOWING A PATH OF FAITH
From a young age, Johnston did not have plans to enter health care and instead wanted to become a veterinarian. Johnston laughed and said, “My dad said no and told me I would bring home too many animals.” She credits her father with encouraging her to explore other fields of study. She volunteered for two summers during high school at White County Memorial Hospital, which is now Unity Health – White County Medical Center. This, in turn, led her to Harding University, where she ultimately enrolled in the nursing program and received her Bachelor of Science in Nursing.
She knew that if she followed her faith and intuition, she’d find the right path in life, even beyond her job. “I married my high school sweetheart, and we built our home in what was originally a bean field across from my parents’ house,” she said.
On the career front, her first employed position at the hospital was as a CCU monitor tech in 1987. “I felt very compelled to stay here and make as big of an impact as I could,” she said. The hospital’s mission aligns with her values of providing compassionate care in the communities of White County and surrounding areas. She continued her education and pursued her Master’s in Nursing from the University of Arkansas for Medical Sciences. Even though she wasn’t vying for a leadership position, opportunities came her way.
LEADING WITH AN OPEN HEART AND TURNING CHALLENGES INTO OPPORTUNITIES
Johnston fosters a strong sense of unity through her leadership. During her career, she has seen the organization purchase nearby facilities and expand its footprint. Today, Unity Health is a regional health care system consisting of four hospitals, numerous outpatient clinics, and an accredited graduate medical education program offering emergency medicine, family medicine, internal medicine, and psychiatry residency
I felt very compelled to stay here and make as much of an impact as I could.
programs. In her current role as President and CEO, Johnston is focused on adding more specialists, expanding key service lines, and continuing to evaluate growth opportunities. She is passionate about expanding access to health care. Johnston and her team work to address access challenges by evaluating partnerships and exploring opportunities for specialists to provide care in outlying communities. Beyond
We are going to do everything we can to bring the best care to our patients.

the access issues, obtaining an adequate workforce continues to be a challenge. Unity Health is addressing these concerns by building partnerships with local schools and offering training opportunities to create a culture where people want to stay and grow their careers. She and her team strive to create an environment that attracts and retains an excellent staff. “We’re embarking on changing our culture here,” said Johnston. “We’re like family, and we want to lead with a servant heart and be the leaders we need to be.”
Another critical area of work is collaborating with community partners across the system to address health care concerns. One recent example includes partnering with United Way to provide more information about mental health. Psychiatrists from Unity Health joined a United Way event to talk about mental health concerns and what help can look like. “We often partner with different organizations and leaders to help where we can,” said Johnston.
Unity Health also partners with other local health care entities via their Community Connect meetings. Unity is an ecosystem in and of itself but is part of a larger system — the health care landscape across the state and region. “A nursing home can’t run

Continued on page 58
Unity Health President and CEO LaDonna Johnston, right, collaborates with a team member. Johnston leads the regional health care system with a focus on expanding access and fostering unity.
(Photos provided)
Q& A LEADERSHIP WITH LADONNA JOHNSTON
What’s on your music playlist?
I love country…old country. George Jones, Merle Haggard, Loretta Lynn, Tammy Wynette, old trangy country.
What is the best advice you were ever given? Life is not fair.
Do you have a favorite movie? Why do you like it?
Not big on movies
Who is someone you greatly admire, and why?
My mother. She lost her mother at a very early age, had to take care of her sibling’s and then God love her, she married my father. She later had a perfect daughter though.
What would you be doing if you weren’t in health care?
I would love to be a vet and take care of animals.
What is something people don’t know about you?
Grew up on a farm and learned to drive a tractor right before I turned 9.
What do you like to do in your down time?

Love to fish. My husband and our dog, Cotton, fish as often as we can.
What’s on your desk right now?
Coffee, some chocolate and a lot of post its.
What are you reading?
I love to read Amish books. Reading of their hard work and faith is inspiring to me.
Where would you travel, if you could go anywhere? I would go to any beach with white sand and water.
What’s a life-changing lesson COVID-19 has taught you?
The unimaginable can happen and we can withstand it. That is a good answer. Life can be over in the blink of an eye. Love hard

When she's not leading Unity Health, Johnston enjoys fishing with her husband and their white Labrador, Cotton. Whether with family or at a work function, Johnston strives to build connections and fosters a sense of community.
without us,” she said, “but we also can’t run without nursing homes. It must be a collaboration.” Community Connect meetings provide an opportunity to check in and ensure that each partner is communicating and collaborating in a way that is best for the patient.
Johnston also stays abreast of upcoming legislation that might lead to
new regulatory changes in health care, thanks to a standing Monday morning meeting led by her local Chamber of Commerce when the legislature is in session. “Representatives are there, and we discuss what is going on and what bills are important to our community,” she said. “That’s a great partnership”.
PROUDLY SERVING
Arkansas
EYES ON THE FUTURE: VISION AND GOALS
Johnston is proud of the strides Unity has made and continues to make toward excellence. In November 2024, Unity’s Cardiology program received the American College of Cardiology’s NCDR Chest Pain - MI Registry Platinum Performance Achievement Award. The work towards that designation involved system-wide collaboration and is something Johnson is proud of being able to offer patients. “That is something we want to be known for because we are in rural communities, and being able to provide life-saving health care to our patients is our goal,” she said.
Unity Health continues to offer new service lines with the recent addition of a Neonatal Intensive Care Unit (NICU). Newborns can receive care close to home from a team of expert providers. This specialty is the first of its kind in Searcy and the surrounding communities, providing care for Unity Health’s tiniest patients. Additionally, Unity will add two new specialties this summer: gastroenterology and interventional pain management.
In the meantime, Johnston is focused on Unity Health’s overall strategic plan. “We are going to do what we can to bring the best care to our patients,” she said. Every three years, the system creates a new community report that offers new initiatives stemming from community data and centered on Unity’s four service links: kindness, excellence, expertise, and stewardship.

Outside of work, Johnston prioritizes living out her faith and is active in her church. She is also very family oriented. “I love, love, love my kids,” she said. Her two children are now grown and married, and she has two grandchildren. “When you empty the nest, you find something else that requires your attention. We now have a white lab named Cotton,” she said laughing, “and he tells us what to do. My husband and I love to fish, and Cotton tags along. Anyone that knows me well will tell you that If I’m off work, there is likely some fishing involved.”


Improving Financial Capacity Through Payer Accountability
By Travis Gentry, CEO, Hyve Health
For hospitals, negative payer behavior often involves delayed payments, claim denials, or underpayments that strain operations and patient care, forcing hospitals to absorb financial losses or pass costs onto patients. This behavior disrupts hospital revenue streams, hinders their ability to maintain adequate staffing and equipment, and can lead to reduced access to care. Additionally, the administrative burden of negotiating and appealing claims consumes valuable time and resources, diverting attention from patient-centered care and eroding trust in the health care system.
Peter Drucker once said, “What gets measured, gets managed.” In health care today, data is a primary reason why payers are winning — and providers are falling behind. The health insurance industry is built on actuarial science and utilization modeling. Payers excel at measuring and managing data; providers must catch up.
Every claim a hospital submits is ultimately aggregated and used by payers — often against the hospitals themselves. These insights, gathered across entire states, are used to drive down reimbursement and increase denials.
It’s time for hospitals to move from defense to offense by leveraging anonymous remittance data to hold payers accountable. That’s why the Arkansas Hospital Association has partnered with Hyve Health to provide all members with free access to the Vitality Payer Scorecard (VPS).
VPS offers hospitals a powerful way to anonymously benchmark their payer experience against their peers — within their state and nationally.
For example, hospitals can:
•Identify outlier trends such as higher denial rates or slower payment cycles
•Break down payer behavior by Financial Class, Payer, Patient Type, and Specialty
•Drill down into combinations like United Healthcare, Medicare Advantage, IP Cardiovascular to see exactly where payer behavior diverges from the norm
A REAL EXAMPLE:
By leveraging VPS, a hospital discovered the following when comparing its UHC Medicare Advantage (UHC MA) performance against Medicare FFS:
•UHC MA claims had a 400% higher denial rate for inpatient cardiac cases
•Documentation denials were 40% vs a state average of 26%
•Medical necessity denials were 50% vs 15% statewide
Meanwhile, the same hospital was outperforming state averages on payment speed and First Pass Yield — yet still receiving lower reimbursement and more denials.
VPS doesn’t just confirm what hospitals already know — it adds critical statewide and national context. It empowers hospitals to answer: “Is this a me problem … or a we problem?”
As Drucker noted, “What gets measured, gets managed.” But we must also seek to manage what we previously couldn’t measure. Data drives us. Unity powers us. There is strength in numbers — and when hospitals unite around shared data, the entire provider community benefits.


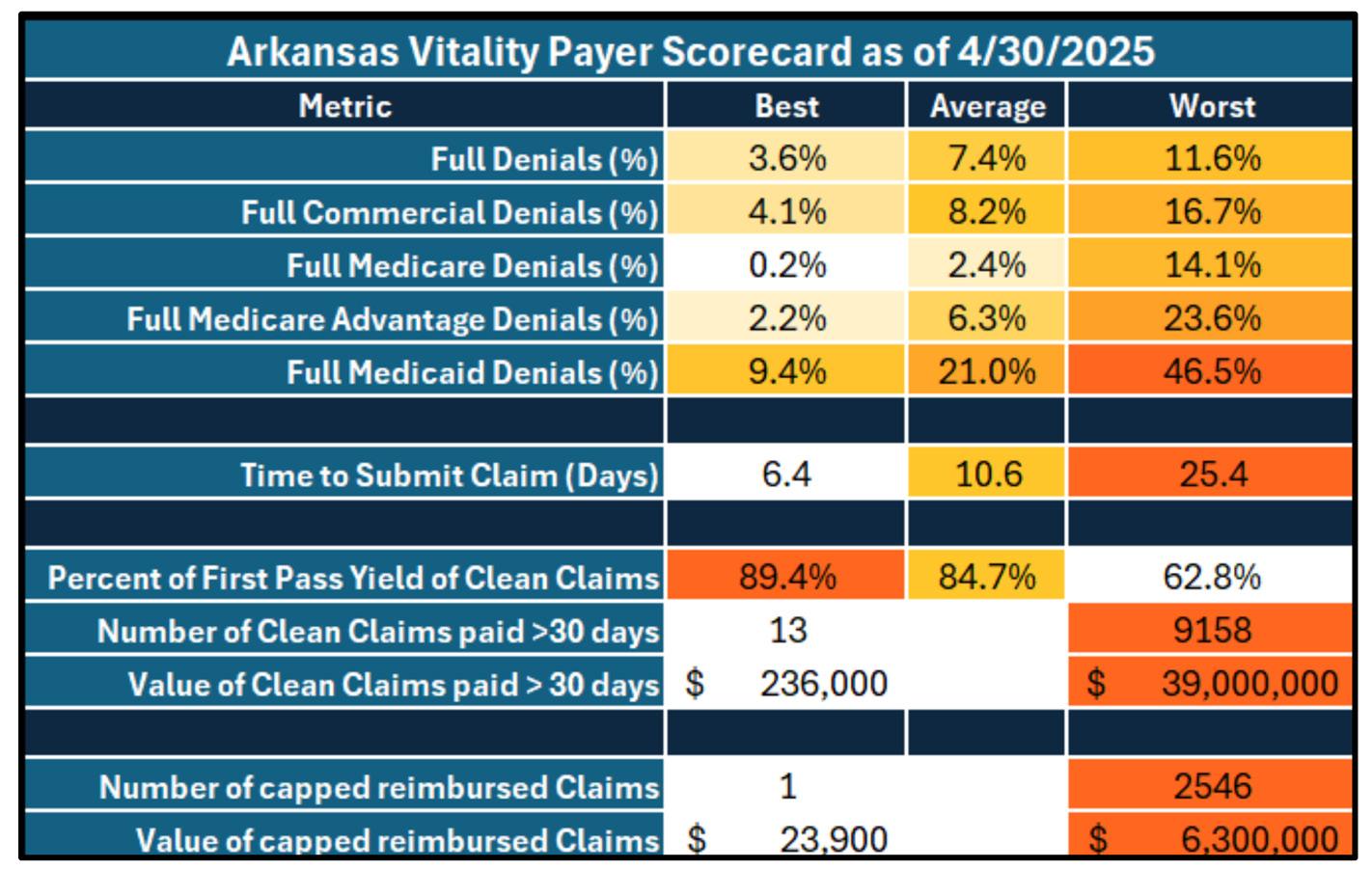
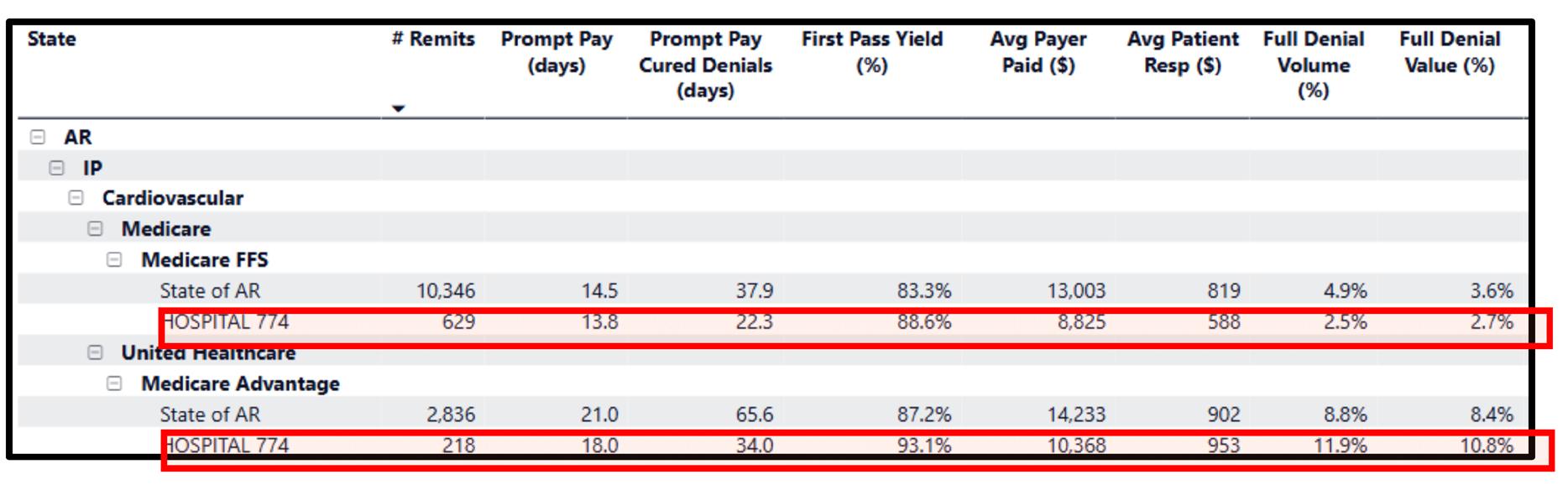
VPS provides data offering statewide and national context, empowering hospitals to shape their decision-making.
A snapshot of the Arkansas Vitality Payer Scorecard. (Photos provided)
UAMS and University of Arkansas Hope-Texarkana Partner to Offer College Credit to Doula Trainees
Participants in the University of Arkansas for Medical Sciences (UAMS) Institute for Community Health Innovation’s doula training program are now able to receive college credit, thanks to a continued partnership between UAMS and the University of Arkansas Hope-Texarkana (UAHT).
By coupling this program with the state’s passage of the Healthy Moms, Healthy Babies Act earlier this year, officials at the institute say they are proud to work with other state leaders to advance the role of doulas in the state. The act, signed into law by Gov. Sarah Sanders in February, also establishes presumptive Medicaid eligibility for pregnant women.
In addition to training participants to navigate selfemployment amid the Medicaid changes, trainees can now receive up to seven hours of college credit through UA HopeTexarkana.
“Arkansas’s approval of Medicaid reimbursement for doula services earlier this year marked a powerful step toward recognizing the essential role doulas play in maternal and infant health,” said Krista Langston, executive director of community programs at the institute. “Pairing that progress with college credit not only elevates the profession but also validates the expertise and dedication doulas bring to the health care system.”
The institute launched its enhanced doula training program earlier this year, enrolling 60 trainees from across the state who will receive doula certification upon program completion later this year. The training program includes 29 hours of training with Birthing Beyond, LLC, an approved DONA International certification program; 40 hours of training with Ujima Maternity Network of Conway; 45 hours of Certified Breastfeeding Counselor training; and six months of mentorship.
“This program has completely transformed my understanding of childbirth and my ability to help families in my community,” said Robin Mero Butler, a participant in the doula training program. “UAMS does everything it can to help you build a new career from the ground up: the business aspects, how to thoroughly and confidently prepare a pregnant woman for birth,

how to conduct yourself in various birth settings, and supporting the new family postpartum. I feel privileged to have participated and hope many others join the program so that all Arkansas families have supported births with the best outcomes.”
Doulas are trained birth coaches who provide continuous emotional and physical support throughout labor and delivery. Research shows that incorporating doula support into maternal care significantly improves birth outcomes, including lower rates of interventions like cesarean sections and preterm births, while enhancing maternal satisfaction, infant health and parental engagement. Additionally, doula-assisted care is linked to reduced maternal and infant mortality, decreased postpartum depression and average health care cost savings of nearly $1,000 per birth.
To learn more about the institute’s doula training program, visit uams.health/doula.
UAMS is the state’s only health sciences university, with colleges of Medicine, Nursing, Pharmacy, Health Professions and Public Health; a graduate school; a hospital; a main campus in Little Rock; a Northwest Arkansas regional campus in Fayetteville; a statewide network of regional campuses; and eight institutes: the Winthrop P. Rockefeller Cancer Institute, Jackson T. Stephens Spine & Neurosciences Institute, Harvey & Bernice Jones Eye Institute, Psychiatric Research Institute, Donald W. Reynolds Institute on Aging, Translational Research Institute, Institute for Digital Health & Innovation and the Institute for Community Health Innovation. UAMS includes UAMS Health, a statewide health system that encompasses all of UAMS’ clinical enterprise. UAMS is the only adult Level 1 trauma center in the state. UAMS has 3,485 students, 915 medical residents and fellows, and seven dental residents. It is the state’s largest public employer with more than 11,000 employees, including 1,200 physicians who provide care to patients at UAMS, its regional campuses, Arkansas Children’s, the VA Medical Center and Baptist Health. Visit www. uams.edu or www.uamshealth.com.
Source: UAMS Office of Communications & Marketing

Engaging Your Volunteers
By Kay Kendall
Irecently reviewed a half dozen application summaries from recent Baldrige Award Recipients in healthcare, all of whom have significant numbers of volunteers. I discovered some common best practices that may allow you to recruit, retain, and engage your own volunteers.
VOLUNTEERS — PART OF THE WORKFORCE
In each case, the hospitals and health systems viewed their volunteers as part of their workforce, including them in many of the same or similar practices as their own employees.
They have expanded the “best place to work” to “best place to volunteer.”
These best practices include:
• An emphasis on the Mission, Vision, and Values during the recruiting and interview processes and reinforced during the onboarding process.
• Assessing the candidates’ interests, capabilities, and willingness to perform different tasks.
• Assigning tasks aligned with their ideal jobs.
• Surveying them at least annually to determine satisfaction and engagement.
• Validating drivers of engagement.
• Involving them on teams to address any gaps identified in the survey.
• Including them on process improvement teams or committees.
• Encouraging them to participate alongside employees in community events and fundraisers.
• Providing regular feedback through a Volunteer Coordinator based on input from the managers and staff in the departments in which they volunteer. Some benefits are also extended to volunteers such as free or discounted meals; free parking; use of on-site fitness centers; and complimentary health screenings, vaccinations, and wellness events.
MEASURING WHAT MATTERS
These same award-winning organizations also have measures to assess the strength of their volunteers by hours donated, number of volunteers, retention, and responses to questions that assess engagement such as, “I would recommend XYZ as a place to receive care,” and “I am proud to be a volunteer at XYZ.”
AND ONE MORE BEST PRACTICE
A 2018 Baldrige Award Recipient, Memorial Hospital and Health Care Center, uses its website to make it easy to explore volunteer opportunities with a tab off of the home page dedicated to “Volunteer Services,” which has descriptions of various volunteer positions, benefits, forms for adults and teens to complete to express interest, and contact information. www.mhhcc.org/about-us/volunteer-services/ And their “Volunteen” program provides 14–19 year olds with an exposure to multiple careers in the healthcare profession.
PART OF A STAFFING STRATEGY
With staffing shortages continuing to hit the health care sector hard, it makes sense to evaluate volunteer capabilities and capacities to assist in tasks that need not be provided by licensed or credentialled employees. How can you better leverage these resources to provide more compassionate care and build your reputation in your community?


The team at BaldrigeCoach would be glad to help guide your hospital’s quest for process improvement. As CEO and Principal of BaldrigeCoach, Kay Kendall coaches organizations on their paths to performance excellence using the Malcolm Baldrige National Quality Award Criteria as a framework. Her team, working with health care and other organizations, has mentored 25 National Quality Award recipients. In each edition of Arkansas Hospitals, Kay offers readers quality improvement tips from her coaching playbook. Contact Kay at 972.489.3611 or Kay@Baldrige-Coach.com.

Scan this code to visit the Volunteer Services page.
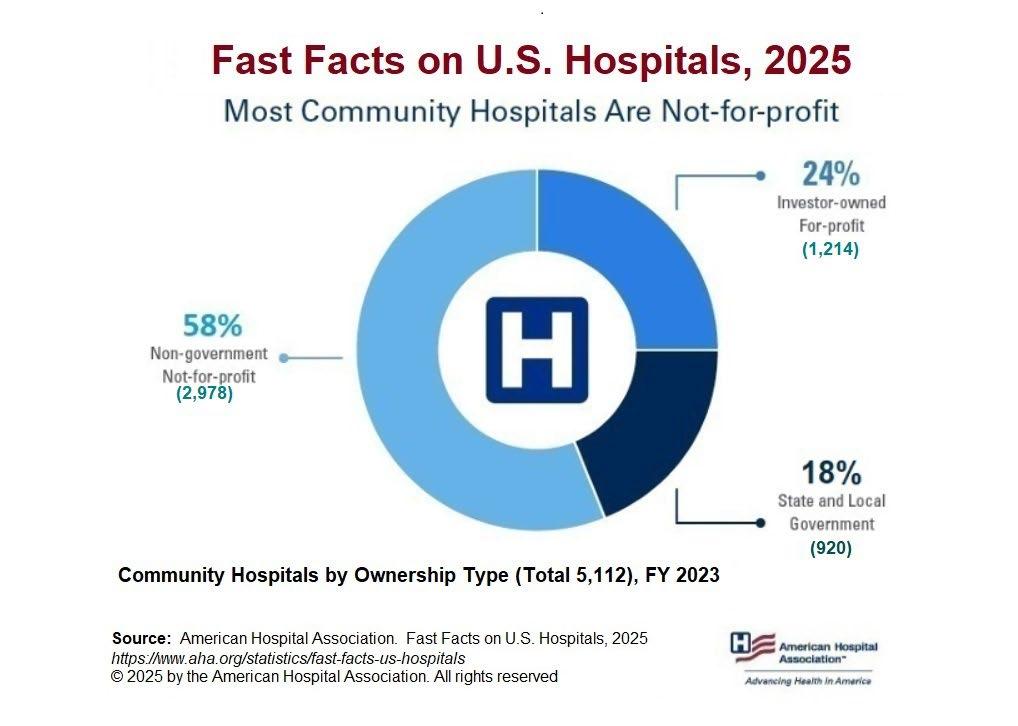
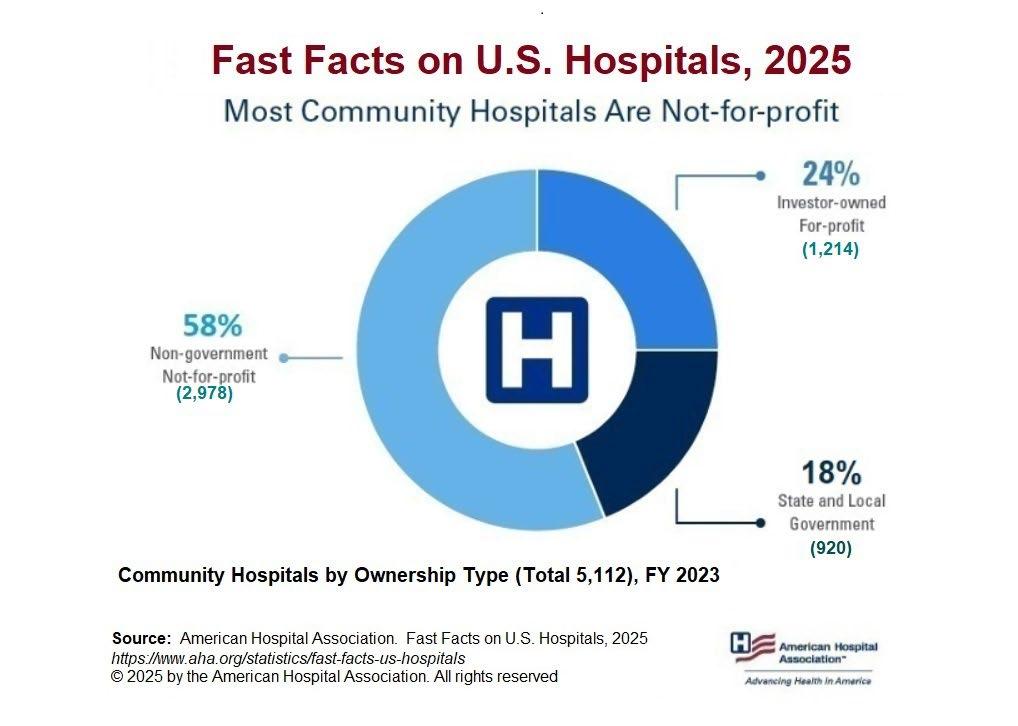
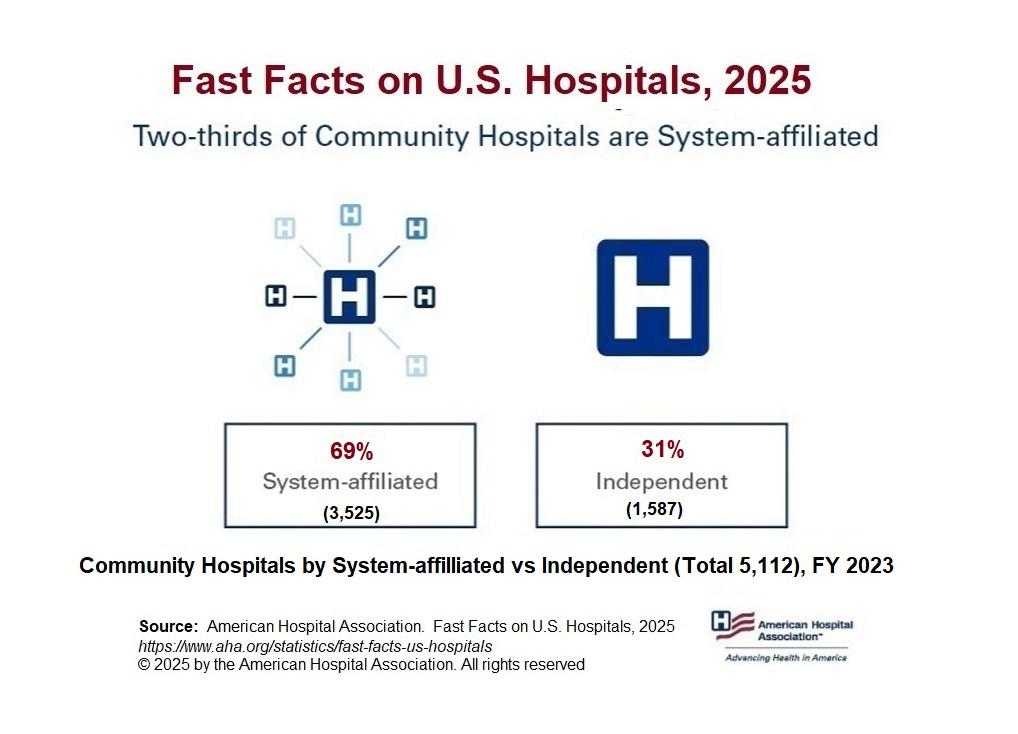
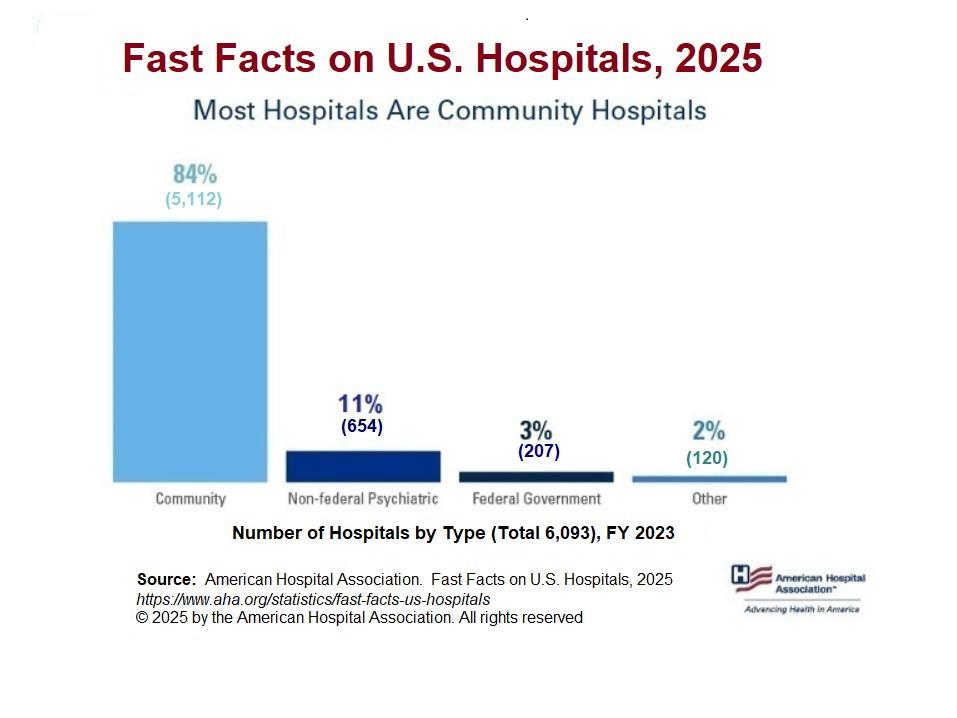
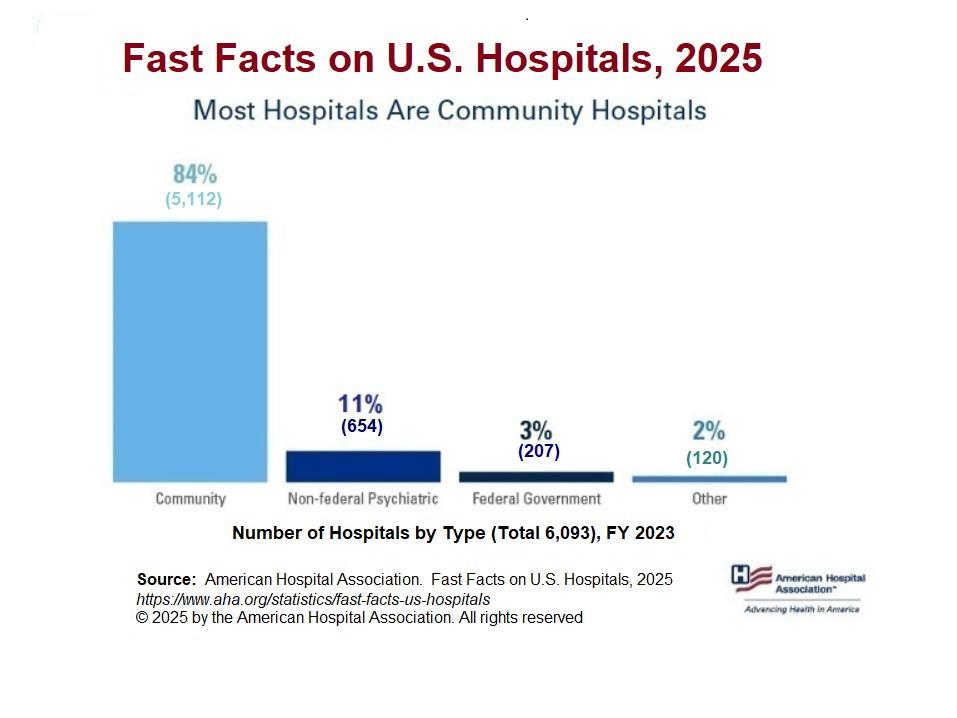
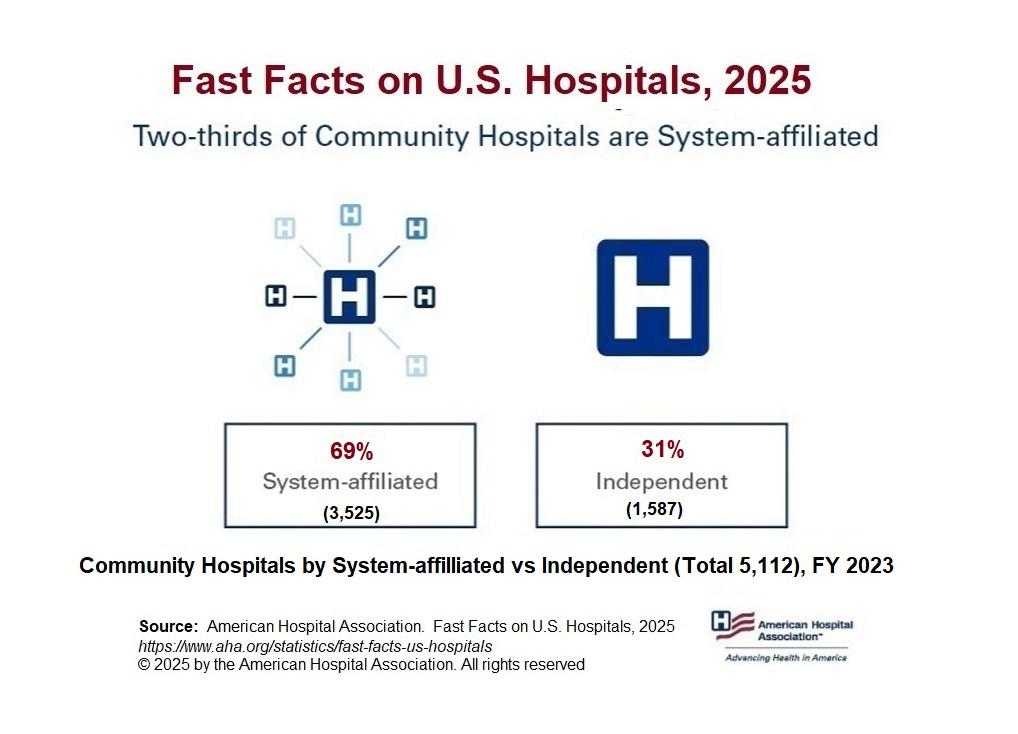

What does it mean to be taken care of?
What does it mean to be taken care of? At Arkansas Blue Cross and Blue Shield, it means providing peace of mind. We’ve been taking care of Arkansans for over 75 years, providing affordable, reliable health insurance … to keep Arkansans healthy and help them heal. We’re investing in communities to keep this diverse and wonderful state strong. We’re committed to a whole person approach to health, including physical and behavioral well-being. And we recognize that total health is influenced by many factors, including medical history, genetics, lifestyle, environment, nutrition, safety and physical activity. We also realize that it will take all healthcare providers working together to ensure future generations of Arkansans can live their best life their whole life long. Let’s take good care, Arkansas.




WE BUILDPlaces for Healing
Founded as a small construction company over 75 years ago, Nabholz has grown into a strong team of professionals serving our clients, communities, and each other. With a wide range of healthcare projects under our belt, we have the experience to deliver your project successfully — regardless of size.
