

INNOVATING CARE












AFMC – A Trusted Resource for Arkansas Providers.




With 50+ years of experience and expertise, our dedicated team has a successful history of delivering exceptional value to Arkansas providers.
• Contact Center Services: Assisting Clients with Access to Care
• Data Sciences: Better Data for Better Health Care



• Outreach Services: A Lifeline to the Provider Community
• Practice Transformation: Your Guide to Value Based Care Success
• Security Risk Analysis: Because Patient Trust Starts with Secure Data
• Event Planning Services: Memorable Events, Minus The Stress
Visit afmc.org to find out more.

Let us help you plan your next conference, meeting, or community event – contact us to reserve your spot! Visit afmc.org/events for more information. Host Your Next Event in
Style at the
District Event Center
Conveniently located in downtown Little Rock, our newly renovated event space offers free parking, seating for up to 100 attendees, a state-of-the-art A/V system, virtual conferencing options, and a fully equipped catering kitchen.
INNOVATING CARE

ARKANSAS HOSPITALS
Arkansas
To advertise, please contact Brooke Wallace magazine@arkhospitals.org
Becca Bona, Editor in Chief
Katie Hassell, Graphic Designer
Roland R. Gladden, Advertising Traffic Manager
BOARD OF DIRECTORS
Larry Shackelford, Fayetteville / Chairman
Greg Crain, Little Rock / Chairman-Elect
Michelle Krause, MD, Little Rock / Treasurer
Ron Peterson, Mountain Home / Past-Chairman
Ryan Gehrig, Fort Smith
Crystal Bohannan, Hot Springs
Connie Castleberry, Camden
Sammie Cribbs Roberson, Harrison
David Deaton, Clinton
Phil Gilmore, Crossett
Michael Givens, Jonesboro
Tommy Hobbs, Clarksville
Charlotte Jackson, Searcy
Eric Pianalto, Rogers
Brian Thomas, Pine Bluff
Matt Troup, Conway

Cody Walker, North Little Rock
EXECUTIVE TEAM
Robert “Bo” Ryall / President and CEO
Jodiane Tritt / Executive Vice President
Tina Creel / President of AHA Services, Inc.
Pam Brown / Vice President of Quality and Patient Safety
Lyndsey Dumas / Vice President of Education
Debbie Love / CFO

Stability, Strength and Service
We’re here to help you navigate these changing times. With more than 40 years of experience, LAMMICO provides medical professional liability insurance coverage for hospitals and facilities so that you can practice with confidence – confidence that your coverage is reliable and your reputation will be protected. Aggressive legal defense, personalized claim handling and accredited risk-management education are the bedrock of our business. Our dedication, financial strength and rock solid track record ensure that with LAMMICO as your partner, you can focus on what matters most: your patients

$10,000 Grant Opportunity
The 2024-2025 LAMMICO Patient Safety Award and Grant topic is early recognition of sepsis. Learn more at lammico.com/grant. Applications are due May 31, 2025.


Advancing Care Through Innovation
Innovation is reshaping health care across the nation. From artificial intelligence integration and digital patient experiences, to telehealth expansion and strategic partnerships, providers are embracing various methods to enhance care. These advancements, whether cutting-edge or time-tested, share a common goal: improving care delivery and patient outcomes.
Hospitals across Arkansas are demonstrating remarkable resilience, continuously adapting to serve their communities. Innovation takes many forms — streamlined internal processes that enhance efficiency, creative collaborations that reduce unnecessary emergency department visits, and technology-driven solutions that expand access to care. These efforts reflect a shared commitment to ensuring patients receive the right care, at the right time, in the right place.
Yet, as hospitals push forward with new solutions, challenges remain. Many of these innovative efforts depend on financial stability, but hospitals across the state continue to struggle with rising costs and inadequate reimbursement rates. Rural hospitals, in particular, face mounting
difficulties in maintaining essential services, recruiting physicians, and implementing new technologies. Without sustainable funding and policy support, the progress Arkansas hospitals are making could be at risk.
Health care leaders understand that progress requires collaboration, but aligning diverse perspectives can be a challenge. At the Arkansas Hospital Association, we see firsthand the dedication of our member hospitals as they navigate complex regulatory environments, workforce shortages, and evolving patient needs. Hospital leaders, clinicians, health care advocates, volunteers and AHA members across the state are working tirelessly to ensure every Arkansan has access to quality care. However, they cannot do this alone.

With the legislative session underway, the AHA remains focused on advocating for policies that support our hospitals and empower health care professionals. Ensuring that providers can prioritize patient care — without being burdened by unnecessary administrative hurdles — is critical to fostering an environment where innovation can thrive. Investments in infrastructure, workforce development, and technology must remain a priority to sustain the advancements already taking place.
In this issue of Arkansas Hospitals, we explore the many ways hospitals are advancing care, offering real-world examples of innovation in action. We also look to the American Hospital Association’s curated strategy for implementing AI solutions, to offer a guidebook to our member hospitals.
The Arkansas Hospital Association will continue to champion solutions that strengthen our health care system, so Arkansas hospitals can remain at the forefront of delivering high-quality, patient-centered care. By working together, we can build a more innovative, resilient, and accessible health care system for all Arkansas.
Bo Ryall President and CEO

FUNDS
HELPING HOSPITALS RECOVER FUNDS
HELPING HOSPITALS RECOVER FUNDS
to
clients'
assess the opportunity, determine if a response is required, and ensure the best possible outcomes. MCAG minimizes the administrative burden by facilitating all inquiries. Our team is always available to discuss current, past and future settlements, and what they might mean for your business.

Managed Care Advisory Group (MCAG) is a leading provider of specialized services that help organizations maximize their recoveries from class action settlements. Since our founding, we have worked with a wide range of industries, with a significant focus on the healthcare sector, helping clients identify and claim their share of settlement funds efficiently and effectively. Our expertise lies in simplifying complex processes, ensuring compliance, and delivering measurable financial outcomes for our clients.
The healthcare industry operates in a highly complex and regulated environment. Class action settlements in this sector often involve intricate eligibility requirements and voluminous data submissions. MCAG excels at managing these challenges, delivering tailored services for healthcare providers, hospitals, clinics, and other organizations.
MCAG’s Settlement Recovery Service helps over 1,400 hospitals recover funds from class action settlements. We identify settled cases applicable to our clients, bring these to our clients' attention, assess the opportunity, determine if a response is required, and ensure the best possible outcomes. MCAG minimizes the administrative burden by facilitating all inquiries. Our team is always available to discuss current, past and future settlements, and what they might mean for your business.
DO NOT LET OPPORTUNITIES PASS YOU BY. CONTACT MCAG TODAY!
MCAG’s Settlement Recovery Service helps over 1,400 hospitals recover funds from class action settlements. We identify settled cases applicable to our clients, bring these to our clients' attention, assess the opportunity, determine if a response is required, and ensure the best possible outcomes. MCAG minimizes the administrative burden by facilitating all inquiries. Our team is always available to discuss current, past and future settlements, and what they might mean for your business. DO NOT LET OPPORTUNITIES PASS YOU BY.
Over $200 Million dollars have been recovered by MCAG for healthcare organizations.
5 out of 10 of the largest for profit health systems utilize MCAG as their Settlement Recovery Expert.
5 out of 10 of largest for profit systems utilize as their Settlement Recovery Expert.
10 out of 25 of the top non-profit hospitals are protected by MCAG’s Settlement Recovery Service.

Over $200 Million dollars have been recovered by MCAG for healthcare organizations.
The Pivot Mindset
Igrew up in a family full of medical professionals, which meant I always believed I wasn’t a dog person. With 14-hour shifts dominating our schedules, pets had to be relatively selfsufficient — so we had cats. That belief, however, took a sharp turn in 2020 when I found myself with a 10-weekold puppy.
Today, Goose is big, fluffy, and extremely communicative. We’re not exactly sure of his breed, but there’s probably some Siberian husky involved. Regardless, despite my lack of training expertise, he and I have developed a our own language over time. Or, more accurately, he innovated his behavior in a way that allowed me to understand him.

One day, Goose started answering my question — “Do you want to go outside?” — by spinning in a tight counterclockwise circle. A clear, enthusiastic “yes.” He spun four more times before I started worrying that he’d get dizzy, so we went outside. Later, he developed another behavior: resting his chin on the couch when asking permission to jump up. These were not tricks I taught him. He created them himself, adapting to our routine to communicate his needs.
My husband, a lifelong dog person, says Goose and I understand each other because of our consistent routine. Every morning at 6 a.m., rain or shine, we walk together. He follows me around as if he is my shadow, and I talk to him as if he understands every word. And, in many ways, he does — his ears perk up at words like “treat” and “walk.” Because of this foundation, I’m considering taking it further and introducing him to those programmable talking buttons you can purchase from pet stores.
Like Goose, society is constantly building on the foundations of communication. From spoken to written word, from print to digital, we push forward. Innovation is woven into our
lives, from artificial intelligence in our phones and cars to its growing role in health care, where AI is transforming imaging, surgery, and administrative workflows.
In this issue, we explore the American Hospital Association’s latest Market Scan on Innovation, which outlines guiding principles for adopting AI in various high-reward use cases. We also look at how hospitals across Arkansas are integrating AI into their practices and how innovation extends beyond technology into strategic partnerships that enhance patient care. For health care professionals — those who enter the field to help others — innovation is ultimately about improving care delivery and patient outcomes. While it often refers to emerging technologies, true innovation extends beyond devices and data. It includes strategic collaboration, process improvements, and new ways of thinking about care. At its core, innovation is about communication — identifying needs and finding solutions that keep patients at the center. Sometimes it’s as simple as recognizing a counterclockwise spin for what it is: an unmistakable, eager yes.

Becca Bona Incoming Editor in Chief

2025 Spring Calendar
APRIL
April 3-4
Arkansas Healthcare Human Resources Association (AHHRA) 2025 Spring Conference
Doubletree by Hilton Hot Springs
April 10
2025 Emergency Preparedness Forum Little Rock
April 10 -11
Society for Arkansas Healthcare Purchasing & Materials Management (SAHPMM)
Annual Meeting & Trade Show
Double Tree by Hilton Hot Springs
April 16-18
Arkansas Association for Healthcare Engineering (AAHE) 2025 Spring Conference & 45th Annual Trade Show
Oaklawn Racing Casino Resort Hot Springs
April 16
AHA Services, Inc. Webinar
Overcoming Rural Recruitment Bias Virtual Event
April 23
Arkansas Organization of Nurse Leaders (ArONL)
Navigating New Measures PSSM, Age Friendly, and OB Emergency Preparedness Virtual Event
April 25
Arkansas Association for Medical Staff Services (ArkAMSS) Spring Meeting
Arkansas Hospital Association Little Rock
MAY
May 1
ACHE of Arkansas & AAHT
Arkansas’s 2025 Legislative Session Regional Dinner St. Bernards Medical Center Jonesboro
May 4-6
American Hospital Association
Annual Meeting Marriott Marquis Washington, D.C.
May 21

THE DATE Arkansas Hospital Education & Research Trust (AHERT) Leadership Conference
June 18-20
Big Cedar Lodge Branson, MO

AHA Services, Inc. Webinar
Pharmacy Benefits: What’s New and Changing in 2025 and Beyond Virtual Event
Register for AHA Events Online!
Employees of AHA member hospitals can now log in to www.arkhospitals.org and register for events online.

October 15-17
Little Rock Marriot
Opening Speaker – Jackie Joyner Kersee
Closing Speaker – RaDonda Vaught

Jackie Joyner Kersee
RaDonda Vaught
Scan this code for our event page.




Arkansas Medicaid Announces 2024 IQI AWARD RECIPIENTS
For nearly two decades, Arkansas Medicaid has embraced the concept of pay-for-performance as a key approach to improving quality of care in Arkansas. This concept entails rewarding hospitals with financial incentives to achieve Medicaid quality goals.
Through a partnership between Arkansas Medicaid, Arkansas Foundation for Medical Care, and the Arkansas Hospital Association, the Inpatient Quality Incentive program was developed in 2006 to assess quality of care through the ways in which hospitals provide medical care to their patients. Since its launch in 2006, Arkansas Medicaid has awarded financial incentives to participating hospitals that demonstrate significant improvements in health outcomes.
At the 2024 Medicaid Educational Conference in December, Arkansas Medicaid recognized 38 hospitals for their dedication of consistent participation of 10 or more years in the IQI program and for their efforts toward improving the health of Arkansans.
Scan this QR code to learn more about the IQI program.


The following hospitals received special recognition for participating in this initiative for 10 plus years:
• Arkansas Methodist Medical Center
• Baptist Health Medical Center - Arkadelphia
• Baptist Health Medical Center - Fort Smith
• Baptist Health Medical Center - Heber Springs
• Baptist Health Medical Center - Hot Spring County
• Baptist Health Medical Center - Little Rock
• Baptist Health Medical Center - North Little Rock
• Baptist Health Medical Center - Stuttgart
• Baptist Health Medical Center - Van Buren
• Baxter Regional Medical Center
• Chambers Memorial Hospital
• CHI St. Vincent Hospital Hot Springs
• CHI St. Vincent Infirmary
• CHI St. Vincent Medical Center North
• Drew Memorial Health System (now Baptist Health Drew County)
• Forrest City Medical Center
• Great River Medical Center
• Jefferson Regional Medical Center
• Johnson Regional Medical Center
• Mena Regional Health System
• Mercy Hospital Fort Smith
• Mercy Hospital Northwest Arkansas
• National Park Medical Center
• NEA Baptist Hospital
• Northwest Medical Center - Bentonville
• Northwest Medical Center - Springdale
• Northwest Medical CenterWillow Creek Women’s Center
• North Arkansas Regional Medical Center
• Ouachita County Medical Center
• Regional One Health Memphis
• Saint Mary’s Regional Medical Center
• Saline Memorial Hospital
• Siloam Springs Regional Hospital
• South Arkansas Regional Hospital
• St. Bernards Medical Center
• Unity Health White County Medical Center
• Washington Regional Medical Center
• White River Medical Center
HOSPITAL NEWSMAKERS

and community members
Baptist Health hosted a ribbon cutting for the opening of Baptist Health Comprehensive Women’s Clinic-North Little Rock on Tuesday, Jan. 28. Ijanae Allgood, MD, MPH, and Sarah Beth Holcomb, MD, will see patients at the clinic. They specialize in primary care, pediatrics, pregnancy, and childbirth. Baptist Health Comprehensive Women’s Clinic-North Little Rock, at 4625 JFK Boulevard, Suite 210, in North Little Rock, provides quality primary care for women of all ages and their children. Each new phase of a woman’s life can bring different health concerns. From annual wellness exams to childbirth, chronic medical conditions to breast health, the clinic delivers the leading care and advanced services patients need to pursue a lifetime of wellness.
Chartis recognized Mercy Hospital - Paris on its 2025 Critical Access Hospitals Top 100 list for excellence in quality, patient care, and rural health care sustainability.
The National Institutes of Health has awarded Arkansas Children’s Research Institute (ACRI) a $3 million grant to explore how forever chemicals impact infant and child development. The project will also look at whether a pregnant mom’s physical activity can offer some protection against those chemicals’ effects.

The Arkansas Perinatal Quality Collaborative , a partnership started last year between the University of Arkansas for Medical Sciences, the Arkansas Department of Health, and 34 birthing hospitals across the state, has launched its second initiative to rapidly address a congenital syphilis problem in Arkansas. Twentytwo hospitals in Arkansas are participating in this new initiative, which started in January 2025 and will run for six months.
ARPQC has developed a maternal safety bundle to guide practice changes at participating hospitals. A key recommendation is to screen all pregnant women at birth as well as at outpatient encounters such as emergency department visits. ARPQC has also prepared clinical guides and educational resources to assist participating facilities with practice changes.
Staff
celebrate the opening of Baptist Health Comprehensive Women’s Clinic–North Little Rock with a ribbon-cutting ceremony and tours on Jan. 28.
Baxter Health in Mountain Home held a ribbon-cutting ceremony to celebrate the completion of the Cline Emergency Center remodel and expansion on Thursday, Feb. 13. The remodel includes additional patient rooms, rapid care rooms, trauma rooms, and waiting areas, and was made possible by Baxter Health Foundation donors. The center was designed to provide more room for treatment and ease in patient flow.
Char Boulch is the new CEO of Saline Health System in Benton . Boulch previously served as the chief nursing officer since 2023. In her more than 22 years of health care expreience, she’s held senior nursing positions in multiple hospitals, where she led strategic initiatives to enhance quality, patient care, and operational performance.
Crystal Bohannan is the new president of CHI St. Vincent Hot Springs. Bohannan has decades of experience in health care, previously serving as vice president of operations at CHI St. Vincent Hot Springs as well as more than 10 years as executive director of operational finance. Bohannan holds a Bachelor of Business Administration degree from Southern Arkansas University in Magnolia and a Master of Business Administration from Mississippi State University in Starkville, Mississippi. She is also a CPA.
Kory Browning is the new Chief Executive Officer of Northwest Medical Center – Springdale . Browning previously served as a chief operating officer in San Antonio. Browning earned a Bachelor of Science in biomedical sciences from Texas A&M University at College Station, Texas, and a Master of Business Administration in health care management from the University of Texas at Tyler, Texas.
Ozarks Community Hospital celebrates 25 years of service in the Ozark region of both Arkansas and Missouri in 2025. Headquartered in Gravette, Arkansas, OCH is a bi-state safety-net healthcare provider dedicated to improving the health and well-being of urban and rural communities throughout the region.
Unity Health – Jacksonville has partnered with New Vision to offer medical detoxification services to help adults overcome withdrawal symptoms from drug and alcohol addiction through the New Vision withdrawal management services. The service treats adults with a medically supervised hospital stay for inpatient stabilization, which usually lasts three days. Discharge planning will occur before leaving the hospital. The patient will be referred to appropriate community-based treatment programs to help prevent relapse and continue their treatment.
Washington Regional in Fayetteville has achieved the American College of Emergency Physicians Geriatric Emergency Department Accreditation. The designation recognizes emergency departments with policies and procedures in place to meet the needs of older patients and improve outcomes.

Washington Regional’s Emergency Department has achieved Geriatric Emergency Department Accreditation, ensuring enhanced care for older patients through specialized policies, protocols, and staffing.
Arkansas awarded $17M grant to support maternal health initiatives. UPDATE: Maternal Health in Arkansas
Arkansas has been awarded a $17 million grant, the Transforming Maternal Health (TMaH) Model, from the U.S. Department of Health and Human Services’ Center for Medicare and Medicaid Services. Applying for the TMaH grant was among the recommendations made by the Strategic Committee for Maternal Health established by Gov. Sarah Huckabee Sanders’ Executive Order last year, and the funds will support key efforts to improve the health of pregnant women, new mothers, and babies, the Arkansas Department of Human Services announced in early January.
This grant will provide the funding over 10 years to several state Medicaid agencies, including Arkansas, with a goal of reducing disparities in access and treatment.
“Healthy moms means healthy babies,” said Governor Sanders. “Pursuing this grant was one of the first major recommendations of the Strategic Committee for Maternal Health I convened, and it will facilitate much of the rest of our work to increase the maternal care workforce, invest in technology and research to help new moms, and connect expecting moms with health care providers in all corners of the state.”
“We are grateful for the support from our federal partners as we work to implement changes that will improve maternal health outcomes in Arkansas,” said DHS Secretary Kristi Putnam. “This grant announcement builds on the momentum that began last year with the Governor’s Executive Order on maternal health, and the subsequent recommendations developed by a tremendous coalition of partners, stakeholders, and other supporters. We are proud to lead the way on key reforms that further these initiatives, and excited that this significant grant will bolster our efforts.”
“This grant and our state’s ongoing commitment will transform how we approach maternal health," said Arkansas Department of Health Secretary Renee Mallory. "Arkansas is devoted to improving maternal health
outcomes and ensuring every mother and child has the support they need. This grant is a significant step toward meeting the state’s vision and goals prioritized by the Strategic Committee for Maternal Health. Together, we will work to ensure healthier futures for families across our state.”
The grant is built on three main pillars: Access to care, infrastructure, and workforce capacity; Quality improvement and safety; and Whole-person care delivery. Specific investments planned in Arkansas with these funds include:
• Analyzing data to better target maternal health services
• Educating providers and pregnant women on the benefits of leveraging doulas, Community Health Workers, and midwives
• Investing in technology to better serve pregnant women and providers
• Building better technology infrastructure to collect and share data tied to maternal health measures
• Redesigning Medicaid reimbursement rates and payment structures, including a focus on incentive payments to providers whose patients have healthier outcomes
• Improving connections between health care providers and community-based organizations like nonprofits and faith-based groups that also serve low-income Arkansas women
DHS will lead the project in coordination with ADH and the University of Arkansas for Medical Sciences. DHS Deputy Secretary for Programs and State Medicaid Director Janet Mann will manage the grant efforts.
“Over the last year, we have directed significant resources to addressing gaps in care for pregnant women, new mothers, and babies, and we remain committed to finding solutions that will improve and save lives,” Mann said. “This grant is an important next step, and I know that this project will be a key driver in helping Arkansas become a leader in maternal health.”

Governor Sanders Announces Healthy Moms, Healthy Babies Act
Governor Sarah Huckabee Sanders announced the Healthy Moms, Healthy Babies Act to improve maternal health in Arkansas at a press conference on Feb. 6, 2025. The plan invests an estimated $45.3 million in maternal health annually. Senator Missy Irvin (District 24) and Representative Aaron Pilkington (District 45) are the lead cosponsors of the bill.
“I’m a mom, so I know how important maternal healthcare is to helping healthy moms have healthy babies, which is why my administration has been focused on building a comprehensive, coordinated approach to maternal health in Arkansas,” said Governor Sanders. “Along with the actions we have taken since I took office, the Healthy Moms, Healthy Babies Act will make real, lasting change to Arkansas’ maternal health landscape and move the needle on this critical issue facing our state.”
“Arkansas mothers and babies are our first priority. Today’s announcement and subsequent legislation is intentional, targeted and smart. It is designed to help our mothers be healthier so they can deliver healthier babies. Unbundling and increasing payments for prenatal, delivery and postpartum care is necessary, way past due and will make a huge impact in stabilizing our healthcare access for expecting mothers,” said Senator Missy Irvin. “I look forward to presenting this plan of action to prioritize and improve maternal health in Arkansas. I applaud the excellent work of our Governor, Secretary Putnam, our teams at DHS and the Governor’s office.”
“The Healthy Moms, Healthy Babies Act strengthens maternal care in Arkansas by unbundling the global payment, increasing provider reimbursements, and expanding access to telemedicine. This bill also improves pregnancy outcomes by empowering community health workers and ensuring Medicaid coverage for expectant mothers,” said Representative Aaron Pilkington.

The legislation includes several reforms recommended by the Governor’s Strategic Committee on Maternal Health, which she formed last year. It establishes Presumptive Medicaid eligibility for pregnant women, meaning pregnant women can receive prenatal care while they complete their Medicaid application. It offers reimbursement pathways for doulas and community health workers. And it establishes pregnancy-related Medicaid coverage for remote ultrasounds, remote blood pressure monitoring, and continuous glucose monitoring. These reforms will result in an additional $7.44 million investment in Arkansas moms.
Additionally, the legislation unbundles Medicaid payments for pregnancy care, paying for up to 14 prenatal and postnatal care visits, encouraging providers to work with pregnant women so they attend more appointments, and increasing Medicaid’s investment in pregnant women by $12.2 million. The Governor also announced that Medicaid will increase reimbursements for traditional deliveries and c-sections by 70%, investing an additional $25.7 million in care for pregnant women and encouraging more providers to participate in the Medicaid program, increasing access to care.
“The changes included in the Healthy Moms, Healthy Babies Act will go a long way toward ensuring women’s access to essential care before, during, and after pregnancy,” said Arkansas Department of Human Services Secretary Kristi Putnam. “I am grateful for the leadership from Governor Sanders, the Legislature, and our many stakeholder partners who have all worked collaboratively on improving our maternal health system and supports. I’m excited to see how these changes will improve the health of pregnant women, new moms, and babies across our state.”
The changes included in the Healthy Moms, Healthy Babies Act will go a long way toward ensuring women’s access to essential care before, during, and after pregnancy.
Funding for these investments is facilitated by the $13 million commitment the Governor made to maternal health in her budget. That investment allows the state to access additional federal Medicaid funding.
“Since the Strategic Committee on Maternal Health met and submitted our report, a number of important initiatives and programs have been started or improved upon,” said Dr. Kay Chandler, Arkansas Surgeon General. “It is exciting to continue this work and see these policy recommendations become reality. They will make important, positive impacts on the health of Arkansas moms and babies for years to come.”
“The Arkansas Department of Health is privileged to see maternity patients in our Local Health Units every day, and we have seen first hand what these policy changes will mean for patients and providers in communities across the state,” said Renee Mallory, Arkansas Secretary of Health. “We look forward to continuing our efforts with our partners to improve maternal health in Arkansas.”
“Medicaid covers approximately half of all births in Arkansas, so investing in changes that expand and improve maternal care within the Medicaid program will have profoundly positive impacts on our state,” said Arkansas Department of Human Services Deputy Secretary for Programs and State Medicaid Director Janet Mann. “These reforms directly align with the recommendations from the Strategic Committee for Maternal Health, and we look forward to making them a reality.”
Governor Sanders established the Strategic Committee on Maternal Health by Executive Order on March 6, 2024, initiating a six-month timeline for stakeholders to meet and discuss potential reforms. More than 100 stakeholders representing dozens of organizations met more than 20 times, crafted and discussed recommendations, and delivered their report to the Governor on Sept. 5, 2024.


St. Bernards Recognized at the Arkansas State Capitol
In a resolution sponsored by Senator Dan Sullivan, St. Bernards Medical Center in Jonesboro was honored at the Arkansas State Capitol on Jan. 22, 2025, for its groundbreaking efforts in maternal health care. This recognition follows St. Bernards’ partnership with the Department of Human Services in November 2024 to establish the state’s first Maternal Life360 HOME, a program dedicated to supporting women with high-risk pregnancies.
Designed to serve women enrolled in the Arkansas Health and Opportunity for Me (ARHOME) Program and traditional Medicaid, the Maternal Life360 HOME provides essential home-visit services throughout pregnancy and for up to two years postpartum. By delivering personalized care, the program not only
improves maternal and infant health outcomes but also addresses critical social determinants of health, such as food security and housing stability.
Recognizing the far-reaching impact of this program, the Arkansas Senate has formally honored St. Bernards for its leadership in advancing maternal health and well-being. The Maternal Life360 HOME not only enhances care for mothers and babies but also strengthens communities by fostering long-term health improvements.
This recognition highlights St. Bernards dedication to innovative, patient-centered care and reaffirms its role as a leader in improving health care access for Arkansas families.

Staff from St. Bernards stand with Senator Dan Sullivan at the Arkansas State Capitol on Jan. 22. From left: Dana Lands, St. Bernards Director of Women’s & Children’s Services; Sen. Dan Sullivan; Emily McGee, St. Bernards Chief Nursing Officer; and Brenda Million, retired Vice President of Women’s & Children’s Services at St. Bernards.
AI & Health Care Innovation: Resources for Hospitals from the American Hospital Association
Experts agree that artificial intelligence has the potential to transform each and every aspect of health care delivery from the simplest administrative task to the most complex clinical procedures and improved organizational and patient care outcomes at lower costs.
Looking at unlimited possibilities with limited budgets, most hospital and health system executives are asking where and how to better invest in the health of their communities. The challenge? There’s no road map. There’s no playbook. Strategically, hospital and health system executives are learning where and how to use AI technology for value creation, and their AI budgets are prioritizing patient access, revenue cycle management, and operational throughput use cases that yield a tangible return on investment. Integrating AI into clinical care can enhance patient outcomes across health care settings and produce significant savings and improvements in health; however, challenges related to data privacy, bias, and the need for human expertise must be addressed to implement AI responsibly and effectively.
As hospital and health system leaders have come to realize, health care AI is experiencing an influx of new technologies, algorithms, and applications, leading to a very dynamic landscape. We organized this report around three pillars: people, process, and technology. The report identifies nine foundational building blocks within those areas for creating an effective AI action plan.
NOTE: This new Market Insights report from the American Hospital Association’s Center for Health Innovation picks up where three Market Insights reports on health care AI published in 2019 left off:
• “Surveying the AI Health Care Landscape”
• “AI and Care Delivery”
• “AI and the Health Care Workforce”
These three reports proved to be prescient and continue to offer useful insights.


full American Hospital Association AI Report.
People: Health Care AI is a Team
Sport Led by the CEO Who Builds the Roster and Sets the Agenda
Transformation endeavors require an action plan, and transforming health care delivery with AI is no different. Like all action plans, the first element of consideration is people. Without people, process and technology mean little.
There are three essential people-related building blocks:
BUILDING BLOCK 1 | LEADERSHIP
1
2 3
The role of the CEO is critical. The CEO sets the vision and leads an executive team that connects proposed AI pilots and projects with the overall strategic objectives of the organization. Overcoming challenges with patient care, patient access, and provider burnout continue to be top of mind for C-level executives. The CEO prioritizes the order and investment in AI pilots and projects. AI doesn’t just change work. AI changes the nature of work. Execution of pilots and projects should be the responsibility of someone with the word “chief” in their title who is conversant in AI — like a chief innovation officer, chief digital officer, chief strategy officer, chief transformation officer, or chief AI officer. That signals that the journey is transformational, not transactional.
BUILDING BLOCK 2 | CHANGE MANAGEMENT
Given that AI deployed in any area or use case changes the nature of work, hospital, and health system AI action plans must have a robust change management component. Changing the nature of work changes the culture of an organization. Involving workers in deploying AI means actively engaging employees throughout the process of implementing AI systems to ensure a smooth transition and adoption. The organization only will realize the benefits of AI if employees become AI literate and are equipped to use the technology effectively. As AI-powered technology reduces the time that clinical and administrative staff spend on repetitive, labor-intensive tasks, staff will be able to use their expertise and focus on higherlevel, nuanced tasks that require human judgment and empathy, which AI cannot fully replicate, such as enhanced patient interactions, clinical quality improvement, team collaboration, and acquiring new skills. That adjustment can be difficult, and it’s up to the organization to provide training programs to equip staff with the necessary skills for new responsibilities and encourage managers to support staff actively as they adapt to new workflows.

BUILDING BLOCK 3 | TEAM
The deployment of AI technology whether extensive or limited is a team sport. It requires participation by all relevant parties early in the pilot or project ideation and vetting process. The CEO, other C-level executive responsible for AI projects, and executive team are prerequisites. Finance, human resources, IT, operations, clinical, and administrative leaders must have seats at the table as the ripple effects of how AI will change how people work and the nature of their work can be far-reaching and often unknown. A nonnegotiable player on the team is someone who knows technology and how it works.
According to the health care AI experts interviewed for this report, getting the people right is the hardest part of an effective AI action plan.
Intentionality Should Be the Word that Best Describes an Organization’s AI Action Plan
With the right leaders and team in place, the next pillar of an effective health care AI action plan is process. In short, what’s the plan? How will the organization do what it says it wants to do?
Again, there are three process-related building blocks:
BUILDING BLOCK 4 | IDEA FLOW
4
5 6
Health care AI action plans must have a system that determines how ideas for AI pilots and projects flow to the leaders and teams vetting them. Absent a systematic approach, AI deployment can be a fragmented landscape of amazing technologies looking for problems to solve. Ideas can flow top-down from leaders and teams to the people who execute them. Ideas can flow bottom-up from people most in need of help to do their jobs or from administrative, clinical, financial, or operational department leaders who have innovative ideas to do what they do better or more efficiently. The organization needs to systematically collect and organize ideas from various sources to improve processes.
BUILDING BLOCK 5 | VETTING IDEAS
Organizations must have a systematic approach to vetting ideas for AI pilots and projects. It must be intentional and use consistent criteria to review each idea. Criteria may include strength of connection to a strategic objective, availability of data to execute the idea, expense, scalability across the enterprise, seriousness of the job to be done, urgency of the job to be done, risk tolerance, potential regulatory issues, etc. The criteria must be transparent to internal stakeholders and there must be a system to track the progress of approved pilots and projects.
BUILDING BLOCK 6 | CENTRALIZATION OF CAPABILITIES
In the early days of an organization’s AI journey, the people, process, and technology capabilities required for an AI pilot or project probably will be decentralized. Administrative, clinical, financial, and operational leaders are trying out new things. Ultimately, though, the organization must centralize system capabilities, not ideation, as they identify the best people, processes, technologies, and practices to do the jobs well and at scale. By centralizing capabilities, the organization learns from every pilot and project and can apply those lessons learned to the next use case. Capabilities mature along with experience and expertise; and rollouts become faster and more cost-efficient.

AI RESOURCES
Although there is no AI adoption road map or playbook for hospitals and health systems to follow, there are health care AI rule books put out by a number of credible organizations. They lay out AI adoption do’s and don’ts. Many call them guardrails to keep health care AI pilots and projects from running off the road or veering into dangerous or unintended consequences.
Here’s a partial list of AI resources from key industry groups available to hospital and health system leaders:
• Artificial Intelligence in the Provision of Health Care (American College of Physicians) (www.acpjournals.org/doi/10.7326/M24-0146)
• Assurance Standards Guide and Reporting Checklist (Coalition for Health AI) (chai.org/chai-releases-draft-responsible-health-ai-framework-for-public-comment/)
• AVIA’s Generative AI Strategic Collaborative (AVIA) (ai.aviahealth.com/ai/collaborative)
• Unveiling the Future of Healthcare with CHIME’s AI Principles (College of Healthcare Information Management Executives) (chimecentral.org/resource-post/chime-ai-principles#gsc.tab=0)
• Ethics and Governance of Artificial Intelligence for Health: Guidance on Large Multi-modal Models (World Health Organization) (www.who.int/publications/i/item/9789240084759)
• Navigating the Responsible and Ethical Incorporation of Artificial Intelligence into Clinical Practice (Federation of State Medical Boards) (www.fsmb.org/siteassets/advocacy/policies/incorporation-of-ai-into-practice.pdf)
• Pathways to Governing AI Technologies in Healthcare (Stanford Institute for Human-Centered AI) (hai.stanford.edu/news/pathways-governing-ai-technologies-healthcare)

• Patient Safety and Artificial Intelligence: Opportunities and Challenges for Care Delivery (Institute for Healthcare Improvement) (www.ihi.org/resources/publications/patient-safety-and-artificial-intelligence-opportunities-and-challenges-care)
• New consortium of healthcare leaders announces formation of Trustworthy & Responsible AI Network (TRAIN), making safe and fair AI accessible to every healthcare organization (Microsoft). (news.microsoft.com/2024/03/11/newconsortium-of-healthcare-leaders-announces-formation-of-trustworthy-responsible-ai-network-train-making-safe-and-fairai-accessible-to-every-healthcare-organization/)
Technology: AI Capabilities
Require Strong IT Infrastructure, Data Stewardship, and Governance
The third pillar is technology. Without a robust IT infrastructure, the benefits of AI in health care cannot be fully realized. In many ways, AI and AI-powered technology may be the most complicated to manage. Like nuclear power, AI is amoral. It is neither inherently good nor evil despite what sci-fi movies portray. The people who use it are responsible for its beneficial or detrimental purposes and outcomes. Hospitals and health systems are drawn to it for its potential to do good and to benefit their patients and communities.
Given the strong attraction, the technology pillar of AI action plans must have the following features:
BUILDING BLOCK 7 | STRONG DATA STEWARDSHIP
7 8 9
Data stewardship refers to how a health care organization uses data responsibly to power its AI pilots and projects. It’s often referred to as “responsible AI,” and protected health information (PHI) or patient health data are used appropriately; for instance, using PHI or patient health data to obtain the best possible outcomes while minimizing potential harm to patients. AI must be set up to de-identify PHI to protect a patient’s privacy and eliminate bias in data sets used for AIbased algorithms to generate actionable insights. To ensure that AI is working properly requires extensive quality control. Data stewardship must be a criterion in an organization’s AI pilot and project vetting process.
BUILDING BLOCK 8 | STRONG DATA GOVERNANCE
Strong data stewardship requires strong data governance. Data governance is knowing and controlling what data are being used in AI pilots and projects, the source of the data and who’s using it. Before data are used in AI pilots and projects, it must be “cleaned,” “scrubbed,” or “standardized,” and the privacy and security of the data must be protected. GenAI has elevated the importance of unstructured data and presents new opportunities in unstructured data management. Who has access to the data? Who has privileges to use the data? Are pilots and projects using opensource data or sharing data with open sources? AI pilots and projects must meet an organization’s data governance standards.
BUILDING BLOCK 9 | STRONG IT INFRASTRUCTURE
Hospitals and health systems shouldn’t build a separate IT infrastructure for AI. AI solutions require a strong data aggregation and analytics base. This involves addressing siloed data that are not easily available in digestible formats. The current IT infrastructure will need significant computational power to process data using AI and should be enough to handle AI pilots and projects. That’s assuming the existing IT infrastructure is interoperable, can accept data from outside sources in the case of open-source AI technology, and adhere to existing data stewardship and governance policies under the strain of AI technology. That should hold true whether an organization is a “maker,” i.e., builds its own AI solution, or a “taker,” i.e., buys a solution off the shelf, or a combination of the two. AI and genAI technology in particular are high-risk, high-reward propositions. The technology pillar of an effective AI action plan must be strong enough to handle the pressure.








UAMS CHAI Promotes AI Collaboration Across Health Care Landscape and Beyond
By Becca Bona
To implement Artificial Intelligence technology within health care, more needs to be understood about required infrastructure and general best practices.
The University of Arkansas for Medical Science recognized this need in 2020 and created the Creativity Hub for Artificial Intelligence (CHAI). Housed within the Department of Biomedical Informatics at UAMS, CHAI is led by Dr. Fred Prior, the department’s inaugural chairman.
CHAI’s goals are multifaceted and range from creating educational opportunities to encouraging statewide collaboration between scientists, health care professionals, and entrepreneurs.
“I direct the health informatics component of our Clinical and Translational Science Award, which is a $28 million grant from the (National Institues of Health) that funds our Translational Research Institute and Translational Science here at UAMS,” Prior explained. “One of the things we proposed, of course, was, how do we translate AI into biomedical research and medical practice?”
A large portion of that question centers on creating AI applications that are reliable and trustworthy in the clinical setting. Prior noted the following questions are paramount when examining different AI use-cases from this viewpoint: “Is this giving us reliable answers that we trust? How do we make sure that this keeps giving us reliable answers?” For Prior and his team, the goal is to carve out a rigorously tested and reliable evaluation process that works every time.
AI research took off in the mid-50s, when scientists began focusing on how machines could simulate human intelligence, following Alan Turing’s famous Turing Test. The test — a screening to determine a machine’s ability to imitate human intelligence — propelled the field for decades. In the ‘90s there was reinvigorated energy devoted to AI, thanks to the rise of computational power and introduction of algorithms.1
The generative AI models that came have appeared in the past few years have instilled a fear that AI will soon replace medical professionals. Prior said that this fear isn’t new. A key point to remember when talking about AI, is
that the complex math behind it lacks a consciousness, he said.
“There’s mathematical proof that says these algorithms cannot think,” Prior explained. “It has the amazing ability to mimic what we do, but it doesn’t know that it’s doing it.”
Five years ago, when Dr. Prior first began presenting on AI at various conferences, he realized that most medical professionals were already using some form of it. “[AI] is being built into tools that are improving performance,” Prior explained. “I think in healthcare, the big thinking and logic behind AI is to get more patient doctor interactions, not fewer,” Prior said. “It’s not to have the AI do your diagnosis but speed up the process by having smarter tools.”
Medical imaging is a great example and use-case, he noted, as the FDA approved AI algorithms for medical imaging in 2018. 2 “An MRI scanner takes a lot of time to create an image, but using very well understood AI models, you can sparsely sample the data space, and then generate high resolution, correct images. You get the same quality image, in a third of the time,” he explained.
brought on by genome sequencing. This opening-up of worldwide collaboration resulted in an increased amount of data local facilities had to safely store.
“Then the question was, what do I do with this terabyte data?” Prior said. “We created chief information officers and chief data officers to try to manage that.”
Recently, the chief AI officer title entered the clinical setting. The Mayo Clinic has a chief AI officer, and so do other large health care systems. “There’s a growing awareness that you need an information officer, that you need a data officer, but you
Since its founding, CHAI has worked with partners across the state to share knowledge of various projects. Prior and his team are specifically working to overcome AI bias in datasets that disproportionately over-represent academic medical regions, like those near Stanford and Harvard. UAMS’s ability to collaborate and curate a more Arkansas-based dataset further highlights the need for collaboration, which he says has been widely receptive across the state. CHAI aims to not only bolster research at UAMS, but the Arkansas health care scene at large.
There’s a growing awareness that you need an information officer, that you need a data officer, but you also need either of those people to understand AI, or you need a new AI czar.
also need either of those people to understand AI or you need a new AI czar,” Prior said.
For instance, CHAI has a voucher program, which offers grant opportunities to get appropriate and interested parties up and running with their own applications. There’s also the CHAI Salon, which offers an opportunity for both internal and external partners to present a problem they’re considering using AI or machine learning to solve but are unsure where to start.
Prior said, however, that while tested algorithms can be an excellent timesaver, they still require a human working in tandem with them for safety. “[T]here always has to be a human in the loop who’s paying attention and not trusting the algorithm. Always check, always verify,” he says.
The rise in AI applications begs for the rise in AI education and experts not only in the research world, but also in the clinical space. Similarly, chief information officers were on the rise in health care facilities a decade ago because of the onslaught of data
The rise of cyberattacks on health care systems in the past decade has increased the need for cybersecurity awareness, knowledge, and practice at the local level, but that added layer makes it difficult to test AI systems in real time in the health care setting. CHAI can nimbly conduct research thanks to added security and rigorous guardrails, making it a perfect collaborator for those in the health care space grappling with AI.
“I think academic medical centers have a better handle on setting the guardrails, because they have departments like mine that build these models, understand how they work, and are aware of what is the bleeding edge of the technology,” Prior noted.
“We sit down and work through how that process would work together,” Prior explained. “We all get excited about it and hopefully that becomes a collaboration.”
To learn more about CHAI visit medicine.uams.edu/dbmi/artificialintelligence-for-health/.


Sources
1. Peter Stone, Rodney Brooks, Erik Brynjolfsson, Ryan Calo, Oren Etzioni, Greg Hager, Julia Hirschberg, Shivaram Kalyanakrishnan, Ece Kamar, Sarit Kraus, Kevin Leyton-Brown, David Parkes, William Press, AnnaLee Saxenian, Julie Shah, Milind Tambe, and Astro Teller. "Artificial Intelligence and Life in 2030." One Hundred Year Study on Artificial Intelligence: Report of the 2015-2016 Study Panel, Stanford University, Stanford, CA, September 2016. Doc: http://ai100.stanford. edu/2016-report
2. Najjar R. Redefining Radiology: A Review of Artificial Intelligence Integration in Medical Imaging. Diagnostics (Basel). 2023 Aug 25;13(17):2760. doi: 10.3390/ diagnostics13172760. PMID: 37685300; PMCID: PMC10487271.

Mercy and Aidoc Bring AI Innovation to Imaging Services
Mercy
and Aidoc CEOs explain how the program will benefit patients across Mercy's footprint.
Mercy is leveraging Aidoc to simplify complex AI integration challenges, ensuring that advanced technology works seamlessly and securely within existing IT systems and electronic health records. By addressing these challenges, Mercy can provide cutting-edge, patient-focused care while maintaining operational efficiency and clinical excellence.
“Mercy has been a leader in AI technologies and this brings imaging into the fold, integrating Aidoc and its aiOS™ platform to continue our commitment to whole-patient care,” said Steve Mackin, Mercy president and CEO. “By empowering our teams with real-time insights and seamless coordination across specialties, this technology ensures we can focus on delivering exceptional care to every patient, every time. It’s a bold leap forward in shaping a future where AI drives both
clinical excellence and compassionate care for the patients we serve. Regardless of where your imaging study is done at Mercy, whether at our largest facility or smallest, everyone will get the additional review by AI and any additional findings shared our radiologists and patients."
Radiologists are vital to patient care, yet rising demand and complex imaging studies are contributing to a global shortage — part of the projected 122,000 physician shortfall by 2032. AI solutions like Aidoc help radiologists manage long days, easing workloads and managing industry demands, all while improving patient care and improving the ability to address health issues earlier.
With an advanced governance framework that serves as a model for health care systems nationwide, Mercy is showcasing
A Mercy radiologist reviews imaging results enhanced by Aidoc’s AI technology, which helps streamline workflows and improve patient care.
Mercy Harnesses AI to Revolutionize Imaging Services and Improve Patient Outcomes in Arkansas
For patients, a CT or X-ray to diagnose health issues is one step in a care journey. With the help of Aidoc (pronounced A-doc) technology, Mercy is transforming its imaging services by giving patients across its footprint extra peace of mind.
“Patients scheduled for most imaging services at any Mercy facility — hospital or outpatient — will benefit from advanced AI technology assisting radiologists in prioritizing and analyzing imaging studies,” said Dr. John Mohart, Mercy Executive Vice President and Chief Operating Officer. “Patients get the same great care they have come to expect from Mercy with a bonus, knowing if there are any suspected abnormalities, even outside of the original imaging study’s purpose, they will be notified.”
Mercy employed a phased rollout of Aidoc’s aiOS™ platform in early winter of 2025. The platform enables a comprehensive additional review of most diagnostic imaging to identify a wide range of suspected conditions, including brain hemorrhage, pulmonary embolism, cervical spine fracture and lung nodules. It also flags possible incidental findings, such as vascular abnormalities, enhancing its ability to provide a holistic assessment. By delivering real-time insights, Aidoc and the aiOS™ platform helps care teams prioritize urgent cases and facilitate timely intervention, while providing an extra value to patients as there will be no additional cost for this service.
Mercy Fort Smith launched the Aidoc program in late January 2025, with Mercy Northwest Arkansas following in mid-February 2025. Hospital staff at both locations eagerly anticipated the rollout and the positive implications for patient service delivery.
“Embracing new technology only enhances the exceptional care we already provide to patients,” said Dr. Sonal Bhakta, Chief Medical Officer for Mercy Northwest Arkansas. “AI has already proven to be a valuable new tool for health care providers. We look forward to what this technology will mean for both patients and providers.”
Ultimately, the time saved by introducing the new platform will be a boon not only for patients, but for providers, as well.
“I am so excited about this new technology, which will be an added layer of protection for our patients,” said Dr. Paul Bean, Chief Medical Officer at Mercy Hospital Fort Smith. “It will assist our fabulous radiologists in their interpretation of diagnostic images. It will allow for more accurate and timely reviewing of radiographs done at all Mercy facilities.”

“AI has already proven to be a valuable new tool for health care providers. We look forward to what this technology will mean for both patients and providers.”
- Dr. Sonal Bhakta

“It will assist our fabulous radiologists in their interpretation of diagnostic images. It will allow for more accurate and timely reviewing of radiographs done at all Mercy facilities.”
- Dr. Paul Bean
Q & A
with Mercy’s DR. JOHN MOHART,
Executive Vice President and Chief Operating Officer
AH: What key factors influenced Mercy’s decision to adopt Aidoc in particular?
JD: Mercy is leading the way in AI adoption, with imaging being the latest addition. When we learned about Aidoc, we knew we had found a trusted AI partner with deep experience in imaging and 25+ FDA cleared AI solutions. Imaging is Aidoc’s only focus, and they can meet the scale Mercy must have to implement this capability everywhere we serve. When we combine their expertise with the skill of our radiology team, everyone benefits — our patients and providers. Aidoc is a gamechanger, providing speed and ability to catch abnormalities faster, getting ahead of disease and health issues.
AH: What challenges did your team encounter during implementation, and how were they addressed?
JD: For a system as large as Mercy, it’s not uncommon to meet a few challenges when putting a new technology in place. We did a phased go-live with on-site support at each location to support providers as they learned the system.
We noticed a system configuration setting was causing some slowness in getting the AI results to the providers. Our Mercy Technology Services Epic support team was able to get a fix in place quickly to resolve.
Our team is also working with Aidoc and our imaging vendor to better incorporate prioritization both from Aidoc and our own stat ordering process, regardless of AI findings. We want to ensure providers can pair these together to create the highest priority as “stat with AI findings” and “stat without AI finding/normal AI findings” and “normal with no AI findings.”
AH: Has the Aidoc integration led to any unexpected benefits or insights beyond its initial intended use?
JD: Not an unexpected benefit, but worth noting on the first day of go-live in one of our communities, our providers caught a pulmonary embolism and a brain bleed with the help of Aidoc that allowed them to prioritize those patients’ care needs.
AH: How does Mercy plan to measure long-term success of Aidoc?

JD: Mercy uses data in many ways, and we plan to tap our analytics team to measure the success of Aidoc in the near term and long term. We will monitor additional findings on imaging studies, impact on length of stay, quality improvement, and reduction in turnaround time. Because Aidoc flags imaging studies with concerning findings and moves them to the top of the queue for our radiologists, we expect this technology to greatly change patient care.
Mercy’s Executive Vice President and Chief Operating Officer John Mohart considers Aidoc to be a gamechanger that enhances care for both patients and providers.
AH: Based on this experience, what advice would you offer to other health systems considering AI adoption in radiology and other applications?
JD: Mercy is a leader in precision medicine and AI, making significant investments for decades in data infrastructure and a single electronic health record. This enables us to scale AI solutions like Aidoc quickly and effectively across our entire system. I strongly encourage other health systems to invest in standardization with an intelligent data platform to be able to implement these AI models successfully at scale which in turn greatly benefits patients everywhere.



Continued from page 23
how thoughtful, patient-focused AI evaluation can lead to impactful innovation. The decision-making process was guided by the ECLAIR guidelines — which stands for evaluating commercial AI solutions in radiology — and emphasizes accountability, transparency, and patient safety in AI adoption. This rigorous evaluation positions Mercy as a leader in responsible AI integration within health care
“Mercy’s forward-thinking approach to AI adoption exemplifies how technology can be harnessed to empower care teams and prioritize patient well-being,” said Elad Walach, Aidoc CEO. "By integrating AI, Mercy is redefining what’s possible in health care — elevating patient outcomes, streamlining workflows and enabling unparalleled collaboration. This alliance showcases the transformative power of aligning innovation with a steadfast focus on delivering better care."
By aligning with frameworks like ECLAIR and CHAI (the coalition for health AI), Mercy ensures that the chosen AI solution delivers exceptional technology while upholding the highest ethical and operational standards. Mercy, one of the 15 largest U.S. health systems and named the top large system in the U.S. for excellent patient experience by NRC Health, serves millions annually with nationally recognized care and one of the nation’s largest and highest performing Accountable Care Organizations in quality and cost. Mercy is a highly integrated, multistate health care system including 50 acute care and specialty (heart, children’s, orthopedic and rehab) hospitals, convenient and urgent care locations, imaging centers and pharmacies. Mercy has over 1,000 physician practice locations and outpatient facilities, more than 5,000 physicians and advanced practitioners and more than 50,000 co-workers serving patients and families across Arkansas, Illinois, Kansas, Missouri and Oklahoma. Mercy also has clinics, outpatient services and outreach ministries in Arkansas, Louisiana, Mississippi, and Texas. In fiscal year 2023 alone, Mercy provided more than half a billion dollars of free care and other community benefits, including traditional charity care and unreimbursed Medicaid.


People First, Success Follows at Johnson Regional
By Becca Bona
Carving a calling and developing a career often involves following two distinct paths. Tommy Hobbs, CEO of Johnson Regional Medical Center in Clarksville, was able to accomplish both, largely because of his people-first approach to life. A young industrial engineer with manufacturing experience, his first foray into the health care industry opened his eyes to a different path, one that inspired him from the beginning.
“The people you work with bring you in,” he remembered. “And that’s what kept me in health care — the people and the culture.”
Born in Arkansas, Hobbs grew up near Fort Smith in Lavaca. He attended the University of Arkansas at Fayetteville with dreams of becoming an engineer as an undergraduate. Health care wasn’t on his radar until his senior year, during his coursework’s required group project. His subject area was manufacturing, but he distinctively remembers learning from his classmates’ shared experiences. “A couple of our groups got to work in the hospital setting,” he said. “I was very intrigued by that.”
Hobbs was interested enough to keep that curiosity alive, even though he took a job right out of school in the manufacturing sector. When an opportunity opened in health care, he jumped at the chance. “I was really excited about it and was fortunate enough to get selected to work at St. Vincent,” he recalled.




Working in the hospital as a management engineer allowed Hobbs endless learning opportunities. His main directive — to increase efficiency and productivity — kept him busy. Additionally, considering ways to improve the quality of care allowed him ample opportunities to learn and explore. “I needed to essentially work in every department of the hospital, which was fun,” he said with a smile.
Even at such an early stage in his career, Hobbs knew he’d found his place. “The difference in the field and the culture of the hospital versus manufacturing was so different and it fit me. It didn’t take me long to figure out that’s what I wanted to do,” he said.
As a young graduate, Hobbs wasn’t vying for a CEO position. Instead, he continued to focus on learning and working hard. After working at St. Vincent, he took a job with Baptist Health for a time before moving out of state to work for a national consulting company, also in the health care sector. He spent more than 20 years out of state, all the while, moving up in leadership positions.
Arkansans, no matter how long they’re gone, have a way of coming back to The Natural State. For Hobbs, the decision to move back centered on a need to be closer to his family. “We had been gone for 25 years, and we didn’t see [our family] that much for all that time,” he said. “So, it was time, from that point of view, and the opportunity with Johnson Regional came open and it all came together.” In 2022, he and his family made the move home, and he went to work as the hospital’s CEO.
From a geographical perspective, Johnson Regional is located in the Arkansas River Valley along the interstate between Fort Smith and Russellville. The 90-bed facility aims to serve a variety of individuals with a diverse set of needs.
Johnson Regional’s surgical team operates with precision using the Mako robotic system, advancing total joint replacement procedures for patients in the River Valley.
From orthopedics and general surgery to obstetric services (OB) and a very busy emergency department, there’s never a dull moment.
“Our goal, and I think we achieve it quite well, is to provide a quality level of care as well as anyone else,” Hobbs said. “That’s what I want people to understand about us. We have a hard time, believe it or not, even in this area, because people don’t know that Johnson Regional provides (obstetric) services, for example.”
Arkansas ranks among the highest in maternal mortality, but new collaborative efforts, with leadership from Governor Sarah Huckabee Sanders, aim to improve maternal health. Hobbs noted that Johnson Regional stands ready to participate in moving the needle forward and improving health outcomes for mothers and babies alike. “I always want to speak of our OB services, because it’s so critical in rural Arkansas, and I think that we do it so well,” he said.
Tackling a complex problem like maternal health outcomes in Arkansas gives a glimpse into Hobb’s leadership style — an inclusive, people-first mantra. “I feel that everyone’s point of view is important,” he said. “I think my style is so typical nowadays of leaders, but it is to be thorough and inclusive of ideas.” His early experience exploring the intricacies of the hospital, combined with his engineering perspective, gives him an understanding that a hospital runs effectively thanks to the efforts of many.
Within this lens, he’s always believed that a range of people should voice their opinions to constantly improve quality of care. “I make decisions that I feel are the best for the organization, and that doesn’t always include all the ideas that I get,” he said. “But I have the belief that two different perspectives can help craft a better outcome if you allow it. I think it’s not always easy to do it, but I try to get people to understand that’s how I view the world, and that’s how I make decisions.”
Q& A WITH
TOMMY HOBBS
What’s on your music playlist?
U2, Coldplay, Van Morrison, Bastille, The Band to name a few.
What is the best advice you were ever given?
There are outcomes/consequences to the decisions we make, so be very thoughtful when making decisions.
Do you have a favorite movie? Why do you like it?
Indiana Jones and the Last Crusade. It is just fun and action packed; where a guy and his father have an incredible adventure.
Who is someone you greatly admire, and why?
My father, John Hobbs. Because of how he loved and cared for my family — his will, intellect, and work ethic to make a better life for our family.
What would you be doing if you weren’t in health care? It is difficult to imagine not being in health care. I would probably be working in the capacity of an industrial engineer given that is my undergraduate degree.
What is something people don’t know about you? I have an unhealthy fear of heights.
What do you like to do in your down time?
I enjoy being outdoors gardening, hiking with my wife, fishing, and other activities that allows time outdoors.
What’s on your desk right now?
Winter edition of Arkansas Hospitals magazine, Cerner implementation dashboard reports, invoices.
What are you reading? (non-work-related material)
The Boys in the Boat.
Where would you travel, if you could go anywhere? There are numerous places in the U.S. that I would like to travel to, and I would take my wife to Europe.
What’s a life-changing lesson COVID-19 has taught you? The unimaginable can happen and we can withstand it.

HOSPITALIZATION
NOTIFICATION SERVICES
SHARE's Daily Hospitalization Reports are given directly to SHARE-connected providers and care teams, to assist with care coordination and patient follow-up.

Real-time notification of hospital visits (admissions, discharges, or ED transfers) for practices' active patients
Allows providers to proactively coordinate their patients' care and schedule any necessary follow-up treatments or visits
Assists in meeting value-based contract arrangements

The key to keeping everyone at the table is to effectively communicate the overarching goals to the entire team, he said. That also includes evaluating the communication. “I think it’s okay to constantly look in the mirror to say ‘Okay, are these thoughts in tune with where we need to go? And is there communication from the leadership for bringing everyone along?’ […] As long as you’re moving forward with your goals and have progress, then I call that a winwin for everyone,” he added.
Another key element to achieving forward progress lies in the community itself. Unlike other hospitals, Johnson Regional owns its own emergency medical services. From a financial standpoint, Hobbs notes that it can be more than difficult to manage but adds that there are benefits beyond the obvious ones. “We’ve done our best to grow that and serve the community well,” he said. “The number of times we go out to calls where people just need to see a face is stunning, and it truly is one of the biggest outreaches we could do for our community, beyond ensuring that they have the help they need when they need it.”
To that end, Hobbs is excited about the strides Johnson Regional has made in the past five years, although he’s quick to note that some of the momentum was in motion before he joined the facility. Highlights include bringing in a new orthopedic surgeon to join the existing team as well as a Mako robot for total joint replacements. “I’m extremely proud of that and excited about it because I think we know that there is certainly a need in the area,” he said. “The ability to provide care to our population is the most critical and is what I’m most proud of.”
Although Hobbs readily credits his team and predecessors for much of the hospital’s recent progress in patient



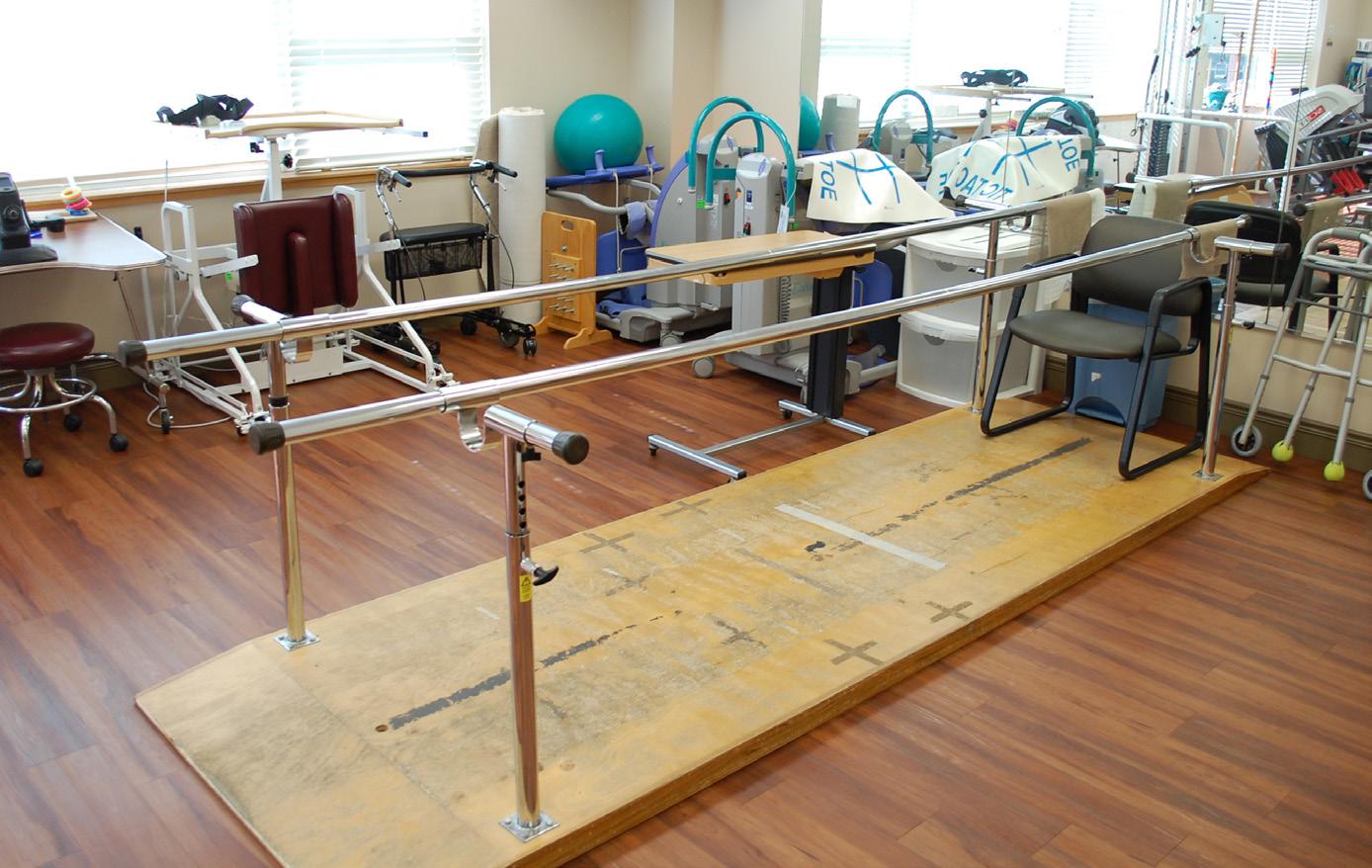
From physical therapy and orthopedics to labor and delivery, surgery, and a range of specialized care, Johnson Regional Medical Center remains a trusted source of care for the River Valley.

Proud blood supplier to over 40 Arkansas hospitals and transfusion sites.


care, he played a hands-on role in one particularly complex endeavor: selecting and implementing a new electronic medical records system. From planning to selection and implementation, finding a new system was not a quick or simple task.
“When you do something like this, you’re trying to improve patient care,” he explained. “And we believe that it will enhance our ability to have improved data flow, with the idea that our providers have the best information, the latest and most important information regarding their patients at their fingertips.”
Hobbs is quick to note that his team was integral to making the process run smoothly. “When you have a good chief information officer who is a very good project manager, that helps a lot,” he noted. The nine-month vetting process was informative, and ultimately, the hospital made the switch from Meditech to Cerner for electronic medical records.
Considering lessons learned, Hobbs notes that no shortcuts should be taken in evaluating and vetting different systems. He stressed the importance of training as well. “Ultimately, you also have to hold the appropriate people accountable for the training,” he explained.
In today’s world, it’s nearly impossible to update an element as important as an EMR system and not consider something as timely as artificial intelligence (AI) and innovation in the patient care delivery space. “How AI fits in the rural hospital at this point, I think, is yet to be determined,” Hobbs said.
However, switching systems helped to establish a starting point for further exploration of AI use-cases. “Going through this process, implementing the new system and getting that system working well, that’s our baseline for reevaluating how AI can further be brought in. We’ve taken a huge leap forward within the last two months,” he said.
I’m excited to see how this organization can become more of a beacon of what a rural health provider can be... We want to see how we can consistently best serve our community.
For Hobbs, staying up to date with innovation — whether it’s AI or something else entirely — goes back to that people-first mantra. “You always want people that are smarter than you, working around you,” he said. “You also have to be willing to understand your staff and understand the world.”
Now that the hospital has gone live with its new system, there have been quite a few positives. Patient care is at the forefront and the hospital continues to work to smooth out the bugs every day. On top of that, Hobbs noted, the switch has made capturing charges a more straightforward process. “We are seeing the uptick in the charges that we were expecting and hoping for,” he adds.
With Hobbs at the helm, Johnson Regional will continue to push forward in the patient care space, constantly evaluating ways to do things better and finding new ways to serve the community. The people-first mantra will always ring true.
“I’m excited to see how this organization can be become more of a beacon of what a rural health provider can be,” he said. “We want to see how we can consistently best serve our community.”


With a focus on innovation and patient-centered care, Johnson Regional continues to make significant advancements in health care delivery under Tommy Hobbs’ leadership.

The Role of AI in Reducing Clinician Burnout
Artificial intelligence is making waves in health care, promising to transform how organizations operate and deliver patient care. In a recent Qualivis webinar titled “Exploring the Role of AI in Reducing Clinician Burnout,” industry experts discussed the current landscape of AI applications in health care, the challenges of implementation, and the significant potential for AI to alleviate clinician burnout.
The session was moderated by Melanie Bell, RN, a consultant with expertise in nursing administration and workforce optimization. Joining her were Cristal McKay, Vice President of Customer Success and Workforce AI at Aya Healthcare, who focuses on using data and technology to advance health care; Barbara Bennett, a partner at Frost Brown Todd with deep expertise in AI governance and health care legal issues; and Taryn Overman, Associate Chief Nursing Officer at VHC Health, who has over 18 years of experience in health care leadership, particularly in operational and leadership development.
THE CURRENT STATE OF CLINICIAN BURNOUT
The session kicked off with an overview of the critical issue of clinician burnout. According to Crystal McKay, burnout among nurses is alarmingly high, with 63% of RNs reporting work-related burnout and 50% considering leaving the profession altogether. Burnout not only affects clinicians but also impacts patient care and organizational performance, leading to higher turnover, more vacancies, and frequent absences.
Nurses today are overwhelmed by administrative tasks such as documentation, care coordination, and medication administration, which leave little time for direct patient care. Crystal emphasized that nurses want more patient interaction, opportunities for professional growth, and less time spent on charting and administrative tasks.
AI AS A SOLUTION TO BURNOUT
AI offers promising solutions to these challenges by automating routine tasks, enhancing care coordination, and providing clinical decision support. Key AI applications discussed included:
• Documentation Support: AI can streamline documentation processes, making them more intuitive and less time-consuming. This allows nurses to spend more time with patients rather than on administrative tasks.
• Care Coordination: AI can automate the distribution of patient information to relevant providers, reducing the time nurses spend digging through records.
• Patient Safety and Risk Management: AI tools can predict fall risks, assess patient care needs, and help prioritize patients for discharge planning, ultimately improving patient outcomes.
• Staffing Optimization: AI can predict staffing needs based on historical data, create flexible schedules, and adjust staffing levels in real-time, aligning resources with patient demand.
OVERCOMING CHALLENGES: TRUST AND IMPLEMENTATION
Despite the potential benefits, the panel acknowledged that implementing AI in health care is not without challenges. A significant concern is trust — clinicians need to be confident that AI systems can understand the nuances of their teams and patient care.
Barbara Bennett highlighted the importance of governance and compliance in AI procurement, noting that AI systems differ from traditional software because they are dynamic and data-driven. Organizations must carefully evaluate data accuracy, bias, privacy, and security when implementing AI solutions.
Taryn Overman stressed the importance of involving all key stakeholders in the evaluation and implementation process, including frontline staff, IT, finance, and providers. She recommended keeping detailed minutes of all meetings and decisions to maintain continuity, especially if team members leave the organization.
THE ROLE OF CHANGE MANAGEMENT
Successful AI implementation requires robust change management. Taryn shared her approach of “socializing” the concept of AI by engaging staff early and frequently. She emphasized the need to prepare teams for change, involve them in the decision-making process, and provide adequate training and support.
Barbara echoed these sentiments, stressing that governance and documentation are critical. Organizations must establish clear policies, evaluate risks, and maintain thorough documentation to manage potential liabilities and ensure the safe use of AI.
MEASURING SUCCESS AND LOOKING FORWARD
The panelists agreed that measuring success is vital when implementing AI. They advised organizations to clearly define what success looks like, set realistic expectations, and continuously assess AI performance and its impact on clinician workload and patient care.
Taryn mentioned that VHC Health is exploring AI applications for virtual nursing, predictive analytics for patient safety, and enhancing patient experience by prioritizing rounding based on predictive data. She emphasized that AI should be seen as a partner, not a replacement for health care professionals.
FINAL THOUGHTS
AI has the potential to revolutionize health care by reducing clinician burnout, improving patient care, and enhancing operational efficiency. However, successful implementation requires careful planning, robust governance, and a commitment to supporting staff through the change. As health care organizations continue to explore AI, the focus must remain on leveraging these tools to create better, more sustainable work environments for clinicians.
For those interested in learning more about AI in health care, consider exploring AI tools already embedded in electronic medical records or predictive analytics applications to address specific clinical challenges. With the right approach, AI can be a powerful ally in the ongoing effort to combat clinician burnout and improve patient outcomes.


COMMUNITY OUTREACH: St. Bernards Medical Center

St. Bernards is expanding its innovative hybrid care model across its rural hospitals, ensuring patients receive high-quality care close to home.
Right Care, Right Place, Right Time
By Mitchell Nai l
The warmth of the conference room defied the cold, rainy weather outside.
This small war room, located along a brick-floor hallway inside St. Bernards Medical Center, housed 10 health care professionals, clinical and nonclinical alike. Nine people sat at a rectangular table. The tenth, Cynthia, stood casually by a large easel. She listened and recorded processes of how a partnering rural hospital facilitates patient care, from admissions to discharge or transfer. Taking copious notes, Cynthia wanted to know what worked and where the group saw opportunities to improve.
Overall, the meeting was not a critique of how health care is delivered to rural communities. It was an exploratory future filled with opportunities, where each person present had a specific role in addressing two major questions:
1. How do you keep patients close to home while receiving the appropriate level of care provided at higher acuity hospitals?
2. How do you maximize available capacity, personnel, and resources?
THE PLAN
Health care systems with rural service areas face unique opportunities, especially when their rural, community hospitals provide essential medical services like emergency, diagnostic, and observation care. St. Bernards Healthcare understands this environment all too well, operating three hospitals and helping with management of a fourth. Within its 23-county service region in northeast Arkansas and southeast Missouri, only one county has a population of more than 50,000 persons.
“It’s an unfortunate reality that patients and their families travel long distances to get the specialized care they need,” says St. Bernards Senior Vice President of Strategic Services Josh Conlee.
To combat this problem, St. Bernards is implementing a hybrid care model that intrinsically connects its system’s rural hospitals with its flagship hospital, St. Bernards Medical Center in Jonesboro.
“We landed on a hybrid care model because they show promising results nationwide where specialty medical
services are lacking or don’t exist,” Conlee says. “Our goal is to combine the skills of onsite and offsite providers by using advanced virtual technology.”
St. Bernards’ most recent enhancement to this model begins this year at Lawrence Memorial Hospital in Walnut Ridge, followed by St. Bernards Five Rivers Medical Center in Pocahontas and St. Bernards CrossRidge Community Hospital in Wynne. The system plans to have it fully implemented by year’s end.
“We want to have a seamless continuum of care that leverages all of our clinical and non-clinical resources,” says Conlee. “The hybrid care model facilitates full connectivity between all our facilities.”
SMART ROOM TECHNOLOGY: ENHANCING PATIENT EXPERIENCE AND ACCESSIBILITY
Through the introduction of smart room technology to rural communities, virtual nurses and physicians enhance patient care. This advanced system includes a mounted camera on top of the patient's television, which activates during virtual rounds.
Conlee explains how it works.
“When a nurse or doctor needs to see the patient, the TV displays an alert, requesting the patient’s permission for the camera to be activated,” he says. “The patient accepts the call before seeing the provider on the screen and talking to the provider. The provider, meanwhile, uses
the camera to communicate face-toface with the patient. The camera has an optical zoom that goes far enough to read the patient's information on their medical bracelet. When the call ends, everything shuts off, letting patients know they have full privacy. It's a remarkable system, and we can easily retrofit standard rooms into smart rooms.”
Beyond patient-provider communication, smart rooms allow family members to participate in discussions through a HIPAA-compliant virtual platform.
“We can connect multiple family members to a single group call,” Conlee says. “Important health decisions can be made collectively, and patients see their loved ones without needing to use their own devices.”
This capability fosters improved patient engagement and ensures that health care decisions are made with the support of caregivers.
VIRTUAL NURSING AND SPECIALTY CARE
With the addition of virtual nursing, the hybrid care model addresses potential staffing deficits and burnout, especially among nurses providing bedside care.
Emily McGee, St. Bernards Vice President of Nursing, says bedside nurses have numerous tasks to complete when they enter patient rooms. It can draw their attentions to checklists instead of personal encounters. A remote virtual nurse can help bedside nurses complete those tasks, giving them more quality patient visits


Emily
Josh Conlee work to refine processes that improve patient access, maximize resources, and enhance rural health care delivery.
St. Bernards Vice President of Nursing
McGee and St. Bernards Senior Vice President of Strategic Services
Arkansas Senior Health Insurance Information Program (AR










COMMUNITY OUTREACH: St. Bernards Medical Center
over a higher quantity of brief encounters.
“The virtual nurse is not located on the floor and can focus solely on patients and their emotional needs,” McGee says. “Not only do our bedside nurses appreciate having an extra set of ‘virtual’ hands, patients comment on how much more time the bedside nurse is able to spend with them. It has been a top-notch experience for our team and patients alike.”
The hybrid model also incorporates specialty physician consults via telemedicine. Initially, the program will include cardiologists, pulmonologists, and hospitalists, but St. Bernards plans to expand beyond doctors, involving other care providers like dietitians and pastoral care staff. Patients will have access to expert medical guidance without the need for long-distance travel, reducing financial and emotional strains on families.
“We know the struggle that families deal with related to caregiving and travel. Traveling impacts their work, home life, stress, pocketbook, and maybe even their health,” Conlee emphasizes. “We have to mitigate these adverse effects wherever we can.”
ADDRESSING FUTURE HEALTHCARE CHALLENGES
One of the driving forces behind this initiative is the evolving landscape of health care staffing and capacity concerns at tertiary hospitals. The health care industry currently faces workforce shortages across the country. Data and projections indicate that over the next decade, fewer caregivers will be available
Smart room technology at St. Bernards allows virtual nurses and physicians to connect with patients, enhancing care, reducing travel burdens, and supporting bedside staff.
Mitchell Nail serves as the Media Relations Manager for St. Bernards Healthcare.
for an increasing number of patients. It also means that hospitals will need more available beds.
“We expect to see an increase in older and younger persons alike needing health care over the next 10 years,” Conlee says. “Leveraging new technologies helps us create innovative strategies that meet the clinical needs of our patients while increasing capacity across our region. We’re taking health care to the patients rather than having them come to us.”
Conlee says he understands that St. Bernards has taken a bold strategy, but he adds that the system must act now to position itself for the next 10 years and beyond.
“When it comes to implementing anything new, I’ve always had a problem with the word ‘can’t.’ We may have challenges, but I believe we’ll find creative solutions. This is our opportunity to transform rural health care, and we’re going to provide the right care, at the right place, at the right time.”



COMMUNITY OUTREACH: Saint Mary’s Celebrates 100 Years
Saint Mary’s Celebrates 100 Years of Caring for the River Valley
In the past century, Saint Mary’s Regional Health System has evolved from a small community hospital to a regional leader in patient care. As the hospital celebrates its centennial year, it reflects on its lasting contributions to the River Valley’s health care landscape.
A LEGACY OF GROWTH AND INNOVATION
For 100 years, Saint Mary’s has evolved to meet the growing health care needs of rural communities in the region. Founded in 1925 by Dr. R.L. Smith, the hospital was named in honor of a nurse who cared for him during a life-threatening illness — a promise that has endured for a century.
Over the decades, Saint Mary’s has expanded its services and facilities to provide more accessible care. The hospital grew under Dr. Martin Heidgen’s leadership, increasing bed capacity and modernizing clinical services. Major expansions in the late 20th century doubled key departments, enhanced surgical and maternity care, and improved emergency services, while its partnership with Millard-Henry Clinic strengthened specialty care access.
Saint Mary’s expanded its services in the 21st century, introducing telemedicine, specialized programs, and emergency air transport through Survival Flight. The hospital enhanced stroke care, grew its behavioral health facilities, and achieved Chest Pain Accreditation. During the COVID-19 pandemic, it provided critical support through a dedicated triage clinic.
Most recently, Saint Mary’s has focused on strengthening neonatal care, expanding critical services, and investing in new technology like the Da Vinci Xi surgical robot to ensure the next 100 years are defined by the same dedication to innovation, growth, and compassionate care that has shaped its legacy.
CELEBRATING THE PAST, LOOKING TO THE FUTURE
Saint Mary’s centennial is more than just a celebration of the past — it is a commitment to the future of health care in Arkansas.
To mark this milestone, the hospital is celebrating yearround with a variety of events and initiatives, including badge reels featuring the 100-year seal, a historical timeline wall installation showcasing key moments from Saint Mary’s century of service, and a commemorative mural painted by local artists in the staff courtyard.






St. Mary’s will continue to celebrate its centennial throughout the year, marked by a special mayoral proclamation on Sept. 18.
This milestone would not be possible without the dedication of health care professionals, nor without the trust of the communities served by Saint Mary’s. This commitment to service inspired the launch of the 100 Acts of Service initiative. CEO Casey Willis stated, “Saint Mary’s was built on a foundation of service and compassion, beginning with a single act of kindness that inspired the hospital’s name. In recognition of this legacy, we want to give back to the community that has supported us for the past century.”
Saint Mary’s will also host a series of special events throughout the year, including a staff appreciation event on the 100th day of the year, as well as a community celebration, time capsule ceremony, and mayoral proclamation on Sept. 18.
ADVANCING RURAL HEALTH CARE FOR THE NEXT 100 YEARS
Looking ahead, Saint Mary’s remains committed to expanding services, investing in technology, enhancing patient care, and developing a strong workforce to ensure the next 100 is as impactful as the first.

This article was provided by Carleigh Powell, Marketing and Communications Manager, Saint Mary’s Regional Health System.
Arkansas Fruit and Vegetable RX Program

Innovation via Collaboration: Exploring the Arkansas Fruit and Vegetable RX Program
By Becca Bona
As vital employers, health care providers, and regional anchors, hospitals help form the cornerstone of what makes a community unique. Along that vein, nonprofit hospitals are required to conduct community health needs assessments every three years to keep their status, and in doing so they often discover issues that, once addressed, can help a community prosper. The rubber truly hits the road when hospitals can let that information drive strategy, collaboration, and ultimately, improve larger community health outcomes.
Food security is one of three top priorities identified from Baptist Health’s most recent needs assessment. While disheartening, this isn’t surprising, as more than 560,000 people experience food insecurity Arkansas, according to
Feeding America’s most recent food map data.1 However, there are a variety of actors working towards combating hunger, including the Arkansas Hunger Relief Alliance (the Alliance), a nonprofit founded in 2004 that collaborates as a statewide voice advancing equitable solutions to hunger. Their vision is to create a hunger-free Arkansas.
In 2022, the Alliance was awarded a USDA Gus Schumacher Nutrition Incentive Program Produce Prescription grant, which funds the Arkansas Fruit and Veggie RX Program — an ongoing three-year project. The Arkansas Fruit and Veggie RX program aims to increase fresh fruit and vegetable consumption by patients struggling with diet-related health conditions like obesity, high blood pressure, and diabetes. The program brings together health care providers and
The Arkansas Fruit and Veggie RX Program brings together strategic partners to provide nutrition education and fresh produce to patients in need, enhancing health outcomes and supporting food security across the state. From left to right: Samantha Stadter, Dawn Yoder, Teresa Conner, Alex Hendrickson, and Liam Hankins-Hill organize produce bags for pick-up.
researchers working to decrease the long-term health care costs associated with food insecurity and dietrelated conditions.
Baptist Health and the University of Arkansas for Medical Sciences are the designated health care providers, offering screening locations that also serve as produce pick-up points for program participants. Now in the early phases, the Alliance is working with 90 patients enrolled at three different Baptist Health Community Outreach Wellness Centers. UAMS will be onboarded in the next phase, via their Obstetrical Clinic for the Management of Hyperglycemia in Pregnancy.
Teresa Conner, System Director for Community Outreach at Baptist Health noted that signing onto the grant and partnering with the Alliance, UAMS, and research team was a brilliant way to lean into their most recent needs assessment. After opening food pantries in both Fort Smith and Little Rock, the Baptist Health Community Outreach team looked for other ways to combat food insecurity and bring nutrition education to the forefront.
“This partnership has been beneficial to the community and the individuals that we serve, so it’s definitely something we’ll continue,” Conner said. “We look for opportunities to partner with groups in the community so that we can expand or enhance what we’re already doing.”
Samantha Stadter, Registered Dietician with Baptist Health Community Outreach, worked with the Alliance before joining Baptist Health. Food security, access, and education are very important to her, especially from an overall health perspective. “We know that a lot of chronic diseases are related to the food you eat,” Stadter explained. “For people who have high blood pressure, diabetes, and obesity, the foods that they eat are an important part of getting treatment, finding care, and getting healthy.”
This partnership has been beneficial to the community and the individuals that we serve, so it’s definitely something we’ll continue.

Participants are deemed eligible for the Alliance’s Fruit and Veggie RX program if they are SNAP eligible or enrolled in Medicaid, and if they meet the screening requirement for a pertinent diet-related condition. They are then screened by community outreach nurses each time they pick up their produce. Participants also take part in a pre- and post-survey.
Baptist Health Community Outreach Nurses Dawn Yoder and Paula Launius conduct health screenings for participants in the Arkansas Fruit and Veggie RX Program.
COMMUNITY OUTREACH: Arkansas Fruit and Vegetable RX Program



Participants in the Arkansas Fruit and Veggie RX Program pick up their weekly supply of fresh fruits and vegetables, empowering them to make healthier dietary choices and manage chronic conditions like diabetes and hypertension.
The beauty of a strategic partnership like this one, is the ability to adapt, when appropriate, to achieve the best possible outcomes. For instance, the Alliance successfully secured Potluck Food Rescue as a partner to receive, pack fresh produce, and deliver bags to clinics. Because of this partnership, the Alliance was able to triple enrollment numbers in a matter of months.
“Whenever your resources are strapped and you don’t have a lot of cash … the foods that you choose tend to be those that aren’t necessarily great for our bodies,” Stadter explained. She is particularly excited about the variety of food available to participants in the bags: “By putting blueberries, avocados or peaches — it creates a way for families who may not be able to get those foods normally to try new stuff expand their food pallets in a way that doesn’t crash the food budget.”
A goal of the Alliance, along with Baptist Health’s Community Outreach team, has been to continue to find ways to provide further support. “We’re also working to provide extra nutrition education to bolster healthy foods,” said Alex Hendrickson, the Alliance’s Nutrition Education Program Manager. “We want to teach people some nice recipes, how to use their produce, and how to store it. It’s exciting to have a partnership where we can have a clear avenue to do that.”
So far, the anecdotal results from participants are promising, especially within Baptist Health’s Pregnancy Wellness Center. Pregnant women or those in the post-partum period face many risk factors, including hypertension. “What we've seen is better management of blood sugar, better management of their high blood pressure, which is really important and phenomenal,” Stadter said. She and the team attribute the positive direction to access and education, of course, but there’s another layer, too. “Coming in and checking up with somebody every month creates a little accountability, and also gives you the opportunity to catch something earlier on before it escalates.”
The Alliance’s Nutrition Programs Director Jami Kirksey noted that she is excited to file an extension with UAMS to continue the next phase. Kirksey was excited to share anecdotal evidence with research partners that seemed promising. One participant shared that they now reach for berries and apples instead of a bowl of candy they used to keep around. Kirksey recalled that the patient told their doctor, after discovering that their A1C was down from 6.5 to 5.5, they “hadn’t had access to healthy foods until now.”








Integrating Innovation with Healthcare
By Kay Kendall
The term “innovation” was added to the Glossary of the 1999 Criteria for Performance Excellence for the Baldrige National Quality Program. Since then, it has continued to evolve and increase in importance, showing up in higher levels of organizational maturity in the Scoring Guidelines and having a place in the Baldrige Core Values and Concepts under, “Focus on Success and Innovation.”
When innovation was added to the Criteria by the Baldrige Program, I was a Senior Examiner and, a few years later, was a Judge. I confess, at first, I had difficulty with thinking of innovation in health care unless we were assessing a teaching or research hospital. Innovation, in my mind, was associated with in-depth research, patents, and engineers and scientists. What place did it have in critical access rural hospitals, freestanding clinics, and even nursing homes? But a careful review of how Baldrige defines innovation convinced me that it applies to every possible health care (and other sector) settings.

“Innovation(s): Making meaningful change to improve products, services, the organization, or societal well-being to increase value for stakeholders …. Innovation involves adopting an idea, technology, service, or business model that is either new or new to its proposed application. Innovation benefits from a supportive environment, a process for identifying strategic opportunities, and a willingness to pursue intelligent risks.”1
There are several key elements in the Baldrige definition and Core Value and Concept of innovation. One is the inclusion of the cultural aspects necessary for being an innovative organization, a supportive environment. What is meant by a supportive environment? First, it not only allows for all levels of the organization to make suggestions for improvement and innovation, but the senior leaders also make it clear that participation at all levels is expected. A second key element, which is also defined in the Baldrige Glossary, is having a systematic process in place to identify strategic opportunities.
“They arrive from outside-the-box thinking, brainstorming, capitalizing on serendipity … and other approaches to imagine a different future.” A third key element is a tolerance for intelligent risk, “Taking intelligent risks requires a tolerance for failure and an expectation that innovations are not achieved by initiating only successful endeavors.”
How do you instill these factors in your organization?
CREATING A SUPPORTIVE ENVIRONMENT
Brian Dieter, CEO of Mary Greeley Medical Center (and one of our clients), begins with the interview and onboarding process where he tells every job candidate that they have two jobs, do their job and improve their job. He reinforces this at his monthly Town Hall meetings. And he serves as a role model by devoting four hours a week to personally facilitate value stream mapping and process improvement in various departments throughout the medical center. It was no surprise to us when Mary Greeley Medical Center won the Baldrige Award in 2019.
A SYSTEMATIC PROCESS TO IDENTIFY STRATEGIC OPPORTUNITIES FOR INNOVATION
Does your organization have a knee-jerk response to new ideas that goes something like this, “But, we’ve always done it this way!” If yes, you’re likely to be overlooking strategic opportunities. As the Baldrige Glossary says, “The generation of ideas that lead to strategic opportunities benefits from an environment that encourages non-directed, free thought.” It’s easy to understand why this may sound counterintuitive in the world of health care that often seems hamstrung by layers and layers of requirements and regulations. However, not every action is under strict control, and exploring ways to add new value, make meaningful change, and create breakthrough improvements is not only useful but engages employees in ways to make their work more productive and more efficient. Involving people closest to the work is a proven way to get buy-in and rapid adoption of process changes.
Endnote
1. Baldrige Performance Excellence Program, 2023, 2023—2024 Baldrige Excellence Framework® (Health Care) Proven Leadership and Management Practices for High Performance. Gaithersburg, MD; U.S. Department of Commerce, National Institute of Standards and Technology. https://www.niost.giv/baldrige.
A TOLERANCE FOR INTELLIGENT RISK
I often ask clients’ senior leaders when was the last time someone came to their office to tell them something they might not want to hear. The point of that question is to determine if they promote frank, two-way communication, which is a Baldrige hallmark of transparency in leadership. One of our long-term care client’s Executive Director (ED) told us that one Monday morning when she got to work, a Care Coordinator came to her office to talk about an intelligent risk she had taken over the weekend. The center was discharging a patient to home, but the ordered assistive equipment had not yet been delivered. To promote a safe discharge, the Care Coordinator “raided” the rehabilitation center and “borrowed” the needed equipment, a wheelchair. The ED praised the staff member for quick thinking and a creative approach to being empowered to provide a temporary solution to the problem. This is also an example of the positive use of any organization’s grapevine because that story was repeated throughout day to other staff members who were then encouraged to take intelligent risks themselves.
A CALL TO ACTION
What one or two steps could you take today to encourage innovation in your organization? And what one or two steps could you take this week to reinforce a culture of continuous improvement and innovation?


The team at BaldrigeCoach would be glad to help guide your hospital’s quest for process improvement. As CEO and Principal of BaldrigeCoach, Kay Kendall coaches organizations on their paths to performance excellence using the Malcolm Baldrige National Quality Award Criteria as a framework. Her team, working with health care and other organizations, has mentored 25 National Quality Award recipients. In each edition of Arkansas Hospitals, Kay offers readers quality improvement tips from her coaching playbook. Contact Kay at 972.489.3611 or Kay@Baldrige-Coach.com.

Impact of Arkansas Medicaid's Inpatient Quality Incentive Program: Nearly Two Decades of Progress
By Steve Chasteen, Administrator of Research & EBP Outreach, AFMC
Over the past 50 years, the rate of cesarean section deliveries in the United States has risen dramatically, from 5% of all births in 1970 to a peak of 33% in 2009.1,2 While this rate has slightly declined to 32% as of 2020, induced deliveries have surged by 223% between 1990 and 2020, now accounting for 31% of all U.S. births. 3,4 C-sections, while lifesaving in medically necessary cases, can pose significant risks when performed without clear medical indications. The rise in preterm C-sections between 1990 and 2004 contributed to improved perinatal survival due to reductions in stillbirths.5 However, non-medically indicated C-sections are associated with increased risks for newborns, 6 long-term health concerns for children,7,8 and surgical complications for mothers.6,8
Since the mid-2000s, professional guidelines and public health initiatives have promoted delaying elective deliveries until at least 39 weeks of gestation. While these efforts have helped curb the rapid rise in C-sections and induced deliveries, their rates remain close to historical highs.9 Notably, while earlier increases in C-sections were linked to reductions in infant and fetal mortality, more recent


increases have not yielded the same benefits. 10 Additionally, maternal mortality has risen by 19% between 2000 and 2017, reflecting broader health challenges.11,12
For nearly two decades, Arkansas Medicaid, in collaboration with the Arkansas Foundation for Medical Care, Arkansas Hospital Association, and health care quality professionals, has worked to improve patient care through the Inpatient Quality Incentive program. This initiative demonstrates the power of collaboration and innovation in addressing health care challenges across the state.
THE IQI PROGRAM: ADVANCING MATERNAL AND INFANT HEALTH


Advertise to Hospitals Across Arkansas
Contact: Brooke at Magazine@arkhospitals.org for Arkansas Hospitals ad options.

Scan to read the past editions of Arkansas Hospitals arkhospitals.org

The IQI program supports hospitals statewide in tracking and improving key health care quality measures. An advisory committee — comprising quality directors, hospital staff, and representatives from Arkansas Medicaid/Division of Medical Services, AFMC, and AHA — selects, analyzes, and validates these measures. Hospitals that demonstrate improvements receive bonus payments as incentives. While all Arkansas and border-state hospitals accepting Medicaid reimbursement can participate, only acute care hospitals qualify for incentive bonuses.
Among the key maternal health indicators tracked through IQI are early elective deliveries and low-risk cesarean deliveries. The program has achieved significant progress:
• Early Elective Deliveries: The national target rate for early elective deliveries is 5%. Arkansas hospitals participating in the IQI program have dramatically reduced their EED rate from 25.7% in SFY 2011 to just 2.42% in SFY 2024 — a 90.6% reduction.
• Low-Risk Cesarean Deliveries: The national average for low-risk, first-time C-sections is 24.6%, according to the Leapfrog Group.13 Arkansas's IQI program has helped reduce the state's rate from 28.4% in SFY 2013 to 20.5% in SFY 2024 — a 28% decrease.
The persistently high rates of elective C-sections and inductions underscore the need for continued health care interventions. The IQI program has played a crucial role in addressing these issues by promoting adherence to updated medical guidelines and fostering ongoing improvements in maternal and neonatal health outcomes.
EXPANDING IQI: TOBACCO CESSATION AND SUICIDE RISK SCREENING
Beyond maternal health, the IQI program has broadened its focus to include tobacco cessation and suicide risk screening — two critical areas impacting public health.
Tobacco Cessation
Tobacco use remains the leading cause of premature disease and death in the U.S., contributing to hospitalizations for cancer, stroke, cardiovascular disease, respiratory conditions, and pregnancy-related complications. 14,15 Additionally, smoking interferes with post-surgical recovery, delaying bone and wound healing while increasing infection risks.
Hospitals provide an ideal setting to support tobacco cessation efforts, and all U.S. hospitals must maintain smoke-free environments to meet accreditation standards. Arkansas hospitals have adopted smoke-free campus policies, and since introducing tobacco cessation measures into the IQI program, year-over-year performance improvements have been consistently observed.
Suicide Risk Screening
Suicide is the 11th leading cause of death in the U.S., with rates continuing to rise.16,17 In 2022, Arkansas had an age-adjusted suicide rate of 18.0 — a 28.6% increase over the past two decades.18 On average, a person dies by suicide every 14 hours in the state, and 1 in 10 suicide victims had visited an emergency department within two months before their death.
Despite existing national guidelines for suicide screening and follow-up care, gaps in emergency department screenings have persisted. Recognizing this critical issue, the IQI program incorporated suicide risk screening as a quality metric in 2018. Initial baseline screening rates were 82.5%, but screenings have improved to 97.6% — an 18.3% increase.
A COMMITMENT TO ONGOING IMPROVEMENT
The Arkansas Medicaid IQI program has demonstrated the value of a collaborative, data-driven approach to health care improvement through nearly two decades of progress. By focusing on maternal health, tobacco cessation, and suicide prevention, the program has made a measurable impact on hospital quality and patient outcomes statewide. Continued investment in these initiatives will help ensure that Arkansas remains at the forefront of health care quality improvement for years to come.

References
1. Placek PJ, Taffel SM. Trends in cesarean section rates for the United States, 1970--78. Public Health Rep. 1980 Nov-Dec;95(6):540-8. PMID: 7433601; PMCID: PMC1422801.
2. Martin JA, Hamilton BE, Osterman MJ, Driscoll AK, Mathews TJ. Births: final data for 2015. National Vital Statistics Report. 2017;66(1):1. https://www.cdc.gov/nchs/data/nvsr/nvsr66/nvsr66_01.pdf.
3. Osterman MJ, Hamilton BE, Martin JA, Driscoll AK, Valenzuela CP. Births: final data for 2020. National Vital Statistics Report. 2022;70(17):1–50. https://www.cdc.gov/nchs/data/nvsr/nvsr70/nvsr70-17.pdf.
4. Osterman MJ, Martin JA. Recent declines in induction of labor by gestational age. NCHS Data Brief. 2014(155):1–8. https://www.cdc.gov/nchs/data/databriefs/db155.pdf.
5. Ananth CV, Vintzileos AM. Trends in cesarean delivery at preterm gestation and association with perinatal mortality. American Journal of Obstetrics & Gynecology. 2011;204(6):505. e1−505.e8.e5058. https://doi. org/10.1016/j.ajog.2011.01.062.
6. Teitler JO, Plaza R, Hegyi T, Kruse L, Reichman NE. Elective deliveries and neonatal outcomes in full-term pregnancies. American Journal of Epidemiology. 2019;188(4):674–683. https://doi.org/10.1093/aje/kwz014.
7. Black M, Bhattacharya S, Philip S, Norman JE, McLernon DJ. Planned Cesarean Delivery at Term and Adverse Outcomes in Childhood Health. JAMA. 2015 Dec 1;314(21):2271-9. doi:10.1001/jama.2015.16176. PMID: 26624826; PMCID: PMC5055095.
8. 8. Liu KY, Teitler JO, Rajananda S, et al. Elective deliveries and the risk of autism. American Journal of Preventive Medicine. 2022;63(1):68–76. https://doi.org/10.1016/j.amepre.2022.01.024.
9. Buckles K, Guldi M. Worth the wait? The effect of early term birth on maternal and infant health. Journal of Policy Analysis and Management. 2017;36(4):748–772. https://doi.org/10.1002/pam.22014.
10. March of Dimes. 2023 March of Dimes Report Card for the United States. https://www.marchofdimes.org/peristats/reports/united-states/report-card
11. Pregnancy mortality surveillance system. Centers for Disease Control and Prevention. https://www.cdc.gov/maternal-mortality/php/pregnancy-mortality-surveillance/?CDC_AAref_Val=https://www.cdc.gov/ reproductivehealth/maternal-mortality/pregnancy-mortality-surveillance-system.htm
12. Teitler JO, Chegwin V, Li L, Liu K, Bearman PS, Gorney-Daley MA, Reichman NE. Trends in Elective Deliveries in California and New Jersey. AJPM Focus. 2022 Nov 24;2(1):100052. https://doi:10.1016/j. focus.2022.100052. PMID: 37789944; PMCID: PMC10546565.
13. The Leapfrog Group. Factsheet: Maternity Care – Leapfrog Ratings. https://ratings.leapfroggroup.org/sites/default/files/inline-files/2023%20Maternity%20Care%20Fact%20Sheet.pdf
14. National Center for Chronic Disease Prevention and Health Promotion (U.S.) Office on Smoking and Health. The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General. Atlanta (GA): Centers for Disease Control and Prevention (U.S.); 2014. http://www.ncbi.nlm.nih.gov/books/NBK179276/.
15. National Center for Chronic Disease Prevention and Health Promotion; Office on Smoking and Health. Cigarette Smoking. Atlanta (GA): Centers for Disease Control and Prevention (U.S.); 17 September 2024.
16. Centers for Disease Control and Prevention. (2024). Web-based Injury Statistics Query and Reporting System (WISQARS). Atlanta, GA: National Centers for Injury Prevention and Control, Centers for Disease Control and Prevention. https://www.cdc.gov/injury/wisqars/index.html.
17. Substance Abuse and Mental Health Services Administration. (2023). Key substance use and mental health indicators in the United States: Results from the 2022 National Survey on Drug Use and Health (HHS Publication No. PEP22-07-01-006, NSDUH Series H-57). Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. https://www.samhsa.gov/ data/report/2022-nsduh-annual-national-report.
18. USAFacts. How many people die by suicide in Arkansas each year. (19 July 2024). https://usafacts.org/answers/how-many-people-die-by-suicide/state/arkansas/
The Promise of AI in Health Care
Artificial intelligence is driving rapid change in health care, generating discussions around its value and the need to understand and mitigate possible negative impacts.
A recent survey found that most Americans are both comfortable with AI in health care and recognize its potential benefits:
75% believe using AI to minimize human errors is important.
71% would like AI to reduce wait times.
70% are comfortable with AI taking notes during an appointment.
66% believe AI should improve work-life balance for health care providers.
Sources: Artificial Intelligence and Health Expert Webinar Series. NIHCM. (2024); Survey finds most Americans are comfortable with AI in health care. The Ohio State University Wexner Medical Center. (August 2024)

What does it mean to be taken care of?
At Arkansas Blue Cross and Blue Shield, it means providing peace of mind. We’ve been taking care of Arkansans for over 75 years, providing affordable, reliable health insurance … to keep Arkansans healthy and to help them heal. We’re investing in communities to keep this diverse and wonderful state strong. We’re committed to a whole person approach to health, including physical and behavioral well-being. And we recognize that total health is influenced by many factors, including medical history, genetics, lifestyle, environment, nutrition, safety and physical activity. We also realize that it will take all healthcare providers working together to ensure future generations of Arkansans can live their best life their whole life long. Let’s take good care, Arkansas.




WE BUILDPlaces for Healing
For the past 75 years, Nabholz has spent every day looking forward. Our extensive work on healthcare facility projects reflects our dedication to the future by giving medical professionals and the surrounding communities the tools they need to succeed.
