
WE BELIEVE

WE BELIEVE

Jennifer L. Smith, JD, RN, CEN
Jennifer rejoins WLJ after working in house at the state’s only academic health sciences university, and she previously practiced as a registered nurse. With 18 years of health law experience, Jennifer provides a wealth of knowledge to guide clients through regulatory, administrative and compliance concerns.

Scott Provencher
Scott Provencher is a healthcare lawyer who assists clients in matters related to compliance with HIPAA and HITECH, the Physician
Self-Referral (Stark) Law, Anti-Kickback and EKRA Statutes, and EMTALA. He also counsels hospitals, physicians, pharmacists and other healthcare providers regarding contracts, proceedings before state licensing boards, and issues related to credentialing and peer review.


With 50+ years of experience and expertise, our dedicated team has a successful history of delivering exceptional value to Arkansas providers.
• AFMC EngageSM: Comprehensive Contact Center Services
• Data Sciences: Better Data for Better Health Care
• Outreach Services: A Lifeline to the Provider Community
• Practice Transformation: Your Guide to Value Based Care Success
• Security Risk Analysis: Because Patient Trust Starts with Secure Data
• Event Planning Services: Memorable Events, Minus The Stress
Visit afmc.org to find out more.

Conveniently located in downtown Little Rock, our newly renovated event space offers free parking, seating for up to 100 attendees, a state-of-the-art A/V system, virtual conferencing options, and a fully equipped catering kitchen.
Let us help you plan your next conference, meeting, or community event – contact us to reserve your spot! Visit afmc.org/events for more information.

Arkansas Hospitals
by The Arkansas Hospital Association 419 Natural Resources Drive | Little Rock, AR 72205
To advertise, please contact Brooke Wallace magazine@arkhospitals.org
Becca Bona, Editor in Chief
Katie Hassell, Graphic Designer
Roland R. Gladden, Advertising Traffic Manager
BOARD OF DIRECTORS
Larry Shackelford, Fayetteville / Chairman
Greg Crain, Little Rock / Chairman-Elect
Michelle Krause, MD, Little Rock / Treasurer
Ron Peterson, Mountain Home / Past-Chairman
Ryan Gehrig, Fort Smith
Crystal Bohannan, Hot Summers
Connie Castleberry, Camden
Sammie Cribbs Roberson, Harrison
David Deaton, Clinton
Phil Gilmore, Crossett
Michael Givens, Jonesboro
Tommy Hobbs, Clarksville
Charlotte Jackson, Searcy
Eric Pianalto, Rogers

Brian Thomas, Pine Bluff
Matt Troup, Conway
Cody Walker, North Little Rock
EXECUTIVE TEAM
Robert “Bo” Ryall / President and CEO
Jodiane Tritt / Executive Vice President
Tina Creel / President of AHA Services, Inc.
Pam Brown / Vice President of Quality and Patient Safety
Lyndsey Dumas / Vice President of Education
Debbie Love / CFO



The best way to solve a problem is to narrow it down and identify it.
There are no simple problems in health care, and achieving progress is often rooted in collaboration. We see this firsthand in our ongoing efforts to improve maternal health outcomes across Arkansas, a cause that has moved from unfavorable statistics to a statewide priority.
In March 2024, Governor Sarah Huckabee Sanders established the Strategic Committee for Maternal Health, providing a centralized location for advocates to catalog information and provide recommendations. The committee’s dedicated work provided lawmakers with the data necessary to create policy to improve health outcomes. The 95th General Legislative Session saw significant victories for maternal health, including the Healthy Moms, Healthy Babies Act, which provided crucial funding through Medicaid to solidify resources for new and expecting mothers.
These early wins, however, are just the beginning. Improving maternal health is complex, and it will require sustained effort from hospitals, health care professionals, state agencies, lawmakers, and advocates to make a lasting impact. The initial energy and legislative action are crucial, but are not a stopping point. We must continue working together to improve outcomes and avoid health
care deserts. Improving maternal health in the state is a powerful example of how a unified voice and shared purpose can lead to real change.
In fact, working to change an unfavorable outcome is at the heart of patient care. Just as improving maternal health involves so many moving parts — from policy to collaboration and community support — so does providing quality care to every patient. Patient care is more than just a single appointment or procedure, it’s the whole process from the first consultation to the final followup. It’s about capturing detailed patient information, streamlining processes, and maintaining compliance with an evergrowing list of regulations.
We know these administrative and reporting burdens can seem endless. It can be easy to get caught up in achieving

the best quality metrics or HCAHPS scores, but it all comes back to the patient at the end of the day. The reason most of us go into health care is to help others. The desire to serve drives us to fight for more resources and better care for everyone, not just for new mothers, but for every Arkansan.
In this issue of Arkansas Hospitals, we share stories of teams and individuals doing just that. You’ll find compelling examples of how our member hospitals are providing exceptional care by staying rooted in their mission. You will also see a dedicated section on maternal health, including highlights from the roundtable we co-hosted with the Arkansas Center for Women & Infants’ Health this past August. The roundtable brought together diverse voices and perspectives, showcasing the kind of collaborative spirit that will be necessary to continue our progress.
We continue to monitor the movement on Capitol Hill, working to advocate for resources for our member hospitals. By staying grounded in our shared mission to support our member hospitals we can advocate for the policies that empower them to do what they do best. The work is not easy, and the challenges are real, but our purpose is clear. Together, we can build on progress, working toward better maternal health outcomes and advocating for every patient in Arkansas.

Bo Ryall President and CEO

Coconut cream pie, the kind that comes in a round, flakybut-moist, decorative shell not unlike a large donut. The little flakes of coconut shifted on the drive over, but that didn’t make my Grandma’s face any less game, cracked with a smile wider than the Arkansas River.
It was her 94th birthday, and I’m sure she didn’t have plans to spend it in a rehabilitation unit at a local hospital. But that’s where we found her, arms laden with balloons, cards, and birthday surprises as we trekked in.
By the time you’re in a hospital, it might feel daunting and extremely clerical with a mysterious rhythm. Maybe you are in a waiting room while you wonder about a loved one,

unsure of the news you crave beyond the closed double doors. Or perhaps you’re a new mom, nervous to give birth for the first time, and unsure what the future holds.
Whether a patient or a loved one, what you remember most about a hospital visit isn’t necessarily the science or minutiae of the care you receive. You remember how you were treated by the doctors, nurses, and staff who attended to you.
And that’s truly the heartbeat of a hospital — it all comes down to patient care. This issue is dedicated to those superheroes who are going above and beyond, all across the Natural State, meeting patients where they are. Whether it’s a home-health visit or the legislative work being done to ensure all Arkansas mothers have access to care, these health advocates and heroes share a staunch belief: a patient is more than a number. A patient comprises all their life experiences, of everyone they have touched and loved up until that point, and all the possibilities of what they can do once they leave through the hospital doors.
A patient is also made of the legacies they leave behind. When my family worked with a hospice team for my Grandma, I knew we were in good hands. They saw her for who she was: a matriarch of a rowdy, multi-generational family, once
full of stories and life, who just happened to be in immense pain. The kind words and little gestures that go above and beyond, to truly make someone feel seen — that’s what it’s all about.
This issue of Arkansas Hospitals highlights the crucial work in maternal health care that extends beyond the delivery room, ensuring mothers and babies are supported long after they leave the hospital. The health care community must work together to improve outcomes across the state. We can’t forget that we’re working to change statistics, but we can’t do that without putting patients at the forefront. We must keep them there to propel our movement forward.
These pages also highlight hospital changemakers dedicated to going above and beyond providing the bare minimum of care. From the cozy AshleyBrew Café at Ashley County Medical Center to the nursing governance at Saline Health System, individuals are waking up every day and going to their jobs, determined to make a difference.
These pages are meant to inspire, especially in a world constantly rocked by regulatory burdens, facing a financial crisis of the cost of care. Sometimes the best way forward is to get back to the basics — with the patient as the heartbeat of health care.

Becca Bona Incoming Editor in Chief

October 24
Society for Arkansas Healthcare Purchasing and Materials Management (SAHPMM) 2025 Fall Conference
AHA Classroom, Little Rock
November 3
2025 Fall Patient Experience Collaborative
CHI St. Vincent Hot Springs
November 5
AHA 2025 Healthcare Cybersecurity Alliance for November
AHA Classroom, Little Rock
November 7
Arkansas Society for Directors of Volunteer Services (ASDVS) 2025 Fall Conference
Location TBD
November 11
Stop the Bleed Program (2 Classes)
AHA Classroom, Little Rock
November 12
Code of Ethics: Surprisingly, not a Sleep Aid!
Virtual Event
November 12
Emergency Medical Transportation Solutions: Connections with Care
Virtual Education
December 17
CPT 2026 Procedure Coding Changes
Virtual Education
Register for AHA Events Online!
Employees of AHA member hospitals can now log in to www.arkhospitals.org and register for events online.
Scan this code for our event page.

By David Wise

Representatives from Baxter Health accept their platinum banner for their accomplishments during the ARPQC’s recently completed “Safe Reduction of Primary Cesarean Birth” initiative. (Photo Provided)
Birthing hospitals are being recognized for their quality improvement work by The Arkansas Perinatal Quality Collaborative (ARPQC), awarding platinum or silver partner banners to 20 birthing hospitals that achieved participation milestones.
“We are extremely proud of the effort and accomplishments of the hospitals that participated in the initiative promoting vaginal birth,” said Jennifer Callaghan-Koru, Ph.D., MHS, executive director of the ARPQC and an associate professor in the Fay W. Boozman College of Public Health at the University of Arkansas for Medical Sciences (UAMS). “These banners communicate their strong commitment and accomplishments in maternal safety to their patients and communities.”
The ARPQC is a network of health care organizations and experts that come together to improve maternal health care in the state. Since it was founded in 2022, the ARPQC has completed two initiatives focused on safely reducing cesarean birth rates and preventing congenital syphilis. While the ARPQC is coordinated by UAMS, all birthing hospitals in the state have participated and contributed to achieving the ARPQC’s mission to ensure a healthy start for all mothers and babies in Arkansas.
This month, the ARPQC is recruiting hospitals to participate in its third initiative focused on maternal health and well-being in the postpartum period. The initiative, “Postpartum Comprehensive Assessment, Resources and Education (CARE),” will support birthing hospitals to improve education and screenings for women before they are discharged from the hospital after birth.
“Over half of maternal deaths in Arkansas occur postpartum,” said William “Sam” Greenfield, M.D., MBA, medical director for the ARPQC, chair of the Arkansas Maternal Mortality Review Committee and professor in the UAMS Department of Obstetrics and Gynecology. “By proactively addressing the postpartum health needs of new moms, we can prevent deaths and hospital readmissions.”
For the Postpartum CARE initiative, the ARPQC is partnering with the new Arkansas Center for Women and Infant’s Health. Hospitals that participate will receive support with implementing best practices, such as free staff training, clinical tools and presentations from national experts. Participation in the state perinatal quality collaborative is also one of the criteria for a “birthing friendly hospital” designation from the Centers for Medicare and Medicaid Services.
“I’m especially encouraged by the upcoming postpartum initiative — it will help us strengthen follow-up care, better screen and support new moms’ physical and mental health, and build the community connections that make recovery safer and more sustainable for families,” said Michelle Pimentel, director of nursing for women’s and infant’s health at Conway Regional Medical Center, which was awarded a platinum banner by ARPQC.
Hospitals that were recognized with platinum banners for their accomplishments during the ARPQC’s recently completed “Safe Reduction of Primary Cesarean Birth” initiative include:
• Arkansas Methodist Medical Center
• Baptist Health, Arkadelphia
• Baptist Health, Conway
• Baptist Health, Drew County
• Baptist Health, Fort Smith
• Baptist Health, Little Rock
• Baxter Health
• Conway Regional Health System
• Mercy Northwest Arkansas
• NEA Baptist Memorial Hospital
• St. Bernard’s Regional Medical Center
• UAMS Medical Center
• White River Medical Center
Hospitals that were recognized with silver banners include:
• Baptist Health, North Little Rock
• Baptist Health, Stuttgart
• Great River Medical Center
• Jefferson Regional Medical Center
• National Park Medical Center
• Ouachita County Medical Center
• Washington Regional Medical Center
“The ARPQC has been a critical factor in enabling Great River to deliver the high-quality care we have achieved,” said Leah Wooldridge, obstetrics director at Great River Medical Center in Blytheville. “Over the past year, the ARPQC has played a pivotal role in the professional growth of our staff and the OB care team. The education provided through each initiative is invaluable, as small rural hospitals often lack alternative resources. By joining the ARPQC, we have gained access to vital resources and collaborative support that have empowered us to implement meaningful changes.”



In a unique collaboration with the Cherokee Nation supporting health care throughout the region, Mercy broke ground on an expansion of oncology services in Fort Smith, an effort to grow access to cancer care for patients on Aug. 8.
In collaboration with the Cherokee Nation, Mercy broke ground on an expansion of oncology services in Fort Smith to grow access to cancer care for patients. The new 40,000-square-foot cancer center will bring together Mercy Fort Smith’s current oncology services, at 7001 Rogers Ave., by moving radiation therapy and expanding infusion services. Plans include upgraded and additional linear accelerators, advanced radiation and imaging, additional infusion chairs and more. The renovation and expansion project has an estimated cost of $41 million, with possible additional phases bringing the total to $55 million. The current timeline calls for construction and renovation of the new cancer center to be completed in spring 2027.
Baptist Health is the first in Arkansas to implement the POST-BIRTH Warning Signs Toolkit, a nationally recognized set of essential resources created by the Association of Women’s Health, Obstetric and Neonatal Nurses. The kit assists nurses and other providers in educating women about the signs and symptoms of potentially life-threatening conditions that can occur after they have given birth.
The South Central Telehealth Resource center, housed at the University of Arkansas for Medical Science (UAMS), has received a $1.3 million, four-year grant from the Health and Resources and Services Administration to implement and expand digital health services. Part of the HRSA Telehealth Resource Center Program that supports regional and national telehealth resource centers, the grant will award $325,000 in funding each year through 2029. The funds will support ongoing efforts to develop, maintain, and expand digital health services and training for health care providers across Arkansas, Mississippi and Tennessee.
UAMS announced a collaboration with Alice L. Walton Foundation, Heartland Whole Health Institute, Mercy and Washington Regional Medical Center to expand its existing Certified Registered Nurse Anesthetist program to the UAMS Northwest Regional Campus in Fayetteville beginning fall 2025. This is the first CRNA program in Northwest Arkansas. The investment in the expansion is composed of $2 million from the Alice L. Walton Foundation and $500,000 each from Mercy and Washington Regional.

Magnolia Regional Medical Center announced the appointment of William D. Giles as the organization’s new Chief Executive Officer. Giles brings over 30 years of experience in health care and financial leadership, including an extensive background in improving operations in rural healthcare settings. Throughout his career, Giles has served in both CEO and CFO roles in various health care settings across the country. Giles holds a Bachelor of Business Administration from Baylor University and is a member of the American College of Healthcare Executives.
Construction on The National Center for Opioid Research & Clinical Effectiveness , a collaboration between Arkansas Children’s Hospital and the Arkansas Attorney General’s Office, began in August. The building will open in 2027. NCOR is a first-of-its-kind center dedicated to understanding the effects of the opioid crisis and other substance misuse on the fetus, newborns, developing children and adolescents, as well as pregnant and parenting individuals. The 65,000-square-foot facility, part of the Arkansas Children’s Research Institute will offer research and community outreach. Dr. Alicia Allen, a distinguished behavioral epidemiologist and expert in opioid use disorder, has been named as NCOR’s director.
The Arkansas Department of Human Services, Division of Children and Family Services and the Arkansas Department of Health announced in July that the Baby & Me program expanded into Johnson, Pope, and White Counties. That brings the total number of counties offering the program to 18. Baby & Me is an innovative program that provides parenting education to pregnant women and parents of newborns who receive benefits at Women, Infants & Children clinics. The seven-month curriculum includes a lesson on essential parenting skills as well as activities aimed at promoting parent and child interactions.
C. Lowry Barnes, M.D., professor and chair of the Department of Orthopaedic Surgery at the University of Arkansas for Medical Science , has been named interim chancellor of the university and began his role on July 11. Barnes replaced Cam Patterson, M.D., who served as chancellor and UAMS health chief executive officer for seven years before. A national search is underway to find UAMS’s next permanent leader, and an advisory search committee representative of UAMS campus leaders, community constituents and a member of the Board of Trustees of the University of Arkansas. The committee will assist in the cultivation of a short list of final candidates for UA System president Jay Silveria to take his top pick to the Board of Trustees of the University of Arkansas.
Ashley County Medical Center dedicated its Safe Haven Baby Box at the hospital’s 1015 Unity Road location on Wednesday, Aug. 20, in a special blessing ceremony attended by community leaders and hospital officials. The Baby Box is designed to offer a secure, anonymous option for parents in crisis. When the door is opened, it activates a silent alarm that notifies first responders, who are expected to arrive within five minutes. The box is equipped with a hospital-style Moses basket to ensure the baby’s comfort and safety. Once the infant is placed inside and the door is closed, it locks to secure the child until help arrives.
Northwest Health announced Juli McWhorter, RN, BSN, MSN, as the Chief Executive Officer at Northwest Medical Center - Bentonville. Together she and Northwest Medical CenterSpringdale CEO Kory Browning will coordinate the Northwest Health market in Northwest Arkansas.

The Eureka Springs Hospital Commission named Tiffany Means as Eureka Springs Hospital’s new CEO, effective Aug. 1, 2025. Tiffany holds a Doctor of Nursing Practice, a Masters in Healthcare Administration, Bachelors in Nursing (licensed in three states), a Certified Executive in Nursing Practice (AONL), and recipient of several community leadership awards. For 20 years, Means worked for the Mercy Health System as Nursing Director, Inpatient and Emergency Services. She served as Director of Emergency Services for Northwest Health System in Springdale and afterward as project director for a stand-alone emergency room in Fayetteville.

Arkansas is at a pivotal moment in its journey to improve maternal health. This issue of Arkansas Hospitals is dedicated to celebrating the momentum of a collective movement that focuses on putting the patient first and changing the environment to better meet the needs of mothers and babies. The following pages offer an inside look at the policy-driven approach to improving outcomes, highlighting a check-in on the progress of enacting updated Medicaid policies and the collaborative initiatives of the Arkansas Center for Women & Infants’ Health. The work thus far illustrates that collaboration is key to changing the face of care for mothers in Arkansas. Future efforts must continue to push the needle forward for real change.

Scan here to watch the Arkansas Maternal Health Roundtable Recap 2025

By Becca Bona
On Wednesday, Aug. 6, 2025, the Arkansas Hospital Association and the Arkansas Center for Women & Infants’ Health co-hosted a Maternal Health Roundtable at the Arkansas Museum of Fine Arts in Little Rock. The event convened health care providers, clinicians, advocates, policymakers, and community members centered around improving maternal health outcomes in Arkansas. The day included an agenda full of panel sessions and presentations bringing leaders from across the state together to discuss everything from maternal health advocacy during the 95th General Assembly to integrating doulas into clinical care.
The day’s agenda included a panel on policy and reimbursement that highlighted the coordinated strategy and significant progress made in maternal health since the Governor convened the Senior Strategic Committee on Maternal Health in 2024. The presentation featured Janet Mann, Secretary of the Arkansas Department of Human Services; Dr. Pearl McElfish, Associate Provost, Community Health and Research, UAMS; and Elizabeth Pitman, Director, Office of Health Information Technology, Arkansas Department of Human Services. Facilitated by Anna Strong, Executive Director, Arkansas Chapter of the American
Academy of Pediatrics; Executive Committee Member, Excel by Eight, the panel provided an overview of the Transforming Maternal Health (TmAH) Model grant, its implementation process, and future opportunities for health care partner’s involvement. The discussion also covered key updates for providers on maternal health policy and reimbursement.
To provide a deeper understanding, Mann offered an overview of the TmAH Model grant, a 10-year, $17 million initiative awarded to Arkansas in January. The grant, which was applied for last September, is a collaborative effort led by the Arkansas Department of Human Services, with support from the Arkansas Department of Health and the University of Arkansas for Medical Sciences. The grant’s strategy is built on three pillars: access to care, infrastructure, workforce capacity; quality improvement and safety; and whole-person care delivery. Initial investment plans focus on several key areas, including using data to target maternal health services, educating providers and pregnant women on the benefits of doulas, community health workers, and midwives, and investing in technology infrastructure. The grant will also support redesigning Medicaid reimbursement rates and payment structures, improving connections between health care providers and communitybased organizations serving low-income women in Arkansas.

All three panelists noted that strategic collaboration within the legislature and the state’s health care community was key to securing the grant and advancing maternal health outcomes in Arkansas. “It’s not just one area, it’s not just one group, it’s all women having children that need to have a safe and healthy place to have a baby,” Mann said. “It was very important to have a collaborative approach.”
McElfish echoed the sentiment: “The important part was the collaboration that happened to get to the Healthy Moms, Healthy Babies Act, and the leadership that Medicaid has shown and so many of you here today in this room who are willing to set aside individual agendas and collaborate.”
Only six months into the 10-year grant’s implementation, the current focus is on implementing new Medicaid policies across the state. The goal is to integrate programs for doulas, community-health workers, and the Arkansas Perinatal Quality Collaborative, among others, to ensure they’re being utilized. While the team is still early in the process, the feedback has been illuminating. As a result of this continued need for provider involvement, stakeholder groups and committees focusing on the grant’s different pillars have been formed. Topics range from birth centers to doulas and lactation consultants, and are just getting started. Pitman explained that every
committee, stakeholder group, and public comment period offers feedback opportunities. “When we put out rules for public comment, read the comments and provide us with comments back. [...] Get engaged as early as possible,” Pitman said.
Initial funding from the TmAH grant is poised to increase access to care. “We know we’ve lost a lot of labor and delivery hospitals here. We know we need more practitioners in rural areas,” Pitman said. Funds are also earmarked for data infrastructure, specifically, encouraging hospitals to use electronic health records for better data sharing.
The health care community will also feel the effects of the policy pieces from Healthy Moms, Healthy Babies, which affect budgets. Mann detailed presumptive eligibility, which promotes immediate care for newly pregnant women, shortens the application process, and provides coverage for a woman’s first two prenatal doctor visits within 60 days. This policy is key to the state’s broader strategy of unbundling payments, shifting from a single global payment for birth to paying for each visit. This change allows the state to collect critical claims data on the frequency and location of prenatal visits, helping to identify trends and care deserts. The unbundling also provides better payment to the provider(s) involved in the delivery. “We heard very loud and clear that the rates have not been updated in
WE HEARD VERY LOUD AND CLEAR that the rates have not been updated in close to 20 years, so we’ve made an honest effort to UPDATE THOSE DELIVERY RATES.




close to 20 years, so we’ve made an honest effort to update those delivery rates,” Mann explained.
Under the Healthy Moms, Healthy Babies Act, Arkansas allocated a little over $45 million in state and federal funds to cover deliveries and up to 14 best-practice office visits for pregnant women, including additional visits for high-risk pregnancies. The initiative, which went live on Jul. 1, also allows for separate billing for services like lab work and remote monitoring, providing the state with valuable data on patient care. “It’s going to be a work in progress,” Mann said, as officials refine the new processes. “We’ve received some constructive feedback, and we are taking all that into account and considering how we can use it in the future.”
The panel also offered an encouraging update on the Maternal Life360 HOME, a program that’s already making a difference for women with high-risk pregnancies. Launched at St. Bernard’s in Jonesboro in November 2024 and followed by Baptist Health, the program directly resulted from recommendations from the Strategic Committee on Maternal Health to Governor Sanders. Pitman detailed how the program partners with a home visiting organization to provide in-home education and support, creating a personalized action plan to address the pregnant woman’s comprehensive needs, including those related to social determinants of health.
Future steps for DHS include implementing policy pieces involving lactation specialists and community health workers, which need to go through the approval process internally at DHS, the Governor’s office, and the legislature. And although the target start-date is Oct. 1, it might not happen until January. Regardless, the panelists kept returning to one crucial point: a unified approach is key. McElfish exuded this sentiment: “I think Arkansas’s secret sauce is that we’re a state that operates like a small town, and the ability to get things done collaboratively and quickly is wonderful.”


By Lee Johnson, M.D., Arkansas House of Representatives, District 47 Representative
Just a year ago, the conversations we were having about Arkansas’s maternal health were just that — conversations. But looking around the room at the recent Arkansas Maternal Health Roundtable, I could feel a tangible shift. It was a day to reflect and celebrate, as so many of those ideas are now policies, thanks to strong leadership and the passage of the Healthy Mom, Healthy Babies Act and many more. We’re pushing the needle forward.
The reality is stark: Arkansas’s maternal mortality rate consistently surpasses the national average. The Arkansas Maternal Mortality Review Committee’s 2023 Report reveals a critical problem: the state’s maternal mortality rate continually goes above the national average. According to the report, an
alarming 92% of these deaths are considered preventable, which tragically translates to approximately 75 Arkansas mothers losing their lives annually and leaving behind devastated families and communities. The contributing factors are complex, including limited access to care, a fragmented system, and a lack of service coordination. We can’t sit back and just hope things get better — we have to build a strategic, comprehensive system of care.
As an emergency physician, I've seen firsthand how a statewide system of care can save lives. When I started working in the ER back in 1997, Arkansas did not have a statewide trauma system. Today, through our statewide trauma system, we’ve effectively reduced preventable
trauma mortality by 50%. We’ve seen similar success with our stroke mortality ranking, which improved from 50th to 37th in the nation from 2011 to 2021.
These successes prove that a data-driven, coordinated approach works. We have a history in Arkansas of overcoming dismal health outcomes by creating accountable, structured systems. I’m a big advocate for this model, and I’m convinced we can apply it to maternal health. Beyond the vital work of the Arkansas Perinatal Quality Collaboration and the ongoing efforts at the Arkansas Center for Women & Infant’s Health, new legislation is introducing powerful, simultaneous moving parts. Specifically, Act 868 introduces the Arkansas Maternal Outcomes Management System (MOMS).
Passing this critical legislation and securing other significant maternal health wins during this past session would simply not have been possible without the tireless collaboration and demonstration of exceptional leadership shown by my colleague, Senator Missy Irvin. I’m deeply grateful to have a collaborator who not only shares a commitment to improving maternal outcomes but also understands the importance of aligning our state’s resources and efforts to achieve this goal.
MOMS is not just one program, but a comprehensive framework designed to revolutionize maternal care across the state. Once this plan receives the full funding we are diligently working to secure, MOMS will be housed within the Arkansas Department of Health, where it can be fully implemented. The focus can be broken down into five key pillars: organizing resources, educating clinicians and patients, incentivizing hospitals to implement best practices, collecting and analyzing data, and establishing a structured peer review process.

We’re working on creating a centralized website that will be a hub of information, from Medicaid enrollment to transportation resources. We're also developing targeted training for healthcare professionals and patients. One of the biggest challenges we’ve discussed is workforce and reimbursement — and MOMS will award grants to delivery hospitals, especially those in rural areas, to help with that.
During the Arkansas Maternal Health Roundtable, I had the honor of facilitating a panel titled “A Unified Hospital Voice for Maternal Health.” My goal was to bring together a variety of stakeholders and experts to discuss the biggest challenges we face. We had:
• Dr. Shannon Case from Johnson Regional Medical Center, representing the perspective of a rural hospital.
• Dr. William Greenfield , an OBGYN at UAMS and Medical Director for Family Health at the Arkansas Department of Health, providing the crucial academic and public health viewpoint.
• Dr. Kalena Jones , Director of Community Health Programs at Baptist Health, with her focus on community-level care.
• Dana Lands , a Nursing Director for Women’s and Children’s Services at St. Bernard’s Healthcare, offering the firsthand perspective from the front lines of patient care.
As we spoke, it became clear that the challenges we face — improving access to care, strengthening our workforce, and addressing the differences between rural and urban areas — are multifaceted. We also discussed the complexities of coordinating patient transfers, which made me think of the proven call systems we have for trauma. The good news is, the MOMS initiative is designed to address this with key deliverables like the MOMS Care Connect Call Center to coordinate transfers and the Postpartum Support Hotline to proactively connect with new mothers. This is exactly the kind of strategic, unified effort that will move us forward.
The success of this program hinges on collaboration. We need policymakers, service providers, and hospital systems all working together. The new delivery hospital designation system will evaluate hospitals’ capabilities for providing high-quality maternity care, and to participate, hospitals will need to become active partners in their communities through outreach and clinician education. The MOMS initiative is built on data-driven decisions because that’s how we create an effective and responsive system of care. We have to do a better job of acting on that data to solicit change. By supporting the implementation of MOMS, we can build on our past successes and create a lasting legacy of healthier mothers and babies for all Arkansans.


We have a history in Arkansas of overcoming dismal health outcomes by creating accountable, structured systems. I’m a big advocate for this model, and I’m convinced we can apply it to maternal health.

By Becca Bona
The Arkansas Hospital Association and the Arkansas Center for Women & Infants’ Health convened the 33 birthing hospitals across the state, as well as advocates, policy makers, and others interested in improving maternal health outcomes during the Arkansas Maternal Health Roundtable on Aug. 6, 2025, at the Arkansas Art Center in Little Rock.
The panels throughout the program shed light on the collective movement surrounding maternal health. One such entity, still relatively new in the space, took center stage: The Arkansas Center for Women & Infants’ Health. Born from funds secured by Senator Boozman through a series of appropriation bills, the Center started as an idea several years ago, and as of January of this year, it is in the process of making an impact.
If there is a system that works better for your hospital , then we want to address it.
I know that one size does not fit all within this process.
Dr. Nirvana Manning, professor and chair of the Department of Obstetrics and Gynecology at the University of Arkansas for Medical Services, serves as the inaugural director of The Arkansas Center for Women & Infants’ Health, and shared the purpose, mission, and goals of the Center for those in attendance. “I think the take-home is that we would like to be pDartners, and we want to show how we can do that better,” Manning said, addressing the room.
The Maternal Mortality Review Committee, convened by Governor Sarah Huckabee Sanders, found in 2024 that over 90% of maternal deaths in Arkansas are preventable. Furthermore, Arkansas consistently ranks worst in the nation for maternal health. “Arkansas is a largely rural state, and many of our communities are considered health care deserts, meaning they lack access to essential medical services, including maternal and prenatal care,” Manning explained. Income, education, transportation, and housing — indicators from social determinants of health — play a role in the maternal health care crisis and affect not only access to care but a woman’s ability to stay healthy during and after pregnancy.
Women are at an increased risk of serious complications after birth, which require close monitoring, including hemorrhage, hypertensive disorders like preeclampsia,
infections, blood clots, cardiac conditions, and mental health crises. “Over 40% of women don’t attend their postpartum visit, which is crucial for identifying and addressing potential health care issues,” Manning said. New mothers may dismiss symptoms or be unable to attend follow-up appointments due to inadequate childcare options or lack of transportation. Further, there are often disconnects if a new mother ultimately arrives in the emergency room. “Emergency providers may not immediately recognize some postpartum-specific risks, leading to delays and misdiagnoses,” Manning continued.
Knowing the multifaceted problems and issues affecting maternal outcomes is the first step in working toward solving the problem. Manning outlined the Center’s primary goal: to change the maternal outcomes in the state by providing innovative solutions, improving access to care, and facilitating support for women in the postpartum period. To do this, the Center’s team identified four key initiatives: postpartum education, mother and infant supply kits, implementation of the “I Gave Birth” bracelet, and the proactive postpartum call center.
First, by standardizing postpartum education, the Center aims to put everyone across the state on the same playing
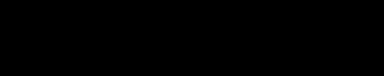
Jan 2025 - Launched
Feb 1: “I Gave Birth” Bracelet
Provides postpartum patients with a bracelet, which signals to health care providers, emergency responders, and their communities to watch for warning signs.
April 7: “Mother & Infant Supply Kit”
Provides baby and postpartum care items to families after delivery.
May 1: “Proactive Postpartum Call Center”
Nurses call every patient in the days after delivery to provide direct follow-up care.
Snapshot from Jan - July 2025
of call center patients answered the call and completed a health assessment 70%
411 patients reached through the call center
1 in 10
screen positive for Postpartum Depression

794 896
Mother + Infant Supply Kits distributed “I Gave Birth” bracelets distributed
30% of patients reported an urgent maternal warning sign
48% of patients had Social Determinants of Health need
field. “We worked with leaders in pediatrics as well as obstetrics and gynecology to streamline education so that every mom and family that leaves their labor and delivery will get the same early maternal warning signs and things to watch out for, as well as infant safety information,” Manning said. Second, the Center introduced infant supply kits to build trust back into the health care system, and a pilot program at UAMS was rolled out in March of 2025. The kits include necessities such as diapers and formula; however, the Center monitors what items seem most sought-after to continue improving the kits.
Third, the “I Gave Birth” bracelets are modeled after successful initiatives in other states and are a communication tool. “It’s a visual for not only the patient to take their health seriously, but also for other health care providers to recognize that that patient may come with different symptoms,”
Manning said. The bracelets also come with a QR code that leads to the Center’s website, offering resources for new mothers to find information on everything from lactation services to car seat safety and mental health to safe sleep and beyond.
The final initiative is the proactive postpartum call center, which is designed to improve maternal health outcomes by ensuring postpartum women receive support and care coordination. The call center provides a timely follow-up for women on the days after delivery, during which nurses utilize medical and social determinants of health questionnaires. If screened positive for a health issue, new mothers will be asked to follow up with a provider. New moms are also asked about insurance and if they have sufficient resources — i.e., formula and diapers. “We then team them up with community health care workers who will help. We hope to see a lot of improvement regarding this,” Manning explained.

Convening the state’s birthing hospitals shows an initiative to marry the funds, stakeholders, and impl ementation resources with the boots on the ground. Manning wants the conversation to continue. In a brief question-and-answer session with those in attendance, Manning answered a question about how the call center was supposed to work — i.e., who would implement it. The Arkansas Center for Women & Infants’ Health plans to use its call center workforce to conduct the questionnaires. However, Manning quickly noted that she and her team are open to discussing what works best for hospital partners across the state. “If there is a system that works better for your hospital, then we want to address it. I know that one size does not fit all within this proces s,” she said. “We have the funds, the resources, and all of the questionnaires, and we are happy to share that.” The team is also committed to updating the website and adding new
and pertinent resources as they become available. “We want these resources in our state to work together to create synergies,” she said.
The roundtable continued crucial conversations and collaborations to improve maternal health outcomes across the state. The next steps for the Center for Women & Infants’ Health include partnering with the Arkansas Perinatal Quality Collaborative to support quality improvements in postpartum care, getting infant kits out to the hospitals that need them, and distributing the “I Gave Birth” bracelets. The Center is also working to scale the call center to reach every postpartum patient in Arkansas by the end of the year.
Looking around the room, Manning ended the day with a call to action: to continue the conversation. “I think the delivering hospitals, the administration, the people with boots on the ground, meeting at a regular interval could be so impactful in changing the momentum and trajectory of maternal health in our state. We have so many good people working on this.”



Scan here to go to the Arkansas Center for Women & Infants' Health website.
By Becca Bona
Raised in Thornton, Arkansas, Crystal Bohannan fondly remembers her family-filled childhood. Bohannan was determined to be a leader from an early age, even if she hadn’t yet pinpointed the cause or organization she wanted to lead. “When I was in kindergarten, kids called me bossy,” she recounted with a laugh. “I said, ‘Well, you still do what I say.’”
At age five, she had aspirations, telling her piano teacher she’d like to be a surgeon one day. “Then in seventh grade, we dissected a frog, and I knew my career path would change because that was not for me,” she said.


| The Gallagher Way. Since 1927.
Gallagher is a global leader in insurance, risk management and consulting for healthcare organizations. We provide innovative, cost-effective solutions to help hospitals and health systems thrive. Our comprehensive approach protects assets, optimizes operations, and supports workforce and community wellbeing.
Partner with a Gallagher consultant to navigate the complexities of today’s healthcare landscape.
© 2025 Arthur J. Gallagher & Co. | GBSUS104196 Connect with us
Chris Newkirk Area Vice President chris_newkirk@ajg.com (501) 485-3082
Bill Birch Senior Area Vice President bill_birch@ajg.com (501) 614-1170


Undaunted, Bohannan stayed open to different career paths. After graduating from Bearden High School, she attended Southern Arkansas University at Magnolia. A professor asked her if she knew of any out-ofwork accountants, she decided the field would be a good career choice, double majoring in accounting and finance. Her intuition served her well, and directly upon graduation, she landed a job with a regional accounting firm stationed in Little Rock known as BKD.
She was randomly assigned to the health care sector as a rookie upand-comer. “Honestly, that’s what got me into the health care world,” she remembered. She was learning quickly that she did not want to be a public accountant for the rest of her life. Still, her time at BKD armed her with the knowledge of her next steps: working toward learning all she could about the business of health care.
In her early career, Bohannan focused heavily on professional growth. “I tried to hone my skills and put them to good use by being a good leader,” she said. The first thing a good leader does is arm themselves with both relational and technical knowledge. Looking back, Bohannan credits her accounting and finance background as an excellent foundation to learn all she could about health care. After working with BKD, she was hired at Jefferson Regional Medical Center (JRMC) in Pine Bluff, where she worked for almost a decade.
Her background opened learning opportunities. “I was allowed to do several different types of jobs, from business analyst focusing on productivity and capital expenditures, all the way to the administrator of the surgery

center and more,” she recounted. Her experiences at JRMC allowed her to interact with more than numbers; she worked closely with physicians and nurses, gaining relational knowledge.
During this time, she discovered a budding interest in logistics and how things flowed at her facility.
“That’s when I found my true love of operations,” she said. “It really bridges that relationship type leadership along with financial operations, and I think that that’s what really drew me in.” She also passed the CPA exam and earned an MBA from Mississippi State University while at JRMC.
After her tenure there, a position opened at CHI St. Vincent in Hot Springs. She applied for the executive director

is to be the role model. If I’m not living it and acting it, how can I expect MY COWORKERS TO?
of operational finance role. She began working in what she describes as more of a traditional CFO position, honing her skills, delving into the month-end financials, and digging deep into revenue cycle. Nevertheless, she couldn’t forget her calling to work in operations.
Bohannan credits the mentorship she received along the way as integral to her journey. “Our president at the time, Tony Houston, was interested in what I wanted

to do, and how I wanted to grow,” she said. After mentoring her and listening to her goals, he worked to promote her to vice president of operations, allowing her to focus on her passion while serving the organization. She held the position for 7 years, and even after Houston left the organization, she found mentorship in his replacement, Dr. Doug Ross. “I told Dr. Ross, I want to sit in your seat,” she remembered. He was very supportive, and through his mentorship, an executive coach, and working with CHI St. Vincent Market CEO, Chad Aduddell, Bohannan received excellent skill development and career guidance.
When Dr. Ross left, Bohannan felt she’d received the support and mentorship needed to apply for his position. After the interview process, she was named President of CHI St. Vincent Hot Springs, taking over in January of this year.
Bohannan hit the six-month mark at the end of the fiscal year in June 2025 and has remained busy. During that time, she named a new CMO, noting that Dr. Ross previously spanned what should have been two positions. “Dr Joshua Keithley is our CMO here,” she said. “He’s been very helpful in working towards our goals as an organization and keeping us connected with the physicians. I’m not their only contact now — they also have a physician contact, too.”
In addition to expanding the team, Bohannan has also worked to end the fiscal year with a positive scorecard internally regarding quality, safety, patient experience, and coworker and physician engagement. “Our scorecard has never been greener than it was this year,” she
said. “Dr. Ross laid the foundation for all of the work, so he gets as much credit as I do.”
Even so, planning in the health care sector becomes more difficult yearly. Still, Bohannan is working toward setting her team up for success. “The reimbursement challenges, trying to combat inflation, and then the pressures overall — it’s a sea of challenges,” she said. “I didn’t think it would be easy when I sat in this seat, but I tell my team, we do really hard things. And, it’s a lot easier to do really hard things when great people work with you for the right reason, with the patient as the focus.”
As for providing the right environment for her team to thrive, Bohannan says building a positive company culture is the goal. “My responsibility is to be the role model. If I’m not living it and acting it, how can I expect my coworkers to?” Acknowledging that a positive working environment stems from a team effort, Bohannan advocates for diverse
We empower Medicare beneficiaries, their families, and caregivers to prevent, detect, and report healthcare fraud, errors, and abuse through education,
SMP helps identify and correct billing errors found on Medicare Summary Notices (MSNs) and works to recover funds to Medicare. Suspected fraud is promptly referred to the U.S. Office of Inspector General for further investigation.
SCAM ALERT FOR PROVIDERS: Be Aware!
Scammers are faxing provider offices requesting signatures on Durable Medical Equipment (DME) orders and asking for patients’ medical records.
Some providers have mistakenly signed and returned these fraudulent faxes. Do not respond to suspicious requests. If in doubt, verify the source before responding.




voices at the table. “When we’re talking about culture, it’s making sure that our coworkers feel like they have a voice too, because we want to make sure they have a voice in their practice.” One of the ways Bohannan sees this at work is through the facility’s Magnet accreditation with distinction. This elite designation provides a governance structure to continually improve outcomes.
Another element that sets CHI St. Vincent apart in Bohannan’s eye is the faith-based aspect of the organization. “Very often we pray with our patients. We always ask first, but you would be surprised at how that little extra thing makes such a difference to patients in their most vulnerable time.”
Finding a way to comfort patients highlights the impact of connection in health care. Bohannan and her team are reminded daily why they serve in the health care field: to help people. Sometimes this all starts with a simple hello. “We take pride in having good Southern hospitality,” she said. “We see it in action, and see it in action in our scores, too.”

As a Southern Arkansas girl, Bohannan is most proud of her facility’s work for the Southwestern quadrant of the state, providing both primary and referral access for the many people who call this area home. “We are the busiest level II Trauma Center in the state, and the only level II Trauma Center in the southern half of the state. For reference, we saw over 47,000 emergency department visits last year,” she explained.
The hospital is more than a Trauma Center, however. From specialty care surrounding surgeries, cardiac, ortho,
I DIDN’T THINK IT WOULD BE EASY WHEN I SAT IN THIS SEAT, but I tell my team, we do really hard things. And, it’s a lot easier to do really hard things when GREAT PEOPLE WORK WITH YOU FOR THE RIGHT REASON, WITH THE PATIENT AS THE FOCUS.
neuro, and OB services, the facility continues to offer services that Bohannan is proud of: “We just want to make sure we’re able to keep doing that in the future.”
One of the areas Bohannan is especially watching includes maternal health services. “There aren’t many places that deliver babies in this area — we’re about it. Some moms already drive two hours to have their baby here. We don’t want them to have to go any further than that,” she said, citing reimbursement issues as one part of the problem.
While she can’t solve the reimbursement issue on her own, she has embraced her legislative duties that come with her position, seeing advocacy as a way to push the needle forward for health care. “Our Market CEO, Chad Aduddell, is very involved in our advocacy work and working with our lobbyists, which helps keep us connected to our advocacy goals,” she said. Bohannan has made it her mission to learn as much as she can about advocacy, crediting her fellows across the CommonSpirit footprint as being helpful resources, as well as the Arkansas Hospital Association’s
advocacy tools and built-in networking. “It’s been a huge growth opportunity for me,” she said.
When not working, Bohannan enjoys spending time with her family. She has been married to her wonderful husband, Brent, for 22 years. Her two boys, Jace (15) and Dax (12), both enjoy playing football and basketball at Lake Hamilton. Bohannan loves watching them play and attending games with them. She and her husband also enjoy fine dining, especially in Hot Springs. “I love to go to a nice restaurant for the experience and eat delicious food and have good drinks,” she said. She’s also fortunate enough to enjoy spending time with her parents, sisters, and in-laws, who are all still in Arkansas. She enjoys traveling and staying active in her church, Old Union Primitive Baptist Church.
Bohannan gets the best of everything in Hot Springs — she’s close to family, enjoys the nearby outdoor amenities, and enjoys her quality of life. “I try to recruit everybody that comes in from our national and regional teams,” she said, smiling. “Look at all these things that we have to offer. I think Hot Springs is a little hidden gem.”




SHARE's Daily Hospitalization Reports are given directly to SHARE-connected providers and care teams, to assist with care coordination and patient follow-up.
Real-time notification of hospital visits (admissions, discharges, or ED transfers) for practices' active patients
Allows providers to proactively coordinate their patients' care and schedule any necessary follow-up treatments or visits
Assists in meeting value-based contract arrangements

In the complex world of health care, the most impactful and highest-quality care stems from a powerful idea: putting the patient first. The following stories celebrate hospitals and the dedicated teams keeping the patient at the forefront of care.
The initiatives at Conway Regional Health System, Saline Health System, and Ashley County Medical Center illustrate a shared vision where care is not just a service, but a personal and collaborative endeavor. Read about the Conway Regional Home Health team that brings care beyond hospital walls, providing intentional and individual support in patients’ homes. Discover how Saline Health System’s Nursing Shared Governance Council empowers nurses to have a stronger voice in improving patient care and safety. Lastly, explore what happens when Ashley County Medical Center dedicates its leadership and staff to providing a “third place,” making every patient’s experience a little more enjoyable at the AshleyBrew Café.

Nurses at Saline Health System now have a stronger voice in improving care and safety, thanks to the new Nursing Shared Governance Council.This initiative allows nurses, like those pictured above, to directly address challenges and concerns they face on the job, leading to positive policy changes and a more engaged team. (Photos by DeAnn Thomas)
By DeAnn Thomas
When two perioperative nurses at Saline Memorial Hospital came across a requirement in the blood transfusion documentation that wasn’t applicable to them in the operating room, they decided to turn it in for peer review with the hospital’s Nursing Shared Governance Council.
The council started exploring options for how to make the process work more smoothly for their peers. After enlisting the help of the IT department and the leader of the quality team, the council created a new document that was tailored specifically for the perioperative department.
“The new documentation came up in play recently, and it was wonderful to see that we had come up with a solution that really works,” said Bryson Berry, council chair. “We addressed a situation that needed some attention,
We have a really engaged team of people in this group right now, who have come up some really great ideas, and I know there is so much more to come.
and it was the Nursing Shared Governance Council that provided the avenue for us to be able to do that.”
Saline Health System CEO Char Boulch, who was the chief nursing officer at the time, started the Nursing Shared Governance Council in April 2024 to empower nurses with a way to address the issues they face.
“Shared governance is recognized now as a standard of care for hospitals who truly value their nurses and their input in the clinical decision-making process,” said Rhonda Hixon, the hospital’s quality performance coordinator and sepsis coordinator. “It allows nurses to have a voice and creates a partnership between nurses and the administration and other decision makers.”
The council is made up of four subcommittees: a peer review committee, a quality committee that reviews procedures for possible quality improvement, a professional development committee that works on the clinical ladder and other related initiatives, and a recruitment and retention committee.
Over the course of the year, the council has proposed several policy changes, especially in the areas of patient care and safety, like handling of jewelry for surgical patients, insulin use in the hospital, and med scanning. The proposed changes go through rigorous testing and reviews before implementation.
Council members have also started rounding in their departments to gather additional feedback.
“The nurses here are feeling more at ease knowing that people are listening, and it’s people just like them who are facing the same situations they face every day,” Berry said. “They have a way to express their cares, their worries and their complaints, and they feel heard a little bit more. That alone makes this a valuable piece of the hospital.”
As the council looks toward the future, they want to expand to having unit-based councils, where each department has its own set of representatives. Council members are also planning to start attending recruitment events and exploring opportunities to improve retention.
“We have a really engaged team of people in this group right now, who have come up some really great ideas, and I know there is so much more to come,” Berry said. “Any time you give people a voice to where they can express their concerns and bring about change, that’s a win for everyone — not only for the team here but also for the patients we are taking care of.”

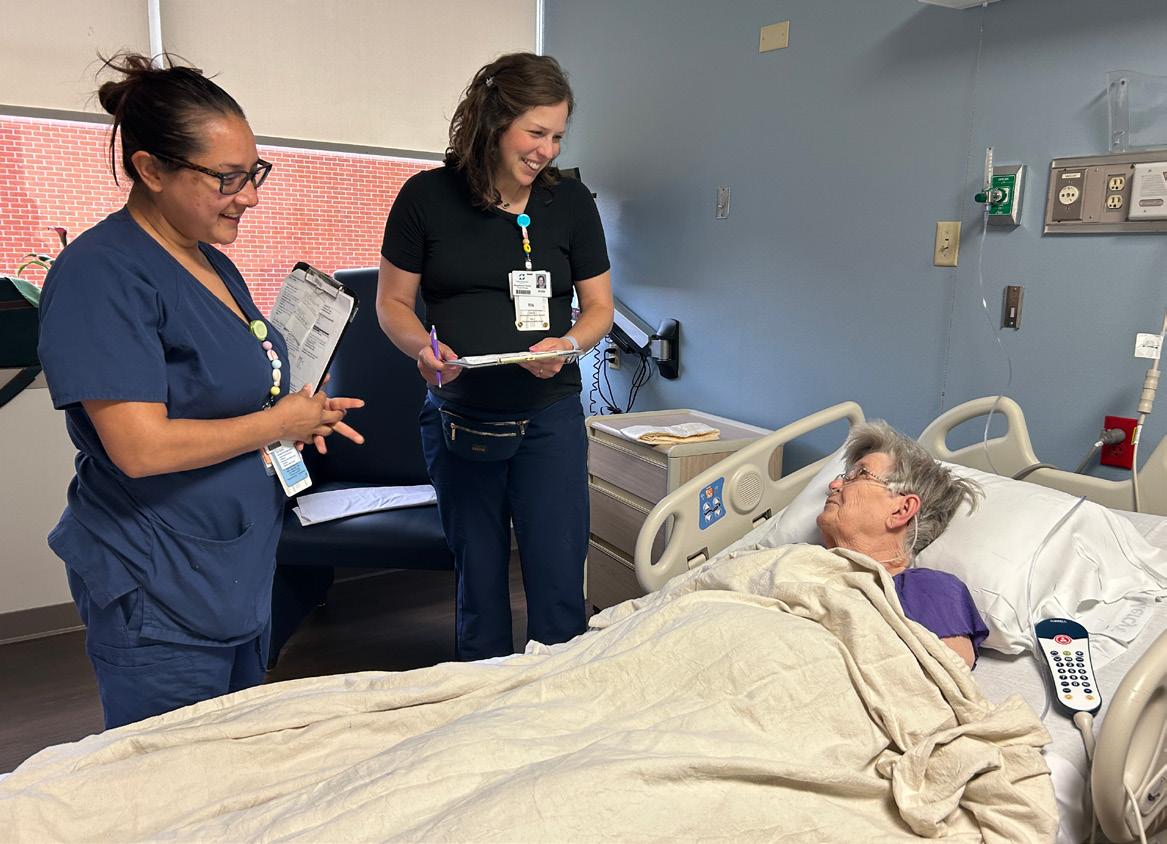
Rounding nurses speak with a patient.

By Miranda Hogg
At Conway Regional Health System, care is highly intentional and refreshingly personal. Through Conway Regional Home Health, patients receive familiar care that is backed by a fierce commitment to keep patients healthy and at home. This department brings together physicians, nurses, therapists, and support staff to help patients recover from illness or disability while maintaining independence.
That commitment is shown in the results. The Centers for Medicare & Medicaid Services has awarded Conway Regional Home Health a 4.5-star rating for the quality of care and patient satisfaction. The team ranked above the national average on 16 of 17 quality measures, from helping patients manage daily activities to treating symptoms, preventing complications, and reducing unplanned hospital visits.
Behind those outcomes are nurses who bring skill and heart into every home they visit. Home health nursing is unlike any other specialty; it requires adaptability, resourcefulness, and compassion. These nurses meet patients where they live, forming close relationships and providing education. For two Conway Regional nurses, Jo Luker, LPN, and Kelsey Robinson, LPN, this role has become both a calling and a source of deep personal fulfillment.
For Luker, nursing was a dream that came later in life. After raising her family and working as a secretary for 25 years, she enrolled in nursing school at the age of 45. “I’d always wanted to be a nurse,” she recalled. “When my son was grown, I decided it was time to take the plunge.” Now, she has found a place where her skills and her heart are in alignment. Her approach extends beyond clinical skills to a mindset of compassion: no judgement, only care.
That compassion has saved lives. After a recent medication change, one of Luker’s patients felt weak. When Luker checked in, she found the patient’s blood pressure dangerously low and blood sugar unstable. She coordinated with the care team and ensured the patient was taken to the emergency room, where she was diagnosed with a life-threatening condition. Later, the patient told Luker, “If it hadn’t been for you checking on me, I would have died.”
term care, specializing in rehabilitation and wound care. She later moved into IT at Conway Regional but soon realized she missed the personal connections of patient care. “I’d always heard people loved home health,” she said. “I wanted to get back to helping the community, and this gave me the chance to care for my neighbors.”
Since joining the team in 2023, Robinson has embraced the unique challenges of working in patients’ homes. “There is no call light and no supply cart in the living room,” she explained. “You have to think two steps ahead because everything you need is in your car. But the goal is always the same: keep patients safe and at home.”
You have to think two steps ahead because everything you need is in your car. But the goal is always the same: keep patients safe and at home.
Luker’s colleagues describe her the same way her patients do: intentional, empathetic, and steadfast. “Jo doesn’t just clock in, she shows up with impact,” one team member said. Known for her honesty and compassionate communication, she has earned the trust of both patients and peers. Her leadership and work ethic make her a steady presence in the fast-paced world of home health.
Robinson’s path to home health came after years in other nursing roles. A nurse since 2010, she spent 13 years in long-
The continuity of care has been especially meaningful for her. She recalled a patient with a chronic wound who asked for her specifically three times a week. Over time, the two built a bond grounded in trust and compassion. “She’s had a hard time, and I hope I’ve given her a glimpse of happiness by showing that someone cares and wants to help.”
Her colleagues echo that sentiment, describing her as selfless, dependable, and a quiet source of strength. She mentors new staff, anticipates needs before they arise, and always steps in to help. “Kelsey is compassionate, reliable, and incredibly knowledgeable,” said one teammate. “She consistently goes above and beyond without ever seeking recognition.”
Together, Luker and Robinson are frequently requested by name, a testament to the impact they have on the families they serve. Their teamwork has become a powerful asset to Conway Regional Home Health, where they model the system’s mission every day. In a field where burnout is common and challenges are constant, they shine as examples of resilience, purpose, and compassion.


The AshleyBrew Café offers a selection of desserts baked fresh daily, providing comforting treats for staff, patients, and visitors. (Photos provided)
By Becca Bona
Known as the South’s Forestry Capital, Crossett was founded as a lumber company town in the late 1890s. The largest township in Ashley County, today’s small-knit community is home to pastoral landscapes, offering residents and visitors ample opportunities to enjoy hunting, camping, hiking, and fishing. Beyond the outdoors, Crossett provides multiple locations in the community that serve as “third places.” The term, coined by Ray Oldenburg in the early 1990s, references a familiar public spot (outside of first place — home, and second place — work) where people share an interest or activity. Third places include cafés,
Families have also shared how much they appreciate being able to step away for a coffee and a moment of normalcy without leaving the hospital. It’s become more than just a café — it’s a gathering spot.
churches, public libraries, parks, and post offices — to name a few.
According to locals, if any particular area is lacking in Crossett, it’s likely in the culinary arena. After working as a postal service officer, Crossett resident Becky Roberts spent 23 years in the food industry as a restaurant owner. Running the restaurant brought her great joy, but eventually, she sold the business to enjoy a slower-paced lifestyle. Unfortunately, her restaurant was closed within the year she sold it, leaving Crossett residents even fewer food options. “There’s really nothing in Crossett if you don’t want fast food,” Roberts said. “I was so excited when I heard that Phil Gilmore [ACMC CEO] was pushing for a café and they were going to bring one to the hospital.”
ACMC, unfortunately, had to close the cafeteria down due to the logistical nightmare of attempting to keep it open during COVID-19. After the cafeteria closed, patients, staff, and visitors had to leave the hospital to get food. The lack of options was neither ideal nor convenient, and ACMC leadership recognized the problem and began working toward a solution for patients and staff alike.


With much support from leadership and planning for logistics and construction, ACMC opened the AshleyBrew Café this past March. “Patients benefit from access to nourishing food and drinks, and families who spend long hours supporting loved ones appreciate having a comfortable place to sit, recharge, and eat, along with a place for the entire community to enjoy,” said Shirley White, Human Resources Director and Accounting Supervisor at ACMC.
Opening the AshleyBrew Café aligns with the hospital’s mission of providing compassionate, quality care and promoting health. “The café reflects our belief that supporting good health goes beyond medical care and includes access to healthy, comforting, and convenient food choices in a welcoming environment,” said White.
Since opening its doors, AshleyBrew has remained busy. Amari Forrest, a food service worker at the café, says she sees support from staff and community members. “I think the community and the hospital love the coffee shop,” she said. “The café brings everybody together, including nurses, employees, and patients.” Forrest notes that many café goers are already regulars who visit daily.
Guests can choose between sandwiches, paninis, breakfast burritos, soups, salads, fruits, and desserts. “We have a variety of fresh ingredients that can also be combined to create any combination that the customer wants,” White added.
AshleyBrew is open daily with extended hours from 6 a.m. to 8 p.m., providing more flexibility for patients and their families, community members, and staff. “We’ve worked to provide a variety — quick grab-and-go items for staff on tight schedules, healthier options for those focused on nutrition, and comforting drinks and meals for families who may be under stress. By offering choices, we can meet people where they are,” White said.









The café participates in the “Starbucks We Proudly Serve Initiative,” a collaboration between Starbucks and Nestlé that allows businesses such as hospitals to use Starbucks beans and sell familiar favorites while operating independently of corporate-run stores. AshleyBrew offers these Starbucks-familiar products, sandwiches, and other fresh items, creating a modern coffee shop vibe instead of a traditional cafeteria.
In fact, the decision to create a cozier, coffee shop aesthetic was intentional. “The ambiance is warm and inviting, designed to be a place where people can relax, meet, and even enjoy a sense of normalcy during what can often be stressful times,” White said.
Many community members have already scoped their favorite items, including Becky Roberts, the former restaurant owner. She and her daughter travel to the café three times a week, sometimes following her physical therapy appointments, and other times to enjoy the food and fellowship. “To me, it’s just great. We need it, we need it badly — if for no other reason than for interaction with people,” Roberts said. “I see a lot of people that I never get to see. I love getting to talk to people, and I love seeing people.”
White notes that, beyond patients and community members, staff also take advantage of the café. AshleyBrew provides a meeting space outside the clinical and office setting. “One of the most encouraging pieces of feedback we’ve heard is that staff now have a place to meet with colleagues outside of the clinical setting,” she said.
Ultimately, the café provides a space for everyone: “Families have also shared how much they appreciate being able to step away for a coffee and a moment of normalcy without leaving the hospital. It’s become more than just a café — it’s a gathering spot.”


By Erik Anderson, Director of Channels, ChartSpan
Care management programs, like Chronic Care Management and Advanced Primary Care Management, offer Medicare patients preventive care from a dedicated care manager between appointments with their provider. This preventive care includes help with care goals and missed quality measures, like screenings and vaccinations — but more importantly, it gives patients an additional source of support to help them manage their health.
ChartSpan care managers have offered patients empathy and assistance with their mental health, troubling symptoms, social determinants of health, and unexpected events, like natural disasters. This commitment to connecting with patients, whether they’re feeling ill or just need someone to talk to, lies at the heart of care management.
Many older adults struggle with social isolation, and these feelings can lead to worse overall health outcomes. Care management addresses patients’ emotional and mental needs by giving them someone to talk to about sad or stressful events in their lives. One patient shared this story: Ms. Smith* expressed that she had been struggling with loneliness since her husband passed away years earlier, leaving her alone with her cats. She thanked her care manager for taking time to check in and make her feel good each month and said that she looks forward to their calls.
*Name changed to protect patient’s identity
Care management programs like Chronic Care Management and Advanced Primary Care Management include 24/7 care lines that patients can call when their provider’s office is closed, including on nights, weekends, or national holidays.
When patients call ChartSpan, a care manager listens to their concerns and determines whether they need to be directed to a nurse for triage. The nurse uses Schmitt-Thompson protocols to decide whether the patient should set an appointment with their provider, go to urgent care, or visit the ER.
Here’s one patient’s story of how the 24/7 care line helped him:
Mr. Williams* called ChartSpan’s 24/7 support line with persistent chest pain, difficulty taking deep breaths, a dry cough, nausea, and pain. He was hesitant to leave work, but a triage RN listened to his concerns and then persuaded him to call 911. The next day, the RN followed up with Mr. Williams, who had been admitted to the hospital for kidney disease. He credited her with saving his life.
Many Medicare patients struggle to afford basic needs that greatly impact quality of life, like nutritious food, safe, clean housing, transportation, and utilities. Low-income patients may face worse health outcomes than higher-income patients because of this lack of resources.
Care coordinators can spend months building relationships with patients, so they’re prepared to step in when patients are comfortable sharing their social determinant of health needs. For example, ChartSpan was able to help this patient with finding nutritious, well-balanced food.
Ms. Jones* performed a Social Determinants of Health Assessment and revealed that she had food insecurities. She declined assistance with food pantries and meal delivery services because she didn’t like the quality of food offered, stating it was canned and processed and didn’t follow her dietary guidelines. Her care manager found a resource for fresh food boxes delivered to her home, with produce that was locally grown and sourced, and shared it with her.
To provide compassionate healthcare, care managers must look beyond patients’ diagnosed health conditions and consider other events that could impact their safety. These events could include approaching natural disasters, like hurricanes or wildfires. One care manager shared this story of helping a patient prepare for a hurricane:
When her care manager asked Ms. Garcia* if she was prepared for an approaching hurricane, the patient responded that she hadn’t filled her car with gas. Her care manager encouraged her to take care of that right away. She also urged Ms. Garcia to fully charge her cell phone and to prepare a go-bag with critical items, such as her medications, diabetic testing supplies, and blood pressure cuff. Ms. Garcia thanked her care manager multiple times for her support at a stressful time.
Care management’s primary goal is to help patients live longer, healthier lives. To achieve this goal, care managers need to consider patients’ whole health: offering emotional support, guidance for new or worsening symptoms, community resources for socioeconomic needs, and quick responses when natural disasters or unexpected events arise. By paying attention to all of patients’ needs, whether physical, environmental, or emotional, a care manager can become one component of a compassionate, patientfocused care team.
To learn more about how care management programs contribute to empathetic, personalized care for patients, you can visit ChartSpan at chartspan.com.



By Kay Kendall
When my editor told me the theme of this issue of Arkansas Hospitals magazine, I wasn’t sure how to approach it in my column. I usually take the theme and weave it together with concepts from the Baldrige Excellence Framework. However, this one started to feel very personal to me.
There are many reasons, some on the providers’ side and some on the patients’ side. Some on the providers’ side include:
• Overly bureaucratic and convoluted forms to be completed, made worse when they are repeatedly required and not provided in a patient’s first language
• A judgmental tone or brusque response to patients’ questions or concerns
• Difficulty in reaching doctor or clinical staff member for follow-up issues
• Not providing timely accessibility
• Unwillingness to discuss alternative options of treatment
• The physical layout of the facility is hard to navigate or requires longdistance walks on the part of the patient
Some on the patients’ side include:
• Shame for having a certain complaint or condition
• Being non-compliant with medications or treatments but embarrassed to admit it
• Embarrassment for socioeconomic conditions, such as food insecurity, rent burden (>35% of income required for housing), homelessness, or job loss
• Fear of the unknown I can speak directly to the last one. While in my mid-20s I suffered a return of clinical depression. I had been diagnosed and treated before, so I shared my symptoms with my primary care doctor and began medication and counseling again. However, I was suddenly bombarded with panic attacks. These went on for almost a year. I had no idea what they were. There was also mental illness in my mother’s family; her brother was a paranoid schizophrenic who was in and out of institutions and jail his whole adult life. I was terrified that my panic attacks were a sign of mental illness and that I would be committed to a mental hospital. I had practically become an extreme agoraphobic when my counselor recognized some of the symptoms and sent me to a psychiatrist for evaluation. That was the hardest appointment I ever made. He quickly made his diagnosis — general anxiety disorder — prescribed medication that had it under control within two weeks, and I began to believe that I could become a functional adult again. In this scenario, my providers met me where I was and allowed me to recover.
One of the Baldrige Core Values and Concepts is “PatientFocused Excellence.” There are so many aspects of this that relate directly to meeting patients where they are. “Your patients and customers are the ultimate judges of your performance and the quality of your health care….Many
factors may influence value and satisfaction over the course of your patients’ and other customers’ experience….Your management of relationships and experience help build trust, confidence, and loyalty.”
We see this reflected in many health care recipients of the Baldrige National Quality Award. Many of them have this approach directly embedded in their mission, vision, and values and reinforced by their core competencies. These show up in patient-centered care where a partnership between patients, families, and healthcare providers assures that treatment decisions are aligned with the patient’s wishes. These often provide a competitive advantage over local competitors that leads to success now and in the future.
Look at your ratings on social media. Review patient satisfaction surveys. What is your patient retention rate? What is your referral rate from current patients?
What can you do to influence this type of inclusive, encouraging culture among your employees and partners?

The team at BaldrigeCoach would be glad to help guide your hospital’s quest for process improvement. As CEO and Principal of BaldrigeCoach, Kay Kendall coaches organizations on their paths to performance excellence using the Malcolm Baldrige National Quality Award Criteria as a framework. Her team, working with health care and other organizations, has mentored 25 National Quality Award recipients. In each edition of Arkansas Hospitals , Kay offers readers quality improvement tips from her coaching playbook. Contact Kay at 972.489.3611 or Kay@Baldrige-Coach.com.


By: Nicole Bonecutter, BSN, RN, RAC-CT, IP-C, ASCOM, CDP
Infection prevention and control are crucial to patient safety and quality care, especially during care transitions. When residents transfer between health care settings, infection-related details can be overlooked, leading to unnecessary hospital readmissions, delays in treatment, and poor antibiotic stewardship. Hospitals and nursing homes can strengthen infection prevention and improve patient outcomes by improving collaboration and communication.



In long-term care facilities, Infection Preventionists (IPs) are often a team of one with many responsibilities, creating little time for education, process improvement, or thorough investigations when outbreaks occur. Similarly, hospital IPs manage competing priorities across multiple units and programs. This makes transitions of care particularly vulnerable to missed information.
Infection control during care transitions is not always prioritized. Direct care staff may not always know what to communicate during patient transfer reports, and the person receiving the report may not be the one providing ongoing care. As a result, hospitals may receive incomplete or delayed information, complicating treatment decisions. When a resident with an infection transfers, crucial details — such as prior multidrug-resistant organism (MDRO) colonization, infection history, pending lab cultures, or current antibiotic use — may not be communicated to the right person. These key details can be lost without direct communication between care settings. Even small communication gaps can have serious effects: unnecessary repeated testing, inappropriate antibiotic use, or delays in appropriate isolation precautions. These can increase costs, hospital length of stay, and the risk of patient harm.
Improving infection control during care transitions requires stronger partnerships between hospital staff and their counterparts in nursing homes. A recent sepsis-focused quality improvement project highlighted how direct collaboration can close this gap. In this project, IPs at a rural nursing home and a local hospital began regular communication to ensure infectionrelated information was exchanged during transfers. Initially sparked by friendly introductions and a shared concern over rising sepsis admissions, the partnership quickly demonstrated results. By connecting directly, the IPs could review MDRO histories, pending cultures, and antibiotic status within 24-48 hours of admission. This allowed hospital clinicians to make better-informed decisions and avoid unnecessary antibiotic use. Over time, the partnership expanded to include discussions of infection trends and challenges, such as determining prior colonization status and resistance patterns. What began as a single initiative evolved into a streamlined communication process, improving patient safety.

Hospital staff can take steps to strengthen communication with nursing homes and improve infection prevention during care transitions:
1. Request infection-related details at transfer. Ask about infection history, MDRO colonization, recent lab results, medication, and antibiotic use.
2. Encourage direct communication between IPs. If your facility does not have a formal process, suggest that your IPs communicate between settings. If you do not know the correct contact, case managers or discharge planners can help.
3. Document and communicate infection risks. Ensure that infection history is documented and passed to hospital staff during transfers. This prevents unnecessary antibiotic use and helps hospitals implement appropriate precautions.
4. Advocate for a structured collaboration. Some hospitals and nursing homes have established scheduled checkins between IPs to review infection-related transfers at regular intervals.
Even a brief phone call, a standing email exchange, or a weekly check-in can make a measurable difference in preventing infections and improving care.
Hospitals are uniquely positioned to set the tone for effective infection prevention partnerships. Because they often serve as the hub for complex care, hospital staff can lead by establishing consistent expectations
for information exchange, modeling best practices, and offering support to nursing homes with fewer resources. With proactive communication, hospitals protect their patients and strengthen the entire continuum of care across the community.
Infection control should not happen in isolation. Nursing home and hospital staff may work in different settings but share the same goal: keeping those they serve safe and healthy. Establishing partnerships between facilities does not just improve infection prevention — it enhances overall care quality, reduces unnecessary hospitalizations, and supports staff by creating clearer, more reliable processes.
If you are an Infection Preventionist, take the first step. Contact your local nursing home IP and start the conversation. A simple phone call today could mean improved resident outcomes tomorrow.
Infection prevention is not just about policies or protocols — it is about relationships. We can reduce avoidable infections, improve stewardship, and ensure safer care transitions by fostering direct communication between hospitals and nursing homes.
You do not have to do this alone. Together, hospital and nursing home staff can create a stronger, more connected approach to infection prevention that puts resident care first.

Nine out of 10 patients (89%) are satisfied with their recent experience receiving care from a hospital system within their community.
A new Morning Consult poll found hospital systems overwhelmingly meet patient expectations when it comes to receiving care.
91%
Nearly all patients surveyed cited the ability of their care team to easily access their medical history, lab results or other essential health information as a benefit of receiving care in a hospital system.
82%
More than 8 in 10 patients agree their care within a hospital system was efficient and accessible.
89%
9 in 10 hospital system patients find comfort in the fact that their hospital system has specialists or provides complex care that they may need in the future.
*Data from 2023

What does it mean to be taken care of? At Arkansas Blue Cross and Blue Shield, it means providing peace of mind. We’ve been taking care of Arkansans for over 75 years, providing affordable, reliable health insurance … to keep Arkansans healthy and help them heal. We’re investing in communities to keep this diverse and wonderful state strong. We’re committed to a whole person approach to health, including physical and behavioral well-being. And we recognize that total health is influenced by many factors, including medical history, genetics, lifestyle, environment, nutrition, safety and physical activity. We also realize that it will take all healthcare providers working together to ensure future generations of Arkansans can live their best life their whole life long. Let’s take good care, Arkansas.




For over 75 years, Nabholz has upheld our purpose: Grow our people. Serve our clients. Build our communities. Our extensive work on healthcare facility projects aligns with just that by giving medical professionals and the surrounding communities the tools they need to succeed.