
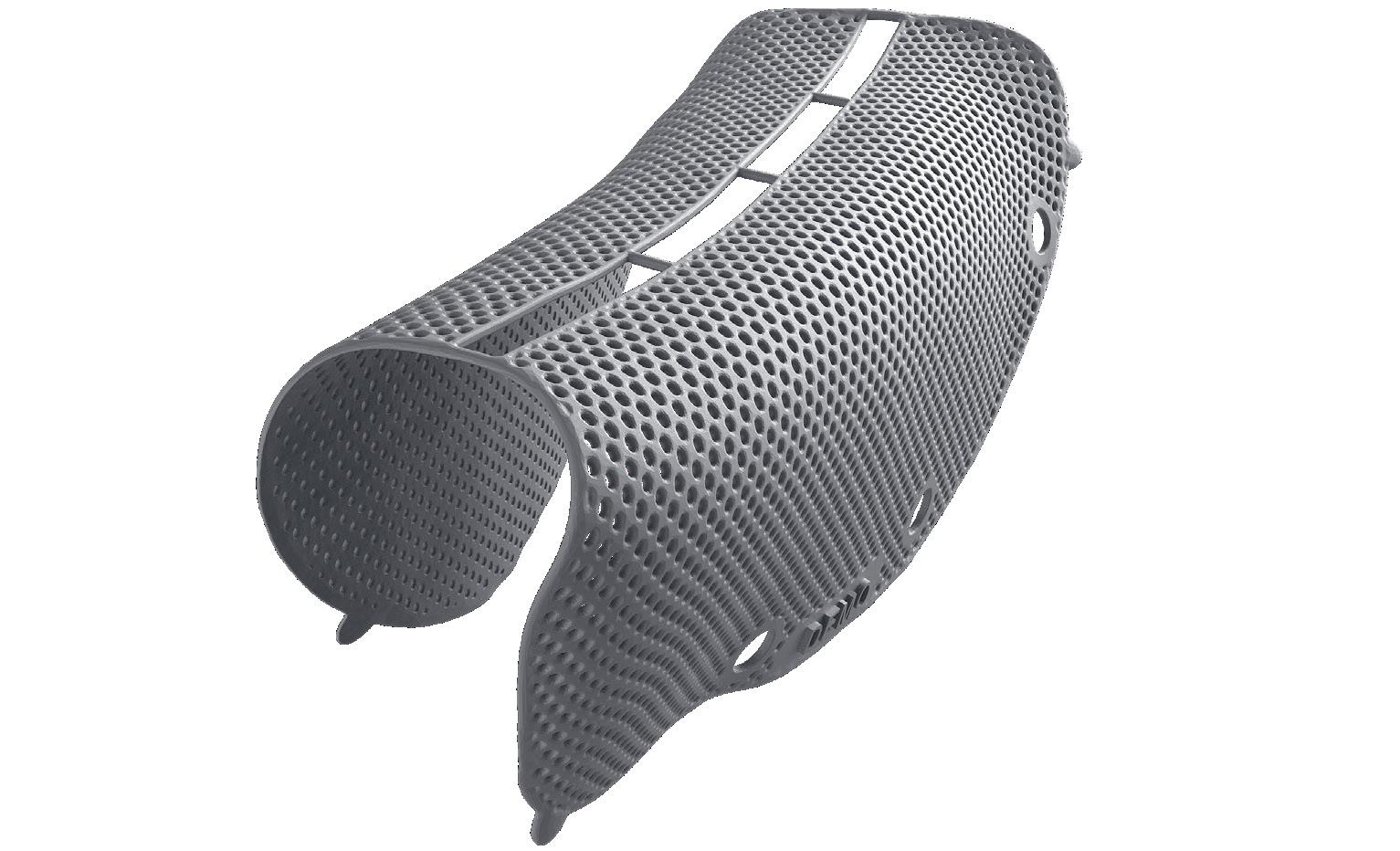
Titanium for reliable stability and space maintenance


Titanium for reliable stability and space maintenance
Precise patient-specific
3-D printing
Fully microstructured surface protects from tissue ingrowth
Titanium for reliable stability and space maintenance
Less surgery time due to perfect fit without shape adaptation
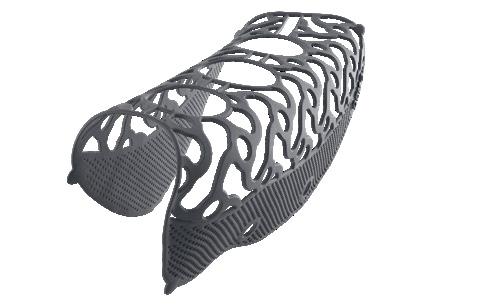
Precise patient-specific
3-D printing
Less surgery time due to perfect fit without shape adaptation
Calculation of augmentation volume (optional)

”I have been using the new Yxoss with a dense structure for the last 2 years and I can state that they are very effective and predictable devices for horizontal and vertical ridge augmentation. When associated with 70% of autogenous bone chips and 30% of DBBM their efficacy is comparable withthe one of traditional PTFE non-resorbable membranes, but much easier and faster to be installed.“
Prof. Massimo Simion
”I have been using the new Yxoss with a dense structure for the last 2 years and I can state that they are very effective and predictable devices for horizontal and vertical ridge augmentation. When associated with 70% of autogenous bone chips and 30% of DBBM their efficacy is comparable withthe one of traditional PTFE non-resorbable membranes, but much easier and faster to be installed.
Integrated implant positioning (optional)
Calculation of augmentation volume (optional)
Integrated implant positioning (optional)
Head-to-head comparison as assessed by Dr. Seiler and Dr. Ronda
Head-to-head comparison as assessed by Dr. Seiler and Dr. Ronda
Prof. Massimo Simion



Head-to-head comparison as assessed by Dr. Seiler and Dr. Ronda
The Australasian
Journal of Oral and Maxillofacial Surgery is the official scientific journal of the Australian and New Zealand Association of Oral and Maxillofacial Surgeons
Aim and Scope
The Australasian Journal of Oral and Maxillofacial Surgery is the premier forum for the exchange of information for new and significant research in oral and maxillofacial surgery, promoting the surgical discipline in the Oceanic region.
Oceania comprises 19 countries, spread over one-sixth of the globe, but with Australia and New Zealand being the dominant developed countries.
The Journal comprises peer-reviewed scientific reports, reviews, case reports of rare and unusual conditions, and perspectives; all of value for continuing professional development.
Information for prospective authors, including author guidelines, publication ethics, malpractice statements and patient consent forms are available for download from the Australian and New Zealand Association of Oral and Maxillofacial Surgeons homepage. All correspondence with the Editor is via editorajoms@anzaoms.org
Advertising Information
The Australasian Journal of Oral and Maxillofacial Surgery accepts paid advertisements from companies involved with the surgical discipline. For information on advertising guidelines and rates contact Ms Belinda Mellowes, Executive Officer, Australian and New Zealand Association of Oral and Maxillofacial Surgeons: eo@anzaoms.org Submit advertisements to ajoms@anzaoms.org
Disclaimer
The Australasian Journal of Oral and Maxillofacial Surgery Editors and Editorial Board cannot be held responsible for error or consequence arising from the information contained in the Journal. The views and opinions expressed herein do not necessarily reflect those of the Australian and New Zealand Association of Oral and Maxillofacial Surgeons, AJOMS Editor or Editorial Board. Neither does publication of advertisements constitute any endorsement of the products advertised. © 2025 ANZAOMS
Alastair Goss
• Emeritus Professor of Oral and Maxillofacial Surgery, The University of Adelaide
• Emeritus Consultant Surgeon, The Royal Adelaide Hospital
Adelaide, SA, Australia
Andrew Heggie, AM
• Clinical Professor, Department of Paediatrics, The University of Melbourne
• Senior Consultant Oral and Maxillofacial Surgeon, Royal Children’s Hospital of Melbourne
Melbourne, VIC, Australia
David Wiesenfeld
• Honorary Clinical Professor, The University of Melbourne
• Lead in Head and Neck Research and Education, The Victorian Comprehensive Cancer Centre
Melbourne, VIC, Australia
Website and Distribution
Belinda Mellowes
• Executive Officer, Australian and New Zealand Association of Oral and Maxillofacial Surgeons
Sydney, NSW, Australia
AMPCo Production Editors
Laura Teruel
Kate Steyn
AMPCo Graphic Design
Peter Humphries
Catherine Offler
• Administrative Assistant to the Editor
Adelaide, SA, Australia
Kathryn Steward
• Advertising Sales and Administration – Membership and Administration Coordinator, Australian and New Zealand Association of Oral and Maxillofacial Surgeons
Sydney, NSW, Australia

Business Manager
Dieter Gebauer
• Senior Consultant in Oral and Maxillofacial Surgery, Royal Perth Hospital
• Clinical Associate Professor in Oral and Maxillofacial Surgery, The University of Western Australia
Perth, WA, Australia
Members
Alexander Bobinskas
• Consultant Oral and Maxillofacial Surgeon, The Canberra Hospital
• Research Fellow, The John Curtin School of Medical Research
Canberra, ACT, Australia
Arun Chandu
• Senior Consultant in Oral and Maxillofacial Surgery, Royal Dental Hospital of Melbourne
• Clinical Associate Professor of Oral and Maxillofacial Surgery, The University of Melbourne
Melbourne, VIC, Australia
Nigel Johnson
• Consultant Oral and Maxillofacial Surgeon, Princess Alexandra Hospital
• Senior Lecturer in Oral and Maxillofacial Surgery, The University of Queensland
Brisbane, QLD, Australia
Paul Sambrook, AM
• Director Oral and Maxillofacial Surgery, The Royal Adelaide Hospital
• Senior Lecturer in Oral and Maxillofacial Surgery, The University of Adelaide
Adelaide, SA, Australia
Darryl Tong
• Professor of Oral and Maxillofacial Surgery, The University of Otago
• Senior Consultant in Oral and Maxillofacial Surgery, Dunedin Public Hospital
Dunedin, New Zealand
Ex Officio Members
Jasvir Singh
• President, Australian and New Zealand Association of Oral and Maxillofacial Surgeons
• Consultant in Oral and Maxillofacial Surgery, Prince of Wales Hospital
Sydney, NSW, Australia
Patrishia Bordbar
• Immediate Past President, Australian and New Zealand Association of Oral and Maxillofacial Surgeons
• Consultant in Oral and Maxillofacial Surgery, The Royal Children’s Hospital of Melbourne
• IAOMS Executive Representative – Oceania Region Melbourne, VIC, Australia
John Harrison
• Regional Councillor for Oceania, International Association of Oral and Maxillofacial Surgeons
• Senior Consultant in Oral and Maxillofacial Surgery, Auckland City and Middlemore Hospital
Auckland, New Zealand
Jocelyn Shand
• Clinical Associate Professor, Department of Paediatrics, The University of Melbourne
• Chair, Australian and New Zealand Association of Oral and Maxillofacial Surgeons Research and Education Foundation
• Head of Section of Oral and Maxillofacial Surgery, The Royal Children’s Hospital of Melbourne
• Vice President Elect, International Association of Oral and Maxillofacial Surgeons
Melbourne, VIC, Australia
Research articles in orthognathic surgery: predictors of their societal and professional impact
Doğramacı EJ and Rao A
Accuracy of virtual surgical planning for orthognathic surgery without the use of a guide splint during radiographic image acquisition
Dreyer DC, Jensen ED, Liau I, Cheng A and Sambrook P 23 CASE REPORT
Computer-guided customised treatment of unilateral condylar hyperplasia by proportional condylectomy and orthognathic surgery
Wang D, Smit R, Harrison J and Sealey C
TECHNICAL INNOVATION
Primary inferior alveolar nerve protection: a CAD/CAM approach
Betar N, Badri D, McCombe A and Finn B
31 CASE REPORT
Myositis ossificans traumatica of the masticatory muscles following orthognathic surgery: a case report
Mian M, Gearing PF, Chen J, Sreedharan S, Kumar R and Nastri A
37 REVIEW ARTICLE
Sir John Walsh Oration 2024: the post-pandemic future of health care in New Zealand
Sir A Bloomfield
41 CASE REPORT
Intraoperative management of the no-reflow phenomenon during microvascular fibula free flap reconstruction using alteplase: a case report
Petterson C, Singh T and Ananth K
44 REVIEW ARTICLE
Management and recurrence of desmoplastic fibroma: a systematic review
Shirky D, Majid H, Chin M, Zachar J and Johnson NR
• Access medico-legal experts, 24/7 in emergencies
• Leading defence, with local support from Avant Law’s 80+ medico-legal solicitors nationwide
• Medical advisors for peer support in a claim
• Personalised advice to reduce your claims risk
By your side, with support to protect your career.


I took a detour to Dinosaur Valley near Winton, far west Queensland, on my way to the Australian and New Zealand Association of Oral and Maxillofacial Surgeons (ANZAOMS) Annual Scientific Meeting 2024. Ninety million years ago, the 20-metre long vegetarian dinosaur Savannasaurus elliottorum roamed the area. It left giant footsteps in the mud during the dinosaur stampede. It became extinct but left enormous, fossilised bones. More successful were the chicken-sized, two-legged, carnivorous velociraptors, which eventually evolved into the forebears of birds.1
Another flight success was the conception of our national airline, Qantas, in nearby Winton. The airline was developed at Longreach, which now houses the Qantas Foundation Museum. Under a gigantic awning are displayed four airplanes key to the development of commercial aviation in Australia: the Douglas DC3, the Lockheed Super Constellation, the Boeing 707 1388, and the Boeing 747 200. They have all evolved in the lifetime of commercial flight; indeed, I have flown commercially on all of them. My first flight was on a modified Fairey bomber, a biplane with many wires and struts called a “Stringbag”. The evolution of flight has not been linear, as exemplified by the extinction of the Comet and Concord airplanes.2
Over a similar lifespan, the specialty of Oral and Maxillofacial Surgery has evolved. In the 1970s, it was a heterogenous, individualistic, university-based dental specialty with wide variation in training. It was in danger of being swallowed up as a dependent subgroup of Plastic Surgery. This risk of extinction was recognised, and a plan for the 1980s was developed.3 A hospital- and university-based training, leading to a single exit College-based Fellowship under a single binational training authority with regular scope and workforce studies was proposed. This was implemented and there is now a well regarded homogenous high level Maxillofacial specialty.4
A further step in the evolution of the specialty has been the development of the Australasian Journal of Oral and Maxillofacial Surgery (AJOMS). The first edition was published in May 2024. This edition is a high quality scientific publication, with an emphasis on head and neck oncology. There were, however, major production difficulties. These have been resolved by engaging the publishers of the Medical Journal of Australia for production of AJOMS. You can see the marked improvement in the scientific presentation in this AJOMS Volume 2, Issue 1 (May 2025) edition. It covers the full scope of the specialty, but with emphasis on the evolution of bimaxillary orthognathic surgery. Virtual surgical planning, computer-assisted design and manufacturing (CAD/CAM) implant guides, and Altmetric Attention Scores are all a long way from plaster models, wax and wires, and the hand/eye coordination of the early orthognathic surgeons.
However, just as some dinosaurs died out and others evolved to fly, we do need to be constantly aware of the challenges and opportunities that face us. Much has been achieved in our recent history with strength through collaboration, innovation, research and education. We should all be diligent in our workplaces and institutions to ensure continued evolution as an essential specialty within our anatomical region. Opportunities for advancement are all around us and need to be embraced.
Alastair Goss
Foundation Editor AJOMS doi: 10.63717/2025.MS0052
1 Australian Age of Dinosaurs. Savannasaurus elliottorum [website]. https://www.australianageofdinosaurs.com/ page/53/australian-age-of-dinosaurs-savannasauruselliottorum (viewed Nov 2024).
2 Qantas Founders Museum. Welcome to the birthplace of Australian aviation. https://www.qfom.com.au/ (viewed Oct 2024).
3 Monsour FN, Goss AN. Oral surgery training in Australia and New Zealand. A plan for the eighties. Education Subcommittee report. Sydney: Australian and New Zealand Association of Oral and Maxillofacial Surgeons, 1982.
4 Ricciardo PV, Vujcich NJ, Bobinskas A, Goss AN. Survey of Australian and New Zealand Oral and Maxillofacial Surgeons 2020. Austral J Oral Maxillofac Surg 2024; 1: 77-84.
Maxillo Facial Imaging (MFI) is Australia’s leading dental radiology provider, focusing solely on CBCT, OPG and Ceph with specialist Oral & Maxillofacial Radiologist reporting.
y The highest quality imaging & work ups
y Oral & Maxillofacial Radiologists
y State-of-the-art imaging technology

Assoc. Prof. Ronnie Ptasznik Senior Radiologist


Emeritus Prof. Paul Monsour Oral & Maxillofacial Radiologist

Dr. Tess Matias Oral & Maxillofacial Radiologist
y Elevated patient care
y Convenient locations
y 24 hour turnaround times available

Dr. Daniel Selim Oral & Maxillofacial Radiologist

Dr. Scott McNab Oral & Maxillofacial Radiologist

Dr. Remy Golding Oral & Maxillofacial Radiologist

Dr. Ivor Berman Radiologist MFI
Doğramacı EJ (PhD, MSc, BDS, PG Cert LTHE, MFDS, MOrth RCSEng, FDS RCSEd, FHEA)1; Rao A (BDS, BSc-Dent Hons)2
Orthognathic surgery (OG) “is a field within two distinct specialities: Oral and Maxillofacial Surgery and Orthodontics”,1 which is defined as “… the surgical repositioning of the maxilla and/or mandible, and/ or their segments thereof, with or without orthodontic repositioning of the teeth, in order to improve dentofacial function and aesthetics (in a stable manner) and health-related quality of life”.2 In Australia, surgery is provided, for the most part, by oral and maxillofacial surgeons, though other specialists including oral-cranio/ maxillofacial surgeons, plastic surgeons, reconstructive surgeons, and otorhinolaryngologists provide surgery in other global settings.3 The surgical team is rounded out by orthodontists and dentists who align and decompensate teeth, or provide restorations and simple extractions, respectively, as part of the multidisciplinary team. Improved dentofacial aesthetics is a key patient-reported outcome4 (versus patient-centred outcome) frequently sought by prospective patients, which makes this subspecialty different to other dental or surgical specialties where treatment or intervention is often initiated following an objective needs-based assessment conducted by clinicians or health professionals.
Prospective patients seek information about their current presentation and possible treatment options; this is often performed online, “… owing to the volume of resources, ease of access, and the convenience of ‘surfing the internet’ whenever and wherever they desire”.5 However, much information that a lay person may access on the internet is of moderate quality, uses moderate to very low levels of evidence and is not always credible, with subject matter often being inaccurate or unreliable.6,7 Scant information about OG, written for a lay audience, exists online, with very few of the available content considered to be suitable for them.8 Moreover, research findings may not be accessible to the lay public, particularly when published behind a subscription-based paywall. Thus, grant-funding institutions often mandate open access (OA) models of publication, particularly when the research is publicly funded, to “maintain, increase and diffuse knowledge” to the wider community.9 In turn, engagement with research such as mentions in multiple social media platforms, news outlets, video websites, patents and policy documents can be quantified in what is known as an Altmetric Attention Score (AAS) (Georg von Holtzbrinck, Germany), a non-metric value that can be
Purpose: This study aimed to identify factors predicting the societal and professional impact of orthognathic surgery research articles.
Methods: This cross-sectional study followed a two-step search strategy to identify orthognathic surgery research articles in Medline; data for included articles were collected from Scopus, Incites, Altmetric Explorer and ProQuest. Analyses comprised descriptive statistics, frequency distributions, cross-tabulations and unadjusted/adjusted negative binomial regression models (P < 0.05).
Results: Of 107 903 articles retrieved, 378 were included; 46.3% of research originated from Asia, 74.1% were published in specialty journals and over three-quarters published in an impact factor journal. Most articles were primary research, 89% of articles were cited, 12 were grant-funded, 14 had a news mention and 84 attained an Altmetric Attention Score. Societal impact was greatest amongst systematic review/meta-analysis articles (Exp B, 20.96; 95% CI, 5.07–86.67; P < 0.001) and non-grant-funded research (Exp B, 18.12; 95% CI, 3.54–92.85; P < 0.001). Open access publication in an impact factor journal and news mentions also predicted societal impact. Professional impact was predicted only by systematic reviews (Exp B, 2.08; 95% CI, 1.02–4.23; P < 0.05).
Conclusions: Societal and professional impact is strongly predicted by article type, particularly systematic reviews. Impact of a research article can be further enhanced by publishing open access and in impact factor journals.
used as a proxy measurement of the societal impact of research,10,11 which generally signifies the impact or influence that is achieved by research at different levels and areas of society, outside the academic or university sector.12,13
1Adelaide Dental School, The University of Adelaide, Adelaide, SA, Australia; 2Adelaide Medical School, The University of Adelaide, Adelaide, SA, Australia. Corresponding author: Esma J Doğramacı ✉ esma.dogramaci@adelaide.edu.au | doi: 10.63717/2025.MS0034
Keywords: interdisciplinary research | multivariate analysis | orthognathic surgery | regression analysis
Citations are traditional metrics that arise from peer-reviewed publications. Although they are unable to glean information about the societal impact of research, they can represent professional impact. Furthermore, citations have been an area of focus in bibliometric studies, first defined by Pritchard14 as “the application of mathematics and statistical methods to books and other media of communication”. In oral and maxillofacial surgery (OMS), the subspecialty of craniomaxillofacial deformity accounts for the second-highest number of citations amongst the top-200 cited articles published in high impact factor (IF) OMS journals over the past four decades.15 Craniomaxillofacial deformity is also one of the most highly cited subspecialties amongst the top-cited systematic reviews published in OMS journals.16 Highly cited OMS articles are characterised as having greater mean abstract and manuscript word counts, more pages and figures, as well as a larger number of references;17 however, these attributes should be considered with caution as they are often influenced by the submission guidelines and house style of journals.
Even though adoption of social media to raise readership levels and enhance knowledge transfer of OMS research has been encouraged, its effectiveness in achieving societal impact remains unexplored.18 The independent variables that interact simultaneously, beyond article-level characteristics, to predict the professional impact of OG research have not been studied, with bibliometric studies criticised as lacking the ability to assess non-scholarly impact beyond the academic and research communities.19 One alternative approach is scientometrics, a specialist field within bibliometrics that in addition to article-level data, integrates social sciences, information science and advanced mathematics to identify “patterns in big data”.20 Through a scientometric approach, the aim of this research is to identify the factors that are predictive of societal and professional impact of OG research, and secondly, to identify the top ten research articles that achieved the greatest societal impact and to describe their characteristics.
This was a cross-sectional scientometric review of all OG articles published in the 2019 calendar year, this being used as a single representative year because of the global COVID pandemic-related disruptions that subsequently affected the nature, conduct and publication of research. The methodology used in this study has previously been applied in similar research in other specialties.10,11
Data collection methods
Identification of articles: search strategy
A two-step search strategy was used to identify OG research articles published in specialty (OMS) and non-specialty journals and indexed in the Medline database. The initial search aimed to determine the titles of OMS journals as sources for published studies. On 22 November 2022, the National Library of Medicine (NLM) Catalog was accessed with three search terms entered into the advanced search builder: “oral and maxillofacial surgery” [Journal] OR
“maxillofacial” [Journal] OR “craniofacial” [Journal]. Next, the identified journal titles were entered into the search field in Medline (via OVID), with a parallel search, also in Medline (via OVID), performed using “orthognathic surgery” OR “orthognathic surgical procedures” as a keyword or abstract or MESH term from inception date through to 20 November 2022. All identified records were pooled within Medline (via OVID), with duplicates removed automatically. The inclusion criteria for this study were primary research articles, systematic reviews with or without meta-analysis, narrative reviews, and case reports or series published between 1 January and 31 December 2019. As editorials, opinion articles, book and article reviews, commentaries, letters, replies and obituaries are not research articles per se, automated exclusion ensued by limiting the search to articles with abstracts. Articles published outside of 2019 or in a language other than English were also ineligible and were also excluded automatically through the application of the respective limits in Medline (via OVID).
After records were identified for possible inclusion, their titles and abstracts were screened by two reviewers, independently and in duplicate, within Medline (via OVID). Any disagreements were resolved through discussion, and the input of an independent colleague would be sought where consensus could not be reached.
Following exclusion of records at the screening stage, data of records that remained for inclusion were exported from Medline into a digital data collection form in Microsoft Excel for Windows, version 2301 (Microsoft, United States) that comprised: PubMed ID, article title, article source (journal name and bibliographic data), authors, author affiliations, digital object identifier (DOI), date of publication and grant information. The 2019 InCites Journal Citation Reports (Clarivate, United Kingdom) was used to determine those journals that had an IF. On 30 November 2022, the DOI of each identified article was entered into Scopus (Elsevier) to establish the number of citations and publishing model of each article. Articles not indexed in Scopus had their OA status verified using their DOI or in its absence, through the article link available from Medline (via OVID).
AAS, a non-metric article-level value, is produced through an automated algorithm, where the number of online mentions that are made about an article (that has a DOI) in an Altmetric-tracked outlet are combined, with variable outlet-based weightings, to produce the final AAS value.21 The AAS of each article was identified on 29 November 2022 by entering the DOI of each article, where available, into the advanced search tool of Altmetric Explorer (Georg von Holtzbrinck, Germany). Results were exported from Altmetric Explorer into a comma-separated values (.csv) file that was then transformed into a Microsoft Excel Workbook (Microsoft Excel for Mac, version 16.43; Microsoft, United States) that included the following: article title, journal/collection title, AAS, the number of mentions each article received in each of the Altmetric-tracked outlets, as well as the nature of the mentioning outlets.
On 9 January 2023, an advanced search was performed in the ProQuest platform (ProQuest, United States) to determine the presence of any news mentions of the identified articles. The subject terms “orthognathic” and “research” were entered in the search field, limited to newspaper items or wire feeds published between 1 January and 31 December 2019. Retrieved items were then limited to document type “news”, with the remaining results read and matched to articles in the digital data collection form using their DOI.
Dependent variables
There were two dependent variables investigated. The first was societal impact of OG research articles. AAS was used as a proxy measurement for societal impact. Where an article had an AAS, this was recorded as a continuous variable. The second dependent variable was professional impact of OG research articles. Citations were used as the proxy measurement for professional impact and was also recorded as a continuous variable.
Independent variables
There were seven independent variables investigated:
1. Origin: The continent where the research was conducted. This was determined using the primary (first) author’s affiliations. Each article was assigned to one of six continents.10,11 In instances where the author had multiple affiliations spanning multiple continents, the article was categorised as “intercontinental”, which acted as the reference variable.
2. Journal type: Whether the article was published in a specialist OMS journal or not. Any article published in a journal identified as oral/maxillofacial surgery was coded “yes” (= 1), which acted as the reference variable. All remaining articles were coded non-oral/ maxillofacial surgery (= 0).
3. Journal IF: Binary coding was used to distinguish those articles published in a journal with an IF; this acted as the reference variable (= 1).
4. Article type: Articles were classified into quintiles labelled primary research, systematic review/metaanalysis, systematic review, narrative review, and case reports, the latter serving as the reference variable.
5. Grant funding: Whether a research article received grant funding
was recorded dichotomously, with grant-funded research (= 1) serving as the reference variable.
6. Publishing model: This was also recorded dichotomously for each article, with articles published OA (ie, not behind a paywall) acting as the reference variable.
7. News mention: If a research article was mentioned in a newspaper item or wire feed, it was coded “yes” (= 1) where present; this acted as the reference variable.
AAS was additionally used as an independent variable for professional impact, where its presence was coded dichotomously with “yes” (= 1) acting as the reference variable.
Where an article was identified as having been published OA, the type of publishing model was classified into all the relevant OA types, which could be more than one type: gold, hybrid gold, green, bronze.22 Altmetric-tracked mentions for articles were assessed by collecting data about their outlet (where the mentions were made) and the number of mentions from each outlet, and where available, the name of the party making the mention.
Data in the digital collection form, as well as data exported from Altmetric Explorer in .csv files, were imported into separate files in IBM SPSS Statistics, version 28 software (IBM, United States). Initial analyses comprised descriptive statistics, frequency distributions and cross-tabulation. Results for categorical outcomes were expressed as unadjusted means. Bivariate analysis for the dependent variables AAS and citations were performed using negative binomial regression on account of overdispersion, which was followed by use of multivariate negative binomial regression models.23 AAS was an

additional categorical variable when analysing citations. Statistical significance was set at P < 0.05.
The NLM search retrieved 18 titles.
Using the journal titles identified in the NLM search, a total of 100 242 records were identified using Medline (via OVID), while 7661 were retrieved using the keyword or abstract or MESH term. This produced a combined total of 107 903 articles (Figure 1). After the application of limits related to publication date, publication in English and published articles having an abstract, 3630 records remained for screening. After excluding records that were not OG research, commentaries/article reviews and withdrawn articles, 378 records remained for analysis. Six articles were not indexed in Scopus and, therefore, their citation counts could not be determined.
Origin
Altmetric Attention Score Citations
Journal
In 2019, 378 orthognathic surgery research articles were published across six continents, almost half (46.3%) originating from Asia (Table 1). Nearly three-quarters (74.1%) of articles were printed in dedicated OMS specialty journals. Over 80% of articles (n = 330) were published in a journal with an IF. More than a quarter of articles (n = 109) were available OA, with the various classifications comprising gold (n = 59), hybrid gold (n = 2), green (n = 92), and bronze (n = 15). Of those articles published OA, nearly two-thirds (n = 68) were in journals with an IF. The majority (n = 303) of articles were primary research, with 37.8% (n = 115) published in a dedicated OMS specialty journal. Over half (n = 9) of narrative review articles were published in dedicated OMS journals as well as two-thirds (n = 10) of systematic reviews. Case reports and meta-analysis articles were mostly published in non-OMS journals. A dozen articles (3.2%) were grantfunded, all of them being primary research in nature. Over half (n = 7) of these were published OA, with all but one published in a non-OMS journal. Five grant-funded research articles originated from Asia and five from North America, and one each from Europe and Oceania. All but one grant-funded research articles were cited. Most OG research articles (71.2%) were published behind a subscription-based paywall, with OMS journals accounting for 39.8% (n = 107) of these articles. Very few articles (3.7%) received a news mention.
SE = standard error. * P < 0.001. † P < 0.01. ‡ P < 0.05.
Table 1. Unadjusted associations of societal and professional impact
Societal impact of orthognathic surgery research and its predictors
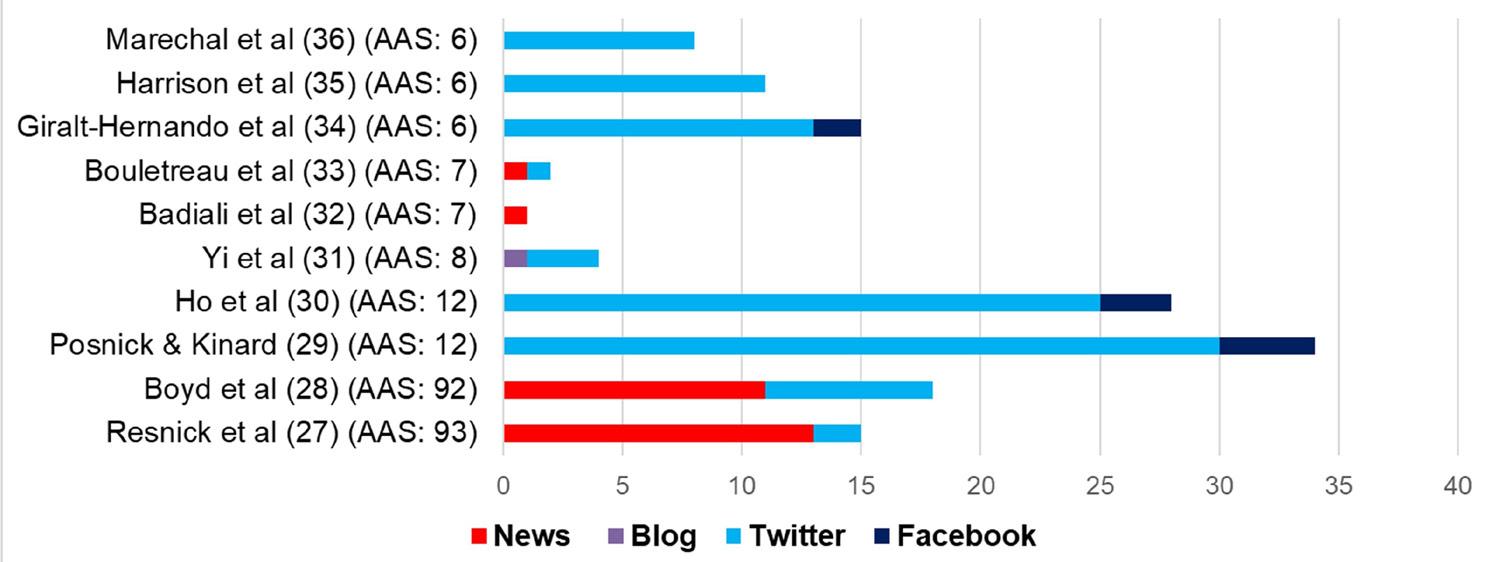
Less than a quarter (n = 84) of articles received a total of 275 mentions, tracked by Altmetric Explorer, that comprised: 192 individual tweets, 42 posts on public Facebook pages, 27 news stories, eight Wikipedia entries, two mentions in policy documents, and a single mention each in a patent, a video upload, a blog and a Google+ post. The top tweeters were @AmerCleftPalate (US) (n = 9; 2348 followers), @ELSSurgery (France) (n = 8; 7897 followers), @prsjournal (unknown origin) (n = 7; 20 873 followers), @EvidenceRobot (UK) (n = 6; 7418 followers) and @RamiKantar1
Maxillomandibular advancement improves multiple health-related and functional outcomes in patients with obstructive sleep apnea: a multicenter study
12 Orthognathic surgery has a significant positive effect on perceived personality traits and perceived emotional facial expressions in subjects with primary maxillary deficiency
Intraoral scanning and setting up the digital final occlusion in threedimensional planning of orthognathic surgery
5 8 Effect of conventional combined orthodontic-surgical treatment on oral health-related quality of life: a systematic review and meta-analysis
6 7 An average three-dimensional virtual human skull for a template-assisted maxillofacial surgery
7 Artificial intelligence: applications in orthognathic surgery
and Kinard29
6 Impact of surgical maxillomandibular advancement upon pharyngeal airway volume and the apnoea-hypopnoea index in the treatment of obstructive sleep apnoea: systematic review and meta-analysis GiraltHernando et al34
6 Further construct validation of the CLEFT-Q: ability to detect differences in outcome for four cleft-specific surgeries
6 Gnathodiaphyseal dysplasia with a novel R597I mutation of ANO5: mandibular reconstruction strategies
al35
et al36
Oral and Maxillofacial Surgery
(US) (n = 6; 2603 followers). More than half (n = 24) of Facebook posts were made by two accounts: “Orthognathic surgery, Maxillofacial surgery information” (n = 15), based in Korea, and “American Cleft Palate-Craniofacial Association” (n = 9), based in the US. Seventeen different Altmetric-tracked news outlets mentioned multiple orthognathic surgery research articles. Most news mentions originated from the US (n = 18), with two each from Guam, Turkey and the UK. A single article had 13 Altmetric-tracked news mentions, another had 11, and three articles were each mentioned once. Two articles were mentioned in two policy documents by the Association of the Scientific Medical Societies in Germany.24,25 A patent titled “Extraoral orthopaedic device for the direct protraction of the maxilla and the indirect protraction of the mandible” cited an article about reverse facelift for facial rejuvenation.26 “The Dental Elf”
(https://www.nationalelfservice.net/dentistry/ ) mentioned a single article in a blog. Of the 84 articles achieving an AAS, 58 were published in dedicated OMS journals. The median AAS was 1, achieved by 50 research articles (Figure 2). The highest AAS (93) was achieved by a single article (Figure 2, Table 2).27 Four articles within the top ten articles ranked on AAS had a news mention, with the top two articles having a combined total of 24 Altmetric-tracked news mentions (Figure 3).27,28 The variety of sources of mentions was limited to Twitter (rebranded to X on 23 July 2023), Facebook, news outlets and a blog; the maximum number of sources of mentions for any of the top ten ranked articles was two (Figure 3). Half of the top ten articles originated from Europe, half were also published OA, though none were grant-funded. All but three of the top ten articles were primary research, and citations ranged between three and 30.
With the exception of news mentions, the societal impact (ie, AAS) achieved by OG research articles was significantly associated with all independent variables (Table 1). Articles from North America, primary research or systematic reviews/metaanalyses, and articles published OA had significantly greater societal impact (P < 0.001). Articles published in dedicated OMS specialty journals also had significantly higher societal impact (P < 0.01), as did non-grant funded research and articles published in IF journals (P < 0.05). The adjusted models confirmed the unadjusted effects of origin of research, article type, grant-funding and OA publication (Table 3). Higher societal impact was achieved by systematic reviews/ meta-analysis articles (Exp B, 20.96; 95% CI, 5.07–86.67; P < 0.001), and primary research articles (Exp B, 3.43; 95% CI, 1.20–9.87; P < 0.05). Interestingly, nongrant funded research also achieved higher societal impact (Exp B, 18.12; 95% CI, 3.54–92.85; P < 0.001), with articles originating from North America also attaining greater societal impact (Exp B, 8.06; 95% CI, 2.86–22.73; P < 0.001). Lower societal impact was associated with research articles published behind a subscription-based paywall (Exp B, 0.37; 95% CI, 0.24–0.57; P < 0.001), publication in a non-IF journal (Exp B, 0.36; 95% CI, 0.19–0.71; P < 0.01), and absence of a news mention (Exp B, 0.21; 95% CI, 0.10–0.47; P < 0.001). Publication in a dedicated OMS specialty journal did not influence societal impact.
Origin
Asia
Europe
South America
Altmetric Attention Score Citations
Exp B
Africa < 0.001 (0.00–0.00)
(0.45–1.54)
Intercontinental Ref Ref
Journal type
Non-oral/maxillofacial
Oral/maxillofacial Ref Ref
Impact factor
Yes Ref Ref
Article type
Case report Ref Ref
Grant funded
Yes Ref Ref
Open access
(0.24–0.57)* 0.78 (0.57–1.07)
Yes Ref Ref
Eighty-nine per cent (n = 338) of all OG research articles were cited, with over a quarter (26.9%) available OA. The median citation number was five, with the highest citation count being 154, achieved by a single article (Figure 4).37 All systematic reviews (n = 15) and meta-analyses (n = 6) were cited, with 91.1% of primary research also being cited. All but one narrative review was cited, and 71.1% of case reports were also cited. OA publication was very significantly associated with professional impact (ie, citations) (P < 0.01), and publication in a journal with an IF had a significant association (P < 0.05) (Table 1). In the adjusted model, systematic reviews had the only significant association (Exp B, 2.08; 95% CI, 1.02–4.23; P < 0.05) (Table 3). No other variables were predictive of professional impact.
News mention No
(0.10–0.47)* 0.67 (0.38–1.18)
Yes Ref Ref
Altmetric Attention Score
No - 0.84 (0.63–1.10)
Yes - Ref
CI = confidence interval; Ex P = exponentiated; Ref = Reference variable. * P < 0.001. † P < 0.01. ‡ P < 0.05.
Table 3. Adjusted associations of societal and professional impact
This present scientometric study aimed to identify the factors that predict societal and professional impact of OG research, and also, to identify the top ten research articles that achieved the greatest societal impact and to describe their characteristics. To our knowledge, this is the first study to apply a scientometric approach
to investigate the societal and professional impact of OMS research, with a focus on OG, thus making an innovative contribution and providing valuable insights into the factors that are predictive of impactful research in this area. Several statistically significant results were found. Systematic review/meta-analysis articles, research that is not grant-funded, research originating from North America, as well as articles that are published in an IF journal, available as OA or have a news mention achieve higher societal impact. Type of article (systematic review) is the only variable predictive of professional impact (ie, higher citations).
Recognising that OG is a subspecialty of both orthodontics and OMS, a more inclusive approach was adopted for identifying peer-reviewed research, as it may be published outside of dedicated OMS journals. This method differs from previous studies that have focused on a single specialty, where studies have been limited to analysing outputs in a single OMS journal, or multiple OMS journals that have “the highest impact factor scores as well as representing the specialty globally”.15 Furthermore, such studies are descriptive bibliometrics in nature, concentrating on publication of bibliographic data, including authorships, and analysing associated citations38,39 to “reveal the historical development of subject fields and patterns of authorship, publication and use”.40 Although scientometrics does have a degree of overlap with bibliometrics, it is not synonymous. Rather, it “uses measuring techniques for evaluation of advancement of science and its level of development, its impact and relevance to human society”,41 by using social sciences, information science and advanced mathematics to identify “patterns in big data”.20 Consequently, this study adopted multivariate modelling to identify the predictors of societal and professional impact of OG research.
Multivariate modelling is an advanced statistical procedure whereby the strength of a multitude of independent variables can be analysed concurrently when studying a particular outcome variable. This approach recognises the synergy that exists between the independent variables, which is contrary to analysing variables piecemeal using basic statistical tests, which has been criticised as potentially generating misleading conclusions or identifying factors that initially appear significant but lose their importance when considered alongside other factors.42 Through adjusted multivariate modelling, several salient factors were identified that contribute to the societal impact of OG research.


The finding that higher societal impact is achieved when publishing in an IF journal, receiving a news mention and not being grant-funded is consistent with endodontic research, whereas an OA publishing model being significantly predictive of higher societal impact is an attribute shared with orthodontic research.10,11 The
present study also confirmed findings from scientometric research into orthodontics and endodontics that systematic review/metaanalysis articles attract the highest AAS.10,11 Though research
from Oceania was predictive of higher AAS in endodontics and orthodontics, OG research from North America achieved the highest societal impact.10,11 Within OG research, only systematic review research articles significantly garner professional impact, whereas narrative reviews achieved higher citations in both orthodontic and endodontic research.10,11 The present study also validated previous findings that AAS is not correlated with citations in oral surgery; however, the opposite was observed in orthodontics and endodontics.10,11,43
These results can help all stakeholders involved in OG research as research and publication strategies could be developed to achieve targeted outcomes. For example, individual researchers working in the OG space may be more inclined to complete and publish systematic reviews in order to achieve higher citation counts, particularly if they are seeking tenure or promotion in an institution that values citations as part of the evaluation process. Researchers and research groups may choose to submit a research article to an IF journal and publish OA, since these approaches are predictive of significantly greater societal impact. Journal editors may prioritise publication of systematic review/meta-analysis research as these also achieve substantially high societal impact. Grant-funding bodies, however, may be disappointed that their funding of OG research is not achieving the societal impact that they may desire. In this study, a little over half of all grant-funded OG research was published in OA. Although OA publication is usually sine qua non, particularly when the research is publicly funded, funders may need to enforce this to enable knowledge translation and dissemination to the wider community. Science communication, particularly through Altmetrictracked news outlets, could be used by individual researchers, institutions, and grant-funding bodies to publicise their research findings, as substantial societal impact was achieved by four of the top ten OG articles, ranked on AAS scores. Non-normal distribution of AAS and citation counts were observed for OG articles published in 2019. The maximum AAS (93) was greater than that achieved in the subspecialty of implant dentistry (13) and orthodontics (63), though less than the scores achieved in endodontics (100), paediatric dentistry (160), and periodontology (308).10,11,44-46
One important limitation of this study is language bias, as only research articles published in English were eligible; research published in any other languages were excluded. This results in otherwise eligible research being overlooked. “Articles published in English have a higher number of citations than those published in other languages”,47 as English is considered the lingua franca for researchers.48 Incidentally, this term has its etymological origin in Arabic (lisan al-farang, literally meaning “Frankish tongue”), when language mediators translated between the Arabic and Romance languages,49 especially in the 12th century.50 Presently, the most widely spoken language by native speakers in the world is Chinese (1.3 billion people), followed by Spanish (486 million), English (380 million), Arabic (362 million) and Hindi (345 million).51 Thus, nonnative English speakers find science communication and knowledge
transfer difficult,52 which has led to suggestions that future research should not impose any language restrictions in the search strategy or as an eligibility criterion, any funds should be budgeted for translating articles when seeking research funding,53 or alternatively, involving co-authors with proficiency in languages other than English, with a recent example evident in a systematic review and meta-analysis on traumatic dental injuries.54 Low societal impact of research produced from non-English speaking countries such as China, Japan, India and Russia has previously been reported, despite their relatively high publication output; this was partially explained by their lower usage of Twitter, the main carrier of Altmetric-tracked mentions.55
Future research could explore how societal and professional impact of OG research changes with time, as well as assessing the research outputs of other subspecialties to understand the similarities and differences in their impact, societally and professionally. This, in turn, could trigger reflection and adoption of specific publication practices to help make research as impactful as possible. In this way, not only can OG research continue to achieve professional impact, but also reach a wider audience, particularly the lay patient who often seeks online information on the means to improve their dentofacial aesthetics through OG.
Within OG research articles, systematic review/meta-analysis articles and non-grant-funded research achieve the greatest societal impact, with systematic review articles being significantly predictive of professional impact. While grant-funded research is mostly published OA, further research could investigate and address the causes behind them not achieving significant societal impact.
Doğramacı EJ: Conceptualisation and methodology, data analysis and interpretation, data curation, validation, visualisation, supervision, project administration, writing (original draft), writing (review and editing), final approval of version to be published, accountable to all aspects of the work.
Rao A: Data acquisition, data analysis and interpretation, data curation, writing (original draft), final approval of version to be published, accountable to all aspects of the work.
Arya Rao was supported by the Adelaide Summer Research Scholarship 2022/2023, The University of Adelaide.
Conflicts of interest
The authors declare that they have no conflicts of interest.
sharing
The data underlying this article are available for sharing upon reasonable request to the corresponding author.
1 Naini FB, Gill DS. Preface. In: Naini FB, Gill DS; editors. Orthognathic surgery: principles, planning and practice. New York (NY): John Wiley and Sons, 2017; pp xxi-xxii.
2 Naini FB, Gill DS. Chapter 3 — Orthognathic surgery: preliminary considerations. In: Naini FB, Gill DS; editors. Orthognathic surgery: principles, planning and practice. New York (NY): John Wiley and Sons, 2017; pp 83-108.
3 Obwegeser HL. Chapter 1 — Introduction: Orthognathic surgery — a life’s work. In: Naini FB, Gill DS; editors. Orthognathic surgery: principles, planning and practice. New York (NY): John Wiley and Sons, 2017; pp 1-20.
4 Doğramacı EJ, Rossi-Fedele G. Patient-related outcomes and oral health-related quality of life in endodontics. Int Endod J 2022; 56 (Suppl): 169-187.
5 Doğramacı EJ. Adult orthodontics: a quality assessment of internet information. J Orthod 2016; 43: 162.
6 Doğramacı EJ, Rossi-Fedele G. The quality of information on the internet on orthodontic retainer wear: a crosssectional study. J Orthod 2016; 43: 47-58.
7 Doğramacı EJ, Peres MA, Peres KG. Breast-feeding and malocclusions: the quality and level of evidence on the internet for the public. J Am Dent Assoc 2016; 147: 817825.
8 Aldairy T, Laverick S, McIntyre GT. Orthognathic surgery: is patient information on the Internet valid? Eur J Orthod 2012; 34: 466-469.
9 Swan A. Policy guidelines for the development and promotion of open access. Paris: UNESCO, 2012. https:// unesdoc.unesco.org/ark:/48223/pf0000215863 (viewed Mar 2025).
10 Doğramacı EJ, Rossi-Fedele G. Predictors of societal and professional impact of orthodontic research. A multivariate, scientometric approach. Scientometrics 2021; 126: 9223-9248.
11 Doğramacı EJ, Rossi-Fedele G. Predictors of societal and professional impact of Endodontology research: a multivariate, scientometric analysis. Int Endod J 2022; 55: 312-325.
12 Holmberg K, Bowman S, Bowman TD, et al. What is societal impact and where do Altmetrics fit into the equation? J Altmetrics 2019; 2: 6.
13 LSE Public Policy Group. Maximizing the impacts of your research: a handbook for social scientists. London: London School of Economics and Political Science, 2011. https:// eprints.lse.ac.uk/35758/1/Handbook_PDF_for_the_LSE_ impact_blog_April_2011.pdf (viewed Feb 2024).
14 Pritchard A. Documentation notes: statistical bibliography or bibliometrics. J Documentation 1969; 24: 348-349.
15 Aslam-Pervez N, Lubek JE. Most cited publications in oral and maxillofacial surgery: a bibliometric analysis. Oral Maxillofac Surg 2018; 22: 25-37.
16 Alkhutari AS, Al-Moraissi EA, Galvão EL, et al. Top 100 cited systematic reviews and meta-analyses in the major journals of oral and maxillofacial surgery: a bibliometric analysis. Oral Maxillofac Surg 2022; 26: 343-356.
17 Warren VT, Borrie KT, Kreger TC, et al. Factors associated with low and high article citations in the oral and maxillofacial surgery literature. J Oral Maxillofac Surg 2020; 78: 335-342.
18 Rekawek P, Gallagher B, Wu B, Karlis V. Oral and maxillofacial surgery journals’ presence on social media: an adaptation to enhance publication readership and interdisciplinary collaboration? J Oral Maxillofac Surg 2021; 79: 1991-1993.
19 Livas C, Delli K. Looking beyond traditional metrics in orthodontics: an Altmetric study on the most discussed articles on the web. Eur J Orthod 2018; 40: 193-199.
20 Leydesdorff L, Milojević S. Scientometrics. In: Wright JW, editor. International encyclopedia of the social and
behavioral sciences, 2nd ed. Amsterdam: Elsevier, 2015; pp 322-327.
21 Altmetric. How is the Altmetric Attention Score calculated? [updated 3 Dec 2024]. https://help.altmetric.com/support/ solutions/articles/6000233311-how-is-the-altmetricattention-score-calculated- (viewed Mar 2025).
22 McCullough R. Scopus filters for OA type and Green OA full-text access option [submitted 13 Jan 2022]. https:// blog.scopus.com/posts/scopus-filters-for-open-accesstype-and-green-oa-full-text-access-option (viewed Mar 2025).
23 Doğramacı EJ, Brennan DS. The influence of orthodontic treatment on dental caries: an Australian cohort study. Community Dent Oral Epidemiol 2019; 47: 210-216.
24 Agirnasligil MO, Gul Amuk N, Kilic E, et al. The changes of self-esteem, sensitivity to criticism, and social appearance anxiety in orthognathic surgery patients: a controlled study. Am J Orthod Dentofacial Orthop 2019; 155: 482489.
25 Frid P, Resnick C, Abramowicz S, et al. Surgical correction of dentofacial deformities in juvenile idiopathic arthritis: a systematic literature review. Int J Oral Maxillofac Surg 2019; 48: 1032-1042.
26 Lorente C, Hernández-Alfaro F, Perez-Vela M, et al. Surgical-orthodontic approach for facial rejuvenation based on a reverse facelift. Prog Orthod 2019; 20: 34.
27 Resnick CM, Frid P, Norholt SE, et al. An algorithm for management of dentofacial deformity resulting from juvenile idiopathic arthritis: results of a multinational consensus conference. J Oral Maxillofac Surg 2019; 77: 1152.e1-1152.e33.
28 Boyd SB, Chigurupati R, Cillo JE Jr, et al. Maxillomandibular advancement improves multiple health-related and functional outcomes in patients with obstructive sleep apnea: a multicenter study. J Oral Maxillofac Surg 2019; 77: 352-370.
29 Posnick JC, Kinard BE. Orthognathic surgery has a significant positive effect on perceived personality traits and perceived emotional facial expressions in subjects with primary maxillary deficiency. Plast Reconstr Surg Glob Open 2019; 7: e2198.
30 Ho CT, Lin HH, Lo LJ. Intraoral scanning and setting up the digital final occlusion in three-dimensional planning of orthognathic surgery: its comparison with the dental model approach. Plast Reconstr Surg 2019; 143: 1027e-1036e.
31 Yi J, Lu W, Xiao J, et al. Effect of conventional combined orthodontic-surgical treatment on oral health-related quality of life: a systematic review and meta-analysis. Am J Orthod Dentofacial Orthop 2019; 156: 29-43.
32 Badiali G, Marcelli E, Bortolani B, et al. An average threedimensional virtual human skull for a template-assisted maxillofacial surgery. Int J Artif Organs 2019; 42: 566-574.
33 Bouletreau P, Makaremi M, Ibrahim B, et al. Artificial Intelligence: applications in orthognathic surgery. J Stomatol Oral Maxillofac Surg 2019; 120: 347-354.
34 Giralt-Hernando M, Valls-Ontañón A, Guijarro-Martínez R, et al. Impact of surgical maxillomandibular advancement upon pharyngeal airway volume and the apnoeahypopnoea index in the treatment of obstructive sleep apnoea: systematic review and meta-analysis. BMJ Open Respir Res 2019; 6: e000402.
35 Harrison CJ, Rae C, Tsangaris E, et al. Further construct validation of the CLEFT-Q: ability to detect differences in outcome for four cleft-specific surgeries. J Plast Reconstr Aesthet Surg 2019; 72: 2049-2055.
36 Marechal G, Schouman T, Mauprivez C, et al. Gnathodiaphyseal dysplasia with a novel R597I mutation of ANO5: Mandibular reconstruction strategies. J Stomatol Oral Maxillofac Surg 2019; 120: 428-431.
37 Vijayakumar Jain S, Muthusekhar MR, Baig MF, et al. Evaluation of three-dimensional changes in pharyngeal airway following isolated lefort one osteotomy for the correction of vertical maxillary excess: a prospective study. J Maxillofac Oral Surg 2019; 18: 139-146.
38 Narin P. Evaluative Bibliometrics: the use of publication and citation analysis in the evaluation of scientific activity. Cherry Hill (NJ): Computer Horizons, 1976.
39 Potter WG. Introduction to library trends 30 (1) summer 1981: bibliometrics. Champaign (IL): Board of Trustees University of Illinois, 1981. https://www.ideals.illinois.edu/ items/7138 (viewed Mar 2025).
40 Young H, editor. The ALA glossary of library and information science. Chicago (IL): American Library Association, 1983; p 22. https://archive.org/details/ alaglossaryoflib00youn/page/n3/mode/2up (viewed Mar 2025)
41 Sengupta IN. Bibliometrics, informetrics, scientometrics and librametrics: an overview. Libri 1992; 42: 75-98.
42 Didegah F, Bowman TD, Holmberg K. Increasing our understanding of Altmetrics: identifying factors that are driving both citation and Altmetric counts. iConference 2016, Philadelphia (US); 20–23 March. https://core.ac.uk/ download/pdf/158312502.pdf (viewed Mar 2025).
43 Warren VT, Patel B, Boyd CJ. Determining the relationship between Altmetric Score and literature citations in the oral and maxillofacial surgery literature. J Oral Maxillofac Surg 2020; 78: 1460.e1-1460.e7.
44 Warren VT, Patel B, Boyd CJ. Analyzing the relationship between Altmetric score and literature citations in the implantology literature. Clin Implant Dent Relat Res 2020; 22: 54-58.
45 Adobes Martin M, Zhou Wu A, Marques Martínez L, et al. What is trending in paediatric dentistry? An Altmetric study on paediatric dentistry journals. Eur Arch Paediatr Dent 2021; 22: 291-299.
46 Meng Z, Xiang Q, Wu X, et al. The level of evidence, scientific impact and social impact of clinical studies in periodontology: a methodological study. J Clin Periodontol 2020; 47: 902-911.
47 Di Bitetti MS, Ferreras JA. Publish (in English) or perish: the effect on citation rate of using languages other than English in scientific publications. Ambio 2017; 46: 121127.
48 Kamadjeu R. English: the lingua franca of scientific research. Lancet Glob Health 2019; 7: e1174.
49 Arifi Q. The understanding of English as lingua franca and its involvement in language education policies in Europe. Thesis 2017; 6: 127-138.
50 Al-Hassani STS, editor. Chapter 3 – House of wisdom. In: Al-Hassani STS, editor. 1001 inventions: the enduring legacy of Muslim civilization, 3rd ed. Washington (DC): National Geographic Society, 2012; pp 62-107.
51 Babbel. The most spoken languages in the world, 2025. https://www.babbel.com/en/magazine/the-10-mostspoken-languages-in-the-world (viewed Mar 2025).
52 Amano T, González-Varo J, Sutherland WJ. Languages are still a major barrier to global science. PLoS Biol 2016; 14: e2000933.
53 Pieper D, Puljak L. Language restrictions in systematic reviews should not be imposed in the search strategy but in the eligibility criteria if necessary. J Clin Epidemiol 2021; 132: 146-147.
54 Arraj GP, Rossi-Fedele G, Doğramacı EJ. The association of overjet size and traumatic dental injuries — a systematic review and meta-analysis. Dent Traumatol 2019; 35: 217-232.
55 Orduna-Malea E, Delgado López-Cózar E. Demography of Altmetrics under the light of dimensions: locations, institutions, journals, disciplines and funding bodies in the global research framework. J Altmetrics 2019; 2: 3.
Dreyer DC (BDS, BScDent(Hons))1; Jensen ED (BDS, BScDent(Hons), DClinDent(Paed))1,2; Liau I (MBBS, BDS, BScDent(Hons), MPhil, FRACDS(OMS))3; Cheng A (MBBS, BDS, FRACDS(OMS))2; Sambrook P (MBBS, MDS, FRACDS(OMS))1,2
Orthognathic surgery, a discipline dating back to the 1840s, addresses maxillomandibular disharmonies and enhances both aesthetic appearance and function.1 This surgical field has had substantial advancements from its inception, particularly following the contributions of Hugo Obwegeser, who introduced techniques such as the bilateral sagittal split and Le Fort I osteotomy, which remain integral to contemporary orthognathic surgery.2 In recent years, advancements in the accuracy of computed tomography (CT) and cone beam computed tomography (CBCT) have spurred a shift towards three-dimensional (3D) virtual surgical planning (VSP).3 The widespread use of VSP has led to evidence supporting its accuracy in orthognathic surgery planning and execution.4
The adoption of VSP has revealed a plethora of advantages. Notably, Swennen and colleagues underscored the potential of VSP planning in assessing treatment outcomes through voxel-based rigid registration and superimposition techniques.3 Additionally, VSP serves as a communication tool among specialists, technicians and patients, with applications in education.3 VSP offers benefits such as enhanced accuracy in condylar positioning through splint construction using computer-aided design and computer-aided manufacturing (CAD and CAM), improved diagnosis and quantification of facial asymmetry, and potentially increased cost-effectiveness.5
Building on prior work by Gateno and colleagues, Swennen and colleagues introduced a novel clinical protocol that eliminated the need for traditional study models and instead relied on a triple CBCT approach with voxel-based rigid registration.6,7 This protocol involves capturing a CBCT scan with the individual in an upright position, occluding on a wax bite registration obtained during clinical assessment. A subsequent low dose CBCT scan is acquired with an impression tray precisely positioned in the individual’s mouth. Finally, the impression is scanned using a high resolution CBCT protocol. These datasets are then semi-automatically aligned using a procrustean method that maximises mutual information, resulting in the creation of an accurate virtual skull model. While this approach
Purpose: This study aimed to validate a simplified protocol for virtual surgical planning in orthognathic surgery.
Methods: Consecutive orthognathic surgeries performed by a single surgeon between January 2018 and December 2019 were planned using a single computed tomography image without a bite splint. The orthognathic plan was produced in collaboration between the surgeon and engineer. The outcome was assessed by comparison of the pre- and post-operative computed tomography scans by an independent assessor.
Results: Seventeen surgeries were assessed. It was found that the method was clinically accurate within 2 mm of all maxillary and most mandibular measurements. The greatest variation was with mandibular measurements distant from the midline and if a genioplasty was performed.
Conclusion: This study shows that this simplified technique was time efficient and clinically accurate.
demonstrated stability and precision, it presented drawbacks, including the need for two CBCT scans of the patient, thereby increasing radiation exposure. Additionally, the process was relatively complex and time consuming, relying on precise patient positioning with the wax bite wafer to avoid errors in subsequent planning stages.
Various protocols, such as 3D CT/CBCT imaging combined with CAD/ CAM technologies, intraoral scanning, and fully digital workflows, provide unique advantages and challenges (Table 1). Traditional preoperative data collection and imaging techniques demand specialised equipment and splints, in addition to pre-operative laboratory time, costs, and overall planning complexity. A promising approach
1Adelaide Dental School, The University of Adelaide, Adelaide, SA, Australia; 2Oral and Maxillofacial Surgery Unit, Royal Adelaide Hospital, Adelaide, SA, Australia; 3Oral and Maxillofacial Surgery Unit, Royal Children’s Hospital, Melbourne, VIC, Australia. Corresponding author: Andrew Cheng ✉ ahacheng@hotmail.com | doi: 10.63717/2025.MS0030
Keywords: orthognathic surgery | virtual surgical planning
Type of protocol Description
3D CT/CBCT imaging and CAD/CAM technology
3D printed splints 8-11
Obtain 3D imaging (CT/CBCT).
Perform virtual osteotomies using software.
Design and 3D print surgical splints or guides.
3D printed plates 12,13 Obtain 3D imaging (CT/CBCT).
Perform virtual osteotomies using software.
Design and 3D print surgical guides and patient specific implants
Protocols using intraoral scanning combined with CBCT
Intraoral scanning for virtual model surger 11
Combine intraoral scans with CBCT images to create a detailed virtual model.
Perform virtual osteotomies and design surgical splints based on this model.
Protocols integrating virtual planning with navigation systems
VSP with intraoperative navigation 14,15
Plan surgery virtually and use intraoperative navigation to guide the execution of the plan.
Protocols based on standardised software platforms
Software platforms (eg, Dolphin Imaging [Dolphin Imaging & Management Solutions, USA], ProPlan CMF [Materialise, Germany]) 3
Fully digital workflow protocols
Use of standardised software for planning and simulating surgery, often with integrated tools for creating splints or guides.
Digital-only workflow 16,17 Entire workflow from imaging, planning, to surgical guide creation is done digitally.
No physical models or splints are created until surgery.
Hybrid protocols combining traditional and digital methods
Hybrid approach with model surgery 18
Digital planning is done, but traditional model surgery is also performed to verify and adjust the plan.
Advantages
High accuracy in planning and transferring the plan to surgery.
Ability to simulate and evaluate different surgical scenarios pre-operatively.
Direct application during surgery without needing splints.
Greater precision in ensuring planned movements are executed.
High accuracy in capturing dental details.
Minimises the radiation exposure compared with full CBCT-based protocols.
Increases intraoperative precision.
Allows real-time adjustments and verification of surgical steps.
Standardisation ensures reproducibility and consistency across cases.
Often includes built-in tools for analysis and simulation.
Streamlined and efficient process.
Reduces physical storage needs and allows easy modifications.
Combines the accuracy of digital planning with the tactile feedback of traditional model surgery.
Provides a safety net if digital planning has discrepancies.
Disadvantages
Expensive and requires specialised equipment.
Additional steps in the workflow, which may prolong the pre-surgical preparation phase.
High cost, especially with custom plates.
May not be adaptable during surgery if intraoperative adjustments are necessary.
Fusion of intraoral scans with CBCT can be technically challenging.
Requires expertise in handling and merging different datasets.
Requires expensive and complex equipment.
Steep learning curve for the surgical team.
May be less flexible in handling unique or complex cases.
Dependency on the software’s limitations and updates.
Requires high proficiency in digital tools.
Potential for issues with digital file compatibility between different systems or devices.
Longer preparation time.
Requires maintaining proficiency in both traditional and digital methods.
3D = three-dimensional; CT = computed tomography; CBCT = cone beam computed tomography; CAD/CAM = computer-aided design/computer-aided manufacturing; CMF = craniomaxillofacial surgery; VSP = virtual surgical planning.
Table 1. Published orthognathic surgery protocols for virtual surgical planning
is the incorporation of segmentation of CT imaging to include digitised scanned occlusion, which merges the benefits of accurate anatomical visualisation with precise occlusal alignment, offering a comprehensive solution that could improve both surgical outcomes and patient satisfaction.
Hence, the aim of this study was to validate a simplified protocol for VSP in orthognathic surgery. This protocol was used in clinical practice and uses the 3D models for movement in each of the anatomical markers that were previously used in traditional orthognathic surgery planning.
This retrospective observational study received approval from the institutional ethics committee at the University of Adelaide (H-2017-127). Individuals were recruited consecutively following routine orthognathic surgery by a single surgeon at a private oral and maxillofacial surgery practice, between January 2018 and December 2019. All individuals provided written informed consent. Exclusion criteria were craniofacial syndromes and patients with specific implants and guides.
Treatment planning protocol was the same for all individuals and included examination, impressions for study models and a clinical bite record using wax and captured in centric relation (CR, the condyle was in the most superior and posterior position in the glenoid fossa). The clinical bite records and study models were subsequently digitised. A pre-operative medical-grade helical CT image was captured with the individual in a supine position with their lips closed, ensuring gentle occlusion in centric occlusion (CO, the position of maximum intercuspation of the dentition) without a bite registration splint. The CT protocol was derived from KLS Martin Group (KLS Martin Group, Germany) including special resolution of 0.5–1.25 mm and gantry tilt of 0°. A virtual skull model was created for each individual by a clinical engineer using Materialise Magics three-dimensional printing software (Materialise, Belgium). This process involved two steps with collaboration between the clinical engineer and the surgeon pivotal in forming the surgical plan, a dynamic process tailored to each patient’s unique requirements, outlined in Figure 1

In all cases that involved the maxilla, a Le Fort I osteotomy was conducted. In cases that involved the mandible, a bilateral sagittal split osteotomy was performed. Standard fixation miniplates and screws were used in all cases. If both mandible and maxilla movements were required, then the Le Fort I osteotomy was completed and fixated with miniplates before the mandibular movements.
A post-operative CT scan was captured within eight days of surgery using the same scanning protocol as the preoperative CT scan. Both scan results were imported into the Materialise Magics program.
To assess the hard tissue accuracy of the surgical procedure, the pre-operative plan and post-operative CT scan were aligned and overlaid by digitising stable surface structures, including the zygomatic buttresses, nasion, foramen magnum, infraorbital foramen, superior orbital notch, mastoid process and external occipital protuberance (Figure 2). Additionally, cephalometric landmarks were digitised on the pre-operative plan and post-operative skull models. Maxillary landmarks included point A, anterior nasal spine (ANS), posterior nasal spine (PNS), maxillary incisive midline, and left and right first maxillary molars. Landmarks on the mandible included point B, pogonion (Pog), left and right gonion (GoL and GoR), left and right condylion (CoL and CoR), mandibular incisive midline, and left and right first mandibular molars. In-depth 3D linear measurements and measurements along each individual axis (x, y and z) were recorded between the hard tissue landmarks in the pre-operative plan and post-operative skull model.
Independent sample t-tests were carried out to assess whether there were statistically significant differences in the outcomes between single-jaw and bimaxillary surgeries. A 2-mm threshold of variability was adopted, aligning with previous research that has established this level of variation as clinically significant.19,20 All statistical analyses were carried out using R Core Team21 and the R package Companion to Applied Regression (CAR).22
To assess potential variation, Levene’s test for homogeneity of variance was employed in the following contexts:
within the same jaw (either maxilla or mandible) for the same surgery type (single-jaw or bimaxillary);
between the maxilla and mandible separately for single-jaw and bimaxillary surgeries;
between single-jaw and bimaxillary surgeries, considered separately for both the maxilla and mandible; and
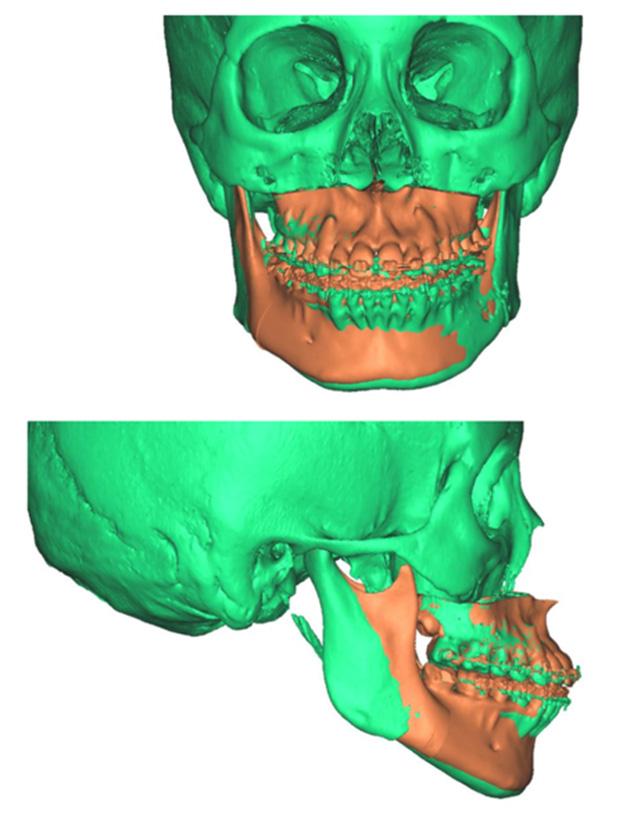

2. Superimposed digital reconstruction skull images from Materialise Magics with the planned final outcome in orange and the post-operative scan data in green
across the three axes (x, y and z) in each of the surgery combinations for jaw-by-surgery type comparison.
Seventeen individuals (12 females, age range between 18 and 61 years) satisfied the inclusion criteria. The number of patients in each surgery type (maxillary, mandibular, bimaxillary) is presented in Figure 3
The disparities between the anticipated positions of selected landmarks and their actual post-operative locations in both singlejaw and bimaxillary surgeries are summarised in Table 2
For the maxillary surgeries, the mean combined difference between anticipated movements and final position along the x, y and z axes was compared between single-jaw (1.33 ± 1.12 mm) and bimaxillary surgeries (1.33 ± 1.30 mm), as seen in Figure 4. An independent samples t-test revealed no statistically significant difference between single-jaw and bimaxillary surgeries (t(210) = 0.01; P = 0.992). The mean combined difference between anticipated movements and final position along the x, y and z axes in the mandible for single-jaw (1.00 ± 1.20 mm) and bimaxillary surgeries (1.75 ± 1.47 mm) was calculated (Figure 5). An independent samples t-test indicated a significant difference (t(257) = 4.91; P < 0.001; d = 0.54).
Three-dimensional linear measurements ranged between a mean of 0.86 mm for the lower right mandibular molar in single-jaw surgery
and 5.75 mm for the pogonion in bimaxillary surgery. Levene’s test did not reveal any statistically significant difference among the variances of the maxillary landmarks in either single-jaw or bimaxillary surgeries (single jaw: F(5, 84) = 0.53, P = 0.752; bimaxillary: F(5, 138) = 0.37, P = 0.871). However, a significant difference was noted between mandibular landmarks in both single-jaw and bimaxillary surgeries (single jaw: F(8, 88) = 4.85, P < 0.001; bimaxillary: F(8, 207) = 2.96, P = 0.004). A significant difference in variance occurred between single-jaw and bimaxillary surgeries in the mandible (F(1, 322) = 7.93; P = 0.005), but not in the maxilla (F(1, 232) = < 0.001; P = 0.996) and not between the maxilla and mandible in single-jaw operations (F(1, 196) = 2.57; P = 0.110) or bimaxillary operations (F(1, 358) = 1.51; P = 0.220). There was a heterogeneic variance among the x, y and z axes in the maxilla in both single and bimaxillary surgeries (single jaw: F(2, 87) = 6.50, P = 0.002; bimaxillary: F(2, 141) = 6.28, P = 0.002), but not in the mandible (single jaw: F(2, 105) = 0.13, P = 0.883; bimaxillary: F(2, 213) = 0.32, P = 0.729).
This article shows that this simplified method of VSP assessment results in a clinically accurate assessment for orthognathic surgery. The accuracy from the planning protocol is derived from segmentation of the CT imaging to incorporate digitised scanned occlusion. Deviations from this position could pose challenges for clinical engineers in determining the correct condylar position, leading to a notable variance between the planned and actual outcome for CoR
and CoL points. Accurate data collection before formulating the surgical plan, including the capture of impressions and centric relation clinically is crucial, as any errors in this phase would propagate through the planning process. This simplified protocol not only achieves clinically acceptable outcomes but also improves surgical and pre-operative efficiency by reducing technique sensitivity, requiring only one consultation appointment, eliminating the need for guide splints, and streamlining the process with a single preoperative radiographic scan.
Most mean landmark variances, except for three, and all median values except one, remained below the 2-mm threshold recognised as clinically significant.19 The findings of this study demonstrate favourable outcomes in the maxilla, both for singlejaw and bimaxillary surgeries, with greater accuracy of maxillary landmark positions (mean, 1.09–1.51 mm). Therefore the maxillary position on the CT scan is not influenced by the position of the condylar seating at the time of the scan. In contrast, the mandibular movements had greater variations in the accuracy of landmark positioning. Landmarks anterior to the osteotomy in the proximal segment of single-jaw surgery (B, mandibular mid-incisor point [Md], Pog) exhibited minimal variance between their planned and actual postoperative positions (mean, 0.43–0.61 mm). However, the points in the distal segment (CoL, CoR, GoL, GoR, lower left first molar [LLM], lower right first molar [LRM]) had larger discrepancies (mean, 1.21–2.34 mm). Notably, GoL exceeded the 2-mm threshold for clinical acceptability.19 This may be explained by intraoperative seating of the condyle being potentially varied from the predicted seating of VSP; influenced by soft tissues within the temporomandibular joint, perimandibular musculature, alignment of the lower border of the mandible and control of torsional movements of the proximal segment.
During bimaxillary surgery, the mandible exhibited the highest degree of variance, particularly at Pog (2.89 mm) and GoL (2.19 mm) and GoR (1.62 mm). This is expected due to the compounded nature of any discrepancy from the initial maxillary movement and fixation position before mandibular movement. Previous studies
Parameter Difference
Single jaw (maxilla)
Bimaxillary (maxilla)
Landmark
Single jaw (mandible)
Landmark B
Bimaxillary (mandible)
Landmark
A = A point; ANS = anterior nasal spine; B = B point; CoL = left condylion; CoR = right condylion; GoL = left gonion; GoR = right gonion; LLM = lower left first molar; LRM = lower right first molar; Md = mandibular mid-incisor point; Mx = maxillary mid-incisor point; PNS = posterior nasal spine; Pog = pogonion; SD = standard deviation; ULM = upper left first molar; URM = upper right first molar.
Table 2. The mean and median difference between planned and postoperative outcome for the x, y and z axes combined

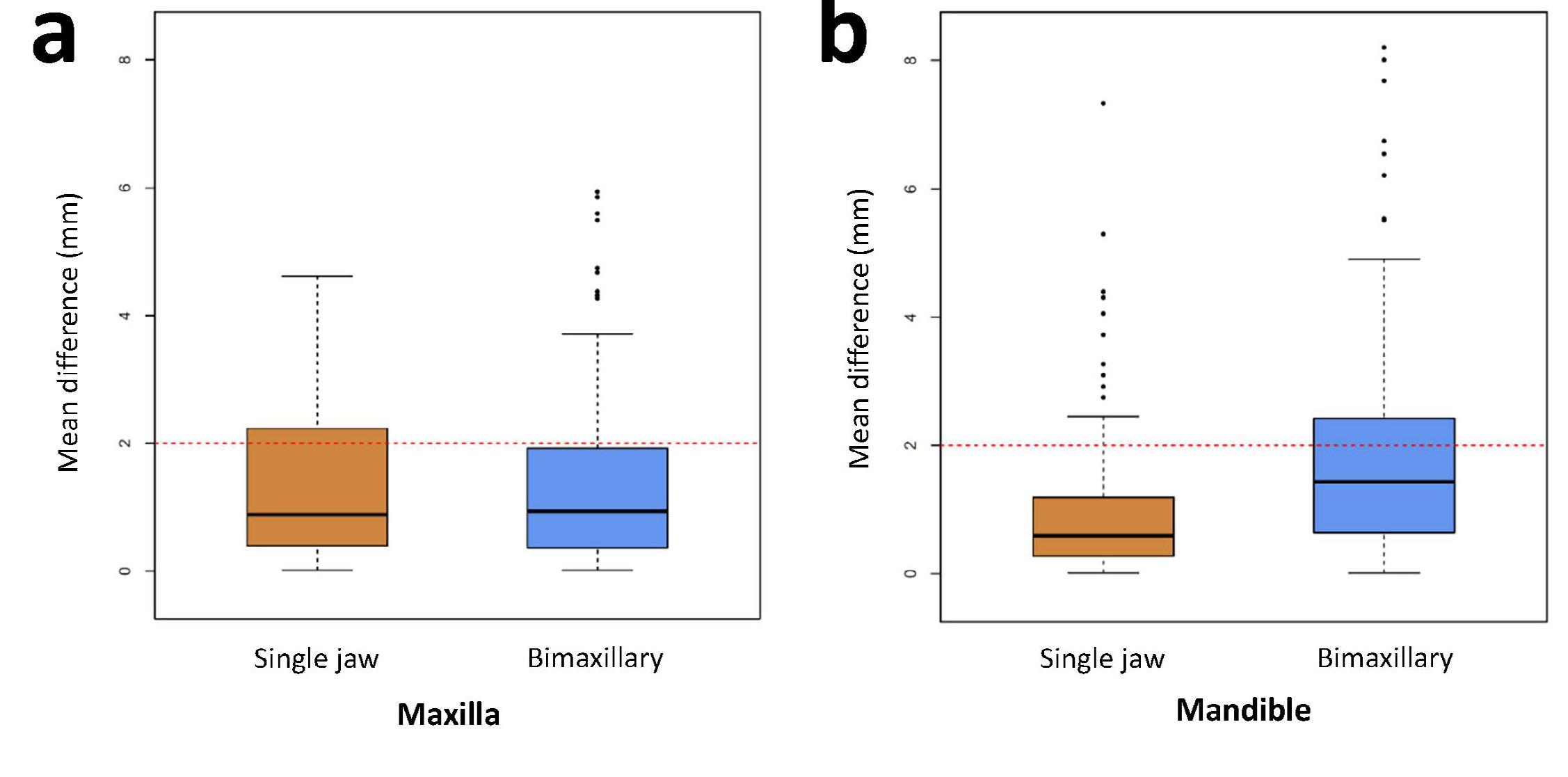
Figure 4. The combined mean difference between anticipated and final movements between single-jaw and bimaxillary surgery with a 2 mm line indicating the threshold for a clinically significant difference in outcome for a) maxilla and b) mandible
assessing the accuracy of VSP did not typically include points distant from the midline, such as Go or Co, likely due to the inclusion of genioplasty in these cases, which would not have translated from VSP to final position when patient-specific cutting guides and implants are not used.9,23,24 However, these findings are consistent with a study that found variances in chin landmarks above the 2 mm clinical threshold and suggested the use of chin templates for enhanced accuracy.23 Additionally, the mandibular variance was more pronounced on the left-hand side, which could be related to the dominant hand of the surgeon or the side of fixation of the mandible. This study also reviewed movements in a mediolateral direction, which were not typically detectable using traditional lateral cephalometric analysis methods. The Levene’s test of homogeneity indicated that mediolateral movement was comparatively lower than movement along the y and z axes for the maxilla in both single-jaw and bimaxillary surgery. This may be attributed to clinicians’ ability to visually identify the facial midline and deviations more effectively than assessing anteroposterior or superior-inferior directions. Nevertheless, there are no established thresholds of clinical significance for measuring linear variances accurately in 3D.
Although this simplified method is not novel, it provides an efficient protocol to transition from the traditional orthognathic surgery model to VSP. The use of intraoral scanners for occlusion measurements has become commonplace, but not all surgical consulting practices have the facilities or staff to adopt this technology. Accuracy of the surgery can be measured using pre- and post-operative CT (or CBCT) scans. The limitations of measuring surgical accuracy using digital scans of the teeth are that the occlusion may be maintained by the fixed orthodontic appliance; therefore, little difference between the occlusal markers will be highlighted by the scan. A range of other protocols have been published, including in-house VSP without the use of engineers, using common orthodontic software for the VSP.25,26 Each
technique brings a varied angle to how to improve efficiency, accuracy and cost. The simplified protocol in this study is similar to that described previously, but with the advantage of being reproducible and efficient for surgeons transitioning from traditional surgical planning to VSP without the need for costly equipment or hardware.27
Several limitations warrant consideration in interpreting the findings of this study. While accuracy in measuring cephalometric landmarks using CT images has been shown to be highly reliable, potential limitations in accuracy measurement may arise from how clinical engineers identified and located these points and the exclusion of dental landmarks (such as overjet, overbite or dental midline position) from the CT cephalometric analysis, which are good indicators of post-operative occlusal accuracy.28 Variability in pinpointing landmark positions, their replicability in predicted versus biologically possible outcomes and other clinical variables such as positioning of the osteotomised segments intraoperatively could contribute to discrepancies in accuracy assessment. The results of orthognathic surgery, even with the use of VSP, are influenced by the clinical judgement of the treating surgeon, including for such positioning nuances as incisal display and vertical seating of the maxillomandibular complex. Other factors may affect condylar positioning on the post-operative CT scan in CO, including postoperative CO or CR shifts, the influence of guiding elastics and the timing of the post-operative CT with potential iatrogenic condylar oedema of the soft tissues. Another limitation lies in the relatively small sample size. While the study yielded meaningful data, the limited number of cases may impact the generalisability of the results to a broader population. A larger sample size and comparison to a control group (comparator being the triple scan protocol) would enhance the robustness of the findings. Careful consideration of these limitations is essential when interpreting the results and their broader applicability in clinical practice.
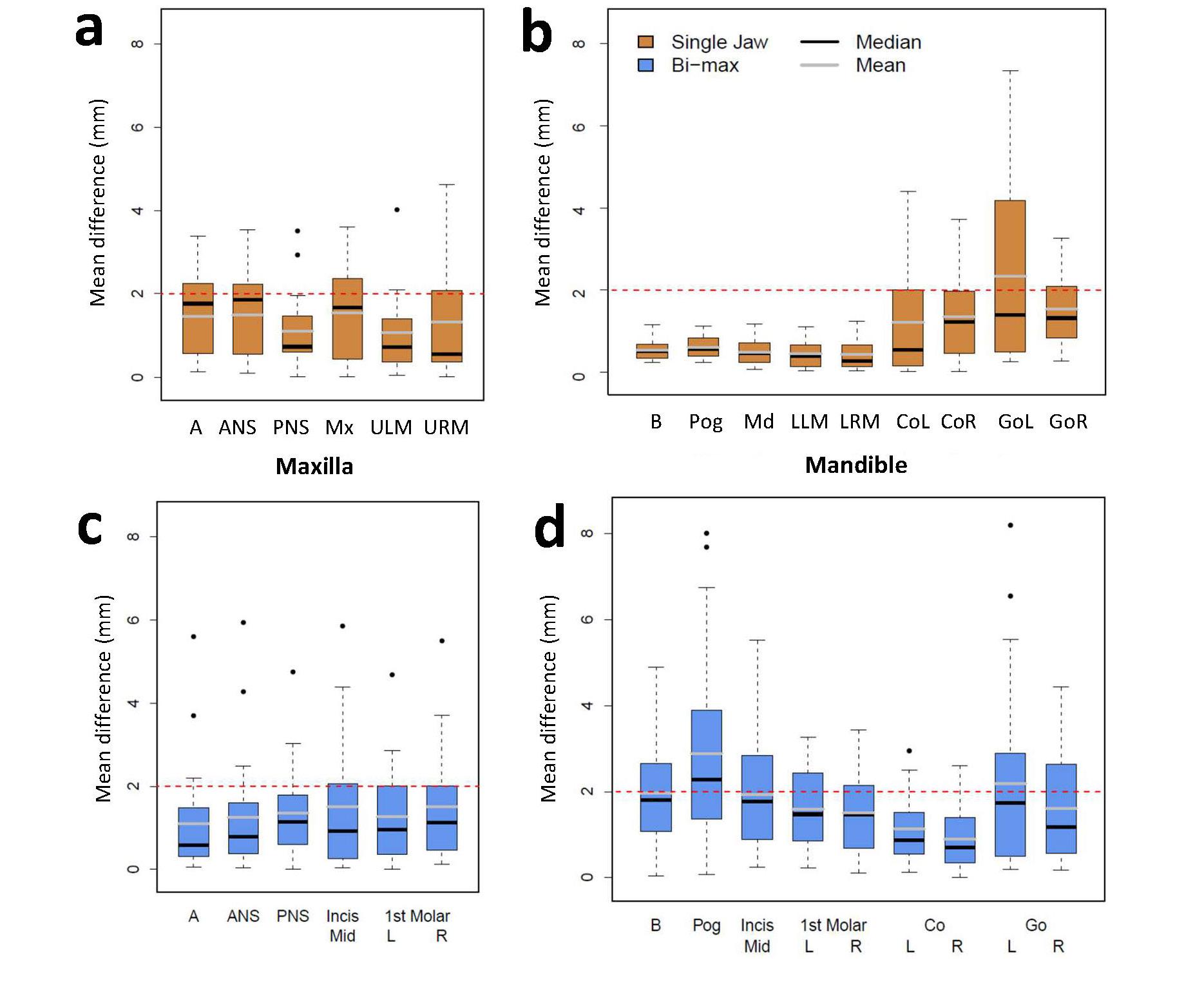
This study introduced a protocol that reduced technique sensitivity, required only one consultation appointment, decreased laboratory time (as guide splints for orientation during radiographic imaging are unnecessary), and streamlined the pre-operative process by requiring a single radiographic scan per patient. During bimaxillary surgery, the mandible exhibited significant variance while mediolateral movements, not typically detectable via plain film assessment, showed lower variance compared with y and z axes in the maxilla. A clinically significant threshold for 3D linear measurements is required to interpret the clinical relevance of these findings.
Dreyer DC: Collected the data and drafted the manuscript, reviewed and approved the final manuscript.
Liau I: Collected the data and drafted the manuscript, reviewed and approved the final manuscript.
Jensen ED: Analysed the data and wrote the manuscript, reviewed and approved the final manuscript.
Cheng A: Conceptualised the project and provided supervision, treating surgeon, reviewed and approved the final manuscript.
Sambrook P: Conceptualised the project and provided supervision, reviewed and approved the final manuscript.
The authors declare that they have no conflicts of interest.
1 Aziz SR. Simon P. Hullihen and the origin of orthognathic surgery. J Oral Maxillofac Surg 2004; 62: 1303-1307.
2 Steinhäuser E. Historical development of orthognathic surgery. J Craniomaxillofac Surg 1996; 24: 195-204.
3 Swennen GR, Mollemans W, Schutyser F. Threedimensional treatment planning of orthognathic surgery in the era of virtual imaging. J Oral Maxillofac Surg 2009; 67: 2080-2092.
4 Alkhayer A, Piffkó J, Lippold C, Segatto E. Accuracy of virtual planning in orthognathic surgery: a systematic review. Head Face Med 2020; 16: 34.
5 Xia JJ, Phillips CV, Gateno J, et al. Cost-effectiveness analysis for computer-aided surgical simulation in complex cranio-maxillofacial surgery. J Oral Maxillofac Surg 2006; 64: 1780-1784.
6 Gateno J, Xia J, Teichgraeber JF, Rosen A. A new technique for the creation of a computerized composite skull model. J Oral Maxillofac Surg 2003; 61: 222-227.
7 Swennen GR, Mollemans W, De Clercq C, et al. A conebeam computed tomography triple scan procedure to obtain a three-dimensional augmented virtual skull model appropriate for orthognathic surgery planning. J Craniofac Surg 2009; 20: 297-307.
8 Xia JJ, Gateno J, Teichgraeber JF. New clinical protocol to evaluate craniomaxillofacial deformity and plan surgical correction. J Oral Maxillofac Surg 2009; 67: 2093-2106.
9 Gateno J, Xia JJ, Teichgraeber JF, et al. Clinical feasibility of computer-aided surgical simulation (CASS) in the treatment of complex cranio-maxillofacial deformities. J Oral Maxillofac Surg 2007; 65: 728-734.
10 Metzger MC, Hohlweg-Majert B, Schön R, et al. Verification of clinical precision after computer-aided reconstruction in craniomaxillofacial surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007; 104: e1-e10.
11 Zinser MJ, Mischkowski RA, Sailer HF, Zöller JE. Computer-assisted orthognathic surgery: feasibility study using multiple CAD/CAM surgical splints. Oral Surg Oral Med Oral Pathol Oral Radiol 2012; 113: 673-687.
12 Sharifi A, Jones R, Ayoub A, et al. How accurate is model planning for orthognathic surgery? Int J Oral Maxillofac Surg 2008; 37: 1089-1093.
13 De Riu G, Virdis PI, Meloni SM, et al. Accuracy of computer-assisted orthognathic surgery. J Craniomaxillofac Surg 2018; 46: 293-298.
14 Heufelder M, Wilde F, Pietzka S, et al. Clinical accuracy of waferless maxillary positioning using customized surgical guides and patient specific osteosynthesis in bimaxillary orthognathic surgery. J Craniomaxillofac Surg 2017; 45: 1578-1585.
15 Naujokat H, Rohnen M, Lichtenstein J, et al. Computerassisted orthognathic surgery: evaluation of mandible registration accuracy and report of the first clinical cases of navigated sagittal split ramus osteotomy. Int J Oral Maxillofac Surg 2017; 46: 1291-1297.
16 Hernández-Alfaro F, Guijarro-Martínez R, Peiró-Guijarro MA. Surgery first in orthognathic surgery: what have we learned? A comprehensive workflow based on 45 consecutive cases. J Oral Maxillofac Surg 2014; 72: 376-390.
17 Lee S-J, Yoo J-Y, Woo S-Y, et al. A complete digital workflow for planning, simulation, and evaluation in orthognathic surgery. J Clin Med 2021; 10: 4000.
18 Stokbro K, Aagaard E, Torkov P, et al. Virtual planning in orthognathic surgery. Int J Oral Maxillofac Surg 2014; 43: 957-965.
19 Donatsky O, Bjørn-Jørgensen J, Holmqvist-Larsen M, Hillerup S. Computerized cephalometric evaluation of orthognathic surgical precision and stability in relation to maxillary superior repositioning combined with
mandibular advancement or setback. J Oral Maxillofac Surg 1997; 55: 1071-1079.
20 Tng TT, Chan TC, Hägg U, Cooke MS. Validity of cephalometric landmarks. An experimental study on human skulls. Eur J Orthod 1994; 16: 110-120.
21 Dalgaard PR, R Development Core Team. R: A language and environment for statistical computing [computer program]. Vienna: R Foundation for Statistical Computing, 2010. http://www.R-project.org
22 Fox J, Weisberg S. An R companion to applied regression. 2nd ed. California: Sage Publications, 2011.
23 Hsu SS-P, Gateno J, Bell RB, et al. Accuracy of a computer-aided surgical simulation protocol for orthognathic surgery: a prospective multicenter study. J Oral Maxillofac Surg 2013; 71: 128-142.
24 Centenero SA-H, Hernández-Alfaro F. 3D planning in orthognathic surgery: CAD/CAM surgical splints and prediction of the soft and hard tissues results – our experience in 16 cases. J Craniomaxillofac Surg 2012; 40: 162-168.
25 Sharkh HA, Makhoul N. In-house surgeon-led virtual surgical planning for maxillofacial reconstruction. J Oral Maxillofac Surg 2020; 78: 651-660.
26 de Britto Teixeira AO, de Oliveira Almeida MA, da Cunha Almeida RC, et al. Three-dimensional accuracy of virtual planning in orthognathic surgery. Am J Orthod Dentofacial Orthop 2020; 158: 674-683.
27 Ritto F, Schmitt A, Pimentel T, et al. Comparison of the accuracy of maxillary position between conventional model surgery and virtual surgical planning. Int J Oral Maxillofac Surg 2018; 47: 160-166.
28 Gribel BF, Gribel MN, Frazão DC, et al. Accuracy and reliability of craniometric measurements on lateral cephalometry and 3D measurements on CBCT scans. Angle Orthod 2011; 81: 26-35.


Wang D (BDentTech, PGDipCDTech(Dist), BDS(Hons), MRACDS(PDS)); Smit R (BDS, MBChB, MRACDS(PDS), FRACDS(OMS)); Harrison J (BDS, MDS(OMFS), MBChB, FRACDS(OMS)); Sealey C (BDS, MBChB, FDSRCPS, FRACDS(OMS))
Condylar hyperplasia is a rare developmental malformation of the mandibular condyle, leading to significant facial asymmetry, occlusal disturbance, chin deviation and temporomandibular joint dysfunction. This idiopathic growth abnormality was first described by Adams in 1836.1 It typically affects patients between 10 and 30 years of age and shows a female predominance of 64%.2 Facial asymmetry affecting the lower third of the face is the most frequently reported reason for clinical presentation. It has been shown that chin deviation of 5 mm or less is not discernible by clinicians or patients.3 However, more extreme asymmetries have an exponentially compounding impact on perceptions of acceptability and desire for surgical intervention.4
Obwegeser and Makek classified condylar hyperplasia according to the vector of excessive growth:
Type I: hemimandibular elongation;
Type II: hemimandibular hyperplasia; and
Type III: combination of Type I and Type II.5
Type I is characterised by excessive growth in the horizontal vector with deviation of the chin and mandibular dental midline to the contralateral side. As a consequence, a contralateral crossbite is often observed with lingual tilting of the mandibular molars to compensate for the malocclusion. Type II condylar hyperplasia patients have abnormal growth in the vertical vector with downgrowth of the affected mandibular condyle and minimal deviation of the chin or occlusal midline. Initially, there may be an ipsilateral open bite but gradual compensatory supra-eruption of the maxillary dentoalveolar complex results in an occlusal cant. The inferior mandibular border is also bowed and thus the entire hemimandible appears enlarged in all three planes, extending from the condyle to the symphysis. Type III encapsulates the characteristics of both Type I and Type II.
The purpose of this case report is to highlight the presentation and review the pathophysiology and management of condylar hyperplasia. Condylar hyperplasia is a rare, non-neoplastic condition that can result in progressive facial asymmetry with significant functional and aesthetic deficits. Although recommendations have been proposed for the management of this debilitating condition, there remains no consensus within the surgical literature. Diagnosis and treatment planning require appropriate investigations to establish the presence or absence of active growth, which in turn modifies the multidisciplinary management. This case report outlines the management of a young, female patient presenting with right-sided condylar hyperplasia with a marked malocclusion, temporomandibular joint dysfunction and significant facial asymmetry. Nuclear medicine imaging confirmed increased metabolic uptake of the right condyle, consistent with ongoing mandibular growth. A combination of orthodontic treatment with orthognathic surgery using virtual surgical planning, customised surgical cutting guides and fixation plates, enabled the provision of a stable and predictable outcome.
More recently, Wolford and colleagues introduced a classification system that includes the various pathological entities contributing to condylar hyperplasia. In this system, condylar hyperplasia is divided into four categories — Types I, II, III and IV — based on clinical, imaging, growth and histological characteristics.6 Types I and II are similar to the classification of Obwegeser and Makek, which describes excessive growth in the horizontal and vertical planes, respectively. However, Wolford and colleagues further divided the categories into:
Department of Oral and Maxillofacial Surgery, Auckland District Health Board, Auckland, New Zealand.
Corresponding author: Darren Wang ✉ darren.wangNZ@gmail.com | doi: 10.63717/2025.MS0029
Keywords: condylar hyperplasia | customised guides | orthognathic | SPECT | surgery

Figure 1. Extra-oral and intra-oral clinical photographs demonstrating mandibular asymmetry with severe right-sided posterior open bite
Type IA: bilateral mandibular elongation;
Type IB: unilateral mandibular elongation;
Type IIA: unilateral vertical mandibular overgrowth;
Type IIB: unilateral vertical mandibular overgrowth with horizontal exophytic condylar growth;
Type III: benign tumours including osteomas, neurofibromas, fibrous dysplasia, giant cell tumour, chondroma and chondroblastomas, manifesting with a unilateral facial enlargement; and
Type IV: malignant tumours including chondrosarcoma, osteosarcoma or metastatic lesions.6
Although non-tumorous condylar hyperplasia is usually self-limiting, an active growth centre means the asymmetry can continue progressing indefinitely. Diagnosis is dependent on an accurate clinical history, examination and appropriate investigations. A multidisciplinary approach can optimise treatment planning and address the associated functional and aesthetic issues. A case of condylar hyperplasia managed by surgical–orthodontic treatment is described.
A 21-year-old, healthy female patient was referred by her orthodontist to the Department of Oral and Maxillofacial Surgery, Auckland District Health Board, with complaints of progressive facial asymmetry, right-sided temporomandibular joint dysfunction and malocclusion. Extraoral clinical examination revealed a vertically elongated right mandible with a chin point that was markedly deviated to the contralateral side. Intraoral examination demonstrated a mandibular occlusal cant (down on the right) with an
associated right posterior open bite, tilting of the mandibular teeth to the right and coincident dental midlines (Figure 1).
Radiographic findings were consistent with the clinical presentation and showed enlargement and elongation of the right condylar head and neck, with bowing of the mandibular border and inferior displacement of the mandibular nerve canal. Single photon emission

Figure 2. Virtual surgical planning images used in the procedures to remove the active growth centre, correct the occlusion and mandibular cant by bilateral sagittal split osteotomy and correct facial asymmetry by extra-oral recontouring of the mandibular body using custom-designed hardware

Figure 3. Extra-oral and intra-oral post-debond photographs
computed tomography (SPECT) imaging demonstrated increased metabolic uptake throughout the mandibular condyle, in keeping with the working diagnosis of active condylar hyperplasia (Obwegeser and Makek Type III/Wolford and colleagues Type IIB).
Pre-surgical orthodontic treatment was followed by virtual surgical planning (VSP) (Figure 2) with a view to:
eliminate the active growth centre by proportional condylectomy; and
correct the malocclusion and mandibular asymmetry or cant by extra-oral recontouring of the right inferior border of mandible and bilateral sagittal split osteotomy (BSSO).
The abnormal right condyle was approached via a pre-auricular incision and a 6 mm proportional condylectomy was completed using a Piezotome (DePuy Synthes, USA). The articular disc was preserved and secured with two Mitek anchors (DePuy Mitek, USA) over the recontoured condylar head. The right body of the mandible was then approached via a submandibular incision, and the lower border was recontoured using a custom-made Synthes cutting guide. Care was taken to identify, skeletonise and protect the inferior alveolar nerve, which was at the level of the planned resection. The BSSO was then completed to correct the occlusion. Custom-made Synthes titanium patient-specific implants (PSI) were used for the dual purpose of correcting the horizontal mandibular deficiency (as onlays) and for fixating the osteotomy on the ipsilateral side. Stock Synthes plates were used on the contralateral side. Tooth 47 was also extracted, as per the VSP, to optimise the occlusion. Post-surgical orthodontic treatment was completed within six months of the procedure. Angle Class I incisor and molar relationships were achieved as planned (Figure 3). Rehabilitation of the right posterior mandibular edentulous
space with a dental implant and fixed prosthodontics is planned for the future.
Condylar hyperplasia is a complex non-neoplastic disorder causing excessive growth of the mandible. Despite being first recognised nearly two centuries ago, the aetiopathogenesis of this condition remains uncertain, with hormonal imbalances, hypervascularity, genetic predisposition, infection and trauma being postulated by various authors.5-8 Histology of the mandibular condyles demonstrates four layers: a fibrous articular layer, an undifferentiated mesenchymal layer, a transitional layer and a hypertrophic cartilaginous layer.9 Active hyperplastic condyles have been found to demonstrate a thicker hyperplastic cartilaginous and mesenchymal cell layer with pathognomonic cartilage “islands” when compared with a normal condyle.10-12 However, the clinical relevance of this has not been ascertained.
Insulin-like growth factor 1 (IGF-1) and its receptor (IGF-1R) have been implicated in the development of condylar hyperplasia. IGF-1 is an essential growth modulator and when added to normal cultured chondrocytes, was found to increase the rate of cell proliferation.10 Both the hormone and receptors appear to be upregulated in hyperplastic condyles. Furthermore, the addition of NVP-AEW541 (an inhibitor of IGF-1 receptor kinase) decreased proliferation of chondrocytes cultured from a hyperplastic condyle.10 These results suggest that IGF-1 has an impact on chondrogenesis of the mandibular condyle. However, a full understanding of the underlying mechanism of excessive condylar growth is yet to be determined.13
The surgical management of condylar hyperplasia usually involves a period of pre- and post-surgical orthodontics. Surgery may involve a combination of condylectomy, orthognathic surgery and bony recontouring. Guidelines in relation to the timing of treatment have been proposed. When active disease is established by SPECT, options include:
deferring surgery until growth ceases;
condylectomy and delayed orthognathic surgery; or combined condylectomy and orthognathic surgery.14
Waiting until growth ceases is likely to provide a more stable surgical outcome, but the duration of growth can be unpredictable and may result in worsening facial asymmetry, during an age range with high social and psychological implications. Pairing the condylectomy with orthognathic surgery, as in the case presented, appears to be reliable, with one group reporting a relapse rate of only 4%.15
Our position, in the presence of persistent active condylar growth, is that resection of the growth centre by condylectomy is essential to prevent relapse. A high condylectomy removes the superior 3–5 mm of the condyle containing the hyperplastic cartilage. A proportional condylectomy refers to complete removal of the hyperplastic cartilage and a proportion of bone to assist with orthognathic correction of the condylar or ramal height and mandibular asymmetry.14
Careful clinical, radiographic and nuclear medicine imaging is required to guide treatment planning. SPECT bone scanning indicates the relative stability or activity of the hyperplastic condyle. Increased condylar uptake of more than 10% in comparison to the contralateral side is indicative of active condylar hyperplasia.16,17
In the case presented, the initial decision was to defer surgery until growth was complete. However, due to the persistence of growth, a proportional condylectomy and concordant orthognathic correction was offered. VSP was fundamental to coordinating the condylectomy procedure with the orthognathic correction and recontouring, while preserving the inferior alveolar nerve. Furthermore, VSP facilitated
1 Neelakandan RS, Bhargava D. Bifid hyperplastic mandibular condyle. J Maxillofac Oral Surg 2013; 12: 466-471.
2 Raijmakers PG, Karssemakers LHE, Tuinzing DB. Female predominance and effect of gender on unilateral condylar hyperplasia: a review and meta-analysis. J Oral Maxillofac Surg 2012; 70: e72-76.
3 Naini FB, Donaldson AN, McDonald F, Cobourne MT. Assessing the influence of asymmetry affecting the mandible and chin point on perceived attractiveness in the orthognathic patient, clinician, and layperson. J Oral Maxillofac Surg 2012; 70: 192-206.
4 Fan B, Chen H, Sun YJ, et al. Clinical effects of 3-D printing-assisted personalized reconstructive surgery for blowout orbital fractures. Graefes Arch Clin Exp Ophthalmol 2017; 255: 2051-2057.
5 Obwegeser HL, Makek MS. Hemimandibular hyperplasia-hemimandibular elongation. J Maxillofac Surg 1986; 14: 183-208.
6 Wolford LM, Movahed R, Perez DE. A classification system for conditions causing condylar hyperplasia. J Oral Maxillofac Surg 2014; 72: 567-595.
the design of the titanium onlay, which addressed the mandibular asymmetry in the horizontal plane, and optimised the aesthetic outcome. The surgical planning was incorporated by means of patient-specific cutting guides and PSIs. This technology enabled the precise intra-operative reproduction of the pre-planned osteotomy cuts, reducing operating time, potential surgical complications, and the duration of the post-surgical orthodontic treatment.18
The timing of surgery to correct the effects of unilateral condylar hyperplasia is challenging and remains controversial. Early cessation of growth enables the orthodontic and surgical treatment to be completed, without interfering with the temporomandibular joint. The duration of the condylar growth, however, is unpredictable. If it is ongoing, the associated facial asymmetry and malocclusion typically become more pronounced and require a more complex corrective surgical procedure, as in the case presented.
Treatment decisions in unilateral condylar hyperplasia rely on establishing the presence or absence of active growth by means of serial clinical examination, serial imaging, SPECT, while incorporating the views and concerns of the patient. Although guidelines for the management of condylar hyperplasia have been proposed, treatment decisions remain contentious. Further work is required to improve the management of and treatment outcomes for this complex disorder.
Author contributions
Wang D: Drafted manuscript, submission for publication.
Smit R: Conception and critical review.
Harrison J: Critical review.
Sealey C: Critical review.
Patient consent
The patient provided written consent for publication.
Conflicts of interest
The authors declare that they have no conflicts of interest.
7 Slootweg PJ, Müller H. Condylar hyperplasia. A clinicopathological analysis of 22 cases. J Maxillofac Surg 1986; 14: 209-214.
8 Matteson SR, Proffit WR, Terry BC, et al. Bone scanning with 99mtechnetium phosphate to assess condylar hyperplasia. Report of two cases. Oral Surg Oral Med Oral Pathol 1985; 60: 356-367.
9 Hansson T, Öberg T, Carlsson GE, Kopp S. Thickness of the soft tissue layers and the articular disk in the temporomandibular joint. Acta Odontol Scand 1977; 35: 77-83.
10 Chen Y, Ke J, Long X, et al. Insulin-like growth factor-1 boosts the developing process of condylar hyperplasia by stimulating chondrocytes proliferation. Osteoarthritis Cartilage 2012; 20: 279-287.
11 Gray RJM, Sloan P, Quayle AA, Carter DH. Histopathological and scintigraphic features of condylar hyperplasia. Int J Oral Maxillofac Surg 1990; 19: 65-71.
12 Eslami B, Behnia H, Javadi H, et al. Histopathologic comparison of normal and hyperplastic condyles. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2003; 96: 711-717.
13 Almeida LE, Zacharias J, Pierce S. Condylar hyperplasia: an updated review of the literature. Korean J Orthod 2015; 45: 333-340.
14 Higginson JA, Bartram AC, Banks RJ, Keith DJW. Condylar hyperplasia: current thinking. Br J Oral Maxillofac Surg 2018; 56: 655-662.
15 Wolford LM, Mehra P, Reiche-Fischel O, et al. Efficacy of high condylectomy for management of condylar hyperplasia. Am J Orthod Dentofacial Orthop 2002; 121: 136-150.
16 Hamed MAG, AlAzzazy MZ, Basha MAA. The validity of SPECT/CT in diagnosis of condylar hyperplasia. The Egyptian Journal of Radiology and Nuclear Medicine 2017; 48: 451-459.
17 Saridin CP, Raijmakers PGHM, Tuinzing DB, Becking AG. Bone scintigraphy as a diagnostic method in unilateral hyperactivity of the mandibular condyles: a review and meta-analysis of the literature. Int J Oral Maxillofac Surg 2011; 40: 11-17.
18 McAllister P, Watson M, Burke E. A cost-effective, in-house, positioning and cutting guide system for orthognathic surgery. J Maxillofac Oral Surg 2018; 17: 112-114.
Betar N (MBBS(Hons), MS, BSc); Badri D (MBBS, MSc, BSc); McCombe A (BMedSc, MD); Finn B (MDS, MBBS, FRACDS(OMS))
In the traditional approach to mandibular sagittal split osteotomies, the emphasis is on variations in the design of the bone cuts, with only passing reference to the inferior alveolar nerve. This results in good bone surface contact and satisfactory bony union in the desired position but sometimes with the potential of significant neuropathy. The position of the inferior alveolar canal is highly variable, thus using standardised bone cut positions may not reliably avoid nerve injury.1
Recent advances made in virtual surgical planning, including computer-assisted design (CAD) and manufacturing (CAM), have led to improvements in the predictability and precision of the procedure.2 CAD/CAM techniques allow patient-specific anatomical information to be incorporated into prefabricated cutting guides and fixation devices that allow precise movement of the jaws. The location of the inferior alveolar canal can also be identified on computed tomography (CT) scan and incorporated into cutting guides to reduce the risk of nerve damage.1
The aim of this study is to demonstrate the use of CAD/CAM techniques to improve the safety of the bilateral sagittal split osteotomy that is individualised to protect the inferior alveolar nerve while ensuring good bony union.
Preoperative protocol
Patients undergo standard planning and preparation in conjunction with a multidisciplinary team including the orthodontist and oral and maxillofacial surgeon. Fine-slice CT data are used preoperatively to plan mandibular movements and to identify the positions of the lingula and mandibular canal. A safe virtual osteotomy path can be planned that accomplishes the required movements while protecting the mandibular canal. Once the virtual surgical plan is confirmed by the team, life-sized three-dimensional (3D) printed translucent skeletal models with an opaque inferior alveolar nerve in the canal are produced along with the novel patient-specific surgical guides for the mandible, custom osteosynthesis plates and screws, and occlusal splints. The patient-specific surgical guides and fixation are checked on the models prior to sterilisation and use.
The most common major complication of bilateral sagittal split osteotomy of the mandible is damage to the inferior alveolar nerve. Current fine slice computed tomography scanning can accurately define in three dimensions the course of the inferior alveolar nerve for the individual patient. Using CAD/CAM techniques, an individual cutting guide can be manufactured to precisely define the depth and direction of the inferior alveolar osteotomy. The planning and use of patient-specific mandibular cutting guides that account for the exact position of the inferior alveolar canal is described. The advantage is precision and patient safety, which is to be balanced against increased operative time and more extensive exposure.
Mandibular mucoperiosteal flaps are raised from the mental foramen anteriorly, lower border to the angle of the mandible, and oblique ridge to the sigmoid notch. The buccal mandibular surgical guide wraps around the lower border and thus requires that an area of periosteum is stripped from the lingual surface of the mandible at the level that the lower border osteotomy will be made. The superior aspect of masseter and medial pterygoid mandibular insertions are partially stripped to allow direct vision of the sigmoid notch and the mandibular nerve as it enters the mandibular foramen.
The mandibular buccal surgical guide is designed with a mesh shield over the course of the nerve in the line of the vertical cut to prevent damage to the contents of the mandibular canal while making accurate vertical and lower border osteotomies (Figure 1 and Figure 2). Accurate positioning of the guide on the mandible is achieved using a separate temporary prosthesis that fits on the occlusal surface of the molar teeth and indicates the vertical and anterior-posterior position of the anterior-most screw-hole of the buccal surgical guide (Figure 3). To protect the inferior alveolar canal during the lower border osteotomy, there are buccal and lingual blocks that stop the sagittal saw blade progressing superiorly to the level of the canal, while allowing for a complete lower border osteotomy (Figure 1 and Figure 4, A and B). Both the vertical cut
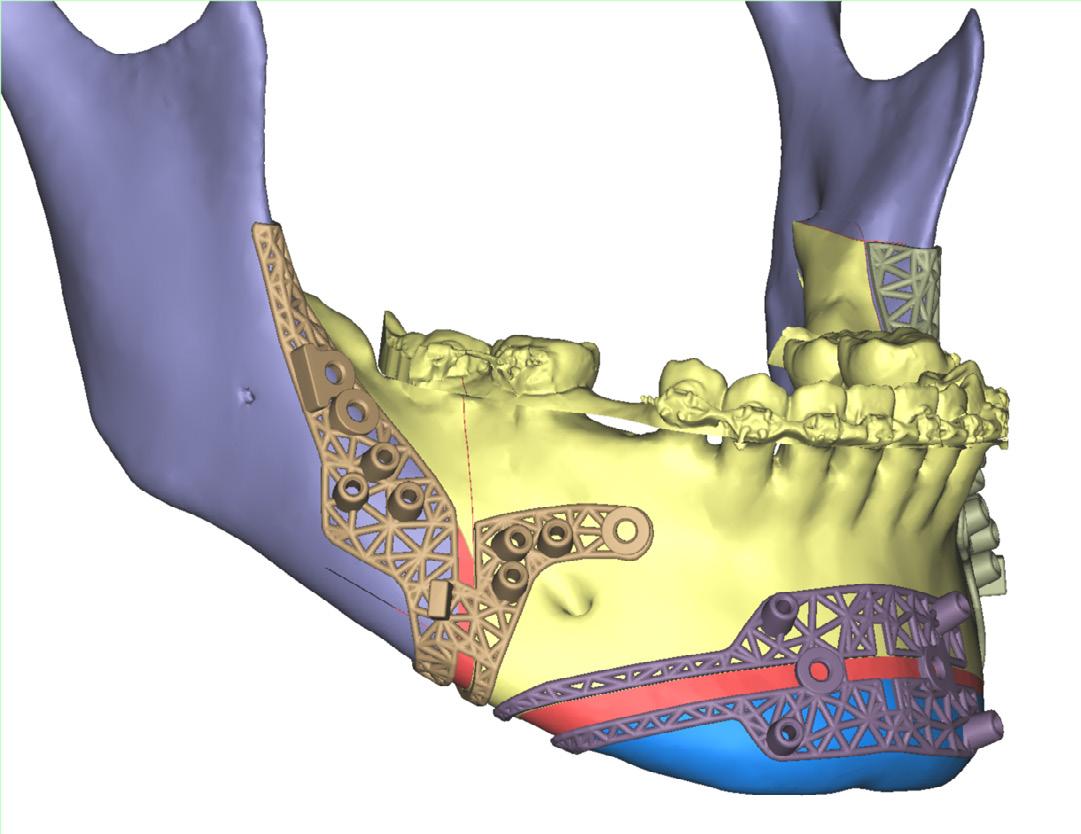
Figure 1. Three-dimensional (3D) rendered images of the mandibular buccal guides and genioplasty guides. The inferior alveolar canal is protected by the cutting block that sits on the buccal and lingual side of the mandible, allowing for safe vertical and lower border osteotomies. The superior extent of the buccal guide is a marker of the level just above the lingula

Figure 2. The extension of the buccal mandibular guides to the lingual side of the mandible allows for a cutting block at the level of the inferior alveolar canal to match that on the buccal side of the mandible, such that a reproducible and complete lower border osteotomy can be made while protecting the inferior alveolar canal contents
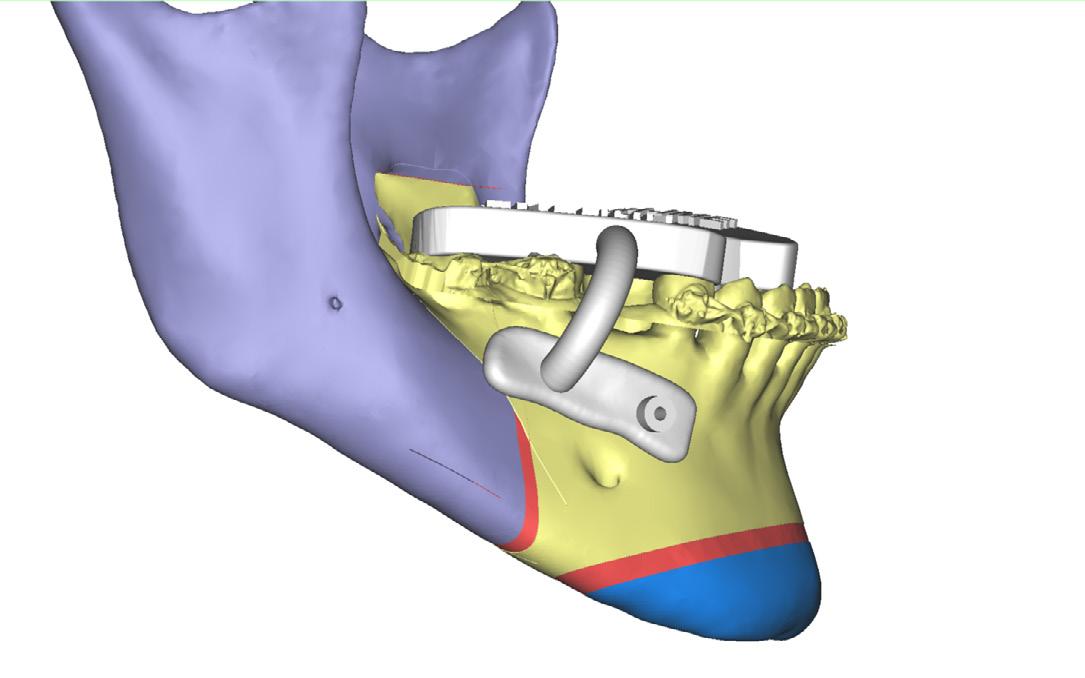
3. Three-dimensional (3D) rendered images of the occlusal guide used to accurately position the mandibular buccal guide

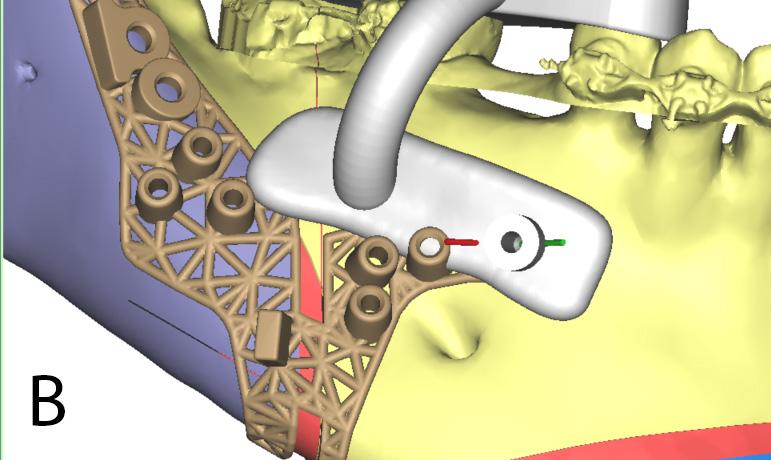
AFigure 4. (A and B) Computer-assisted design and manufacturing (CAD/ CAM) is used to place the screw holes associated with the occlusal guide and the other guides away from the teeth roots, demonstrated by the schematic showing a cross-section of the mandible (panel A) at the level of the guide screw hole
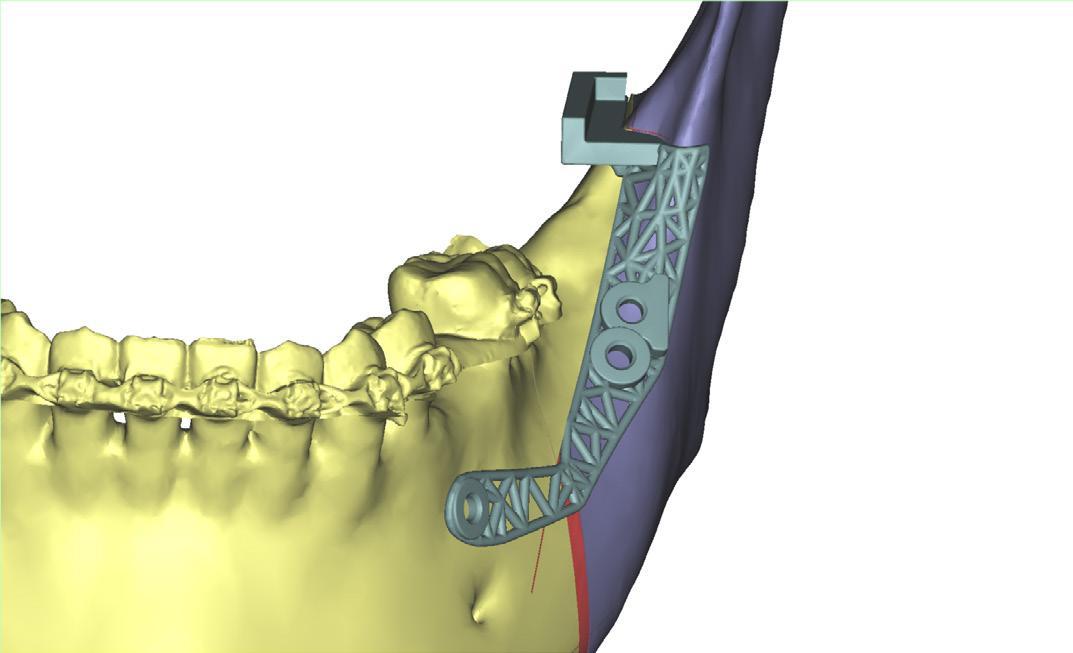
Figure 5. Three-dimensional (3D) rendered image of a left mandibular lingual cutting guide
above the canal and the lower border cut can be made with impunity, as the canal is protected by the buccal and lingual blocks. The upper border of the surgical guide running posteriorly from the vertical cut guides the sagittal osteotomy using the saw, which continues to the superior-most extent of the guide (which indicates a point just above the level of the lingula). After the buccal surgical guide is removed, the buccal plate of bone overlying the mandibular canal is carefully osteotomised freehand to complete the vertical osteotomy in full knowledge of the exact position of the nerve relative to the buccal cortex of the mandible. To further improve the safety of the nerve

Figure 6. Three-dimensional (3D) model of the mandibular ramus bilaterally in coronal cross-section, used to make the lingual mandibular guides by accounting for the position of the lingula, mandibular canal, and the superiormost level of separation of lingual and buccal cortical bone around the medullary cavity
during this step, the position of the vertical osteotomy is planned and placed at the point where the mandibular canal is furthest from the buccal mandibular cortex for that patient, rather than anatomically placed between the first and second molars.
The lingual surgical guide is placed on the mandible to facilitate a safe horizontal osteotomy above the lingula, but at a height low enough that the buccal and lingual cortices of the ramus are separated by medullary bone for sectioning (Figure 5 and Figure 6). The guide
is accurately positioned using pre-drilled screw holes previously made based on the buccal surgical guide. A cutting block sits on the medial side of the ramus that prevents angling of the saw towards the mandibular foramen (Figure 5). After the horizontal osteotomy is completed, the lingual surgical guide is removed and the sagittal split can be completed with a wedge, osteotome, or spreader anteriorly and a curved osteotome posteriorly. Placement of an osteotome for section can thus be made with knowledge of the position of the canal by using cross-sectional images that highlight the position of the nerve as it transits through the mandible (Figure 7). After establishing the final occlusion with a splint, fixation of the mandible is achieved using prefabricated plates and screws.
When compared with other currently available patient-specific surgical guides, this technique has several advantages. The mandibular surgical guides allow for accurate guide placement on the mandible to protect the inferior alveolar canal throughout its course, and for a safe and reproducible lower border and horizontal ramus osteotomy.
In our subjective experience over ten years, modified surgical guides have evolved to the current form through surgery on more than 50 patients. There have been no cases of inferior alveolar nerve transection resulting in permanent anaesthesia, but a formal evaluation will be the subject of further study.
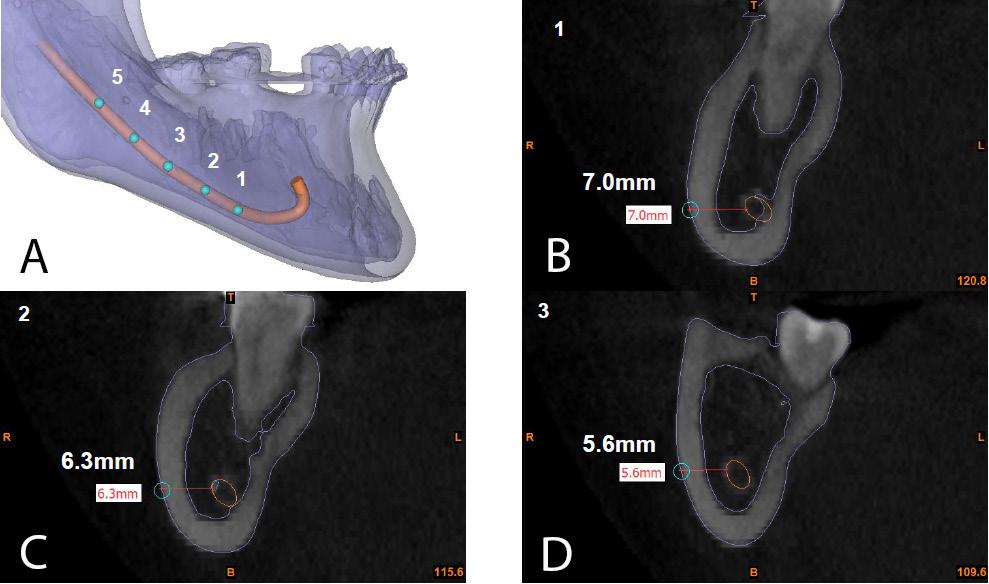
There are two main drawbacks to using these guides. Our experience has been that overall operative time is increased. In addition, the financial cost of the complete set of temporary and permanent prosthetics at the time of writing is significant, though this should be weighed against a potential decrease in the risk of complications and the costs associated with their treatment. A further disadvantage is the extensive exposure required to position the mandibular guides, but this does not appear to increase postoperative morbidity.
The technique and equipment modifications described in this manuscript were the work of Brian Finn in collaboration with the oral and maxillofacial surgery team at DePuy Synthes. The first draft of the
1 Yeh AYE, Finn BP, Jones RHB, Goss AN. The variable position of the inferior alveolar nerve (IAN) in the mandibular ramus: a computed tomography (CT) study.
Surg Radiol Anat 2018; 40: 653-665.
manuscript was written primarily by Noah Betar with contributions from Danniel Badri, Alistair McCombe and Brian Finn. All authors contributed to revisions and read and approved the final manuscript.
The authors wish to acknowledge the oral and maxillofacial surgery team at DePuy Synthes for their contributions to iterating designs and producing the modified surgical guides.
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript. The authors declare that they have no conflicts of interest.
2 Hammoudeh JA, Howell LK, Boutros S, Scott MA, Urata MM. Current status of surgical planning for orthognathic surgery: traditional methods versus 3D surgical planning. Plast Reconstr Surg Glob Open 2015; 3: e307.


Mian M (BDS, BScDent, MD, MPH)1; Gearing PF (MD, MSc(Surg), DipAnatSurg)1; Chen J (MD)1; Sreedharan S (MD, MPH)2; Kumar R (BHB, MBChB, BDS, FRACDS(OMS))1; Nastri A (BDSc, MBBS, MDSc, FRACDS(OMS))1
Delayed pain and a decrease in mouth opening are frequently encountered complications following orthognathic surgery. Previously described common causes include pre-existing muscle or temporomandibular joint (TMJ) dysfunction, surgically induced internal derangement, myostatic or myofibrotic contracture and lack of post-surgical muscular rehabilitation.1 Connective tissue conditions involving the muscles of mastication presenting after orthognathic surgery are relatively rare and not well described in the literature. Myositis ossificans describes non-neoplastic heterotopic bone formation in extraskeletal soft tissues such as skeletal muscle, tendons, nerves and subcutaneous fat.2 Depending on the cause, it is commonly classified into either myositis ossificans progressiva, which describes an autosomal dominant genetic disease affecting one-intwo-million people,3 and myositis ossificans traumatica, which occurs following a trauma.4 Myositis ossificans traumatica is most reported in the orthopaedic literature, typically affecting large skeletal muscles of the extremities, such as the quadriceps and brachialis muscles.2
Descriptions of myositis ossificans traumatica in masticatory muscles are rare, with fewer than 100 cases reported in the literature.5 Literature reviews of myositis ossificans affecting masticatory muscles have demonstrated a predilection for males in a ratio of 1.5–2.6:1, with a mean age of about 38 years.5,6 The most commonly affected masticatory muscle is the masseter (39%), followed by temporalis (24%), medial pterygoid (23%) and lateral pterygoid (13%).5 In two-thirds of cases, only a single masticatory muscle is involved, with two or more muscles involved in the remainder of cases.6 Myositis ossificans of non-masticatory muscles in the head and neck region has also been described, including the buccinator, platysma and sternocleidomastoid.7 This article is the first to describe a case of myositis ossificans traumatica following orthognathic surgery.
A 22-year-old male patient was referred by a private oral and maxillofacial surgeon to the oral and maxillofacial surgery unit of
Myositis ossificans traumatica describes non-neoplastic heterotopic bone formation in extraskeletal soft tissues following trauma. When the muscles of mastication are involved, the most reported symptoms are trismus, swelling and pain. We report the first published case of myositis ossificans involving masticatory muscles following elective orthognathic surgery.
In this case report, myositis ossificans developed in a young patient following an uncomplicated bilateral sagittal split mandibular osteotomy. The patient underwent bilateral coronoidectomy, then commenced non-steroidal antiinflammatory treatment and physical therapy.
Treatment of myositis ossificans of the masticatory muscles is controversial, with no consensus in the literature with regards to the need for surgical intervention, surgical timing, recurrence rates and the role of non-operative therapies. In this case, despite relapse following bilateral coronoidectomy, with radiographic evidence of further heterotopic bone formation, sustained increases in mouth opening were achieved with aggressive physical therapy.
Myositis ossificans traumatica of the masticatory muscles is rare. In this case, bilateral sagittal split osteotomy was the likely triggering event. Although a range of treatments have been described in the literature, there is no strong evidence to support their use. In our experience, aggressive physical therapy may be an effective treatment option.
the Royal Melbourne Hospital in September 2022 with a history of painless progressively reduced mouth opening, commencing one month after an uncomplicated bilateral sagittal split mandibular osteotomy and surgical removal of teeth 18, 38 and 48 in June 2022. His medical history included eczema and asthma, for which he was
1Department of Oral and Maxillofacial Surgery, The Royal Melbourne Hospital, Melbourne, VIC, Australia; 2Department of Radiology, The Royal Melbourne Hospital, Melbourne, VIC, Australia.
Corresponding author: Peter Gearing ✉ peter.gearing@mh.org.au | doi: 10.63717/2025.MS0031
Keywords: myositis ossificans | orthognathic surgery | bilateral sagittal split osteotomy

taking belimumab fortnightly and using a salbutamol inhaler as required. There was no family history of myositis ossificans or similar conditions. On examination, he had a maximal incisal opening of 3 mm with a hard end feel. A magnetic resonance imaging scan of both temporomandibular joints showed established bilateral degenerative changes (Figure 1).
The patient underwent bilateral TMJ arthrocenteses and intramuscular botulinum injections to the masseter and temporalis muscles bilaterally in mid-September with no intraoperative or post-operative change in his mouth opening. Subsequent blood
rheumatology screening (including anti-neutrophil cytoplasmic antibodies, double-stranded DNA antibodies, extractable nuclear antigen antibodies, antinuclear antibodies, cyclic citrullinated peptide antibodies and rheumatoid factor antibodies) and serum electrolyte levels were all within normal limits. A post-treatment computed tomography (CT) scan demonstrated no bony pathology of either TMJ but showed calcifications within the temporalis and lateral pterygoid muscles bilaterally (Figure 2).
Following a provisional diagnosis of myositis ossificans traumatica, the patient underwent a bilateral coronoidectomy in October 2022 and their mouth was manipulated open, following an audible “clunk”, to 30 mm mouth opening, which was maintained in the immediate post-operative period (Figure 3). Histopathological analysis of both coronoid processes showed normal cortical bone with no other significant findings. The patient was treated with celecoxib (100 mg, twice a day) and aggressive physical therapy using a TheraBite appliance (Atos, Australia). On review, one week after the bilateral coronoidectomy, his mouth opening had reduced to 20 mm and at six weeks post-coronoidectomy, had reduced to 3 mm. This was able to be increased to 6 mm over the following three months with physical therapy.
A repeat CT at six months after his initial osteotomy (ie, two months following coronoidectomy) showed further bone maturation bilaterally in the temporalis and lateral pterygoid muscles (Figure 4). With ongoing physical therapy, his mouth opening increased to 11 mm at 10 months after his initial osteotomy (Figure 5). He completed post-surgical orthodontic treatment and was debanded in September


2023. His mouth opening increased to 14 mm at his next 6-month review (16 months after the initial osteotomy; 12 months after the bilateral coronoidectomy) (Figure 6). The patient continues to be reviewed by our unit and consented for their clinical photography to be included in this report.
Myositis ossificans of the masticatory muscles is a rare complication following orthognathic surgery. This case report highlights the challenges in the management of this condition. Given the rarity of this condition, there is limited evidence regarding the need for and timing of surgical intervention, or the effectiveness of nonsurgical therapies. In this case, despite relapse following bilateral coronoidectomy with radiographic evidence of further heterotopic bone formation, sustained increases in mouth opening were achieved with continued aggressive physical therapy.
The pathogenesis of myositis ossificans traumatica is poorly understood. It is generally thought to result from inappropriate differentiation of fibroblasts into osteogenic cells.8 In the most widely accepted hypothesis, the lesion begins with an acute traumatic injury of skeletal muscle, followed by a local inflammatory cascade, including the release of osteogenic cytokines. These include bone morphogenetic protein 2 (BMP-2), BMP-4 and transforming growth factor. Perivascular mesenchymal cells respond by undergoing
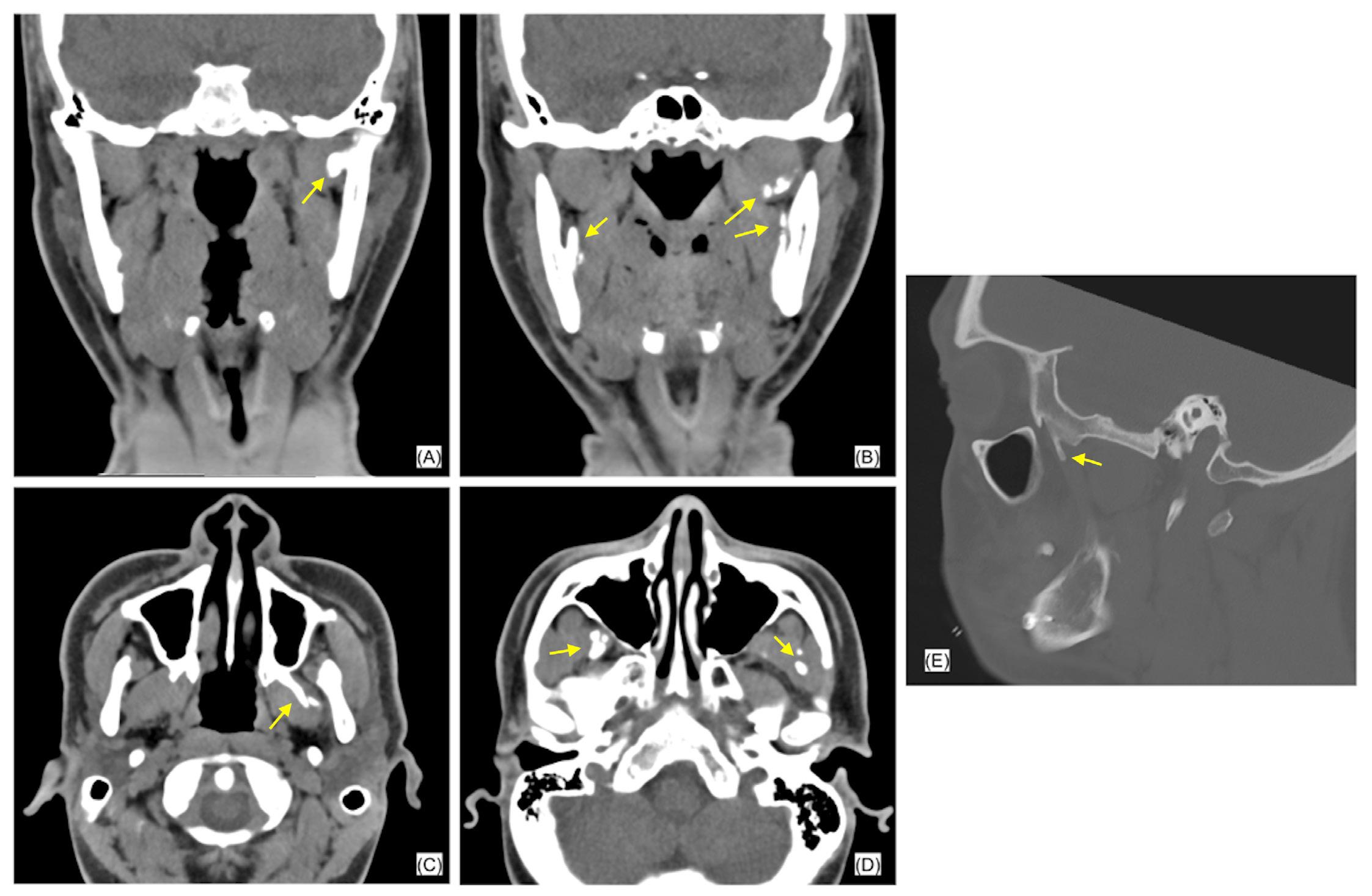


aberrant endothelial–mesenchymal transition, with some cells differentiating into chondrocytes and osteoblasts when exposed to an inflammatory-rich environment. This leads to heterotopic bone formation via endochondral ossification.9
Histopathological findings occur in stages. First, a highly cellular lesion forms with benign-appearing immature mesenchymal cells with high mitotic activity. This can be difficult to distinguish microscopically from malignant lesions such as sarcoma.10 Four to eight weeks after the triggering event, there is benign-appearing cartilage and immature bone formation. A centrifugal zonal pattern is seen due to immature osteoid gradually becoming more organised and mature at the periphery of the lesion.10 This differs from osteosarcoma, which matures from the centre to the periphery.11 Once mature, the lesion is characterised almost exclusively by lamellar bone.10
The clinical presentation of myositis ossificans is variable. In the extremities, the typical presentation is pain and joint stiffness following blunt soft tissue trauma, although repetitive minor trauma is also a common trigger.9 Subjectively, patients report muscle pain that persists longer than expected for a simple strain or contusion that is thought to be the result of the lesion causing mechanical irritation of a surrounding bursa, tendon or joint.9 Paraesthesia, weakness, lymphoedema and venous thromboembolic disease have also been reported as a result of the lesion compressing nearby neurovascular structures.7 When the muscles of mastication are involved, the most commonly reported symptoms are trismus (86%), swelling (27%) and pain (21%).5 Mouth opening in reported cases ranges from 0 to 15 mm, with a mean of 7.3 mm.5 A range of triggering events have been identified in the aetiology of myositis ossificans traumatica of the masticatory muscles including dental infection, inferior alveolar nerve blocks, dental extractions and mandible fractures.5 In about 20% of cases, a triggering event is not identified.5
The diagnosis of myositis ossificans is challenging and an accurate history is essential as a previous trauma or surgery is a common trigger. Computed tomography imaging is essential. The key radiographical feature of myositis ossificans is a lesion with a well circumscribed, high attenuating periphery with a low attenuating central portion.6 The lesion may be attached to adjacent bone,
depending on its maturity.6 Laboratory test results are generally within normal limits, except for a few reported cases that presented with an elevation in alkaline phosphatase levels.6 Histopathology may demonstrate peripheral mature lamellar bone, intermediate osteoid and cartilage, and a central area with proliferating fibroblasts, spindle cells and prominent giant mesenchymal cells.10
The treatment of myositis ossificans of the masticatory muscles is controversial. There is no consensus in the literature with regards to the need for and timing of surgical intervention, nor effectiveness of non-surgical therapies. The most common treatment reported is surgical excision of the lesion or affected muscle.5,6 In cases involving the temporalis muscle, coronoidectomy is the most frequently cited surgical treatment.12-21 While these cases report a high rate of cure, it should be noted that they are subject to significant bias and limited by short follow-up periods of three to 30 months. Some authors recommend excision in the mature phase of the disease, when the lesion is well delineated from surrounding skeletal muscle and bone activity is diminished, reducing the risk of recurrence.22,23 In contrast, other authors advocate for excision at an earlier stage due to the debilitating nature of the disease.24,25
A systematic review of published case reports found no correlation between the frequency of recurrence and the timing of treatment.4 Similar inconsistences exist with regards to post-operative physical therapy. Most authors recommend aggressive physical therapy after surgical excision; however, it has been suggested that this may stimulate further hematoma formation and osseous development.26,27 The use of interpositional materials following surgical resection attempts to reduce fibrosis and further heterotopic bone formation as well as inhibit reattachment of separated muscles. Published methods have used abdominal fat, silastic implants and buccal fat; however, the recurrence rate in these cases is high.26-30
A range of non-surgical treatments have been proposed in the management of myositis ossificans traumatica of the masticatory muscles, all with variable anecdotal reports regarding their success and no strong evidence to support their use. Non-steroidal antiinflammatory drugs (NSAIDs), including celecoxib and indomethacin, are thought to inhibit the differentiation of pre-osteoblasts and have
been used in orthopaedics to reduce heterotopic bone formation following hip surgery.31 A number of authors have used NSAIDs in the adjunctive treatment of myositis ossificans of masticatory muscles with variable results.5,29,32 Corticosteroids have been used in two cases, in addition to surgical excision, with recurrence shortly after initial surgery in both patients.29,33 Etidronate, a non-nitrogenous oral bisphosphonate, has been used in a number of cases both pre-operatively and up to three months post-operatively.26,27,29 It is thought that etidronate adheres to hydroxyapatite to prevent aggregation, growth and calcification of hydroxyapatite crystals.27 Finally, low dose radiation, similar to that which is used to prevent heterotopic bone formation in pelvic surgery has been suggested as a potential therapy by inhibiting the differentiation of mesenchymal cells into osteoblasts.34,35 Descriptions of both pre-operative treatment with a single dose of 6 Gy,5 and post-operative treatment, with a single dose of 7 Gy,29 have been published previously; however, recurrence occurred in both cases.
Although no particular drugs, other than intramuscular injections, have been associated with the development of myositis ossificans, it should be noted that in the presented case, the patient was on regular belimumab, a human monoclonal antibody that inhibits B-cell activating factor.10 Myositis ossificans is not an accepted adverse effect of belimumab, although three cases of trismus associated with the drug have been reported via the Food and Drug Administration’s Adverse Events Reporting System, but no further information is available regarding these cases. In the absence of a clear causal mechanism, the link between belimumab and the presented case remains unclear.11,12
Myositis ossificans traumatica of the masticatory muscles is rare. Patients, commonly middle-aged males, typically present following a history of trauma with reduced mouth opening and pain. In the case presented, a previous bilateral sagittal split osteotomy was the
1 Storum K, Bell W. Hypomobility after maxillary and mandibular osteotomies. Oral Surg Oral Med Oral Pathol 1984; 57: 7-12.
2 Saad A, Azzopardi C, Patel A, et al. Myositis ossificans revisited - The largest reported case series. J Clin Orthop Trauma 2021; 17: 123-127.
3 Ram GG, K KA, Vijayaraghavan PV. The stone womenMyositis ossificans Progressiva. J Orthop Case Rep 2015; 5: 10-13.
4 Nizel AE, Prigge EK. Trismus due to myositis ossificans traumatica; report of a case. J Oral Surg (Chic) 1946; 4: 93-101.
5 Hanisch M, Hanisch L, Fröhlich LF, et al. Myositis ossificans traumatica of the masticatory muscles: etiology, diagnosis and treatment. Head Face Med 2018; 14: 23.
6 Boffano P, Zavattero E, Bosco G, Berrone S. Myositis ossificans of the left medial pterygoid muscle: case report and review of the literature of myositis ossificans of masticatory muscles. Craniomaxillofac Trauma Reconstr 2014; 7: 43-50.
7 Godhi S, Singh A, Kukreja P, Singh V. Myositis ossificans circumscripta involving bilateral masticatory muscles. J Craniofac Surg 2011; 6: e11-e13.
likely triggering event. Diagnosis of myositis ossificans traumatica is made with characteristic radiographic and histopathological findings. A limited number of cases and lack of follow-up data prevent recommendations around optimum treatment. Surgical excision of the lesion or involved muscle is commonly performed with variable degrees of success. Although a range of adjunctive treatments have been described in the literature, there is no strong evidence to support their use. In the presented case, despite a relapse in reduction of mouth opening following bilateral coronoidectomy, with radiographic evidence of further heterotopic bone formation, sustained increases in mouth opening were achieved with aggressive physical therapy. This may represent the most effective treatment option in these cases.
Mian M: Case identification and data collection, literature review, writing original draft, approved final manuscript.
Gearing PF: Literature review, writing original draft, approved final manuscript.
Chen J: Literature review, approved final manuscript.
Sreedharan S: Literature review, approved final manuscript.
Kumar R: Case identification and data collection, provided oversight, expert guidance, and final approval of the manuscript, approved final manuscript.
Nastri A: Case identification and data collection, provided oversight, expert guidance, and final approval of the manuscript, approved final manuscript.
The patient provided written consent for publication.
The authors declare that they have no conflicts of interest.
8 Mavrogenis A, Soucacos P, Papagelopoulos P. Heterotopic ossification revisited. Orthopedics 2011; 34: 177.
9 Walczak B, Johnson C, Howe B. Myositis ossificans. J Am Acad Orthop Surg 2015; 23: 612-622.
10 Fabbri N. Myositis ossificans. In: Picci P, Manfrini M, Fabbri N, et al, editors. Atlas of musculoskeletal tumors and tumorlike lesions. New York: Springer, 2014; pp 271-275.
11 Devilbiss Z, Hess M, Ho G. Myositis ossificans in sport: a review. Curr Sports Med Rep 2018; 17: 290-295.
12 Nemoto H, Sumiya N, Ito Y, et al. Myositis ossificans traumatica of the masticatory muscles. J Craniofac Surg 2012; 23: e514–e516.
13 Becker OE, Avelar RL, Rivero ER, et al. Myositis ossificans of the temporalis muscle. Head Neck Pathol 2016; 10: 340-344.
14 Jayade B, Adirajaiah S, Vadera H, et al. Myositis ossificans in medial, lateral pterygoid, and contralateral temporalis muscles: a rare case report. Oral Surg Oral Med Oral Pathol Oral Radiol 2013; 116: e261-e266.
15 Ramos EADA, Munhoz L, Milani BA, et al. Myositis ossificans traumatica of the temporal muscle: a case report and literature review emphasizing radiographic features on computed tomography and magnetic resonance imaging. J Oral Maxillofac Res 2019; 10: e5.
16 Myoken Y, Sugata T, Tanaka S. Traumatic myositis ossificans of the temporal and masseter muscle. Br J Oral Maxillofac Surg 1998; 36: 76.
17 Schiff MJ, Meara DJ. Myositis ossificans of the temporalis muscle: case report and review of the literature. J Oral Maxillofac Surg 2013; 71: 1893-1898.
18 Mevio E, Rizzi L, Bernasconi G. Myositis ossificans traumatica of the temporal muscle: a case report. Auris Nasus Larynx 2001; 28: 345-347.
19 Guarda-Nardini L, Piccotti F, Ferronato G, Manfredini D. Myositis ossificans traumatica of the temporalis muscle: a case report and diagnostic considerations. Oral Maxillofac Surg 2012; 16: 221-225.
20 Reddy SP, Prakash AP, Keerthi M, Rao BJ. Myositis ossificans traumatica of temporalis and medial pterygoid muscle. J Oral Maxillofac Pathol 2014; 18: 271-275.
21 Yano H, Yamamoto H, Hirata R, Hirano A. Post-traumatic severe trismus caused by impairment of the masticatory muscle. J Craniofac Surg 2005; 16: 277-280.
22 Thangavelu A, Vaidhyanathan A, Narendar R. Myositis ossificans traumatica of the medial pterygoid. Int J Oral Maxillofac Surg 2011; 40: 545-549.
23 Thorndike A. Myositis ossificans traumatica. J Bone Joint Surg 1940; 22: 315.
24 Parnes E, Hinds EC. Traumatic myositis ossificans of the masseter muscle: report of case. J Oral Surg 1965; 23: 245-250.
25 Arima R, Shiba R, Hayashi T. Traumatic myositis ossificans in the masseter muscle. J Oral Maxillofac Surg 1984; 42: 521-526.
26 Spinazze RP, Heffez LB, Bays RA. Chronic, progressive limitation of mouth opening. J Oral Maxillofac Surg 1998; 56: 1178-1186.
27 Conner GA, Duffy M. Myositis ossificans: a case report of multiple recurrences following third molar extractions and review of the literature. J Oral Maxillofac Surg 2009; 67: 920-926.
28 Torres AM, Nardis AC, da Silva RA, Savioli C. Myositis ossificans traumatica of the medial pterygoid muscle following a third molar extraction. Int J Oral Maxillofac Surg 2015; 44: 488-490.
29 Kim DD, Lazow SK, Har-El G, Berger JR. Myositis ossificans traumatica of masticatory musculature: a case report and literature review. J Oral Maxillofac Surg 2002; 60: 1072-1076.
30 Rattan V, Rai S, Vaiphei K. Use of buccal pad of fat to prevent heterotopic bone formation after excision of myositis ossificans of medial pterygoid muscle. J Oral Maxillofac Surg 2008; 66: 1518-1522.
31 Romanò CL, Duci D, Romanò D, et al. Celecoxib versus indomethacin in the prevention of heterotopic ossification after total hip arthroplasty. J Arthroplasty 2004; 19: 14-18.
32 Jiang Q, Chen MJ, Yang C, et al. Post-infectious myositis ossificans in medial, lateral pterygoid muscles: a case report and review of the literature. Oncol Lett 2015; 9: 920-926.
33 Almeida LE, Doetzer A, Camejo F, Bosio J. Operative management of idiopathic myositis ossificans of lateral pterygoid muscle. Int J Surg Case Rep 2014; 5: 796-799.
34 Georhakopoulos I, Kouloulias V, Kougiountzopoulou A, et al. Radiation therapy for the prevention of heterotopic ossification: efficacy and toxicity of single fraction radiotherapy. Orthop Rev (Pavia) 2020; 12: 8577.
35 Hildebrandt G, Seed MP, Freemantle CN, et al. Mechanisms of the anti-inflammatory activity of low-dose radiation therapy. Int J Radiat Biol 1998; 74: 367-378.
13-15 NOVEMBER 2025 ADELAIDE CONVENTION CENTRE SOUTH AUSTRALIA
The ANZAOMS 2025 Annual Scientific Meeting will be held in the beautiful City of Adelaide in South Australia. The 2025 ASM promises to deliver an engaging and thought-provoking scientific program alongside a dynamic exhibition and social program.

Professor Krishnamurthy Bonanthaya
MBBS, MDS, FDSRCS, FFDSRCS Bangalore Institute of Dental Sciences India





Professor Xudong Wang DDS, MD
Professor
Department of Oral and Craniomaxillofacial Surgery
Vice President Ninth People’s Hospital


KEY DATES
CALL FOR ABSTRACTS OPEN 7 April 2025
REGISTRATION OPEN 5 May 2025
CALL FOR ABSTRACTS CLOSE 9 July 2025
EARLY BIRD REGISTRATION CLOSES
22 September 2025
ANZAOMS 2025 ASM 13 - 15 November 2025
Sir A Bloomfield (KNZM, MBChB, MPH, FNZCPHM)
The Sir John Walsh Oration was instituted by the Australian and New Zealand Association of Oral and Maxillofacial Surgeons (ANZAOMS) (New Zealand) to honour Sir John Walsh who was the dynamic Dean of Dentistry at the University of Otago from 1956 to 1972.
Sir Ashley Bloomfield was the Director-General of Health in New Zealand over the period of the COVID-19 pandemic. This is an edited version of his oration, presented at the ANZAOMS conference in Queenstown, August 2024.
It is exactly 40 years since I started medical school in Auckland. I certainly had no inclination that I would pursue a career in public health, public service and health care leadership and ultimately find myself as Director-General of Health during a one-in-100-year pandemic.
Back in 1984, there were just over 100 medical students in each year and females outnumbered males. Our national adult smoking rate was 33%, and over 50% for Māori (they are now 7% and 17%, respectively). Human immunodeficiency virus had been discovered just the previous year and had yet to be identified as the cause of acquired immunodeficiency syndrome (AIDS). Clinicians at the National Women’s Hospital, which was the main obstetrics and gynaecology hospital in New Zealand at the time, published an article on the invasive potential of cervical carcinoma in situ, based on research in which the women who were the research subjects didn’t know they were part of an experiment.1 This led to a cascade of events, commencing with the Cartwright Inquiry in 1987–1988 and included the subsequent development and implementation of routine informed consent processes and the establishment (six years later) of the Health and Disability Commissioner.
One thing that has not changed is that the health system is complex, and getting more complex as time passes. There are many reasons for this, including:
There are multiple, often conflicting, political and policy objectives, for example, efficiency and equity.
There is a high degree of political, public and media scrutiny.
There are many stakeholders with different agendas.
The health system needs a highly skilled workforce, both clinical and administrative. Just as an army wins or loses based on the quality of its logistics, so too are administrative staff essential members of the health care team.
Health professionals have a high degree of individual autonomy that drives resource use and can sometimes be at odds with overall system objectives.
Population needs differ; it is challenging to deliver equity of access, experience and outcomes from care, as well as the specific obligation to improve Māori health under Te Tiriti o Waitangi in New Zealand.
It can be difficult to measure and report on performance, especially productivity.
Assuring quality and safety in such a complex system is challenging and sometimes there are poor outcomes for individuals.
And finally, there are ongoing cost increases, driven by an ageing population, technological advances, changing expectations and international workforce shortages. Funding in health is always an issue; there is never enough money to go round. This generates political debate as a false dichotomy of “insufficient funding” versus “inefficient or inappropriate spending” is presented.
High income countries spend about 10% of their gross domestic product (GDP) on health (except for the United States of America, which spends 20%). The 10% includes both public and non-public funding. This has been increasing slowly for many years, including in New Zealand. The threat of “unaffordable” increases in health spending has been raised for decades in New Zealand and other high
School of Public Health, The University of Auckland, Auckland, New Zealand. Corresponding author: Sir Ashley Bloomfield ✉ bloomfielda.who@gmail.com | doi: 10.63717/2025.MS0039
Keywords: public health | COVID-19 | workforce strategies
income countries. The reality is that these “doom” scenarios have not eventuated as predicted — at least not yet!
In terms of health’s proportion of core government spending, and public spending as a proportion of GDP, New Zealand is by no means an outlier compared with Australia, the United Kingdom and Canada, which all have predominantly publicly funded health care systems. Despite Australia’s public spending as a proportion of GDP (38%) being 5% lower than New Zealand’s (43%), Australia still spends more on public services per capita (US$24 700) than New Zealand (US$20 800).
The key issue that needs to be considered is where the money is spent. The New Zealand Ministry of Health has estimated that by 2025, more than 50% of health care funding will be spent on people over 65 years of age. To be clear, ageing is humankind’s greatest achievement, and we want people to live long and healthy lives, but ageing is by far the most important driver of increasing health system costs and complexity. A key reason for this is that age is the largest risk factor for non-communicable diseases, with cancer, cardiovascular disease, respiratory disease and diabetes being the “big four”. Our economic planning needs to take into account that a large proportion of future spending will be focused on the “care economy”. That is not a bad thing, and careful planning and public discussion of the issues and trade-offs will be essential.
Beware the person with a simple solution to a complex problem, especially a structural solution! Returning to the 1980s, a landmark report by the Hospital and Related Services Taskforce and Gibbs2 titled “Unshackling the hospitals” was released in 1988 and identified key challenges: equity; access, including waiting lists; efficiency; morale and a range of “management deficiencies”, and concluded:
“Our recommendations relate largely to changes in structure. … We believe that the structure we have developed, which separates the roles of funder and provider would unshackle those who provide our health services from most bureaucratic control ... In the improved environment that should develop from this independence, we expect many dynamic, creative and unforeseeable adaptations to take place”. 2
Since 1988, New Zealand has introduced a range of organisational bodies such as: area health boards, regional health authorities, the Ministry of Health (previously the Department of Health), Crown health enterprises, health and hospital services, a health funding authority, district health boards, public health organisation, Te Whatu Ora (Health New Zealand) and the unfortunately short-lived Te Aka Whai Ora (Māori Health Authority).
Before we consider the future of the system, let’s consider briefly where we are now. Judging by what is in the media, our health system is one big “crisis and failure”; we now also have the “polycrisis”, which is like a layered wedding cake of crises.
However, our health system is not failing, and it is not helpful to play into the polycrisis narrative because:
the challenges are not unique to New Zealand, and they are not unique to now;
if everything is a crisis, then it is hard to identify and act on the real crises; and
a prevailing “crisis and failure” story can make people feel that there is nothing that can be done, it undermines trust in the system and hope that things can get better.
Also, it is important for us to always remember that we are making a difference, and if there is one thing we need to do more of, it is to celebrate and communicate our successes, which are manifold. Two examples of our successes include:
An analysis by Business and Economic Research Ltd noted:
“In our April 2021 series on government expenditure, we have argued that in other key areas of government expenditure, increased spending has not necessarily resulted in improved outcomes. However, health is a notable exception. The steady increase in health spending by the government has translated to higher life expectancies, on average. Government spending in this area has contributed to improvements in technology, better nutrition and cleaner living, all of which have resulted in people living longer. Since the early 90s, average life expectancy in New Zealand has gone up by nearly six years, with the average New Zealander now living up to 82 years of age. This demonstrates just how vital investment in public health resources is to improving the overall health of a nation’s population.” 3
Māori life expectancy has increased; the gap with non-Māori persists but is closing.
Smoking rates among 14- to 15-year-olds in New Zealand Māori females have decreased from 35% in 2000 to 3% in 2024.4 The intergenerational effect of this is profound. However, prevention saves lives, but it does not save money.
Humans singularly have the ability to both imagine a better future, and make it happen. So how do we imagine and realise a stronger, sustainable, better future health system? This goal is complex and multidimensional. I want to share one central idea that I think is key to evolving New Zealand’s future health system to deal with the extant and future challenges; how we think about and address the health workforce.
The central point is that we need to think very differently about our workforce if it is going to be sustainable and affordable in future.
Almost all countries are facing funding challenges and health workforce shortages and there is international competition for health care workers, for example:
A Times UK article published on 8 March 2024: “Nurses quit NHS in ‘exodus’ for better pay overseas” (including New Zealand!).5 More recently, the new UK Labour Government has stated that the NHS is “broken” and their Secretary of State has determined that this is the government’s “official policy”.
In the ‘World’ section of New Zealand’s Sunday Star Times on 16 June 2024, there was an article titled “Call to lift funding amid national crisis for health”. This referred to Australia, not New Zealand.
The key health workforce challenges have been present for years. The issues are manifold: unfilled vacancies; recruitment and retention challenges; pay and conditions (including for us in New Zealand, the gravitational pull of Australia), and insufficient Māori and Pacific staff being some of them.
What is new is that the workload in some areas is unmanageable, and the work environment has become unrewarding for many people due to its increasing complexity and a lack of hope that the challenges can be addressed, especially post-COVID. A key point is that work needs to be both rewarded and rewarding.
It is not simply a matter of increasing the number of health professionals. There were 7600 doctors registered to practice in New Zealand in 1984, which had climbed to 18 800 by 2023, a 150% increase.6 By comparison, the New Zealand population increased by about 60% over the same period. There have been significant increases in the number of nurses, especially in the last five years, and whole new professional specialties and groups have emerged over that period, for example, anaesthetic technicians and emergency medicine specialists.
I suggest that a central challenge and focus for us is how might we create workplaces where work is more rewarding and where people enjoy their work. Of course, having sufficient staff is vital in achieving rewarding work, but if we keep thinking about the workforce largely in terms of numbers, pay and conditions, we will always find we have shortages, ever increasing numbers of vacancies, a pay differential with Australia, and so on. We need to shift the focus towards work and workplaces that are rewarding.
The first thought is how care is delivered, that is, models of care. If we have more staff than ever, and we are increasing the number of staff at a rate much higher than population growth and demographic change, we really need to reconsider how and where we are deploying staff in the health system.
One area where there is a major mismatch between policy intent and implementation is strengthening the role that primary care plays in the system. Successive governments over the last three decades
have signed up to this policy; however, the opposite has happened: a greater proportion of health funding has gone into specialist services, more doctors are specialising rather than training in general practice or as generalists, and primary care is arguably the most precarious part of the system. This absolutely needs to change. If we are to deal well with the ongoing impact of population ageing, the focus of the health system needs to be fairly and squarely on primary care and other community-based services, including community nursing and allied health services, home-based support services, aged residential care, Māori and Pacific providers, mental health and additional providers and community pharmacy.
Related to this is the question of whether emergency departments are still the right “front door” for hospitals, or whether we need to rethink this. While there is an ongoing slow increase in the complexity of presentations to the emergency departments as befits the ageing population, many of the people arriving are first-contact, undifferentiated presentations, like those seen and dealt with rapidly within primary care. Yet emergency department staff seldom do any training in primary care. The whole emergency department model is a very fruitful potential area for evolving our health system through rapid cycles of implementing small changes through “review, learn, adjust”; I also think a joint general practitioner/emergency medicine training pathway is worth serious consideration.
A second focus is the use of data, information, and generative AI to support more efficient, rewarding and equitable care. We made huge gains in this area during COVID because of the urgent imperative and the availability of resources.
Simple AI functions can rapidly free up workforce capacity in the system, reduce the administrative burden and make the work environment more rewarding. One example is the use of the Nabla app in primary care to transcribe consultations, thus freeing up capacity and reducing both the administrative and cognitive burden on practitioners.7 Over 400 general practitioners are now subscribing to this app. The experience for both the clinician and patient is great; clinicians are reducing both their cognitive and administrative burden, while patients feel better listened to because the clinician is not typing during the consultation. For the AI program to work, the general practitioners have to vocalise their thinking, so patients have a much better idea of what is or might be going on. Teams in Te Whatu Ora are working on an even better version of Nabla for deployment in both hospital (specialist) and community settings, addressing New Zealand privacy and security issues and integrating it with other key information systems.
The pace at which generative AI is developing provides cause for concern, in that it is potentially a values-free ecosystem (similar to social media), and the pace with which it is developing is well ahead of appropriate regulation and oversight by governments. These concerns will need to be addressed. However, there is a significant opportunity here and we should use it to our advantage. Given that governments are likely to lag in developing an adequate regulatory approach, the private sector can and maybe should take a lead here on behalf of the public.
A third area of focus that I think would make the work environment more rewarding and improve equity, efficiency and sustainability is the routine use of research-informed implementation, innovation and quality improvement, to learn fast in an agile way. We had to do this during COVID and, I dare say, despite the stress and challenges we all faced then, it was also immensely rewarding. This will require a new sort of relationship and partnership between researchers and clinicians/leaders/implementers, to an integrated, transdisciplinary approach that, by design, also involves patients, whanau and communities, and would support a move towards much greater public value for the research we undertake and more timely and agile system changes.
All the above are not necessarily new ideas, and none are particularly easy, but then neither was mounting such an effective response to COVID-19.
Finally, the essential ingredient for achieving these changes, and the many other changes needed to evolve our system into the future that we imagine, is great leadership.
One definition of leadership is that “Leadership is an invitation to collective action”. Good leaders are in the arena every day facing up to the challenges, ensuring clarity of purpose and direction, listening, making connections between different pieces of information and knowledge, building and sustaining relationships, finding a way forward on small and big issues, empowering others, and inspiring action. The health system works largely through a “convene and collaborate” approach; it is rarely a “command and control” system except when the need arises, for example, in emergencies. This is a huge advantage, because this is exactly the sort of leadership that
1 McCredie MR, Paul C, Sharples KJ, et al. Consequences in women of participating in a study of the natural history of cervical intraepithelial neoplasia 3. Aust N Z J Obstet Gynaecol 2010; 50: 363-370.
2 Hospital and Related Services Taskforce, Gibbs A. Unshackling the hospitals: report of the Hospital and Related Services Taskforce. Wellington, New Zealand: The Taskforce, 1988.
3 Yadav U. Health’s insatiable demand for expenditure. Business and Economic Research, 21 Apr 2021. https://
is needed to solve current and future challenges, both known and unknown.
Training and supporting great health system leaders is the most important action we can take as a country to ensure our health system delivers for New Zealanders in the future. Leaders are not born; leading is a set of learned skills and behaviours based on clear values that generates a strong organisational culture; this creates an environment where staff feel valued and that their work is rewarding as well as rewarded.
In summary, delivering health care is complex, challenging and costly. This is not new but has been more apparent since we navigated through the biggest global pandemic in a century. Repeatedly pointing out the problems and labelling them as crises or failures doesn’t create an environment that will ensure excellent and more equitable health care in the future. Responding rather than reacting to these challenges requires great leaders who are technically competent and also tenacious, trustworthy, engaging, values driven, and relentlessly positive. These are the leaders who, like Sir John, have made a difference over the years, and there are many of them in the system now, which gives me great hope that we will continue to navigate our way successfully through the challenges.
Author contributions
Bloomfield A: Conception, public health data analysis, final presentation.
of interests
The author declares that they have no conflicts of interest.
berl.co.nz/economic-insights/healths-insatiabledemand-expenditure (viewed Oct 2024).
4 New Zealand Government Ministry of Health. New Zealand’s smoking rates continue to decline [media release]. 14 Dec 2023. https://www.health.govt.nz/ news/new-zealands-smoking-rates-continue-to-decline (viewed Oct 2024).
5 The Times. Nurses quit NHS in ‘exodus’ for better pay overseas. The Times (London); Oct 2024. https://www.
thetimes.com/uk/article/nurses-quit-nhs-exodus-betterpay-qrfwmctf0 (viewed Oct 2024).
6 Medical Council of New Zealand. The New Zealand Medical Workforce 2023. New Zealand: Medical Council of New Zealand, 2023. https://www.mcnz.org.nz/assets/ Publications/Workforce-Survey/Workforce-SurveyReport-2023.pdf (viewed Oct 2024).
7 Nabla Copilot. https://www.nabla.com/ (viewed Oct 2024).
Petterson C (BDS); Singh T (BDS, MBChB, MPhil, FRACDS(OMS)); Ananth K (BDS)
Microvascular free flap reconstruction is considered the gold standard for the management of head and neck surgical defects.1 The success of such flaps relies on the perfusion through local anastomoses and, indirectly, systemic factors. The overall head and neck free flap failure rate is less than 5%, according to a large multicentre prospective study.2 Khouri and colleagues2 also observed that identification of intraoperative thrombosis allowed for successful revision of anastomoses at the time, with only 4.1% of these flaps failing. A process known as the “no-reflow phenomenon” describes poor reperfusion of tissue despite the lack of evidence of mechanical vessel obstruction, and may occur during microvascular free flap reconstruction. No-reflow is described across several specialties, such as interventional cardiology, when reperfusion of cardiac tissue fails despite lack of angiographic evidence of thrombosis.3
Alteplase is a fibrinolytic drug. Specifically, it is a recombinant human tissue-type plasminogen activator. The usual indication for its use is in thrombotic events such as acute myocardial infarction, massive pulmonary embolism, and acute ischaemic stroke. Alteplase activates plasminogen to form plasmin, which degrades the fibrin clot. Currently, the use of alteplase in free flap surgery is considered “off-label”.4
There are many publications describing the use of thrombolytics in free flap reconstruction, including streptokinase, urokinase, aspirin, dextran and heparin.5,6 Alteplase has been described in intraoperative salvage during radial forearm flap reconstruction of the palate and a deep inferior epigastric perforator flap (DIEP) in reconstructive breast surgery.7,8 However, no literature could be found supporting the use of alteplase to manage a no-reflow situation during a fibula free flap reconstruction in head and neck surgery.
This case report describes the successful intraoperative management of a fibula free flap, which demonstrated the noreflow phenomenon, using locally administered alteplase in an otherwise well 17-year-old male patient with a right mandibular odontogenic myxoma.
Microvascular free flap reconstruction is considered the gold standard for the management of many head and neck surgical defects. The vitality of the flap is reliant on the perfusion of the reconstructed tissue with vascular anastomoses to the recipient site. Alteplase is a fibrinolytic drug normally indicated for use in thrombotic events.
There are very few case reports in the literature to support the use of fibrinolytic agents in microvascular flap surgery, and alteplase may provide an option for intraoperative flap salvage when all other avenues have been exhausted.
A 17-year-old male patient was referred to the Oral and Maxillofacial Surgery department at Waikato Hospital (Hamilton, New Zealand) when his dentist found an incidental multilocular lesion on the posterior right mandible during routine imaging (Figure 1). A magnetic resonance imaging scan showed intramedullary extension of the lesion towards the angle and symphysis of the mandible. Clinically, a right sided facial deformity could be seen, but the patient was otherwise asymptomatic (Figure 2). Incisional biopsy confirmed the lesion as an odontogenic myxoma. The patient was otherwise well, took no regular medications, and did not smoke or drink alcohol.
Waikato Hospital, Te Whatu Ora, Hamilton, New Zealand. Corresponding author: Chantelle Petterson ✉ chantelle.rsa@gmail.com | doi: 10.63717/2025.MS0028
Keywords: alteplase | anastomosis | fibrinolytic | microvascular | myxoma
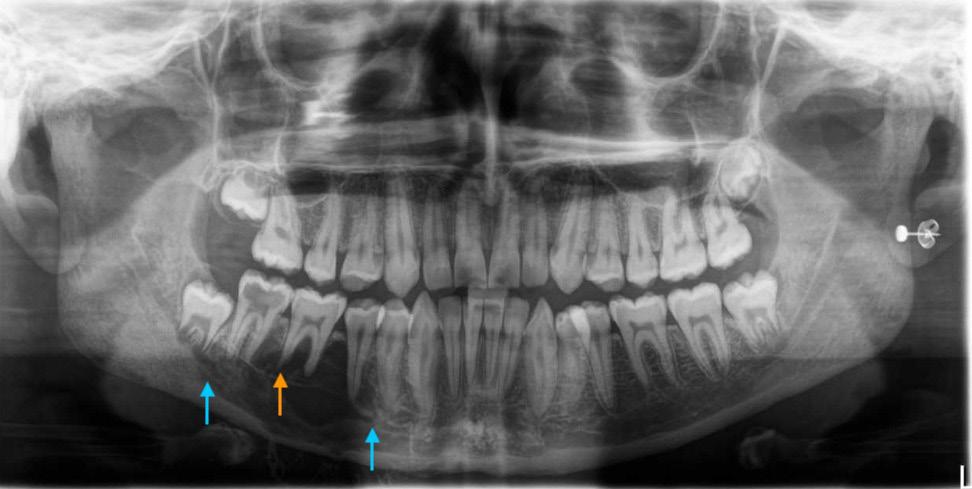
Figure 1. Preoperative mandible orthopantomogram: a multiloculated radiolucency is seen in the right mandibular body associated with teeth 44–47 (blue arrows). Evidence of root resorption of 46 is seen (orange arrow). Expansion of the lesion into the soft tissue seen by the calcified margins of the lesion inferior to the mandibular border

2. Preoperative photograph demonstrating deformity at the right mandibular body extending towards the mandibular midline
Various treatment options were discussed, and the patient underwent virtual surgical planning to plan his resection and design a fibula free flap to reconstruct the mandible. The fibula bone can be shaped into a structure similar to the native mandible and is therefore commonly used in head and neck reconstructive surgery.9 He underwent a right segmental mandibulectomy and reconstruction with a left fibula free flap in late 2022. As a young and physically well patient, no preoperative deep vein thrombosis prophylaxis was deemed necessary.
Following tumour resection, a composite osseocutaneous fibula flap was raised without complication. Heparin (5000 units) was
administered subcutaneously, as per the department protocol, prior to disconnecting the flap from the donor site. The peroneal artery and two veins were prepared for anastomosis to the facial artery, common facial vein and external jugular vein, respectively. The flap was flushed with heparinised saline (10 000 IU heparin/50 mL saline) solution prior to anastomosis. A total ischaemic time of 42 minutes was recorded between flap disconnection from the donor site to initial anastomosis in the neck. After initial anastomosis, there was adequate flap perfusion, and the flap was left to run for 15 minutes before finalising the inset and closure. However, on assessment of the flap, it was noted that the skin paddle and muscle had lost perfusion. Inconsistent and intermittent blood flow was detected through the veins and artery after clinical assessment and with both implantable and external doppler probes. Application of papaverine, which is an anti-vasospasmodic agent, did not improve the situation. The arterial anastomosis was repositioned to a more proximal location on the facial artery, resulting in improved arterial flow. On inspection of the previous anastomosis, there was no thrombus nor any technical microsurgical error. However, the venous flow continued to be sluggish. After more time to review flow, the distal aspect of the muscle and skin paddle still lacked circulation. The venous anastomoses were also revised, but again no technical microsurgical error or thrombus was noted at either site. The arterial anastomosis was once again revised, with the peroneal artery anastomosed to the external carotid artery. Initially good perfusion was noted, prior to again reduced venous outflow, then poor skin and muscle perfusion.
The decision was made to excise the skin paddle due to future risk of congestion and flap failure and the muscle was debrided to proximal bleeding regions, although this was limited. As an attempt to improve vascularity, the peroneal artery was partially accessed by incision through the vessel wall (arteriotomy) with a small cannula, and alteplase 2 mg (Actilyse 2 mg; Boehringer Ingelheim, New Zealand) was injected into the arterial pedicle over the course of ten minutes with the anatomosed veins clamped closely beyond the anastomosis site (ie, a closed system). The solution was prepared in a 1 mg/1 mL concentration by mixing the 10 mg Actilyse powder with 10 mL sterile water. A 3 cc syringe was used to administer the 2 mL solution through the cannula at 0.2 mL per minute intervals. The flap was allowed to rest and flushed with copious heparinised saline to clear the remaining alteplase prior to clamp removal. A revised arterial anastomosis was performed, yielding positive perfusion results throughout the flap upon clamp release (Figure 3).

procedure demonstrating findings and subsequent interventions
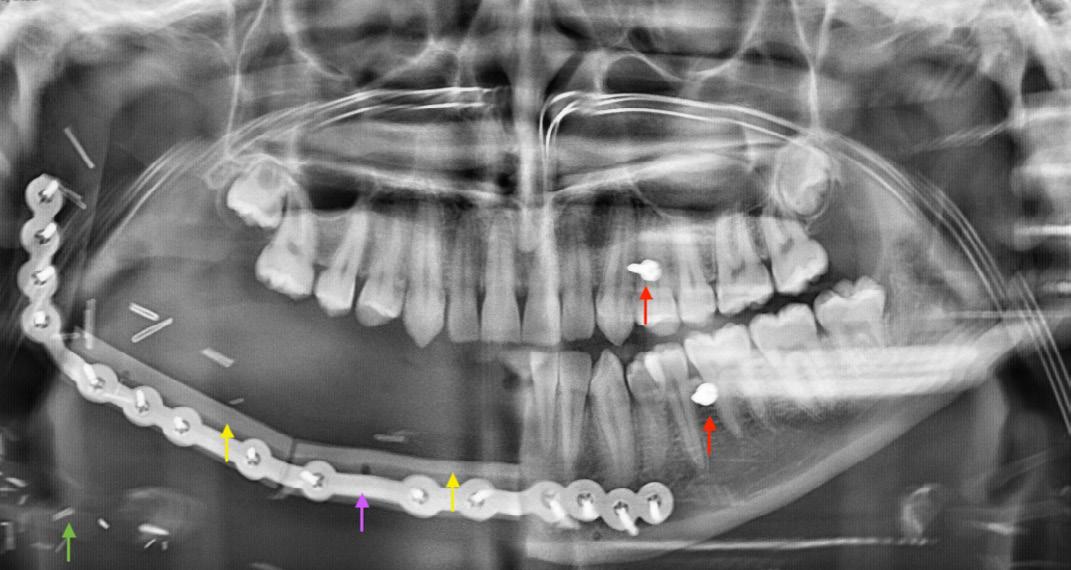
Figure 4. Postoperative orthopantomogram showing fibula flap (yellow arrows) with associated metal ware (purple arrow) and soft tissue vessel clips (green arrow). Left maxillary and mandibular intermaxillary fixation screws (red arrows) in situ for dental approximation. There are plans for dental implant placement and prosthetic rehabilitation in the near future
At the conclusion of the anastomosis, a further 2500 IU heparin was administered subcutaneously, and flap inset was completed with no obvious cause for the previously poor perfusion identified. The patient was haemodynamically stable with blood pressure sufficient for flap perfusion in the postoperative period. A heparin infusion was commenced, and a thrombotic screen and haematology consultation did not reveal any predisposing factors. The patient was discharged on day 13 postoperatively with no signs of flap failure (Figure 4).
The patient was reviewed regularly by the oral and maxillofacial surgery team and demonstrated an excellent and uneventful recovery. At the 12-month postoperative review, the flap appeared to have fully integrated and there were no signs of infection, flap failure or odontogenic myxoma recurrence on cone beam computer tomography imaging. He continued with his schooling and has maintained his nutritional intake with a normal diet.
Microvascular flap surgery provides patients with head and neck surgical defects an option for reconstruction and rehabilitation. The use of alteplase, a fibrinolytic agent, has only been reported in a small number of case studies for use in microvascular flap surgery. To our knowledge, its use has not previously been reported in a fibula free flap reconstruction. This case demonstrates the successful intraoperative use of alteplase in an otherwise systemically well 17-year-old patient for the salvage of his fibula free flap, which repeatedly lost vascular perfusion, as an example of the no-reflow
1 Vila PM, Rich JT, Desai SC. Defining quality in head and neck reconstruction. Otolaryngol Head Neck Surg 2017; 157: 545-547.
2 Khouri RK, Cooley BC, Kunselman AR, et al. A prospective study of microvascular free-flap surgery and outcome. Plast Reconstr Surg 1998; 102: 711-721.
3 Ramjane K, Han L, Jin C. The diagnosis and treatment of the no-reflow phenomenon in patients with myocardial infarction undergoing percutaneous coronary intervention. Exp Clin Cardiol 2008; 13: 121-128.
phenomenon. While the underlying cause was not determined, the administration of intravascular alteplase has proven to be successful, with evidence of complete flap integration 12-months postoperatively.
The failure of a vascularised flap reconstruction is devastating for the patient and surgical team. Therefore, options for flap salvage should be exhausted intraoperatively when there is evidence of flap compromised. This is supported by Khouri and colleagues,2 who report a lower rate of flap failure when flap thrombosis is identified and managed intraoperatively. The initial procedure provides the best visualisation of the surgical field and is the easiest time to identify anatomical structures before postoperative oedema sets in. In instances where efforts such as re-anastomosis and systemic heparin have been unsuccessful, the off-label use of locally applied alteplase can be considered for flap salvage.
Petterson C: Conceptualisation (present during the surgical procedure and scrubbed during the administration of alteplase, initial discussions with Mr Singh regarding writing the case presentation, gained consent from the patient); data curation (requested clinical records from the Medical Records Department); writing original draft (primary author for the original draft including searching and adding the reference articles); editing; reviewing (provided the initial responses to the review points from the review panel); patient management (gained original consent for the article, managed the patient postoperatively as the on-call staff member).
Singh T: Conceptualisation (primary operator for the surgical procedure, provided expert knowledge on head and neck cancer surgery, and offered to supervise the writing of the article); data curation; writing original draft; editing (primary editor after the original draft was created, provided any additional information about the case and expert knowledge on the topic); reviewing (all responses to review points were checked and contributed to as the supervisor); patient management (provides ongoing review of the patient’s progress postoperatively with planned follow-up appointments).
Ananth K: Conceptualisation; data curation (provided the necessary radiological images and clinical data from the onsite computers); formal analysis; methodology; writing original draft (drafted the original case details); editing; reviewing; patient management (remains a staff member within the department and assists with reviews and booking investigations as required).
The patient provided written consent for publication.
All authors declare that they have no conflicts of interest.
4 Boehringer Ingelheim (NZ) Ltd. [Internet]. Actilyse data sheet. 1987. https://www.medsafe.govt.nz/profs/ datasheet/a/Actilyseinj.pdf (viewed Aug 2023).
5 Panchapakesan V, Addison P, Beausang E, et al. Role of thrombolysis in free-flap salvage. J Reconstr Microsurg 2003; 19: 523-530.
6 Askari M, Fisher C, Weniger FG, et al. Anticoagulation therapy in microsurgery: a review. J Hand Surg Am 2006; 31: 836-846.
7 Barhoum F, Tschaikowsky K, Koch M, et al. Successful free flap salvage surgery with off-label use of alteplase:
a case report, review of the literature and our free flap salvage algorithm. Int J Surg Case Rep 2020; 75: 398402.
8 Wimbauer JM, Heinrich KM, Schwaiger K, et al. Anterograde injection of alteplase salvages deep inferior epigastric perforator flap in reconstructive breast surgery. Plast Reconstr Surg Glob Open 2022; 10: 4415.
9 Taqi M, Raju S. Fibula free flaps. 2022. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing, 2024
Shirky D (BDSc(Hons))1; Majid H1; Chin M (BDSc(Hons)) 1; Zachar J (BSc, BDSc(Hons), Grad Dip Clin Dent, MClinDent(Oral Surgery))1; Johnson NR (BDSc(Hons), MBBS, MPhil(Surgery), FRACDS(OMS)) 1,2,3
Desmoplastic fibroma (DF) is a rare benign osseous tumour, representing around 0.1–1% of primary bone tumours.1-3 Despite its benign nature, DF typically presents with aggressive characteristics and is locally destructive.1,2,4,5 Although DM is non-odontogenic in origin, it commonly occurs in the jaws, especially the mandible.1,4,6 DF was first described as a distinct entity in 1958 by Jaffe.7 Its locally aggressive nature without potential for metastasis lead to its classification by the World Health Organization as an “intermediate” desmoid tumour.8
The diagnosis of DF is challenging and requires careful histological analysis. The histological characteristics of DF include proliferation of spindle-shaped fibroblasts and fibroblast-adjacent cells in a uniform arrangement which are enlarged and elongated in a collagenous matrix.5,9,10 The lesion displays variable areas of hyalinisation, and often a whorled or sweeping pattern.5,9,10 Critically, there is minimal mitotic activity within cells, no necrosis, and rare nuclear atypia.5,11,12 A distinction should be made between DF and desmoplastic fibroblastoma (or desmoid-type fibromatosis), which has been thought to be the soft tissue counterpart of DF. Immunohistochemical research has shown differences in tumorigenesis between the two lesions, with DF lacking the b-catenin pathway, suggesting that DF and desmoplastic fibroblastoma are distinct entities.1,13 Radiographically, DF presents with considerable variation, with lesions ranging from poorly defined to well delineated, and from unilocular to multilocular.2,14,15 Cortical perforation into surrounding structures is often present in large lesions.16 Immunohistochemistry and other biochemical investigations have been used frequently in the literature for further information gathering to assist differential diagnosis.17-19 The main challenge in diagnosis is differentiation of DF from fibrosarcoma and osteosarcoma, which contains markers of malignancy, such as cellular pleomorphism and mitotic activity.8,20,21 Other differentials with similar presentations include fibrous dysplasia, simple bone cyst, non-ossifying fibroma, ameloblastoma, metastatic disease, and other tumours.20,22,23
Desmoplastic fibroma (DF) is a rare, benign bone tumour that is locally aggressive, and occurs commonly in the jaws. DF carries significant morbidity and requires histological confirmation for diagnosis. Historically, treatment methods for DF have varied widely, often resulting in high recurrence rates. This systematic review aims to present the clinical and demographic characteristics of DF and examine if there are any differences in recurrence rates following from different treatment modalities.
The PubMed, Embase, Ovid and Scopus databases were systematically searched. Exclusion criteria were applied, resulting in inclusion of 124 case reports and case series. Data from 274 cases were extracted, codified and analysed.
The mean age at diagnosis was 23.3 years, and the most commonly involved site was the mandible. The most common treatment methods were resection, excision and curettage. Curettage alone resulted in high recurrence (54.3%). Resection without continuity defect had the least percentage of recurrence (11.1%), which is still high.
This review summarises the main clinical and demographic characteristics of DF and compares these characteristics between maxillofacial cases and cases in other sites. Based on the findings of this systematic review, it is suggested that, where possible, the preferred method of treating DF should be resection without reconstruction.
The signs and symptoms of DF demonstrate a wide variance throughout the literature. Some patients present with pain, tenderness to palpation of the area of the lesion, or swelling, whereas others are asymptomatic, with detection purely coincidental on routine imaging.6,18,24-26 In the jaw, DF tends to present as an asymptomatic firm mass with gradual growth.14 Its precise aetiological mechanisms
1School of Dentistry, University of Queensland, Brisbane, QLD, Australia; 2Faculty of Medicine, University of Queensland, Brisbane, QLD, Australia; 3Oral and Maxillofacial Department, Princess Alexandra Hospital, Brisbane, QLD, Australia. Corresponding author: Darren Shirky ✉ d.shirky@uq.net.au | doi: 10.63717/2025.MS0032
Keywords: desmoplastic fibroma | maxillofacial tumour | tumour management | recurrence
are yet to be uncovered but it has been posited that genetic factors and trauma play major roles.5 It has often been observed that DF is associated with tumorous conditions such as tuberous sclerosis.27-29
Treatment modalities have included curettage, excision, en bloc resection, and segmental resection, with radiotherapy, chemotherapy, and oxidative therapy as rare adjuncts.2,4,26 Various reconstructive options exist, largely determined by the location of the tumour.4,6,16,30,31 Historically, localised excision has resulted in high recurrence rates, reportedly ranging from 37% to 72%.3,32,33
The first aim of this systematic review is to establish the demographic and clinical features of DF. The second is to compare the characteristics and management of DF cases in the gnathic (or maxillofacial) bones with cases elsewhere in the body. Finally, the systematic review aims to explore how various management modalities affect its recurrence rate. These aims were met by the following objectives:
systematic review of the literature to produce a summary of the features, management, and recurrence of DF in the maxillofacial area and other sites;
compare the above outcomes for maxillofacial cases versus presentation in other bones;
use data reported in the literature to assign a recurrence rate to each treatment method. To date there has been no systematic review on DF, and studies have been limited to case reports and case series. Therefore, a summary of its features is appropriate for categorisation and recognition of the disease. Investigating our second aim will be useful in identifying possible differences in the characteristics of DF in the maxillofacial region compared with other sites, and how these differences may inform management options. Data of how different surgical treatment methods affect recurrence rate will allow a more informed recommendation to be made to surgeons on the most appropriate management of DF.
Information sources and search strategy
A search strategy was used across the PubMed, Embase, Scopus and Ovid databases,
on page 46)
1. Demographic and treatment data of desmoplastic fibroma cases
Table 2. Recurrence rate (Continued
using the following filters: publishing dates from 1990 to present (due to advances in diagnostic and surgical techniques), language (English), and human studies. Removal of duplicates, screening by title and abstract, and assessment of the full text was done according
to the exclusion criteria below. The sample search strategy is available from the authors on request.
This review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) protocol to guide the review process and maximise reliability.34 It was registered with the International Prospective Register of Systematic Reviews (PROSPERO) in November 2022 (identification number 368938).
Our study includes two sets of exclusion criteria. One set is for studies used in the summarisation of the treatment, demographic, histological and clinical features of DF. These criteria are duplicate studies, non-full text publications, non-English language studies, and studies with insufficient demographic, histopathologic or treatment data. The exclusion criteria for studies included in analysis of treatment and recurrence are as above, plus insufficient data on recurrence, or a follow-up period of less than one year. The minimum one-year follow-up period was necessary to allow enough bone healing time in order to determine recurrence.
Data extraction was carried out by two reviewers working independently (DS, HM). A third reviewer checked over the data for reliability (MC).
The primary variables of interest were site, treatment method, and recurrence of DF.
Site: This variable was determined according to which specific bone the tumour occurred in (Table 1 and Table 2). Bones that are classified as maxillofacial include the mandible, maxilla, and zygomatic bone.
Treatment method: Treatment methods were classified according to level of invasiveness, as detailed in Table 1
“Resection” was defined as tumour removal with a wide margin of healthy tissue. “Resection with continuity defect” refers to a surgical defect that results in loss of continuity of the bone. “Resection without continuity defect” refers to a surgical defect where bone continuity was maintained (ie, marginal resection). “Excision” was defined as full tumour removal without wide margins.
Recurrence: Recurrence was defined as a repeat diagnosis of DF after treatment of the original tumour, in the same location
as the previous tumour. A follow-up period of at least one year was necessary for cases to be categorised as having either “recurrence” or “no recurrence”, due to bone turnover and healing times post-reconstructive surgery. Tumours that underwent malignant change were categorised separately.
Secondary variables of interest were age, sex, histology, reconstruction, and dental rehabilitation. Age was classified as less than 25 years, 25–50 years, greater than 50 years, and not stated.
The extracted data were input into a Microsoft Excel spreadsheet and then codified by two reviewers and verified by a third. The codified data were then imported into Jamovi (Version 2.3 13.0) to carry out a quantitative analysis.
The risk of bias in the included studies were assessed using the Joanna Briggs Institute (JBI) 2020 Checklist for Case Reports.35 The risk of bias analysis was carried out by two reviewers working independently (MC, DS).
Data analysis took the form of descriptive statistics. Data from the studies that met the exclusion criteria for treatment, demographic, and clinical features were tabulated and stratified by location (maxillofacial v other sites) to allow for comparison (Synthesis 1). The effect measure used for all outcomes was percentage of the frequencies of occurrence.
Data from studies with sufficient information on follow-up and recurrence were also tabulated, and a recurrence rate was assigned to each treatment method (expressed as the percentage of cases with recurrence for each treatment option). Recurrence rates were then compared for each treatment method (Synthesis 2). The dataset was checked for entry errors by obtaining univariate summary tables.
Inferential statistics was considered for additional analysis of recurrence rate, using the c2 test to test for significant association between treatment method and recurrence. However, the dataset did not meet some of the key assumptions of the c2 test, such as the expected frequency (count of at least 5 in 80% of cells). Consequently, our analysis was limited to descriptive statistics.
The study selection process identified 546 records after applying the appropriate filters (Figure 1). Of these, 323 duplicates were removed. Screening by title and abstract excluded a further 86 records. All but one of the remaining 137 studies were retrieved, and full text assessment resulted in exclusion of ten more studies. The 124 studies included in this review were further assessed for inclusion in Synthesis 1 or 2. A total of 32 studies were selected for Synthesis 1 alone, and the remaining 92 were included in both Syntheses.
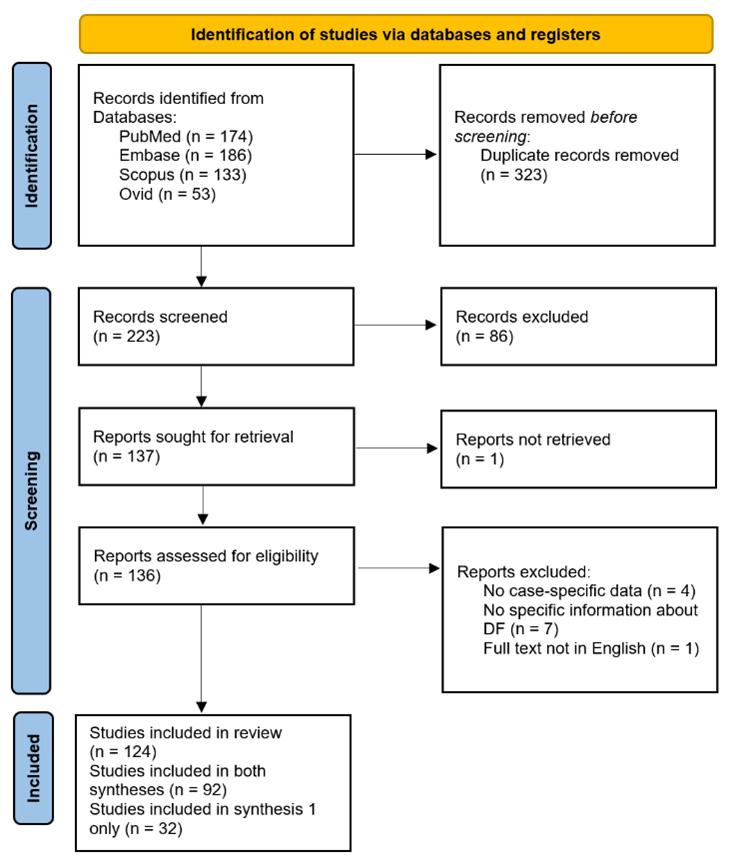
DF = desmoplastic fibroma.
Figure 1. Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) flow diagram of study selection
All included studies were case reports (n = 103) and case series (n = 21), with a total of 274 individual cases.1-6,9-33,36-130 Fifty-two of the studies featured DF of the maxillofacial area, and the other 73 addressed DF cases in other sites.1-6,9-33,36-130 Of these, 92 studies containing 202 cases met the requirements for inclusion in recurrence rate calculation (Synthesis 2).1,3-6,10,12,14,18-20,23-30,32,33,37,39-49,5154,56-64,66-68,70-82,84-87,89-93,98,101-107,109,111-113,116,117,121-128 Details and results of each separate study are available from the authors on request.
The 124 included studies were assessed for risk of bias using the JBI Critical Appraisal Checklist for Case Reports. Overall, good reliability was achieved, and inter-rater reliability was consistent. The data articles and data extracted matched the criteria of the JBI tool. The excluded articles using the JBI tool were consistent with the exclusion criteria. Detailed results of risk of bias for each study is available on request from the authors.
Results of syntheses: demographic and treatment data
The pooled demographic and treatment data are recorded in Table 1 More than half the cases (55.9%) were in the 0–24 years age group (Table 1). The mean age of cases with DF in the maxillofacial region was 17.6 years, while the mean age for cases in other sites was 27.2
years. The overall average age was 23.3 years. Sex was roughly evenly distributed, with 50.4% overall being female. Maxillofacial cases were 57.7% female (Table 1). The mandible was the most commonly involved site, followed by femur, radius, spine, skull, and pelvis respectively (Table 1). The most common treatment methods were resection with or without continuity defects (41.2%), excision (16.9%), and curettage (16.2%). Other treatment methods were rare (6.7% total).
The percentage of recurrence (or recurrence rate) is shown in Table 2. Where more than one treatment or recurrence occurred in the same patient, each was counted separately for the purposes of this analysis. Curettage alone had the highest recurrence (54.3%), followed by curettage with adjunct (25.0%), excision (19.0%), resection with continuity defect (13.7%) and resection without continuity defect (11.1%) (Table 2). Other treatment methods had a very low number of cases and had a recurrence rate of 0.0%.
This review consolidates much of the published demographic data of patients with DF, as well as its clinical features. These data are beneficial for a more complete understanding of the disease, and for communication between surgeons and patients with DF.
Our results indicate that most cases of DF are diagnosed in the first three decades of life, as previously suggested.1,2 Maxillofacial cases had a somewhat younger demographic, with 68.3% of patients in the under 25 years age bracket. Only 48.5% of non-maxillofacial cases were in patients aged under 25 years. There were still a significant number of cases in older patients, with 12.9% of individuals aged over 50 years. Age at diagnosis ranged from under one year to 77 years. Sex distribution was even overall (50.4% female). Maxillofacial cases showed a slight female predilection (57.7%), and other cases were 53.3% male.
By far, the most commonly involved site was the mandible, with more than twice the number of cases as the second most common (femur), and six times more than the maxilla. Although, as observed by other authors, long bones were commonly involved, DF was roughly as common in other bone types, notably the pelvis, vertebrae, and bones of the skull.55,81 It should be noted that publication bias prioritising the publication of rare DF presentations may have affected these values.
All the cases considered for the analyses carried out histological confirmation of DF prior to diagnosis. This reflects the non-specific clinical and radiological presentations of DF, and highlights the importance of biopsy and histological examination before definitive treatment.
Of the treatment methods, curettage showed the least efficacy, with over half of cases experiencing recurrence (54.3%). The addition of adjunct measures (such as radiotherapy and cryotherapy) to curettage reduced recurrence to 25.0%. Excision showed a moderately higher recurrence rate (19.0%) than resection with
continuity defect (13.7%) and resection without continuity defect (11.1%). These results are consistent with the literature, which reports a high recurrence following curettage.1,2,93,104 Curettage may still remain a viable treatment option in patients where extensive surgery is not an option, or where resection without reconstruction would result in extreme morbidity. In these cases, adjunct measures can be considered to reduce recurrence.
Maxillofacial cases showed a significantly lower rate of recurrence (9.0%) compared with other cases (19.0%). This result is consistent with the finding that curettage was much more common in other cases (23.8%) than maxillofacial cases (4.5%). Three studies documented cases in which DF recurred as malignant osteosarcoma, highlighting the need for continued careful monitoring following treatment.40,71,105 Many studies did not include information about reconstruction following surgery. It was found that 29.7% of maxillofacial cases underwent reconstruction, with only 8.7% having recorded dental rehabilitation; and 39.4% of other cases recorded some kind of reconstruction.
Adjunct treatments such as radiotherapy and chemotherapy were rarely used alone. In such cases, these treatments were considered appropriate due to patient factors, such as unacceptable morbidity following resection or inability to tolerate surgery.32,94,96 The role of chemotherapeutics such as denosumab and antiangiogenics was also discussed in one study.125 Further studies could investigate the role of adjunct measures, such as radiotherapy and chemotherapeutics, to allow for a more robust conclusion on the use of these agents.
There are limitations present with this study due to the quality of the evidence being reviewed, and the type of analysis used. Since the studies included in this review are all case reports and case series, the evidence comes with a lack of generalisability.131 There is also a risk of selection bias being present in the articles reviewed.131 Although the JBI appraisal tool was used to minimise bias, the sources listed may still somewhat affect the conclusions of this review. Since DF is a rare disease, a small case sample size is another limitation. As this article was limited to descriptive analysis, there is a risk of subjectivity and lack of precision in estimating the effect size and statistical significance in the findings of this study.132 Despite these limitations, we believe that the conclusions of our study will be as strong as possible given the available literature and the rareness of DF.
This review presents the overall demographic and clinical characteristics of DF, and some of the differences in these characteristics between maxillofacial and other cases. Through this systematic review, it is evident that the best recommendation from the current data available is to surgically manage the DF lesion by resection followed by full reconstruction and rehabilitation. Due to the high recurrence rates following curettage, it is recommended that it be avoided in DF treatment. Where this is not possible, adjunct measures may lessen the chance of recurrence following curettage. Future research should allow adequate follow-up periods and include data on reconstruction.
Editor’s note
The challenges in diagnosis and management of desmoplastic fibroma are well illustrated in the following article: Daniel F, Tocaciu S, Barrowman R, et al. Recurrent desmoplastic fibroma of the maxilla: case report and review of the literature. Australasian Journal of Oral and Maxillofacial Surgery 2024; 1: 63-67.
Author contributions
Shirky D: Data curation, methodology, formal analysis, writing original draft, review and editing.
Majid H: Data curation, methodology, formal analysis, writing original draft.
Chin M: Data curation, methodology, formal analysis, writing original draft.
Zachar J: Formal analysis, review and editing.
Johnson NR: Conceptualisation, review and editing.
1 Woods TR, Cohen DM, Islam MN, et al. Desmoplastic fibroma of the mandible: a series of three cases and review of literature. Head Neck Pathol 2015; 9: 196-204.
2 Shekhar MG, Reddy RS, Ravikanth M, et al. Desmoplastic fibroma of the mandible: case report and review of literature. Prim Dent Care 2011; 18: 115-118.
3 Evans S, Ramasamy A, Jeys L, Grimer R. Desmoplastic fibroma of bone: a rare bone tumour. J Bone Oncol 2014; 3: 77-79.
4 Khatib B, Pogrel MA. Desmoplastic fibroma of the mandible in young children-a case series. Int J Oral Maxillofac Surg 2017; 46: 173-180.
5 Mir-Mari J, Aguirre-Urizar JM, Berini-Aytes L, Gay-Escoda C. Giant desmoplastic fibroma in the anterior zone of the maxilla. J Craniofac Surg 2011; 22: 2350-2353.
6 Nishida J, Tajima K, Abe M, et al. Desmoplastic fibroma. Aggressive curettage as a surgical alternative for treatment. Clin Orthop Relat Res 1995: 142-148.
7 Jaffe HL. Tumors and tumorous conditions of the bones and joints. Cancer 1959; 12: 210.
8 Schajowicz F, World Health Organization. Histological typing of bone tumours. Berlin: Springer-Verlag, 1993.
9 Nithya S, Sundaravel S, Uppala D, Rao K. Desmoplastic fibroma — a rare case report. J Oral Maxillofac Pathol 2015; 19: 270.
10 Joshua B-Z, Silberstein E, Diomin V, Bodner L. Desmoplastic fibroma of the mandible associated with pathological fracture in a pediatric patient. Int J Ped Oto 2014; 9: 60-63.
11 Cho BH, Tye GW, Fuller CE, Rhodes JL. Desmoplastic fibroma of the pediatric cranium: case report and review of the literature. Childs Nerv Syst 2013; 29: 2311-2315.
12 Ferri A, Leporati M, Corradi D, et al. Huge desmoplastic fibroma of the paediatric mandible: surgical considerations and follow-up in three cases. J Craniomaxillofac Surg 2013; 41: 367-370.
13 Hauben EI, Jundt G, Cleton-Jansen AM, et al. Desmoplastic fibroma of bone: an immunohistochemical study including beta-catenin expression and mutational analysis for betacatenin. Hum Pathol 2005; 36: 1025-1030.
14 Haney J, Olson PN, Griffiths HJ. Radiologic case study. The clinical and radiologic features of desmoplastic fibroma of bone. Orthopedics 1994; 17: 77, 80-85, 88.
15 Azola AM, Wartmann CT, et al. Desmoplastic fibroma arising from the anterior maxillary sinus in a child. Arch Otolaryngol Head Neck Surg 2012; 138: 859-862.
16 Suarez-Soto A, Baquero-Ruiz de la Hermosa MC, Minguez-Martínez I, et al. Management of fibro-osseous lesions of the craniofacial area. Presentation of 19 cases
All authors declare that they have no conflicts of interest.
and review of the literature. Med Oral Patol Oral Cir Bucal 2013; 18: e479-e485.
17 Vargas-Gonzalez R, San Martin-Brieke W, Gil-Orduña C, Lara-Hernandez F. Desmoplastic fibroma-like tumor of maxillofacial region associated with tuberous sclerosis. Pathol Oncol Res 2004; 10: 237-239.
18 Böhm P, Kröber S, Greschniok A, et al. Desmoplastic fibroma of the bone. A report of two patients, review of the literature, and therapeutic implications. Cancer 1996; 78: 1011-1023.
19 Aggarwal S, Gopinathan NR, Dhillon MS, Viswanathan VK. Diaphyseal desmoplastic fibroma of humerus — report of a rare presentation. BMJ Case Rep 2012; bcr1020114954.
20 Wolfe SQ, Cervantes L, Olavarria G, et al. Desmoplastic fibroma of the pediatric skull. Report of three cases. J Neurosurg 2005; 103 (Suppl): 362-365.
21 Takazawa K, Tsuchiya H, Yamamoto N, et al. Osteosarcoma arising from desmoplastic fibroma treated 16 years earlier: a case report. J Orthop Sci 2003; 8: 864-868.
22 Nedopil A, Raab P, Rudert M. Desmoplastic fibroma: a case report with three years of clinical and radiographic observation and review of the literature. Open Orthop J 2013; 8: 40-46.
23 Deniz K, Ceylan D. Desmoplastic fibroma of the skull. Acta Neurochir (Wien) 2008; 150: 285-290.
24 González MR, Bryce-Alberti M, Subhawong T, et al. Intramedullary fixation with a short nail in a young patient presenting with a pathological proximal femur fracture. J Am Acad Orthop Surg Glob Res Rev 2021; 5: e21.00055- e21.00057.
25 Ishizaka T, Susa M, Sato C, et al. Desmoplastic fibroma of bone arising in the cortex of the proximal femur. J Orthop Sci 2021; 26: 306-310.
26 Hopkins KM, Huttula CS, Kahn MA, Albright JE. Desmoplastic fibroma of the mandible: review and report of two cases. J Oral Maxillofac Surg 1996; 54: 1249-1254.
27 Espinoza-Coronado AM, Loyola-Rodríguez JP, OlveraDelgado JH, et al. Desmoplastic fibroma recurrence associated with tuberous sclerosis in a young patient. Case Rep Dent 2018; 18: 1370184.
28 Miyamoto Y, Satomura K, Rikimaru K, Hayashi Y. Desmoplastic fibroma of the mandible associated with tuberous sclerosis. J Oral Pathol Med 1995; 24: 93-96.
29 Fahmy MD, Gupta A, Padilla RJ, et al. Desmoplastic fibroma associated with tuberous sclerosis: case report and literature review. Oral Surg Oral Med Oral Pathol Oral Radiol 2019; 128: e92-e99.
30 Iatrou IA, Theologie-Lygidakis N, Leventis MD. Case report: desmoplastic fibroma of the mandible in a child presenting with TMJ dysfunction. Eur Arch Paediatr Dent 2008; 9: 105-108.
31 Boon LC, Phaik KS, Khanijow V. Desmoplastic fibroma: report of a case with proliferative myositis. Ann Dent 1991; 50: 28-32.
32 Inwards CY, Unni KK, Beabout JW, Sim FH. Desmoplastic fibroma of bone. Cancer 1991; 68: 1978-1983.
33 Stefanidis K, Benakis S, Tsatalou E, et al. Computed tomography and magnetic resonance imaging of desmoplastic fibroma with simultaneous manifestation in two unusual locations: a case report. J Med Case Rep 2011; 5: 28.
34 Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009; 6: e1000097.
35 Moola S, Munn Z, Tufanaru C, et al. Chapter 7: Systematic reviews of etiology and risk. In: Aromataris E, Munn Z; editors. Joanna Briggs Institute reviewer’s manual. The Joanna Briggs Institute, 2017. https://synthesismanual.jbi. global (viewed Nov 2022).
36 Kwee TC, de Klerk JMH, Nix M, et al. Benign bone conditions that may be FDG-avid and mimic malignancy. Semin Nucl Med 2017; 47: 322-351.
37 Smith ML, Williams JK, Gruss JS. Desmoplastic fibroma of the zygoma. Plast Reconstr Surg 1999; 103: 1964-1969.
38 Nisha S, Chetana C, Ranjini K, Adarsh K. Desmoplastic fibroma of the mandible with unusual histopathological features. Indian J Pathol Microbiol 2021; 64: 548-552.
39 Taconis WK, Schutte HE, van der Heul RO. Desmoplastic fibroma of bone: a report of 18 cases. Skeletal Radiol 1994; 23: 283-288.
40 Vally IM, Altini M. Fibromatoses of the oral and paraoral soft tissues and jaws. Review of the literature and report of 12 new cases. Oral Surg Oral Med Oral Pathol 1990; 69: 191-198.
41 Summa A, Cerasti D, Crisi G, et al. Desmoplastic fibroma of the mandible: usefulness of CT and MR imaging in diagnosis and treatment. A case report. Neuroradiol J 2010; 23: 109-113.
42 Sandrini FA, do Egito Vasconcelos BC, Bessa-Nogueira RV. Desmoplastic fibroma of mandible in a child: case report. Indian J Surg 2007; 69: 254-256.
43 Wippold FJ, White FV, Jamroz G, et al. Desmoplastic fibroma of the mandible in an infant. Pediatr Radiol 2005; 35: 906-909.
44 Averna R, De Filippo M, Ferrari S, et al. Desmoplastic fibroma of the mandible. Acta Biomed 2011; 82: 69-73.
45 Cupero TM, Thomas RW, Manning SC. Desmoplastic fibroma of the maxillary sinus. Otolaryngol Head Neck Surg 2001; 125: 661-662.
46 Jamali M, Lazow SK, Solomon MP, Berger J. Desmoplastic fibroma: report of rare lesion in unusual craniofacial location. N Y State Dent J 2013; 79: 43-45. Erratum in: N Y State Dent J 2013; 79: 13.
47 Christiansen RL. Desmoplastic fibroma of the ramus and body of the mandible. Cranio 1990; 8: 271-275.
48 Cranin AN, Gallo L, Madan S. Desmoplastic fibroma. A rare oral tumor in children. N Y State Dent J 1994; 60: 34-39.
49 Skinner HR, Vargas A, Solar A, et al. Desmoplastic fibroma of the mandible in a pediatric patient: a case report of resection and Reconstruction with a six-year follow-up. J Oral Max Surg 2017; 75: 1568.e1-1568.e10.
50 Gersak MM, Lenghel LM, Baciut G, et al. Ultrasonography of desmoplastic fibroma of the mandible; a case report. Med Ultrason 2015; 17: 407-410.
51 Flucke U, Tops BB, van Diest PJ, Slootweg PJ. Desmoidtype fibromatosis of the head and neck region in the paediatric population: a Clinicopathological and genetic study of seven cases. Histopath 2013; 64: 769-776.
52 Gondak RO, Corrêa MB, da Costa MV, et al. Maxillary desmoplastic fibroma with initial symptoms suggestive of sinusitis. Oral Surg Oral Med Oral Pathol 2013; 116: e510-e513.
53 Tandon S, Garg RK. Intraoral desmoplastic fibroma: a manifestation of tuberous sclerosis. Fetal Pediatr Pathol 2012; 31: 195-201.
54 Schneider M, Zimmermann AC, Depprich RA, et al. Desmoplastic fibroma of the mandible — review of the literature and presentation of a rare case. Head Face Med 2009; 5: 25.
55 Reid EN, Lawoyin DO, Suresh L, Longwe E. Desmoplastic fibroma of the anterior mandible. Case report and review of literature. N Y State Dent J 2009; 75: 32-33.
56 Shi H, Wang P, Wang S, Yu Q. Desmoplastic fibroma of the mandible. Dentomaxillofac Radiol 2008; 37: 408-411.
57 Troulis MJ, Williams WB, Kaban LB. Staged protocol for resection, skeletal reconstruction, and oral rehabilitation of children with jaw tumors. J Oral Maxillofac Surg 2004; 62: 335-343.
58 Said-Al-Naief N, Fernandes R, Louis P, et al. Desmoplastic fibroma of the jaw: a case report and review of literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006; 101: 82-94.
59 Bakaeen G, Rajab LD. Desmoplastic fibroma of the mandible: report of a case. Int J Paediatr Dent 1999; 9: 117-121.
60 Templeton K, Glass N, Young SK. Desmoplastic fibroma of the mandible in a child: report of a case. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1997; 84: 620-623.
61 Iwai S, Matsumoto K, Sakuda M. Desmoplastic fibroma of the mandible mimicking osteogenic sarcoma: report of a case. J Oral Maxillofac Surg 1996; 54: 1370-1373.
62 Dhaif D, Satir AA, Sharif S. Desmoplastic fibroma of the mandible: a 5 year follow-up. Bahrain Med Bull 2008; 30: 180-184.
63 Karimi A, Derakhshan S, Moradzadeh Khiavi M, et al. Desmoplastic fibroma of the jaws: a case series and review of literature. Iran J Pathol 2020; 15: 134-143.
64 Konikoth S, Bose T, Anupama I, Yogidas R. Desmoplastic fibroma of the mandible – a rare benign tumor mimicking malignancy. J Indian Acad Oral Med Radiol 2019; 31: 74.
65 Kahraman D, Karakoyunlu B, Karagece U, et al. Desmoplastic fibroma of the jaw bones: a series of twenty-two cases. J Bone Oncol 2020; 26: 100333.
66 Makita H, Hatakeyama D, Yonemoto K, et al. A case of desmoplastic fibroma occurring at the mandible: serial observations suggesting the successful effects of antihistamine agent and interaction of estrogen hormone. J Oral Maxillofac Surg Med Pathol 2017; 29: 275-280.
67 Guruprasad Y, Chauhan D. Desmoplastic fibroma of mandible. J Cranio-Max Dis 2013; 2: 93.
68 Gonçalves FLN, de Oliveira JI, Gonçalves PFS, et al. A rare case of desmoplastic fibroma. Spontaneous mandibular regeneration with 3 years follow up — case report. Indian J Otolaryngol Head Neck Surg 2022; 74 (Suppl): 45624564.
69 Titidej A, Jolehar M. Rare desmoplastic fibroma in Ramus and mandibular angle: Presentation of a case report with review of literature. Acta Medica Iranica 2020; 57: 456-460.
70 Kadowaki H, Oyama Y, Nishida H, et al. A case of desmoplastic fibroma of bone with CTNNB1 point mutation. Oral Surg Oral Med Oral Pathol Oral Radiol 2020; 129: e230-e233.
71 Min HS, Kang HG, Lee JH, et al. Desmoplastic fibroma with malignant transformation. Ann Diagn Pathol 2010; 14: 50-55.
72 Moorjani V, Stockton V. Desmoplastic fibroma with perineural extension. AJR Am J Roentgenol 2005; 185: 1498-1499.
73 Herford AS, Reder P, Ducic Y. Multifocal desmoplastic fibromas of the mandible. J Oral Maxillofac Surg 2001; 59: 1078-1081.
74 Yin H, Zhang D, Wu Z, et al. Desmoplastic fibroma of the spine: a series of 12 cases and outcomes. Spine J 2014; 14: 1622-1628.
75 Sferopoulos NK. Periosteal desmoplastic fibroma of the tibia in a 3-year-old child. Eur J Orthop Surg Traumatol 2015; 25: 1233-1238.
76 Celli P, Cervoni L, Trillò G. Desmoplastic fibroma of the skull. Case report and review of the literature. Neurochirurgie 1997; 43: 260-264.
77 Bernstein ML, Chung KC. Desmoplastic fibroma of the hand: case report. J Hand Surg Am 2008; 33: 1405-1408.
78 Shinomiya K, Furuya K, Mutoh N. Desmoplastic fibroma in the thoracic spine. J Spinal Disord 1991; 4: 229-233.
79 Jamshidi K, Bagherifard A, Mirzaei A. Desmoplastic fibroma versus soft-tissue desmoid tumour of forearm: a case series of diagnosis, surgical approach, and outcome. J Hand Surg Eur Vol 2017; 42: 952-958.
80 Callahan KS, Eberhardt SC, Fechner RE, Cerilli LA. Desmoplastic fibroma of bone with extensive cartilaginous metaplasia. Ann Diagn Pathol 2006; 10: 343-346.
81 Koba T, Susa M, Nakayama R, et al. Desmoplastic fibroma arising in the distal phalanx of the great toe: a case report. J Foot Ankle Surg 2014; 53: 71-74.
82 Stevens J, Moin S, Salter D, Patton JT. Desmoplastic fibroma: a rare pathological midshaft femoral fracture treated with resection, acute shortening, and relengthening: a case report. JBJS Case Connect 2019; 9: e0022.
83 Okubo T, Saito T, Takagi T, et al. Desmoplastic fibroma of the scapula with fluorodeoxyglucose uptake on positron emission tomography: a case report and literature review. Int J Clin Exp Pathol 2013; 6: 2230-2236.
84 Koiso T, Muroi A, Yamamoto T, et al. Desmoplastic fibroma of the pediatric cranium: an aggressive skull tumor with local recurrence. Neurol Med Chir 2016; 56: 85-88.
85 Daneyemez M, Akay KM, Izci Y. Desmoplastic fibroma of the cervical spine. Eur Spine J 2005; 14: 799-802.
86 Yoon SH, Kim SH, Shin YS, et al. Desmoplastic fibroma of the skull in an infant. Childs Nerv Syst 2006; 22: 176-181.
87 Bell SW, Young PS, Mahendra A. Primary bone tumours of the talus: the Scottish Bone Tumour Registry experience. Foot Ankle Surg 2012; 18: 277-282.
88 Lau D, Yarlagadda J, Jahan T, et al. Desmoplastic fibroma of the spine causing severe mediastinal compression and brachial plexus encasement: report of 2 cases. J Neurosurg Spine 2013; 19: 515-520.
89 Goldberg AN, Janecka IP, Sekhar LN. Desmoplastic fibroma of the skull: a case report. Otolaryngol Head Neck Surg 1995; 112: 589-591.
90 Rastogi S, Varshney MK, Trikha V, et al. Desmoplastic fibroma: a report of three cases at unusual locations. Joint Bone Spine 2008; 75: 222-225.
92 Mahnken AH, Nolte-Ernsting CC, Wildberger JE, et al. Cross-sectional imaging patterns of desmoplastic fibroma. Eur Radiol 2001; 11: 1105-1110.
93 Xie HQ, Huang FG, Zhao YF, et al. Tissue-engineered ribs for chest wall reconstruction: a case with 12-year followup. Regen Med 2014; 9: 431-436.
94 Sanfilippo NJ, Wang GJ, Larner JM. Desmoplastic fibroma: a role for radiotherapy? South Med J 1995; 88: 1267-1269.
95 Settle WJ, Ebraheim NA, Coombs R, et al. CT-guided biopsy of metastatic sacral tumors. Orthopedics 1990; 13: 753-758.
96 Nag HL, Kumar R, Bhan S, et al. Radiotherapy for desmoplastic fibroma of bone: a case report. J Orthop Surg (Hong Kong) 2003; 11: 90-93.
97 Juergens KU, Bullmann V, Link TM, et al. Desmoplastic fibroma in the thoracic spine: an unusual localization of a rare primary bone tumor. Eur Radiol 2001; 11: 273-275.
98 Opdenakker Y, Swennen G, Abeloos J. Application of a non-invasive reference headband and a surgical splint for intraoperative paediatric navigation. Int J Oral Maxillofac Surg 2017; 46: 360-362.
99 Savy JM, Laredo JD, Prier A, et al. Case report 728: desmoplastic fibroma. Skeletal Radiol 1992; 21: 388-391.
100 George A, Srivastava VM, Sundararaj GD. Desmoplastic fibroma of the proximal ulna. Australas Radiol 1997; 41: 199-200.
101 Clayer M, Oakeshott R. Allograft bone in the treatment of desmoplastic fibroma. A case report. Clin Orthop Relat Res 1994; 300: 219-224.
102 Raatikainen TK, Kaarela OI, Holmström T, et al. Desmoplastic fibroma of the calcaneus treated with a microvascular bone graft. Case report. Scand J Plast Reconstr Surg Hand Surg 1999; 33: 111-116.
103 Boyd J, Jonard B, Weiner S. Desmoplastic fibroma in the distal humerus of a 14-year-old boy: a case report. JBJS Case Connect 2019; 9: e0155.
104 Lans J, Chebib IA, Castelein RM, et al. Reconstruction of the proximal aspect of the radius after desmoplastic fibroma resection: a case report. JBJS Case Connect 2019; 9: e12.
105 Abdel Rahman M, Elgebeily M, El Masry AM, Ishak SE. Desmoplastic fibroma of the tibia: review of the literature and case presentation of an unusual huge lesion. Current Ortho Pract 2019; 30: 112-116.
106 Xu Y, Wang Y, Yan J, et al. Desmoplastic fibroma of the femur with atypical image findings: a case report. Medicine (Baltimore) 2018; 97: e13787.
107 Park JW, Kang HG, Lim KM, et al. Three-dimensionally printed personalized implant design and reconstructive surgery for a bone tumor of the calcaneus: a case report. JBJS Case Connect 2018; 8: e25.
108 Ma XN, Qiang S, Liu TY, et al. Massive rare desmoplastic fibroma of the ilium and ischium in a young adult: a case report. Medicine (Baltimore) 2017; 96: e8962.
109 Majumder A, Gupta S, Friedman P, Isaacson B. Desmoplastic fibroma of the temporal bone. Otol Neurotol 2015; 36: e119-e120.
110 Zhang F, Ni B, Zhao L, et al. Desmoplastic fibroma of the cervical spine: case report and review of the literature. Spine (Phila PA 1976) 2010; 35: 667-671.
111 Hardes J, Gosheger G, Halm H, et al. Three-level en bloc spondylectomy for desmoplastic fibroma of the thoracic spine: a case report. Spine (Phila PA 1976) 2003; 28: e169-e172.
112 Kamimura M, Itoh H, Kinoshita T, et al. Thoracic epidural desmoplastic fibroma. J Spinal Disord 2000; 13: 267-270.
113 Pensak ML, Nestok BR, Van Loveren H, Shumrick KA. Desmoplastic fibroma of the temporal bone. Am J Otol 1997; 18: 627-631.
114 Okubo T, Saito T, Takagi T, et al. Desmoplastic fibroma of the rib with cystic change: a case report and literature review. Skeletal Radiol 2014; 43: 703-708.
91 de Tomas-Cabrera AR, Marcial-Seoane RA, Marcial-Rojas RA. Desmoplastic fibroma of bone: report of one case and review of the literature. Bol Asoc Med P R 1990; 82: 18-24.
115 Armanasco P, Ali S, John L, Williamson D. A rare tumour in a rare location: desmoplastic fibroma in a toe. Foot Ankle Surg 2011; 17: e37-e39.
116 Lath R, Ranjan A, Ratnam BG, Gowrishankar S. Desmoplastic fibroma of the frontal bone. Neurol India 2006; 54: 314-315.
117 Kendi TK, Erakar A, Saglik Y, et al. Desmoplastic fibroma of bone: case report. Clin Imaging 2003; 27: 200-202.
118 Rabin D, Ang LC, Megyesi J, et al. Desmoplastic fibroma of the cranium: case report and review of the literature. Neurosurgery 2003; 52: 950-954; discussion 954.
119 Barbashina V, Karabakhtsian R, Aisner S, et al. Desmoplastic fibroma of the rib. Arch Pathol Lab Med 2002; 126: 721-722.
120 Dutt SN, Mirza S, Irving RM, Jones EL. Desmoplastic fibroma of the temporal bone. J Laryngol Otol 2000; 114: 314-317.
121 Kocher MS, Gebhardt MC, Mankin HJ. Reconstruction of the distal aspect of the radius with use of an osteoarticular
allograft after excision of a skeletal tumor. J Bone Joint Surg Am 1998; 80: 407-419.
122 Abdelwahab IF, Klein MJ, Hermann G, et al. Osteosarcoma arising in a desmoplastic fibroma of the proximal tibia. AJR Am J Roentgenol 2002; 178: 613-615.
123 Li J, Jiao Y, Guo Z, et al. Comparison of osteoarticular allograft reconstruction with and without the SauvéKapandji procedure following tumour resection in distal radius. J Plast Reconstr Aesthet Surg 2015; 68: 995-1002.
124 De Vita A, Vanni S, Miserocchi G, et al. A rationale for the activity of bone target therapy and tyrosine kinase inhibitor combination in giant cell tumor of bone and desmoplastic fibroma: translational evidences. Biomedicines 2022; 10: 372.
125 Gao S, Cai Q, Yao W, et al. Desmoplastic (collagenous) fibroma of the femur: a case report and review of the literature. Oncol Lett 2013; 6: 1285-1288.
126 Goyal T, Rastogi S, Tripathy SK. Desmoplastic fibroma of ulna: excision and reconstruction of olecranon with a fibular graft. Indian J Orthop 2013; 47: 207-210.
127 Rui J, Guan W, Gu Y, Lao J. Treatment and functional result of desmoplastic fibroma with repeated recurrences in the forearm: a case report. Oncol Lett 2016; 11: 1506-1508.
128 Tanwar YS, Kharbanda Y, Rastogi R, Singh R. Desmoplastic fibroma of bone: a case series and review of literature. Indian J Surg Oncol 2018; 9: 585-591.
129 Yokouchi M, Ueno Y, Nagano S, et al. Extended curettage and heat ablation for desmoplastic fibroma of the distal femur with a 12-year follow-up period: a case report. Oncol Lett 2014; 8: 1103-1106.
130 Kato MG, Varadarajan VV, Rivera AC, Mattingly JK. Desmoplastic fibroma of the temporal bone. Otolaryngol Case Rep 2021; 20: 100326.
131 Nissen T, Wynn R. The clinical case report: a review of its merits and limitations. BMC Res Notes 2014; 7: 264.
132 Murad MH, Sultan S, Haffar S, Bazerbachi F. Methodological quality and synthesis of case series and case reports. BMJ Evid Based Med 2018; 23: 60-63.
The ANZAOMS 2025 Annual Scientific Meeting will be held in the beautiful City of Adelaide in South Australia. The 2025 ASM promises to deliver an engaging and thoughtprovoking scientific program alongside a dynamic exhibition and social program.

Professor Krishnamurthy














eoplewhohavemissingteethmaybenefitfromtechniquesthatallowartificialteeth to be implanted firmly in jaw bone. These techniques range from replacing one missingtoothtoreplacingmostteethintheupperandlowerjaws.Dentalimplants have become a common treatment and an important part of modern dentistry over the past30years.Millionsofpeoplearoundtheworldhavehadavarietyofdentalimplants. Asshowninthefigure(right),thebasicstructureconsistsoftheimplantandthedental prosthesis.
Implant: Animplantisinsertedintothe jawbonetoprovideabaseforsupporting andattachingtheprosthesis.
Prosthesis: A prosthesis is an artificial tooth, or row of artificial teeth, attached to the implant. The prosthesis may be a “crown”toreplaceonemissingtoothora “bridge”toreplaceseveralmissingteeth.




In a jaw with no teeth, the





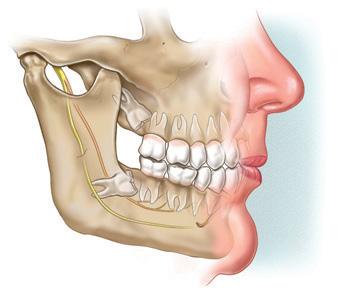
ASK YOUR SURGEON
Important:Fillinalldetailsonthestickerbelow. thispeelitoff,andputitonthepatient'smedicalhistoryorcard.Thiswillremindyouandyourpatientthat pamphlethasbeengiventothepatient.Somesurgeonsasktheirpatientstosignthesticker.
ConsumerandCarerFeedback:Toprovidefeedbackaboutthispamphlet,sendcommentsto:feedback@mitec.com.auorbyposttoMi-tec,POBox24,Camberwell,VIC,3124,Australia.
Patientinformationtoassistinformedconsent

generalinformation.Itisnotasubstitute doesforadvicefromyoursurgeon.Thispamphlet
andtopic.Ifyouarenotsureaboutthebenefits

Patientinformationtoassistinformedconsent
T he temporomandibular joint (TMJ)islocatedwherethelower jaw(mandible)attachestothe baseofyourskulloneachsideofyour head.Placeyourfingersinfrontofyour earsandopenyourmouth,andyoucan feelthesejointsmove.TheTMJallowsyourmouthtoopen andclose,andmovefromsidetoside.A discwithineachTMJactsasacushion andprotectsthemandiblefromwear.MusclesattachedtotheTMJcontrol itspositionandjawmovementsduring talking,chewingandswallowing.Temporomandibulardisorders(TMDs) areagroupofrelateddisordersthatcan involveoneorbothTMJs,chewingmusclesandsurroundingtissues.TMDscan causepain,clicking,grating,locking,
withyoursurgeon.Thisinformationwillchange
isanyspeciallytrainedandwillbeabletoanswer
about diagnosis, surgery and anaesthesia. willYoursurgeoncannotguaranteethattreatment meetallofyourexpectationsandthatit advicehasnorisks.Ifyouareuncertainaboutthe youaregiven,youmaywishtoseek a second opinion from another oral andinmaxillofacialsurgeon.Usethispamphletonly consultationwithyoursurgeon. If you decide to have teetharemoved,yoursurgeonmayaskyoutosign questionsconsentform.Readitcarefully.Ifyouhave abouttheconsentformorrelated









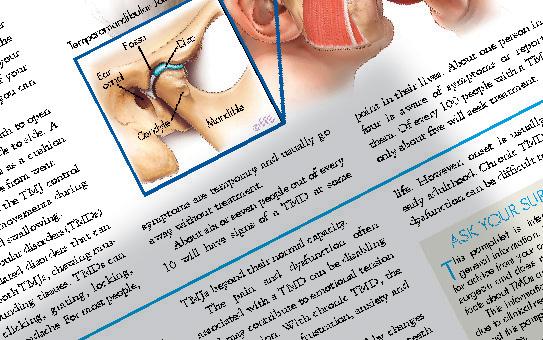
Apointintheirlives.Aboutonepersonin






Patientinformationtoassistinformedconsent

Aretrognathicjawisarecedinglowerjaw, isAprognathicjawoccurswhenthelowerjaw overdevelopedandprotrudesbeyondthe Oonrthognathicsurgeryisperformed correctthejawstoputthemintothe position.Orthognathic (pronounced or-thog-na-thik) means literally “straight jaws”. This willspeak.improveaperson’sabilitytochewand Thesurgerymayalsoimprove easierfacialappearance.Breathingmaybecome forsomepeople. ■protrudingrecedingchin jaw loweropenbite(spacebetweenupperand frontteethorbackteethwheninabilitythemouthisclosed)tomakelipsmeetwithoutmouthchronicmouthbreathingwithdry andinflamedgums problemssleepapnea(whensleeping,breathing suchassnoring). jaws,Yoursurgeonwillinspectyourfaceand andmaymakefacialmeasurements, ortakephotographsorusevideoimaging, YourrecommendX-rayexaminationsof surgeonmayassesstoothwear andtoothpositiontodeterminewhether

upperAn"openbite"leavesspacebetweenthe closed.andlowerteethwhenthemouthis








Aidstoorthodonticssurgerytohelpanuneruptedtooth moveintoitsnormalpositionextractionofaneruptedandnormal tooththatiscrowdingotherteethor, inuncommoncases,oneormoreextra permanentteeth(supernumeraryteeth)
varietyofproblemswiththe teeth,gum,jawboneandother bonyorsofttissuesofthemouth mayrequiretreatmentbyanoraland maxillofacialsurgeon.AlveolarThisiscalleddentoalveolarsurgery. boneisthebonethatsurrounds andsupportstheteeth.Thefollowingare commonsurgicalprocedures.Extractionofatoothorretainedrootextractionofadeadtooth(oftenweakenedbylargefillings)thatmayhavehad rootcanaltreatment;typicallyinmiddle-extractionofimpactedormisplaced




Aidstofittingofpartialorcompletetissueremovalofexcessgumtissueorscar onoraroundthe dentoalveolar removalofbonyoutgrowthsfrom


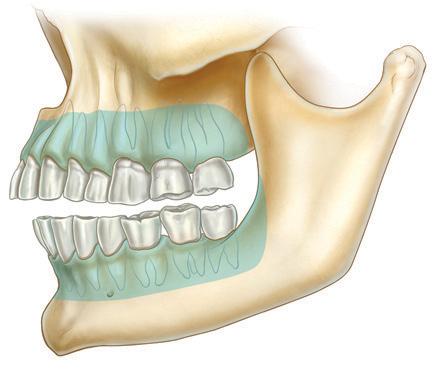

Toplanthebest

To celebrate the latest edition of AJOMS, we are offering 10% off all ANZAOMS pamphlets.
Order online at www.mitec.com.au/ANZAOMS and enter code “AJOMS10” at the checkout.

ecklumpsareacommoncondition. Most,butnotall, neck lumpsarebenign (non-cancerous). A persistent lump should be thoroughly investigatedandtreated,inaccordancewiththediagnosis. Malignant (cancerous) neck lumps haveusuallyspreadfromcancerslocated intheskinofthehead,neckororopharnyx(themiddlepartofthethroat,behind themouth).Anylumpthathasbeenpresentfor twoweeksormore,evenwithoutsymptoms,requires diagnosis.Notallnecklumpsrequiresurgery.Anecklumpmightdevelopfrom:



TellyoursurgeonifyouareYour surgeonwilladviseyouwhetherthe procedureshouldbedoneinthesurgery, ahospitalorinaday-surgeryclinic.
Patientinformationtoassistinformedconsent TALKTOYOUR SURGEON Thispamphletprovidesgeneralinformation.Itisnota substituteforadvicefrom yoursurgeon.Termsareusedthatmay requirefurtherexplanationbyyoursurgeon. Thisinformationwillchangewithtime,due toclinicalresearchandnewtherapies.Read thispamphletcarefully,andsaveitforreference.Everyaspectofthesurgerycannotbe coveredinthispamphlet.Seekafullexplanationofyourcasefromyoursurgeon.Yoursurgeoncannotguaranteethatsurgerywillmeetallyour expectationsorthat surgeryhasnorisks.Ifuncertain,seekthe opinionofanotherspecialist.Usethispamphletonlyinconsultationwithyoursurgeon.
■ swollen lymph nodes (also called lymphglands),whicharethemostcommonnecklumps
■ epidermoid,pilarorsebaceouscysts

■ abscesses
■ benignfattygrowthcalledalipoma
■ thyroidorparathyroidglands
■ abnormal blood vessels (haemangioma)
■ conditionsof the salivary glands, whicharetheparotidglands,submandibularglandsandsublingualglands.Specificcausesofalumpcaninclude:
■ inflamedtissue,duetovariouscauses (forexample,ablockedsalivaryduct)
■ infectionbybacteria,virusesorother infectiousorganisms
■ lymphomaorleukaemia
■ a tumour, which is an abnormal growthoftissue.A tumourmightbe benignormalignant(cancerous).Benign lumpscangrowfromvarioustissues,such asnerves,fat,bloodvessels,muscles,or thesalivaryglands.Ifthelumpiscancerous,thenitislikelytohavespreadto necklymphnodesfromotherareas.The originalsiteofthecancermaybeinthe (whetherbenignor malignant)increases withage.In children,necklumpsare uncommonandareusuallybenign.Lymphnodesandotheranatomy Theneckandtissuesabovethe collarbone containmanylymphnodes.Lymphnodes fightinfection.Theyaresmall,soft,nontenderlumps.Iftheygetbigger,then theirsizecanbefeltwhenexaminedby touch(palpation).Enlargedlymphnodes canbepainful,butthismaynotoccur withcancerouslymphnodes. Thelumpmaybe closeto blood vessels,nerves,lymphnodesandother tissues.Themostimportantneckstructuresinclude:




■ thecarotidarteryandjugularvein, whichcarrybloodtoandfromthebrain ■ nervesthatcomefromthebrain:the accessory nerve, hypoglossal nerve, lingualnerve,facialnerve,vagusnerve, andtrigeminalnerve.Seepage4formore informationaboutpossible complicationscausedbyinjurytothesenerves.
Important:Fillinalldetailsonthestickerbelow.
DEARSURGEON: Afteryoudiscussthispamphletwithyourpatient,fillintheinformationonthissticker, peelitoff,andputitonthepatient'smedicalhistoryorcard.Thiswillremindyouandyourpatientthat thispamphlethasbeengiventothepatient.Somesurgeonsasktheirpatientstosignthesticker.
1number:Edition
ConsumerandCarerFeedback:Toprovidefeedbackaboutthispamphlet,sendcommentsto: feedback@mitec.com.auorbyposttoMi-tec,POBox24, Camberwell,VIC,3124,Australia.
The ANZAOMS pamphlets provide high-quality and peer-reviewed treatment information for the benefit of surgeons and their patients.
