




Laksmana Adi Krista Nugraha

Greetings, People of Tomorrow. Perkenalkan, nama saya Laksmana Adi Krista Nugraha selaku Representative AMSA-Undip 2022. Suatu kehormatan bagi saya dan teman – teman untuk mempersembahkan Academic Hall of Fame ini sebagai bentuk apresiasi terhadap prestasi anggota AMSA-Undip terutama dalam bidang Research and Academic. Suatu inovasi yang bertujuan untuk meningkatkan prestasi AMSAUndip, keberadaan buku ini mengamplifikasikan arti tersebut. Akhir kata, semoga buku ini dapat menginspirasi teman – teman semua dalam memulai langkah dan meningkatkan kontribusi nya di bidang Research and Academic. Terima kasih, Viva AMSA!
“Enriching Potentials, Advancing Toward Possibilities”

Academic Hall of Fame merupakan program kerja dari divisi research and academic AMSAUndip yang bertujuan untuk mengapresiasi teman teman AMSA-Undip yang telah berprestasi dan mengharumkan nama AMSAUndip. Saya mengapresiasi sebesar besarnya kepada semua orang yang telah berkontribusi meningkatkan minat dan bakat dibidang riset dan akademik. Harapan saya dengan adanya program ini teman teman sekalian dapat terinspirasi untuk dapat mengeksplor lebih dalam dunia riset dan akademik dan bahkan dapat mengaplikasikan ilmunya melalui kompetisi kompetisi yang ada di AMSA. Sekian pengantar dari saya selamat membaca !




Pertama kali mendengar pengumuman tentang PCC EAMSC temanya sangat menarik. Saya sangat senang karena ada banyak area baru yang bisa dieksplorasi tentangnya. Tim kami juga ingin belajar dan berlatih lebih banyak dalam menulis karya ilmiah, dan acara ini adalah kesempatan yang tepat untuk mencapai hal tersebut. Membangun tim pendukung adalah salah satu bagian terpenting dalam menjalankan karya ilmiah. Sikap kerja sama yang suportif dan baik dapat sangat membantu karena akan mempermudah proses pembuatan makalah dan juga dapat meringankan tekanan psikologis dari pembuatan makalah. Menulis ulasan ini memberi penghargaan kepada kita dengan pengetahuan dan keterampilan dalam membuat karya ilmiah. PCC memberi kami kesempatan untuk meningkatkan keterampilan kami dalam karya ilmiah. Pengetahuan tentang menulis makalah yang dapat dicapai melalui PCC seperti menulis tinjauan sistematis dan metaanalisis dapat berguna untuk memperluas pengetahuan kita dalam penulisan ilmiah dan mungkin dapat membantu untuk masa depan karir kita sebagai seorang dokter. Saya merekomendasikan PCC sebagai platform pembelajaran untuk karya ilmiah. Jangan menyerah dan selalu nikmati prosesnya, saya yakin semua usaha kita akan terbayar suatu saat nanti
Introduction: Acute mountain sickness (AMS) is a high altitude disease characterized by headache, dizziness, fatigue, and gastrointestinal symptoms. AMS leads to hypobaric hypoxia and potentially develops into dangerous conditions such as pulmonary or cerebral edema. Current pharmacological treatments such as acetazolamide, dexamethasone, and analgesics have not been proven to be consistently effective to prevent AMS and shown unpleasant adverse effects. Alternatively, positive pressure ventilation therapy has shown some promising results in treating AMS.
Objective: The aim of this systematic review and meta-analysis is to evaluate the efficacy of positive pressure ventilation therapy in improving symptoms and physiological measurement in acute mountain sickness.
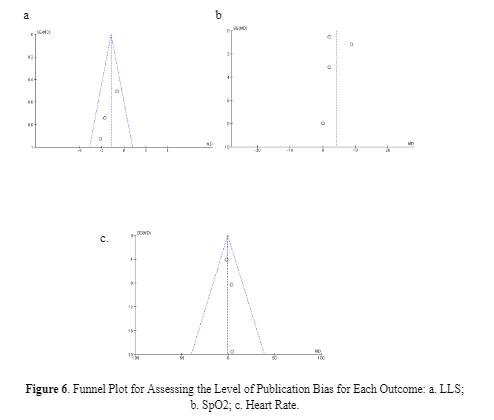
Method: This systematic review and meta-analysis was reported based on the PRISMA statement. The literature search was conducted on several databases, such as PubMed, Cochrane, Science Direct, and Scopus. Results were shown as mean difference (MD) and standard deviation (SD). A fixed-effect model (FEM was used when the included studies were considered homogenous), which were indicated by an I2 value less than 40%. Risk of bias was assessed using the cochrane risk-of-bias tool for randomized trials (RoB 2).
Result: This systematic review and meta-analysis included four randomized control studies with the total of 277 participants. Lake Louise Score declining with a significant pooled mean difference (MD) of -1.16 [95% CI: (-1.90) - (-0.41), P = 0.002]. Arterial oxygenation improvement with a significant pooled MD of 4.13 [95% CI: (-0.83) - 9.08, P < 0.00001]. Heart rate measurement showed no significant effect, MD of -0.19 [95% CI: (-7.26) - 6.68, P = 0.96]
Conclusion: This systematic review and meta-analysis showed evidence that positive pressure ventilation therapy is a prospective therapy to significantly improve acute mountain sickness symptoms and arterial oxygenation, but has no significant effect on heart rate.
Keyword: acute mountain sickness, positive pressure ventilation therapy, arterial oxygen saturation, heart rate.
Acute mountain sickness (AMS) is a common syndrome found in inexperienced travelers after arriving in high-altitude areas, characterized by headache, dizziness, fatigue, and gastrointestinal symptoms such as nausea, vomiting, loss of appetite, due to low partial pressure of oxygen.[1] Ascent to high altitude, approximately above 2500 m,[2] leads to hypobaric hypoxia, a state in which the inspired oxygen partial pressure (PiO2) is reduced due to low air pressure in the atmosphere, resulting in decreased arterial oxygenation.[3] Since the severity, onset, and duration of symptoms are influenced by the level of altitude, rate of speed, and personal susceptibility, its prevalence ranges from 15% to 80%%, with an increasing incidence as the altitude increases. The proportion of unacclimatized travelers affected at 3000 m was approximately 75% .[4] Although AMS is typically not life-threatening, it could potentially develop into dangerous conditions such as pulmonary or cerebral edema.[5] Consequently, the prevention of these severe conditions is crucial. Pharmacological treatments with acetazolamide, dexamethasone, and analgesic have been used for the prevention of AMS. However, these drugs have not been proven to be consistently effective to prevent the occurrence of AMS,[5,6] and have unpleasant adverse effects such as peripheral and circumoral paresthesias, nausea, and dry mouth .[7] Hence, beneficial non-pharmacological treatment was promoted.
The mechanism of AMS is associated with brain response to hypoxia, since the brain has the greatest oxygen demand.[8] At higher altitude, the level of carbon dioxide in the blood increased as the result of low partial pressure of oxygen. This condition is detected by medullary chemoreceptors, leading to hypoxic ventilatory response (HVR) in which the rate and depth of ventilation increased as the compensation of the reduced partial pressure of oxygen. The failure to intensify the HVR leads to hypoxemia the development of AMS.[9] Altitude hypoxemia leads to both increased sympathetic activity which leads to increased heart rate and endothelial alteration, causing vasogenic edema in the brain, which increases intracranial pressure, causing headache, nausea, vomiting, and weakness.
Since the reduced arterial oxygenation plays a significant role in the development of AMS, the ability to reduce the hypoxemic stress, especially in the first hours of exposure, may determine the probability of subsequent altitude illness.[10]
Improving pulmonary gas exchange is another mechanism linked to improved blood oxygenation and altitude acclimatization, in addition to increased HVR. Pulmonary gas exchange improvement can be gained by respiratory treatment of positive pressure ventilation therapy in which air or a combination of oxygen and other gasses is delivered into the lungs under positive pressure, leading to an increase of gas exchange. Positive expiratory pressure (PEP) has been found as a non-pharmacological respiratory treatment and easy method to treat acute mountain sickness by producing pressure contrary to the pressure produced by airways (expiratory flow resistance), causing an increase in alveolar pressure, leading to increasing of pulmonary gas exchange and arterial oxygen saturation, [11] with the rapid increases in SpO2 ranging between 0-23% have been reported with PEP breathing at high altitude.[12,13]
As well as PEP, another pressure-based respiratory therapy named positive end expiratory pressure (PEEP) was also known to be efficient in preventing acute mountain sickness in a hypobaric chamber without any side-effects.[14]
Utilizing positive expiratory pressure while sleeping enhances ventilation by attracting microatelctatic alveoli and changing breathing pattern, resulting in improvement of oxyhaemoglobin saturation.[18]
Although PEP and PEEP were thought to be successful as a treatment to improve conditions at hypobaric chamber and prevent severe complications, it is necessary to assess the efficacy of those interventions in actual field settings at high altitudes. Currently, there was no meta-analysis assessing these pressurebased therapy. Therefore, the current study was conducted to analyze the efficacy of PEP and PEEP as a treatment of AMS symptoms.
This systematic review was conducted based on Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guideline that can be accessed through (https://prisma-statement.org/)
Criterias that are considered eligible for this systematic review are:
Original research article or research reports using human study with randomized controlled trial design were included in this study. Narrative review, systematic review, meta-analysis, non comparative research, in silico studies, in vitro studies, in vivo studies, technical reports, editor response, scientific posters, study protocol, and conference abstracts were excluded. Unavailable full-text articles, non-english, irrelevant topics were also excluded.
Outcome measures that are assessed in this systematic review are Lake Louis Score (LLS), arterial oxygen saturation, and heart rate. LLS is a robust and practical tool to diagnose and score the severity of acute mountain sickness.
Lake Louise AMS scoring system is divided into three parts: a self-report questionnaire, a clinical assessment, and a functional score. The AMS self-report questionnaire consists of five questions regarding headache, gastrointestinal symptoms, fatigue and/or weakness, dizziness/light-headedness, and functional score each scoring from 0 to 3. The clinical assessment score is given through clinical examination by a physician of three signs: mental status rating from 0 to 4, ataxia rating from 0 to 4 and peripheral oedema rating 0 to 2. After clinical assessments have been conducted, the results can be added to the AMS selfreport score. The funcional score is one optional question regarding functional consequences of recorded signs rating from 0 to 3. The Lake Louise AMS plus the clinical assessment was defined as the sum of the both scoring. Representative point of AMS is when the result of assessment on the self-report questionnaire alone, or in combination with the clinical assessment score as three-point or greater score.[20]
Physiological measurements such as arterial oxygen saturation (SpO2) and heart rate (HR) were also assessed in this study. Arterial oxygen saturation (SaO2) is a measure of hemoglobin oxygenation in the arterial compartment of the circulatory system. The value of SaO2 is the same throughout the whole arterial system and directly related to the oxygen supply to organs, and normal values lie between 95% and 100%. Arterial oxygen saturation has been studied to be a predictor of acute mountain sickness.[21] HR were measured to represent the cardiovascular physiology from participants in the high altitude compared to low altitude.
Studies included were evaluating the LLS AMS Score, arterial oxygen saturation, and heart rate that presented the data with mean difference and standard deviation. Studies that do not present mean data scores before and after intervention were excluded.
Reference standards are randomized controlled trial studies performed by professionals by evaluating the effect of PEEP, EPAP, and CPAP on LLS score alteration.
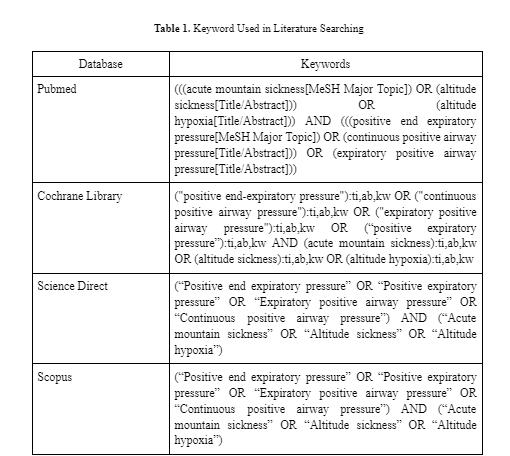
This study acquired studies by using searching databases, such as PubMed, Cochrane, Science Direct, and Scopus. Search was conducted from the inception of the database until October 2022. The keywords used were using Boolean operator and mesh. Keywords used in each database can be seen in Table 1. The studies are stored in the authors’ library using mendeley group reference manager.
After searching keywords written in Table 1, studies with non-RCTs were excluded through article type filters of each database. Results from 5 databases were later combined and screened by four independent reviewers (AIR, INSS, IOK, EAN) through title, year of publication, and DOIs for duplicate removal. After duplicate removal, studies were later screened through abstract and fullpaper for irrelevance removal. The study selection processes were recorded in the PRISMA flow chart.
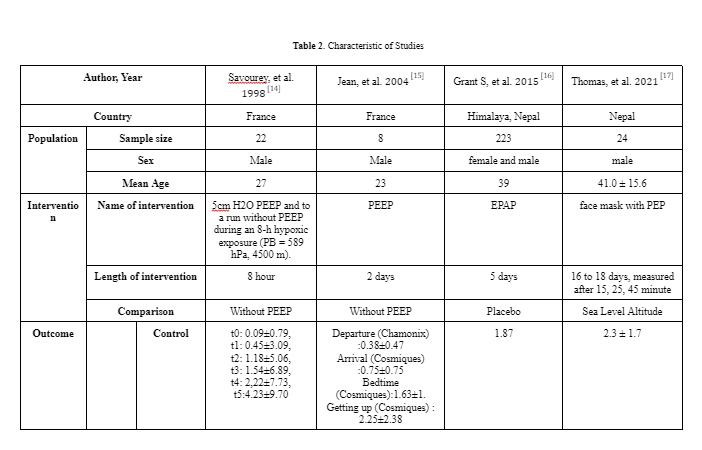
Studies after final screening are extracted for the relevant data and recorded in Google Spreadsheet. The recorded datas were: (1) first author, year, (2) country, (3) study design, (4) sample size, (5) gender, (6) mean age, (7) name of intervention, length of intervention, comparison, and (8) outcome that consist of LLS AMS Score, arterial oxygen saturation, and heart rate. All statistical tests for this meta-analysis were conducted using Review Manager (RevMan) v5.4 (Cochrane Collaboration, UK).
Each study included in this study was assessed by four independent reviewers (AIR, INSS, IOK, EAN) according to the Cochrane risk-of-bias tool for randomized trials (RoB 2) which can be accessed in (https://methods.cochrane.org/bias/resources/rob-2-revised-cochrane-risk-biastool-randomized-trials) The discrepancies were later discussed and resolved between reviewers. To maintain the present study’s robustness, we excluded studies that are assessed with a high risk of bias from the meta-analysis.
Mean Difference (MD) and Standard Deviation (SD) with the Confidence Interval (CI) of 95% were calculated in this review. A fixed-effect model (FEM was used when the included studies were considered homogenous (low variability in studies’ results or variation due to random error), which were indicated by an I2 value less than 40%. Otherwise, we used a random-effect model (REM). The pooled estimate was presented in a forest plot.
After conducting literature searching from 4 databases which are PubMed, Cochrane Library, Scopus, and ScienceDirect, 292 studies were generated. Automation tools from each database were used to exclude non-rct studies and resulted in 176 articles being excluded. Afterward, 33 duplicate study articles were removed. Subsequently, authors assessed all of the remaining articles from the title and abstract for irrelevance to the topic, resulting in 75 articles excluded. 7 articles were then retrieved for the full text availability. Lastly, the author assessed eligibility for all the studies and agreed to exclude 3 studies because of an uncontrolled study group and 1 study for an unpresent outcome of interest. This review included 4 studies to be in the systematic review and meta analysis. Our study selection process is presented in the PRISMA diagram flow chart in Figure 1.
Figure 1. PRISMA 2020 Flow Diagram.
From 4 studies included in this review, the total participants are 277 participants. Most of the studies (n=3) are conducted in field conditions in nepal and france such as Mount Blanc; the Khumbu region of the Himalayas; and Larkye Pass, Manaslu Circuit in the Nepali Himalaya. the other study are conducted in laboratory condition using hypobaric chamber to simulate the condition in the high altitude.
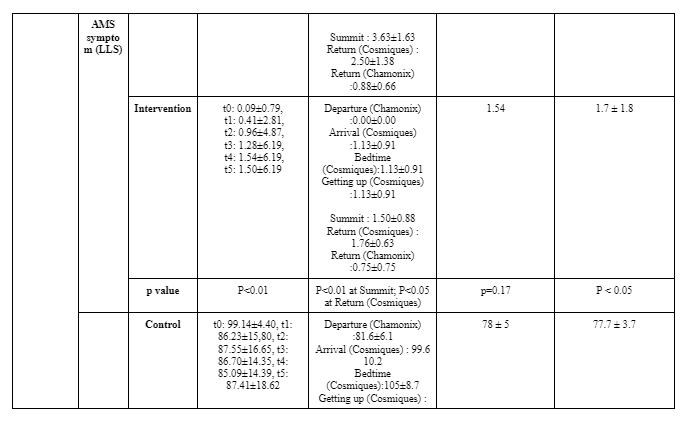
The quality of each study were carefully analyzed by using the Cochrane risk-ofbias tool for randomized trials (RoB 2) l. 3 studies showed high risk of bias (Savorey et al; Jean et al; Thomas et al) and one study showed some concern (Grants et. al). The risk of bias were summarized in Figure 2.
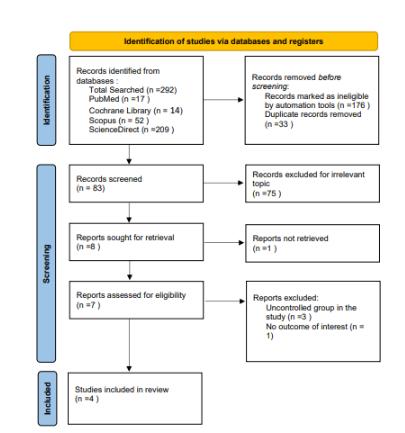
Figure 2. Risk of Bias Assessment Result.
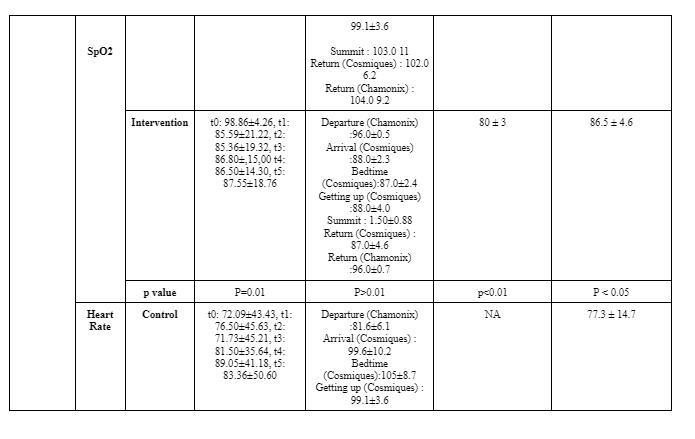

Statistical analysis was performed using Review Manager (RevMan) v5.4 (Cochrane Collaboration, UK) . Mean Difference (MD) and Standard Deviation (SD) with the Confidence Interval (CI) of 95% were then calculated in this review
The data then processed into pooled standardized mean difference forest plot form. Our study assessed extractable quantitative data and group them into 3 outcomes which include Lake louise Score, Sp02, and Heart rate. The forest plot of the meta-analysis can be seen in Figure 3-5.

Positive pressure ventilation therapy influence on AMS Severity AMS symptoms severity was assessed by Lake Louise Questionnaire, containing 4 symptoms which are headache, nausea/vomiting, fatigue, and dizziness/lightheadedness. A headache score of at least one point and a total score of at least three points are required for a positive AMS definition.[22] Positive pressure ventilation therapy that was conducted in all studies which are positive expiratory pressure (PEP) and positive end expiratory pressure (PEEP) has proven to be successful in reducing Lake Louise Score with a significant pooled mean difference (MD) of -1.16 [95%CI: (-1.90)-(-0.41), P = 0.002]. The reduction of Lake Louise Score, approximately ≤ 3, showed the improvement of individual condition obtained by the positive pressure breathing.[17] Furthermore, all of the studies were found to significantly reduce the score of LLS, with the exception of Grant S, et al. 2015 (p=0.17) which possibly due to wide range demographic variety of the participant. Thus, in general, positive pressure ventilation therapy is effective to relieve severity of AMS symptoms and yet, preventing the complication of AMS.
Ascending to high altitude causes a significant decrease in arterial oxygen saturation that leads to the development of AMS symptoms, and if occurs continuously, resulting in serious complications such as high altitude pulmonary or cerebral edema.[23] Positive pressure ventilation therapy has been shown to successfully increase arterial oxygenation during acute hypoxic exposure with a significant pooled main difference (MD) of 3.18 [95%CI : (2.19) (4.17), P < 0.00001].
An increase of oxygen saturation was facilitated by increased pulmonary gas exchanges due to improvement of intrathoracic pressure that was obtained from the positive pressure breathing-therapy.[18,23] Since the low oxygen saturation is highly associated with the worsening of the symptoms,[24] increased oxygen saturation provides better prognosis of symptoms development.
Acute high-altitude hypoxia induces cardiovascular changes through 3 pathways which are cardiac response due to depletion of oxygen delivery, increased pulmonary vascular constriction, and enhancement of sympathetic activity through β-adrenergic stimulation, leading to increased heart rate.[25,26] As a compensation for depletion of oxygen at high altitude, the heart beats faster to increase cardiac output, so that the body could maintain appropriate oxygen delivery to tissues.[27] Theoretically, increasing oxygen saturation would help to remove the hypoxic condition, thus, the heart could beat at its normal rhythm. However, it has been shown that the positive pressure breathing ventilation does not give a significant effect on heart rate, as shown by pooled MD of -0.19 [95% CI: (-7.26)-6.68, P = 0.96]. This is possibly due to the complex pathway of the cardiovascular system, so that the respiratory intervention does not directly and significantly cause heart rate alteration. The detailed mechanism of this case requires further investigation.
This study is the first systematic review and meta analysis that evaluated the positive pressure ventilation therapy efficacy towards acute mountain sickness. This systematic review assessed different types of positive pressure ventilation therapy effects in reducing acute mountain sickness symptoms on samples that were exposed to hypoxia conditions in mountain hiking. All studies included are randomized controlled trial with significant results in several aspects, such as reducing Lake Louis Score and improving oxygen saturation. Nonetheless this study is not without limitation. The study that was included have a high and moderate risk of bias. The sample size of the included study also were limited in size and conducted in homogeneous places. Therapies used in studies also varied between PEEP and PEP. Positive pressure ventilation therapy is also found to be not significant in reducing heart rate on high altitude induced hypoxia. Other external factors, such as individual detailed backgrounds including ethnicity were not explored and discussed in included studies. Hence, identifying a broader population in mountain settings in the futures studies is necessary. There might be a possibility to miss some important information in studies written in other language than English or Indonesian. Irretrievable full-text is also the limitation of this study.
This systematic review and meta analysis revealed that the use of positive pressure ventilation therapy which includes PEEP and PEP is a prospective therapy in acute mountain sickness. It has been shown that positive pressure ventilation therapy is quantitatively significant in improving AMS symptoms and arterial oxygen saturation. However, it has no significant effect on heart rate. We recommend further randomized control study with a larger sample size to be conducted to observe more about the efficacy of positive pressure ventilation therapy.
All authors declared there are no competing interests in this study.
This study is the first systematic review and meta analysis that evaluated the positive pressure ventilation therapy efficacy towards acute mountain sickness. This systematic review assessed different types of positive pressure ventilation therapy effects in reducing acute mountain sickness symptoms on samples that were exposed to hypoxia conditions in mountain hiking. All studies included are randomized controlled trial with significant results in several aspects, such as reducing Lake Louis Score and improving oxygen saturation. Nonetheless this study is not without limitation. The study that was included have a high and moderate risk of bias. The sample size of the included study also were limited in size and conducted in homogeneous places. Therapies used in studies also varied between PEEP and PEP. Positive pressure ventilation therapy is also found to be not significant in reducing heart rate on high altitude induced hypoxia. Other external factors, such as individual detailed backgrounds including ethnicity were not explored and discussed in included studies. Hence, identifying a broader population in mountain settings in the futures studies is necessary. There might be a possibility to miss some important information in studies written in other language than English or Indonesian. Irretrievable full-text is also the limitation of this study.
This systematic review and meta analysis revealed that the use of positive pressure ventilation therapy which includes PEEP and PEP is a prospective therapy in acute mountain sickness. It has been shown that positive pressure ventilation therapy is quantitatively significant in improving AMS symptoms and arterial oxygen saturation. However, it has no significant effect on heart rate. We recommend further randomized control study with a larger sample size to be conducted to observe more about the efficacy of positive pressure ventilation therapy.
All authors declared there are no competing interests in this study.
Prince TS, Thurman J, Huebner K. Acute Mountain Sickness. [Updated 2022 Jul 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430716/. Luks AM, Swenson ER, Bärtsch P. Acute high-altitude sickness. Eur Respir Rev. 2017 Jan 31;26(143):160096. doi: 10.1183/16000617.0096-2016. PMID: 28143879. https://pubmed.ncbi.nlm.nih.gov/28143879/. Rupp T, Saugy JJ, Bourdillon N, Verges S, Millet GP. Positive expiratory pressure improves arterial and cerebral oxygenation in acute normobaric and hypobaric hypoxia. Am J Physiol Regul Integr Comp Physiol. 2019 Nov 1;317(5):R754-R762. doi: 10.1152/ajpregu.00025.2019. Epub 2019 Sep 18. PMID: 31530174. https://pubmed.ncbi.nlm.nih.gov/31530174/. Mairer K, Wille M, Burtscher M. The prevalence of and risk factors for acute mountain sickness in the Eastern and Western Alps. High Alt Med Biol. 2010 Winter;11(4):343-8. doi: 10.1089/ham.2010.1039. PMID: 21190503. Taylor AT. High-altitude illnesses: physiology, risk factors, prevention, and treatment. Rambam Maimonides Med J. 2011;2(1):e0022. Published 2011 Jan 31. doi:10.5041/RMMJ.10022. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3678789/ Larson EB, Roach RC, Schoene RB (1982) Acute mountain sickness and acetazolanide. J Am Med Assoc 248:328-332. Hackett PH, Roach RC. High-altitude illness. New Engl J Med. 2001;345:107–14. doi: 10.1056/NEJM200107123450206.
Masuet-Aumatell C, Sánchez-Mascuñano A, Santangelo FA, Ramos SM, Ramon-Torrell JM. Relationship between Smoking and Acute Mountain Sickness: A Meta-Analysis of Observational Studies. Biomed Res Int. 2017;2017:1409656.
Bärtsch P, Swenson ER, Paul A, Julg B, Hohenhause E. Hypoxic ventilatory response, ventilation, gas exchange and fluid balance in acute mountain sickness. High Alt Med Biol. 2002;3:361–76. doi: 10.1089/15270290260512846. Roach RC, Greene ER, Schoene RB, Hackett PH. Arterial oxygen saturation for prediction of acute mountain sickness. Aviat Space Environ Med. 1998 Dec;69(12):1182-5. PMID: 9856544. https://pubmed.ncbi.nlm.nih.gov/9856544/. Acosta P, Santisbon E, Varon J. “The use of positive end-expiratory pressure in mechanical ventilation”. Crit Care Clin 23: 251–261, 2007. doi:10.1016/j.ccc.2006.12.012.
12. Tannheimer M, Tannheimer S, Thomas A, Engelhardt M, Schmidt R. AutoPEEP in the therapy of AMS in one person at 4,330 m. Sleep Breath. 2009 May;13(2):195-9. doi: 10.1007/s11325-008-0237-z. Epub 2008 Dec 4. PMID: 19052788. https://pubmed.ncbi.nlm.nih.gov/19052788/.
13. Lipman GS, Kanaan NC, Phillips C, Pomeranz D, Cain P, Fontes K, Higbee B, Meyer C, Shaheen M, Wentworth S, Walsh D. Study Looking at End Expiratory Pressure for Altitude Illness Decrease (SLEEP-AID). High Alt Med Biol 16: 154–161, 2015.
14. Savorey G, Caterini R, Launay JC, Guinet A, Besnard Y, Hanniquet AM, et al. Positive end expiratory pressure as a method for preventing acute mountain sickness. Eur J Appl Physiol 1998;77(1–2):32–6.
15. Jean, L. C., Nespoulos, O., Guinet-Lebreton, A., Besnard, Y., & Savourey, G. (2004). Prevention of acute mountain sickness by low positive end-expiratory pressure in field conditions. Scandinavian Journal of Work, Environment and Health, 30(4), 322–326. https://doi.org/10.5271/sjweh.801.
16. Grant. S., Kanaan, N. C., Phillips, C., Pomeranz, D., Cain, P., Fontes, K., Higbee, B., Meyer, C., Shaheen, M., Wentworth, S., & Walsh, D. (2015). Study Looking at End Expiratory Pressure for Altitude Illness Decrease (SLEEP-AID). High Altitude Medicine and Biology, 16(2), 154–161. https://doi.org/10.1089/ham.2014.1110.
17. Thomas, R., Saugy, J. J., Bourdillon, N., Verges, S., & Millet, G. P. (2019). Positive expiratory pressure improves arterial and cerebral oxygenation in acute normobaric and hypobaric hypoxia. American Journal of PhysiologyRegulatory Integrative and Comparative Physiology, 317(5), R754–R762. https://doi.org/10.1152/ajpregu.00025.2019.
18. Johnson PL, Popa DA, Prisk GK, Edwards N, Sullivan CE. Non-invasive positive pressure ventilation during sleep at 3800 m: Relationship to acute mountain sickness and sleeping oxyhaemoglobin saturation. Respirology. 2010 Feb;15(2):277-82. doi: 10.1111/j.1440-1843.2009.01678.x. Epub 2009 Dec 27. PMID: 20051046; PMCID: PMC4183457 https://pubmed.ncbi.nlm.nih.gov/20051046/.
19. Potchileev I, Doroshenko M, Mohammed AN. Positive Pressure Ventilation. [Updated 2022 May 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560916/
Roach, R. C., Hackett, P. H., Oelz, O., Bärtsch, P., Luks, A. M., MacInnis, M. J., Baillie, J. K., Achatz, E., Albert, E., Zafren, K., Yaron, M., Willmann, G., Wilkes, M., West, J. B., Wang, S. H., Wagner, D. R., Voituron, N., Ulrich, S., Twomey, R., … Andrews, J. S. (2018). The 2018 Lake Louise Acute Mountain Sickness Score. High Altitude Medicine & Biology, 19(1), 4. https://doi.org/10.1089/HAM.2017.0164.
Karinen HM, Peltonen JE, Kähönen M, Tikkanen HO. Prediction of acute mountain sickness by monitoring arterial oxygen saturation during ascent. High Alt Med Biol. 2010 Winter;11(4):325-32. doi: 10.1089/ham.2009.1060. PMID: 21190501.
Roach RC, Hackett PH, Oelz O, et al. The 2018 Lake Louise Acute Mountain Sickness Score. High Alt Med Biol. 2018;19(1):4-6. doi:10.1089/ham.2017.0164. Nespoulet H, Rupp T, Bachasson D, Tamisier R, Wuyam B, Lévy P, Verges S. Positive expiratory pressure improves oxygenation in healthy subjects exposed to hypoxia. PLoS One. 2013 Dec 23;8(12):e85219. doi: 10.1371/journal.pone.0085219. PMID: 24376872; PMCID: PMC3871630. Oliver SJ, Sanders SJ, Williams CJ, Smith ZA, Lloyd-Davies E, Roberts 576 R, Arthur C, Hardy L, MacDonald JH. Physiological and psychological 577 illness symptoms at high altitude and their relationship with acute mountain 578 sickness: A prospective cohort study. J Travel Med 19: 210–219, 2012. Gonggalanzi, Labasangzhu, Bjertness E, Wu T, Stigum H, Nafstad P. Acute mountain sickness, arterial oxygen saturation and heart rate among Tibetan students who reascend to Lhasa after 7 years at low altitude: a prospective cohort study. BMJ Open. 2017;7(7):e016460. Published 2017 Jul 10. doi:10.1136/bmjopen-2017-016460. Bärtsch P, Gibbs JS. Effect of altitude on the heart and the lungs. Circulation. 2007 Nov 6;116(19):2191-202. doi: 10.1161/CIRCULATIONAHA.106.650796. PMID: 17984389.
Mallet RT, Burtscher J, Richalet JP, Millet GP, Burtscher M. Impact of High Altitude on Cardiovascular Health: Current Perspectives. Vasc Health Risk Manag. 2021;17:317-335. Published 2021 Jun 8. doi:10.2147/VHRM.S294121



Anggota tim saya dan saya tidak memiliki pengalaman dalam penulisan ilmiah sebelumnya. Namun, kami tertarik dengan kesempatan untuk mempelajarinya lebih lanjut. Untungnya, bergabung dengan AMSA memberi kami panduan dan referensi dalam menulis melalui programprogram seperti LAT, AMINO, dan A-Book. Dengan kesempatan yang diberikan oleh AMSA, kami menantang diri kami sendiri untuk berpartisipasi dalam kompetisi akademik, dan Kompetisi Hari Hemofilia Sedunia yang diselenggarakan oleh AMSA-Internasional datang pada waktu yang tepat bagi kami.
Awalnya kami tidak tahu bagaimana cara menulis karya ilmiah yang baik. Kami juga berjuang untuk menemukan topik yang tepat dan memilah-milah referensi. Selama masa itu, kerja sama tim dan komunikasi memainkan peran penting, terutama saat kami juga berkutat dengan tanggung jawab akademis kami.
Bagi saya pribadi, WHDC bukanlah kompetisi pertama yang saya ikuti di AMSA. Sebelumnya, saya berpartisipasi dalam kategori Buku Putih PCC EAMSC dan mendapat juara 3, berkat usaha tim saya. Namun, ini adalah percobaan pertama saya di makalah ilmiah. Selama proses tersebut, tim kami belajar banyak tentang penulisan ilmiah. Itu adalah kesempatan besar yang kami ambil, dan merupakan kehormatan besar untuk bisa finis di posisi ke-2 terlepas dari kekurangan kami.
Introduction: Hemophilia is a blood clotting disorder due to a hereditary lack of blood coagulation factor. According to the Annual Global Survey 2019 of the World Federation of Hemophilia, the most cases of hemophilia is hemophilia A with different severity levels such as mild, moderate, and severe. Current treatment of hemophilia appears to have some issues such as mental and physical burden for the multiple intravenous infusions, requires dose adjustment and the development of FVIII inhibitors. Emicizumab prophylaxis is an emerging new treatment which has primary safety and efficacy. This study aims to evaluate the efficacy and safety of Emicizumab treatment for patients with mild hemophilia A.
Methods: A systematic review was conducted in accordance to PRISMA (Preferred Reporting Items for Systematic Review and Meta-Analysis) statement, using databases such as PubMed, ScienceDirect, and Scopus using the keywords “Emicizumab AND Mild Hemophilia”, ”Emicizumab AND Safety”, ”Emicizumab AND Efficacy”, and ”Mild Hemophilia AND Prophylaxis”.
Results: The search yielded 11 studies, with a total of 1168 patients. Among 184 patients who had Emicizumab as a prophylaxis reduces bleeding rate in 93% patients and causes 0 bleeding in 67% patients. A single subcutaneous injection of Emicizumab in 40 healthy patients demonstrated no clinically significant changes of blood pressure, pulse rate, and body temperature. Moreover, Emicizumab recipient has no hypercoagulation risk even at the upper FVIII levels seen in mild hemophilia A, mild or no adverse effect, no thrombosis, and more cost-effective than rFVIIa.
Conclusion: Emicizumab as a routine prophylaxis in hemophilia treatment yielded promising primary efficacy and safety with mild or no adverse effect, thus demonstrated statistically significant and clinically meaningful reductions of bleeding rate. Further, this study hopes to help in regards to formulate strategies and comprehensive guidelines of mild hemophilia treatment.
Key words: Emicizumab, efficacy, safety, mild hemophilia A, systematic review
According to the Annual Global Survey 2019 of the World Federation of Hemophilia, the worldwide identified patients of hemophilia is 195.263 patients, with most cases being represented by Hemophilia A (157.517 patients). Hemophilia can be mild, moderate, or severe depending on how much of the clotting factor is in a person’s blood. International Society of Thrombosis and Haemostasis (ISTH) defines mild hemophilia A as the less severe type of hemophilia A with FVIII:C >5 IU d/L and <40 d/L. (The definition, diagnosis and management of mild hemophilia A: communication from the SSC of the ISTH) As for the prevalence of all three severity categories, 39,52% Hemophilia A patients in high-income countries have mild disease, 14,64% have moderate disease, 45,52% have severe disease and 0,31% unknown. 22,32% Hemophilia A patients in upper middle-income countries have mild disease, 22,66% have moderate disease, 43,76% have severe disease and 11,25 % unknown. 10,84% Hemophilia A patients in lower middle-income countries have mild disease, 21,60% have moderate disease, 45,29% have severe disease and 22,28% unknown. (World Federation of Hemophilia. 2020. Report on The Annual Global Survey 2019. Canada : World Federation of Hemophilia)
Hemophilia is a blood clotting disorder due to a hereditary lack of blood coagulation factor. It is inherited in sex-linked recessive in the X chromosome (Xh), characterized by spontaneous bleeding in patients with no previous family or personal history of bleeding. Hemophilia inheritance is caused by a defect in one of the genes that determine how the body makes blood coagulation factor VIII or IX. F VIII gene and F IX gene is located in the X chromosome and it is recessive. according to that, this disease is carried by a woman (XXh) and manifest clinically in man (XhY). It is also manifest clinically in a woman if there is an abnormality 2 chromosome X (XhXh). (L.J. Jameson, A. Fauci, D. Kasper, S. Hauser, D. Longo, J. Loscalzo. 2018. Harrison's Principles of Internal Medicine, Twentieth Edition (Vol.1 & Vol.2).McGraw-Hill Education / Medical )
The primary aim of care is to prevent and treat bleeding with the deficient clotting factor. The current treatment of hemophilia is based upon replacing the missing factor and can be done either as needed when bleeding episodes
occur (episodic or on-demand therapy) or in a preventative manner (prophylaxis). Referral to a hemophilia treatment center (HTC) to facilitate treatment, intravenous infusion of factor VIII concentrate is most effective when infused within one hour of the onset of bleeding. Prophylaxis is the treatment by intravenous injection of factor concentrate in order to prevent anticipated bleeding. Prophylactic infusions of factor VIII concentrate three times a week or every other day to maintain factor VIII clotting activity higher than 1% nearly eliminates spontaneous bleeding and prevents chronic joint disease. Prior to the advent of factor therapy and prophylaxis, the lack of effective treatment for hemophilia resulted in a shortened lifespan and severe morbidity. (Harrison's Principles of Internal Medicine, Twentieth Edition Sep 21 [Updated 2017 Jun 22]. In: Adam MP, Ardinger HH, Pagon RA, et al., editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2021. https://www.ncbi.nlm.nih.gov/books/ ) ( Balkaransingh, P., & Young, G. (2017). Novel therapies and current clinical progress in hemophilia A. Therapeutic Advances in Hematology, 9(2), 49–61. https://doi.org/10.1177/2040620717746312)
The infusion of Factor VIII as therapy develops several issues to the hemophilia patients. One is mental and physical burden for the multiple intravenous infusions, and the other one is and requires dose or dosing frequency adjustment to maintain FVIII:C > 1%. Other than that, hemophilia A patients treated with factor VIII are found to develop FVIII inhibitors. Frequent intravenous administration of these agents is required because of their unstable hemostatic efficacy caused by short half-lives. In order to solve issues found in FVIII infusion, new treatments with more convenient, effective and safe. Emicizumab, is a recombinant, humanized, bispecific monoclonal antibody (mAb) that binds to FIX/FIXa and FX/FXa and mimics FVIIIa cofactor activity in the tenase complex. Emicizumab prophylaxis is a promising treatment to develop in mild hemophilia cases judging by the good result of research with severe hemophilia patients. (Uchida, N., Sambe, T., Yoneyama, K., Fukazawa, N., Kawanishi, T., Kobayashi, S., & Shima, M. (2016). A first-in-human phase 1 study of ACE910, a novel factor VIII-mimetic bispecific antibody, in healthy subjects. Blood, 127(13), 1633–1641. https://doi.org/10.1182/blood-201506-650226)
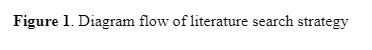
This systematic review was conducted in accordance to PRISMA (Preferred Reporting Items for Systematic Review and Meta-Analysis) statement. The literature search was conducted using databases such as PubMed, ScienceDirect, and Scopus using the keywords “Emicizumab AND Mild Hemophilia”, ”Emicizumab AND Safety”, ”Emicizumab AND Efficacy”, and ”Mild Hemophilia AND Prophylaxis”. The search were limited to studies with English or Bahasa Indonesia, as these were the language compatible with the authors. Studies were screened according to inclusion criteria as follows: (1) studies of emicizumab treatment on hemophilia, (2) not older than 2011, and (3) written in English or Bahasa Indonesia. Afterwards, exclusion criteria were also set, including (1) irretrievable full-text article, and (2) irrelevant article. Details of study search strategy are shown in Figure 1.
The process of literature searching and selection is illustrated in Figure 1. From the databases such as PubMed, ScienceDirect, and Scopus, 3559 studies were yielded. After duplicates were removed, titles and abstracts were screened, and full-text articles were then assessed. 149 studies were excluded due to irrelevant study variables, language restrictions, irretrievable full-text, and irrelevant outcomes. This resulted in a final of 11 studies to be included in qualitative synthesis, consisting of 4 clinical trials, 2 cohort studies, 1 meta analysis, 1 review, 2 RCTs (Randomized Controlled Trial), and 1 case report. Study characteristics are shown in Table 1.

Based on the studies included above, we analyze the safety and efficacy of emicizumab on patients with mild hemophilia which has a higher titre of FVII than severe hemophilia.
Emicizumab has been approved by the US Food and Drug Association as a routine prophylaxis to prevent or reduce bleeding episodes in patients with blood clotting disorders such as hemophilia. Emicizumab itself has gone through a few clinical trials, namely HAVEN 1-4. Throughout the 4 clinical trials, there were adverse effects observed on the patients with emicizumab treatment. The most frequent AE was injection site reaction (ISR), which happened on 23% of patients across the 4 trials. (mahlangu20117) This frequency is comparable to that seen in other medications which are given through subcutaneous injection. However, a study by Uchida, 2016 found that Emicizumab injected to healthy patients did not cause hypersensitivity reactions. On the HAVEN 1 trial, microangiopathies and thrombosis events, which were the most severe and unexpected adverse events were found in 3 patients who also received aPCC treatment for acute kidney injury. (langer2018) This however did not happen to other 381 patients who experienced mild adverse effects.
Based on a study by Nakajima, 2020, the coagulation activity during the registered dosing of emicizumab is currently not a problem. Derived to the adjusted clot, Emicizumab does not seem to potentially cause hypercoagulation even when combined with FVII treatment. In mild or moderate hemophilia patients, Emicizumab does enhance coagulation function, and does not cause clot forming above the normal range. This proves that Emicizumab is safe in terms of patients with mild hemophilia, who have higher titre of FVIII.
Uchida 2016, the first-in-human phase 1 study, showed no clinically significant changes of blood pressure, pulse rate, and body temperature on 40 healthy subjects that were randomized to receive a single subcutaneous injection of
Emicizumab.
A case was reported on a patient with mild hemophilia A and FVIII inhibitors. The patient received six months of Emicizumab as a prophylaxis treatment. The patient did a self-injection of 3 mg/kg Emicizumab one weekly for 4 weeks, and maintained the treatment. The patient did not show any puncture site adverse effect or thrombosis event.
400 participants were included in the efficacy analysis of the HAVEN 1-4 studies by Callaghan 2020. The study demonstrated statistically significant and clinically meaningful reductions in Annual Bleeding Rates during the Emicizumab prophylaxis and continued to decrease with maintained Emicizumab treatment after 24 weeks of prophylaxis. During weeks 121-144, the vast majority (99.4%) of participants had ≤ 3 treated target joint bleeds and 82.4% of participants reported zero treated bleeds. Moreover, a study conducted by Mahlanggu in 2019 found that the infrequent emicizumab injection will have a direct impact on reducing treatment and disease burden of patients. Other than that, the effect of Emicizumab is also still clinically meaningful and real. Preliminary data from HAVEN 4 show consistently high efficacy and acceptable Emicizumab given at a dose of 6 mg/kg once a month.
Another study done on 184 adult and pediatric patients with hemophilia A showed that Emicizumabsuccessfully reduced the number of bleeding rates on 93,5% patients while the number of patients with 0 bleeding was 67%. The study concluded that Emicizumab could improve the patients’ quality of life by reducing the number of hemorrhagic events. A study by Yaoi, 2021 assessed the effect of Emicizumab on type 2N Von Willebrand disease patients, a disease phenotypically similar to mild hemophilia through perfusion chamber experiment with 100 µg/ml Emicizumab as the intervention. The study found that Emicizumab effectively enhanced high shear-induced thrombus formation in all 3 cases. Emicizumab is also found to be more convenient and stable in the circulation than FVIII products, which had been the gold standard for hemophilia patients.
The strength of this study lies in the comprehensive assessment of the safety and efficacy of Emicizumab on mild hemophilia A patient on a relatively large number of samples and a wide range of areas. However, since the studies for Emicizumab are currently still on-going, the Randomized Controlled Trials (RCT) study on mild hemophilia patients is still lacking. This could be the limitation of this paper, as this paper relies not only on studies conducted by RCT design but also case reports and reviews, which might not be as reliable. The inaccessible full-text articles and incompatible language also serve as limitations for this study.
The result of this systematic review could be applied to formulate strategies in regards to Emicizumab use in mild hemophilia patients, thus improving the effectiveness and efficiency of mild hemophilia treatment. Based on the aforementioned result, we suggest further studies done with larger sample size of patients with mild hemophilia A to reduce bias of studies with small sample size. We also recommend more studies to be done regarding mild hemophilia, as there have been a considerable number of mild hemophilia cases but less studies regarding the therapy for mild hemophilia. And since Emicizumab as a bispecific monoclonal antibody has shown significant effect on hemophilia patient compared to coagulation factors products, it is also recommended that more studies regarding monoclonal antibody therapy should be done to improve the efficacy and safety of hemophilia treatment.
Based on the results and discussion above, it could be concluded that Emicizumab is effective in reducing the bleeding rate in mild hemophilia patients. Emicizumab also improves blood clotting function and thrombus formation. While the coagulation-enhancing trait of Emicizumab could help significantly in severe hemophilia cases, questions arose as to whether Emicizumab is safe for mild hemophilia patients, who have a higher titre of FVIII. From the studies observed, there seem to be almost no report of hypercoagulation on mild hemophilia patients from Emicizumab treatment. Other than that, the adverse effects of Emicizumab treatment are mostly mild and could happen in other subcutan-admission drugs. Healthy patients who
received Emicizumab in the clinical trials also showed no significant changes in vital sign or adverse effects. This further proves the safety of Emicizumab treatment on mild hemophilia patients. However, studies with larger sample size are required in order to reduce the bias of studies conducted on small sample size. This study hopes to help in regards to formulate strategies and comprehensive guidelines to improve the efficacy and safety of mild hemophilia treatment.




Hello, People of Tomorrow!
Nama saya I Nyoman Sebastian Sudiasa, kalian bisa memanggil saya Bastian. Berpartisipasi dalam PCC EAMSC 2023 merupakan kompetisi yang sangat berharga bagi saya dan teman-teman. Saat membuat poster ilmiah, bagian tersulit adalah menentukan topik artikel kita. Kami mengambil begitu banyak waktu untuk menemukan ide. Kami mencari inspirasi dari basis data hingga buletin elektronik. Kami menemukan banyak ide, tetapi memutuskan untuk memilih vaksin kolera sebagai topik utama kami. Saat berpartisipasi dalam kompetisi, temanteman saya adalah rekan tim terbaik yang pernah saya minta. Kami saling mendukung dan juga bersenang-senang selama proses tersebut.
Kami telah mengikuti kompetisi AMSA sebelumnya, dan tidak sekali pun kami menang. Namun, dengan berpartisipasi dalam kompetisi tersebut kami belajar bagaimana menyelesaikan hal-hal yang kurang kami miliki. Oleh karena itu, penting untuk terus mencoba karena meskipun kita tidak bisa menang, kita tetap mendapatkan pengetahuan baru dan pengalaman yang menyenangkan bersama teman-teman kita. Karena kegagalan bukanlah akhir, melainkan awal menuju kesuksesan.
“Sukses tidak instan, itu adalah kemajuan melalui banyak kegagalan”
Introduction: Cholera is an acute diarrheal illness that remainsa public healthproblem in more than 50 developing countrieswith 4 million cases globallyevery year, primarilyattacking unprivileged populations, and responsible for over 140,000 fatalities. Due to its fatality and severity of symptoms, oral cholera vaccination (OCV) was promoted as a preventive action in people traveling to cholera-endemic areas. CVD 103-HgR, a live attenuated oral cholera vaccine, was recommended, since it could potentially improve serum vibriocidal antibodies (SVAs) produced by natural or experimental Vibrio cholerae infection, providing protection against cholera.
Objective: To assess the efficacy of oral cholera vaccine for improving immunity against cholera infection, specifically antibodies seroconversion rate, in tropical countries.
Methods: The studies included were obtained by performing a literature search in 5 databases, namely PubMed, Science Direct, EBSCOhost, Cochrane Library, and Google Scholar, then assessed according to the PRISMA flow diagram, resulting in 13 studies for quantitative analysis. Risk of bias was assessed using the Cochrane risk-of-bias tool for randomized controlled trials (RoB 2).
Results and Discussion : Thirteen studies were included in this study. We found that CVD 103-HgR OCV is effective to improve SVA. Thus, offer protection against cholera infection (Risk Ratio 22.35 [95% CI: 12.49 - 40.01, P < 0.00001]). CVD 103-HgR OCV also has been shown to significantly increase anti-CT antibody GMT (geometric mean titer), resulting in increasing immunogenicity. However, the data obtained shows heterogeneity (��2> 40%).
Conclusion: CVD 103-HgR OCV significantly and robustly improved the SVA seroconversion rate as a prevention against cholera. CVD 103-HgR OCV is an excellent choice for preventive action against cholera disease. However, higherquality studies are required to examine the adverseeffect of CVD 103-HgR OCV. Thus, CVD 103-HgR OCV needs to be includedin health policies in cholera-endemic countries.
Keywords: oral choleravaccine, prevention, vibriocholerae, traveling






Ikut lomba-lomba di AMSA tentunya menambah ilmu dan pengalaman yang unik. Lomba yang diadakan macammacam dan tidak ada ruginya untuk coba ikut berbagai lomba, baik dari tingkat yang paling dekat dulu--misal mulai dari universitas, distrik, sampai nasional dan internasional). Dari awal aku masuk di AMSA, aku sudah sering ikut berbagai lomba terutama di bidang poster publik, dan awalnya pun belum pernah masuk final ataupun menang, tapi aku terus mencoba aja, sampai akhirnya di lomba terakhirku, yaitu AMSA International Summit yang diselenggarakan oleh AMSA-International cabang Public Poster, dengan bantuan serta dukungan dari teman-teman AMSA-Undip khususnya RnA, aku berhasil memperoleh juara 1.
Jadi, jangan ragu teman-teman untuk ikut lomba! Apalagi sekarang RnA sudah menambah banyak program untuk memfasilitasi teman-teman yang ingin ikut lomba, jangan disia-siakan yaa!
Trauma is one of the major causes of deaths in the world, especially at a young age. Annually, there are 5.8 million deaths caused by trauma. This number is expected to rise up to 8.4 million deaths annually in the year 2020. In low- and middle-income countries, mortality related to trauma before 70 years of age happens more often than in high-income countries. Attention should be given to trauma care to improve treatment of trauma patients, preventing trauma itself, and developing emergency medical services to reduce preventable trauma care.1
First aid is the assistance given immediately to an injured person before professional help arrives to give proper medical treatment. First aid interventions seek to “preserve life, alleviate suffering, prevent further illness or injury and promote recovery.”2 First aid plays a major role in adequate trauma care to decrease morbidity and mortality, which is gained by fast, systematic, and effective treatment of the injured patient. Injuries are usually diagnosed and treated by the ABCDE principle consisting of airway, breathing, circulation, disability, and exposure.3
An important part of trauma care is the “Golden Hour”, which is the immediate time after the injury happens. Ineffective use of the golden hour could lead to the less favorable outcome after, or even before, the patient finally gets appropriate medical treatment in the hospital. With trauma as one of the leading causes of death annually worldwide, prehospital emergency medical services are of utmost importance. However, low- and middle-income countries tend to lack provision in emergency medical services. Furthermore, when an emergency trauma case happens, there is a big chance that there are no medical professionals nearby.
Citizens nearby such a case should be ready to help give first aid when needed, yet most citizens do not know how to give the proper first aid for those patients who are in emergency cases without a medical professional nearby. This white paper and video aim to propose a solution to increase efficient use of golden hours by non-medical civilians who happen to be nearby in an emergency trauma situation.
This white paper was written by acquiring sources from Google Scholar, PubMed, and ScienceDirect. Keywords used to search for literature include “Trauma Care”; “Prehospital Time”; and “First Aid”. The literatures are included if they meet certain criterias such as: (1) written in English, (2) published in between the year 2011 - 2021, and (3) relevant to the topic. Studies are excluded if they are: (1) written with incompatible language or written before the year 2011 and (2) not correlated to the aim of this study.
Millions of people each year die as a result of traumatic injuries. Emergency Medical Services (EMS) worldwide are continuously improving to reduce these numbers and give better medical care to victims of traumatic injuries. Prehospital time after an injury takes place proves to be an important part of trauma care. This is also known as the “Golden Hour”, the immediate time after injury where resuscitating, stabilizing, and rapidly transporting patients are proven to be beneficial to the patient. Treatment given to the patient during this time will greatly determine the outcome of the patient after, or even before, getting professional medical care in hospitals.4
Prehospital time, which includes response time, on-scene time and transport time, is an important parameter of emergency medical services and plays an important role in trauma care. Although some countries already have sufficient trauma care systems, there are many countries that still have incomplete trauma care.
A study in Asian countries did not show the association of an increased 30days mortality after with an inefficient use of prehospital time.
However, inefficient use of prehospital time does show great association with increased risk of poor functional outcome. Functional outcome is an index of neurological status that shows the quality of life and the ability of a person to return to normal life and work. This is a crucial index of outcome as achieving a favorable functional outcome should be prioritized in patient care.5
The biggest problem in countries without proper emergency medical services is the lack of first aid knowledge among civilians. Trauma cases do not always happen when a medical professional is around to help, yet there are usually other non-medical people who are around at that time. Civilians hold the key to potential life-saving of patients in emergency trauma cases, yet such potential is lost because of their lack of knowledge regarding first aid.
A study in Great Britain shows that 85% of trauma victims that died before reaching the hospital were probably because of airway obstruction. A large amount of pre-hospital deaths can be prevented by simple first aid techniques that can be taught to society. Several other studies show that many deaths caused by trauma were due to the lack of first aid. Simple first aid interventions such as changing posture, opening an airway, and controlling bleeding are very important actions that can be done by anyone and have the potential to save lives.6
Trauma being a leading cause of death worldwide and insufficient first aid affecting a patient’s health outcome after a traumatic injury calls for an innovation to overcome this problem and improve emergency medical services. Certainly, such an innovation requires the help of the government as funders, hospitals as medical centers, and healthcare professionals as trained experts to be recognized as a qualified and efficient solution to such a problem.
The lack of first aid readiness among society calls for an innovation in providing sufficient first aid guidance when needed as the first aid given to patients before they arrive at the hospital to get professional care is of utmost importance. We would like to propose a solution to help the lack of first aid readiness when it is needed by non-medical professionals.
We would like to propose an application that provides guidance videos to assist civilians to do proper first aid when they are in emergency situations. The application will ask quick multiple-choice questions to identify the emergency that is taking place. All kinds of emergencies will be included in this application such as traffic accidents, heart attacks, seizures, burns, choking, intoxication, drowning, common injuries, and many more. It will then provide a short video to show the proper technique of giving first aid according to the situation. It will also give crucial information on things that should and should not be done to prevent further unwanted injuries. The video would be very short so that first aid can immediately be given to the patient to reduce the chance of loss before the patient can be taken to a medical professional.
When needed, this application will also connect civilians to the nearest hospital to get an ambulance heading toward their location as fast as possible. They will also be connected to a medical professional on standby in the emergency department from that same hospital to get assistance on what to do when an unexpected incident comes up and to keep encouraging them until the ambulance comes to help. We believe that the development of this application will be of great use since many emergency trauma cases happen when there are no medical professions nearby that can give immediate medical care. Therefore, we need civilians who are nearby to be able to give necessary first aid to increase the patient’s ability to have better functional outcomes after receiving medical care in the hospital.
Trauma being a leading cause of deaths worldwide and insufficient first aid affecting a patient’s health outcome after a traumatic injury calls for an innovation to overcome this problem and improve emergency medical services. We would like to propose a solution to help the lack of first aid readiness when it is needed by non-medical professionals in the form of an application to provide guidance videos to assist civilians to do proper first aid when they are in emergency situations. When needed, this application will also connect civilians to the nearest hospital to get an ambulance and be connected to a medical professional from that same hospital in case unexpected incidents occur. With this solution, we hope to increase first aid readiness among civilians to help improve emergency medical services in their country.
We hope that the government would support funding allocations on the development of this application. Hospitals should also collaborate with this application so that those in emergency situations can have an ambulance headed their way immediately and easily get connected to medical professionals on standby at the nearest hospital. We also hope that those trained in the medical field would be willing to help make these videos to assist those in need and also help make qualified questions that would lead to the proper and accurate identification of the emergency situation. In order for this to work, the participation of society is also needed as active users of this application and also as a means to socialize and further spread this application.
The authors acknowledge all sources used for excellent information and data provided concerning first aid and prehospital time in different countries. The authors would also like to thank AMSA-Indonesia for the opportunity to write this paper and all parties that were willing to take part in the making of this paper and video
1. Byun CS, Park IH, Oh JH, Bae KS, Lee KH, Lee E. Epidemiology of Trauma Patients and Analysis of 268 Mortality Cases: Trends of a Single Center in Korea. Yonsei Med J. 2015;56(1):220.
2. International Federation of Red Cross and Red Crescent Societies, Geneva [Internet]. Koninklijke Brill NV; [cited 2021 Apr 3]. Available from: https://primarysources.brillonline.com/browse/human-rights-documentsonline/international-federation-of-red-cross-and-red-crescent-societiesgeneva;hrdhrd98132015012
3. Dn K, Kiran A. Emergency Trauma Care: ATLS. Journal of Advanced Oral Research. 2011 Jan;2(1):13–6.
4. Harmsen AMK, Giannakopoulos GF, Moerbeek PR, Jansma EP, Bonjer HJ, Bloemers FW. The influence of prehospital time on trauma patients outcome: A systematic review. Injury. 2015 Apr;46(4):602–9.
5. Chen C-H, Shin SD, Sun J-T, Jamaluddin SF, Tanaka H, Song KJ, et al. Association between prehospital time and outcome of trauma patients in 4 Asian countries: A cross-national, multicenter cohort study. PLoS medicine. 2020;17(10):e1003360.
6. Arbon P, Hayes J, Woodman R. First Aid and Harm Minimization for Victims of Road Trauma: A Population Study. Prehosp Disaster med. 2011 Aug;26(4):276–82.




Mengikuti cabang White Paper dan Video merupakan suatu hal yang baru bagi kami. Kami memulai untuk memahami prosedur dan unsur-unsur dalam membuat white paper dari 0. Membuat white paper merupakan proses yang menyenangkan karena menuntut banyak ide dan inovasi baru Di dalam pembuatan white paper dibutuhkan banyak kreativitas dan penggalian ide yang nantinya bisa bermanfaat buat masyarakat khususnya di bidang kesehatan. Dalam proses pembuatannya, kami dimentori oleh Kak Prudence yang merupakan pemenang white paper pada tahun sebelumnya sehingga kami bisa mendapat arahan baik tahapan yang harus kami lakukan dan revisi-revisi agar kami dapat memberikan karya yang maksimal. Ada banyak manfaat yang bisa didapat dengan mengikuti kegiatan akademik anatara lain : Mendukung kemampuan sebagai mahasiswa kedokteran untuk memiliki skill update dengan ilmu pengetahuan yang baru, yang mana dapat berasal dari jurnal penelitian terbaru; Lebih terpacu untuk mengasah kemampuan untuk mereview jurnal-jurnal dan mengkonversikannya sebagai sebuah karya yang baru; Mengasah kreativitas, terutama dari penyusunan skenario, take video , dan juga skill editing; dan juga Membawa nama baik AMSA-Universitas; Meningkatkan rasa cinta terhadap AMSA-Indonesia Seperti yang kita tahu, banyak pengalaman dan kesempatan yang tersedia dengan kita mengikuti AMSA. Dengan ketiga filosofi tersebut terus dikembangkan program kerja yang bertujuan untuk mengembangkan potensi yang kita miliki. Jadi menurut kami, sangat disayangkan ketika kita sudah masuk menjadi bagian AMSA, tetapi tidak mengambil kesempatan tersebut.
Jadi, jangan ragu teman-teman untuk ikut lomba! Apalagi sekarang RnA sudah menambah banyak program untuk memfasilitasi teman-teman yang ingin ikut lomba, jangan disiasiakan yaa!
Based on the Center for Disease Control and Prevention (CDC), mental health is all about emotional, psychological, and social well-being. It describes the way we think, feel, and act.1 Although the terms are often used interchangeably, poor mental healthand mental illnessare not the same. A person can experience poor mental health and not be diagnosed with a mental illness. Likewise, someone diagnosed with a mental illness can feel good physical, mental, and social well-being periods.
In Indonesia, mental illness is one of the significant problems often encountered lately. In 2018,the prevalence of mental-emotional disorders as indicated by symptoms of depression and anxiety for ages 15 years and overreaches 6.1% of the total population of Indonesia, or the equivalent of 11 million people. Teenagers (15-24 years) have a depression percentage of 6.2%. Thosewith severe depression will tend to hurt themselves (self-harm) to suicide.Suicide cases in Indonesia can reach 10,000or the equivalent of everyhour there is a suicidecase. Depression in adolescents can be caused by several things,such as pressurein the academic field, bullying,family factors, and economic problems.2,3
However, understanding of mental health in Indonesia tends to be low. The knowledgeabout mental health in Indonesia is evidenced by the deprivation rate of people with mental disorders of 14% who have been in our lives and 31.5% in the last three months. In addition, 91% of Indonesian people who experience mental disorders are not handled properly, andonlythe remaining 9% can be handled. Not being appropriately handled can indicate a lack of mentalhealth facilities and a lack of understanding of mental health. Society tends to give a negative stigma to people with mental disorder by criticizing and considering them a disgrace.In addition,
people do not understand the signs of mental disorderssuch as depression, where depression is the most common mental health disorder.4
Situations that happennow explain the urge to have accessible and fast mediato handle mental illness cases correctly and to prevent the rate of suicide. Currently, many telemedicine platforms can be accessed and used by the public. Telemedicine gives easy access to health services that can be done online. Telemedicine will help reach out to people who live in remote areas,and due to its accessibility, it can be accessed anytimeand will help more people.
In this digital era, there are already many platforms that provide online consulting servicesfor free or paid, and also there is already a suicide hotline in Indonesia. However,those platforms are not integrated with the health facilitators, mental health centers, police stations, and every citizen’s phone. We think this feature will be handy to help emergency cases such as preventing suicide cases. Other than that, we also find that some platforms which provide online consulting do not give a chance to do a free trial first with the doctors, which will be very helpful for the patients to decide with whom they will consult. Therefore, this white paper andvideo will offer an effective solution to help people with mental illness and decrease the suiciderate in Indonesia using telemedicine.
We identified our initial ideas based on the theme of the paper, which was telemedicine. Then we analyze telemedicine that exists in the society, and we consider what problems have a significant effect on the people so that we can give some solutions, enhancement, and innovation. Therefore, we choose telemedicine for mental health. Most people must have experienced mental problems, ranging from minor to significant mental problems. We alsothink about the urgency of the mental health problem and the possibility of advanced mental health telemedicine.
This white paper was written by acquiring sources from several books and journals (NCBI, PubMed, and ScienceDirect). Keywords used to search for literature in the journal include “Mental Health”; “Mental Illness”; and “Telemedicine.” The kinds of literature are includedif they meet specific criteria,such as (1) written in English, (2) published betweenthe years 20122022, and (3) relevant to the topic. Studies are excluded if they are (1) written with incompatible languageor written beforethe year 2012 and (2) not correlated to the aim of this study.
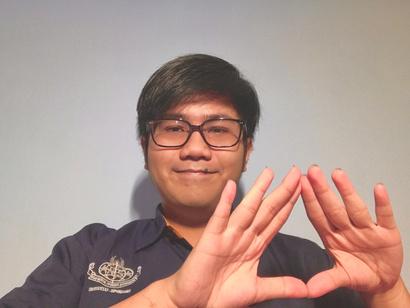
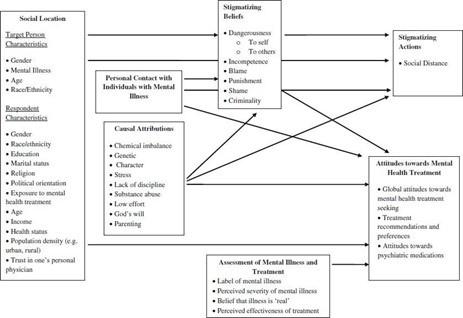
Figure 1 shows the thinking method from an identified correlated factor of mental health until the solutionrelating to telemedicine for mental illness.
There are many problems related to the proper treatment for mental health problems, such as bad social stigma about the mentalhealth problems, dangersof mental health problems that can refer to suicidal attempt, lack of proper facilities to treat mental health problems, and also there are some reasons that lower patient’s desireto go to seek help.
People with mental disorders struggleto recover from their illness,but society stigmatizes them.
Stigma shapes a lousy image of mental disorders. Second, it also causes people with mental illness to lose self-esteem and effectiveness and prevents them from seeking medical help for their clinical conditions. Therefore, stigma could prevent someone from going to health facilities becausethey are frightened about people’s opinions.Stigmatization could lead to creating barriers that prevent someone from seeking help. They find it difficult to have supportand trust from their surroundings. 5
Figure 2 show the correlation between stigma and other factor related to mental illness. The picture is fully taken from Parcesepe AM, Cabassa LJ. Public stigma of mental illness in the United States: A systematic literature review. Administration and Policy in Mental Health and Mental Health Services Research. 2013.
Some of the side effects of mental health medication include nausea, headache, changesin appetite, dry mouth, increased urination, change in libido, irritability, blurred vision, and drowsiness. Other side effects can occur; each person’s body and brain chemistry is unique, and it is impossible to predict how a given medication will affect someone or how well it will work. People prescribed these medications should regularly communicate with their doctors and notify them of any side effects.
In the short-term, mental health problems can cause people to be alienated from their peers because of perceived unattractive personality traits or behaviors. They can also cause anger, fear, sadness, and helplessness if the person does not know or understand what is happening. In the long term, mental health disorders can cause a person to commit suicide. According to the National Institute for Mental Health, more than 90% of people who commit suicide have depression or another mentaldisorder.
Today’s maintenance treatments for mental illnesses are complex for the clinician because his responsibility for patient adherence goes beyond simply making an accurate diagnosisand choosing medicine.Therefore, the treatmentfor mental illnessis still ineffective.6
Too many people with mental illness do not seek professional help, but it remains unclearwhy people with clinically relevant mental illness chooseto self-manage mentalhealth. It is considered relatedto stigma. They do not think they need it. Their condition makes it hard, there are practical issues, and they are scared of treatment.7
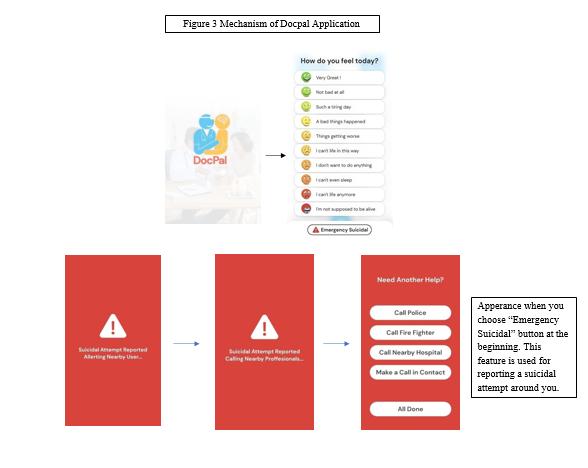
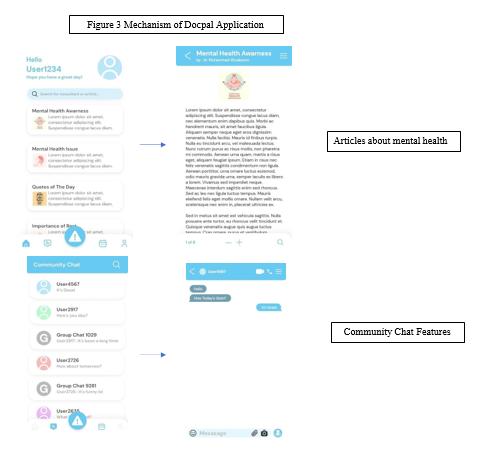
The lack of accessible emergency facilitation to treat mental health disorders and the terrible stigma in society about people who have mental health disorders make many people with the diseasenot appropriately treatedand lead to a fatal situation. We believe that using telemedicine to help treat these problemswill be a good solutionin this digital era. Telepsychiatry is a method that provides psychiatrists to communicate with people from a distance. We propose a solution using a telepsychiatry called a Docpal Application. Through Docpal,we will provide some features,which consist of :
1) Crisis hotline, which provides quick access to Indonesia’s suicide hotline. The application will connect with a locationtracker or GPS (Global Positioning System) on the user’s smartphone. If an emergency needs a fast community helper, we will offer this feature to prevent a suicide attempt.
This feature will connect to the device of police, health facilitator, mental health center, and the suicide prevention community. The application will alert the nearest facilitators that there was a suicidaltrial near them.This feature aims toreduce the suicide rate in Indonesia.
2) Consultation service with many choices of professional psychologists and psychiatrists. This feature will give a free trial consultation. Therefore, if the patient does not feel comfortable with the helper, they are free to change it. This feature aimsto help the users find the exact helpers they need, and by that, the consultation will be sustained in the future with a better result for the patient.
3) Information and planner to maintain users’ mental health. This app will facilitate a media to seek users’ hobbies and interests more to keep users’ minds stable. This featurealso gives a challengeor planner to help users know more about themselves.
4) Community chat is a feature that helps the users find friends or community going through situations with them. Through this feature, we hope that someone who has the illness will feel that they are not alone and will think that many people out there are also fighting the disease they have.
1. When users open the app, there will be a mental health pain scale questionnaire that they have to fill out. Besides that, there will be an emergency suicidal call button.Users should selectthis button if users are not usingit as a patient but as someonewho wants to report a suicidal attempt near them.
2. After choosing the scale, the app will direct the users to a different part of the app basedon the mental health scale.
3. The mild category. The app will direct to the consultation service, the communitychat, other features,including information about mental healthand planning.
4.The moderatecategory. The app will direct the users to three options: emergency, consultation service, and community chat.
a. The emergency will work the same as explained below
b. If the users choose the consultation service by choosing the option, there will be a question that asks what kind of topic they want to consult. After that, a choice of helpers will show essential data such as track records that might help the users choose the right one. After choosing, there will be a free consultationfor 20 minutes, and the app will charge it after 20 minutes.
c. The community chat will be divided into a similarity of the common problems they want to share.
5.The severe category. The app will direct the users to the crisis hotline’s emergency service.The app will connect the users with someone, and the users will do a conversation with the professionals to prevent a suicide attempt that might happen inthe worst case.
If the users suddenly lose the conversation and the professionals are sure there might be a possibility the user will attempt suicide, the suicidal alarm will alert the nearest people from the community or health facilitator to check them. This mechanism alsoworks on the emergency suicidalbutton which at the beginning of the app.
To make this solution applicable and able to achieve the objectives, we have to propose this idea and collaborate with the Ministryof Health, police, health facilitators, and the community to socialize this to society.
There are still many people with mental health disorders who are not appropriately treatedand ended up in a fatal situation. This condition is due to a lack of awareness, accessible media, and the stigma that airs in society. Using telepsychiatry will make access to treat and prevent mental health issues easier. Docpal will provide two critical features to support mental health disorders: a crisis hotline and a consultation service. We hope that through this application, emergency and non-emergency cases of mental health disorders could be treated, and the suiciderate will be decreased.
We hope that this projectcan be helpful for the surrounding environment in today's onlineworld and that this project can be released. We will pay close attentionto every usage detail and become supervisors in this Docpal application. In addition, we also expect support from the university in the sustainability of this project. We also hope to get approval from the local government and can be recommended by the nearesthealth facilitators and other organizations that focus on mental health disorders. Also, hopefully, we can partner with doctors, especially those in the psychological field, to become consultants in this application. In our opinion, various applications are needed to support telemedicine at this time and especially for those engagedin mental health.
The authors acknowledge all sources used for information and data provided concerning mental health problems worldwide. The authors would like to thank AMSA-Indonesia and AMSA- Universitas Diponegoro for the opportunity to write this paper. The authors would also like to thank Prudence Lucianus for the guidance, revisions, and feedback on making this white paper and video. Authors report there is no potential competing interest in the making of this white paper.
1.Centersfor Disease Control and Prevention. Health-related quality of life (HRQOL):Well- being concepts. Reference from https://www. cdc. gov/hrqol/wellbeing. htm. 2016.
2.WorldHealth Organization. Depression and other commonmental disorders: global health estimates. World Health Organization; 2017
3.Indrayani YA, Wahyudi T. InfoDATIN Pusat Data dan Informasi Kementrian Kesehatan RI: Situasi Kesehatan Jiwa di Indonesia. Pusat Data dan Informasi Kementrian KesehatanRI. 2018.
4.Tsugawa S, Kikuchi Y, Kishino F, Nakajima K, Itoh Y, Ohsaki H. Recognizing depression from twitter activity. InProceedings of the 33rd annual ACM conference on human factors in computingsystems 2015 Apr 18 (pp. 31873196).
5.HartiniN, Fardana NA, Ariana AD, Wardana ND. Stigma toward people with mental health problems in Indonesia. Psychologyresearch and behaviormanagement. 2018;11:535.
6.Carvajal C. Poor responseto treatment: beyond medication. Dialoguesin Clinical Neuroscience. 2022 Apr 1.
7.Stolzenburg S, Freitag S, Evans-Lacko S, Speerforck S, Schmidt S, Schomerus
G. Individuals with currently untreated mental illness: causal beliefs and readiness to seek help. Epidemiology and psychiatric sciences.2019 Aug;28(4):446-57.


Ikut lomba-lomba di AMSA tentunya menambah ilmu dan pengalaman yang unik. Lomba yang diadakan macam-macam dan tidak ada ruginya untuk coba ikut berbagai lomba, baik dari tingkat yang paling dekat dulu--misal mulai dari universitas, distrik, sampai nasional dan internasional). Dari awal aku masuk di AMSA, aku sudah sering ikut berbagai lomba terutama di bidang poster publik, dan awalnya pun belum pernah masuk final ataupun menang, tapi aku terus mencoba aja, sampai akhirnya di lomba terakhirku, yaitu AMSA International Summit yang diselenggarakan oleh AMSA-International cabang Public Poster, dengan bantuan serta dukungan dari teman-teman AMSAUndip khususnya RnA, aku berhasil memperoleh juara 1.
Jadi, jangan ragu teman-teman untuk ikut lomba! Apalagi sekarang RnA sudah menambah banyak program untuk memfasilitasi teman-teman yang ingin ikut lomba, jangan disia-siakan yaa!
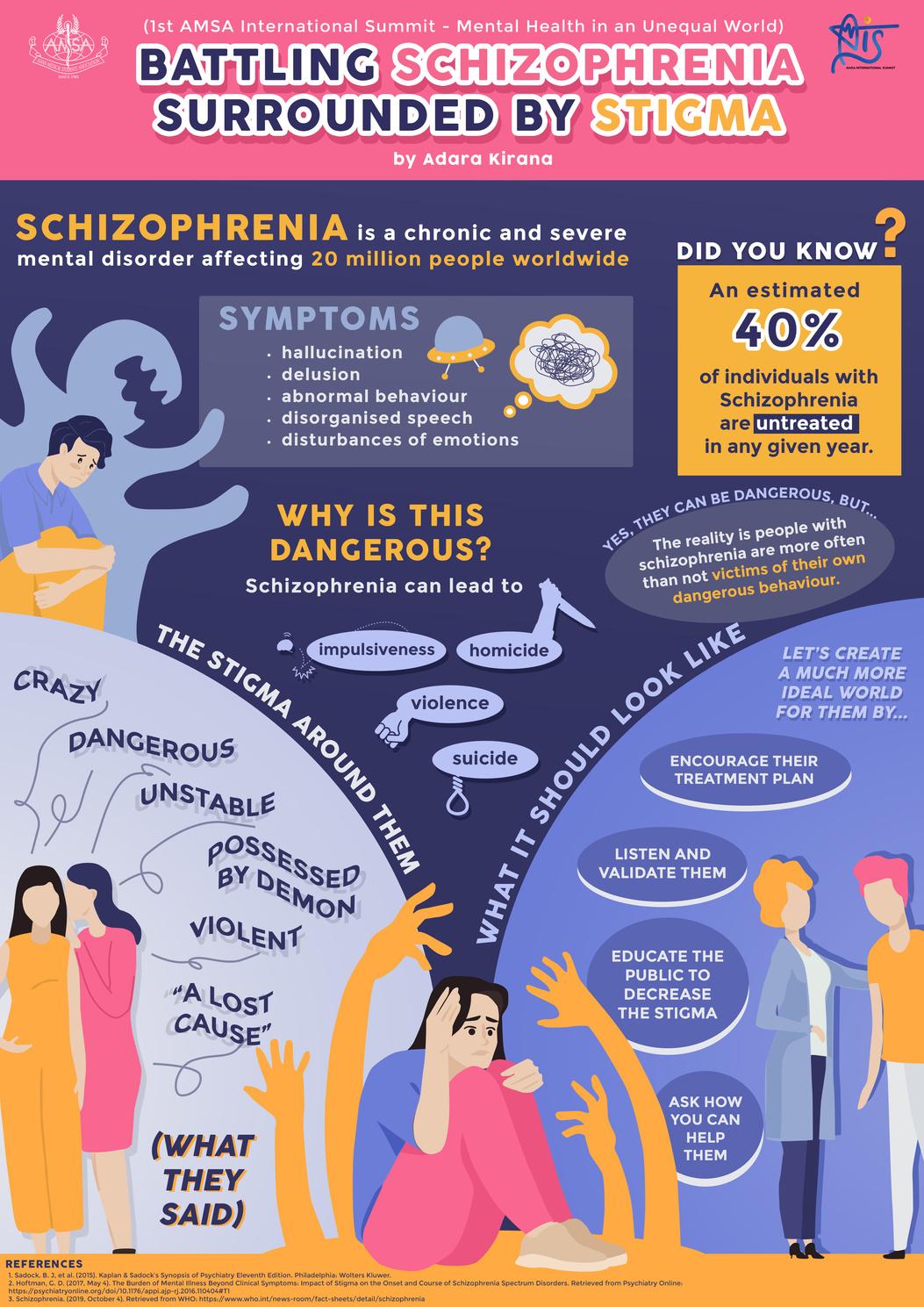


Jujur saja, sejak saya bergabung di AMSA-Universitas Diponegoro, saya tidak tahu apa itu IMSTC dan apa saja kompetisinya. hingga akhirnya seorang teman saya merekomendasikan saya untuk mengikuti lomba fotografi di IMSTC. setelah membaca lebih jauh akhirnya saya mengerti tentang IMSTC dan saya merasa tertantang karena ini adalah kompetisi pertama saya di AMSA, bahkan kompetisi pertama saya ketika masih kuliah. Awalnya mungkin terasa sulit hanya karena temanya telemedicine. Seperti yang kita tahu, tidak banyak hal menarik yang bisa difoto dengan tema telemedicine. Karena itu, saya mencoba berpikir out of the box dan bereksperimen sedikit, pada akhirnya saya sangat puas dengan hasilnya. dan saya tidak berpikir saya akan sampai ke tempat ketiga. terima kasih banyak IMSTC dan AMSA Indonesia telah mengizinkan saya berpartisipasi dalam kegiatan ini. Saya tidak akan pernah melupakan pengalaman yang luar biasa ini.
Background: Telemedicine is a health service based on information technology. With telemedicine, patient can consulta doctor without the need to meet in person.Since the COVID-19pandemic, people are required to limit activities outside home and encouraged to do all work from home. Starting from work, school, everything is done from home, including health services. Society began to introduce telemedicine. Some of the advantages of telemedicine are ease of access,saving time, and preventing the transmission of COVID-19
Description & philosophy: Despite the advantages, telemedicine also has disadvantages. Telemedicine cannot be applied100% because health services must be objectiveand require physicalexamination that’s directlyexamined to the patient. Without a real physical examination, a fatal misdiagnosis can occur. A disease diagnosis requires history and physical examination component. Although from the history itself, 60% of the diagnoses can be known, and physical examination completes 40% of the accuracy of the diagnosis. Without physical examination, misdiagnosis is very likely.Health services actually doesn’t treat patient's physique, but also patient's mental. With direct interaction from doctor, a patient can feel better because he gets "tender loving care" as well as direct attention from someone. It will give positive suggestions and a senseof security. Impact: By its virtue, the interaction between doctor and patientrequires direct contact.Because the treatmentdoesn’t necessarily only doctors give medicine. There are other factors in the form of suggestion, a sense of security, and trust. A person whose sick doesn’t only recover using medicine. Sometimes even without medicine can be cured just because of suggestions. With direct contact, patients feel satisfiedand get real empathy.
Conclusion: Although telemedicine is effective for some casesthat aren’t seriousand urgent, a health servicestill requires directcontact, that’s what distinguishes a "real doctor" from a "witch doctor".
Keywords: Contact, Doctor, Examination, Telemedicine

