KEEP YOUR MEDICARE BILLING PRIVILEGES INTACT 12
SNEAK PEEK AT THE 2025 AOPA NATIONAL ASSEMBLY EDUCATIONAL SESSIONS 22
ENTREPRENEUR SHARES HER O&P STARTUP JOURNEY 30


KEEP YOUR MEDICARE BILLING PRIVILEGES INTACT 12
SNEAK PEEK AT THE 2025 AOPA NATIONAL ASSEMBLY EDUCATIONAL SESSIONS 22
ENTREPRENEUR SHARES HER O&P STARTUP JOURNEY 30

Researchers test promising new strategies for combating phantom limb pain P.16

THE PREMIER MEETING FOR ORTHOTIC, PROSTHETIC, AND PEDORTHIC









September 3–6, 2025, for an ideal combination of top-notch education and entertainment at the 108th AOPA National Assembly in Orlando, FL, at the Orange County Convention Center (OCCC).










EXHIBITS EDUCATION NETWORKING






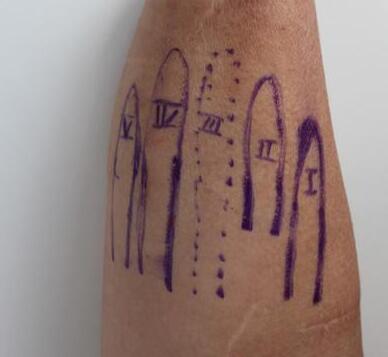
Naked Prosthetics offers four functional, high-quality finger prostheses:


®
A body-driven prosthesis designed for finger and partial-hand limb difference at the middle or distal phalanx. The design of this device anatomically matches the PIP and DIP joints so it operates predictably and naturally.
®
A body-driven prosthesis designed for finger and partial-hand difference at the proximal phalanx of digits two through five. Adding an MCPDriver restores digit length to help recreate natural grip patterns.
A body-driven prosthesis designed for finger and partial-hand limb difference at the proximal phalanx of the thumb. The addition of a ThumbDriver can restore 2- and 3-point pinch, allow for secure medium and large diameter grasp patterns, and can increase fine motor/dexterity function.
® ®
A passive, positionable prosthesis designed for amputations proximal to the MCP joint of digits two through five. It is intended for use in conjunction with a custom socket fitted by a certified prosthetist. Adding a GripLock Finger can restore length and be a valuable tool for every day tasks.


Researchers are developing new, more effective strategies to combat phantom limb pain (PLP). Find out how targeted sensory reinnervation, tactile vibrations, phantom motor execution, and advances in osseointegration may lead to a lower incidence of PLP.
By JENNIFER DAVIS


Preview the most highly anticipated educational sessions planned for the 2025 AOPA National Assembly in Orlando in September. View highlights from the Clinical Care, Digital Care, Business, Technical, and Pedorthic Education Tracks, and start setting your itinerary.
Prevent your Medicare billing privileges from being revoked by following these suggestions.
to earn CE credits by taking the online quiz.


Meet Sydney Robinson, MEng, who co-founded Vessl Prosthetics three years ago to develop socket fit solutions and design innovative technologies for prosthetic patients.
Find out how Sara Beyler, CO, LO, helped a young patient with Type II spinal muscular atrophy learn to stand and move throughout his home—with the help of specialized care and KAFOs.
in Texas, Pennsylvania, Georgia, Oregon, and more


FASTPro adapters provide exceptional flexibility in a compact design, featuring up to ±0.45 inches of horizontal slide adjustment, up to ±12° of angular adjustment, and a full 360° of rotation.
• 3 proximal alignment options
• 2 distal adapters
• Choice of aluminum or titanium
President
Rick Riley
O&P Boost, Bakersfield, CA
President-Elect
Kimberly Hanson, CPRH Ottobock, Austin, TX
Vice President
Matt Swiggum Proteor, Tempe, AZ
Treasurer
Chris Nolan
Immediate Past President
Mitchell Dobson, CPO Hanger Clinic, Austin, TX
Interim Executive Director
Teri Kuffel, JD
Arise Orthotics & Prosthetics, Spring Lake Park, MN
DIRECTORS
Jeff Erenstone, CPO
Mountain Orthotic and Prosthetic Services, Lake Placid, NY
Deanna Fish, MS, CPO Orthomerica Products Inc., Orlando, FL
Arlene Gillis, MEd, CP, LPO International Institute of Orthotics and Prosthetics, Tampa, FL
Adrienne Hill, MHA, CPO, LPO, FAAOP Kennesaw State University, Kennesaw, GA
Shane Kelly
Thuasne North America, Bakersfield, CA
Jim Kingsley
Hanger Clinic, Oak Brook Terrace, IL
Andrew L. Steele, MBA, CPO, LPO Clark & Associates Prosthetics and Orthotics, Waterloo, IA
Shane Wurdeman, PhD, CP, FAAOP(D) Research Chair
Hanger Clinic, Houston Medical Center, Houston, TX
AMERICAN ORTHOTIC & PROSTHETIC ASSOCIATION (AOPA)
330 John Carlyle St., Ste. 200 Alexandria, VA 22314 Office: 571-431-0876 Fax: 571-431-0899 AOPAnet.org
EXECUTIVE OFFICES
Teri Kuffel, JD, interim executive director, 571-431-0876, executivedirector@AOPAnet.org
Akilah Williams, MBA, SHRM-CP, director of finance and strategic operations, 571-431-0819, awilliams@AOPAnet.org
HEALTH POLICY AND ADVOCACY
Joe McTernan, director of health policy and advocacy, 571-431-0811, jmcternan@AOPAnet.org
Devon Bernard, assistant director of coding and reimbursement services, education, and programming, 571-431-0854, dbernard@AOPAnet.org
Morgan Fabber, MPH, manager of state and federal advocacy, 571-431-0814, mfabber@AOPAnet.org
MEETINGS & EDUCATION
Ashley Vande Bunte, CMP, director, meetings and education, 571/431-0860, avandebunte@AOPAnet.org
Kelly O’Neill, CEM, assistant director, meetings and exhibitions, 571-431-0852, kelly.oneill@AOPAnet.org
Jules Gohng, meetings and education coordinator, 571-431-0843, jgohng@AOPAnet.org
MEMBERSHIP & COMMUNICATIONS
Joy Klapp, director of communications and membership, 571-431-0817, jklapp@AOPAnet.org
Betty Leppin, senior manager of member services, 571-431-0810, bleppin@AOPAnet.org
Madison McTernan, coordinator of membership and communications, 571-431-0852, mmcternan@AOPAnet.org
AOPA Bookstore: 571-431-0876
Reimbursement/Coding: 571-431-0833, LCodeSearch.com
O&P ALMANAC
AOPA, publisher
Josephine Rossi, editor, 703-662-5828, jrossi@contentcommunicators.com
Catherine Marinoff, art director, 786-252-1667, catherine@marinoffdesign.com
Bob Heiman, director of sales, 856-520-9632, bob.rhmedia@comcast.net
PUBLISHER AOPA
EDITORIAL MANAGEMENT CONTENT
COMMUNICATORS LLC
ADVERTISING SALES RH MEDIA LLC
DESIGN & PRODUCTION MARINOFF DESIGN LLC
PRINTING SHERIDAN
O&P Almanac (ISSN: 1061-4621) is published bimonthly by the American Orthotic & Prosthetic Association, 330 John Carlyle St., Ste. 200, Alexandria, VA 22314. To subscribe, contact 571-431-0876, fax 571-431-0899, or email info@ aopanet.org. Yearly subscription rates: $59 domestic, $99 foreign. All foreign subscriptions must be prepaid in U.S. currency, and payment should come from a U.S. affiliate bank. A $35 processing fee must be added for non-affiliate bank checks. O&P Almanac does not issue refunds. Periodical postage paid at Alexandria, VA, and additional mailing offices.
Postmaster: Send address changes to: O&P Almanac 330 John Carlyle St., Ste. 200, Alexandria, VA 22314.
Copyright © 2025 American Orthotic and Prosthetic Association. All rights reserved. This publication may not be copied in part or in whole without written permission from the publisher. The opinions expressed by authors do not necessarily reflect the official views of AOPA, nor does the association necessarily endorse products shown in the O&P Almanac. The O&P Almanac is not responsible for returning any unsolicited materials. All letters, press releases, announcements, and articles submitted to the O&P Almanac may be edited for space and content. The magazine is meant to provide accurate, authoritative information about the subject matter covered. It is provided and disseminated with the understanding that the publisher is not engaged in rendering legal or other professional services. If legal advice and/or expert assistance is required, a competent professional should be consulted.
Share your message with AOPA membership— approximately 9,000 orthotic and prosthetic professionals, facility owners, and industry personnel. Contact Bob Heiman at 856-520-9632 or email bob.rhmedia@comcast.net. Learn more at bit.ly/AlmanacMediaKit25.

Our first priority is to bring you reliable and accurate foot orthotics. We embrace continuous improvement to deliver the latest advances in technology. Customer service is at the heart of every decision we make. We work endlessly to help you be effective and efficient in your practice.
Because individuals with upperlimb absence experience a high prevalence of falls, researchers are investigating whether upper-limb absence alters recovery mechanisms in response to perturbations. A team from Northwestern University led a study of 10 upper-limb prosthesis users and 10 matched able-bodied control participants. Subjects completed a variety of treadmill tasks, including a steady-state walking baseline trial at 1 meter per second and 12 perturbation trials containing an unexpected, rapid treadmill belt acceleration and deceleration. Participants with upper-limb absence completed these tasks both with and without wearing their customary prosthesis.
Prosthesis users were found to exhibit greater whole-body angular momentum ranges than their control counterparts, in the sagittal plane. This response was significantly greater when participants with limb absence were not wearing their prosthesis.
“Perturbations may present a greater recovery challenge to people with transradial upper-limb absence partially due to a mass and inertia imbalance between the sound and impaired limbs when not wearing a prosthesis,” reported the researchers. They recommend holistic rehabilitation regimes, including both prosthesis and balance training, for upper-limb prosthesis wearers. The study was published in April in Human Movement Science
Infants diagnosed with deformational plagiocephaly experienced larger reductions in cranial vault asymmetry with longer wear times of cranial remolding orthoses (CROs), according to a new study.
Researchers at Shriners Children’s, Children’s Healthcare of Atlanta, and Shirley Ryan AbilityLab studied the wear patterns and results of 69 infants ages 3-18 months who were treated with a CRO for plagiocephaly. They compared self-reported CRO wear times, reported by caregivers, with actual wear times as measured by iButton temperature loggers. Self-reported wear times averaged 22-23 hours per day, while measured wear times were only 17-18 hours per day. “Results showed longer average daily wear increased effectiveness in CRO treatment of plagiocephaly,” concluded the study authors. “Increased sample sizing is required to determine if generalizable to brachycephalic and asymmetrical brachycephalic head shapes.” The study was published in April in Journal of Prosthetics and Orthotics
In a survey of 152 O&P professionals, 63% reported chronic, acute, or both types of pain. Younger and less experienced professionals were more likely to report pain. Activities like fabrication work, computer-based tasks, and frequent reaching above shoulder height correlated with the presence of pain.
Expanding the number and types of strategies available to manage daily residual limb fluid volume changes among belowknee prosthesis users may help improve socket fit, according to researchers from the University of Washington. The team investigated the effects of partial-doff frequency on residual limb fluid volume among participants in two controlled laboratory sessions.
The participants—transtibial prosthesis users—were fitted with a custom limb fluid volume monitoring device and a socket release-relock mechanism. Participants completed a series of lowand high-activity ambulation trials mimicking daily prosthesis use.
The researchers found that mean limb fluid volume measures from the anterior compartment of the residual limb were significantly different between the one- and three-partial doff experimental protocols. “Partial doffing may offer prosthesis users an alternative means to accommodate limb fluid volume changes,” concluded the UW researchers. “More frequent partial doffing appears to better mitigate limb fluid volume loss when compared to less frequent partial doffing.” The study was published in April in Clinical Biomechanics

The AOPA Board of Directors announced that its contract with Teri Kuffel, JD, to serve as AOPA’s interim executive director has been extended an additional six months to Dec. 31, 2025.
Kuffel stepped into the role Jan. 1, 2025, following the resignation of AOPA’s previous executive director, Eve Lee, MBA, CAE. Over the past four months, Kuffel has effectively managed AOPA’s staff and daily operations while also increasing collaboration with the sister organizations and the association’s engagement with its members.
“As AOPA president, I have had the opportunity to communicate with Teri on a regular basis. Teri’s innate understanding of the O&P profession, her proven and passionate abilities as a state and national advocate, as well as her eight years of volunteer service on AOPA’s Board of Directors, collectively bring high value to the organization and its members,” said Rick Riley, AOPA president. “By extending her contract, we have created a longer runway for Teri to work with the board and staff to align our programs, services, and strategies with the evolving needs and expectations
BY THE NUMBERS

of our members. By the end of summer, AOPA will have an updated strategic plan and refreshed vision for the future.”
As an attorney and co-owner of Arise Orthotics & Prosthetics in Minnesota, and as a former AOPA Board member, including serving as president, Teri is a respected leader in the O&P profession. She has actively engaged in federal and state legislative advocacy work, including the passage of O&P licensure and So Every BODY Can Move initiatives in Minnesota. With her background in law, organizational management, and O&P operations, Kuffel will continue to be an asset to AOPA as she leads the organization through this transition period. The Board is confident in her ability to maintain strong momentum and success in fulfilling AOPA’s 2025 goals and strategic objectives.
“The Board’s Executive Committee is exploring the timing and scope of our search for AOPA’s next executive director,” said Riley. “We plan to communicate our recruitment plans to members in September, with the intention of having a permanent leader in place by the beginning of 2026.”
If you have any questions, contact AOPA’s director of communications and membership, Joy Klapp, at jklapp@AOPAnet.org
Milo, a brown stoat who loves to play in the snow, has been named the 2026 Paralympic mascot. Born without a paw, Milo learned how to walk with his tail. Milo’s sister, Tina, is the Olympic mascot.

Adults with functional disabilities have a higher prevalence of diabetes, according to CDC researchers. The study, published in Diabetes Care in January, found that 11.2% of adults with disabilities have diabetes, compared with 5.8% of those without disabilities. The rate is 18.3% among those with moderate to severe disabilities.
“Prevalence of diabetes was higher among adults with any functional disability than without and increased with increasing number of disability types,” reported the CDC authors. “Adults with multiple disability types, or those who have difficulty with self-care or communication or other moderate to more severe disabilities, may benefit from diabetes prevention programs.”
In a separate study, CDC researchers found that diabetes deaths in the U.S. have fallen to some of the lowest rates in years. Death rates from diabetes peaked in 2021 at 31.1 deaths per 100,000 people. At that time, diabetes was the eighth leading cause of death.
More than one in five Medicaid enrollees have a disability, with the rate of disability among Medicaid enrollees rising steeply with age.
Research shows the COVID-19 pandemic may have made it harder for Americans to properly manage the disease. In the more recent study, the rate had fallen to 26.4 deaths attributed to diabetes per 100,000 people in 2024.

The durable medical equipment Medicare administrative contractors and the Pricing, Data Analysis, and Coding (PDAC) contractor have released a Correct Coding bulletin for code L6700: upper-extremity addition, external powered feature, myoelectric control module, additional electromyographic (EMG) inputs, patternrecognition decoding intent movement.
L6700 became effective April 1, 2025, and the predicate products for L6700 are Coapt’s Complete Control Gen2, Ottobock’s MyoPlus, and Infinite Biomedical Technologies’ Sense.
The bulletin states that L6700 describes an addition to an upperextremity prosthesis and has the following components/features:
• The capacity to gather, decode, and integrate simultaneous myographic signals from a minimum array of three EMG sites.
• The product’s machine learning algorithms recognize and simultaneously decode complex EMG patterns in determining an individual’s real-time movement intent. The product translates command signals into commands to direct functional motion of electric powered components.
• The product provides intuitive control of myoelectric prosthetic components, such as terminal devices, wrist units, elbows, etc.
The bulletin also introduces a code verification requirement for the L6700. Beginning July 1, 2025, the only items that may be billed using L6700 are those reviewed by PDAC and published on the PDAC Product Classification List.
Contact AOPA’s Joe McTernan at jmcternan@AOPAnet.org or Devon Bernard at dbernard@AOPAnet.org with any questions.
AOPA concluded its 2025 Policy Forum in May with more than 110 meetings with members of Congress and their staff. Eight three O&P professionals, patients, and advocates from 26 states participated in the comprehensive two-week lobbying effort targeting federal legislative priorities to strengthen the future of orthotic and prosthetic care.

Join a committee and become part of a dynamic community—where passionate professionals share knowledge, collaborate, and achieve more together than they could alone. Lending your voice, expertise, and energy to shape the future of AOPA and O&P.
The advocacy campaign began with a virtual educational session designed to prepare participants for congressional meetings, followed by a fireside chat featuring AOPA Interim Executive Director Teri Kuffel, JD, and Sen. Tammy Duckworth. Participants then conducted both in-person and virtual meetings with lawmakers on Capitol Hill, including 52 Senate- and 62 House-side meetings. Participants leveraged personal stories, clinical expertise, and data to demonstrate to Congress the profession’s role in restoring mobility, independence, and dignity to hundreds of thousands of Americans living with limb loss and limb difference.
Their lobbying effort centered on five key policy areas. First, advocates pushed for support of the Medicare Orthotics and Prosthetics Patient-Centered Care Act, legislation aimed at improving patient access, strengthening clinical care, and reducing fraud. Second, they sought fair coverage and reimbursement policies for orthotic and prosthetic services. The group also promoted increased federal investment in research funding and innovation, specifically targeting O&P-related research, clinical trials, and academic programs. Additionally, advocates discussed the potential impacts of tariffs on the profession and patients, while reinforcing the importance of O&P licensure and professional standards to ensure quality patient care.
The momentum from the Policy Forum as it works toward introduction of the Medicare Orthotics and Prosthetics Patient-Centered Care Act and addresses other legislative priorities. AOPA has encouraged advocates to monitor for updates on additional advocacy opportunities for the O&P profession and the limb loss and limb difference community.

Contact info@AOPAnet.org or 571-431-0876.


BrainRobotics has hired Margaret Swerdloff, PhD, as R&D engineer—advanced prosthetics and Benton Maglinger, MD, MS, as director of medical affairs. Swerdloff recently worked at Shirley Ryan AbilityLab, where she specialized in brain-machine interface technologies and prosthetic devices. Maglinger underwent medical training in the Harvard hospital network and has significant experience in neurotechnology.
“These additions to our team show our dedication to prosthetic advancement with human-centered design,” said Brian Long, president of BrainRobotics. “Margaret and Benton share our vision of creating accessible technology that truly empowers the limb-different community.”

OPGA and Össur Americas have announced the recipients of two O&P grants designed to provide funding to O&P residents and certified orthotists or prosthetists that will allow them to attend and participate in two nonclinical events in the O&P profession.
Avery-Claire Littleton has been selected as the 2025 recipient of the Russell Walker CP, LP, Emerging Leader Grant. Receiving the grant “is an incredible honor that affirms my commitment to advocacy and inclusion in the O&P field. It’s a reminder that the work I’m doing matters,” said Littleton. “This grant gives me the chance to keep showing up for the people who inspire me every day, and I’m incredibly grateful for the opportunity to grow as a leader in this field.”

Nicole Bakovich has been selected as the 2025 recipient of the Todd Eagen Advocacy in Action Memorial Grant. “I am truly honored to be attending the events commemorating Todd Eagen and Russell Walker—two individuals whose compassion and advocacy clearly left a lasting legacy in the O&P profession,” said Bakovich. “Legislation changes are needed to provide the highest quality of care for our patients, and I am grateful to be a part of that. I’m beyond excited to be there to support, cheer on, and celebrate these incredible individuals’ accomplishments at the CAF Triathlon.”
Drew Hittenberger, CPO, passed away April 19. Hittenberger was a fourth-generation O&P professional: His great-grandfather was a leather craftsman and inventor who immigrated from Germany. His grandfather, Carl, founded the C.H. Hittenberger Co. in 1902, which became known as “Hittenberger’s” after World War II, under the leadership of his father, Herman C. Hittenberger. By 1975, Hittenberger’s had more than 100 employees and offices throughout Northern California. The family and their employees participated in leadership roles in AOPA, the Veterans Administration, ISPO, ABC, schools and universities, and affiliated organizations.

Hittenberger studied prosthetics at Northwestern University in Chicago and completed his clinical work at Rancho Los Amigos Hospital in Los Angeles. After receiving his CP certification, he became a lead researcher at Prosthetic Research Study in Seattle. He returned to the family company in California during a critical period of its expansion. One of his career highlights was traveling to Russia to join a team of prosthetists, U.S. Vietnam veterans, and Soviet soldiers who had fought in Afghanistan, where they collaborated in designing and rapidly delivering affordable, adjustable prostheses.
Hittenberger established his own independent practice in Petaluma, California. He conducted pioneering work in veterinary prosthetics, contributed to adaptive ski programs, and became a medical-legal consultant. His reputation for invention, compassionate care, humor, and generosity garnered many business, service, and humanitarian awards.
In honor of Drew Hittenberger, his friends and family have established the Hittenberger Family Legacy Fund offering annual scholarships for students enrolled in the Northwestern University Prosthetics-Orthotics Center. For details, contact Jordan Sund at 312-503-2706 or jordan.sund@northwestern.edu. To make a gift online, visit giving.nu/feinberg, select “Other,” and enter Hittenberger Legacy Fund—NUPOC.

Operate at optimum efficiency, retain quality staff, focus on patient care





Facing higher operating costs? Struggling to find and retain qualified employees? Wondering how your business stacks up in the current market?
The 2025 O&P Compensation, Benefit, & Operations Survey* is your opportunity as the business owner or manager of an O&P patient care facility to get the answers you need.
By completing the survey, you’ll gain access to essential insights that will help you address your top business concerns:
Managing higher operating costs
Maintaining profitability
Finding and retaining qualified employees
Understanding employee healthcare costs
Benchmarking compensation and benefits
But your participation doesn’t just help you—it strengthens the entire O&P profession by providing critical industry-wide data.

This year’s survey is even easier and quicker to complete with the additional improvements made to last year’s revamped survey. The survey is now broken into modules that can be assigned to di erent people and can be completed in multiple sessions with the save and return functionality.
After completing the survey:
Every organization will receive a FREE copy of the final reports providing financial and compensation benchmarks against which you can compare your own operations and compensation practices.
All participating organizations will also receive a confidential Company Performance Report that will compare your own performance against other O&P facilities most like yours.

Participant organizations will also be entered into a ra e to win one of 10 gift cards worth $500 each.

Didn’t get a link to the survey? Request one here
They survey is now open and will close on June 30. Final tabulated results available in September. Emails with links to access the survey have been sent.
Questions? Contact bleppin@AOPAnet.org
* For the second year, the survey will be conducted independently by Kai Analytics, a market research firm that compiles the results and ensures the confidentiality of data provided by each facility participant. AOPA only has access to the aggregate data to interpret industry trends.

COMPLETE THE SURVEY FOR A CHANCE TO WIN 1 of 10 $500 GIFT CARDS


BY DEVON BERNARD

Follow these suggestions to avoid losing your Medicare billing privileges
AOPA has received several requests for help because of a Medicare billing number being suspended or revoked. Many of these requests relate to failed site inspections as part of the revalidation process conducted by Novitas Solutions. Most of them have been the result of incorrectly interpreting the Medicare Durable Medical Equipment, Prosthetics, Orthotics, and Supplies (DMEPOS) Supplier Standards.
According to the Code of Federal Regulations, a supplier number can be suspended or revoked for any of 23 reasons. Most reasons may never apply to you, but it’s important to be aware of all of them.
In this month’s Reimbursement Page, we examine some of the reasons for suspension or revocation and explore how you can guard against them.
Noncompliance. The provider or supplier is determined not to be following the enrollment requirements described in this section, or in the enrollment application applicable for its provider or supplier type, and has not submitted a plan of corrective action. The provider or supplier also may be determined not to be in compliance if it has failed to pay any user fees as assessed.
An example of this type of noncompliance is allowing your insurance or your surety bond to lapse. If your liability insurer or surety bond holder notifies one of the National Provider Enrollment (NPE) contractors—Palmetto GBA or Novitas Solutions—of such a lapse, it will consider you in noncompliance; this could result in revocation if you cannot fix the situation in a timely manner— for example, by obtaining a new bond or new insurance.
Supplier conduct. The supplier, or any owner, managing employee, authorized or delegated official, or other healthcare personnel of the supplier, is excluded from Medicare, Medicaid, or any other federal
healthcare program, or is debarred, suspended, or otherwise excluded from participating in any other federal procurement or nonprocurement program.
To ensure compliance with supplier conduct rules, check all employees—new and old—to be sure they are not excluded from any federal programs. Visit the Office of Inspector General (OIG) exclusion list at exclusions.oig.hhs.gov. These checks should be done on a regular basis and not just at the time of hiring.
On-site review. CMS determines upon an on-site review that the supplier is no longer operational to furnish Medicare covered services, or the supplier has failed to satisfy any or all of the Medicare enrollment requirements.
In essence, this means you failed an on-site inspection. This may happen, for example, if an inspector came by for an
inspection and the office was closed during posted hours, or a sign was not visibly noticeable—an indicator that the location is “no longer operational.” To avoid such a situation, make sure your facility is always staffed and open during posted hours, and ensure your company’s name and hours are clearly visible. Also, document the names of any inspectors, their questions, and any information or documents you provided to them during or after the visit.
Misuse of billing number. The provider or supplier knowingly sells, or allows another individual or entity to use, its billing number.
To avoid this scenario, do not share or allow others to use your supplier number to bill for items and services. There are some exemptions—such as when setting up valid contractual agreements, or when a business is sold and there is a change of ownership.
Failure to report. The provider or supplier did not comply with the reporting requirements.
This means that you did not notify Medicare within 30 days of any adverse legal action or of any change in your practice location—for example, change of address, change of ownership, change of hours, changes in products/services, etc. If you make any changes to your enrollment form, you must notify Medicare within 30 days of that change.
Failure to document or provide CMS access to documentation. The provider or supplier did not comply with the documentation or CMS access requirements.
You must maintain all documentation for seven years from the date of service, and you must be able to provide this documentation upon request from CMS or any of its approved contractors.



Sizes: 7, 7.5 - 11.5, 12-17
Widths: D, 4E, 6E, 9E

Billing from noncompliant locations. CMS may revoke a provider’s or supplier’s Medicare enrollment or enrollments, even if all of the practice locations associated with a particular enrollment comply with Medicare enrollment requirements, if the provider or supplier billed for services performed at or items furnished from a location that it knew or should have known did not comply with Medicare enrollment requirements.
Be sure that each location where you see and treat patients has its own supplier number and meets all applicable Supplier Standards. Also be sure that each location submits claims using its own supplier number.
Supplier Standard or condition violation. The DMEPOS supplier is noncompliant with any provision in § 424.57(c). This is just a fancy way of saying you didn’t comply with all of the DMEPOS Supplier Standards—and this is the most likely reason for the revocation of billing privileges.
Supplier Standards 4 and 5 are the most frequently misinterpreted standards. Under Supplier Standard 4, you must be able to demonstrate that you have an adequate inventory on hand or the ability to obtain an adequate inventory to fill orders. You are not required to have formal contracts with all of your vendors; a purchasing agreement or a credit letter is acceptable. However, the document should contain, at minimum, an established credit limit, credit terms, the identities of both companies, and the length of the contract or agreement. If any of these elements are missing, consider obtaining a letter from your sales representative or supplier indicating that you are a valued customer with a stable payment history and are in good standing. Make sure you are able to provide copies of past invoices indicating products and supplies being purchased. Finally, show the inspector any inventory of off-the-shelf items you may have in stock and your fabrication labs with any raw materials required for custom fabrication. Make a routine check of the OIG exclusion list to ensure any company with which you have a contract is not excluded from Medicare or any other federally funded program.

According to Supplier Standard 5, you must advise beneficiaries that they may rent or purchase inexpensive or routinely purchased durable medical equipment (DME) and let them know about the purchase option for capped rental equipment. This standard will typically not apply to an O&P supplier because O&P items do not have a rental option, as they are not designated as capped rental items. In addition, the standard directly calls out DME and does not mention orthotics and prosthetics. However, a site inspector may ask to see a form that you use to notify patients about the rental option. The NPEs do have a notification form to download and place in your operations manual to demonstrate that you have a form ready and available, if you ever elect to provide items designated as capped rental or DME. Also, review your most recent Medicare enrollment application and verify that you have not accidentally selected any items or services that would be considered DME or capped rental, or this standard could apply to you.
In general, prior to revocation, you will receive a notice outlining why your billing privileges are about to be revoked and when the revocation will take effect. However, your revocation is not 100% automatic, and you have the ability to appeal the revocation—and possibly prevent it from being finalized.
Your first option is to create and submit what is known as a corrective action plan (CAP). The CAP must be submitted within 35 days of the postmarked date on your revocation notice. Submit a CAP if you can show that the NPE has made a factual mistake in its review and/or the noncompliance issued cited in the revocation notice has been addressed and corrected. The CAP should state that you are in compliance with the standard in question and provide assurances that you intend to comply with the standards. In essence, the CAP should be used to acknowledge there was a problem or issue, and that you have addressed and fixed it. As an example, if your facility’s hours of operation were not posted, you could submit a CAP showing that you have now posted your hours, demonstrating your compliance.
In certain instances, a CAP will not be accepted, and you will have to go to the next option. For example, if your billing privileges are being revoked because the owner, director, or authorized or delegated official was found to be on the OIG exclusion list, a CAP will not suffice.
A decision on your submitted CAP is supposed to be made within 60 days of receipt. Recently, some individuals have reported that responses are taking much longer than 60 days. In these cases, you should consider contacting CMS and the NPE, and you may want to consider starting on the next option: filing a reconsideration or appealing the revocation.
You must file any reconsideration or appeal within 65 days of the postmarked date on your revocation notice. Your request should include a cover letter that states the issues or the findings of fact with which you disagree and the reasons for disagreement. Because the reconsideration will be done as an “on the record” review, submit all documentation needed to prove compliance with the Supplier Standards and all other issues identified in your notice. If you fail to submit all evidence before a decision is made, you may not be allowed to submit new evidence at a higher appeal level. In essence, the reconsideration states or argues that there was no problem or issues.
For example, if you are appealing a revocation based on not having contracts on file, you could provide your letters of credit or payment history (via invoices) or letter of good standing from your vendor and show that you have the

ability to provide the items you are billing to Medicare. In cases where they may not have asked for any of this information during the site visit, you could mention that as well.
The timeframe to file a CAP and receive a response may expire before you have a chance to file a reconsideration—in other words, you must file a reconsideration request within 65 days of the revocation notice regardless of whether you have filed a CAP, and a failure to file a reconsideration can result in the loss of any future appeal rights. So be prepared to file a reconsideration request along with your CAP; it is acceptable to submit both.
A decision on your reconsideration should be made and issued within 90 days. If your reconsideration is not successful, you still have the option of an administrative law judge review and then a Departmental Appeals Board review, as you would with a claim denial appeal.


No one wants to go through the hassle, hurdles, time, and expense of having their billing privileges revoked, so make sure that you and your staff are familiar with the Medicare Supplier Standards, Medicare enrollment requirements, and reimbursement policies, and always keep an eye out for announcements and mailings from CMS and its contractors. Don’t let important notices get buried or lost. Most importantly, respond to any notices in a timely manner. If you are an AOPA member and are having issues with supplier number revocations, please call and let us help you. Reporting issues also helps AOPA identify any patterns and address these issues with the appropriate officials.

Devon Bernard is AOPA’s assistant director of coding and reimbursement services, education, and programming. Reach him at dbernard@AOPAnet.org






Story COVER STORY BY
JENNIFER DAVIS

Researchers are deciphering the mysteries of phantom limb pain, unlocking new treatments
Two of the most significant challenges facing individuals with limb loss or limb differences are so closely intertwined that solving one may unlock the solution to the other.
Phantom limb pain (PLP)—the perception of pain or discomfort in a limb that is no longer there—is prevalent among many individuals with limb loss and greatly impacts quality of life. Simultaneously, the limitations of prosthetics and difficulty in adjusting to a prosthesis lead many amputees to abandon them. But researchers are making substantial strides in understanding how PLP works, what can be done to facilitate embodiment of a prosthetic limb, and how the two goals may complement each other, resulting in improved treatments.
Each year more than 500,000 individuals lose limbs or are born with a limb difference in the United States, according to a study commissioned by the Amputee Coalition. The study reports that 95% of people who experience limb loss also experience residual limb pain, phantom limb sensation, PLP, or a combination of these. PLP is most common, affecting nearly 80% of this patient population.
f Phantom limb pain (PLP), or the perception of pain or discomfort in a missing limb, is reported as a problem among approximately three-quarters of the limb loss population.
f Some researchers are studying ways to alleviate PLP among individuals with upper-limb absence using targeted sensory reinnervation.
f Another novel system, which leverages tactile vibrations and sensors to transmit
While the cause of PLP isn’t fully understood, it’s believed that the loss of sensory feedback from the missing limb triggers a brain response that’s interpreted as pain, tingling, or pulling by the central nervous system. As a result, efforts to relieve PLP center around restoring or replacing sensory feedback from the missing limb to the brain.
Building upon more than a decade of study on targeted muscle reinnervation (TMR), a group of researchers from around the globe are looking at ways to alleviate PLP by rerouting sensory nerves from residual limbs in a way that can close the communication loop between the missing limb and the brain.
TMR, the process of directing severed nerve endings to nearby motor nerve branches in the residual limb, has led to better control of myoelectric prostheses. Targeted sensory reinnervation (TSR) redirects smaller sensory nerves from the residual limb to a patch of skin on the residual limb, reactivating them in specific areas and creating sensory pathways for the brain to associate with the missing limb.
feedback from lower-limb prostheses to patients’ residual limbs, is designed to enhance proprioception and reduce PLP.
f With phantom motor execution— an advanced form of mirror therapy—sensors attached to the residual limb help detect muscle activity and confirm when a patient is trying to make a movement, enabling users to learn to manipulate a phantom limb on a screen and potentially alleviate pain.
f Researchers are studying how advancements in osseointegration—which allows for prostheses to attach directly to bone and eliminates the need for a socket—may help reduce phantom pain.
f Reducing PLP among individuals with limb loss will likely lead to greater acceptance and use of prostheses.

representations of the limbs in the somatosensory cortex,” according to Saphenus Medical Technology, which launched its Suralis tactile vibration system commercially in the U.S. last year.
Italian plastic surgeon Alexander Gardetto, who serves as chief medical officer of Saphenus Medical Technology, performs the TSR procedure, and his patients’ results were published this year in the Journal of Clinical Medicine. Diane J. Atkins, OTR/L, FISPO, an occupational therapist who has treated patients with upperlimb amputations for more than 40 years, met Gardetto at a Bionic Reconstruction Conference she helped organize in New York in 2023 and was drawn to his research team by TSR’s promise for restoring sensation and eliminating PLP. In 2024, she visited eight of his patients in Italy and saw the life-changing outcomes for upper-limb amputees who previously were unable to manage severe, unrelenting, nine-out-of-10 level PLP with opioids or other traditional medication regimens.
“They’d retreat into their homes and just be in pain,” says Atkins. “Each one that I met, however, following TSR, experienced the complete elimination of pain. I’ve never seen anything so extraordinary.”
Atkins, an assistant clinical professor in the Department of Physical Medicine and Rehabilitation at Baylor College of Medicine in Houston, says within two to three months following surgery, patients have been able to draw an image of a hand on their residual limb illustrating areas that, when touched, initiates the feeling of sensation in each of the phantom hand’s fingers.
All patients interviewed for the study reported being completely or nearly completely pain free and said they’d recommend the surgery to others.
“In my opinion, TSR represents a paradigm shift in PLP therapy and will play a central role in future multidisciplinary approaches to post-amputation care," Gardetto says. "Given the consistently positive outcomes we have observed—particularly in terms of pain reduction, improved proprioception, and embodiment—it is very likely that TSR will continue to gain traction internationally.”
The concept of using somatosensory feedback to reduce, PLP has been around for more than a decade. The brain “‘recognizes' the information as that of the lost limb and adopts pre-amputation
The Suralis system works with any prosthesis to transmit sensory feedback from the prosthesis to the patient’s residual limb. Using a sensor cover that fits over the prosthetic foot, Suralis detects contact between the foot and the ground and transmits that contact as vibration to the residual limb via a pad worn in the prosthesis socket, actuators applied directly to the skin of the residual limb, or a cuff worn outside of the prosthesis. The device allows the patient to “feel” the ground under their feet, recognize terrain, and experience the heel-to-toe rolling motion of typical walking once again.
Patients can generally handle stairs more deftly and walk and talk simultaneously without difficulty, according to Saphenus CEO Ranier Schultheis. “Within a few minutes, the person doesn’t have to look down.”
In a summary of 98 people with leg amputations who used its sensory feedback system for at least 30 days, Saphenus reported 81% improved their Four Square Step Test score, 86% did better on the Timed Up and Go test, and 74% realized better results on the 10-Meter Walk Test. When worn consistently, patients typically notice an additional benefit of dramatically decreased PLP within two weeks, or after about 20,000 steps, according to Saphenus.
“The amputees suddenly say the prothesis is getting warm, or they’ll look to check if it’s still there,” Schultheis says. “That’s the embodiment effect, and their pain goes down immediately then.”
In a 2018 German study on electrocutaneous lower-limb sensory feedback, most patients reported lower PLP intensities at the end of the day following feedback training while they previously experienced the most severe PLP late in the day.
Virtual reality (VR) and augmented reality technologies are bringing new utility to a previously established treatment method for PLP.
Phantom motor imagery—imagining the movement of a phantom limb without actually executing a movement—has been used to treat PLP with some success. Using mirrors to create the illusion that the phantom limb is moving as the patient performs exercises with their intact limb can be helpful in tricking the brain into thinking the missing limb is present.
“With mirror therapy, you can’t be sure if they’re imagining the movement or trying to actually do the movement,” explains Levi Hargrove, PhD, P. Eng., director of the Regenstein Foundation Center for Bionic Medicine at Shirley Ryan AbilityLab in Chicago.
Phantom motor execution (PME) takes the therapy a step further using sensors attached to the residual limb to detect muscle activity and confirm whether the patient is trying to make the movement. When the patient attempts to move the phantom limb, a corresponding virtual limb on a screen will complete the movement they’re attempting, providing real-time feedback. With practice, patients can learn to manipulate the phantom limb, and this mental connection typically results in reduced PLP.

Back in 2018, Abani Heller suffered a devastating ankle injury. After two surgeries, years of physical therapy, and multiple failed solutions, the pain still controlled his life.
That all changed when a local surgeon introduced him to the Re-Aktiv™ brace.
Custom-built and precisely tuned to his unique needs, the Re-Aktiv brace was the first—and only—solution that worked. The results? Instant relief.
Today, Abani is pain-free and back to everything he loves—from walking his kids to school to tearing up mountain bike


Shirley Ryan AbilityLab participated in the first major randomized, controlled clinical study of PME published in 2022, which showed participants averaged a 33% reduction in pain after just one week of PME, ramping up to an average of 50% midway through the 15-week study, and leveling off there. While the pain reduction was significant, there was only 10% difference in pain reduction between the test group and control group.
“The mechanism of why it’s working is similar for both imagery and execution,” Hargrove says. “What you really get from putting sensors on is adherence to the therapy. If you get slightly better results, and you can measure and confirm they’re actually doing the therapy and deliver data back to the patient and clinician—that is where I think the power is going to lie.”
“Phantom Motor Execution Therapy for Phantom Limb Pain: A 45-Participant Home-Based Connected Health Clinical Trial”
Levi Hargrove, PhD 2025 Thranhardt Award Winner
Friday, Sept. 5, 8 a.m.
To address a confounding factor that could impact the effectiveness of PME, Hargrove’s research program recently completed a study investigating the efficacy of entirely remote PME. Thus far, PME has largely been administered by trained therapists in clinical settings, which could result in a placebo effect.
“With less clinician interaction, if we still see a large effect from PME, that tells us there isn’t so much of a placebo effect, if any,” Hargrove says.
The study, which will be presented at AOPA’s National Assembly in September as part of the Thranhardt Lectures, provided an at-home VR-based PME tool for participants and telehealth instruction for its use prior to an eight-week treatment period. Forty-five individuals with either upper- or lower-limb amputations completed the study, and more than half experienced a reduction in PLP larger than the minimum clinically important difference.
Shirley Ryan AbilityLab’s at-home PME study also will prove useful in helping clinicians predict which types of patients are most likely to have a positive response to PME, according to Hargrove. By analyzing participants’ outcomes and comparing them with variables such as age, sex, pain level, and prosthesis use, researchers can determine who is likely to respond to treatment and make more tailored recommendations.
“If we can predict with high confidence that someone would respond, perhaps it may become a first-line treatment, rather than drugs with potential side effects,” Hargrove says. “Even if it’s 50/50 that they’ll respond—with so few side effects, we might want to give them a go anyway.”
Additionally, Hargrove says a commercial or clinical version of the at-home tool is in the works to allow occupational therapists and prosthetists to monitor and administer PME treatment in their offices. The tool provides clinicians with a dashboard and collects data to help them make treatment plans for patients.
Hargrove says osseointegration (OI) of prostheses is an exciting realm that could decrease PLP in the future. While traditional sockets suspend prostheses from the body through soft tissue and muscle, OI uses a titanium or steel implant anchored directly into bone as the attachment point for prosthetic devices.
As a result, the weight of the device is directly connected to the skeleton, which makes the prosthesis feel lighter. For some patients, OI eliminates problems associated with sockets, including restrictions to range of motion, friction, and resulting skin irritation. There’s also potential for reducing PLP both by encouraging increased usage of the prosthesis, which is shown to reduce PLP, and by possibly incorporating sensory feedback devices into the body through the implant.
Saphenus is currently working on ways to adapt its sensory feedback system for use in upper-limb amputation cases. Schultheis says eliminating PLP is the first step in improving the overall quality of life for amputees and is critical for encouraging the use of prostheses, particularly in upper-limb amputation cases. “It’s never accepted as a hand if you have phantom limb pain,” he says. “Most of the amputees put it away.”
As research continues to make prostheses feel more real to the patient, Schultheis says Saphenus is looking at ways to help patients feel things like humidity and temperature through visual feedback. Decreasing PLP while increasing sensory feedback is a critical combination required to help patients feel connected to their missing limb and their prosthesis. “You should love your prosthesis,” Schultheis says. “It’s so important, and getting this feedback could help so much.
Meanwhile, Atkins and Gardetto are preparing a research study in which up to 15 international Amputee Centers of Excellence will investigate how the transfer of sensory feedback, following TSR, could improve the utility of myoelectric hands and quality of life. In a daunting federal funding environment, Atkins says U.S. centers are pursuing funding to join centers in Europe, Canada, and Africa in the trial.
Re-establishing communication between the brain and a phantom limb offers new opportunities for reducing PLP while simultaneously increasing the acceptance of prosthetics. Both surgical interventions and vibrotactile feedback can decrease pain as individuals with limb loss regain “feeling” in their missing limb, potentially improving the functionality of prosthetics and providing a more intuitive user experience.
Jennifer Davis is a contributing freelance writer for O&P Almanac






Prepare now for this year’s AOPA National Assembly by previewing the latest in education
Orange County Convention Center





nvest in your O&P professional development by exploring the expansive slate of top-tier O&P educational sessions featured at the AOPA 2025 National Assembly in Orlando, Florida, Sept. 3-6. There’s something to inspire everyone at this year’s Assembly—whether you’re an O&P clinician, business owner, manufacturer, student, educator, researcher, or advocate. The National Assembly Planning Committee has been working at full capacity to bring you an engaging, enjoyable, and innovative experience that will broaden your knowledge and inform you of the latest trends and breakthrough topics. By participating in the wide range of sessions offering an estimated 100 CE credits within Clinical Care, Digital Care, Business, Technical, and Pedorthic Education Tracks, you’ll hear key perspectives from industry leaders during unique panel sessions, access timely updates and tips on cutting-edge technologies, improve your techniques to better serve patients, and boost your business practices.
Here’s a preview of just a few of the most highly anticipated educational sessions planned for the Assembly—be sure to consider them when developing your personal conference schedule.

This year’s Digital Track promises to be more comprehensive than ever, featuring groundbreaking sessions that will transform how you approach O&P care in the modern age.
Don’t miss the forward-thinking “Guided Comparisons of O&P-Specific Electronic Medical Record and Practice Management Systems” session on Thursday, Sept. 4, at 2 p.m. This insightful presentation brings together leading EMR/EHR companies, industry experts, and healthcare professionals to discuss the latest advancements, challenges, and innovations shaping the next generation of electronic medical records in the O&P profession. Attendees will explore groundbreaking developments in interoperability, artificial intelligence, patientcentered data management, and security enhancements that are driving efficiency and improving patient outcomes.
Friday | Sept. 5
8 – 9 a.m.
Hear the two abstracts selected as the award-winning “Best of Show” Thranhardt Lectures on Friday, Sept. 5, at 8 a.m. The prestigious Howard R. Thranhardt Award is given to the bestin-show clinical orthotic and prosthetic abstracts submitted to the annual National Assembly. The award was founded by an endowment from the Hanger Southeast Company in recognition of Howard R. Thranhardt, who was a lifelong learner and dedicated to the scientific advancement of O&P. The award is now supported by the O&P Foundation.
Prosthetics:
“Phantom Motor Execution Therapy for Phantom Limb Pain: A 45 Participant HomeBased Connected Health Clinical Trial”
Levi Hargrove, PhD, Shirley Ryan AbilityLab
This presentation will discuss the results of a completed clinical trial evaluating a portable, take-home phantom limb pain (PLP) management system using virtual reality (VR)-based therapy. The study assessed the effectiveness of an electromyography (EMG)-driven VR system in reducing PLP symptoms in individuals with upper and lower limb loss. Findings indicate a statistically significant and clinically meaningful reduction in pain over 32 weeks, highlighting the potential of VR-based therapy for long-term PLP management and telerehabilitation.
Orthotics:
“Improvement in Walking Speed and Reduction in Falls and Risk of Falling in SCI Patients in the C-Brace® Registry”

Later in the afternoon, “Bridging Innovation and Tradition: Implementing Digital Technologies in O&P Care and Education” will take place 4-5:30 p.m. This essential two-part session will guide you through successfully integrating digital scanning and modification tools into your practice while enhancing prosthetic and pediatric orthotic care. First, Stella A. Thai, CPO, from Mary Free Bed Orthotics & Prosthetics + Bionics, will share real-world lessons from Mary Free Bed’s implementation across 11 O&P offices, discussing workflow transitions, vendor partnerships, and how to overcome growing pains to achieve digital success.
Tyler Klenow, MBA, MSPO, CPO, FAAOP, Ottobock HealthCare LP; and Russell Lundstrom Jr., MS, Ottobock
The C-Brace Registry was designed to gather real-world safety and effectiveness data from patients fitted with a C-Brace. A sub-analysis of patients with spinal cord injury (SCI) revealed that the C-Brace improved walking speed, functional mobility, and balance confidence; reduced fall frequency; and improved QoL in these SCI patients after one year of use.

The second presentation will be led by Cara Negri, CP, LP, FAAOP, and Mary-Kate Dennis from Gainesville Prosthetics. Winner of the prestigious Näder Digital O&P Care Award, this presentation explores how residency directors can apply a hybrid approach that gives students and residents the best of both traditional manufacturing and 3D printing worlds. This session is perfect for clinical leaders, educators, and anyone navigating the digital shift in O&P.
On Friday, Sept. 5, at 4 p.m., “3D Printing in O&P: From Materials to Modern Workflows,” addresses the ever-growing knowledge gap in materials, methods, and workflows. This session explores iterative design and use of TPU (thermoplastic polyurethane) for 3D printing foot orthoses and liners, and features a candid panel of clinicians sharing real-world applications and lessons learned. Whether you’re just getting started or refining an existing process, you’ll gain practical insights into materials, technology, and strategies driving increased efficiency and optimal patient outcomes.

This year both the Technical and Pedorthic Tracks offer exceptional hands-on learning opportunities that you can immediately apply in your practice.
On Thursday, Sept. 4, at 10:30 a.m., “Custom Sandal Fabrication” is a first-hand opportunity to learn how to fabricate a custom Birkenstock-type sandal for complex foot deformities and special foot needs. Jason Wilson, CPed, will offer a live demonstration that promises to be both educational and immediately practical.
“The Most Practical Alternative to Custom Shoes: Relasting” on Thursday, Sept. 4, at 2 p.m., provides a practical live laboratory demonstration addressing a common clinical challenge. Custom shoes are expensive, time-consuming, and often unappealing to patients. This session teaches step-by-step relast modifications—widening commercially available shoes to accommodate foot deformities, particularly Charcot foot. Learn this valuable technique to provide faster, more cost-effective, and aesthetically appealing solutions for your patients.
At 4 p.m., adaptive sports enthusiasts should check out “Personalized Performance: Creating Bespoke Adaptive Sports Equipment,” a hands-on laboratory session featuring a streamlined, five-step process for designing and fabricating one-off adaptive sports devices. Attendees will learn each development stage—from assessing unique needs to rapid prototyping and final adjustments. Case studies will demonstrate how collaboration between engineers, clinicians, and athletes drives innovation in adaptive sports technology.
Friday | Sept. 5 2 – 3:30 p.m.
The Sam E. Hamontree, CP (E) Business Education Award was created to recognize the best business education paper, idea, and/or proposal submitted for presentation. This award is a counterpart to the Thranhardt Award given each year to the best clinical abstract. Presentations by the 2025 Hamontree award contenders will take place on Friday, Sept. 5, at 2 p.m.
The audience will be invited to cast their vote for the award winner. The award will be given to the winner on Saturday, Sept. 6, at 8 a.m. as part of the AOPA Annual Member Business and Awards Ceremony.
Dale Berry, CP, FAAOP, LP, Prosthetic Xpert Consultation SOAP charting was developed in 1974 and has remained unchanged over the past 50 years. In comparison, the regulatory requirements and prior authorization demands have increased dramatically. The presentation will introduce an updated SOAP charting paradigm to focus on capturing the key details and specifics for the current prior authorization landscape. The new SOAP process results in cleaner and more accurate communication to deliver more efficient and timely prior authorization approvals.
Curt Bertam, CPO, FAAOP, O&P Insight; Lesleigh Sisson, CFo, CFm, O&P Insight
Navigating a Unified Program Integrity Contractor (UPIC) audit can be a complex and daunting process for orthotics and prosthetics providers. This session will explore critical lessons learned from real-world UPIC audits, highlighting common documentation pitfalls, billing errors, and compliance risks that can trigger scrutiny. Attendees will gain practical insights on how to refine documentation practices, improve claim accuracy, and mitigate risk through proactive compliance strategies. By understanding these key takeaways, O&P providers can better prepare for audits, protect their reimbursements, and enhance patient care.


Saturday | Sept. 6, 11 a.m.
The fourth annual O&P Digital Care Showcase offers a hands-on opportunity to learn about computer-based 3D design software tools and their application to prosthetic, orthotic, and pedorthic patient cases. Exhibitors will present fabricated molds, devices, or 3D prints, and attendees will vote on the “Best in Digital Care Showcase” Award.

Safety takes center stage on Saturday, Sept. 6, at 9:15 a.m. with “Quantitative Safety Standards for Orthotic and Prosthetic Fabrication.” This crucial session outlines the need to standardize four main areas: fire safety, chemical handling and storage, fume extraction, and dust collection.
The 2025 Clinical Track is the largest in Assembly history, with more than 30 sessions on topics addressing patient care and clinical outcomes.
“Adjustable-Volume Prosthetic Sockets: Evidence, Reimbursement, and System Selection” brings together researchers, manufacturers, and reimbursement experts to provide a comprehensive overview of adjustable-volume technology. This panel discussion, set for Thursday, Sept. 4, at 10:30 a.m., will provide a summary of evidence for existing systems and examine the state of reimbursement after 1.5 years of Medicare coverage. Panelists also will present several systems and new evidence of their effectiveness.
At 2 p.m., “Bridging the Gap: Transforming Innovation Into Tangible Clinical Success” addresses the significant investment in the O&P field over the past decade, which has led to remarkable advancements in technology and clinical practice. This session convenes grant-funded researchers who are creating the next generation of device science and explores new and emerging innovations that will soon impact your clinical practice.
“Exploring the Opportunities of Sensory Feedback in Improving Usability and Functionality of Lower-Limb Prostheses” takes place on Saturday, Sept. 6, at 1 p.m. and presents new research on closing the sensory motor loop between artificial limbs and the human body. This symposium shares the speakers’ experience with more than 100 users of sensory feedback for prosthetic legs, demonstrating how noninvasive vibrotactile feedback improves gait stability, mobility, and user acceptance while reducing phantom limb pain and fall risk. Learn how sensory feedback increases prosthesis embodiment and reduces delivery time for faster rehabilitation, including outcome measures for assessing improvements.

Wednesday | Sept. 3 1 – 5 p.m.
Breastcare Fitting in an O&P Facility in 2025 and Beyond
Whether you’re just getting started or looking to grow, this session offers practical insights to help you and your clinic thrive. Learn the basics of providing breastcare products in an O&P setting. Discover how to successfully integrate a postmastectomy division into your orthotics and prosthetics clinic in a way that supports both profitability and patient care. This pre-conference workshop will walk you through the essential steps to getting started in providing both OTS and custom options and will cover ways to help you grow your practice within your community. Speakers will cover key business and clinical touchpoints, including how to build from a starter inventory pack, understanding credentialing and scope of practice, and identifying new opportunities to meet community needs through properly credentialed care. Pre-registration required ($50 for conference attendees; $100 for non-attendees).
CROSS™ is intended for mild to moderate knee hyperextension due to neuromuscular diseases or other injuries. The brace can also be used together with Allard AFOs when knee hyperextension is present together with foot drop.

ҋ One-hand donning and doffing.
ҋ Easy adjustment of hyperextension resistance, both through ROM stops and popliteal cross.
ҋ Smooth, low friction liner for comfort and easy application.


Saturday | Sept. 6
1 – 5 p.m.
This intensive four-hour workshop integrates didactic instruction with hands-on training to equip prosthetists with the essential knowledge and skills for managing bone-anchored prosthesis patients. Designed for both newcomers and experienced practitioners, the course covers foundational concepts and advanced techniques to enhance clinical proficiency.
The topics to be covered include the benefits and risks associated with the procedure, the available implants, acute and long-term care, connectors, componentry, maintenance requirements, alignment considerations, shower systems, non-invasive pain management strategies, and solutions to commonly encountered problems.
Pre-registration required ($75).
Does AFO stiffness matter? Evidence and clinic experience suggest it matters much more than we may think. The aim of this session is to discuss why AFO stiffness matters and how to leverage it to improve the treatment of patients. Speakers will discuss designs and technologies, research findings, evaluation and casting techniques, and keys to successful fittings that will equip you to level up your orthotic care.
Pre-registration required ($75).
This immersive, hands-on workshop will guide attendees through best practices for casting and modifying prosthetic sockets across all levels of upper-limb loss, including partial hand, transradial, transhumeral, and shoulder disarticulation presentations. Participants will gain practical experience with clinical techniques, surface anatomy landmarks, and strategies for optimizing fit and function. Whether you’re new to upperlimb care or looking to refine your skills, this session offers valuable insights and take-home techniques for immediate clinical application.
Pre-registration required ($75).

The Business Track delivers the practical knowledge you need to thrive in today’s changing healthcare landscape.
The popular “ALJ Mock Trial” returns for another year on Thursday, Sept. 4, at 2 p.m. This interactive simulation of an ALJ trial identifies key elements of the process and procedure from the viewpoints of the plaintiff (prosthetic provider), the defendant (Medicare), and the administrative law judge. The presentation focuses on identifying the most common errors, omissions, and misconceptions to provide real-life examples of effective trial procedures.
“Exploring Models for Orthotic & Prosthetic Care Within a Hospital System” will examine multiple models for providing O&P services within a hospital setting on Saturday, Sept. 6. at 1 p.m. Chrysta Irolla, MSPO, CPO, MS, from the Hospital for Special Surgery will discuss different forms of the vendor model, the internal department model, and hybrid approaches, helping you understand the strengths and challenges of each approach.
At 1:45 p.m., panelists speaking at the “Rightsizing an Effective Compliance Program” session will provide an in-depth review of the Seven Elements of a Compliance Program, offering practical strategies for tailoring each element to fit your organization’s unique size and needs. By aligning compliance efforts with your resources and risk profile, you’ll enhance efficiency, cost-effectiveness, and overall compliance effectiveness. Participants will leave the session understanding how to implement tailored strategies to adapt at their organization.
The 2025 AOPA National Assembly promises to offer these highlights—and so much more. It will take place Sept. 3-6 at the Orange County Convention Center and Hyatt Regency in Orlando. Visit AOPA’s Assembly website, www.AOPAassembly.org, to access registration information and stay updated on the full program as it develops. With Orlando’s vibrant atmosphere as your backdrop, prepare to be inspired, educated, and connected with the future of orthotic and prosthetic care!
*Also available in silicone





A one-of-a-kind seal-in solution.
LOW Ring: Available in Cushion or Locking Begins 5in from the center of the distal end.
HIGH Ring: Available in Cushion or Locking Begins 7in from the center of the distal end.
EXTRA LOW Ring: Available in Cushion or Locking Begins 3in from the center of the distal end.
It’s the only seal-in liner available in gel.
OptiGel has a smooth, soft texture that ensures gentle skin contact and a tailored fit around the residual limb.
It’s made with less constrictive fabric.
Outer knitted fabric combines strength, durability, and differentiated stretch for comfortable elasticity.
It’s available in both locking and cushion.
The locking feature ensures users are provided with a suspension that is secure, firm, and comfortable.


Engineer and entrepreneur shares what it takes to establish an O&P startup
The Fresh Faces column introduces readers to prominent O&P professionals who are making an impact with their contributions to the orthotics and prosthetics profession. This month, we speak with Vessl Prosthetic’s Sydney Robinson, MEng.
Sydney Robinson, MEng, is CEO and co-founder of Vessl Prosthetics, a company that is ready to launch its first product: an automatic volume management system designed to improve socket fit. Robinson earned a bachelor’s degree in mechanical engineering from Queen’s University and a master’s degree in biomedical engineering from Western University. She subsequently completed a Medical Innovation Fellowship, which brings together engineers, scientists, and doctors to innovate in medicine.
During her fellowship, Robinson discovered the “age-old problem in prosthetics,” poor socket fit. She co-founded Vessl in 2022 to develop socket fit solutions and design innovative technologies for prosthetic patients.
O&P Almanac: How did your engineering background prepare you for a career in O&P research and development?
Sydney Robinson, MEng: My background in engineering gave me the technical foundation I needed, but what really shaped my path toward O&P was a mix of curiosity about the human body and a pull toward
designing things that actually make people’s lives easier.
I was always drawn to how the body moves—how muscles, joints, and forces all work together. That fascination led me to biomechanics, and from there, to prosthetics. It felt like this perfect overlap between engineering and human experience. Learning how to apply user-centered design principles was a game-changer. It shifted my thinking from, “How do I make this work?” to “How will someone actually use this, and how can I make that experience better?”
That mindset has stuck with me ever since. I’m still constantly learning about the body, technology, and the real-world challenges people face every day with mobility. And that learning is what keeps me motivated in this field.
O&P Almanac: Why did you focus on socket fit during your fellowship?
Robinson: During my fellowship, our team interviewed over 60 clinicians across all areas of medicine and ended up with a list of more than 200 unmet medical needs. We knew we couldn’t tackle everything, so
we started narrowing it down based on a few things: where our skills aligned, what we were genuinely interested in, and what could become a viable business. After all, if you can’t commercialize a solution, it can’t help anyone.
Poor socket fit stood out right away. It’s a massive global problem that affects millions of people every day. But more than that, it impacts something deeply personal: how someone moves, lives, and feels in their own body. The industry was also ready for that kind of innovation with new L codes supporting adjustable sockets being a clear indicator that the industry saw value in these solutions. Plus, I have always been passionate about prosthetics, so I was thrilled that we decided to focus on socket fit!
O&P Almanac: How did Vessl get started?
Robinson: Vessl started as a collaboration between me and my co-founder, Oleksiy Zaika, during our time in the Medical Innovation Fellowship at Western University. We were immersed in clinical environments to identify unmet medical needs. One of our


assignments took us to a diabetes clinic, where we learned that diabetes is the leading cause of leg amputations. We noticed that many amputees struggled with prosthetic sockets that didn’t fit well throughout the day due to limb volume changes, leading to discomfort and reduced mobility.
This issue of poor socket fit was a recurring theme in our observations and interviews. It struck us as a significant problem that hadn’t been adequately addressed. We realized that our combined backgrounds in engineering and biomedical research positioned us well to tackle this challenge. We began developing a solution that could automatically adjust to limb volume changes, aiming to improve comfort and quality of life for amputees.
Our work led to the creation of Vessl Prosthetics, where we’re focused on developing adaptive prosthetic solutions like the Kinn Automatic Volume Management System. This technology is designed to provide a more comfortable and secure fit for prosthetic users, adapting to their needs throughout the day.
O&P Almanac: What are your current professional responsibilities?
Robinson: I wear a lot of hats, as you do in any startup. I lead our sales and marketing efforts, work closely with clinicians to make sure we’re building something that truly fits into their workflow, and help shape the
product strategy alongside our engineering team. I also spend time on the quality and regulatory side, since we’re getting close to launch, and everything has to be rock solid. When we need to, I raise funds from investors and through grants to support our growing company.
What I enjoy most is the variety. No two days are the same. One day I might be interviewing a prosthetist about their clinic workflow; the next I’m pitching to investors; and the next I’m reviewing our messaging for an upcoming event. Or, more often, that all happens in one day! But what keeps me going is the connection to real people, whether it’s the amputees who test our prototypes or the clinicians who’ve been asking for something like this for years.
O&P Almanac: You have said that you are passionate about engaging “people with lived experience” early in the design process—why is that so important?
Robinson: To me, involving people with lived experience early on isn’t just important, it’s essential. Especially in O&P, where you’re designing something that literally becomes part of someone’s body and daily life, you can’t afford to make assumptions. And especially when you are an able-bodied designer, like me; I need those perspectives to ensure my team and I are designing a device that people want to use, not just a fancy paperweight.

At Vessl, we bring amputees into the process as early as possible. We test ideas when they’re still rough sketches, we ask questions that go beyond function—like, “What do you think about the appearance of this device?” or “How do you see yourself using this on a busy day?” It keeps us grounded and helps us build tech that’s not just innovative, but actually useful. It’s easy to focus on your solution. Talking to people with lived experience keeps you focused on the problem—and that’s where the real impact happens.
O&P Almanac: You also have said that you are “obsessed with how the human body works.” How might that translate into future projects?
Robinson: It’s true, I’m totally obsessed with how the human body works. That fascination is what pulled me into this field in the first place, and it’s still what drives me. I’m constantly amazed by the way our bodies adapt, compensate, and respond to change, especially after something as life-altering as limb loss.
Even in my personal life, it shows up. I’m a recreational runner, and I’ve spent way too much time analyzing my own stride, watching slow-mo videos, and adjusting my form to avoid injury. I love understanding how movement works and how small changes can make a big impact.
At Vessl, that same curiosity shows up in how we think about designing with the body, not just for it. Our work on dynamic socket fit is just the beginning. I’m excited about future projects that continue to blend biomechanics, responsive design, and user-centered thinking, whether that’s in lower-limb prosthetics or even expanding into the whole patient-care pathway postamputation.
Long term, I want to keep exploring how we can make assistive devices smarter, more adaptive, and more in tune with the people using them. The body is this incredible system, and the closer our tools can come to understanding and working with it, the more empowering they’ll be.
O&P Almanac: What areas of O&P are ripe for more R&D by startups like yours?
Robinson: One area is managing heat in prosthetic sockets. For many amputees, this is a major pain point that doesn’t get enough attention. The heat buildup inside a prosthetic socket can be uncomfortable, lead to skin irritation, or even cause long-term issues like pressure sores. It’s a problem that affects a lot of people daily, but there are still very few solutions on the market that effectively address it.
We know that heat is a natural byproduct of friction, especially in a confined space like a prosthetic socket. But as much as
prostheses have evolved in terms of fit and functionality, heat management has been a bit of an afterthought. That’s where I think startups like Vessl can make a big impact— by focusing not just on how the socket fits but also on how it feels in everyday life.
It’s not just about making things more comfortable; it’s about making prosthetics more livable day in and day out.
O&P Almanac: What do you believe are the biggest challenges and opportunities for the future of O&P?
Robinson: One of the biggest challenges is the limited reimbursement that prosthetists and clinics face. It’s tough to innovate and provide the best care when the financial model doesn’t fully support the advanced technologies and materials that could really improve patient outcomes. This is something we’re seeing more and more as we push the boundaries of what’s possible with prosthetic design and function.
Another challenge is the historical lack of reliable data, especially around things like inner socket pressure and long-term outcomes. Without that data, it’s hard to prove what works, what doesn’t, and how to improve on the existing designs. This gap really holds us back from making informed decisions at scale and advancing the field as rapidly as it could.
That said, these challenges also present huge opportunities. Advances in data capture and remote monitoring are opening up new possibilities to collect the kind of detailed data we’ve been missing. Imagine being able to monitor socket fit in real time or track a patient’s outcomes continuously over time. This kind of data can completely change how we approach prosthetics and prosthetic innovation.
The biggest opportunity, in my mind, is making the prosthetic leg feel like an extension of the body—something that’s not just worn but truly integrated with the user’s body. We’re already seeing new technologies that bring us closer to this, from adaptive materials to sensors that monitor pressure and movement, and, of course, automatically adjusting technologies. The future is about making these technologies seamless, where the prosthetic leg is just as natural to wear and use as any part of your own body.



The Transformations column features the success story of an O&P clinician who has worked with an inspiring or challenging patient. This issue, we speak with Sara Beyler, CO, LO, who fit an international patient with spinal muscular atrophy with custom KFOs.
An old proverb tells us it takes a village to raise a child. It’s taken a global medical village and the unique expertise of a Chicago orthotist to ensure an Argentinian teen with Type II spinal muscular atrophy (SMA) can lead his best life.
Joaquin Mollard began traveling to Ann & Robert H. Lurie Children’s Hospital of Chicago for bracing and orthotic care in 2021 when he was 9. At home in Buenos Aires, Mollard has an aggressive physical therapy schedule, optimal family support and medical services to manage his SMA, a genetic disorder causing progressive muscle weakness and atrophy. But he didn’t have access to clinical trials or SMA-focused orthotic care.
“It has been—and still is—extremely difficult to find the correct care for Joaquin,” his mother, Vanina Sanchez, says. “At Columbia (University), where Joaquin also receives treatment, they recommended Sara and her team, and it was really a game changer for us!”
Sara Beyler, CO, LO, graduated from Springfield College in Massachusetts with an undergraduate degree in therapeutic recreation in 2005 and began working with athletes with primary physical disabilities. Observing “her” athletes’ experiences with orthoses and prostheses first piqued her interest in the O&P field.
A volunteer stint working alongside prosthetists and orthotists serving amputees through the Range of Motion Project in Guatemala sealed the deal for Beyler. “It opened my eyes to what I could do, and I immediately started a shift in my career,” she remembers.
She earned orthotics certification from Northwestern University’s Feinberg School of Medicine in 2009. On the path to her degree, she interned with an adaptive sports program for individuals with spinal cord injuries at the Rehabilitation Institute of Chicago. Beyler also served as a program supervisor and recreation therapist at the Great Lakes Adaptive Sports Association,
where she continued as a volunteer power wheelchair soccer coach for nearly a decade.
The drive to help patients access physical and social activities that can help them lead fuller lives led her to Lurie Children’s, where she sees all types of cases, including a significant population of children with SMA and muscular dystrophies.
“Working at a children’s hospital, I make numerous referrals for patients to get access into appropriate recreation and sports programs and that’s something I value a lot in what I do,” Beyler says.

The community of providers working with children with SMA is a close and communicative network across the United States.
When a Chicago-based physical therapist who specializes in treating kids with SMA was in New York City for training, she learned of Mollard’s case and felt he could benefit from Beyler’s expertise. Lurie Children’s follows 75 children with SMA, affording Beyler unique insight into the bracing needs of that population.
Mollard was traveling to New York regularly in 2021 to participate in Columbia University’s trial of apitegromab, an investigational SMA treatment that disrupts the production of a protein that limits muscle growth. By inhibiting the protein myostatin, apitegromab has the potential to preserve muscle mass and improve motor function in SMA patients.
“They didn’t have a local orthotist experienced in that patient profile,” Beyler says. “Orthotists can see the whole spectrum of patient profiles, and I’m really lucky I get to see so many kids with SMA each week in my clinic. That experience makes me potentially more competent to see these kids.”
Beyler’s time working with SMA patients has coincided with notable research trials and the introduction of medications and gene therapy interventions that
dramatically changed the treatment landscape. Children who previously were never expected to walk are demonstrating the capacity for upright mobility and need creative orthotic intervention to support their independence.
Presenting at Lurie Children’s with anklefoot orthoses, Mollard struggled to ambulate and couldn’t stand hands-free. Beyler and her team were confident they could support him in both standing without using his hands for support and walking. “Joaquin was under braced and not meeting his full potential,” she recalls.
Mollard and his family visited Lurie Children’s for a month to fit him with his initial custom ischial weight-bearing knee-ankle-foot orthoses (KAFOs) to provide better joint alignment, support, and stability for standing and walking. Historically used in a variety of neurological populations, KAFOs are gaining traction with SMA patients. Taking care to align the braces to promote balance in the sagittal plane and address proximal weakness, Beyler devised bracing with an anterior inclination, which allowed for Mollard to stand hands-free immediately.
The Lurie Children’s team provided an initial burst of therapy with an SMA-trained physical therapist four times weekly for two weeks to work on adaptive life skills like safe falling and to ensure his comfort using the new KAFOs and a gait trainer. Since then, the team communicates with Mollard’s local physical therapist to address questions and concerns about his ongoing therapy and progress back in Argentina.
Since 2021, Mollard has seen Beyler in her clinic once or twice a year for brace adjustments or new KAFOs. He soon will visit for his third set.
“Every time we make a little change, we either see improvement or he adapts,” Beyler says. “He really is the ideal patient.”
Mollard went from standing for 30 seconds at a time during his first visit to standing hands-free for two to seven hours per day—time he uses to do homework, build with Legos, and socialize with peers at eye level. He cut his 10-meter walk-run test time in half within six months of his initial fitting, and his ability to ambulate at home continues to improve. Mollard now walks with the assistance of his KAFOs, a gait trainer, and a reverse walker.
Maintaining his ability to stand and move throughout his home are the chief goals of Mollard’s family and therapy teams. Continually working to improve his joint flexibility, trunk mobility, and ambulation has prevented Mollard’s mild scoliosis from progressing and enabled him to avoid surgical interventions. His parents are hopeful he can delay surgery until he’s closer to adulthood.

“It is really miraculous for a child with SMA type II of almost 13 years, to have not yet had spinal surgery,” Mollard’s mother says. “We are very grateful to the whole team that has helped us so much to continue on the way to that goal.”
Following kids like Mollard for years as they move through childhood and adolescence is an aspect of working in Lurie Children’s specialized multidisciplinary pediatric O&P clinic that Beyler appreciates. She’s now watching children she started treating as babies navigate high school. “It’s one of the perks of being in a specialized clinic. I see the kids over the lifespan of their treatment and make suggestions and support them.”
FACILITY: Perry Prosthetics



Why Am I an AOPA Member?
“We belong to AOPA because it helps us stay on top of new developments and keeps us informed about business, politics, and coding. It offers so many online resources for staff.”
—Chris Perry, CP, LP
OWNER:
Chris Perry, CP, LP
CLOCATIONS:
Perrysburg, Ohio; Findlay, Ohio; and Ann Arbor, Michigan
HISTORY: 25 years
Midwest facility has grown and evolved since its founding 25 years ago
hris Perry, CP, LP, lost his leg in a motorcycle accident at age 16. He spent the next eight years limping and in pain. Finally, he connected with prosthetist Jan Stokosa, CP, FAAOP, who fit him into his schedule on a weekend.
The result was “night and day different from what I had experienced,” recalls Perry. “I knew I had a complicated situation with a short residual limb, but after seeing Jan I got my mobility back—it was an amazing difference.”
Perry’s experience with Stokosa fueled his interest in prosthetics, so he asked for a job. “Jan hired me, and I went from an entry-level position to working in the lab to becoming his assistant,” Perry recalls. “It was an incredible learning experience. I fell in love with the profession—how I saw people’s lives being changed, just as mine had.”
Perry began his journey toward certification, working for different facilities and taking classes. “I was working with Joe Springer, CP, when they asked me to fabricate a custom liner for a six-month-old girl who had been born without an arm. I met the mother out socially about 18 months later—and ended up marrying her, and having three more children!”
Perry finished his certification with the Board of Certification and, in 2000, opened his own facility in Perrysburg, Ohio—the name of which was just a happy coincidence. In 2005, he took advantage of crossover certification offered by the American Board for Certification in Orthotics, Prosthetics, and Pedorthics and became a CP.
“I was a one-man band until 2015, and then I decided to level up. I needed to be a leader, so I did research in leadership, went to seminars, listened to podcasts, read books—and it helped me build a team that is terrific,” Perry says. His facility provides mostly lower-extremity devices but has grown enough in upper-extremity clients that Perry developed an advanced upper-extremity team four years ago. The facility’s 14 employees include two CPOs, two CPs, and an upper-extremity specialist. Today the facility has two additional offices: one in Findlay, Ohio, and another in Ann Arbor, Michigan.
Perry Prosthetics leverages emerging technologies, including beta testing of microprocessor limbs
and treating patients who have osseointegrated prostheses. “We work with central fab facilities to create the first test socket, and do everything else in house,” Perry says. His team is researching 3D printers for making prototypes in the diagnostic and fitting process.
The practice embraces community and charitable involvement. Perry’s team started offering a free, monthly walking clinic that has evolved into the “Empower Hour,” with each session focusing on a particular activity. Recent sessions included a fitness and nutrition clinic for amputees, adaptive golf, and bowling.
Perry also joined one of the American teams that travelled to Ukraine to fit prosthetic arms on wounded soldiers. “We spent just over two weeks in Ukraine, including 10 days at the Superhumans Center in Lviv—a place for prosthetics, reconstructive surgery, and rehabilitation for war victims,” says Perry. “It was one of the most rewarding things I’ve ever done.”
The facility will host an Amputee Symposium in October, an event aimed at physicians, limb loss patients, and physical and occupational therapists in Ohio and Michigan, who can attend courses to earn continuing education credits. Individuals with limb loss will have the opportunity to meet with the Perry team and other prosthetic specialists, get second opinions, and learn about new technologies and adaptive solutions. The event will feature presentations by Robert Gailey, PhD, DPT, and Jason M. Souza, MD, FACS, as well as a product expo.
Perry notes that he founded CARE™—the Cooperative Amputee Rehabilitation and Education program—15 years ago. “We have provided hundreds of CARE courses over the years that are aimed at bringing education to the entire interdisciplinary team that works with amputees.”
Patients remain the highest priority at Perry’s facility. “People throw the term ‘patient-centric’ around pretty freely. For us, it means doing the right thing every time,” he explains. “No matter what is going on, you find a way to do the right thing for the patient.”
Deborah Conn is a contributing writer to O&P Almanac. Reach her at deborahconn@verizon.net

BY DEBORAH CONN
OWNERS:
Hidie Bowman



Am I
“We belong to AOPA because its members are the expert people who get our products to those who need them. The organization allows us to keep our finger on the pulse of the industry, and we rely on orthotists’ feedback to continually improve our products.”
—Amy
LOCATION:
Ann Arbor, Michigan
HISTORY: 57 years
anmar Products dates back to 1968, when Jack Marcello and Harland Danner combined their last names to create a company to develop and manufacture specialty helmets. Starting with wrestling headgear, the business soon began to focus on protective helmets for those with special needs.
In 2020, Hidie Bowman—who had started at the company as a customer service representative, moved into management, and eventually became part owner—purchased the business from Karen Linder and became CEO and sole owner. Her husband, Roger, is president, and their son, Cody Bowman, and daughter-in-law, Amy Bowman, are vice president and COO, respectively.
“Our mission is to make sensible products for highly specialized use, providing protection or support for various activities,” explains Amy Bowman. “Many of those who use our products have autism or other conditions that may involve self-abusive behaviors, seizures, weak muscles, or poor balance. We pride ourselves on providing exceptional products for individuals with specific, high needs—specializing in helmet solutions and customization.”
Helmets include soft- and hard-shell models, as well as a range of Comfy Caps, the lightest of which is only 3 ounces. One of Danmar’s newest products is the FlexCap, tailored for those with medical conditions requiring light protection. The soft EVA foam helmet has a distinctive design, says Bowman. The helmets are available in a variety of sizes, with modifications that can be adjusted for individual fit and function—including cutouts to accommodate a ponytail and accessories like visors, chin guards, face guards, and hard-shell ear coverings. Custom headgear also is available for those who require it.
“We are problem solvers,” says Bowman, “and we work with orthotists and others to find the right solution for each patient.” Danmar collaborates with orthotists and distributors, as well as occupational therapists and special educators, to reach its final customers.
“We have only about 30 employees, so everyone wears a lot of hats,” Bowman says. “We make everything by hand, and we try to buy all our
materials from domestic sources. We pride ourselves on being American made.”
In addition to helmets, Danmar makes chest and head supports for children and adults who may require help in sitting during eating or while engaging in social, recreational, or educational activities. Another line of products features aquatic therapy equipment designed for nonambulatory individuals and those with poor head and trunk control.
Patients who are unable to grip may benefit from Danmar’s Handy Helpers, including a strap that allows children to hold a toy and a device that enables users to hold writing implements, toothbrushes, and eating utensils. Other products include toileting aids and foam mitts for patients with aggressive or self-abuse behaviors.
As technology advances, Bowman predicts further integration of software and hardware. “Devices will include more feedback, so that we’ll be able to measure the force of impact on a helmet,” she says. “We will stay on top of new developments and incorporate them into our products as appropriate.”
Danmar’s website features videos that demonstrate how to determine helmet size, how to make fit adjustments, and how to take measurements for custom-made helmets. The company welcomes calls from practitioners who have specific questions or difficult cases.
The company has been in Ann Arbor for more than 55 years and directs its corporate giving to local organizations, including support groups for autism. “We also donate to different foundations that will cover the cost of products for people who can’t afford them, as well as to local hospital support groups for seniors and programs aimed at fall prevention,” says Bowman.
“The bottom line is that we want people to be safe. And we try to reduce the profile to reduce stigma, and to make it fun by offering different designs and colors. We still make wrestling headgear, but today we do so much more.”
Deborah Conn is a contributing writer to O&P Almanac. Reach her at deborahconn@verizon.net
Registration is open for the most anticipated meeting of the year for orthotic, prosthetic, and pedorthic professionals.
Full conference registration includes the following:
• Manufacturer workshops
• Educational sessions focusing on orthotics, prosthetics, pedorthics, digital, technical, and business education
• Hands-on practice and demonstrations in the Pedorthic/Technical Lab
• Attendance at the three general sessions: the Opening Plenary, “Shine on O&P”; the Thranhardt Award winners; and the AOPA Awards Ceremony and Business Meeting
• An estimated 37 CEU credits onsite
• Virtual education access for two months post-event
• Access to the Exhibit Hall
• Interactive, hands-on experiences, including the third annual O&P Digital Showcase
• Networking time with more than 2,000 industry leaders
• Several meals, including three breakfasts, two lunches, refreshment breaks, and a reception.
Register by July 19 to receive the Advanced Rate discounts! Visit aopaassembly.org today.

Orlando is also known as “The City Beautiful” and “O-Town.” Orlando’s history dates back to 1838. It was originally named “Jernigan,” after the first permanent settler in the area. The name was officially changed to Orlando in 1857.
Know a young professional in O&P who’s making waves? Now’s your chance to help them shine and help AOPA celebrate the future of O&P. AOPA’s O&P Rising Star Award was created to spotlight bold thinkers, passionate advocates, and rising leaders 35 and under who are shaping the future of O&P.
Who Are We Looking For? Nominate a young professional making a powerful impact in any of these areas: clinical practice; research and innovation; advocacy and community outreach; education and mentorship; or business and leadership.
If they’re inspiring others and moving the profession forward, we want to know about them. Winners will receive several benefits—visit the O&P Rising Star Call for Nominations page at aopanet.org/call-for-nominations-aopas-op-risingstars/ for details.
To nominate someone, fill out the O&P Rising Stars Nomination Form at aopa.wufoo.com/forms/x18ap0il0inq69v/ Nominations are due July 31
How does your organization stack up against other O&P businesses? Find out by purchasing AOPA’s “2024 O&P Operating Performance Report” and “2024 Compensation and Benefits Report.”
These timely, in-depth reports provide up-todate insights and data, empowering you to make informed decisions, drive growth, and stay ahead in a rapidly evolving landscape.
The reports feature key performance metrics; information on trends and opportunities; and data-driven insights. Executives and leadership teams, operations and finance professionals, marketing and sales team, and clinic managers will gain a strategic advantage from accessing these reports.
Purchase the full reports on the AOPA Hub, aopahub.aopanet.org, and contact Betty Leppin with questions, bleppin@aopanet.org

The officers and directors of the American Orthotic & Prosthetic Association (AOPA) are pleased to present these applicants for membership. Each company will become an official member of AOPA if, within 30 days of publication, no objections are made regarding the company’s ability to meet the qualifications and requirements of membership.
AtlanticProCare
1274 Congress Street Portland, ME 04102 207-774-1002
atlanticprocare.com
J.P. Donovan, CPO Patient-Care Facility
Cobblestone LLC/dba AMPRIA 7 Merion Way Cumberland, ME 04021
207-831-0471
ampria.net
J.P. Donovan, CPO Supplier Startup
Cranial Kids
520 W. Buena Ventura Street, Ste. 102 Colorado Springs, CO 80907
719-684-4008
cranialkids.com
Kristen Thessing, CPO Patient-Care Facility
O&P Cloud CAD 1013 Harbor Walk Court Fort Collins, CO 80525
240-498-3429
oandpcloudcad.com
Juaquin Buchanan Supplier Startup
Orthotics Limited
26 Grove Street, Ste. 101 Harriman, NY 10926 914-337-8600
orthoticslimited.com
Moshe Brooks, BOCP Patient-Care Facility
Looking for a new position? Seeking new employees? Visit the AOPA Job Board on AOPA’s website to post an open position announcement or look for a new job. Visit jobs. aopanet.org.

Enhance your skills with Allard’s free, ABC/BOC CEU-approved courses!
Access a variety of topics, including Bracing Solutions for Genu-Recurvatum — 24/7 access!
Earn your points today! allard.re/education


Embrace the comfort of custom-fit with Mt Emey®’s Custom Shoe (Medical) Program. Our precise 3D scanning captures your unique foot contours, promising a perfect fit without the wait or waste. From stylish athletics to roomy comfort designs, our handcrafted shoes adapt to your needs. Satisfaction guaranteed before payment. Plus, qualified wholesale accounts receive a free 3D scanner. Step into the Mt Emey difference— where every shoe is made for you.



The Motion Arm is a sleek, low-profile hybrid elbow with a highcapacity 3000-mAhr internal battery to power the hand longer throughout the day. Designed to accommodate higher loads, the arm supports up to 50 ft·lb in the locked position. Paired with the TASKA hand, this ultimate combination has an IP67 waterproof rating and unbeatable performance. Visit fillauer.com to find out more.
For more information, call 1-888-937-2747 or visit emeys.com

Download the Hersco app on your iPhone and connect to the lab anytime. The Hersco app and order portal makes scanning and ordering seamless. Scan patients for foot orthotics, Richie braces, and ankle gauntlets, and submit at your convenience. Our digital workflow allows you to easily track jobs, re-order devices, and manage your account. Download the app and get your username and password.
Our 3D printers produce accurate and precise orthotics, reducing landfill waste by over 90%!
Email us today at fastorthotics@hersco.com or call 800- 301-8275 to get a free product sample. Visit hersco.com




Contact Bob Heiman at bob.rhmedia@comcast.net
ABC: Application Deadlines, Exams Dates, O&P Conferences, and More! Check out ABC’s Calendar of Events at abcop.org/calendar for the latest dates and event details, so you can plan ahead and be in the know. Questions? Contact us at info@abcop.org or visit abcop.org/contact-us

The Pedorthic Footcare Association: The Active Foot—From 1st Step to Last! 10-session online education program series. Approved CEs by ABC and BOC, monthly classes are 2 hours each. For more information and to register, visit pedorthics.org.
June 30
AOPA 2026 Call for Volunteers Application Deadline. Contact Betty Leppin, bleppin@aopanet.org, or visit aopanet.org/volunteer/
July 19
Deadline to Register for AOPA National Assembly at the Advanced Rate. Visit aopaassembly.org
September 3–6
AOPA National Assembly. Orange County Convention Center, Orlando. For information, visit aopanet.org
October 17–18
PrimeFare Central—NEW VENUE!
Waterford Renaissance Hotel, OK City. For information, contact Cathie Pruitt at 901-359-3936, primecarepruitt@gmail.com, or visit primecareop.com




A large number of O&P Almanac readers view the digital issue— If you’re missing out, visit issuu.com/americanoandp to view your trusted source of everything O&P.
Scan the QR code to start advertising in the O&P Almanac or visit bit.ly/AlmanacMediaKit25
2026
January 9–11
2026 Leadership Conference. Huntington Beach, CA. For more information, visit aopanet.org
September 9–12
AOPA National Assembly. Las Vegas, NV. For more information, visit aopanet.org
September 22–25
AOPA National Assembly. Long Beach, CA. For more information, visit aopanet.org
August 29-September 1
AOPA National Assembly. Washington, DC. For more information, visit aopanet.org
Advertise O&P events for maximum exposure with O&P Almanac Contact Bob Heiman at bob.rhmedia@comcast.net or learn more at bit.ly/ AlmanacMediaKit25. Announcement and payment may also be sent to O&P Almanac, Calendar, P.O. Box 34711, Alexandria, VA 22334-0711, or emailed to jklapp@AOPAnet.org along with VISA or MasterCard number, cardholder name, and expiration date. Make checks payable in U.S. currency to AOPA. Note: AOPA reserves the right to edit calendar listings for space and style considerations.
Texas’s House Bill (HB) 426, legislation that would require Medicaid and the Children’s Health Insurance Program to fully cover cranial remolding orthoses in accordance with clinically accepted guidelines, has passed in the House and the Senate. It has been sent to Gov. Greg Abbott.
Pennsylvania Senate Bill (SB) 537, introduced in April, seeks to amend medical assistance fee-for-service reimbursement rates for O&P to no less than the current Medicare fee schedule for durable medical equipment, prosthetics, orthotics, and supplies (DMEPOS). The bill also seeks to update the medical assistance fee-for-service program to include all codes that are in the current Medicare DMEPOS fee schedule.

As of June 12, NY Assembly Bill (AB) 2520/SB 1616, legislation that would require Medicaid managed care organization plans to reimburse DMEPOS items at no less than 100% of New York's Medicaid fee schedule, has passed in the Assembly and the Senate. Next, it will be sent to Gov. Kathy Hochul's desk.
Advocates have been active in pushing forth So Every BODY Can Move (SEBCM) legislation in pursuit of creating equitable and life-changing access to prosthetic and orthotic care and devices for physical activity.
Georgia’s governor, Brian Kemp, signed SB 101 into law May 13, making Georgia the 10th state to enact SEBCM legislation.

Oregon’s SB 699 was recently signed by Gov. Tina

New Jersey's bill, AB 3856/SB 1439, passed in the Assembly floor vote. SB 1439 passed in the state's Senate last year. The next step for the bill to become law is to be signed by Gov. Phil Murphy.
Oregon’s SB 699 passed in the Senate and the House of Representatives, with unanimous votes through every committee. SB 699 was then signed by Oregon Gov. Tina Kotek on June 3. Oregon has become the 11th state to pass SEBCM legislation.
Join this year’s 28x28 Mobility Challenge, presented by On’s social impact program Right to Run, in celebration of Disability Pride Month in July. Last year, more than 500 participants helped make a difference. For 2025, we’re back and ready to make an even bigger impact.
Whether you walk, roll, climb, swim, dance, or play, every move matters in our collective push to ensure access to O&P care across the country. Join as an individual or by creating or joining a team.
For 28 days, dedicate 28 minutes of your day to physical activity, and raise money to enact vital So Every BODY Can Move legislation in 28 states by the 2028 Paralympic Games. Plus, win prizes! For details and to register, visit soeverybodycanmove.org/28-x-28/ mobility-challenge

















