@aestheticsgroup
@aestheticsjournaluk
Aesthetics
aestheticsjournal.com
Understanding Tear Trough Anatomy
2020
Dr Eleanor Reid, Miss Lara Watson and Miss Priyanka Chadha explore the anatomy of the tear trough for successful injectable treatments The tear trough deformity is characterised by a sunken appearance of the eye and a resultant dark shadow cast in the lower eyelid region. It is not exclusively a result of facial ageing and a mild tear trough may be seen in younger patients. It is the deepening of the trough and changes to the surrounding soft tissue architecture that occur with age, which leads to the characteristic features of the tear trough deformity.1 Patients who request correction of the tear trough deformity often present complaining of dark circles, a fatigued appearance, or aged or an un-aesthetically pleasing groove around the eye. Traditional techniques to address this cosmetic issue previously relied on chemical peels or surgical excision of skin, muscle and fat.2 More recently the need to restore volume to the orbit as part of an overall rejuvenation strategy has been appreciated, with treatment of the tear trough with hyaluronic acid (HA) dermal fillers gaining huge popularity. It is widely recognised that diagnosis and management of complications that arise from medical aesthetic treatments are an unmet training need.3 This is particularly true with regards to treatment of the tear trough region, where there is very little safety data supporting treatment modalities regarding potential periocular complications and their management.3 Although the range of potential complications that arise are similar to other areas in the face, the delicate nature of the eyes means that complications from treatment arise more commonly in this region.4 Understanding soft tissue and vascular anatomy is essential to rejuvenation of the undereye area.
Definitions and nomenclature The term ‘tear trough’ applies to the medial one-third of the periorbital hollow that extends obliquely from the medial canthus to the mid-pupillary line, forming a sulcus. The sulcus involves the thin, loose skin of the eyelid where it originates at the lower eyelid inner canthus and extends down to the thicker skin of the cheek.5 This indentation where the thin eyelid skin above meets the thicker nasal and medial cheek skin below defines the tear trough
0
1
2
0
Palpebral line
1
Tear trough
2
Palpebromalar groove
3
Mediojugal fold
3
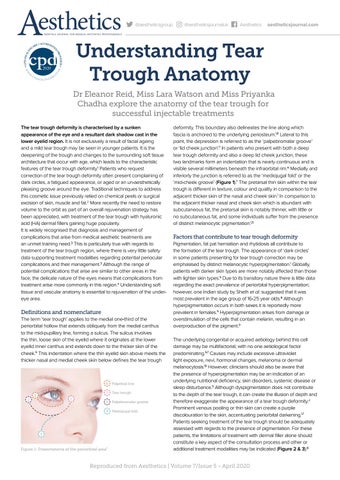
Figure 1: Presentations of the periorbital area7
deformity. This boundary also delineates the line along which fascia is anchored to the underlying periosteum.1,6 Lateral to this point, the depression is referred to as the ‘palpebromalar groove’ or ‘lid cheek junction’.7 In patients who present with both a deep tear trough deformity and also a deep lid cheek junction, these two landmarks form an indentation that is nearly continuous and is visible several millimeters beneath the infraorbital rim.6 Medially and inferiorly the junction is referred to as the ‘mediojugal fold’ or the ‘mid-cheek groove’ (Figure 1).7 The pretarsal thin skin within the tear trough is different in texture, colour and quality in comparison to the adjacent thicker skin of the nasal and cheek skin.1 In comparison to the adjacent thicker nasal and cheek skin which is abundant with subcutaneous fat, the pretarsal skin is notably thinner, with little or no subcutaneous fat, and some individuals suffer from the presence of distinct melanocytic pigmentation.1,5
Factors that contribute to tear trough deformity Pigmentation, fat pat herniation and rhytidosis all contribute to the formation of the tear trough. The appearance of ‘dark circles’ in some patients presenting for tear trough correction may be emphasised by distinct melanocytic hyperpigmentation.1 Globally, patients with darker skin types are more notably affected than those with lighter skin types.5 Due to its transitory nature there is little data regarding the exact prevalence of periorbital hyperpigmentation; however, one Indian study by Sheth et al. suggested that it was most prevalent in the age group of 16-25 year olds.8 Although hyperpigmentation occurs in both sexes it is reportedly more prevalent in females.5 Hyperpigmentation arises from damage or overstimulation of the cells that contain melanin, resulting in an overproduction of the pigment.9 The underlying congenital or acquired aetiology behind this cell damage may be multifactorial, with no one aetiological factor predominating.5,7 Causes may include excessive ultraviolet light exposure, nevi, hormonal changes, melanoma or dermal melanocytosis.10 However, clinicians should also be aware that the presence of hyperpigmentation may be an indication of an underlying nutritional deficiency, skin disorders, systemic disease or sleep disturbance.5 Although dyspigmentation does not contribute to the depth of the tear trough, it can create the illusion of depth and therefore exaggerate the appearance of a tear trough deformity.2 Prominent venous pooling or thin skin can create a purple discolouration to the skin, accentuating periorbital darkening.1,7 Patients seeking treatment of the tear trough should be adequately assessed with regards to the presence of pigmentation. For these patients, the limitations of treatment with dermal filler alone should constitute a key aspect of the consultation process and other or additional treatment modalities may be indicated (Figure 2 & 3).8
Reproduced from Aesthetics | Volume 7/Issue 5 - April 2020