






4
6 Reflections of volunteerism
Dr Russell Gordon shares his experience.
12
The many benefits of
17









4
6 Reflections of volunteerism
Dr Russell Gordon shares his experience.
12
The many benefits of
17

Welcome to 2024 everyone! As most of us would have been hectically busy in the lead up to the end of last year, I do hope that we have all had time to recover and recharge for the new year. We welcomed a new cohort of around 50 graduate dentists late last year, and hosted the ADAWA “Welcome to the Profession” dinner in December. We hope to see and meet the new graduates at our ADAWA events, CPD events and New Practitioner Program events during the year.
Members should have received their WA Dental CPD 2024 course book in the mail and the calendar is full to the brim with courses to suit everybody. If you have not yet received it, please contact us at ADAWA.
As some of you may already be aware, our colleagues on the East Coast have been actively lobbying against the changes to the payroll tax in their respective states. WA is currently unaffected by these changes, however; we are monitoring the situation closely.
On a nicer note, one of our own Councillors, Dr Peter Duke, has
CEO Trevor Lovelle President Dr Gwen Chin Editorial Brooke Evans-Butler Designer Michelle Walkerbeen involved in a project that is close to all our hearts. The Mindful Smiles Hub has been launched and it serves to provide resources and information on mental wellbeing, mental health and understanding mental illness in our community. Health practitioners, in general, have always had their mental health placed on the backburner, as we are always expected to look after others. A resource like this provides the appropriate information and guidance that is needed for members of our profession and their families.
In view of the emerging acceptance of talking about mental health and wellbeing, a number of ADAWA Councillors themselves have attended Mental Health First Aid courses, in order to be able to provide assistance to our members.
This edition of the Western Articulator includes an article to kick off a wellbeing series in the next few editions. We hope it encourages our members to take the time to take care of themselves and look into options to increase their wellbeing.

my association. my adawa.
For me, key benefits of ADAWA membership are collegiality, the professional indemnity insurance offered, access to the world-class CPD program plus professional support such as HR and legal advice. These are no doubt important benefits for many members. Overall, the strength of the ADAWA comes from having a strong membership base. This enables the association to also serve more effectively in its advocacy role for both the profession as well as for improved oral health in the community more broadly. This role benefits us all as dental practitioners and hopefully leads
to better outcomes for patients."
Dr Tim Clair
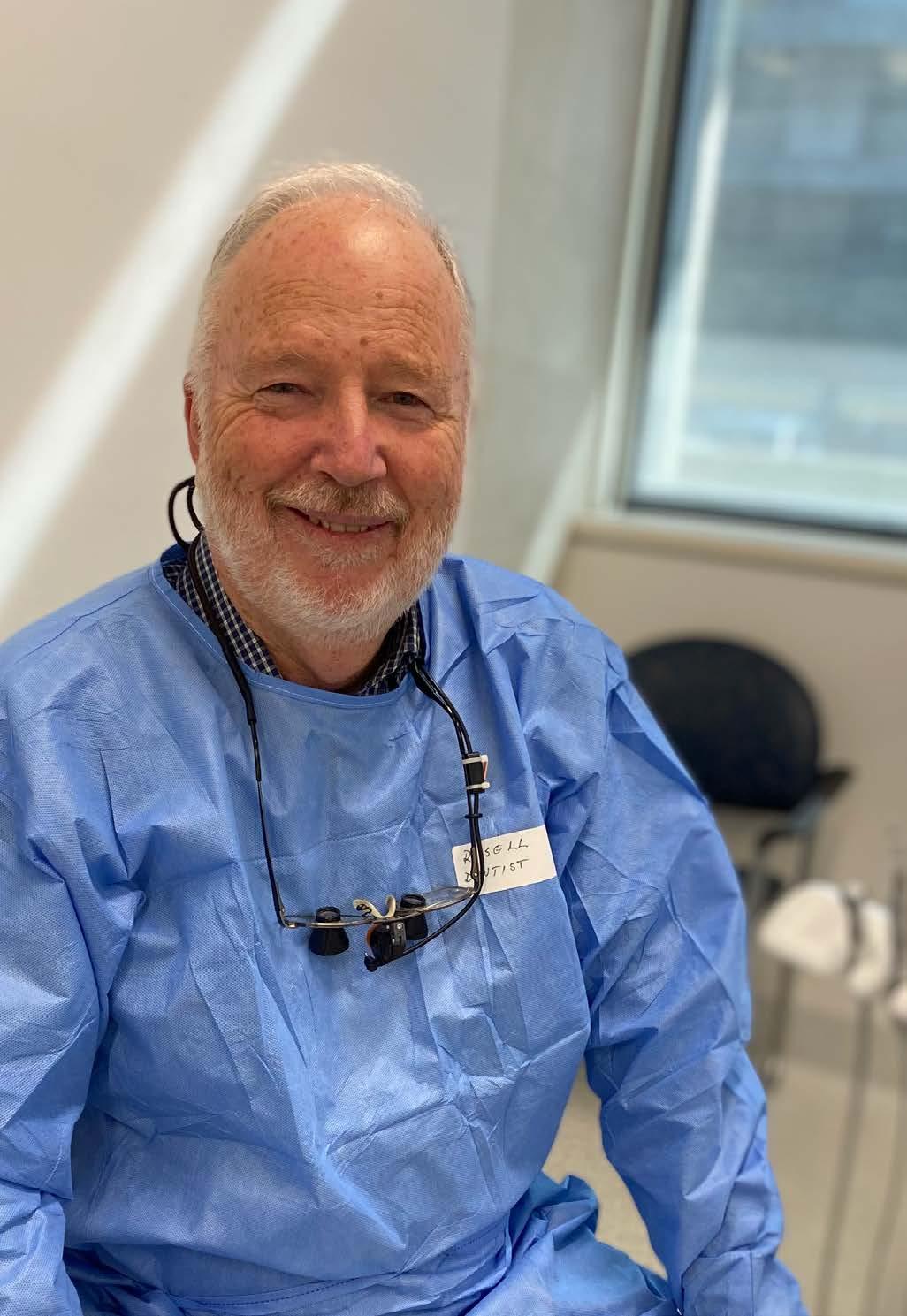
As well as serving as the current Chair of the ADA DHF in WA, Dr Russell Gordon has a long history of volunteerism. We spoke to him about the importance of giving back.
Russell says the importance of pro bono work was instilled back in his days as a dental student. “Most of us came out with the same haircuts; we were taught we are professionals, so should do no harm and do what we thought was the best for the patient,” he recalls. “Back in those days only a dentist could own a dental surgery and as part of that, lecturers would talk to us about the obligation to provide pro bono work for people who couldn’t pay. In my practice I did lots of free extractions when people would turn up in pain. I didn’t put a sign up that said: ‘free dentistry’, but I felt it was part of my obligation.”
On a personal level, Russell says his desire to do more volunteerism increased when he had children –reflecting on the contrast between the upbringing of his children, his own upbringing, and that of his father. “My father’s mother died during childbirth and then he spent four years in an orphanage,” Russell says. “He grew up during the Depression, then they sent him to war and a lot of his friends got killed. You think about how lucky you have the parents that you’ve got, lucky to be born in Australia – there is an awful lot of luck in life, so it is nice to give back. You think more about that when you have children; it changes your attitude.”
As happens in life, Russell was very busy running a dental practice (from 1980 to 2019) so it was when his children got a bit older, Russell considered going overseas to volunteer, with the thought that his wife could then join him after a volunteering stint for a well-deserved holiday.
It was around this time, Russell noticed Dr Dennis Gregory’s advertisement in the Western Articulator for practices to run a Dental Rescue Day (DRD). It seemed to be the perfect fit, so Russell first hosted a Dental Rescue Day at his former practice, Rockingham Dental Centre, back in 2006.
“I had a seven-surgery practice with my associate Dr Gerard Parkinson,” Russell recalls. “When I mentioned the ad to Gerard, he was immediately on board, and we asked our staff if they would be willing to work on a Saturday to provide treatment free for homeless people. I was surprised and gratified that we had 100 per cent turn up to that day, plus the daughter of our practice nurse manager who was still at high school but wanted to help out.
“The atmosphere that first day was like a carnival,” he says. “Dentistry is
a helping profession, and it was easy to see the people drawn to it were really enjoying the fact that they had particular skills that they could use to change some people’s lives. All the dentists adopted some patients that day to finish off treatment that required further appointments.”
The rest, they say, is history. Russell, Gerard and the Rockingham Dental Centre team hosted many Dental Rescue Days and to this day, the practice is active in volunteerism and Dental Rescue Days.
“Once you hear some people’s stories it inspires you to help them if you can,” Russell adds. “I also feel that it strengthened the regard of our staff for the place they worked at as they enjoyed being a part of a caring practice. In those days we used to print practice updates for our patients and would include photos from DRDs. From the conversations they initiated with our regular patients, I always felt that our standing in the community was enhanced by our volunteering efforts. Subsequently, Hari Menon took over the practice from us. He had worked for us and volunteered in our DRDs and now continues that tradition.
“I never ended up going overseas to volunteer – there was so much to do here,” he laughs.
Russell says at Dental Rescue Days in private clinics, the aim is to provide the most urgent treatment. “Our aim is to relieve pain and try and keep people safe untill they can get more comprehensive treatment in the Government system,” he says.
“The Adopt a Patient Scheme allows individual dentists to bring patients back to do more extensive work,” he adds. “Sometimes just by restoring an anterior tooth or making a denture you can totally turn around someone’s appearance for a job interview, which is the most basic way you can help someone get themselves out of homelessness.
“The Rebuilding Smiles Programme has some funding that is designed to help survivors of domestic violence. Some wonderful work has been done by volunteering dentists in rehabilitating patients under this programme.”
Russell has also had a long-standing involvement with St Pat’s.
“The ADHF had acquired some donated dental equipment and I heard that St Pat’s Community Centre wanted to open a dental clinic, so we offered the equipment to them,” he recalls. “They gratefully accepted the equipment but said that although they had sourced funds to build a clinic, they had no expertise to run it and would we partner them. The clinic opened in 2016 initially with student DAs from Dental Nursing Australia and volunteer dentists. Over time, St Pat’s has raised money and the ADHF won a $100,000 grant from Impact 100 Fremantle, which has allowed a full-time nurse to be employed. The ADHF was also lucky enough to secure an account from Henry Schein Cares to supply materials. A-dec has supplied a lot of equipment and support and Oceanic Dental provide free laboratory work. Many other dentists have donated instruments and materials.
“It has taken a lot of work not the least of which is guiding an institution not familiar with the exacting requirements of running a safe and efficient dental surgery. However, St Pat's clinic has been a great addition to the volunteer options of dentists who don’t have their own clinics and has been extremely successful in providing many hundreds of thousands of dollars’ worth of free treatment for homeless people.”
Russell adds there are many people with goodwill in the industry that have made the running of the clinic possible, including the team at Henry Schien that provide a monthly account for materials and A-dec’s Joe Minervini, who maintains the equipment at St Pat’s on an ongoing basis.

Russell admits he has certainly had more hugs from patients at Dental Rescue Days than he has ever received from his regular private practice patients. “I think it is because they often feel overwhelmed. Firstly, because their life situation may be such that they can’t see a way they can access treatment even through the Government system because of its waiting lists and the fact it requires a co-payment.
Secondly many homeless people have slipped through the cracks in our community and feel that no one cares about them. When they come across a friendly face (even though
they are often mortally afraid of the dentist) their gratitude is magnified.“ADA DHF WA Coordinator Andrea Paterson often tells us of letters from case workers passing on the appreciation of patients who lack the resources to do that themselves,” he adds.
Russell says the Dental Rescue Day that stands out most in his memory was one where he had two female patients in the same morning who were about the same age as his elder daughter. “It happened that both required a full upper clearance and immediate denture,” he recalls.

“When I told them I would take them on under the Adopt a Patient scheme they both broke down in tears of thanks. I couldn’t help contrasting that reaction with my own daughter whose tears would have been in grief if I had told her she required even one tooth removed. One of the patients was a victim of domestic abuse. The other had a history of drug use, which had contributed to her tooth loss but more importantly to her, she had lost custody of her children. Now rehabilitated she needed her appearance to reflect that, so she could plead her case at an upcoming hearing. With the help of Oceanic Dental who provided pro bono lab work, we were able to rush the job to meet her deadline. Once again, the patient broke down in tears of gratitude when we showed her the result in a mirror. It was only basic dentistry we were providing but to her it was life changing.”
“Obviously I would encourage all dentists to consider volunteering,” Russell says. “The need in our community is great. By using even the most basic of our skills, we can make huge differences to people’s lives. I think volunteering reflects well on us as individuals, as well as on our profession as a whole. It emphasises to the community that we aren’t normal businesses but in fact professionals who put the welfare of patients before all else in our daily work and of course it just makes us feel better about ourselves when we are able to help others.
“I must mention that ADAWA have always been very supportive of efforts by the profession to supply pro bono work for disadvantaged people and continue to be so in many ways,” he adds. “For example, ADAWA has a Volunteers Committee, which brings together all the volunteer groups to allow cross fertilisation of ideas and resources between us. Also, the ADAWA provide tremendous support for the ADA DHF state coordinator Andrea Paterson as she finds the people in need through the different agencies and introduces them to volunteer dentists.”
There are many advantages of opening your practice to inclusive employment.
It can be difficult finding employees – but chances are you might not have considered all employment options.
If you are looking for a hard worker, who can take care of all the small but essential tasks that are getting on top of your practice staff, employing a person who has an intellectual disability might be the perfect fit.
Nia Parker, Chair of Down Syndrome WA, says there are many advantages of inclusive employment for businesses such as dental practices.
“I think there is a financial benefit in having someone with an intellectual disability to do the lower-level tasks that need to be done,” she says. “This way a business is not paying someone who perhaps is at a higher rate of pay or is more qualified to do a task someone else could do.
“You are not creating work for them; they are doing essential, meaningful tasks that someone in that practice needs to do,” she explains. “Someone needs to tidy up the reception area, someone needs to make up the oral hygiene packs, tidy the staff room, make sure the cupboards are fully stocked, step in to empty out the sterilising unit…there are a whole lot of small jobs that need doing.
“It can often be difficult to attract people who only want to work say two four-hour shifts in a week,” she adds. “However, that is perfect for someone who has Down Syndrome because that may be all they are looking for and it means you are filling a need that you might not otherwise be able to fill.”
Nia points out there is the opportunity to be a good corporate citizen by giving an opportunity to someone with an intellectual disability. “You get to give someone meaningful employment that they might not otherwise get,” she says. Nia’s daughter Rachel has been employed by Rockingham Dental Centre for the last three years, and Nia says she personally knows of three families who have moved specifically to Rockingham Dental

Centre because the practice has chosen to employ someone with a disability.
“(The attitude of the families) was that the practice is obviously a caring environment, so it was somewhere they wanted to be as a patient,” Nia says. “From a business point of view, you can attract clients because it is a very demonstrable way of showing that you are a caring environment and that is what people look for in a dental professional.”
Rachel works for a few hours, two days a week at Rockingham Dental Centre. “I like the team; they are great to work with,” Rachel says. “My bosses are great – they are funny, and I am always included.
“When I first started, I had to do the hygiene packs and that was the only thing I had to do, but I then moved
onto other jobs. I like being busy and I like being efficient.”
Nia adds the opportunity to have meaningful employment, doing something that is necessary and feeling needed is important for everyone. “It means they earn money of their own,” she explains. “Rachel, for example, colours her hair and she can go to the hairdresser every two months to get a colour, go buy some shoes that take her fancy – it allows her to buy the extras, the luxuries with her own money.”
“We wholeheartedly encourage other dental practices to explore employment options with DSWA,” says Dr Hari Menon from Rockingham Dental Centre.
“Rachel brings to the practice a unique and refreshing perspective to our team that has been truly invaluable. Her commitment to her work and colleagues has been remarkable and has brought even more inclusivity and diversity to our workplace.
“Rachel's achievements in and out of the workplace, remind us that individuals with diverse abilities are fully capable of excelling in professional settings when given the right support and opportunities. She serves as a testament to the potential for success that can be unlocked when we provide inclusive employment opportunities. Our experience with Rachel has been both rewarding and enlightening.
“We are grateful to be able to offer a more inclusive and accepting work environment while tapping into the talents and abilities of individuals like Rachel.”

To practice owners or managers who are thinking about contacting Down Syndrome WA about employment options, Nia advises having the conversation – there is information and support available for practices wanting to look into inclusive employment.
“We have an employment coordinator at DSWA, so a practice owner can reach out and say they are thinking of possibly employing someone. Someone from DSWA would come out and have a chat about what some of the tasks might be and identify the right person for that. Once someone is hired, a mentor will be organised to accompany the employee until they are confident with their tasks."
“You train any new person that comes into your workplace but normally you train them and let them get on with their job. What happens here is you train the young person and the mentor and then the mentor would do the repetitive teaching, working sideby-side until that person is capable and confident to do that work independently."
“You are not using a staff member to do the repetitive learning. The extra help the new employee needs will be provided by an outside person, and this mentor will be with them for as long as they need. There is no cost
to the dental practice for the mentor.”
She adds working at a dental practice is very suitable for someone with Down Syndrome, because as a generalisation they are good with small repetitive tasks and fit well into a social environment.
“The team at the practice where Rachel works like having her there – they say she is so much fun to have around,” Nia says. “Also studies show that people with disabilities have lower rates of absenteeism and higher rates of loyalty to their employer.”
To find out about employing a person with Down Syndrome at your practice, please contact the Down Syndrome WA Employment Coordinator at employment@downsyndromewa.org.au







It’s important to look after yourself away from the practice. In the first part of our wellbeing series, we look into the benefits of mindset coaching and yoga therapy.
Did you have good intentions of going to the gym regularly in the new year, but it has already fallen by the wayside? If you would like to work on your physical fitness, Shay Liggett, Director at Mind You Performance, recommends looking into mindset coaching to help you focus via a mix of coaching and mentoring.
“Most clients that come through our doors will want a physical transformation – they want to go to the gym, lose weight or improve their health – the focus is on the physical first,” Shay explains.
“What we have noticed however, is once they start to change their routines, some blocks appear. There are habits and behaviours that they need to unpack. Perhaps that is a sleep routine or time on the phone – things that people struggle with making a lifestyle change rather than just focusing on physical changes, because they can then revert back to what they were doing before – that’s where we focus on the mindset part.
“An example could be that a client wants to lose weight but focuses on the number on the scales and the stats. It sometimes takes away from why they are doing what they are doing – this is why we get our clients to focus on how they want to feel and how they desire to experience their life. Then they are no longer focusing on that they want to lose 10 kilos, but that happens as a byproduct because of their change of mindset.”
Shay says that people have a desire to make a difference, but their motivation can be impacted when they are not getting the results they are expecting. “Often, many can’t really see the blocks they have in preventing them to make long, impactful changes in their life, so I think a big benefit of health and performance coaching is having someone to lead you through,” she says. “Yes, you have a plan to perform in the gym and correct technique – we can help busy professionals like dentists who have time constraints be more efficient – creating an efficient program that is tailored to them that is well-rounded and fits in their lifestyle.
“The other benefit is having accountability,” she adds. “You would be more inclined to succeed when someone is guiding you and
supporting you through the process. A year is a good time period to spend with a Health and Performance coach as it gives the person guidance and support during different periods and holidays and how to manage that. For example, during the Christmas period many people have an ‘all or nothing’ mentality. ‘I’m not going to do anything and then I’ll start in the new year’ and that often leads to a stop-cycle of ‘dieting’ resulting in procrastination to get back into routine. Our clients however, we highly encourage instead of adopting an ‘all or nothing approach’ to just take their foot of the gas. If they usually train five times a week, then it is three times a week. If they go on holidays, it might just be a goal to get moving, maybe go for a walk. That mindset shift of: ‘How do I incorporate this to enhance my life?’ more than a stop-start cycle of exercising is the sort of mindset shift that we help our clients navigate. As a result clients are living a more fulfilled lifestyle gaining freedom, flexibility and getting results for the long-term.
“Many people are focused on outcomes and results instead of the journey,” Shay adds. “The journey or lifestyle change allows you to focus on how you want to live your life on a daily basis – we want to be better every day, and this is what we help clients to see.
"For dentists to perform at the high level they do without facing burnout, it is important that we take care of ourselves first,” she adds. “My philosophy is that if you prioritise yourself first; then we can perform better and can look after our patients better.”
Mind You Performance offers a free consultation, mindyouperformance.com

Tanaya Ti’en, C-AAYT yoga therapist from Mind Body Collective and committee member at the Australasian Association of Yoga Therapists, says: “Yoga therapy takes the age-old tradition of yoga and brings it into a clinical setting – offering many benefits to someone’s mental, emotional and physical health.”
Where a yoga teacher may have the basic 200 hours of yoga teacher training, a Yoga Therapist has completed several more years of study
and research to be able to offer a very individualised approach to yoga.
“Going into a group yoga class, I will often teach up to 50 people,” Tanaya says. “These will be 50 very different people of different shapes and sizes, different health conditions and different circumstances – I will read the room and deliver a class to the general consensus depending on their experience and physical capacity, but you can’t deal with individuals in a class of 50 people. Yoga therapy, on the other hand, is a one-to-one personalised approach to yoga. We work through an extensive assessment process which provides a picture of the whole person, not merely the physical aspects. We look at your day-to-day activities, family life, medical history etc. The more honest you are in the assessment, the more effective the program is that I can put together for you.”
Physically, there are benefits of yoga therapy for dentists, who can suffer from the repetitive nature of their work. “Dentists will often be in what is called the ‘text neck’ position when they are working,” she says. “Text neck is a repetitive stress syndrome, usually resulting from excessive strain on the neck from too much time spent in a
forward head position. This can lead to headaches, neck pain, shoulder and arm pain, and poor breath quality which can initiate an array of other symptoms. With personalised yoga therapy, from a physical perspective, we would counterpose the forward head posture and work through specific practices to alleviate built up tension in the areas of imbalance.” She says ultimately yoga is a psychology, or ‘science of the mind’. “The practices we do in yoga are all for one common goal – to tame the mind,” she says. “The physical benefits of yoga are just the tip of the iceberg. What yoga can do for the mind is it can set people up for a lifetime of self-regulation. “For a dentist, for example, if you are in the middle of a busy work day and are feeling overwhelmed, physically tense or fatigued, there are specific yoga therapy based practices and techniques that you can draw upon in that moment to reboot and take your best self to your next patient,” she says.
Tanaya offers a free 15-minute consult for anyone curious to know more about how yoga therapy may be able to improve your quality of life; mind, body and spirit. mindbodycollective.com.au

We wish to inform members of the passing of Dr Ravinder Singh Sandhu on 2 January 2024. Dr Sandhu graduated from UWA in 1990 and opened his Wanneroo practice, Timberlands Dental Clinic, in 1992. He was a dedicated practice owner for nearly 30 years. Outside of dentistry, Dr Sandhu was a loving family man. He also coached and provided financial support to his son's soccer and daughter's netball teams. In addition, Dr Sandhu was a very community orientated individual, providing his time and donations to various causes, including those involving the Sikh community. Dr Sandhu was well respected and liked by his patients. With many of his original patients, he treated several generations, and they considered Dr Sandhu as not just their dentist but their friend. His patients often came to Dr Sandhu, even after he had stopped practicing, with, for example, homemade cakes and biscuits,
fruits and vegetables, and other produce that they knew Dr Sandhu enjoyed eating. Dr Sandhu stopped practicing as a dentist when he was diagnosed with colon rectal cancer, which had metastasized to his lungs and liver. Dr Sandhu battled with cancer for just under two-and-a-half years. During the last six months of his life, he bravely battled through the pain, with the support of his medical team and his loving wife, children, and extended family. Dr Sandhu was much loved and respected by people from all walks of life. His funeral was attended by close to 800 people, including many from his Sikh community, his patients, the local postman, his gardener, and other tradesmen who had worked on Dr Sandhu's home, his kids' ex teachers, his neighbours, and his large extended family. It was a beautiful, elegant service. We send our condolences to Dr Sandhu's family and loved ones.


Meet Dr Davis Thomas In the lead-up to his first visit to Perth to present his highly anticipated Orofacial Pain and TMD course in April, we caught up with Dr Davis Thomas.
We are lucky to have some of the best local and international speakers presenting the 2024 WA Dental CPD courses – and Dr Davis Thomas is bring his wealth of experience to Perth for this first time in April.
Davis completed his Bachelor of Dental Surgery in India – receiving an Advanced Education in General Dentistry from NYU. He then progressed to three different Master’s degrees in Orofacial Pain (Rutgers University, USA), Headache management (University of Edinburgh) and Sleep Medicine (Sydney Medical School), so it isn’t surprising that he says he believes in perpetual learning and is just as passionate about educating others.
“I love to see the glitter in the clinicians’ eyes when they learn new things and sometimes ‘unlearn’ old un-scientific philosophies,” he says.
“Also, knowledge is the only wealth that grows when you share!”
He adds he most enjoys finding the diagnosis of the ‘needle in the haystack’ condition, and considers it a blessing to give relief to countless numbers of chronic pain patients.
Davis will be presenting the Orofacial Pain and TMD Hands-On course in Perth on April 20.
This one-day course will provide a review of OFP and TMD, screening for these disorders, help identify ominous signs of OFP and make succinct, prompt referrals to oral medicine specialists and medical colleagues and suggest ways to help avoid the frustration of managing these conditions.
Learning outcomes will include:
• To have a broad understanding of Orofacial Pain and TMD.

• To understand the clinical screening for OFP conditions and ominous signs of pain.
• Learn basic cranial nerve screening.
• Learn basic clinical OFP examination and TMJ examination.
• To learn head and neck screening in the context of OFP and TMD.
• To begin to understand when and to whom to refer a case of OFP/TMD to.
“It will be a robust full day course with didactic and active hands-on components,” Davis explains. “Clinicians should be able to screen for TMD/Orofacial Pain/ Obstructive Sleep Apnea upon its completion. In the hands-on portion, they should be able to familiarise with Cranial nerve screening and basic TMJ exam and begin to format some diagnostic philosophies. Also, for clinicians to pick up red flags for more ominous diagnoses that masquerade as ‘TMJ/TMD’.” The course is a great opportunity to learn from this passionate educator, who has been inducted into several international universities over the past couple of years (including India, Chile, UAE and the USA). “I am super excited to visit and teach all those programs,” Davis says. “I am also continuing my mentorship for international dentists.”
Dr Davis Thomas will be presenting Orofacial Pain and TMD Hands-On Course on April 20 at ADA House. To book, visit our website: adawa.com.au/ product/orofacial-pain-and-tmd-handson-course
What three words best describe you?
Passionate, Compassionate, Enthusiastic.
If you weren’t in the dentistry field, what would you be doing for a living? Neuroscience.
What do you enjoy doing in your spare time?
Traveling internationally a lot; Family gettogethers, and road trips with family.
What is your favourite book?
Bhagavatam (an Indian spiritual book written 3000-5000 years ago: the best psychological counselling for the human mind, I believe).
If there anything people might be surprised to learn about you?
I love music; and known to be a good singer.
In a fast-paced and high-stress practice environment, emotions can run high, and tensions can escalate rapidly. On occasion, this pressure may lead to heat-of-the-moment resignations, where an employee impulsively decides to quit their job.
As a dental practice owner or manager, knowing how to handle such situations professionally and effectively is crucial to maintaining a well-functioning team and ensuring continuity of high-quality care for your patients. This article will explore how to manage heat-of-the-moment resignations in a dental setting.
When an employee announces their resignation in the heat-of-the-moment, it can be surprising and emotionally charged. Heat-of-the-moment resignations may arise in relation to performance, investigation, or disciplinary proceedings, or in response to a stressful situation that has unfolded in the clinic. It's essential to stay calm and collected, even if you're feeling frustrated or upset in response to the employee. Avoid reacting with anger, blame, or making impulsive decisions and statements that may be inflammatory. Instead, aim to de-escalate the situation by inviting the employee into a private space to discuss their view and decision.
A heated resignation may not necessarily be final, so maintaining a composed demeanour can create an opportunity for open communication. Give the employee

a chance to express their concerns and frustrations. Sometimes, merely allowing them to vent can help defuse the situation.
After the initial resignation announcement, schedule a follow-up meeting once emotions have settled. This gives the employee time to reflect and consider the consequences of the resignation. During this meeting, encourage open and honest dialogue. Ask the employee about their reasons for resigning and be open to discussing potential solutions to their concerns.
It is important to listen actively and empathetically, acknowledging the employee’s feelings and concerns that have led to the heat-of-themoment resignation. Even if you ultimately accept the employee’s resignation, a collaborative approach can help both parties’ part amicably.
Once the initial emotions have subsided and you've had a chance to discuss the resignation with the employee, take time to assess the situation objectively. Consider the

impact of their departure on the practice, the team, and patient care. Are there any specific issues or challenges within the practice that contributed to their decision? This may include but is not limited to bullying or harassment concerns, or attitude challenges among the team. Evaluate if there is any merit in their concerns and whether changes can be made to prevent future resignations of this nature.
If you believe that retaining the employee would be beneficial for the practice, explore ways to address their concerns and improve their work environment. Keep in mind that some issues may be beyond your control, but if there are actionable steps you can take to create a more positive workplace, is it in the practice’s best interests to explore these options.
Where the employee has raised that their resignation is due to bullying or a work health and safety matter, the practice should take all reasonable steps to assess and action the risk to ensure the wellbeing for all employees working in the practice.

In some cases, employees might resign impulsively due to personal or work-related stress, rather than any deep-seated dissatisfaction. As a responsible employer, consider offering support and resources to help them deal with these issues. This might include access to an employee assistance program (EAP). Providing assistance can not only help the individual but also create a more supportive workplace culture generally. It is always more beneficial to catch and address any work-related stress issues before they result in a resignation, however where this has been raised as a reason for the employee’s resignation, the practice should holistically assess and address the team’s work-related stressors more broadly.
To minimise heat-of-the-moment resignations in the future, establish a clear protocol for resignations within your dental practice. This protocol should include guidelines for how employees should communicate their intentions to resign, who they should notify, and the notice period required. By having these procedures in place, you can ensure that resignations are handled professionally and with minimal disruption.
Where an employee has verbally resigned, it is best to confirm that this is their intention via writing. This may be via an email or letter addressing the date and time that the employee made remarks about resignation and asking that they confirm in writing that this was their intention.
The continuity of patient care is a top priority in the dental industry. When an employee resigns in the heat of the moment, it can disrupt patient appointments and care plans. Therefore, it's essential to have a contingency plan in place to manage
patient care during the transition period. Depending on the role of the resigning employee, you might need to reassign their responsibilities temporarily or hire additional employees. Communicate with patients affected by the transition, explaining the situation and any changes to their appointments if necessary. Ensure that patient care remains a top priority throughout this process.
Proper documentation of the resignation is vital for maintaining clear records and protecting your practice from potential legal issues. Document the date and circumstances of the resignation, any discussions that took place, and any agreements or resolutions that were reached during the follow-up meeting. This documentation can be valuable in case of any future disputes or questions regarding the resignation.
Overall, managing heat-of-the-moment resignations in the dental industry requires a combination of emotional intelligence, effective communication, and a proactive approach. By staying calm, assessing the situation, offering support, setting clear protocols, considering the impact on patient care, and documenting the resignation, practices can navigate these challenging situations with professionalism and minimise the overall impact on the dental practice. Remember that prevention is always preferable to reaction, so work to create a positive work environment where open communication and problem-solving are the norm, reducing the likelihood of impulsive resignations in the first place.
For more information on this article please call the ADA HR Advisory Service on 1300 232 462.

6.5 CPD
Saturday 20 April 9.00am - 5.00pm
ADA HOUSE $828 members
COURSE OUTLINE
The science of Orofacial Pain and Temporomandibular Disorders have gone through explosive changes over the past five decades. This one day course will provide a review of OFP and TMD, screening for these disorders, help identify ominous signs of OFP and make succinct, prompt referrals to oral medicine specialists and medical colleagues and suggest ways to help avoid the frustration of managing these conditions.
There will be a hands-on component to the course.
LEARNING OUTCOMES
• To have a broad understanding of Orofacial Pain and TMD
• To understand the clinical screening for OFP conditions and ominous signs of pain
• Learn basic cranial nerve screening
• Learn basic clinical OFP examination and TMJ examination
• To learn head and neck screening in the context of OFP and TMD
• To begin to understand when and to whom to refer a case of OFP/TMD to.
Dr Davis Thomas completed his Bachelor of Dental Surgery (BDS) from India. He received his Doctor of Dental Surgery (DDS) and one year of Advanced Education in General Dentistry from NYU. While in private practice, he then went on to further his education in the following twenty years to include multiple master’s degrees including orofacial pain (Rutgers University), headache pain management (University of Edinburgh), and sleep medicine (University of Sydney). As an Associate Clinical Professor (14 years), Dr. Thomas now continues his research in Pain Management at Rutgers School of Dental Medicine and Eastman Dental Center, Rochester, New York.
30 TUES
AUGUST
9 FRI
10 SAT
15
16
31
Drs El-Hakim, Alex Park and Jenny Ball
UWA Dental School
Business Series 4
Enore Panetta, Drs Martin Webb, Amit Gurbaxani, Brian Koch and Alex Park
ADA House
Restore My First Implant - August
Drs Graham Carmichael and Glen Liddelow
THE BRANEMARK CENTRE
Practical Oral Surgery - August
Drs Carolyn Stulner, Mario Alberghini, Sophie Mougos, Magdalen Foo, Lee Kaing, Frank Chang
UWA Dental School
Dr Greg Celine
Dr Mark Johnstone
ADA House
Drs G Cheung, L Leask and Mr D Owen
ADA House
september
7
Drs Leticia Algarves Miranda and Mahnaz Syed
ADA House
UWA
14
20
21
27
Drs
THE
12
13
Dr Vishal Gupta
UWA
Dr Vishal Gupta
UWA
J Ryan, K Creasy, G Bishop, A Maurice, B Potter ADA House
Drs Carolyn Stulner, Mario Alberghini, Sophie Mougos, Magdalen Foo, Lee Kaing, Frank Chang
CTEC
November 1 FRI
Beautiful Periodontics In Beautiful Albany
Dr Ahmed Saleh
Hilton Garden Inn Albany
8/9 FRI/SAT
13 WED
14 THUR
23 SAT
30 SAT
Porcelain Veneers and Ceramic Onlays
Drs Asheen Behari and Paul Gorgolis
UWA DENTAL SCHOOL
CPR Refresher Hands-On Course
Surf Life Saving WA
ADA House
Digital Smile Design Dinner
Dr Sally McMullen UNIVERSITY CLUB
Endodontic Series 5
Dr Sharzad Nazari, Stephen Kwang, Jane McCarthy, Colm Harney, Gaurav Vasudeva
ADA House
Direct Veneers
Dr Joshua Graieg and Clin A Prof Glen Liddelow
4
29 March – 14 April
29 June – 14 July
21 Sept – 6 Oct
3
25
13 Dec – 4 Feb

3 CPD Saturday 4 May 12.15pm - 3.00pm
COURSE OUTLINE
Join Dr Wendy Gill for a long lunch to talk about all things gums.
TOPICS COVERED
• Keys to communicating periodontitis to patients
• What’s new in preventing and dealing with recession
• Is there a role for the use of laser in periodontology?
Amelia Park Restaurant is a family-owned and run restaurant where down to earth service, a sophisticated setting and honest food meet – all for exceptional value. To dine here is to experience Margaret River the way one should: through locally-sourced produce, expressive wine and quintessential vineyard views.
Course includes: A bespoke 3 course menu with wine.
Dr Wendy Gill graduated from UWA in 1994 and spent 9 years in general practice before completing her Masters Degree in Periodontology in 2006. Wendy obtained her Fellowship of the Royal Australasian College of Dental Surgeons (Perio) in the same year and started Alliance Periodontics and Implant Dentistry in 2008. In 2014 Wendy underwent extensive additional training in the use of dental lasers for treatment of periodontal and peri implant diseases. She is actively involved with the International Team for Implantology and runs a study club for dentists and dental specialists in Perth. She also lectures locally, nationally and internationally on periodontal and dental implant topics.
The final fixture of 2023 was held at the Royal Fremantle Golf Club, where a strong field of 31 golfers gathered to contest the Lester Charlesworth Trophy, sponsored by David Owen from Swan Valley Dental Laboratory. This trophy dates back to 1980, which is contested as a Better Ball par event, with a concurrent individual par competition.
Following golf, presentations and dinner were held in the RFGC with announcement of the Cec White Trophy winner for the best golfer of the year.
The Course was in great condition, but the strong sea breeze ensured a difficult day out on the field – also a couple of temporary greens added to the drama of the day.
Individually it was difficult to garner great scores but as teams many players paired well and only one combination had a minus score. Several players had returned from rests during the year including Garry Bishop after shoulder surgery, which seems to have given him ‘turbo’ powered golf now!
3rd hole Patrick Douglas
Health Practice Brokers
8th hole Frank Welten
Dentsply Sirona
11th hole Richard Williams
Insight Ceramics
12th hole Ian McCarrey
Healthlinc
17th hole Garry Bishop
Swan Valley Dental Laboratory
Individual Par event
Third on +3: Keenan Inderjeeth
Second on +4: Frank Welten
First on +6: Garry Bishop
Lester Charlesworth Trophy winners were Michael Welten and Nav Mahendran on +9 Pts. Well done!
The evening concluded with presentation of the Cec White Trophy; the winner determined by an aggregate of results over the nine WADA Golf events during the year. It was a well fought battle between the two Scots Patrick Douglas and Russell Gordon, but in the end with two wins and a second on 35pts was Patrick Douglas.
We enjoyed a strong membership in 2023 with just on 50 dental golfers and industry representatives participating in the various events. There is always room for more and should you be interested in a game; please get in touch via email to be included on our mailing list.
We have been fortunate to have financial support from several corporate sponsors throughout the year and once again thank Brad Potter from The Health Linc, the team from Dentsply Sirona, Garry Bishop from Health Practice Brokers, David Owen from Swan Valley Dental Laboratory and Andreas Vivanco and Angus Wilshaw from Insight Dental Ceramics and ADAWA for their support of WADA Golf.
Good golfing
Frank Welten
WADA Golf Captain
Dentistgolf@gmail.com

From the dawn of the internet and virtual communication, it became apparent this new and exciting medium that could democratise and open the world to all, had significant potential to be a double-edged sword.
On the plus side of the ledger, the benefits of constructive engagement with the internet/social media for dental professionals can be:
• Building an online presence, alongside the bricks and mortar practice premises.
• Branding and marketing, which with clever optimisation can direct messaging in a much more targeted fashion based on, for example, locations, demographics, interests –anyone remember the blunt tool of the Yellow Pages?
• Patient education to enhance branding, provide resources and even assist with consent.
• Patient engagement/ communication – everything from booking appointments to current messaging about COVID protocols.
• Networking and professional development with peers both locally, nationally and globally became instant and seamless. However, as with everything in life, with benefits and rights comes downsides and responsibilities. Back in the day it really was a new frontier where rules around responsible use and ethical behaviour were generally several steps behind the day-to-day reality of online interaction. Very quickly, flaming, as it
became known, emerged as a recognised phenomenon from the anonymity of forums and chatrooms –the act of posting insulting, hurtful, and often offensive content on the internet.
Once identified, it was soon followed up by academic studies and one of the most well-known was Suler in 2004 who identified and named the online disinhibition effect1. This study suggested, something that we all intuitively know now, that people often feel more liberated and less inhibited when communicating online, compared to face-to-face interactions. This can lead to both positive and negative behaviours.
A lowering of inhibition can have positive effects:
• Self-expression: The anonymity and perceived distance from realworld consequences can empower people to share their thoughts, feelings, and experiences more openly.
• Supportive communities: Online communities, such as support groups or forums, can foster a sense of belonging and provide individuals with a safe space to discuss sensitive issues.
• Creativity and collaboration: Online disinhibition can lead to creative collaborations and brainstorming sessions.
Very quickly categories of negative outcomes were identified:
• Cyberbullying: The anonymity and reduced empathy in online interactions can lead some individuals to engage in hurtful behaviour they might never consider in face-to-face situations.
• Trolling: Some people use anonymity as a shield to provoke reactions and create chaos, disrupting online spaces and causing harm.
• Hate speech and extremism: People may feel emboldened to express extreme views online, leading to the formation of echo chambers and radicalisation.

Suler identified the primary factors that contribute to online disinhibition:
• Anonymity: Many online platforms allow users to interact without revealing their true identities, leading to a sense of detachment from real-world consequences.
• Invisibility: Online interactions often lack physical cues, such as body language and facial expressions, making it easier for individuals to misinterpret messages and express themselves without the usual inhibitions.
• Dissociative imagination: Some individuals create personas or adopt online alter egos, further distancing themselves from their offline identities, which can result in more extreme behaviours.
• Minimisation of authority: The absence of traditional authority figures online
can lead to a lack of social norms and consequences, encouraging people to express themselves more freely.
Interestingly, a study from 2015 from the Australian Medical Journal2, which surveyed medical students from the 20 medical schools across Australia, found that social media use by the study population of medical students was nearly universal – not surprising; however, 34.7% of respondents, about 1 in 3, reported evidence of unprofessional content on their accounts. This unprofessional content was reported despite exposure to guidelines (in place since 2010) and education about online professionalism. This is relevant, as unprofessional conduct (online or offline) by a medical student may lead to disciplinary action and has also been found to be associated with lapses during later professional practice. When we at Dental Protection review cases and claims, part of what can be very relevant to the genesis of a complaint is the communication between patient and the practitioner – for example additional discussions around consent or variations in plans, patients signalling dissatisfaction with some aspect of care well before things blow up or evidence of increasing non-compliance or disengagement such as frequent rescheduling by either patient or practice. Many of these communications now occur online either by emails, messaging apps or even via online reviews.
It is a given that the practitioner, and by default the practice, must be the adult in the room in all communications – engaging responsibly and demonstrating they have the best interest of the patient at heart in all interactions. Importantly, just because a patient behaves inappropriately online does not mean we have to engage or behave the same way.
Sadly, looking over cases and how they spiral downwards, we sometimes see instances of the online disinhibition
effect in both patient and practitioner communications. For example:
• Patients being abusive or swearing in online messaging, which they would never otherwise do in a face-to-face interaction at the surgery.
• Patients demonstrating impulsive behaviour or constantly changing their minds. For certain patients, every unfiltered thought bubble is offloaded into the ether for the practitioner’s consideration as they believe they have 24/7 access to the practitioner via messaging apps. Again, this erratic interaction would be impossible in a face-to-face interaction.
• Online reviews, which bend or distort facts to suit a narrative or are posted as a consequence of emotional venting.
• Practitioners inadvertently breaching patient confidentiality by, for example, communicating with a party other than the patient about their care. The common trap is a response to the emotive and hurtful online review, divulging clinical information in a public forum.
• Practitioners getting bombarded by messaging at all times of the day and responding from a place of exasperation, or even worse with a few drinks on board after hours – it is easy to see how the disinhibition effect might be compounded.
• Practitioners initiating or responding to communications with a patient that may be sailing close to or crossing personal boundaries. For example subsequent conversations of a personal nature flowing from a friend/ follow request on social media (see above reference to alcohol/ after hours).
Social media platforms are continually evolving, with new features and algorithms. If dentists are going to enter the arena and engage in the virtual world, they must not only stay informed and adapt their
strategies to remain effective in reaching their audience – they must ensure they are compliant with guidelines, for example set down by our regulator, and be mindful of the online disinhibition effect. In broad terms, this necessitates a commitment to ongoing learning and improvement.
• Education and training: Healthcare professionals should educate themselves in the responsible use of social media. This should cover privacy regulations, ethical considerations, and the potential risks associated with social media engagement. The 2015 study cited earlier stated that medical educators “should consider approaches beyond simply providing guidelines or policies on professional behaviour, and students should be regularly prompted to reflect on their activities, to evaluate their online behaviours, and to temper them if appropriate”.
• Professional codes of conduct: Professionals should have a good working understanding of these codes, which can help clarify the boundaries and expectations for healthcare professionals. The Dental Board has specific guidelines in relation to social media use3 .
• Privacy controls: It goes without saying that healthcare organizations should implement strict privacy controls to protect patient information, and we have a podcast on that very topic. These controls should loop back to education on Privacy requirements and boundaries for appropriate behaviour online.
• Patient consent: Before sharing patient-related content on social media, healthcare providers must obtain informed consent from the patient. Patients should be informed about the potential risks and benefits of sharing their stories or medical information.
• Fact-checking and verification: To combat the spread of misinformation, healthcare professionals and organisations should be diligent in fact-checking information before sharing it. Encouraging critical thinking and providing credible sources can help patients distinguish reliable information from unreliable content. Remember, if you want increased and targeted access to patients via direct messaging or social media, the reverse will be true – they will expect more access and responsiveness from you and your practice too.
While there is much to consider here, most of this knowledge is now embedded in the culture and something we are all conscious of as members of the digital community. The point, however, is that once we move from interactions in the presence of our patients where we can look them in the eyes, to the online space, we need to be vigilant of the online disinhibition effect –where we might be provoked into reacting without considering the consequences or even communicating innocently in a manner where we can’t see social cues and messages that may be misinterpreted. Regardless of the medium, an old adage that is now truer than ever in this world of immediate communication – if in doubt about pressing Send, sleep on it and it will still be there tomorrow – hopefully, in the cold light of day, common sense will prevail. And finally, we are always here to help too –it’s not just if you have a case or a claim, but as dental practitioners too we understand these dilemmas and can help you take a deep breath and form an objective view on the question at hand.
1Cyberpsychology & behavior: the impact of the Internet, multimedia and virtual reality on behavior and society 7(3):321-6; 2004
2Unprofessional behaviour on social media by medical students, The Medical Journal of Australia · December 2015 DOI: 10.5694/mja15.00272
3https://www.dentalboard.gov.au/Codes-Guidelines/PoliciesCodes-Guidelines/Social-media-guidance.aspx
Thank you, Oceanic Dental Oceanic Dental have renewed their sponsorship agreement and will continue to support the ADA Dental Health Foundation’s pro bono dental programs for 2024. Claire Rawlinson, National Manager of ADA DHF says:
“The positive impact of our programs on patients fortunate enough to benefit from our services is undeniable. Oceanic Dental sponsorship has played a crucial role in our mission to provide timely dental care to those from disadvantaged backgrounds who would otherwise face challenges in accessing such essential services. We are grateful for Oceanic Dental commitment to making a meaningful difference in the lives of those in need, and we look forward to the possibility of continuing this impactful journey together.”


The Class of 1983 gathered for their 40-year reunion in November. Organised by Stuart Phillips, Graeme Washbourne and Jenny Ball, the reunion was held at Una Més, Menora.
The Young Dentists’ Conference held in November was a roaring success. Thank you to the attendees, speakers and organisers, who all contributed to such a great event.
Congratulations to Dr Gary Mack who was named the Town of Cambridge Mayor late last year. All the best for this exciting role!


Congratulations to WA’s newest dentists
Congratulations to the class of 2023, who had their graduation ceremony late last year at Winthrop Hall. ADAWA was also pleased to host a Transition to Practice dinner, to welcome the graduating students to the profession.
Remember, World Oral Health Day is on March 20. The new theme for the next three years from FDI World Dental Federation for World Oral Health Day is “A Happy Mouth is…”, with Toothie the beaver mascot – in 2024, the message is ‘A Happy Mouth is a Happy Body!’. For details and resources go to worldoralhealthday.org
Drs Peter Duke and Amit Gurbuxani received ADAWA Honorary Life Memberships at our Annual General Meeting – both recognised for their contribution to the association.
Congratulations to Peter and Amit!

Thank you, Dr Jenny Ball
We celebrated the contribution of Dr Jenny Ball to the association at her last ADAWA Council meeting late last year. Jenny has been on the ADAWA Council for well over a decade (including 7 years on Executive and 2 years as President). Even though she will not be at Council meetings, Jenny will continue in her role as coordinator of the joint ADAWA / UWA Dental CPD program, which will continue to provide high quality education and support to WA dentists.

Dr Vincenzo Figliomeni has compiled a list of tips which he has found to personally assist positive clinical outcomes to share with the membership and maybe make patients more comfortable too.
When placing rolls, rotate the roll along its length to insert it by rolling it down rather than simply placing/ pushing it. This will create lift of the tongue/vestibule which when recoiling will result in it being retained quite securely against the gingiva when the recoil effect causes it to try to derotate.
By placing a thin line of flowable composite at the gingival margin/ gingival floor will ensure adaptation of composite, avoiding ‘tug back’ at the margin and the eventual black line due to microleakage and also risk impaired bonding strength causing debonding. Prior careful placement of thin dry cord will also assist in controlling GCF which may contaminate the bonding interface leading to the black line of microleakage but also impaired bonding strength increased debonding. Some 'Conservative mechanical retentive groove elements (e.g. using a 006 round bur) which may also assist in reducing risk of debonding, these can be located apically at the gingivo-axial line angle and in the mesio and distoaxial line angles to triangulate the mechanical retention points resisting the buccally/outward orientated dislodgement forces.
Aesthetically positioned composite restorations may be challenging to perfectly blend in the transition line. One method of assisting is to not only bevel, but to also scallop the bevel and create corrugations within that scalloping. This will not only increase bonding surface area, but serve to refract the light through the transition zone better to blend the union of the material with the tooth. This is also useful for the coronal enamel in class V composite margins.
In office whitening systems have a higher concentration of peroxide resulting in the faster whitening effect. The sensitivity can occur due to the peroxide diffiusion to the pulp where catalase can trigger micro bubbles of oxygen at the odontoblastic layer and stretch of the axon receptor and resulting pain. A potassium nitrate sensitive toothpaste can reduce the depolarization threshold of the neurons and may be more effective than obtundent type pastes which work at the tooth surface. Mandibular incisors are smaller in cross section and the peroxide diffusion will reach the pulp sooner than other teeth, rather than applying gels over all teeth initially, consider staggering the gel application on

these teeth to a subsequent round to reduce sensitivity.
Will remove the microscopically contaminated root surface to allow for gingival reattachment. The removal of the higher content of fluoridated tooth surface may predispose to higher risk of root caries but also sensitivity due to tubule exposure. Consider a 5000 ppm toothpaste with potassium nitrate (e.g. Neutrafluor 5000 sensitive) which offers protection from root caries and post procedural pulpal hypersensitivity, improving patient comfort.
Is quite simple when using a 1:5 handpiece, using a tungsten carbide flat fissure type bur or similar and no irrigation and high speed approx. 150000 RPM, press the flat side against the tooth with sufficient pressure on and off to create heat which fractures the cement interface. Cool periodically, the heat is to be transmitted to the interface and not the pulp!
It can be easy to trap bubbles in the labial vestibule. When the impression has just been seated, pull the lip out labially, and gently press the tray posteriorly towards the back of the mouth, this will extrude the material apically and then muscle trimming will allow for the vestibule to be captured accurately.
It is good to remember bone is not always rigid and does have some
elasticity especially in younger patients. When luxating or using forceps on the tooth, hold some pressure in an actively luxated position for 10-30 seconds before luxating in a different position/ angulation/location. This will allow some time for the bone and periodontal ligament to stretch.
When taking bitewing radiographs at any age, but in particular with children with a shallow lingual vestibule, the edges of the film can feel sharp. To avoid film impingement, have the patient open wide and poke the tongue on the contralateral side while resting the film holder or tab on the mandibular teeth. Ask the patient to bite down slowly, this will move the film with the teeth during closure then the only area of discomfort will be if the positioning needs adjustment due to impingement on the palate.
Modern zirconia crown options often have improved aesthetics. Even so, depending on the brand and type of zirconia used, it may have a tendency for higher values/ brightness as generally the improved aesthetics is coupled with inferior physical properties. Consider trying a D shade to offset the high value with some grey. It often looks more natural to use a D2 than a standard A2 and can often match the properties of the natural tooth almost identically. The use of an appropriate cement can assist with modifying the value or blocking the stump discolouration when using a zirconia-based crown. Considering opaque or even glass ionomer for dark stumps vs
translucent can further assist the basic shade selection outcome.
Drags
When taking PVS impressions are often due to lack of sufficient wash material. Generosity with the wash in the undercut areas and all over the teeth will usually avoid bubbles and drags.
Post restoration occlusal contacts
When finalising post restoration occlusal contacts for largely intact dentitions, certain materials do not mimic the percussion of enamel. After checking with the usual routines, consider having the patient ‘snap’ the teeth together. This will quickly identify whether the centric contacts are still in enamel or whether more adjustment is required if there is a new restorative interference.
Glass ionomer cements
Achieve ionic bonding due to an acidic reaction with the tooth during

the acid base reaction. The highest acidity is immediately after mixing, therefore do not delay placement on the tooth and do not overmanipulate when it has been placed. This is also why the tooth must not be desiccated, to allow for ion exchange/movement through the damp.
While performing restorations in children careful education and guidance and allowing the child to respond to the sensations will facilitate trust. Often the child can raise their hand if tooth is ‘too itchy’ but a ‘little bit itchy is ok’, when ‘taking bugs out’ to let you know if you need to stop and being thankful to them for letting you know will retain trust and compliance. Sometimes switching from high speed to slow speed when too itchy ‘to try shake the bugs out instead’ will show you are responding to their action and that alone can be reassuring for them to allow for completion often without anaesthesia.
Dr Vincenzo Figliomeni is a ADAWA member dentist. He graduated in 2008 and after working in various private practices, currently owns and runs a private practice with his wife Angela who is also a dentist. Vincenzo works several roles including a long term on-call at Perth Children’s Hospital and remote oral health care provision through the Royal Flying Doctor Service. He was awarded Fellowship with the Royal Australasian College of Dental Surgeons in 2019 having completed his primary examinations with 5 subject commendations in 2015 and serves the college with positions on the WA Regional Committee as well as being the Assistant Registrar for the FRACDS(GDP) Program.

AMA Finance Brokers
ADA members are eligible to receive up to $2,000^ cashback on top of the cashback offer from the bank or lender (if eligible) on home loans successfully settled between 1 January 2024 and 31 December 2024.
Phone 1800 262 346 or email info@amafinance.com.au
Credabl has built a strong reputation offering tailored financial solutions. Whether you are looking to expand your practice, invest in medical equipment or explore personal finance options, Credabl's has you covered. Their suite of financial products includes medical equipment finance, practice loans, residential and commercial property loans, car finance and personal loans. credabl.com.au



Panetta McGrath Lawyers
We are excited to offer a member benefits program exclusive to ADAWA members. As a member of ADAWA, the member benefits program entitles you to an initial 30-minute consultation in person, by phone, or via video conference. ADAWA members are also eligible for a 15% discount on our standard hourly rates. pmlawyers.com.au

ADAWA members are entitled to a 12% discount on health cover each year when premiums are paid by direct debit. Existing HIF members need only call or email to have the discount applied to their membership.
Visit hif.com.au/adawa and use the access code ADAWA Alternatively call HIF on 1300 13 40 60 or email sales@hif.com.au

Dr Elizabeth Lam – new addition to the team
Bob Childs, Michael O'Halloran, Gareth Davies and Adrian Best are delighted to welcome Specialist Periodontist Dr Liz Lam to our Specialist Team at Cambridge Periodontics and Specialist Oral Surgery Perth. Liz looks forward to accepting referrals for all aspects of periodontics and implant surgery.
T (08) 9388 3453
F (08) 9388 3442
E cambridgeperio@bigpond.com
A 174 Cambridge St, West Leederville, WA 6007

Dr Biun, Oral and Maxillofacial Radiologist, has joined Clinical Professor Bernard Koong and Doctors Tom Huang, Dayea Oh and May Lam at Envision Medical Imaging. John is looking forward to assisting you with your radiological needs.
Wembley
T (08) 6382 3888
E bookings@envisionmi.com.au

A 178-190 Cambridge Street Wembley WA 6014
Booragoon
T (08) 6382 3888
E bookings@envisionmi.com.au
A 175 Davy Street Booragoon WA 6168
W envisionmi.com.au

Dr Samuel Bennett is delighted to announce the commencement of his contemporary boutique specialist orthodontic practice located in Nedlands. Sam and Team are committed to providing excellence and value of customised orthodontic treatment and care, in a relaxed and personable style. Referrals for children, teenagers, and adults are welcome for any orthodontic case, ranging from those requiring simple interceptive treatments to complex interdisciplinary care. Sam’s practice is situated at the corner of Stirling Highway and Loftus Street, with parking on premises.
T (08) 6507 4049
E bennettsamuelc@outlook.com
A Unit 1, 189 Stirling Hwy Nedlands WA 6009
W orthodontist-sb.com
Join us at the General Meeting with a presentation by Dr Andrew Savundra on Volunteer Orthodontics in East Timor.
ADA House
54-58 Havelock St West Perth
6.15pm Eat and Meet
7.15pm Meeting Followed by Lecture
RSVP to adawa.com.au/membership/rsvp

Dr Maleeha Gilani - new addition to the team
We are delighted to announce Specialist Paediatric Dentist Dr Maleeha Gilani has joined Dr Timothy Johnston and the team at iKids. Dr Gilani brings years of extensive dental experience and is now accepting referrals for all aspects of paediatric dental care.
T (08) 9433 6082
E ikids@ikidsdentalcare.com.au
A 94 Stirling Highway North Fremantle WA 6159 W ikidsdentalcare.com.au


Dr Gordon Cheung is excited to share the launch of his boutique specialised orthodontic practice located in Winthrop. Together with his team, Gordon is dedicated to delivering top-tier contemporary orthodontic care within a warm and inviting atmosphere. Dr Gordon personally treats each patient's treatment during every visit, ensuring the utmost quality in results. Referrals for patients of all ages are welcome, and Dr Gordon is available to consult in English, Mandarin or Cantonese.

(08) 9310 4911
admin@winthroportho.com.au
8/52 Hatherly Parade, Winthrop 6150 winthroportho.com.au
At Dental Essentials, we’ll take care of all your insurance needs big and small.
As the leading insurance broker for dentists in Australia, our team will work closely with you to create a tailored insurance policy that offers ultimate peace of mind.
With our extensive services covering Practice Insurance, Management Liability, Practice Indemnity, Cyber Insurance and Personal Insurance, at Dental Essentials, we take care to do things right.

1300

Everyday
At BOQ Specialist, we’ve been helping dentists with their banking needs for over 30 years. Not only do we understand your practice finance requirements, but your personal financial goals as well.
That’s why we offer a range of personal banking products, all with features and benefits to make day-to-day banking as easy as possible for you.
So, dive in today and enjoy the freedom of complete access to our suite of everyday banking products.
Visit boqspecialist.com.au/personal-banking or speak to your local finance specialist on 1300 160 160.