ACTS



Acts offers a holistic philosophy which supports residents along their life journey to well-being, consistent with the Acts Culture of Loving-Kindness, which integrates body, mind, and spirit across the continuum of living. Acts recognizes an individual’s uniqueness and affords each person the opportunity to achieve their best life through personal choice, engagement, spirituality, health, and wellness.


SECTION 1 Introduction pg 4
SECTION 2 Prospect to 365 (New Acts Residents) pg 10

SECTION 3 My Life Journey pg 12
SECTION 4 Engagement/Lifestyle pg 15
SECTION
SECTION
SECTION
SECTION
SECTION
SECTION
SECTION
SECTION
SECTION
Spiritual Life pg 21
Primary Care pg 25
Rehab Services pg 49
Fitness pg 55
Nutrition pg 66
Mental Health pg 74
Memory Support pg 76
Well-Being Product Process Outline pg
Well Being Protocols pg
SECTION 14 Alpha Pilot, St. Andrews Estates, Getting Started letter of interest, selection criteria, consent form pg
SECTION 15 Resident Well-Being Portfolio Sample pg 106
SECTION 16 Technology pg
SECTION
SECTION
Costs, Billing, Projected Financials pg
Research & Resources pg

The Acts Signature Well Being Product is a multidisciplinary integrated approach to develop a person centered, holistic scope of a Well Being Experience for the Independent Living Resident, with the goal of delivering a personalized Acts Signature Portfolio for each resident from a resident’s move in, to annual updates and ongoing touchpoints throughout the year.
Much like a financial portfolio, all Acts residents have many options to building their signature portfolio based on personal preferences, wants and needs. Development of a signature portfolio will be accomplished by:
• unifying concierge/navigation/coaching services that will support administrative, intake, scheduling, reminders, and routine support across all of our existing settings as a virtual, distributed location agnostic service.
• coordinating all health and wellness service touchpoints into an all-encompassed signature well being product that optimizes revenue capture and well being outcomes.
• incorporating risk sharing models (Medicare Advantage/other) to realize full benefits of our optimized signature well being outcomes.
There are many facets to the Acts Signature Well-Being Portfolio. The beginning stages of building the portfolio occur during the new resident move in process. By gathering general information pertinent to the resident, the structure of an Acts Signature Well-Being Portfolio is initiated, including topics such as:
• Previous Living Arrangements
Marital Status
Family and Cultural Heritage
Occupation/Previous Occupation
Education Level
Military
Religion
Milestones (Life)
A Well Being Health Coach and Well Being Concierge are assigned to each resident to provide continuous guidance in all facets of the Acts Signature Well Being Portfolio. Building upon the structure of information gathered during the new resident move in process, the Well Being Health Coach and Concierge will assist in expanding upon the resident’s portfolio with various questions based around the Seven Dimensions of Wellness (Physical, Spiritual, Vocational, Environmental, Intellectual, Social, and Emotional).
A variety of multi media means will be used based on resident preference (videotape, audio tape, one on-one interview, resident driven recording through the use of technology, hand written or typed documentation). This segment of data gathering is intended to be conversational in nature with the direction of the conversation driven by resident responses. Conversation starters include topics such as:
• Interesting stories or memories
• Love stories, vacation, family time, adventures, historical events
• A photo book, painting, or objects that have meaning
• Childhood upbringing or memories
• Relationships and family
• Historical and cultural
• Milestones, significant life events and accomplishments
Physical activity as we age offers a variety of health benefits like lessening chronic pain, delaying and preventing certain diseases, and helping recover quicker from an illness or injury. Staying connected with others helps give a sense of purpose and belonging and also has a major impact on overall well being. Social activity and engaged experiences provide a variety of benefits like better cognitive function, maintaining good emotional health, boosted immune system, enjoying restful sleep and increased longevity.
Further expansion of developing the Acts Signature Well Being Portfolio is around interests and activity previous, current or things a resident may have an interest in pursuing, everything from Art to Writing, to group activities, fitness, sporting events or joining a club. The Well being Coach will evaluate and connect a resident with others that have like interests; expand capabilities and opportunities for accessing interests; and provide avenues for new interests.
The spirit is an integral part of the overall well being of an individual. In many ways, it is a significant determinant of the well being of the other two dimensions -- body and mind. Community chaplains are a vital part of the interdisciplinary team. The community chaplain will conduct an initial spiritual assessment of new residents upon arrival to the community, followed by an annual assessment to determine each individual residents spiritual aspirations, needs and goals.
These assessments inform the spiritual services that the chaplain will provide to the individual resident.
Chaplains provide high quality Sunday worship experience, Bible studies, support groups, opportunities for talent utilization, opportunities for giving back to the community, as well as mission trips.
Chaplains also provide counseling with residents especially during times of loss, stress or turmoil in one's life (such as hospital visits).
All of these services are designed to help meet the spiritual needs of each individual. The overall goal is to provide each resident with a purposeful filled life throughout their residency at an Acts community.
Primary Care
A significant component of the Acts Well-Being Portfolio is healthcare and aging in place is vital. All independent living residents will receive an annual health and wellness evaluation. The Annual Health and Wellness Evaluation (AHWE) is a comprehensive medical visit designed to develop or update a personalized prevention plan to help prevent disease and disability, based on the resident’s current health and risk factors. Well Being expands beyond primary care and includes Rehabilitation, Nutritional Services, Behavioral/Mental Health Services and Memory Support, in addition to referrals as needed to specialists.
Performance of Medical Evaluation and Various Diagnostic Testing
Performance of Various Health Assessments such as Assessment of Cognitive Functions, Psychosocial and Behavioral risks, Mini Nutritional Assessment, Polypharmacy, Chronic conditions and Signs of elder mistreatment, In Home Risks and Activities of Daily Living and Instrumental ADLs
Audio screening
Cognitive testing
Mental Health Evaluation
Depression screening
High blood pressure
High cholesterol
Review of medical, legal and advance care planning
Risk Assessment
transmitted
management assessment
Screening
Completion of a personalized resident health advice and referral(s) for healthcare services and specialty providers such as:
Audiology
Behavioral Health/Mental Health Services
Cardiology
Dentistry
Diatitian
Home Health
Imaging Services
Many of these services (based on location) are offered on campus by visiting medical providers, if not an Acts provided service.
Completion of a Personalized Education, Preventive Counseling and Support Services Plan community based lifestyle interventions to reduce health risks and promote self-management and wellness:
Exercise Is The Best Medicine: THRIVE With Acts® is based on the recommendation that all older adults should be engaged in appropriately dosed exercise prescriptions for Energy, Flexibility, Strength, Balance and Mind In addition to THRIVE, the Acts Rehab team will complete assessments including:
• Physical Readiness Questionnaire
Pelvic Health
Pain recovery
Thrive Mind
Balance and Gait for Fall prevention
Acts therapists are medical professionals who are trained to assess all body systems and how they relate to one another in order achieve optimal physical and functional health. This includes taking into account the many diseases and conditions that tend to accumulate in older adults.
Acts Fitness programs are designed to offer a variety of opportunities to meet the physical activity needs and interests of our residents. Fitness programming includes a fully equipped fitness center, a variety of group exercise classes, recreational sports opportunities, and aquatic programming in communities with swimming pools. The certified fitness instructors are available to create a personalized fitness program to assist residents with meeting their health, fitness or functional goals and living to their full potential.
The fitness instructors work with each resident to create a program that will meet individual goals. They collaborate with the Nurse Practitioner, rehab and dieticians to assure that all programming is safe and effective. Recommendations are based on the interests of the residents and may include group exercise classes, aquatic programming, supervised individual exercise programming or exercise programs that can be done independently. The fitness/rehab partnership allows all residents to continue to exercise and continue to THRIVE following discharge from rehab.
A Mini Nutritional Assessment (MNA) is completed as part of the Annal Wellness Evaluation with referrals to the community’s Registered Dietitian Nutritionist (RDN) for further evaluation as needed.
Acts residents have the opportunity to consult with the Registered Dietitian Nutritionist (RDN) and receive in depth nutritional assessment and counseling to set priorities, establish goals, and create individualized vitality plans which acknowledge and foster responsibility for self care. The RDN works with the resident to find appropriate programs and services offered within the community to support resident needs and promote well-being Nutrition and independence.
Participation in the Acts meal plan provides a variety of dining options for the resident to select foods that align with their personal nutrition plan. Nutritional facts panels can be accessed through the resident portal to provide in depth information about macro- and micro-nutrient content and allergens. Community wellness programming by the RDN offers opportunities for resident exploration in current nutrition topics and healthy lifestyle.
Through the Annual Health and Wellness Evaluation (AHWE), the community’s Nurse Practitioner will complete assessments that will determine the potential need for mental health intervention or services. The Acts Mental Health Clinicians (MHC) serve as key members of the interdisciplinary care team and provide behavioral health assessments, care planning, therapy services, behavioral intervention, and case management to the ILU population.
The MHCs are clinical licensed Social Workers or Psychologists that conduct diagnostic interviews to identify psychosocial strengths and weaknesses and inform care planning. They also provide individual, family and group psychotherapy services, as indicated through assessment and care planning processes; they offer caregiver support and education to family members and provides educational programs to the Acts community staff.
The Acts Lifestyle Empowerment program, led by the Well Being Coach, provides structured guidance for residents (and their spouses) when experiencing mild cognitive impairment. Through participation in a comprehensive individualized lifestyle program, members experience empowerment, purpose, well being and joy while maintaining independence to live their best life, as well as they can, as long as they can. The Well Being Coach will guide member engagement in the program that addresses lifestyle factors including: cognitive engagement ♥ social engagement ♥ physical activity and exercise nutrition ♥ stress management ♥ sleep ♥ environmental sensitivity


The beginning stages of building the Acts Signature Well Being Portfolio occurs during the new resident move in process. The Life Care Consultant or Move In Coordinator gathers general information pertinent to the resident, including topics such as:
Marital Status
Family
Cultural Heritage
Occupation/Previous Occupation
Education Level
Military
Religion
Milestones (Life)
The information is documented and stored in SalesForce. Technology goals are being investigated to determine how this information can be shared with other system. The information will be made available to the Well Being Coach and Well Being Concierge.

Building upon the structure of information gathered during the new resident move in process, the Well Being Health Coach and/or Concierge will assist in expanding upon the resident’s portfolio with various questions based around the Seven dimensions of Wellness (Intellectual, Physical, Social, Spiritual, Vocational, Environmental, and Emotional).
Engaging in creative pursuits and intellectually stimulating activities is a proven approach to keeping minds alert and interested:
•
Tell us about the hobbies and interests that you currently enjoy.
• What is a new adventure, project, or hobby that you would like to try?
•
Tell us something new you would like to learn.
• What could we offer or develop via outside partnerships to help you reach your intellectual well being goals?
The goal of living independently is one shared by many people, and physical health and wellness is necessary to achieve this goal:
• What physical activities do you currently enjoy?
• What aspect of your physical health would you like to improve?
• What nutritional topic would you benefit most from learning more about?
• What physical activities are you doing now that you would like to still be doing in five years?
• What could we offer or develop via outside partnerships to help you reach your physical well-being goals?
Social interactions with family, friends, neighbors, and chosen peer groups can be valuable for maintaining health:
• What do you like to do when spending time with family and/or friends?
• How often do you like to get together with others?
• What similar interests would you like a new friend to have? How do you like to celebrate your birthday?
• What could we offer or develop via outside partnerships to help you reach your social well-being goals.
Living with meaning and purpose in life, guided by personal values, is key to feelings of well-being and connection to the larger world:
• Would you like to know about the spiritual activities and services we offer?
•
Would you like to tell us about your religious beliefs and the role they play in your life?
• Is there a spiritual milestone, a significant event, in your life about which you would like to tell us?
• Death is one of the realities of life and I’m curious to know your thoughts about it.
• What could the community offer or develop via outside partnerships to help you reach your spiritual well-being goals?
Work that utilizes a person’s skills while providing personal satisfaction is valuable for society as well as the individual:
•
If you would want to volunteer anywhere, now, where/what would you choose?
• If you were writing a resume today, what skill would you list as your most valuable?
• What could the community offer or develop via outside partnerships to help you reach your vocational well being goals?
• Have a list of volunteer opportunities available at the community
Environmental wellness is an awareness of the unstable state of the earth and the effects of your daily habits on the physical environment. It consists of maintaining a way of life that maximizes harmony with the earth and minimizes harm to the environment. It includes being involved in socially responsible activities to protect the environment.
Feelings are the lens through which people view the world, and the ability to be aware of and direct one’s feelings helps to create balance in life.
• Please describe one of the simple pleasures in life that you truly enjoy.
• How do you overcome feelings such as sadness and anxiety?
• Who/what brings joy to your life?
• What safety concerns do you have now?
• What could we offer or develop via outside partnerships to help you reach your emotional well being goals?
A variety of multi media means will be used based on resident preference (videotape, audio tape, one-on-one interview, resident driven recording through the use of technology, hand written or typed documentation). This segment of data gathering is intended to be conversational in nature with the direction of the conversation driven by resident responses.
*Technology to be used and electronic storage of the resident’s information – under investigation. For existing resident (vs new), the original My Story document (if previously completed by the resident) will be reviewed, updated and converted to the My Life Journey living document. This information will be made available to the Well Being Coach/Concierge for insertion into the residents Signature Well Being Portfolio.

The concierge will review the collected information from the Life Care Consultant and the resident’s My Life Journey documentation to date, captured by the Well Being Coach. The Well Being Concierge meets with the resident to orient them to community life (new residents) and will describe the many opportunities available within and outside the community. This visit is conducted in the resident’s apartment. For ease into community life, a resident buddy with similar interests, experiences and life goals is connected with the new resident. Newcomer socials are routinely scheduled.
Based on resident preferences, the Concierge will seek similar groups, individuals, events and opportunities and provide assistance for participation.
The Well Being Concierge will meet annually with the residents as well as conduct various touchpoints to review and update the residents’ interests, goals, and desires. The annual and intermittent touch points will continue to focus on the Seven Dimensions of Wellness:
• Intellectual
o Lecture series, Lifelong learning classes, museums, brain/memory classes, book clubs, volunteer opportunities, computer classes, movies
• Physical
o Walking paths, fitness centers, fitness classes, personal fitness training, bird watching, travel (day and overnight trips), healthy eating, dancing, recreational sports (pickleball, bocce, shuffleboard)
• Social
o Card and board games, happy hour, concerts, theatre, book clubs, sporting events, art classes, gardening
• Spiritual,
o Prayer and meditation group, religious services, writing classes – memoir
• Vocational
o Volunteer (committees, clubs, engagement, hospitality, marketing, grounds, buddy, culinary, fitness, call a friend)
• Environmental
o Recycling, taking care of the environment, getting outdoors and enjoy its beauty
• Emotional
o Stress reduction, meditation, mindfulness, connect with friends, yoga, tia chi, sleep, spa, massage therapist
In conjunction with the New Wellbeing pilot project at St. Andrews Estates, we conducted an online-only survey of IL residents to measure the level of interest in various events and opportunities that might be offered at the community. Residents for whom we had email addresses on file received an email invitation with a link to the survey. All residents received a letter in their mailboxes with a link and QR code directing them to the survey. Life Engagement staff also provided personal assistance to residents as requested.
As an incentive to respond, residents were eligible to win a $150 gift card for Ruth’s Chris Steakhouse. We received 189 responses: a response rate of 43%.
The survey was executed by the Acts IT Department using the Salesforce Surveys platform.
Residents indicated their likelihood to participate in various events and opportunities on the following scale:

The tables below show the average rating scores. Scores of 3.5 and above are the highest priority events and opportunities. Scores between 3.0 and 3.4 are secondary priorities. Scores below 3 are Lower priorities. Note that the events and opportunities are categorized as “Clinical” or “Engagement.”
Clinical Lab for bloodwork 4.7
Clinical Podiatrist (feet) 4.1
Clinical Fall prevention 3.9
Clinical Care coordinator for health care 3.8
Engagement Outdoor walking paths 4.6
Engagement Attend concerts 4.5
Engagement Attend theater 4.4
Engagement Travel day trips 4.3
Engagement Lecture series 4.1
Engagement Spa for massage, facials, mani/pedi, etc. 4.1
Engagement
Computer/Technology Classes 4.1
Engagement Attend movies 4.1
Engagement Lifelong Learning classes 4.1
Engagement Museum visits 4.0
Engagement Attend comedian performances 3.9
Engagement Attend dance troupe performances 3.8
Engagement Brain fitness/Memory improvement 3.7
Engagement Play cards 3.6
Engagement Go out to dinner at a local area restaurant 3.5
Clinical Optometrist/Ophthalmologist (vision) 3.4
Clinical Audiologist (hearing) 3.3
Clinical Mental health counseling 2.7
Clinical Dentist 2.7
Clinical Mammograms 2.1
Engagement Dietician/Nutritionist 3.2
Engagement Board games 3.2
Engagement Caregiver support 3.1
Engagement Personal fitness trainer 3.1
Engagement Travel overnight trips 2.9
Engagement Arts & Crafts 2.8
Engagement Book club 2.8
Engagement Other volunteer opportunities 2.6
Engagement Cruise trip 2.5
Engagement Bird watching 2.4
Engagement Attend sporting events 2.4
Engagement Learn a new language 2.4
Engagement Bible/Scriptures study 2.3
Engagement Art/Painting/Drawing 2.3
Engagement Room for prayer/meditation 2.2
Engagement Prayer/Meditation group 2.2
Engagement Virtual reality experience 2.1
Engagement Community gardening plot 2.1
Engagement Line dancing 2.1
Engagement Shuffleboard 2.0
Engagement Square dancing 2.0
Engagement Investment club 2.0
Engagement Mentoring younger people 2.0
Engagement Corn hole/bag toss 2.0
Engagement Bocce ball 1.9
Engagement
Writing memoir 1.8
Engagement Volunteer in OBT, WBC, or daytime respite program on campus 1.8
Engagement Calligraphy 1.8
Engagement Sewing/Knitting 1.8
Engagement Photography 1.7
Engagement Pottery/Sculpting 1.7
Engagement Hiking 1.7
Engagement Billiards/Pool table 1.6
Engagement Ballroom Dancing 1.6
Engagement Sing in a group/choir 1.6
Engagement Cooking class 1.5
Engagement Play chess 1.5
Engagement Casino trip 1.5
Engagement Biking 1.4
Engagement Videography 1.4
Engagement Acting 1.4
Engagement Play musical instrument 1.3
Engagement Writing creative/poetry 1.3
Engagement Horseshoes 1.3
Engagement Woodworking/Building 1.2
Engagement Tutor school age children 1.2
Engagement Baking 1.1
Engagement Camping 0.9
Engagement Play in a musical group 0.9
Engagement Fishing 0.8
Engagement Running/Jogging 0.8
Engagement Child care volunteer (day care, pre school) 0.7
Engagement Skydiving 0.3
We gave respondents the opportunity to write in additional suggestions. Most of the suggestions were more specific explanations of the rated events and opportunities, such as lecture topics, subjects for classes, and locations for trips.
One new suggestion was offered by ten residents: an indoor swimming pool All of the written suggestions are available on PowerBI at this link: https://app.powerbi.com/links/cOO94LTpty?ctid=595c195a 52dd 4ba2 aeea 1eaa7cccfe7a&pbi_source=linkShare
Residents offered suggestions for local organizations that SAE can partner with to offer events and opportunities. The most frequently mentioned are:
• Florida Atlantic University
• Lynne University
• Various local churches
The complete list of partnership suggestions is available on PowerBI at this link: https://app.powerbi.com/links/cOO94LTpty?ctid=595c195a 52dd 4ba2 aeea 1eaa7cccfe7a&pbi_source=linkShare
Based on these pilot survey results, it is recommend to shorten the questionnaire by eliminating events/opportunities that received an average score below 2.0. This will leave 48 events/opportunities for residents to rate.
Engagement and opportunity information based on residents goals, interests and desires will be made available to the Well Being Coach/Concierge for implementation and ongoing additions to the resident’s Signature Well Being Portfolio.

The Chaplain will meet with the resident and complete a spiritual assessment, A Purpose Filled Life. The goal for the Chaplain is to help each individual resident to find their God given purpose and meaning in life.
Within the first two weeks of a new move in, the Chaplain will make an initial visit to meet and welcome the resident. At this visit, the Chaplain will also complete initial spiritual assessment that focuses on building the spiritual component of “My Life Journey” using the following questions:
1. May I ask you about your religious beliefs?
2. What would you like us to know in relation to your faith background?
3. What role would you say your religious beliefs play in your life?
4. What spiritual activities, practices, or rituals are most significant to you?
5. Is there a spiritual milestone, a significant spiritual event, in your life you would like to tell us?
6. Are you experiencing spiritual struggles that you would like share with me?
7. What do you consider to be your spiritual gifts, talents, skills?
8. Would you like to know about the spiritual activities/services we offer?
9. Death is one of the realities of life and I’m curious to hear your thoughts about it.
10. How can I assist you to achieve your spiritual goals and preferences?
This information would then inform the overall ministry of the Chaplain to that individual resident, shape discussions in future visitation, inform focus areas of support group, Sunda y sermons, Bible studies, payer, meditation groups, etc.
These could occur monthly, or quarterly, but at least annually per resident. At these visits the Chaplain will make a follow up of the initial spiritual assessment visit to determine any changes or additions to the resident’s spiritual goals, needs, and aspirations. The Chaplain will use these on-going visits to keep the resident engaged and to build stronger connections & relationships with resident as a way of learning best ways to meet their spiritual needs and hence to inform the Chaplain’s ministry. The Chaplain will discuss with the resident any observations about the resident’s spiritual aspirations, expectations, and preferences the Chaplain may have noted since the last scheduled visit.
The Chaplain will write notes of his/her observations and discussions with the resident in the appropriate shared website area for the information of other stakeholders. As is the case with the initial visit, these observation statements will help to connect, maintain relationship, and shape the overall chaplain’s ministry to the individual resident.
We will endeavor to offer alternative in house TV worship service experiences of a quality that matches the in person chapel service experience, and this way help to increase choice, which is an important value of the baby boomer generation.
• The IT will do what it takes to ensure high quality of picture and other functions of our in house TV.
• The Chaplain will utilize PowerPoint presentations with songs, scriptures, sermon title, (including sermon main points is encouraged) for Sunday services, and other main services.
o This will enable the chaplain to bring the worship service experience to the resident apartment.
o It will increase participation (in singing, reading, sermon etc) of residents who may choose to attend the service remotely in the comfort of their apartments.
o It will enable the chaplain to engage those unable/unwilling to attend in person
• Of course, the chaplain must beware of the danger of isolation/seclusion of residents who may choose to only participate remotely.
We will present a clear and sound preaching and teaching of sermons and Bible Study lessons that bring the truth of biblical story alive and relevant to modern day seniors through the ministry of our chaplains.
• Each chaplain will be given access to Logos Bible Software a sermon preparation & Bible Study tool operated by Faithlife Corporation since 1992.
• Resources include commentaries, books on historical background of the biblical narrative, church history, systematic theology, Bible maps, several Bible versions critical for understanding a text.
• It’s non denominational and interdenominational, hence aligns with the Acts chaplains’ commitment to provide a non denominational service.
o This will help chaplains prepare high quality sermons & Bible Study lessons at a much shorter time.
Based upon the rationale that baby boomers want more participation and less spectatorship, we will provide a variety of opportunities that foster participation such as:
o Chaplains will create opportunities in which residents can continue to utilize their talents (time, skills, treasure, experience) as a way of worship.
o Chaplains will be creative in identifying these talents (painting, coloring etc) and engaging residents in pertinent activity.
o Chaplains will create opportunities in which residents can get involved in the society to give back in service to the community, such as the following:
Serving in a Community Soup Kitchen.
Donating items to the less fortunate: local community clothing banks, food pantry, refugees, inmates.
Writing encouraging letters to military or missionary people.
Participating in worship service: Assigning residents to lead in singing, scripture reading, responsive reading, Bible Study, prayer meetings, playing instruments, serving communion, editing bulletins, folding bulletins, serving in the spiritual life committee, setting up chapel, alter guild.
Praying for others during national-day-of prayer, prayer service for employees during employee recognition week.
o Chaplains will arrange and take residents on mission trips.
1. Need to purchase “Logos Bible Software”
2. IT to assist with installation and Chaplain accessibility
3. IT to assist with ensuring high quality In House TV Picture Quality which in some communities it may require installing new system.
4. Electronic storage of the Spiritual Assessment is undetermined but under investigation Assessment data will be made available to the Well-Being Coach/Concierge for insertion into the residents Signature Well-Being Portfolio

Effective management of the unique needs of geriatric health requires routine health screenings, medical assessments and evaluation with a primary care provider. The Acts Nurse Practitioners offer primary care services in all its communities to participate in the care of our residents by providing high quality primary, acute, and specialty senior health care services, helping our residents live longer, healthier, happier lives.
Acts residents are provided with an ANNUAL HEALTH AND WELLNESS EVALUATION (AHWE) each calendar year. The AHWE is a comprehensive medical visit designed to develop and update a personalized prevention plan to help prevent disease and disability, based on the resident’s current health and risk factors. The AHWE includes the following:
Completion of a Health History Assessment and Resident Information Update
Performance of a Comprehensive Medical Evaluation
Performance of Various Health Screenings and Assessments
A Personalized Resident Health Advice and Referral Plan
Review of Medical, Legal and Advance Care Planning
The Acts NP Primary Care Practices are located on campus in the Wellness Suites. The Wellness Suites are staffed with Nurse Practitioners, Wellness Office Nurses, Wellness Office Coordinators and (in select communities), a Nurse Navigator. The Wellness staff play an integral role in the AWE and ongoing healthcare needs of the Acts residents.
1. Resident is scheduled for their pre annual interview by the Well Being Coach. The resident reports to the Wellness Office at the time of the appointment.
2. Wellness Office Coordinator reviews and updates (in real time) the resident’s health history and information and documents all changes and updates in the electronic medical record.
3. The Mini Nutritional Assessment and height and weight measurements are completed by the Wellness Office Nurse and recorded in the electronic medical record
4. Blood draw is done for routine blood testing. Processing is completed inhouse and/or sent to an outside lab for processing
5. Performance of Testing: EKG, Urinalysis, Body Comp Analysis, Bladder Scanning (as indicated)
Resident reports to the Wellness Suite for their scheduled visit with the Nurse Practitioner
• The NP will review all of the data provided by the Well Being Coach prior to the resident’s scheduled visit. The NP will conduct a physical exam and complete the assessments listed below. The majority of the assessments are incorporate in an Annual Wellness template that is available in the electronic health record system (NextGen).
and
of
(IADLs)
of
A
of
Following the visit, the NP will create a personalized resident health advise and referral plan and provide the completed plan to the Well Being Coach for insertion to the resident’s Signature Well Being Portfolio.
Guidelines for the Acts Signature Well-Being Annual Health and Wellness Visit are derived from CMS guidelines for Annual Wellness Visit for Medicare beneficiaries:
A review of any current opioid prescriptions means, with respect to the individual determined to have a current prescription for opioids, all of the following:
(i) A review of the potential risk factors to the individual for opioid use disorder;
(ii) An evaluation of the individual's severity of pain and current treatment plan;
(iii) The provision of information on non opioid treatment options; and (iv) A referral to a specialist, as appropriate.
Detection of any cognitive impairment means assessment of an individual's cognitive function by direct observation, with due consideration of information obtained by way of patient report, concerns raised by family members, friends, caretakers or others.
Eligible beneficiary means an individual who is no longer within 12 months after the effective date of his or her first Medicare Part B coverage period and who has not received either an initial preventive physical examination or an annual wellness visit providing a personalized prevention plan within the past 12 months.
Establishment of, or an update to the individual's medical and family history means, at minimum, the collection and documentation of the following:
(i) Past medical and surgical history, including experiences with illnesses, hospital stays, operations, allergies, injuries and treatments.
(ii) Use or exposure to medications and supplements, including calcium and vitamins.
(iii) Medical events in the beneficiary's parents and any siblings and children, including diseases that may be hereditary or place the individual at increased risk.
First annual wellness visit providing personalized prevention plan services means the following services furnished to an eligible beneficiary by a health professional that include, and take into account the results of, a health risk assessment, as those terms are defined in this section:
(i) Review (and administration if needed) of a health risk assessment (as defined in this section).
(ii) Establishment of an individual's medical and family history.
(iii) Establishment of a list of current providers and suppliers that are regularly involved in providing medical care to the individual.
(iv) Measurement of an individual's height, weight, body mass index (or waist circumference, if appropriate), blood pressure, and other routine measurements as deemed appropriate, based on the beneficiary's medical and family history.
(v) Detection of any cognitive impairment that the individual may have, as that term is defined in this section.
(vi) Review of the individual's potential (risk factors) for depression, including current or past experiences with depression or other mood disorders, based on the use of an appropriate screening instrument for persons without a current diagnosis of depression, which the health professional may select from various available standardized screening tests designed for this purpose and recognized by national medical professional organizations.
(vii)
Review of the individual's functional ability and level of safety, based on direct observation or the use of appropriate screening questions or a screening questionnaire, which the health professional as defined in this section may select from various available screening questions or standardized questionnaires designed for this purpose and recognized by national professional medical organizations.
(viii) Establishment of the following:
(A) A written screening schedule for the individual such as a checklist for the next 5 to 10 years, as appropriate, based on recommendations of the United States Preventive Services Task Force and the Advisory Committee on Immunization Practices, and the individual's health risk assessment (as that term is defined in this section), health status, screening history, and age appropriate preventive services covered by Medicare.
(B) A list of risk factors and conditions for which primary, secondary or tertiary interventions are recommended or are underway for the individual, including any mental health conditions or any such risk factors or conditions that have been identified through an initial preventive physical examination (as described under § 410.16 of this subpart), and a list of treatment options and their associated risks and benefits.
(ix) Furnishing of personalized health advice to the individual and a referral, as appropriate, to health education or preventive counseling services or programs aimed at reducing identified risk factors and improving self management, or community based lifestyle interventions to reduce health risks and promote self management and wellness, including weight loss, physical activity, smoking cessation, fall prevention, and nutrition.
(x) At the discretion of the beneficiary, furnish advance care planning services to include discussion about future care decisions that may need to be made, how the beneficiary can let others know about care preferences, and explanation of advance directives which may involve the completion of standard forms.
(xi) Furnishing of a review of any current opioid prescriptions as that term is defined in this section.
(xii) Screening for potential substance use disorders including a review of the individual's potential risk factors for substance use disorder and referral for treatment as appropriate.
(xiii) Any other element determined appropriate through the national coverage determination process.
(i) A physician who is a doctor of medicine or osteopathy (as defined in section 1861(r)(1) of the Act); or
(ii) A physician assistant, nurse practitioner, or clinical nurse specialist (as defined in section 1861(aa)(5) of the Act); or
(iii) A medical professional (including a health educator, a registered dietitian, or nutrition professional, or other licensed practitioner) or a team of such medical professionals, working under the direct supervision (as defined in § 410.32(b)(3)(ii)) of a physician as defined in paragraph (i) of this definition.
Health risk assessment means, for the purposes of this section, an evaluation tool that meets the following criteria:
(i) Collects self reported information about the beneficiary.
(ii) Can be administered independently by the beneficiary or administered by a health professional prior to or as part of the AWV encounter.
(iii) Is appropriately tailored to and takes into account the communication needs of underserved populations, persons with limited English proficiency, and persons with health literacy needs.
(iv) Takes no more than 20 minutes to complete.
(v) Addresses, at a minimum, the following topics:
(A) Demographic data, including but not limited to age, gender, race, and ethnicity.
(B) Self assessment of health status, frailty, and physical functioning.
(C) Psychosocial risks, including but not limited to, depression/life satisfaction, stress, anger, loneliness/social isolation, pain, and fatigue.
(D) Behavioral risks, including but not limited to, tobacco use, physical activity, nutrition and oral health, alcohol consumption, sexual health, motor vehicle safety (seat belt use), and home safety.
(E) Activities of daily living (ADLs), including but not limited to, dressing, feeding, toileting, grooming, physical ambulation (including balance/risk of falls), and bathing.
(F) Instrumental activities of daily living (IADLs), including but not limited to, shopping, food preparation, using the telephone, housekeeping, laundry, mode of transportation, responsibility for own medications, and ability to handle finances.
Review of the individual's functional ability and level of safety means, at minimum, assessment of the following topics:
(i) Hearing impairment.
(ii) Ability to successfully perform activities of daily living.
(iii) Fall risk.
(iv) Home safety.
Subsequent annual wellness visit providing personalized prevention plan services means the following services furnished to an eligible beneficiary by a health professional that include, and take into account the results of an updated health risk assessment, as those terms are defined in this section:
(i) Review (and administration, if needed) of an updated health risk assessment (as defined in this section).
(ii) An update of the individual's medical and family history.
(iii) An update of the list of current providers and suppliers that are regularly involved in providing medical care to the individual as that list was developed for the first annual wellness visit providing personalized prevention plan services or the previous subsequent annual wellness visit providing personalized prevention plan services.
(iv) Measurement of an individual's weight (or waist circumference), blood pressure and other routine measurements as deemed appropriate, based on the individual's medical and family history.
(v) Detection of any cognitive impairment that the individual may have, as that term is defined in this section.
(vi) An update to the following:
(A) The written screening schedule for the individual as that schedule is defined in paragraph (a) of this section for the first annual wellness visit providing personalized prevention plan services.
(B) The list of risk factors and conditions for which primary, secondary or tertiary interventions are recommended or are underway for the individual as that list was developed at the first annual wellness visit providing personalized prevention plan services or the previous subsequent annual wellness visit providing personalized prevention plan services.
(vii) Furnishing of personalized health advice to the individual and a referral, as appropriate, to health education or preventive counseling services or programs as that advice and related services are defined in paragraph (a) of this section.
(viii) At the discretion of the beneficiary, furnish advance care planning services to include discussion about future care decisions that may need to be made, how the beneficiary can let others know about care preferences, and explanation of advance directives which may involve the completion of standard forms.
(ix) Furnishing of a review of any current opioid prescriptions as that term is defined in this section.
(x) Screening for potential substance use disorders including a review of the individual's potential risk factors for substance use disorder and referral for treatment as appropriate.
(xi) Any other element determined appropriate through the national coverage determination process.
(b) Conditions for coverage of annual wellness visits providing personalized prevention plan services. Medicare Part B pays for first and subsequent annual wellness visits providing personalized prevention plan services that are furnished to an eligible beneficiary, as described in this section, if they are furnished by a health professional, as defined in this section.
(c) Limitations on coverage of an annual wellness visit providing personalized prevention plan services. Payment may not be made for either a first or a subsequent annual wellness visit providing personalized prevention plan services that is performed for an individual who is -
(1) Not an eligible beneficiary as described in this section.
(2) An eligible beneficiary as described in this section and who has had either an initial preventive physical examination as specified in § 410.16 of this subpart or either a first or a subsequent annual wellness visit providing personalized prevention plan services performed within the past 12 months.
(d) Effective date. Coverage for an annual wellness visit providing personalized prevention plan services is effective for services furnished on or after January 1, 2011.
Source: Code of Federal Regulation, Title 42, Chapter 4, Subchapter B, Part 410, Subpart B
A significant number of the primary care assessments are embedded within one comprehensive Annual Wellness Assessment Template:







The Pittsburgh Sleep Quality Index (PSQI) is an effective instrument used to measure the quality and patterns of sleep in adults. It differentiates “poor” from “good” sleep quality by measuring seven areas (components): subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medications, and daytime dysfunction over the last month.
The following questions relate to your usual sleep habits during the past month only. Your answers should indicate the most accurate reply for the majority of days and nights in the past month. Please answer all questions.
1. When have you usually gone to bed?
2. How long (in minutes) has it taken you to fall asleep each night?
3. What time have you usually gotten up in the morning?
4. How many hours of actual sleep did you get at night? How many hours were you in bed?
5. During the past month, how often have you had trouble sleeping because you Not during the past month (0) Less than once a week (1) Once or twice a week (2)
A. Cannot get to sleep within 30 minutes
B. Wake up in the middle of the night or early morning
C. Have to get up to use the bathroom
Cannot breathe comfortably
Cough or snore loudly
Feel too cold
Feel too hot
Have bad dreams
Have pain
Other reason (s), please describe, including how often you have had trouble sleeping because of this reason (s):
6. During the past month, how often have you taken medicine (prescribed or “over the
7. During the past month, how often have you had trouble staying awake while driving, eating meals, or engaging in social activity?
8. During the past month, how much of a problem has it been for you to keep up enthusiasm to get things done?
Three or more times a week (3)
9. During the past month, how would you rate your sleep quality overall? Very good (0) Fairly good (1) Fairly bad (2) Very bad (3)
Component 1 #9 Score
Component 2 #2 Score (<15min (0), 16 30min (1), 31 60 min (2), >60min (3)) + #5a Score (if sum is equal 0=0; 1 2=1; 3 4=2; 5 6=3)
C1
C2
Component 3 #4 Score (>7(0), 6 7 (1), 5 6 (2), <5 (3) C3
Component 4 (total # of hours asleep) / (total # of hours in bed) x 100 >85%=0, 75% 84%=!, 65% 74%=2, <65%=3
C4
Component 5 # sum of scores 5b to 5j (0=0; 1 9=1; 10 18=2; 19 27=3) C5
Component 6 #6 Score C6
Component 7 #7 Score + #8 score (0=0; 1 2=1; 3 4=2; 5 6=3) C7
Add the seven component scores together Global PSQI
A total score of “5” or greater is indicative of poor sleep quality.
If you scored “5” or more it is suggested that you discuss your sleep habits with a healthcare provider

NO supervision, direction or personal assistance.
WITH supervision, direction, personal assistance or total care.
Points:
(1 POINT) Bathes self completely or needs help in bathing only a single part of the body such as the back, genital area or disabled extremity.
(0 POINTS) Need help with bathing more than one part of the body, getting in or out of the tub or shower. Requires total bathing
Points:
(1 POINT) Get clothes from closets and drawers and puts on clothes and outer garments complete with fasteners. May have help tying shoes.
(1 POINT) Goes to toilet, gets on and off, arranges clothes, cleans genital area without help.
(0 POINTS) Needs help with dressing self or needs to be completely dressed.
(0 POINTS) Needs help transferring to the toilet, cleaning self or uses bedpan or commode.
Points:
(1 POINT) Moves in and out of bed or chair unassisted. Mechanical transfer aids are acceptable
Points:
CONTINENCE
(1 POINT) Exercises complete self control over urination and defecation.
(0 POINTS) Needs help in moving from bed to chair or requires a complete transfer.
(0 POINTS) Is partially or totally incontinent of bowel or bladder
Points:
FEEDING
(1 POINT) Gets food from plate into mouth without help. Preparation of food may be done by another person.
(0 POINTS) Needs partial or total help with feeding or requires parenteral feeding.
Points:
TOTAL POINTS: SCORING: 6 = High (patient independent) 0 = Low (patient very dependent
Source: try this: Best Practices in Nursing
Care to Older Adults, The Hartford Institute for Geriatric Nursing, New York University, College ofNursing, www.hartfordign.org.
Visual acuity (VA) is commonly referred to as the sharpness of vision, measured by the ability to discern letters or numbers at a given distance according to a fixed standard.
20/20 vision is considered "normal" vision, meaning you can read at 20 feet a letter that most people should be able to read at 20 feet.
If a patient reads the 20/200 line that means they can read at 20 feet the letters that people with "normal" vision can read at 200 feet. So at 20/200, your visual acuity is very poor.
1. Have patient stand at appropriate marking on floor.
2. If patient has glasses make sure they are wearing the proper glasses for distance vision.
3. Give patient occluder and have them cover the eye not being tested.
4. Have patient read the smallest line they can see on the chart
5. If patient reads all 5 letters correctly and there are more lines below then ask them to try the next line.
6. Repeat steps for opposite eye.
1. If the patient reads all the letters on the 20/30 line you would record their vision as 20/30.
2. If the patient is reading the 20/30 line and reads 3 out of the 5 letters correctly you would record that vision as 20/30 2.
3. If the patient is reading the 20/30 line and reads all the letters correctly and then reads 2 letters of the next line correct their vision would be 20/30+2.
4. You can use that notation with any line of vision no matter what the number of letters are.
1. If the patient can’t see any better than 20/40 try using the pinhole technique. This technique helps to focus the light and removes the effects of refractive errors such as myopia.
2. Using the occluder put the pinhole flap over the opening and have the patient wiggle the occluder back and forth until they find a hold that makes it look clearer for them.
3. Then have the patient read the next clearest line of vision that they can see.
4. Record the vision as PH: 20/___.
This questionnaire asks about difficulties due to health/mental health conditions. Health conditions include diseases or illnesses, other health problems that may be short or long lasting, injuries, mental or emotional problems, and problems with alcohol or drugs. Think back over the past 30 days and answer these questions thinking about how much difficulty you had doing the following activities. For each question, please circle only one response.
Numeric scores assigned to each of the items:
In the last 30 days, how much difficulty did you have in:
D1.1 Concentrating on doing something for ten
minutes?
D1.2 Remembering to do important things?
None Mild Moderate Severe Extreme or cannot do
None Mild Moderate Severe Extreme or cannot do
D1.3 Analyzing and finding solutions to problems in None Mild Moderate Severe Extreme or cannot doday to day life?
D1.4 Learning a new task, for example, learning how None Mild Moderate Severe Extreme or cannot doto get to a new place?
D1.5 Generally understanding what people say? None Mild Moderate Severe Extreme or cannot do
D1.6 Starting and maintaining a conversation?
None Mild Moderate Severe Extreme or cannot do
D2.2 Standing up from sitting down? None Mild Moderate Severe Extreme or cannot do
D2.3 Moving around inside your home?
D2.4 Getting out of your home?
None Mild Moderate Severe Extreme or cannot do
D2.1 Standing for long periods, such as 30 minutes? None Mild Moderate Severe Extreme or cannot do 25 5
None Mild Moderate Severe Extreme or cannot do
D2.5 Walking a long distance, such as a kilometer (or None Mild Moderate Severe Extreme or cannot doequivalent)?
D3.1 Washing your whole body?
D3.2 Getting dressed?
D3.3 Eating? None Mild Moderate Severe Extreme or cannot do
D3.4 Staying by yourself for a few days?
D4.2 Maintaining a friendship?
None Mild Moderate Severe Extreme or cannot do
None Mild Moderate Severe Extreme or cannot do 20 5
None Mild Moderate Severe Extreme or cannot do
None Mild Moderate Severe Extreme or cannot do
D4.3 Getting along with people who are close to None Mild Moderate Severe Extreme or cannot doyou?
D4.4 Making new friends?
D41 N Mild Mdt S Extreme or 25 5
D4.5 Sexual activities?
None Mild Moderate Severe Extreme or cannot do
None Mild Moderate Severe Extreme or cannot do
Numeric scores assigned to each of the items: 1
In the last 30 days, how much difficulty did you have in: Life activities—Household
D5.2 Doing most important household tasks well? None Mild Moderate Severe Extreme or cannot do
D5.3 Getting all of the household work done that None Mild Moderate Severe Extreme or cannot doyou needed to do?
D5.1 Taking care of your household responsibilities? None Mild Moderate Severe Extreme or cannot do 20 5
D5.4 Getting your household work done as quickly as None Mild Moderate Severe Extreme or cannot doneeded?
If you work (paid, non paid, self employed) or go to school, complete questions D5.5 D5.8, below. Otherwise, skip to D6.1. Because of your health condition, in the past 30 days, how much difficulty did you have in:
D5.5 Your day to day work/school?
D5.6 Doing your most important work/school tasks well?
D5.7 Getting all of the work done that you need to None Mild Moderate Severe Extreme or cannot dodo?
None Mild Moderate Severe Extreme or cannot do 20 5
None Mild Moderate Severe Extreme or cannot do
D5.8 Getting your work done as quickly as needed? None Mild Moderate Severe Extreme or cannot do
In the past 30 days:
D6.1 How much of a problem did you have in joining
in community activities (for example, festivities, religious, or other activities) in the same way as anyone else can?
D6.2 How much of a problem did you have because of barriers or hindrances around you?
How much of a problem did you have living
D6.3
D6.4 How much time did you spend on your health
None Mild Moderate Severe Extreme or cannot do
None Mild Moderate Severe Extreme or cannot dowith dignity because of the attitudes and actions of others?
None Some Moderate A Lot Extreme or cannot docondition or its consequences?
None Mild Moderate Severe Extreme or cannot do 40 5
D6.5 How much have you been emotionally affected None Mild Moderate Severe Extreme or cannot doby your health condition?
D6.6 How much has your health been a drain on the None Mild Moderate Severe Extreme or cannot dofinancial resources of you or your family?
D6.7 How much of a problem did your family have
None Mild Moderate Severe Extreme or cannot dobecause of your health problems?
D6.8 How much of a problem did you have in doing things by yourself for relaxation or pleasure?
None Mild Moderate Severe Extreme or cannot do
The adult self administered version of the World Health Organization Disability Assessment Schedule 2.0 (WHODAS 2.0) is a 36 item measure that assesses disability in adults age 18 years and older. It assesses disability across six domains, including understanding and communicating, getting around, self care, getting along with people, life activities (i.e., household, work, and/or school activities), and participation in society. If the adult individual is of impaired capacity and unable to complete the form (e.g., a patient with dementia), a knowledgeable informant may complete the proxy administered version of the measure, which is available at www.psychiatry.org/dsm5 Each item on the self administered version of the WHODAS 2.0 asks the individual to rate how much difficulty he or she has had in specific areas of functioning during the past 30 days.
WHODAS 2.0 Summary Scores: There are two basic options for computing the summary scores for the WHODAS 2.0 36 item full version.
Simple: The scores assigned to each of the items “none” (1), “mild” (2), “moderate” (3), “severe” (4), and “extreme” (5) are summed. This method is referred to as simple scoring because the scores from each of the items are simply added up without recoding or collapsing of response categories; thus, there is no weighting of individual items. This approach is practical to use as a hand scoring approach, and may be the method of choice in busy clinical settings or in paper and pencil interview situations. As a result, the simple sum of the scores of the items across all domains constitutes a statistic that is sufficient to describe the degree of functional limitations.
Complex: The more complex method of scoring is called “item-response-theory” (IRT) based scoring. It takes into account multiple levels of difficulty for each WHODAS 2.0 item. It takes the coding for each item response as “none,” “mild,” “moderate,” “severe,” and “extreme” separately, and then uses a computer to determine the summary score by differentially weighting the items and the levels of severity. The computer program is available from the WHO Web site. The scoring has three steps:
• Step 1 Summing of recoded item scores within each domain.
• Step 2 Summing of all six domain scores.
• Step 3 Converting the summary score into a metric ranging from 0 to 100 (where 0 = no disability; 100 = full disability).
WHODAS 2.0 Domain Scores: WHODAS 2.0 produces domain specific scores for six different functioning domains: cognition, mobility, self care, getting along, life activities (household and work/school) and participation.
WHODAS 2.0 Population Norms: For the population norms for IRT based scoring of the WHODAS 2.0 and for the population distribution of IRT based scores for WHODAS 2.0, please see http://www.who.int/classifications/icf/Pop_norms_distrib_IRT_scores.pdf
The clinician is asked to review the individual’s response on each item on the measure during the clinical interview and to indicate the self reported score for each item in the section provided for “Clinician Use Only.” However, if the clinician determines that the score on an item should be different based on the clinical interview and other information available, he or she may indicate a corrected score in the raw item score box. Based on findings from the DSM 5 Field Trials in adult patient samples across six sites in the United States and one in Canada, DSM 5 recommends calculation and use of average scores for each domain and for general disability. The average scores are comparable to the WHODAS 5 point scale, which allows the clinician to think of the individual’s disability in terms of none (1), mild (2), moderate (3), severe (4), or extreme (5). The average domain and general disability
scores were found to be reliable, easy to use, and clinically useful to the clinicians in the DSM 5 Field Trials. The average domain score is calculated by dividing the raw domain score by the number of items in the domain (e.g.,
if all the items within the “understanding and communicating” domain are rated as being moderate then the average domain score would be 18/6 = 3, indicating moderate disability). The average general disability score is calculated by dividing the raw overall score by number of items in the measure (i.e., 36). The individual should be encouraged to complete all of the items on the WHODAS 2.0. If no response is given on 10 or more items of the measure (i.e., more than 25% of the 36 total items), calculation of the simple and average general disability scores may not be helpful. If 10 or more of the total items on the measure are missing but the items for some of the domains are 75% 100% complete, the simple or average domain scores may be used for those domains.
To track change in the individual’s level of disability over time, the measure may be completed at regular intervals as clinically indicated, depending on the stability of the individual’s symptoms and treatment status. Consistently high scores on a particular domain may indicate significant and problematic areas for the individual that might warrant further assessment and intervention.


THRIVE with Acts was created to help seniors maintain the independent lifestyle they’re currently enjoying. It’s an individualized program that helps you to live better today, and stave off problems in the future. The sooner a resident is evaluated, the easier any issues are to resolve.
Our therapists are medical professionals who are trained to assess all bodily systems and how they relate to one another to achieve optimal physical and functional health. Their specialized skills and treatments provide a jump start or provide a tune up to allow full benefits of Acts Fit ness and Wellness programs. Because THRIVE with Acts dovetails with fitness programs, it’s easy to continue to maintain the gains made when transitioning from THRIVE with Acts to the Fitness Team.
A lot of older adults accept pain, shortness of breath, memory problems, and loss of balance as normal consequences of the aging process. At THRIVE with Acts, it doesn’t have to be that way. If a resident is happily leading an independent lifestyle, we’re here to make sure that continues. We not only maintain quality of life, often times we can improve it. THRIVE with Acts utilizes the skilled physical, occupational and speech therapists who are already on site to help residents maintain quality of life. We’re here to keep our residents thriving.
We start with a 15 minute screening to determine if a resident is aging normally. We examine flexibility, strength, energy, balance and memory, using gender and age specific standardized tests that give you an idea of where your individual capabilities fall. Our experts are trained to identify subtle signs of abnormal aging that could lead to more serious life altering consequences somewhere down the road. If we think there are areas where quality of life could be improved, we make recommendations.
Why it’s important: Strength is critical for independent living. Physician and researcher Mary Tinetti says “leg strength – not age or other measurements – was the single most powerful predictor as to whether a person was going to have to enter a nursing home.”
What we can do about it: Our physical and occupational therapists determine which muscles you need to strengthen in order to develop a safe strengthening plan.
Why it’s important: Two thirds of adults over 65 report falls every year, and two thirds of those will fall again within six months. For people over 85, one fall in ten results in a hip fracture –from which most individuals fail to fully recover.
What we can do about it: Balance improves only with regular practice that challenges your balance systems. We help to safely challenge balance and progress skills, while incorporating balance training into daily life.
Why it’s important: Flexibility exercises can reduce pain and the risk of injuries, reduce postural problems that can lead to falls, and improve blood flow to joints for pain relief.
What we can do about it: Our physical and occupational therapists know what muscles to stretch, and can provide education on how to stretch for lasting results, as well as what exercises to avoid. According to the American College of Sports Medicine, it takes as little as 150 minutes a week to...
Why it’s important: THRIVE WITH ACTS MIND is designed to protect Acts residents from developing dementia and to slow the progression of dementia before it is even noticeable.
What we can do about it: We address your unique set of risk factors and provide a personally tailored program of brain exercises and challenges that help to build attentiveness and mental processing, aid decision making and more.
Why it’s important: Energy is like love. The more you give, the more you get back.
What we can do about it: Our physical and occupational therapists will help determine what exercise and duration will work best to improve vital heart and lung functions. While maintaining the residents safety, we we’re working hard enough to make a difference
Instructions:
• Allow 6’ at the beginning and end of the measure to allow for acceleration and deceleration.
• Instruct client to walk at their usual pace .
• Do not tell the client where the timing will start and stop . One practice trial permitted. Test is not appropriate if human assistance is needed to walk.
• Start the timer when the midsagittal line of the trunk crosses the start line (after the 6’ pre walk)
• End the timer when the midsagittal line of the trunk crossed the end line (before the 6’ post walk)
• Repeat 3 times and calculate the average time
• <.5 m/sec is correlated with Frailty
• < .57 m/sec correlated with fall risk
• < .6m/sec is associated with increased risk of hospitalization
• Determine a 30 meter (98 feet, 5 inches) course to minimize turns. Minimal distance permitted for test is 50’
• Place a cone at each end
• Client sits in a chair at the starting line for 10 minutes
• Use the script in Rehab EBTK. Let the client know you will be nearby but cannot walk with them and do not talk to anyone. May use assistive device and O2 if needed . No practice session permitted
• Take pre test vitals
• Take RPE as soon as the client stands.
• In the last 15 seconds of test, prepare a chair for the client to sit immediately. If the client needs to sit before 2 minutes, the test is completed. May take standing rests, but timer continues.
• Take post vitals and compare to pre vitals
Gender/age
179 meters or 587 feet 166 meters or 544 feet
184 meters or 603 feet 155 meters or 508 feet
172 meters or 564 feet 146 meters or 479 feet
158 meters or 518 feet 141 meters or 462 feet
144 meters or 472 feet 134 meters or 439 feet
Instructions:
• Client stands against a wall with buttocks, back, and heels touching the wall
• Instruct the client to stand as tall as possible and attempt to push the back of the head into the wall.
• Ensure the client maintains a neutral cervical spine and does not substitute with cervical spine extension.
• Using a ruler from a lateral view, measure the distance between the occipital prominence and the wall.
0 cm (occiput touches wall) Reduced risk of thoracic compression fracture >1.2 cm Increased risk of compression fracture >4 cm Recommend x ray to rule out compression fracture. (consider pain, recent trauma or new change in posture when considering xray)
Instructions
• Client wears their regular footwear and uses their customary walking aid
• No physical assistance permitted.
• Clients starts by sitting is a seat that is 18” high, with back against the chair back, feet flat on the floor, and arms on the arm rests.
• Place a line on the floor (do not use a cone) 3 meters or 9’10” from the client’s toes.
• Instruct the patient as follows: “When I say GO, walk at your normal pace to the line on the floor, turn around, walk back to the chair and sit down.” The client is permitted one practice trial
• A gait belt may be used if safety is questionable The timer begins when the client’s buttocks leave the chair and stops when the client’s buttocks contact the chair.
Instructions
•
• Instruct the client to cross arms across their chest and rise to stand without use of hands
• Allow client to practice 1-2 times . Instruct the client that upon “Go”, they are to rise to full standing and sit again as many times as possible in 30 seconds
• If more than half way up at 30 seconds, the rep may be counted
• Record the number of repetitions completed in 30 seconds
0= health failure functional marker
1-8= Frail functional marker
• Client is seated with arm at side, shoulder in neutral rotation, elbow at 90 degrees flexion, forearm in neutral pronation/supination, wrist at 0 30 degrees extension. (Client can rest the forearm on an armrest of a chair with wrist positioned just over the end of the armrest) Dynamometer is set on second handle position
• Client is instructed to squeeze as hard as possible for 3 seconds. Cue to client to “squeeze harder”
• Clinician should watch for the needle to stop rising
• Complete 3 trials on each hand, alternating sides. Use maximum of the 6 trials as result
Gender Normal lbs Intermediate lbs. Weak lbs
Male 70.55 or greater 57.32 70.54 <57.32
Female 44.09 or greater 35.27 44.08 <35.27
Instructions:
• Client stands next to but not touching a wall and raises arm to 90 degrees of flexion , forearm in neutral with the hand open (Therapist should be sure the shoulder is not protracted or retracted Feet should be facing forward and a comfortable distance apart
• Mark the wall with tape the end of the 3rd finger. Instruct the client to “Reach as far forward as you can without taking a step or losing your balance. You are not allowed to touch the wall as you reach”
• Client is free to use various reaching strategies
• Clients may have 2 practice trials
• Mark the wall at the end of the 3rd finger
• Measure the distance between the starting and ending position. Repeat the test 3 times and average the scores
<6”=4x more likely to have 2 falls in next 6 months
6-10”=2x more likely to have 2 falls in next 6 months
Instructions
• Client stands barefoot or in safe footwear. Feet should be apart (about the length of the client’s foot)
• Client places hands on hips Guard client closely
• Instruct the client to slowly shift weight to either leg and lift the other foot slightly off the floor (client chooses).
•
Time how long the resident can hold the one leg stand position
• Start the timer when the foot clears the ground. Stop the timer when any of the following occurs:
o 30 seconds elapses
o Suspended foot touches the ground
o hands come off the hips
o Client uses suspended limb to support weight bearing limb, displacement of the weight bearing limb
<5 seconds =Increased risk of injurious fall
Instructions
• Give the patient a copy of the Trail Making Test Part A worksheet and a pen or pencil Demonstrate the test to the client using the sample sheet
• Time the client as he or she follows the “trail” made by the numbers on the test
• Record the time
• Repeat the procedure for Trail Making Test Part B using letters and numbers
Average MCI Alzheimer’s 29 seconds >48.1 seconds >67.1 seconds
Instructions
• Give the patient a copy of the Trail Making Test Part B worksheet and a pen or pencil. Demonstrate the test to the client using the sample sheet
• Time the client as he or she follows the “trail” made by the numbers on the test
• Record the time
Average MCI Alzheimer’s 75 seconds >136 seconds >190.8 seconds
Instructions
• Determine a 30 meter (98 feet, 5 inches) course to minimize turns
• Minimal distance permitted for test is 50’. Place a cone at each end
• Client sits in a chair at the starting line for 10 minutes
• Use the script in Rehab EBTK
• Let the client know you will be nearby but cannot walk with them and do not to talk to anyone. May use assistive device and O2 if needed
• No practice session permitted
• Take pre test vitals
• Take RPE as soon as the client stands
In the last 15 seconds of test, prepare a chair for the client to sit immediately. If the client needs to sit before 2 minutes, the test is completed.
• May take standing rests, but timer continues.
• Take post vitals and compare to pre vitals
Instructions
• Take resting vital signs
• Have client stand next to a wall
• Measure the height of the iliac crest and patella and mark it on the wall. Then place a piece of tape on the wall half the distance between the two
• On the signal “go” the client begins stepping (not running) in place, raising each knee to the mark on the wall, for as many times as possible in the 2 minute period. Only count the number of times the right knee reaches the required height. That is the score
• If the proper knee height cannot be maintained, ask the participant to slow down, or to stop until they can regain the proper form, but keep the stopwatch running
• At the end of the test, provide a cool down by asking the client to walk slowly for a minute
• A client with impaired balance may use the back of a chair or wall as a touch hold for stability
• Take post exercise vital signs
Scores less than 65 were associated with lower levels of functional ability community residing older adults ages 60 94
Instructions
• Utilize a chair 16.93 to 17.72” high. Chair should be free standing and not against a wall
• Instruct the client to cross arms across their chest and rise to stand without use of hands
• Demonstrate the test and allow client to practice 1-2 times
• Instruct the client that upon “Go”, they are to rise to full standing and sit again as fast as possible 5 times
• Examiner should count the reps out loud. If more than half way up at 5 seconds, the rep may be counted
• Record the time to complete 5 reps
Predictive of disability within 2 years >10 sec
Individuals in need of further fall risk assessment
sec
Identification of balance dysfunction ≥14.2 sec
Future fallers verses non fallers cut off time
sec
Parkinson’s Disease fall risk cut off >16 sec
• Client sits with back against the backrest of an ARMLESS chair
• Client is not permitted to lean forward from the backrest
• Client should use dominant hand. Start position: Arm should be fully extended to the side of the chair in neutral supination/pronation
• Place 5 lb. dumbbell in hand for women and 8 lb. for men
• Client is instructed to perform a biceps curl by flexing the elbow and supinating the forearm. Client needs to complete the curl by aiming palm to shoulder and return to full starting position. Start the timer when the client assumes the start test position
• Count the number of curls the client completes in 30 secs (1 rep = flex and return to extended elbow). If the client has completed 50% of the up motion at the end of 30 seconds, the rep can be counted
70 74 <14 14
79 <13
>21
>19
<13 13-19 >19
<11
94 <10 10
70-74 <12
<11
84 <10
89 <10
94 <8
>17
>14
>17
>17
>16
>15
>13
• Client sits on the edge of a 17”chair with one knee flexed to 90 degrees and foot flat on floor
• The other leg is extended at the knee with the ankle in dorsiflexion and the heel on the floor
• Client is instructed to place one hand on top of the other so the middle fingers overlap evenly
• Instruct the client to inhale and then exhale while reaching toward the toes of the outstretched leg
• Monitor and ensure the client flexes from the hip and keeps the trunk in neutral with the head up .Note how far the client can reach (without illiciting pain )
• Repeat with the other leg in order to determine the best side to measure
• Have the client practice 2 times on the chosen leg
• Measure the distance in inches from the tip of the extended middle finger and the tip of the great toe to the nearest ½ inch
• Perform 2 more trials and record the best of the 2.
• Great toe is reached: 0
• Great toe is not reached: - (inches from great toe)
• Great toe is passed: + (inches past great toe
Risk Markers/Norms
Age 60 64
Women (inches) 0.5±5.0 .5±4.5 1.0±4.0 1.5±3.5 2 ±3.0 2.5±2.5 4.5±1.0 Men (inches) 2.5±4.0 3.0±3.0 3.0±3.0 4.0±2.0 5.5±1.5 5.5±0.5 6.5±0.5
Instructions:
• Client stands and reaches one hand over the same shoulder with the palm facing toward the trunk and fingers extended
• Client takes other hand up from the waist with palm facing outward and fingers extended upward .
• Instruct the client to reach both hands toward each other as far as possible trying to touch or overlap the middle fingers
• Repeat the other direction of each arm
• Choose the direction that appears to give the best result. Client then practices on the chosen side 2 times.
• Measure the 3rd and 4th attempt and record the best score
• Measure the distance in inches between the 2 middle fingers .Record as “+” if the middle fingers overlap and as “ – “ if the middle fingers do not reach each other
• Do not allow the following: Breath holding, Rapid or ballistic movements, client grabbing of fingers or wrist in an attempt to gain additional range of motion, watch for scapular winging
70-74 75-79 80-84 85-89 90-94
4.0 ±1.0 5.0 ±.5 5.5±1.0 7.0 ±1.0 8.0 ±1.0
8.0 ±1.0 4.0 ±1.0 9.0 ±2.0 9.5 ±2.0 10.5±6.5
Instructions:
• Client wears their regular footwear and uses their customary walking aid .No physical assistance is given for the test
• Clients starts by sitting is a seat that is 18” high, with back against the chair back, feet flat on the floor, and arms on the arm rests.
• Place a line on the floor (do not use a cone) 3 meters or 9’10” from the client’s toes.
• Instruct the patient as follows: “When I say GO, walk at your normal pace to the line on the floor, turn around, walk back to the chair and sit down.” The client is permitted one practice trial . A gait belt may be used if safety is questionable
• The timer begins when the client’s buttocks leave the chair and stops when the client’s buttocks contact the chair.
• Record time for regular TUG, then repeat the test carrying a glass of water filled 1” from the top of the cup.
• Place the cup on a table next to the client .Give the following instructions:
• “When I say GO, walk at your normal pace to the line on the floor, turn around, walk back to the chair and sit down. Take the glass of water with you by any means you choose” (The client may pick up the cup and proceed or may stand, then pick up the cup.
• The client may set the cup on the table before sitting if they choose).
Difference of >4.5 sec between TUG and TUG manual predictive of risk of fall within the next 6 months.
Instructions:
• Client stands barefoot or in safe footwear
• Client places feet in tandem (heel to toe position with preferred limb in back). Guard client closely.
• Time how long the client can hold the test position
• Client may use a chair back support to attain test position
• Start the timer when the client assumes the test position
• Stop the timer when any of the following occurs: 30 seconds elapses/ Client takes a step or loses balance .
• Give 3 trials and average
< 10 sec=risk of falls
Instructions:
• Form a square by using 4 canes or 1” dowels so there are 4 18’x 18” squares (do not use tape).
• Demonstrate the test the test first
• Client begins in bottom left square and steps forward with each foot into square above, then to the right into square, then backward into square, then left to beginning square
• The client then reverses the same path stepping to the right, then forward, then to the left, then backward into the beginning square
• Client is permitted one practice trial, then 3 trials to obtain 2 valid timed trials
• Start the timer when the first foot touches square 2 and stops when both feet touch the original square 1.
• No instructions should be given during the test
• Guard closely trying not to make contact with the client
• Invalid trial: feet touching the canes, any loss of balance, not getting both feet into any of the squares
Fall risk indicators Risk Group >15 seconds community dwelling adults= risk multiple falls >12 seconds
Vestibular clients= risk of > 1 fall
Inability to obtain 2 valid trails in 3 attempts Risk of fall
Results of the THRIVE assessment and recommendations are recorded in the Rehab electronic medical record and made available to Well Being Coach for insertion into the resident’s Signature Well-Being Portfolio.

Physical activity and exercise play a vital role in health and wellbeing. The Acts fitness and recreational programs provide a variety of opportunities to engage in individual exercises, group exercise classes and recreational sports. The fitness staff work with each resident to design a personalized approach to physical activity or exercise to improve the ability to live longer, healthier, happier lives.
Acts residents are provided with an orientation to the fitness program and regular consultations to update programs as needs, goals and interests change. The orientation and consultations may include an individualized exercise program, recommendations for participation in group fitness classes and recreational sports programs.
Individualized exercise program include recommendations for the frequency, intensity, duration and mode of cardiovascular, muscular strength and endurance, flexibility, and balance training
Recommendations for participation in group exercise classes may include aerobic, strength, flexibility, balance, or aquatic classes as well as specialty classes such as Tai Chi, Yoga, Zumba, Line Dancing etc.
Recommendations for participation in recreational sports may include Bocce, Pickle Ball, Shuffleboard, Billiards, Bridge etc.
Fitness programming recommendations will include programs offered within the community as well as with partners within the community at large.
The Acts fitness instructors are certified fitness and aquatic professionals. The fitness instructors work in collaboration with the Wellness staff, Rehab staff, Life Engagement staff and Dietitians to provide safe and effective physical activity and exercise programs that meet the needs and interests of the Acts residents.
and strength
apps/devices to track
An introduction to fitness and recreational programming is available to new residents, residents that are interested in beginning an exercise or physical activity program or residents that are recently completing a THRIVE program.
• Fitness staff schedules a time to meet with residents to introduce themselves and the fitness and recreational program.
• Discuss the resident’s overall health, needs and interest, previous experiences and current participation in physical activity and recreational sports.
• Review programs that are offered within the community as well as in the community at large.
• Answer any questions and identify a plan for participation in physical activity and recreational programming.
The Well Being Coach will schedule a Fitness Assessment with the Fitness Center following the resident’s pre visit screening in the Wellness Suite. Fitness instructors will:
• Provide training on the use of the tracking devise
• Review tracking device data at predetermined intervals
• Complete assessment and goal setting
• Develop and schedule an exercise plan
The personalized approach to fitness and recreational programming may include a combination of an individual exercise program, attendance in group exercise classes and/or participation in recreational sports:
• Resident will schedule an orientation with the fitness director/trainer to identify programming options that will meet their needs and interests.
• Prior to meeting with the resident, the fitness staff will review the results of the AWE and the THRIVE screen and discuss potential limitations to physical activity with the NP, Wellness and Rehab staff
• It is recommended that residents that have not had a recent medical evaluation consult the NP, Wellness staff, medical provider or Rehab staff prior to engaging in a physical activity or exercise program
• Residents interested in an individualized exercise program will:
o Sign the Acknowledgement Form prior to beginning an exercise program
o Receive an orientation to the fitness equipment and policies for using the Fitness Center, and swimming pool if appropriate
o Receive a personalized exercise program, based on the resident’s specific fitness level, health and goals and interests
• Residents interested in participating in group exercise classes will:
o Receive an overview of the classes that will meet their specific fitness level, health and goals and interests
• Residents interested in participating in recreation sports will:
o Sign the Acknowledgement Form prior to participation in any program
o Receive information on the schedule and policies for participating in recreational programs
o Receive contact information for committees or individual residents that oversee recreational programming if appropriate
Fitness staff will follow up with residents:
• Every 6 months to provide motivation and encouragement and adjust programming based on new goals and interest
• Meetings to adjust programming will also be scheduled anytime there is a change in medical status, a change in participation or the resident shares a new goal or obtainment of a previous goal
Residents reporting or exhibiting changes in medical or functional status will be immediately referred to the NP, Wellness staff or Rehab staff for an evaluation.
Fitness assessments, goals and recommendations are made available to the Well Being Coach and implemented into the resident’s Signature Well Being Portfolio.
To the best of my knowledge, I am in good physical condition for exercise. I am fully aware of the risks and hazards connected with exercise and the use of exercise equipment, including physical injury (including but not limited to broken bones; muscle, tendon and ligament strains and tears; heart attack; stroke and the like) or even death, and hereby voluntarily elect to utilize the ACTS exercise space, amenities and equipment. I acknowledge that ACTS has recommended that I obtain a physical examination from my health care provider before utilizing the ACTS exercise space, amenities or equipment or beginning or changing any exercise program. I acknowledge that I will be using the ACTS exercise space, amenities and equipment (including, without limitation the exercise weights and machines, the pool, and my participation in any activity, class, program, or personal training) entirely at my own risk.
I agree that ACTS, its parents, members, su bsidiaries, affiliates, successors and assigns and each of their respective officers, directors, volunteers, employees, agents, representatives, owners, members and operators (collectively, the “Indemnified Parties”) shall not be liable for any accident, injury, damage, or loss or for any other matter that may happen to me or my property as a result of my use of the ACTS exercise space, amenities or equipment. I VOLUNTARILY ASSUME FULL RESPONSIBILITY FOR ANY RISK OR LOSS, PROPERTY DAMAGE, OR PERSONAL INJURY, INCLUDING DEATH that may be sustained by me as a result of my use of the ACTS exercise space, amenities or equipment. I shall indemnify, defend and hold harmless the Indemnified Parties from any and all costs (including but not limited to attorneys’ fees), losses or damages arising from or associated with my use of the ACTS exercise space, amenities and/or equipment.
I, on behalf of myself and my heirs, executors, administrators, personal representatives, successors and assigns, hereby RELEASE, WAIVE, HOLD HARMLESS, AND FOREVER DISCHARGE the Indemnified Parties from any and all claims, actions, causes of action, suits, damages, judgments and demands whatsoever, in law or equity whatsoever that I, my heirs, executors, administrators, personal representatives, successors and/or assigns may have ever had, now have, or hereafter can, shall or may ever have against the Indemnified Parties relating in any way to my use of the ACTS exercise space, amenities or equipment. In giving the foregoing, I hereby waive any and all rights which I may have to make any demands and claims against the Indemnified Parties related to my use of the ACTS exercise space, amenities or equipment and the same are forever barred.
In signing this Form, I acknowledge and represent that I understand that I am giving up, among other things, any and all rights I may have to sue the Indemnified Parties for injuries, damages or losses that I may incur as a result of my use of the ACTS exercise space, amenities and equipment. I HAVE READ THE FORGOING FORM, UNDERSTAND IT AND SIGN IT VOLUNTARILY. No oral representations, statements or inducements, apart from this Form, have been made. I EXECUTE THIS FORM FOR FULL, ADEQUATE AND COMPLETE CONSIDERATION FOR MY RIGHT TO USE THE ACTS EXERCISE SPACE, AMENITIES AND EQUIPMENT AND FULLY INTEND TO BE BOUND BY THE SAME.
By signing below I acknowledge that I have read this Form, understand that this is a legal document, and understand I have the right to consult with an attorney before signing the Form and using the ACTS exercise space, amenities and equipment.
NuStep Seat Setting Arm Setting Load # Time Distance

Cybercycle Seat # Level Time Distance Rider ID:
Recumbent Bike Seat # Level Time Distance


Treadmill Speed Incline Time Distance

1. Abdominal/ lower back extension Torso Setting Leg setting Weight
# Reps # Sets
Weight # Reps # Sets



Weight # Reps # Sets
Reps # Sets


A Mini Nutritional Assessment (MNA) is completed by the Wellness Office Nurse during the pre Annual Health and Wellness Exam. Residents that score at risk for malnutrition or malnourished on the Mini Nutritional Assessment (MNA) will be referred to the registered dietitian nutritionist (RDN) for further assessment and medical nutritional therapy (MNT).
Residents that score at normal nutritional status are entitled to meet with the RDN to address any nutrition questions or receive nutrition counseling. MNT or counseling provided by the RDN focuses on an individualized plan for well-being using a food as medicine approach. Food as medicine is a philosophy where food and nutrition aids individuals through interventions that support health and wellness. This approach incorporates a variety of programs and experiential opportunities to support/improve healthful eating at home and in the dining venues.
Acts residents have the opportunity to consult with the Registered Dietitian Nutritionist (RDN) and receive in depth nutritional assessment and counseling to set priorities, establish goals, and create individualized vitality plans which acknowledge and foster responsibility for self care. The RDN works with the resident to find appropriate programs and services offered within the community to support resident needs and promote well being Nutrition and independence.
Participation in the Acts meal plan provides a variety of dining options for the resident to select foods that align with their personal nutrition plan. Nutritional facts panels can be accessed through the resident portal to provide in depth information about macro- and micro nutrient content and allergens. Community wellness programming by the RDN offers opportunities for resident exploration in current nutrition topics and healthy lifestyle.
• The Mini Nutritional Assessment (MNA) is completed by the Wellness Office Nurse during the pre Annual Health and Wellness Exam along with the resident’s Health History and Information Update.
• The MNA score is recorded in the primary care electronic medical record (NextGen).
• Residents that score at risk of malnutrition or malnourished status (11 points or less) on the MNA will be referred to the RDN for follow up and assessment.
• Wellness staff contacts RDN to schedule for an appointment and provides the
• Medical Nutrition Therapy Wellbeing Assessment Preparation Form to be completed by the resident prior to the appointment with the RDN.
• Resident reports to the RDN for their scheduled visit.
• RDN provides individualized medical nutrition therapy as indicated using the nutrition care process and records the results of the visit in the electronic health record system.
• RDN refers the resident to adjunct services, as needed.
• RDN arranges follow up and monitoring with the Wellness Suite and resident, quarterly or as needed.
• Mini Nutritional Assessment (MNA) is completed by the Wellness staff as part of the Health History and Information Update.
• The MNA score is recorded in the electronic medical record.
• Residents that score at normal nutritional status (12-14 points) on the MNA do not need to be referred to the RDN for follow up and assessment, however, the resident is entitled to meet with the RDN to address any nutrition questions or concerns.
• If the Resident wishes to meet with the RDN, Wellness staff contacts RDN to schedule an appointment and provides the Medical Nutrition Therapy Wellbeing Assessment Preparation Form to be completed by the resident prior to the appointment with the RDN.
• Resident reports to the RDN for their scheduled visit.
• RDN provides individualized nutrition counseling, based on resident interest or need. The RDN and Resident set priorities, establish goals, and create individualized action plans which acknowledge and foster responsibility for self care.
• RDN assists the resident in accessing community and local resources, as needed.
• RDN records the results of the visit in the electronic health record system.
The Registered Dietitian Nutritionist is located on campus in the Wellness Suites.
•
Please complete this form and bring it with you to your meeting with the registered dietitian nutritionist.
1. I would like to visit with the dietitian today because….
2. My food and nutrition related goals are…
3. My overall health goals are…
4. The biggest challenge(s) to reaching my goals is(are):
5. In the past, I have tried the following techniques, diets, behaviors, etc. to reach my goals…
6. I would like to take away from this visit: or I would like to leave this visit today with:
On a scale of 1 (not willing) to 5 (very willing), please indicate your readiness/willingness to do the following:
To improve your health, how ready/willing are you to… 1 2 3 4 5 Modify your diet
Take nutritional supplements each day (if appropriate) Keep a record of everything you eat each day Modify your lifestyle (example sleep, exercise, etc.)
Practice relaxation techniques
Engage in regular exercise/physical activity Have periodic lab tests to assess your progress
1. Usual weight
2. Weight changes in the past year? 1 month, 6 months, 12 months
3. Concerns with weight changes?
4. Highest Adult Weight When?
1. Are there any foods that you avoid? Reason?
2. Has your food intake changed in the past month? Unchanged/more/less
3. Do you have any digestive issues related to food?
4. Have you had any of the following problems during the past month?
Mouth sores
Dry mouth
Difficulty chewing
Difficulty swallowing
1. Do you prepare your own food?
2. How many meals per week do you eat in your home?
3. How many meals do you eat per week in the café/dining room?
4. How many meals per week do you eat at or take out from a restaurant?
5. Which restaurants do you eat at regularly?
Please keep a diary of the food and beverages that you consume for 3 days. Choose any days that you wish. If you have a different eating pattern on any given days, such as the weekend, record one of these days. Include the amount you ate (serving size) and any preparation information, for example grilled, fried, breaded. If you drink alcoholic beverages, include type and serving size.
A food as medicine approach will be adopted in the overall wellness care provided by the registered dietitian (RD) and culinary services. Food as medicine is a philosophy where food and nutrition aids individuals through interventions that support health and wellness. This approach incorporates a variety of programs and experiential opportunities to support/improve healthful eating at home and in the dining venues.
Food as medicine intervention categories are broken down into five focus areas. These categories, alone and in combination, assist the resident in the self management and prevention of many chronic conditions.
Prescription Program the RD and resident develop an individualized nutrition prescription to meet food consumption benchmarks.
Incentive Program price discounts or other incentives will be offered in the dining venues to encourage choice of foods and meal combinations that are nutrient dense (vs. indulgent) and align with guidelines for a healthy diet.
Medically Tailored Nutrition in conjunction with medical nutrition therapy, the resident may opt to have meals planned for them and delivered daily.
Path to Purchase Marketing residents will be influenced in the dining and living environment through the use of signage and displays, choice architecture, nutrition information, food sampling, cooking demonstrations, and menu promotion to nudge them towards better food choices.
Personalized Nutrition Education in addition to the annual visit, the resident will have ample opportunities through group classes, one-on-one education, and nutrition resources to explore, learn, and find actionable ways to consume a healthful diet.
The following are examples of opportunities within the five focus areas that support the resident in meeting their nutrition wellness goals:
In house Resident Channel or Touchtown “Nutrition Nuggets” video played at targeted times (released quarterly) and general reminders on working on wellness portfolio; video also available on the resident portal. Can also play on TV in Wellness Suite.
Virtual Wellness Group private group on the resident portal moderated by the community RD Newsletter article quarterly
Resident Portal Menu Highlight the “dietitian’s choice” meal of the day in addition nutrition information; can also be available for the week in print and priced to promote selection
Featured plate Display plate of dietitian’s choice entrée and sides positioned near the entrance of the dining room, priced to promote selection
Wellness Chats coordinated with wellness team
Cooking Demo (with Chef) Easy recipes for residents who still like to cook or minimal preparation for those who don’t want to or highlights the dietitian’s choice on the menu or a new item on the menu
Shopping List Creation Session Spotlight on nutrient dense items to create a shopping list for the resident’s next grocery trip
Snack Carts/Produce Stands Featuring nutrient dense snacks and fruits and/or vegetables available to sample and purchase.
Coffee Talk/Happy Hour Small group, casual discussion on focused topic that includes coffee/tea or mocktails and nutrient dense snacks that tie back to the discussion
Tech Cafes (with IT) Encouragement and training to get residents comfortable with the resident portal to access nutrition information or other resources in groups available at the community
Farmer’s Market Outing (with LEC) During season, to promote purchase of nutrient dense items for meals at home
Group Coaching 4 week sessions to help residents stay on track or explore other goals coordinated by RD or wellness coach
MyPlate.gov Workshop Assist residents in accessing MyPlate resources to develop their own eating plans, recipes, and tools for shopping
Check In Sessions scheduled periodically, can be group or individual sessions with RD or wellness coach
Create a standard menu framework with minimum numbers of indulgent and standard entrees and sides, fruit based desserts, and guidelines for increasing bean and grain options.
Create a robust database of Acts recipes that are lower in sodium and plant based. Incentives in the café and restaurants, e.g. choose fruit over fries as a side and get your beverage for free.
Arrange cafes to make healthier items visible and easy to access (e.g. chips not at eye level or by register).
Tag recipes in Mealsuite with red, yellow, green light system. DCNS/Chef/RD work together to balance menu with dishes that are indulgent, moderate, or better for you. (not sure if possible)
Allow residents to choose if they want nutrition goal reminders attached to their account (e.g. make sure to offer catch of the day and fruit dessert). (Not sure if possible)
•
Several states licensure statutes describe that a physician or a health care provider authorized to prescribe dietary treatments initiate a referral for nutrition services. It will be noted, therefore, that the referral of a qualified health care provider, such as a physician, is apparently an essential antecedent to the RDN's ability to practice dietetics or nutritional services of any kind. The statutes of some other states also contain references to a physician's participation or supervision in the nutrition care process, but they are not nearly as restrictive as Alabama and California.
• Alabama
"[A] dietitian/nutritionist or registered dietitian … may [provide such dietetic services as nutritional assessments and nutrition counseling] upon referral by a health care provider authorized to prescribe dietary treatments", and "[d]ietitians/nutritionists may offer advice and counsel on dietetics and nutrition as adjunct medical therapy when advice and counsel is given upon referral of a licensed physician." Ala. Code 1975 §§ 34 34 2 and 34 34A 5 (emphasis added). ["Adjunct medical therapy" is not otherwise defined.]
• Certain states, while not requiring referrals in all cases, have included statutory provisions designed to address conduct when physicians are already involved.
• Florida
"[A] licensee under this part shall not implement a dietary plan for a condition for which the patient is under the active care of a [licensed] physician … without the oral or written dietary order of the referring physician," except that "[i]n the event the licensee is unable to obtain authorization or consultation after a good faith effort to obtain it from the physician, the licensee may use professional discretion in providing nutrition services until authorization or consultation is obtained from the physician." West's F.S.A, § 468.516(1)(a).
• Some states mandate the involvement of a physician when the treatment or the condition being treated becomes what the state defines as medical in nature.
• South Carolina
"Nutrition care services" will include, among a number of other things, "implementing a physician's written and verbal orders which pertain to the practice of dietetics, if the practice of dietetics is specifically authorized by the medical director and the health care facility where the care is taking place. In the delivery of dietetic home care, this care must be authorized specifically by the physician sponsor…." Code of Laws of South Carolina Anno., Sec. 40 20 20.

Through the Annual Health and Wellness Evaluation (AHWE), the community’s Nurse Practitioner will complete assessments that will determine the potential need for mental health intervention or services. The Acts Mental Health Clinicians (MHC) serve as key members of the interdisciplinary care team and provide behavioral health, assessments, care planning, therapy services, behavioral intervention, and case management to the ILU population.
The MHCs are clinical licensed Social Workers or Psychologists that conduct diagnostic interviews to identify psychosocial strengths and weaknesses and inform care planning. They also provide individual, family and group psychotherapy services, as indicated through assessment and care planning processes; they offer caregiver support and education to family members and provides educational programs to the Acts community staff.

Acts Lifestyle Empowerment program provides structured guidance for residents experiencing mild cognitive impairment and their spouses. Through participation in a comprehensive, individualized lifestyle program, members experience empowerment, purpose, wellbeing, and joy while maintaining independence to live their best life, as well as they can, as long as they can. A Memory Support Navigator will guide member engagement in the program that addresses the following lifestyle factors:
• Cognitive Engagement
• Social Engagement
• Physical activity and exercise
• Nutrition
• Stress management
• Sleep
• Environmental sensitivity
• Memory Support Navigator: Licensed clinical social worker (LCSW) credential with additional wellness/personal coaching certification and case management certification. One LCSW for every 50 residents.
• Expressive Therapist: Master’s Degree in Expressive Arts Therapies
• Administrative assistant
• Beautician (CDP credentialed)
• Massage Therapist (CDP credentialed)
• Day Care Staff (CDP credentialed) (Program members could be volunteer staff)
• Playground equipment for child Daycare
• Devices that play recorded reminders (e.g., time to take medication, attend program, etc.)
• Talking clocks
• Pill dispensers
• Location tracking devices (shoe inserts, wrist bands, numerous options)
• Virtual assistants (Alexa, Siri)
• Simple remote control
• Simple music player
• Digital photo frame
• Fur real pets (later stage)
• Dementia-friendly cellphones
• Dementia-friendly watches
• Dementia-friendly scale
• Dementia-friendly food scale
• Dodow sleep aid
• Ambient sound machine
• Virtual reality
• Weighted blanket
• Bright light therapy
• Ring Doorbell
• Personal Golf Cart
• Adult tandem 3 wheeled bicycle
• Apps:
o Brain stimulating apps: My Reef 3D Aquarium, Lumosity, Greymatters: Reaching Beyond Dementia, AmuseIT, Constant therapy, SingFit, Let’s Create Pottery, MindMate, Flower Garden
o Apps promoting independence/organization: It’s Done, Iridis, Nymbl
o Care partner support apps: Teepa Snow GEMs, A Walk Through Dementia, Alzheimer’s Daily Companion.
Part 1a: Support to new IL residents without MCI
Within 30 days of move in, the Memory Support Navigator welcomes new independent living residents and presents a general overview of services available to promote brain health and address modifiable risk factors.
Part 1b: Support to new IL residents with MCI
Prior to move in, the Memory Support Navigator meets with the resident and their care partner/spouse and presents an in depth overview of Lifestyle Empowerment programming and services available that will support their transition plan and assimilation into the community.
Part 1c: Support to existing IL residents that develop MCI
The Memory Support Navigator engages residents identified as living with mild cognitive impairment either through team referral or self-referral. The Navigator meets with the new member and their spouse (if applicable), either individually or with the spouse/care partner in their home:
• The Navigator initiates membership in the program with a detailed review of program offerings and assessment of needs to design a custom, person centered plan of support with action steps to extend the duration of independent living and overall quality of life.
o The Navigator and member/spouse decide frequency of contact.
o Action steps may include connecting with other disciplines e.g., nurse practitioner, rehab (Thrive assessment if needed), implementing a home safety evaluation, identification of IL program buddy/mentor, etc.
Lifestyle Empowerment Program Member Portal (similar to “My Chart”): Resource Center that provides online platform with educational resources, weekly chat opportunities, schedule appointments/request a visit, interface with other members, program reminders, etc.
• Members and their care partners will work with their Navigator to engage in the multi disciplinary curriculum. Goal setting is implemented upon initial assessment and monitored continuously to address changing abilities, track progress and review and adjust frequency of touchpoints as needed.
• As part of their participation in the Lifestyle Empowerment Program, members and their care partners will be afforded the opportunity to participate in research opportunities aimed at improving the lives of individuals living with MCI.
The Memory Support Navigator will have the ability to build respectful and trusting relationships with IL residents through an ongoing and notable presence in IL community life by offering engagement programs and educational opportunities that include:
• Quarterly resource and information seminars
• Workshops on care partnering
• Support groups for individuals living with memory loss or care partners
• Memory Café
• Safety assessment (in partnership with rehab)
• Information on advanced directives
• Connections Program (respite care)
• Home Health support
• Legal planning
• Financial counseling
• Support of dementia-friendly community initiatives
• Lending Library
Engagement programs will be evidence based and reflect current research regarding beneficial practices for people living with MCI. Programming will be offered in person and virtually and will involve interdisciplinary team members with expertise in the following areas:
Fitness
Walking club
Trips in the community at large, e.g., Boardwalk, area parks
Yoga
Tai Chi
Self Defense classes
Bike Riders Club
Stress Management
Caregiver support group
Grief/Loss support group
Connections (respite opportunity)
Self-care – resources to support and encourage self care (Emotional Wellbeing Resource Center on Member portal will have printable handouts on Understanding Stress, Strategies to Manage Stress, Mindfulness, Deep Breathing, Progressive Muscle Relaxation, Stretching).
Spiritual support
Daily Devotional for community
Prayer groups – centering prayer
Cognitive/Behavioral Therapy to address issues contributing to stress
Community gardens
Pet therapy
Nutritional education
MIND Diet – Culinary options offered in dining room and Bistro
Weight checks
Nutritional counseling
Healthy snacks
Meal reminders
Kitchen – safety assessment
Cooking classes
• Community cookbook featuring healthy recipes
Food Demos
Meal planning class
Coupon swap for groceries
Sleep
• Sleep specialist – presentation to community
Resources for improving sleep (portal)
Nutritional recommendations to improve sleep (limit caffeine, sugar, and alcohol in afternoon)
Cognitive/Behavioral Therapy to address emotional issues affecting sleep
Sleep environment – guidance on how to create an environment that supports sleep
Rehab functional independence
Creative arts engagement
Visual art classes
Movement/dance
Dramatic arts performances
Guided Affective Imagery
Music therapy
Museum visits
Cognitive engagement
Total Brain Health
Linked Senior (on IL resident’s iPad)
Language classes (including sign language)
Music classes
Life Long Learning Series
Great Courses Series
New hobby club
University/Community Colleges offerings – courses at local universities
Game competitions (similar to OlympiActs)
Community trips to concerts, orchestra, opera, theatrical productions, museums (with class offered prior to the event to prepare residents to enjoy the experience)
Visiting artists
Education on how to live well with MCI
Social engagement
Volunteer opportunities (Acts community {Gift Shop} and larger community)
Intergenerational programming (Members have a “Job” at in house child day care)
Happy Hour
Prom
Memory Café
Travel Club – plan group trips
New resident welcome group
Buddy system (seasoned care partner paired with a new care partner)
Support groups
Technology classes
Services (specific to this program)
Music therapy






with
with
and History
Visit with the Wellness
all
from the
and provide them to the
prior to the
with
prior to the
by
will finalize the
and
(ADLs)
prior to the
scheduled visit. The
Support Services,
with
include
(IADLs)
Education, Preventive
Advise and Referral Plan and (ongoing)
to
Journey to date.
a
and
Sub task force mtg held on Thursday, Oct., 20th to discuss and request creation of protocols for each discipline


The “Acts Life Care” Product Has Been Redefined as “Acts Well-Being”. The history of the Acts Life Care product offering has been anchored in the concept that seniors want to manage the future uncertainty of needing long term care and other support services. The Acts Life Care product has met that need in providing a complete continuum of care that is affordable and accessible, offered in desirable facilities and provided by an organization that embraces Christian values, all together providing “peace of mind” and security.
As we look to the post-pandemic future, the product offering needs to change its emphasis to a model of enhanced wellness (often viewed as “come here to live”) from a continuum of care model (often viewed as “come here to die”). The new “Acts Well-Being” product will focus on extending an active, vibrant, full lifestyle for all those choosing to live with us by engaging them in a variety of physical, mental, and spiritual activities that have been personally scripted by analyzing their preferences and monitoring their existing and/or changing medical condition, data, and issues.
From the moment prospects sign a Resident Contract, we will assist them in designing their well-being lifestyle experience and frequently review and adjust this personalized well-being portfolio as they age and their abilities change throughout their life at Acts.
An “experience portfolio plan” is created with (not for the resident) the resident, while data analytics inform the community staff on adjustments to meet each resident’s needs and desires. The “continuum of care” as a term is dropped, and now is viewed as continuing “supportive services” which include home health, telemedicine, therapy, counseling, and much more.
The success of the Acts “Well Being” program will be ultimately measured and promoted in statistics that demonstrate a reduced utilization of assisted living/memory care/skilled care and extended life expectancy compared to alternative senior living/care options. This is an evolution of the Life Care model to one that is more flexible and pro-active – and more inclusive of other services to potentially delay or even remove the need to move into a higher-level care setting. Ultimately this adds control and flexibility for our residents to the foundation of providing peace of mind and security.
The Acts Well Being Lifestyle Fully Challenges Our Greatest Competitive Threat: “Aging in Place” The pandemic experience has left many seniors feeling like the safest and happiest place to age is in their own homes. As service delivery became more readily available and customary during the pandemic, aging adults became more comfortable with managing the delivery of needed services (food, groceries, pharmacy supplies, telemedicine, home repair, etc.). Prior to the pandemic, the many channels of social interaction available via the explosion in restaurants, theater, fitness, outdoor/nature along with accessibility of in home entertainment via streaming--made walkable towns, on-demand transportation and social interaction even more easily accessed and desirable. Along with this change in lifestyle came an increasing fear that congregate living was now dangerous (from an infection perspective). Post-pandemic, it is expected that businesses specializing in enabling seniors to age-in-place (at home) will become even more prominent, and seniors could themselves now find virtual ways to stay connected and social. Fortunately, the attractiveness of a CCRC environment, offering senior-tailored amenities and services and the opportunity to extend one’s quality of life and life expectancy, will remain. To compete with the “aging in-place” product offering, we will need to demonstrate to seniors, and to their adult children who may be the decision makers to their parents that aging-in place outside a CCRC falls short in meeting the social and overall well-being needs of seniors who are living in isolation left to manage
their own supportive services and that the offering is limited in providing all the necessary healthcare needs in a home environment.
Design the “Well-Being” product to replace “Life Care,” centered on customized lifestyle experience planning with each resident, with a simple and flexible contract with pricing options for al a cart services.
Develop new service packages for onsite dining and concierge services (travel, transportation, housekeeping, shopping, entertainment, education, etc.) customizable for each resident.
Repackage the continuum of care, adjusting to an umbrella of support services and guidance for thriving-in place through the Wellness Clinic (e.g. utilization of the nurse practitioner).
Develop programs designed to reduce utilization of OBT and WBC stays (fitness, nutrition, home health, therapy, counseling, etc.), applying resources from OBT/WBC to clinic staffing and services.
Design a nurse navigator program to provide clinical coordination for residents needing medical care, with medical and home health assistants providing routine healthcare and follow up services to IL residents.
Evaluate what should be added to on-campus services that enhance the comprehensive solution we offer to seniors such as dental, vision, hearing, pharmacy, supplies, telemedicine, counseling, therapy, and technology.
Develop or obtain technology designed to capture data and monitor resident activities and utilization of resources daily and in alerting areas of concerns.
The community resources are redefined/reallocated to provide professional services to meet the demands of the “Well-Being” product (model operational budget).
Implement the “Well-Being” product as a pilot, with assessment and adjustments identified to ensure success and growth/expansion.
Build Acts Well-Being Lifestyle Pathways for multiple applied research opportunities to gain recognition in Acts being a Center/s of Excellence for various individual needs: Example: Brain-Health: Dementia prevention/maintaining and building one’s Cognition reserves; others?
Reports To: Corporate Director of PCS, dotted line to ED Department: Special project fund dept.
Summary Statement: The Well Being Coach serves as the key leader of the interdisciplinary well being team, oversees the well being comprehensive assessment and coordinates the resident’s well being portfolio plan. Provides the oversight and coordination of well being interdisciplinary assessments, facilitates the interdisciplinary well being portfolio (care and services) planning; and may provide individualized mental health services and behavioral interventions to the independent living population, as needed per the well-being assessment.
Describe the specific Duties and Responsibilities of the position from most critical to least.
1. Provides leadership for the interdisciplinary person centered well being services, including observation and analysis, referrals, aiding in the creation of well being portfolio with individualized support plans, and provides caregiver education regarding recommended interventions and provides touchpoints to progress
Conducts diagnostic interviews to identify psychosocial strengths and weaknesses and incorporates these into the resident’s well being portfolio plan
Provides individual, family, and group psychotherapy services, as indicated through the well being assessment and portfolio plan
Participates in interdisciplinary team well being meetings and resident’s well being portfolio planning, serving as the wellbeing coach that can also provide behavioral health to ensure that psychosocial aspects of IL residents are identified and addressed
Offers caregiver support and education to spouse/family members as determined necessary
Offers quarterly educational programs as a support to residents and a means of highlighting services and benefits of the Well Being Services and the Wellness Suite
Offers a monthly well being caregiver support group for caregivers within the community
Responsible for timely and accurate documentation of all medically necessary visits; providing mental health services in compliance with applicable federal and state regulations and policies for any billable services with third party payors
Responsible for remaining abreast of emerging research, best practices and therapeutic approaches related to meeting the psychosocial needs of individuals living with mental health needs, cognitive disorders, and for their caregivers’ needs
Actively participates in re evaluating the well being services to ensure quality of well being outcomes and create continuous service evolution
Participates in and supports quality improvement activities, community outreach, marketing, and other operational processes to benefit the Well Being services being provided and adding new services as identified
Works closely with and supervises the Well Being Concierge
Education & Experience: The critical skills and knowledge required to successfully perform the functions of the position are normally obtained thru:
• Education Level: Masters or doctoral degree in social work with experience with older adults. A Board certification in Geriatrics and expertise in serving people living with dementia is preferred, but not necessary.
• Required Credentials: Maintains a state license as a mental health services provider, i.e., Licensed Clinical Social Worker. Eligible for National Provider Identification number AND credentialing as a behavioral health clinician by Medicare and other third party payors.
• Years of Relevant Work Experience: At least 3 years of experience as a licensed behavioral health clinician providing assessment and psychotherapy treatment services.
•
Expertise in assessment, therapy, behavioral intervention and case management for older adults.
• Expertise in supporting people living with dementia.
• Comprehensive knowledge of state and federal related to provision, documentation and billing for behavioral health services.
• Excellent interdisciplinary collaboration skills.
• Effective in providing education and public presentations.
• Effective group facilitation skills.
• Must have good analytical, educational, and communication skills
• Frequent sitting
Occasional standing and walking
• Occasional operation of hand controls
• Occasional reaching from below knees to above shoulder level
• Lifting, pushing and pulling 50 pounds occasionally
• General visual skills
• Frequent fine finger dexterity
• Ability to make presentations to large and small audiences
• Inside 95%
• Hazards infectious diseases
• Must be proficient in Microsoft Office
• Must be able to meet deadlines as required
• Excellent written, verbal and grammatical skills within the English language
• Exceptional customer service, quick evaluation and decision making
• Work efficiently with minimal supervision
• Must be able to manage multiple projects and should be organized
• Can operate all office equipment (including telephone, computer, copier)
Frequent talking and hearing
Frequent near acuity
Sitting, standing and walking occasionally.
Bending, squatting and kneeling occasionally.
Climbing stairs occasionally
• Able to use hand to perform frequent grasping, writing and typing.
• Talking and hearing in person and on phone
I understand that I am responsible for performing the duties and responsibilities of my position in a manner that is consistent with the Acts Culture of Loving Kindness.
I will observe safety guidelines and perform essential tasks in line with the company's safety policy and procedures.
By my signature, I acknowledge that I have received a copy of the Job Description and have read and understand its contents.
Employee Name (Please Print)
Employee Signature Date
Employer’s Signature
Company provides equal employment opportunities to all qualified individuals without regard to race, creed, color, religion, national origin, age, sex, marital status, sexual orientation, or non‐disqualifying physical or mental handicap or disability in each aspect of the human resources function. Applicants as well as employees who are or become disabled must be able to perform the essential job functions with or without reasonable accommodation. The Company shall determine reasonable accommodation on a case‐by‐ case basis in accordance with applicable law.
The following statements reflect the general duties and responsibilities considered necessary to perform the essential functions of the job and should not be considered as a detailed description of all the work requirements of the position. Company may change the specific job duties with or without prior notice based on the needs of the organization.
Code:
Reports To: Well Being Health Coach Departme nt: 2200 resident services
The Well Being Concierge develops highly engaged resident relationships to facilitate an individualized approach to residents’ health and wellbeing by coordinating access and awareness to services and events inside and outside the campus that supports sustainable well being and behavior changes. This position will work closely with the Well Being Health Coach, Life Engagement, fitness, spiritual, culinary, and clinical staff to inspire residents to enhance their lifestyles by developing healthy habits and reaching health and well being goals. The Concierge is motivated and passionate about working with residents to live healthier, happier, more fulfilled lives. This position also embraces the hospitality culture of Acts by acknowledging all residents, staff, and guests according to company standards.
Describe the specific Duties and Responsibilities of the position from most critical to least.
Job Functions Time
1. Uses effective communication, engaging techniques, and positive encouragement to engage residents and interact with clinical and non clinical staff regarding programming to enhance health and wellbeing.
2. Provides informal coaching elements to provide residents with the opportunity to experience a personalized approach to wellbeing
3. Uses motivational techniques to assess needs based on physical, emotional, intellectual, social, and spiritual wellbeing
4. Works with residents to determine areas of interest, setting goals, identify obstacles, implement effective solutions, and create a comprehensive well being plan to achieve their individual health and wellbeing goals
5. Applies appropriate motivational techniques to encourage residents to adopt sustainable behavior changes
6. Coordinates with clinical and non clinical staff and the resident to determine the best services or events that are available to provide a personalized, well rounded experience to achieve health and wellbeing goals.
7. Promoting resources available in the community and in the outside general community to meet the health and wellbeing needs of the residents
8. Communicates any noticeable or reported changes in the status of residents to the Well Being Coach and other interdisciplinary team members
9. Proficiency in Microsoft Word, Calendar, and Outlook and the ability to use technology to communicate and encourage resident participation in events that lead to behavior change
10. Facilitates access to events and services and communicates with residents in person, virtually or through email to these events and services
11. Creates and distributes informational flyers, email alerts, and other electronic means of communication to promote programs and information related to wellbeing
12. Develops and conducts presentations for residents, guests, family members and employees who are interested in learning more about health and wellbeing events.
13. Other duties as needed.
Education & Experience: The critical skills and knowledge required to successfully perform the functions of the position are normally obtained thru:
Education Level:
Associate or bachelor's degree in psychology, counseling, or health sciences preferred
Health Coach Certification (American Council on Exercise)
Two years' experience in the hospitality industry as a concierge or experience as a health coach, previous experience working with seniors or working in a retirement community is very desirable.
(The following bullet points are samples to use if they apply)
Efficient organization skills
Effective interpersonal & communication skills
Must be able to work well in a team-oriented environment
Exceptional customer service orientation
Adept evaluation and decision making skills
Excellent written, verbal and grammatical skills within the English language
Computer software knowledge (MS Word, Excel, Outlook, AOD, Millennium)
Must be able to meet deadlines as required
Work effectively with minimal supervision
Proficient with office equipment (telephone, computer, copier)
Physical Demands (adjust as appropriate)
Continuous Frequently Occasionall N/A -
Sitting
Walking
Standing
Working at
Crawling
Repetitive hand / finger
Talking on the phone
Push/Pull (up to 25 lbs.)
Pulling (up to 25 lbs.)
Lifting (up to 20 lbs.)
Pulling (up to 25 lbs.)
Lifting (up to 20 lbs.)
Environmental Conditions (adjust as appropriate)
% Exposure to: Continuous Frequency Occasionally N/A
I understand that I am responsible for performing the duties and responsibilities of my position in a manner that is consistent with the Acts Culture of Loving Kindness.
I will observe safety guidelines and perform essential tasks in line with the company's safety policy and procedures.
By my signature, I acknowledge that I have received a copy of the Job Description and have read and understand its contents.
Employee Name (Please Print)
Employee Signature
Employer’s
Company provides equal employment opportunities to all qualified individuals without regard to race, creed, color, religion, national origin, age, sex, marital status, sexual orientation, or non‐disqualifying physical or mental handicap or disability in each aspect of the human resources function. Applicants as well as employees who are or become disabled must be able to perform the essential job functions with or without reasonable accommodation. The Company shall determine reasonable accommodation on a case‐by‐ case basis in accordance with applicable law.
The following statements reflect the general duties and responsibilities considered necessary to perform the essential functions of the job and should not be considered as a detailed description of all the work requirements of the position. Company may change the specific job duties with or without prior notice based on the needs of the organization.
Dear Resident, We are excited to announce an opportunity for you to participate in the Acts Well-being pilot at St. Andrews Estates! The Acts Well being pilot provides each participant an opportunity to create a personalized well being plan. Our well being coach and concierge collaborates with each resident to create an individual plan designed to promote health and enhanced wellness. The new Acts Well being pilot focuses on extending an active, vibrant, full lifestyle by engaging residents in a variety of physical, mental, and spiritual activities that have been personally scripted based on individual preferences and monitoring existing and/or changing medical conditions.
The plan may include personalized education, preventive counseling, supportive services, health advice and referral plans, as well as fitness, spiritual, nutrition and life engaging goals. Access to specialized health and wellness screenings, comprehensive nurse practitioner physicals, specialty medicine, and health sensor devices such as an Apple watch are just some of the opportunities available to residents in the pilot.
As we develop our new well being program, we are looking for thirty residents to participate in the pilot project. Enrolled residents will partner with Acts to create a well being product designed to transform life care by focusing on prevention and creating proactive plans to enhance health and wellness. If you are interested in joining our pilot, please sign up at the front desk. If we have more than thirty resident volunteers, we will randomly select the initial participants.
Please feel free to contact Joya Marotta at (561) 210 0188 or Susan George at (561) 210 0293 for additional information.
Sincerely,
(ALPHA Pilot group of initially 30 IL residents at St. Andrew Estates) (Up to a 60/90-day pilot period, starting on 11/01/2022
Dear (resident name):
Thank you for your willingness to participate in this Acts Well being pilot at St. Andrews Estates! Please read the following outline of the Well Being Program and what to expect during this pilot.
{Insert the well Being Philosophy Statement here}
Acts Well-being Program provides personalized preventative wellness and health promotion well-being services for an individuals’ body, mind, and spirit by offering direct access to customized diagnostic and consultative well being and health services to build your customized well-being portfolio pan with routine touchpoints by the Acts Well-Being Coach and Concierge being completed throughout the year to assist you in meeting your personalized well being goals.
1. You will need to use a wearable well being tracking device during this pilot period: i.e. Apple Watch, Fit Bit, Samsung Watch, etc. and if so, you will be asked for your consent in to sharing this iwellness-fitness informational data with the Acts Wellness Coach, Nurse Practitioner, and other key well being team members at St. Andrews Estates in order to monitor your progress and in utilizing your data in creating your personalized Well Being portfolio plan and established goals. Note: If currently do not own a tracker device- a “loaner” device will be provided to you “free” during this initial pilot. Your health and wellness data will only be shared as needed and only with the interdisciplinary team members in the formation of your personalized portfolio plan with you.
2. You are asked to keep a food and health journal for the time leading up to your initial well-being assessment. It is recommended that this journal will be utilized throughout the pilot period. This journal will be included in your Acts Well Being welcome packet.
Providing customized health promoting experiences and services on maintaining health and mitigating the impact of existing medical conditions. The health and medical program of the
Well Bing offers direct care access to customized diagnostic and consultative health services, including a comprehensive assessment by the Acts nurse practitioner, laboratory and radiologic testing, sophisticated screening procedures and update evaluations for Rehab, nutrition and fitness.
A Global Well Being Assessment will be Completed Prior to Your Initial Customized Well Being Health and Medical Assessment:
The Acts Well Being Coach, a licensed clinical social worker, will conduct a scheduled pre visit in home consultation and review your current medical and life story records that are currently available at St. Andrews Estates. The Well-Being Coach will consider your entire well-being picture, taking into account your social and medical history; age and genetic predispositions; psychosocial needs; and identify any risk factors. The in home consultation will provide a forum for you to discuss any concerns about your health and well being and allow your Coach to consider any additional interdisciplinary screenings or referrals that may be indicated. Your Coach will schedule a THRIVE assessment with a trained, licensed therapist prior to your Well Being Assessment appointment with your Acts Nurse Practitioner.
If indicated and decided upon your pre visit consultation with the Acts Well Being Coach, other in-house Acts well-being consultations can be arranged by the Well-Being Concierge in implementing your unique and personalized Well being portfolio plan:
• Spiritual consultation with the Chaplain at St. Andrews Estates
• Mental health services and counseling provided by a Licensed Clinical Social Worker, Well Being Coach
• Chronic Care Management by the Nurse Navigator at St. Andrews Estates
• Detailed cognitive assessments and testing by the Acts Nurse Practitioners and/or a Licensed Speech Therapist at St. Andrews Estates
• More detailed standardized assessments and testing by the Acts in house rehabilitation team at St. Andrews Estates including a personalized THRIVE exercise prescription that will be shared with the Fitness Coach at your community
• More in depth fitness evaluation, training, and in implementing the personalized created exercise plan by your Fitness Coach
• Life Engagement Director at your community to review additional activities, clubs, volunteerism opportunities, and events based on your interests
• More nutritional consultations provided by the Acts Registered Dietician to meet your dietary goals, weight management plans, etc.
• Referral to Acts Home Services/Care Management and Acts Medicare Home Health Agency
• A Well Being Concierge is readily available to assist in accessing these services at St. Andrews Estates and services in the general outside community
You will arrive at the Wellness Suite on the _________ side of the campus. You will be welcomed by the Wellness Office staff who will escort you to a comfortable, private exam suite. Depending
on your appointment time and if you are fasting for the initial blood work panel a lite healthy breakfast or snacks will be provided after your fasting blood work is obtained.
Your initial visit with the Acts nurse practitioner will include a complete medical history, family history, risk assessments, and a thorough physical examination. A review of any necessary immunizations and vaccines will also be provided. An Acts THRIVE initial assessment will be completed prior to this visit by a trained, licensed therapist, your fitness assessment will be managed by a trained, certified fitness instructor and in taking a full body composition analysis screen, while the initial nutrition assessment will be conducted by a licensed dietician, aimed at optimizing your diet for good health and to reduce the risk of illness.
• Vital signs, heigh and weight, pulse oximetry (oxygen saturation level)
• Complete blood count to evaluate for anemia and other hematologic disorders
• Complete metabolic panel to assess for diabetes, kidney disorders and other metabolic problems- A1C is included. If clinically indicated, a continuous blood glucose monitoring for two weeks will be ordered by the nurse practitioner.
• Cardiac risk profile, including lipid panel and advanced studies, to assess for cardiovascular and cerebrovascular risk
• Urinalysis to screen for urologic and kidney disorders. Use of a bladder scan may also be indicated
• Thyroid testing for over or underactive thyroid disorder
• Prostate specific antigen (PSA) to screen for prostate cancer, if necessary, as decided between you and the nurse practitioner
• Electrocardiogram (EKG) to screen for cardiac disease, including coronary and electrophysiologic problems
• Audiometric testing to detect hearing problems
• Spirometry testing to detect lung or pulmonary problems
• Vision testing and evaluation for ocular health
• Chest Xray can be scheduled for a date and time after your initial health assessment, if indicated by the nurse practitioner for suspected cardiac or pulmonary issues
• If indicated, a referral for a GYN exam will be initiated and/or an order for receiving a mammogram will be provided by the NP
If indicated and decided upon your consultation with the Acts Well Being Coach and based on the full comprehensive assessment completed by the Acts Nurse Practitioner, other outside healthcare consultations may be arranged by the Well Being Concierge in implementing your unique and personalized Well being portfolio plan: This include but not limited to-
• Podiatrist/Audiologist/Ophthalmologist/Dentist
• Other specialized medical consultants, i.e. dermatologist, Gastroenteric physician
• Reflexology/Massage/Chiropractic/ and other complementary alternative treatments
• Dexascan to screen osteoporosis for those individuals identified being at risk
• Psychologist/Psychiatric services
• Professional counseling services- grief, depression, alcohol use, etc.
• Comprehensive Cognitive Screening and Assessment at Florida Atlantic University (FAU)
At the end of your comprehensive Well Being Assessment:
• You will receive a person directed goal setting and coaching session.
• You will also receive a personalized report including exam findings, internal lab test results and other external lab results will be shared upon their receipt, and nutrition, Rehab and fitness advice, and additional nurse practitioner clinical findings and recommendations.
• If follow up care with outside healthcare professionals and advance diagnostic testing is recommended or requested, our Acts Well Being team can assist in making those appointments.
• You will also receive a personalized Well Being Support Plan that will assist you in implementing your own well being plans and goals to reach your optimum you!
The Acts Well Being Coach and Well Being Concierge will both be reaching out to you throughout the year to assist you in your progress and in making any adjustments to your plan and your goals and in accessing any other well being services.
We thank you again for your active ongoing participation in the Acts Well Being Pilot at St. Andrews Estates!!
For more information and in scheduling your Comprehensive Well Being Assessment, please contact the Acts Well-Being coach, by calling # ( ), or by email at _________@actslife.org


https://actsretirementlife.sharepoint.com/:b:/r/sites/NewWell20/Shared%20Documents/Annual%2 0Visit/Prevounce AWV Checklist.pdf?csf=1&web=1&e=NLJCcs
https://actsretirementlife.sharepoint.com/:b:/r/sites/NewWell20/Shared%20Documents/Annual%2 0Visit/Prevounce AWV Checklist.pdf?csf=1&web=1&e=NLJCcs
https://actsretirementlife.sharepoint.com/:b:/r/sites/NewWell20/Shared%20Documents/Annual%2 0Visit/Prevounce AWV Checklist.pdf?csf=1&web=1&e=NLJCcs
https://actsretirementlife.sharepoint.com/:b:/r/sites/NewWell20/Shared%20Documents/Technolog y%20Solutions/Health-Report July 2022.pdf?csf=1&web=1&e=McD0w9
https://actsretirementlife.sharepoint.com/:b:/r/sites/NewWell20/Shared%20Documents/Technolog y%20Solutions/Health-Report July 2022.pdf?csf=1&web=1&e=McD0w9
https://www.greatagereboot.com/
https://www.fiercebiotech.com/medtech/rockley photonics unveils clinic wrist system-offering-aglimpse-at-apple-watch-s-future
►PDHI Built to support various program designs for occupational and population health. Configurable to support corporate wellness & benefits programs. ConXus Profile is a configurable health risk assessment (HRA) engine that delivers PDHI’s NCQA certified assessments and can also be used to deploy client developed assessments.
ConXus Profile supports question completion from any PC, tablet, or smartphone. The questionnaire may also be completed using paper forms or facilitated by a health navigator.
PDHI has received Wellness and Health Promotion (WHP) 5 certification from the National Committee for Quality Assurance (NCQA) for health risk assessments for the following populations:
adult and pediatric
adult and pediatric
seniors
These health appraisals use evidence based guidelines and aim for a sixth grade reading level. They follow the National Standards for Culturally and Linguistically Appropriate Services (CLAS) in Health Care in their use of texts and images. To ensure currency with clinical guidelines, PDHI reviews and updates assessments annually, or more frequently when a guideline changes.
The online health assessment can be completed on any PC, tablet, and smartphone. The questionnaire uses conditional branching logic to present relevant question sets to each user based on age, gender, and program options. Clients may configure the questionnaire to add or remove questions.

Data is saved automatically, and the participant may stop and return to complete the questionnaire at a later date. The questions can be switched between over 100 languages at any time using the Google Translate feature.
Upon completion, responses are locked before the personalized report is displayed to the participant. Optional review mode delays the display of the report until biometric data is available.
Demi – recorded: PDHI Wellness Platform Capabilities 20221019_110203-Meeting Recording.mp4
InBody 570 body composition analyzer provides standard outputs like Percent Body Fat, Skeletal Muscle Mass, and BMR, plus total body water, visceral fat assessment, and other vital measurements.
Corporate Wellness Diabetes Disease Prevention Fraility and Aging Intensive Cre Unit Lymphdema
Starting at
Get an in depth analysis of an individual’s lean body mass. Evaluate if an individual has a sufficient level of lean body mass in each segment of the body (arms, legs, and trunk) and spot any imbalances between the limbs.
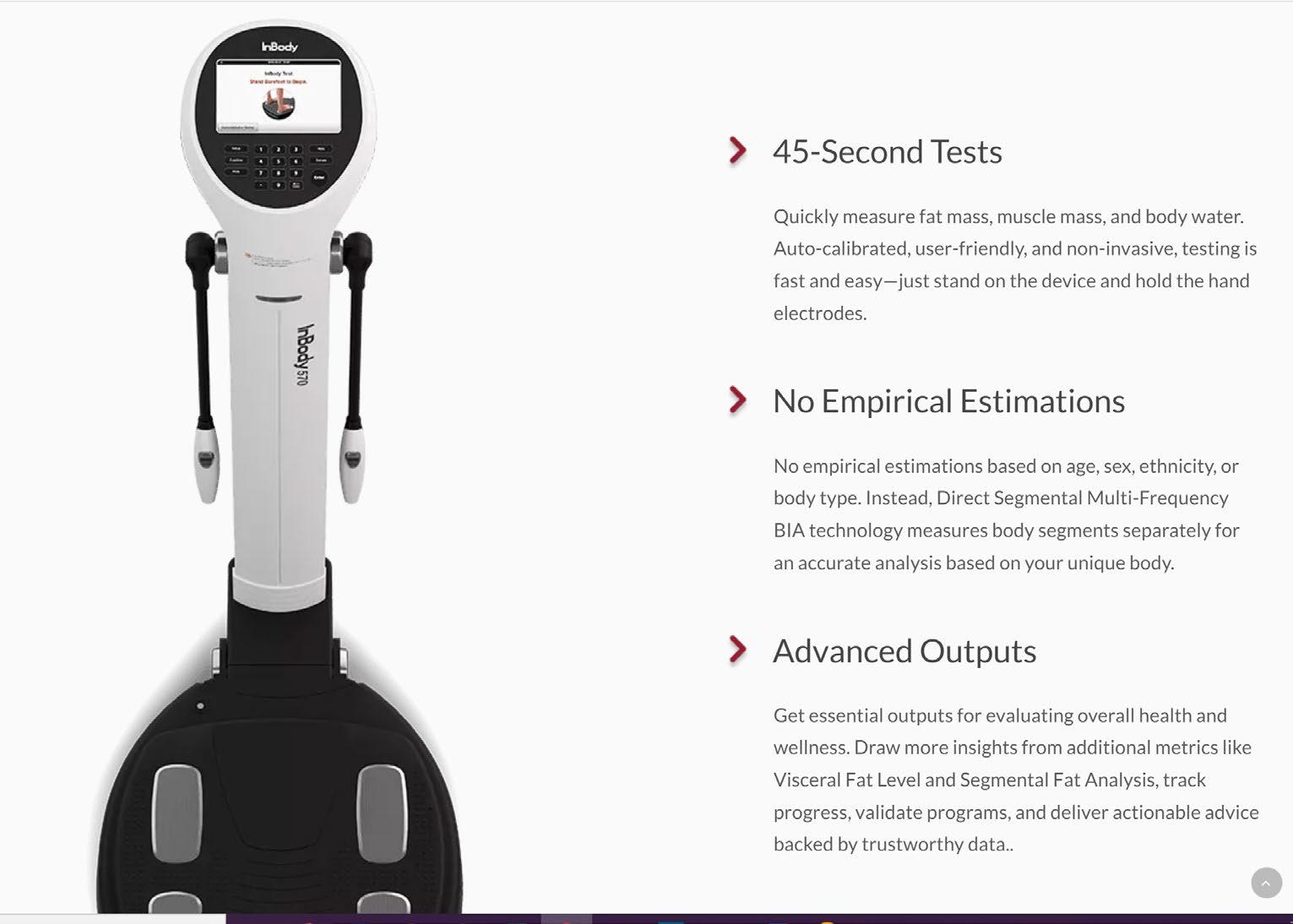
Understand how body water impacts an individual’s body by identifying swelling and other types of water retention in the body.
Where your body fat is located is just as important as how much you have. Focus on important areas like Visceral Fat, the type of fat that surrounds your vital organs, and help individuals reduce their levels for long-term health benefits.
Track changes in Weight, Skeletal Muscle Mass, and Percent Body Fat over time. Spot trends and make timely adjustments to keep your clients headed in the right direction. InBody 570 Result Sheet
Every InBody Test includes a full page Result Sheet printout that details muscle, fat, and water measurements and highlights specific areas to focus on.

Clients get exclusive access to a personal online learning platform with over 7 hours of self paced learning. Master the fundamentals, including testing and Result Sheet breakdown, and become InBody Certified.
Every client gets a dedicated account manager focused on helping you achieve your goals with InBody. From onboarding training to advice on improving your test experience, we will put you in a position to succeed.
Whether you need technical support or you have a question about a Result Sheet, we are here to help. Our experts are available by phone, email, or online chat.
We have the blogs, ebooks, and resources to help you further your understanding of body composition and get the most out of your InBody.
InBody 270 – starting at $6260
InBody 770 – starting at $19,360
InBody 970 – starting at $29,595
The Piccolo Xpress is a portable clinical chemistry system designed for accurate, near patient testing. With the Piccolo’s 12 minute test time, healthcare providers can diagnose and treat within the span of a single office visit, thereby increasing the efficiency of care, reducing costs, and improving patient management.
The menu features 31 blood chemistry tests that range from liver, kidney and metabolic functions to lipids, electrolytes and other specialty analytes. These 31 tests are conveniently configured into 16 completely self contained reagent discs, 11 of which are CLIA waived.
Abbott Point of Care is proud to be the exclusive US distributor of Piccolo Xpress, a fully-automated advanced diagnostic instrument that provides lab accurate results within minutes for a wide range of clinical chemistry needs.
• Enables results in just 12 minutes
• Stores up to 5,000 patient records
• Requires only 0.1 cc (100 ul) of blood, serum, or plasma
• Supports electronic medical records (EMR) connectivity
•
Includes a broad diagnostic menu for routine testing, general health screening, and chronic conditions
• Requires very little maintenance
• CD Software makes testing upgrades easy
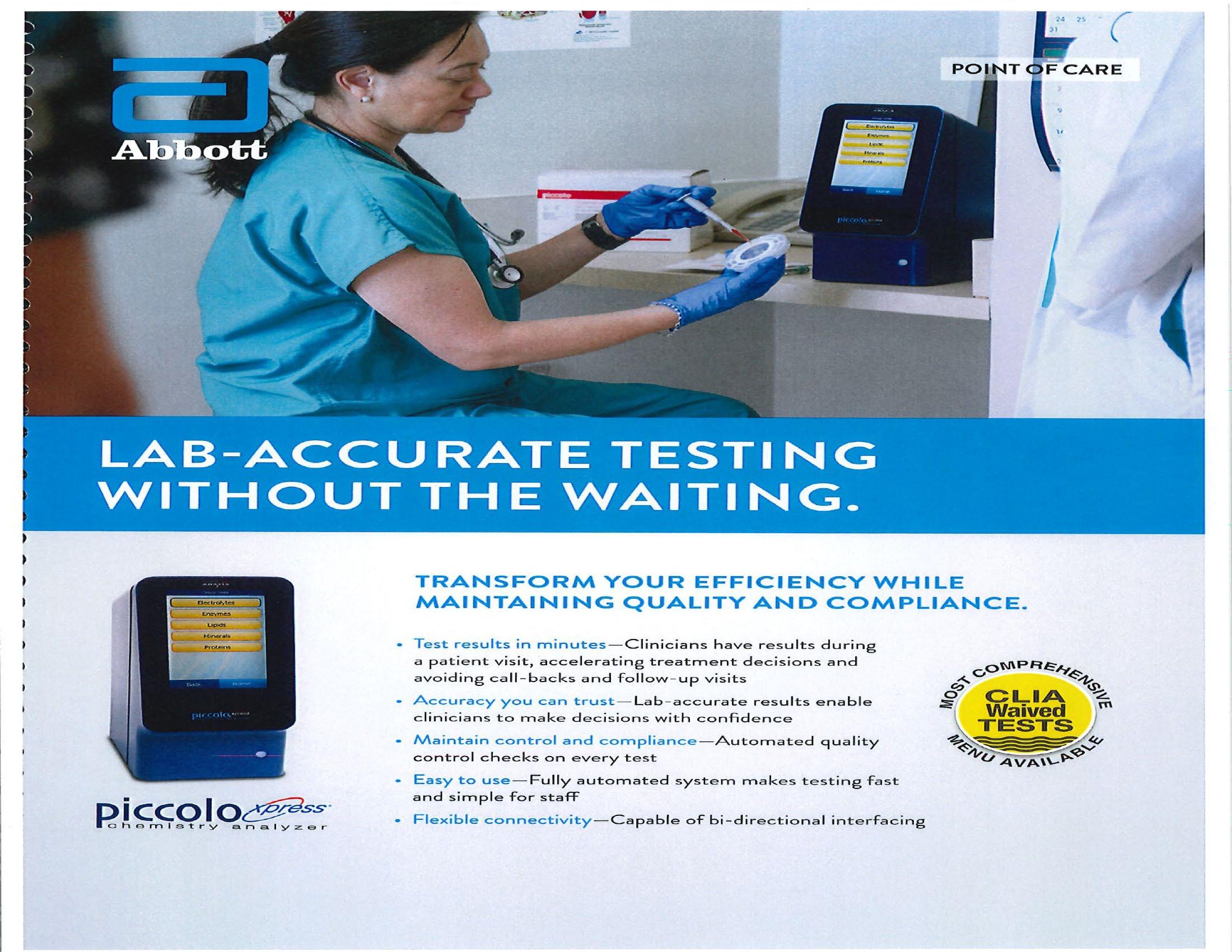
• Operates from line or 15 volt battery power
• Every reagent disc automatically self calibrates
• Self-contained, disposable reagent discs are easy to handle
• The Piccolo Xpress procedure is quick and easy to perform
• No special operating skills are needed to run the Piccolo Xpress
• Flexible alpha numeric data entry options and analyzer settings
• Easy to use color touch screen guides the operator through the process
• Integrated intelligent Quality Control (iQC) checks performance and accuracy
• Direct compatibility supported with USB peripherals including bar code readers, keyboards, personal computers and printers.
Cost per Analyzer: $17,000
•
The CLINITEK Status®+ Analyzer is an automated point-of-care urinalysis analyzer that aids in the assessment, diagnosis, and monitoring of chronic conditions.

• Frees staff for patient care with true walkaway convenience.
• Add sample and the analyzer does the rest.
• Provides results in 1 minute. No waiting for lab results.
• Accurately times test for you no watching the clock!
• Automates and removes subjectivity of result interpretation.
• Automatically transmits test results to minimize transcription errors (when interfaced).
• Proprietary Auto-checks® technology will automatically identify Siemens Healthineers strip type and detect test strip humidity for overexposure.
• Operator lockout prevents use by unauthorized users.
Future ready ask about our upgrade kit for adding connectivity and bar coding.






The Acts Annual IL Review for independent living residents is a commitment to residents to conduct a face-to face clinic visit each year. This visit is unbillable unless the resident is a Medicare (part B) or Medicare Advantage beneficiary AND has elected the community’s NP as their Primary Care Provider. In addition, Medicare (part B) and Medicare Advantage beneficiaries are eligible for Medicare’s Annual Wellness Visit (AWV) for the purpose of creating or updating a personalized prevention plan that may help prevent illness based on current health and risk factors. The Acts NPs may also complete an AWV for Medicare beneficiaries when a resident is not their primary care patient so long as the AWV has not been conducted by the resident’s PCP or other healthcare provider. In these cases, the AWV is completed in lieu of the Annual IL Review and billed to Medicare for reimbursement.
►AWV billing codes and reimbursement rates:
Description CPT Billing Code
Annual Medicare Wellness Visit, initial G0438 $169.23 $143.85
Annual Medicare Wellness Visit, subsequent G0439 $133.64 $113.59
Advanced Care Planning (same day as AWV), first 30 minutes 99497
$ 85.84 $72.96
Advanced Care Planning (same day as AWV), additional 30 minutes 99498 $ 74.32 $63.17
*NPs are reimbursed at 85% of the Medicare Fee Schedule.
►Bloodwork is not currently included in the Annual IL Review but there are options for low cost lab studies to be conducted on campus.
Recommended testing options to be added to the Annual IL Visit:
• CBC panel**
• Basic metabolic panel
• Comprehensive metabolic panel
Lipid panel
• CBC panel (anemia, autoimmune disorders, bone marrow problems, cancer, dehydration, heart disease, infection, inflammation, vitamin and mineral deficiencies
• Basic metabolic panel (Medication side-effects, kidney function, lung function, severe infection, undiagnosed diabetes or inadequately controlled diabetes, hypoglycemia.
• Comprehensive metabolic panel (cognitive dysfunction, problem with the liver, malnutrition, gallstones or another issue blocking the bile ducts, problem affecting bone metabolism
• Lipid panel (total cholesterol, triglycerides, for the evaluation of cardiovascular risk in older adults)
Equipment Identified: Piccolo Xpress Chemical Analyzer
Manufacturer:
$23.63
$20.68
►Nutritional Services
Description
Medical nutrition,
performed by
CPT
(RD) are
to
as follows:
$37.69 $30.15
nutrition, individual, subsequent
therapy subs therapy for change in
malnutrition therapy 2
30
RDs are paid at 80% of the Medicare Fee Schedule
Rehab/Therapy Services
Therapist are
select services performed by
$17.10 $13.68
$32.45 $25.96 Medical Nutrition, group
$32.45 $25.96
$17.10 $13.68
Therapeutic
Description
$35.24 $31.72
$30.36 $27.32
$39.43 $35.49
$33.85 $30.47

https://actsretirementlife.sharepoint.com/:b:/r/sites/NewWell20/Shared%20Documents/Technolog y%20Solutions/Health-Report July 2022.pdf?csf=1&web=1&e=McD0w9
https://actsretirementlife.sharepoint.com/:b:/r/sites/NewWell20/Shared%20Documents/Annual%2 0Visit/Prevounce AWV rates White%20Paper.pdf?csf=1&web=1&e=NFSpnH
https://actsretirementlife.sharepoint.com/:b:/r/sites/NewWell20/Shared%20Documents/Annual%2 0Visit/Wellness visit.pdf?csf=1&web=1&e=rx2sKJ
https://actsretirementlife.sharepoint.com/:b:/r/sites/NewWell20/Shared%20Documents/Annual%2 0Visit/Wellness visit.pdf?csf=1&web=1&e=rx2sKJ
https://actsretirementlife.sharepoint.com/:b:/r/sites/NewWell20/Shared%20Documents/Annual%2 0Visit/Prevounce-AWV-Checklist.pdf?csf=1&web=1&e=NLJCcs
►New Aegis Living Community Pilots Wellness Program
https://www.mcknightsseniorliving.com/home/news/new-aegis-living community pilots-wellnessprogram incorporates nature into design
A Long Life Does Not Always Mean a Happy Life in Old Age https://www.census.gov/library/stories/2021/05/long life-does-not always-mean-a-healthy life in old-age.html
►Hospital At Home White Paper
https://www.fiercebiotech.com/medtech/rockley photonics unveils clinic wrist system-offering-aglimpse at apple watch-s-future
►Matthers Wellness Coaching https://actsretirementlife.sharepoint.com/:b:/r/sites/NewWell20/Shared%20Documents/General/M ather_WellnessCoaching_FINAL.pdf?csf=1&web=1&e=zhl9qU
►AI Technology for Residents
https://www.youtube.com/watch?v=hDcnbL7FM9o
►Book "The Handbook of Structured Life Review" by Barbara K. Haight and Barrett S. Haight.
►CVS Health and Microsoft Announce Strategic Alliance to Re Imagine Personal Care
https://news.microsoft.com/2021/12/02/cvs health and microsoft announce new strategic alliance to reimagine-personalized-care and-accelerate-digital transformation/
►When You Control Your Health Data, You Control Your Options
https://www.ciitizen.com/
►Creating a Personalized Model for Senior Living https://info.seniorlivinginnovationforum.com/blog/creating-a-personalized-model-for-senior-living
►Person Centric Wellness Orange Paper https://info.seniorlivinginnovationforum.com/blog/creating-a-personalized-model-for-senior-living
►A Primer for Evaluation and Integration of Dietary Intake and Physical Activity https://info.seniorlivinginnovationforum.com/blog/creating-a-personalized-model-for-senior-living
►Forward’s Innovative Doctor’s Office Visit https://youtu.be/_h8QvIoSTsE
►Florida Atlantic University (FAU), Center for Advanced Nursing https://youtu.be/_h8QvIoSTsE
►FAU Research Driving 2022 https://youtu.be/_h8QvIoSTsE
►ICAA State of the Wellness Industry https://files.constantcontact.com/b6e71aa6201/e3b7c56f e6d1 46e2 b952 fe4fc7ebbae2.pdf
►Array of Technology Helps Providers Better Serve Residents
https://www.qgdigitalpublishing.com/article/Array+of+technology+helps+providers+better+serve +residents/4283589/749152/article.html
►ACAR Brain Health Intervention Study https://www.youtube.com/watch?v=bk4Mc5ukYw8
►REACT Neuro, A Brain Health Tool https://reactneuro.com/
►How Scientists are Shifting their Search for Links Between Diet and Dementia https://www.sciencenews.org/article/diet food-dementia-alzheimers disease research