Themanagementofpersonalprotective equipmentduringtheCOVID-19pandemic: ThecaseoftheprovinceofQuebec
MartinBeaulieu1 ,JacquesRoy2,ClaudiaRebolledo 2,and SylvainLandry2
Abstract
HealthcareManagementForum 2022,Vol.35(2)48–52 ©2022TheCanadianCollegeof HealthLeaders.Allrightsreserved.
Articlereuseguidelines: sagepub.com/journals-permissions DOI:10.1177/08404704211053996 journals.sagepub.com/home/hmf
LikeotherCanadianprovinces,QuebecmanagedshortagesofPersonalProtectiveEquipment(PPE)intheearlyweeksofthe COVID-19pandemic.Twoyearslater,withhindsight,whatlessonscanwelearnfromthislogisticscrisis?Itispreciselytobetter understandthedecisionsmadebythesupplychainplayersintheprovinceofQuebecthatthispaperwaswritten.Tofully understandtheevents,thispaper firstdescribestheQuebechealthcaresystem.Thenitretracestheseriesofeventsandactions duringthe firstwave,atatimewhenitwasmostchallengingtoprocurePPE.Italsospeci fiesthemaincharacteristicsofthesupply chainintheQuebechealthcaresector.Finally,itanalyzedthesedatatocomeupwithrecommendationstohelppublicdecision makersadoptbettersupplychainmanagementpractices.
Introduction
ThesupplyofPersonalProtectiveEquipment(PPE)wasoneof themostcriticalissuesinthe firstwaveoftheCOVID-19 pandemic.Inaraceagainsttheclock,mostoftheindustrialized countriesweresearchingforthesameproductstomeet increasinglydesperateneeds.Butnow,twoyearslater,with hindsight,whatlessonscanwelearnfromthislogisticscrisis? Itispreciselytobetterunderstandthedecisionsmadeby thesupplychainplayersintheprovinceofQuebecthatthis paperwaswritten.ThiscasemadeuppartofanationalCIHR RapidResearchGrant(#CIHRRef.VR5172669)entitled “DevelopmentofanImplementationFrameworktoAdvance ProvincialandNationalHealthSystemSupplyChain ManagementoftheCOVID-19Pandemic. ”
Beforepresentingourrecommendations,we firstdescribethe methodologyofourstudyandtheQuebechealthcaresystem. Thenwecharttheseriesofeventsandactionsofthe firstwave, whenitwasmostchallengingtoprocurePPE.Finally,we analyzethesedatatocomeupwithrecommendationstohelp publicdecisionmakersadoptbettersupplychainmanagement practices.
Methodology
Thecaseisbuiltoninterviewsofsupplychainmanagersfrom eightQuebechospitals,selectedtoreflectthediversityof healthcareinstitutionsintheprovinceandregionaldifferencesin thepandemic’simpact.Apurposivesamplingwasusedto obtainadiversityofrespondentsfollowingsomerelevant criteria.Forexample,wewantedtohaverespondentsfrom regionsharshlyaffectedbythe firstwaveofCOVID-19.We alsowantedtogetinformationfromhospitalswithdifferent missions:short-termhospitals,long-termcarecentres,and universityhospitals.Theeightselectedhospitalscoveralmost onequarterofallestablishmentsintheprovince.Theinterview
guideintendedtocollectinformationabouttheorganizational structureofthehospitalanditslogisticsdepartment,duringand afterthe firstwaveofthepandemic.Wealsointerviewedtwo PPEsuppliersandseveralmanagersfromQuebec’sMinistryof HealthandSocialServiceslogisticsdirectorateandfromthe healthcarepurchasinggroup.Theselasttwoorganizations playedacentralroleintheprovincialmanagementofPPE. Intotal,morethan20semi-structuredinterviews,lasting60to 120minuteseach,wereconductedbetweenSeptember2020and February2021.
Quebec’shealthcaresystem1
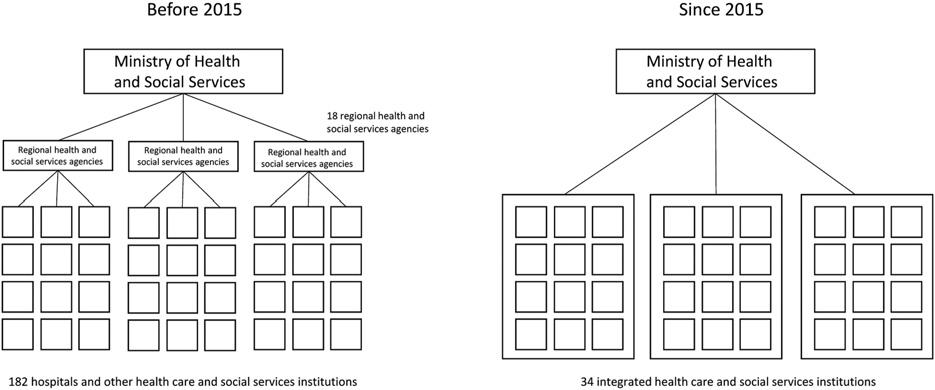
IntheprovinceofQuebec,areformcarriedoutinthespringof 2015decreasedthenumberofpublichealthinstitutionsfrom 182to34. Figure1 illustratesthemajorchangesmadebythe reform.Priortothattime,the rehadbeenregionalhealthand socialserviceagenciesinplacetocoordinateanddevelop thehealthcareofferingwithineachregion ’shealthcare institutions.Theseagenciesprovidedcoordinationatthe intersectionpointbetweentheinstitutionsthemselvesand theguidancegivenbytheprovincialMinistryofHealthand SocialServices.Butthislevelofgovernancewaseliminated duringthereform.Now,institutionsaredirectlyaccountableto theMinistry.Thesenewconsolidatedinstitutionsaresimilarto theIntegratedDeliveryNetworks(IDNs)modelthatappeared intheUnitedStatesinthelate1990s,whosegoalwastooffer awiderangeofhealthservicesunderasingleadministration inordertofacilitatethepatient’scaretrajectory. 2 When
1 HECMontreal,Montreal,Quebec,Canada.
2 HECMontr ´ eal,Montreal,Quebec,Canada.
Correspondingauthor: MartinBeaulieu,HECMontreal,Montreal,Quebec,Canada. E-mail: martin.beaulieu@hec.ca
presentinghisreform,theministermentionedexplicitlythe KaiserPermanentemodelasoneofthemostperformantIDN intheUnitedStates. 3
Quebec’snewinstitutionsnotonlymanageshort-termcare hospitalsbutalsolong-termcarecentresandcommunity services.Thiscanresultininstitutionsconsistingofabout 100facilitiesspreadoveranareaofthousandsofsquare kilometres.Thenetworkofpubliclong-termcarehospitalsis completedwithprivate-unfundedandprivate-fundedinstitutions. Thislastcategoryismadeupofpr ivateorganiza tionsthathave aserviceagreementwiththeregionalinstitutiontooffer “ beds ” andlong-termcare,oftenforsemi-autonomous patients.
Unlikemostotherprovincesinthecountry,Quebec ’s MinistryofHealthandSocialServiceshasitsown logisticsdirectorate.Thetraditionalroleofthisdirectorate istocoordinateprocurementandlogisticsinitiativesbetween institutionswithinthesystemorbetweenthesefacilitiesand otherpartsofthegovernment.Thedirectoratedoesnotcarry outoperationalactivitiessuchasproductorservice contractingorinventorymanagement.Rather,itsprimary roleistoprovideguidanceonsupplychainissues.While theroleoflogisticshasprogressedincrementallyinthe Quebechealthsystemsincethe2000s, 4 thespring2015 reformcreatedtheconditionsforrevaluatinghealthcare logisticsininstitutions.Thereformhasbeenaccompanied bythecreationoflogisticsdepartments,andalogistics directornowsitsoneachboardofdirectors.
OnefeatureofQuebec ’shealthcaresectorhadbeenthe presenceofthreepurchasinggroupsthathandledthe contractingofabout30%ofthehealthcareinstitutions ’ procurementbudget. 5 Aswithothercommoditiesinthe healthcaresector,contractsforPPEinQuebecarevery oftenawardedthroughgrouppurchasingorganizationsthat leveragetheconsolidated volumesfromtheirmember institutionstoobtainlowpricesfortheseitems. 6 Theuse ofgrouppurchasingorganiza tionsputspressureonsuppliers tostaycompetitivetoobtainorretainasigni fi cantmarket share.ThisphenomenonisnotuniquetoQuebecasgroup purchasingorganizationsarefoundelsewhereinCanadaand
intheUnitedStates. 7 , 8 Itshouldbenotedthat,inwinter2019, afurtherQuebecgovernmentreformmergedthethree healthcarepurchasinggroupsintoasingleorganization thatwouldnolongerbeaccountabletotheMinistryof HealthandSocialServicesbutinsteadtotheTreasury Board.Thisneworganizationwastoenterintoserviceon April1,2020,butthiswaspushedbacktoSeptember1,2020, duetothepandemic.
Keydates
Toprovideatimelineofthedecisionsmadebythemainplayers intheQuebechealthcaresector, Table1 outlinesthemajor eventsinthePPEcrisis.Thistableplacesthekeydecisions relatedtoPPEmanagementinthetimelineofthemajoreventsof thepandemic.
Thetimelineofeventsshowsthat,longbeforetheCOVID19pandemicstruckQuebec,therewasalogisticscrisisinthe supplyofPPE.UnlikeinEuropeortheUnitedStates,where 50%ofPPEneedsaregenerallymetbylocalproduction, 9 Canadawasalmostentirelydependentonforeignmarkets fortheseitemspriortotheCOVID-19pandemic. 10 The characteristicsofthePPEsupplychain(low-coststrategy andproductionoffshoredtoAsia)hadledtoChina,and specificallytheWuhanregion,becomingtheworld’smain PPEproductioncentre.11 The firstimpactsofthepandemic arrivedjustatthestartoftheChineseNewYearfestivitieson January24,2020,andthesubsequentfour-weekinterruptionin China’seconomicactivity.Also,theWuhanareawasplaced underastrictlockdowntostopthespreadofthevirus.China’s reducedactivityduringthistimemeantthatglobalPPE productioncapacitywassignificantlytruncatedforovertwo months.12 Underthesespecificcircumstances,thewindowof opportunityforsecuringaninventoryofPPEhadbecomevery narrow.
StartinginearlyFebruary2020,theHealthMinistry’s logisticsdirectorateestablishedaPPEcrisisunit,which becamethecontrolcentreforprovincialneedsandtheoffer availableonthesupplymarket.Thisunitbeganwithjustafew individuals,butitincorporatedotheremployeesfromthehealth system(institutionsandpurchasinggroups)asnewneedsor
Table1. Timelineofmajorevents.
DateEvent
2019-12-01Patientzero(unofficial)identifiedinChina’sWuhanregion
2019-12-31Chinarevealsithasidenti fiedanewcoronavirusstrain
Early2020HealthcaresupplierswithinternationaloperationspickupsignalsfromtheirofficesinAsiathatsometroublingthingsare happeninginChina
Mid-January 2020 OnehospitalintheprovinceofQuebecplacesalargePPEorder,equivalenttosixmonths’ worthofnormalconsumption
2020-01-23PublichealthpublishesaninternalMinistryofHealthreportonthecoronavirus
2020-01-24StartoftheChineseNewYearfestivities,andstrictlockdownoftheWuhanregionuntilApril8,2020
2020-02-05FirstmeetingofatacticalcommitteeonPPE,ledbythelogisticsdirectorateofQuebec’sMinistryofHealthandSocialServices. ThiscommitteeincludedPPEproviders,amongothers
2020-02-27Theprovince’ s fi rstCOVID-19caseisconfirmed
2020-03-13Quebecdeclaresapublichealthemergency.TheMinisterofHealthandSocialServicesandthehealthandsocialservices institutionsmay,withoutdelayandwithoutformality[ ],enterintonewcontractsastheydeemnecessary
2020-03-16The firstCOVID-relateddeathoccursintheprovinceofQuebec
2020-03-20TheMinistrysendsalettertoall34institutionsstatingthattheycannolongerorderfromPPEsuppliersandthattheMinistrywill allocatesupplies.TheMinistrybecomestheintermediarybetweentheneedsofinstitutionsandtheofferfromthesupplier market.The34institutionsthenbecomehubsresponsibleforredistributingPPEtootherpublicinstitutions(schools,daycare centres,andprisons)andseniorresidences
2020-03-31Inapressconference,theQuebecpremieracknowledgesthatashortageofsomeequipment,particularlymasks,threatenstohit Quebecwithin3to5days
Mid-April2020Theprovincialstockpilehasagrowinginventory
2020-04-22Quebecexceeds20COVID-19deathsper100,000inhabitants
2020-05-17Quebecexceeds50COVID-19deathsper100,000inhabitants
2020-06-29Theallocationstrategyismodified,movingfromacentralizedmanagementofPPEsupplierrelationshipsandreturningto decentralizedordermanagementbyhealthcareinstitutions
Abbreviation:PPE,personalprotectiveequipment.
problemsarose,anditeventuallybecametheCOVID-19 operationsteam.Upto60peopleweredirectlyinvolvedin thiscommittee,whichhadregularcontactwiththeindustry’s majorsuppliers.ItsmandatewasinitiallyfocusedonPPE management,butiteventuallyalsotookonneedsrelatingto screeningtestsandtothepurchaseoftreatmentequipment,such asrespirators,forthehospitals.
Thestateofthesupplychaininfrastructure beforethecrisis
Afterconductinginterviewswithstakeholders,weidentified fourbasicfeaturesthatunderminedtheefficiencyofthePPE procurementprocessduringthepandemic.First,relationsbetween theHealthMinistry’slogisticsdirectorate andthe34healthcare institutionshadhistoricallybeenconsensusbased.Thedirectorate didnotseektoimposeguidelines.Ittooktimetoconsultwith,and listentotheopinionsof,thevariouspartners.However,thistypeof managementbyconsensuswasill-suitedtoacrisis,whenitbecame criticaltobeabletomakedecisionsquickly.
Second,informationsystemswereunfitforlogistics operations.Thesesystemswereoriginallydevelopedwitha viewto financialreporting.Forinstance,theproductscoming outoftheregionalwarehouseofahealthcareinstitutionisconsidered anexpense,althoughtheproductmaybephysicallystoredinacare
unit.Thisshortcomingmakesitmoredifficulttoknowtheactual stockconditionsinagivenhospital.Also,theseinformationsystems arenotabletoproduceconsumptionforecasts.And finally,each healthcareinstitutionhasitsownproductnomenclature(eg, productnumbers),makingitcomplextogetanexactsnapshotof stocksinhealthcareinstitutions.
Third,relationswithsuppliersweremostlylimitedto transactions.Quebec’sregulatoryframeworkinthisareamay bethemostcomplexamongCanadianprovinces.In2008, Quebecadoptedalawandregulationsoncontractsforpublic organizations,whichincludedsome250articles.Thatnumber hasnowmorethandoubled.Thisframeworksetsparametersfor thecontractualprocessandthenatureofrelationshipswith suppliers.Giventhiscontext,relationshipsbetweenhealthcare institutionsandsupplierstendtobehighlytransactionalin nature.
Lastly,embryonicperformancemanagementsystemswerein place.ResearchbyBeaulieuandRoyshowedthattherewasnoreal performancemanagementsystemforlogisticsactivitiesin healthcareinstitutionspriortothesystem’sreform.13 Generally, veryfewperformanceindicatorsareusedinhealthcare institutions ’ logisticsdepartments,andwhentheyare,they areusedataverylowfrequencyrate.Thelogisticsdepartments ofhealthcareinstitutionsareoftenreactivetoanydisruptions thatmayariseinthecourseofday-to-dayoperations.
Recommendations
Inthelightoftheseobservations,weoffersomerecommendations basedonbestpractices,inordertobebetterpreparedforfuture crises.
1. Identifypredictorstoanticipatetheemergenceof futurepandemics: OneQuebechospitalmadea massivePPEpurchaseinmid-January,anticipatingthe effectsofthepandemic(seeTable1).Thisinstitution tooknoteofearlywarningsigns,forexample,the geographicspreadoftheviruscombinedwithits modeoftransmission,thatwerevisibletoall.Infact, pandemicscanbeanticipated,especiallyinNorth America,whichtendstobethelastplaceinwhich theygainafoothold. 14 However,themonitoringof earlypandemicsignsshouldbedoneattheprovincial level.Thereshouldbeaprovincialauthorityincharge ofthis.Inthespecificcontextofhealth,twoteamscould possiblytakeonthisresponsibility:publichealthdecision makersorlogisticsdecisionmakers.Intheory,public healthdecisionmakersshouldbetheonesmonitoring forthepotentialemergenceofapandemic.However,itis difficultforpublichealthdepartmentstopredicthowa pandemicmightimpactonthesupplyofproductsand supplies,suchasPPE.TheQuebecexperienceshowsthat thesedecisionmakersprimarilybasetheirdecisionson scientificevidencefrommultiplevalidatedsources. Quebec’spublichealthdepartmentissuedaninitial advisoryonCOVID-19justasthewindowof opportunityforimplementinganeffectivelogistics contingencyplanwasclosing.However,supplychain decisionmakersareaccustomedtomakingpredictions andweightingrisks.Theseapproacheswouldmakeit possibletoproposepreventivemeasuressuchasstocking uponproductsandlaunchinganoperationalpandemic managementteam.
2. Developprocurementexpertise: Thisisrequiredto makepurchasesthatconsidertheparticularcharacteristics andchallengesofinternationalmarketsandtoanalyzethe risksassociatedwithsupplysources.Duringthe pandemic,itwasnecessarytonegotiatedirectlywith foreignmanufacturers,andveryfewbuyersfromthe publicsectorwerefamiliarwiththespecificregulations involvedininternationalprocurement.
3. Defineacentralizedlogistics-managementstructure andallocationpoliciesforapandemicorothercrisis: Acentralizedstructurewouldsimplifycommunications betweensuppliersandhealthcareinstitutions,thereby reducingcompetitionwithinthesystem.Personal protectiveequipmentallocationpoliciesmustbe regularlyupdatedtoreflectthecurrentsituation.Weare notcallingforapermanentcentralizedstructure;however, theexperienceinQuebecandelsewhereconfirmsthat suchastructureisnecessaryintimesofcrisis.15
4. Ensurethatkeyinformationforademandmanagementsystemthat’sindispensableduringa pandemiciskeptuptodate: Itissimplertomaintain thisbasicinformationfromdaytodaythantotrytoupdate itinthemidstofacrisis.Untilthiscrisis,logistical informationmanagementwasnotapriorityinQuebec’s healthsector,andagreatdealofeffortwasrequiredto overcomethisshortcomingduringthepandemic.
5. Maintainclosecollaborationbetweenlogistics decisionmakersandtheinfectionpreventionand controldepartmentsinhealthcareinstitutions: This kindofcollaborationwouldgivelogisticsmanagersmore legitimacywhenitcomestoensuringrespectforPPEuser protocols,andexpertiseforqualitycontrolinpurchasing. Theinstitutionsthatwereabletoquicklyimplementthis typeofcollaborationavoidedpointlesspurchasesofthe wrongproductsandwereabletocontrolconsumption withintheirinstitution.
6.
Improvecollaborationbetweenhealthcareinstitutions
andsuppliers: Suchcollaborationcangivesuppliersmore insightintodemand,sothattheycansuggestsolutionsin theeventofshortages.Inreturn,supplierscouldshare strategicinformationonmarketsandtheirconstraintswith healthcareinstitutions.ForQuebec’shealthcaresector,such acollaborativeapproachisaradicalchangeofphilosophy intermsofsuppliermanagement.
Figure2 makesalinkbetweentherecommendations formulatedandthebasicfeaturesofQuebec’shealthsector, whichwerepresentedintheprevioussection.Asstatedearlier, someofthesefeaturesarenotshortcomingsassuchbutdo hindereffectivecrisismanagement.
Onefundamentalchallengeintersectswithseveralofthe formulatedrecommendations:breakingdownorganizational silostofostercommunicationbetweenlogisticsdecisionmakers, clinicaldecisionmakers,publichealthdecisionmakers,and suppliers.Thiscommunicationmustnotbethoughtof exclusivelyintermsofinformationtechnologybutshould encompassotherintegrativemechanisms(multidisciplinary teams,diverseprofessionalprofi les,andmore).
Last,theserecommendationsfallmostlyundertheheading ofpreparednessmeasures,whichdonotpreventcrisesbut ratherminimizetheirmanagementchallenges.16 Preventive measuresconstitutea fi rst-levelresponsetohelpmanagers concentratetheireffortsinto fi ndingsolutionstounexpected problemsonceacrisisoccurs.Furthermore,publicdecision makersshouldnotlimittheirfocustoonlypreparedness measures.EventhoughPPEmanagementinQuebecwas thestartingpointfortheserecommendations,manyofthem alsoaddresslong-standingshortcomingsinthelogisticschain thatarealsopresentinmanyotherjurisdictionsinCanadaand inotherindustria lizedcountries. 17 Publicdecidersshould supportinvestmentsintonewinformationtechnologyand intoskillstraininganddevelopmentforthelogisticsstaffof healthestablishments,andtheyshouldimplementnewpractices withsuppliers.Theideahereisnotonlytopreventanew procurementcrisisbutalsotoenhancetheday-to-day performanceofthelogisticschain.Thisisarealchallenge thatwillrequireagreatdealofperseverance,sincethelogistics chainforhealthcareispossiblythemostcomplexofall.
ORCIDiD
MartinBeaulieu https://orcid.org/0000-0002-7998-801X
References
1.BeaulieuM,BentaharO,BenzidiaS.Theevolutionofhealthcare logistics:theCanadianexperience. JApplBusEcon.2020;22(14): 196-202.
2.CuellarAE,GertlerPJ.Trendsinhospitalconsolidation:the formationoflocalsystems. HealthAff.2003;22(6):77-87.
3.BoyerT.LemodèleKaiserPermanentecommefondementdela r ´ eformedusystèmequ ´ eb ´ ecoisdelasant ´ eetdesservicessociaux:
quefaut-ilenretenir? RevueCNRIS.2015;6(3). https://oraprdnt. uqtr.uquebec.ca/pls/public/gscw031?owa_no_site=357&owa_no_ fiche=233
4.LandryS,BeaulieuM,RoyJ.Strategydeploymentinhealthcare services:acasestudyapproach. TechnolForecastSocChange. 2016;113(B):429-437.
5.BeaulieuM. Logistiquehospitalière:performancedesactivit ´ esde gestiondel’approvisionnementdes ´ etablissementsqu ´ eb ´ ecois Montr ´ eal:Centresurlaproductivit ´ eetdelaprosp ´ erit ´ e;2019.
6.BeaulieuM,RebolledoC.Repenserlaperformancedesongroupe d’achats.In:BentaharO,BenzidiaS,eds. SupplyChain Managementdelasant ´ e.Caen,FR: ´ EditionsManagement& Soci ´ et ´ e;2019:359.
7.ArneyL,YadavP,MillerR,WilkersonT.Strategiccontracting practicestoimproveprocurementofhealthcommodities. Glob HealthSciPract.2014;2(3):295-306.
8.NolletJ,BeaulieuM,Fabbe-CostesN.Measuringpurchasing groupsperformanceinthehealthcaresector. CanJAdmSci 2019;36(4):514-526.
9.BownCP.COVID-19:China’sexportsofmedicalsuppliesprovide arayofhope.Availableat: https://www.piie.com/blogs/trade-andinvestment-policy-watch/covid-19-chinas-exports-medicalsupplies-provide-ray-hope .PublishedMarch26,2020.
10.DeMontignyP.LeCanadaest-ilautosuffisanten ´ equipementde protectionindividuelle?Availableat: https://ici.radio-canada.ca/ nouvelle/1731924/autosuffisance-canada-masques-equipementprotection-individuelle .PublishedOctober7,2020
11.TorsekarM.Medtech ’ssupplychain:adecadeinreview. Availableat: https://www.mpo-mag.com/issues/2020-01-29/ view_columns/medtechs-supply-chain-a-decade-in-review/ PublishedJanuary29,2020.
12.WadhwaP.GlobalannualspendonPPEcanhit$50-80bn;China keyplayer:Jefferies. BusinessStandard.Availableat: https://www. business-standard.com/article/current-affairs/global-annual-spendon-ppe-can-hit-50-80bn-china-key-player-jefferies-120063000576_1. html.June3,2020.
13.BeaulieuM,RoyJ.Benchmarkingdelagestiondesachatsetdes stocksenmilieuhospitalier:unedemarchecanadienne. Logistique Manag.2015;23(3):17-27.
14.Saunders-HastingsPR,KrewskiD.Reviewingthehistoryof pandemicInfluenza:understandingpatternsofemergenceand transmission. Pathogens.2016;5(4):66.
15.BohmerRMJ,PisanoGP,SadunR,TsaiTC.Howhospitalscan managesupplyshortagesasdemandsurges. HarvardBusiness Review.Availableat: https://hbr.org/2020/04/how-hospitals-canmanage-supply-shortages-as-demand-surges .April3,2020.
16.NatarajarathinamM,CaparI,NarayananA.Managingsupply chainsintimesofcrisis:areviewofliteratureandinsights. IntJnl PhysDistLogManage.2009;39(7):535-573.
17.SrivastavaS,GargD,AgarwalA.Asteptowardsresponsive healthcaresupplychainmanagement:anoverview.In:Singari RM,MathiyazhaganK,KumarH,eds. AdvancesinManufacturing andIndustrialEngineering.LectureNotesinMechanical Engineering.Singapore:Springer;2021.
