




















Dear patients, families and care partners,
On behalf of the entire team at Michael Garron Hospital (MGH), I would like to welcome you to our hospital and to the East Toronto community. We understand this may be a difficult time for you and your family. Our staff, physicians and volunteers are committed to offering you a supportive and inclusive place of healing during your stay with us.
This Patient Guide will help answer any questions you may have while visiting our hospital. If you wish to speak to someone, we encourage you to reach out to a member of your care team, the manager on the unit where you are being cared for, or the Patient Experience Department.
For more than 95 years, MGH has been the heart of East Toronto. Today, we proudly serve more than 400,000 people across East Toronto and provide care during some of the most cherished and difficult moments in their lives. Whether it’s delivering babies, caring for children during their formative years, providing emergency care, mental health support or surgical services – we are here for you.
We believe in partnering with you to deliver high-quality, compassionate care that is tailored to your needs – because your voice matters when it comes to making decisions about your health.
We can also connect you and your loved ones with the many care partners we have in East Toronto. This ensures a more seamless transition from the hospital, and that you are part of a more connected healthcare system.
This patient guide is your resource to connect with MGH and beyond. I encourage you to read it and understand the many services that are available. Sincerely,
Melanie Kohn President and CEO, Michael Garron Hospital


- 215 acute care inpatient beds
- 80% single-patient bedrooms with private washrooms
- Use of natural light
- Clear, intuitive signage
- Four levels of underground parking
- Green rooftop gardens
- Expansive vehicular drop off
- Lush community landscaping
- Central food court and retail spaces
- Co-located clinics for ease of access
- State of the art technology and equipment
- Spacious and efficient clinical workspaces
Throughout history, MGH has continually adapted its campus and facilities to meet the changing healthcare needs of the community.
Today, we find ourselves in a position where we can no longer rely on expansion. We must replace some of our most outdated clinical care areas to ensure we can continue to provide a welcoming, safe and efficient facility for our patients and their families.
MGH’s redevelopment project included the creation of the eight-storey Ken and Marilyn Thomson Patient Care Centre (Thomson Centre) at the corner of Coxwell and Sammon Avenues, which opened in early 2023; renovations to some of our existing spaces; and the demolition of several outdated wings.
After the opening of the Thomson Centre in early 2023, MGH, in partnership with EllisDon and Infrastructure Ontario, is embarking on the next phase of its campus redevelopment project, which includes renovation, demolition and landscaping work. This next phase is ongoing and will continue until 2026. Some milestones of this phase include interior renovations to existing spaces (e.g. Maternal, Newborn and Child clinics; an expanded Moez and Marissa Kassam Food Court); construction of a new entrance on Coxwell Avenue; and the demolition of A, B and C wings.
During this time, patients and visitors can expect to experience noise, hallway closures and detours around the hospital. We’re very excited about the next phase of this transformational project as it is the largest construction project in the history of MGH – a project that will forever change the organization and the care we provide the East Toronto community.

Our Vision
Great care inspired by community.
Our Purpose
Building a healthier community together.
Our Values
Compassion. Respect. Integrity. Inclusion. Courage.
Please note: Due to MGH’s ongoing campus redevelopment, this map may be out of date. Please visit our website for the most recent map: tehn.ca/hospital-campus-map
We acknowledge the sacred land which we are situated upon, the traditional territories of the Wendat, Haudenosaunee (Ho-den- oh-shonee), the Anishinabeg (Ah-nish-in-nah-beg), and the Mississaugas of the Credit. This territory is covered by the Dish with One Spoon Wampum Belt Covenant, an agreement between the allied nations to peaceably share and care for the lands around the Great Lakes.
We recognize the many Indigenous Peoples who presently live on this land known as Turtle Island as well as their ancestors. We further recognize that the contributions and historic importance of Indigenous Peoples must be clearly and overtly connected to our collective commitment to make the Truth and Reconciliation Commission of Canada: Calls to Action real in our communities and in our work.
The hospital will remain committed to advancing Indigenous sovereignty in the work that we do, knowing that this is not a single action, but an intentional journey.
MGH is committed to providing barrier-free access for all persons to its environments, programs and services. We are continually working to make our space more accessible and have embarked on a multi-year redevelopment project that will modernize our physical space to meet and exceed the accessibility requirements under the Accessibility for Ontarians with Disabilities Act (AODA) and its regulations, including the Accessibility Standards for Customer Service.
See and learn more about the hospital’s Accessibility Plan at tehn.ca/ accessibility.
We acknowledge the rich diversity, history and heritage of Indigenous people across the Greater Toronto Area and Southern Ontario. We are honoured and privileged to live and work on these lands.
We are committed to building stronger relationships with Indigenous communities and to creating an environment that supports culture and tradition and improves health outcomes for Indigenous peoples. If you identify as First Nations, Inuit or Métis, and are coming to MGH for care, the Spiritual Health Team will work with community health partners to access traditional medicines, ceremony and traditional healers.
If you are receiving treatment in our Oncology Department, staff and Spiritual Health can help you access our sacred drum, which was gifted to the hospital in partnership with the Indigenous Cancer Care Program.
At MGH, patients, family members, care partners, friends, staff, physicians, volunteers and learners are committed to working together.
When we work together, care is safe, appropriate, patient-centred and in line with our values.
Everyone at MGH will:
• Give and receive fair and compassionate treatment regardless of religion, ethnic origin, age, sex, gender identity, gender expression, sexual orientation or ability.
• Commit to respecting and integrating traditional healing practices, ceremonies and medicines as part of a community member’s healing journey.
• Welcome family and friends to be a part of care, as wanted by the patient.
• Communicate in a way that is clear, open and honest.
• Share information that will help make informed care and treatment decisions.
• Listen to and respect each other’s ideas and choices.
• Respect each other’s privacy.
• Create a safe place to talk about what went well and what can be improved.
• Work together to build a safe environment.
• Work together to make things better.
We are here to support you. If you have feedback or a concern, please contact the unit manager or Patient Experience.
At MGH, we value feedback from patients and families so that we can better understand how they experience our care and services. The Patient Experience Office provides patients and families a supportive opportunity to share compliments, concerns, questions or suggestions about their experiences at MGH.
The Patient Experience Office supports patients, families, and community members by:
• Answering questions about services at the hospital and explaining hospital policies and procedures.
• Assisting with healthcare system navigation.
• Listening to concerns and discussing reasonable follow-up options.
• Identifying the appropriate staff member, leader or physician to address concerns.
• Facilitating the complaint resolution process.
Contacting the Patient Experience Office:
• In-person: The office is located on the main floor - G Wing, Room G1-221. It is open Monday to Friday, from 9 a.m. to 3 p.m. (excluding holidays)
• By phone: 416-469-6096
Outside of office hours, please leave a message and we will return your call within one business day.
• By email: PatientExperience@tehn.ca
• By mail: Patient Experience Specialist
Michael Garron Hospital 825 Coxwell Avenue Toronto, ON M4C 3E7
MGH learns about the care that we provide by sending surveys to patients by email after their discharge. If you have provided an email address you may receive a survey shortly after you go home. These surveys let us know what we are doing right and where we need to improve. Your advice and feedback will directly impact the care and services we provide to future patients and families. If you do not receive a survey and want to provide feedback you can contact the Patient Experience Office at 416469-6096 or PatientExperience@tehn.ca.
Your medical team will help care for you while you are in the hospital. Your medical team will include:
• Attending Physician: A doctor who is in charge of your care while you are in hospital. They also supervise the fellows, residents or medical students who may also be involved in your care.
• Resident or Fellow: A doctor or clinician who is completing their training at the hospital.
• Registered Nurses: A nurse who keeps track of your health and well-being, and teaches you about your illness or injury. They also supervise nursing students who may also be involved in your care. Each day, you may have two to three different nurses.
Your medical team may also include:
• Consulting Physician: A specialist doctor who is asked by the Attending Physician to give recommendations about specific aspects of your care. They also supervise the fellows, residents or medical students who may also be involved with the consultation.
• Physician Assistant: A medically educated clinician who works with the doctors. They help assess and manage your health and medical needs while you are in the hospital.
• Nurse Practitioner: A nurse who has additional education and specialized training to assess and manage your medical needs and plan your care. They can make diagnoses, order tests, interpret results and prescribe medications.
Depending on your needs, other care team members may also help support you and help you prepare to leave the hospital. This may include:
• Dietitian: Helps you choose the right foods for your meal planning.
• Occupational Therapist: Helps you plan how to safely do everyday activities such as eating, bathing and getting dressed.
• Physiotherapist: Helps you plan how to be more independent by building your strength, balance and coordination.
• Social Worker: Helps you manage your feelings, relationships and financial needs. They may help you plan for when you go home.
• Speech-Language Pathologist: Helps you with problems talking or swallowing.
• Home and Community Care Support Services Staff: Help set you up with care in the community to support your transition home or find you a long-term care home, if needed.
MGH is a teaching partner with the University of Toronto and a number of other learning institutes. During your time at the hospital, you may be seen by medical trainees and students. In addition, the hospital continuously participates in research studies and innovative initiatives.
MGH’s Spiritual Health Practitioners are Registered Psychotherapists (CRPO) and are affiliated with the Canadian Association for Spiritual Care (CASC). They are available to provide:
• Emotional support (suffering and coping)
• Religious support (prayers and rituals)
• Spiritual support (meaning and purpose)
• Grief support (death and loss)
• Family and caregiver support
If you, or one of your family members, would like to speak with a Spiritual Health Practitioner, please ask any member of your care team to connect you. You can also contact Spiritual Health directly at 416-461-8272 ext. 6550. Spiritual Health Practitioners are on-site Monday to Friday, from 8:30 a.m. to 4:30 p.m.
More than 550 volunteers give thousands of hours each year to help in over 40 areas of the hospital. Volunteers are an important part of providing patients with excellent care at the hospital.
Volunteers offer many services, including:
• Pet therapy
• Therapeutic touch
• Friendly visiting
• Comfort choir
• Knitted blanket delivery

To access services or to become a volunteer at the hospital, please contact Volunteer Services at volunteer@tehn.ca.
MGH’s main public parking is in the Dewji Family and Mr. Lube Parking Garage (entrance on Sammon Avenue east of Coxwell Avenue). Patients and visitors are encouraged to park on P1 and P2 of this underground parking garage. Please note, as of November 1, 2022, the Sammon Avenue Visitor Lot (west of Coxwell Avenue) is no longer available for public parking. Metered parking is available around the hospital.
Monday to Friday
Maximum (7 a.m. – 6 p.m.) ............................ $5 for every 20 minutes (Maximum $27.50)
Flat rate (6 p.m. – 7 a.m.) ............................... $12 flat rate
24-hour maximum ......................................... $31.20
Flat rate (7 a.m. – 6 p.m.) .............$12 flat rate
Flat rate (6 p.m. – 7 a.m.) .............$12 flat rate
Lost ticket (minimum fee) ..................... $27.50
We have 5-, 10- and 30-day hospital parking passes available to patients, families and visitors. Parking passes provide access for patients and visitors with in-and-out privileges 24 hours a day and are transferable for up to three vehicles for the Dewji Family and Mr. Lube Parking Garage. Parking passes can be obtained by visiting Patient Registration (M1) on the first floor, which is open Monday to Friday from 5:45 a.m. to 11:30 p.m. and weekends and statutory holidays from 7:30 a.m. to 11:00 p.m.
5-day pass ................................................. $78
10-day pass ............................................. $156
30-day pass ............................................. $468
‘Extend-by-phone’ is a feature that will remind you when your parking is about to expire and allow you to extend your parking through your mobile phone. To use this feature, look for the ‘extend-by- phone’ marking on the parking meter. Once you have successfully paid for parking with a credit card, the parking meter will prompt you to enter your mobile phone number. This phone number will receive a text message when parking is about to expire and offer an option to add additional time. For more information on this feature, watch the video in this link: youtube.com/watch?v=Ih_YjkT6v3E.
Designated parking spaces for persons with disabilities are available in the Dewji Family and Mr. Lube Parking Garage (main public parking, entrance on Sammon Avenue east of Coxwell Avenue). The Sammon Avenue entrance also serves as a drop-off zone. However, parking in this zone is not permitted. Parking meters are also located throughout the campus and are monitored 24 hours a day, seven days a week. Please be aware that all street parking meters are operated and enforced by the City of Toronto in accordance with the City of Toronto parking bylaws. Vehicles parked at expired meters or spaces will be ticketed.
Parking machines are located in hospital parking lots. They accept bills, coins and credit cards.
Parking is prohibited in the Coxwell Avenue driveway as it is a fire route. Vehicles parked in the driveway will be ticketed by the City of Toronto.
If you or a family member is being admitted to the hospital, or you are visiting a friend or family member, we want your stay to be as comfortable as possible and for everyone to be informed. Please speak to a member of your care team if you have any questions or concerns. This section of the Patient and Family Guide shares information about what you can expect when admitted to the hospital and preparing to go home.
We prepare and serve over 1,300 patient meals daily, ensuring that meals and menus are nutritionally balanced.
We offer a choice menu system based on individual dietary requirements and preferences as per your and/or your clinician’s guidance. Meal items are chosen for the next day.
Food Services staff will serve your meals during the following times:
• Breakfast: 7:40 a.m. to 9 a.m.
• Lunch: 11:40 a.m. to 1 p.m.
• Dinner 4:40 p.m. to 6 p.m.
Bedside telephone services are available only in some of the patient rooms. This enables you to make and receive external calls. External calls can be received from 7:30 a.m. to 9 p.m. To place a local call from a bedside phone, please dial “9” followed by the phone number. To make a long-distance call, please dial “9” then “0” to reach the Bell operator. Once you are discharged, please remember to let your friends and family know that you are leaving so the next patient does not receive your calls.
You are welcome to bring your personal cellphone for use while in hospital.
MGH offers free guest Wi-Fi. To access MGH’s Wi-Fi, simply connect to the “MGH_ Guest” network, which will require an acceptance of the Guest Wi-Fi terms of service. There is no password required.
When you press your call bell button, a call will go to your nurse. Your nurse will get an alert on a device they are carrying. If your nurse doesn’t answer right away, they may be with another patient, in a public area or unable to receive your call. All clinical or confidential discussions about your care should happen in-person and not through the call bell system.
If you are a resident of Canada, you must have your health card with you on every visit. This shows that your healthcare services are paid for by your government health insurance plan. In Ontario, this is the Ontario Health Insurance Plan (OHIP).
Please let us know if you have private insurance coverage. We are not able to contact insurance companies to ask about coverage.
• Ask your insurance company if you have semi-private or private room coverage. If your insurance does not cover the total cost of the room you have selected, you need to pay the difference. Specific room types are subject to availability.
• If you are on maternity leave and are the primary holder of the insurance policy, ask your insurance company if you have coverage while on leave.
We do not bill travel insurance companies for charges. You will need to pay these charges directly to the hospital and request payment from your insurance company. Government health insurance plans pay for services that are medically necessary and pay for standard ward rooms.
The following are not covered by government insurance:
• Semi-private and private rooms
• Ambulance transfer services
• Orthopaedic equipment and other assistive devices (e.g. crutches, canes, walkers, collars)
• Specialized intraocular lens for cataract surgery
• Chronic Care / Alternative Level of Care (ALC) co-payment
• The Deluxe Private Birthing Suite with jacuzzi for maternity patients
If you do not have valid federal and provincial government insurance coverage, you will pay for all charges during your stay. This includes standard room fees, physician fees, and diagnostic exams or tests. If you do not have insurance coverage, you will be asked to sign a guarantee of
payment agreement. Payments can be made by cash, cheque, debit, Visa, Mastercard or American Express. You can also pay online by selecting “Michael Garron Hospital” or “Toronto East Health Network” through your online banking service.
What is a Substitute Decision-Maker (SDM)?
A SDM is someone who is legally able to make healthcare decisions on your behalf. This is only if you are not able to make them for yourself. You automatically have an SDM if you live in Ontario.
Who is my SDM?

• By law, your SDM is your closest living relative(s) by blood or marriage, unless you legally appoint a SDM.
• Please see the chart on the right to determine who your SDM is.
• If you have appointed an Attorney for Personal Care, this person(s) will be your SDM.
Why would I appoint an Attorney for Personal Care?
• You want to choose someone other than your automatic SDM.
• You want a specific person (or people) to act as your SDM(s).
• You have multiple people at the same level in the hierarchy (for example, multiple children, siblings, etc.) and you want only one or a few to act as your SDM(s).
• You want to choose a specific order or choose a backup SDM. For example, you may want your spouse first but a close friend as a second/backup Power of Attorney (POA).
Why are you asking about my SDM if I can make my own decisions?
We want to make sure we have your correct SDM on file. This is part of keeping a correct record of your healthcare. The people asking you to confirm your SDM do not ask you because they know something scary about your health that you don’t know about. Your SDM will not be contacted or asked to make healthcare decisions unless you are unable to
make them for yourself. Examples could be if you are in surgery, or if you are on medications that affect your ability to think clearly. Your SDM may also have to make decisions in life-threatening or emergency situations. It’s important that your SDM knows what’s important to you and how you make your healthcare decisions.
What’s the difference between an SDM and an alternate contact?
The alternate contact is not a decision-maker. This person cannot legally make healthcare decisions for you. This might be a friend or family member who is not your SDM. This person may be able to help reach your SDM, especially in cases when your SDM is out of town. Your alternate contact may be someone who helps you get to medical appointments or knows another way of reaching you or your SDM.
At MGH, we know that the support of family and friends (chosen by the patient) is an essential part of the healing process. We are committed to growing our culture of patient- and family-centered care, where friends and family members are seen as essential care partners who are key players in the quality, safety and experience of patient care. In November 2020, MGH launched a Care Partners Program to formally recognize the role of family caregivers. A Care Partner is someone that a patient chooses to support their care. The Care Partner role will vary depending on the patient’s needs and may include:
• Communicating with the healthcare team and helping them better understand the patient’s needs and preferences.
• Helping to relieve stress and anxiety.
• Helping patients with their daily activities, such as eating and drinking, going to the washroom or getting up out of bed.
• Working with the team to create the patient’s care plan. If you are interested in becoming a Care Partner or want to know more information about the program, please speak to the clinical team or contact Patient Experience (416-469-6096; PatientExperience@tehn.ca).
Keeping patients safe is a priority for everyone at the hospital. We want you and your family to be an active member of your own healthcare team. You can do this by asking questions when you do not understand information that is shared with you and speaking up if you have questions. This section provides you with information on how to stay safe while in the hospital. During your stay, if you develop unexpected diarrhea or respiratory symptoms, notify your care team immediately. If your family members or visitors report active diarrhea, vomiting, a new rash, or respiratory symptoms (cough, fever, sore throat, runny nose), they should go home and visit only when symptoms have resolved.
Seasonal respiratory viruses are easily spread through coughing and sneezing. One highly infectious seasonal virus is the flu (influenza). Symptoms of the flu can include fever, chills, cough, sneezing, runny nose, headache, body aches and weakness. The flu can be spread by breathing in droplets that have been coughed or sneezed into the air by a person who has the flu. The flu virus can live on surfaces (e.g. doorknobs, chairs, tables) for several hours. You can get the flu if you touch contaminated surfaces, and then touch your eyes, mouth and nose.
Here’s what you can do to help prevent the spread of the flu
• Get your flu vaccine. This is one of the best ways to protect yourself from the flu.
• Do not visit the hospital if you are feeling sick.
• Clean your hands often. You can use soap and water, or alcoholbased hand rub.
Some of our providers may wear a mask when they are treating patients. Please do not be alarmed. They are doing their part to help prevent the spread of respiratory viruses.
In the event of an outbreak of an infectious disease, hospital staff will work with Toronto Public Health to stop its spread in the hospital. Should an outbreak be declared, steps are taken to keep patients, visitors, staff and volunteers safe. MGH may limit visiting in some areas/units if there is an outbreak. During an outbreak, MGH will share information with patients, families and visitors. We will tell you when the outbreak is over, and when the control measures are lifted.
What can you do to prevent a fall in the hospital?
• Know what you can and cannot do.
• Listen to staff members who will tell you if it is safe to get in and out of bed or off the toilet by yourself.

• Do not climb over the bed rails or the end of the bed. Call staff for help.
• Wear flat, supportive shoes with non-skid soles when you are walking or getting in and out of a bed or a chair.
• Turn the lights on before getting up, especially at night.
• Use the aids or devices you need when moving about (e.g. glasses, hearing aids, walkers and canes).
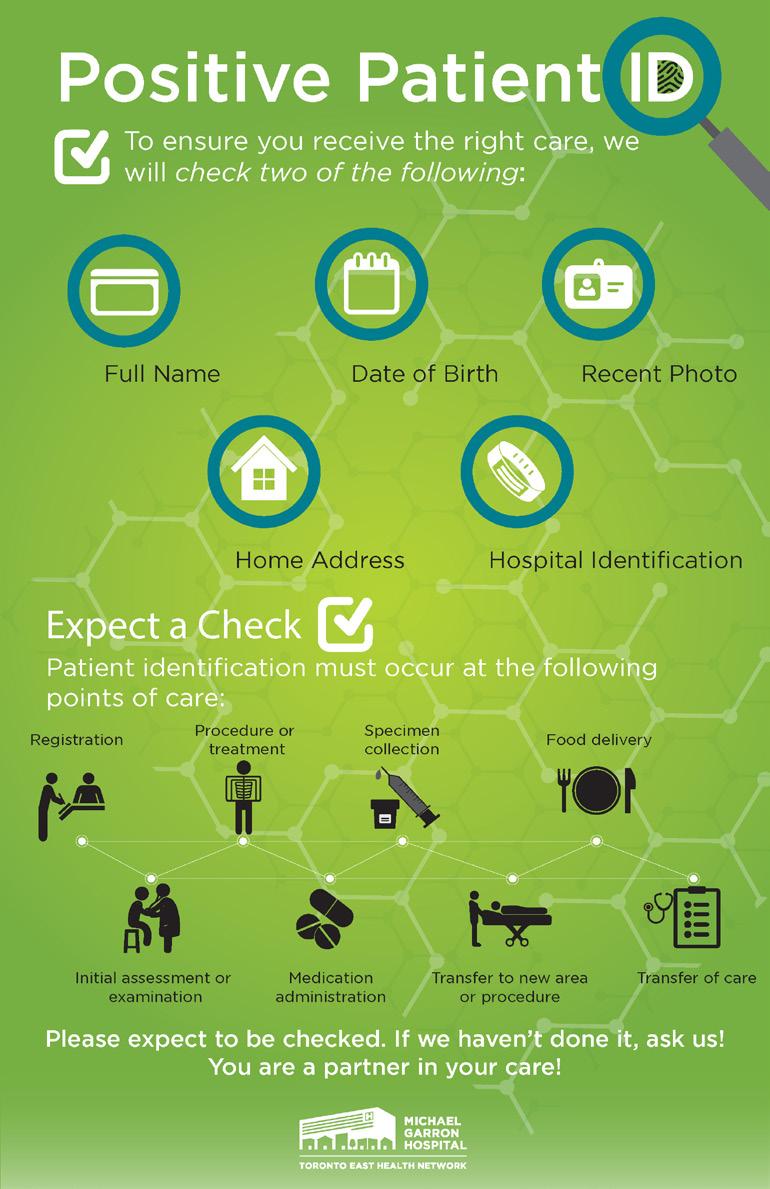
• Hospital staff and physicians will check your identity before providing you with care, a service or a procedure. Examples include:
• When filling out paperwork
• When you get medication
• Before a blood sample
• Before treatment
• Before an x-ray
• To check your identity, staff need two of the following:
• Full name
• Home address
• Birth date
• Approved photo
• Health card number
• Staff must check your identity before every care interaction. This means you will be checked multiple times a day, even if you are familiar with your care team and/or have been at the hospital for a while.
• You should expect a check. Ask us if you are not sure if your provider has checked your identity. Remember, you are a partner in your care.
Your care team needs to know the medications you are taking. This will help them give you the best medication for your situation. You should keep an updated list of all the medications you take and any allergies you have. You can keep this list on your fridge or in your wallet. This list should include:
• All your medications, including prescription and non-prescription drugs, supplements, vitamins and herbal remedies.
• Information about your medications, including the name, the dose, the reasons for taking it and the doctor that prescribed it.
• Any allergic or bad reactions you have to medicine or food.
• Pharmacy information.
• Here is an example of a Medication List:
Medication Name and Strength
Lipitor 10 mg
Vitamin D 1000 IU
Allergies: Advil – caused rash
Medication Instructions (how much and how often)
Take 1 tablet by mouth once a day
Take 1 tablet by mouth once a day
Reason for Taking Medication Doctor that prescribed
Here is a template for a Medication List you can use for your medications.
Medication Name and Strength
Medication Instructions Reason for Taking Medication
Doctor that Prescribed Medication
Allergies and Reactions
Pharmacy name and phone number
• If possible, bring your medications in their original containers when you come to the hospital.
• The medications you need while in the hospital will be given to you by the hospital. Do not take your own medications unless the healthcare team has told you to do so.
You may get prescriptions for new medications, or you may be told to change or stop taking your medications from home. Make sure you understand any changes:
• Ask why you were given new medications.
• Ask how you are supposed to take your new medications.
• Ask how long you are supposed to take your new medications.
• Ask if you think you are missing a medication.
• Ask how you will know if your medication is working.
• Ask about the side effects of your medications. When you are back at home, update your Medication List.
• If you have any questions regarding your medications at any point during your stay, you may request a consultation from the pharmacist on your unit.
A person has a greater risk of getting a blood clot once they have been admitted to the hospital. Deep vein thrombosis (DVT) is a clot that forms in the deep veins of the body, often in the legs because it is harder to maintain blood flow in the lower body. A blood clot may break off and move through the bloodstream, getting stuck in the lungs. This is called a pulmonary embolism and can be life-threatening.
There are many factors that increase blood clot risk. Some examples are reduced mobility, surgery or trauma; increased estrogen (e.g. pregnancy, birth control); medical conditions (e.g. cancer); previous blood clot history; family history of blood clots; smoking; obesity; and older age. Ask your doctor or provider if you are at risk for blood clots.
During your hospital stay, you may be given an injection medication in your abdomen to prevent blood clots. This is usually only needed while you are in the hospital and should not continue after discharge unless told by your care team.
Know the symptoms of a blood clot
The symptoms of DVT are usually in the leg, but may also be in the foot, ankle, calf, whole leg or arm. Symptoms include pain, swelling, skin discolouration (blue, purple or red) and warmth.
Pulmonary embolism symptoms include shortness of breath, chest pain, cough and a very fast heart rate. Tell your care team right away if you have any of these symptoms.
Antibiotics can be used to treat infections caused by bacteria. They are a common medication but there are still risks to taking antibiotics. If you need antibiotics, your care team will make sure they are used properly. If antibiotics are not used properly, it can lead to side effects, antibiotic resistance and put you at an increased risk of other serious infections. An example is Clostridium difficile infection (also called C. difficile or C. diff). If you have questions about our approach to antibiotics, you can speak to the pharmacist on your unit. You can also email the antimicrobial stewardship pharmacist at aspinfo@tehn.ca.
What is a pressure injury?
Pressure injuries are sores on the skin (also called bedsores). They can
happen when you are lying in bed in one position for a long time. They usually happen over bony areas such as the hips, ankles, heels and tailbone. They can also happen over the bridge of the nose or top of the ears when a patient is wearing an oxygen mask for long periods.
You can help with bedsores by:
• Changing your position every two hours during the day, and every four hours at night. Patients in wheelchairs need to shift their weight every 15 minutes or change their position every hour.
• If you are unable to move, let your care team know that you need to move to a new position.
• Staying away from things that could harm the skin, like hot water and harsh soaps.
• Using a moisture cream to keep your skin hydrated.
• Eating well and drinking at least 1.5 litres of liquid per day.
You may hear “Code Red” announced on the overhead system. It is used when a fire alarm has been activated, there is fire or smoke, or if there is a fire drill. Fire drills are done every month. Staff will tell you what to do and where to go. Fire exits are clearly marked in the hospital.
Disclosure
When you visit a health professional or hospital, you expect the safest healthcare available. Even in the best circumstances, the unexpected can happen. We call this an accident or adverse event. We take these safety issues very seriously.
Accidents or adverse events do not happen very often. When they do, we believe the patient and their representative should know about it. This process is called disclosure. We will share what happened, why it happened, and what we are doing to stop a similar event from happening again.
If there is an adverse event during your care, your care team will talk to you and, if you wish, your family, about what happened. You can also talk to your care team about any changes to your care plan that may be needed because of the event.
When there is an adverse event, we take steps to stop it from happening
again. The care team will investigate what went wrong. You will be told about what we’re doing to stop the same thing from happening to someone else.
We will keep you up-to-date with the investigation. If you wish, we can set up a meeting to tell you about what changes we’ve made to try to stop the same event from happening again.
We will answer all of your questions honestly and openly.
Our Protection Services staff are highly trained and dedicated to the safety of patients, visitors and staff. To report an incident, contact Protection Services at 416- 469-6016 (ext. 6016 on internal phones), 24 hours a day, seven days a week.
All staff, physicians and volunteers at MGH wear a hospital identification badge, which includes their name, department and picture.
If you are unsure about any person with whom you are interacting with, the hospital encourages you to ask for identification, or if necessary, call a nurse for assistance.
Everyone’s safety and security is our number one priority.
Violence Prevention
• For the protection of everyone, we have a Zero Tolerance Policy for any and all forms of abuse.
• Our hospital has the right to ask patients and visitors to leave, or to take legal action, if we feel our violence prevention policy has been violated.
• If you experience any form of abuse, please speak with your care provider, supervisor or manager of the department right away.
Crime Prevention
• Protection Services monitors all areas of the hospital, including the hospital parking areas and the hospital exterior.
• To ensure everyone’s safety, Protection Services staff ensures all hospital policies are observed and criminal activity on hospital property is prevented.
• Everyone’s safety and security is our number one priority.
During your stay at MGH, please do not bring valuables to the hospital. Examples of valuables include cash, credit cards and expensive jewelry.
If you come to MGH with valuables, please ask your family and friends to take them home. If this is not possible, please let your care team know. They can arrange for Protection Services to pick up and hold the items. Items will be recorded and stored in a safe. You will get a receipt.
To get items from the safe when you leave, call Protection Services at ext. 6016. You will need to give them your receipt.
To keep personal belongings safe, we recommend that patients, caregivers or family members:
• Label items whenever possible.
• Check with your denture provider about the options available for labeling dentures.
• Bring an appropriate storage container for belongings and ensure it can be accessed daily.
• Never leave dentures, hearing aids, glasses or phones on the meal tray.
• Check the tray table, bedside table and patient locker for belongings when transferring rooms or being discharged home.
• Ask staff to return any medications brought to hospital.
If you have lost your belongings while at the hospital, we will do our best to help locate them. Please report the missing items to the unit/ area manager immediately. If you have already left the hospital, please contact Patient Experience to coordinate a search.

MGH is committed to protecting the privacy and personal health information of our patients.
During your hospital stay, if you do not want anyone to know you are at MGH, please let your healthcare team know and we will put a confidentiality flag beside your name in our computer system. Then, if anyone asks about you (including family and friends calling or arriving to visit), they will be told that we do not have any information about you. Otherwise, if someone does call to inquire about you, we will tell them you are staying in our hospital; however, we will not release any details about your visit, health or personal information.
Please speak to your nurse if you would like your confidentiality status changed. For more information about privacy rights related to your personal health information, please ask your care provider for a copy of our privacy pamphlet. Michael Garron Hospital Foundation raises money to enhance the hospital’s programs and services. The Foundation may write to you when they are raising money or send you mailings about their services or upcoming special events. If you do not wish to be contacted by the Foundation, please let us know by contacting the Privacy Office.
If you need more information about how the hospital protects the privacy of your information, or if you have questions regarding our practices, contact: Privacy Officer 416-469-6580 ext. 7781 (ext. 7781 on internal phones) or privacy@tehn.ca.
No photography, video recording or audio recording is permitted on hospital property without expressed permission. This is to ensure the privacy and confidentiality rights of patients, physicians, staff, volunteers, and other members of the public, including patients and visitors, are protected. Please speak with your care provider to obtain appropriate permission. If following a discussion with the care provider you have any further questions, please, contact the hospital’s Privacy Office.
Too much noise in hospitals can have harmful effects, such as:
• Interrupting needed rest and sleep.
• Making your heart beat faster and harder.
• Slowing down wound healing.
• Changing the way you deal with everyday worries.
We want to reduce noise so you can get the rest you need during your hospital stay.
• Most inpatient areas have a special Quiet Time when staff make an extra effort to lower noise so you can get the rest you need.
• We encourage you to use earphones to enjoy your TV and music.
• You will always get the care you need. Your care providers will check on you as usual but will not wake you up unless it is important.
Family members or visitors reporting active diarrhea, vomiting, a new rash or respiratory symptoms (cough, fever, sore throat, runny nose), visit only when symptoms are resolved.
• The healthcare team will work with the patient to decide the number of visitors welcomed at a time. The size of the patient’s room, and whether it is a shared room, may limit the number of visitors at one time. Please check with your loved one’s healthcare team to learn about special guidelines for that unit.
• Clean your hands with soap and water or alcohol-based hand sanitizer:
• Before you go into a patient’s room.
• After you leave a patient’s room.
• Before and after touching and/or feeding your loved one.
• After assisting your loved one with toileting activities (do not dispose of incontinent pads/briefs in the patient’s garbage).
• Please do not use the bathroom in the patient’s room. Staff can tell you where to find the nearest public washroom.
• Please do not leave any leftover food in the patient’s room. Patient rooms are not able to safely store or heat perishable food items, which may lead to food related illness.
• Children aged 12 and under are welcome to visit if they are with an adult who is not the patient.
• Please enter through the Emergency Department if you are visiting between 11 p.m. and 6 a.m. Staff will give you a “family” sticker.
• Please talk to the healthcare team if you would like to bring your family pet (cat or dog) to visit.
• If you would like to set up a video visit, please email PatientExperience@tehn.ca.
Please speak to the supervisor or manager of the unit/department if you have questions or concerns about visiting.
At MGH, our top priority is keeping patients, visitors, staff and volunteers safe and healthy. Everyone has a role in keeping the hospital safe and healthy.
Please do not visit if you have any of these symptoms:
• Fever or chills.
• Nausea, vomiting and/or diarrhea.
• Cough, sore throat, runny or stuffy nose.
• An eye infection (such as pink eye).
• A new or unexplained rash.
• Any other symptom that might be infectious.
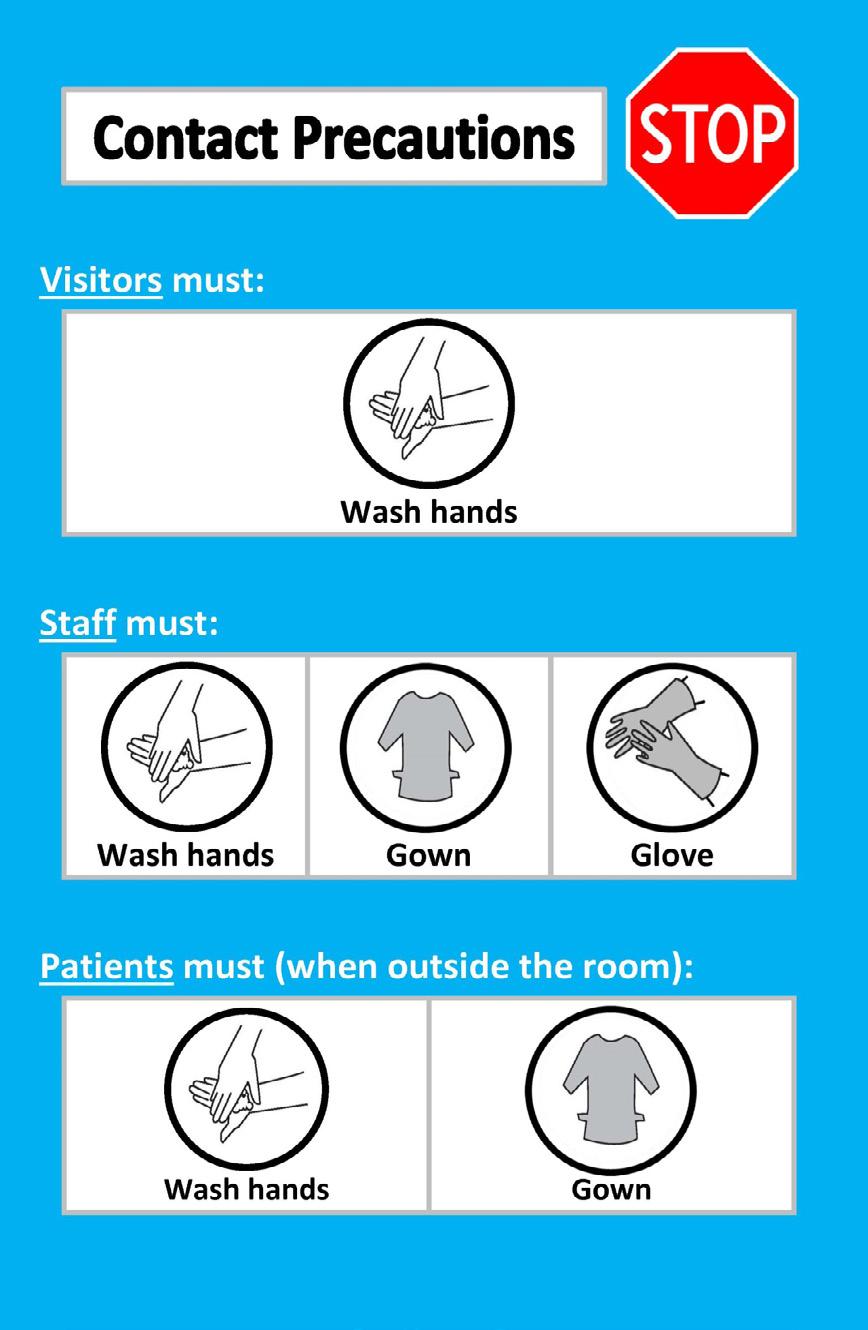
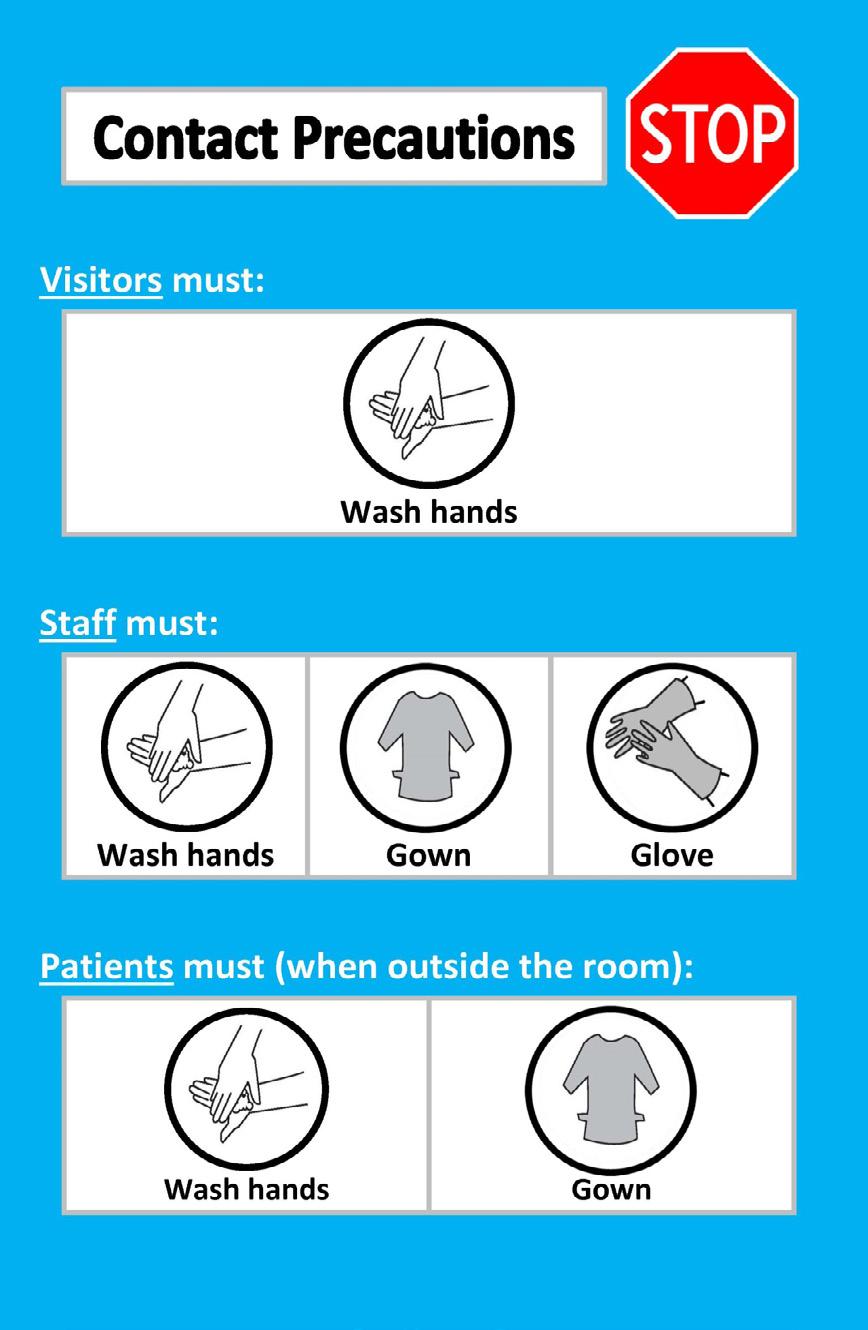
Patients with symptoms of an infectious illness are separated from other patients. Anyone seeing these patients needs to wear special protection. A sign is put on the room door to let people know what type of protection is needed. You may need to wear a mask, gown or gloves to keep yourself and the patient safe. An example of an additional precaution sign you may see at the hospital can be seen on page 30. If you are visiting a loved one who requires additional precautions, you must follow the directions on the sign. These directions will keep you and others safe during and after the visit. Please ask a nurse if you do not understand the directions on the sign.
Cleaning or washing your hands is the best way to stop the spread of germs. In hospitals, alcohol-based hand rub (also called hand sanitizer) is the best way to clean your hands when they are not visibly dirty. Hand sanitizer is faster than soap and water, is found throughout the hospital, and has moisturizers that help your hands from getting dry and chapped.
While at the hospital, you must clean your hands:
• When you come into the hospital.
• Before you go into the patient’s room.
• Before you eat or drink.
• When you leave the patient’s room.
• When you leave the hospital.

Add 1-2 pumps of sanitizer to dry hands.

Rub the fingertips of each hand in the palm of the other hand.
Rub hands together, with palms facing each other.
Rub each thumb with the opposite hand.
Rub in between and around fingers.
Rub hands until dry. Do not use paper towel.
Rub the back of each hand with the palm of the other hand.
Hands are clean once they are dry. This will take about 15 seconds.
Plants and flowers are cheerful gifts for patients, but soil and plants have bacteria. These items may not be healthy for patients who are recovering. Plants and flowers are not allowed in critical care areas of the hospital, including:
• Neonatal Intensive Care Unit (NICU)
• Intensive Care Unit (ICU)
• Cardiac Integrated Unit (CIU)
• High-risk patients (for example, those in Oncology and who require long term ventilation)
The hospital is a fragrance-free building. Some people may have scent sensitivities or allergies. Please do not wear perfumes, colognes and scented creams.
The hospital is a smoke-free building. There is no smoking or using e-cigarettes both inside and outside. Outside includes the grounds of the hospital, driveways and parking lots.
We know that preparing for discharge, either to your home or to another facility, can feel confusing and overwhelming, especially at the beginning of your care journey. Your care team will work with you, your family and/or your caregiver(s) to provide the best plan possible for your safe transition from hospital.
How does discharge work at Michael Garron Hospital?
After you are admitted to the hospital, your healthcare team will work with you to determine your care goals and plan for the day when you will leave the hospital.
This is called your day of discharge. You are considered ready for discharge when your health care team determines that you no longer need medical care at the hospital.
Conversations about your discharge will take place soon after you are admitted. Knowing when you will leave the hospital can help you, your family and your caregiver(s) plan ahead and explore your options. Your healthcare team can also arrange any follow-up care you may need in time for when you leave the hospital.
You might be transferred to a different unit or another site or hospital during your stay. This depends on your needs and where you can best receive the care you require. Your healthcare team will keep you informed of any possible transfers. No matter which unit, site, or hospital you are transferred to, they will always help you prepare to leave the hospital.
Most patients will go home from the hospital. This is called the homefirst approach. If your healthcare team identifies that you require home care supports to assist with your transition home, they will ask for your consent to submit a referral to Ontario Health atHome or other services you are eligible for. Representatives from these organizations may contact you by phone or in-person, depending on your situation. Ask your healthcare team for more information.
What do I need to do to prepare for discharge home?
Once you know your day of discharge, you need to arrange your own transportation home. If you need help, ask your healthcare team for a list of phone numbers for travel options, such as an ambulance, taxi or wheelchair-accessible taxi. Please note MGH does not pay for your transportation to leave the hospital.
What if I am being discharged to another location before I go home?
Depending on the reason for your hospital admission, you may require additional care from another type of facility before you are ready to go home. Your healthcare team will work with you to decide what type of facility can best provide the care you need. A care site could include:
• Inpatient rehabilitation
• A reactivation care centre
• A transitional care unit
• Complex continuing care
• Convalescent care
• A retirement home
• Supportive housing
• Palliative care
• A hospital in your local community
If you are eligible for one or more of these care sites, your healthcare team will help you apply to and transfer there.
What happens if I need long-term care?
Before referring to long-term care, your healthcare team will work with you and your caregivers to ensure all services and supports in the community are explored to support you in your home. Once every option has been reviewed, a Care Coordinator from Ontario Health atHome will be required to confirm that your care needs cannot be supported in the community before assessing your eligibility for long-term care. If you are eligible, the Care Coordinator will work with you to start your long-term care application or update an existing application as applicable. This may result in waiting at home for long-term care and sometimes placement in a long-term care home where you will wait until a space becomes available in your preferred home. If you have questions about this, please ask your healthcare team about the First Bed Policy.
Can I wait in the hospital for a long-term care home?
Hospitals are not designed to meet a person’s supportive or rehabilitative needs. There is evidence that while you wait in the hospital, in an unfamiliar environment without the social and recreational supports of the community, you could be at risk for physical and cognitive decline. You may also be at risk for hospital-based infections. Therefore, the majority of patients will not wait in hospital for long-term care. Rather,
your care team will explore all available options to try and support your care needs while you wait for long-term care at home.
Who do I contact if I have questions about leaving the hospital? Speak with any member of your care team. They are here to support you.
You should receive instructions for new medications (with prescriptions), what is changed, what medications to stop and what to continue. Depending on the unit you are discharged from, this is provided using the Medication Discharge Summary or the Patient Oriented Discharge Form.
You or your family may ask the care team to fax the prescriptions to your own pharmacy if you have the Fax number. Other local pharmacies are available inside (see retailer section at the end of this book) and just outside of the hospital. It is recommended that you fill all medications at a single preferred pharmacy and update your medication lists with any changes after your discharge.
If you and/or your family are worried about going home, please talk to your healthcare team early on in your stay. Your family can use the whiteboard in your room to write down any questions.
Ontario Health atHome and other community support services agencies may be able to offer some support if you need help at home. Many services that used to only be offered in hospitals are now provided in the community. These services will need to be coordinated with your care team.
When you leave the hospital, you may go home, or you may go to another facility.
If you are going to another facility, we will help with this planning. To help us plan the best place for you to be, we may need to talk with you and your family member/substitute decision-maker each day you are in the hospital.
If you need to wait for a bed in another facility, we will do our best to get you support so you can wait at home. If you are approved to stay in the hospital while you are waiting for long-term care or Complex Continuing Care, you will need to pay a co-payment fee. The cost is set by the
Ontario Ministry of Health. We know that you and your family will need to make many choices before you leave the hospital. Your healthcare team is here to support you in making the healthcare choices that are best for you.
Ontario Health atHome: 310-2222 (no area code required)
Toronto Seniors Helpline: 1-877-621-2077
To pay your bill, please visit the Business Office on the first floor, G-Zone beside the food court. The Business Office hours are Monday to Friday, from 8 a.m. to 4 p.m. We accept credit card, cheque and debit card payments.

For help finding social services, financial assistance programs or community supports. Need
Your local pharmacy
If you have a family doctor or nurse practitioner, contact them first. They may offer afterhours care for their patients.

If you have a family doctor or nurse practitioner, contact them first. They may offer afterhours care for their patients.
Pharmacists in Ontario can now treat and prescribe medications for 19 minor health concerns, including pink eye, tick bites, urinary tract infections (UTIs), acne and more. Visit ontario.ca/pages/pharmacies to learn more.
Your local pharmacy
Health Access Taylor-Massey (4 The Market Place)
Pharmacists in Ontario can now treat and prescribe medications for 19 minor health concerns, including pink eye, tick bites, urinary tract infections (UTIs), acne and more. Visit ontario.ca/pages/pharmacies to learn more.
Visit or call Health Access Taylor Massey to talk to a resource navigator. This is a healthcare professional who can help connect you with the services you need in the health, social and community services systems. Visit ethp.ca/HATM to learn more.
Health Access Taylor-Massey (4 The Market Place)
Health Access Thorncliffe Park (45 Overlea Blvd.)
Use this resource to find seniors and caregiver services, mental health (wellness) services, newcomer supports and more! In
Visit or call Health Access Thorncliffe Park for health and wellness services and other resources. Services are free and open to people who live in the M4H postal code. Visit fhc-chc.com/health-access-thorncliffe-park to learn more.
Visit or call Health Access Taylor Massey to talk to a resource navigator. This is a healthcare professional who can help connect you with the services you need in the health, social and community services systems. Visit ethp.ca/HATM to learn more.
Use this resource to find seniors and caregiver services, mental health (wellness) services, newcomer supports and more!
A great place to start if you are looking for health, social and community services in East Toronto.

Available 24/7 in different languages! By phone
A great place to start if you are looking for health, social and community services in East Toronto.

Talk to a healthcare professional who can give you advice or help you find a family doctor, nurse practitioner or other service provider.
Available 24/7 in different languages!
Talk to a healthcare professional who can give you advice or help you find a family doctor, nurse practitioner or other service provider.
If you or someone you know is experiencing a health or wellness emergency, please call 9-1-1 or go to your nearest hospital emergency department.
If you or someone you know is experiencing a health or wellness emergency, please call 9-1-1 or go to your nearest hospital emergency department.

If you have questions about your health records while in the hospital, please ask your healthcare provider.
The Health Records Department is located on the main floor, G-Zone, room G1-220.1. It is open Monday to Friday, from 9 a.m. to 5 p.m.
If you would like to receive a copy of your health record following your discharge, you will be required to complete a Request Access to Personal Health Records form and present valid photo identification that includes your signature. You can find the necessary form on our website, and once completed, you can email the form to roirecords@tehn.ca for processing. There is a fee associated with this service.
Your family doctor will automatically receive copies of your medical reports at no cost to you unless you have specified during the registration process that you do not want to send the copies to them.
Please note: If your family doctor requests a copy of your medical reports and they are not listed as your doctor in the hospital system, we will not be able to provide a copy. Please check with your healthcare provider to make sure your family doctor’s information is correct on your medical record. If your doctor’s name is incorrect or missing, please call Patient Registration at 416-469-6381 to have your records updated.
MyChart is a secure website that allows you to access your health records 24 hours a day, seven days a week, anywhere in the world. With MyChart access, you can:
• View your health records, such as test results, medications and other medical information.
• Share your records with your family members, caregivers and other loved ones.
• View your upcoming appointments.
• Create appointment reminders.
To sign up for MyChart, you have two options:
• Please visit our Health Records Department in room G2-220.1
• Complete the My Chart registration form available on our hospital website and email the form to roirecords@tehn.ca. Once your request is processed, the health records team will email you a unique user code that you can use to sign up for MyChart.
Bank machines can be found beside the business office and in the Thomson Centre.
Fresh arrangements of flowers are available in the hospital’s gift shop- The General Store, located in the Coxwell Lobby. Flowers can be delivered by volunteers directly to a patient’s room by dialing ext. 6050 on internal phones. Plants and flowers are not allowed in critical care areas of the hospital.
Located in the Coxwell Lobby.
Open weekdays from 9 a.m. to 6 p.m. and Saturdays from 9 a.m. to 4 p.m. In the shop, you can find snacks, beverages, gift items, books, stuffed animals, cards and much more.
For our non-English speaking patients, an interpretation service is available 24 hours a day, seven days a week. Please ask your care provider about the service. Learn more at tehn.ca/interpretation.
Operating hours may be subject to change.
• Located at 840 Coxwell Ave. (across the street from the hospital)
• Weekdays: 7 a.m. to 4 p.m.
Oriental Chopsticks
• Located in the Moez & Marissa Kassam Food Court on M1
• Weekdays: 10 a.m. to 8 p.m.
• Weekends: 10 a.m. to 6 p.m.
JK Pizza
• Located in the Moez & Marissa Kassam Food Court on M1
• Weekdays: 7 a.m. to 6 p.m.
Pharmasave Pharmacy
• Located on the 1st floor, G-Zone
• Weekdays: 8 a.m. to 7:30 p.m.
• Saturdays: 9 a.m. to 5 p.m.
• Sundays: 10 a.m. to 5 p.m.
Subway
• Located in the Moez & Marissa Kassam Food Court on G1
• Weekdays: 8 a.m. to 11 p.m.
• Weekends: 9 a.m. to 9 p.m.
Tim Hortons
• Located in the Moez & Marissa Kassam Food Court on M1
• Monday to Sunday: 8 a.m. to 9 p.m.
U-naru Sushi
• Located in the Moez & Marissa Kassam Food Court on M1
• Weekdays: 10 a.m. to 7 p.m.
Vending Machines
Vending machines are located in the following locations:
• Moez & Marissa Kassam Food Court on M1
• Elevator waiting area on T2
• Coxwell Lobby on A2
• Maternal, Newborn and Child Health Services’ reception area on J7

































