COUNTING THE MINUTES
CARE
RESHAPING AGED CARE IN AN AGE OF INCREASING DIVERSITY
DESIGNING THE AGED CARE ACCOMMODATION OF THE FUTURE HOW HARMFUL GUT BACTERIA TRIGGER ALZHEIMER’S



FROM THE EDITOR
Welcome to the August issue of Aged Health magazine — which features allied health and wound care. Australians in aged care are currently receiving eight minutes of allied health care per day, on average. However, the Final Report of the Royal Commission into Aged Care Quality and Safety recommended that this amount be raised to 22 minutes per day, in order to bring Australia into line with international standards. However, as Terry Haines points out, a model developed by the Australian Council of Deans of Health Sciences found that in order to achieve this goal, Australia would need to train an additional 25,000 allied health professionals. Turn to page six to find out more.
Scientists from Monash University have identified a key step in the wound healing process that becomes disabled as a person ages. The article on page 14 takes a closer look at the study that was conducted, and what it means for the treatment of wounds affecting older people.
Other topics explored in this issue of the magazine include diversity in aged care, designing the aged care accommodation of the future, the role that harmful gut bacteria have to play in triggering Alzheimer’s disease and how dementia could be predicted nine years before an official diagnosis.
As always, I hope you enjoy the issue.
Amy Steed Editor ah@wfmedia.com.au
CONTRIBUTORS


Phillips CEO of Peninsula Home Hospice


Janet
Cath Scarth CEO of AMES Australia
Samantha Fuller General Manager at Service Works Global
Professor Terry Haines AM Chair of the ACDHS Board











CONTENTS

Counting the minutes on allied
Using software for safety compliance in residential care
Key step uncovered in the wound healing process
How harmful gut bacteria trigger
Lowering the risk of a fall on psychotropic drugs
Reshaping aged care in an age of increasing diversity
In conversation with
ACIPC International Conference speakers announced
Predicting dementia nine years
Why women need to get active



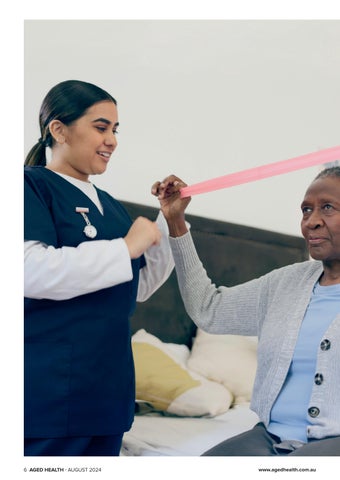
COUNTING THE MINUTES ON ALLIED HEALTH CARE
At the end of 2023, the Australian Council of Deans of Health Sciences launched a model that it had commissioned — designed to allow policymakers to see how different policy settings would affect the numbers of allied health workers needed in Australia over the coming years.
Currently, Australians receiving aged care are, on average, only obtaining eight minutes of allied health care per day. The Final Report of the Royal Commission into Aged Care Quality and Safety recommended that be raised to 22 minutes a day to bring Australia in line with international standards.
However, the ACDHS model found that in order to achieve 22 minutes a day by 2033, Australia would need to train another 25,000 allied health professionals. Due to the high demand, obstacles to supply and the overall time required to increase the number of fully qualified allied health professionals, the training would have needed to start when the model was first released.
By the time this article has been published, we will already be eight months behind that timeline. >>

And that was just to meet the international benchmark cited by the Royal Commission report. If Australia decided that its older people deserved better care — say, for instance, 30 minutes a day of allied health care — then another 38,000 trained professionals would be required in order for this to be successfully delivered.
Allied healthcare professionals include occupational therapists, psychologists, nutritionists, pharmacists and speech pathologists, who help maintain the good health of older Australians. Without this care, these Australians are more likely to end up in hospital, where beds are already scarce and staff stretched. Preventative care is good for individuals and good for the whole healthcare system.
The ACDHS model found that there are other ways to ensure there are enough allied health workers to meet the international benchmark. Increasing pay for allied health workers could, for instance, increase retention in professions with high attrition rates. Similarly, making studying these professions more affordable could make them attractive to a greater number of students.
The ACDHS has been advocating that the Commonwealth Prac Payment scheme, which helps students studying nursing, teaching and social work to afford to complete the practical element of their training, be extended to allied health professionals.
THE ACDHS MODEL FOUND THAT IN ORDER TO ACHIEVE 22 MINUTES A DAY BY 2033, AUSTRALIA WOULD NEED TO TRAIN ANOTHER 25,000 ALLIED HEALTH PROFESSIONALS.
However, eight months after the model demonstrated the challenge, the government is yet to declare whether it backs the international benchmark of 22 minutes or whether it is content to let Australians in aged care make do with the eight minutes the Royal Commission found to be inadequate.
If it still wants to work towards the Royal Commission target of improving care, the government will need to commit to one of the solutions proposed by the ACDHS — or otherwise back further research to understand what level of allied health in aged care is adequate to deliver care to residents and prevent an undue burden on the wider health system.
If the government does nothing, one might assume that it tacitly endorses a target which falls short of international best practice. In that case, it is over to Australians to declare whether or not they believe that target is good enough for their loved ones — and indeed themselves — in old age.

Professor Terry Haines is Head of the School of Primary and Allied Health Care at Monash University, overseeing five departments, 150+ staff and 180+ research higher degree students. With a background in physiotherapy and health economics, he has over 15 years of research experience in health services. He is a founding investigator of the National Centre for Healthy Ageing and has led groundbreaking trials in falls prevention in hospitals and developed innovative research trial methodologies. Professor Haines has over 400 published works and received over $80 million in research funding. He has received multiple awards for his leadership and contributions to health research and education.
USING SOFTWARE FOR SAFETY COMPLIANCE IN RESIDENTIAL CARE

Many aged care providers rely on spreadsheets, notebooks and informal knowledge for their dayto-day operations. The lack of centralised data can cause lost, deleted or out-of-date information. This complicates and delays reporting and is a big threat to health and safety compliance, writes SAMANTHA FULLER, general manager at Service Works Global.
Indeed, a recent article by Aged Health warned of impending regulatory changes taking place within aged care, including stricter civil and criminal penalties for care settings that don’t comply with health and safety law.
The 2018 Royal Commission into aged care quality recommended a focus on transparency and modernisation. As a consequence, care settings around the globe are now implementing computerised maintenance management systems (CMMS) to automate their estates and support compliance. A push of a button can handle complex reporting, and software can be adapted to the needs of the care setting while remaining compliant.
MAINTENANCE
Asset management and lifecycle planning is a critical aspect of keeping aged care facilities operating safely and maintaining a comfortable, high-quality service environment as per the government’s Aged Care Quality Standards. It’s not enough to respond to issues and failures reactively; effective planned preventative maintenance (PPM) schedules need to be implemented. This regular maintenance ensures that assets work as they should, and can also extend their life, increase reliability and help facility teams manage their time better.
Mandatory reporting is enforced in NSW, with providers undertaking a comprehensive assessment of all assets and buildings. Data required includes long-term asset lifecycle plans, including maintenance and replacement, and a financial forecast that backs these schedules. CMMS software provides a great advantage
to reporting by highlighting the most cost-effective method of maintaining an asset and capturing maintenance costs across the life of each asset. Even for those not required to submit such reporting, this level of insight is essential to the smooth running of a facility.
The number of residential aged care providers decreased last year due to financial and regulatory pressures, while the need for access to accurate data for decision-making has increased.
COMPLIANCE
CMMS systems can automate the management of tests and inspections, creating job sheets and recording results to ensure complete auditability. Users can also import health and safety regulations for specialist supplier registers and professional bodies for easier management of aged care legislation.
The safety and wellbeing of residents can be improved through a comprehensive incident management process. Safety officers are promptly notified of incidents, facilitating immediate responses and subsequent analysis. By centralising incident data, care homes can identify trends, enhance safety measures, and minimise the likelihood of future preventable incidents. CMMS software can also reduce costs by enhancing efficiency.
THE FUTURE OF AGED CARE
The number of Australians receiving aged care is projected to increase by around 150% over the next 40 years. Insufficient funding puts further pressure on residential care and neglecting improvements may put certain sites at risk of failure and closure. Care settings that have implemented an agile approach with CMMS will be better placed to adapt to any future changes.
Using software that can create maintenance schedules and deliver accurate reports is essential in ensuring resident safety, maintaining compliance and saving costs.

Samantha Fuller is the general manager at Service Works Global.
DESIGN MATTERS
DESIGNING THE AGED CARE ACCOMMODATION OF THE FUTURE



Second prize, Urban Metro site


Architects and designers have been recognised by the federal government for their innovative aged care home designs.
The Reimagining Where We Live design ideas competition invited architects and designers to use the draft National Aged Care Design Principles and Guidelines to design innovative aged care homes that are welcoming, safe, accessible and dementiafriendly. Categories included Urban Metro and Regional Town.
“The design entries show what is possible when we think about aged care from a new perspective. I encourage providers to engage with and adopt the National Aged Care Design Principles and Guidelines, as recommended by the Aged Care Taskforce,” said Anika Wells, Minister for Aged Care.
“Through this design challenge, we’ve seen innovative ideas and accommodation solutions that will shape the future of aged care accommodation and support older people to live meaningful lives in safe, high-quality residential care when it is needed.”
The Principles and Guidelines have been developed in response to recommendation 45 of the Royal Commission into Aged Care Quality and Safety Final Report and were introduced on 1 July 2024.
Entries were judged by an eminent jury with diverse and extensive experience in architecture, design and aged care. The jury received valuable feedback on the shortlisted designs from six advisers who are living with dementia.
URBAN METRO SITE
• First prize : $50,000 – ‘Scales of care’ by LM2A with Super Natural, a design that explored the relationship between care and the environment in which it takes place.
• Second prize : $20,000 – ‘Connection, community and movement’ by Walter&Walter, which flipped the inward looking institutional model to an outward focused community model.
• Highly commended: ‘Reflection Home’ by CultivAR + Wild Studio, which adopted the increasingly popular small household model.
• Highly commended: ‘Canopy’ by Jacqueline Bartholomeusz, David Sutherland, Lorraine Calder and Oculus, which clustered living spaces to create a neighbourhood model with ‘get together’ spaces.
• Commended : ‘An ordinary life’ by T&Z Architects + Aspect Studios, which explored the concept of aged care as a continuum that binds generations together.
REGIONAL TOWN SITE
• First prize : $50,000 – ‘Manu Place’ by Monash Urban Lab with NMBW Architecture Studio, BoardGrove Architects, BLOXAS and Glas Landscape Architects, which featured central cloistered courtyards between private living spaces that featured natural light, air and greenery.
• Second prize : $20,000 – ‘All together now’ by Other Architects, Openwork, Andy Fergus and Alicia Pozniak, which created a miniature town with an intergenerational focus, featuring a community childcare cooperative.
• Highly commended: ‘The connected garden’ by Mark Boffa, Guruge Ruwani Dharmasiri, Pulasthi Wijekoon, Jana Osvald and Julie Ockerby, which recreated a classic Australian country town.
First prize, Urban Metro site
First prize, Urban Metro site


KEY STEP UNCOVERED IN THE

Sthis new research published in reveals a molecule involved in the healing of tissues that — when injected into animal models — leads to a drastic acceleration of wound closure, up to 2.5 times faster, and 1.6 times more muscle regeneration.
Lead researcher Associate Professor Mikaël Martino, from Monash University’s Australian Regenerative Medicine Institute (ARMI) in Melbourne, said the discovery “could transform regenerative medicine, because it sheds light on the crucial role of sensory neurons in orchestrating the repair and regeneration of tissues, offering promising implications for improving patient outcomes.”
“In adults with diabetes alone — where poor blood flow can lead to quickly worsening wounds that are often very slow or impossible to heal — the lifetime risk of developing a diabetic foot ulcer (DFU), the most common diabetesrelated wound, is 20 to 35% and this number is rising with increased longevity and medical complexity of people with diabetes,” said Dr Yen-Zhen Lu, co-lead author from ARMI.
Nociceptive sensory neurons, also called nociceptors, are the nerves in our body that sense pain. These neurons alert us to potentially damaging stimuli in tissues by detecting dangers like tissue damage, inflammation, extremes in temperature, and pressure.
The researchers discovered that — during the healing process — sensory neuron endings grow into injured skin and muscle tissues, communicating with immune cells through a neuropeptide called calcitonin gene-related peptide (CGRP).
“Remarkably, this neuropeptide acts on immune cells to control them, facilitating tissue healing after injury,” Martino said.
Importantly they found that sensory neurons are crucial to the dissemination of CGRP because they showed that the selective removal of sensory neurons in mice reduces CGRP and significantly impairs skin wound healing and muscle regeneration following injury.
When the scientists administered an engineered version of CGRP to mice with neuropathy similar to that seen in diabetic patients, it led to rapid wound healing and muscle regeneration.
According to Martino, these findings hold significant promise for regenerative medicine, particularly for the treatment of poorly-healing tissues and chronic wounds.
“By harnessing neuro-immune interactions, the team aims to develop innovative therapies that address one of the root causes of impaired tissue healing, offering hope to millions,” he said.
“This study has uncovered significant implications for advancing our understanding of the tissue healing process after acute injury. Harnessing the potential of this neuro-immuno-regenerative axis opens new avenues for effective therapies, whether as standalone treatments or in combination with existing therapeutic approaches.”
Breathe easy

Freestyle Comfort
Expand your comfort zone with this innovative and powerful design: Compact and Lightweight
• Lasts all day
• Ergonomically Designed Quiet

Caire provides everything you need for your oxygen therapy, from oxygen concentrators to accessories, we are dedicated to helping you breathe easy.

Eclipse 5
Combining portability with clinical efficiencygiving you the freedom to travel and enjoy life on the go: Compact and transportable
• Extended Battery Life
• Quiet 24/7 Use


NewLife Intensity 10
Stationary oxygen concentrator that’s durable with a high continuous flow: Higher flow options for patients in hospitals or long-term care facilities
• Dual flow option allowing two patients to use simultaneously
• Easy to service and maintain
A power efficient stationary oxygen concentrator is the must have for your home oxygen delivery needs:

• Lightweight and easily transportable
• Low failure rate with no preventative maintenance schedule
Lockable flow meter

AirSep VisionAire 5

HOW HARMFUL GUT BACTERIA TRIGGER ALZHEIMER’S
Agrowing body of evidence now suggests that it is not only age — but also diet — that affects the brain.
Indeed, a correlation between Alzheimer’s disease and an unhealthy gut has been uncovered, and Australian scientists are hoping to take this a step further by exploring how harmful gut bacteria access the brain and lead to dementia.
According to University of South Australia nano bio-scientist Dr Ibrahim Javed, tiny metabolites released by bad bacteria in the gut can travel to the brain, causing inflammation and triggering Alzheimer’s disease — for which there is no cure.
In younger people this is less likely because the blood–brain barrier is much stronger. However, this barrier weakens as people age, allowing harmful substances to damage neurons. When the microbiome in the gut ages, it also loses the ability to fight disease.
By identifying how metabolites released by bad bacteria damage neurons — and hopefully developing new drug therapies to block them — Javed said it should be possible to slow down or halt the progression of Alzheimer’s.
A second aim of the three-year research project is to investigate how probiotics and nutritional supplements, both of which contain friendly bacteria, can stamp out bad bacteria and stop metabolites escaping from the gut.
This follows on from several international clinical research studies that have demonstrated that probiotics improve digestive and cognitive issues in people with acute and chronic COVID-19.
“Our research indicates that harmful gut bacteria can trigger early onset dementia as well as accelerate dementia in patients already battling the neurodegenerative disease,” Javed said.
“A poor diet is one of several factors that harm gut bacteria, increasing your chances of developing dementia. Aging, lack of exercise, exposure to pesticides and genetics also play a role, although the latter is responsible for a very small number of cases. In most cases, dementia is preventable.”
Most types of bacteria are harmless — many are even essential for human survival — but bad bacteria create biofilms which cause gastrointestinal infections, chronic diseases, bowel cancer and brain diseases.
Alzheimer’s disease affects up to 55 million people worldwide and with an aging population, this number is expected to double every 20 years, according to Alzheimer’s Disease International.
Early onset dementia — under the age of 65 — is becoming more common in the global population, attributed to preventable factors such as a poor diet and a sedentary lifestyle, smoking, excessive alcohol consumption, social isolation, exposure to pesticides and air pollution.
Javed’s team is also collaborating with UniSA neuroscientist Associate Professor Larisa Bobrovskaya on a potential link between stress and Alzheimer’s disease, and whether women are more at risk.


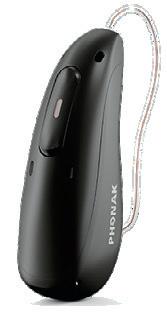
Hearing aid powered by AI chip
The Phonak Audéo Sphere Infinio hearing aid is powered by a dedicated real-time AI chip for speech-from-noise separation. Speech understanding in background noise remains the biggest challenge for people with hearing loss. This technology provides speech clarity from any direction, with an improvement in SNR (signal-to-noise ratio) in noise of 10 dB.
The hearing aid features ERA and DEEPSONIC AI chips and offers a 45% reduction in listening effort, according to the company. It also enables uninterrupted handsfree calls and streaming across twice the distance, and is compatible with all Bluetooth-enabled devices.
The DEEPSONIC chip provides real-time AI processing to instantly separate speech from background noise. It enables dynamic, real-time adjustments, allowing users to engage in conversations from any direction. The chip’s AI architecture includes a deep neural network (DNN) — with 4.5 million neural connections trained with over 22 million sound samples — and is 53 times more powerful than existing chips according to the company.
Phonak Hearing Systems
www.phonak.com.au
Assistive listening solutions
The MadisonAV Bettear Wi-Fi and Auracast assistive listening solutions are designed to assist hearing-impaired Australians to experience audio in public spaces such as theatres, conference rooms and places of worship.
The Bettear Wi-Fi solution provides users with the ability to connect their personal devices to a venue’s audio system via Wi-Fi. This allows for a seamless and personalised listening experience, ensuring that everyone, regardless of hearing ability, can enjoy crystal-clear sound. The Bettear Wi-Fi system is easy to use, requiring only a smartphone or tablet and the Bettear app, which is available for download on both iOS and Android platforms.
Auracast offers a high-quality, low-latency audio broadcast directly to compatible hearing aids, cochlear implants, earbuds and other listening devices. Designed to enhance accessibility, Auracast helps everyone in the audience to hear more clearly, without the need for additional equipment. This technology not only improves the listening experience but also promotes inclusivity, making public spaces more accessible to individuals with hearing impairments.
MadisonAV www.madisonav.com.au



LOWERING THE RISK OF A FALL ON P SYC HOTROPIC DRUGS

Asignificant finding has been made by Macquarie University researchers studying the impact of psychotropic drugs on the risk of falls among older people.
The study, which was published in the Journal of Post-Acute and Long-Term Care Medicine, showed that 83.6% of aged care residents receive psychotropic medication and 77.3% are on cardiovascular disease drugs. Both are classified as fall-risk-increasing drugs (FRIDs).
However, it also found that older people who had been prescribed psychotropic medication, and were also consistently taking cardiovascular disease medication at the same time, may be at lesser risk for serious falls.
The research, led by senior research fellow Dr Nasir Wabe from the Australian Institute of Health Innovation, showed that those residents receiving high levels of psychotropic medication along with high levels of cardiovascular disease drugs were less likely to fall than other residents receiving high levels of psychotropic medication but low levels of cardiovascular disease drugs.
“Our analysis revealed a potential preventative effect when high dose psychotropic medication was used with high dose cardiovascular disease medication,” Wabe said.
With residents of aged care facilities three times more likely to fall compared to those living in the community, potentially leading to serious injury and reduced quality of life, it is important to understand the additional risk associated with FRIDs, Wabe said.
“Understanding the impact of these drugs on people in residential aged care and monitoring their usage is crucial for ensuring safety,” he said.
Wabe and Professor Johanna Westbrook, also from the Australian Institute of Health Innovation, are leading work to ensure residents, their families, aged care providers and care staff have access to accurate and timely information about medication being prescribed and administered. Issues with medication administration and management that can lead to serious consequences — including hospitalisation, reduced quality of life, and death — were the basis of many concerns raised during the Royal Commission into Aged Care Quality and Safety.
The research included data from the medical records of 4207 permanent residents newly admitted to 27 residential aged care homes in Sydney, Australia.

CAREGIVER WELL-BEING: SMALL STRATEGIES, BIG IMPACT
Making thoughtful changes to create healthier work environments for caregivers can help organizations address many of the challenges facing care today. Investing in positive work experience not only strengthens your people—it can foster better patient care.
We cover the current drivers impacting well-being and retention with actionable ideas that can help renew and revitalize caregivers in the short and long term.
Short-term fixes and understanding your current environment is a good starting point, but to make the largest impact on caregiver well-being and retention, plan for long-term initiatives:
Update
Technology for New Workflows
A McKinsey study found that telehealth usage is currently 38 times higher than it was prepandemic. Experts believe telehealth usage will continue, solidifying this shift in how we provide and receive care.
Care organizations now can replace any temporary telehealth set-ups with long-term, professional-grade solutions that support flexible workflows and improved communication between patients and providers. Choose either a combination of mobile workstations with cameras that can move from room to room, or wall-mounted workstations that offer space saving and privacy.
Investing in videoconferencing technology and equipment that can be mobile and ergonomic for the end users, provides the flexibility of using telecommunication solutions between patients, families and professional medical practitioners supporting positive caregiver and patient experience.
Invest in Ergonomic Solutions
Caring for nurses in the long-term goes beyond technology updates. It’s about recognizing the importance of ergonomics, neutral postures and the balance between movement and rest. In a recent survey, 95% of respondents said that better ergonomic equipment could improve their well-being at work.
In today’s digital care environments, caregivers spend hours each shift completing documentation. It’s critical that this time spent on a computer is health-promoting and does not add mental and physical stress. The right ergonomic solutions are height-adjustable with easy monitor movement that provides a personalized charting experience.
The option to sit or stand allows caregivers to choose the right position for them—whether it’s standing to quickly add vital numbers or sitting to complete a more comprehensive task. Checking payback calculator for ergonomic workspace investment: www.ergotron.com/ en-au/tools/payback-calculator.
Limit Overtime Requirements
To help mitigate the risk of burnout for nurses, carefully consider any overtime requirements in place—both voluntary and mandatory. Overtime is often an unfortunate reality of the continued staffing crisis, but it can have a negative impact on caregiver health, retention and performance.
Longer shifts and fewer days off force nurses to sacrifice the time they need to rest physically and recharge mentally. Without this much-needed time, nurses may be more likely to burn out or contribute to small or large errors. Overtime can be a major income source for nurses, so establishing caps on weekly hours can help support balance and overall well-being.
Create Resimercial Spaces
There’s no better time to recommit to caregiver well-being than during a redesign or new build. The residential-commercial trend (“resimercial”) is already ushering in more home-like, warm designs in healthcare spaces to promote healing environments for patients. This can, in turn, benefi t the caregivers who work in these areas daily.
Private rooms, careful sound-proofing and natural light can lessen distractions and uplift the spirits of nurses, providers and other staff. Incorporating medical vendors into the design process to ensure their products will be a good fit in the space or thoughtfully considering the placement of supply closets and other resources can also go a long way in improving the daily workflows of staff.
Build Environments for Caregivers to Feel Their Best
There are many opportunities to make small changes that can have a meaningful impact on caregiver well-being and retention. By creating environments where caregivers feel physically and mentally at their best, they’ll be able to better care for themselves and their patients. Listen to a full discussion about strategies for improving caregiver well-being here:
Robin Burgess
Email: robin.burgess@ergotron.com
Mobile: +61 421 080 303
RESHAPING AGED CARE IN AN AGE OF INCREASING DIVERSITY

The Australian population is getting older and living longer, as well as becoming more culturally and linguistically diverse than ever before. This diversity needs to be kept in mind as Australia’s aged care system is reshaped in the wake of the ‘Final report of the Aged Care Taskforce’, writes CATH SCARTH, CEO of AMES Australia.
Nowadays, around one in five Australians over 65 were born overseas and one-third have at least one parent born overseas.
In 2022, 40,000 Australians from diverse cultural backgrounds were in some form of aged care and this number is expected to grow to 160,000 in the next 30 years, according to the Scanlon Foundation.
The Foundation also states that around 28% of people using home care were from multicultural backgrounds, although the Australian Institute of Health and Welfare (AIHW) suggests this proportion may be even higher.
Since 2020–21, across all mainstream aged care services, about 33% of people were born
overseas — of whom 66% were born in non-English-speaking countries. These figures paint a picture of the rich tapestry of cultural backgrounds among aged people in Australia — a cohort which is projected to nearly double by 2025.
CATERING TO DIVERSE CULTURAL BACKGROUNDS
This evolving cultural and linguistic landscape of Australia’s aging population is becoming a critical consideration for aged care providers. Projections highlight the need for aged care services to adapt and increasingly cater to the nuanced needs of CALD communities.
A significant proportion of aged care users — particularly those over 65 who were born overseas — may face language barriers, with less than one-third speaking English proficiently, according to data from the AIHW. In addition, people from non-English-speaking backgrounds often revert to their first language as they age.
But the challenges faced by individuals from CALD backgrounds extend beyond language barriers.
Limited digital literacy, smaller social networks and historical experiences of marginalisation can contribute to feelings of loneliness and isolation among these populations, exacerbating the complexities of aging.

Indigenous Australians also confront unique challenges stemming from historical trauma, cultural disparities and geographical isolation, which impede their access to and engagement with aged care services.
These issues can affect the ability of older adults to access and engage with essential support and services that can improve their quality of life and contribute to generally better outcomes.
DEMENTIA ON THE RISE
Leaving aside issues around cultural diversity, the prevalence of dementia and cognitive impairment among elderly populations also significantly impacts aged care needs.
Dementia not only affects cognitive function but also requires specialised care and support tailored to individual needs.
From memory loss to difficulties with communication and daily activities, dementia can profoundly affect an individual’s ability to live independently, necessitating comprehensive and person-centred aged care services.
As Australia’s population ages, addressing the unique needs of individuals living with dementia and cognitive impairment becomes increasingly crucial for ensuring quality aged care provision and enhancing the wellbeing of older adults across diverse communities.
For example, AMES Australia recently met with ‘Ellie’, an elderly migrant women who was beset by dementia. She was reverting to first language, struggling to look after herself and hadn’t left the home she shared with her son for five years.
AMES Australia was able to match Ellie with a carer who had appropriate language skills, and set up a care plan. Six weeks later, Ellie was again able to access community services and attend a Christmas party.
Ellie’s case shows that understanding the nuanced demographics and needs of aging populations within service areas is imperative for delivering tailored, relevant and sensitive aged care assessments.
CUSTOMISING CARE
Across Australia, regions exhibit distinct demographic compositions and care requirements, necessitating customised approaches to service provision.
For instance, regions within Victoria reveal varying proportions of CALD populations, ranging from higher concentrations in some places to significant Indigenous representation in others.
Looking at this data, it’s obvious that Australia’s aged care needs are multifaceted and dynamic, requiring a paradigm shift towards culturally competent and community-centric, client-led care models.
The experience AMES Australia has had working with multicultural communities across the country demonstrates that culturally competent communication is the first step in removing some of the difficulties and barriers.
Including members of CALD communities within the aged care workforce, while also providing cultural competency training and resources to all of the work force, is also a step in the right direction.
Adopting an aged care framework that recognises that individuals flourish when they are connected to family, to co-ethnic groups and to the broader community provides a significant opportunity to improve the wellbeing and outcomes of older Australians from non-EuropeanAustralian backgrounds.
By embracing diversity as a cornerstone of aged care provision and by fostering inclusive and responsive services, Australia can navigate the complexities of an aging population while honouring the diverse cultural identities and experiences of its older citizens.

Cath Scarth is the CEO of AMES Australia, a migrant and refugee settlement agency supporting both aged and disabled people who are new to Australia.
Cath has worked in the settlement and humanitarian sector for more than 20 years in Australia and the UK designing, implementing and overseeing a wide range of innovative social programs and enterprises.
iStock.com/FG Trade
WITH JANET PHILLIPS

A
s CEO of Peninsula Home Hospice, I witness daily the profound impact of palliative care on individuals facing life’s final chapter. Our mission is clear: to ensure every person can embrace their last moments with comfort, dignity and the freedom to choose how and where they receive care. However, this commitment is under threat due to severe funding shortages that jeopardise our ability to provide these essential services.
THE HEART OF THE ISSUE
Victoria faces a dire funding crisis in aged care palliative services, raising concerns that an increasing number of elderly Victorians may be denied the opportunity to die with dignity. With only about a year’s funding remaining, the palliative care sector — crucial for providing endof-life comfort — teeters on the brink, leaving its future uncertain and the industry scrambling for solutions.
A CASE FOR COMPASSIONATE CARE
Dying with dignity is about honouring and respecting the client’s choices. It includes symptoms management, whether these be physical or psychosocial. It also encompasses preferences for place of care, how the individual wants their care to be managed and their choice in place of death. We are dedicated to supporting the client’s significant others, including their own support network of family and friends.
I vividly recall Sue Kutrolli’s experience with Peninsula Home Hospice. Sue’s parents, battling Alzheimer’s and melanoma, found solace in our care during their final years. The compassionate support they received from Vasey RSL Care and our team ensured their comfort and dignity until the very end. As a nurse with 50 years of experience, Sue was profoundly impressed by the exceptional care her mother, Pat, received. Regular medication reviews from specialist pain staff at Peninsula Home Hospice ensured Pat’s comfort in her last year. However, the prospect of
such a compassionate end-of-life experience is now at risk for many Victorians due to imminent funding cuts.
Lack of funding would mean that, due to the increasing number of aged care facilities and an aging population in the Peninsula Home Hospice catchment area, we could no longer provide the necessary palliative care needs rounds. This would halt the crucial upskilling of aged care staff in palliative care, potentially forcing residents to be transferred to hospitals when their preference may have been to remain in their home.
THE URGENT NEED FOR FUNDING
Recognition of the urgency of this situation and interventions to secure the future of palliative care are crucial. Strategic allocations can alleviate strain on hospital systems and cultivate compassionate environments where individuals find solace in their final moments. Ensuring everyone has the opportunity to die with dignity and comfort is not just a goal — it is a societal obligation that demands immediate action.
For us at Peninsula Home Hospice, funding is specifically sought to continue the Community Palliative Care in Aged Care project, which aims to extend these vital services to all facilities within our reach. An increase in funding would allow us to continue upskilling staff in residential aged care and ensure that all residents receive the best palliative care — every resident, every time.
LOOKING AHEAD
Sustained funding and partnerships are essential in safeguarding quality end-of-life experiences for all Australians amidst the challenges of an aging population. The looming funding crisis threatens to rob many Victorians of the right to die with dignity and choice. The stories of families like Sue’s serve as poignant reminders of the critical need for continued investment in palliative care.
In a society judged by its compassion, our humanity is measured by how we care for our most vulnerable. Funding palliative care isn’t just about budgets — it’s about upholding human dignity. As we navigate the complexities of healthcare funding, let us remember that the value of life extends to its very end. Let us advocate, support and demand a future where dying with dignity is not a luxury but a fundamental right.

Janet Phillips is the Chief Executive Officer at Peninsula Home Hospice. She is an experienced senior executive in community palliative care, oncology, disability and aged care. Having worked in the health industry for 36 years, she has spent the last 20 years in the NFP sector and is approaching four years at Peninsula Home Hospice. Janet has extensive experience in stakeholder advocacy and engagement with government, the palliative care sector and industry bodies.
ACIPC INTERNATIONAL CONFERENCE
Infection prevention and control (IPC) is vitally important across all healthcare settings in reducing the risks of transmission of infections and the development of antimicrobial resistance.
The Australasian College for Infection Prevention and Control (ACIPC) is the peak body for infection prevention and control professionals (ICPs) in the region. ACIPC advocates for ICPs and IPC by focusing on leadership, education and evidence-based practice for a healthy community.
This year’s ACIPC International Conference, to be held from 17–20 November 2024 at the Melbourne Convention and Exhibition Centre and online, has the theme: Succession, sustainability, and the advancement of infection prevention and control.
SPEAKERS

The conference aims to address emerging challenges, promote innovative approaches and create a collaborative environment where diverse perspectives are valued. By attending the conference, you will learn from national and international experts, network with like-minded professionals and meet with Australasia’s largest collection of IPC industry suppliers.
Confirmed speakers include:
• Michael Borg, Head, Department of Infection Prevention and Control, Mater Dei Hospital, Malta
• Glenn Browning, Director, Asia-Pacific Centre for Animal Health
• Frances Geraghty-Dusan, Senior One Health Advisor, Indo-Pacific Centre for Health Security
• Heather Gilmartin, Health Senior Researcher, Implementation Scientist, Denver/Seattle Centre of Innovation, Rocky Mountain Regional Veterinary Health Administration Medical Centre
• Bronwyn King AO, Public health champion; Founder, Director, and CEO, Tobacco Free portfolios
• Lisa Hall, Director, Teaching and Learning & Professor – School of Public Health, Qld University
For more speakers and presentation topics, visit the conference website: https://acipcconference.com.au/.
AGED CARE PRE-CONFERENCE WORKSHOP
To be held Sunday 17 November 10:00am – 5:00pm at the Melbourne Convention and Exhibition Centre and online.
The 2024 ACIPC Aged Care Workshop aims to immerse in-person and online delegates in an interactive experience. This year’s workshop will feature a total focus on engagement, hands-on learning, collaboration and feedback, rather than presentation only.
The workshop will be opened by ACIPC President A/Prof Stéphane Bouchoucha, followed by a brief overview of the ACIPC Aged Care Strategy.
The day will include three different workshop sessions, targeting topics that are on the forefront of IPC change in aged care.
Navigating surveillance in aged care will kick off the first workshop. Delegates will review aged care surveillance and current research outcomes, undertaking collaborative activities and discussions to enhance surveillance understanding and knowledge.
A team from the Aged Care Quality and Safety Commission will facilitate the second workshop, AMS implementation in aged care. Discussions will focus on AMR SAT, working with various AMS tools, and exploring strategies to achieve sustainable improvements.
The final workshop is Animals in health care, which connects with the principle of ‘person-centred care.’ Using the guide Safe Animal Friendly Environments (University of South Australia), the audience will be on an interactive journey to embrace, enable, and manage animals in aged care.
The Aged Care Workshop is targeted to those involved in, responsible for, or interested in aged care IPC.
All graduates of the ACIPC Foundations of IPC course receive ACIPC educational membership, and will again receive free registration to the workshop (online). Delegates attending in-person and online must register.
For more information and registration, visit: https://acipcconference. com.au/.

PREDICTING DEMENTIA NINE YEARS BEFORE DIAGNOSIS
Anew test can predict the onset of dementia with 80% accuracy, according to researchers at Queen Mary University of London.
The new method can predict dementia up to nine years prior to diagnosis. In addition, it is more accurate than memory tests or measurements of brain shrinkage — two commonly used methods for diagnosing dementia.
The team, led by Professor Charles Marshall, developed the predictive test by analysing functional MRI (fMRI) scans to detect changes in the brain’s ‘default mode network’ (DMN). The DMN connects regions of the brain to perform specific cognitive functions and is the first neural network to be affected by Alzheimer’s disease.
HOW WAS THE RESEARCH CONDUCTED?
The researchers used fMRI scans from over 1100 volunteers from UK Biobank, a large-scale biomedical database and research resource containing genetic and health information from half a million UK participants, to estimate the effective connectivity between 10 regions of the brain that constitute the DMN.
The researchers assigned each patient with a probability of dementia value based on the extent to which their effective connectivity pattern conforms to a pattern that indicates dementia or a control-like pattern.
They compared these predictions to the medical data of each patient on record with the UK Biobank. The findings showed that the model had accurately predicted onset of dementia up to nine years before an official diagnosis was made, and with greater than 80% accuracy. In the cases where the volunteers had gone on to develop dementia, it was also found that the model could predict within a two-year margin of error exactly how long it would take that diagnosis to be made.
The researchers also examined whether changes to the DMN might be caused by known risk factors for dementia. Their analysis showed that genetic risk for Alzheimer’s disease was strongly associated with connectivity changes in the DMN, supporting the idea that these changes are specific to Alzheimer’s disease. They also found that social isolation was likely to increase risk of dementia through its effect on connectivity in the DMN.
“Predicting who is going to get dementia in the future will be vital for developing treatments that can prevent the irreversible loss of brain cells that causes the symptoms of dementia,” said Charles Marshall, Professor and Honorary Consultant Neurologist.
“Although we are getting better at detecting the proteins in the brain that can cause Alzheimer’s disease, many people live for decades with these proteins in their brain without developing symptoms of dementia. We hope that the measure of brain function that we have developed will allow us to be much more precise about whether someone is actually going to develop dementia, and how soon, so that we can identify whether they might benefit from future treatments.”
A DAY IN THE LIFE

PAULA REID
“TAKING THE OPPORTUNITY TO MAKE A DIFFERENCE”
After Paula Reid commenced her career in nursing, she discovered that alongside her keen interest in chronic health conditions, she also thoroughly enjoyed caring for older people. So when she made a move from the city to a rural area, she immediately sought a nursing opportunity within the aged care sector.
“I found that through this work, I could develop my comprehensive assessment skills. But rather than focusing simply on a disease, I was able to take a more holistic approach — seeking to understand the individual, their health and independence, and also acknowledging their life story,” Paula said.
Now the Clinical Lead at the Resthaven Community Services Murray Mallee Hills Region & Fleurieu Region, Paula works to ensure that the professional standards of contemporary nursing practice are in line with Resthaven’s policies and procedures. In addition, she provides clinical support and guidance to the Resthaven nursing team and its home support workers.
“The tasks I do vary from day to day,” Paula said. “But I generally start my day by reviewing any consumers who have had issues over the weekend and previous day, including a review of high-risk clients and incidents to make sure that remedial and preventative action has been put in place. This may require consultation with the consumer and their representatives and other health professionals.”
Over time, Paula has witnessed multiple changes taking place within the aged care section. For instance, she has seen alterations made to funding instruments, and subsequent improvements in the programs delivered to Resthaven’s aged consumers.
“The consumer’s needs have changed and accordingly, the Aged Care Quality Standards have changed,” she said.
“Nursing and the need to continue to provide best practice care are continually evolving. Completing assessments that identify health issues — and being involved in working with the person to achieve positive outcomes — continues to be a real focus, as we support older people to exercise their choice and independence while recognising their cultural, spiritual and physical needs.”
Witnessing the positive outcomes that aged care nursing brings to older people continues to inspire Paula every day. She relishes being involved in programs such as “Short-Term Restorative Care”, where the focus is on working alongside consumers and their health teams to identify and achieve their goals.
“I monitor participants and assess them for improved outcomes and impact on their wellbeing. And I go home each day with a feeling of satisfaction that I have been instrumental in enabling these people to continue to live in their own homes with dignity and respect — maintaining the way they choose to live,” she said.
“I really enjoy seeing people adapt to their abilities and enjoying positive outcomes so that they can continue to maximise their activities and pursuits.”
At the end of the day, Paula views aged care nursing as an opportunity to make a difference to a large proportion of the community.
“In the time that I have been at Resthaven, I have had the amazing opportunity to work in various aspects of aged care options — from residential care to community care. I have held several positions and have always been supported to take on new challenges within the organisation. The work I do is varied and very satisfying.”
WHY WOMEN NEED TO GET ACTIVE BY AGE 55

Anew study has linked activity levels in middle age with improved physical health in later life.
The research from Charles Perkins Centre and University of Sydney’s School of Public Health — published in PLOS Medicine open-access journal — assessed more than 10,000 Australian women.
It showed a significant link between regular exercise during mid-age and physical health later in life, even when the exercise routine was not started until their mid-50s.
“Our study shows that it’s important for women to be active throughout mid-age to gain the most benefits for physical health in later life. Ideally, women should increase their activity levels to meet the guidelines by age 55,” said lead author Dr Binh Nguyen, from the Faculty of Medicine and Health at the University of Sydney.
CONDUCTING A LONGITUDINAL STUDY
The evidence for an association between physical activity and health-related quality of life has been based primarily on crosssectional studies and short-term randomised controlled trials. Few longitudinal studies have measured physical activity at more than one time point and examined the long-term causal effects of exercise.
In the new study, researchers used data collected at three-year intervals beginning
in 1996 from 11,336 participants in the Australian Longitudinal Study on Women’s Health. The study participants were 47 to 52 years old when the study began.
Participants were classified as either meeting WHO physical activity guidelines (150 minutes of activity a week) consistently throughout the 15-year exposure period; not initially meeting the guidelines but starting to meet them at age 55, 60 or 65; or never meeting the guidelines. Healthrelated quality of life was assessed using the physical health composite score (PCS) and mental health composite score (MCS) from the Short Form 36 Health Survey, which included 36 questions about functional health and wellbeing.
WHAT WERE THE STUDY FINDINGS?
On average, women who consistently met physical activity guidelines throughout mid-age and those who first started to meet guidelines at age 55 had a three-point higher PCS — 46.93 and 46.96 respectively. Those that did not consistently meet physical activity guidelines throughout mid-age returned a lower PCS, 43.90.
The effect of physical activity on the PCS was significant even after controlling for socioeconomic factors and pre-existing health diagnoses. However, there was no significant association between physical activity and mental health composite score (MCS).
“Combined with existing evidence, this study contributes to growing evidence of the benefits of maintaining or adopting an active lifestyle in mid-age,” said the authors.
“An important public health message is that being active for as many years as possible, even if women start to meet physical activity guidelines in their mid-50s, could have important health benefits in terms of physical health, especially in physical functioning,” Nguyen said.
“Overall, the findings from this study highlight the importance of being physically active for as long as possible to gain the most benefits for quality of life, especially in relation to physical health.”
INTEGRATING SPORTS TECHNOLOGY TO BOOST WELLNESS FOR OLDER PEOPLE
CASE STUDY
PROBLEM
LiveWell Health was presented with the challenge of finding a better way to evaluate strength within the aging population.
SOLUTION
VALD technologies have enabled LiveWell Health clinicians to better understand movement at the individual joint level.
Presented with the challenge of finding a better way to evaluate strength within the aging population, LiveWell Health turned to VALD technology.
Founder of LiveWell Health, Andrew Sokolowski — who is passionate about using exercise as medicine for older people — decided to take the technology, science and practices that are typically adopted by professional athletes and use them to make a difference in the lives of average people.
“Being in the senior care industry, we work with a number of providers — most commonly physicians, but also skilled nursing homes, senior care (caregiver) agencies, home healthcare agencies and outpatient physical therapy clinics,” Sokolowski said.
“Prior to implementing VALD’s technologies, we were seen as ‘just another group of personal trainers’. But after we described our processes and protocols with each of the various providers, we were looked upon very differently. We were seen as a true partner, and could easily measure the impact we were having on their patients, clients and members.
“By adopting VALD technologies we’ve had an exponential increase of referrals and revenue growth of 645% in the same period, through the combination of excellent service via health technology and the team’s professionalism.”

Previously, the only way LiveWell Health had been able to evaluate strength in an individual was to establish a one-repetition maximum (1RM), or — playing it a little more safely — establish a 10RM in order to approximate a 1RM. While this method had the capacity to be successful for a highly motivated older person, it was not as effective for people who were newer to exercise. For these people, a maximal effort test at initial evaluation was often an unpleasant experience that had the potential to turn them off exercise entirely.
Instead, the VALD technologies have enabled LiveWell Health clinicians to better understand movement at the individual joint level. They are now able to test with DynaMo to accurately collect and understand objective data, which allows them to create and implement exercise programs with ease. It also allows clinicians to better verbalise their findings with patients and families.
“‘Your father is quite weak in this area’ doesn’t quite cut it anymore,” Sokolowski said.
“Now we can provide meaningful data insights to say: ‘When you compare your father with others in this cohort you can see he generates 1.04 Newtons of force per kilogram of body weight (N/kg); the average among skilled nursing residents is 1.26 N/kg. With that said, if we want him to be ambulating independently once again, we must focus at the individual joint level with a progression into functional movement.’ This resonates with members far more effectively.”
With more information at hand, LiveWell Health has also been able to establish better strategies to accomplish attainable goals on an ongoing basis. VALD technologies are easily transported, so when it seems that a person’s progression or regression may have occurred, clinicians can readily reassess and divert course if needed.
“Our members are not left wondering whether they are making progress — the data can confirm it,” Sokolowski said.

VIRTUAL ALLIED HEALTH PLATFORM ROLLS OUT FOR REMOTE CLIENTS
A24/7 virtual allied healthcare platform that allows clients to receive support from their homes will be made available by Roper Gulf Regional Council and iAgeHealth. Typically when a client requires an allied health support, a specialist is required to fly in several times a year to provide the services. This is often costly and time-consuming, as well as having an impact on recovery and treatment times — which in turn negatively affects the quality of life for age care clients.
To assist with this problem, the iAgeHealth program — which is staffed by experienced allied health professionals who are able to assist with recovery following illness or injury, and manage chronic health conditions — removes the barrier of remote living for many clients.
“We are passionate about finding the right solutions to overcome the tyranny of distance and access to regular, experienced clinical staff,” said David Hurst, Acting CEO for Roper Gulf Regional Council.
“As soon as the council recognised iAgeHealth’s allied health services innovative approach, and its ability to address long wait periods, streamline appointment scheduling and provide more affordable options for age care client packages, it was evident that these solutions needed to be integrated into our local communities.
Initially, services within the Roper Gulf will be focused on providing occupational therapy services to conduct home modification assessments, physiotherapy assessments and treatment plans.
Additionally, dietetic meal planning, assessment and monitoring will be provided, as these are the areas of greatest immediate need.
“Our intent with developing iAgeHealth was to meet the needs of our own clients across regional Australia and share that with those areas in greatest need,” said Sue Thomson, CEO of McLean Care, the parent company of iAgeHealth.
“Roper Gulf is a perfect example of an area who continues to work really hard to support local people, but simply cannot offer the same level of support that their counterparts in metro or even regional areas can.
“Access to high-quality clinical care simply isn’t equitable across Australia — and it should be. iAgeHealth means it can be.”
It is expected that, once embedded, the partnership in this area will continue to access more of the specialist services that iAgeHealth provides such as speech pathology and exercise physiologists.
Editor: Amy Steed ah@wfmedia.com.au
Publishing Director/MD: Janice Williams
Art Director/Production Manager: Linda Klobusiak
Art/Production: Marija Tutkovska
Circulation: Alex Dalland, circulation@wfmedia.com.au
Copy Control: Ashna Mehta copy@wfmedia.com.au
Advertising Manager: Kerrie Robinson +61 400 886 311 krobinson@wfmedia.com.au
PUBLISHED BY Westwick-Farrow Media A.B.N. 22 152 305 336
www.wfmedia.com.au
Head Office
Unit 5, 6-8 Byfield Street, North Ryde Locked Bag 2226 North Ryde BC NSW 1670 AUSTRALIA ph: +61 2 9168 2500
If you have any queries regarding our privacy policy please email privacy@wfmedia.com.au
Subscriptions for unregistered readersprice on application