OnCenter

MEET PRESIDENT AND CEO KEITH HOBBS
Celebrating a culture of teamwork
PUBLICATION FOR OUR FAMILY OF EMPLOYEES, MEDICAL STAFF AND VOLUNTEERS
2024
A
SPRING
Welcome

From the CEO
It’s been nearly five months since I became CEO, and I have enjoyed getting out and meeting staff, working with leadership and the board of trustees, and getting to know community members better.
In this edition of OnCenter, I am honored to share more about myself, my family, my career and the vision for the future of Torrance Memorial. You will also learn more about our amazing imaging department and its crucial role in determining a proper and thorough diagnosis. This issue also explores service from the heart of our employees who give back and volunteer their time away from work.
Hear from one of our physicians who put his health care and trust in the expert hands of our Torrance Memorial Physician Network doctors and cardiovascular team—a great story of resilience, excellence and the importance of getting an annual routine exam! We’re also proud to report that six years into our collaboration with the leading academic health system CedarsSinai, patients have access to the latest technology, advanced treatment options and more clinical expertise in neuroscience, oncology and cardiology.
Recently, Torrance Memorial Medical Center was recognized by Newsweek as part of its list of World’s Best Hospitals 2024. This year, Torrance Memorial ranks as the 43rd best hospital in the nation and 10th best in California. This places Torrance Memorial in the top elite 150 to 250 hospitals worldwide.
Looking ahead, we continue to focus on preparing to expand the Lundquist Leach Emergency Department for the future, developing a teaching hospital program and serving our community.
I am grateful for your support.
Keith Hobbs
President and CEO, Torrance Memorial Medical Center
2 ONCENTER — SPRING 2024 Editor Julie Taylor Executive Director Marketing Erin Fiorito Publisher, Creative Director Vincent Rios Copy Editor Laura Watts Contributors Lisa Buffington John Ferrari Diane Krieger Dalia Silva Nancy Sokoler Steiner Laura Roe Stevens Julie Taylor Photographers Peter Cooper Philicia Endelman Michael Neveux Vincent Rios Published by Vincent Rios Creative, Inc. VincentRiosCreative.com ©2024 Torrance Memorial Medical Center. All rights reserved. Reproduction or use in whole or in part without written permission is prohibited. This publication is for informational purposes only and should not be relied upon as medical advice. It has not been designed to replace a physician’s medical assessment and medical judgment. Always consult first with your physician regarding anything related to your personal health.
4



Louis
TORRANCEMEMORIAL.ORG 3
Awards and Accolades Celebrating the many prestigious awards at Torrance Memorial
Social Scene Highlighting social posts and news from around the hospital +TMU class schedule
Cover Story Meet president and CEO Keith Hobbs
Under the Surface
imaging department provides information critical to diagnosis and treatment Contents SPRING 2024
the Cover
6
12
16
The
On
Tanada, RN, Anthony Chen, MD, President and CEO Keith Hobbs, Lisa Araujo, outpatient laboratory volunteers Donna Imhoff and golden retriever Abigail. Photo: Vincent Rios OnCenter magazine welcomes your feedback at oncenter@tmmc.com
Career Exploration Day Inspiring the next generation of medical professionals
Celebrating Six-Year Affiliation with Cedars-Sinai
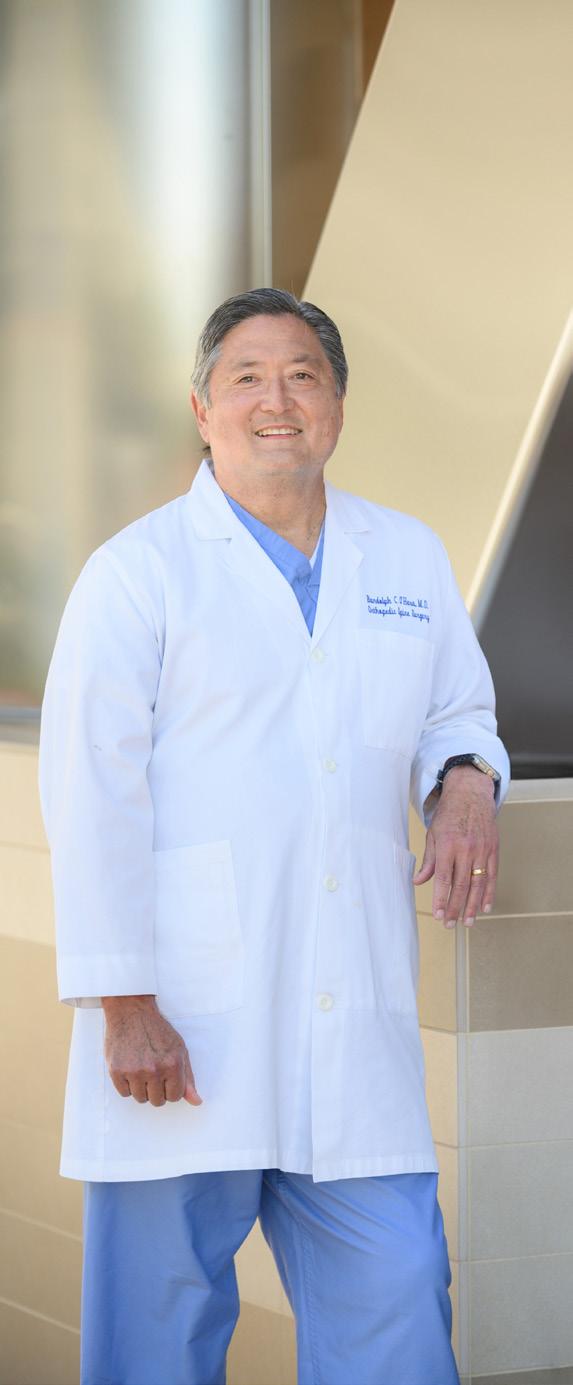
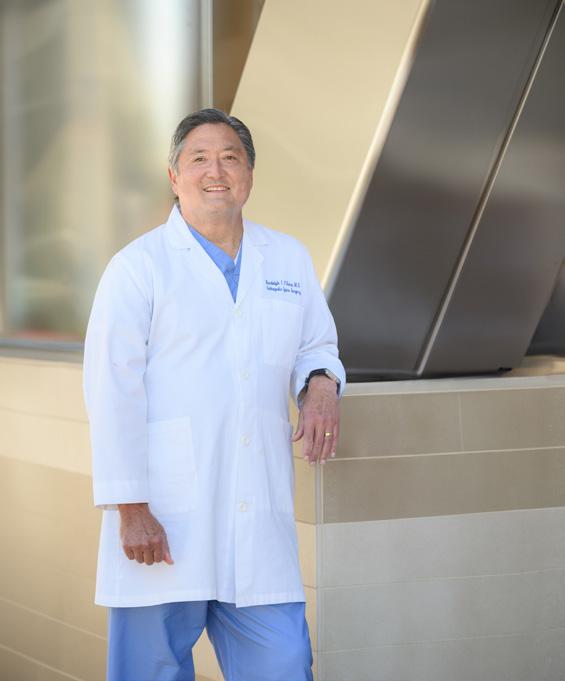
Physician and Patient at Torrance Memorial Orthopedic surgeon Randolph O’Hara, MD, became a patient
In Service of Others Inspiring stories of employee volunteerism 24 12 16
20
22
24
26

Awards&Accolades

Newsweek Best Hospitals in the World
Torrance Memorial Medical Center has been recognized by Newsweek as part of its list of World’s Best Hospitals 2024. This year Torrance Memorial ranks as the 43rd best hospital in the nation and 10th best in California. This places Torrance Memorial in the top elite 150 to 250 hospitals worldwide.

American College of Emergency Physicians
Torrance Memorial is now accredited by the American College of Emergency Physicians (ACEP) Geriatric Emergency Department Accreditation Program. This bronze (level 3) accreditation provides an excellent avenue to convey to our patients, colleagues and hospital administration that our program is first-rate and meets the interdisciplinary geriatric standards set forth by ACEP focused on the highest care for our South Bay community’s older adults.

Silver Designation for Antimicrobial Stewardship
Torrance Memorial is recognized with a Silver honor roll designation for Antimicrobial Stewardship by the California Department of HealthcareAssociated Infections Program. Thanks to the Torrance Memorial team that developed a program embodying each of the CDC’s Core Elements, making this designation period for three years.
4 ONCENTER — SPRING 2024 Awards

Aetna’s Institutes of Quality Seal
Congratulations to Torrance Memorial for meeting the criteria for Aetna’s Institutes of Quality® seal in Total Joint Replacement. IOQ designation is for the current three-year review cycle of 2023 to 2025.

Blue Distinction Centers for Maternity Care 2023 Program
Torrance Memorial’s maternal care center was awarded the Blue Distinction Centers (BDC) designation for maternity care as a national center of excellence program that encompasses 1,030 facilities, accounting for almost 25% of all birthing hospitals nationwide. Sponsored by Blue Cross Blue Shield, Blue Distinction-designated maternity care centers must meet rigorous quality evaluations that measure structure, process and patient outcomes. BDC maternity facilities are evaluated on outcomes and procedures for all patients regardless of insurance coverage, which increases quality care for all women.

Healthgrades
Torrance Memorial Medical Center has been nationally recognized by Healthgrades with both the Patient Safety Excellence Award and the Outstanding Patient Experience Award. Only top-performing hospitals are recognized as national leaders in both categories.

American College of Radiology
Torrance Memorial’s ultrasound breast staff received the Breast Diagnostic Center Award from the American College of Radiology (ACR), achieving another three years of ACR breast accreditation. Receiving this prestigious Breast Imaging Center of Excellence designation from the ACR demonstrates our excellence and hard work in supporting our patients and community.

American College of Surgeons
Torrance Memorial recently earned the distinction of being named an American College of Surgeons Surgical Quality Partner. The Surgical Quality Partner designation highlights Torrance Memorial’s dedication to maintaining the highest standards in surgical care as evidenced by our participation in the following quality programs: Commission on Cancer, National Accreditation Program of Breast Centers, and Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program. Accreditation of Torrance Memorial’s cancer program, breast program and bariatric program reflects our proven record of adhering to the most rigorous standards in surgical quality to minimize complications, improve outcomes and save lives.
TORRANCEMEMORIAL.ORG 5
Posts curated by Dalia Silva

POLARx Technology
Our Heart Rhythm Center is committed to monitoring, mapping and treating cardiac arrhythmias at the Torrance Memorial Lundquist Lurie Cardiovascular Institute. In a rapidly evolving field driven by cutting-edge technology, we are dedicated to delivering the most advanced care to our community. On September 19, Sang Yong Ji, MD, and the exceptional Heart Rhythm Center team achieved a significant milestone by becoming the first in California to perform an atrial fibrillation ablation using the groundbreaking Boston Scientific POLARx technology. Treating atrial fibrillation and safeguarding the hearts of our community remain our top priorities at the Lundquist Lurie Cardiovascular Institute.
ENA Conference
Every year, the Emergency Nurses Association holds a conference that brings together emergency department nurses from all over the world, with approximately 5,000 nurses in attendance. Attendees range from new to experienced to retired nurses, all wanting to provide the best care for their patients. This year’s conference provided insightful classes and lectures, networking with other ED nurses to share best practices, and insights into the latest equipment and technology. Torrance Memorial has always supported the emergency department by annually sending our nurses to these conferences. As a winner of the Lantern Award from 2021 to 2024, our nurses were proud to represent our hospital and the hard work of our entire emergency team.


Employee BBQ
We celebrated the end of summer with our annual employee BBQ—Caribbean style! Thanks to our HR, Employee Health and Nutrition & Food Services teams for hosting a fun day filled with delicious food, music, dancing and flu shots!
#TeamTorranceMemorial
6 ONCENTER — SPRING 2024
Social Scene

Veterans Day Ceremony
Torrance Memorial held a special Veterans Day ceremony and presentation of brass pins to recognize and honor the veterans among our dedicated staff and volunteers. We are beyond grateful for the men and women who have served our country. Thank you to all active-duty members and veterans for your bravery and patriotism. We salute you!

City of Carson Proclamation
On September 5, the city of Carson bestowed a proclamation to Torrance Memorial for Prostate Cancer Awareness Month. The Hunt Cancer Institute, an affiliate of Cedars-Sinai Cancer, is at the forefront of pioneering treatments and continues to excel in the battle against prostate cancer. Let’s join hands to raise awareness and champion the cause!
#prostatecancerawarenessmonth

Walk From Obesity
Torrance Memorial partnered with Cedars-Sinai and Marina del Rey Hospital to host the #SoCalWalkFromObesity. The walk raised funds for the American Society for Metabolic and Bariatric Surgery Foundation to support obesity treatment research, education and access to care initiatives. Thank you to all who came out to make a difference!
TORRANCEMEMORIAL.ORG 7 Social Scene

Drug Take Back Day
Drug Take Back Day with the Torrance Police Department was a success! Thanks to our outstanding community, we collected 165.2 pounds of expired meds and drugs. Your efforts will help reduce prescription drug abuse and diversion throughout our communities. Thank you!
Worldwide Pressure Injury Day
On November 16, Torrance Memorial’s wound care team joined hospitals nationwide in observing #WorldwidePressureInjuryDay by educating staff and visitors on the importance of preventing pressure injuries. If you or your loved one is at risk for a pressure injury or develops a pressure injury, talk with your health care provider to make a plan.


Kindness Week 2023
Kindness Week 2023 was a success! We celebrated kindness all week with wellness events like guided gratitude journaling, clown visits, a lemonade cart, snack cart rounds, cookie pop-up, rock art therapy, sound bath meditation, walks with leadership, a community book library and so much more! #KindnessisContagious
8 ONCENTER — SPRING 2024 Social Scene

Torrance Memorial Auxiliary Donation
Torrance Memorial’s Volunteer Auxiliary presented a check for $209,000 to the Torrance Memorial Foundation at its 2024 Auxiliary annual meeting. This donation supports the Torrance Memorial emergency department expansion campaign. Thank you, volunteers, for providing over 110,000 hours of service last year and for this generous donation!
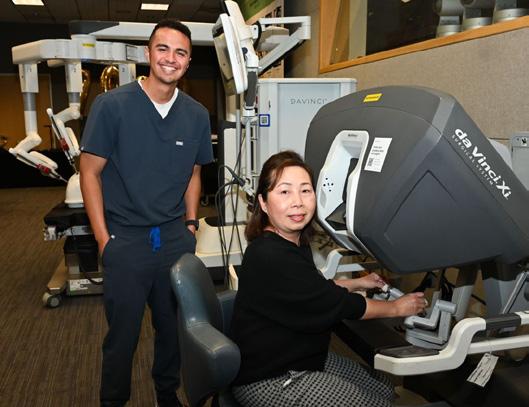
7,000th da Vinci Procedure
Torrance Memorial celebrated the 7,000th da Vinci procedure with an employee demonstration of the da Vinci Xi surgical robot!

Aizenjai Group Tour
The Aizenjai Group from Hokkaido, Japan, visited Torrance Memorial to tour our campus, engage with our health care teams, knowledge-share and gain insights on patient care. Thank you for visiting!

Law Enforcement Appreciation Day
Law Enforcement Appreciation Day is a special time to thank officers for their daily sacrifices for the communities they serve and protect. We want to send a special thank-you to our outstanding local law agencies. You are always there for us. We appreciate all your support—helping with our disaster drills, decorating a Holiday Festival tree, attending our events, and protecting our staff and patients. We appreciate you all!
#LawEnforcementAppreciationDay
TORRANCEMEMORIAL.ORG 9 Social Scene

Holiday Festival 2023
Cheers to another successful Holiday Festival! Thank you to our hardworking volunteers and supportive community who made our 40th celebration magical for the entire South Bay! Wishing you a happy holiday season! #40YearsofHolidayFestival
Martin Luther King Jr. Day
In honor of civil rights leader Dr. Martin Luther King Jr.’s contributions, we are inspired by his words of wisdom. As we celebrate his legacy, we reflect on our dedication to providing quality care and improving community health.
In January, CARE&J sponsored the third annual food drive, honoring Dr. Martin Luther King Jr. Torrance Memorial Health System employees donated food and personal items to support our community. Collections benefit New Challenge Ministries and Fresh Rescue Food Bank, our partners in addressing local food insecurity. This year, we collected a recordbreaking 4,500+ pounds of donations!

Follow Us on Social

10 ONCENTER — SPRING 2024 Social Scene

To register for any of our upcoming events, please contact Krista Canetti (krista.canetti@tmmc.com) or Elaine McRae (elaine.mcrae@tmmc.com).
Leadership & Communication Classes
Coach if you Care (for managers and leads)
April 9
9 a.m. to noon
West Tower Auditorium
Conflict Mediation Skills (for managers)
April 23
11 a.m. to 1 p.m.
West Tower Conference Room A
Fostering an Inclusive Workplace Through Acceptance
April 25
11 a.m. to 1 p.m.
West Tower Conference Room C
Exploring Leadership in Health Care
May 21
9 a.m. to noon
West Tower Auditorium
CERTIFICATE PROGRAMS:
Transitioning to Leadership Fundamentals (4-part series for ancillary leads)
Every Thursday
April 4, 11, 18, 25
9 a.m. to noon
Hoffman Health Conference Center Room 1 & 2
Health & Wellness Events:
Ayurveda Workshop – Part 1
Discover your mind-body constitution, learn balancing practices, and identify how to sync your rhythm for more energy, happiness and better mental health.
April 29
Noon to 1 p.m.
Zoom
Ayurveda Integration – Part 2
Apply what you’ve learned in Part 1 into your daily life.
April 30–May 5
(5-day text message challenge)
To RSVP text “BALANCE” to Jamie, 213-219-4788

VISION 2024
Sound Bath
May 14
5:30 to 6:30 p.m.
Hoffman Health Conference Center Room 1 & 2
Rock Painting
June 4
11 a.m. to 1 p.m.
Drop in anytime at Yang Patio
Employee Forum/Vision Sessions
Learn how our Torrance Memorial leaders assess the current situation and their vision for future success. Register for these annual Zoom and in-person events on your preferred date and time through the TMU website.
Employee Forum (all staff)
May 30
7:45 a.m., 2 p.m. and 3:45 p.m.
Director Vision (in-person)
July 25, 9 to 10:30 a.m.
Hoffman Health Conference Center Room 1 & 2
Manager Vision (in-person)
July 30, 9 to 10:30 a.m.
Hoffman Health Conference Center Room 1 & 2
Staff Vision (in-person)
August 7
Hoffman Health Conference Center Room 1 & 2
Staff Vision (via Zoom)
August 8 and 13
8:30 to 9:30 a.m.
August 15
3:30 to 4:30 p.m.
August 20 and 21
8:30 to 9:30 a.m.
TORRANCEMEMORIAL.ORG 11
Support and Education
Written by Diane Krieger
Photographed by Vincent Rios
November 1, 2023, wasn’t in any way remarkable. Just an ordinary Wednesday. It happened to be Keith Hobbs’ first day behind the CEO desk—long occupied by retiring chief executive Craig Leach.
A major milestone in Torrance Memorial history to be sure. But for the hospital community at large, it was a perfectly normal weekday in a carefully planned, seamless transition of leadership. Nothing had been left to chance.
Leach had carefully timed his exit, bringing Hobbs on board as executive vice president in March 2021. He’d calculated two years would be enough time for his successor “to really get to know the culture of the organization, to fit in and build relationships.” And that’s exactly what happened.
Hobbs has been an integral part of the Torrance Memorial leadership team for almost three years now. He’s spearheaded the new ambulatory surgery center set to break ground within the coming year, shepherded the dramatic expansion of laboratory outreach programs and overseen the strategy for growing the physician network. Last February, he was formally promoted to president, and his elevation to CEO was announced in June—several months before he stepped into that role.
“It’s hard replacing a trusted, longtime leader like Craig Leach,” says Torrance Memorial board chairman Greg Geiger, “but the task was made easier with Keith Hobbs as the candidate. We already know what kind of leader he’s going to be because he’s been here for a few years. We have all the confidence in the world in him.”
Cedars-Sinai Health System CEO Tom Priselac echoes that confidence. “I’m excited to be working with Keith,” he says. “He’s already proven himself a great asset as we increase our footprint across the region.”
Newly appointed chief medical officer Zachary Gray can vouch for Hobbs’ personal style. “I can honestly say Keith is a genuinely warm, caring, good person,” says Gray, who spent the past year in close collaboration with Hobbs as they meticulously planned Torrance Memorial’s rotating residency in internal medicine, slated to debut in July. “Keith has all the bona fides and all the experience necessary.”
ALL IN THE FAMILY
Hobbs grew up in Glendale, California. Both his parents worked in sales for Pacific Bell and AT&T. The first in his family to graduate from college, Hobbs started out as a compensation analyst at a bank in 1989. He moved over to Walt Disney Imagineering in a similar role after two years. The Indiana Jones ride, Fantasmic and Disneyland Paris were launched during his tenure.
“It makes total sense going from banking to entertainment to health care,” Hobbs reflects playfully, then adds in earnest: “I found my calling in hospital administration. Since I was young, I’ve always been involved in helping others. I really enjoy the healthcare environment. The mission resonates with who I am as a person.”
In 1992, Hobbs joined the HR department of USC-affiliated Children’s Hospital Los Angeles (CHLA). His wife of 33 years, Merilee, was already a reimbursement rep in the billing department and loved her job.
They’d met at church a few years earlier. At the time, she was a candy striper in what is now USC Verdugo Hills Hospital in their hometown of Glendale. Together, they raised three children: Amanda, 28, Kameron, 26, and Landon, 21, and are proud grandparents to 18-month-old granddaughter Scarlett. Rounding out the Hobbs family is Tillie, a Yorkie rescue dog.
12 ONCENTER — SPRING 2024
 Keith Hobbs took the helm as president/CEO of Torrance Memorial Medical Center in November.
Keith Hobbs took the helm as president/CEO of Torrance Memorial Medical Center in November.

For recreation, the family fixates on sports. Everyone roots for Trojan football, the Dodgers, the Rams, the Lakers and the Kings.
Golf is a big part of their lives. Hobbs taught everyone—starting with his wife. For their first date, he took Merilee to a local golf course and used swing-coaching as an excuse to put his arms around her. When it came time to pop the question five years later, he hid the engagement ring inside the ninth-hole cup.
All three kids grew into serious golfers—especially Amanda, who attended college on a golf scholarship. As youngsters, they had all played AYSO soccer with their dad as team coach. Hobbs himself is a former mini-triathlete, but he no longer competes. At 57, he gets his exercise playing pickleball; he’s a regular with the hospital’s Thursday night pickleball group.
LEARNING THE ROPES
Like his predecessor, Hobbs pours much of his energy into work. His 24-year career at CHLA spanned many roles. As administrative director of surgery, Hobbs led the 300-physician pediatric, multispecialty medical group and oversaw the USC-affiliated surgical residency program.
Later as vice president, he managed everything
from anesthesiology to laundry-and-linen to telecommunications. He spearheaded a pediatric vision center that’s now internationally recognized, cut the ribbon on a new 317-bed inpatient tower and helped expand CHLA’s Saban Research Institute.
In 2016 he moved from a CHLA vice presidency into the top job at USC Verdugo Hills Hospital, then a struggling community hospital within Keck Medicine of USC. In his first year as CEO, Hobbs ratcheted up the 158-bed facility’s net revenue by 50%. Over the following three years, he boosted financials by $20 million annually. He catapulted the low-ranked emergency department into the top 25% tier.
Among his other accomplishments at USC Verdugo Hills: Hobbs opened a neonatal intensive care unit, developed a teaching hospital program, crafted a physician network strategy, and drove the development and approval process to bring interventional radiology and catheter lab capabilities to the hospital. His decision to leave his hometown community hospital—a place he’d known all his life, part of a USC system he also knew intimately—was not undertaken lightly.
In accepting Leach’s plan for a gradual transition, Hobbs effectively was resigning as CEO to take up an executive vice presidency. To the casual observ-
14 ONCENTER — SPRING 2024
The Hobbs family, left to right: Carley Laliberte, Kameron, Merilee, Keith, Landon, Scarlett, Amanda, Corey Kimball
PHOTO BY PHILICIA ENDELMAN
er, it might look like a curious setback in an unblemished career. But the challenge was irresistible.
Listing his reasons for joining Torrance Memorial, Hobbs says, “The stature of this hospital, is top of the market in Southern California.” And “Being affiliated with Cedars-Sinai, which in my opinion is the health system of Southern California. The longevity and success of Craig Leach and the rest of the leaders—it was ultimately a no-brainer.”
Merilee was all in. “After we got married,” Hobbs recalls, “she asked if we ever had a chance to be closer to the ocean, would I consider it? I promised I would.”
The whole family has fallen in love with the South Bay. “Merilee loves to hike the different trails near our home in Rancho Palos Verdes,” he says. “And after six months, my boys, who still live with us, wondered why we hadn’t moved here years ago.”
A TRUE FIT
The executive search firm Spencer Stuart identified Hobbs through its “CEO succession planning” process. After a string of interviews, Leach and Torrance Memorial’s leadership gave Hobbs the vote of confidence.
Chief nursing officer Mary Wright, who is also senior vice president for patient services, vividly recalls her favorable first impression. “Keith was one of the very few candidates who could demonstrate how he collaborated with nursing—true collaboration, really solving problems together,” she says.
Hobbs’ rapport with physicians is equally robust. “From the very beginning, Keith went out of his way to engage with us and try to build relationships,” says Gray, who was medical director of the emergency department when Hobbs arrived in 2021. “His natural inclination is to fit in exactly with the way the culture at Torrance Memorial works. I remember him saying repeatedly how at home he felt here.”
That’s hardly surprising because Hobbs “fits in” almost everywhere. He prides himself on being a multifaceted leader, serving on the boards of the Torrance Area Chamber of Commerce and Communities Lifting Communities, a nonprofit focused on health inequities and housing for the homeless.
In the realm of health care governance, he is vice chair of the executive committee of the Hospital Association of Southern California, made up of CEOs across Southern California. He serves on the California Hospital Association Board, reviewing key health care legislation for the State. He’s also a fellow of the American College of Healthcare Executives and a member of the Medical Group Management Association.
Like his predecessor, Hobbs demonstrates an uncanny ability to steer clear of zero-sum options and find win-win solutions—all of which made it possible for November 1 to be just an ordinary Wednesday. Torrance Memorial’s new CEO possesses all the tools to build on a tradition of excellence while moving toward a rapidly evolving future. •
Vision for the future of Torrance Memorial
Some short-term goals are to get the academic medical center up and running, expand the ambulatory surgery center strategy and add solar power capabilities. That’s over the next two or three years. We’re also continuing to expand our Torrance Memorial Physician Network.
Some of our medium-term goals will be expanding the Lundquist Leach Emergency Department to double its current size, adding more treatment and consultation spaces. This expansion will greatly improve the patient experience while enhancing flexibility, efficiency and safety. We are evaluating several other campus expansion plans to increase capacity and meet the growing needs of our community. These projects should be completed between 2026 and 2030.
President and CEO Keith Hobbs is known for his friendly fist-bumps when he makes rounds in the hospital, embracing the culture of Torrance Memorial.

As for the long-term vision for the hospital, we own the Honeywell parking lot across the street. Through our affliatiion with Cedars-Sinai we also own the TorMed office buildings next to the West Tower. One of the greatest attributes of Torrance Memorial is it’s not landlocked. We have the ability to grow where most other hospitals in California can’t. We own our destiny. When the time is right, we will have the ability to add a new tower and new medical office buildings to serve the South Bay into the future.
TORRANCEMEMORIAL.ORG 15
Imaging provides information critical to diagnosis and treatment
Under the Surface
Written by Nancy Sokoler Steiner

16 ONCENTER — SPRING 2024
Photographed by Michael Neveux
Sam
Christine
Andy

Belal
William
Khalid
TORRANCEMEMORIAL.ORG 17
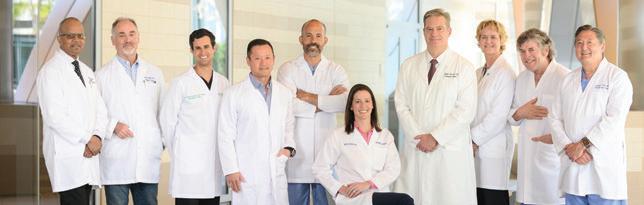
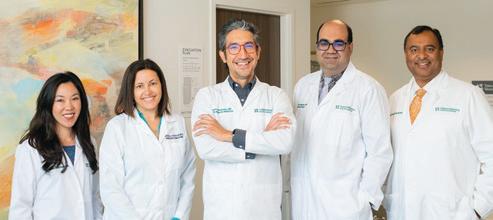
Imaging Department Managers and Leadership team, left to right:
Susan Castillo, Manager of MRI
Derek Berz, SVP and Chief Operating Officer
Rodriguez, Manager of Ultrasound
Thune, Manager of Diagnostic Radiology
Tran, Manager of Nuclear Medicine & PET/CT and Imaging Assistants
Yolanda Gonzalez, Manager of Imaging Nursing and 4E Outpatient
Dianna Tyndall, Radiology Clerical Supervisor
Madha, Manager of CT
Ogan, Manager of Interventional Radiology
Shariff, Director of Imaging Services
Naween Syed Ilyas, Imaging Educator
Struggling to breathe, the patient is rushed to the emergency department. The emergency physician orders a chest X-ray, which rules out pneumonia and other chest-related diseases. Next, the patient undergoes an ultrasound to check for a clot in his legs and a CT scan to look for clots in his chest. The CT scan reveals a pulmonary embolism—a clot in the arteries sending blood to the lungs. He then goes to the interventional radiology suite, where physicians pinpoint and remove his clot.
“At this point, the patient has undergone four modalities of imaging: X-ray, ultrasound, CT and interventional radiology,” notes Khalid Shariff, Torrance Memorial Medical Center’s director of imaging services. “Thanks to the skill of practitioners and advances in technology, the patient is able to go home the same day he experienced what was previously a fatal condition.”
Imaging reveals what’s happening inside the body, helping physicians diagnose and treat problems as well as confirm a problem was successfully treated. Using sophisticated equipment, Torrance Memorial’s team of more than 300 imaging technologists, radiologists, nurses and support staff provided 337,000 imaging procedures in the hospital last year. (Another 50 experts provide comprehensive imaging services at the Vasek and Anna Maria Polak Breast Diagnostic Center’s four locations.)
“Maintaining a state-of-the-art imaging department with cutting-edge technology and highly skilled professionals is paramount for a hospital’s diagnostic and interventional care capabilities,” says Derek Berz, senior vice president and chief operating officer. “Torrance Memorial continues to have advanced imaging capabilities that not only enhance the accuracy and efficiency of diagnostics but also enable specialized consulting, ensuring patients receive precise and tailored medical interventions. This ultimately elevates the overall standard of health care within
the institution.”
Imaging technologists must earn certification from an accredited program for their specific imaging modality, which takes at least two years. Torrance Memorial also requires its technologists to obtain state and national licenses. Because imaging is so crucial to providing care, the department maintains 24-hour staffing for most modalities. Technologists work in concert with radiologists as well as other physicians in the medical center.
“Our radiologists are always looking at evolving technology, and we in the imaging department have visited equipment manufacturing plants to see what they’re working on,” says Shariff. “This allows us to plan for equipment additions and replacements over the coming decade. We like to remain ahead of the curve.”
The medical center’s imaging department offers the full breadth of services including state-of-the-art technologies and procedures, some of which are typically found only in academic facilities. Each type of imaging has its unique function and uses:
X-ray:
How it works: When X-ray beams pass through the body, organs, tissues and bone absorb the rays at different rates. A detector converts this absorption into images.
When it’s used: Common uses for X-rays include detecting bone fractures, pneumonia and certain cancers. Portable radiography allows for digital images to be taken at the bedside. It helps physicians and nurses with procedures such as inserting and precisely placing ventilator tubes, feeding tubes and central lines.
Fluoroscopy:
How it works: A sort of continuous X-ray, fluoroscopy provides continuous, real-time X-ray video rather than producing single images.
When it’s used: Fluoroscopy helps physicians diagnose a range of problems, including gastrointestinal and cardiac con-
ditions, and issues involving the bladder, kidneys, musculoskeletal system and reproductive organs. For example, doctors can see a patient swallowing in real time. Fluoroscopy may also take place during procedures such as placing screws or plates during orthopedic surgery or inserting a catheter into the heart. Portable fluoroscopy allows for imaging at the bedside of patients too ill to be transported.
Ultrasound:
How it works: Ultrasound uses high-frequency sound waves to create images of organs, tissue or blood flow.
When it’s used: Commonly used to monitor the growth and development of the fetus during pregnancy, ultrasound also helps physicians visualize the heart and blood vessels, abdominal organs, brain, thyroid, skin and muscle.
CT (Computed Tomography) Scan:
How it works: The donut-shaped Computed Tomography Scanner uses rotating X-rays to produce cross-sectional images—or slices—of the body. Spectral technology provides images of anatomical features previously not available, such as certain tumors or calcifications. Torrance Memorial has multiple CT machines, as well as a Portable Cone Beam CT scanner—also known as an O-Arm—which makes this technology available right in the operating room.
When it’s used: Individual images and those combined to produce 3D images show bones, muscles, organs and blood vessels. They aid in diagnosing a wide range of diseases or injuries, including pneumonia, tumors, blood clots, strokes and bone fractures. CT can help guide lung biopsies and catheter insertions, among other procedures.
PET (Positron Emission Tomography) Scan and Nuclear Medicine:
How it works: Using the same equipment as a CT scan, positron emission tomography involves a patient intrave-
18 ONCENTER — SPRING 2024
nously receiving a small amount of a radioactive substance that allows for continuous images. PET and CT are frequently performed together.
When it’s used: Nuclear medicine provides functional information and enables early detection of certain diseases. It is used in cardiology for assessing heart function. The bone scans detect abnormalities, aiding in orthopedic diagnoses.
MRI (Magnetic Resonance Imaging):
How it works: MRI uses magnets and radio waves to produce images of organs and structures inside the body. MRIs typically require patients to be inside a narrow tube-like space, but Torrance Memorial’s MRI machines have a more open design and produce exceptionally detailed images.
When it’s used: Particularly helpful for examining the brain and spinal cord, MRI is used for practically all areas of the body, including the abdomen, chest and limbs.
Mammography
How it works: Using a special X-ray machine, a technologist places the breast between two plastic plates to be compressed. The compression flattens and spreads out the breast tissue. The breast stays under compression for about 10 to 15 seconds per image while the X-ray is being taken. The technologist takes a minimum of two images of each breast.
When it’s used: A mammogram can be a screening or diagnostic evaluation of the breast tissue to detect cancer or other changes in the breast.
Interventional Radiology:
How it works: Using catheters (small, hollow tubes) and tiny instruments, interventional radiologists perform image-guided procedures on veins and arteries. Many of the conditions treated with interventional radiology previously required open surgeries. Torrance Memorial recently completed a state-of-the-art Interventional Radiology Suite featuring biplane imaging, which uses two sets of cameras to provide re-
al-time 3D images that can be rotated to view anatomy at all angles (see sidebar).
When it’s used: Treatments performed by interventional radiologists include repairing blocked arteries, stopping gastrointestinal bleeding, and destroying tumors and fibroids.
Imaging physicians, nurses and technologists stay up to date on safety and best practices thanks to imaging services educator Naween Q. Syed. She creates and implements standard operating procedures for the department and trains department personnel to function safely and effectively.
The many scans and procedures performed by the imaging department require meticulous coordination. In August 2022, Syed oversaw the adoption and implementation of the Clinical Workflow Suite (CWS), a tracking system that monitors the status and timing of cases to ensure radiologists, staff, patients and equipment are deployed most effectively. “We were able to design CWS in a way that works best for our hospital,” Syed says.
The software helps the transportation room staff route technologists and patients most efficiently, thus minimizing wait times. “This is especially important in cases where time is of the essence, such as with stroke patients,” she says.
Torrance Memorial dedicates substantial financial resources to provide the finest imaging equipment and services. In addition, notes Shariff, “We’re lucky to have philanthropic support from the community for our department and the hospital in general. Community members see what we do and recognize the importance of the role we play.”
He adds: “Even more important than our sophisticated equipment and technology, it’s the commitment and skill of our people that makes our department so strong. I’m particularly proud of the longevity of our staff. Many have been here for 20+ years, and some have been working here for more than 40 years. That’s unusual, but it reflects the support of management, the institutional culture and the people we work with.” •

Impact on the Future
The new IR Suite at Torrance Memorial
Biplane imaging is one of the most advanced interventional medical technologies. It captures CT images of the (lying down) body from top to bottom and side to side. Biplane imaging brings enhanced precision to complicated vascular and neurological procedures by providing 3D anatomical views in real time. Torrance Memorial Medical Center created the new Interventional Radiology Suite with biplane imaging, thanks to the generous $5.1 million donation from Patricia and Gerald Turpanjian. The suite, which debuted in the summer of 2023, has been used for such procedures as opening blocked or narrowed blood vessels, repairing aortic aneurysms and administering clot-busting medications to treat stroke.
TORRANCEMEMORIAL.ORG 19

Multiple Pathways to a Health Care Career
Inspiring the next generation of medical professionals
Written by Laura Roe Stevens | Photographed by Philicia Endelman
Nearly 180 local high school students gathered at Torrance Memorial Medical Center on December 9 to learn about options for working in the health care industry. At the first annual Healthcare Career Exploration Day, Torrance high school students met with physicians, nurses, medical staff and medical device and pharmaceutical vendor reps who gave presentations and provided live-action demonstrations.
The hands-on activities were a big hit among the students. These insightful exercises included teaching students how to use a da Vinci surgical robot, which is used to remove brain clots; demonstrating how to operate ultrasound equipment and accurately read the results; working with pharmacy specialists to compound medicine; teaching students how to draw medicine with
a syringe; exploring 3D technology; and demonstrating an AED machine that delivers electric shock to someone experiencing cardiac arrest.
“We were excited to collaborate with the Torrance Unified School District and to connect with the students to inspire and educate them about the various career opportunities within the health care industry,” says Andrew Lee, PhD, director of health equity and talent management at Torrance Memorial. “Our vision is to help them learn, explore and grow. And we hope to build a long-term relationship and to spark interest too, as there is a dire need for talented people to enter the health care field.”
In fact, an additional 500,000 new health care professionals—including medical assistants and imaging
20 ONCENTER — SPRING 2024 Life & Health
A Torrance Unified School District student engages in a hands-on demonstration exploring 3D technology.
specialists—are needed in the state, according to the California Hospital Association (CHA). The CHA report estimates more than 22% of Californians live in areas that lack sufficient primary care providers. While the South Bay may not qualify as one of those areas, Lee says Torrance Memorial needs more health care professionals as it continues to grow and meet community needs.
One of the daunting aspects of pursuing a medical career is the rising costs of higher education. This event highlighted the many careers outside traditional medical or nursing school routes, including positions within radiology, pharmacology, physical and occupational therapy, technology, finance and security.
Makenna Esparza, a sophomore at North High School, said the event was eye-opening. “Before this (career exploration day), I was a little lost. I knew I wanted to pursue a medical career, but this event gave me clarity,” Makenna says. “And it showed me there are more openings in what I want to do.”
In a post-event survey, students agreed overwhelmingly the Healthcare Career Exploration Day was a success and provided valuable information. When asked what their favorite parts of the day were, one student replied: “Everything! Especially about radiology and the IT health care information.”
Most students agreed the hands-on booths were a highlight. One student wrote: “My favorite part was dealing with the robotics and with the virtual reality [equipment]. I now know what path I will take after high school.”
For the health care professionals and educators who worked so hard to put the Torrance Memorial Healthcare Career Exploration Day together, it just doesn’t get any better than that. •



Top: Local high school students exploring options for a future career in health care.
Bottom: Medical device vendor rep and interventional radiologist Dr. George So use an ultrasound machine to demonstrate how highfrequency sound waves create images of organs, tissue or blood flow.
Torrance Memorial Physicians Teach Biomedical Series
Did you know both El Segundo High School and Da Vinci High School have biomedical pathway classes? Or that Torrance Memorial physicians and clinical educators volunteer their time to teach these students monthly? It’s all part of Torrance Memorial’s outreach effort to inspire the next generation of health care workers, says Mary Ford, coordinator of community outreach for the hospital.
“This series is amazing. One month respiratory therapist Anthony Co brought in a case study of a child with asthma,” Mary explains. “The students developed an action and rescue plan as part of their third-year study in the biomedical pathway series. That was huge. The students got so much out of it.”
TORRANCEMEMORIAL.ORG 21
Panelists Mary Matson, director of service excellence, patient experience and volunteer services; Naween Syed, imaging educator; and Chris Bacon, director of employee health services and occupational health and safety, field questions from students about a career in health care.
Torrance Memorial’s Six-Year Affiliation with Cedars-Sinai Brings Life-Saving Treatments to South Bay Residents
Written by Lisa Buffington

When Torrance Memorial Medical Center and Cedars-Sinai began their affiliation in 2018, the organizations made a shared commitment to bring South Bay communities the gold standard of care. Six years later, the team continues to deliver on that promise. In collaboration with the leading academic health system, Cedars-Sinai, patients have access to the latest technology, advanced treatment options and more clinical expertise in the areas of neuroscience, oncology and cardiology.
ADVANCING COMMUNITY-BASED CARDIOVASCULAR CARE
Torrance Memorial’s affiliation with Cedars-Sinai means South Bay residents can receive everything from advanced cardiac surgery procedures and minimally invasive heart valve care to extracorporeal membrane oxygenation (ECMO) and pre- and post-heart transplant treatment, close to home.“
We can offer Torrance Memorial patients the same expertise, investigational devices and therapies available at Cedars-Sinai—options not previously available in the South Bay,” says Aziz Ghaly, MD, Cedars-Sinai
22 ONCENTER — SPRING 2024 Life & Health
cardiac surgeon and director of cardiac surgery at Torrance Memorial’s Lundquist Lurie Cardiovascular Institute. “In addition to expanding our capabilities to treat high-risk and complex patients at Torrance Memorial, we can also make immediate referrals to our colleagues at Cedars-Sinai if a patient needs an advanced procedure, such as a heart transplant.”
For cardiac emergencies, Dr. Ghaly performs complex cardiac surgeries and minimally invasive procedures such as temporary Impella heart pump placement. Torrance Memorial’s ECMO program is another example of the life-saving benefits of local access to advanced care, according to Dr. Ghaly.
“Torrance Memorial is the only medical center in the South Bay—and one of the few non-academic medical centers in southern California—to have an ECMO machine, which means we can offer temporary heart and lung support for critically ill patients,” says Dr. Ghaly. “As a result, we were able to save many lives during COVID-19 because we could care for patients locally and didn’t have to transfer them.”
EXPANDED ONCOLOGY SERVICES AND CLINICAL TRIALS
Hugo Hool, MD, medical director of the Hunt Cancer Institute, an affiliate of Cedars-Sinai Cancer, has been involved with the affiliation since its inception—and he has witnessed the benefits of the collaboration firsthand.
“Years ago, if a patient in our community had an aggressive form of cancer and they didn’t have support or transportation to travel to an academic medical center, they may not have had access to the best care or outcomes,” says Dr. Hool. “Now, patients can access stellar care locally, right where they live.”
And that access has expanded over the years. The affiliation with Cedars-Sinai Cancer started with a focus on blood and breast cancer care and has since grown to include Cedars-Sinai experts who provide surgical oncology, head and neck cancer, neuro-oncology, thoracic surgery, pancreatic cancer/biliary disease and genitourinary cancer care support at Torrance Memorial.
Through the Cedars-Sinai affiliation, Dr. Hool and the Hunt Cancer Institute team are also involved in dozens of clinical trials for advanced therapies that aren’t widely available.
“This early access to promising treatments benefits hundreds of patients who enroll each year and ultimately from the research we perform,” says Dr. Hool. “Our researchers are now able to use an individual’s tumor DNA to direct them to the specific trial tailored to deliver the best chance of an improved outcome.”
Current clinical trials available to patients include studies on chimeric antigen receptor T-cell therapy (CAR-T), which involves engineering T-cells to fight cancer, and a newer iteration of that therapy called CAR-NK therapy, which uses natural killer cells. Physician-researchers are also investigating emerging therapies such as bispecific T-cell engagers and antibody drug conjugates, as well as radiation oncology and interventional radiology treatments.
The oncology team also emphasizes holistic patient care that goes beyond just treating the cancer. “Our integrative medicine program provides supportive therapies to augment cancer treatment so we can care for the whole patient,” says Dr. Hool. “We are also involved in clinical trials focused on improving quality of life and well-being for our patients in a scientific way.”
LEADING THE WAY IN NEUROLOGY CARE
Neurological conditions are among the most complex to diagnose and treat. Through the affiliation with Cedars-Sinai, Torrance Memorial has been able to expand its expertise and access to more neurological services. The neurologists, neurosurgeons and neurointerventionists at the Torrance Memorial Lundquist Neurosciences Institute offer leading-edge, collaborative care and clinical trials to successfully treat a wide range of neurological disorders, including serious stroke, brain tumors, movement disorders and more—all without leaving the South Bay.
“We can perform the full range of complex neurosurgeries, including vascular, endovascular and brain tumor surgery,” says Paula Eboli, MD, director of endovascular and neurosurgery. “Our goal has been to bring the highest level of expertise to the South Bay through our affiliation with Cedars-Sinai, and we have built a very successful program.”
In addition to the Institute’s experienced team, patients also have access to more subspecialty services, including the new Torrance Memorial Movement Disorders Clinic.
“The Movement Disorders Clinic is definitely meeting a need in our community,” says Heidi Assigal, senior vice president of business and operations, Torrance Memorial Physician Network. “For patients who are living with a movement disorder, traveling to an academic medical center for care may be challenging. That’s why we wanted to bring convenient, coordinated care from academic medical center experts closer to home.”
“Our affiliation with Cedars-Sinai has made Torrance Memorial even stronger. It’s led to new clinical trial access, and newfound resources, investments and collaboration that comes with being a part of a leading academic health system,” says Torrance Memorial president and CEO Keith Hobbs. •
TORRANCEMEMORIAL.ORG 23
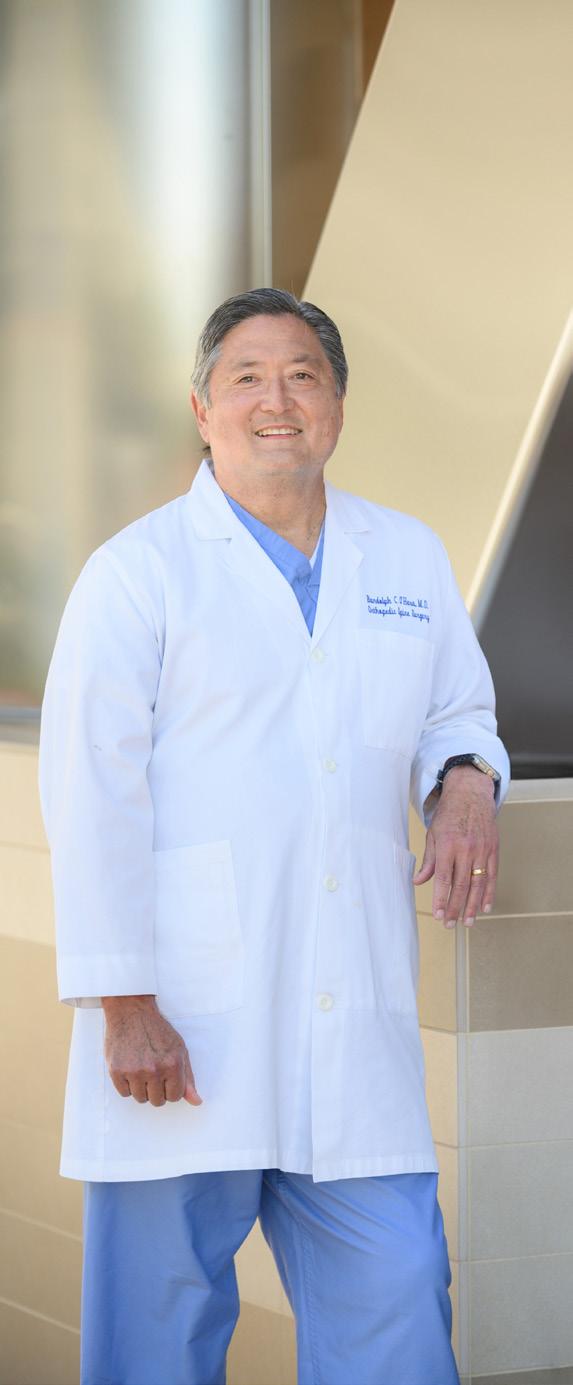
“Being a patient gave me a whole new perspective.”
– Dr. Randolph O’Hara
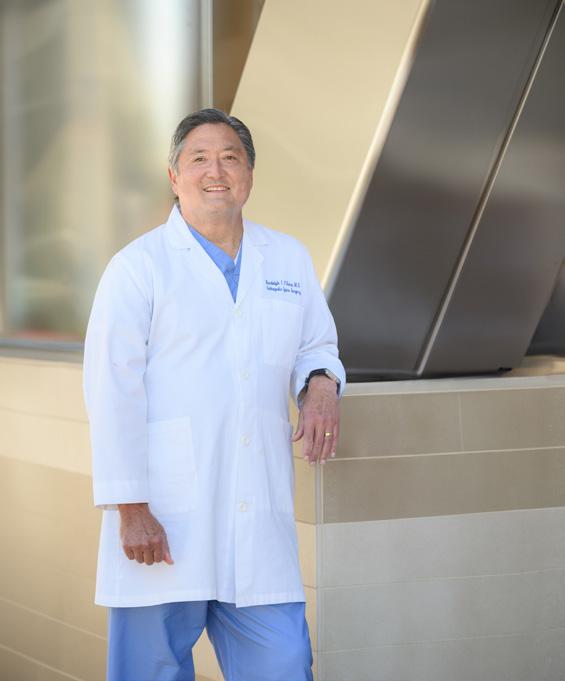
Physician and Patient at Torrance Memorial
“Exceptional care, exceptionally close” is the right choice for Dr. Randolph O’Hara.
Written by John Ferrari | Photographed by Peter Cooper
Exceptional care, exceptionally close. Torrance Memorial’s promise means a lot to South Bay residents and patients. It means even more to the hospital’s physicians when they become patients.
Whether you’re at the hospital for a routine physical exam, diagnostic procedure or surgery, doctors are the voice of authority. But doctors are patients too, with all the concerns any patient has.
“I thought I’d go in and my cholesterol would be a little high, and that would be that,” says Torrance Memorial orthopedic surgeon Randolph O’Hara, MD, referring to his annual (and overdue) checkup with his primary care physician, Rumi Cader, MD. His cholesterol was high, but Dr. Cader also noticed a high heart rate and ordered an electrocardiogram. It revealed atrial fibrillation (A-fib), an irregular and often very rapid heart rhythm.
A-fib is not uncommon, affecting some 5 million adults in the United States. Still, Dr. O’Hara was surprised. “I’m in my early 60s. I do cardio exercise regularly, on the elliptical and the rowing machine,” he says. “I had no symptoms.”
That’s a hallmark of A-fib—it’s often asymptomatic until a diagnostic test uncovers it. (A-fib also can be symptomatic. The most common symptoms include a noticeably rapid heartbeat or heart palpitations, dizziness, shortness of breath, weakness, fainting or fatigue—all of which are symptoms of many other conditions too.) A-fib is associated with a fivefold increase in the risk of stroke.
Dr. O’Hara also has a family history of heart attacks. With that in mind as well as his newly diagnosed A-fib, Dr. Cader referred Dr. O’Hara to a Torrance Memorial cardiologist, Eric Castleman, MD. Dr. Castleman ran several tests including a coronary calcium scan to identify any calcium buildup narrowing the coronary arteries, and an angiogram to reveal narrow or blocked arteries. The test results revealed significant coronary artery disease: three of Dr. O’Hara’s arteries were narrowed, two of them by 80%.
24 ONCENTER — SPRING 2024 Life & Health
Dr. O’Hara was referred to cardiothoracic surgeon John Stoneburner, MD, who recommended a triple bypass and cardiac ablation surgery—a complex combined procedure but the best option. Dr. O’Hara could have opted for treatment at one of SoCal’s large university or research hospitals but chose Torrance Memorial for the staff’s experience and capabilities.
“I’ve been involved with Torrance Memorial for about 30 years,” he explains. “I know the staff very well, and I’ve seen the staff grow over the years. For me, having that relationship with the staff over all these years means I had complete confidence in them. Plus I know Torrance Memorial has state-of-the-art technology.”
Bypass surgery to treat blocked or narrowed arteries is a well-known surgery; cardiac ablation is less so. The procedure uses heat or cold to cause targeted micro-scarring in the heart, blocking the electrical signals that cause arrhythmia. While cardiac ablation can be performed as a minimally invasive procedure using a catheter inserted into the heart, “that doesn’t work as well on patients with persistent atrial fibrillation” like Dr. O’Hara, Dr. Stoneburner says.
Dr. Stoneburner couldn’t leave the A-fib untreated though. “It’s like the timing on a car,” he explains. “When the timing is off, the car loses power. It’s hard on the car’s engine; it won’t last as long. But A-fib is worse than just an engine timing issue because A-fib can cause blood clots, potentially leading to a stroke.”
In Dr. O’Hara’s case, Dr. Stoneburner was able to use a new technology: the EnCompass Clamp, which increases the speed and efficiency of surgical ablations. The surgery—both the bypass and the ablation—took less than four hours. Although he has been performing ablations for 10 years, “a lot of people don’t know tachycardia can be fixed with ablation—catheter-based or surgical,” Dr. Stoneburner says. “There are good options for surgical or minimally invasive procedures, and they work.”
Dr. O’Hara spent five days in the ICU recovering from his cardiothoracic surgery, which he says was “an absolutely humbling experience that gave me a whole new perspective. You rely on the ICU nurses and staff. They were fantastic. I think they’re that way with everyone—they have to be to do their jobs.”

Rumi Cader, MD, FACP, MPH Specialites: Internal Medicine and Primary Care

Eric Castleman, MD Specialties: Cardiology and Interventional Cardiology

John Stoneburner, MD Specialties: Cardiothoracic, Vascular and Thoracic Surgery
That was last winter. Dr. O’Hara was able to return to work—albeit slowly—six weeks after his surgery. He was back to performing his own surgeries a month after that. That points to the beauty of preventive heart surgery, Dr. Cader says. Because Dr. O’Hara’s coronary disease was treated before it led to a stroke or heart attack, there are no limitations on his activities.
“Once someone has had a heart attack, there can be a weakness of the heart muscle that can lead to problems like congestive heart failure. By opening coronary arteries and preventing a heart attack, we’ve opened the patient’s options. For Dr. O’Hara there are no contraindications to do everything he wants to do.”
Dr. O’Hara is making some changes, though, to stay healthy—like improving his diet to lower his cholesterol level. “That’s a work in progress,” he admits. “I’m more aware of how I’m feeling and trying to keep from working too much, to balance a little more.”
Dr. O’Hara and his wife recently downsized, moving from Palos Verdes to Hermosa Beach. “We had a big house, but we had to drive everywhere,” he notes. “Now we can walk to restaurants and the beach. The house also happens to be right next to one of our offices.” Dr. O’Hara does plenty of walking: 5 miles along the beach most mornings before his workday begins.
Besides improving his physical health, the walks give him time to think and reflect. “Looking back, it was a great experience for me,” he says. “I have to give kudos to Dr. Cader. He’s the one who started the whole thing.”
For his part, Dr. Cader says this is the kind of case—and outcome—he likes to see. “We were fortunate to catch and treat the problems before Dr. O’Hara had a heart attack,” he explains. “Everyone 18 and older should have annual exams. Most people don’t have any notion they have cardiac risk factors—hypertension or hyperlipidemia—until they experience something serious later on, like a heart attack. These are the cases we love as physicians because we save lives this way—the ones where you prevent something potentially catastrophic. That’s the beauty of seeing your doctor and preventing these things from happening.” •
TORRANCEMEMORIAL.ORG 25

In Service of Others
What inspires someone to volunteer time outside their work, particularly those in the health care profession?
Written by Julie Taylor
Many of our dedicated Torrance Memorial health care professionals view their work as more than just a job—it’s a calling. This innate desire to help others often extends into their personal lives, motivating them to continue serving their communities through volunteer work.
Health care professionals witness the impact of illness, injury and other challenges firsthand. This exposure can instill a commitment to make a positive difference beyond their day-to-day job and contribute to a broader cause with compassion and empathy.
Volunteering can provide many benefits to those who give of themselves, such as personal growth, improved mental health and a sense of fulfillment. It offers opportunities to develop new skills, share expertise, expand social networks and gain a broader perspective on life. Connecting with individuals from diverse backgrounds and developing meaningful relationships outside one’s professional circles can be rewarding and inspiring.
The following stories shared by Torrance Memorial employees contribute to our health system’s culture of compassion, altruism and service to others. Would you like to share your volunteer experience for a future issue? Please connect with us at OnCenter@tmmc.com.

Honoring college-bound mentees, Barbara Demming Lurie and Mark Lurie, MD, celebrate their success at the PSP graduation ceremony.
Mark Lurie, MD, and Barbara Demming Lurie
Physician Mark Lurie retired in June as the medical director of the Lundquist Lurie Cardiovascular Institute after four decades of service. He and his remarkable wife, Barbara, have been mentors in the Partnership Scholars Program (PSP) for the past 13 years. This nonprofit matches low-income, motivated middle and high school students with prescreened volunteer mentors who act as friends, coaches, companions, role models and one-person rooting sections.
Volunteers like the Luries help kids bridge the cultural divide by engaging in community activities and encouraging their pursuit of higher education. Their involvement has been a particularly enriching experience for them, and Dr. Lurie never misses an opportunity to share his love of The Ohio State University and “The Best Damn Band in the Land” with these young, impressionable mentees.
How successful is the PSP? Ninety-six percent of the students have gone on to four-year colleges, landing an average of over $112,000 in scholarship aid. To learn more, visit partnershipscholarsprogram.org.

The Luries treat mentees to The Ohio State Rose Bowl experience.
26 ONCENTER — SPRING 2024 Life & Health

Stacey Shames
Stacey Shames, RN, is the lead nurse of the ICU burn and wound unit at Torrance Memorial. For the past 24 years she has volunteered one week of her time every summer at Champ Camp. Created in 1971, Champ Camp is supported by the Alisa Ann Ruch Burn Foundation, established after Alisa perished at age 8 in a backyard barbecue accident in Southern California.
Champ Camp is a weeklong, residential summer camp for child burn survivors ages 5 to 17 who have been treated at California hospitals or are current residents of California. Approximately 150 children attend this experience at Wonder Valley in Sanger, California, each year.
Sean Yokoe
When Sean Yokoe, RN, director of progressive care services at Torrance Memorial, first heard about the fires in Lahaina, Hawaii, his first thought was to check in with his friend Zac Yamada, who grew up on the island of Maui, and offer to help. Zac connected Sean with his sister, Char, who lives in Nāpili, the neighborhood next to Lahaina. She is involved in the Nāpili Noho’ charity group, which distributes donated food, produce, dry goods, hygiene items and more. They also serve as a site for health services, lomilomi, job and benefits assistance, and internet access. The focus is to aid those most directly affected and displaced by the Lahaina fire disaster.
Without hesitation, Sean and his wife, Veronica, booked their flights and signed up to join the effort. The couple volunteered for two days, helping distribute food and supplies. It was a humbling experience talking to people who lost so much and are still displaced after losing their homes and places of employment, Sean says. The community was very thankful and welcoming, and it made the trip unforgettable. Sean would like to thank the Torrance Memorial employees who donated to charities supporting Lahaina residents. To learn more, visit napilinoho.com.
Champ Camp is free to all burn survivors, and it is fully staffed by medical doctors, nurses, program staff, volunteers and counselors—many of whom are also burn unit nurses, burn doctors, adult burn survivors and firefighters. Activities at the camp include fishing, horseback riding, crafts, canoeing, archery, waterslides, campfire, dance and team-building activities. Stacey loves being involved because the camp’s focus is for burn survivors to have fun and just be kids away from medical procedures and financial hardships.
Campers can also engage with other kids who bear similar burn wounds without feeling different. Champ Camp provides a safe environment where burn survivors can play, learn, grow, gain self-esteem and make new friends.
To learn more, visit aarbf.org/project/ champ-camp.


Kelli Vieweg
After spending a career in human resources and development, information technology and finance, Kelli Vieweg retired and found she had some time on her calendar. She actively volunteered with her daughter in the National Charity League and enjoyed the experience, which led her to volunteer at Torrance Memorial for the past two years. Currently serving on the Auxiliary’s board of directors, Kelli’s volunteering doesn’t stop at Torrance Memorial.
After helping her mother through a breast cancer journey, she became engaged with Cancer Support Community South Bay (CSCSB). The mission of CSCSB is to uplift and strengthen people impacted by cancer by providing support, fostering compassionate communities and breaking down barriers to care. Considering her career expertise and strengths, she quickly found a niche in mentoring, reaching back in and being able to help and advise the group. Now, almost five years later, Kelli serves as president of the board of directors and has helped create brand awareness of the global network, normalizing the conversations around cancer.
In a tribute to her Navy veteran father, Kelli also spends time as an online mentor for America Corporate Partners (ACP), based in Virginia. ACP’s free Mentoring Program connects post-9/11 veterans, active-duty spouses and eligible military spouses with corporate professionals (mentors). By leveraging her career expertise and strengths, Kelli is a valuable mentor and life coach, helping veterans transition into civilian work with confidence and success.
To learn more, visit cscsouthbay.org and acp-usa.org/mentoring-program. •
TORRANCEMEMORIAL.ORG 27
Sean and Veronica Yokoe volunteer at Nāpili Park—the community-based emergency distribution hub dispensing mother/baby supplies set up by the Nāpili Noho’ group.
Camp counselors, Bacon, Snoopy (aka Stacey Shames), camper and past burn patient Gladys Solis, and Carrot Sticks being silly at Champ Camp.
Kelli Vieweg with Jillian Van Leuven, executive director of Cancer Support Community South Bay
PHOTO: STEVE TABOR





3330 Lomita Blvd. Torrance, CA 90505 310-325-9110
NONPROFIT ORGANIZATION U.S. POSTAGE PAID PERMIT NO. 381 TORRANCE, CA
www.TorranceMemorial.org
































 Keith Hobbs took the helm as president/CEO of Torrance Memorial Medical Center in November.
Keith Hobbs took the helm as president/CEO of Torrance Memorial Medical Center in November.