Galveston Island Beach Patrol improves island health, safety

IN THE FIELD




UTMB expert physicians speak to EMS agencies regularly on emergency medicine topics
UTMB emergency doctors share their expertise with area EMS agencies on various topics.
For example, four UTMB experts spoke at the Webster Fire Department earlier this year.
Each doctor shared an hour-long presentation. In the morning, Dr. Marie Dawlett spoke about pediatric emergencies, and Dr. Dispu Patel talked about heart attacks. After lunch, Dr. Hoang Pham addressed trauma, and Dr. Hashem Shaltoni discussed stroke. During lunch, UTMB staff answered questions.
Also, Drs. Dawlett, Patel and Pham spoke to Santa Fe EMS earlier this year. Joining them was Dr. Arun Chhabra, who discussed stroke.
UTMB Health offers this type of lecture series and similar lunch-and-learn events to area EMS providers. UTMB provides the experts and the lunch at your location.

To arrange a similar educational opportunity for medics at your organization, contact Richard Arocho at (281) 939-6822.
The Dispatch is a publication of UTMB Health and is produced by UTMB’s Office of Marketing and Communications quarterly for our EMS partners. The purpose of this publication is to celebrate the incredible work of the EMS agencies in our communities while sharing news about the services available at UTMB’s Emergency Rooms.
This newsletter is focused on telling your stories, answering your questions and sharing your successes. Send us your questions, your story ideas, your photos or any EMS-related news you’d like to brag about to EMS@utmb.edu
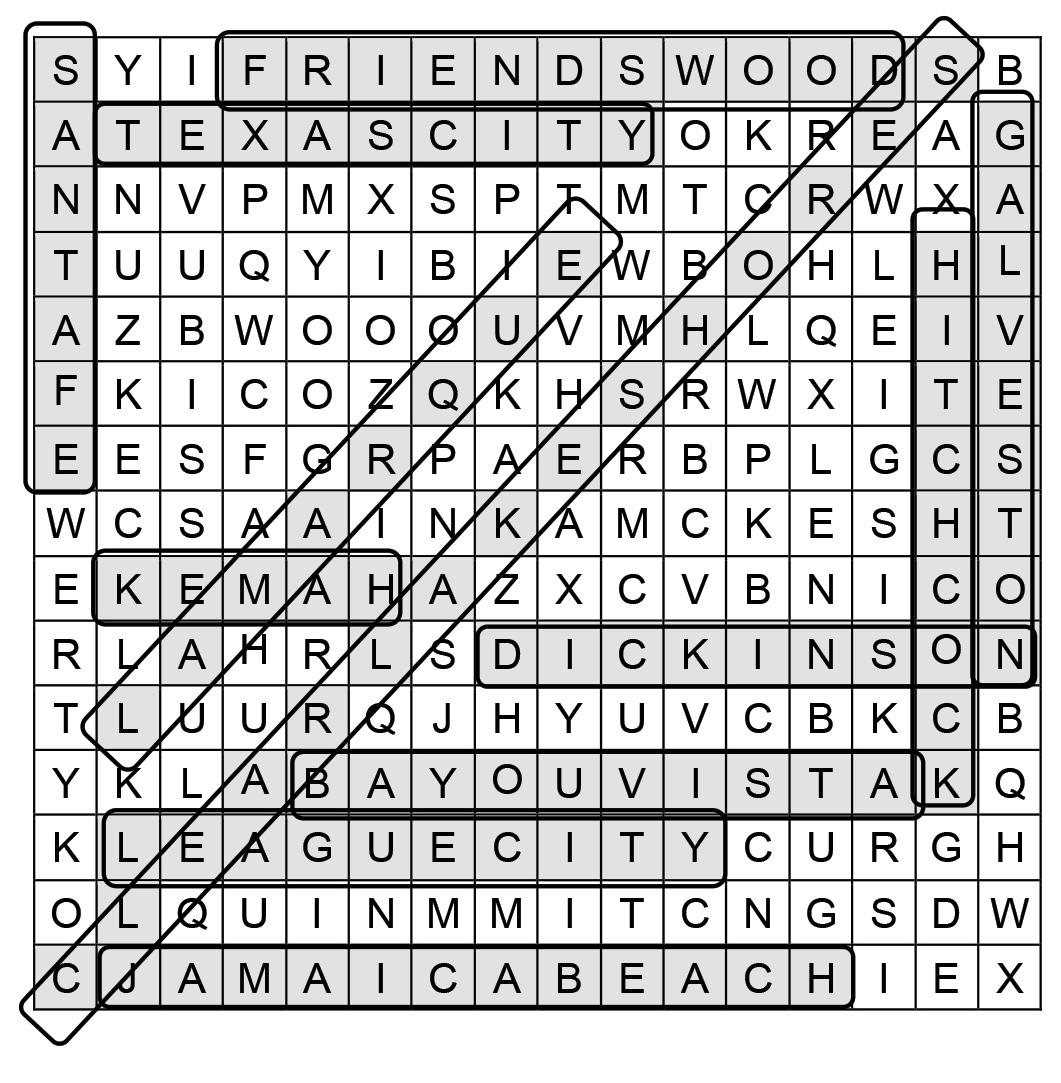
A E S D R C H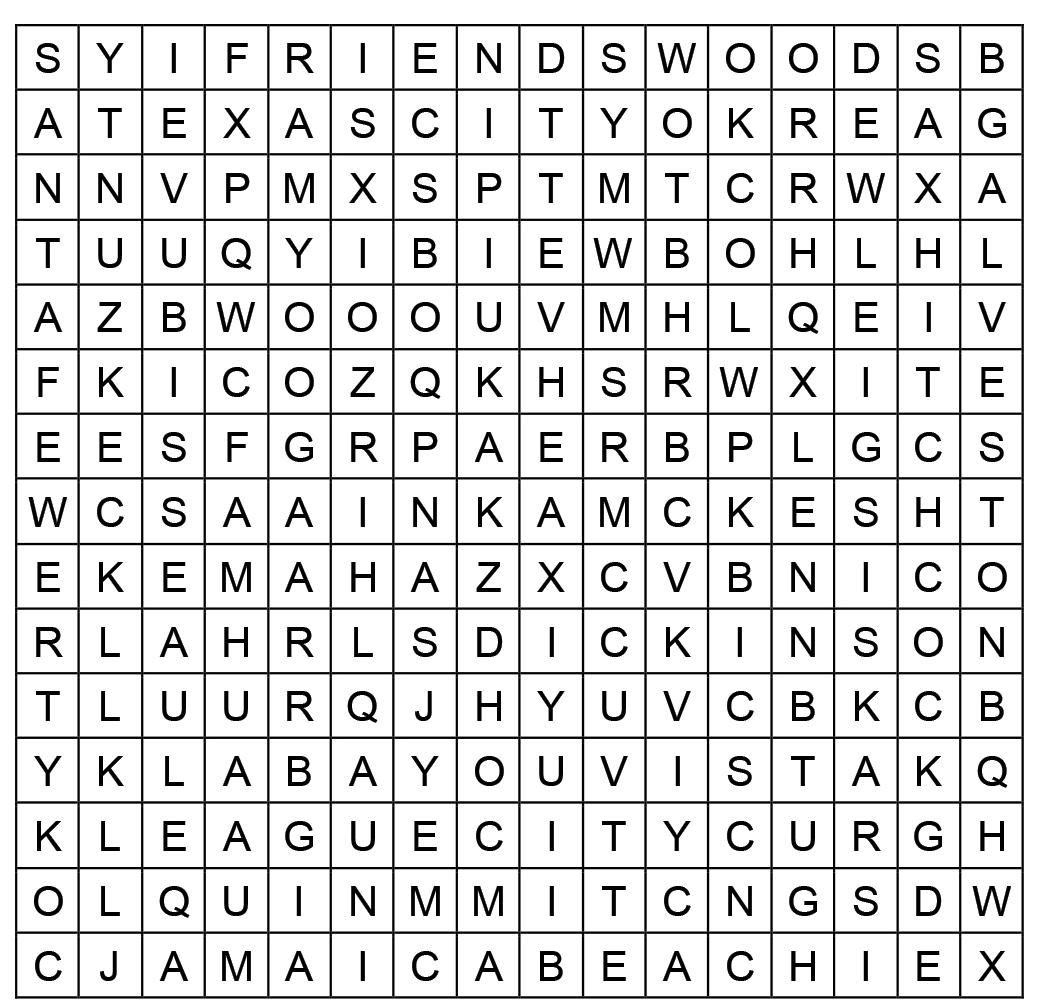
Solution is on the back page*

For a swimmer caught in a rip current, floating unresponsive in frigid waters off Galveston in the heart of winter, the two or three minutes it can take to get to shore can mean the difference between life and death.
And while Galveston Island Beach Patrol enjoys a symbiotic partnership with the island’s police and fire department and other EMS personnel, water rescues are one area that sets it apart.

Beach Patrol Chief Peter Davis, who has been guarding the Galveston beach and its waters for nearly 40 years, shared a story about his colleague, Beach Patrol Capt. Tony Pryor, who went into the cold surf to rescue someone who was caught in a rip current at 59th Street.
“When he got to him, he wasn’t breathing,” Davis said. “Tony drifted around through the poles at 61st Street and brought him back to shore. And while they were in the water,
he was able to start rescue breaths and the patient was breathing when he brought him to shore.
“That kind of early intervention is critical because if you think about it, had Tony not done that and drifted that two minutes or so that it would take him to get him to shore, then the person could have gone into, cardiac arrest,” he said. “So, a lot of the areas that we can specialize in are related to medical response involving water where other groups aren’t able to get in there and do that stuff.”
As for the rescued man, “he ended up being fine,” Davis said.
The job of the Beach Patrol has five components, according to Beach Patrol Sgt. Dain Buck: protect, rescue, enforce, prevent and educate.
Davis breaks that down. Water safety, including prevention and response is No. 1, followed closely by medical response.
Galveston EMS was the first emergency services group in the country to carry portable continuous positive airway pressure (CPAP) machines in its ambulances in the late 1980s and early 1990s. Galveston Island Beach Patrol partnered with EMS in using the portable devices to help to clear the lungs of near-drowning victims.
Today’s portable CPAP machines are better than the originals: slimmer, smaller and more portable. The improvements were the result of studies done with Galveston EMS and Beach Patrol using them early on.
Fully staffed, Beach Patrol has about 155 members, including dispatchers, office support, lifeguards, senior lifeguards, supervisors and 12 full-time rescue staff.
20 members are EMTs (a requirement for supervisors).
Then comes enforcement of beach etiquette and behavior. Finally, there’s education of the public, which are preventions that happen before people even arrive to the water.
“The big overriding thing that envelopes all that is public education,” Davis said, explaining Beach Patrol aims for “herd immunity” when it comes to water safety.
“Yeah, we stole that. I guess we stole that from public health,” he said. “I feel like if we could be as proactive as possible—not just in what we’re doing on the beach, but also what we do for people before they get to the beach—that they’re better protected. And so, we do our annual school outreach program. We teach about 30,000 kids a year, just in the county on up to the Houston area. We’re trying to affect a public health concept with immunization, except it’s with water safety information.
“The idea is if a group of kids goes out and more than half of them have a basic concept of how to be safe in the water, like avoiding rip currents or not going in certain areas, then overall the group will be protected,” Davis said.
What it takes Fully staffed, the Galveston Island Beach Patrol has about 155 members, including dispatchers, office support, lifeguards, senior lifeguards and supervisors. Each of its 12 emergency response vehicles is required to always have an EMT on board, so all 12 of the patrol’s supervisors are EMTs. All the guards are, at a minimum, certified in “Emergency Response” through the Red Cross.
“Beach Patrol EMTs deal with a lot of nature and other nonmedical factors, including unsafe scenes,” Buck said. “The first step for a Galveston Island Beach Patrol EMT is getting the victim to a safe area.
They are often in a dire situation that has them in a dangerous area, be it the middle of the ocean or bay or stranded on a sandbar or jetty.”
Since water rescue is at the heart of what Beach Patrol does, water skills are critical, and the criteria for swim standards are high. Jet Ski prowess is vital, as well as proficiency with rescue boards and other specialized equipment. Beyond that, Davis said, compassion is an essential competency.

“If you don’t have that sort of base of liking to work with people and liking to help them, then this job gets really hard and annoying quickly,” Davis said.
“Cultural competency” also is important—especially in a town that attracts visitors from all over the world, he said.
“Everybody doesn’t come from
the same perspective as you do. So, you have to kind of get in people’s heads when you’re trying to help them,” Davis said, explaining that even how bodies of the deceased are handled can vary in different cultures. “A certain level in intercultural competency really makes the job more enjoyable, but it makes you also a lot better at it as well.”
For Buck, dedication to the job and the ability to stay calm in intense situations are the characteristics that set the men and women of Galveston Island Beach Patrol apart.
He talks about a rescue on an evening in November 2019 when a boat wrecked onto Galveston’s South Jetty about a mile and a half offshore, when he and Beach Patrol Supervisor Kevin Anderson responded. A large incoming storm made it impossible for them to launch a
marine rescue boat.
“We then were to assist Coast Guard with the rescue as they flew their helicopters out to the stranded fisherman,” Buck recalled. “Unfortunately, both helicopters were unable to launch. We then took it upon ourselves to swim all the way out to the stranded fishermen on the leeward side of the jetty protecting us from the harsh weather. It was pitch black, winds howling at 30+ mph and the temp dropping to below 50 degrees.
“After about a 45-minute swim, we were able to locate the fishermen,” he said. “While checking the vitals on all the stranded fishermen we were able to have another beach patrol member launch a Jet Ski after approval for the night rescue. After about three hours, we had all the fishermen back to shore healthy and happy.”
- Chief Peter Davis Galveston Island Beach Patrol“Beach Patrol EMTs deal with a lot of nature and other non-medical factors, including unsafe scenes.”Lifeguards train regularly to save lives.
For many of the lifeguards, it’s their first job.
Beach Patrol is the first responder to all coastline and oceanic calls, Buck said. They work closely with the island’s medical response agencies, who can provide more advanced life care and transport patients to the hospital.
Like other first-responder organizations in Galveston County, Beach Patrol is registered with the county health district, with the same medical directors as EMS, Davis said, so the protocols are the same.
“We’re all speaking the same language out there,” he said.
Beach Patrol’s medical training and police enforcement capabilities also allow the organization to lighten the load for the island’s emergency services and police personnel.
Calling it “catch and release,” Davis said that only a small percentage of the 2,500 to 3,500 medical calls beach patrol responds to each year have to be transported to the hospital by EMS. In the same vein, he said, the 3,000 law enforcement calls Beach Patrol handles each year take a burden off local police.
Beach Patrol has its own police department, of which Davis also is chief.
services and beach patrol have worked together to ensure the health and safety of island residents and tourists for decades, Davis said, adding he personally learned from some “paramedic giants” on the island in the 1980s.
“We’re really aware of that legacy and that connection with EMS as a partner for us,” he said. “Just like they’ve always been there for us anytime we ever need anything, we want to make sure that they’re aware that we want to reciprocate. If there’s anything they ever need from us, we’re always there for them.
“We’re constantly in contact with them to adjust policies and to make sure we’re all working on the same page,” he said. “And they’ve just consistently always been there for us anytime we needed anything.”
Beach Patrol also has a close relationship with UTMB.

“We rely heavily on EMS and UTMB Galveston for all of our major calls,” Buck said. “When we have any major medical, be it cardiac arrest or near drowning, we always have our patients checked out by EMS and transported to UTMB for further medical care.
“We will check on our patients after the initial care to see what
the end result is,” Buck said.
Beach Patrol works closely with UTMB to ensure that its air- and water-quality reports are communicated to beachgoers, as well, Davis said.
Davis is famously proud of his team, especially, he said, by the level of professionalism that even the youngest and newest members exhibit. For many of the guards, some as young as 16, it’s their first job ever.
“We have a really good training program, but it’s really amazing to watch them use that and rise to the occasion for doing such a difficult job,” Davis said. “They’re out there doing the kind of work that a lot of midlife adults couldn’t really do. And I don’t just mean physically. I just mean able to get in there and deal with all these difficult situations and stay positive and really be good tourist ambassadors.”
As chief, Davis would love to take credit for that, he admits, but it’s the Beach Patrol culture that is passed down through generations that makes the team what it is.
“It really is cool to work with so many people who are so into what they’re doing,” he said. “And so positive about it and not cynical about the work.”
Q: As an EMS professional, what do you find most fulfilling about working Beach Patrol?
Q: As an EMS professional, what do you find most fulfilling about working Beach Patrol?
A: The ability to save a life. Beach Patrol is well respected in the area, and there comes with that a large degree of responsibility and pride when working.
A: The direct impact that my job can have on the lives of the people in this community and those of the visitors to our island year-round.
Q. What is the most interesting thing that has happened to you in your role with Beach Patrol?
Q: What is the most interesting thing that has happened to you in your role with Beach Patrol?
A: In Galveston we experience many different types of calls. From paragliding accidents to boaters in distress. I would say though that the most interesting thing I have worked are drowning calls in open water. There are so many variables to consider that critical thinking plays a major role.
A: Earlier this summer I responded to a call of a stranded Jet Ski 5 miles offshore. I was able to get in contact with the stranded fishermen and got their GPS coordinates while I was enroute to our launch location. I, along with my partner, launched our Jet Skis and navigated to their last known location. It took us around 30 minutes of travel time from when we launched until we found them anchored to a radio tower five miles offshore.
They had been fishing out there for a few hours when they realized their Jet Ski wouldn’t turn on. Shortly after we arrived on location, a Coast Guard vessel arrived and transported the two fishermen and their disabled vessel back to the Coast Guard station. Overall, from when the call dropped to us returning to shore, it took around two hours.
From a high school volunteer to a certified EMT to a fellow specializing in EMS, one new UTMB doctor knows emergency medicine from the ground up.
Dr. Matt Talbott joined UTMB this summer as an assistant professor of Emergency Medicine and Emergency Medical Services at the John Sealy School of Medicine.

He is working on a curriculum for future emergency medicine residents and finding opportunities for them to get first responder experience. That means working with EMS agencies.
“For a resident, EMS exposure involves riding on the ambulances and fire engines or riding in a helicopter,” Talbott said. “It also can be learning how to be a medical director or provide medical direction for a fire or EMS agency.”
Talbott was a fellow at the Medical College
of Georgia at Augusta University in its Emergency Medical Services Fellowship Program. While there, he worked with area EMS crews to respond to emergencies, provided tactical medicine support and learned about providing medical direction.
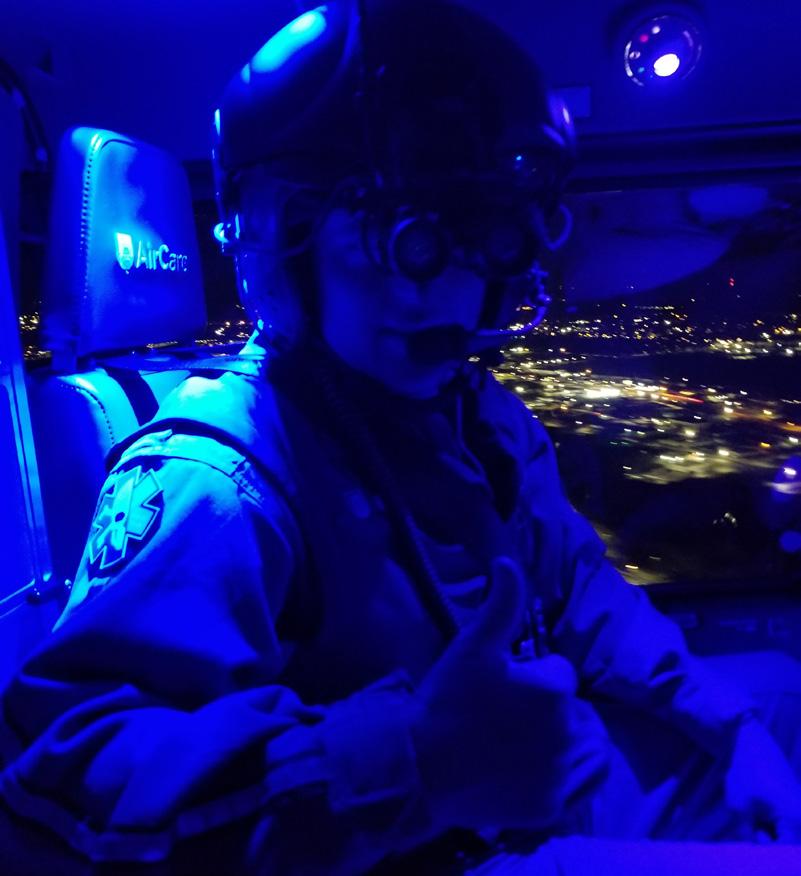

The emergency fellows also provided support for mass gatherings, such as sporting events and concerts. In Augusta, Georgia, that included The Masters golf tournament.
“We would staff The Masters tournament all week with the local EMS agencies on course and in the first aid stations,” he said.
Talbott and the other EMS fellows had a physician response vehicle to respond to 911 calls for a three-county area covering about 1,700 square miles.

“We went on calls where we could potentially make a big difference and support the Advanced EMTs and paramedics on scene,” he said.
Talbott envisions having a similar response vehicle for UTMB emergency residents.
“It helps them see what it’s like in the field because it can be vastly different from
having a patient show up in your ER where it’s a very controlled setting versus providing patient care on scene, which can be completely chaotic,” he said.
In high school, Talbott began volunteering for a rescue squad when he got his EMT certification. He continued to volunteer with EMS through college and medical school.
Talbott is open to being a resource for area EMS agencies either to present lectures, provide training sessions or to give advice.
“You know, ultimately, I want to be a resource to help improve pre-hospital care and the community and the region,” he said.
“I’m helping the Galveston Fire Department develop its tactical medicine program.”
Working on ambulances and flying on a helicopter, Talbott has seen some tough cases—the worst involving children, he said.
“That reinforced my desire to continue doing EMS-related things,” Talbott said.
“It’s challenging, tough and rewarding all at the same time, but when you do have a good save, it makes all the hard work worth it.”
Dr. Matt Talbott volunteered for a rescue squad when he got his EMT certification. He continued to volunteer with EMS through medical school.Why did you choose emergency medicine? Did someone or something influence you?
When I was a kid, I would pretend my Nintendo was a defibrillator and use the controllers as the paddles. I’d rub them together, place them on my sister’s chest and yell “clear,” and she would jolt her whole body upward. You know, completely normal childhood activities.
When I was in elementary school, I found an unconscious man at the bottom of a swimming pool. Everyone I was with went running to call 911 (ah, life before cellphones), but not me. I stayed behind to help my friends’ father get the man out of the pool and start CPR.
I felt that adrenaline rush, and I was hooked.
My dad worked as a volunteer EMT for a few years when I was younger, and I would always sneak off to flip through his textbooks. I’d find the gruesome photos and read the text on that page. By age 11, I knew you never pull out a protruding object, you stabilize it, and that on a sucking chest wound you only tape down three sides of the bandage.
Those pieces of knowledge really came in handy in my suburban upbringing.
They achieved ROSC (return of spontaneous circulation) in the field and rolled in with a completely awake and alert patient.
The patient was having a STEMI, and EMS gave all the meds including Heparin prior to arrival. It was great.
We were able to get that patient to the cath lab in under an hour. He was discharged from the hospital a few days later, neurologically intact.
I would not say it was a specific medic that made the difference, it was all of them; the whole team of EMS and fire personnel. Very impressive.
What is your favorite type of food? Do you have a recipe for that?
Hmm. Well, my go-to potluck dish is buffalo chicken dip, and it’s delish. Shredded chicken, Ranch, Franks buffalo sauce, shredded cheese and cream cheese.
Throw that in a crockpot and you’re done. It’s legit.
What’s something you want people to know about you?
Humor. There is always something to laugh about during a shift.
What do you do to relax when you are not at work? And why do you do that?
I enjoy partaking in sampling Martin House Sour beverages. Why? Because they’re delicious, and it makes me happy. (And most are 8% BBV.)
What can you tell us about a recent EMS-related case that was a success? Was there a medic who made a difference? Tell us about it.
A case that I know will stick with me: League City EMS brought in a status post-CPR.
I am not as angry as I appear.
My face has a way of always making people think that I am mad about something, when I am probably just thinking about my baby, or food or how my compression socks seem tighter today.

I originally chose emergency medicine after having experience in a large-scale cardiovascular intensive care unit for multiple years. I thrived in the fast-paced environment, and wanted to get experience in a different area of nursing while maintaining a similar type of pace. I chose to start picking up extra shifts in the ER near my home, and immediately felt a calling to this type of nursing. I stepped away from the bedside for about six years to develop a high school career and technical education health science program. However, the ER continued to call my name. I left the teaching position three years ago and became full-time in emergency medicine.
Having a solid team is essential to getting through a tough shift. Another quality I think that makes it somewhat easier is to have a sense of humor. Being able to step away from the trauma, stress, emotions or the feelings of being overwhelmed and be able to find something humorous in a situation is an excellent way to reset your spirit.
What do you do to relax when you are not at work? And why do you do that?
ARecently, we had a 60-yearold male who arrived with an allergic reaction to a bee sting. The medics were Diana Villasana and Trevlynn Scott (with Angleton Area Emergency Medical Corps). They were first on scene. The patient received IV Benadryl and IV Solu-medrol enroute to the emergency department. The patient also received an Albuterol and Atrovent nebulizer to assist with the wheezing. When the patient arrived, additional medications were given along with racemic epinephrine. Their quick work and IV access prior to arrival, along with first-line medications, prevented the patient from losing his airway and provided a positive outcome for the patient.
What is your favorite type of food? Do you have a recipe for that?
My absolute favorite type of food is crawfish! I don’t have a recipe that I can share since it is top secret! But I can say that my favorite thing to add to the boiling pot with the crawfish is fresh green beans!
I raise and train bucking bulls for competition. I also haul bulls to compete in bucking events across the country such as Professional Bull Riding. I do not ride the bulls, I leave that to the young, rubber-bodied bull riders! That takes a large chunk of my personal time; however, I love the bulls and the adrenaline rush from competing. I also

enjoy fishing and spending time with friends and family.
What can you tell us about a recent EMS-related case that was a success? Was there a medic who made a difference?
I really care about patients and their families, and even if the outcome for the patient is poor, I try to focus on providing the best care possible to all involved. I am constantly seeking out learning opportunities, and I ask lots of questions to the EMS that I encounter each shift. I recognize and appreciate the knowledge that they can bring to the ER staff to help continue to improve our skills, knowledge and overall patient care.
Ten to 15 times a month, medics in Galveston County follow an antibiotic protocol when treating open fractures.
The Galveston Area Ambulance Authority and Galveston County Emergency Services District No. 2 have had an active open fracture protocol for about two years.
“We found that often there was a missed opportunity for early antibiotics in patients with obvious or suspected open, long bone fractures,” said Dr. Kent Harkey, medical director for both EMS agencies. “We have a standing protocol where if an open fracture is suspected, we load IV Ancef (cefazolin) assuming there are not any contraindications—such as allergies to the medications.”
This protocol has received positive feedback from the Emergency Department at UTMB
“An open fracture requires different treatment than a closed fracture, in which there is no open wound. This is because, once the skin is broken, bacteria from dirt and other contaminants can enter the wound and cause infection. For this reason, early treatment for an open fracture focuses on preventing infection at the site of the injury.
The wound, tissues and bone must be cleaned during a surgical procedure as soon as possible. The fractured bone must also be stabilized to allow the wound to heal.”
and the surgeons, said Harkey, who is also a clinical assistant professor of medicine at UTMB as well as the assistant medical director of Emergency Medicine at the UTMB League City Campus.

“The American College of Surgeons were very supportive of this move in their last site visit to Galveston,” Harkey said.
Earlier administering of antibiotics for open fractures helps reduce the rate of infection, which often are serious and can lead to long-term complications. Bone infections are notoriously hard to permanently treat once they are established, often recurring over time and causing lifelong issues.
“I have standing orders in the form of protocols that empower the medics in the field to use their judgment and the best interest of the patient,” Harkey said.
The protocols go through indications, contraindications, dosing and pearls, which
are short and to-the-point tidbits of clinical information. When the medic suspects an open fracture, they use the protocol and administer the antibiotics. Some open fractures are obvious with the bone sticking out, but sometimes the bone retracts, and it appears to be just a laceration.

Harkey is collecting data to analyze the outcomes of this protocol.
“I have no doubt that the early antibiotics have helped with decreasing the morbidity and mortality associated with open fractures and severe trauma,” Harkey said. “It is my hope that as more agencies come under my medical direction, we can expand this protocol to help the citizens of Galveston County.”
—American Academy of Orthopaedic SurgeonsEveryone knew it was coming, but the sound of someone panicked, yelling, “There’s been a crash! It looks like somebody died!” was shocking nonetheless.
The wailing sirens and flashing lights were real. The wrecked car, though from a different nonstaged crash, was real. The EMTs and other emergency personnel … very real.
The teenager who laid “dying” in the street was an actor, but her distressed presence still weighed heavy in the air.
The whole scenario—including the tense, pre-filmed ER scene where the teenager was “pronounced dead” and the somber coffinside funeral service—was part of the “Is It Worth It?” event produced by UTMB Trauma Services, in conjunction with the UTMB Center

for Addiction Research.
The event, designed for ages 15 and up due to the graphic and unsettling nature of the demonstration, was funded by a grant from the Texas Department of Transportation and organized by Miranda Culligan, injury prevention specialist with UTMB Trauma Services.
“This is a very emotional production. It can be very upsetting,” Culligan explained. “But we feel passionately that it can save a life by accurately depicting the dangers and consequences of impaired driving.”
The three-hour event, which took place Aug. 28 at the Health Education Center on UTMB’s Galveston Campus, also included presentations by local authorities and people who lost family members in impaireddriving crashes, a virtual-reality drunken—or distracted—driving simulator, three levels of “drunk goggles” that re-create a sense

of driving impaired either by alcohol or drugs; and tours of emergency vehicles.
The demonstration and other elements of the event were intended to vividly depict the consequences of impaired driving. But along with that, participants got a first-hand look at the role emergency services first-responders play in dealing with the aftermath of a crash, no matter what the cause.
“EMS as a whole is a chronically underrepresented demographic when it comes to first responders. I chose to participate in this event because I wanted to increase awareness of what EMS does and how vital it is to allied health as whole,” said Ian Davis, operations manager for the Galveston Area Ambulance Authority
Davis added that in the state of Texas only about 26 percent of EMS personnel actually perform patient care in some capacity.
Re-enactment of deadly scene sends message about impaired driving – and, as an aside, about EMSA wrecked vehicle set the scene for this re-enactment. Galveston Area Ambulance Authority (GAAA) assisted in the re-enactment.
“This likely has to do with pay, fatigue and under appreciation. Some of this is our own fault because medics tend to focus on their job and the medicine and not how we’re perceived by the public,” he said. “However, in order to begin making paramedicine a career, instead of a steppingstone to nursing or firefighting or any of the other myriad professions that paramedics leave to join, we need to participate in events like this so that we get recognized for what we do.
“In addition, it builds closer bonds with our partnering agencies and facilities, UTMB in this case, and the more effectively we work together the better the patient outcomes can be,” he said.
Galveston Area Ambulance Authority paramedic Dahnia Rees concurs.“I wanted to participate so people could see what it is that we actually do out in the field
and hopefully help kids make better decisions,” she said.
In the end, it’s all about the job and the lives saved. Davis said he’s not convinced events like “Is It Worth It” make as big an impact on the public, especially teens, as organizers might hope—but that’s no reason not to present them.

“Events and PSAs like this have existed for a long time, and the general public doesn’t seem to change that drastically in response to it,” he said.
“However, even if we’re able to impress upon one person the importance of the message, maybe that is one life saved.
“And though that may not make my job as a whole easier, I think it’s worth it in the long run because I didn’t get into EMS to make my job easier or to change the whole world,” Davis said.
“I got into it to help the limited number of people I’m able to make contact with, and that’s good enough for me.”
UTMB Health offers a free Advanced Stroke Life Support (ASLS) course to its EMS partners.
This is an 8-hour stroke continuing education unit for all paramedics and emergency medical technicians. This hands-on, 8-hour simulation-based provider course provides caregivers tools to manage the acute stroke patient.
This includes the MEND exam, an easy-to-learn and easyto-use tool that enhances communication among EMS personnel, nurses and physicians. EMS agencies and hospitals across the United States use the ASLS curriculum.

The course covers:
• recognizing the five main stroke syndromes.
• performing a focused evaluation.
• understanding pre-hospital protocol.
• communicating t-PA contraindications and knowing how and when to administer t-PA to acute ischemic stroke patients.
• applying the six aspects of acute stroke care to hospitalized patients.
For information or to register for the free course, contact Michelle Vu at mlvu@utmb.edu
A trauma scene can trigger stress for EMTs and paramedics. Strong feelings of overwhelm might flood their thoughts. The physiological levels of cortisol and adrenaline rise in their bodies.
It’s part of the job, but it’s also something to watch and manage. Stress can build up over time.
“Stress reactions like fear, palpitations, anger or emotional numbness—even nightmares— are a normal part of the human response to trauma,” said Dr. Kim Gushanas, a licensed psychologist and assistant professor in the Department of Psychiatry and Behavioral Sciences at UTMB. “It’s just the brain trying to sort all of that out. Usually, those acute reactions

Stay hydrated.
Stretch.
Stay connected to your friends and family.
Have lunch with a colleague.
Go to your place of worship.
Express your thoughts.
Go outside and appreciate nature.
Spend time with animals.
Spend time with young children.
Create art.
decrease over time, but when someone is exposed to it over and over again, it can become harder for the body to naturally cope.”
Many EMTs and paramedics work split shifts and some also work for more than one agency. That work schedule alone is enough to cause stress.
But stress is not a “bad” thing. Stress helps medics when they respond to emergencies.
Stress is a natural hormone and a motivator that is part of an important process in our nervous system, one that historically has been the reason for our survival when we face threats or traumatic experiences.

Stress becomes dangerous when people judge themselves—thinking thoughts like “I can’t deal with this” or “This is too much”— or when they avoid the issue, pretending like it’s not there.
“Try to remind yourself when you’re stressed that your body is just doing its job,” Gushanas said. “There’s a great video of a TED Talk from a well-known health psychologist, Kelly McGonigal, on making stress your friend that is worth a watch.”
Mental health matters for first responders because they have a significantly greater risk for being exposed to trauma. Even simple exposure is just as much of a

predictor of stress as being directly involved, Gushanas said.
The stigma of getting help for mental health issues has decreased significantly in recent years. More first responders participate in therapy and treatment, and they continue to learn about their experiences and what helps and what hurts.
“If we aren’t taking care of ourselves in ways that are within our control, this can become harmful to our emotional and physical health and how we function at work, socially or emotionally,” Gushanas said.
Flight attendants tell people to put on
• Eat enough food.
• Get enough sleep.
• Try not to sign up for shifts longer than 12 hours without a break.
• Try not to work alone.
• Avoid over-caffeinating.
• Avoid using alcohol or other substances on a regular basis.
• Practice deep breathing.
• Release and relax your muscles.
• Exercise.
• Take a hot shower.
• Cuddle with your dog.
• Listen to music.
• Talk to a buddy.
• Write in a journal.
• Make a private video blog.
• Visit a therapist.
their own oxygen mask before trying to help others. It’s a simple metaphor but it’s very relatable. If you aren’t saving yourself first, you will run out of oxygen and will be useless to the rest of the world.
“In my field, we are trained that self-care is an ethical responsibility—an obligation if you are caring for others’ wellbeing,” Gushanas said.
“There’s no way anyone got into being a medic without a desire to help others, so remember your values that got you there, and add yourself to the top of that list if for no other reason than being able to do your job the best you can, when you’re at work,” she said.
UTMB Health Trauma Services holds Pre-hospital Performance Improvement and Patient Safety (PIPs) meetings every other month for EMS and other pre-hospital medical providers.

These free events include presentations on various trauma topics with specific case scenarios. Spinal cord trauma and injuries was one topic covered earlier this year. Another was burns.
Trauma Services distributes a feedback form after every meeting to get suggestions from the audience for topics medics want covered.
“We encourage active participation,” said April Vaughan, nursing program manager for Trauma Services at the Galveston campus.
Medics can receive continuing education credits for attending PIPs meetings, which are still virtual, but organizers are considering a return to in-person gatherings soon.
To learn more about these bimonthly meetings, email Vaughan at asvaugha@utmb.edu
When a vehicle struck a Galveston County Sheriff’s Office deputy during Jeep Weekend this summer in Crystal Beach, EMTs took immediate action.
The medics of Galveston County Emergency Services District No. 2 (GCESD2) treated and stabilized the deputy for a quick helicopter ride across the water to the UTMB emergency room in Galveston.
Doug Saunders, manager of the EMS crew for the district that covers the Bolivar Peninsula, watched nine of his medics work in the back of an ambulance with efficient, organized and focused moves.

“I’ve been doing this for 31 years, and he (the deputy) received injuries that were–let’s just say that’s the most injuries I’ve seen for one person in 31 years,” Saunders said. “From the time they called for assistance, he was at UTMB within 19 minutes.”
A helicopter from PHI Air Medical Ellington
CONTINUINGwas standing by at the Crystal Beach Fire Department, not far from the middle-of-thenight accident scene.
“Nobody was trying to be the hero that night,” Saunders said. “If you had seen the injuries, you would have said it’s not going to be positive. But it was a positive outcome— it was phenomenal.”
The district funds the emergency medical services and the three volunteer fire departments on the Bolivar Peninsula: Crystal Beach, High Island and Port Bolivar. The EMS component was previously called Peninsula EMS.


“An hour and eight minutes is the average patient contact time for our medics,” Saunders said. “And 90 percent of our patients are transported to UTMB.”
Those patients often get to UTMB on a GCESD2 ambulance that rides on the Galveston-Port Arthur Ferry. The Texas
Department of Transportation operates the free ferry as an extension of Highway 87.
On average, it takes the ferry 18 minutes to cross the 2.7 miles to Galveston Island from the peninsula. Loading time can take 9 minutes. And the wait time can be 45 minutes or longer depending on traffic and the season.
“We can call ahead if we know we have a priority patient,” Saunders said. The ferry crew can hold a trip for an ambulance.
The district also has to consider the possibility of a ferry losing propulsion during a ride or the choppiness of the water in the Ship Channel. If the water is extremely choppy, it might not be the best option for some passengers who are already sick or injured.
Another challenge is the dominance of elevated structures that have been constructed on the peninsula.
“About 80 percent of our patients are on an elevated structure,” Saunders said. “We use the stair chair and other ways to get them down that normal agencies don’t have to use on a daily basis. When we get a 911 call, it’s a two-unit response even when we don’t know what type of call it is, just because of the stairs involved.”


On average, elevated structures calls from start to finish take two hours and two minutes.
The agency’s biggest challenge is the seasonal influx of people. The population of the area is about 4,000 residents. Saunders estimates the summer influx varies from 12,000 to 16,000 people.
“A lot of times we have these social mediadriven events, so we don’t have a point of contact,” he said. “We don’t know to expect 4,000 or if 40,000 will show up on that weekend.”
“An hour and eight minutes is the average patient contact time for our medics.”
- Doug Sanders
Manager, Galveston County Emergency Services District No. 2 (GCESD2)

Keep up with the news from other EMS agencies. Get tips from UTMB Health experts. Sign up today and learn more about UTMB emergency services.
Scan the QR code to Sign-up, or visit: utmbhealth.com/partners/EMS
• Learn more about the UTMB Health League City Hospital Campus implementing new trauma protocols. The changes come as a direct result of collected data that show the trends in trauma cases arriving in the emergency room.

• The UTMB Health Clear Lake Hospital Campus now has a variety of specialists available 24/7 as the hospital begins the process of obtaining Level 2 Trauma Center certification. That process can take a year or two, but as of Oct. 1, the Clear Lake hospital is “Level 2 capable.”
• Friendswood EMS takes centerstage in The Dispatch’s Partner Spotlight. Meet the medics and learn more about the agency’s background.