

NEUROSURGERY
Ernest
Distinguished Professor of Neuromedicine
Chairman of Neurosurgery
University of Rochester Medical Center
Concerning the Teaching of Neurological
A Tribute to Joseph McDonald, MD
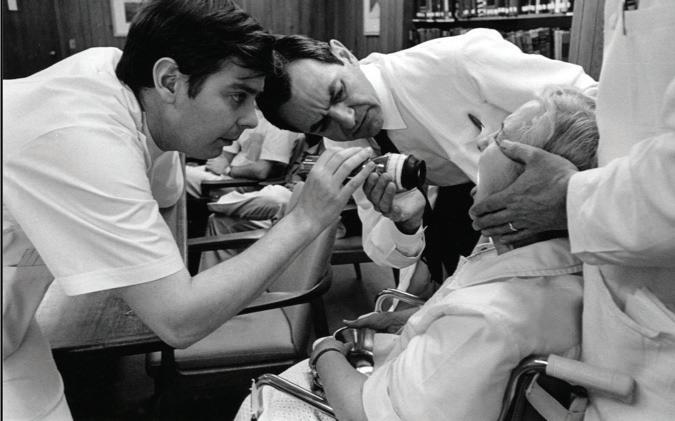
At the inaugural Cushing Society meeting in Boston on May 5, 1932, Dr. William P. Van Wagenen was elected as the first President of the Harvey Cushing Society, and he entitled his Presidential Address: Concerning the Teaching of Neurological Surgery.
With the recent passing of our Department’s third Chairman, Dr. Joseph V. McDonald, at the age of 98, I was inspired to reflect on his contributions to resident education and the culture of resident education which has distinguished Rochester Neurosurgery for nearly 100 years.







Department of Neurosurgery
University of Rochester Medical Center
601 Elmwood Avenue
Rochester, NY 14627
Dr. McDonald joined our faculty in 1956, following residency at Johns Hopkins and two years after Van Wagenen’s retirement. When Dr. Frank Smith transitioned to California in 1974, Dr. McDonald became the third Chief of the Division of Neurosurgery as well as Residency Program Director, and he established a tradition of collaborative mentorship that continues to this day. Dr. McDonald was endowed with a brilliant academic mind and unparalleled diagnostic and patient management skills, which, in the “pre-CT/MRI” era, were critical assets in neurosurgical practice. In his mind the patient came first, and he embraced the approaches of “measure twice, cut once” and “do no harm.”

Copyright © 2024 University of Rochester
All rights reserved. No part of this publication may be reproduced in any form or by any electronic or mechanical means, including information storage and retrieval systems, without written permission from the university.
Dr. McDonald was at once intellectually demanding and personally humble in a way that was disarming and welcoming for his residents. He had an uncanny ability to give us responsibility in the operating room early in our training while at the same time ensuring the best outcomes for his patients. This approach to surgical education was adopted by his faculty partner, Dr. Shige-Hisa Okawara, as they guided us through complex surgical procedures. This collaborative environment established a spirit of camaraderie between faculty and residents that continues to be a strength of our training program today.
Webster Pilcher, MD, PhD & Thelma Del MonteSurgery
This emphasis upon thoughtful surgical decision making, patient-centric care and surgical experience early in residency is reflected in the recent top 15 ranking of UR Neurosurgery in terms of the surgical case volumes of graduating Chief Residents.
When Dr. McDonald retired in 1990, just over 30 years ago, even he could not have imagined the impact of new technologies on neurosurgical care: image guided brain tumor resection, aneurysm coiling, intravenous thrombolytics and endovascular thrombectomy, radiosurgery, minimally invasive spine and brain surgery, deep brain stimulation, laser interstitial thermal therapies, robotic spine and brain surgery and a revolution in functional and structural neuroimaging
Over the 34 years that elapsed since his retirement, we continued to ask: “What is the best that we can give to our residents? How should we prepare the next generation of gifted young surgeons to become leaders in patient care, education, and research in our specialty?”
A key contributor to surgical education of Neurosurgery residents is the volume and diversity of cases. With the expansion of our Department faculty over the past 20 years to include 14 practicing neurosurgeons covering every subspecialty, we are now able to offer a clinical training experience which is second to none. During Dr. McDonald’s tenure the faculty complement of
2–3 faculty provided 500–600 cases annually for resident education. Today our residents are exposed to 3000 cases performed by the aggregate faculty across every subspecialty of our profession. Our typical daily census of 80 inpatients at Strong Hospital is a testimonial to the growth of our Department’s practice.
Beyond case volumes, resident education is impacted by faculty mentorship, individualized clinical, technical and educational experiences, and opportunities to pursue clinical and translational research pertinent to our field.
To support this aspect of resident education, and with help from alumni and Departmental faculty, we have raised endowments and funds which have impacted resident education in our Department. These include a $2.5M resident education endowment fund in honor of Dr. McDonald and Dr. Okawara, which supports monthly visiting professorships, national and international clinical/ research and educational experiences for our residents, and opportunities to pursue individualized approaches to career development. We recently raised > $3 million to build a state-ofthe-art Surgical Skills Laboratory that provides cadaver and simulation labs, microsurgical training, and exposure to new devices and technologies. The Skills Lab accelerates the acquisition of surgical skills in brain, spine, and peripheral nerve surgery.

Joseph McDonald, MD Chairman of Neurosurgery 1974-1990 University of Rochester Medical Center
With the establishment in 2023 of the Rusyniak Memorial Medical Student Research endowment, medical students considering a career in Neurosurgery can now spend a summer or a year out to work with a Neurosurgery faculty member on research projects leading to publication. With these advances, our residency program is nationally competitive for the best and brightest applicants for neurosurgical training.
We have many reasons to be grateful to Dr. McDonald for the standards he set during his time as Chair, both in terms of patient care and resident education. Today we stand on his shoulders, as well as on those of Dr. Van Wagenen and Dr. Smith, whose efforts and contributions provided a solid foundation for one of the nation’s strongest neurosurgery departments here at UR Medicine.
Saving Lives
UR Medicine Department of Neurosurgery Mobile Stroke Unit Program Improves Time to Treatment and Access to Healthcare in Underserved Areas.

The UR Medicine Department of Neurosurgery Mobile Stroke Unit has become a familiar sight throughout the greater Rochester area.
In 2018, UR Medicine and the Department of Neurosurgery launched the first and only Mobile Stroke Unit (MSU) serving the Upstate New York region, joining a small but impactful group of MSUs serving stroke patients throughout the U.S. Though the MSU concept is a relatively new one—the first US MSU began operations in Houston, TX in 2013—this innovative mobile technology has impacted many patients in our community by reducing the mortality and disability associated with ischemic stroke.
MSUs are designed as stroke emergency rooms on wheels, bringing stroke care directly to the patient. The units are staffed with highly trained medical professionals: on the rig are a stroke trained critical care nurse, a CT technologist, a paramedic and

an EMT. Crucially, a vascular neurologist is also onboard, either in person or via telemedicine. The neurologist and nurse assess the patient’s symptoms and CT images and determine whether the patient is eligible for clot-busting intravenous thrombolytic medication. If eligible, the patient receives these IV thrombolytics immediately on the mobile stroke unit.
The launch of the UR Medicine MSU was the culmination of years of work, championed by endovascular neurosurgeon Tarun Bhalla, M.D., PhD, the Surgical Director of the UR Medicine Comprehensive Stroke Center (CSC) and an Associate Professor of Neurosurgery, Neurology and Imaging Sciences. Together with the leadership of neurologist Curtis Benesch, M.D., MPH, medical director of the CSC;
Adam Kelly, M.D., director of tele-neurology; and a team of nurses, technologists, emergency personnel, and physicians, the MSU has provided care for hundreds of stroke victims since it started operation in 2018.
To date, the mobile unit has evaluated over 1100 patients in the field and transported over 750 patients to local stroke centers, and it has administered clot-busting intravenous thrombolytics (IVT) to 137 patients.

Achieving Goals of Expediting Access to Care
“Results of the first four years of UR Medicine’s MSU operations are very promising,” said Dr. Bhalla. “Our own data show that when compared to local emergency room care in the Finger Lakes region, the MSU administers IV thrombolysis to stroke patients 25-30 minutes faster from arrival, 45 minutes faster from 911 activation, and 60-70 minutes faster from the patient’s last known normal time.”
Perhaps most critical is the MSU’s ability to provide IV thrombolytics within the “golden hour,” or the first 60 minutes from the time the patient was last known to be stroke symptom free. Treatment during the golden hour is associated with optimal stroke outcomes and provides the best opportunity for complete stroke recovery. When transport and diagnostic workup does not begin until after hospital arrival, local emergency rooms are only able to administer IV thrombolysis within the golden hour in about 2% of stroke cases. However, because the MSU is designed to remove those transport and post-arrival diagnostic barriers to care, UR Medicine
can administer IV thrombolysis within the first hour in 30-33% of cases. These results are consistent with those reported in 2021 by the national multi-center Best-MSU Study.
In addition, patients may also be diagnosed with large vessel strokes using CT angiography (CTA) on the MSU. In many cases, this on-board diagnosis allows patients to go directly from the rig to the nearest operating room capable of large vessel clot removal.
In one recent case, an MSU patient was diagnosed with a large vessel occlusion on MSU CTA, received IV thrombolysis on the MSU, and was then able to go directly to the OR because results were reviewed by the surgical team while patient was en route. The patient underwent surgical revascularization within 90 minutes of stroke symptom onset, with successful reperfusion within 120 minutes. The patient regained full functionality post treatment.
Furthermore, research by Matt Bender, MD, Associate Professor of Neurosurgery (2024), confirmed that the MSU is more likely than traditional EMS to treat and transport patients residing in Rochester’s poorest zip codes.
“The vast majority of the 911 calls to which the MSU is dispatched come from zip codes with the lowest household incomes in Rochester,” said Dr. Bender. Among MSU transports, “Forty percent of the patients receiving IV thrombolytic or endovascular thrombectomy came from the 10 zip codes with the lowest median household income.” This finding confirms the MSU’s mission to improve access to care among underserved residents who experience both higher rates of stroke and significant barriers to effective stroke treatment.
Finally, MSU data also indicates that all of these efforts to improve times to treatment on the MSU translate into overall average reductions in length of stay among those treated on the MSU, as well as greater likelihood of discharge to home as opposed to rehabilitation facilities.

Forty percent of the patients receiving IV thrombolytic or endovascular thrombectomy came from the 10 zip codes with the lowest median household income. - Dr. Matthew Bender
Improving Care Access Through Stroke Literacy
“The essential first step in expediting stroke intervention via an MSU is patient recognition of stroke symptoms and immediate activation of emergency medical services,” said Dr. Bhalla. “That is why we felt it was so essential to make stroke literacy a part of the MSU program.”
With this as a goal, Dr. Bhalla successfully secured grant funding from the Mother Cabrini Health Foundation, worth over $1 million, to build a stroke literacy initiative that brings together local nonprofit agencies dedicated to providing stroke education in underserved communities.
The Stroke Literacy Coalition includes the MSU team and community organizations Action for a Better Community (ABC), Ibero American Action League, and Lifespan of Greater Rochester. Together, the Coalition developed and distributes stroke literacy materials and embeds stroke educators within underserved neighborhoods to educate local citizens about signs and symptoms of stroke, and the importance
of activating 911 when strokes occur. “The stroke literacy program strives to improve access to care by providing greater stroke knowledge that ultimately leads to faster stroke recognition and treatment response, said Diana Proper MS, RT(VI), Surgical Stroke Clinical Administrator and MSU Program Manager. “This should lead to a reduction in stroke death and disability in our region.”
The MSU team supports stroke literacy with widespread multimedia messaging, recognizing that an MSU is only as effective as its ability to reach patients quickly. “A community can be fortunate enough to have this wonderful resource, but if people are not aware of stroke symptoms and don’t know if and when to call, we can’t help them,” said Rose Gilbert, UR Neuromedicine Director of Program Development. “So, we developed a bilingual campaign with social media, radio, bus wraps and signs at the local bus station. Some of the people featured in the ads were actual patients and residents of local underserved neighborhoods. We knew
that, ultimately, people want to see messaging with individuals that are reflective of them.”
The MSU team also created and distributes T-shirts, pens, water bottles, magnets, and reusable grocery bags containing reminders of symptom recognition guidelines. These multimedia efforts reinforce stroke literacy among local and regional patients.
The MSU team reiterates that the MSU is a community resource that belongs to local citizens, and MSU team and Stroke Literacy Coalition remain dedicated to the mission to improve stroke outcomes in the Monroe County area. This includes providing these services to more citizens, including underserved rural communities.
“We are committed to MSU service and literacy expansion,” said Dr. Bhalla, “and to utilizing both in efforts to remove barriers to stroke care, particularly within underserved communities.”
Matthew Bender, MD
Associate Professor, Neurosurgery, Neurology, Imaging Sciences
Division of Stroke and Cerebrovascular Disease
New, Effective Solution for Intracranial Hypotension
With a laboratory focused on acute ischemic stroke thrombus proteomics (see Education, page 10), Matthew Bender, MD, maintains close connections with researchers across the country to bring new treatment and surgical techniques to patients in Rochester.
Dr. Bender recently leveraged that network to bring a new procedure to Strong Memorial Hospital. The procedure, called “transvenous cerebrospinal fluid (CSF) fistula embolization,” is a treatment for spontaneous intracranial hypotension (SIH). SIH occurs when a patient has inadequate volume of cerebrospinal fluid and presents with orthostatic (positional) headaches, tinnitus and/or hearing loss, and brain fog.
“The positionality is really a cardinal feature,” Dr. Bender said. “Patients will tell you they feel OK when they awaken but develop headaches within an hour of being vertical that resolve when they lie flat again. It leaves them bed-bound.”
In affected patients a fistula develops between the CSF-space and the venous system, typically along a thoracic nerve root sleeve. Its description resolved the puzzling question of where CSF goes in SIH patients who so clearly have inadequate CSF volume.
“There is physiologic reabsorption of CSF into veins,” Dr. Bender said. “This is really just an extreme case of excessive, pathological reabsorption.”
It’s
exhilarating to discover new pathologies and develop new procedural skills after finishing training.
- Matthew Bender, MD
1. Efficacy of transvenous embolization of CSF-venous fistula in spontaneous intracranial hypotension: Case-series. Interventional Neuroradiology. 2023 Dec 21; 15910199231221449
2. Prevalence of SLEC-negative spontaneous intracranial hypotension in patients with spinal nerve root sleeve diverticula on MRI. Neuroradiol J. 2023 Dec;36(6):736-739
CSF-venous fistula was first described at Cedars-Sinai Hospital in 2014 by Dr. Wouter Schievink, who treats most such patients through open surgical ligation (closing the connection to the fistula). While the incidence is low, SIH and CSF-venous fistulas remain underdiagnosed.
Dr. Bender credits Dr. Waleed Brinjikji at the Mayo Clinic in Rochester, MN, with developing the minimally invasive alternative of gluing off the fistula through the venous system. Dr. Bender’s team recently published a series of transvenous embolization of CSF-venous fistulae, showing excellent clinical and radiographic outcomes in a series of seven patients.
Intracranial hypotension and CSF-venous fistulae are now an active area of research at URMC. Through a collaboration with Professor Jianhui Zhong in the Department of Imaging Sciences, Dr. Bender’s team has suggested SIH also may be associated with glial lymphatic dysfunction that is improved after successful treatment.
“It’s exhilarating to discover new pathologies and develop new procedural skills after finishing training,” Dr. Bender said.

Rusyniak (R’92) Memorial Endowed Medical Student Research Fellowship
With a lead gift of $125,000 provided by Kevin Mullins, MD (R’97), the Department of Neurosurgery has established the George Rusyniak Memorial Medical Student Research Fellowship. The Rusyniak Memorial Medical Student Research Endowment allows medical students to engage in clinical or translational research in Neurosurgery with mentorship by a Neurosurgery faculty member.
George Rusyniak, MD (R’92) passed away unexpectedly on February 9, 2022, leaving behind his wife Sue and his daughter Alexandra. George was a Professor of Neurosurgery at the University of South Alabama Medical School and had established a career-long legacy of inspiring medical students to engage in neuroscience and neurosurgical research. A 1986 magna cum laude graduate of the University of Rochester, George distinguished himself during medical school and was accepted into the UR Neurosurgery training program.
As a resident he distinguished himself as intellectually and technically gifted. Over his career as a resident and faculty member, he inspired many medical students to pursue research in Neuroscience and Neurosurgery, and many of his mentees chose Neurosurgery as a career.
Our initial recipients of the 2023–2024 Rusyniak Fellowship are Sajal Akkipeddi (MS3) and Emma Strawderman (MS2).
Sajal is completing a yearlong fellowship working with Neurosurgery faculty
member Matt Bender, MD, and Emma completed a three-month summer fellowship with Neurosurgery faculty Webster Pilcher, MD, PhD, Frank Garcea, PhD and Bradford Mahon, PhD.

EDUCATION
Inaugural Rusyniak Fellowship Recipient Sajal Akkipeddi (MS3)
Dr. Matthew Bender’s interest in endovascular thrombectomy as a treatment for acute ischemic stroke has provided a rich investigative opportunity for medical student Sajal Akkipeddi, who is taking a year out between the third and fourth years of medical school to work in Dr. Bender’s laboratory.
In the year of research afforded him by the Rusyniak Fellowship, Akkipeddi’s work is focused on studies of the anatomy of blood clots harvested during endovascular thrombectomies in acute stroke patients and the many proteins they share.
“Not all clots that cause stroke are the same,” he explained. “Clots are very complicated, involving a complex interplay between proteins in the blood. We’re using mass spectrometry to categorize all the proteins in clots harvested from our stroke patients and so far, we’ve identified 2,900 protein signatures. We hope that by characterizing the proteomic signatures of these clots we will find clues that will lead to the development of even more effective thrombolytic (clot-busting) agents.”
Clots are very complicated, involving a complex interplay between proteins in the blood. We’re using mass spectrometry to categorize all the proteins in clots harvested from our stroke patients and so far, we’ve identified 2,900 protein signatures.
- Sajal Medha Akkipeddi
From a treatment standpoint, Alteplase is the only thrombolytic currently available for patients with ischemic stroke. Alternatively, in patients with a large vessel occlusion in the brain, endovascular approaches can be used to surgically remove these clots and return many patients to productive lives. These clots are the subject of active investigations ongoing in Bender’s laboratory.
In addition to studying the proteomic signatures of clots after their removal by endovascular thrombectomy, Akipeddi says that specialized CT scans have the potential to characterize the protein composition of intracranial thrombi in patients with a stroke in progress, leading to dynamic therapeutic interventions with specialized thrombolytic or neuroprotective agents.
“We are breaking down clots in the lab using a variety of thrombolytic agents,” said Akkipeddi. “We hope that a marriage of dynamic imaging studies and thrombolytic therapies will lead to personalized treatments and even better outcomes.”
Sajal Medha Akkipeddi Student, UR School of Medicine Rusyniak Fellowship RecipientLike most researchers at the University, Akkipeddi is engaged in several projects at the same time—and he has managed to engage residents and staff throughout Strong Memorial Hospital in providing the material he needs to continue his work. That material is stool samples—the product of a function that may hold the key to the connection between the gut microbiome and atrial fibrillation (AFib).
One in three people who come in with stroke have AFib, he noted, and in certain conditions during a stroke, the gut microbiome spews out DNA to make a neutrophil extracellular trap (NET), which is good at trapping blood clots. This seemed significant to Akkipeddi. “If the DNA produced is contributing to the structure of the clots, we may be able to target that,” he said. “If you have clots that are rich in DNA, are they better broken down by one enzyme or another? If we can prevent the side effects of bleeding with people who are at risk of forming NET-rich clots, it may give us completely new and safer treatment alternatives.”
The gut microbiome is already associated with treatment responses to cancer therapy, he said, so it may contain other clues to treatment for a range of issues. “Stroke engenders inflammation without infection,” he said. “The enzymes that break down the blood-brain barrier in ischemic stroke also break down barriers in the gut. In ischemic stroke, many cells die even after the ischemia that caused the stroke is resolved. One of the things that affects that is the immune system.”
Stroke staff throughout the hospital now collect blood and stool samples to send to Akkipeddi for his research, a collaborative bonus that he credits to the culture at URMC. “It really is a village,” he said. “I’m so grateful to the OR staff—they put out a sample cup and a syringe for blood, for science. Even if all the people don’t have a sense of where all the samples are going, it truly is a collaborative effort.” Thanks to this cooperation and to the research made possible, UR Medicine now has the only biobank in the world for stool from stroke patients.
This basic research is very preliminary to the actual development of pharmaceuticals, he said, but it’s a step in the right direction. “Dr. Bender has been the most wonderful mentor—I am grateful for his support and for all the things he makes happen. There’s a lot of foundational research that needs to be done for vascular pathologies, and he has pushed this forward. I’m very grateful to the department staff who allow this to happen here.”
1. Akkipeddi SMK, Ellens NR, Singh R, Jalal I, Schartz D, Bender MT. “Empty Cyst Sign” appearance of CSF-venous fistula on digital spinal myelography. World Neurosurgery (submitted).
2. Rahmani R, et al. LACROSSE Study: Lumbar Drainage Compared to External Ventricular Drainage for Aneurysmal Subarachnoid Hemorrhage, A Multicenter Randomized Control Trial. Lancet (submitted).
3. Brown NJ, Musmar B, Kuo CC, Pennington Z, Horowitz MA, Singh R, Akkipeddi SMK, Bocanegra-Becerra JE, El Naamani K, Franco D, Rahmani R, Catapano J, Jabbour P, Bender MT, Lawton MT. Endovascular versus open microsurgical intervention for craniocervical junction dural arteriovenous fistulas: A review of the current evidence. World Neurosurgery (submitted).
4. Gupta N, Doad J, Chien D, Cotroneo M, Akkipeddi SMK, Gajjar AA, Singh R, Sharestani S. Incidence, Prevalence, Burden, and Interregional Analysis of Ischemic Stroke in India: 1990-2019. Stroke (submitted).
5. Jalal MI, Lally J, Akkipeddi SMK, Ellens NR, Burgett JL, Proper D, Hodge D, Pilcher, WH, Kelly AG, Benesch CG, Vates GE, Mattingly TK, Bhalla T, Bender MT. Mobile Stroke Units Address Disparities in Care As Demonstrated By Demographic and Zip Code Level Socioeconomic Status. Stroke (submitted).
6. Akkipeddi SMK, Rahmani R, Schartz DA, Chittaranjan S, Gunturi A, Ellens NR, Kohli GS, Bhalla T, Mattingly TK, Welle K, Morrell CN, Bender MT. Neutrophil extracellular traps (NETs) enriched in emboli retrieved from stroke patients with atrial fibrillation. Res Pract Thromb Haemost Published Online First: 14 February 2024. doi: 10.1016/j. rpth.2024.102347.
7. Akkipeddi SMK, Rahmani R, Ellens NR, Kohli GS, Houk C, Schartz DA, Chittaranjan S, Worley L, Gunturi A, Bhalla T, Mattingly TK, Welle K, Morrell CN, Bender MT. Histone content, and thus DNA content, is associated with differential in vitro lysis of acute ischemic stroke clots. J Thromb Haemost. Published Online First: 29 January 2024. doi:10.1016/j.jtha.2024.01.013.
8. Schartz DA, Ellens NR, Houk C, Akkipeddi SMK, Mattingly T, Bhalla T, Bender MT, Symptomatic carotid artery intraluminal thrombus: Risk of medical management failure and distal embolization. J Neurointerv Surg. Published Online First: 24 November 2023. doi: 10.1136/jnis-2023-021044.
9. Schartz DA, Akkipeddi SMK, Ellens NR, Rahmani R, Kohli GS, Ismail R, Chittaranjan S, Welle K, Bhalla T, Mattingly TK, Morrell CN, Bender MT. Ischemic stroke thrombus perviousness is associated with distinguishable proteomic features and susceptibility to ADAMTS13-augmented thrombolysis. AJNR Am J Neuroradiol. 2023;45(1):22-29. doi:10.3174/ajnr.A8069.

EmmaStrawderman Student, UR School of Medicine
RusyniakFellowship Recipient
EDUCATION
Inaugural Rusyniak Fellowship Recipient Emma Strawderman (MS2)
Second-year UR SMD student Emma Strawderman is in the MD–PhD program, and she received a three-month Rusyniak Memorial Fellowship that she completed between the first and second years of medical school. Her area of interest is to advance the understanding of the brain’s ability to adapt and reorganize cognitive functions around brain tumors.
For her 2023 summer project, Emma evaluated structural and resting state MRI scans in patients with intrinsic gliomas, working with Department Chair Web Pilcher and Research Assistant Professor Frank Garcea, Ph.D., as well as their collaborators, Brad Mahon Ph.D. and Madalina Tivarus, Ph.D. Emma used machine learning to predict whether the pattern of functional connectivity in the non-lesioned hemisphere of the brain (opposite the side with the tumor) could predict where the lesion is located spatially in the other hemisphere. “If we could do that reliably, that would suggest that there are consistent patterns of neural network reorganization that happen in the healthy brain to compensate for lesion infiltration in the other hemisphere,” she said. “We wanted to see if this ability to reorganize was influenced by how aggressively the tumor grows, and by stratifying results based on WHO grade and IDH mutation status.”
So far, the research has yielded interesting results. “We have found that you can make those predictions reliably for certain regions, especially for lesions impacting the parietal lobe,” she said. The pattern is also more predictive in patients with a slow-growing tumor: “The hypothesis is that the brain has more time to modulate functional connectivity to support cognitive functions when the tumor is less aggressive.”
We wanted to see if this ability to reorganize was influenced by how aggressively the tumor grows, and by stratifying results based on WHO grade and IDH mutation status. - Emma Strawderman
This preliminary research would benefit from behavioral and neuropsychological studies of these patients to substantiate that these functional connectivity changes correlate with better cognitive outcomes, she noted, but “it’s assumed that the altered connectivity we’re seeing could be advantageous. With brain cancer, patients can experience deleterious effects in many domains of cognition, but if the tumor is located in a region where there is a high predilection to reorganize, that could possibly give hope to a patient. We’re not there yet; the idea is to understand how and why these changes are happening and ultimately be able to use that information prognostically.”
Emma’s proposed manuscript documenting this work, Contralesional connectivity fingerprint of unilateral gliomas: a resting-state fMRI study, is currently under preparation.
Strawderman is excited to enter the PhD portion of her MD–PhD program this summer. “Rochester is a really special place,” she said. “The faculty are extremely supportive of students. I’m one of the leaders of the Neurosurgery Focus Group for medical students, and the faculty are always available to get us into the OR, where a lot of the learning happens. This is also really important for getting students enmeshed in the Department. It’s great that we have donors who make this possible, so students can get the same wonderful experience as I did.”
RESIDENTS & GRADUATES
PGY-7, Chief Resident Catherine Wassef, MD
A PGY-7 resident in neurosurgery, Catherine Wassef comes from East Windsor, NJ, and studied Human Biology, Health, and Society at Cornell University, where she was one of the founding members of the Dial of Ahaz Society. She received a USDA Hatch Fund grant to research neural correlates of the fuzzy trace theory with neuroimaging in the Lab for Rational Decision Making. She graduated from Cornell with honors in 2012 after completing her thesis on voxel-based morphometry and personality traits.
Dr. Wassef then studied at Temple University’s St. Luke’s School of Medicine, where she volunteered at the Kenderton elementary school as well as with the Global Medical Brigades in Honduras. She co-founded the pediatric interest group at Temple and published on spinal cord stimulator infection rates.
While Rochester provides fairly close proximity to her home state of New Jersey, she has found other important benefits to choosing this medical center for her residency. “I was a sub-I here, and the culture is one of curiosity,” she said. “That’s what helps me stay interested when I’m working 80 hours a week. And the department is doing its best to make our lives easier when they can. They make sure things are not unnecessarily difficult for us. We have a very large complement of Nurse Practitioners, even in the off hours. It helps the residents focus on clinical decision-making and patient care, which is what they will do as attendings.”
In her seven years of residency at URMC, Dr. Wassef made the decision to pursue pediatric neurosurgery. “In my opinion, it’s the best field in neurosurgery, and includes components of neurosurgery,” she said. After her residency, Dr. Wassef will move on to a fellowship at the University of Colorado, where she will continue her work in pediatric neurosurgery.
 Catherine Wassef, MD Chief Resident
Catherine Wassef, MD Chief Resident
In my opinion, it’s (pediatric neurosurgery) the best field in neurosurgery.
- Catherine Wassef, MD

RESIDENTS & GRADUATES
PGY-6 (Senior Resident) Nathaniel Ellens, MD
As a PGY-5 neurosurgery resident at the University of Rochester, Dr. Ellens had the opportunity to complete an enfolded endovascular neurosurgery fellowship. This was the direct result of significant exposure he had to the angiography suite earlier in his residency, making it possible for him to transition quickly to the role of an enfolded fellow. He has participated in a wide variety of procedures including coiling aneurysms, treating AVMs and fistulas, and performing mechanical thrombectomies. “Obtaining this endovascular experience during residency is atypical,” he said, “but it’s extremely valuable and provides a strong foundation for me to build off as I pursue a career in vascular neurosurgery.”
Now in his PGY-6 year, Dr. Ellens is assisting Dr. Wassef with chief resident duties. In his upcoming PGY-7 year, he will become the Neurosurgery chief resident along with Dr. Santangelo. “These two years will allow me to develop my open surgical skills as I operate on the broad scope of cranial and spinal neurosurgical patients,” he said.
After graduating from residency at URMC, Dr. Ellens has accepted an endovascular fellowship position at Thomas Jefferson University in Philadelphia, PA. This was the first CAST accredited endovascular neurosurgery fellowship program and, under the leadership of Drs. Jabbour and Tjoumakaris, remains one of the busiest in the country. “This experience will provide a final layer of technical training and mentorship to round out my vascular training experience,” he said, “and it will position me well as I pursue my career in vascular neurosurgery.”
This experience will provide a final layer of technical training and mentorship to round out my vascular training experience.
- Nathaniel Ellens, MD

Dr. Ellens details a typical day in the life of a UR Medicine Neurosurgery resident in a YouTube video he produced.
Nathaniel Ellens, MD PGY-6 (Senior Resident)RESIDENTS & GRADUATES
PGY-6 (Senior Resident) Gabrielle Santangelo, MD
During her PGY-5 year at the University of Rochester, Dr. Gabrielle Santangelo completed a research year focusing primarily on surgical simulation for education and spine outcomes. In Dr. Stone’s laboratory at URMC, she developed a whole-task simulator for durotomy repair and a 3D printed skull for microvascular practice, among other clinical projects.
“Additionally, I was involved in several multi-institutional collaborative efforts studying outcomes in adult deformity, degenerative spine and peripheral nerve with the University of Pennsylvania and the Mayo Clinic,” she said. “I also spent time working on the CNS neurosurgery survival guide content and on the CNS guidelines podcasts.”
As a PGY-6 resident, Dr Santangelo is completing an enfolded fellowship in complex spine at the University of Pennsylvania,working with William Welch, MD (R ’91) who is Chair, Department of Neurosurgery, Pennsylvania Hospital. “This affords me the opportunity to be exposed to a wide breadth of spine surgery, with rotations in deformity, MIS, tumor and trauma,” she said. “I will also continue to be academically productive by forwarding ongoing collaborative efforts and will remain active in organized neurosurgery during this year.”
In her upcoming PGY-7 year, Dr Santangelo will return to the University of Rochester to serve as Chief Resident. She has accepted a postgraduate fellowship position at Northwell Health in New York in spine oncology with Dr. Dan Sciubba, where she will complete her subspecialty training in academic spine surgery, with a focus in oncology and deformity.

I will also continue to be academically productive by forwarding ongoing collaborative efforts and will remain active in organized neurosurgery during this year.
- Gabrielle Santangelo, MD
Gabrielle Santangelo, MD PGY-6 (Senior Resident)
Redi Rahmani, MD (‘23)
Cerebrovascular and Skull Base Fellow
Barrow Neurological Institute
RESIDENTS & GRADUATES
Cerebrovascular and Skull Base Fellow Redi Rahmani, MD (‘23)
Since completing his residency at UR Medicine Neurosurgery in June of 2023, Dr. Redi Rahmani has been hard at work at the Barrow Neurological Institute, where he is pursuing an open vascular Neurosurgery fellowship with Michael Lawton, MD, Chair of Neurosurgery at Barrow. Outside the operating room, Dr. Rahmani stays busy working on as many as 40 different research initiatives at Barrow. When we caught up with him for this newsletter, he and his colleagues had just completed work on a study (published in the January 19, 2024 issue of the Journal of Cerebral Blood Flow & Metabolism) on vitamin D deficiency and whether it contributed to higher rates of intracranial aneurysm rupture.
“We created vitamin D deficiency in mice, created aneurysms using the Tomoki Hasimoto model, and looked at the rate of rupture compared with mice who were not vitamin D deficient,” he said. “With mice, you can delete certain genes, so we eliminated the Vitamin D receptors in mice, which created the same effect as a vitamin D deficiency. What we found is that the deletion of this receptor in the smooth muscle cells of the arterial wall causes an increased risk of rupture in mice.”
But if we can develop an interactive Zeiss microscope to assist surgeons during microsurgical procedures, this would positively impact surgical outcomes.
- Redi Rahmani, MD
The search for new ways to treat aneurysms in the brain has led Rahmani and his colleagues to examine senescent cells, cells that are aging abnormally quickly. “Cells that appear in an aneurysm have aged a lot faster, and these continue to weaken the arterial wall,” he said. “If you can stop these cells from aging prematurely, you can reverse that process. It’s yet another way to think about how we may one day treat aneurysms in the brain.”
Rahmani’s work also involves artificial intelligence (AI), and its potential role in intracranial neurosurgery. Working with Zeiss, a global leader in microscopy, the team at Barrow aims to use AI and machine learning to break down visual data into bits of information, to help direct the surgeon to the next steps in microsurgical procedures. “It’s a bit behind compared to the spine, where we’ve been using robots to help the surgeon navigate during surgery” said Rahmani. “But if we can develop an interactive Zeiss microscope to assist surgeons during microsurgical procedures, this would positively impact surgical outcomes.”
In addition to these and many other projects, Rahmani says he’s having a “heavily operative year,” taking part in highly complex surgeries. “People come from all over the world to have these things taken care of here,” he said. “I’m seeing pathology in the OR that is quite rare and quite difficult. That’s been the bulk of my time this year.”
RESIDENTS & GRADUATES
Spine and Neurotrauma Fellow David Paul, MD (‘23)
With a focus on complex spine and neurotrauma surgery, David Paul. MD is now completing a fellowship in Brain and Spine Trauma and Spinal Deformity at the University of Pittsburgh Neurosurgery before he returns to UR Medicine in summer 2024 as an Assistant Professor of Neurosurgery.
“I’m working with David Okonkwo, who is one of the leaders in both clinical management of traumatic brain and spinal cord injuries and research in this area,” said Dr. Paul. “I’m seeing a lot of traumatic, complicated spine injuries, and a lot of adult degenerative scoliosis.”
Dr. Paul completed his MS in neurobiology and anatomy and his medical degree at the University of Rochester School of Medicine and Dentistry, during which he became an Academic Research Track Fellow. During this two-year fellowship, he did cross-departmental research in Neurosurgery and Brain and Cognitive Sciences (BCS) in the labs of Dr. G. Edward Vates and Dr. Bradford Mahon. His research focused on using diffusion MRI techniques to better understand secondary white matter injury in patients with pituitary tumors and optic nerve compression. Following Medical School, David served a seven-year residency at URMC in Neurosurgery.
“I thought it was phenomenal,” he said of his years as a researcher and resident. “What I took from it was a very strong clinical acumen. I was nurtured in a collaborative and collegial environment that sparked curiosity and a passion—not just for being a good surgeon, but for being a good doctor and caring about individuals.”
Dr. Paul also continues to manage Bold & Gritty, a business he founded while in Rochester with a twofold mission: build community around marketing quality coffee roasted here in Rochester, and leverage the brand to highlight stories of Black male success. “We are exposing the city to people they may not have realized were important,” he said. “Just recently, we got a shout-out in the Democrat & Chronicle when they used our website as a source to update their list of notable Rochesterians, with Edwin A. Robinson, the first Black man accepted to the UR School of Medicine.”

David Paul, MD (‘23) Spine and Neurotrauma Fellow University of Pittsburgh Neurosurgery
I was nurtured in a collaborative and collegial environment that sparked curiosity and a passion—not just for being a good surgeon, but for being a good doctor and caring about individuals. - David Paul, MD
Melissa A. LoPresti, MD,MPH Assistant Professor, Department of Neurosurgery Assistant Professor, Department of Public Health Sciences
NEW FACULTY
Assistant Professor
Melissa A. LoPresti, MD, MPH
Dr. Melissa LoPresti comes to UR Medicine from her most recent appointment as a fellow and clinical instructor in the Division of Pediatric Neurosurgery at Lurie Children’s Hospital, Northwestern University in Chicago. Not only does she bring her expertise in neuromodulation and minimally invasive endoscopic approaches to epilepsy surgery, but she also has a passion for serving the underserved and understanding the social determinants that creates disparities in health care.
Dr. LoPresti entered the BS/MD program at the Sophie Davis School of Biomedical Education at CCNY, which immerses medical students in looking at health and health care through a public health lens. Elected Class President at CCNT, Melissa transitioned to NYU Medical School, where she completed a concentration in health disparities and was elected to the AOA honor medical society.
She then transitioned to Baylor College of Medicine for neurosurgery residency, training at the five Baylor affiliate hospitals: MD Anderson Cancer Center, Texas Children’s Hospital, Baylor St. Luke’s Hospital, Ben Taub General Hospital, and the Houston VA Hospital. She completed clinical research in pediatric neurosurgery at Texas Children’s Hospital and earned a Master of Public Health degree at the University of Texas School of Public Health in Houston, becoming the first neurosurgery resident at Baylor to obtain an advanced degree during residency. She also completed a CAST enfolded fellowship in Neuro–Critical Care during residency. Dr. LoPresti was awarded the Kinjiro Iwata Excellence and Leadership Award prior to transitioning to Northwestern for fellowship.
Epilepsy disproportionately affects minorities, and we know that they engage with and receive less care.
- Melissa A. LoPresti, MD, MPH
She selected URMC because of its collaborative culture. “This was the only place I visited that involved the residents in the interview process,” she said. “I thought that represented values and a culture that I want to be part of.”
She intends to build a robust clinical program here for pediatric neurosurgery and epilepsy surgery, she noted—and more. “I really want to build a research infrastructure that engages with the community,” she said. “Epilepsy disproportionately affects minorities, and we know that they engage with and receive less care. I want to identify what these disparities are and why they exist, and I want to really partner with the community to help them engage in their own care, promoting health equity.”
She has several projects in the works at UR. “We’re looking at children with epilepsy and the role of neuromodulation—implanting electrodes in the brain to see where the seizure is coming from and implanting different devices to interrupt the seizure foci or network to reduce seizures.” Other projects include building a framework for community-based participatory research programs. She is also exploring the use of endoscopic surgery for epilepsy, a less invasive approach than the standard neurosurgery. “I hope to break down some of the barriers that go up when you tell a parent that their child needs brain surgery,” she said. “We’ll be looking at how to accomplish our surgical goals in the least invasive way possible in our population.”
Assistant Professor
Steven Matthew Soler, MD
Most neurosurgery departments do not include specialists in pain management, noted Steven Soler, MD, who recently joined UR Medicine Neurosurgery after completing a fellowship in pain medicine at the University of Virginia Hospitals. “Dr. Pilcher uniquely supports the pain management program in Rochester,” he said. “We can work very closely with a lot of the surgeons, and the surgeons work with us. Patients move very seamlessly between us and the surgeons. They say it really does feel like we’re working as a team.”
Dr. Soler completed his medical degree at Boston University School of Medicine and went on to an internship and residency at Boston Medical Center, where he became chief resident in his final year. After his fellowship, he made the decision to return to his hometown. “I went to Penfield High School,” he said, “and then I did the city life in Boston, and moved down to Virginia, and I realized that Rochester has that homey feel. It’s a good place to raise a family.”
He got his wish when he connected with UR Medicine Neurosurgery and the stroke division of the Neurology department. Now practicing in the medical complex on South Clinton Avenue, he began the work of building a patient population. “More than 50 percent of our patients have spine-related pain, whether it’s neck or lower back,” he said. “We see orthopedic injuries, joint pain, and post-traumatic injuries. It’s a pretty wide variety.”
His goal is to manage the pain without surgery, using nerve blocks, injections, spinal cord stimulators, and implants. “I’m seeing a lot of patients who are post-surgical and still have some pain, or people who are trying to avoid surgery altogether,” he said. “The chronic pain management field has exploded, and a lot of it is to get away from opioids. We try to exhaust all the other options before we prescribe them.”
In addition to a busy clinical schedule, Dr. Soler has begun work on several research projects, exploring aspects of trigeminal neuralgia and effectiveness of spinal cord stimulators. He is also participating in a clinical trial looking at headaches after subarachnoid hemorrhages. “Most pain physicians come from anesthesiology, but my background is in neurology,” he said. “Neurology is a small fraction of people treating pain, but it gives us an advantage as far as spine and nerve damage goes. We are in a unique position to treat chronic pain. It’s one of the advantages we provide.”
Steven Matthew Soler, MD
Assistant Professor, Clinical Neurosurgery, Department of Neurosurgery
Assistant Professor, Clinical Neurology, Department of Neurology, Stroke Division
Neurology is a small fraction of people treating pain, but it gives us an advantage as far as spine and nerve damage goes.
- Steven Matthew Soler, MD
Upcoming Events
URMC Neurosurgery
Alumni Dinner at AANS
Saturday, May 4, 2024
Four Seasons Hotel Chicago
Delaware Room on the 7th Floor
120 E Delaware Place
Chicago, IL 60611
Cocktails at 6:30 p.m. and Dinner at 7:00 p.m.
STAR- NY (Stroke Treatment Alliance of Rochester of New York)
Thursday, May 16, 2024
Hyatt Regency Rochester 125 East Main Street Rochester, NY 14604
29th Van Wagenen Visiting Professorship/ Resident Recognition. Howard Weiner, MD (Chief, Pediatric Neurosurgery Texas Children’s Hospital)
Friday, June 21, 2024
Resident Celebration at 6:00 p.m.
27th Frank P. Smith Visiting Professorship October 2024 (Date TBD)
Great Lakes Neuromodulation Conference
Friday, October 18, 2024

