NURSING
UNIVERSITY OF ROCHESTER SCHOOL OF NURSING
INNOVATION UNLEASHED
How the UR School of Nursing has embraced VR and cutting-edge technologies to revolutionize the way we teach nurses.


2023 | VOLUME 1
2023 | VOLUME 1 14
16
FEATURES
16 From Classroom to Clinical: Embracing Technology to Prepare Tomorrow’s Nurses
24 A Decade of Inspiration and Impact
Patrick Hopkins Reflects on His Journey as Co-Director of the University of Rochester School of Nursing’s Accelerated Program for Non-Nurses

DEPARTMENTS
News
Publications & Presentations
NURSING MAGAZINE credits
Interim Editor
Tim Cook
Art Director/Graphic Designer
Christine Kennedy
Feature Photography
Matt Wittmeyer
John Schlia
Gianluca D’Elia
Contributing Writers
Gianluca D’Elia
Robin Flanigan
Sandra Parker
Nora Williamson
URMC Communications
B. Chip Partner
Assistant Vice President, Director of External Communications
Alumni & Advancement Relations
Melissa L. Head ’99W (MS) Executive Director for Advancement
Andrea J. Allen Senior Director of Advancement & Alumni Relations
NURSING is published twice a year for alumni, students, and friends of the University of Rochester School of Nursing. It is published by the University of Rochester Medical Center Departments of Communications, Alumni Relations, and Advancement.


On the Cover…
Daniel Lee, an accelerated bachelor’s student who previously worked as a combat medic for the Republic of Korea Army, practices a patient scenario with VR goggles.
26 From High School to Health Care: East High Partnership Prepares the Next Generation of Nurses
30
Write to Us Editor, NURSING Magazine 601 Elmwood Avenue, Box SON Rochester, NY 14642
Share Feedback SON-Communications@urmc.rochester.edu
Read More NURSING urson.us/mag
www.son.rochester.edu
facebook.com/UofRSchoolofNursing twitter.com/UofRSON instagram.com/urnursing urson.us/LinkedInURSON
2 N URSING 2023 | Volume 1
28 Cutting Edge Courses: Inclusive, High-Tech Learning Sets UR Nursing’s Childbirth Class Apart 24
A lumni Relations & Advancement
Class Notes
4
& Events 14
33
NURSING
UNIVERSITY OF ROCHESTER SCHOOL OF NURSING
A Message from the Dean

DEAR FRIENDS,
This summer, I want to take a moment to reflect on the incredible achievements at the University of Rochester School of Nursing. Together, we have made remarkable progress that fills me with pride and hope for the future.
Our spring semester began with the exciting launch of our UR Nursing Scholars program. This unique collaboration with UR Medicine opens doors for college graduates seeking new or second careers in nursing and reflects our commitment to cultivating a diverse and inclusive educational environment. I am thrilled to meet and support our first cohort of students as they embark on this fulfilling journey.
Excellence remains at the heart of our mission. Through the efforts of our faculty, staff, students, and alumni, we have again established ourselves as the No. 1 nursing graduate school in Upstate NY, and No. 22 nationally. In April, we underwent a 10-year reaccreditation evaluation with overwhelmingly positive feedback, highlighting the outstanding work taking place within our school.
In this issue of NURSING Magazine, you’ll see how our dedication to technological advancement has helped us transform nursing education:
• How, through innovative teaching and technology, we provide our students with an unmatched learning experience that empowers them and propels their nursing careers to new heights.
• And how our state-of-the-art facility, opened just over a year ago, has quickly become an innovation and collaboration hub, fostering exciting partnerships within the University and the community.
As someone new to Rochester, I have been deeply impressed by the spirit of innovation that defines this remarkable city. During our recent graduation ceremony, keynote speaker Michael Hasselberg spoke about the Rochester way of pushing boundaries. It is a mindset that I have witnessed firsthand and one that the school will continue to embrace as we forge ahead.
In the coming months, we will come together to reassess and align our strategic goals with the evolving needs of our students and the healthcare landscape. This new strategic plan will guide us as we navigate and shape nursing’s future, ensuring that we remain at the forefront of excellence in education, practice, and research.
Throughout this season, let us continue to connect with one another and embrace the possibilities that lie ahead.
WITH WARMEST REGARDS,
 Lisa Kitko, PhD, RN, FAHA, FAAN
Lisa Kitko, PhD, RN, FAHA, FAAN
 Dean, School of Nursing Vice President, University of Rochester Medical Center Professor of Nursing
Dean, School of Nursing Vice President, University of Rochester Medical Center Professor of Nursing
N U RSING 2023 | Volume 1 3
UR NURSING Job Opportunities
Paving a Path to a New Nursing Career


UR Nursing Scholars program strengthens pipeline for nursing workforce with tuition-free nursing education, guaranteed job placement at UR Medicine.
To combat the region’s nursing shortage, the University of Rochester Medical Center and School of Nursing announced an innovative program in early 2023 to provide a tuition-free nursing education. This fall, the first cohort of 40 UR Nursing Scholars will begin the accelerated program and just one year later start practicing as nurses at Strong Memorial or Highland hospitals.
New York State faces a projected registered-nurse shortage of nearly 40,000 by 2030 due to burnout from the pandemic, an aging population, and a wave of retirements. University leadership believes this program is the first to combine guaranteed employment as a registered nurse with a fully paid education for college graduates at a nationally ranked nursing school. The UR Nursing Scholars program will cover 100 percent of tuition costs for Accelerated Bachelor’s in Nursing students at the University, after they pass their NCLEX-RN® licensure exam and in exchange for committing to work at participating UR Medicine facilities for three years after graduation.
“This innovative program leverages multiple strengths of our academic medical center to address a critical community need,” said Mark Taubman, MD, CEO of URMC and dean of its School of Medicine & Dentistry. “We provide world-class nursing education programs with hands-on experience in virtually every clinical specialty area. By making education available at no cost to students who are new to nursing, we provide them with outstanding career

opportunities, while helping Strong Memorial and Highland hospitals address nurse shortages and expand access to care for our patients.”
The 12-Month Accelerated Bachelor’s in Nursing Program offers a unique opportunity for bachelor’s-prepared college graduates to pursue a second nursing career. The program has attracted students from across the US and New York State with diverse backgrounds and experiences—some with previous careers in public health, business, or education. Each cohort is guided through a rigorous yearlong immersion into nursing, including 700 hours of clinical training in med-surg, obstetrics, pediatrics, psychiatry, and other specialties at URMC.
“Our school has earned a reputation for preparing highly skilled nurses who are ready to enter the workforce and care for patients immediately after graduation,” said Lisa Kitko, PhD, RN, FAHA, FAAN, dean of the School of Nursing and vice president of URMC. “The UR Nursing Scholars program will make this outstanding education more accessible to students from our community and across the nation, helping us to recruit from groups underrepresented in nursing and create a more diverse workforce that better represents all the patients served by UR Medicine.”
The full-time program enrolls students across three cohorts per year, with more than 100 students to be accepted into the UR Nursing Scholars program annually and matched with Strong
4 N URSING 2023 | Volume 1
NEWS AND EVENTS
Memorial or Highland hospitals. Once accepted, students will receive funding in the form of a scholarship and a forgivable loan from the School of Nursing to cover all tuition costs.*
Students accepted to the program will work closely with a career coach to explore specialties and career opportunities in nursing. Scholars will also meet with nursing recruitment and retention offices to match their interests with an employment opportunity at participating UR Medicine facilities.
“UR Medicine hospitals are committed to offering all our nurses competitive pay and benefits, along with a supportive work environment, flexible scheduling to support work-life balance, and opportunities for growth,” said Karen Keady, PhD, RN, NEA-BC, vice president and chief nursing executive at URMC and assistant dean of clinical practice at the School of Nursing. “As our UR Nursing Scholars gain on-the-job experience, they will become eligible for tuition benefits to further their nursing education and advance their careers as far as they want to go, without ever needing to leave the Medical Center.”

Graduates then sit for the NCLEX-RN® exam to obtain RN licensure and start practicing as nurses within three months of completing the program. Salarys and benefits offered to UR Nursing Scholars will be competitive for new bachelor’s-prepared nurses.

SHARE THIS OPPORTUNITY
Know someone interested in pursuing a new career in nursing? Applications are being accepted every semester for the UR Nursing Scholars program. For details and requirements visit urson.us/nursing.
“I worked alongside various medical professionals during my time as a nursing home phlebotomist and activities assistant. I witnessed firsthand how a positive interaction with residents can benefit them by improving their mental health. They were looking forward to our visits, even if it meant having their blood drawn! That’s when I knew nursing was the right fit for me.”
JILLIAN KELLY
UR Nursing Scholar Fall ’23
Current Role: Phlebotomist at the Montgomery Nursing & Rehabilitation Center Previous Degrees: BS in human biology, BA in emergency preparedness, homeland security, and cybersecurity
“I am making the transition into nursing because I want to connect with people and have an immediate impact in their lives. I have learned so much working in scientific research, and I’m excited to bring that knowledge into my connection with my patients.”
MICHELLE MILLAR
UR Nursing Scholar Fall ’23
Current Role: Postdoctoral associate, Rahman Lab at the University of Rochester School of Medicine & Dentistry Previous Degrees: BS in biology, PhD in biomedical genetics
“I am thrilled to be accepted to the UR Nursing Scholars program as it will enable me to serve the Rochester community as an RN upon graduation. I never want to stay stagnant and look forward to a life full of learning … Our community needs nurses and I am honored to join this profession and serve the Rochester area.”
Caroline Roets


UR Nursing Scholar Fall ’23
Current Role: Lead pharmacy technician, CVS Previous Degrees: BS in biology and psychology, minor in neuroscience
N U RSING 2023 | Volume 1 5
UR Nursing Ranks in Top 25 for Best Graduate Schools
The UR School of Nursing has been ranked No. 22 among U.S. nursing schools for its master’s programs, according to the 2023–24 Best Graduate Schools guide produced by U.S. News and World Report.
The school’s master’s programs have ranked in the Top 30 for the past four years and consistently appeared in the Top 40 over the past two decades. Among its regional competitors, the UR School of Nursing is the only New York school outside of New York City to rank in the Top 25 in master’s programs.

“These rankings underscore the school’s continued commitment to nursing excellence,” said Lisa Kitko, PhD, RN, FAHA, FAAN, dean of the School of Nursing and vice president of the University of Rochester Medical Center. “We have a talented team of faculty and staff who continuously seek new and innovative ways to teach and support our nursing students. Our goal is to produce highly skilled and compassionate leaders, educators, and practitioners who are prepared to play a crucial role in shaping and leading the future of health care to improve patients’ outcomes.”
“This ranking is not only a recognition of our past achievements but also a celebration of the bright future
IN THE NEWS
Dean Lisa Kitko, PhD, RN, FAHA, FAAN, spoke to WXXI News and Medscape about the launch of the UR Nursing Scholars Program and its role in reducing the statewide nursing shortage.
Assistant Professor Meghan-Underhill Blazey, PhD, APRN, AOCNS, spoke to 13WHAM about colon-cancer screenings and prevention during the Wilmot Cancer Institute’s colorectal cancer awareness event, where visitors were invited to walk through an interactive, inflatable colon exhibit and talk to experts about gut health.
ahead for our school and our graduates,” said Lydia Rotondo, DNP, RN, CNS, FNAP, associate dean for education and student affairs. “Our students are exposed to cutting-edge curricula, innovative experiential learning experiences, and an incredible support system, all of which prepares them to tackle the challenges ahead and make a difference in the lives of their patients and communities.”
U.S. News surveyed 648 nursing schools with master’s or doctoral programs accredited by either the Commission on Collegiate Nursing Education or the Accreditation Commission for Education in Nursing. In total, 296 nursing programs responded to this U.S. News nursing statistical data collection survey sent in fall 2022 and early 2023.
From this data collection, U.S. News calculated the rankings based on several factors, including research productivity, faculty resources and preparation, program size, student excellence, and qualitative ratings from colleagues.
Jennifer Dry De Santo, MSEd, care manager for The Western New York Comprehensive Care Center for Eating Disorders, appeared on News10NBC for a live interview about Eating Disorders Awareness Week. News10NBC also featured Santo Caruana, a local college student in recovery who volunteers in WNYCCCED’s advocacy efforts.
Assistant Professor of Clinical Nursing Maria Marconi, EdD, RN, CNE, spoke to WROC News 8 and News10NBC about the in-person return of the “Pathways to Nursing” course, which welcomes local students from East High School to discover different possibilities in nursing careers and to learn clinical, research, and professional skills.
6 N URSING 2023 | Volume 1 NEWS AND EVENTS
UR Nursing Earns International Endorsement for Simulation Education
The School of Nursing received an endorsement from the International Nursing Association of Clinical and Simulation Learning (INACSL) for its simulation education programming— the first New York nursing school to earn this recognition.
This recognition came just months after the opening of the school’s vertical expansion, a state-of-the-art facility that includes four debriefing rooms to accompany four simulation suites, a skills lab with 20 patient beds that replicates a hospital environment, and high-fidelity human simulation mannequins for a wide range of scenarios involving adult, child, and infant patients.
“This endorsement demonstrates the School of Nursing’s leadership in innovative nursing education, and our commitment to creating learning experiences that prepare the next generation of nurses,” said Lydia Rotondo, DNP, RN, CNS, FNAP, associate dean of education and student affairs.
“We are proud to have a dynamic learning environment and a team of experts that prepare our nurses to respond to ever-changing health system demands.”
INACSL’s endorsement recognizes excellence in applying the organization’s four core Health Care Simulation Standards of Best Practice: pre-briefing, facilitation, professional integrity, and the debriefing process.

“Engaging students in activities that foster critical thinking and improve clinical judgment is an important part of our curriculum,” said Director of Simulation Erin S. Baylor, DNP, RN, PNP-BC, ONP. “By providing high-quality simulation education, we equip students with the clinical skills and confidence that will set them up for success when they leave the classroom.”
Professor Wang Named JMIR Aging Co-Editor-in-Chief
Assistant Professor Jinjiao Wang, PhD, RN, MPhil, has been named co-editor -in-chief of JMIR Aging, an open-access journal focused on digital health, clinical care, patient education, and other older-adult health topics.

Wang is a nurse scientist at the Elaine C. Hubbard Center for Nursing Research on Aging and director of postdoctoral programs at the School of Nursing. Her research focuses on improving the quality, equity, and efficiency of home-based health care services for older

adults. Her goal as a nurse and researcher is to help older adults maintain independence and safety at home through targeted and effective home-based services.

In her new role, Wang will focus on expanding JMIR Aging’s editorial board and peer-reviewer community, and facilitating the publication of more high-quality articles in the field of aging that can transform, advance, and innovate geriatric care models and delivery. Wang will serve in this role alongside co-editor-in-chief Yun Jiang, PhD, MS, RN, FAMIA, an assistant professor at the University of Michigan School of Nursing.
Pilot Funding Supports Heart Attack Treatment, Rural Health Literacy Studies
Two members of the School of Nursing community received funding from UR’s Clinical & Translational Science Institute in support of upcoming research projects.
Postdoctoral Research Associate Sukardi Suba, PhD, RN, and fourth-year PhD student Lindsay Batek, ND, RN, FNP-C, received faculty and trainee awards from CTSI’s Pilot Study Program, which helps UR researchers lay the foundation for innovative projects that move new discoveries forward to patients and the community.
Suba’s pilot study, “Significance of Symptom Onset-ToAngiography Time in Non-ST-Segment Elevation Myocardial Infarction (NSTEMI),” will explore whether the time from onset of symptoms to angiography is a significant factor in the management of non-ST-elevation myocardial infarction.
Batek’s project, “Positive Deviance and Health Literacy: Underexplored Constructs for Successful Translational Science,” is a community-engaged, mixed-methods study that will explore the relationship between health literacy and health care access from the perspective of rural Mexican American young women.
N U RSING 2023 | Volume 1 7
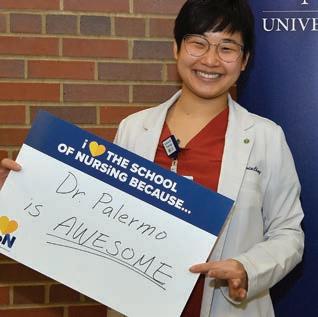
I HEART SON DAY

Every year, the School of Nursing’s “I Heart SON Day” event invites current students to share what they love about the School of Nursing and write thank-you notes to alumni and donors who have helped make it a place they love. Here’s a look at how we celebrated in 2023.
Adult-Gerontology

Acute Care Nurse

Practitioner graduate student

Sylvia Chang shares why she loves the School of Nursing with a shout-out to her program director, Assistant Professor of Clinical Nursing Beth Palermo.

A group of accelerated bachelor’s students celebrate “I Heart SON Day” with Francis the therapy dog. Front: Madi Potter, Alysia Hommes; Back: Johnnathan Lopez, Kelly Malepe, Esther Shin, and Honesty Washington.

Accelerated bachelor’s students Natasha Blaise and Grace Smith share their favorite things about the school.
Members of the School of Nursing Student Affairs Office–Dave Hoffman, Liz Bremer, Olivia Harrington, and Sara Stabley–share what they love about the school.

Accelerated bachelor’s student Alice Fiatsonu writes a thank-you note to donors and alumni.




Bachelor’s student Andrew Barbour celebrates with an “I Heart SON” cookie and this year’s gift: a free water bottle.

8 N URSING 2023 | Volume 1
NEWS AND EVENTS
Remembering Our ‘Why’ December Grads Step into New Nursing Careers

Every year, hundreds of new students come to the School of Nursing from varying backgrounds, with the common goal of launching a nursing career. Their ages, previous bachelor’s degrees, and past careers cover a wide spectrum.
At the school’s most recent pinning ceremony on Dec. 14, 2023, more than 60 of the school’s newest accelerated bachelor’s in nursing graduates were reminded that their diversity and common goals were among their greatest strengths as a cohort.






“Wanting to be nurses is the commonality that holds us together,” said class speaker Dean Viggiano ’22N. “We’ve learned and grown so much together over the course of this past year. We’ve learned to always remember our ‘why’ as we step into our new careers, and we’ve learned firsthand from our professors and clinical instructors just how far a passion for caring for others can get you.”
December’s pinning ceremony also marked significant milestones.
Lukira “Lucy” Carroll, former executive assistant to the dean and special events coordinator, celebrated her last pinning ceremony before retiring at the end of December. She worked for the University for 44 years and spent 28 of those years at the School of Nursing.
Beloved by students, faculty, and staff, Carroll is known by many for her warmth, bright personality, infectious sense of humor, and constant care for those around her. She has even appeared on stage as a pinner for several nursing graduates in past ceremonies.

Lisa A. Kitko, PhD, RN, FAHA, FAAN, celebrated her first ceremony as the school’s new dean. Kitko shared encouragement for the newest nursing graduates and advice based on her own nursing experiences as a nurse and researcher.

“As nurses, we have the distinct privilege and honor to interact with patients and their family members during some of their most challenging times,” Kitko said. “Based on my research, not only will you remember that as a nurse, but the patients and families will remember that as well.”
“Always be an advocate and a voice for your patients, and always take the time to listen to family members and caregivers,” she added.
N U RSING 2023 | Volume 1 9
Catalysts of Change: Celebrating the Class of 2023
That’s what URMC CEO Mark Taubman, MD, told more than 240 graduates at the School of Nursing’s Spring 2023 graduation ceremony before they received their diplomas at the Eastman Theatre’s Kodak Hall on May 12.



“In the case of nursing, we have seen a veritable explosion of options in the past decade,” Taubman said. “This graduation is perhaps the best example of this, in that many of you are getting your second, or even third, degree.”

Taubman’s message of self-reinvention rings true for the Class of 2023, as many of them prepare to advance as nurse practitioners, educators, and leaders.

“We are uniquely positioned to affect the lives of our patients and their loved ones in their most vulnerable times,” said graduate speaker Javauni Forrest ’18N, ’23N (MS), a graduate of the Psychiatric Mental Health Nurse Practitioner program who is pursuing his Doctor of Nursing Practice.
“Use that privilege to not only embrace your students, employees, and patients for all that they are, regardless of race,
gender, socioeconomic status, or sexual orientation, but to imbue them with the understanding that they are valued and worthwhile simply because they are.”
Accelerated bachelor’s students, too, have undergone a significant transformation. Most of them changed careers to nursing from other fields, such as social work, education, or scientific research. They will soon be starting their first jobs as registered nurses.
“I have witnessed my classmates, all of them former nonnurses, go above and beyond for their patients, time and time again,” said class speaker Beau Iverson ’23N. They’ve inspired meaningful, positive change in the lives of their patients and team members around them, and they’ve inspired me to do the same.”
As graduates prepare to start new chapters in a broad range of roles, School of Nursing Dean Lisa Kitko, PhD, RN, FAHA, FAAN, said it’s a reminder of how founding dean Loretta C. Ford’s vision for the nursing profession has become a reality.

10 N URSING 2023 | Volume 1 NEWS AND EVENTS
During a nursing career, it’s possible to reinvent oneself many times.
More than 50 years ago, Ford and pediatrician Henry Silver originated the nurse practitioner position, sparking new possibilities for nurses’ roles in health care.
“Dr. Ford recognized the opportunities for nurses to play a key role in providing patient-centered care,” Kitko said. “Her willingness to challenge the status quo and mobilize support across health care paved the way for the advancement of the nursing profession.”
“You have an opportunity to think creatively, ask tough questions, and draw upon your experiences to discover new solutions that will change patient care as we know it.”
family. It was nurse practitioners who launched telehealth in a matter of days to reach those in rural and urban areas.”
During the ceremony, School of Nursing Instructor of Clinical Nursing Kristina Santory ’06, ’14W (MS) received the annual Dean’s Award for Excellence in Teaching. Student nominators praised Santory, who is also a registered nurse in URMC’s Cardiac Catheterization Lab, as a “beacon of advocacy” who prioritizes students’ wellness and goes above and beyond to help them succeed.
This year also marked a significant milestone for Taubman, who celebrated his last graduation ceremonies as dean of the School of Medicine & Dentistry and CEO of URMC


In his keynote address, UR Medicine Chief Digital Health Officer Michael Hasselberg ’07N (MS), ’13N (PhD) reflected on the spirit of technology innovation that has been the hallmark of Rochester‘s history—from Eastman Kodak Company’s pioneering work in digital imaging to URMC’s digital reimagining of health care equity for people of all walks of life.
after announcing in September that he will step down from his role. Kitko shared her gratitude for Taubman’s leadership and collaborative spirit.
“Dr. Taubman has been a true partner in advancing the health of our community,” Kitko said. “Thanks to Dr. Taubman’s commitment, we have been able to work together to better prepare a new generation of health-care professionals.”
Taubman reminded the Class of 2023 that the future of health care is bright, thanks to them.
Many nursing graduates started their journeys into health care careers when the COVID-19 pandemic was at its worst. Hasselberg recognized the courage and commitment of nurses who followed their calling to care for others through challenging times.

“We can’t ignore the context of celebrating your achievements: COVID upended life as we know it, and few have been as deeply impacted as nurses,” Hasselberg said. “It was our inpatient nurses who shared iPads so patients could speak with
“We have given you the foundation to make a difference in how health care is delivered in the 21st century,” Taubman said. “As you move forward in your careers, you will have the satisfaction of shaping how we deliver health care true to the University’s motto—Meliora, to something Ever Better … When I look at our graduates, I know we are in great hands.”
N U RSING 2023 | Volume 1 11
“Be bold, dream big, and let your passion for nursing be the catalyst of change,” he told graduates. “May you push the boundaries of what is possible. That is the Rochester way.”
Dean’s Diamond Circle Dinner HONORS
ALUMNI, DONORS
At this year’s Dean’s Diamond Circle dinner, hosted by the School of Nursing, the following alumni and donors were honored for making a lasting impact in the community:


Distinguished Alumnus Award: Dianne C. MorrisonBeedy ‘93N, PhD, RN, WHNP, CGNC, FFNMRCSI, FNAP, FAANP, FAAN, the chief talent and global strategy officer and centennial professor of nursing at The Ohio State University. Morrison-Beedy has successfully established student education, faculty research endeavors, and collaborative global partnerships across multiple continents.
Legacy Award: Dennis L. Kitzman, who together with his late wife, Harriet J. Kitzman, ’61W (MS), ’84N (PhD), RN, FAAN, has left an indelible mark on the School of Nursing, most recently by establishing the Dennis L. and Harriet J. Kitzman Endowed Fellowship Fund. Harriet Kitzman, who passed away in March 2020, was the longtime senior associate dean of research at the School of Nursing.
Dean’s Medal: Professor Emerita Margaret (Maggie) H. Kearney, PhD, RN, FAAN, a nationally recognized expert on rigorous qualitative research. Kearney’s early research centered on the health perceptions and decisions of socially high-risk pregnant and parenting women, health perceptions and decisions, and she specialized in the study of health behavior using systematic naturalistic approaches to the analysis of open-ended interviews and observations.
DILLON DZIKOWICZ Earns Accolades for Dissertation

In spring 2023, Dillon Dzikowicz ’17N, ’21N (MS), ’23N (PhD), PCCN, CMC, CSC, successfully defended his dissertation, “Differentiating NSTEMI Patients with and without an Occluded Culprit Artery.” Shortly after, he was named the recipient of the 2023 Eastern Nursing Research Society/ Council for the Advancement of Nursing Science Dissertation Award, and the International Society for Computerized Electrocardiology recognized his dissertation work with the Best Poster Award during the annual ISCE conference in California.
Dzikowicz’s research aims to utilize machine learning and novel electrocardiographic features to improve the treatment stratification of patients suffering from heart attacks. After graduating from the PhD program in May, he will continue his research as an assistant professor at the School of Nursing.
WONKYUNG CHANG
Accepted to Minority Fellowship Program
MS-PhD student
Wonkyung Chang, RN, BSN, has been named the recipient of a minority fellowship from the U.S. Department of Health and Human Services’ Substance Abuse and Mental Health Services Administration (SAMHSA).

The minority fellowship program prepares doctoral and master’s students in health care professions to support SAMHSA’s mission of eliminating behavioral health disparities among racial and ethnic minority populations.

T he SAMHSA fellowship is a perfect match for Chang’s research interest in substance use disorders among minority populations, particularly immigrants and sexual minorities within immigrant groups.
“I felt so happy and honored when the committee members told me that I was accepted to this prestigious program as a doctoral fellow,” Chang said. “Through my practice and research, I would like to help minority populations and immigrants who need more mental health support. That is my goal during my PhD program, and my life goal.”
Chang is a combined master’s and PhD student and is pursuing the Psychiatric Mental Health Nurse Practitioner specialty. She works as a certified nurse at Hillside Children’s Center, where she cares for youth who have experienced trauma. Before moving to the US, she worked as a psychiatric nurse in an inpatient alcohol treatment center in her home country, South Korea.
“I am impressed with Wonkyung’s efforts and passion in her research and community involvement to demonstrate a commitment to diversity, equity, and inclusion during her studies at the School of Nursing,” said Assistant Professor Chen Zhang, PhD, MPH, Chang’s adviser. “I am confident that through the SAMHSA Minority Fellowship Program, Wonkyung will not only be able to help numerous patients but will also contribute to furthering addiction treatment and research.”
MARTEZ SMITH
Earns UR Presidential Diversity Award
Nursing and Health Science PhD candidate Martez D.R. Smith, LMSW, was recognized at the University of Rochester’s annual Presidential Stronger As One Diversity Awards. Smith is a recipient of the Change Maker Award, which recognizes a student who aims to cultivate a fair and just climate, culture, and community at the University and in surrounding communities.
“He has all the hallmarks of an exceptional researcher: curiosity, rigor, resourcefulness, and persistence,” said Associate Professor James McMahon, PhD, Smith’s dissertation advisor. “Most importantly, he has a deep passion for improving the health and quality of life of those he serves, especially members of marginalized communities.”
Smith is a licensed social worker, sexual health researcher, and activist who has dedicated his life to educating and caring for individuals affected by AIDS and other health disparities. For his dissertation, Smith examined associations between sexual health communication and motivations for sexual health behaviors among Black and Latino men who have sex with men and who participate in New York City’s House Ball Community. His work has been supported by the National Institutes of Health and the School of Nursing’s Interdisciplinary Sexual Health and HIV Research Group.
A member of the ballroom community himself since age 18, Smith has experienced firsthand the direct impact of HIV/AIDS on fellow house members. Personal experience has motivated Smith to raise awareness, promote education, support advocacy efforts, and implement impactful strategies to end the HIV epidemic.
Smith will continue to focus on HIV and sexual health after he completes his PhD. He was offered a postdoctoral fellowship with the HIV Center for Clinical and Behavioral Studies at the New York State Psychiatric Institute and Columbia University, focusing on behavioral sciences training in HIV infection.

N U RSING 2023 | Volume 1 13 STUDENT AWARD NEWS
Dillon Dzikowicz receives the 2023 ENRS/Council for Advancement of Nursing Dissertation Award.
PH D STUDENTS, FACULTY REPRESENT UR Nursing at ENRS Scientific Sessions

Below is a selection of publications and presentations from UR Nursing researchers. Read more about our research at son.rochester.edu/research.
Highlighting Health Disparities at the Society of Behavioral Medicine Conference

Maria M. Quiñones-Cordero, PhD, presented her research findings at the 2023 Society of Behavioral Medicine’s Annual Meeting in Phoenix, Arizona. These findings highlight disparities in the recruitment of socially disconnected middle-aged and older Latino dementia caregivers. Her research findings were recently published in Clinical Gerontologist. She also chaired a panel titled “Latinos’ Engagement in Behavioral Medicine Trials: Fostering Success,” in which Professor of Nursing Kathi Heffner, PhD, also presented as a panelist.
Alarm Database Helps Train Computer Algorithms to Better Recognize and Predict Fatal VT Arrhythmias among Hospitalized Patients, Research Shows
Ventricular tachycardia (VT) is a lethal cardiac arrhythmia; and computer accuracy of identifying VT is less than 10 percent; which jeopardizes patient safety and significantly contributes to alarm fatigue among clinicians. Five PhD-prepared nurse scientists, including Professor of Nursing Mary Carey, PhD, RN, FAHA, FAAN, collaborated across the University of California San Francisco, University of Rochester, University of Pittsburgh Medical Center, and the University of North Carolina-Chapel Hill. Together, the team manually annotated over 22,000 VT alarms from more than 500,000 hours of ECG monitoring to generate one of the largest collections for training computer algorithms to accurately recognize and predict fatal VT arrhythmias among hospitalized patients. The study found that creating high-quality, well-annotated datasets for algorithm development and testing can ultimately improve patient outcomes and reduce alarm burden. The study was published in the Annals of Noninvasive Electrocardiology.
CARDIAC CARE RESEARCH

14 N URSING 2023 | Volume 1
A team of PhD students and faculty represented the School of Nursing at the Eastern Nursing Research Society’s (ENRS) 2023 Scientific Sessions in Philadelphia in March. The school was also an exhibitor at the conference this year.
AGING RESEARCH
PUBLICATIONS & PRESENTATIONS
ONCOLOGY RESEARCH
Unsupervised Machine Learning Identifies High-Risk Symptom Clusters in Older Adults With Advanced Cancer, Study Finds
A secondary analysis of a cluster-randomized trial found that unsupervised machine-learning methods can effectively be used to identify older adult patients with advanced cancers who are at higher risk for adverse outcomes based on their baseline, patient-reported symptoms. Wilmot Cancer Institute and School of Nursing researchers, including Associate Professor of Nursing Marie Flannery, PhD, RN, were among the collaborators on this study, which was published in JAMA Network Open in March. The findings also reinforce the importance of routine symptom assessment prior to treatment initiation as a best-practice standard, the authors said. In invited commentary on the study, Carolyn Presley, MD, MHS, an oncologist at The Ohio State University, said the study can improve care teams’ understanding of who will experience cancer treatment-related side effects, especially as the number of new cancer drugs rapidly grows.

Nursing Researchers Present Studies on Adolescent Body Image, Sexual Health
Postdoctoral Research Associate Sadandaula Rose Muheriwa, PhD, and Assistant Professor Meredith Kells, PhD, RN, CPNP, attended the Society for Adolescent Health and Medicine’s (SAHM) annual meeting in Chicago, Illinois, in March. Muheriwa, a newly minted SAHM member, presented a study titled “Community Stakeholders’ Perspectives on Young Adolescents Sexual Health Research in Western New York, USA: A Qualitative Descriptive Study.” The study, conducted in a partnership with the City of Rochester Department of Recreation and Human Services, was advised by Assistant Professor Natalie Leblanc, PhD, MPH, RN, BSN, and involved collaboration with community members. Kells has been a SAHM member for more than 10 years, and has served on the Planning Subcommittee for Networking and Career Development for the last two years. She presented the study “Weight/ Shape-Related Motivators for Use Moderates the Relationship Between Social Media Use and Body Image.” Both studies have been published in The Journal of Adolescent Health.

PARENT-CHILD, ADOLESCENT, & TRANSGENERATIONAL HEALTH RESEARCH
Researchers Represent UR Nursing at ANAC Conference
Researchers from the School of Nursing’s Interdisciplinary Sexual Health & HIV Research group (INSHHR) attended the Association of Nurses in AIDS Care’s (ANAC) annual conference in November: Chen Zhang, PhD, MPH; Sadandaula Rose Muheriwa, PhD; Natalie Leblanc, PhD, MPH, RN, BSN; Faith Lambert, MS, RN, FNP-BC, who was a 2021 Diversity, Equity, and Inclusion Student Fellow for ANAC; and Mitchell J. Wharton, PhD, RN, FNP-BC, CNS, ACRN, president-elect of ANAC. Zhang delivered two presentations: “You don’t think about it until someone else brings it up to you: Women’s Sexual Health and PrEP care at the Primary Care Settings in the United States” and “Understanding the association between PrEP stigma and PrEP cascade: a moderation analysis.”

N U RSING 2023 | Volume 1 15
SEXUAL HEALTH & HIV RESEARCH
From Classroom to
Clinical: Embracing Technology to Prepare Tomorrow’s Nurses
Nursing’s future is marked by disruption, driven by such factors as the global nurse shortage, changes in technology, and a shift toward disease prevention and health equity. During the past five years, the School of Nursing has revamped its education approach to prepare nurses for this future. Embedded in this innovative approach are cutting-edge tools and technologies to create learning environments that promote active learning, student engagement, and collaboration.

16 N URSING 2023 | Volume 1 COVER STORY
A group of East High School students from the City of Rochester huddle around a mannequin lying on a hospital bed. In a room behind the one-way glass wall, the simulation educator halts our conversation and presses a button on the control panel.
“I’m sore right there,” he says into the microphone. The words appear to come from the mannequin, causing the students to burst into laughter and jump back from the bed. The students know that real nursing doesn’t involve a talking doll, but it’s a fun way to learn about the field.
The mannequin, a high-tech patient simulator, is one of the technological innovations used by the University of Rochester School of Nursing in transforming its curriculum from the didactic to the interactive and experiential. The result is graduates who are more competent, confident, and prepared to contribute immediately upon entering the workforce and throughout their nursing careers.
The curriculum pivot is vital because lectures are inadequate preparation when searching for a plump vein in the arm of a quivering patient.
However, innovative education is about more than purchasing the latest equipment and using it as directed— the School of Nursing continuously reinvents its curriculum in anticipation of the health care challenges still to come in the 21st century.
In recognition of its innovative use of iPads and Apple TV, the School of Nursing has earned Apple Distinguished School status. And judging by the approbation received at a recent conference and requests from other schools for advice, the school is in the vanguard of transforming nursing education.
“We tell potential applicants that if you want to just sit and learn passively through PowerPoints, this isn’t the school for you,” said Erin Baylor, DNP, RN, PNP-BC, ONP, director of simulation.
Message received.
“The technology swayed me into choosing this program,” said Laura-Ann Fierro, who graduated in the spring from the accelerated bachelor’s degree program. “It makes our learning so much easier. I’m as ready as I could ever be coming from nursing school.”
Students practice a wide range of technical, social, and critical skills through simulation with mannequins and standardized patients as well as interactive exercises on the
school-issued iPads. For scenarios impractical to reproduce, the school’s virtual technology transports students there. If you have to do it on the job, you can do it here first.
“Thirty years ago, there was no opportunity to safely practice. The first time I inserted a catheter, my hand was shaking,” Baylor said. “Now a student can learn about heart disease and then come in the next day and work on a ‘patient’ with cardiac complaints. It reinforces concepts and translates well to real patients.”
Everyone and everything at the school are linked via an array of the latest software applications. In fact, for most students there is no paper at all except for the diploma. The school-issued student iPad is a curriculum vault, holding textbooks, lectures, interactive clinical exercises, and simulation recordings.
Students have full access anytime to information, which better prepares them for class time that focuses primarily on experiential learning. And no more huddling around the standardized patient being examined; cameras send a live closeup directly to student iPads and to the immense television sets dotting the rooms. The goal is to not only incorporate more technology into the old framework, but to use it to create an entirely new framework.
“We’re officially changing the culture, and now it becomes the norm,” said Tara Serwetnyk, EdD, RN, NPD-BC, director of academic innovation. “We can focus on activities that not only provide practice but foster critical thinking and improve clinical judgment.”


To integrate advanced technology into the curriculum, the school looked to an old Hollywood tactic. Need a hospital? Just make one. And that’s exactly what the School of Nursing did.
SIMULATION: BRINGING THE CLINICAL SETTING TO THE CLASSROOM
To accommodate the school’s reimagined curriculum and technological advancements, three floors were built onto the single-story Helen Wood Hall on Crittenden Boulevard. The $15.1 million expansion added 26,000 square feet and was completed in May 2022. The no-nonsense, brick-and-glass structure is now part hospital, high-tech conference center, classroom, office, and study space. The expansion also allowed ample space for the 169 faculty and nearly 700 students, a 50 percent rise in enrollment since 2016.
N U RSING 2023 | Volume 1 17
Four years earlier, the School of Nursing introduced the iROC initiative to kick off its journey to redefine nursing education. Since then, the curriculum has been radically altered to make it more flexible, efficient, interactive, and relevant to actual clinical practice.
“Today, we live in a world where technology advances at an unprecedented pace, and the profession of nursing is no exception,” said Lydia Rotondo, DNP, RN, CNS, FNAP, associate dean for education and student affairs and DNP program director.
“As educators, it’s our responsibility to stay on top of technological advancements and find innovative ways to integrate them into our curriculum,” Rotondo added. “By doing so, we provide our students with more personalized and engaging learning experiences, improve access to resources and flexibility, and enhance collaboration and communication among students and faculty. This digital-learning environment enables us to meet learning challenges head on to ensure our graduates have the skills and knowledge needed to succeed in a rapidly changing health-care landscape.”
Nursing education had already moved past the days when students dutifully carried around thick textbooks, listened for hours to anatomy lectures, and occasionally practiced on real
patients. But more change was needed to advance deeper into the flipped classroom concept, in which foundational learning is done at home, and class time is free for interactive, collaborative, and critical skill practice. Many nurses working today did few or no simulations in school.
In recognition of the value of simulation, a bill signed by New York Governor Kathy Hochul will allow simulation exercises to count for 30 percent of clinical training hours. Baylor points out that simulation is more varied than clinical training and also more efficient because there is no downtime.

Simulation training begins in the second week for students in the Accelerated Nursing Programs for Non-Nurses. In one year, students will participate in 15 virtual-reality scenarios and 43 simulations. Students are prepared ahead of time with lecture content, followed by a pre-briefing of the scenario, the simulation, and a debriefing.

Some simulations are done with the mannequins, spelled manikins to distinguish them from the non-tech ones common in the fashion industry.
The School of Nursing has two SimMan 3G and four SimMan Essential adult manikins. They are high-fidelity, or lifelike, with options for skin tones and gender. Each manikin has a pulse and a port for fluids. Its lungs and intestines make sounds. It can blink, bleed, breathe, and urinate. You can inject it, intubate it, defibrillate it. There is also a baby manikin, a juvenile one that can have a seizure, and a
18 N URSING 2023 | Volume 1
As educators, it’s our responsibility to stay on top of technological advancements and find innovative ways to integrate them into our curriculum.”
-Lydia Rotondo, DNP, RN, CNS, FNAP, associate dean for education and student affairs and DNP program director
pregnant one that gives birth. Despite these functions, the manikins, of course, still look fake, with their blank stares and perfectly coiffed hair. “We say to the student that we are establishing a fiction contract,” said Kimberly Buholtz, EdD, RN, PED-BC, CHSE. “This might not feel real, but we ask you to treat this as a real patient.”
At first there are a few nervous chuckles, but students quickly become immersed and serious. The simulations are not just about practicing technical skills; students work in pairs to practice collaborating and developing clinical judgment.
“Their actions are very realistic,” said Buholtz. “They’re not treating it as a piece of plastic.”
Students speak to the manikins, who respond, and can also give medications; order and review labs; and call the pharmacy, charge nurse, or the patient’s primary doctor and receive an immediate response. Faculty in the control room are always rooting for the students to make the best decisions. “Sometimes we yell ‘YES!’ and throw our arms up in the air when the students make clinical connections,” Buholtz said.
Students are encouraged to be curious and to explore treatment possibilities. The faculty view it as a psychologically safe place to learn. “They’ll be corrected but not punished for mistakes, which are puzzles to solve,” Buholtz added. “It’s not a gotcha. It’s designed to be a learning experience in a safe way.”
Joshua Billings, a recent graduate of the accelerated program for non-nurses, said the simulations felt realistic. “You’re taking actions as if in a clinical setting, and the effect is weightier than just getting a question answered in class.” The bulk of the learning takes place in the debriefing room, where students assess the simulation and review the comments made by the faculty member during the session directly onto the video, using SimulationiQ software. Buholtz said she points out the positive actions, not just the areas for improvement. “A lot of times they’re catching it first. It’s really powerful for them to see it themselves. That’s where the magic is for an educator.”
Recent graduate Fierro found the simulations particularly helpful. “Nursing is not a cookie-cutter profession; there are many different ways to do things,” Fierro said. “A faculty member might ask why we decided to put in a nasal cannula instead of a non-rebreather. And then we can talk about it.”


The simulation videos are saved on the students’ iPads, allowing for later review. In clinical practice, a nurse might not experience a similar scenario for weeks, by which time the particulars aren’t as fresh. With the videos, students can review soon and often, solidifying retention.
In addition to providing practice, simulations also present an opportunity for students to take the role of an RN and stretch their skills, which they would not be able to do as a new nurse. Faculty are constantly retooling and reinventing the scenarios. One in development follows up a clinical simulation with a legal proceeding that centers on the completeness of the nurse’s documentation. The idea is to show the importance of careful notes, which can become part of a lawsuit months or even years later.
For situations that are difficult to re-create, there are 10 virtual-reality headsets for a gaming-style, 3D experience of 80 scenarios from Oxford Medical Simulation. With a handheld controller, students participate in the experience by selecting options from a drop-down menu. If it’s a patient visit, they assess the patient, conduct the clinical exam via the nurse avatar, select from a list of questions (the patient answers), order X-rays, read lab reports, and decide on treatment.
N U RSING 2023 | Volume 1 19
“You’re taking actions as if in a clinical setting, and the effect is weightier than just getting a question answered in class.” - Joshua Billings, recent graduate
The simulation experiences with the manikins and the virtual-reality headset transfer well to the clinical setting, Billings said. “Instead of being worried so much about what I learned step-by-step in class, I’ve done that already, and now I can focus on the patient.”
Billings added that the faculty “did a good job of making it intense enough to mimic but not so intense that it violated that feeling of safety.” The intensity paid off when he had to give CPR to a patient in the hospital. “I felt that I knew exactly what to do because they prepare you well for the high-pressure scenarios.”
The standardized patients also deliver a wide-ranging experience. Some scripts call for shy, confused, or belligerent patients; speakers of languages other than English; and those with a variety of ailments, which can involve wearing a fake bloody wound.
Marlena Gaby-Dater, coordinator of the University of Rochester Standardized Patient Program, said she is impressed with the faculty’s approach to learning.
“They don’t just say that the learner’s actions are wrong; they say, ‘These are the things to think about,’” she said. “It’s overall a very supportive environment. You can see that the student is encouraged.”
Gaby-Dater is appreciative of the school’s encouragement of empathy. “They are open to being yourself, and they ask learners what they will do to make patients feel comfortable.”
A FOCUS ON INNOVATION AND COLLABORATION
The School of Nursing’s status as an Apple Distinguished School for 2021–2024 makes it one of only five nursing schools across the country to earn the achievement, which recognizes schools that leverage technology to inspire students to learn and empower them to imagine new possibilities.

Earning the achievement means that technology and digital resources help develop new paths to learning, the faculty are proficient, and the school leadership is focused on continuous innovation.
New students are issued an iPad and immediately trained on its use. In addition to the many standard apps, the school loads several specialty apps that enable students to participate in myriad interactive and collaborative learning activities. There is Panopto for online quizzes, Notability for notetaking, Kahoot! for learning games, AhaSlides for creating presentations, Padlet for sharing information, and VoiceThread for online commenting.
20 N URSING 2023 | Volume 1
“With the iPad, we can combine didactic and lab and clinical. We’re bringing clinical to the student,” said Kaitlyn Burke, MS, RN, CCRN, CNEcl.



Everywhere you look in the school, there are 70-inch television screens equipped with Apple TV. And with AirDrop, sharing is easy. It takes only a tap on the iPad to show a presentation or an image to everyone in the room.
Sharing images comes in handy in the lab and when examining standardized patients. Instead of huddling around the person demonstrating a skill, the view can be shown on the TV so everyone can see and record for later playback.
“Technology can enhance learning,” Serwetnyk said. “It allows us to do less talking at them and more practicing. Students come to class with their pump primed and ready to apply what they’re learning.”
In the lab, students use the iPads to practice electronic documentation. And to coordinate with the day’s skills training, students use Padlet to anonymously share their perspectives on a case study, which facilitates class discussion by drawing in students who might be reluctant to speak up in class. Building competency is more efficient with the many interactive quizzes and other assessments on the iPad, Burke said. So is assessing competency with a tool that shows the number of times students practiced a skill and their level of independence.
The school’s preliminary results show that students in the collaborative flipped classroom are more satisfied with the experience and earn higher grades.
Jon Kuppinger, RN, EMT-P, a recent graduate of the RN to BS program, appreciates the fact that everything he needed for the program was loaded on his iPad. As a working nurse, he needed flexibility. “You could do it anytime; I could log on at three in the morning.”

Billings, who has moved to Salt Lake City, said that the constant practice with technology has given him confidence that he can quickly learn whatever technology is used at his new position.
Unlike the isolating role technology played in remote learning during the pandemic, the technology here serves as a unifying force, according to Kuppinger. “It made it a lot more personable. We were able to see each other’s videos and make comments. It keeps you engaged.”
He also found that receiving faculty comments on videos was similar to meeting individually with a professor during office hours and also more convenient.
Fierro, another recent graduate, said it boosted her confidence. “We’re not alone,” she said.
Collaboration is a key goal of the program, and the software makes it easy for students to work together to solve clinical problems. So does the arrangement of the tables, which are in groups rather than rows. Redefining nursing education to be more learner-centered means also redefining the role of faculty from lecturer to mentor.

“Nursing is a team sport,” Serwetnyk said. “That’s how you work in the hospital.”
THE FUTURE OF NURSING
Factors such as the COVID-19 pandemic and the resulting burnout rate, the nurse shortage, technology changes, and telehealth and other new modes of delivery all disrupted the standard model of nursing education and a nurse’s role in the changing health care environment.
Nurses stand at the intersection of these changes. They will likely be the ones to deliver in-home health care and advocate for health equity and, therefore, need to be aware of the social determinants of health—economic stability, access to quality education and health care, and social and community support.
To prepare nurses to address these emerging priorities, the School of Nursing conducts a poverty simulation that turns students into thespians as they role-play the life of a low-income patient. Sometimes the patient’s car breaks down and they can’t get to work. Sometimes they lose childcare or lose their job. Sometimes racism gets in the way. Ultimately, the patient is forced to choose between buying food or medicine and typically winds up at the pawn shop.
And with 40 million Americans and nearly half of the City of Rochester’s children living in poverty, the simulation is unflinchingly real.
As part of the focus on health equity, nurses need to be aware of health care obstacles so they can advocate for patients who need additional services. Students go into the community to do a windshield survey, in which they
22 N URSING 2023 | Volume 1
videotape and comment on the location and quality of grocery stores, condition of sidewalks, and proximity to transportation. For some students this is an eye-opening experience. It becomes clear that it is not enough to simply advise a patient to take medicine or to exercise or to eat healthy foods. Obstacles can make that advice difficult or even impossible to follow.
“Nurses need to advocate for patients and understand how social, cultural, and economic factors affect health. They need to assess the patient as a whole person,” Baylor said.
Advances in technology will continue to redefine a nurse’s role. And, as the role evolves, so too does the style and content of nursing education. The goal, according to Baylor, is to use “a student-centered approach with patient-centered outcomes.”

Transforming the curriculum at the School of Nursing better prepares nurses for the workforce and makes education more accessible by offering flexible pathways, such as the 16-month RN to BSN degree being online and an accelerated program offering second bachelor’s degrees in 12 or 24 months. Nine specialties are offered in the master’s programs.
It’s not enough to simply adopt technology; it’s also about constantly reinventing and retooling it to, as the saying goes around here, make it ever better.
Health care has been disrupted many times before. Florence Nightingale was a courageous innovator who officially created a new caregiving role—the nurse. In the following decades, however, the contribution of nurses was downplayed; they were referred to as the “physician’s handmaiden.”
A century later, the first dean of the School of Nursing, Loretta Ford, RN, EdD, disrupted health care on a monumental scale by creating another new role—the nurse practitioner. Ford’s views were prescient. She advocated for a healthy lifestyle, health equity, a holistic view of patients, and an expanded role for nurses to deliver quality health care to all communities.
“Nursing must address itself to the health issues of the day,” Ford said in her inaugural address in 1972. “It cannot remain in ivory towers, ignoring the political and social scenes which affect our educational endeavors of practice and our research … Together, we will create a new order of things at the University of Rochester School of Nursing.”
The new order she was creating in the 1960s and beyond wasn’t always welcomed by doctors and others in the
medical community. Nevertheless, she persisted. To Ford, there was no hierarchy in medicine. Just caregivers all.
Today, the School of Nursing embodies Ford’s notion of “a new order of things” as it disrupts the standard nursing education paradigm with one goal in mind: redefining the role of nurses to meet the health care challenges of the 21st century.
FIRST NURSING SCHOOL TO USE THE BUTTERFLY TOOL
The School of Nursing added a point-of-care ultrasound device to its curriculum that is designed to increase access to health care. In 2022, URMC became the first health care system in the world to supply the Butterfly to all its primary care providers, and the School of Nursing became the first nursing school to use the device, which provides information quickly to rule out certain conditions at the point of care. About the size of an electric shaver, the Butterfly connects to an iPhone or iPad, and images can be saved and transferred to another office for closer scrutiny.
Visit butterflynetwork.com to learn more about the technology.
N U RSING 2023 | Volume 1 23
A Decade of Inspiration and Impact
Patrick Hopkins, DNP, APRN, C-PNP, NNP, has been reflective since stepping down recently, after a decade as co-director of the University of Rochester School of Nursing’s Accelerated Program for Non-Nurses.

“It isn’t always an easy role—there have often been very difficult decisions to make, and that has been challenging,” he said. “But hearing how students go on to be successful spreading the philosophy we have here across the nation, and sometimes around the globe, has been inspirational for me. We can leave the world in a better place.”
Hopkins remains in his position as associate professor of clinical nursing, though now works part-time teaching pathopharmacology, and continues both to review applicants for the program and serve as a mentor and confidant.

As a former student and current colleague, Andrew Udkovich, MS, PPCNP-BC, has found Hopkins’ open-door policy to be like none other.
“Whether you have a problem with the curriculum or something stressful in your personal life, he encourages you to talk with him—and that’s rare, especially in an academic setting,” explained Udkovich, instructor of clinical nursing.
That door leads to a serene, dimly lit office, a place that has been playfully dubbed “dangerous” by students who find themselves opening up about both academic and personal challenges more than they expected to when entering.
“It’s about being grounded, and being present, and actually listening,” Hopkins said of his philosophy. “Teaching is all about building relationships.”
Hopkins equates that philosophy to being a parent. Instead of acting like a carpenter, in which he would measure everything twice to ensure precision, he is more like a gardener when it comes to nurturing students. “You throw out some seeds, water them, give them fertilizer to survive,” he said. “You don’t know which ones will thrive, but at the end you have a beautiful garden because they grow into who they need to be, not what you’re pushing them into.”
Some of that fertilizer comes in a shiny wrapper. Hopkins tells students on the first day of orientation that he always has Dove chocolates on hand if they need a snack break. (“And I say, ‘If I really like you, it will be Cadbury chocolate that I bring back from England.’”)
24 N URSING 2023 | Volume 1
Ma. Melita Hebert, RN, MSN, AGPCNP-C, attended the Accelerated Nursing Program in 2015 and often sought career advice from Hopkins.
FACULTY PROFILE
Patrick Hopkins Reflects on His Journey as Co-Director of the University of Rochester School of Nursing’s Accelerated Program for Non-Nurses
“Always soft-spoken, calm, and clear, he knows when to provide positive support when students are struggling,” she said. “He always makes things interesting with his anecdotes and dry sense of humor.”
The accent Hopkins brought from his hometown of Sheffield, a steel town in northern England, doesn’t hurt.
He noted: “People have said to me, ‘You could tell me to go to hell and I’d still say thank you.’”
Over the years, Hopkins has seen the biggest changes in nursing take place in the neonatal unit. With family centered, developmentally supportive care, premature newborns not only are surviving more often but thriving better than ever.
One thing that has remained the same is that the smallest of human interactions make nurses in all specialties invaluable. He said, “A kind word, a touch on the shoulder, a back rub can do more for a person who is suffering than some of the most expensive medications we have. We never know what effect we’re going to have on another human being by our presence.”
Now that Hopkins will be working fewer hours, he hopes to make it back to England more frequently, given that one of his two daughters, four younger brothers, and 13 nieces and nephews live there.

“This role has taken up a lot of my time,” he added. “I also need to paint the garage, get the hardwood floors redone, and do something with the garden.”
HABERYAN
TAKES ON ROLE
as Accelerated Program Co-Director


As new co-director of the School of Nursing’s Accelerated Program for Non-Nurses, April Haberyan, PhD, MS, RN, CNE plans to incorporate more gerontology into the curriculum.

She recently applied for a grant to do just that.
“I think there aren’t a lot of nurses who see gerontology as a viable option for them,” she said. ‘They’re drawn more toward pediatrics, intensive-care units, and emergency departments. But with the population aging, there’s such a need.”
In her post since March, alongside continuing co-director Louis Rosario-McCabe, DNP, RN, CNE, CNL, WHNP-BC, Haberyan’s breadth of experience includes being a recognized expert in disaster response. She hopes to create a comprehensive simulation exercise to train students on responding to mass casualties.
An award-winning educator, scholar, and nurse, Haberyan has extensive experience in behavioral and mental health and wellness, and she appreciates the field’s increasing attention on stemming workplace violence, particularly when it comes to verbal and physical abuse against nurses.
She plans to improve student outcomes by emphasizing emotional intelligence and active-learning strategies.
“This is very interesting and gratifying work,” Haberyan said. “I want our students to be excellent nurses, but also compassionate, kind, and well-qualified to care for patients wherever they work—not just in the hospital.”
From High School to Health Care:
East High Partnership Prepares the Next Generation of Nurses


Dressed in a white coat and standing in front of a colorful evidence-based research poster on heat stroke prevention in Evarts Lounge, Martha Beltran was just weeks away from graduating from East High School, as she presented the final project for her Pathways to Nursing course this past April. She would soon be moving on to her next chapter: attending Niagara University on a full scholarship to study nursing.
Beltran is among more than two dozen students who participated in the School of Nursing’s and East High School’s Career Exploration Internship program over the past year. The grant-funded initiative is one of several partnership programs developed between the high school and the University of Rochester, which became East’s educational partnership organization in 2015.
“This course has helped me get closer to my goal of becoming a nurse and gave me great exposure,” said Beltran, who also works at Strong Memorial Hospital as a patient care technician.
The career exploration program affirmed Beltran’s choice to pursue a career she had already been thinking about for most of her life. “I’ve always known I wanted to be a nurse since I was little. I even remember my mom getting me a doctor’s coat for kids and a toy stethoscope.”
Under the leadership of the Master’s of Nursing Education (MNE) program, the Pathways to Nursing course introduces students to the multitude of career paths within nursing, as well as local and national health care priorities, while seeking to promote diverse representation in the nursing workforce. It begins with an overview of local health care systems and introduces students to medical terminology, basic and emergency first aid, self and family care, and basic clinical skills. Students also explore critical public-health issues such as nutrition, immunizations, home safety, disease prevention, health promotion, and health care disparities, which several East students report first-hand experiences with.
The course was first launched in 2018 and paused during the pandemic. At the request of East’s faculty, the program returned in the Fall 2022. The New York State Regents credit-bearing class now offers students hands-on experience in the new, state-of-the-art skills lab, simulation suites, and other experiential learning spaces at the School’s newly opened expansion. Two full-day immersion field trips provide clinical skills demonstrations and simulations, tours of the University of Rochester Medical Center, and guest speakers from URMC’s Teen Health & Success Partnership Program.
Caitlyn Paris-Woods ’23N (MS) designed and taught the course as her MNE student teaching and capstone project, under the supervision of Maria Marconi, ’14W (EdD), RN, CNE, director of the MNE program. Paris-Woods called the opportunity to bring students to the School of Nursing’s new facilities a blessing.
Maria Marconi
“These students thrive when we provide hands-on experiences,” Paris-Woods said. “By starting our course with a tour of the new wing, students become instantly fascinated and inquisitive about the world of nursing.”

Program leaders hope that Pathways to Nursing can be part of the long-term solution to significant challenges in nursing and health care, such as the national nurse shortage, distrust in health care systems among marginalized communities, and the need for a more diverse nursing workforce. The 2020 National Nursing Workforce Survey reported that more than 80 percent of working registered nurses are white. East’s student population is more than half Black, and about one-third Hispanic or Latino.
“The University and the School of Nursing are committed to diversifying our workforce so that our caregivers look like the patient population we work with,” Marconi said. “One way to
26 N URSING 2023 | Volume 1
COMMUNITY PARTNERSHIPS
diversify our nursing workforce, and to provide a pipeline for future nursing educators, researchers and leaders, is to have evidence-based pipeline programs like this, where we engage with high school students and help them plan their careers.”
Outside of the nursing profession, there are wider community implications, too, Marconi said. By offering an inside look at how a hospital operates, the course ultimately prepares students to be better consumers and seeks to increase trust between health care systems and communities.
“Many of our students are the only English-speakers in their homes, and many of them serve as decision-makers and translators between their family members and health care institutions. When these students have more knowledge about health issues and health care resources, it helps their families significantly. Indirectly, it also helps us ensure a healthier community.”
For MNE graduate students, the program also ensures rich, community-based experiences in which they can work with diverse student populations and develop a wide range of teaching skills.
Stephanie Schechter ’23N (MS) joined Paris-Woods in the Pathways course as her semester-long student teaching capstone project to develop a mentorship program for East scholars, in partnership with the Rochester Black Nurses Association. Both of them plan to continue staying involved in the program after graduation.
The mentoring program aims to enhance students’ experiences in Pathways, both through informal, general mentoring, and through one-on-one connections with nurses working in the clinical areas students are most interested in. In a field that might not always reflect the student population she works with, Schechter also hopes that mentors can foster a stronger sense of belonging and guide students through the college application process and preparation for nursing school.
“There aren’t necessarily mentors out there who have gone through similar experiences or have similar backgrounds to our students,” Schechter said. “That’s the motivation behind this mentoring program. I’m hoping to give them a well-rounded amount of support.”
Shaun Nelms ’04W (MS), ’13W (EdD), the University’s new vice president for community partnerships and former superintendent of East, said Pathways to Nursing is one of the most successful career technical education partnerships at the high school, with a high rate of students going on to pursue health science jobs and college degrees.

“Partnering with the School of Nursing is allowing our students to see themselves contributing to the field of medicine,” Nelms
said. “They’re meeting professionals—particularly, professionals of color—and they are able to imagine being in those spaces because others before them are making an impact and leading in the field.”
The idea of improving representation in the nursing field drew recent East graduate Marcus Moore to the program in Fall 2022. Moore received several college acceptances and chose Benedict College in South Carolina.
“There are not a lot of Black men and Black staff in the nursing field. For me to actually be doing this as a Black teen in this program, it pushes me to be an example for other kids,” Moore said at the fall reception.
Paris-Woods has seen several of the students she instructed over the past year go on to pursue degrees at local nursing schools and secure jobs as patient care technicians and home health aides.
“The most rewarding part of this program is hearing the excitement from the students when they tell us that they have found success in health care, whether through a job or a college acceptance,” she said.
As the program prepares to welcome new East High scholars for Fall 2023, leaders on both ends of the partnership are enthusiastic about its continued growth.
“This project is an example of everything that we envisioned in 2015 when the UR-East partnership began,” Nelms said. “To see cohorts of students thriving with the guidance of professional nurses is a dream come true.”
East High School scholars visited the School of Nursing on April 19 for a full-day field trip, where they learned new clinical skills.
(Back row: Mo’Asia Ferrell, LeAsia Hill, Moises Perez, Martha Beltran, Elijah Delgado, Kaviyah Cole; Middle row: Jonathan Velazquez, Stephanie Ros-Suy, Malise Kong; Front row: Master’s of Nursing Education alumni Caitlyn Paris-Woods and Stephanie Schechter, Instructor of Clinical Nursing Andrew Udkovich)

N U RSING 2023 | Volume 1 27
Inclusive, High-Tech Learning
Sets UR Nursing’s Childbirth Class Apart

This story is part of a series called Cutting-Edge Courses, through which NURSING magazine takes readers inside the School of Nursing’s classrooms to highlight interesting, innovative courses that are making an impact.

Earlier this year, Nicole Goodnough ’23N was among the first nursing students to engage in a birth simulation with the School of Nursing’s new high-fidelity, maternal-care manikin. By the end of the summer, she will be practicing as a full-time labor and delivery nurse at Strong Memorial Hospital.
Two of the reasons she enjoyed her experience in the course were the faculty and the technology to which she and her classmates had access. She credits the school’s obstetrical nursing course for helping her achieve her dream job.
“It really is so incredible to be able to experience hands-on learning without the fear of making mistakes that will harm your patient,” Goodnough said. “We got to learn in the new simulation rooms, where it is safe to make those mistakes and learn from them.”
The course, titled “Nursing Care and Health Promotion for Childbearing Clients and Their Families,” is constantly evolving to address the needs of today’s patient population and to harness the school’s newest technology and expanded building.
The course has thrived under the direction of Instructor of Clinical Nursing Jennifer Truax, MS, RNC-OB, C-EFM, and Associate Professor Luis RosarioMcCabe, DNP, RN, CNE, CNL, WHNP-BC, who have taken the course to new heights.

Partnering with the School of Nursing’s Education Innovation Team (EdIT), Truax and Rosario-McCabe have sought to enhance the course experience in numerous ways through digital learning.
Before the course begins, pre-learning takes place on the eLearning tool Rise360. Truax has also made didactic learning more interactive by utilizing AhaSlides, a presentation software with features such as live polls, quizzes, real-time charts, and word clouds.
Modules on fetal assessment take place on iPads, with each element broken down to help students understand it at the granular level. It’s typically one of the most challenging concepts in the class, but with the right tools, Truax said her students have been able to assess a fetal monitoring strip within two hours.
28 N URSING 2023 | Volume 1
CUTTING-EDGE COURSES
Last semester, Truax transformed the third floor’s clinical-learning rooms into escape rooms, where students had to utilize their knowledge from the class to decode clues and unlock boxes as they helped a client.
“It’s the most fun I’ve ever had designing active learning for students,” Truax said.
Opportunities to practice in the school’s new skills lab and simulation suites, often with high-fidelity manikins, have also been course highlights. Last summer, the school introduced its first maternal care patient simulator, NOELLE®, which includes a mother and two babies, which enables practice in providing care before, during, and after delivery.
“Using the new building was incredible for simulation,” said Sarah Cox ’23N, who is starting a new role as a labor and delivery nurse at Strong Memorial Hospital in August. “During OB, we had the opportunity to catch a baby, and it was an exciting experience where we got to do something brand new in a safe and supportive environment.”
One of the course’s most unique assets is its increased inclusion of LGBTQ+ patient scenarios, through which students can prepare to work with same-sex couples, transgender men, or non-binary individuals who are having a baby.
“Not all female-bodied people identify as being women, so it’s important to ensure an inclusive women’s and gender-related health course,” Rosario-McCabe said. “That inclusivity is what is so cool about our course and the School of Nursing.”

The curriculum is reflective of experiences future nurses might have with patients. “Bringing what actually occurs in clinical practice into a simulation environment allows students to interact with the various clientele that they will see in real life,” Truax said.

These classroom experiences will ultimately help students have a better understanding of the needs and challenges of various populations they work with, while challenging them to reconsider their preconceived notions, according to the professors.
“One of the goals we have for all of our baccalaureate students is for them to be global nurses,” Rosario-McCabe said. “They can take what they learn here and change not only nursing, but health care. Our current generation of students is amped up to do that.”
A REASON TO Smile
The first time Melisande Ploutz ’13N (MS) took care of a patient with cleft palate, she was working as a registered nurse in Golisano Children’s Hospital’s (GCH) pediatric surgical suite and pursuing her master’s degree as a pediatric nurse practitioner at the University of Rochester. She realized quickly that cleft and craniofacial care was a specialty area she wanted to stay in.
A decade after joining GCH’s Cleft and Craniofacial Center as its nurse practitioner and team leader, Ploutz is now being recognized at a national level for her leadership and expertise. At the beginning of 2023, she started a three-year term as the only nurse on the American Cleft Palate-Craniofacial Association’s (ACPA) board of directors.

“This is a very big goal achieved for me,” said Ploutz, who had previously served as chair of the ACPA’s Care Coordination special interest group.
Ploutz has known since her first year as a nursing student at Case Western Reserve University that working with children was her dream. Originally from Geneva, New York, she returned to the region after college to work at GCH, first in the pediatric intensive care unit, and, later, the pediatric surgical suite.

Building relationships with patients and families affirmed Ploutz’s instinct to pursue a career in pediatric nursing. In her current role, she has a unique opportunity to be part of her patients’ lives both before they are born and throughout their childhoods. The first babies she treated as a nurse practitioner are now turning 10 and 11 years old.
“This is the type of specialty where the patients become family,” Ploutz said. “I meet moms and families when they’re expecting babies and get some abnormalities in the ultrasound. I provide that initial contact and reassurance that no matter what their child is born with, we are going to be able to take care of them, they are in great hands, and we know how to handle it.”
Children with cleft and craniofacial differences might see as many as nine specialists in a two-hour visit. Utilizing their combined expertise, the team comes together to confer on patients and create individualized treatment plans for each child they see. After earning her master’s degree from the University of Rochester, Ploutz said she gained the knowledge

ALUMNI PROFILE
Alumna Melisande Ploutz finds her niche as a national and local advocate in cleft and craniofacial care
and confidence to practice autonomously and to lead the interdisciplinary team of surgeons, dentists, psychologists, speech-language pathologists, and other specialists to provide the best care.
Throughout her career at GCH, Ploutz has been passionate about pursuing professional-development opportunities. She often encourages newer colleagues to work with their administrators and attending physicians to set aside administrative time for joining organizations, getting involved in special interest groups, going to conferences, and pursuing continuing-education opportunities.
Former Associate Dean of Education and Student Affairs
Pamela A. Herendeen ’09N (DNP), PNP-BC, a senior nurse practitioner at GCH, recognized Ploutz’s leadership skills and sense of curiosity early on in her graduate education.
“Mel is a strong patient and family advocate,” Herendeen said. “As a student, she was a curious, smart, and engaged learner who set high goals for herself.”
Ploutz’s eagerness to grow as a leader and continue her education has not only been beneficial to herself and her team, but to patients and families, too. In addition to her work with the ACPA, Ploutz completed a lactation counselor training course through the Healthy Children Project’s Center for Breastfeeding in 2021. A mother of two, she was interested in learning more about lactation support and sought to incorporate it into her clinical practice.
“Any baby with a medical problem can benefit from breast milk and breastfeeding. In my specialty area, it’s tricky, because many babies with facial anomalies might not be able to feed at the breast,” she explained.
She offers counseling on pumping for parents when a baby’s facial anomalies prevent them from breastfeeding and supports them in getting a breast pump, learning how to use it, and creating a schedule. She also supports parents’ transition to breastfeeding when babies are able to do so.
It’s an area of cleft and craniofacial care that is often overlooked, but Ploutz hopes to change that and aims to inspire other nurses to pursue the certification she received. At the ACPA’s annual conference in May, she spoke at a session for nurses with the presentation, “A Beginner’s Guide to Lactation Counseling: Educating and Empowering Families of Newborns with Clefts about the Benefits of Breast Milk.” Since she became a certified lactation counselor, Ploutz said she has seen an uptick in breast-milk
production and breastfeeding among families the GCH Cleft and Craniofacial Center sees.

Her leadership experience has empowered her to step out of her daily clinical setting and into the world to advocate for individuals with cleft and craniofacial differences. She currently travels around the region to present to fellow nurses, pediatrician’s offices, and elementary-school classes.

N U RSING 2023 | Volume 1 31
“I have the most fulfilling, amazing job in the world, and I’m very lucky. I love to educate, do community outreach, and advocate for our population, because they are special people.” - Melisande Ploutz
Now, It’s Part of Their Next Chapter.
From Neurovirology Researcher to WELLNESS ADVOCATE
Christina Mather ’17, ’18N found an interest in health care at the University of Rochester. She earned her first bachelor’s degree in microbiology and immunology at the School of Arts & Sciences, where she participated in neurovirology research studies but craved more personal connections in her daily work. Mather, who is from Rhode Island, knew the School of Nursing would be an excellent fit: “They welcomed diverse students like me from many different career paths in their program.”
The accelerated bachelor’s program helped Mather successfully start a career in the Neuromedicine ICU at Strong Memorial Hospital after graduation.

As an alumna, Mather found a supportive environment at the School of Nursing once again when she transitioned to a new role as a project nurse at the Center for Employee Wellness (CEW), and just recently, started to pursue her master’s degree in the Family Nurse Practitioner specialty.
Being part of the Employee Wellness team has helped Christina channel her love for preventive medicine.
A HAND TO HOLD in Tough Times
Stephen Romas ’20N came to URMC as a lung-biology researcher after earning his bachelor’s degree at Mercyhurst University.
Following a calling to make a difference at the bedside, he earned his second bachelor’s degree through the accelerated program in 2020, and became an MICU nurse at Strong. His experiences in the URMC community have affirmed his choice to pursue a new career in nursing.

“I love that nurses are the backbone and the heartbeat of the health-care industry in this and many other countries,” Romas said. “We are the advocates at the bedside for the patient and their families.”
Romas is now continuing his education as a graduate student in the Adult Gerontology Acute Care Nurse Practitioner program.
How did you know you wanted to become a nurse?
I worked in lung-biology research after my first undergraduate degree. I knew I wanted to pursue clinical medicine but was unsure which track I wanted to pursue. I shadowed doctors,
Why did you choose URMC to start your nursing career?
My lab instructor, Jenna Gonillo-Davis ’15N (MS), encouraged me to pursue a critical-care nursing career in Strong’s Neuromedicine ICU.
The Neuromedicine ICU welcomed me into my first nursing role and supported me through all the challenges that come with being a new bedside nurse. My preceptors, co-workers, and patients helped me foster strong critical thinking skills and inspired me to pursue a degree as an FNP in the future, hopefully specializing in neurological rehab.
Most importantly, URMC supported me after a severe car accident that shattered my right lower leg and left me physically unable to fulfill the role of a bedside ICU nurse. They provided me with both excellent medical care and job security and connected me to new career opportunities when it became clear I could no longer work in the ICU.
While grieving the loss of my identity as a bedside nurse, I wasn’t sure what jobs would be physically feasible for me to pursue. The CEW helped reignite my passion for nursing and has supported me as I advance my education.
physician assistants, nurse practitioners, and registered nurses, and fell in love with the RN role, with the idea that I would advance to become an NP.


What’s the most rewarding part of being a nurse?
I take pride in helping patients and families through some of the scariest and most emotionally fragile times in their lives and watching them build back up and move on from the ICU. Holding a patient’s hand during a procedure and providing comfort, education, and treatment to them in all other aspects is what I take pride in most.
What was the best part of your School of Nursing experience?
I enjoy feeling like I am prepared to do my job and that what I am learning has meaning. I often find that topics or case studies discussed in my NP classes show up the next day in my clinical practice as an RN. I am gaining a true broad perspective of acute care from the RN role and now the provider role on a daily basis.
32 N URSING 2023 | Volume 1
UR Nursing Helped These Alumni Change
Careers.
University of Rochester Reunion with Nursing Connections

Although their numbers have been diminished over the years for several reasons, the Theta Chi men of the U of R Class of 1957 met once again—this time to celebrate their 65th graduation anniversary. Over the years they have met a number of times, beginning with their first postgraduation gathering at their 50th reunion in 2007 in Rochester. This summer, from July 21 to 29, a limited group gathered on the MS American Melody of the American Cruise Lines for a Mark Twain–themed cruise up the Mississippi River beginning in St. Louis and ending in Minneapolis. Attendees included Bill Anderson ’53; Kay Stiles Anderson ’59N; Mark Sharnoff and his wife, Marcia Halio; “Mark Twain” (aka “Samuel L. Clemens,” aka Richard Garey); Roy Whitney ’73S (MBA); and Fay Wadsworth Whitney ’60, ’61N.
Claudina S. Ashelman ’77N was awarded the Community Service Award for Saratoga Hospital for 2021 for her service to the Saratoga Springs community over the last 25 years, while also recognizing her work providing nurse practitioners with numerous preceptorships and for coordinating meetings for her local chapter of The Nurse Practitioner Association New York State. Ashelman has worked as a family nurse practitioner at the Saratoga Hospital Community Center since its opening in 2013 and
retired in July 2021. She then went on to provide primary care in the Backstretch Clinic and is currently working with Saratoga County Mental Health in addiction medicine and with the Saratoga County Health Department in tuberculosis and STD clinics.
Ivy Braun ’90N; sends a photograph (above) from a mini reunion celebrating Michelle Saperstein Coppola’s birthday and “38 years of University of Rochester friendship, family, and fun.” From left: Shane Coppola ’88, ’89S (MBA); Jennifer Saperstein Kalapoutis ’94; Gary Worobow ’87, ’89S (MBA); Jill Tuchman Harris ’89; Michelle Saper-stein Coppola ’89; Tracy Frommer Duberman ’89; Ivy Braun; and Lisa Shaari ’87.
Dianne C. Morrison-Beedy ’93N, (PhD), the centennial professor of nursing and chief talent and global strategy officer at The Ohio State University’s nursing school, was recently honored by the Royal College of Surgeons in Ireland. She was conferred as a Fellow Ad Eundem for her contributions to nursing, healthcare, education, and research. Dianne also received the 2022 Global Intrapreneur of the Year Award in Education from the Global Intrapreneurs Institute in Australia for her creative approaches to expanding nursing education.
N U RSING 2023 | Volume 1 33
CLASS NOTES
TEA FOR LEE PROGRAM
More than 120 guests from all over the country celebrated Dr. Loretta C. Ford at the Florida Nursing History Project’s “Tea For Lee” program on May 7 at the University of Tampa. The nursing program at the University of Tampa presented Dr. Ford, pictured on the left, its first Honorary Clinical Professor of Nursing Award. Pictured (right) is Rotondo, DNP, RN, CNS, FANP, dean for education and student the school, and Marcia ’99 (MS), DNP. The University of Rochester School of Nursing was a platinum sponsor for the event, and Dr. Rotondo spoke about Dr. Ford’s impact on our school and the nursing profession. Dr. Ford received an honorary degree from the School of Nursing in 2000.


Robert Scott Davis ’95N was recently promoted to the position of president of Health Professional Services at Koniage Government Services. Koniag is an AlaskaNative-owned corporation that supports several federal agencies, including the Department of Health and Human Services, the Centers for Disease Control, and the Defense Health Agency. Davis will lead Koniag’s Health Professional Services product line in serving the increasing health-related needs of the federal government.
Cheryl Lustik ’00N, ’03N (MS), ’20N (DNP), who graduated as part of the inaugural cohort of Doctor of Nursing Practice Fellows in 2020, is now the director of advanced practice at the University of Rochester Medical Center’s Sovie Center for Advanced Practice. She supports professional development for more than 1,000 advanced practice providers through advancement models, fellowships, publications, and research.
Desiree’ M. Branson ’04N (BS), ’07N (MS), ’15N (DNP) began her term as president of the Nurse Practitioner Association New York State (NPA) in January 2023. Branson, who is currently a nurse practitioner in the University of Rochester Medical Center’s Center for Perioperative Medicine and an assistant professor at St. John Fisher University, hopes to inspire other nurse practitioners to get involved in professional organizations and pursue leadership roles.
Lauren N. O’Meal ’10N (MS) opened her own psychiatric practice in Pittsford, New York, serving adults through psychotherapy and medication management services.
Solutions Center at Massachusetts General Hospital. The first of its kind in the nation, this education program helps health care leaders develop strategies to eliminate racial and ethnic disparities. Wensley will represent the University of Rochester with Drs. Tina Sosa and Jeffrey Yaeger.
Kim Olfano ’18N is now a project nurse at UR Medicine Employee Wellness. after spending two years as a hyperbaric oxygen therapy nurse. Olfano, a native of Rochester, was the beneficiary of hyperbaric oxygen therapy herself after suffering a catastrophic car accident in 2009.
Farrell Cooke ’19N, currently an MBA student at the Simon Business School, writes that she and Tyler Viterise got engaged on campus last July. They are planning a fall 2024 wedding “surrounded by family and our fellow Yellowjackets.”
Kate Valcin ’20N (DNP) was inducted as a fellow in the American College of Critical Care Medicine ACCM on Sunday, Jan. 22, at the Critical Care Congress in San Francisco. Valcin is the director of adult critical-care nursing at Strong Memorial Hospital and has served as a preceptor for graduate students in UR Nursing’s Clinical Nurse Leader and Leadership in Health Care Systems programs.
34 N URSING 2023 | Volume 1
CLASS NOTES
KAITLEY WOZER ’18N Labor and Delivery Nurse
Oishei Children’s Hospital | Buffalo, New York University of Rochester School of Nursing McLouth Scholarship Recipient

A healing touch begins with you.
For Kaitley Wozer ’18N, scholarship support made all the difference. She graduated with greater financial freedom and an incredible education—a powerful combination that paved the way for her to begin her career with confidence. Since then, Kaitley has made a significant impact in the lives of countless patients.
For more about Kaitley’s story and how you can inspire the next generation of nurse leaders, visit: uofr.us/healingtouch

“
What I find the most rewarding in the field of nursing is no profound revelation; quite simply the greatest reward in this challenging profession is knowing you made someone’s day a little bit easier by caring for them.
DON’T STOP
the music

This photo from the University archives features two nursing students sitting at the piano in Evarts Lounge and singing, surrounded by five of their fellow students. Do you recognize these students or the date the photo was taken? Let us know your thoughts by commenting or messaging us on our Facebook page: www.facebook.com/ UofRSchoolofNursing.

We enlisted the help of Melissa Mead, archivist and librarian at the Department of Rare Books and Special Collections at the University of Rochester, to identify the nurses in this photo. She identified the nurse receiving flowers as Sylvera Maclava, from the Philippines, along with Dr. Marilyn Gray McClellan ’59W (MS), Lore Sander, and Maria Hartmann.

36 N URSING 2023 | Volume 1
FROM THE ARCHIVES
_
In MEMORIAM
Renowned nursing educator and leader Katherine S. Detherage, PhD, RN, a former UR Nursing faculty member, passed away April 13 at 83. Detherage was passionate about nursing education and helping students of African descent excel in the profession.

She was the first Black graduate of the University of Kentucky College of Nursing’s master’s program in 1974. After earning her PhD from Boston University in 1980, she started her postdoctoral career at the University of Rochester as a Robert Wood Johnson Fellow and later became part of the faculty.
1940s
Elsie (Hotchkin) Moon ’47N
Oct. 3, 2022, Lady Lake, FL
Jean (McKown) Jeschke ’48N
April 6, 2023, Salem, OR
1950s
Margery (Knight) Kibler ’50N
Feb. 14, 2023, Erie, PA
Alice (Armstrong)
McKernan ’53N
Feb. 27, 2023, Tuscon, AZ
After her time at UR Nursing, she went on to serve as the vice president of nursing practice at the Anthony Jordan Health Center for 10 years. Known among the local nursing community for her kind, gentle leadership, Detherage served as the first Black president of the Genesee Valley Nurses Association.
She also served on the boards of directors of the Catholic Family Center, the Rochester Health Commission, the McCree McCuller Wellness Center, St. Joseph’s Neighborhood Center, the Regional Review Council of Finger Lakes Health Systems Agency, and the Finger Lakes Donor Recovery Network.
As an educator, Detherage was also chair of the nursing departments at St. John Fisher University and at Nazareth College, where she served with distinction until she retired.

Carol (Joustra) Kinzly ’54N
Nov. 30, 2022, Getzville, NY
Betty J. Sullivan ’56N
Dec. 24, 2022, Wilkes-Barre, PA
Marcia (Collins) Hayes ’56N
Jan. 26, 2023, Avon, NY
Elizabeth (Agan) Horn ’58N
Jan. 12, 2023, Washington, DC
1970s
Elizabeth Wywialowski
’74N (MS)
Jan. 2, 2023, Oregon, WI
Mary J. Kniep-Hardy
’75N (MS)
Feb. 7, 2023, Rochester, NY
1990s
Jeannette (Rosenthal)
King ’96N (MS)
April 10, 2023, Marion, MA
2000s
Mindie (Melinda) Maggio ’05
May 18, 2023, Webster, NY
N U RSING 2023 | Volume 1 37
Word has reached us of the passing of the following alumni and faculty. The School of Nursing expresses its sympathy to their loved ones.
Katherine S. Detherage, PhD, RN (1939–2023)
Calling all UR Nursing Alumni:




Did you receive a promotion? Move to a new city? Publish your research findings? We want to hear from you! Submit your news and we will share it with your classmates and the UR Nursing community in the next NURSING Magazine. Fill out the alumni class notes form online or mail to: Name Class Year (include maiden name, if applicable) Address City State, Zip














38 N URSING 2023 | Volume 1
NEWS
I’ve not submitted before.
publish
news in N URSING magazine and share
University publications. TODAY’S DATE: ____/____/ 20_____
SHARE YOUR NEWS & UPDATES School of Nursing Office of Advancement and Alumni Relations Larry & Cindy Bloch Alumni & Advancement Center P.O. Box 278996 | Rochester, NY 14627-8996
Email Phone ( ) - Cell Phone ( )Occupation Employer Family information (Spouse, children names) HERE IS MY
This is new information which
Please
my
with other

N U RSING 2023 | Volume 1 39 #WilmotWarrior Giving 100% to conquer cancer. Register | Form a team | Sponsor warriorweekend.urmc.edu September 30, 2023 Inaugural Breakaway Ride October 1, 2023 Warrior Walk and 5K Maddy Falletti Uterine Cancer Survivor WARRIOR WEEKEND WILMOT WARRIOR WEEKEND leaving cancer in the dust
601 Elmwood Avenue, Box 643
Rochester, New York 14642
Change Service Requested
your SWING SWING

provided on-site medical services during the PGA Championship at Oak Hill Country Club.

The PGA Championship brought together two generations of the UR Nursing community: current students Sarah Wolf and Grace Smith met two alumni who graduated 50 years before them: Joan Ferrara ‘73N, and Lynne Hall Blanchard ‘73N.

Non-Profit U.S. Postage PAID Permit No. 780 Rochester,
NY







 Lisa Kitko, PhD, RN, FAHA, FAAN
Lisa Kitko, PhD, RN, FAHA, FAAN
 Dean, School of Nursing Vice President, University of Rochester Medical Center Professor of Nursing
Dean, School of Nursing Vice President, University of Rochester Medical Center Professor of Nursing