NE UR OSCIENCE
 University
University
of
Rochester | Ernest J. Del Monte
Institute for Neuroscience Vol. 15 - 2022
A serendipitous discovery and the choreographed dance of fragile X research
PG 4
John J. Foxe, Ph.D.

FROM THE DIRECTOR’S DESK
Fall is a bittersweet time of the year. As nature heads into its big winter sleep, the days shorten, and the promise of the winter freeze hangs in the air. The paradox though, is that it is precisely this time of the year that sees our labs fill up again with the vibrancy of new students, new ideas, new hopes, and aspirations. Those cold dark days will yield rich datasets, new findings and insights, and hopefully great progress as we tackle the wicked problems of neuroscience.
Our cover story profiles a dynamic multidisciplinary team of scientists, including a molecular biologist, neurotologist, geneticist, neuroscientist, and vision scientist who are taking on the complexity of fragile X syndrome. Fragile X is the most common known cause of inherited intellectual and developmental disabilities, including autism. Their research is pivotal to understanding this disorder and its response to targeted therapy.
We are delighted to introduce Dr. Emily Knight, our most recent Neuroscience faculty recruit. Emily excelled at the Medical Center as a fellow and is now an assistant professor of Neuroscience and Pediatrics.
The student spotlight shines on a fourthyear graduate student, MaKenna Cealie, who works in the Majewska Lab. She was recently awarded a highly competitive F31 grant from the National Institutes of Health for her work that takes a cellular approach
to understanding fetal alcohol spectrum disorders.
The impact of the work of our Neuroscience Diversity Commission continues to have major effect on our community. This summer, 11 students completed the second year of the NEUROCITY program. This partnership with City College of New York has resulted in students co-authoring papers and others enrolling in doctoral programs at the University of Rochester. Recently, the Commission launched the new postdoctoral speaking series, NEURO YES, designed to elevate and highlight early career investigators. Words cannot convey my pride and gratitude to all those who have developed, implemented, and now run these programs to create a pathway for historically marginalized groups.
I look forward to seeing many in our Neuroscience community at the Society for Neuroscience Conference in San Diego in November. I hope you are able to join us for one night as we host a social event to spark collaborations, reunite old friends, and celebrate the success of our alumni and colleagues.
On the cover
From left: Christoph Pröschel, Ph.D., Michael Telias, Ph.D., Hitomi Sakano, M.D., Ph.D., Tatsuaki Kurosaki, Ph.D., and Lynne Maquat, Ph.D.
Photo: John Schlia Photography
Del Monte Institute for Neuroscience Executive Committee
John Foxe, Ph.D., Chair, Department of Neuroscience Bradford Berk M.D., Ph.D., Professor of Medicine, Cardiology

Robert Dirksen, Ph.D., Chair, Department of Pharmacology & Physiology
Diane Dalecki, Ph.D., Chair, Department of Biomedical Engineering
Jennifer Harvey, M.D., Chair, Department of Imaging Sciences
Robert Holloway, M.D., M.P.H., Chair, Department of Neurology
Paige Lawrence, Ph.D., Chair, Department of Environmental Medicine
Hochang (Ben) Lee, M.D., Chair, Department of Psychiatry
Shawn Newlands, M.D., Ph.D., M.B.A., Chair, Department of Otolaryngology
Webster Pilcher, M.D., Ph.D., Chair, Department of Neurosurgery
Steven Silverstein, Ph.D., Professor, Department of Psychiatry
Duje Tadin, Ph.D., Chair, Department of Brain & Cognitive Sciences
NEUROSCIENCE
Editor/Writer
Kelsie Smith Hayduk
Kelsie_Smith-Hayduk@ urmc.rochester.edu
Contributors
Mark Michaud
Bethany Bushen
Feature Photography
John Schlia Photography
Designer Beth Carr
In Science, John J. Foxe, Ph.D.
Kilian J. and Caroline F. Schmitt Chair in Neuroscience
Director, Ernest J. Del Monte Institute for Neuroscience
Professor & Chair, Department of Neuroscience
UNIVERSITY OF ROCHESTER | ERNEST J. DEL MONTE INSTITUTE FOR NEUROSCIENCE
New grant will unlock workings of brain’s waste removal system
With an eye toward developing new therapies for diseases like Alzheimer’s - a new $15 million grant from the National Institutes of Health (NIH) will bring together several teams of researchers to accelerate our understanding of the complex mechanics that control the glymphatic system – the brain’s waste removal system. The new research program will be led by Maiken Nedergaard, M.D., D.M.Sc., co-director of the Center for Translational Neuromedicine. Nedergaard’s lab discovered the glymphatic system and subsequent research has transformed a range of how neurological disorders and critical brain functions are studied.
The program seeks to develop a detailed, mechanistic understanding how cerebrospinal fluid (CSF) moves across sleep and wakefulness and the neural processes that control it. It will also seek to deepen our understanding of how the system specifically functions in the human brain. The research teams will include a range of scientists and engineers from the University of Rochester, Penn State University, Boston University, and the University of Copenhagen. The research is being funded through The BRAIN Initiative, a massive research program supported by NIH and several other federal research agencies that aim to fill gaps in our current knowledge of the brain’s organization and function.
 NEWS BRIEFS
NEWS BRIEFS
NE UR OSCIENCE | VOL. 15 | 2022 1
BRIEFS
Brain’s support cells may hold key to new Huntington’s treatments

A new study in the journal Cell Reports suggests Huntington’s disease may also flow from defects in glia, important support cells found in the brain. The research expands our understanding of the underlying mechanisms of the disease and reinforces the potential of therapies that target glia cells.
Huntington’s disease – a hereditary and fatal genetic disorder –has long been considered a neuronal disease due to the permanent loss of medium spiny motor neurons, the death of which over time is responsible for the clinical hallmarks of the disease: involuntary movements, problems with coordination, cognitive decline, depression, and psychosis.
Years of research in the lab of University of Rochester Medical Center (URMC) neurologist Steve Goldman, M.D., Ph.D., have shown that the two populations of glia found in the brain – astrocytes and oligodendrocytes – are dysfunctional in Huntington’s disease. These may trigger much of the neuronal pathology seen in the disease.
Goldman is co-director of the URMC Center for Translational Neuromedicine and senior author of the new study. Glia cells play a critical role in maintaining the health of neurons and facilitating the chemical signaling between nerve cells. In Huntington’s, glia are unable to perform these functions, leading to a breakdown in communication between neurons and, over time, cell death.
At-home sensors can spot Parkinson’s disease
A new study shows a device that passively monitors breathing during sleep can not only detect Parkinson’s but also track the progression of the disease over time. The researchers used an artificial intelligence tool to sift through mountains of data from study participants to find patterns that identify the disease and determine its severity.

“We have a very limited insight into how Parkinson’s disease impacts people’s daily lives,” said Ray Dorsey, M.D., professor of Neurology and co-author of the study. “This study shows that remote monitoring has the potential to identify individuals with Parkinson’s and create an objective measure of severity and progression. This could be a powerful tool to detect the disease early and conduct research more efficiently.”
The research, published in Nature Medicine, was led by Dina Katabi, Ph.D., professor of Electrical Engineering and Computer Science at MIT. Katabi worked closely with researchers at the URMC Center for Health + Technology (CHeT), including Dorsey and Chris Tarolli, M.D., assistant professor of Neurology. This study is one of several projects supported by CHeT exploring new ways to harness remote monitoring, smartphones, smartwatches, and other technologies to improve care and advance research in Parkinson’s and other diseases. The study also included researchers from the Mayo Clinic, Massachusetts General Hospital, and Boston University.
2 UNIVERSITY OF ROCHESTER | ERNEST J. DEL MONTE INSTITUTE FOR NEUROSCIENCE NEWS
Mild traumatic brain injury increases risk of behavioral and emotional problems in kids

University of Rochester researchers have been at the forefront of efforts to understand how blows to the head impact the brain, including how concussions change brain structure. Now researchers have found that kids who experience a traumatic brain injury (TBI), even a mild one, have more emotional and behavioral problems than kids who do not.
The study published in NeuroImage and led by Neuroscience associate professor Ed Freedman, Ph.D., used MRI and behavioral data collected from thousands of children who participated in the Adolescence Brain Cognitive Development (ABCD) Study. They revealed children with a mild TBI experienced a 15 percent increased risk of an emotional or behavioral problem. This risk was the highest in children around ten years old of developing. Researchers found that children who had a significant hit to the head but did not meet diagnostic criteria for a mild TBI also had an increased risk of these behavioral and emotional problems. URMC is one of 21 research sites collecting data for the National Institutes of Health ABCD Study.
Dr. Seuss prose shines a light on how the brain processes speech

Researchers have expanded the understanding of how the brain engages during complex audiovisual speech perception. The study in NeuroImage describes how listening and watching a narrator tell a story activates an extensive network of brain regions involved in sensory processing, multisensory integration, and cognitive functions associated with comprehension of the story content. Understanding the involvement of this larger network gives researchers new ways to investigate neurodevelopmental disorders.
The research, led by John Foxe, Ph.D., Neuroscience department chair, used fMRI to examine the brain activity
of 53 participants as they watched a video recording of a speaker reading “The Lorax.” They found that along with the previously identified sites of multisensory integration, viewing the speaker’s facial movements also enhanced brain activity in the broader semantic network and extralinguistic regions not usually associated with multisensory integration, such as the amygdala and primary visual cortex. Researchers also found activity in thalamic brain regions, which are known to be very early locations at which sensory information from our eyes and ears interact. Researchers designed this experiment with children in mind, according to the investigators who have already begun working with children and adults on the autism spectrum, in an effort to gain insight into how their ability to process audiovisual speech develops over time.
There is a concern in the scientific community that COVID infection may accelerate cognitive decline in older adults, resulting in a wave of dementia cases as the population ages. Several reports have highlighted the presence of cognitive and psychiatric symptoms associated with COVID infection, particularly in older adults who experienced moderate to severe infection. Other studies suggest that the COVID virus can damage the endothelial cells that line blood vessels through both direct infection and immune response. A new $3.7 million grant from the National Institutes of Aging will allow researchers to more precisely understand how the virus triggers damage in the brain and the long-term impact on cognitive performance. The research will be led by URMC neurologist Giovanni Schifitto, M.D., and a multidisciplinary team of URMC neurologists, infectious disease experts, radiologists, and computer scientists, including Nasir Uddin, Ph.D., Meera Singh, Ph.D., Miriam Weber, Ph.D., Henry Wang, M.D., Ph.D., Hongmei Yang, Ph.D., and Angela Branche, M.D.
The study will recruit 300 volunteers 65 and older who were hospitalized by a severe COVID infection, excluding individuals who required intensive care and had to be on a ventilator. Researchers will follow participants for two years with neurocognitive evaluations and advanced quantitative neuroimaging that will search for changes in white matter, blood flow, the integrity of blood vessels, and blood biomarkers of inflammation and brain injury.
NE UR OSCIENCE | VOL. 15 | 2022 3
New study will explore COVID’s potential link to dementia
A serendipitous discovery and the choreographed dance of fragile X research
The choreography of development is a delicate dance. Beginning in utero, chromosomes, DNA, genes and RNA twirl, tap, and sashay their way in a precise pattern. A misstep or a missing step that changes the routine causes body and brain functions to go awry – as is the case with many intellectual and developmental disabilities (IDD).
Fragile X syndrome is the most common known single-gene cause of inherited IDDs, including autism. Scientists know the misstep in this syndrome is in the gene FMR1. FMR1 is responsible for making the protein FMRP, which is necessary for typical brain development.
Lynne Maquat, Ph.D., founding director of the Center for RNA Biology at the University of Rochester,

and professor of Biochemistry & Biophysics, Oncology and Pediatrics, did not set out to study fragile X. It was through another line of research – her seminal discovery of and decades’ worth of work on nonsense-mediated mRNA decay (NMD) – that fragile X syndrome entered her radar. NMD is a cellular quality-control mechanism that plays a role in both healthy and disease states, and her lab discovered that it is overactive in people with fragile X.
“It was complete serendipity,” Maquat said. “No one ever thought to look at NMD and fragile X. So now we’re trying to figure out what happens at the molecular level when FMRP is absent; we want to understand the network of altered gene expression by identifying mis-regulated messenger RNAs (mRNAs).”
4 UNIVERSITY OF ROCHESTER | ERNEST J. DEL MONTE INSTITUTE FOR NEUROSCIENCE
FEATURE
From left: Christoph Pröschel, Ph.D., Michael Telias, Ph.D., Lynne Maquat, Ph.D., Hitomi Sakano, M.D., Ph.D., and Tatsuaki Kurosaki, Ph.D.
Into the brain
Associate professor of Biomedical Genetics Christoph Pröschel, Ph.D., has spent much of his career interested in neurogenetic diseases that primarily affect the white matter of the brain, which carries signals throughout the organ. His lab started working with induced pluripotent stem cells (iPSCs) to understand different neural cell types, providing a solid foundation for their IDD research. “My lab and the Maquat lab have a mutual interest in the molecular mechanism of fragile X,” said Pröschel. “It is key to finding any kind of hope for a future therapy.”
The Pröschel lab makes and differentiates neural stem cells that mimic fragile X syndrome, allowing his team to test hypotheses and understand how different therapies impact cell biology and function. He and Tatsuaki Kurosaki, Ph.D., research assistant professor in the Maquat lab, used these neural stem cells to understand the relationship between FMRP and NMD. They discovered that NMD controls the amounts of messenger RNAs deriving from a wide range of genes throughout the brain, including genes that govern motor control and cognitive processes related to attention, learning, and language. They also found that when FMRP is absent from cells, as it is in people with fragile X syndrome, NMD shifts into overdrive.

This work was part of a 2021 study published in Nature Cell Biology led by Maquat that revealed that tamping down NMD with small molecule inhibitors restored a large proportion of neurological functions in these cells.
Most recently, Pröschel co-authored research published in Molecular Cell led by Maquat and co-authored by Hana Cho, Ph.D., and Elizabeth Abshire, Ph.D., of her lab The study highlighted a complex molecular dance between NMD and the enzyme AKT, which plays a key role in cell growth and survival. Both AKT and NMD are overactive in fragile X. Using neural stem cells that lack the FMRP protein, they tested a drug called Afuresertib, which inhibits AKT. They discovered that blocking AKT in the fragile X cells decreased its activity and decreased NMD. These cells then acted more like typical, non-disease cells.

One of the most prominent surveillance systems in the body that protects against mistakes in gene expression that lead to disease, NMD is a complex pathway that is at the heart of many of the collaborations between Maquat and other University of Rochester scientists. Together, with funding from the National Institutes of Health (NIH) and the FRAXA Research Foundation, they aim to gain a deeper understanding of the sophisticated mechanisms related to NMD that will contribute to developing new drug therapies for genetic disorders such as fragile X syndrome, cystic fibrosis, and hundreds of others.
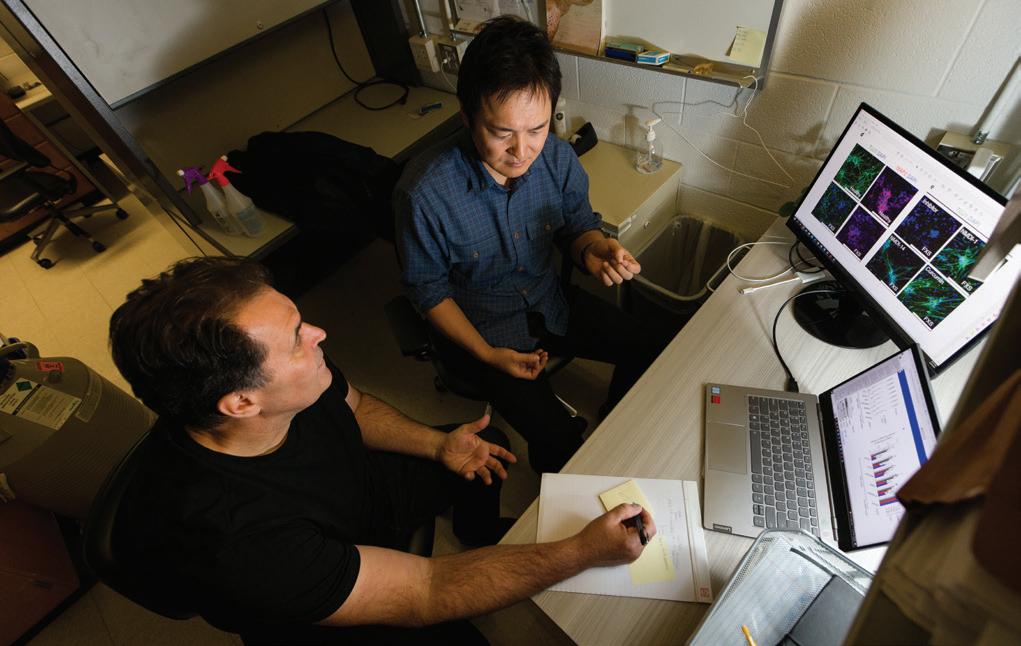
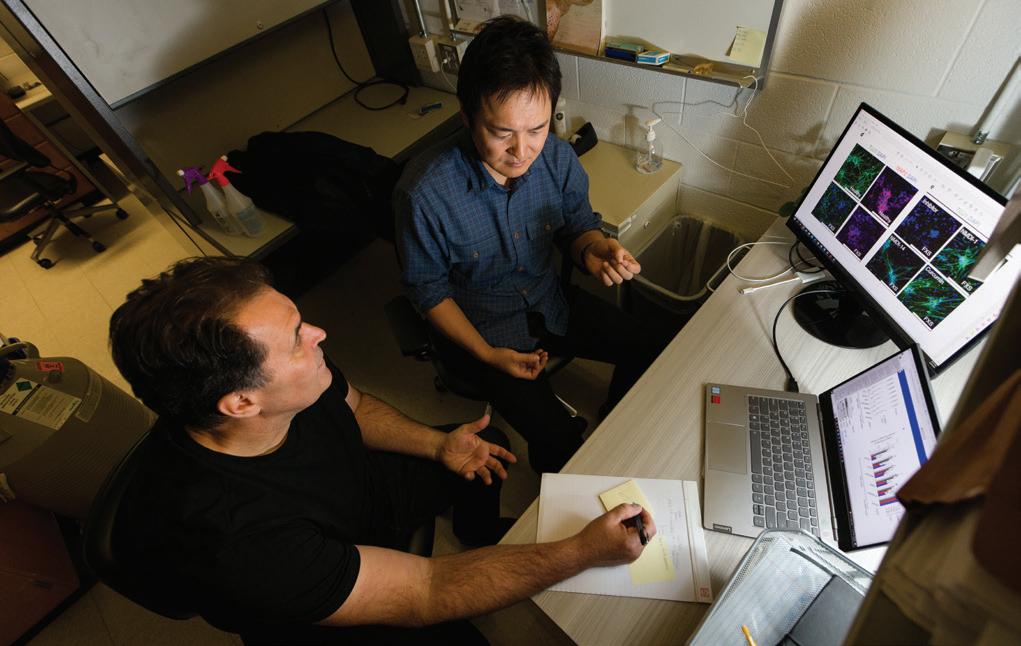
From left: Kurosaki and Maquat.
NE UR OSCIENCE | VOL. 15 | 2022 5
"It is the key to finding any kind of future hope for a therapy."
There is still a lot the team doesn’t know about how AKT and NMD interact, because they both influence and regulate multiple activities in cells, but this work provides good direction that could inform the development of future treatments for fragile X syndrome.


“This has been one of the real fun chapters of my career –working with this group,” said Pröschel. “Everyone brings such a different perspective to the project.”
From surgery to the lab
As a neurotologist (subspecialist of Otolaryngology), Hitomi Sakano, M.D., Ph.D., spends time in the clinic with patients with hearing issues or hearing loss. In the lab, she aims to understand how the brain adapts to sound information.

Her work with fragile X syndrome began as a resident at the University of Washington when she took interest in FMRP, which is highly expressed in the auditory brainstem nuclei of a typical brain and is the same protein missing in fragile X patients. When Sakano came to the Medical Center in 2018, she brought the fragile X mouse model to study this and joined the Center for RNA Biology.
“I also use the [knockout] mouse model to study hyperacusis – extreme sensitivity to sound,” said Sakano. “We know that fragile X patients have sensory and auditory sensitivity, so this model is a great tool to study both.” Hyperacusis is also very common in the general population (some report up to 15 percent) so understanding the mechanism could potentially impact our broader community.
Sakano hypothesizes that FMRP regulates genes that enable neuroplasticity to maintain normal processing of auditory information. If true, there may be therapeutic targets for symptoms like auditory hypersensitivity in fragile X. Funding from the Schmitt Program in Integrative Neuroscience (SPIN) through the Del Monte Institute for Neuroscience Pilot Program and a NIH Research Career Development Award for clinician-scientists are supporting her research, which involves investigating the gene expression abnormalities in the auditory brainstem of the fragile X mouse model that might explain the auditory hypersensitivity in these mice. To date, she has found some interesting RNAs that encode synaptic proteins. These findings open up the possibility of targeting these genes for the treatment of hyperacusis.
She co-authored a study with the Maquat and Pröschel labs in Genome Biology. The research used the mouse model whose FMR1 gene is knocked-out. These findings build upon Maquat’s previous research that showed NMD hyperactivation in neuronally induced stem cells from fragile X patients. This hyperactivity negatively impacts many neuronal mRNAs important to brain development. The Genome Biology paper
6 UNIVERSITY OF ROCHESTER | ERNEST J. DEL MONTE INSTITUTE FOR NEUROSCIENCE
From left: Sakano and Maquat.
From left: Pröschel and Kurosaki.
Immunofluorescence microscopy of normal or induced pluripotent stem cell (iPSC) – derived fragile X syndrome neurons, which were established in the Maquat and Pröschel labs.
showed NMD goes into overdrive in the brain during early development in a mouse with fragile X. These researchers are now testing various therapeutics to inhibit NMD.

“Being able to collaborate to gain meaningful results to move this science forward is the value of being at an academic medical center like Rochester,” said Sakano. “These steps are what will ultimately lead to treatments and therapies that I use in the clinic someday to help my patients.”
On the horizon
Forthcoming research aims to broaden the scope of the fragile X work at the Medical Center. One of the world’s largest clinics for fragile X is in Israel, where an estimated 80 percent of women are screened for the inherited disease. Michael Telias, Ph.D., assistant professor of Ophthalmology, Neuroscience, and Center for Visual Science, began studying fragile X as a graduate student in Israel. He uses human embryonic stem cells that carry the mutation for fragile X to look inside neurons at the molecular and cellular levels to shed light on the human-specific mechanisms affected by this syndrome.
“Human neurons have shown us that these cells have a problem receiving information and communicating information to the next cell,” said Telias. “We cannot do this work in humans, so using human cells enables us to know what to target in the cell. That is the only way we will be able to develop treatments that work.”
In the Frederick J. and Marion A. Schindler Cognitive Neurophysiology Laboratory, research assistant professor Tufikameni Brima, Ph.D., is aiming to use electroencephalography (EEG) and event-related potentials (ERP) to better understand how the brains of patients with fragile X respond to various stimuli. This work has the potential to build upon the ongoing molecular research being conducted by Telias and others.
“Ultimately, what we are figuring out is what happens when FMRP is absent. We don’t know the whole story,” Maquat said. “However, FMRP is an RNA-binding protein, and in work soon to be published in Molecular Cell, Kurosaki and I have now defined those messenger RNAs that are normally bound by FMRP and how the absence of FMRP binding results in those mRNAs making too much protein. These results have allowed us to identify which genes are affected and how. Our work will pave the way for better therapeutics for those living with fragile X.”
UR designatedIntellectual and Developmental Disabilities Research Center
In 2020, the National Institute of Child Health and Human Development (NICHD) designated the University of Rochester as an Intellectual and Developmental Disabilities Research Center. This recognition acknowledged the Medical Center’s national leadership in research for conditions such as autism, Batten disease, Rett syndrome, and most recently fragile X syndrome. The Center’s researchers, including Maquat, Pröschel, Sakano, Telias, and Brima, work to translate scientific insights into new ways to diagnose and treat these conditions.

NE UR OSCIENCE | VOL. 15 | 2022 7
From left: Pröschel and Telias.
From left: Pröschel, Maquat, and Telias.
Emily Knight, M.D., Ph.D.

Q&A with Emily Knight
Emily Knight, M.D., Ph.D., is an assistant professor of Neuroscience and Pediatrics at the University of Rochester Medical Center. She received her B.S. in neuroscience at Bucknell University and completed her M.D./Ph.D. training at Mayo Clinic in Rochester, Minnesota. She went on to New York Presbyterian Weill Cornell campus for her general pediatrics residency. In 2018, she came to URMC as a fellow in Developmental Behavioral Pediatrics with a combined postdoctoral research fellowship in Neuroscience. Her research aims to understand neural mechanisms of sensory perception in individuals on the autism spectrum.
Can you summarize your research?
Using tools like electrophysiology (EEG) and neuroimaging, while incorporating some newer technologies like virtual reality we’re interested in identifying specific autism-related differences in the neural processing of visual, auditory, and other types of sensory stimuli in the brain. What is especially important to me is that we are looking at these questions through a translational lens. We are trying to understand how these mechanistic differences in sensory processing relate to real-world development and experiences for people on the autism spectrum. As we are building that knowledge base, we can then use it to help us refine diagnostic and intervention strategies that would be more directly linked to the underlying mechanisms and that would actually transform how we approach autism. That’s the future goal.
How did you become interested in this field?
I have always been interested in the brain. I think we can all probably relate to the experience of being tricked by a visual illusion, and mis-hearing lyrics or what someone said in a noisy party environment. It is those types of experiences that have always led me to wonder what is happening in the brain as it takes in the world around us. I became focused on autism during my undergraduate career. I was studying Neuroscience and was working as a summer teacher aid for students on the autism spectrum. It was very fun and rewarding, and it was also immediately clear to me that these students were processing and responding to things in the environment in a way that seemed different than their neurotypical peers in the classroom. When I delved into the neuroscience literature for an explanation, I realized there was a need for more research in this area, and that I could potentially contribute to that.
Why is it important to do research along with clinical work?
It is important to me to have a foot in both domains because I think it offers me a unique perspective. The studies that I have in the lab are directly inspired by observations in the clinic and questions that either the individuals on the autism spectrum or their families may ask. I can then bring them back to the lab and start to systematically dissect them using some of our neuroscience technology. Frequently, I have conversations with families where I will say, here’s what we know currently about the brain, but we are actively working on answering this question to develop new knowledge.
What led you to the University of Rochester?
I was drawn to the institutional tradition and commitment to advancing science in order to improve the health and lives of children in the community. That’s a challenging mission, and I am not alone at URMC. On a personal note, I grew up in the Rochester area so I’m able to give back to the community I was raised in, and that’s a big part of why I trained here and I am staying on as faculty.
Favorite piece of advice.
I take my inspiration from the children I see in the clinic, because children across the developmental spectrum are inherently curious, and not burdened by traditional expectations or viewpoints. Those are the same qualities you need to do good science. They have taught me that it is okay to challenge the status quo and that you need to maintain that sense of curiosity and wonder so that you can keep asking questions like, “why?” and “what if?” That’s how we can keep pushing boundaries forward.
FACULTY
PROFILE
8 UNIVERSITY OF ROCHESTER | ERNEST J. DEL MONTE INSTITUTE FOR NEUROSCIENCE
Knight finds brains of children with autism may not always ‘see’ body language
Noticing and understanding what it means when a person leans into a conversation or takes a step back and crosses their arms is a vital part of human communication. Researchers have found that children with autism spectrum disorder may not always process body movements effectively, especially if they are distracted by something else.
“Being able to read and respond to someone’s body language is important in our daily interactions with others,” said Emily Knight, M.D., Ph.D., assistant professor of Neuroscience and Pediatrics, who is the first author of the study recently published in Molecular Autism. “Our findings suggest that when children with autism are distracted by something else, their brains process the movements of another person differently than their peers.”
Using an electroencephalogram (EEG), researchers recorded the brain waves of children with and without autism as they watched videos of moving dots that were arranged to look like a person. In these videos, the dots moved to represent actions such as running, kicking, or jumping, and at times were turned in different directions or jumbled to no longer move like a person. The six to 16 years old were asked to focus on the color of the dots or to focus on whether the dots moved like a person. Researchers found the brainwaves of children with autism did not process when the dots moved like a person if they were focused on the dot color.

MaKenna Cealie is a fourth year in the Neuroscience Graduate Program at the University of Rochester School of Medicine and Dentistry (SMD). Cealie graduated from Colgate University with a B.A. in Neuroscience and a minor in Anthropology.
Cealie is currently working in the lab of Ania Majewska, Ph.D., where her research takes a cellular approach to understanding the affected mechanisms of fetal alcohol spectrum disorders (FASD).
The National Institute on Alcohol Abuse and Alcoholism (NIAAA) recently awarded Cealie an F31 for her project titled “Effects of Developmental Ethanol Exposure on Cerebellar Microglia and Purkinje Cells.” This work will use two-photon, in vivo imaging to examine microglia dynamics and their interactions with Purkinje cells after developmental ethanol exposure.

“This work is moving to the cerebellum, which is a relatively understudied area affected by FASD,” Cealie said. “I thought that would be a great place to look using a model I’m familiar with from my previous study published in 2021. A big difference is we’re increasing the period of alcohol exposure, which more accurately models human FASD.”
Cealie co-authored a paper in Journal of Neuroscience Research that suggests that two of the brain’s support cell types – astrocytes and microglia – may be particularly sensitive to alcohol. She and her co-workers found these cell types rapidly undergo subtle changes in response to a single exposure to alcohol early in brain development.
Science has fascinated Cealie since a young age. “I have
always enjoyed learning new things. There is still so much to discover about the brain. That is what drew me to neuroscience, a field I have been interested in since high school, and the research I was able to do in undergrad solidified that I wanted to pursue graduate school.”
Cealie also holds various leadership roles outside the lab, which include treasurer of the Graduate Student Society (GSS) at SMD, and a graduate community assistant in graduate housing.
NE UR OSCIENCE | VOL. 15 | 2022 9
MaKenna Cealie
STUDENT SPOTLIGHT








University of Rochester Medical Center 601 Elmwood Avenue, Box 603 Rochester, New York 14642 Visit us online: delmonte.urmc.edu Follow us on Twitter @URNeuroscience Scan to receive the Neuroscience Newsletter giveto.urmc.edu/delmonte Sunday, November 13th ● 6:30 pm 8:30 pm Sally’s Fish House & Bar ● 1 Market Place Manchester Grand Hya� ● San Diego You’re invited! Sunday, November 13th ● 6:30 pm 8:30 pm Sally’s Fish House & Bar ● 1 Market Place Manchester Grand Hya� ● San Diego University of Rochester Neuroscience Graduate Program Social at S N 3rd Annual Join University of Rochester Neuroscience faculty, alumni, and students for an evening of networking and celebra�on. Everyone interested in learning more about the Program or Ins�tute is welcome to a�end. For more informa�on, please contact victoria_dagos�no@urmc.rochester.edu Sponsored by Please join us as we honor our 2022 NGP Alumni Award recipient SfN NS Social invite sized 4 nwltr 101222.pdf 1 10/12/2022 10:21:00 AM
 University
University



 NEWS BRIEFS
NEWS BRIEFS