

MAKING A DIFFERENCE

Making a Difference for Children and Families
A Children’s Hospital Without Walls
The University of Vermont Children’s Hospital and Department of Pediatrics consists of six academic hospital sites and five primary care locations in Vermont and northern New York, a Children’s Specialty Care Center with more than 20 pediatric subspecialties, and inpatient services including general pediatric and nursery care, pediatric intensive care, and neonatal intensive care. Our vision is to provide a children’s hospital and pediatrics department that extends beyond our hospital walls into the communities we serve, drawing upon the inclusive talents of our faculty, staff, learners, patients and their families to provide high-quality, child-friendly, familycentered health care.
LARNER COLLEGE OF MEDICINE DEPARTMENT OF PEDIATRICS
THE UNIVERSITY OF VERMONT CHILDREN’S HOSPITAL
Our Strategic Priorities
CLINICAL CARE
Provide expert consultation, diagnosis, and treatment for the unique health issues facing babies, children, and young adults.
QUALITY & SAFETY
Constantly strive to improve patient safety and care quality and engineer solutions across the network.
RESEARCH
Continually pursue better ways to treat children’s health issues and facilitate the translation of research from the laboratory to the bedside and to the community.
EDUCATION
Provide educational opportunities for faculty, staff, pediatric residents, medical students and other learners across all sites, along with opportunities for educational leadership.
CULTURE & BELONGING
Recognize and value a compassionate and collaborative work environment that promotes inclusiveness and cultural humility of our faculty, staff, and trainees, in safe environments free from bias and discrimination.
ADVOCACY & LEGISLATION
Advocate for children through partnerships with local and national organizations and commit to initiatives that allow children and their families to thrive.
PHILANTHROPY

Engage community members throughout the region in the spirit of service and generosity to support the work of the UVM Children’s Hospital that translates into meaningful support for patients and their families.
Letter from the Chair

It gives me great pleasure to introduce this year’s annual report for the Department of Pediatrics at the Robert Larner, M.D. College of Medicine and the University of Vermont Children’s Hospital (UVMCH).
Because there is such breadth and depth in all that we have accomplished over the past year, I hope you will enjoy the new format of this report that showcases our work in the areas of Clinical Care, Research, Education, Quality and Safety, Culture and Belonging, Philanthropy, and Advocacy in ways that are making a difference in the lives of all children in the communities we serve. There is plenty to share in terms of quantitative as well as qualitative accomplishments and we found ourselves this year with enough highlights to more than fill the pages of this year’s report.
Our department continues to grow with now over 100 physicians and advanced practice professionals who are part of our network department and many more in other departments (e.g., pediatric surgery, neurology, anesthesia, emergency medicine). I hope you will join me in expressing appreciation and gratitude for the work that they do but also extend that appreciation to our phenomenal teams of nurses, staff, trainees, administrators and our patient and family advisors for the outstanding and ongoing commitment they have made to making us the high-quality child-friendly familycentered network department and children’s hospital that we are today and will continue to be as we look to the future. Special thanks once again goes to Sue Victory, who, though retired (or so she tells me), has continued to give of her time to special projects including her editorial work on this year’s annual report. I’d also like to take the time to recognize the remarkable work of the Larner Medical Communications team who helped us reimagine this report.
The start of 2025 represents my 31st year as a department chair and children’s hospital chief and the 75th anniversary of our founding as a department in 1950 by Dr. R. James McKay. Initially Dr. McKay was the lone faculty member in the department. Today, I hope he would be proud to see how far we have come in three quarters of a century— and how far I know we will continue to go as we look to the future.
As you read this year’s annual report, you’ll see just what I mean!

Lewis R. First, M.D. Professor and Chair, Department of Pediatrics, UVM Larner College of Medicine Chief of Pediatrics, UVM Children’s Hospital

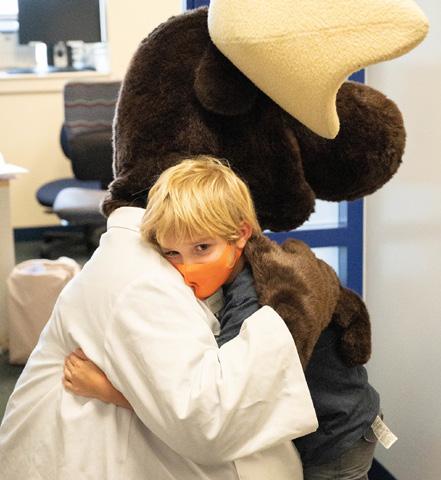
On the cover: Dr. Lauren Iacono demonstrates that Jackson, a patient, is now officially taller than she is!
Meet our mascot, Monty the Moose. Throughout the region, Monty has brightened children’s lives since 2002.

The University of Vermont Children’s Hospital 2024 Annual Report is produced by the UVM Larner College of Medicine Office of Medical Communications.
Contributors: Janet Essman Franz, John Turner, Susan Victory
Photography: Andy Duback, Ceilidh Kehoe, David Seaver, UVM Health Network Design: Ann Howard | © 2025
Major Milestones in FY2024
ENGAGED WITH 31,000
Patient visits to the Children’s Specialty Center and more than 3,750 specialty telehealth visits.
PROVIDED 28,000
Well child visits
CARED FOR 19,000+
Patients in primary care offices
That’s approximately 5,000 visits per month across all locations and via telehealth services.
PROVIDED 5,000+
Pediatric Emergency Department visits
COMPLETED
2,000
Transthoracic and fetal echocardiograms
The UVM Children’s Hospital supports the only nationally accredited pediatric echocardiograph lab in Vermont and upstate New York.

The UVM Pediatric Fitness Club launched in 2024 with the support of a Children’s Miracle Network grant. Led by Danielle Burstein, M.D., assistant professor of cardiology, the PFC provides a structured exercise program and cardiopulmonary testing for children with special health care needs.

PROVIDED 2,850+ Primary care telehealth visits
Full-time complex care social worker Leah Pence, M.S.W., joined our faculty to provide care for families with children who require complex care. For these families, the anxiety, grief, and uncertainties can feel overwhelming, especially when pediatric patients who receive care from three or more specialists and require interventions like oxygen or an alternative way of receiving nutrition.


Pediatric Critical Care has achieved 4 years without a documented central line acquired blood stream infection and 7 years without a catheter-acquired urinary tract infection
Pediatric Cystic Fibrosis Center attained the highest composite lung function and nutritional metrics in the U.S.
KidsSafe Collaborative Award for Outstanding Collaboration
UVM Children’s Hospital Child Safe Program
The Child Safe Program, our division specializing in the diagnosis and prevention of child abuse and neglect, was the recipient of the 2024 KidSafe Collaborative award for Outstanding Collaboration. KidSafe Collaborative is a collaboration of 30+ programs and community organizations dedicated to the prevention of child abuse and neglect in our region. This award celebrates the collaborative efforts of our Child Safe Program. Our program is staffed by a board-certified child abuse physician, nurse practitioner, pediatric forensic nurse and social worker who work in partnership with families and communities in Vermont and northern New York to assess, treat, and prevent the physical, behavioral and emotional impacts of child maltreatment.
Press Ganey Human Experience Guardians of Excellence Award
Neonatal Intensive Care Unit
This national recognition places the UVM Children’s Hospital among the top 5% of health care providers nationwide for patient experience, underscoring their unwavering commitment to clinical excellence and empathetic patient care.
Honors and Awards
Newsweek America’s Best Maternity Hospitals 2024 “A” Grade on the 2024 March of Dimes Report Card
UVM Children’s Hospital Inpatient Labor and Delivery Unit
This ranking recognizes the highest-quality health care and patient experience. It illuminates the remarkable impact of high-quality patient care, including topics such as cleanliness, perinatal care, and communication about medication.
Perinatal services at UVM Children’s Hospital earned an “A”, making Vermont the only state to achieve that grade in 2024, setting a new benchmark for maternal and infant health across the United States.

American Diabetes Association Education Recognition Program Endorsement
The UVM Children’s Hospital Pediatric Diabetes Clinic
This endorsement recognizes the delivery of outstanding diabetes self-management education and support services.


Making a Difference in Clinical Care

The University of Vermont Children’s Hospital includes six network hospital sites and five outpatient pediatrics primary care sites across Vermont and northern New York, and a Children’s Specialty Center in Burlington. Our pediatricians are backed by teams of specialists found only at an academic medical center. Our workflows include screening patient families for social determinants of health and providing social support when needed.


Primary Care Services
Comprehensive health care for all infants, children and adolescents
Routine health supervision and physical
School, camp and sports physicals
Immunizations


• Mental health services and referrals
• Dental screening and referrals
• Acute illness care
• On-site laboratory services

236 children vaccinated with the new RSV vaccine
Improved
autism assessment, diagnosis, and follow-up in collaboration with the Vermont Child Health Improvement Program

School-based health clinics reduce health disparities.
The Winooski (Vermont) School District clinic saw more than 300 students and administered 190 flu shots to children


Specialty
Care Highlights
Diabetes Care
Developmental Behavioral
Hematology and Oncology


Neurosurgery Urology

We successfully treated the first patient in Vermont with teplizumab, the only therapy approved in the U.S. for delaying the onset of clinical type 1 diabetes in individuals with preclinical disease.
Our faculty participates in the Barton Center diabetes summer camp, that provides diabetic children the opportunity to attend camp and learn to manage their diabetes.
Gastroenterology
We are only one of a handful of children’s hospitals in North America to offer point of care ultrasound for diagnosing inflammatory bowel disease.
We also implemented a new non-pharmaceutical treatment approach to children with inflammatory bowel diseases.
Child Safe Program
• An advanced nurse practitioner and a social worker were added to our Child Safe Team, thanks to new funding from the Vermont Department for Children and Families
• Child safe programs expanded, thanks to funding from the Department for Children and Families
Otolaryngology and Pulmonology
Our new multidisciplinary sleep clinic with pediatric pulmonology/sleep medicine and otolaryngology provides services for children with complicated obstructive sleep apnea.


Pediatric Advanced Care
• Subspecialty palliative and hospice medicine services
• Interprofessional approach that meets families where they are
• Longitudinal outpatient follow-up through in-person visits, telehealth, and home visits
Emergency Medicine Highlights
• New, dedicated pediatric waiting area
• 5 specialized treatment rooms
• Dedicated pediatric nursing staff
• 5 pediatric emergency specialists
Inpatient Pediatrics
Our inpatient pediatrics units in Vermont and northern New York provide high quality care for infants, children, and adolescents, with emphasis on patient- and family-centered care.
Neonatal Intensive Care

• 29-bed NICU in Burlington, Vermont, serves a wide catchment area that includes Vermont and northern New York.
• In 2024, our providers and nurses cared for more than 480 critically ill or premature infants.
Pediatric Intensive Care
• Multi-bed unit provides highly specialized critical care for children with life-threatening illnesses or injuries.
• More than 50% of children sequenced had diagnostic genetic results that impacted their care.
Pediatric Sedation Comfort Zone
• We develop individualized plans with methods including distracting technology, mindfulness, and calming medications to make children feel as comfortable as possible.
Child Life focuses on hospitalized children’s psychological and social health.

Five pediatric critical care intensivists provide round-the-clock care for children with life-threatening illness or injuries.
Integrative Therapies
• Massage Therapy available 4 hours a week for patients and families
• Music Therapy available 10 hours a week
• Therapy dogs
• Art from the Heart



Making a Difference in Quality & Safety
The University of Vermont Children’s Hospital is committed to providing patients and their families with the safest, highest-quality care every day and during every patient encounter across the network. We do this through clinical, research, educational, and advocacy activities that make an equitable and inclusive difference.
• A dedicated quality and safety team meet weekly to review reports regarding patient safety and engineer solutions across the hospital network.
• Representatives from pediatric inpatient, outpatient, specialty care, emergency care, family medicine, and family advisors gather regularly to share concerns and ideas.
• We standardize care delivery across the network to ensure patients receive equitable care, and that our care teams have needed resources.
• All quality metrics are evaluated holistically to ensure equity for all patient populations.

Through VCHIP, the University of Vermont Children’s Hospital collaborates closely with our clinical, public health, policy, community, family, and academic partners to strengthen and improve the quality of health care for children and their families. VCHIP works across the age spectrum, settings, and areas affecting child and family well-being.
2024 VCHIP Highlights
Engaged medical homes serving more than 70% of children in Vermont:
• birthing hospitals
• emergency medical services
• school nurses and school health liaisons
Supported implementation of the Vermont Psychiatry Access Program:
• provides real-time peer-to-peer consultation services to primary care providers seeking support in caring for their patients’ mental health
• conducted consults on over 1,000 psychiatry cases from more than 200 providers. A quarter of these calls had a suicidality component
Vermont Child Health Improvement Program (VCHIP)
60%
Decrease in minutes for completing admission intake for infants born at less than 32 weeks, from 200 to 80 minutes
40 Coaches trained from 10 departments in the expanded Safety Coach Program +60% Lipid screening of pediatric cardiology patients

Social worker Leah Pence, M.S.W. (below, right) supports parents and families whose children with medical complexities require use of our children’s hospital.

UVMCH Quality and Safety team members (left to right)
Stanley Weinburger, M.D., Kathy Browne, LICSW, Keith Robinson, M.D., and Caroline Hesko, M.D., M.P.H.
Patient Family Advisory Council
Patients and their families have valuable wisdom gained from their health care experiences that can help us make improvements to how we deliver health care.
• Patient and family advisors bring the patient and family voice and perspective to all aspects of planning and decision making.
• Patient and family advisors participate with our team on committees and workgroups designed to improve patient care, including educating and training hospital staff and providers.
• Phlebotomy experience has improved for patients and families, thanks to a Patient Family Advisory Council quality improvement project.

Each month, representatives from pediatric inpatient, outpatient, specialty care, emergency care, family medicine, and family advisors gather to share concerns and ideas.
“We look at processes and health outcomes centrally with site leaders from all the health care partners to improve pediatric outcomes across the network.”
– Keith Robinson, M.D., associate professor of pediatrics and vice chair of quality improvement and population health at UVM Children’s Hospital

Making a Difference in Research

Jessica Heath, M.D., associate professor and vice chair of research for the Department of Pediatrics, investigates high-risk pediatric leukemia. She examines how certain genetic mutations in some of these leukemias can cause chemotherapy resistance, with an aim to discover new ways to treat these leukemias.
As a university hospital, we foster an integrated research environment where no boundaries exist between science and medicine. Patients benefit from the knowledge that comes from an active research program where physicians, scientists, academic colleagues and community partners work together to translate ideas and scientific breakthroughs into new diagnostics, medicines, and treatments. These discoveries give young patients access to the most advanced pediatric health care.
+18% Increase in grant funding over the past year +12% Increase in scholarly publications across all divisions
65 Clinical trials in progress

As part of her research, Leslie Young, M.D., neonatologist at the UVM Children’s Hospital and associate professor of pediatrics at the UVM Larner College of Medicine, assesses care approaches for newborns exposed to opioids in the womb. This research benefits infants and families in our region, and across the nation.



A virtual parent-peer mentorship pilot study aims to reduce distress and improve perinatal outcomes in pregnant persons receiving a new prenatal diagnosis of congenital heart disease. The study is a collaboration between researchers in the Department of Pediatrics and the Department

We participate in a national multisite quality improvement initiative through the national Children’s Oncology Group to increase clinical trial opportunities for adolescents and young adults with cancer. These trials include front-line treatment for many types of childhood cancers, studies aimed at determining the underlying biology of these diseases, and trials involving new and emerging treatments, supportive care, and survivorship.
Pulmonology
Research funded by the National Institutes of Health Researching COVID to Enhance Recovery (NIH RECOVER) aims to learn about the long-term health effects of COVID and inform ways to diagnose and treat long COVID.
Emergency Medicine
Rigorous research efforts focus on topics including children with medical complexity, childhood firearm injuries, and emergency medical services for children. In 2024, pediatric emergency medicine physicians published 13 studies in peer-reviewed publications and secured multiple federal research grants.
Rheumatology

Research on a wide variety of rheumatic diseases affecting children includes medication trials, patient registries, and collaborations with national partners to advance effective treatments for rheumatic and inflammatory disorders. Pediatric patients receive treatments and therapies based on the latest research and developments in the field.


Jerold and Ingela Lucey
Early Career Investigator Prize
The annual Jerold and Ingela Lucey Early Career Investigator Prize for Innovations in Infant or Child Health inspires and encourages those early in their pediatric medicine careers to pursue their innovative ideas.

The following awardees and their respective projects received the 2024 Lucey Prize:
• John Cullen, graduate student, accelerated master’s degree program “The Impact of the CALM-AF10 Fusion Protein on Wnt Signaling in Leukemia”
• Benjamin Kim, M.D., pediatric resident “Elevating Marginalized Youth Voices into Medical Education”
• Adrienne Pahl, M.D., assistant professor of pediatrics, neonatal-perinatal medicine “Maternal Social Deprivation Index and Characteristics, Care, and Outcomes of Maternal-Infant Dyads in the ESC-NOW Randomized Controlled Trial”
• Anisha Rimal, M.D., assistant professor of pediatrics, hospital medicine “Interprofessional Mentorship to Promote a Sense of Belonging for BIPOC Medical and Nursing Students”

Jerold Lucey, M.D.
Making a Difference in Education

Medical student Varsha
listens to a patient’s heart during a Doctoring In Vermont learning session.
Pudi ’27
Medical student education is an essential mission of the Department of Pediatrics and one that we relish. Our goal is to ensure that all students at The Robert Larner, M.D. College of Medicine understand children and their families, including the importance of community and culture in health and illness. Faculty across the network participate in all aspects of the Vermont Integrated Curriculum and serve as mentors or advisors to students interested in pediatrics.
2024 Highlights

100%
10% of Vermont’s 14 hospitals and 13 EMS districts personnel received pediatric emergency preparedness training through the Division of Pediatric Emergency Medicine.
30
media appearances and educational programs offered by members of the Division of Child Psychiatry. These have reached from local Vermont newspapers to media outlets in Brazil.
episodes of First With Kids for radio, television, and print media. Since 1995, Dr. Lewis First has produced more than 1,450 of these segments designed to educate the community on ways to improve the health and wellbeing of children. of Larner medical graduates matched into pediatrics.
52
Curricular Innovations
• Residents and Students as Teachers course
• Expanded community pediatric practice opportunities for students
• Resident mental-behavioral health curriculum
• Global health curriculum
• Fourth year longitudinal pediatric concentration, culminating in a two-week bootcamp experience prior to graduation
• Mobile pediatric difficult airway simulation boxes created by Pediatric Otolaryngology team are used for provider education at locations throughout the UVM Health Network.

Education Insights
American Academy of Pediatrics Honors
Leah Burke, M.D., FAAP, professor emerita of pediatrics, received the David Smith Award for Excellence in Genetics and Birth Defects Education.
Ann Guillot, M.D., professor emerita of pediatrics, received the AAP Lifetime Achievement Award for Outstanding Teaching, Clinical Care, and Advocacy in Pediatric Nephrology.


Pediatric faculty teach medical students in foundations and longitudinal courses.
Three pediatrics faculty selected to become preclinical course directors.

Olubunmi Salako, M.D., assistant professor, Pediatrics, demonstrates infant care in the Clinical Simulation Lab

at
Patient
play while visiting Alice Hyde Medical Center, Malone, NY.
Making a Difference in Culture & Belonging

Hillary Anderson, M.D., assistant professor, Pediatrics, teaches a class at the Understanding Pathways to Pediatrics program.
We believe our workforce is strengthened by individuals with a broad range of experiences and backgrounds. When varied perspectives are represented, we are better equipped to serve all children and families and to advance health outcomes.
To support this commitment, we are developing programs that not only help individuals from different walks of life pursue medical school but also provide early exposure to the field of medicine.
Highlights
Health Equity Rounds
A pediatric hospitalist and child psychologist established triannual Health Equity Rounds bringing together members of our community with our children’s hospital team of providers, staff, and trainees.
Understanding Pathways to Pediatrics
The Understanding Pathways to Pediatrics program (UPP) is a one-day program designed for undergraduate students who are thinking about a career in the field. Through hands-on and interactive activities throughout the day participants get a glimpse into the world of what it really means to be a pediatrician. The program engaged 23 UVM Larner College of Medicine medical students and 46 undergraduate students from regional institutions over the last 3 years.
Student Scholarship Rotation
A new visiting student scholarship rotation was started for fourth-year students committed to improving health care delivery to underserved areas and populations—and two students were welcomed into our first cohort.
“I loved the program. I didn’t consider medicine as something I could get into but now it seems like a possibility.” – UPP participant
“I learned the importance of gaining trust from both patients and parents. Being kind, considerate, and empathetic towards families can calm everyone’s nerves and offer a better experience for everyone involved.” – PATH participant
Pathways in Pediatric Education
The Pathways in Pediatric Education (PATH) is a year-long preceptorship designed to provide undergraduate students who are considering careers in medicine, with shadowing and mentorship opportunities within the department. This may include time in clinic, the inpatient hospital floor, procedural areas, laboratory or research meetings. There were 22 pediatric faculty preceptors in 2023-24, and all students who completed the program reported increased interest in pediatrics as a career.
Making a Difference in Advocacy & Legislation

Larner medical students
Olivia Domingue ’25, Stefanie Kelsey ’25, Kassondra Little ’25, Mikaela Mari ’26, and McLaine Rich ’25, and pediatrics resident Julie Ehrlich, M.D., joined Associate Professor of Pediatrics
Rebecca Bell, M.D., at the recent national American Academy of Pediatrics (AAP) Advocacy Conference in Washington, D.C., where they met with Rep. Becca Balint (D-VT).
Effective advocacy helps position the Children’s Hospital for success, by informing lawmakers about ongoing and future critical health issues. These efforts help influence policies and legislation that promote public health, such as tobacco prevention, safe drinking water, and nutrition labeling laws and can bring resources to help address them. Advocacy efforts can also empower communities by providing them with the knowledge and resources needed to make informed health decisions. This is especially important for vulnerable populations, who may struggle to access or understand healthcare information, get the care and resources they need.
Highlights
• Faculty and trainees provided expert testimony on firearm injury and violence prevention measures before the Vermont Legislature.
• Children’s Hospital pediatricians held important leadership roles in the American Academy of Pediatrics councils and committees this past year, including Chair of the Council on Community Pediatrics and Chair of the National Nominating Committee.
• Rebecca Bell, M.D., associate professor of pediatrics, served this past year as President of the Vermont Medical Society.
• Paul Zimakas, M.D., associate professor of pediatrics, is the endocrine consultant for the Vermont Department of Health Newborn Screening Advisory Committee, helping develop and expand guidelines for screening of newborn disorders.

Dr. Heidi Schumacher, assistant professor of pediatrics and member of VCHIP gave a plenary talk on Addressing Barriers to School Attendance at the AAP National Conference and Exhibition in Orlando, FL.
More than 500 pinwheels were planted in front of the hospital for April Child Abuse Awareness Month

• Faculty and trainees met with congressional representatives in Washington D.C. regarding pending legislation aimed at improving child mental health care in Vermont.
• More patient voices from across the state were added to health system efforts via the Vermont Child Health Improvement Program (VCHIP) outreach.
• Children’s Hospital faculty were elected to serve on executive committees in the American Academy of Pediatrics including the Section on Pulmonary and Sleep Medicine, the Council on Child Abuse and Neglect and were appointed to serve on the Committee on Pediatric Emergency Medicine.

An Extraordinary Year of Support
Making a Difference in Philanthropy
Countless grateful parents, local businesses and community members shared their appreciation for our care and expressed their gratitude by making a gift to support the work of the UVM Children’s Hospital. These acts of kindness and generosity generate a ripple effect and enable accessible, affordable, sustainable and highquality health care for kids and families in our region to live their best lives. Donations support identified areas of greatest need including new initiatives, innovative programs and critically needed equipment.

Big Change Round Up for Kids
$353,484.41 Raised
Of note, this included the largest donation in history for the Big Change Roundup for Kids of $113,973.15 from Maplefields. The top 3 fundraising participants were Stacey Ingalls, The Woods Family, and the Gravel Family.

Key sponsors:
• EastRise Credit Union
• Med Associates
• Walmart Ticonderoga
• Maplefields
Children’s Miracle Network Hospitals
National Partners
$395,541 Raised
Top fundraising partners: Walmart/Sam’s Club, Costco, Log a Load for Kids, Kinney Drugs, Rite Aid Foundation, Ace Hardware, Child’s Play, Shaws Foundation
Outside of CMN Hospitals Corporate Partners:
• Dunkin’ Joy in Childhood Foundation $14,000
• Spirit of Children $33,783

Rallython
$106,532.19 Raised
• 535 participants registered Extra Life Gaming Marathon
$48,600.46 Raised
• 157 gamers registered Golf Classic

Third Party Fundraising, Events, and In-Kind Donations
$35,312 Raised
for pediatric initiatives from more than 25 different events, promotions and donors
Donations Supported
• Child abuse advanced training for social workers and nurse practitioners
• Establishing a standard pediatric legacy and bereavement package
• Reach Out and Read: a national literacy project
$165,858 Raised
• 192 golfers • 48 teams • 23 sponsors
Key sponsors:
• Farrington Construction
• Vermont Mechanical
• EchoStor Technologies


20 grants were awarded in 2024, totaling $901,499.16 dedicated to improving the lives of pediatric patients and their families. Initiatives, services and programs supported include:
• Baby Steps: implementation of family centered neuro-protective care in the NICU
• Dedicated inpatient and outpatient pediatric psychology
• Complex care social worker and associated program
• Infant safe sleep swaddle sack
• Pediatric research support fund
• Kids Fest
• Specialized training and support for the pediatric advanced (palliative) care team and bereavement coordinator
• Child Life Services programs
• Child protection team
• Developmental screening and resource connection in primary care facilities
PEOPLE WHO MAKE A DIFFERENCE
Faculty
UVM Health Network
Medical Group
Clinicians
Adolescent Medicine
Erica Gibson, M.D.
Anesthesiology
Kevin Abnet, M.D.
Ann Lawrence, D.O.
Robin Leopold, M.D.
Monika Modlinski, M.D.
Jennifer Soares, M.D.
Emily Stebbins, M.D.
Brian Waldschmidt, M.D.
Cardiology
Danielle Burstein, M.D.
Jonathan Flyer, M.D.
Caitlin Haxel, M.D.
Joshua Price, M.D.
Child Abuse
James Metz, M.D.
Beth Paquin, NP
Child Development
Elizabeth Forbes, M.D.
Child Psychiatry
Yasmin Abdul-Karim, M.D.
Robert Althoff, M.D., Ph.D.
Alexis Bailey, M.D.
Jeremiah Dickerson, M.D.
James Edwards, M.D.
Sarah Guth, M.D.
Michael Hernandez, M.D.
Michael Hoffnung, D.O.
Peter Jackson, M.D.
Nathaniel Kouns, M.D.
Haley McGowan, D.O.
Sara Pawlowski, M.D.
Andrew Rosenfeld, M.D.
Steven Schlozman, M.D.
Dhruv Shah, D.O.
Eva Spratt, M.D.
Maya Strange, M.D.
Colleen Victor, M.D.
Child Psychology
Courtney Fleisher, Ph.D.
Logan Hegg, Psy.D.
Marlene Maron, Ph.D.
Kimberly Roy, Ph.D.
Rebecca Ruid, Ph.D.
Isaac Smith, Ph.D.
Pamela Swift, Ph.D.
Critical Care
Rebecca Bell, M.D., M.P.H.
Kristin Crosby, M.D.
Amelia Hopkins, M.D.
Iris Toedt-Pingel, M.D.
Liz Ulano, M.D.
Dermatology
Keith Morley, M.D.
Emergency Medicine
Christine Campbell, M.D.
David Nelson, M.D.
Christian Pulcini, M.D.
Molly Stevens, M.D.
Endocrinology
Lauren Iacono, M.D.
Jennifer Todd, M.D.
Paul Zimakas, M.D.
Gastroenterology
Richard Colletti, M.D.
Michael D’Amico, M.D.
Nina Gluchowski, M.D.
Jillian Sullivan, M.D.
Genetics
Katherine Anderson, M.D.
Julie Refkin, M.D.
Hematology/Oncology
Heather Bradeen, M.D.
Elisabeth Friesen, NP
Jessica Heath, M.D.
Caroline Hesko, M.D.
Monica Ploof, NP
Matthew Shiel, M.D.
Hospitalists
Abigail Adler, M.D.
Leigh-Anne Cioffredi, M.D.
Jen Covino, M.D.
Georgia Farrell, M.D.
Barry Finette, M.D., Ph.D.
Lewis First, M.D.
Jeremy Hassan, M.D.
Christina Imming, M.D.
Scarlett Johnson, M.D.
Karen Leonard, M.D.
Jana Lichtenfeld, M.D.
James Metz, M.D.
Nathnaiel Meuser-Herr, M.D.
Molly Rideout, M.D.
Valerie Riss, M.D.
Paul Rosenau, M.D.
Olubunmi Salako, M.D.
John Saunders, M.D.
Katrina Thornburgh, M.D.
Cameron Ulmer, M.D.
Christa Zehle, M.D.
Infectious Disease
Ben Lee, M.D.
William Raszka Jr., M.D.
McKay Green and
Gold Professor
Marshall Land, Jr., M.D.
Metabolism and Nutrition
C. Lawrence Kien, M.D., Ph.D.
Neonatology
Brittney Accavallo, NNP
Lisa Atwood, NNP
Whittney Barkhuff, M.D.
Merja Cahoon, NNP
Holly Cetrangolo, NNP
Dia Chakravarty. NNP
Nicole Cloutier, NNP
Katherine Dawber, PA
Danielle Ehret, M.D.
Jeffrey Horbar, M.D., M.P.H.
Delia Horn, M.D.
Kimberly Kaufhold, PA
Kaitlin Johnson Kessler, NNP
Samuel Loren, M.D.
Charles Mercier, M.D.
Shane Molinari, NNP
Morgan Nealy, NNP
Meagan Oakes, PA
Deirdre O’Reilly, M.D., M.P.H.
Adrienne Pahl, M.D.
Deborah Saltus, NNP
Jacquelyn Schnackel, NNP
Roger Soll, M.D.
Alexa Visco, NNP
Aaron Wallman-Stokes, M.D.
Susan White, NP
Amanda Woods, NNP
Leslie Young, M.D.
Nephrology
Sarah Couser, M.D.
Liz Hunt, M.D.
Sarah Twichell, M.D.
Neurology
Peter Bingham, M.D.
Deborah Hirtz, M.D.
Gregory Holmes, M.D.
Safoora Syeda, M.D.
Neurosurgery
Katrina Ducis, M.D.
Ophthalmology
Sujata Singh, M.D.
Orthopedics
Jennifer Lisle, M.D.
Otolaryngology
Richard Hubbell, M.D.
Heather Herrington, M.D.
Daniel Gerges, M.D.
Palliative Care
Kaitlin Ostrander, M.D.
Lisa Anne Rasmussen, M.D.
Pathology
Amelia Sybenga, D.O.
Primary Care
Hillary Anderson, M.D.
Monica Benjamin, DNP
Elizabeth Coogan, M.D.
Francisco Corbalan, M.D.
Katherine Cornell, D.O.
Kelsy Good, DNP
Andrea Green, M.D.
Meredith Walker Hanson, FNP
Laura Henderson, M.D.
Elsa Ingpen, DNP
Rachel Larocca, M.D.
Carolyn Lorenz-Greenberg, M.D.
Nathaniel Lesser, NP
Pamela Jackson, M.D.
Heather Link, M.D.
Libby McDonald, NP
Margaret Nelson, M.D.
Julia Ordonez. M.D.
Elizabeth Perzanowski, M.D.
Lori Racha, M.D.
Jill Rinehart, M.D.
Elizabeth Robinson, NP
Matthew Saia, M.D.
Miriam Salameh, M.D.
Heidi Schumacher, M.D.
Michael Seaton, M.D.
Michelle Shepard, M.D.
Jennifer Shull, NP
Nancy Sullivan, DNP
Aaron Wallace, M.D.
Stanley Weinberger, M.D.
Nilgun Zimakas, M.D.
Pulmonology
Kelly Cowan, M.D.
L. E. Faricy, M.D.
Sigfus Gunnlaugson, M.D.
Thomas Lahiri, M.D.
Keith Robinson, M.D.
Radiology
Timothy Higgins, M.D.
Rheumatology
Matthew Hollander, M.D.
Surgery
Martin Keller, M.D.
James Murphy, M.D.
Kennith Sartorelli, M.D.
Urology
Gerald Mingin, M.D.
Vermont Child Health Improvement Program
Rachel Garfield, Ph.D., M.H.S.
Valerie Harder, Ph.D.
Breena Holmes, M.D.
Keith Robinson, M.D.
Heidi Schumacher, M.D.
PEOPLE WHO MAKE A DIFFERENCE
VT LEND
Maria Mercedes Avila, Ph.D.
Residents
Kelly Blanchet, M.D.
Chief Resident
Rachel Adelsheim, M.D.
Erika Aryal, M.B.B.S.
Joanna Berg, M.D.
Lindsay Caldarone, M.D.
Erin Callahan, D.O.
Trevor Coles, M.D.
Julie Erlich, M.D.
Bryan Harrison, M.D.
Til Kus, M.D.
Sehar Laljee, M.D.
Shelby Lawrence, D.O.
Brianna Leahy, M.D.
Adessa Morano, M.D.
Marianna Paradise, M.D.
Jillian Phillips, M.D.
Megan Prue, M.D.
Meredith Stanhope, M.D..
Coral Walker, M.D.
Abigail Watson, M.D.
Alexander Zajack, M.D.
Neonatology Fellows
Luis Bolanos, M.D.
Esther King, M.D.
Julia Litzky, M.D.
Community Clinicians
Allison Adams, M.D.
Denise Aronzon, M.D.
Saraya Balu, M.D.
Alexandra Bannach, M.D.
David Beguin, M.D.
Laura Bellstrom, M.D.
Emile Bernadot, M.D.
Nick Bonenfant, M.D.
Leslie Brodie, M.D.
Aaron Burley, M.D.
Jennifer Carlson, M.D.
Harold Chaskey, M.D.
Sheva Chervinsky, M.D.
Emanuele Chiappinelli, M.D.
Anthony Ching, M.D.
Gregory Connolly, M.D.
Kristen Connolly, M.D.
Leah Costello, M.D.
Sarah Davidson, M.D.
Christina DiNicola, M.D.
Louis DiNicola, M.D.
Jaclyn Dy Lozier, M.D.
Amy Ferguson, M.D.
Monica Fiorenza, M.D.
Bradley Friesen, M.D.
Erin Fuller, M.D.
Anthony Garami, M.D.
Vanessa Garlick, M.B.B.S.
William Gerson, M.D.
Meghan Gunn, M.D.
Deanna Haag, M.D.
Jerry Steve Hale, M.D.
Anna Hankins, M.D.
Breena Holmes, M.D.
Elizabeth Hunt, M.D.
Sandra Kapsalis, M.D.
Tawnya Kiernan, M.D.
Clark Knutson, M.D.
Mark Lazarovich, M.D.
Indra Lovko, M.D.
Philip Magcalas, M.D.
Lynn Mann, M.D.
Emeriti Faculty
The UVM Children’s Hospital honors the faculty members who have spent years serving patients and families in Vermont and Upstate New York. The following faculty have earned emeriti status in recognition of their dedication to patient care, research and teaching.
Stephen Contompasls, M.D. 1994 – 2016
Ann Guillot, M.D. 1979 – 2017
Barbara Frankowski, M.D. 1985 – 2018
Eliot Nelson, M.D. 1991 – 2018
Richard Wasserman, M.D. 1983 – 2019
Craig Lawrence Kien, M.D., Ph.D. 2004 – 2019
Barry Heath, M.D. 1981 – 2020
Ann Wittpenn, M.D. 1997 – 2020
Leah Burke, M.D. 2001 – 2020
Richard Colletti, M.D. 1974 – 2020
Roya Mansoorani, M.D.
Eva Mayer, M.D.
Jack Mayer, M.D.
Sarah McAuliff, M.D.
Anna McCloy, M.D.
Jennifer Menon, M.D.
Melissa Meyer, M.D.
Ashley Miller, M.D.
Meredith Monahan, M.D.
Robert Moore, M.D.
Stephanie Moore, M.D.
Colleen Moran, M.D.
Joseph Nasca, M.D.
Judy Nelson, M.D.
Freda Neyman, M.D.
Judy Orton, M.D.
Alyssa Parker, M.D.
Paul Parker, M.D.
Sobia Qudsi, M.D.
Courtney Riley, M.D.
Patty Rissacher, M.D.
Valerie Rooney, M.D.
Casey Sanner, M.D.
John Saroyan, M.D.
Susan Slowinski, M.D.
Deirdre Schaefer, D.O.
David Schneider, M.D.
Helen Schottel, M.D.
Harriot Shea, M.D.
Steve Soriano, M.D.
Erin Spees, M.D.
Scott Spicer, M.D.
Stacey Strouse, M.D.
Andrea Tidman, M.D.
Robert Tyson, M.D.
Tracy Tyson, M.D.
Alicia Veit, M.D.
Mike Visker, M.D.
Stephen Wood, M.D.
Caroline Yavetz, M.D.
Alan Homans, M.D. 1992 – 2021
Judith Shaw, Ed.D., M.P.H., RN 2000 – 2021
Wendy Davis, M.D. 1987 – 2022
Neils Giddins, M.D. 2007 – 2022
Scott Yeager, M.D. 1985 – 2022
Joseph D. Dickerman, M.D. 1972 – 2024
Nancy A. Drucker, M.D. 1992 – 2024








