August 24, © 2023 UnityPoint Health Proprietary and Confidential
to Protect Yourself 2023
Bloodborne Pathogens How
Objectives
At the end of this course, the learner should be able to:
• Recognize tasks that may involve exposure to blood or other infectious materials
• Select safety equipment to use in the clinical area to prevent exposure to bloodborne pathogens (BBP)
• Discuss reporting an exposure to BBP
© 2023 UnityPoint Health Proprietary and Confidential 2
What are Bloodborne Pathogens?

Bloodborne pathogens (BBP) are infectious viruses in
• Human blood
• Body fluids (but not sweat)
• Other potentially infectious material
Bloodborne pathogens cause disease
© 2023 UnityPoint Health Proprietary and Confidential 3
How can exposure to BBP happen?
• Needle stick or cut
• Contact with mucous membranes or nonintact skin (e.g. skin that is chapped, scraped, or has dermatitis)
• Splash of blood or fluid to eyes or mucous membranes
• Human bites

© 2023 UnityPoint Health Proprietary and Confidential 4
What is the risk from exposure?
The risk is based on the:
• Bloodborne pathogen
• Depth of the wound
• Viral load of the patient who is the source
• Amount of blood/body fluid
• Type of exposure
© 2023 UnityPoint Health Proprietary and Confidential 5
What exposures have more or less risk?
• Deep needle sticks and sharps injuries have a higher risk of BBP

• Hollow-bore needles have the highest risk
• Splashes to mucous membranes have a lower risk for BBP
© 2023 UnityPoint Health Proprietary and Confidential 6
What common diseases can occur from BBP?
The three most common bloodborne disease risks for health care workers (HCW) are from

• Human Immunodeficiency Virus (HIV)
• Hepatitis B Virus (HBV)
• Hepatitis C Virus (HCV)
August 24, © 2023 UnityPoint Health Proprietary and Confidential 7
HIV
HIV is a viral infection of the immune system. The person is unable to fight off other disease.
• HIV can be spread by:
• Sexual contact with an infected partner
• Sharing needles
• Infected mother to her baby
• HIV is NOT spread by:
• Telephones, door knobs, toilet seats, or mosquito bites
• Shaking hands, a hug, being coughed or sneezed on
• Eating food prepared by an HIV-positive person
• Donating blood
© 2023 UnityPoint Health Proprietary and Confidential 8
HIV (continued)
• The risk of getting HIV from a blood transfusion is very low. Blood supplies are tested.
• If exposed to HIV through a needle stick, sharps injury, or a splash, the risk of getting the disease is 0.09-0.3%
• The risk is much less when preventative medicines are taken as soon as possible after the exposure
• Signs of HIV may be many years after the infection
• Aperson can infect others even though they do not look or feel sick
August 24, © 2023 UnityPoint Health Proprietary and Confidential 9
Hepatitis B
Hepatitis B is a virus that affects the liver. Many people who are infected with the virus do not have signs.
• Signs of Hepatitis B include:
• Yellow skin color
• Dark urine
• Lightened stool color
• Nausea
• Vomiting
• Feeling of illness
August 24, © 2023 UnityPoint Health Proprietary and Confidential 10
Hepatitis B (continued)
Hepatitis B can be spread by:
• Sexual contact with an infected partner
• Sharing needles
• Infected mother to her baby during birth
© 2023 UnityPoint Health Proprietary and Confidential 11
Hepatitis B (continued)
The Hepatitis B vaccine is available to all employees who may be exposed to blood or other potentially infectious material (OPIM)
• The vaccine (a series of two or three injections, depending on which brand of vaccine is used) is offered at no charge
• The vaccine may be started at any time
• If exposed to Hepatitis B by a needle stick, sharps injury, or a splash, the risk of getting the disease is anywhere from 1-62%, based on the severity of the exposure
• The risk drops to almost 0% if the series of injections has been completed
• If you are confirmed immune to Hepatitis B, there is no recommendation to be checked again or to be given boosters
• Search for “Hepatitis B Vaccine” at UPH Policies
© 2023 UnityPoint Health Proprietary and Confidential 12
Hepatitis C
Hepatitis C is a virus similar to Hepatitis B
• Hepatitis C is the most common BBP transmitted through blood exposure
• 70% of Hepatitis C patients have no signs
• Hepatitis C can be spread even when there are no signs
• About 15% of people who become infected with Hepatitis C fight off the infection and do not spread it to others
© 2023 UnityPoint Health Proprietary and Confidential 13
Hepatitis C (continued)
• If exposed to Hepatitis C through a needle stick, sharps injury, or a splash, the risk of getting the disease is 0 to 7%
• The virus may be dormant (or not do anything) for 10 to 20 years before causing signs of fatigue, loss of appetite, and abdominal pain
• Screening tests for Hepatitis C started in the early 1990s
• Blood transfusions are no longer a source of Hepatitis C
• There is no vaccine to prevent Hepatitis C, but there is treatment
© 2023 UnityPoint Health Proprietary and Confidential 14
What if I am exposed to BBP?
• First, wash needle sticks and cuts with soap and water
• Flush splashes with water
• Irrigate eyes with water, saline, or sterile solution for 15 minutes
• Notify your immediate supervisor and seek evaluation and treatment through:
• Regional Employee Health or

• Emergency Department
• Complete an incident report through RL Datix Reporting
© 2023 UnityPoint Health Proprietary and Confidential 15
Report the exposure right away
• Treatment should start within 1 to 2 hours of the exposure
• Prompt treatment reduces the risk of the virus infecting cells
• In high risk exposures, treatment should start before waiting on source patient testing
• Prompt reporting ensures the source patient can be contacted before they leave the hospital
• Blood is tested for Hepatitis B, Hepatitis C, and HIV
• Rapid HIV testing of source patients can help with timely decisions about the use of HIV Post-Exposure Prophylaxis (PEP)
© 2023 UnityPoint Health Proprietary and Confidential 16
What is PEP?
• PEP is Post-Exposure Prophylaxis, or prevention after an exposure
• PEP for HIV involves taking medicines as soon as possible within 2 hours, but no more than 72 hours (3 days), after exposure. This reduces the chance of becoming HIV-positive
• The medicines prevent HIV from making copies of the virus and spreading through the body
• Three medicines are usually prescribed and must be taken for 28 days
© 2023 UnityPoint Health Proprietary and Confidential 17
How do I prevent BBP exposure?
• Refuse to rush or be distracted
• Ask for help if the patient is fighting, not cooperating or semi-sedated
• Protect your eyes and mucous membranes – consider when splashes/sprays may occur, and wear face and eye protection
• Double glove during surgical procedures
• Use the smallest gauge needle that will do the task
• Use hands-free passing of sharps to others, i.e., place sharps in a neutral zone or dispose of sharp after use rather than handing it to a coworker for disposal
© 2023 UnityPoint Health Proprietary and Confidential 18
How do I prevent BBP exposure?
• Know where needles and sharp objects are placed
• Never handle devices by the sharp end, even if covered by a safety device
• Activate safety on needle or sharp immediately after use
• Dispose of needle or sharp immediately – do not lay it down for disposal later
© 2023 UnityPoint Health Proprietary and Confidential 19
Prevent BBP exposures
Labeling and Disposal
• Containers that may have infectious materials or biohazard wastes are labeled with the universal biohazard symbol and the word “Biohazard”
• Used sharps need to be put in the biohazard boxes in patient care areas and medicine rooms

• Counter sharps containers must be secured in needle box stabilizers

© 2023 UnityPoint Health Proprietary and Confidential 20
Prevent BBP exposures
Personal Protective Equipment (PPE)
PPE includes: gloves, liquid-resistant gowns, goggles/face shields, masks

• PPE is provided for all employees
• It is your responsibility to use the PPE for the clinical situation
• Wear gloves for exposure to blood, body fluids, contaminated items, mucous membranes, and non-intact skin
• Wear gowns when clothing/scrubs may be soiled
• Wear eye protection … see the next slide
© 2023 UnityPoint Health Proprietary and Confidential 21
Prevent BBP exposures
• Wear eye protection when blood is very likely to be involved, such as:
• Starting and discontinuing an IV
• Drawing blood andABGs
• Turning/caring for patient who has a ventilator

• During intubation
• Irrigation of any type
• Stoma/Fistula care
• Emptying urine bag, urinal, JP drain, and bed pan
• Handling and disposing of blood and body fluids
• Dressing change
• Glucometer testing
• Lumbar Puncture
• Surgery
• Baby delivery
• Trauma
• Endoscopy procedure
• Medical emergency
• Patients who are known to spit
© 2023 UnityPoint Health Proprietary and Confidential 22
Prevent BBP exposures
• Eye glasses do not give enough protection

• Wear masks and eye protection during procedures and patient care when there can be splashes or sprays of blood, body fluids, secretions, and excretions
• Before leaving the patient care area, remove PPE and place it in the trash
What’s wrong with this picture?
This picture shows safer use of PPE was needed.
Based on the bloodsplatter,
1. a face shield should have been used
2. gloves should be used to handle these items
© 2023 UnityPoint Health Proprietary and Confidential 23
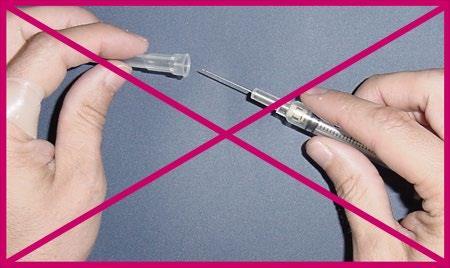
Prevent BBP exposures
Safety Devices
Practice activation of safety devices before use on a patient
• Activate the safety device immediately after use
• Ensure safety device is fully engaged – hear the click and see the needle is covered
• Never recap a used needle unless properly trained to use a mechanical device or a one-handed technique

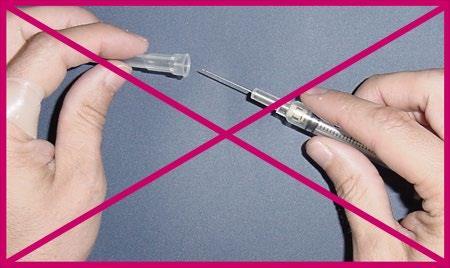
August 24, © 2023 UnityPoint Health Proprietary and Confidential 24
Prevent BBP exposures
Safety Devices continued
Practice activation of safety devices before use on a patient
• Keep hands away from needle tip at all times, both before and after activation of the safety device
• Do not try to override or defeat the safety lock
• Report defective safety devices or problems with activation to your manager
© 2023 UnityPoint Health Proprietary and Confidential 25
Use safety devices and protect yourself
Remember: Safety devices are not perfect. Do not rely only on the safety feature to protect you. Never hold a syringe at the needle end. The best person to prevent needlestick and sharps injuries is you!
• Dirty broken glass is cleaned up using tongs, broom, pieces of cardboard, or what you have in your work area… Not your hands

© 2023 UnityPoint Health Proprietary and Confidential 26
Bloodborne Pathogen Exposure Control Plan?
Please contact the UnityPoint Health – Des Moines Volunteer Services Team:
Blank Children’s Hospital and Iowa Methodist Medical Center
Iowa Lutheran Hospital



Methodist West Hospital
Office Location: Powell 2, Room 218

Phone: (515) 241-6414
Email: dm_volunteers@unitypoint.org
Hospital Location: First Floor, Mid Wing


Phone: (515) 263-5227
Email: dm_volunteers@unitypoint.org
Office Location: Ground Floor, Room 1188
Phone: (515) 343-1088
Email: dm_volunteers@unitypoint.org
How do I learn more and where do I find our
© 2023 UnityPoint Health Proprietary and Confidential 27
Attestation of Completion
Thank you for completing this training module.
You must now electronically sign the completion form to acknowledge that you have:
• Read the Bloodborne Pathogens Training document in full.
• Understand how to obtain a copy of UnityPoint Health’s Bloodborne Pathogen Exposure Control Plan.
The electronic/online form is accessible through a separate link that was provided to you by UnityPoint Health – Des Moines Volunteer Services. If you do not have the link to the completion form, please contact your Volunteer Coordinator for this information.
August 24, © 2023 UnityPoint Health
28
Proprietary and Confidential