Carolina scıentific
SPRING 2025 | Volume 20 | Issue 2

—USING AI TO DETECT PAIN IN MICE— full story on page 10

SPRING 2025 | Volume 20 | Issue 2

—USING AI TO DETECT PAIN IN MICE— full story on page 10





Check out all of our previous issues at issuu.com/uncsci. As the organization continues to grow, we would like to thank our Faculty Advisor, Dr. Lillian Zwemer, for her continued support and mentorship.










Mission Statement:
Founded in Spring 2008, Carolina Scientific serves to educate undergraduates by focusing on the exciting innovations in science and current research that are taking place at UNC-Chapel Hill. Carolina Scientific strives to provide a way for students to discover and express their knowledge of new scientific advances, to encourage students to explore and report on the latest scientific research at UNC-Chapel Hill, and to educate and inform readers while promoting interest in science and research.
Letter from the Editors:
We have had the privilege to lead Carolina Scientific for the past two years, and during this time, we have witnessed remarkable growth—both in our members and in the organization as a whole. From members who began as copy editors and quickly developed into skilled writers and associate editors, to the expansion of our publication into new formats like the blog series, the progress has been nothing short of inspiring. Our mission to make science more engaging and accessible has remained steadfast, and it has been incredible to see our larger Carolina community embrace this vision. This issue reflects the hard work and dedication of every individual involved. As we prepare to “pass the torch”, we are confident Carolina Scientific will continue to thrive. Thank you for supporting us, and we hope you enjoy this issue as much as we’ve enjoyed creating it.
- Sarah Giang & Isaac Hwang Editors-in-Chief

Editors-in-Chiefs Sarah Giang
Isaac Hwang
Design Editor Tanisha Choudhury
Copy Editor Corinne Drabenstott
Managing Editor Daniela Danilova
Treasurer Natalie Druffner
Secretary Reagan Gulledge
Publicity Chair Masha Dixon
Fundraising Chair Ria Patel
Associate Editors
Andrew Phan
Alex Li
Julia Boltz
Sprihaa Kolanukuduru
Andrew Phan
Online Content Manager Kirina Shah
Faculty Advisor Lillian Zwemer, Ph.D.
Travis Alegria
Tulsi Asokan
Erin Kirsten Atos
Brantley Aycock
Julianna Bryant
Ava Carlton
Britney Munguia
Castillo
Daniela Danilova
Shadi Darawsheh
Anooshka Deshpande
Aria Dhupkar
Sarah Edmonds
Julia Ellington
Sanjana Farmah
Aditi Gajavelly
Olivia Gatto
Shritha Gayathri
Gargi Gole
Ashley Hardner
Alexis Hirth
Angelina Ho
Madelyn Holleman
Emma Johnson
Sai Kolla
Kameryn Lloyd
Liyuan(Alisa) Luo
Lana Maizel
Gerald Ofosu
Siri Pandi
Ryan Parsaee
Ambika Puri
Emily Rajappan
Avery Sallean
Julia Sallean
Vina Senthil
Sanjita Srinath
Paige Twohill
Akshara Venkatesan
Gayatri Venkatesan
John Wadington
Fiona Yeung
Rachel Zeisloft
Selinda Zhu
Aditi Deshpande
Alacia McClary
Alexander Kinrade
Alin Campos-Martinez
Amelia Bruns
Ana Barton
Angela Liu
Caroline Varma
Cindy Lam
Corinne Drabenstott
Diana McLean
Dianne Celemen
Erin Kirsten Atos
Evan Raines
Gayatri Venkatesan
Hana Nakhle
Jacob Allred
Jacqueline Bodycomb
Jay Sedam
Jonah Ettore
Marley Boyer
Bhavika Chirumamilla
Tanisha Choudhury
Srinithi Gali
Prisha Gautam
Lillian Guo
Angelina Ho
Veda Komera
Cindy Lam
Clara Lord
Spoorthi Marada
Lainey McDermott
Holland Mickle
Estella Monica
Josey Beavers
Kameryn Lloyd
Kate Golden
Lainey McDermott
Magdalena Araya
Mckenzie Miller
Nastia Hnatov
Natalie Druffner
Nicholas Boyer
Oliver Ewy
Olivia Gatto
Paige Strecker
Risha Solanki
Ryan Guzman
Sai Satvik Kolla
Veda Komera
Sajni Patel
Sam Jump
Sarah Edmonds
Shivank Kancharla
Sneha Adayapalam
Taylor O’Connor
Victoria Yang
Vina Senthil
Yasmine Ackall
Youyou Zheng
Britney Munguia
Hana Nakhle
Matthew Rodzen
Ruhi Saldanha
Heidi Segars
Caroline Varma

Drug Design Made Easy
Travis Alegria
From Whiskers to Wincing: Using AI to Detect Pain in Mice
Tulsi Asokan
Sky to Soil: Remote Sensing Uncovers Hidden Carbon Losses
Emma Johnson
Computational Combat
Sai Satvik Kolla
BYOB: bring your own blood vessels
Kameryn Lloyd
Precision Without Incision: Focused
Ultrasound as a Therapeutic
Avery Sallean
Picturing a Pixel-Perfect Medical Image
Fiona Yeung
Bending the Rules: The Geometry Behind What Holds Us Together
Selinda Zhu
Histones: Unraveling the Mysteries of DNA
Erin Kirsten Atos
“Sleep Like a Baby: Infant Sleep as a Determinant for Behavior“
Brantley Aycock
Mice Mothers Might Know Best
Julianna Bryant
The Secret To Living Longer
Britney Munguia Castillo
On The Bleeding Edge: Understanding the Liquid of Life
Daniela Danilova
Putting the Parrot in Parrotfish: Understanding Territorialism in Caribbean Parrotfish
Sarah Edmonds
Two Sides of the Same Cell
Gargi Gole
Speciation in the Small: Adaptation and Genetic Divergence in Copepods
Siri Pandi
Wrapping Our Heads Around It: Histones and Gene Activity
Vina Senthil
Bridging the Gaps: Understanding the Framework of DNA Mismatch Repair
Rachel Zeisloft
When Worry Worsens: How OCD and Anxiety
Sensitivity Amplify Pandemic Fear
Julia Ellington
Are You Just ‘On Your Period’? Women Deserve Better
Olivia Gatto
The Hidden Epidemic-Understanding Physician Burnout
Alexis Hirth
The Key to Immortality: Stress Less, Live Longer
Emily Rajappan
Understanding Alcohol’s Grip: The Neural Mechanisms of Stress and Addiction
Gayatri Venkatesan
The Future of Psychedelics: A Cure Without the Kaleidoscope
John Wadington
Mice and Medicine: The Neuroscience of Alcohol Use
Ava Carlton
Medicine is Transforming
Deshpande
Beyond the Knee: Healing the Knee Through the Mind
Sanjana Farmah
Medicine’s Got Your Back: Optimizing Chronic Pain Treatment
Aditi Gajavelly
Uncovering the Dynamic Molecular Landscape of Uterine Cancer Development
Shritha Gayathri
Personal Decisions Require Personalized Approaches
Ashley Hardner
The Diagnosis Dilemma: Unveiling
Angelina
School Meals for All: Fighting to Secure Free School Meals for NC Students
Madelyn Holleman
Long-Acting Hope: The Evolution of HIV Treatment in a Decade Liyuan (Alisa) Luo
A Change in Heart: Reanalyzing the Genetic Link Between Brain and Cardiovascular Health
Lana Maizel
The science behind heartbreak: An inside look at Atherosclerosis
Gerald Ofosu
Further Away, The Harder
Ambika
Chew On This: The Role of Omega-3 Fatty Acids in Obesity
Julia Sallean
A Smarter Way to
Sanjita
What to Eat for Relief: Managing Migraines with Diet
Akshara Venkatesan
Shadi
Aria
Ryan
By Travis Alegria

Organic chemistry has many amazing applications in the real world, but many students never get to see the magic behind the scenes. Look no further than the pharmaceutical industry, which shapes the lives of everyone you know. The development of drugs has long been a complex process, where even small modifications to drugs can pose a significant challenge. The National Institute of Health (NIH) estimates that research and development for a new drug can range from $300 million to $4.5 billion.1
Dr. Erik Alexanian, a Professor of Organic Chemistry at the University of North Carolina – Chapel Hill, along with his research lab, seeks to develop new synthetic reactions applicable to drug development, hoping to revolutionise how we approach drug discovery and creation. Dr. Alexanian, who earned his chemistry doctorate at Princeton University, has worked in this research field for over seventeen years. He highlights that “researchers in organic chemistry have ventured outside their comfort zone to tackle problems relating to polymer chemistry, inorganic chemistry, and biological chemistry”.2
One of the most challenging aspects of drug optimization has been the ability to make precise, single-carbon modifications to existing compounds.


Think of this process like adding a single LEGO brick, analogous to a carbon, to the end of your LEGO sword, analogous to the carboxylic acid chain. That single LEGO brick addition does not visually make a huge difference, but on a molecular scale this addition changes the mass, the reactivity, and ultimately the behaviour of that structure. Now zooming back into the world of organic chemistry, homologation of carboxylic acids, which as previously described is extending their carbon chain by one -CH2- group, has been identified as a potential means to address the problem of drug optimization.
Carboxylic acids are “fundamental building blocks that appear frequently in both drug molecules and natural products”.2
Traditional methods for modifying carboxylic acids used the Arndt-Eistert reaction, pictured in Figure 1, which required multiple steps leading to the involvement of hazardous and explosive reagents which limit their practical uses in drug research.
To expand upon the outdated technique, Dr. Alexanian’s groundbreaking advancement proposes a novel one-step homologation process involving a stable (1-phosphoryl) vinyl sulfonate reagent, which reacts under mild conditions (Reagent).2 The process goes as follows:
1. Identify: Begin with the carboxylic acid of interest.
2. First Radical reaction: Remove the hydrogen off of the oxygenhydrogen (-OH) bond, forming a carboxyl radical – which is a carboxylic


acid group without the hydrogen that is normally bonded to the single-bonded oxygen atom – resulting in unpaired electrons on the oxygen. This makes it an unstable molecule.
3. Second Radical reaction: Due to the instability, this radical then loses carbon dioxide and becomes a carboncentered radical – which means the unpaired electrons are now closest to the carbon of the carboxylic acid functional group.
4. Reagent Addition: Finally, the (1-phosphoryl) vinyl sulfonate reagent reacts with the radical and adds an extra carbon onto the original carboxylic acid structure (Proposed mechanism).3
This novel approach addresses a long-standing challenge scientists have faced in organic synthesis and offers several advantages such as direct modification of carboxylic acid, reaction under mild conditions, and versatility of products that can be formed from the reaction depending on the desired use of the drug. However, there is a downside. Due to the precision required in chemistry, some challenges come with the formation of the compound in one step. Regarding this reaction specifically, the process forms an unstable acyl phosphonate intermediate that is highly reactive. The details of what this intermediate looks like, or what it even is, isn’t crucial to understanding
the challenge it creates. Ultimately, the instability creates a challenging process where you must utilize the product’s reactivity, while ensuring perfect atmospheric conditions are present. This was the key challenge that once resolved allowed for a smooth process forward in his research.
The addition or homologation of one carbon to a different compound may seem like a simple change. However, think of this like a lock and key for your house/apartment door. That one key has been precisely constructed to open only your door, and it must be carefully etched to fit properly. Similarly, drug compounds react in extremely specific ways in your body and therefore require precise structures to bind properly and carry out their intended function. “The addition of one extra carbon can significantly increase the potency of a biologically active molecule”. Essentially, this means that the addition of a carbon can allow a drug to have 99% effectivity on treating a major disease, such as diabetes, rather than only 50% effectivity. Homologation improves these structural properties by optimizing the time of absorption and metabolism of drugs, allowing the drug to work in hours rather than days.
The introduction of this novel technique opens several exciting new possibilities within drug development.
Firstly, this technique can create efficient modification – alteration of chemical structure - of drug candidates to help improve properties, and ultimately, increase the potency of drugs. In the immediate future, it can serve to generate novel building blocks for the rapid creation of library chemicals, which are general ingredients used in the drug discovery process. This further evokes excitement that this research will be widely applicable in all labs around the country, and eventually worldwide.
The development of direct modification of carboxylic acids via homologation signifies a solution to a century-old problem in synthetic chemistry. This one-step reaction provides pharmaceutical researchers with a powerful new tool for drug development. If used properly, this has the potential to accelerate the development of more effective therapeutic agents, consequently allowing healthcare the ability to address unmet medical needs and lowering the costs of life-saving drugs. This innovative approach demonstrates how a foundational advancement in chemistry can produce wide-scale impacts on medical research and human health. As this technique becomes a staple tool within researcher’s toolbox we can anticipate more advances in the development of the next generation of pharmaceutical compounds.
1. Aylin S., Trinidad B., Amber J., Benjamin S. Costo f Drug Development and Research and Development Intensity in the US, 2000-2018. https://pmc.ncbi.nlm.nih.gov/articles/PMC11214120/ (accessed February 22nd, 2025)
2. Interview with Erik Alexanian, Ph.D. 02/18/2025
3. Jonathan N. Gruhin, Richard Kim, Aristidis Vasilopoulos, Eric A. Voight, and Erik J. Alexanian Journal of the ACS 2024 146 (48), 32919-32924
DOI: 10.1021/jacs.4c13687
By Tulsi Asokan

One of the most challenging concepts for researchers to measure is something that everyone experiences: pain. Unlike blood pressure or temperature, pain is subjective—one person’s mild discomfort could be another’s unbearable agony. Subjectivity makes it difficult to assess pain consistently, especially in non-verbal patients and animals. Dr. Mark Zylka, a W.R. Kenan, Jr. Distinguished Professor at the University of North Carolina at Chapel Hill, is working to change that. His team has developed an artificial intelligence-driven tool (AI) that standardizes pain measurement in mice, called PainFace.1 This software is a critical step in making pain research more precise, reproducible, and ultimately, applicable to human medicine.
When it comes to research on various pain relief methods and drugs, a mouse model is the most common. The Mouse Grimace Scale (MGS)2 was developed in 2010 and is now widely used to quantify levels of discomfort in mice, allowing researchers to model human pain and test potential therapeutics. Until now, researchers used this scale to manually score pain levels by watching videos of mice and assigning scores to specific facial expressions, such as narrowed eyes or tense facial muscles. But this method is labor intensive, time-consuming, and inconsistent. Analyzing videos can take minutes per each individual frame, and different researchers may assign different pain scores based on their own interpretations. PainFace aims to solve this problem by automating the process of grimace analysis.
PainFace is a cloud-based platform allowing researchers to upload mouse grimace visuals via the internet from any location without having to install the software locally. This
data is then stored, processed, and analyzed within a single system so that researchers can interpret pain levels quickly and accurately. To develop PainFace, researchers in the Zylka lab used a machine learning model to train the AI to recognize pain levels from different parts of a mouse’s face. Training included sorting images from 30 minute-long footage into categories based on changes in the eyes, ears, whiskers, and noses of different mice (Figure 2). The AI was coached separately for each facial feature and given images with different backgrounds, colors, and orientations to weed out discrepancies in analysis. This ensured that the technology could be used again in different labs where videos were taken with slight differences.
“Because of machine learning, if you have variability in your training data, then the machine learning model is going to have variability,” Dr. Zylka says. “It is only as good as what you train it to do.”


Each time the AI made a mistake, an advanced optimization algorithm was used to help PainFace adjust and improve. This type of algorithm, or series of instructional code, is used to direct AI towards the most accurate analysis through trial and error. This repetitive process used a set of data from expert scorers in the Zylka lab to make PainFace faster and more accurate. The completed software can process up to 32 grimace videos at once, dramatically improving efficiency compared to manual scoring, which typically involves analyzing only a single frame every few minutes. The program is built with a RESTful API (Application Programming Interface), meaning it can easily integrate with other research software, allowing labs around the world to use the same standardized pain measurement system.
To ensure PainFace’s accuracy, Dr. Zylka’s team ran a series of validation experiments.
The first data pool used videos of mice before and after laparotomy surgery, a procedure in which the abdomen is surgically opened and explored. The mice were divided into three groups: the Sham Surgery Group (preparation and anesthesia without incision), the Laparotomy Group (full surgery), and the Laparotomy with Carprofen Group (surgery with a pain-relieving drug). After surgery, PainFace analyzed the grimace scores of each group using videos of the mice during recovery. As expected, the Laparotomy Group displayed significantly more pain grimaces than the Sham group, while the Carprofen Group group showed reduced grimacing from the medication.
Further testing involved injecting an inflammatory agent called formalin into the hindpaws of mice. Formalin is commonly used in research to create standardized levels of pain or discomfort. PainFace was able to successfully quantify grimace scores across different concentrations of formalin, aligning with existing research showing that higher concentrations result in greater pain responses.
Dr. Zylka said, “The bottom line is, any mammal has a grimace to read. It’s just a matter of generating enough training data.”
The Zylka lab is currently collaborating with researchers across the department to translate PainFace findings for rats, horses, and pigs. But PainFace isn’t just about improving
animal research. Zylka believes that with enough data and funding, PainFace could be used to advance human health. In addition to testing the effectiveness of preclinical pain relief drugs, PainFace provides a blueprint for an automated and objective pain assessment tool that could be adapted for human patients. One of the biggest problems in clinical pain management is that doctors often rely on patient self-reports, thus the traditional “Rate your pain from 1 to 10” scale. But pain tolerance varies between individuals, making comparisons difficult. Additionally, nonverbal patients, like infants and non-communicative adults, cannot self-report their pain levels. PainFace could be part of a future where hospitals use AI to monitor facial expressions in real-time, leading to more efficient and effective pain treatment.
The implications of this research extend far beyond the lab. By eliminating subjectivity from pain assessment, PainFace makes preclinical pain research more reliable and reproducible. It lays the groundwork for AI-driven pain analysis in human medicine and standardizes the way researchers recognize pain.
Dr. Zylka’s team at UNC Chapel Hill isn’t just improving animal research; they’re paving the way for a future where pain can be measured instead of estimated.

Mark Zylka
1.Zylka, M.; Mogil, J.; et al. Development of PainFace software to simplify, standardize, and automate mouse grimace analyses.
Pain2024, 165 (8), 1515–529.
2.Langford, D.J.; Bailey, A.L.; Chanda, M.L.; Clarke, S.E.; Drummond, T.E.; Echols, S.; Glick, S.; Ingrao, J.; Klassen -Ross, T.;Lacroix-Fralish, M.L.; et al. Coding of facial expressions of pain in the laboratory mouse. Nat. Methods 2010, 7 (6), 447–449.
3.Interview with Mark Zylka, Ph.D. 03/11/25.
By Emma Johnson

When a hurricane hits North Carolina, there are obvious signs of destruction in its wake. However, where there is a fallen tree, there is the invisible loss of carbon stored inside. As the material decomposes, the carbon once locked up as leaf and plant fiber is either stored as long-term soil carbon or released back into the atmosphere as decomposers breathe out carbon dioxide. As deforestation, changing land use, and natural disasters push plant carbon back into the atmosphere, it is crucial to account for carbon during global carbon cycle studies in the face of a changing climate. As researchers work to build a robust account of global carbon fluxes, the Carolina Population Center, in collaboration with other geographic and Earth science researchers at the University of North Carolina at Chapel Hill (UNC), is turning to remote sensing — the science of getting information about areas from a distance using satellites or aircraft — to assess losses in plant material that are hard to account for on the ground.
When Dr. Conghe Song first began his time at Carolina, he witnessed firsthand the devastation that Hurricane Floyd had wreaked, even in the inland parts of the state. During fieldwork in Duke Forest, the scale of downed trees and debris was striking. That level of damage extends across the state in the wake of any hurricane. Song’s group has projects on a global scale and is especially interested in how to map land use across large areas. However, a combination of timing and collaboration presented a more local opportunity.
Though Dr. Song’s group advances research in remote sensing and land use mapping, his background is in forestry, and he brings this perspective to the world of carbon cycling. He claims that “Biomass is key ecosystem information for managers and ecologists. It’s a bottleneck for global carbon accounting.” In emerging carbon credit industries, which monetize carbon sequestration to offset emissions, environmental organizations and industry stakeholders point to forests as nature-based carbon removal solutions. Carbon
dioxide in the atmosphere removed through photosynthesis and stored in wood can stay there as long as the tree is alive, for decades, or even centuries, making it a semi-permanent removal of carbon dioxide from the atmosphere. However, as slowly as the vegetation takes up carbon dioxide, natural disasters can release the locked up carbon dioxide quickly.
For carbon measurements, there are many natural and unnatural processes that can tip the scale. Fire, deforestation, and storm damage all contribute some amount of loss in sequestered carbon.
Quantifying biomass is hard. Technically, biomass is the weight of living material over a given surface area. It is one of many factors to consider when accounting for all the carbon locked up at various points throughout Earth processes. Dr. Song says that “this is a problem where everyone is struggling. It’s not easy to solve.”
To account for the carbon locked up in vegetation, first you have to account for the amount of biomass. Traditionally, biomass is measured by cutting the vegetation, drying it, and measuring its dry weight. Alternatively, researchers can measure how thick the trunk is and how tall the tree is to quantify biomass, but in the absence of drying and

measuring, even ground observations of vegetation sizes are indirect measurements. One strong approach that is both environmentally friendly and easier to scale is remote sensing, the science of obtaining information about the Earth’s surface from a distance. Song’s lab relies on the multiple sources of remote sensing data to estimate biomass. One of those sources is called LiDAR, which stands for Light Detection and RAnging. LiDAR is a remote sensing technology that sends out a pulse of light from a satellite, aircraft, or above-ground sensor, to measure distances to objects that can then be used to make a precise 3D map of Earth’s surface. For forests in eastern North Carolina that are vulnerable to hurricanes, LiDAR can measure features like tree canopy height. However, canopy height is still not a direct measurement of biomass. Therefore, LiDAR data must be paired with data from the ground that can relate the optical height with biomass checkpoints.
Song’s lab uses LiDAR data to measure features like tree canopy height for forests in Eastern North Carolina, where forests are vulnerable to hurricanes. However, canopy height is still not enough to estimate biomass. Therefore, LiDAR data must be paired with other remotely sensed data, such as optical remote sensing that captures reflected sunlight from Earth’s surface and can provide seasonal variation of different plant species. Additionally, RaDAR, or Radio Detection and Ranging, which is like LiDAR but uses radio waves instead of lasers, can provide canopy volume information. These remotely sensed data will be fused together and connect to ground biomass sampling plots. With this data, Song’s lab can then produce biomass maps using machine learning tools.
Dealing with large datasets from different sources is challenging. Logistical challenges, such as matching spatial coordinates between ground data and satellite imagery, can complicate the process. Improving GPS technology can tackle some of the issues, but obstacles remain that make quantifying biomass and its carbon flux difficult. Crucially, the US Department of Agriculture has collected sampling


plots across the country via the Forest Inventory and Analysis (FIA) program, including North Carolina. These plots provide key anchor points for Song’s effort in mapping biomass over large area. By comparing a pre-hurricane and post-hurricane biomass map, researchers can determine the loss of biomass, thus carbon dioxide, from the storm.
Outside of storm-related carbon loss, broader work from UNC’s Remote Sensing and Ecological Modeling Group on mapping above-ground biomass will inform future land managers and policymakers in data-driven decision-making. The carbon that vegetation removes from the atmosphere transcends borders, and so does the group’s research. Internationally, the group is working on understanding the influence of community forestry on local, social, and environmental systems in Nepal. As climate change intensifies, their research will become increasingly critical for understanding how biomass cycles carbon.
By leveraging a combination of remotely sensed imagery and machine learning, UNC’s Remote Sensing and Ecological Modeling Group is making it possible to assess carbon losses at a scale that was once unattainable. As climate change continues to drive more frequent and intense storms, this work will be instrumental in shaping resilient land management strategies and improving our understanding of carbon dynamics. The invisible carbon losses caused by extreme weather events may be difficult to measure, but with cutting-edge technology and interdisciplinary collaboration, scientists are uncovering critical insights that will help guide future conservation and climate mitigation efforts. Dr. Song remains excited to tackle the global challenges that come with global processes. As he puts it, “A couple of decades ago, this kind of work was unimaginable. Nowadays, all these images are at your fingertips.”
1. Interview with Dr. Conghe Song, 2/28/2025
2. Ehlers, D., Wang, C., Coulston, J., Zhang, Y., Pavelsky, T., Frankenberg, E., Woodcock, C., & Song, C. (2022).
Mapping Forest Aboveground Biomass Using Multisource Remotely Sensed Data. Remote Sensing, 14(5), 1115. https:// doi.org/10.3390/rs14051115
By Sai Satvik Kolla

At the University of North Carolina at Chapel Hill, the Brunk Lab is pioneering innovative approaches to understanding cancer cell biology through computational methods and imaging analysis. The lab’s groundbreaking research combines experimental and computational techniques to analyze DNA variants in cancer cells, focusing on developing strategies for taking and interpreting pictures of cellular nuclei (where DNA is stored).¹ This interdisciplinary approach is becoming increasingly crucial as cancer research faces new challenges in understanding complex cellular mechanisms and drug resistance patterns.²
Dr. Elizabeth Brunk’s journey to becoming a leading computational biology researcher was guided by mentorship and scientific curiosity. As a biochemistry undergraduate at the University of Michigan, Dr. Brunk’s research career began when she discovered computational biophysics — a field that applies physical laws to understand biological phenomena. This early exposure to computational methods and supportive mentorship led her to pursue advanced studies in pharmacology. Now, established in the Pharmacology department at UNC-Chapel Hill, Dr. Brunk applies her computational expertise to understand drug interactions and cellular pathways critical to cancer development. This

specialized focus emerged naturally, as she recognized how pharmacological approaches (studying drugs and their effects on biological systems) could address fundamental questions in cancer biology. Her approach enabled her to develop novel therapeutic strategies targeting cancer-specific vulnerabilities.¹
“Existing computer programs only catch about one-third of these critical structures in detailed pictures and often miss many that are present.”
Her work today reflects a critical area of cancer biology: understanding the impact of DNA variants on cancer cell behavior. DNA variants are changes in our genetic code that can be as small as a single letter change or as large as missing or added sections. Some of these changes are harmless or helpful, but others can be harmful, primarily when they affect genes controlling how cells grow and divide. Specific variants in these critical genes can disrupt standard cellular controls, causing cells to multiply uncontrollably and form cancers.² In the lab, team members grow cancer cells from actual patient tumors and study how these cells react when treated with different drugs.² This hands-on approach allows them to observe how actual cancer cells respond to potential treatments directly. Then, the computational team uses advanced artificial intelligence and machine learning techniques to analyze massive datasets from thousands of cancer cell lines.² These datasets contain detailed genetic information, drug response measurements, and protein expression patterns from various types of cancers. These methods can identify patterns showing how specific genetic

variations influence biological processes like cell growth, survival, and response to treatments.² This dual approach allows for a more complete understanding of cancer cell behavior and therapeutic responses.²
Their current project uses AI to examine the control centers of cells in microscopic images to address a significant challenge in cancer research. This project focuses on improved methods to analyze cellular photos, particularly those showing unusual DNA structures outside the normal chromosomes in cancer cells. Scientists must study thousands of cell images to accurately detect and count these unique DNA pieces that help cancer cells survive treatments. Traditional methods require researchers to manually examine many images of individual cells - a process that takes too much time and limits how much research can be done.
The manual approach to analyzing these images creates significant slowdowns in research. Current practices involve experts carefully identifying and counting these unique DNA structures in each image, which is highly time-consuming and prone to mistakes. Existing computer programs only catch about one-third of these critical structures in detailed pictures and often miss many that are present.² The team aims to dramatically increase the speed and accuracy of analyzing these critical cancer cell features by developing advanced AI vision systems. AI systems make it possible to conduct research at a previously impossible scale with manual methods.
The significance of this approach becomes evident when considering the complexity of cancer cell analysis.² Cancer cells often show unusual changes in their DNA. Some DNA pieces break from normal chromosomes and exist separately within the cell, while other unusual DNA regions remain attached to chromosomes.² These different arrangements affect how cancer behaves and responds to treatment.
The lab’s AI vision methods can identify and analyze these DNA changes faster and more accurately than traditional approaches.² While expert scientists might take hours to examine only a hundred cells and miss up to 70% of these vital DNA structures, the team’s AI systems can process thousands of cells in minutes with higher detection rates.² This improved capability to quickly and reliably detect DNA changes is
crucial for understanding how cancer cells adapt to survive treatments and why some patients don’t respond to therapy.²
The implications of this research extend beyond efficiency gains. The team’s findings contribute to growing knowledge about cancer cell adaptation and drug resistance.² By combining high-throughput imaging analysis with computational methods,
the lab can better understand how cancer cells respond to treatment and adapt over time.² The ability to quickly and accurately analyze large numbers of cells helps researchers identify patterns and relationships that might otherwise go unnoticed.²
Looking to the future, the Brunk Lab aims to scale up analysis capabilities to examine more cancer cell lines and patient tumors.¹ This expansion will provide deeper insights into cancer cell behavior and lead to more effective treatment strategies.² The automated analysis methods developed by the team will be crucial in managing the increased volume of data this scaling will generate and could revolutionize how scientists analyze cancer cells and develop targeted therapies.²
Through creative approaches to cancer research, combining computational methods with experimental biology, the Brunk Lab is helping to reshape our understanding of cancer cell biology. The team’s efforts advance knowledge of cancer cell behavior and develop new tools and methods that benefit the broader research community.² As the lab continues to expand its capabilities and research scope, its work promises to contribute significantly to the field of cancer research and lead to more effective treatment strategies.² The integration of computational and experimental approaches, coupled with advanced imaging techniques, positions the Brunk Lab at the forefront of modern cancer biology.²
1.Interview with Elizabeth Brunk, Ph.D. 02/18/2025
2.Goble, K; Mehta, A; Guilbaud, D; Fessler, J; Chen, J; Nenad, W; Ford, C. G; Cope, O; Cheng, D; Dennis, W; Gurumurthy, N; Wang, Y; Shukla, K; Brunk, E. Front. Pharmacology. 2025, Vol 15., 15:1516621.
By Kameryn Lloyd

Dr. William Polacheck fell into biological engineering by accident when he overslept and missed the curriculum session for pre-med undergraduate students, leading to a chance discovery of the field as it was the next available session. Through his time as an undergraduate and graduate student, Dr. Polacheck began to study microfluidics and mechanical engineering. As his love for both engineering and biology grew, he “began to see cells as living

materials” that could be manipulated the same as engineering tools. After training as a post-doctorate in cell biology, Dr. Polacheck started his lab, bringing the field of microfluidics to UNC-Chapel Hill in a different way: combining engineering techniques with a background in biology.
The unifying theme for the Polacheck Lab is how mechanical forces affect cells. In biology classes, we often focus on individual cell signaling pathways or proteins, but all of these systems and tissues are made up of cells that are structural. As people interact with their surroundings from simply poking their skin to their heart beating, they apply forces to the cells. Scientists have increasingly begun to consider how these forces affect cell function just as much as signaling pathways do. The Polacheck Lab creates materials that allow scientists to apply forces to cells to see how they respond. Specifically, the lab uses microprocessors, which are the small chips in your phone that create the electrical channels that run it. They are able to adapt the microprocessors so that instead of controlling the flow of electricity, the small chips control the flow of fluid at the scale of a single or several cells. They can then test how these cells respond to changes in fluid
flow. The lab also collaborates with other groups to apply these techniques to diseased states for cells. This is known as their vessel-on-chip 3D microfluidic model.
Most work to study blood vessels is in mice, even though their vasculature functions differ from humans at a basic mechanical level. While mice work is very important, diseases that are found in humans but not in mice—such as fibrosis—have been very hard to study and find treatments for. The vesselon-chip model provides the major advantage of being built using human samples. Researchers can take cells from patients with different diseases, create vessels from them, and study how they differ. This method of collecting patients’ cells and putting them in a flat 2D flask has been used for years. However, vessels in our bodies experience many forces, from the flowing fluid of blood to the stretching from the heart pumping—all forces a 2D model cannot capture. The 3D structure of the chip model functions more similarly to the native vessels and better captures the barrier separation between blood and tissue.
One of the challenges that Dr. Polacheck faces with his research is how to combine students with biology backgrounds with students with
engineering backgrounds. He has found that there are fundamentally different ways of thinking between biology and engineering and that individuals often work better in one way of thinking than the other. Originally Dr. Polacheck had wanted to take biologists and teach them engineering and vice versa; however, after starting his own lab, he found the opposite was more effective. Allowing each person to have their own area of expertise and then collaborating created better results. In many papers for his lab, almost every member is a coauthor, highlighting the need for collaboration while also maintaining individual expertise. Through this, Dr. Polacheck has found excitement in not understanding everything everyone is working on in his lab. His role as a principal investigator has evolved into trusting his lab members’ knowledge, asking the right questions, and offering the right advice to push their work forward into something even bigger.
The work from the Polacheck Lab has helped make the vessel-onchip model much more accessible to researchers and academic labs. Therefore, looking toward the future, Dr.
Polacheck is working on how to pivot and broaden the lab. One emerging area of research focuses on applying knowledge of blood vessel formation to vascularizing tissue, which involves growing functional blood vessels within engineered tissues. Organoids are 3D organ models that allow scientists to study organ development, disease progression, and drug responses in a controlled environment.2 However, a major limitation of current organoid models is their lack of a robust vascular system, which is essential for delivering nutrients, oxygen, and waste removal like real organs. Without proper vasculature, these models struggle to fully replicate the complexity of human tissues. Advancing vascularization techniques within organoids could greatly enhance their functionality, making them more realistic. The lab is currently collaborating with a genetic lab to work on vascularizing brain organoids. The next new area of interest is engineering dynamic tissues. Most experiments apply forces to cells by poking them once and then measuring them, even though most of these forces are cyclic in reality, like running and your

Figure 1. Image of a blood vessel in a microfluidic device. The cells used to fabricate the vessel express genetic mutations that are associated with a disorder known as vascular malformations. The orange color is cytoskeleton (filamentous actin) and the blue color is the nucleus. That these cells are invading the black space around the vessel is a sign that they are behaving much like the vasculature in patients with vascular malformations. Courtesy of Dr. Polacheck.
heartbeat. Dr. Polacheck hopes to adjust these methods to maintain signals more dynamically to better model the reality of vascular function.
From accidentally discovering biological engineering to pioneering the vessel-on-chip model, Dr. Polacheck has learned many lessons throughout his journey. One major lesson is that people who are successful scientists can be interested in anything. However, there are good and bad lab environments based on the individual, and being in the wrong environment can damper your excitement for science. Dr. Polacheck’s advice to undergraduates is to keep an open mind to the area of research they want to work on and prioritize finding an environment that “makes you excited to come in every day and do science.”1 After all, as Dr. Polacheck has seen, sometimes the best things happen when you least expect them.
1. Interview with Dr Polacheck, Ph.D 02/19/25
2. Yang, S., Hu, H., Kung, H., Zou, R., Dai, Y., Hu, Y., Wang, T., Lv, T., Yu, J., & Li, F. (2023). Organoids: The current status and biomedical applications. MedComm, 4(3). https://doi. org/10.1002/mco2.274
By Avery Sallean

Over the last decade, incredible advancements in technology and pharmaceuticals have allowed for patients with a variety of different neurological conditions to better manage their symptoms and improve their quality of life. But in certain conditions, including neuropathic pain, drug-refractory epilepsy, and essential tremor, available treatments are still falling short. Dr. Vibhor Krishna, a neurosurgeon-scientist at the University of North Carolina at Chapel Hill, is attempting to bridge this gap with his research in optimizing the use of an incisionless procedure known as Focused Ultrasound (FUS). This technology uses high intensity ultrasound waves to ablate, or lesion,

structures in the brain without the need for open brain surgery.1
Precise locations of therapeutic targets for FUS in the brain are determined with the use of MRI (Magnetic Resonance Imaging) guidance. MRI guidance provides clinicians with information about brain structures and temperatures and allows for real-time feedback. Surgeons begin by using low intensity ultrasound to perturb the target area but not permanently lesion it. They then record whether perturbing this area caused a reduction in patient symptoms and adjust the target area to provide maximal therapeutic benefit to the patient and minimal risk before switching to higher frequency waves.1 Dr. Krishna and his team studied the effects of utilizing FUS
to reduce the occurrence of tremors in patients with essential tremor, and recent findings from Phase 3 clinical trials have proven FUS to be a safe and effective treatment option for these patients.2 However, utilization of FUS to treat other neurological disorders is an area of research that is currently being explored by Dr. Krishna and his colleagues.
As both a clinician and a researcher, Dr. Krishna is passionate about discovering ways to optimize this surgical procedure and utilize it to treat neurological disorders. “I’ve always been excited about studying brain function,” Dr Krishna recalls, “and leveraging research to improve our treatments to have an impact for patient care”. After obtaining his medical degree


Figure 2. Focused Ultrasound. The above image represent a typical setup for a patient undergoing FUS therapy. The patient’s head is placed inside an MRI scanner while wearing a helmet containing the FUS transducer. This allows physicians to use guided MRI technology to ensure accurate targeting. Courtesy of Dr. Krishna.
from the All India Medical Institute in New Delhi India, Dr. Krishna obtained an M.S. from the Department of Epidemiology in the Harvard School of Public Health. From there, he went on to complete an internship at Creighton University Medical School, a residency at the Medical University of South Carolina, and a fellowship in Stereotactic and Functional Neurosurgery at the University of Toronto. Dr. Krishna now works as a board-certified neurosurgeon and associate professor at the University of North Carolina at Chapel Hill and is passionate about conducting research that improves the quality of life for
his patients. “We have been engaged in research around optimizing the surgical techniques with the underlying assumption that we can make our treatments highly individualized and develop steps to reduce side effects,” Dr. Krishna reports.1

In addition to finding ways to make FUS safer for patients, Dr. Krishna and his team are also exploring its utilization to treat diseases like glioblastoma, an aggressive brain cancer. For most types of cancer, a process known as tumor surveillance is possible. This occurs when a patient’s blood can be taken and cell-free DNA, produced by tumor cells called circulating tumor DNA (ctDNA), can be obtained and tested. This allows clinicians to detect tumor mutations, track how the composition of the tumor is changing, and even predict how the tumor might respond to treatment.3 In glioblastoma, however, the blood brain barrier, which is a filter made up of tightly packed cells lining the blood vessels that controls which substances enter the brain, prevents the exit of ctDNA into the bloodstream. Dr. Krishna and his team are exploring how temporarily opening the blood brain barrier in specific brain regions may allow for the exit of ctDNA into the bloodstream and provide a less invasive alternative than open biopsy to perform tumor surveillance in patients with glioblastoma. To temporarily open the blood brain barrier, microbubbles are injected into the bloodstream. Low intensity ultrasound is targeted at a region of the blood brain barrier near the tumor, and when these waves hit the microbubbles, they vibrate and expand, pushing apart the tight junctions of the cells in the blood brain barrier temporarily.4 While research into this potential incisionless tumor surveillance procedure is still in its early stages, Dr. Krishna is cautiously
Figure 3. Alternative FUS targets. The ventralis intermediate (VIM) nuclei of the thalmus is another therapeutic target that can be utilized to help treat patient tremors. Courtesy of Dr. Krishna.
optimistic about its potential use as an alternative to open biopsy. He is currently working with collaborators at the University of Maryland, the University of Toronto, Cornell University, and colleagues at the UNCUniversity of North Carolina at Chapel Hill to explore other uses for FUS and investigate ways to maximize its benefits.
In addition to his other projects, Dr. Krishna is excited about a new project he is conducting that will investigate how focused ultrasound can be used to treat drug-refractory epilepsy, which refers to a population of patients with epilepsy that don’t respond to medications or have experienced adverse side effects while taking them. In his new Phase 1 trial, Dr. Krishna will study the safety and efficacy of ablating the anterior nucleus of the thalamus, a brain region implicated in the seizure pathway. He is currently enrolling patients in this trial, and additional data will reveal if this can be a safe and beneficial treatment modality for these patients.
Exploring the uses of focused ultrasound as a therapeutic is an expanding area of research that will result in further optimization of this procedure. Important contributions from researchers like Dr. Krishna could lead to the use of focused ultrasound as a treatment modality for conditions like drug-refractory epilepsy or neuropathic pain, where current methods are not meeting patient needs.
1. Interview with Dr. Krishna M.B.B.S MS, 02/17/25
2. Rovinsky K. 2024b Jul 30. Bilateral Focused Ultrasound Shown to be Safe, Effective for Patients with Lingering or Severe Essential Tremor | Newsroom. Newsroom. [accessed 2025 Feb 7].
3. Telekes A, Horváth A. 2022. The Role of Cell-Free DNA in Cancer Treatment Decision Making. Cancers. 14(24):6115. doi:https://doi. org/10.3390/cancers14246115.
4. Lapin NA, Gill K, Shah B, Chopra R. 2020. Consistent opening of the blood brain barrier using focused ultrasound with constant intravenous infusion of microbubble agent. Scientific Reports. 10(1). doi:https://doi.org/10.1038/ s41598-020-73312-9.
By Fiona Yeung

Medical imaging—through methods such as CT scans and MRIs—is the backbone of modern medicine. They allow physicians to detect disease at an early stage, monitor the course of treatment, and giver wellinformed diagnoses. However, these imaging methods have inherent limitations. Image resolution is less than optimal, important information is lost, and repeated scans expose patients to potentially harmful radiation.1
To fight against these limitations, applied mathematics professor Dr. Yifei Lou uses mathematical methods to enhance the efficiency, safety, and accuracy of medical imaging. She studies how math can complete the missing pieces when data is incomplete, producing clearer images with fewer scans.1
One of the significant challenges in CT imaging is when the number of scans is decreased to reduce exposure of a patient to radiation. While this is good news from a health perspective, it creates gaps in the data and ambiguity in the reconstructed image. Mathematically, it creates what’s known as an “underdetermined system”—a scenario where many possible solutions could fit the same incomplete information. Dr. Lou gets around this by using mathematical and anatomical knowledge to guide image reconstruction. As body tissues tend to be smooth, homogeneous areas, it can be used to assist computers in recreating more accurate and realistic images. Compressed sensing and total variation minimization are examples of algorithms that assist in filling in missing details and creating high-quality images from low scan data.2

Having joined the University of North Carolina at Chapel Hill in 2023, Dr. Lou has collaborated with professionals from many different disciplines. An ongoing collaboration is with computer scientist Dr. Guorong Wu, who is in the psychiatry department. Although such interdisciplinary collaboration is valuable, it is not without communication challenges. “I need a translator,” Dr. Lou jokes, acknowledging the
difficulty of translating mathematical jargon into medical jargon. However, she takes part in cross-disciplinary meetings and sees the ability to communicate across disciplines as an integral part of her job.1
Dr. Lou doesn’t just specialize in imaging. She also performs EEG signal processing, which attempts to decipher brain function by interpreting electrical signals measured from the scalp. Similar to CT imaging, EEG data is incomplete and noisy. Dr. Lou uses mathematical techniques like Bayesian inference– which uses probability–and inverse problemsolving– which involves working backward from the data–to invert these signals back to their origin in the brain. They sharpen our knowledge of neurological function and provide the foundation for investigation into neurological and mental disorders.3
Her mathematical research is also useful in monitoring the environment. Through her remote sensing¬– which is how we study the Earth from a distance using satellites and drones– Dr. Lou examines hyperspectral imaging data that are gathered by satellites. The images capture hundreds of wavelengths of light—far more than visible light—and offer precise information on the surface of the Earth.4
One of the greatest difficulties is resolution: a single pixel in a hyperspectral image can define anywhere from 3 by 3 meters to even more extensive areas, routinely blending signals from multiple distinct materials such as vegetation, soil, and water. To untangle the ambiguity, Dr. Lou uses

of the extended brain source estimation architecture with unrolled optimization techniques, providing a glimpse into complex methods for EEG source imaging. Courtesy of Dr. Lou.

Figure 2. The application of graph-based active learning techniques for hyperspectral unmixing, portraying how the techniques improve the identification of material components in hyperspectral images. Courtesy of Dr. Lou.
spectral unmixing, which separates the blended data into single materials. Methods such as non-negative matrix factorization (NMF) breaks down the data into simpler parts that only contain positive values, which helps identify the basic components—like different materials—in satellite imagery. Sparse coding builds on this by assuming that only a few
Dr. Lou points out that the ability to explain complicated ideas is as valuable as possessing them.
materials are present in any given pixel, allowing for a cleaner and more precise separation. Together, these methods extract the unique “signatures” of each material, making it easier to accurately interpret complex environmental data.5
Along with her research, Dr. Lou is also heavily involved in data science education. As a faculty member in UNC’s School of Data Science, she is playing a role in developing new undergraduate and graduate programs. The programs feature an accelerated 18-month online master’s program and a growing undergraduate program with both Bachelor of Arts and Bachelor of Science tracks.1 She aims to have students graduate with a solid theoretical background along with practical skills for the work force.
Dr. Lou points out that the ability to explain complicated ideas is as valuable as possessing them. “In the Math Department, we’re doing three-minute lightning talks,” she says—short lectures that attempt to boil down intricate research into understandable language. This is in the service not just of collaboration but of career development. Dr. Lou says her students are moving on to find employment at elite tech firms like Google and Facebook. The program also collaborates with industry giants like General Electric (GE) to give students an opportunity to apply knowledge to realworld research problems through internships and capstone projects.1
While deep learning and artificial intelligence are receiving increasingly more attention in medical imaging, Dr. Lou also mentions a few practical limitations. These models need vast amounts of data to learn from—data which are
tricky to obtain in healthcare due to privacy issues. Furthermore, the computational infrastructure of most universities is not apt to facilitate these types of large-scale applications of AI. Therefore, Dr. Lou is working on hybrid methods, such as physics-informed neural networks, which combine classical mathematical models with machine learning to make precise predictions from smaller, more manageable datasets.6
Looking forward, Dr. Lou continues to be dedicated to the growth of data science education and more dynamic interaction between industry and academia. She also focuses strongly on educating fundamental technical skills to thoroughly prepare her students for the future demands of the technology-driven business world.1
Her own interest in math started early, thanks to the influence of her mother, who was a mathematician. “Female representation in STEM remains an issue,” she notes. “Having a role model made me think that women can do math.” Now, as a professor and mentor herself, she is returning that experience—urging female students to have confidence in themselves and pursue careers in science and technology with confidence.1
1. Interview with Dr. Yifei Lou
2. Lustig, M., Donoho, D., & Pauly, J. M. (2007). Sparse MRI: The application of compressed sensing for rapid MR imaging. Magnetic Resonance in Medicine, 58(6), 1182–1195.
3. Grech, R., et al. (2008). Review on solving the inverse problem in EEG source analysis. Journal of NeuroEngineering and Rehabilitation, 5(25).
4. Bioucas-Dias, J. M., et al. (2012). Hyperspectral unmixing overview: Geometrical, statistical, and sparse regression-based approaches. IEEE Journal of Selected Topics in Applied Earth Observations and Remote Sensing, 5(2), 354–379.
5. Lou, Y., & Zhuang, Y. (2015). Manifold regularized sparse NMF for hyperspectral unmixing. IEEE Geoscience and Remote Sensing Letters, 12(6), 1241–1245.
6. Raissi, M., Perdikaris, P., & Karniadakis, G. E. (2019). Physics-informed neural networks: A deep learning framework for solving forward and inverse problems involving nonlinear partial differential equations. Journal of Computational Physics, 378, 686–707.
By Selinda Zhu
Mathematics can seem like a foreign language to many, with its complex equations and abstract concepts.
But if we dig a little deeper, we realize that math is not only about numbers or solving for x — it’s about understanding the structures around us. One of the most intriguing branches of math, geometry, is a perfect example of this. As Dr. Arunima Bhattacharya, an assistant professor of mathematics puts it, “geometry blends rigorous logic with deep intuition, offering a natural way to understand space.” 1 This combination allows us to approach problems with both precision and creativity, making geometry a powerful tool for exploring the world. The research of Dr. Bhattacharya connects the study of geometry and partial differential equations with physics, engineering, and material science, helping us understand things that are invisible to the naked eye, like how materials bend or the flow of shapes over time.
Geometry is often thought of as the study of shapes like triangles, circles, and squares. And while that is true, the geometry Dr. Bhattacharya studies dive much deeper. Imagine crumpling a piece of paper — over time, it will gradually try to flatten out. Or picture bending a straw; it will slowly straighten itself out when let go. These are simple, everyday examples of what Dr. Bhattacharya studies: How shapes bend and evolve over time, specifically through something called the Lagrangian mean curvature flow.

Dr. Arunima Bhattacharya
In this research, the “flow” refers to how shapes try to “smooth” out their curves. In simpler terms, it’s like smoothing out a wrinkle in a shirt by gently pulling on the fabric. Surfaces in Dr. Bhattacharya’s study will adjust to minimize the bends or irregularities, eventually trying to become smoother and minimize their area. This behavior is a key part of what we understand as mean curvature flow- where mean
curvature is the average of how much the surface bends at each point.
To study these complex shapes and their structures, Dr. Bhattacharya uses a powerful mathematical tool called nonlinear partial differential equations (PDEs). While these words might sound intimidating, they are actually a way to describe how things change over time and space, much like how a piece of ice melts in a warm room. These equations help describe how things evolve, and they are essential for understanding everything from physics to engineering.
To break it down, there are two broad classes of PDEs: Linear and nonlinear. Linear PDEs are simpler, with equations that behave predictably. For example, imagine having an ice cube— the rate at which the ice melts at each point are proportional to the heat at that point. But fully nonlinear PDEs, which are what Dr. Bhattacharya works with, are much more complicated. They involve equations where the rate of change can depend on multiple factors at once, making the solutions harder to predict. For example, having an irregular chunk of ice, some parts might melt faster or slower, and these changes can affect other parts of the ice in unpredictable ways.
One of the fully nonlinear PDEs that Dr. Bhattacharya

Figure 1. The Jacobian matrix of the derivatives of a function with respect to x1, x2, ..., xn is called the Hessian H. Courtesy of Hessian Matrix.

Figure 2. A Whitney sphere developing a type-II singularity under Lagrangian mean curvature flow, rescaling to a grim reaper curve times a flat Lagrangian plane. Courtesy of Savas-Halilaj, Andreas.; Smoczyk Knut. (2018). Lagrangian mean curvature flow of Whitney spheres.
studies is the Lagrangian mean curvature equation and its associated flow. This flow describes how the bending of a surface evolves over time. It involves the arctangent of the eigenvalues of the Hessian matrix (Figure 1)— a mathematical quantity that measures how these surfaces bend in different directions. The equation looks at how these bending properties change as the surface evolves, and this is what allows Dr. Bhattacharya to predict how surfaces will behave over time.
“It is this mystery that makes mathematics so compelling: A neverending exploration of the unknown, where the answers are waiting to be uncovered, one step at a time. ”
The term Lagrangian refers to the type of surface that Dr. Bhattacharya is studying. The Lagrangian surface (Figure 2) is a shape that exists in a space that is twice its dimension. For example, imagine taking a pencil and drawing a curve on a piece of paper. The curve is a 1-dimensional object (a line), but it lives on the paper (a 2-dimensional surface). This kind of surface behaves differently from ordinary shapes and requires a unique set of tools to study. These surfaces are important in geometry because they appear in many areas of physics, especially in theories about the construction of our physical universe.
The mean curvature part refers to on an average how much a surface bends or how curved it is at each point. Think of it like the surface of a hill. The steeper the hill, the greater the curvature. Rolling a ball on the hill would naturally cause it to move toward the flattest area, as that’s where the surface has the least curvature. The same idea applies to shapes in Dr. Bhattacharya’s research. These surfaces will “flow” toward areas of least curvature, smoothing out the bends over time, or they might crumble into singularities- where pitches collapse like black holes.
The key to Lagrangian mean curvature flow is that it is trying to minimize the volume of the lagrangian surface —
imagine trying to shrink the surface to be as small as possible while also reducing its curvature (bending). This process is governed by a parabolic PDE, a type of equation that helps describe the gradual and smooth change of a surface.
At first, studying abstract surfaces and mathematical equations might seem disconnected from everyday life. However, Dr. Bhattacharya’s work has important real-world applications in fields like physics, material science, and engineering. By understanding how surfaces evolve, we can better predict how materials will behave under stress, such as the bending of metal in construction or the flow of air over an airplane wing. This knowledge helps engineers design safer and more efficient structures.
Moreover, the insights from Lagrangian mean curvature flow are also essential in theoretical physics, especially in understanding the structure of the universe. Some theories, such as string theory, rely on these complex geometric structures to describe the forces that govern everything from gravity to quantum mechanics. The abstract concepts Dr. Bhattacharya studies may one day provide the key to unlocking new discoveries in physics, much like how the development of geometry and algebra centuries ago led to the technologies we use today.
As Dr Bhattacharya describes it, “mathematics is like a puzzle” 1 — its pieces are hidden and waiting to be discovered. The challenge lies not only in putting them together, but in unravelling the mystery of what they are, how they fit and what they reveal. It is this mystery that makes mathematics so compelling: A never-ending exploration of the unknown, where the answers are waiting to be uncovered, one step at a time.
References
1. Interview with Arunima Bhattacharya, Ph.D., 2/21/2025
2. Bhattacharya, A.; Mooney, C.; Shankar, R., arXiv 2022, 2205, 13096.

Some of the biggest scientific innovations have come from studying the smallest creatures. Depending on the research, scientists choose model organisms that best suit their needs. Many might think of mice or frogs for genetic studies, one organism that has proven invaluable in understanding chromatin architecture, and is surprisingly similar to humans, is the Drosophila melanogaster, or fruit fly. The aforementioned genetic similarity between fruit flies and humans makes them wonderful candidates for

chromatin studies. Chromatin describes the mixture of DNA and proteins that make chromosomes in eukaryotic cells. Typically, these long strands of DNA are wound up very tightly around proteins called histones. These histones are vital for gene regulation and specifying which genes are turned on or off for cellular function. Dr. Robert “Bob” Duronio and his team aim to use histone manipulation as a tool to explore how turning genes on and off influences gene expression, cell functioning, and subsequently organisms as a whole.
Dr. Duronio is a Professor of Biology and Genetics at the University of North Carolina at Chapel Hill, where he also serves as Chair of the Department of Biology and is a member of the Integrative Program for Biological and Genome Sciences. With 28 years of experience at UNC-Chapel Hill, his research has focused on the developmental control of the cell cycle with one current emphasis: histones. Although Drosophila are distant relatives to humans, they are ideal for genetic research for a number of reasons. One extremely important point is that histone proteins in a fruit fly are nearly identical to the histone proteins in humans.1 Many human genes that act
on chromatin and other organisms were discovered in fruit flies, so fruit flies have been a leading experimental organism in the chromatin field. As seen in Figure 2, when compared to other models (zebra fish, mice, frogs, and roundworms), fruit flies displayed high identity, or the percentage of amino acid sequence similarity between histones of different species. For example, the identity of the histone tails were: 88.5% (H2a), 85.7% (H2b), 99.3% (H3), and 99.5% (H4).
Furthermore, the replication-dependent (RD) genes that are responsible for encoding histones vital to DNA replication are commonly found across many loci, or different genetic locations, in a single genome. In fruit flies, however, these RD genes, genes that are primarily expressed during the cell cycle and replication, are found in a single locus, which makes it simpler to delete or manipulate the wildtype, or normal genes, with a new genetic construct called a trans-gene. Genetic manipulation has long been a key approach in developmental biology for studying mutated genes and their effects on animal development. As Dr. Duronio explains, “Without proper regulation of the access to the information encoded in DNA, then you can’t control

Figure 2. Comparison of replication-dependent histone genes and proteins among metazoan model organisms. Figure courtesy of Duronio et al.
when you turn genes on that you need at the right time and place or turn them off to make all the different cell types”.1
Advancing this approach, Dr. Duronio and his team first focused their sights on the HisC locus on chromosome 2L: the single locus in which all five RD histone genes are clustered in fruit flies. This locus contains approximately 100 short tandem repeats of a five kilobase (kb) histone gene unit. Essentially, all the genes responsible for producing histone proteins are arranged in repeating units of approximately 5,000 nucleotide base pairs—the basic building blocks of DNA—making it an ideal target for genetic manipulation. Using CRISPRCas9, a precise gene editing system, the team was able to remove all histone genes within the fruit fly. The deletion was confirmed using a transgene containing a red fluorescent marker that was introduced in place of the original RD histone gene sequence. This artificially introduced gene allowed the team to visually track the absence of histone gene expression. Unsurprisingly, this deletion and insertion yielded fruit flies without any histones. Histones are vital for DNA compaction, gene expression, and replication, so the absence of these proteins made the flies non-viable, or unable to survive.
The next step to this process was to rescue histone function. Once again
using the editing system CRISPR-Cas9, they engineered a plasmid, a small and circular extrachromosomal DNA molecule, to contain a synthetic histone gene array for insertion. To integrate the synthetic histone gene array into the fly genome, the team used, ΦC31 recombinase, a site-specific recombination system that facilitates targeted gene insertion at predetermined locations. Initially, these genes were inserted ectopically, or in a position where the gene is not normally expressed. With time, the team was able to insert the engineered transgene where the wildtype gene originally was and minimizes any factors that may impact gene expression. These embryos were screened during development to determine whether this integration was successful. Remarkably, these modified fruit flies were viable and developed normally without the wildtype HisC locus.1, 2
The improved approach to mutating, reintegrating, and tracking these synthetic histone genes is an exciting new development for those within the chromatin community. Another benefit is the platform’s backward compatibility with previously existing systems and techniques, such as Golden Gate cloning technologies. This technique uses a precise “cut and paste” like method with proteins called
restriction enzymes to cut DNA at specific sequences before sticking the fragments together using another protein called DNA ligase to create the newly designed strand of DNA.2
A major surprise within this project was that all 100 deleted histone genes were successfully replaced by the insertion of only 12 histone transgenes. Furthermore, fruit flies are diploid organisms and have two copies of each chromosome, so a total of 200 histone genes were deleted over 2 chromosomes. This means that approximately 6% of the endogenous histone genes are required for normal histone functioning.2 While 12 genes seem comparatively small against a total of 200 genes, inserting said genes proved an arduous process. Individually, genes are small and easy to create and insert mutations but begin to snowball in size when cloned. A single histone multimer, a gene unit encoding five polypeptide chains, is 5kb long. Now, multiply that value by 12 to create all necessary gene units and that creates a DNA chain that is 60 kb long. Adding onto that is the plasmid vector to carry those genes bumps that length up to around 70 kb, or 70,000 base pairs of DNA. Suddenly, inserting 12 transgenes seems much more difficult.1
Reiterating their immense importance, Dr. Duronio makes the statement that, “Histone proteins package our genome and regulate access to the information encoded in our DNA and therefore control all biological processes”.1 He encourages the general scientific community to use and build upon the system in hopes of unraveling the mysteries encoded in DNA.
1. Interview with Dr. Duronio, Ph.D. 02/03/25
2. Duronio RJ. 2024. Redesigning the Drosophila histone gene cluster: an improved genetic platform for spatiotemporal manipulation of histone function. Genetics. 228(1):iyae117. doi:10.1093/genetics/iyae117.
By Brantley Aycock

Sleep: you can never seem to get enough. While adults should get between seven to nine hours of sleep a night, the need for sleep increases as age decreases. Teenagers need eight to 10 hours, young children need 10 to 13, and infants need 12 to 16 hours of sleep a day.1 In fact, babies’ brains grow and develop while they sleep, giving sleep a critical role in their physical, mental, emotional, and social development.2 Due to this importance, issues with falling or staying asleep can disrupt brain development. An important factor that affects a child’s quality of sleep is their parent’s parenting style.
To study this, Dr. Cathi Propper set out to investigate how parental behavior affects children’s sleep.3 Dr. Propper is a Principal Investigator and Associate Professor at the University of North Carolina at Chapel Hill. She first earned her Ph.D. in Developmental Psychology from Duke University.2 Her initial research interests in human development were in adolescent family and peer relationships, then moved into early childhood research, then finally settled with infancy and prenatal research.2 She ultimately realized that our environments and experiences as early as the prenatal period can have
effects into other life stages.2
In a study from 2022, Dr. Propper and colleagues found that harshintrusive parenting, or parenting that includes excessive criticism or punishment, detected when the baby was 6 months old, led to sleep problems in children at 18 months.3 In addition, persistent sleep problems at 18 months led to aggressive behavior in children at kindergarten and second-grade age. This finding fits with current literature, as harsh-intrusive parenting is associated with behavior problems and decreased ability to self-regulate, or control your own thoughts, emotions, and behaviors.

Dr. Cathi Propper
An explanation for sleep problems as a result of harsh-intrusive parenting is that continuous criticism disrupts a child’s development of self-regulation, leading them to externalize their challenges and therefore act out aggressively.3
Dr. Propper and researchers identified parenting styles by observing parent and child interactions when the two were given a playful task to complete together.3 Sleep problems, aggression, and attention were additionally reported by parents and teachers via a Child Behavior Checklist. Child attention was not predicted by sleep, but children of families with lower income-to-need ratios showed lower attention spans.3
Although the Child Behavior Checklist is a convenient and costeffective data collection tool, Dr. Propper also measures biological markers in her research whenever relevant.2 Measurements may include taking magnetic resonance images (MRIs) to monitor brain activity and tracking heart rate to investigate the autonomic nervous system – the system that regulates things like blood pressure, breathing, and digestion. Additionally, collecting hair, saliva, urine, and fecal samples can help measure the stress hormone cortisol, inflammation,
exposure to outside chemicals, and the microbiome, respectively.2 A person’s microbiome is the collection of microbes, like bacteria, fungi, and viruses, that naturally live in the body. These biological markers are important to collect. Dr. Propper says when she asks a subject how stressed they feel, they could be feeling less stressed than usual, so they report low stress. But maybe the subject’s usual stress levels are high, so a low-stress day for them is still high-stress on a typical scale.2
The younger the participant, the fewer the variables impacting their participation in a long-term behavioral study, therefore it is most effective when researchers can follow participants from the prenatal period into adulthood to track relationships


between determinants and health.2 Because of this, the biggest obstacle in developmental science is ensuring the long-term engagement of participating families.2 Sustained and consistent data collection is the best way to observe and understand changes in subjects over time, but families may get busy or become uninterested, or they can move away.
“We can start to learn how to undo that damage and prevent it in the future.”
Dr. Propper’s research often surprises her.2 In a 2019 study, her team found that infants whose mothers smoked cigarettes while pregnant slept longer and more deeply than infants whose mothers did not smoke.2 On the surface, longer and deeper infant sleep seems like a good thing. However, as the researchers looked into these results, they learned that such deep sleep can be harmful to infants. Babies who sleep longer and more deeply may not be able to wake up from hunger cues or other signs of need or stress, putting their health at risk.2
The biggest takeaway from Dr. Propper’s research is the importance of understanding how our surrounding environment impacts our mental, emotional, and physical development.2 Studies like Dr. Propper’s research into
parenting, sleep, and behavior can help parents better understand how they affect their child’s growth and what they can do to facilitate it.3 “When we can see and understand how all these things along the way may be hurting or helping, we can start to learn how to undo that damage and prevent it in the future.”2
1. National Institute of Health. How Much Sleep is Enough?. https://www. nhlbi.nih.gov/health/sleep/howmuch-sleep. (accessed March 16 2025)
2. Interview with Cathi Propper, Ph.D. 02/20/2025
3.ropper, C.B.; McLaughlin, K.; Goldblum, J.: Camerota, M.; Gueron-Sela, N.; Mills-Koonce, W.R.; Wagner, N.J.; Sleep Health 2021, 8, 1-7.

Mother mice are taking “a mother’s intuition” to a whole new level through the use of their auditory cortex (AC), which processes auditory information. The AC uses the combination of multiple senses to enhance the processing of certain social sounds in mice. For maternal and surrogate mice, sexually naïve female mice that have been cohoused with a mom and her pups, the most important use of this skill is to identify their young. Simply put, maternal mice are known to use their sense of smell paired with cries from their young (ultrasonic pup vocalizations) to identify them. While multisensory interactions involving the AC have been studied, more specific questions remain regarding the link between the olfactory and auditory systems regarding raising mice offspring.
Dr. Alexandra Nowlan is a teaching assistant professor at the University of North Carolina at Chapel Hill, with a PhD from Cold Spring Harbor Laboratory School for Biological Sciences, who led research that answers questions connecting the olfactory and auditory systems of mice.1 Maternal behavior in mice particularly intrigues Dr. Nowlan because these behaviors are innate, meaning that mice can increase their own survival rates without any training. Mice rely on their sense of smell to identify their young, communicate social information, and avoid predators. However, for a complete survey of their environment, their behavior is influenced by more than just smell.

The reaction to various observed scenarios in the environment is often the product of multisensory pathways in an organism’s brain. If information input was reduced to a single signal, the organism would lack the context and details to accurately inform their reaction. Dr. Nowlan uses the example of a fire alarm going off, which may annoy people but not disturb them enough to rush out the door.1 However, hearing a fire alarm combined with the smell of smoke would elicit a different, and more informed, reaction. Following this
By Julianna Bryant
analogy, Dr. Nowlan says, “Mice, like humans, also use multimodal signals [which are] very important to convey important social information and respond with appropriate behavior.”1 Dr. Nowlan’s research relies on this foundation of multisensory processing, or “cross-modal interaction”, to observe maternal behavior in mice and the use of these multimodal signals in communication.
Newborn mouse pups are vulnerable and very dependent on their mothers. In the case that they are separated from the nest, their chances of survival decrease and they call for their mother using ultrasonic vocalizations. Newborn pups also carry a unique odor that mothers and surrogate mothers depend on to communicate with and retrieve their pups. Both senses of smell and sound are vital for a mother-pup relationship and the survival of mice, and Dr. Nowlan’s research clarifies the link between the two.
Dr. Nowlan’s study, Multisensory integration of social signals by a pathway from the basal amygdala to the auditory cortex in maternal mice, began with injecting a retrograde, or backward-moving, viral tracer (AAVrg-CAG-tdTomato) into the left auditory cortex for neural tracing experiments.2 The tracer includes a fluorescent protein that highlights target neurons red. This was to identify the pathways capable of transporting olfactory information to the auditory cortex. Through this method, axons that project into the auditory cortex take up the virus, which contains the gene encoding the fluorescent protein. This allows for inputs to the AC to be visualized. A significant projection was found in the basal amygdala, a part of the amygdala, the emotional control center of the brain, in the medial temporal lobe of the brain (Figure 1). The basal amygdala is involved in memory, reward processing, and tying sensory stimuli to emotional significance. Dr. Nowlan captures the thrill of scientific discovery, saying, “we know that the auditory cortex projects into the basal amygdala… the fact that there is a reciprocal projection is…not what we were expecting.”1
With the focus now on the basal amygdala, fiber photometry calcium imaging experiments were used to label the neural projection from the basal amygdala to the auditory cortex as a participant mouse was given different smells.2 Calcium imaging experiments work by expressing a genetically encoded calcium indicator using a modified

Figure 1. (A) Retrograde tracing of the viral fluorescent tracer from the auditory cortex reveals cell bodies labeled within the basal amygdala, (B) throughout the ipsilateral AC, (C) contralateral AC, and (D) medial geniculate body, part of the thalamus where the brain receives sensory information. Courtesy of Dr. Nowlan.
fluorescent protein that is fused to a calcium binding element (Figure 2). This process is called optogenetic activation.
When calcium enters a neuron, it binds to the protein, causing a conformational change that allows the fluorescent protein to emit green light. Calcium influx determined whether or not the projection neurons identified in the tracing experiment were capable of responding to olfactory stimuli. This procedure was repeated as a surrogate mother tried to locate her pup and the results showed that cell activity increased during the search and then ended abruptly upon contact (Figure 3).
One of the final parts of this research investigated whether optogenetic activation of this neural pathway could influence auditory processing.2 While the mice were under anesthesia, auditory neurons in the AC were recorded as optogenetics was used to activate the projection. It was found that changes in auditory responses and the direction of the change depended on if the mouse was a mother and cohabitation with pups.
The next step for Dr. Nowlan’s research will be conducted by Hoda Tromblee, a graduate student in Cold Spring Harbor Laboratory’s Shea Lab. The focus will shift to the termination of the BA-AC projection when the surrogate reaches the pup along with what causes the influence of this circuit on auditory processing to shift after maternal experience. Further research should also be conducted to see if fear in mice mothers upon

Figure 2. (A) represents the setup for selectively labeling BA-AC projection neurons with GCaMP6s (a genetically encoded calcium indicator) and recording calcium activity. (B) displays the strategy for head-fixed recording of calcium while mice were exposed to monomolecular odorants or pup odor. Courtesy of Dr. Nowlan.
separation from their pups is causing basal amygdala activity. There are many unanswered questions about the rewarding nature of these neural signals, but this project is a stepping stone to learning more.

Figure 3. This figure consists of a heatmap in the upper panel, which depicts the average response to pup search that ends when the pup is found. Each row shows the mean response to a pup encounter. The black and white panel plots the mean Z-dFF for the mice in the study in relation to the time of pup contact. Courtesy of Dr. Nowlan.
No matter what the next steps are for this research, Dr. Nowlan has elevated the conversation of multisensory integration. In the future, there is potential to apply parts of this research on neural pathways to individuals with autism spectrum disorder. Many individuals with autism find it challenging to interpret social cues. Research on how our brains support social-emotional processing can provide greater insight into how these neural circuits differ between individuals with and without autism and how this influences their response to social cues. The complexity of these systems and the interconnectedness of our senses create not only our perception, but also our ability to connect with the world around us. More insight into these systems will help people regulate their senses and better understand their relationship with their surroundings.
1. Interview with Dr. Alexandra Nowlan, Ph.D. 2/20/2025
2. Nowlan, A. C.; Choe, J.; Tromblee, H.; Kelahan, C.; Hellevik, K.; Shea, S. D. Multisensory Integration of Social Signals by a Pathway from the Basal Amygdala to the Auditory Cortex in Maternal Mice. Curr Biol 2024. https:// doi.org/10.1016/j.cub.2024.10.078.
By Britney Munguia
Eating more, [being] skinnier, living longer—all the things we want in life,” says Dr. Matthew Ulgherait, and he may have found the secret formula to do just that.1 Dr. Ulgherait began his undergraduate studies at Drexel University, where he found his passion for lab work. He went on to get his PhD in Biochemistry and wrote his dissertation on aging. “Why do we break down…as we get older?” was the question that propelled his research in extending lifespans.1
Around 2019 to 2020, time-restricted (or intermittent) feeding/fasting—TRF (or IF)—was “very hot”, as Dr. Ulgherait puts it. It was known that restricting food intake at certain times of the day could extend mouse lifespans, reduce diabetes and bodyweight, and improve glucose tolerance.1, 2 But little was known about the mechanisms behind it.

Since time-restricted fasting relies on when you eat, and not nutrient or caloric content, it’s suspected to deal with circadian rhythms: the natural, 24-hour cycle changes the body undergoes to regulate bodily functions like sleep and wake patterns, body temperature, and hormone release.3 As humans evolved on a rotating planet, relatively getting 12 hours of day and 12 hours of night, certain genes evolved to turn on or off during the day, and vice versa during the night.1 Many metabolic genes, those that help convert food into energy, are up-regulated during the day and go off at night, as there’s supposed to be less activity when the body is meant to be sleeping. We see this reflected in night workers.

Figure 1. The three time-framed diets Dr. Ulgherait tested. Courtesy of Ulgherait M. “You are when you eat: TimeRestricted Feeding/Fasting and Lifespan Extension in Drosophila.”
Since they eat at the incorrect evolutionary time—during the night—no metabolic processes occur because the metabolic genes are inactive.1 This “flip” in circadian schedules is linked to increased risk of diabetes, obesity, and certain cancers.1 Intrigued, Dr. Ulgherait began thinking about the connections between metabolism and circadian rhythms.
Dr. Ulgherait began with testing different TRF schedules on Drosophila, also known as fruit flies. The schedules included ad libitum (ad lib.) (24-hour access to food), nightbias TRF (fasting from approximately 4 PM till 6 AM), and daybias TRF (circadian rhythm switched; fasting through the day (approximately 4 AM to 6 PM) and eating at night). He grew his control and experimental populations of 200-300 flies in controlled environments: sealed, 25 degrees Celsius, 60% humidity, and free from as many pathogens as possible. Over a period of time, he simply “counted the dead”. 1
Results showed that under night-bias TRF, the flies’

lifespans were extended by 15-20%.1-2 In day-bias TRF (shiftworker diet), there was no life-span extension. The flies on the night-bias TRF were also eating 20-25% more than the flies on the ad lib. diet, yet they were leaner.1-2 Not only were flies that fasted throughout the night living longer, but they were healthier and skinnier.
Dr. Ulgherait then asked which genes controlled by the circadian clock are being affected by night-bias TRF. Through experiments, he obtained a lead. He noticed the recycling of protein aggregates. As humans, and fruit flies age, the decrease in the ability to move is caused by the accumulation of big protein aggregates, or protein clumps, within muscle tissue. Under night-bias TRF, these aggregates are reduced by 60-70%! When getting rid of these aggregates, autophagy comes into play. Autophagy is the cell’s way of dealing with unwanted products by reusing them to build new molecules.1, 2 Lysosomes, a cell organelle whose job is to break down molecules, can be seen co-localizing if there’s lots of autophagy going on. The term co-localizing refers to the “grouping up” of a substance. In this case, many lysosomes pile up within the muscle tissue to reduce protein aggregates. Dr. Ulgherait tested whether ATG8, the key autophagy protein, was affected under different TRF schedules. He saw that there was a stronger bump in signaling under night-bias TRF. This shows that when you’re restricting yourself from eating beginning late afternoon and on through the night, your body is under higher autophagy levels, causing more lysosome co-localization, which breaks down the protein aggregates within your muscle tissue.
Some humans, like some fruit flies, don’t have a circadian clock; they’re better known as “night owls”. In these circadian mutants, we don’t see much lysosome colocalization, meaning there’s less “autophagy going on”.1 This proves that autophagy is a key component in circadianregulated processes involved in lifespan extension. Using

Figure 2. The lifespan extension that comes with daybiased fasting, in comparison to ad lib and night-biased fasting. Courtesy of Ulgherait M. “You are when you eat: Time-Restricted Feeding/Fasting and Lifespan Extension in Drosophila”

Figure 3. (Left) The protein aggregates within muscle tissue normally, and (right) the decreased protein aggregates when under iTRF. Courtesy of Ulgherait M. “You are when you eat: Time-Restricted Feeding/Fasting and Lifespan Extension in Drosophila”
CRISPR (Clustered Regularly Interspaced Short Palindromic Repeats), a technology used to modify DNA in living organisms, Dr. Ulgherait turned on autophagy genes during the “right time” of day, mimicking night-bias fasting, forcing the increase of autophagy signaling even when the flies were eating whenever they wanted (not fasting).2 When graphed, only when the over-expression of autophagy genes was forced, did they get the same result as the night-bias TFR— meaning an extension in lifespan. What happens if you undergo night-bias TRF on top of genetically overexpressing autophagy genes? Though we would expect an even higher extension of lifespan, there wasn’t much of a difference. Whether you’re under night-bias TRF or genetically modified your genes to mimic the effects of night-bias fasting, your circadian and autophagy isolations are heightened, which results in more clearance of protein aggregates with age. This is what increases lifespan by 15-20%. As more is discovered on how DNA can be manipulated to mimic gene signaling, longer life extensions could be obtained without having to do any fasting at all.
1. Interview with Dr. Matt Ulgherait, PhD. 2/27/25
2. Ulgherait et al. Nature, 2021. https://www.nature.com/ articles/s41586-021-03934-0
3. Regmi, P.; Heilbronn, L. K. PMC 2024, 23.
4. Circadian Rhythms. https://www.nigms.nih.gov/education/fact-sheets/Pages/circadian-rhythms#:~:text=Study%20Circadian%20Rhythms-,What%20Are%20Circadian%20Rhythms%3F,and%20temperature%20also%20 affect%20them. (accessed February 28th, 2025).
By Daniela Danilova

Illustrated by Spoorthi Marada
Black bile, yellow bile, phlegm, blood. As far as the Greeks knew, these were the essential components of the red liquid that courses through our veins. Like the classical elements of the physical world, these so-called “humors” were believed to be the foundation of human being. Hippocrates himself was adamant that they were the source of our all our pains and our health, that the latter could only be obtained if these substances were present in perfect proportion. He wasn’t completely wrong. From an early age, humans have had an obsession with organization. Though our catalog of biological ingredients has expanded quite a bit, our desire to assign wellness based on this vital concoction has persisted. Dr. Karin Leiderman of the Leiderman Research Group is no stranger to this hunt.
As an undergraduate, Dr. Leiderman found herself bouncing between majors, intending at first to pursue the medical route before realizing her deeper affinity for mathematics. The latter eventually won this tug of war, yet she still felt a phantom pull towards the study of life. Unaware of the existence of a middle ground, she was at a crossroads; but thankfully, an experience in graduate school began to ease the tension. Her mathematics professor was intrigued by her natural science background and recruited her as a research assistant at a newly-established center for modeling and biology. Her first project there tackled receptor clustering in membranes using spatial statistics. Despite the novelty of this perspective, she realized that statistical processes didn’t quite satisfy her growing quantitative curiosity. The seed, however, was planted; and it was a program for women in math at Princeton University that allowed it to take root. That summer, the program’s theme was biological fluid dynamics; and, suddenly, Dr. Leiderman had found her spark. Her subsequent Ph.D. at the University of Utah continued to explore these biofluids, analyzing the effect of blood flow on clotting via numerical models.


1. Reactions included in the mathematical coagulation model. Courtesy of Dr. Leiderman.
Countless cells jostle against their neighbors as a cascade of chemical reactions speckle their surfaces, racing down the highways of the cardiovascular network. With so many moving parts, Dr. Leiderman believes that a mathematical approach is uniquely equipped to make sense of this turbulent realm. By developing mechanistic models stemming from fundamental behaviors of biological systems, she aims to uncover the unwritten rule book for coagulation. While there were computational studies into this process before Dr. Leiderman’s work, many were laser-focused on its biochemical aspects, ignoring the mechanical aspects of flow. They constrained the problem to a static environment in a well plate or test tube. Other studies demonstrated the opposite problem by fixating on cell aggregation, with less focus on the chemical steps leading up to it. Dr. Leiderman decided to draw from the best of both worlds, integrating fluid dynamics into her coagulation research.
One of her ongoing inquiries delves into the phenotypic heterogeneity of bleeding disorders. Something is said to have phenotypic heterogeneity if it possesses a variety of physical presentations, all of which can technically be classified under the same name. For Dr. Leiderman, this means that a bleeding disorder characterized by the deficiency of a certain clotting protein can have broad effects across affected individuals. The problem lies not in irregularity but rather in Dr. Karin
Coagulation, the transformation of blood from a liquid to a gel-like substance, is an inherently complex process.

Figure 2. Every simulation resulting in adequate thrombin production had a factor V level at least a quarter below normal. Courtesy of Dr. Leiderman.
unpredictability: If a person is only moderately deficient, how severe of a phenotype will they show, and what treatment plan should they follow? One such condition marred by this dilemma is Hemophilia A. A patient who severely lacks the affected protein, factor VIII, will surely suffer from excessive bleeding, bruising, and other striking symptoms. Thankfully, there exists conventional treatment for this demographic. The milder “grey zone” is where the problem gains depth. Here, factor VIII becomes a poor predictor of the disorder’s manifestation, meaning other details must be filling in the gaps. Dr. Leiderman spends her time trying to skillfully peel this delicate case, taking care not to miss any of the subtle layers that may explain why certain people fare better than others and even serve as potential targets for novel therapies.
When it comes to hemophilia’s heterogeneity, few explanations are off the table. The black box nature of its emergence paints virtually all variables as suspects, including proteins, platelets, and even other blood cells. At some point, material experiments cannot keep up with the rigor of such a sensitive benchmark, giving way to models. Unlike the wet lab, computations are efficient, fast, and cheap. Unfettered by the need for physical space and the daunting task of trying to balance replication rigor with resource availability, the simulated environment becomes an infinite playground for hypothesis-testing galore. Occasionally, a promising theory makes it out of this cycle, worthy of real-life replication; but even though these ideas pass the initial interest screening, they never paint the full picture. Subsequent lab experiments will need to confirm some aspects of a given model and, importantly, single out its shortcomings. These misses become

Figure 3. Whole blood assays on factor VIII-deficient blood showed an increase in the rate and maximum accumulation of fibrin when factor V was partially inhibited. Courtesy of Dr. Leiderman.
a guide for tweaking the original framework, setting up for the next iteration of study.
Although models are open-ended by design, the types of conclusions that can be made are constrained by their purpose. Some are meant to simply point out features of the environment in which the system operates, linking the circumstances of the investigation to its outcomes. Mechanistic models, by contrast, go beyond correlation, showing that a given variable helps drive the result. Dr. Leiderman leveraged one of these powerful tools in her own research on the interactions governing clotting with hemophilia A.2 The process’s incredible complexity shields it from attempts to boil it down to a few parameters, yet it’s at moments like these when the ground-up approach shines. Her team performed copious simulations of a model depicting the blood’s clotting response as it flows over a small injury, screening over one hundred thousand combinations of plasma protein levels while fixing the signature factor VIII at a low concentration. The proxy for the performance of each scenario was chosen to be the production of thrombin, a key protein in the coagulation pathway (Figure 1). Thrombin transforms fibrinogen into fibrin, significantly promoting the clotting process. Setting a threshold for adequate thrombin presence, Dr. Leiderman’s team noticed that these samples had a strikingly low level of one particular plasma protein, factor V. Another statistical test showed that adjusting the amount of factor V accounted for half of the variance in total thrombin output (Figure 2). With a clear theoretical frontrunner, it was time to put this protein to the physical test. Using whole blood assays, they were able to mimic the compelling conditions by mixing blood from donors with mild to moderate factor VIII deficiencies with an antibody against factor V, lowering its concentration. Compared to the negative control, these blood samples showed both higher and quicker accumulation of fibrin (Figure 3), agreeing with the hypothesis and provoking some thoughts as to how factor V helps complete the functional puzzle.
In recent years, Dr. Leiderman has finally begun to see her team’s computational techniques gain traction in the coagulation field. This recognition is an invitation for bench scientists and clinicians to trust her contributions and seek common ground. Working in isolation, neither side is likely to bear new fruit, and the path to discovery often lies somewhere in between. Dr. Leiderman hopes that the ultimate win will be for the patients, who may someday gain access to personalized, cost-effective remedies. While biology can streak the canvas with paint, math can craft a fresco of life from its immutable logic. “That’s the dream.”1
References
1. Interview with Karin Leiderman, Ph.D. 02/28/2025.
2. Link KG, Stobb MT, Sorrells MG, Bortot M, Ruegg K, Manco -Johnson MJ, Di Paola JA, Sindi SS, Fogelson AL, Leiderman K, et al. 2020. A mathematical model of coagulation under flow identifies factor V as a modifier of thrombin generation in hemophilia A. Journal of Thrombosis and Haemostasis. 18(2):306–317. doi:https://doi.org/10.1111/ jth.14653. https://www.sciencedirect.com/science/article/ pii/S1538783622014945.
By Sarah Edmonds

Parrotfish are brightly colored tropical fish that live along coral reefs around the world. Their beak-shaped mouths–formed by fused teeth–make them resemble parrots more than other fish. Like birds with nesting behaviors, parrotfish exhibit territorial behaviors and create specific home ranges they defend. Dr. Sophie McCoy’s parrotfish research in the Caribbean investigates these home ranges and how parrotfish utilize space differently from other reef fish.
Dr. McCoy is an ecologist and microbiologist at the University of North Carolina at Chapel Hill (UNC) with broad interests in all kinds of ecosystem interactions, especially in marine systems. While she specializes in microbiomes, like algal interactions on coral reefs, Dr. McCoy’s then PhD student (now postdoctoral researcher at UC Boulder) Josh Manning, was considered the “fish expert” of this operation.1 Inspired by the feeding habits exhibited by parrotfish, originally studied by McCoy because of their herbivorous diet consisting of bacterial growths on reefs–the researchers decided to focus their study on these fish and the other ways they interact with their coral reef environment. They learned that parrotfish have complex social interactions marked by territorial behaviors. For example, they flap their fins at other animals that threaten their home spaces, like how birds would flap their wings at perceived threats. Dr. McCoy’s comparison helps illustrate the rarely seen behaviors of parrotfish by relating them to a species observed more regularly.

Social interactions in parrotfish dictate how they use their environment and protect their space. This study helps to expand on this idea and explores how these interactions impact the entire coral reef. In parrotfish, older, sexually mature males (referred to as terminal phase) display territorial aggressive behaviors and occupy
the most space on the reef. Sexually underdeveloped males (referred to as initial phase) spend most of their time skirting around other territories to take over when the large males die. Females spend time inside these protected territories benefitting from territorial males.1 To study how parrotfish use space on a reef, Dr. McCoy and Dr. Manning looked at these “home ranges,” the self-contained areas where parrotfish conducted their daily activities. They examined parrotfish of different ages and sizes in Bonaire of the Caribbean to compare the way they utilize reef ecosystems.2 They also wished to explore how much of these home ranges could overlap between individuals of different species, and how these interactions would occur. To do this, they used GPS tracking and filming of individual parrotfish over time to collect data on their outlined home range. This portion of the experiment resulted in the creation of Figure 3, a graphed illustration of spatial home range tracks collected for different parrotfish species over time. Just as a GPS watch would be able to track a path, the researchers were able to track the fish’s movements. Then, with this information in mind, they mapped average home range sizes and looked at collected GoPro videos with a social interaction framework, collecting data on behavioral

patterns exhibited around their spaces between terminal phase and initial phase parrotfish from different species. For instance, they collected behavioral data by marking each time one fish ran into another one.1 This allowed them to not only look at the spatial boundaries of each fish but also to illustrate their social boundaries as well.
behavior.
Together, these findings suggest that parrotfish use of space is heavily shaped by social interactions, especially competition and territorial behavior within the same species. This supports the central idea that territory holders in these communities have almost exclusive access to the resources of the ecosystem by holding their space.2 This alters how the community functions, feeds, and interacts. Understanding how these parrotfish interact with one another and their environment will help us understand how their ecosystems function and the future of the coral reefs depending on the presence of parrotfish. Dr. McCoy suggests research like this could play a large role in ecosystem management and resilience. If scientists can understand what the fish are doing, researchers can understand how space in the ecosystem is created and how diversity is maintained— leading the scientific community on a path towards maintaining more resilient coral reefs in the face of climate shifts.

Dr. McCoy and Dr. Manning confirmed that these parrotfish exhibited complex patterns of territorialism around their home ranges, comparable to nesting behaviors of many birds. They flap their fins in fits of aggression, showing off to protect their space, much like male birds that tote around fancy feathers and puff their chest at other males. Sometimes, Dr. McCoy said, “...parrotfish were even seen biting into coral just to show others where their territory is and not even eating the bite...,” defending their space using complex social signals.1 These behaviors varied by species; smaller species had smaller home ranges, and terminal-phase males had less spatial overlap with other males of the same species, suggesting they have exclusive access to resources having larger territories and not sharing them. These large male fish are also usually found to exhibit the most aggressive behavior towards other males in their species—protecting their territory.2 One of the key findings Dr. McCoy emphasized was the “parallel universes” that existed between the home ranges of different species; they found, surprisingly, that these strict territory ranges did not necessarily mean no other fish from other species existed there, and in some cases that was far from the truth.1 These spaces often overlapped on top of one another, layering the worlds of different species of parrotfish and creating a tangled web of social interaction oblivious to the other fish. A smaller species could live right on top of a larger one. The researchers, based on this observation, learned a lot about the parrotfish’s individual behavior and how similar their space use patterns develop alongside social separations and
Figure 3. GPS Tracks of Parrotfish Home Ranges Graphed in RStudio. Illustrates proposed home ranges based on different species. Courtesy of Figure 1 of Publication.
More research on the behavioral interactions of parrotfish is in the works, in discussion with experts on bird behavior comparing the ways fish “keep their enemies close” to birds and many other animals on Earth.2 Future explorations would help to flesh out exactly what is happening inside these complex territorial spaces in coral reefs and why. Dr. Manning is currently undertaking postdoctoral research on this, researching deeper into parrotfish behavior and uncovering so much about the ways in which they interact with each other and their environment.1 Studies like this one push forward our knowledge of community function and ecology, providing vital connections across scientific research. As climate change continues to alter ecosystems such as Caribbean coral reefs, research like this could offer key insights into the future of our natural world!

Figure 4. Dr. Joshua Manning in the Field. Courtesy of Dr. Ethan Cissel.
1. Interview with Sophie McCoy, Ph.D. 2/28/252.Manning JC, McCoy SJ. 2023.
2. Territoriality drives patterns of fixed space use in Caribbean parrotfishes. Ecology and Evolution. 13(2).doi:https:// doi.org/10.1002/ece3.9833.
By Gargi Gole

Can cells be placed in a category that defines them as good or bad? The fact is that cells cannot be placed into either category: good or bad. Rather, cells like most organisms are more nuanced; they play different roles in the body to ensure that it remains healthy. This is because their functions can change and often differ based on how they respond to conditions presented to them. Microglia 3, for example, are the main immune cells in the central nervous system that help keep the brain healthy,and can promote both positive or negative responses in the brain. Dr. Coleman, an MD-PhD, works at the Bowles Center for Alcohol Studies in the Department of Pharmacology. His research has primarily focused on finding treatments for immune related diseases like Alzheimer’s, addiction, and cancer. Recently, his research on creating Alzheimer’s Treatments led him to study the versatile microglia cells, which are immune cells commonly present in the brain.
A recent study done by Dr. Coleman focused on how microglia impact the brain along with their association with Alzheimer’s disease2. He and his research team focused on studying Alzheimer’s disease, which is predominantly seen in older people, to understand how the functions of microglia change over time. They also wanted to understand how their functional presence is different to different people. It can
cause dementia and can detrimentally impair an individual’s cognitive functions. The characteristic of Alzheimer’s being associated with aging mirrored that of microglia. One of the key observations made was that those with Alzheimer’s Disease have amyloid plaque, an abnormal protein that builds up commonly on grey matter, which is responsible for helping to process information in the brain. However, prior research studies have shown that even those who don’t have Alzheimer’s disease can have amyloid plaques as they get older. This led to the question of how individuals responses to amyloid plaque can vary which Dr. Coleman and his team studied by observing how microglia, the main immune cells in the brain react by either protecting or damaging cells. Microglia are often associated with having negative impacts on the brain and to test this the microglia were inhibited in experimental cultures. In this study, Dr. Coleman used hippocampal entorhinal brain slice culture, which were cells that were artificially grown in controlled environments in a petri dish. The culture can function outside of the body and the impacts of microglia are seen. They then treated the cultures with the protein that is specific to Alzheimer’s to see how the cells would respond. They then observed how microglia affected this process, whether they positively impacted the cells or negatively impacted them.He found that


Figure 2. This image depicts the comparison between the brain of a person without Alzheimer’s disease and one with Alzheimer’s disease. Courtesy of Wikimedia Commons.
when the function of microglia was inhibited the brain culture expressed negative effects suggesting that microglia are not always harmful. He emphasized that throughout the study “following the data and understanding the results he got helped him find a treatment”. He tested different hypotheses based on the results he was getting to be able to understand the function of microglia. For example, he tested whether microglia removal positively impacted the cells,which did not lead him to believe that microglia are not always harmful.
To better understand the functions of microglia and how they impact those with Alzheimer’s disease, Dr. Coleman focused on how microglia specifically affected TRAIL (Tumor Necrosis Factor-Related Apoptosis-Inducing Ligand) which can lead to cell death, apoptosis, which is a symptom of Alzheimer’s disease. He found that microglia with the M1 Phenotype increased the presence of TRAIL while those with the M2 Phenotype decreased the occurrence of TRAIL in decreasing the promotion of cell death. Additionally, when microglia interacted with Aβ1-42oligomers (pieces of amyloid plaque) the microglia expressed positive impacts with the brain, although previously microglia had negative impacts associated with amyloid plaque in relation to Alzheimer’s disease. However, when they continued to interact with Aβ142 oligomers for a prolonged period negative effects were expressed leading to eventual cell death, apoptosis.
The function of microglia changed in the brain over time. The results supported the reason why Alzheimer’s disease is more commonly seen in older adults, beyond the age of 40. As adults get older their cells also age often resulting in amyloid plaque buildup. Dr. Coleman’s research showed that while Alzheimer’s disease is not always present in those with amyloid plaque buildup, there is an association between aging and the way that cells behave.
Dr. Coleman’s study emphasized that cells, like microglia, must be balanced. They cannot just be put off as beneficial and harmful. Further, it is important to study different cells through cell biology and other fields to create beneficial treatments. These studies conducted to find these beneficial treatments can further research in human disease and help doctors and researchers better understand how diseases progress. The understanding of disease progression helps better diagnose diseases as well. The research of cells is essential to furthering medical innovation and helps us
better understand the functions of the human body.The continuation of this research conducted by researchers like Dr. Coleman has and will continue to advance treatments in the medical field to help individuals live healthy lives.

1. Interview with Dr. Coleman
2. Garrondo. 2008 Jul 16. English: Drawing comparing how a brain of an Alzheimer Disease patient is affected to a normal brain. Wikimedia Commons.https://commons. wikimedia.org/wiki/File:Brain-ALZH.png.
3. File:Mikroglej 1.jpg-Wikimedia Commons. 2022. Wikimediaorg. [accessed2025 Apr 3].https://commons.wikimedia.org/wiki/File:Mikroglej_1.jpg.
4. Zou J, McNair E, DeCastro S, Lyons SP, Mordant A, Herring LE, Vetreno RP, ColemanLG. 2024. Microglia either promote or restrain TRAIL-mediated excitotoxicity caused byA142oligomers. Journal of Neuroinflammation. 21(1). doi:https://doi.org/10.1186/s12974-024-03208-2
By Siri Pandi

Evolution, often thought of as happening on a timescale of thousands of years, is being observed in a little beaker by Dr. Christopher S. Willett at the University of North Carolina at Chapel Hill using small, diverse crustaceans called copepods. The concept of evolution, also known as the concept of common descent, refers to the idea that all life on Earth shares a common origin. Genetic divergence in DNA sequences, propelled by natural selection and genetic drift, is the main driving force of evolution. Genetic divergence occurs when populations of the same species accumulate genetic differences over time, usually due to factors like geographic separation or different environmental conditions.1 These genetic changes can result in adaptations that better suit each population to its specific habitat. As the genetic differences become more pronounced, these populations may eventually become distinct species in a process known as speciation.
could lead to eventual sterility and decreased viability known as hybrid breakdown. Additionally, studying speciation helps us understand the impacts of environmental changes, such as climate change and habitat loss, on species’ ability to adapt and survive.

As the need for conserving vulnerable species and maintaining biological diversity increases, learning about speciation is crucial for species conservation efforts because it provides insights into how new species form and adapt to their environments. This understanding helps conservationists identify the genetic diversity within and between species, which is essential for their long-term survival. By recognizing the unique adaptations and evolutionary paths of different populations, we can develop targeted strategies to protect and preserve these populations, ensuring that they can continue to thrive in their natural habitats. These strategies may include studying how an endangered species interacts with different organisms in an ecosystem and how individuals from related species may interbreed to produce offspring with a unique combination of DNA. This can either increase genetic variation and allow the offspring to resist more changes in environment, or it
Dr. Christopher Willett is a research associate professor at UNC-Chapel Hill, both teaching in the department of Biology and heading the Willett Lab, with a focus on studying the genetic causes behind evolutionary processes such as adaptation and speciation. In addition to using the copepod (Tigriopus californicus) to model genetic speciation, he has also used the tobacco hornworm (Manduca sexta) to find how organisms respond to thermal changes over time. While getting his doctorate in Genetics and Development from Cornell University, Dr. Willett was greatly inspired by his time at the Richard Harrison Lab, where the study of evolution was a unifying factor that led graduate students to experiment with a range of organisms by observing the genetic changes that would lead to species divergence.2 With his work in his own

Figure 2. A beaker containing copepods in the Willett Lab, which are then used in experiments to observe how their genetic changes lead to speciation. Figure courtesy of Dr. Willett.
lab, he aims to model evolution in a manageable setting that allows for broader research on how organisms adapt to their surroundings through the accumulation of genetic changes. This information could help conservation biologists determine whether vulnerable organisms can be left isolated or whether more genetic diversity should be added to help their population survive against potentially changing situations.
Dr. Willett focused on the species Tigriopus californicus, which occurs in isolated tidepools in genetically divergent populations along the Pacific coast of North America. These populations possess slight genetic differences as they have adapted to varying physiological conditions such as salinity or temperature. These copepods are unique enough to exhibit differences in their traits, but not distant enough that they have become completely new species. When they were incubated and reared in glass beakers in the lab, Dr. Willett ultimately found that the accumulation of genetic divergence can lead to reproductive isolation and speciation through the phenomenon of hybrid breakdown, gradually preventing two genetically divergent populations from producing viable offspring. Dr. Willett says, “the first-generation hybrids are generally fine, and sometimes have better fitness than the parents. And that’s kind of like a hybrid, bigger effect where you see this in things like corn, where when you make crosses between 2 divergent corn lineages, you get hybrid corn, which does way better... But then, in the second generation of hybridization is when you tend to see lower fitness and more variable. Some individuals do badly, and some individuals are okay.”1 In other words, due to the already present genetic variation in the copepods from traits that were favored by their specific environments, if two different types of copepods were to reproduce, they would have healthy offspring, sometimes with a greater ability to survive and pass on their traits to the next generation. This would be the first hybrid generation; when this generation reproduces, however, the second hybrid generation produced has a lower
“[Dr.Willett’s work] reaffirms the fact that evolution is a branching, sometimes cyclic process rather than a linear one, and longterm observations are crucial to make accurate predictions.”
fitness, meaning it may not even survive long enough to pass on its genes to the next generation.
In the long run, hybrid breakdown means that it is unlikely for offspring from the interbreeding different varieties of the copepods to be healthy and survive, leading to increased divergence between the populations and a possibility of becoming two different species as genetic differences. Dr. Willett further explores this phenomenon by relating it to DobzhanskyMuller incompatibilities, which state that when two genetically different populations interbreed, their offspring may receive deleterious combinations of alleles, which are versions of genes that are disadvantageous to the organisms given their specific environments.3 These deleterious alleles had been present in the original populations, but did not affect the parental generation. When inbreeding occurs, harmful genes that may have been otherwise rare will appear in higher frequencies, and if the hybrid offspring receive multiple copies of those genes, they would suffer from the potentially dangerous phenotype.
Dr. Willett’s research on the genetic basis of speciation has provided an incredibly informative, yet sustainable model using copepods that can be used to monitor the specific changes that species undergo before completely diverging. His work reaffirms the fact that evolution is a branching, sometimes cyclic process rather than a linear one, and long-term observations are crucial to make accurate predictions. His research continues to help biologists understand the best ways to preserve the fitness of both the parental generations and offspring in vulnerable populations, especially considering the benefits and disadvantages of potential hybridization that may occur when genetically different populations are introduced together. Most exciting, though, is the realization that speciation truly can show up in seemingly unassuming species such as these copepods. Dr. Willett’s exciting research proves that with careful observation, the smallest of nature’s creations can perfectly reveal its greatest secrets.
References
1. Patrik Nosil; Jeffrey L Leder. Philosophical Transactions of the Royal Society of London 2012, 367, 332-342.
2. Interview with Christopher S. Willett, Ph.D. 02/12/2025.
3. Christopher Willett. Genetica 2012, 139, 575–588.

By Vina Senthil
n many organisms, DNA primarily exists in tightly wrapped bundles located within the nuclei of cells. The levels of DNA compactness are astounding—in humans, most nuclei contain about two meters of DNA. At the core of these bundles are histones, proteins responsible for “packaging” the genome in chromatin, a dense DNA complex.1 Though they aren’t genes themselves, histones play an integral role in gene expression, which is often dependent on both the gene being read and its associated proteins.1
other specialized cells, rely on differential gene expression to develop their unique, cellular identity. The McKay Lab studies the role played by histone PTMs in cell fate specialization. In other words, they study how histone PTMs enable cells to remember who they are. This field of research is known as epigenetic gene regulation.

Dr. Dan McKay, a developmental biologist and associate professor of biology at the University of North Carolina at Chapel Hill, investigates the function of posttranslational modifications (PTMs) of histones. Histone PTMs are chemical marks placed on histones after translation, the process by which proteins are synthesized from messenger RNA (mRNA). mRNA is transcribed from genomic, or genecontaining, DNA. Modifications of histones typically entail the addition of a methyl group (CH3) through methylation or an acetyl group (COCH3) through acetylation to a histone protein (Figure 1). Dr. McKay’s Lab tests the hypothesis that histone PTMs are essential to a gene’s activity state, which dictates whether the expression of a particular gene is turned off or on. Gene expression is directly tied to changes in chromatin packaging, and histone PTMs are proposed to regulate chromatin packaging. Methylation often results in tighter packaging of DNA around histones, leading to a less active, “repressive” gene activity state. On the other hand, acetylation loosens chromatin, enabling a more active, “permissive” gene activity state. Differences in histone activity can be observed between various cell types, as gene expression differs based on the specific functions of a cell.3 This personalized gene expression, also known as differential expression, is the primary driver of cell specialization, the process by which a cell decides what type of cell it will ultimately become. Neurons, pancreatic cells, epithelial cells, among
By creating histone mutations in Drosophila, commonly known as the fruit fly, the McKay Lab strives to better understand the specific functions of histones and their PTMs. Though humans and fruit flies share no physical resemblance, and Drosophila evolutionarily separated from humans hundreds of millions of years ago,3 Dr. McKay says they have remarkably similar mechanisms of gene regulation, in part because their histone proteins are so similar. For example, their histone H3 protein is identical to H3 in humans. In fact, the histone H3 protein is the only protein that is 100% conserved between flies and humans.
Mutating histones in fruit flies is not as straightforward as simply cutting out the gene encoding a specific histone: without histones, the fruit flies would not be able to survive, as their cells’ ability to replicate DNA would be compromised. Instead, the lab uses transgenes, larger DNA segments featuring cloned histone genes. The transgenes are then reintroduced into the fly genome and undergo transcription and translation as usual. Because the histone genes are present, the fly can survive, but the transgenes allow for an

Figure 1. Chromatin consists of DNA wrapped tightly around histone proteins and non-histone proteins. Histone tails, pictured above in dark brown, can be methylated or acetylated. Courtesy of Dr. McKay.
exception—the histone genes are not wildtype. In other words, they are not the naturally occurring, non-mutated version of the gene. Instead, they can carry small, intentional mutations. The research team mutates individual codons, sequences of three nucleotides found in DNA or RNA, such that a specific instance of methylation or acetylation is prevented from occurring. The team then observes the consequences of the mutations they created, gaining insight into the significance of such chemical marks (Figure 2).3
According to Dr. McKay, one of the most challenging aspects of the lab’s research is studying epigenetic gene regulation in early Drosophila embryos. This is an important time in development to study gene regulation because it is when cell types are first becoming specialized. However, creating gene mutants is difficult in early embryos. The lab has taken two approaches to overcome this challenge. One graduate student in the lab, Oscar Arroyo, has generated a new genetic platform to selectively deplete histones in early Drosophila embryos. A second graduate student, Sean Johnsen, used an “optogenetic tool” that inactivates protein function in Drosophila embryos through the absorption of light. Optogenetic tools use light to control biological systems.5 Upon exposure of a Drosophila embryo to blue light, the structure of certain proteins may be altered, inactivating or activating it. Optogenetic tools allow the research team to inactivate genes involved in epigenetic regulation in the early embryos without risking damage.3
The significance of the McKay Lab’s research extends beyond answering questions about the function of histones— it can shed light on possible clinical treatments for deadly diseases. Onco-histones, for example, are implicated in diseases such as pediatric glioblastoma, an aggressive brain cancer in children. Mutations in onco-histones cause them to develop cancer-promoting activity in cells, or oncogenesis. If

Figure 2.The McKay Lab introduces mutations to histones via transgenes. The loss of a histone PTM in the mutant Drosophila embryos may result in a specific phenotype. Courtesy of Dr. McKay.

Figure 3. Onco-histones feature mutations that resulting in the mis-expression of a gene, resulting in tumorigenesis. Courtesy of Dr. McKay.
histones receive chemical marks that direct them to loosen DNA and continuously activate the transcription of specific genes, excess cell division may occur, resulting in the formation of tumors (Figure 3). Through study of their histones and PTMs, the McKay Lab believes the developmental mechanisms underpinning deadly disease can be better understood. Furthermore, clinical research geared towards devising treatment plans for patients afflicted with a life-threatening disease can be boosted.3 Given the unpredictable nature of scientific research, Dr. McKay’s research team will likely face obstacles in the future, but they are determined to further elucidate how histone mutations relate to certain phenotypic outcomes.3
1. DNA packaging: nucleosomes and chromatin | Learn Science at Scitable. 2. Kobs, G. (2018, February 12). Mass spec analysis of ptms using minimal sample material. Promega Connections.
3. Interview with Dan McKay, Ph.D. 03/03/25 (3) McKay, D. J., Klusza, S., Penke, T. J. R., Meers, M. P., Curry, K. P., McDaniel, S. L., Malek, P. Y., Cooper, S. W., Tatomer, D. C., Lieb, J. D., Strahl, B. D., Duronio, R. J., & Matera, A. G. (2015). Interrogating the function of metazoan histones using engineered gene clusters. Developmental Cell, 32(3), 373–386.
4. Rost B, Schneider-Warme F, Schmitz D, Hegemann P. Optogenetic Tools for Subcellular Applications in Neuroscience. Neuron. 2017 Nov.
5. Nacev, B. A., Feng, L., Bagert, J. D., Lemiesz, A. E., Gao, J., Soshnev, A. A., Kundra, R., Schultz, N., Muir, T. W., & Allis, C. D. (2019). The expanding landscape of ‘oncohistone’ mutations in human cancers.
By Rachel Zeisloft
Imagine you’re driving across a bridge when you spot a crack forming in the middle. If left unattended, that tiny flaw could lead to catastrophic failure. This same principle applies to our DNA. Every time a cell divides, errors—or mismatches—can occur. Without a precise repair mechanism, these errors could accumulate, leading to cancer and other genetic diseases. Dr. Dorothy Erie, a leading researcher in the field of DNA repair, is on a mission to understand how cells identify and fix these mistakes. Her groundbreaking research on mismatch repair is helping to unravel the mystery of the molecular signals that maintain our genetic integrity.
Raised as the youngest of nine children in South Louisiana, Dr. Erie had an unconventional path into the sciences. Inspired by her older sister, who shared a love for science, she found a deep connection to the scientific world.1 Her journey began in a small classroom taught by a nun, where she first became fascinated by Mendelian genetics. However, her dyslexia made it challenging to memorize information easily—but chemistry, with its logical and structured nature, became her passion. This early spark evolved into a career studying the physical chemistry of DNA stability and, eventually, the complex world of DNA repair. After receiving a B.S. in Chemistry from Louisiana State University, Dr. Erie followed this passion, receiving a M.S. and a Ph.D. in Physical Chemistry.1 Building on her early fascination with DNA, Dr. Erie’s work now focuses on one of the cell’s most critical maintenance systems—mismatch repair.

Dr. Dorothy Erie

Mismatch repair is a cellular quality control system, ensuring that errors made during DNA replication are corrected. Dr. Erie describes it as being akin to bridge repair: “Just like with a bridge, every time you do something [to DNA], you actually make it worse than it was. Every step has to be tightly coordinated.” Her research focuses on
Image courtesy of Adobe Stock
understanding how the cell recognizes mismatches and the series of molecular signals that guide the repair process.
The mismatch repair process begins when a protein complex known as MutS scans the DNA for errors, specifically mismatched base pairs. Upon identifying a mismatch, MutS undergoes a conformational change—a structural shift—that activates the next stage of the repair pathway. This structural change, facilitated by adenosine triphosphate (ATP), the cell’s primary energy source, recruits additional repair proteins to the site of the error, initiating the correction process. Once recruited, the MutL protein interacts with a critical cofactor

Figure 1. In eukaryotes, MMR is performed by MutS and MutL homologs, and the interaction between PCNA and MutL plays a crucial role in recognizing the daughter strand. Courtesy of the Erie Lab.

Figure 2. Free-energy landscape illustrating the transition of MutS from mismatch recognition (state 1) to the mobile clamp (state 4), including ATP-dependent conformational changes, mismatch rebinding, and stochastic events affecting ATPase turnover, with key states (1–5) and transition pathways represented. Courtesy of Hao et. al.
called PCNA (Proliferating Cell Nuclear Antigen) to activate an enzyme called endonuclease. This enzyme makes a precise cut in the newly synthesized, error-containing DNA strand near the mismatch site. The damaged section is then excised, removing the incorrect nucleotides and creating a clean space for accurate repair. This targeted removal ensures that only the faulty portion of the DNA is replaced. With the erroneous segment removed, the DNA polymerase enzyme synthesizes a new strand by inserting the correct nucleotides. The final step involves DNA ligase, which seals the repaired strand by forming a continuous DNA backbone. This highly coordinated process maintains genomic integrity, preventing mutations that could lead to cellular dysfunction or disease. This multi-step repair mechanism is crucial for preserving genetic accuracy, ensuring that errors introduced during DNA replication are swiftly identified and corrected.
Understanding how these molecular players work together is no small feat. Using cutting-edge techniques like atomic force microscopy (AFM) and single-molecule fluorescence, Dr. Erie is shedding light on how ATP drives the conformational changes necessary for the repair machinery to function. AFM allows her team to visualize how these protein complexes assemble on the DNA, while Förster resonance energy transfer (FRET) reveals how proteins move and interact in real-time.2 These insights not only deepen our understanding of fundamental DNA repair mechanisms, but also highlight their broader implications for human health.
Defects in mismatch repair have serious consequences. Lynch syndrome, the most common form of hereditary colorectal cancer, arises from the inactivation of mutations of
DNA mismatch-repair genes.3 “Mismatch repair proteins don’t just fix errors—they also play a role in drug resistance,” Dr. Erie explains. Epigenetic silencing of these repair genes can render cancer cells resistant to chemotherapy, making them even more difficult to treat.
Erie’s research also extends to neurodegenerative diseases like Huntington’s disease, a disorder caused by the expansion of the cytosine-adenine-guanine (CAG) trinucleotide repeat. While the clinical presentation varies with the age of onset, it is primarily marked by cognitive, motor, and psychiatric impairments.⁴ Normally, mismatch repair corrects these errors, but in Huntington’s, the system gets hijacked. “It’s like a Jekyll and Hyde situation,” she says. “The very proteins that usually protect us can also promote the expansion of these harmful repeats.” This expansion worsens with age, and her team is investigating how to inhibit the proteins involved before symptoms emerge. Dr. Erie and her collaborators are now focused on dissecting the intricate relationship between PCNA and MutL. By understanding how these proteins interact, they aim to uncover new therapeutic strategies for cancers and other diseases linked to mismatch repair dysfunction.
Her work not only advances our scientific understanding but also holds promise for developing targeted treatments. From bridge repairs to cellular repairs, the parallels are clear— precision and coordination are key to maintaining stability. As research continues to evolve, so does the potential to harness these molecular mechanisms to improve human health. With each new discovery, the mysteries of DNA repair become a little less opaque—and the bridge to better health grows stronger.
1. Interview with Dr. Dorothy Erie, Ph.D. [date needed]
2. Satusky MJ, Johnson CV, Erie DA. 2023. Rapid, inexpensive, sequence-independent fluorescent labeling of phosphorothioate DNA. Biophysical Journal. 122(7):1211–1218. doi:https://doi.org/10.1016/j.bpj.2023.02.011. [accessed 2025 Mar 5]. https://www.cell.com/biophysj/fulltext/S00063495(23)00103-0.
3. Barnetson RA, Tenesa A, Farrington SM, Nicholl ID, Cetnarskyj R, Porteous ME, Campbell H, Dunlop MG. 2006. Identification and Survival of Carriers of Mutations in DNA Mismatch-Repair Genes in Colon Cancer. New England Journal of Medicine. 354(26):2751–2763. doi:https://doi. org/10.1056/nejmoa053493.
4. Rojas NG, Cesarini ME, Peker G, Prat GAD, Etcheverry JL, Gatto EM. 2022. Review of Huntington’s Disease: From Basics to Advances in Diagnosis and Treatment. Journal of Neurology Research. 12(3):93–113. doi:https://doi. org/10.14740/jnr.v12i3.721. https://www.neurores.org/index. php/neurores/article/view/721/701#s6.
By Julia Ellington

The COVID-19 pandemic not only contributed to global health, but also raised unprecedented levels of psychological distress across the globe. A study by researchers from various institutions, including Dr. Jonathan Abramowitz, has been shedding light on the factors that heighten anxiety related to COVID-19, especially for individuals with obsessive-compulsive (OC) symptoms. The study, “Psychological Predictors of COVID-19 Anxiety: The Role of Obsessive-Com-

pulsive Symptoms,” examines how contamination-related OC symptoms, anxiety sensitivity, and body vigilance contribute to pandemic-related anxiety, offering crucial insights into mental health during these uncertain times.
To understand Dr. Abramowitz’s research, it is critical to define anxiety. “Anxiety is our body’s response to the perception of threat…as soon as we perceive some sort of threat, our body… keeps us worried, keeps us focused on the potential threat,” Abramowitz explains. In the context of his work on obsessive compulsive symptoms, Abramowitz notes that these symptoms manifest when “people have these obsessional thoughts, which are these persistent… doubts and ideas that something bad is going to happen”.
The significance of this research is particularly poignant given the rise in mental health struggles brought about by the pandemic. Drawing on years of relevant expertise, Dr. Abramowitz explains, “Our lab has studied other pandemics in the past, like the Ebola outbreak... My lab is interested in the way that people perceive threats... When COVID hit, we were naturally curious about how it would affect people’s anxiety.”
While the emphasis has been on the physical impacts of COVID-19, many individuals’ psychological health has been greatly affected. The study emphasizes that “Individuals
with obsessive-compulsive symptoms are particularly vulnerable to heightened anxiety during situations that involve uncertainty and fear of contamination,” such as the pandemic. Dr. Abramowitz’s lab hypothesized that individuals who already had contamination-related OCD fears would be especially anxious during the pandemic, and they found that this was indeed the case. Those who were already anxious about germs, viruses, and sickness found COVID-19 even more distressing.
The research focuses on two main factors: obsessivecompulsive (OC) symptoms related to contamination fears, and anxiety sensitivity, the tendency to fear anxiety-related bodily sensations. By using comprehensive psychological assessments and measuring anxiety levels, this study highlights key predictors of COVID-19 anxiety. Anxiety sensitivity—particularly related to physical symptoms—has been shown to worsen anxiety during health-related crises like the COVID-19 pandemic, causing individuals to misinterpret normal bodily sensations as indicators of illness.
The study’s participants included a diverse group of individuals, ranging from those with mild OC symptoms to those with clinically significant obsessive-compulsive disorder. Through a series of surveys, including the Coronavirus Anxiety Scale (CAS) and Anxiety Sensitivity Index (ASI), researchers were able to assess individuals’ levels of anxiety, body vigilance, and susceptibility to panic symptoms. The study ultimately demonstrated that individuals with contamination-related OC symptoms exhibited higher levels of COVID-19-related anxiety than those without these symptoms, indicating a distinct relationship between OC symptom severity and pandemic-induced stress.
Additionally, the research uncovers the relationship between body vigilance—the tendency to monitor one’s body for signs of illness—and COVID-19 anxiety. The more individuals were vigilant about potential signs of the virus in their bodies, the greater their anxiety about contracting COVID-19. Dr. Abramowitz explains how body vigilance plays a role, noting that “If you’re already worried about germs and sickness, of course, the pandemic isn’t going to make you feel better about that—it’s going to make it even worse.” These findings highlight the importance of addressing both cognitive and physiological responses to anxiety in understanding how individuals experience pandemic stress.
Dr. Abramowitz and colleagues also explored demographic variables that may influence anxiety levels. They found that younger individuals, particularly those with a history of anxiety disorders, reported higher levels of COVID-19-related anxiety. Interestingly, the study did not find a significant gender difference in COVID-19 anxiety levels, suggesting that both men and women with certain psychological traits are similarly affected by pandemicrelated stressors. This is compelling because in general, Dr. Abramowitz noted that “women tend to have more anxiety than men”.
The study also highlights the impact of cognitive recovery in the context of anxiety. Dr. Abramowicz suggested therapeutic approaches like Exposure and Response Prevention (ERP) therapy, which helps individuals confront
their fears in a controlled, manageable way. “For example, people who were afraid of touching their mail because they feared contracting COVID would be helped to touch the mail, without washing their hands afterward, to see that the worstcase scenario doesn’t come true,” he advised.
As we look ahead, it’s important to understand that such mental health issues can continue to affect people even as the pandemic subsides. Dr. Abramowicz offers several strategies for coping with health-related anxiety, particularly OCD, underscoring the importance of social support and maintaining healthy routines. “make sure that you are sleeping well, make sure you’re eating healthy, make sure you’re getting exercise”. Notably, Abramowitz explained that “You don’t have to eliminate anxiety entirely; rather, it’s about learning to manage it. Make room for it”. Overall, even if one is not receiving cognitive behavioral therapy, ensuring the maintenance of a balanced, healthy life with regular sleep, exercise, and meaningful social connections can combat anxiety.
Dr. Abramowitz’s groundbreaking research on psychological predictors of COVID-19-related anxiety reveals the critical interplay between OC symptoms, anxiety sensitivity, and body vigilance in determining pandemic-related distress. These findings aren’t merely academic—they provide essential insights for developing targeted clinical interventions that could transform how we address psychological suffering during global health crises. By identifying specific vulnerability factors, mental health professionals can now craft more effective, personalized treatment approaches that address the root causes of pandemic anxiety. As we face an increasingly unpredictable world, this research serves as a foundation for building psychological resilience across populations. Future investigations with diverse clinical populations will undoubtedly expand this vital work, ultimately strengthening our collective capacity to protect mental health during times of unprecedented global challenge and uncertainty.
References
1. Interview with Dr. Abramowitz, March 4, 2025
2. Heidi J. Ojalehto, Jonathan S. Abramowitz, Samantha N. Hellberg, Megan W. Butcher, Jennifer L. Buchholz, “Psychological Predictors of COVID-19 Anxiety: The Role of Obsessive-Compulsive Symptoms,” Journal of Anxiety Disorders, 2021.
By Olivia Gatto

Women’s mood swings have been laughed off, mocked, and misunderstood for generations. But research shows they’re not just in their head—they’re in their hormones. Dr. Crystal Schiller, an associate professor in the UNC Psychiatry Department, has dedicated her career to understanding how hormonal shifts impact mental health. The first in her family to attend a fouryear college, she initially planned to become a doctor—until a high school psychology class, chosen on a whim, changed everything. Captivated by the

Dr. Crystal Schiller
science of the mind, she shifted from pre-med to psychology, earning her BS, MA, and PhD from the University of Iowa. Her curiosity led her to study the role of hormones in mood disorders, a field that would become her life’s work. Today, a portion of her research focuses on why women experience depression and anxiety during reproductive transitions—such as the menstrual cycle—and how science can both treat and prevent these mood shifts.
One of the hormone-linked conditions Dr. Schiller studies is Premenstrual Dysphoric Disorder (PMDD), a severe form of PMS that disrupts the mind as well as the body. While PMS is commonly associated with bloating, cramps, and mild mood changes, PMDD is far more extreme. “PMDD is a psychiatric diagnosis that people can get if they have a menstrual cycle and if they experience both physical symptoms and mood symptoms in the time leading up to their period,” Schiller explains. These symptoms include intense irritability, mood swings, sadness, and a loss of interest in things people usually enjoy—signs similar to depression but with a distinctive pattern linked to the menstrual cycle. People with PMDD also experience disrupted sleep, heightened
anxiety, and in some cases, increased sensitivity to pain. This can make the already distressing physical symptoms, such as cramps, breast tenderness, and bloating, even more unbearable.
Despite affecting an estimated 3 to 5% of people with menstrual cycles, PMDD remains difficult to diagnose and often goes unrecognized. In contrast, PMS—which consists of mostly physical symptoms without severe mood disturbances—affects about 50% of people with menstrual cycles and is much more commonly discussed. Because PMDD involves both mental and physical health symptoms, it has a much stricter diagnostic process. Dr. Schiller elaborates that “it requires prospective assessment of mood on a daily basis for at least two months in order to make a PMDD diagnosis.” This means that when someone visits a clinician suspecting they have PMDD, they are often told they have to track their mood every day for two full menstrual cycles before a diagnosis can be made. This presents a major challenge: patients seeking help are often in distress or have been suffering for years, yet the diagnostic process demands even more time. There are also barriers to when and how often a person is able to schedule a doctor’s appointment. As a result, some

clinicians, feeling compelled to provide immediate care, may diagnose PMDD prematurely or prescribe treatments that may not be appropriate. Dr. Schiller notes that providing treatment for PMDD for a premature diagnosis could lead to no result, as it is uncertain whether the patient even has PMDD.
“Wearable technology could revolutionize how mood disorders are diagnosed and managed, offering a more personalized and accessible way to care for those affected.”
This gap in diagnosis and treatment has sparked interest in technology-based solutions that could make PMDD diagnosis more efficient and accessible. There are mood trackers out there that are commercially available, but they don’t necessarily diagnose PMDD. Many apps allow users to log emotions and symptoms, but few integrate the structured, clinical approach needed to confirm a PMDD diagnosis. This is where digital health advancements come in. “Having a medical device like an app that could assist physicians in making the diagnosis would be hugely beneficial,” Dr. Schiller says. If properly developed, such a tool could provide consistent, standardized data tracking, allowing physicians to analyze patterns in mood and symptoms without requiring patients to manually track everything themselves. This could streamline the diagnostic process, reduce misdiagnosis, and lead to more effective treatment strategies.
One of the most promising advancements in understanding PMDD and other mood disorders lies
in the use of wearable technology to track physiological changes. Research suggests that heart rate variability (HRV), sleep patterns, and physical activity— metrics that can now be reliably measured with smartwatches and fitness trackers—could provide valuable insights into mood fluctuations. In individuals with PMDD, physiological changes often occur alongside emotional symptoms, making these objective measures a potential tool for early detection and intervention. By continuously monitoring these biomarkers, clinicians could identify patterns that predict mood shifts, allowing for a more proactive approach to treatment. Dr. Schiller and other researchers are exploring how this remote monitoring paradigm could transform psychiatric care—not just for PMDD, but for other depressive disorders as well. With real-time data collection, physicians could track symptom progression, assess treatment efficacy, and even intervene before severe episodes occur, reducing the trial-and-error approach often required in mental health treatment. If integrated into clinical practice, wearable technology could revolutionize how mood disorders are diagnosed and managed, offering a more personalized and accessible way to care for those affected.
The implications of Schiller’s
research extend far beyond PMDD. Her work is part of a larger movement to acknowledge women’s mental health as a biological issue, not just an emotional one. For too long, hormonal mood disorders have been trivialized or misunderstood, leaving those who suffer feeling unheard. But research is proving that these conditions are real, measurable, and treatable. By understanding the complex relationship between hormones and mood, science is moving toward more effective treatments, better accessibility to care, and, ultimately, greater recognition of the mental health challenges tied to reproductive transitions. With researchers like Dr. Schiller leading the way, the conversation around women’s health is shifting—from outdated stereotypes to groundbreaking solutions.
1. Interview with Dr. Crystal Schiller 2. Brown RD, Bondy E, Prim J, Dichter G, Schiller CE. The behavioral and physiological correlates of affective mood switching in premenstrual dysphoric disorder. Front Psychiatry. 2024 Nov 4;15:1448914. doi: 10.3389/ fpsyt.2024.1448914.
By Alexis Hirth

Image courtesy of Adobe Stock.
Physician burnout has become a hidden epidemic, affecting both physicians and the patients they care for. Research estimates that 50% of physicians are burned out.1 The field of medicine is an incredibly demanding profession, requiring extensive years of education, long hours, and immense resilience. Despite their crucial role in healthcare, physicians are increasingly facing burnout - exhaustion, cynicism or depersonalization, and reduced professional efficacy due to workrelated stress.2 So, what is driving these outcomes?
A prominent researcher tackling this issue is Dr. Tania Jenkins. Dr. Jenkins, an assistant professor at UNC and a faculty research fellow at UNC’s Cecil G. Sheps Center for Health Services Research, started her career fifteen years ago studying the Cuban

health care system. Today, Dr. Jenkins’ research focuses on the intersections of medicine, work and professions, and stratification. Approaching the issue through a sociological lens, Dr. Jenkins examines the broader structural factors that impact physicians’ well-being. Her work contributes to the growing field of medical sociology, seeking to understand how social, professional, and systemic factors influence health outcomes and work-life satisfaction.
Dr. Jenkins was drawn to the question of physician burnout out of her first book project, Doctor’s Orders: The Making of Status Hierarchies in an Elite Profession, which examines the construction and consequences of status distinctions between physicians before, during, and after residency. Her book introduces a theory of status separation to describe how physicians are differentiated into strata according to their social and professional worth.
“What I noticed was that, even though they were considered lower status, almost second class citizens, osteopathic and international medical graduates were extremely satisfied in their jobs. However, a lot of the US medical graduates I observed were disillusioned even though they were high-status. And so I started to get intrigued by this idea of physician burnout and the pervasiveness of burnout in medicine.”3
To gain an in-depth understanding of physician burnout, Dr. Jenkins integrates qualitative and quantitative data. Over the course of
fifteen months, Dr. Jenkins conducted a comparative ethnography in which she observed the day-to-day lives of general pediatricians and pediatric surgical subspecialists. By immersing herself in the clinics where physicians and trainees worked, Jenkins gained firsthand insights into how they balanced their clinical duties with the overall demands of the healthcare system. In addition, Dr. Jenkins conducted 95 interviews with physicians at different stages of their careers, ranging from pre-med students to senior attending physicians. These interviews, along with surveys measuring burnout and job satisfaction, provided data that allowed Jenkins to draw connections between physicians’ burnout and the systemic pressures they faced. The data gathered was analyzed using abductive reasoning, a process that combines both deductive and inductive approaches to identify emerging themes and patterns.
From her research, Dr. Jenkins identifies a key factor in the burnout crisis: a broken social contract between the medical profession and society.
“What I’m finding is that since the 1970s, the social landscape has been changing such that physicians are putting up their end of the bargain. But they’re not getting the autonomy, respect, and trust that they thought they would receive as a result of pursuing medicine.”3
Physicians enter the field of medicine with high expectations promised in exchange for their years of education, training, and sacrifice.

However, once in practice, many physicians find themselves facing a different reality. Instead of autonomy, they face bureaucratic hurdles and third-party interference. Instead of respect, they feel unvalued and ignored. Instead of trust, they face skepticism and increasing demands from patients. According to Dr. Jenkins, this disillusionment is central to the emotional strain doctors experience. This was true for the general pediatricians, who served as “shock absorbers,” absorbing countless bureaucratic and professional demands (“shocks”) and needing to convert them into competent medical care.4 Examples of these “shocks” include the pressure to see more patients in less time and attempting to treat complex social situations (i.e., food insecurity) from the exam room. Surprisingly, this wasn’t true for pediatric surgical subspecialists. Despite working in a
“Physicians
are putting up their end of the bargain. But they’re not getting the autonomy, respect, and trust that they thought they would receive as a result of pursuing medicine.”
high-stress environment, pediatric surgical subspecialists reported higher levels of job satisfaction. The reason for this: surgeons are doing more of what they expected, facing less of a broken social contract. They not only have more control over their work, but they are more likely to engage in tasks they find fulfilling rather than administrative duties. The healthcare system supports the surgical profession, protecting them from doing nonsurgical tasks and allowing them to spend the most amount of time doing surgery. Based on this insight, Dr. Jenkins argues for the alignment of physicians’ expectations with the reality of their work. To better align career expectations with lived reality, work needs to be done within medical training and the healthcare system itself. By exposing trainees to the less glamorous aspects of the profession and implementing

changes to ensure that physicians can focus on the work they are trained to do, significant improvements will be seen in physician well-being and patient care. Physician burnout is a critical issue with consequences for both doctors and the patients they serve. Dr. Jenkins’ research offers a unique perspective, shifting the focus from individual experiences to the systemic factors that shape physician well-being. By examining the broken social contract between physicians and society, Dr. Jenkins calls for a reevaluation of medical training and the healthcare system to better align the reality of medicine with the promises made to physicians. As the medical profession evolves, Dr. Jenkins’ research will serve as a guide for policymakers and educators striving to create a healthier, more satisfied medical workforce.
1. Linzer M, Jin JO, Shah P, Stillman M, Brown R, Poplau S, Nankivil N, Cappelucci K, Sinsky CA. Trends in Clinician Burnout With Associated Mitigating and Aggravating Factors During the COVID-19 Pandemic. JAMA Health Forum. 2022;3(11):e224163. https:// doi.org/10.1001/jamahealthforum.2022.4163.
2. World Health Organization: WHO. Burn-out an “occupational phenomenon”: International Classification of Diseases. World Health Organization. 2019 May 28. https://www.who.int/news/ item/28-05-2019-burn-out-an-occupational-phenomenon-international-classification-of-diseases
3. Interview with Dr. Tania Jenkins. 4. Jenkins TM. Physicians as shock absorbers: The system of structural factors driving burnout and dissatisfaction in medicine. Social Science & Medicine. 2023;337:116311. https://doi. org/10.1016/j.socscimed.2023.116311.


Imagine a world where the secrets of our genes unlock the key to everyone living past 100 years, guided by the genetic patterns that influence aging and longevity. The field of genetics offers insights into the mechanisms that regulate lifespan, which can help scientists find ways to slow aging, prevent age-related diseases, and extend healthy living. Dr. Shawn Ahmed, a biologist and geneticist at The University of North Carolina at Chapel Hill, investigates these mechanisms through the lens of genetic changes and stress responses.
One major focus of aging research lies within the shortening of DNA. This occurs in the chromosomes, which are long strands of genetic material that carry the instructions for cell function and reproduction. These chromosomes

contain telomeres at their end, which consist of repetitive DNA, and these telomeres essentially act as caps to protect the chromosome from damage. As cells divide, the telomeres get shorter and shorter until the cell can no longer divide, causing the cell to enter an inactive state that contributes to aging and tissue decline
To understand the connection between telomere biology and aging, Dr. Ahmed conducted a series of research projects through the use of the model organism, Caenorhabditis elegans (C.elegans) to explore telomere shortening and the genetic basis of longevity and infertility. C. elegans are small, transparent worms that are widely used in scientific research for their simple anatomy, short lifespan, and well-understood genetic makeup.
Dr. Ahmed conducted lifespan studies on C. elegans that had defects in their telomeres, such as shortened telomeres or mutations that caused the telomeres to be fused together. However, despite these defects, the overall lifespans of C. elegans remained unchanged. This finding contradicted the widely held hypothesis that telomere length directly determines lifespan. Instead, it suggested that although telomeres may play a role in aging, other factors, such as genetic changes or stress-related mechanisms, may also influence longevity.
Building upon this, Dr. Ahmed turned his attention to the epigenetic regulation of telomeres. This involved
By Emily Rajappan
studying how RNA molecules influence telomere structure and function. This effect can be seen through transcription where the cell reads the DNA sequence at the telomeres and creates an RNA copy. One key focus of Dr. Ahmed’s research involved looking at this process through the discovery of a non-coding RNA transcribed from telomeres called TERRA (Telomeric Repeat-Containing RNA). This is a type of RNA that does not code for proteins but instead helps regulate telomere function and stability. Dr. Ahmed hypothesizes that it may regulate chromosome stability and cellular aging. His research proposes that another non-coding RNA, with a complementary sequence, may also interact with TERRA to influence telomere maintenance and aging pathways. It has been observed that TERRA levels increase in older individuals with short telomeres as well as in astronauts who experience telomere lengthening in the stressful environment of space. Using gene editing techniques, the Ahmed Lab is investigating whether this RNA plays a role in stress-induced telomere shortening and its extent of contribution to lifespan regulation. However, it is also important to note that studying this particular RNA presents some challenges. This RNA sequence changes rapidly, making it difficult to identify in other related species outside of C. elegans. Ultimately, Dr. Ahmed’s findings suggest that telomeric noncoding RNAs may be critical regulators of aging, potentially offering new

Figure 1. The progression of a germline cell mutants becoming sterile overtime. Courtesy of Dr. Ahmed.
insights into how epigenetic and stress factors shape longevity and aging.
Another promising avenue of Dr. Ahmed’s research includes investigating the connection between stress and reproduction age in C. elegans. To do this, he studied C. elegans germline cells. Germline cells are cells that are passed on over multiple generations and thus need certain cellular machinery to continuously divide. They are essentially considered “immortal” as they do not undergo the same aging process as regular body cells, allowing genetic information to be passed down indefinitely. However, a mutant version of the germline cells cannot continuously divide and eventually becomes sterile and unable to reproduce due to damage to their cellular machinery.
Dr. Ahmed discovered a mutant that can “transmit some type of signal that actually induces longevity”. Essentially, if an organism has a strong stress response, it can adapt and live longer. However, if it fails to respond effectively, such as with the mutant
germline cells, its lifespan is shortened. This connection was revealed when Dr. Ahmed examined a mutant deficient for PRG-1, a protein that associates with thousands of small non-coding molecules, known as piRNAs, that helps to protect genome stability by silencing harmful genetic elements such as jumping genes (DNA sequences that can relocate and disrupt genes) or DNA viruses. In C. elegans, the loss of PRG-1 leads to sterility, not due to direct DNA damage, but because of disruptions in germ granules—structures essential for regulating stress responses at the cellular level. Dr. Ahmed discovered that the fertility defect of PRG-1 mutants can cause longevity, further reinforcing the idea that this sterility acts as a stress response, where the organism prioritizes survival over reproduction. Interestingly, while these mutants lose fertility, they also tend to live longer, illustrating that aging is closely tied to how cells manage stress. Dr. Ahmed’s research suggests that the ability of germ cells to transmit stress to their offspring could be a key

Figure 2. Telomerase extends telomeres by adding repetitive DNA sequences using its RNA template, a process potentially regulated by the telomeric RNA TERRA. Courtesy of Dr. Ahmed.
factor in determining lifespan and that fertility reduction can be used as potential indicator of aging processes. Beyond his own lab, Dr. Ahmed’s lab actively collaborates with researchers outside his department, including researchers in pharmacology, evolutionary biology, the UNC Lineberger Comprehensive Cancer Center and the Duke Center for RNA Biology. Looking ahead, Dr. Ahmed aims to expand his research by further exploring other non-coding RNAs, and their potential role in aging, genome stability, and telomere function. Dr. Ahmed hopes to apply these findings to better understand how stress and aging are connected, particularly in other areas like cancer development and inherited stress. By bridging molecular biology with broader physiological processes, Dr. Ahmed’s work continues to push the boundaries of aging research, offering new insights into how the smallest molecules can shape life’s biggest transitions
1. Chadwick, L. National Human Genome Research Institute: Telomere. https://www.genome.gov/ genetics-glossary/Telomere (accessed March 2, 2025)
2. Interview with Dr. Shawn Ahmed, Ph.D
3. Spichal M, Heestand B, Billmyre KK, Frenk S, Mello CC, Ahmed S. Germ granule dysfunction is a hallmark and mirror of Piwi mutant sterility. Nat Commun. 2021, 12, 1420.
By Gayatri Venkatesan
Despite its well-known risks, alcohol use disorder remains a widespread and deeply complex condition. At the heart of this disorder are intricate brain mechanisms that drive cravings, consumption, and dependence. Understanding these mechanisms could pave the way for better treatments, yet many crucial questions remain unanswered. Dr. Joyce Besheer, a Professor of Psychiatry at the University of North Carolina at Chapel Hill School of Medicine and the Associate Director of the Bowles Center for Alcohol Studies, has dedicated her career to unraveling the neurobiology of alcohol use disorder. Her research focuses on how the brain perceives alcohol’s effects and how these perceptions influence drinking behavior, as well as stressinduced drinking and potential treatment targets for alcohol use disorder.
One of the primary areas of Dr. Besheer’s research is understanding the interoceptive effects of alcohol—how the substance changes one’s internal state and, in turn, affects behavior.2 When a person drinks alcohol, they experience physical sensations such as lightheadedness or dizziness, which help them gauge how much they’ve consumed. These sensations can either act as a signal to stop drinking or, in cases where drinking alcohol may alleviate anxiety, encourage further consumption.1 The Besheer Lab uses animal models to study these effects, training rats to report whether they

Dr. Joyce Besheer
“feel” the effects of alcohol through a method known as drug discrimination.
To employ drug discrimination methods, rats are placed in a controlled environment where they learn to associate pressing a specific lever with receiving a sugar reward, depending on whether they have been given alcohol. Over time, they develop a highly accurate ability to distinguish when they have alcohol in their system versus when they do not.1 This method allows the Besheer Lab to test how different drugs or neural manipulations alter the perception of alcohol’s effects. As Dr. Besheer explains, “We can look at novel drugs and answer the question: does this drug feel like alcohol, or does it not feel like alcohol?”1 By identifying the regions and circuits of the brain responsible for these interoceptive effects, the neurobiological basis of alcohol use disorder and the impact of factors such as stress and prior substance exposure on an individual’s sensitivity to alcohol’s effects can be determined. This information has the potential to reveal new treatment targets for alcohol use disorder.1
Another key component of Dr. Besheer’s research involves alcohol self-administration models, which allow researchers to measure voluntary alcohol consumption in animals during times of stress. Her team has found that certain active behavioral responses to stress in rats, such as digging in their bedding and increased movement, are associated with increased alcohol consumption.1 In other words, rats that exhibit more of these active stress behaviors tend to drink more alcohol.
By analyzing brain activity in these animals when they are stressed, the Besheer Lab aims to identify the neural mechanisms that drive alcohol-seeking behavior following stress. This work is particularly relevant given the high comorbidity between stress-related disorders, such as PTSD and alcohol use disorder.3 Understanding how stress alters alcohol intake at the neural level may lead to targeted interventions for individuals at high risk of developing alcohol

use disorder. Ongoing studies in the lab focus on how stress induces long-term changes in the brain, especially in systems important for learning and memory.1 One key area of focus is glutamatergic signaling, which plays a key role in synaptic plasticity and involves brain chemicals that help nerve cells communicate with each other. The lab also studies brain circuits that connect the cortex, the thinking part of the brain that is crucial for decision-making, and the limbic system, which helps regulate emotions and stress responses.4
One fascinating avenue of Dr. Besheer’s work explores the potential to treat alcohol use disorder through medications like Ozempic (semaglutide), a glucagon-like peptide-1 (GLP-1) receptor agonist initially designed for diabetes and weight management but now gaining attention for its perceived effects on substance use behaviors. Anecdotal reports suggest that individuals taking Ozempic for weight loss also experience a reduced desire to drink. In Dr. Besheer's studies, rats treated with the drug showed a blunted response to alcohol’s interoceptive effects, mirroring human reports.1 Her team is now expanding their studies to explore other GLP-1based compounds to determine whether similar effects can be replicated and to identify the mechanisms underlying this phenomenon. Since GLP-1 receptors are involved in regulating reward and motivation, they suspect that these compounds may alter alcohol-related behaviors by reducing their reinforcing properties. Understanding these pathways could open the door to novel treatments that help curb cravings

Figure 2. This image shows a representation of the alcohol self-administration cage in the
and prevent relapse, as the lab has collaborations with medicinal chemists seeking to develop novel compounds that target interoceptive pathways or stress-related drinking behaviors.1
Dr. Besheer also emphasizes the importance of studying sex differences in alcohol use disorder. Historically, addiction research has been heavily male-focused, but her lab incorporates both male and female subjects to understand differences in alcohol’s effects and treatment responses. Preliminary findings suggest that males and females exhibit distinct neurobiological changes.5 For example, the lab’s studies have revealed that female rats exhibit increased drinking behaviors following stress exposure, while males show heightened sensitivity to alcohol’s interoceptive effects. Dr. Besheer believes these behavioral responses may be driven by sex-specific molecular changes in the brain. By identifying these differences, she hopes to develop treatment strategies tailored to an individual’s biological and behavioral profile, improving the effectiveness of future interventions.1
One of the greatest challenges in addiction neuroscience is the need for personalized treatment approaches. Because alcohol use disorder manifests differently across individuals— driven by unique genetic, environmental, and chemical factors—there is no one-size-fits-all treatment. By identifying characteristics such as sensitivity to alcohol’s interoceptive effects, stress responses, and sex differences, targeted therapies that address the specific mechanisms driving alcohol consumption in different populations can be developed.1
Despite the complexity of customized care, Dr. Besheer remains optimistic about the future of addiction neuroscience. With only three FDA-approved medications for individuals with alcohol use disorder, she hopes that ongoing research will lead to more targeted treatments.1 “There’s no magic pill that works for everyone,” she explains, “but if people have more options, it increases the chances of finding something that helps.” By bridging the gap between basic science and clinical application, Dr. Besheer’s work not only enhances our understanding of alcohol use disorder but also brings the field closer to groundbreaking, individualized treatments that could transform the future of addiction care.
1. Interview with Joyce Besheer, Ph.D. 1/31/202
2. Lovelock, D.F.; Tyler, R.E.; Besheer, J. Neuropharmacol. 2021, 200.
3. Ornelas, L.C.; Tyler, R.E.; Irukulapati, P.; Paladugu, S.; Besheer, J. Behav. Brain Res. 2021, 402.
4. Jaramillo, A.A.; Randall, P.A.; Stewart, S.; Fortino, B.; Van Voorhies, K.; Besheer, J. Neuropharmacol. 2018, 130, 42-53.
5. Randall, P.A.; Stewart, R.T.; Besheer, J. Pharmacol. Biochem. Behav. 2017, 156, 1-9.
By John Wadington

Psychedelic compounds can be powerful antidepressants – but also a one-way ticket to seeing your couch talk. Now, computationallydesigned molecules can offer the same mental health benefits, minus the hallucinogenic detour.
Since their discovery, psychedelic substances have been used ritualistically or recreationally around the world. In the last few decades, they have been found to have a unique clinical aptitude for treating mental illnesses. In the United States alone, an estimated 60 million people suffer from one form of a serious mental disorder or another.1
Some “diseases of despair”

Dr. Bryan Roth
like depression and PTSD present unique challenges in treatment with therapeutic or psychiatric means. One of the most formidable roadblocks for this application of psychedelic compounds is the often unwanted hallucinogenic and perception-altering side effects.
While separating the antidepressant and hallucinogenic effects would vastly improve their clinical efficacy, such a division was seen as impossible without changing the structure of the hallucinogens themselves, which risked eliminating the therapeutic effects entirely. And even if that perfect structure existed, finding it in the innumerable chemical possibilities would be nearly impossible. Psychiatrist-turned-molecular pharmacologist Dr. Bryan Roth is tackling exactly that challenge.
Roth is the Michael Hooker Distinguished Professor of Pharmacology at the University of North Carolina at Chapel Hill School of Medicine, as well as the Director of the National Institute of Mental Health Psychoactive Drug Screening Program. Renowned for his pioneering work in G protein-coupled receptor pharmacology and synthetic neurobiology, his research focuses on designing new psychiatric drugs. Roth witnessed mental health
issues in his family from a young age, so he said he was drawn to understanding neuropharmacology before he even reached high school. He set his focus to developing non-hallucinogenic psychedelics for treating mental health issues.2
In his research, Roth explains how current psychiatric treatments for common mental health disorders like depression and PTSD rely on serotonintargeting drugs. These approaches work by increasing levels of serotonin in the brain, a neurotransmitter integral for regulating mood and other essential functions. Increased serotonin receptor binding, specifically the 5-HT2A receptor, produces profound antidepressant effects. However, these drugs require weeks to take effect, can produce undesirable side effects, and do not work at all for many.2
Conversely, psychedelics like psilocybin (found in “magic mushrooms”) and LSD activate the same 5-HT2A receptor but far quicker and with higher effectiveness. But these drugs also induce powerful hallucinations. And while these effects themselves can be undesirable, they also make the drugs difficult to test given the lack of ability to conduct a proper blind study. Their effects are not subtle. Roth said, “if

you’re in the psilocybin group, you know you got psilocybin, there’s no question”.2
For both a comfortable patient experience and proper research conduction, separating the hallucinogenic effects from the therapeutic ones is essential. To that end, Roth and his team utilized a bespoke virtual library to assess “hundreds of thousands of unique chemotypes, new to the known universe”.2,3 Such a library is a collection of theoretically possible molecules (or groups of them called chemotypes) that do not exist in nature but can be digitally generated to screen for desired properties.
Each of the millions of molecules was designed to bind to 5-HT2A receptors without inducing hallucinogenic effects, but each varied in the degree of both factors. Computational analysis was used to filter the molecules down to a short list of viable drug candidates by how strongly they would bind to the 5-HT2A receptor. The top candidates ((R)69 and (R)-70) were then synthesized, introduced in vitro to human cells, and confirmed to bind strongly to 5-HT2A receptors while avoiding stimulation of pathways which induce hallucinogenic effects (Fig. 1).3
With the success of in vitro trials, they began in vivo trials in mice and measured indicators of psychedelic activity and depressive symptoms against psychedelic and antidepressant controls. The mice, induced to have depression-like behavior, showed no signs of psychedelic activity and markedly improved behaviors. “Psychedelic drugs make mice twitch
their heads – it’s a reliable predictor of hallucinations in humans; our compounds didn’t do that” (Fig. 2).2,3
This was the first instance of an antidepressant molecule binding to the 5-HT2A receptor without the associated hallucinations. That outcome came with 1/40th the dose of the control antidepressants.3 While there is still plenty of research and development to be done before this can be tested on humans, mental health treatment could undergo a complete paradigm shift if it is ultimately successful. Treatments will no longer have to rely on slow-acting, sideeffect-heavy drugs, but rather on fast, efficient, and safe compounds. Drugs like (R)-69 and (R)-70 “will transform how we treat serious mental illnesses,” Roth said.2
While the discovery of this specific drug was undoubtedly a breakthrough, the speed and accuracy of the computational tools used was equally as groundbreaking. Utilizing

Figure 2. Head-twitch responses of mice to (R)-69, (R)-70, and LSD in varying dosages. Courtesy of Dr. Roth.
programmatic tools took the typical drug discovery timeline from years to only a few months with complete accuracy in both the molecular properties and physiological interactions. It marks a fundamental shift in how drugs for treatment-resistant disorders – or anything else – are created and tested. Even still, Roth is advancing this computational approach with a recent study of his using the deep-learning structure prediction tool AlphaFold2 (AF2). He and his team demonstrated it can match the accuracy of experimental approaches when discovering new molecules and their effects on known receptors.4 The ability to design, refine, and test completely novel compounds with such speed could revolutionize medicine as a whole, possibly even allowing for individually-designed drugs.
While Roth and his team still have refinements and tests ahead of them, with tools like virtual libraries and AF2, their research – and molecular science as a whole – is actively being redefined, one molecule at a time.
1. National Institute of Mental Health. Mental illness. National Institute of Mental Health. https://www.nimh. nih.gov/health/statistics/mental-illness.
2. Interview with Bryan Roth, MD, PhD. 2/14/25.
3. Kaplan, A. L.; Confair, D. N.; Kim, K.; Barros-Álvarez, X.; Rodriguiz, R. M.; Yang, Y.; Kweon, O. S.; Che, T.; McCorvy, J. D.; Kamber, D. N.; et al. Bespoke Library Docking for 5-HT2A Receptor Agonists with Antidepressant Activity. Nature 2022, 610, 582–591.
4. Lyu, J.; Kapolka, N.; Gumpper, R.; Alon, A.; Wang, L.; Jain, M. K.; Sakamoto, K.; Kim, Y.; DiBerto, J.; Kim, K.; et al. AlphaFold2 Structures Guide Prospective Ligand Discovery. Science 2024, 384 (6702).

By Ava Carlton
espite affecting millions globally, alcohol use disorder (AUD) remains one of the most elusive and misunderstood conditions. Heavy binge drinking can lead to severe health consequences, including addiction, liver diseases, and cognitive impairment. Despite advancements in understanding addiction’s effects, developing effective treatments remains a challenge. Researchers, like Dr. Kash, have been exploring the neurological mechanisms that direct compulsive drinking behaviors and how targeted interventions can mitigate these effects. Dr. Kash received his Ph.D. in Neuroscience at Cornell University and now researches the neurological and behavioral impacts of AUD, emphasizing the need for improved treatment approaches.
Dr. Kash focuses particularly on the amygdala, a brain region that regulates fear responses and emotional behavior. The amygdala’s function is closely tied to anxiety and stress responses, which are often linked to AUD. His research investigates how excessive drinking behaviors can cause disruptions in serotonin signaling within the amygdala and may alter stress responses, as serotonin is a neurotransmitter associated with mood regulation. Dr. Kash states, “We’ve been interested in trying to understand what alcohol is doing in the brain in terms of emotional processing and decisionmaking…we’re looking at anxiety and depressive behaviors related to heavy drinking.”2 His research team designs experiments where mice are given access to large amounts of alcohol within a short period, effectively mimicking binge drinking behavior. “We can measure serotonin levels in different brain regions during alcohol consumption and track how it fluctuates over time.”2 These experiments provide a means of observing the immediate effects of heavy alcohol

consumption on the body and brain, including physical signs of intoxication and changes in brain activity.
Understanding how these disruptions occur is vital, as serotonin plays a broader role beyond just fear responses. It is also involved in impulse control, social behavior, and the ability to regulate emotions. When these processes are compromised, individuals struggling with AUD may find themselves caught in a cycle of negative emotions and poor decision-making, ultimately leading to repeated episodes of heavy drinking. Dr. Kash’s findings indicate that reduced serotonin levels may heighten both anxiety and impulsivity, contributing to the compulsive nature of alcohol use.
The Robogator experiment is used to determine how serotonin levels and the amygdala are affected during binge drinking. The Robogator is an alligator made from Legos used to trick mice into believing a predator is attacking them. Typically, Dr. Kash found that a mouse would take about 40 seconds in this stress-induced environment to approach the cereal sitting in the middle of the room. However, the mice that were exposed to binge drinking took almost 4 minutes to approach the cereal.2 This behavior suggests that binge drinking impairs the mice’s ability to properly assess and respond to threats, likely due to alterations in serotonin levels and the amygdala’s functioning. Normally, serotonin helps regulate fear responses and decision-making, but with chronic alcohol exposure, serotonin levels in critical brain regions, like the cortex and amygdala, are lowered. As a result, the mice exhibit heightened anxiety and reduced exploratory behavior,

which could indicate an exaggerated sense of danger. This heightened anxiety and altered threat assessment can be further examined using behavioral tests, such as the light/dark box test. Rodents placed in this apparatus choose between a brightly lit, exposed area and a dark, enclosed area such as a hut. After the rodents get comfortable in their new environment, a shadow appears that resembles a predator. Rodents that are exposed to alcohol often show an increased preference for the dark area, which is interpreted as a sign of increased anxiety.2 The behavior observed in this test helps researchers assess anxiety levels and how alcohol influences stress responses. Mice that spend more time in the dark zone after being exposed to alcohol are considered more anxietyprone, which reflects an increased tendency to seek relief from stress or fear through alcohol consumption.
“It prevents people from taking care of themselves in a good ways, and I think it would be great if we lived in a country that was broadly more supportive of that.”
What makes Dr. Kash’s research particularly significant is its potential to bridge the gap between basic neuroscience and clinical application. By identifying the specific brain circuits and chemical imbalances involved in AUD, this research could open doors to novel treatments, such as medications targeting serotonin systems or therapeutic interventions aimed at restoring healthy emotional processing. His aim is to take the data he has accumulated to clinics. He emphasized the importance of cross-disciplinary collaboration, to ensure that their findings are relevant to real-world patients, allowing his work to directly benefit patients.
After dedicating most of his career to this research, Dr. Kash strongly advises the need for a more supportive and comprehensive approach to alcohol and addiction treatment. He believes that AUD should be treated with the


same level of medical attention and resources as other health conditions; “[This disparity] prevents people from taking care of themselves in good ways, and I think it would be great if we lived in a country that was broadly more supportive of that.”2 AUD is a significant public health issue due to the legality of alcohol and the normality of its consumption, and it seems to fall through the cracks of importance to government officials. Dr. Kash is striving to develop better solutions for people struggling with alcohol use disorder, believing that with the right resources and approach, meaningful change can be made in how addiction is understood and treated.
References
1. Understanding Alcohol Use Disorder | National Institute on Alcohol Abuse and Alcoholism (NIAAA). (n.d.). https:// www.niaaa.nih.gov/publications/brochures-and-factsheets/understanding-alcohol-use-disorder
2. Interview with Thomas Kash, Ph.D. 2/18/2025
By Anooshka Deshpande

Nearly 500,000 people die of intracranial aneurysms every year.1 An intracranial aneurysm, also known as a brain aneurysm, occurs when blood flow through a brain artery exerts pressure on a weakened area of the arterial wall, causing the blood vessel wall to bulge. Eventually, the vessel wall ruptures and bleeds into the surrounding tissue, leading to brain damage. Intracranial aneurysms can be life threatening in some cases. However, a healthy lifestyle can help reduce their chances.
Intracranial aneurysms have multiple treatments. A commonly used treatment is a flow diversion stent, which may be preferred over other options due to its safety, efficacy, shorter recovery period, and minimal exposure to radiation. In this technique, a mesh-shaped piece of metal called a stent is inserted into the vessel. This diverts blood flow away from the aneurysm, enabling the weakened vessel wall to heal and shrink over time. However, platelets – cells that assist in

blood clot formation at a site of a wound – may recognize the stent as a foreign object and aggregate around it. As a result, patients with a flow diversion stent need multiple months of antiplatelet therapy to prevent clot formation that could lead to poor cardiovascular outcomes. The efficacy of antiplatelet drugs varies in each patient due to individual differences in drug metabolism and response.
Dr. Craig Lee, a professor at the UNC Eshelman School of Pharmacy’s Division of Pharmacotherapy and Experimental

Figure 1. Intracranial aneurysm. An intracranial aneurysm occurs when a weakened part of a blood vessel wall bulges, exerting pressure on the surrounding tissue. Eventually, it can rupture and lead to hemorrhage in the area, which can lead to brain damage. Courtesy of Wikimedia commons.

Figure 2. Placement of stent in percutaneous coronary intervention procedure. The procedure is used to treat obstructed coronary arteries, which supply blood to the heart. Courtesy of Wikimedia commons.
Therapeutics, investigates inter-individual variability in drug response. His research focuses on how genetic factors can influence drug metabolism by the cytochrome p450 enzyme system in the liver. He conducts research studies on patients to evaluate various factors associated with their response to cardiovascular disease medications. His objective is to develop personalized medicine and improve outcomes for patients with cardiovascular and metabolic diseases.2
The cytochrome p450 enzymes are a large family of enzymes expressed predominantly in the liver. They have multiple subclasses that metabolize and detoxify drugs and various other substances in the body. An individual’s genes can affect their liver enzymes and ability to metabolize drugs. In a recent study, Dr. Lee investigated how the cytochrome p450 2C19 subclass, encoded by the gene CYP2C19, can be used to select the most effective anti-platelet drug for patients with different CYP2C19 alleles. Cytochrome p450 2C19 was studied because it metabolizes a commonly prescribed antiplatelet drug called clopidogrel. CYP2C19 converts clopidogrel to its active metabolite. Once active, the drug binds to platelets at the site of the stent and prevents them from aggregating.
The study spanned seven years and consisted of 112 patients with an intracranial aneurysm that were treated with a flow diversion stent. The researchers assessed when genetic tests were ordered and compared the frequency with which the patients used clopidogrel, an antiplatelet drug, or the alternative therapy drugs ticagrelor and prasugrel. The alternative therapy drugs used in this study belong to the same class as clopidogrel but are not metabolized by the CYP2C19 enzyme. The researchers found that CYP2C19 genetic tests were routinely ordered by physicians and patients who were poor or intermediate metabolizers of clopidogrel used alternative therapy drugs more often. They also observed that the number of thromboembolic events, which occur when a blood clot obstructs a vessel, did not vary drastically across patients who received clopidogrel or who took alternative therapy drugs. This reveals that CYP2C19 testing can be successfully used to determine the appropriate antiplatelet drug a patient should receive after undergoing an intracranial stent procedure.3
Although more research is needed, the results of this
study suggest that patients who undergo genetic testing and are prescribed antiplatelet agents according to their testing results have better outcomes. CYP2C19 testing can be used in a variety of procedures that place stents in blood vessels to improve blood flow. For instance, patients undergoing a percutaneous coronary intervention procedure, where a stent is placed inside the coronary arteries due to plaque buildup, routinely undergo CYP2C19 testing at UNC Medical Center to determine the antiplatelet drug that will be most effective for them.4
Patients who undergo genetic testing and are prescribed antiplatelet agents according to their testing results have better outcomes.
In the future, Dr. Lee anticipates collaborating with neurovascular specialists, cardiologists, and pharmacists to test the effectiveness of this strategy in patients with neurovascular diseases. He also hopes to identify factors that are responsible for certain subsets of patients experiencing a higher benefit from taking certain cardiovascular medications. An obstacle that he foresees is educating healthcare professionals on how and when to use genetic testing to optimize prescription of medications. Genetic testing can raise ethical questions about the circumstances under which it should be used, and every provider has a different opinion about it. As a result, it may take time for the use of genetic testing to select treatment options to become widespread. However, genetic testing has proven to be powerful in predicting responses to antiplatelet and other treatments. Wouldn’t it be incredible if we could optimize patient outcomes by delivering medications that maximize benefits for all patients?
1. “Statistics and Facts.” Brain Aneurysm Foundation, https://www.bafound.org/statistics-and-facts/#:~:text=The%20annual%20rate%20of%20 rupture,victims%20 are%20 younger%20than%2050.
2. Interview with Craig Lee, Pharm.D., Ph.D., 02/06/2025.
3. Fox, Layna P et al. “Real-world evaluation of CYP2C19 guided antiplatelet therapy in patients undergoing intracranial aneurysm repair.” Pharmacogenomics vol. 25,12-13 (2024): 503-513. doi:10.1080/14622416.2024.2406213
4. Lee, Craig R et al. “Clinical Outcomes and Sustainability of Using CYP2C19 Genotype-Guided Antiplatelet Therapy After Percutaneous Coronary Intervention.” Circulation. Genomic and precision medicine vol. 11,4 (2018): e002069. doi:10.1161/CIRCGEN.117.002069
By Sanjana Farmah

Close your eyes. Breathe. Take a moment to think about a mindful moment that brings you peace. Is it the beach?
The mountains? An ice cream shop? You playing your sport? Whatever it is, just think about. Now, exhale”. What did you think about? If it was your sport, you may not be the only one who finds peace from it. Sports psychology is a growing field and Dr. Shelby Baez, an Assistant Professor in the Exercise and Sport Science Department at the University of North Carolina at Chapel Hill, is at the forefront.
A UNC-Chapel Hill alumna, Dr. Baez earned her Master of Science in Athletic Training at the University of Kentucky. During that time, Dr. Baez worked as an athletic trainer for the University of Kentucky’s equestrian, archery, volleyball, basketball, soccer, and softball teams. Here, Dr. Baez personally witnessed an athlete tear their ACL and immediately thought, “How can I motivate [this athlete]? How can I help this [athlete] feel more confident to do this jump?”. This inspired Dr. Baez to gain a passion for research. She continued on to earn her

Ph.D. at the University of Kentucky and returned to UNCChapel Hill in 2022. At UNC-Chapel Hill, Dr. Baez is the Director and Principal Investigator of the Psychology of Sport Injury Laboratory at the MOTION Science Institute. Her lab studies how mindful mediation techniques and virtual reality can help rehabilitation in athletes who have injured their Anterior Cruciate Ligament (ACL). Currently, sports injury research primarily focuses on how biological factors, such as age, race, and gender affect sports injuries. However, Dr. Baez believes that is also important to think about how “psychological and the social factors may be impacting [patient] outcomes after injury”. 1
The ACL, the center of Dr. Baez’s research, is a key ligament in the knee and is responsible for connecting the femur (thigh bone) to the tibia (shin bone). Injuries to the ACL occur in sports with sudden stops, sudden changes in direction, jumping, and landing like soccer, basketball, and gymnastics. ACL injuries.2 Between 100,000 and 200,000


Figure 2. Functional MRI depicting activation of thalamus after participant was shown a series of 40 sport-specific movement pictures and 20 daily living moving pictures. This study aimed to understand what neural factors can cause fear post-ACL construction in female athletes. Courtesy of Dr. Baez.
Americans tear their ACL each year.3 Additionally, one-third of athletes who suffer an ACL tear in one leg are likely to tear their ACL in the non-injured one.2 Recovery can take anywhere from 6-12 months.3 Dr. Vehniah Tjong from Northwestern Medicine states that “...if you tear your ACL, you may lack the ability to control any cutting or pivoting through the knee”. ⁴
Women are two to eight times more likely to tear their ACL then men because of anatomical and hormonal differences between the sexes.2 For example, woman have wider hips then men, which causes their knees to tilt inward more than men. This inward tilt is known as knee valgus, and can put an individual more at risk for injury. Women also land with straighter knees and less core engagement then men. Hormones also play a huge role in this difference. Testosterone causes men to have thicker ACLs then women, while the menstrual cycle enables women’s ligaments to become loose and more prone to injury.⁴ For example, in the pre-ovulatory phase of their menstrual cycle, women become more likely to injure their ACL because estrogen levels increase. This increase in estrogen decreases the body’s synthesis of collagen, which is essential for skin, bones, and cartilage, and makes the already thin ACL even more elastic. Thus, overall, women are more at risk of tearing their ACL.⁵
Currently, Dr. Baez is conducting a study with both male and female participants who had an ACL injury and are now between six months to ten years post-operation. The study requires participants to come into the lab three times per week for eight weeks. During their first visit, Dr. Baez meets with the participant to establish a baseline assessment about how they are feeling. Virtual reality techniques focus on improving jump-landing mechanics and brain activity. Additionally, through the use of 3D Motion Capture (similar to CGI in Hollywood), the lab can look at reaction times and limb symmetry between the injured and uninjured limb. She assesses their equal limb symmetry and conducts a functional MRI. Equal limb symmetry can decrease the likelihood of injury and ensure that both limbs are gaining strength equally. A functional MRI, during which participants will be shown
images of people doing various activities such as simply walking on the beach, playing with their dog, and more, will assess how the injured athlete’s mind is responding to certain cues.1
The emphasis on biopsychosocial factors on injury recovery is a growing field that has garnered support following the COVID-19 Pandemic
Dr. Baez’s lab also collaborates with two other faculty members from the Exercise and Sport Science department: Dr. Brian Pietrosimone and Dr. Erik Wikstrom. The Pietrosimone Lab focuses mainly on how walking gait patterns changes following ACL injuries in female athletes. The Wikstrom Lab looks at how the psychological assessments that the Baez Lab uses can help with ankle instability. She also collaborates with an orthopedic surgeon at UNC to see if the techniques used in her lab can help with discovering more about the rotator cuff. Dr. Baez hopes that these collaborations can help to uncover more about the various extremities of the body and continue to promote a more biopsychosocial (biological, psychological, and social) approach to helping injured athletes. She says that “while these things are influencing each other, we can’t just measure one thing and substitute it for [something else]”.1
Other than learning more about ACL injuries, Dr. Baez hopes to find a way to help injured athletes overcome the fear of reinjury so they can go back to the sport they so dearly love. Fear can cause changes in form and dangerous compensations that can put the athlete at risk for a repeated injury, or even a more severe one. Ultimately, Dr. Baez and her team hope that the recovery techniques they are developing can be used by both injured athletes and non-athletes to help reduce risk of injury in everyday life.1
1. Interview with Baez, Ph.D., ATC. 02/13/25.
2. Mayo Clinic Staff. ACL Injury. Mayo Clinic. https://www. mayoclinic.org/diseases-conditions/acl-injury/symptoms-causes/syc-20350738 (accessed March 5th, 2025).
3. Cleaveland Clinic Staff. ACL Tear. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/16576-acl-tear (accessed March 17th, 2025)
4. Tjong, K. V. Why Women Have More ACL Injuries Than Men. Northwestern Medicine. https://www.nm.org/healthbeat/healthy-tips/why-women-have-more-acl-injuriesthan-men (accessed March 5th, 2025).
5. Balachandar, Vivek. et al. Effects of the menstrual cycle on lower-limb biomechanics, neuromuscular control, and anterior cruciate ligament injury risk: a systematic review. Muscles Ligaments Tendons J. 2017, 7(1), 136–146. https:// doi.org/10.11138/mltj/2017.7.1.136 (accessed March 17th, 2025).

There’s an immense amount of human suffering in the chronic pain population,” Dr. Mauck says earnestly as he discusses his research involving chronic lower back pain.1 Dr. Matt Mauck is an anesthesiologist at the University of North Carolina at Chapel Hill School of Medicine whose research focuses on analyzing patterns in chronic pain to devise optimal treatments and discovering the pathogenesis, or the process of development, of chronic pain. Dr. Mauck is part of a group of investigators in the NIH Biomarkers for Evaluating Spine Treatments (BEST) study, a clinical research program that aims to address the limitations in chronic lower back pain (cLBP) diagnosis and treatment.
In the past, chronic pain such as cLBP was treated most often with opioids, but, in the wake of the opioid epidemic, there are now a number of opioid-free treatments that exist to treat this condition. However, not all treatments work on all patients, and there’s no set criteria for prescribing patients a specific treatment based on their personal health profiles.2

By Aditi Gajavelly
The BEST trial targets this issue by analyzing the effectiveness of various back pain treatments in relation to patients’ biomarkers, a wide range of measurable signs and signals within the body. This type of analysis, in which treatment is selected based on a patient’s personal health and history, is called precision medicine.
To apply precision medicine algorithms to cLBP, researchers in the BEST trial worked to determine four types of effective, non-opioid treatments.2 Next, a wide range of participants were enrolled in the study across 14 sites throughout the country. These participants were randomly assigned a treatment out of the four, and their progress was then monitored over a 12 week period. After that period, participants in the study were then assigned a second treatment depending on their response to the first intervention.1 Biomarker data–including everything from blood tests and brain imaging to movement analysis using advanced biomechanical techniques–was collected in an initial patient

1. This image shows blood tests, which are one of the many ways that biomarkers are collected for precision medicine. Courtesy of rawpixel.com.
screening. This data is essential to precision medicine, as it enables the development of an algorithm which helps predict the most optimal treatment options for each individual patient. The data analysis is currently an ongoing process, but the hope is to eventually be able to link particular biomarkers to more effective treatment options, so that in the future, a patient with a specific biomarker will be able to find an optimal treatment without much trial and error.
But why is it important to find these optimal treatments in a timely manner? If back pain is chronic, does that not mean that we have more time to treat it? While it is true that back pain is often a life-long condition, finding working treatments early can not only decrease the intensity of the pain, but can also improve day-to-day functionality. Dr. Mauck said that when they “ask patients: do you care about functionality or pain intensity, they say functionality.”1 Functionality is crucial to treating chronic pain, because it allows patients to perform activities essential to their daily lives and be there for their friends and family. By finding optimal treatment options more quickly, a patient is offered a higher quality of life for a longer period of time.
“There’s an immense amount of human suffering in the chronic pain population”
While precision medicine is incredibly useful, its relevance is derived directly from the data that is collected. Therefore, it is important that the data is representative of the overall population. Dr. Mauck stressed that the BEST trial focused on collecting data from a diverse range of patients, focusing specifically on racial and gender diversity, so as to better replicate the population of the United States suffering from cLBP.1
The researchers also focused on diversity within the four treatment options given. Each treatment selected falls into a separate category of treatments: behavioral, medication, movement, and self-management. For the first category of behavioral treatments, acceptance-commitment therapy was selected as an option. This therapy is offered by licensed therapists who help the patients do exactly what the name says– accept their pain and commit to devising a plan to reduce the effect of pain on their functionality. It strives to help patients mentally prepare to live and thrive with their chronic pain, thereby allowing it to exert less control over their lives. The second treatment is the use of an antidepressant medication called duloxetine. Though this medication is an antidepressant, duloxetine is able to target pain by blocking the reuptake of serotonin and norepinephrine. These neurotransmitters, or chemicals in the brain, help control the brain’s perception of pain and can therefore lower the intensity of chronic pain.3 The third treatment option involves exercise and manual therapy intervention, in which the patients work with physical therapists to develop an exercise treatment plan to lessen the effect of their symptoms. The fourth and final treatment option is more abstract in nature, and is simply

Figure 2. This image demonstrates manual therapy, which was one of the four back pain treatments used in the trial. Courtesy of Snyder Family Chiropractic.
labeled self-management.⁴ Dr. Mauck mentions that some patients would rather take the initiative of managing their own pain. He says that for such patients, more freedom is given in terms of a treatment plan.1 All four of these treatments were clinically proven to be beneficial to cLBP and were carefully chosen due to the strength of the evidence supporting their effect.⁴
Chronic pain is one of the most widespread ailments in the adult population and is a leading cause of disability, with nearly 59% of adults reporting some kind of pain, and 39% specifically reporting back pain.2 Chronic lower back pain is an issue that almost everyone will have to face at some point in their lives, whether it be personally or through a friend or family member. By investing our time into developing a more streamlined and precise method of treatment for back pain, day-to-day functionality can be maintained and patients’ quality of life can be drastically improved. But above all, treating chronic pain will help erase at least some aspects of human suffering, allowing us to contribute to a world with fewer limitations and more living.
References
1. Interview with Dr. Matthew Mauck, MD. Ph.D. 2/20/25
2. Mauck MC; Lotz J; Psioda MA; Carey TS; Clauw DJ; Majumdar S; Marras WS; Vo N; Aylward A; Hoffmeyer A; et al. Pain Medicine 2023 24
3. Lunn MPT; Hughes RAC; Wiffen PJ; CDSR 2014 1:CD007115
4. Mauck MC; Aylward AF; Barton CE; Birckhead B; Carey T; Dalton DM; Fields AJ; Fritz J; Hassett AL; Hoffmeyer A; et al. PAIN Reports 2022 7(5)
By Shritha Gayathri


The U.S. healthcare system has historically been built with a reactive mindset, focusing significantly on symptom and treatment management after an illness has emerged. As a result, the critical value of early detection and preventative care has been extensively overlooked in the medical and scientific community. Having grown up in a medical desert in rural Indiana, Dr. Melinda Yates is no stranger to the prevalence of inadequate health care in underserved communities. An Associate Professor at UNC School of Medicine’s Department of Pathology and Lab Medicine, Dr. Yates is committed to shining light on the complex and dynamic molecular character of uterine cancer, a severely understudied disease despite being the most common gynecologic cancer in the United States. Her passion lies in improving cancer prevention and cancer interception, which she believes is the key to drastically improving health outcomes for women at increased risk for developing uterine cancer and eliminating disparities in underserved populations.
The Yates Lab studies cancers
that form in the lining of the uterus (the endometrium) and specifically works to discover blood-based or tissue biomarkers that link social and environmental factors to the development of endometrial cancer. Cancer interception relies heavily on biomarkers, defined as “measurable biological indicators that can reveal information about a person’s health, including the presence, type, or progression of cancer”.2 Some commonly encountered biomarkers for disease risk include genetic mutations, body mass index (BMI), and hormone levels. In cancer, biomarkers serve as an important tool for diagnosing and monitoring cancer during and after treatment.2 In the context of uterine cancer, obesity is considered to be a very significant risk factor, with nearly 57% of endometrial cancers in the United States believed to be attributable to being overweight or obese.3 However, using obesity as the sole biomarker can
be problematic because it is determined by measuring a person’s BMI based on height and weight, and BMI is not a universal measure of health or metabolic dysfunction. Therefore, BMI cannot be used to make medical generalizations across diverse populations. Furthermore, most women with obesity will never develop uterine cancer. Obesity itself is also a multifactorial and complex condition that is heavily influenced by genetic, environmental, and behavioral components. Dr. Yates adds that, “the clinical and biological heterogeneity within the label of “obese” is extraordinary…” and “using these labels has prevented us from really understanding the biology behind uterine cancer”.1 Stigma or shame around high BMI or an “obesity” label can negatively impact patientdoctor relationships.3
use a variety of approaches to decipher the specific biomolecular differences between tissue samples, including analyzing certain cell signaling pathways and evaluating the role of inflammation across a spectrum of risk. Such biomarkers provide precision beyond just height and weight, which allows for a better assessment of risk in each patient and ultimately maximizes the targeted medical support and intervention available to them.
“UNC is thinking about health over a lifespan… and we have the opportunity to engage with and learn from people.”
The task of researching preventative health is not an easy feat–especially for diseases affecting an organ as dynamic and ever-changing as the uterus. Through menstrual cycles, childbirth, and menopause, the uterus is constantly adapting and changing. These remarkable changes highlight a need for context-specific and rigorous research methodology when studying uterine cancer. Dr. Yates and her team can discover more specific biomarkers for characterizing uterine cancer by examining molecular changes in tissues. They use uterine tissue from biopsies and hysterectomies from patients with a broad range of clinical characteristics. One patient, for example, may currently have endometrial cancer, while another may have a precancerous lesion. A third sample may come from someone who does not have cancer but is solely at risk due to hereditary conditions. Using tissues from a diverse mix of participants, all representing various levels of cancer risk in the uterus, enables the Yates group to draw patterns between tissue samples to understand how the organ is evolving over time and how this reflects risk of developing cancer. They
Uterine cancer is a highly intersectional field, demanding specificity and dedicated attention when crafting preventative testing. The Yates Lab tackles these challenges with hope and determination. The research done at the Yates Lab will provide medical professionals with the knowledge needed to not only efficiently identify the greatest risk, but also to track and address it. Yates hopes these results can eventually inform clinical trials and provide insight into patient selection and prediction of treatment response.
Dr. Yates’ research mission undoubtedly embodies the principles of public health and preventative care. UNC-Chapel Hill, she claims, is the perfect place for her to combine her love for women’s health, public health, and cancer research: “UNC is thinking about health over a lifespan… and we have the opportunity to engage with and learn from people before we’re thinking about how to treat this nasty advanced cancer”.1 By working with professionals across various health sub-specialties, from biomedical engineering to geriatrics, Dr. Yates can help instill a lasting impact and account for the multi-dimensional nature of women’s health. She is also dedicated to transcending her research beyond the laboratory, aiming to improve science literacy and engage patient perspectives in her methodology.
As America’s aging population is projected to grow in the next decade, the prevalence of cancer will only increase.
There is a dire need for preventative care in this field, and Dr. Yates is committed to ensuring that the health of minority and overlooked populations remains at its forefront.
1. Interview with Melinda Yates, Ph.D. 02/28/2025.
2. Biomarker Testing for Cancer Treatment. https://www.cancer. gov/about-cancer/treatment/types/ biomarker-testing-cancer-treatment (accessed March 10th, 2025)
3. Tomiyama, A. J.; Carr, D.; Granberg, E. M.; Major, B.; Robinson, E.; Sutin, A. R.; Brewis, A. How and Why Weight Stigma Drives the Obesity ‘Epidemic’ and Harms Health. BMC Med. 2018, 16 (1), 123. https://doi. org/10.1186/s12916-018-1116-5.
By Ashley Hardner

New surgical, pharmacological, and even biotechnology to restore and improve human life are being continuously developed, seemingly shattering existing limitations with every new iteration. However, other fundamental areas of patient care are lagging behind. Decision-making, a powerful tool in patient care, notably falls into this category. Based on their

unique training and field experience, different physicians may suggest different solutions to the same problem. Some will be closer to the perfect offer than others, and this variability inevitably leads to a small percentage of unexpected poor outcomes, but how do we narrow the gap? Dr. Mark Attiah, a neurosurgeon at UNC Hospitals who specializes in spine and peripheral nerve surgery, is working to tackle this question.
Dr. Attiah hopes to develop a machine learning algorithm that harnesses large databases of patient outcomes to curate a unique outcome prediction for each patient who enters his clinic. The algorithm will help physicians and their patients determine what procedures or treatments will be the most beneficial for the individual: “I am not interested in discovering a novel cure for a disease, but I am very interested in how we optimize patients’ outcomes with what we’re already doing and trying to maximize the practices we currently have.”
The first step in developing his
model is growing databases of pertinent patient outcomes.1 Dr. Attiah, along with spine surgeons from UNC Orthopedics, is working on collecting this kind of information via a pilot program called Patient IQ. This pilot program aims to create a UNC specific spine registry and hopefully leading to a merger with the American Spine Registry, which would allow for a much larger database to be accessed for the computer model to learn from. The data collection will occur by having patients fill out a questionnaire, the answers of which can then be uploaded into their chart and added to the UNC specific database. Dr. Attiah and his colleagues are particularly excited for this vast amount of data collection because, “The more diverse patient outcomes and types of patients or scenarios that the computer sees, the better it can recognize different issues. Ideally, we would get as much data from as many different places as possible.”1
An algorithm trained on these databases will have the capability to generate patient specific options for their unique demographics by sorting
through significantly larger volumes of data than a physician is able to, which is vital because “In surgery, a lot of the success of the surgery has already been determined just by selecting the right patient,”1,6 and using a computer model to sift through the vast amounts of information required to make such a decision will hopefully minimize the chance of poor patient selection. This work is particularly important “... for peripheral nerve and spine cases, [where] pain and subjective outcomes are the gold standard of outcomes... We
”We are not looking at survival, mortality, or progression of disease, we’re looking at how well the patient feels.”
are not looking at survival, mortality, or progression of disease, we’re looking at how well the patient feels.”1
Another consideration pertinent to the world of spine surgery is the outsized role of imaging in determining the care plan for a patient. However, Dr. Attiah explains that simply knowing that there is an anatomical difference is not always helpful when determining how to help the patient. If a patient complains of back pain, there are plenty of other factors that might be causing it, and thus different options for treatment may be suggested. Instead of simply looking at the image and saying, “it looks like this, so we will do this to fix it,” Dr. Attiah and his colleagues worked on a way to use machine learning to quantify MRI scans. This form of image analysis is one key component Dr. Attiah plants to incorporate in his computer model for spine surgery. 1,3,⁴
Dr. Attiah believes that this concept is much closer to being a reality in spine surgery than peripheral nerve surgery. Given that the computer model’s accuracy relies on referencing extensive amounts of data, the data must exist to begin with. Peripheral nerve surgery remains a small subspeciality with only a few surgeons nationwide specializing in this field. Because of that, there is simply less data, and few substantial outcomes publications to be referenced,
an area where Dr. Attiah is actively contributing. He hopes to bring more resources to UNC Health not only so that UNC can serve patients in need of these procedures, but to subsequently enable him to continue improving the field by incorporating these patient outcomes into his research models.1
Although the field remains in its infancy, Dr. Attiah is excited by the prospect of incorporating peripheral nerve surgery outcomes into his computer model in the future and is eager to continue his endeavor to create a personalized decision-making model regarding spine surgery. While so much of the focus on modern medical innovation remains in the realm of developing new drugs or ways to sustain life, Dr. Attiah’s goals are bound to be just as highly important when it comes to positively impacting patient care.
1. Interview with Dr. Mark Attiah (9/24/24)
2. Wilson, B., Gaonkar, B., Yoo, B., Salehi, B., Attiah, M., Villaroman, D., Ahn, C., Edwards, M., Laiwalla, A., Ratnaparkhi, A., Li, I., Cook, K., Beckett, J., & Macyszyn, L. (2021). Predicting spinal surgery candidacy from Imaging Data Using Machine Learning. Neurosurgery, 89(1), 116–121. https:// doi.org/10.1093/neuros/nyab085
3. Gaonkar, B., Beckett, J., Attiah, M., Ahn, C., Edwards, M., Wilson, B., Laiwalla, A., Salehi, B., Yoo, B., Bui, A. A. T., & Macyszyn, L. (2021). Eigenrank by committee: Von-Neumann entropy based data subset selection and failure prediction for deep learning based medical image segmentation. Medical Image Analysis, 67, 101834. https://doi. org/10.1016/j.media.2020.101834
4. Stein, S. C., & Attiah, M. A. (2015). Clinical prediction and decision rules in Neurosurgery. Neurosurgery, 77(2), 149–156. https://doi.org/10.1227/ neu.0000000000000818
Image courtesy of FMT

By Angelina Ho
nfectious diseases are an everpresent threat, requiring continuous advancements in diagnostic research to manage outbreaks effectively. With extensive experience in pandemic flu, Zika virus, and COVID-19 research, Dr. Melissa Miller has dedicated her career to improving real-time detection methods that enhance patient care and public health responses. Her journey in medical microbiology sparked during the first SARS outbreak, where she was involved in the early stages of diagnostic test development. Over the years, her expertise expanded as she tackled emerging diseases, adapting diagnostic test development methodologies to evolving pathogen challenges.

In early 2020, as SARS-CoV-2 rapidly spread despite pandemic precautions like mask-wearing and social distancing, Dr. Miller and her team recognized the urgent need for more accurate diagnostic tools to distinguish COVID-19 from other illnesses with similar symptoms. Faced with many unknowns surrounding the virus, Dr. Miller aimed to contribute to the scientific understanding and literature of COVID-19. “The ultimate goal for me is how do I walk away from this project and know we impact healthcare and improve patient care,” said Dr. Miller, Director of the Clinical Molecular Microbiology Laboratory and Principal Investigator.1 Driven by this mission, she and her team set out to develop molecular assays—laboratory techniques designed to detect genetic material with high specificity and sensitivity—to identify SARS-CoV-2. Their work soon expanded to include other respiratory and non-respiratory viruses, underscoring the need for accurate, swift, and comprehensive diagnostic solutions.
A critical component of her research involved analyzing patient samples to assess the prevalence of various viruses. Using high-level biosafety laboratories, Dr. Miller
“Research isn’t about publishing papers; it’s about making a realworld impact.”
and her team conducted controlled experiments to study viral genetic material. By late 2020, her team had begun investigating genomic sequencing for SARS-CoV-2 to identify specific resistance factors in the virus that limit efficient and enhanced patient treatment. This work underscored the critical need for precise molecular testing, particularly in differentiating between closely related viral families like rhinovirus and enterovirus D68 (EV-D68). More specifically, the research focused on analyzing the 5’ untranslated section of messenger RNA—a region evolutionarily preserved in viral genetic makeup, essential in regulating protein production for reproduction. Thus, investigating the 5’ UTR offers vital insights for refining diagnostic tools and guiding treatment strategies, improving patient outcomes in the face of emerging viral threats.
The Open Forum Infectious Diseases reported that EV-D68 cases
spiked during specific seasons, leading to significant respiratory complications in children.2 “We began receiving inquiries from clinicians noticing an uptick in asthmarelated hospitalizations,” Dr. Miller recalled.1 In response, her team launched a retrospective study in 2022 to determine if EV-D68 contributes to the rise in respiratory issues. For two years (2022 and 2024), Dr. Miller’s team collected and analyzed hundreds of patient samples using real-time reverse polymerase chain reaction (RT-PCR), a key technique for detecting genetic material in DNA and RNA viruses. The process begins with the purification of the samples to isolate nucleic acids—the genetic material of DNA and RNA—using an advanced machine called eMAG. These purified nucleic acids are then amplified and detected through RT-PCR after being mixed with a master mix—a pre-formulated solution containing all the necessary components for the RT-PCR reaction (Figure 1).
“We had to test an extensive number of samples from both the fall and winter seasons, which at times made us wonder if we could even complete the study,” said Dr. Miller.1 Therefore, collaboration was also fundamental to these projects. Dr. Miller worked closely with infectious disease specialists, pediatrics, fellows, and an undergraduate student to ensure research goals aligned with clinical needs. “One of my favorite aspects of my work is the ability to partner with clinicians and researchers from various fields,” said Dr. Miller.1 They identified many positive EV-D68 cases, revealing important insights into the virus’s prevalence in pediatric populations and reinforcing the critical need for ongoing surveillance of emerging respiratory pathogens (Figure 2).

Currently, a major research focus involves examining the ongoing circulation of Mpox (formerly known as monkeypox). According to the Division of Infectious Diseases and Geographic Medicine, global Mpox testing rates in 2022 suggested that decreased testing efforts may cause unreported cases.3 This raises concerns that the virus had become endemic (regularly occurring within an area or community) but was overlooked. To explore this hypothesis, Dr. Miller’s team analyzed stored clinical samples initially tested for the herpes virus. The study


sought to determine whether Mpox was still circulating at low levels but not detected due to a lack of routine testing. After months of rigorous testing (and still ongoing), Dr. Miller’s research team has found no positive Mpox case. “We expected to see at least a few positive cases based on previous outbreak trends, but so far, we have found none,”1 Dr. Miller said. As this challenged their hypothesis about its persistence, it raised imperative questions about whether their sample selection represents at-risk populations. It also prompted discussions on whether the decline in cases was due to natural reductions in transmission or simply a reflection of decreased surveillance effort. Therefore, Dr. Miller emphasizes the importance of well-designed methodologies in scientific research. “You have to be clear about your hypothesis and ensure you have appropriate control groups,” Dr. Miller shared.1
Dr. Miller aims to transform public health interventions and improve patient outcomes across diverse healthcare settings. “Research isn’t just about publishing papers; it’s about making a real-world impact,” she emphasized.1 Dr. Miller highlights the importance of turning scientific knowledge into tangible benefits for individuals and communities. By enhancing diagnostic capabilities, her studies contribute to more accurate disease surveillance, leading to better patient care, earlier interventions, and a deeper understanding of emerging infectious threats. As new challenges arise, Dr. Miller’s unwavering commitment to transforming research into practical solutions lays the groundwork for a future where healthcare is more responsive, effective, and accessible to all.
1. Interview with Melissa Miller, PhD. 02/27/25.
2. Amary Fall.; Omar Abdullah.; Lijie Han.; Julie M Norton.; Nicholas Gallagher.; Michael Forman.; C Paul Morris.; Eili Klein.; Heba H Mostafa.; et al. Open Forum. 2024.
3. Dhillon, R. S.; Karan, A.; Srikrishna, D.; Mombouli, J.-V.; et al. The Lancet. 2024, 1193–1194.

By Madelyn Holleman
When we think about school lunches, we often think of square pizza and milk. We might not have fond memories of it, but most of us agree that even lessthan-stellar lunches were better than nothing. Unfortunately, some children only get the latter; they do not get to choose to opt out of the hamburger surprise because they cannot afford to opt in. Fortunately, researchers such as Dr. Jessica Soldavini and her team– consisting of nine core staff and varying numbers of students– are trying to help.1 Dr. Soldavini studied nutrition at UC Berkeley and eventually earned a Ph.D. in the field at the University of North Carolina at Chapel Hill.1

Image courtesy of USDA
Before earning her Ph.D., Dr. Soldavini worked as a public health nutritionist, during which she worked with the SNAPEd (Supplemental Nutrition Assistance Program – Education), which focuses on helping low-income individuals and those eligible for SNAP make healthy choices. Once she came to UNC-Chapel Hill, she became involved with No Kid Hungry NC and started doing work on the summer and school meal programs.1
Dr. Soldavini’s work involves different federal assistance programs, including SNAP and SUN Bucks (the newest USDA nutrition assistance program, providing food benefits to families of eligible children to be able to purchase groceries when the kids are not in school), as well as nutrition and culinary education in K-12 and college students.1 One of her most recent projects involved working with Albert Pan, a former student, to investigate school meal charge policies for students who are required to pay for reduced or full-price meals (as opposed to those who receive them for free).3 North Carolina does not currently provide free meals for all students;2 however, there is the Community Eligibility Provision, which allows schools with a high enough proportion of students who qualify for free and reduced meals to serve free meals to all students.4 Some students come from families that cannot afford the cost of the meals and end up with unpaid meal charges, likely because they are barely above the minimum income requirement.2 As Dr. Soldavini and her team found, school districts across the state have different policies regarding this debt: some will still provide students meals, others will not; some even send debt collectors after the families or call social services for potential child neglect.
According to Dr. Soldavini, one of the biggest challenges posed by these programs is that many children may benefit from school meals but cannot afford them. There are
also barriers to participation for eligible children; when some students receive free meals and others do not, there is a stigma against those who do.1 This stigma explains why high schools have the lowest rates of participation in free meal programs. The main strategy she suggested to address these obstacles is making school meals available at no cost to all students. Making school meals free for all students would eliminate the stigma surrounding students who receive free meals, as well as ensure access to students whose families are above the minimum income requirement but still cannot afford meals.1 During the COVID-19 pandemic, there were waivers in place that made meals available at no cost to students.1 After the pandemic, these waivers went away. Some states, including New Mexico, Maine, and others, proposed legislation where all students could eat for free, though North Carolina was not one of them.5 Dr. Soldavini and her team are part of School Meals for All NC, which is a coalition fighting to ensure free school meals for all students.1
According to Dr. Soldavini, one of the biggest challenges posed by these programs is that many children may benefit from school meals but cannot afford them.
When conducting her research, Dr. Soldavini described using a variety of methods, including literature reviews, surveys and interviews with school nutrition directors and other individuals involved with school meal programs, content analysis, and analyzing administrative data. Much of her work is very collaborative, as she explains here: “It is very important, especially given the nature of my work, to collaborate with those from the organizations who are doing this work.”1 Some of these organizations include the North Carolina Department of Public Instruction, which oversees school and summer meals programs, and the North Carolina Department of Health and Human Services, which oversees SNAP and SUN Bucks; and various school districts. She does most of her work in collaboration with Carolina Hunger Initiative and No Kid Hungry NC. She works with the former to create annual profiles with data on school meal programs, allowing people across the state to have that information. Her team consists of individuals from a variety of backgrounds aside from nutrition and public health, including communications, social work, and others.1
Dr. Soldavini says the most exciting aspect of her work is its potential impact, knowing that she is doing work that can make a difference. When deciding what to research, she asks herself, “How can I help get information that is going to be of value to people, that they can use?”1 She considers herself a researcher, a practitioner, and an educator, with the desire to apply research to practice and policy-based work
at the core of her work. To her, one of the best parts of her research is that people can use the data. Instead of it sitting somewhere for another researcher to maybe read and cite, people in the field can use it.1
In the future, Dr. Soldavini would like to continue to evaluate the different school and nutrition programs, particularly for college students.1 Her team launched NC College Food Benefits, a state-wide SNAP outreach campaign focused on helping college students become connected to federal nutrition assistance. She has another study working on creating a nutrition and culinary education intervention for college students. There is still much to be done regarding school nutrition programs and providing access to meals for all children, but the work done by Dr. Soldavini and her team is helping us get there faster.
1. Interview with Jessica Soldavini, Ph.D. 2/7/25.
2. Pan, A.; Soldavini, J. Journal of Nutrition Education and Behavior 2024, 56, 736-741.
3. North Carolina Department of Public Instruction. Eligibility for Free or Reduced Price Meals in the National School Lunch Program. https://www.dpi.nc.gov/ news/press-releases/2024/08/08/eligibility-free-or-reduced-price-meals-national-school-lunch-program (accessed Feb 28, 2025).
4. United States Department of Agriculture. Community Eligibility Provision. https://www.fns.usda.gov/cn/cep (accessed Feb 20, 2025).
5. Karnowski, S., & Bryan, S. M. Schoolkids in 8 states can now eat free school meals, advocates urge Congress for nationwide policy. https://apnews.com/article/ free-school-meals-0c927f491b2ee9d4ce7e04b44da79e51 (accessed March 26, 2025).
By

For decades, an HIV diagnosis meant a death sentence. Today, with the help of antiretroviral therapy (ART), infection has become largely controllable. It has helped patients live a normal lifespan with a healthier body and significantly reduced the risk of transmitting the virus to others. The “treatment as prevention approach” became the major direction of HIV research in large part thanks to Dr. Myron S. Cohen and his groundbreaking clinical trial on antiretroviral therapy benefits. Over a decade later, ART is still evolving, driven by goals of improving the treatment’s longevity and accessibility to more diverse populations.
Dr. Cohen, a physician scientist, received his M.D. at Rush Medical College and attended residency in Internal Medicine at the University of Michigan. While in training, he was unsure whether he wanted to pursue being a clinician,

but a mentor of his inspired him to continue down this path and pursue a fellowship in infectious disease at Yale. In 1980, Dr. Cohen arrived at UNC-Chapel Hill to conduct research on sexually transmitted disease (STDs); the following year, the HIV pandemic took root. At the time, the university was a leader in hemophilia research thanks to the contributions of the prominent pathologist Dr. Kenneth Brinkhous, and many patients with hemophilia flocked to Chapel Hill for care. Hemophilia is a condition in which the blood lack necessary clotting proteins, and the treatment involved infusions of concentrated clotting factors from a human plasma pool. Those patients were vulnerable for HIV infection because the


Figure 2. The government of west Africa is using the local language to educate the population in differents domains. Courtesy of Wikimedia.
plasma pool could be contaminated by even one HIV-positive donor, and sine HIV was not yet discovered, there was no HIV screening at that point. By 1985, at least 15% of people admitted to the hospital were diagnosed with AIDS, and the proportion was increasing sharply. Dr. Cohen quickly became preoccupied with prevention of this novel and dangerous disease.
In the late 80s, ART were developed and clinically demonstrated to reduce the virus’s replication rate in the body. Dr. Cohen hypothesized that if a drug can effectively reduce the amount of HIV in the blood and genital tract, those infected would no longer be contagious. But he also had concerns, “To what extent are people living with HIV and treated longer contagious? How effective is treatment and how durable is the prevention benefit ? Will [the effect] go on for a day, a week, a month, or a year?”1
In 2005, Dr. Cohen started a large clinical trial, the NIH HIV Prevention NetworkTrial (HPTN) 052 study, to determine whether early ART prevented transmission of the virus in “discordant couples”, where one partner was infected with HIV and the other was not. The study enrolled over 1300 couples from 9 countries across Asia, Africa, and the Americas. Participants were randomly assigned to one of the two study groups: one received ART immediately, and the other received the drug after a modest decline in the number CD4+ T cells. CD4T cells are immune cells that are killed by by HIV and their decline is a hallmark of untreated infection. After several years of study follow-up the results showed that early ART reduced the risk of sexual transmission by at least 96%.2
The study results were published in 2011, and the pivotal evidence drove major shifts in international HIV treatment, inspiring early intervention. This strategy achieved a global success: In 2023, there was 1.3 million new infections -- a 39% decline since 2010 and a 60% drop since the peak in 19953. Dr. Cohen also mentioned the PHIA project, which measured the status of HIV epidemic in most-affected countries, especially in sub-Saharan Africa. The data showed that the incidence of HIV infection had decreased from 20% in the early 2000s to around 0.2% now.1
One of the key challenges in HIV treatment has been ensuring that patients consistently remain on the therapy. Taking a daily pill, though effective, can be difficult due to stigma, forgetfulness, or lack of access to medication. To address these challenges, Dr. Cohen and his colleagues have been working on developing long-acting ART. Instead of frequent dosing, patients can receive periodic injections. A
major milestone was the development of cabotegravir, an injectable drug that remains effective for up to two months. More recently, another injectable drug, lenacapavir, has shown potential to last up to six months or longer. These drugs were also used for “pre-exposure prophylaxis (PrEP),” which prevented infection in people at high risk of exposure to HIV, as Dr. Cohen said, “You can have people stop having sex, but that’s hard. So either you treat people so they’re not infectious, or you find people at risk and you give them sort of preventive treatment, and that’s as close as we can currently get to a vaccine like strategy.”1
The success of ART also depends on public outreach. Many health researchers now focus on ensuring early HIV diagnosis and immediate treatment initiation. The “Undetectable = Untransmittable” (U=U) campaign has also helped reduce stigma by emphasizing that people with HIV who maintain viral suppression through ART cannot transmit the virus to others. Increasing public awareness remains a powerful tool in prevention, especially in resource constrained countries where misinformation continues to hinder progress. Several organizations have incorporated culturally relevant approaches, including community lectures, posters, and social media promotion to promote safe sex and legal blood supply.
Dr. Cohen describes biomedical research as a cyclical process with creativity and discovery. Every research begins with forming a meaningful hypothesis, followed by designing an ethical and fundable strategy to test it. The most exciting moment for him is when the hypothesis was proven correct, especially when it can impact medical care or public health. The results are then shared, and often lead to new questions and hypothesis. He also emphasizes that research is never solitary. His collaborations with students, young researchers, and global partners have been a vital part of his work. Without such intricate connections, his research would have never reached such a global scale. Above all, Dr. Cohen finds fulfillment in mentoring the next generation of scientists, guiding them through the process of inquiry and innovation.
References
1. Interview with Myron S. Cohen, M.D., 02/27/2025.
2. Cohen MS, Gamble T, McCauley M. 2019. Prevention of HIV Transmission and the HPTN 052 Study. Annual Review of Medicine. 71(1). doi:https://doi.org/10.1146/annurev-med-110918-034551.
3. HIV.gov. 2025 Feb 7. The global HIV/AIDS epidemic. HIVgov. https://www.hiv.gov/hiv-basics/overview/dataand-trends/global-statistics.
By Lana Maizel

The heart and brain share a genetic playbook—and decoding it could transform how clinicians treat disease.
In a groundbreaking 2023 study, researchers from the University of North Carolina at Chapel Hill and the University of Pennsylvania identified 80 specific regions of DNA responsible for the structure and function of both the brain and heart.1 Such genetic overlap offers an explanation as to why mental health disorders like depression often coincide with heart disease, suggesting that the body’s organs are interconnected on a genetic level—a discovery which can reshape illness prevention, diagnosis, and treatment.2
Leading this research is Dr. Hongtu Zhu, a professor of biostatistics at UNC Chapel Hill’s Gillings School of Global Public Health. Since launching the project in 2016, Zhu and his colleagues have meticulously analyzed medical data from over 40,000 participants in the UK Biobank—the world’s largest biomedical database, which contains health information from more than half a million individuals—to uncover complex genetic connections between the body’s organs. His work is reshaping the world’s understanding of how the heart and brain communicate at a molecular level.

“This is the first paper that tells you the heart and the brain have underlying common genetic architectures,” Dr. Zhu said.3
Dr. Zhu and his colleagues studied two key types of data from the UK Biobank: MRI scans of the brain and heart and genetic data. Using
this information, they conducted a Genome-Wide Association Study (GWAS) to look for genetic differences linked to how the heart and brain are built and function. A GWAS scans the DNA of many people to find small genetic differences that might be linked to specific traits—such as heart size or brain structure. Genetic differences like these are called single nucleotide polymorphisms (SNPs). DNA is made up of four chemical building blocks called nucleotides: adenine (A), thymine (T), cytosine (C), and guanine (G). These four letters form the genetic code that instructs cells how to function. An SNP occurs when a single letter in the DNA sequence is swapped for another—for example, an “A” might be replaced with a “G.” Even though these mutations are small, they can affect how genes work and influence traits like heart thickness or brain connectivity.
For example, if a certain SNP is found more often in people with a larger left heart ventricle, that suggests this SNP might play a role in determining heart size — or, at the very least, is correlated with it. Dr. Zhu’s team analyzed 82 traits related to the heart—such as left ventricle size, heart wall thickness, and aortic diameter—and 458 traits related to the brain—including gray matter volume, white matter integrity, and brain connectivity (Figure 1). Their GWAS of heart MRI traits identified 80 associated genomic loci.
Next, the researchers wanted to see if any of the same genetic regions (called genetic loci, from the Latin word locus, meaning “place”) were responsible for traits in both the heart and brain. To do this, they compared the specific DNA regions that influenced heart traits with those that influenced brain traits. Researchers found 80 genetic loci that were shared by both the heart and brain (Figure 2). This means that certain portions of DNA help shape both organs, suggesting a deeper genetic connection between heart and brain health than previously understood. Dr. Zhu’s study also revealed genetic correlations between heart traits and various psychiatric traits.
“If you have a certain degree of mental disorders like schizophrenia, bipolar disorder, epilepsy and depression, they will increase the risk of cardiovascular disease. [Similarly], acute mental stress also has a major impact on cardiovascular outcomes,” Dr. Zhu said.4 Dr. Zhu’s conclusion is supported by the fact that individuals with depression face up to double the risk of heart disease.5
While the initial study focused on individuals of British ancestry, Dr. Zhu and his team expanded their research to other ethnic groups using Genome-Wide Association Studies (GWAS). Such large-scale analyses scanned DNA from diverse populations to identify the same genetic links between heart and brain health. The results remained consistent and statistically significant across all groups, reinforcing the universality of these genetic connections.
Individuals with mental health conditions like depression or schizophrenia, which have been shown to have genetic links to cardiovascular issues, could benefit from proactive cardiovascular screenings and preventive strategies. Similarly, patients with heart disease may also receive preventive care for brain health, potentially reducing the risk of mental health complications in the future. Dr. Zhu’s research not only opens new avenues for understanding the heart-brain connection at a genetic level but also has significant implications for the future of medical treatments and disease prevention.

Figure 1. Above: This graph maps genetic heart MRI traits (x-axis)—such as heart chamber size and aortic diameter—against complex neurological and behavioral traits (y-axis), including schizophrenia, intelligence, and anorexia. Asterisks (*) indicate statistically significant correlations between specific heart structures and brainrelated conditions. Below: Four heart diagrams highlight structural traits linked to neurological disorders.
Courtesy of “Heart-brain connections: Phenotypic and genetic insights from magnetic resonance images.”

Figure 2. The genetic loci of the 80 specific parts of the DNA where heart and brain traits overlapped. Image courtesy of “Heart-brain connections: Phenotypic and genetic insights from magnetic resonance images.”
“What you could do is basically develop some drug, a treatment, for this type of disease associated with the heart and brain,” Dr. Zhu said, noting that a potential cause for these diseases could be a genetic link between the two organs. “I think potentially you can develop a drug to target some specific genetic markers for such a treatment.”3
Dr. Zhu plans to continue his research to study other interorgan links within the body to better understand their effects in hopes of improving medicine. With a clearer understanding of the shared genetic architecture between the heart and brain, healthcare providers could begin to develop treatments tailored not only to the specific organ involved but to the interconnected nature of these systems. Ultimately, this work could help prevent, diagnose, and treat diseases more effectively, benefitting a wider range of people and improving health outcomes worldwide.
1. Zhao, B.; Li, T.; Fan, Z.; Yang, Y.; Shu, J.; Yang, X.; Wang, X.; Luo, T.; Tang, J.; Xiong, D.; et al. Science. 2023, 380.
2. Heart disease and depression: A two-way relationship. NHLBI. https://www.nhlbi.nih.gov/news/2017/heart-disease-and-depression-two-way-relationship (accessed March 14th, 2025).
3. Interview with Hongtu Zhu, Ph. D. 2/7/2025.
4. Depression and heart disease: A two-way street. Harvard Medical School. https://www.health.harvard.edu/ heart-health/depression-and-heart-disease-a-two-waystreet. (accessed March 14th, 2025).
5. De Hert, M.; Detraux, J.; Vancampfort, D. Dialogues in clinical neuroscience 2018,20, 31-40.
By Gerald Ofosu
Atherosclerosis is a sneaky but serious condition that creeps through the arteries, thickening their walls and filling them with endless layers of fat and cholesterol. As plaques build up, they restrict blood flow, increasing the risk of heart attacks and strokes — causing heartbreak in a biological sense. Characterizing the disease has been difficult. We do know that lipid-filled macrophages, foam cell accumulation, and the body’s inflammatory response are contributors, but despite developing knowledge, much is still unknown.2 Cardiovascular researchers like Dr. Edward Moreira Bahnson seek to find answers to the many questions surrounding atherosclerosis and hopefully create targeted therapies to inhibit or reverse the progression of the disease.
Dr. Edward Bahnson lived in Uruguay from birth until his early 20s. Growing up, he was very curious about the world around him. He loved learning about everything from different earth-based species to the great depths of outer space. In high school, a chemistry professor ignited his interest in biochemistry, which he decided to pursue at college. During his undergraduate years at the University of Uruguay, he was mentored by a professor emeritus in the lab, getting his first glimpse at research. Following his undergraduate experiences, Dr. Bahnson moved to the US to attend Kent State University for his doctorate. In a joint program with the Cleveland Clinic, he studied vitamin B12 metabolism in blood vessel cells, sparking his curiosity in vascular biology. In his postdoctoral years at Northwestern University, he trained under Vascular Surgeon, Dr. Melina Kibbe to focus on targeted therapies for vascular disease. In 2016, Dr. Bahnson found his current home: The University of North Carolina at Chapel Hill. At UNC-Chapel Hill, he enjoys the interdisciplinary culture and a close-knit research community: “I’ve met colleagues just
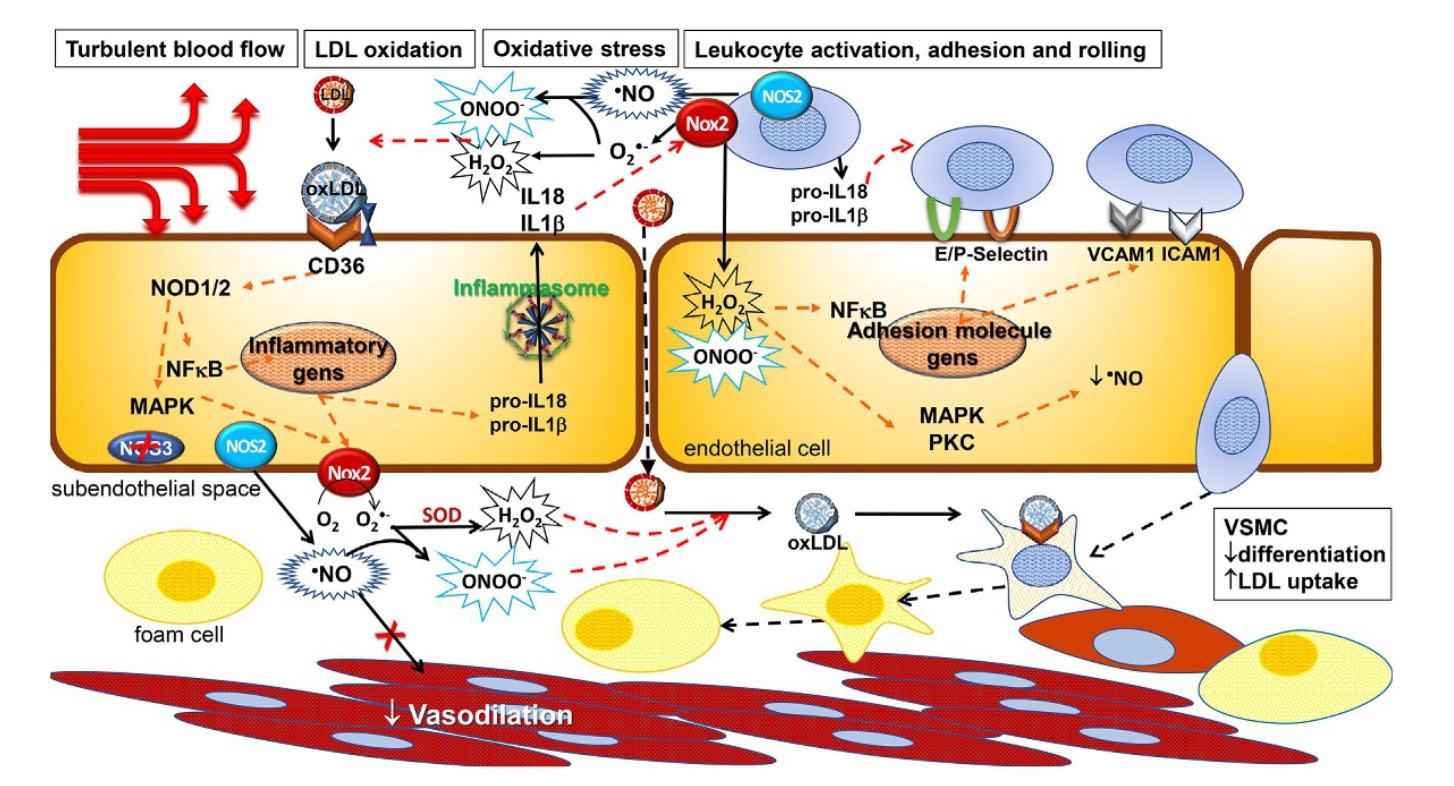
Figure 1. Inflammatory process of Atherosclerosis. Specifically featuring LDL oxidation, LDL uptake, and the NFkB stimulatory pathway. Courtesy of Dr. Bahnson.
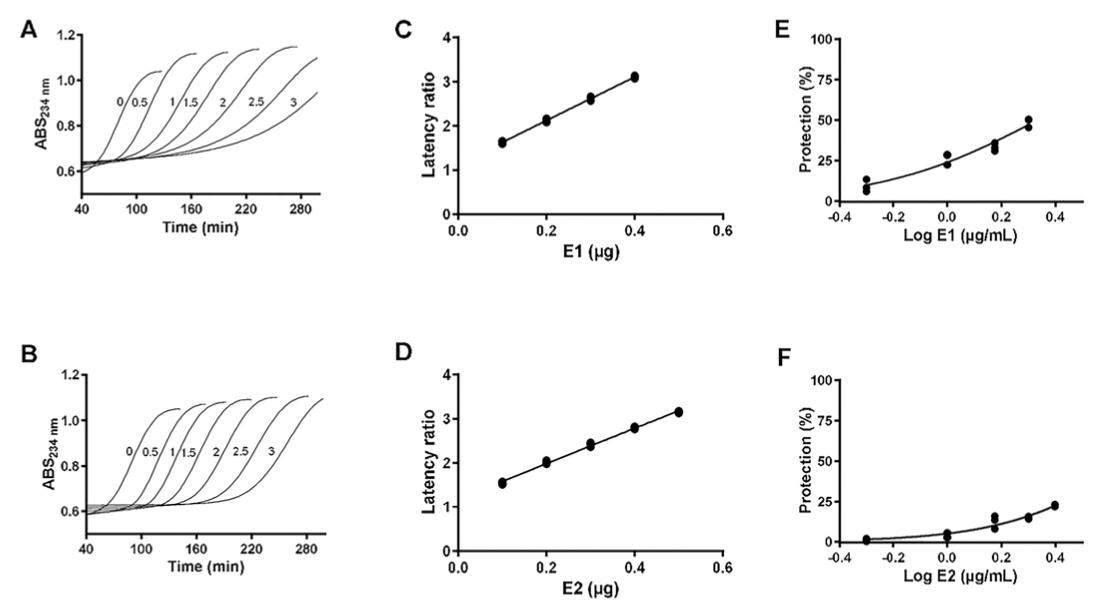
Figure 2. Graphs showing the positive correlation between increased levels of E1(C) and E2(D) LDL oxidation inhibition using ratio of latencies (latency/control latency) and the amount of extract. Courtesy of Dr. Bahnson.
walking and going to grab a cup of coffee, and that sparked a conversation. Everybody’s interested in helping out... it’s a very supportive environment.”1
Dr. Bahnson’s latest studies focus on the role of cannabis extracts, or cannabinoids, in on the progression of atherosclerosis. He and his collaborators showed that cannabinoids reduce Low Density Lipoprotein (LDL) oxidation and hinder the receptors responsible for intaking LDL, ultimately inhibiting the processes that drive atherosclerosis. As previously noted, the arterial inflammation that causes atherosclerosis is further mediated by several crucial factors, including LDL oxidation, macrophages, and foam cells. Dr. Bahnson explained the relationship he discovered between the factors: “We found that macrophages took up less oxidized LDL in the presence of these cannabinoids."1 Dr. Bahnson’s explanation suggests that cannabinoids may help reduce foam cell formation, potentially slowing down the progression of atherosclerosis by decreasing lipid buildup and plaque development. Under normal conditions, LDL is quite helpful in carrying cholesterol through the bloodstream, an indispensable role in proper cellular function. However, the oxidation of LDL is unfavorable because it leads to the substance losing its electrons, which diminishes its normal properties. After oxidation, macrophage scavenger receptors detect and absorb LDL. Inside the macrophage, oxidized LDL accumulates, leading to the buildup of lipids within the cell. As the macrophage continues to engulf the LDL, excess lipid concentrations within the macrophage transform it into a foam cell — the main culprit in the formation of atherosclerotic plaques and inflammation (Figure 1).
One of Dr. Bahnson’s most intriguing experiments

Figure 3. Western blot results showing the effects of cannabinoid extracts on the expression of OLR1, CD36, and SRA1 in J774.1 cells, with and without oxLDL stimulation. The data indicate significant changes in OLR1, CD36, and SRA1 protein levels upon treatment with the extracts. Courtesy of Dr. Bahnson.
measured the inhibition of LDL oxidation, expression of scavenger receptors, and activation of the NF-kB pathway. To analyze LDL oxidation, he and fellow researchers first isolated three cannabis extracts (E1, E2, E3), and determined their THC concentrations using ultra-performance liquid chromatography (UPLC-DAD). E1 had the highest concentration, followed by decreasing concentrations in E2 and E3, . Using techniques such as UV-Vis spectrometry, confocal microscopy, and western blot, they then examined the copper-induced oxidation of LDL to compare oxidation intensities between cells exposed to increasing cannabis concentration levels against a control group. The results of the UV-Vis spectrometry signified the efficiency of the two extracts with a higher concentration, presenting a positive correlation between the increase in cannabis concentration and the latency period of LDL propagation (Figure 2).2
To test the effect of cannabinoids on scavenger receptor expression, Dr. Bahnson treated an experimental group of J774.1 macrophages with oxidized LDL and a control group of macrophages with DMSO for 24 hours, using western blots to assess scavenger receptor expression following the period. The results revealed that treating the experimental group with oxidized LDL increased the expression of two scavenger receptors, ORL1 and CD36, and had minimal effect on another, SR-A1. Then, the experimental macrophages were treated with cannabis extract. The results displayed a significant decrease in ORL1 and CD36 expression with a moderate reduction in SR-A1 expression, caused primarily by the two lower cannabis extracts concentrations. Cannabis extracts were shown to down-regulate scavenger receptor expression, and likely inhibit the NF-κB pathway. The NF-κB pathway’s known role is promoting the expression of scavenger receptors, meaning that its suppression by cannabinoids likely reduces receptor availability and, in turn, limits oxidized LDL uptake (Figure 3).2
The experiment was repeated to examine specifically NF-kB activation; this time, a western blot was used to detect phosphorylation levels of p65, a protein subunit involved in the pathway, and the inhibitory protein IkBa. Phosphorylation is a process where a phosphate group is added to a protein, often altering its activity. IkBa inhibits p65 when dephosphorylated, whereas p65 itself stimulates Nf-κ B. The results showed
that exposure to oxidized LDL increased phosphorylation of p65, whereas treatment with cannabinoid groups higher in cannabinoid concentration decreased p65 phosphorylation, demonstrating their limiting effects. Additionally, the highly concentrated cannabis extracts dephosphorylated IkBa. From these findings, the researchers concluded that in circumstances where cannabis concentration is increased, NFκb activation will be reduced.2
Ultimately, it is clear based on Dr. Bahnson's research that cannabinoids inhibit key processes of atherosclerosis development. By understanding their effects, cannabis extracts can offer a practical approach to cardiovascular therapy. However, just like healing a broken heart, repairing the arteries is easier said than done — only time will tell if cannabinoids are the answer.

1. Interview with Edward Bahnson, Ph.D. 02/21/25.
2. Musetti B, Kun A, Menchaca D, Rodríguez-Haralambides A, Varela J, Thomson L, et al. (2024) Cannabis sativa extracts inhibit LDL oxidation and the formation of foam cells in vitro, acting as potential multi-step inhibitors of atherosclerosis development. PLoS ONE 19(12): e0310777. https://doi.org/10.1371/journal. Pone.0310777
3. Preedy V.R., Patel V.B., Martin C.R., eds. Medicinal Usage of Cannabis and Cannabinoids. Academic Press; 2023:160164.
By Ambika Puri

Does location make a difference in behavior? Could the physical location of an establishment make an impact on its customer base? What type of establishment outnumbers the number of McDonalds located in Chapel Hill by nearly 10 times? Some of the answers to these questions are subject to one’s personal interpretation, but an article published in 2016 helped put these questions to the test.
One of the people hoping to answer these questions is Kurt M. Ribisl, PhD. Dr. Ribisl is the chair of and Jo Anne Earp Distinguished Professor in the Department of Health Behavior at Gilling’s School of Global Public Health at the University of North Carolina at Chapel Hill. Dr. Ribisl is also the program

leader for Cancer Prevention and Control at UNC Lineberger Comprehensive Cancer Center. He served as a member of the congressionally mandated Tobacco Products Scientific Advisory Committee (TPSAC) for the United States Food and Drug Administration Center for Tobacco Products from 2012 to 2016. Dr. Ribisl has ties to our state not just as a long-time faculty member at the UNC Chapel Hill, but he also completed his undergraduate work at Wake Forest University before getting his Masters and Doctoral degree from Michigan State University. He later went on to do his postdoctoral fellowship at Stanford University.
In 2016, Dr. Ribisl and his team conducted a study titled “Reducing Disparities in Tobacco Retailer Density by Banning Tobacco Product Sales Near Schools”. The purpose of this study was to determine whether a policy banning tobacco product retailers should be in relation to their physical location. The policy was to restrict these retailers from 1000 feet of school campuses and if that made an impact on the community and young people from using tobacco products. Traditionally retailers try to place their establishments closest to their clientele, and students are frequent users of tobacco products regardless of whether they are of legal age. This study involved geocoding all the tobacco outlets that were physically located within 1000 feet of schools in the state of Missouri and the state of New York. “Missouri and New York were chosen because they have a good mix of urban, suburban, and rural areas and have good data available on tobacco retailer locations from retailer licenses according to the review team led by Dr. Ribisl”.2 Using this Geographic Information System spatial analysis, the team was then able to see on the map where the tobacco retailers were and their proximity to school boundaries, giving the team a visual canvas with which to view the data. After data analysis the study found

Figure 1. This image describes retailer pre and post ban proximity to schools in New York and Missouri. Courtesy of Dr. Ribisl’s paper.
and presented pre and post bans disparities in density and used this comparison to try and explain why policies may end up working differently based on neighborhood comparisons, which included economic and societal factors. This analysis is important because it helped to exemplify how the economic status of a neighborhood impacts why tobacco retailers are located there. These tobacco companies targeted certain locations as they believed they would have a larger customer base in those locations.
As the team looked at pre-ban conditions, existing retailers were assessed by looking at the number of tobacco retailers per 1000 people. They concluded that tobacco retailer density was greater in the lowest income quartiles as compared to the highest income quartiles in both data sets from Missouri and New York. “For New York, the density was the highest (1.28 retailers per 1000 people) in the lowest income quintile but then appeared to level off for the remaining four quintiles (range: 0.76 to 0.88). Retailer density in New York was 52.4% higher in the poorest quintile compared to the wealthiest.”2 This helped to validate how tobacco retailers are drawn to these areas as they tend to target that population. This was able to show that there was greater tobacco retailer density in areas with lower income and more racially or ethnically diverse residents. The team then ran a similar test with a policy that banned the location of tobacco retailers within 1000 feet of schools and discovered that the disparities were lessened and, in some cases, no longer existed. It also indicated that the most affected areas were the quintiles that had a higher rate of African American and Hispanic populations, as these areas contained the highest density of tobacco retailers. The pattern showed that the policy to ban these retailers from their proximity had the greatest impact in
these areas. (Figure 1)
Dr. Ribisl stated that around the United States, there are 26 tobacco retailers for every one McDonalds. “In Chapel Hill there are over 60 tobacco retailers and only about 3 or 4 McDonalds with over a dozen of these tobacco retailers on Franklin Street alone”1, he stated. That is all to demonstrate that tobacco retailers strategically place their establishments closest to where they believe their customers are. This study helped to reiterate how the tobacco industry targets areas which are higher in minorities and young people, as this encompasses much of their customer base. This study was a follow up to a previous one that Dr. Ribisl and his team had conducted, but this study specifically looked at the issue of equity and focused more on the impact on lower income areas of a community. There are no definitive plans to do another study as a follow-up to this, but that could always be a possibility. This study supported the belief that tobacco retailers are known to target certain population groups, such as minority population and lower economic bases to build their customer base.
1. Interview with Kurt M. Ribisl, PhD. 02/17/2025.
2. Ribisl, K., Luke, D., et al. Reducing Disparities in Tobacco Retailer Density by Banning Tobacco Product Sales Near Schools. Nicotine & Tobacco Research, 2017, 239–244.
By Julia Sallean

It is no secret that diet is a risk factor for many of America’s most common diseases. For most people, food isn’t just seen as a way to fuel the body, but as a determining factor in health. This is why people are often encouraged to take supplementary vitamins or “eat the rainbow” in order to best support metabolic health. And yet, it’s not only vitamins and minerals that are important. Key regulators of metabolic health that have recently gained attention are nutrients called omega-3 fatty acids, also known as n-3 PUFAs (polyunsaturated fatty acids). Omega-3 fatty acids are important regulators in many processes in the body, such as brain development and inflammation. New research being conducted at the University of North Carolina at Chapel Hill has indicated that n-3 PUFAs may play an even bigger role in the body than previously suspected, indicating that the influence of diet on health is more important than ever.
Long chain n-3 PUFAs are a class of fatty acids, which are important molecules for cellular structure, signaling, and whole-body metabolism. Despite having the word“fat”in them, fatty acids aren’t necessarily bad fat; in fact, they are essential to many aspects of human metabolism. Long chain n-3 PUFAs are called conditionally essential fatty acids because it is more efficient to get these molecules directly through the diet, rather than synthesizing them. Long chain n-3 PUFAs are most

commonly found in oily, cold-water fish such as salmon and mackerel, though they are also present in other foods like oysters or walnuts (Figure 1). The recommended serving of long chain n-3 PUFAs in the diet is around 2-3 servings of fish (around 6oz) per week. Due to factors such as availability, cost, or personal preference, most Americans fall well below this threshold. Importantly, omega-3 fatty acids have been linked to lower inflammation, improved cardiovascular health, improved brain development, and decreased cognitive decline. However, there is still much more to understand about their effect on the immune system, especially in the context of obesity, which impacts a significant proportion of the U.S. population.
New research has indicated that n-3 PUFAs may play an even larger role in the body than previously suspected, further indicating the influence of diet on health. Dr. Saame “Raz” Shaikh of the Gillings School of Public Health conducts research centered around how n-3 PUFAs and their downstream products regulate the immune system and other metabolic responses in individuals with obesity (Figure 2)1 The core focus of Dr. Shaikh’s research includes two long chain n-3 PUFAs called EPA (Eicosapentaenoic acid) and DHA (Docosahexaenoic acid)2 These two fatty acids are structurally similar, and both EPA and DHA play roles in inflammation and cardiovascular health. In fact, EPA and DHA


Figure 2. The rold of oxylipins in immunity and inflammation pathways. Image courtesy of Dr. Raz Shaikh.
supplements have been approved by the FDA for lowering triglycerides, a major risk factor for cardiometabolic diseases. EPA is also FDA approved for lowering cardiovascular disease risk. Interestingly, DHA also plays a significant role in brain development and prevention of pre-term birth and is the most common fatty acid found in the brain.
To investigate the role of these omega-3 fatty acids in the immune system of individuals with obesity, Dr. Shaikh performed an experiment on obese and healthy mice to examine the downstream molecules generated from EPA and DHA during metabolism, called “oxylipins”. He discovered that there was a group of these molecules that were decreased in obese mice across multiple tissues. Dr. Shaikh also found that some oxylipins generated from DHA were decreased in adults with morbid obesity. Others have shown that EPA-derived oxylipins are also decreased in adults with obesity. When obese mice were given back oxylipins, a variety of immune responses improved in the body. For example, indicators of antibody production and inflammation improved with increased DHA, indicating that n-3 PUFAs can boost immunity and lower inflammation (Figure 2). As summarized by Dr. Shaikh, “When we give these molecules back, we can drive improvements in both immunological and metabolic outcomes”.
Dr. Shaikh recently followed up on his rodent research to determine if administering EPA and DHA to adults with obesity can increase the levels of EPA- and DHA-derived oxylipins. The first clinical study, published recently, showed that some, but not all, of these oxylipins were increased after a one-month period3. A new clinical trial is currently underway to determine if a longer treatment period of three months will generate a stronger response in adults with obesity accompanied by a reduction in inflammation. Overall, results found in mice have been promising and indicate that n-3 PUFAs do play a crucial role in regulating inflammation and immunity.4
Some researchers argue that increased inflammation is driven by the imbalance between n-3 and n-6 (omega-6) pathways in individuals with obesity. Omega-6 fatty acids are found in a variety of foods such as seed oils. Omega-6 fatty acids are beneficial, although some argue that too much n-6 relative to the level of n-3 PUFAs in the body can have negative effects on inflammation. For example, one omega-6 fatty acid called arachidonic acid gives rise to many metabolites critical for starting inflammation, and is blocked to lower inflammation in many medicines such as ibuprofen. Therefore, retaining a balance between omega-6 and omega-3 fatty acids by consuming omega-3s is crucial for regulating inflammation in the body, which is why Dr. Shaikh’s research is focused on increasing omega-3 fatty acids in the western diet.
An increase of n-3 PUFAs in the diet or through supplements could prove beneficial to many people, though it is important to note that different populations will respond differently to increased n-3 PUFA intake. As Dr. Shaikh notes, “It’s really about trying to find cohorts of people that you can give advice to and say ‘this is what would be a good intake of omega-3’s for you’”. One such population that is recommended to increase their n-3 PUFA intake is pregnant women. In particular, these women are encouraged to supplement their diet with DHA and EPA, which is important for brain development and can reduce risk of preterm birth in the second and third trimester of pregnancy. For this reason, the European Board and College of Obstetrics and Gynecology recently made a positional statement recommending that pregnant women consume increased n-3 PUFAs4.
It seems inevitable that the future of precision nutrition will likely include n-3 PUFAs, though we cannot yet be certain of which populations these fatty acids will be the most helpful for. In the meantime, it is important to make sure that a balance of all nutrients—including omega-3 fatty acids—is maintained, in order to support the overall health of everyone.
1. “Emerging mechanisms of obesity-associated immune dysfunction.”PubMed,https://pubmed.ncbi.nlm.nih. gov/38129700/.Accessed 4 March 2025.
2. “Omega-3 fatty acid supply in pregnancy for risk reduction of preterm and early preterm birth: A position statement by the European Board and College of Obstetrics and Gynaecology (EBCOG).”PubMed,https://pubmed.ncbi.nlm. nih.gov/38354604/.Accessed 4 March 2025.
3.“Saame “Raz” Shaikh, PhD.”UNC Gillings School of Global Public Health,https://sph.unc.edu/adv_profile/raz-shaikhphd/. Accessed 4 March 2025.
4.“Shaikh Lab.”TarHeels.live, https://tarheels.live/shaikhlab/. Accessed 4 March 2025.

By Sanjita Srinath
Multiple sclerosis (MS) is a relentless autoimmune disease affecting over 1 million Americans that disrupts the central nervous system, leading to motor dysfunction, cognitive decline, and, in severe cases, paralysis. Current treatment options rely on broad immunosuppressants, essentially limiting the immune system and leaving patients vulnerable to infections and other complications. But what if there was a way to reprogram the immune system to tolerate the immune cells

attacking the nervous system without compromising overall immune function?
A novel particle-based therapy, developed by Dr. Kristy Ainslie of University of North Carolina at Chapel Hill’s Eshelman School of Pharmacy, aims to do just that. Dr. Ainslie (pictured below) is an Eshelman Distinguished Professor and Chair of the Division of Pharmacoengineering and Molecular Pharmaceutics. She received her Ph.D and M.S. in Chemical Engineering from Pennsylvania State University and her B.S. in Chemical Engineering from Michigan State University, with a postdoctoral fellowship at the University of California, San Francisco. With her background in chemical engineering, she had always been fascinated by the intersection of engineering, polymers, and immunology, and saw an opportunity to tackle one of the biggest challenges in MS treatment.
MS is a condition that happens when the immune system mistakenly attacks myelin, the protective sheath around nerve fibers, because it perceives it as a threat. This leads to inflammation and progressive nerve damage, disrupting communication between the brain and the rest of the
body. The challenge for scientists is to stop this attack without weakening the immune system overall or relying on broad immunosuppressants.
Dr. Ainslie’s new approach leverages polymer-based drug delivery which induces antigen specific tolerance. Essentially, the polymer is carrying agents to teach the immune system to recognize the myelin sheaths and stopping the immune system from attacking its own nervous system. Therefore, this approach would theoretically preserve the body’s ability to fight infections.
The polymer-based drug delivery carrier uses tiny biodegradable particles to deliver therapy to train the immune system to dampen the autoimmune response. One of the therapies released is a protein similar to myelin, MOG (Myelin oligodendrocyte glycoprotein), to help “convince” the immune system that myelin is not a threat. The other substance is called rapamycin and helps guide the immune system towards tolerance. Working together, these particles act as tiny training programs, slowly releasing their contents and re-educating the immune system and immune cells to combat them attacking myelin, while still allowing them to fight
harmful infections.
To test the efficacy of this therapy, Dr. Ainslie tested in mice with MS-like symptoms, using the mouse model of MS, known as experimental autoimmune encephalomyelitis. Since MS is a humanspecific disease, researchers induce MSlike symptoms in mice to study potential treatments in a controlled setting. These symptoms include inflammation, nerve damage, and paralysis, which mimic key aspects of MS.
The study was conducted in two treatment groups: an early therapeutic group and a late therapeutic group. In the early therapeutic group, the mice were treated at disease onset. In the early treatment group, the therapy significantly reduced disease severity,
It holds promising results for the future of MS treatment, and possibly other autoimmune diseases
meaning mice showed lower clinical scores, a measure of neurological impairment, compared to untreated mice. This suggests that the treatment helped limit disease progression.
However, the most striking results came from the late treatment group, where mice had already developed severe paralysis. Incredibly, both types of particles, those containing only the MOG and those containing both MOG and rapamycin, helped reverse paralysis, allowing the mice to regain movement. This dramatic improvement highlights the potential for this therapy to not just slow MS, but actively restore function, offering hope for future treatments in human patients.
One important concern for Dr. Ainslie’s team was ensuring this treatment only targeted MS and did not weaken the entire immune system like the current MS treatments. To test this, they first vaccinated mice against influenza and then gave them the new MS therapy. If the treatment had suppressed the immune system too broadly, the mice would not have been able to fight off influenza properly, meaning their response to the vaccine
would have been weak. But that is not what happened. The mice still had a strong immune response to vaccine, proving that the therapy was highly specific to MS rather than just shutting down the immune system entirely. While this approach is still in the early stages of development, it holds promising results for the future of MS treatment, and possibly other autoimmune diseases like type 1 diabetes and rheumatoid arthritis. With more research and human trials, this therapy could help millions of people without forcing them to choose between treating their disease and protecting their immune system.
References
1. Interview with Kristy Ainslie, Ph.D., 02/05/2024
By Paige Twohill

Cells are commonly known as the “building-blocks” of life within living organisms. They are composed of organelles that do specific tasks within the cell allowing the cell to survive and perform its necessary functions. Each cell’s functions are just tiny working parts that contribute to the function of the entire organism. Though it is often taught as a simple process where each piece of the “puzzle” functions independently, there are factors that influence the proteins and cell’s functions, disrupting the notion of the cell as the most organized unit of life.
One example of this in cells would be the development of cancer, which is caused by uncontrolled cell growth. This means that the cancerous cells may have lost the ability to regulate proper gene expression that is specific to cell proliferation or growth and

Dr. Lindsey James

Figure 1. This image shows UNC 6934, which underwent optimization as a chemical probe for NSD2. Courtesy of Nie DY, et al.
eventual division. When expression of a gene occurs when it should not, the functions of a cell may be compromised. Gene expression is also controlled by epigenetic factors, which can “turn on” or “turn off” certain genes without changing the sequence of the DNA. Over time, epigenetic mechanisms may inhibit or induce certain genes, which may lead to diseases like cancer if the genes are related to cell growth or division. It is thought that harnessing epigenetic mechanisms and targeting genes with molecules that can correct these effects may be a potential therapeutic path. Through research, some of which has been completed here at the
University of North Carolina at Chapel Hill, small molecules can be identified that inhibit the function of proteins when they are dysregulated in cancer. These molecules can be screened for efficacy in acting as a therapeutic agent for the prevention of cancer or other diseases.
Dr. Lindsey James is an Associate Professor of Medicinal Chemistry and Chemical Biology in the Eshelman School of Pharmacy, as well as the Director for Chemical Biology in the Center for Integrative Chemical Biology and Drug Discovery at UNC-Chapel Hill. Her lab is interested in studying epigenetic regulatory factors, specifically methyllysine reader proteins. Methylation of

lysine is a common post-translational modification that occurs and these methyl-lysine markers on certain proteins act as “tags” to recruit methyllysine reader proteins and other protein complexes involved in regulating gene expression.
From a therapeutic standpoint, some methyl-lysine reader proteins show promising results when experimentally “knocked out” in certain types of cancer cells. In these experiments, it is suggested that methyl-lysine reader proteins may play a role in the development of certain types of cancer. In the James Lab, they aim to develop potent and selective small molecule binders that block the function of methyl-lysine reader proteins implicated in disease. They hope to “discover [potent and selective] small molecule tools that researchers can use to better gauge whether antagonizing these proteins is likely to lead to a positive therapeutic outcome.”1
The typical experimental process in the James Lab involves traditional medicinal chemistry and usually begins with a purified protein that is known to bind to a methyl-lysine substrate. They can develop biochemical assays, screen for binders of the protein, and use structure-based design to improve binding affinity. Sometimes, a trial-anderror approach is used to find which functional groups on the molecule increase, decrease, or have no effect on the potency of its binding. Another way that the James Lab find hit molecules
to test in binding assays is to use computational methods in collaboration with computational chemists at UNCChapel Hill, where a known structure of the protein can be used to predict high-affinity ligands. All compounds can be tested in vitro and in cellular assays involving relevant cancer cells.
A prominent example of Dr. James’s work is her efforts to target NSD2, an oncogene and histone methyltransferase protein. Oncogenes are overactive genes that cause uncontrolled cell growth and are derived from proto-oncogenes which have normal expression in the cell. Histone methyltransferase proteins are involved in the installation of the methyl-lysine post-translational modification and play a role in the regulation of gene expression. When dysregulated, histone methyltransferase proteins can be involved in causing cancer. When the NSD2 protein acquires a gain-of-function mutation or is translocated, it is involved in causing uncontrolled cell growth and in some cases, resistance to known drugs.2 The James lab has developed potent ligands for NSD2 (Figure 1)2 and more recently discovered molecules that can completely degrade the NSD2 protein (Figure 2). They found that the FBXO22 protein could be recruited by the synthesized molecule UNC8732 to NSD2 and induce degradation, or breakdown, of NSD2 (Figure 2).2 This prevents NSD2’s methyltransferase activity (where overactivity contributes to cancer cell growth) or from
functioning as an epigenetic regulator, as well as prompts effects like growth suppression and apoptosis of cells. This suggests that targeting NSD2 with small molecules like the ones synthesized in the James Lab could have beneficial therapeutic effects.3
Dr. James’s lab focuses primarily on synthesizing and testing small molecules targeting proteins involved in cancer. When a molecule shows particularly promising potency or efficiency in an assay, she often collaborates with members of the Lineberger Cancer Center or other departments at UNC-Chapel Hill to test her molecule in relevant biological settings. Dr. James emphasizes that “In general, [we] really want to understand how our molecules are working at the molecular level.”1 The process of taking a potential therapeutic molecule to a drug is complex and knowing why the molecules she makes have the observed effect in cells is important to future research in drug development. In the future, her lab aims to discover molecules that can be useful tools for studying cancer biology and potentially translate into molecules that provide therapeutic benefits.
1. Interview with Dr. Lindsey James, Ph. D. 1/28/25.
2. Nie DY, Tabor JR, Li J, Kutera M, St-Germain J, Hanley RP, Wolf E, Paulakonis E, Kenney TMG, Duan S, et al. Recruitment of FBXO22 for targeted degradation of NSD2. Nat Chem Biol, 2024, 20(12):1597–1607.
3. Dilworth D, Hanley RP, Ferreira De Freitas R, Allali-Hassani A, Zhou M, Mehta N, Marunde MR, Ackloo S, Carvalho Machado RA, Khalili Yazdi A, et al. A chemical probe targeting the PWWP domain alters NSD2 nucleolar localization. Nat. Chem. Biol, 2022, 18(1):56–63.
By Akshara Venkatesan

courtesy of Adobe Stock
About 12% to 15% of the people in the world experience migraines.1 While symptoms differ for every person, migraines are typically characterized by throbbing, pulsing pain on one side of the head, and their duration ranges from four hours to as long as a whole day. The symptoms of this disorder make it almost impossible to function in daily life. Unlike headaches, where the pain affects the head or face, migraines directly affect the brain, and often affect other parts of the body as well. While studies have shown that migraines are genetically caused, everyday factors such as one’s lifestyle, environment and food,especially, are crucial in preventing and managing attacks. Dr. Keturah Faurot, an assistant professor in the Department of Physical Medicine and Rehabilitation at the University of North Carolina at Chapel Hill investigated the effects of fatty acids on pain, specifically chronic daily headaches to further determine how integrative therapies such as diet management can aid in migraine management, especially since there is no known cure for migraines.

While migraines can be genetic, other physiological processes have been known to cause these throbbing headaches. These include shifts in levels of neurotransmitters like serotonin and nerves in blood vessels sending pain signals to the brain. The latter causes inflammatory substances to be released into the nerves and blood vessels in the head, which is what causes the migraines.2
Fat, or adipose tissue, present in everyone’s body, is one such substance that can send these signals. Fat is known to be a very energetic substance, as it is constantly sending signals to all parts of the body, through the secretion of molecules. When there’s an over abundance of fat cells, such as in people who are obese, the fat cells are sending signals for the body to make inflammatory proteins.
When the body is producing plenty of these proteins, it enters an ‘inflammatory state and the fat cells start producing pain generating hormones.3 Migraines are found to have these same pain generating hormones, meaning people who are obese are at a higher risk for increased frequency of headaches and pain level.
While fat or adipose is the tissue itself, fatty acids are what make up this tissue. Specifically, Omega-3 fatty acids are a type of fatty acids that the human body cannot produce, and hence can only be gained through the diet. It has numerous health benefits including improving heart and mental health, decreasing liver fat, and fighting inflammation4. The body also needs Omega-6 fatty acids, another type of fatty acids that are obtained from the diet. They provide energy, and the most common Omega-6 fatty acid is linoleic acid. The body converts this acid into arachidonic acid (AA), which is longer and produces eicosanoids which are signaling molecules.4 When produced in excess amounts, it can cause inflammatory diseases. As discussed above, obesity can trigger inflammatory proteins, which in turn trigger pain generating hormones (which are what trigger migraines). With the intake of Omega-3
fatty acids, there is a reduction in these inflammatory proteins, which can help tackle obesity and can aid in the reduction of migraines. On the contrary, the intake of Omega-6 fatty acids can lead to increased inflammation and through a series of physiological events, increased migraines. The goal is to have an increased intake of Omega-3 fatty acids and a reduced intake of Omega-6 fatty acids.
In their series of recent studies, Dr. Faurot and her team conducted an investigation into how fatty acid manipulation can affect migraines, specifically reduction of headaches. The study involved 182 adults who had chronic migraines (characterized by 5-20 migraine days per month)5. They were randomized to three different diet categories: A high Omega-3 and low Omega-6 (H3L6) diet, a high Omega-3 and average Omega-6 diet (H3), and a control diet (average Omega-3 and Omega-6 diet), and had blood measurements every four weeks to monitor their levels. The participants kept track of their migraines and headaches using a headache diary. The results showed an improvement in the participants’ sleep quality and perceived health. The most significant results included the huge influence the H3L6 diet had on pain interference and the pain intensity of the migraines (Figure 1).
While the series of studies yielded favorable outcomes, it wasn’t an easy process. Regarding the processes involved in this study, Dr. Faurot says, ‘[The study] was very hard to do epidemiologically, and the reason for that is that….there isn’t enough variation in Omega-3 intakes in the general population.”6 This was the primary reason why the team had to conduct the dietary interventions, and conduct a clinically randomized trial to obtain the results for this study. She emphasizes the importance of variation in the independent variables of the study, especially for studies conducted over a period of time.
Dr. Faurot believes that integrative therapies, such as diet management, are ways of helping people in addition to

Figure 1. This image describes the results from the study and how pain levels have gone down for H3L6 diets. Courtesy of Dr. Faurot.

Figure 2. This image describes the pathophysiology of a migraine and how neurotransmitters and blood vessels are involved in this process. Courtesy of cnbytes.
the medical and pharmacological therapies they are receiving for their treatment. Manipulating the diet to manage chronic pain has proven to yield positive outcomes. Migraines are not going anywhere. They continue to affect about 1 billion people all over the world. Though a cure doesn’t exist, simple changes to the diet, through the increase of Omega-3 fatty acids and the decrease of Omega-6 fatty acids, could hugely help manage the pain a migraine induces. A little management can go a long way, especially for a life filled with migraines.
1. Chronic migraine: What it is, causes, symptoms & treatment. (n.d.). Cleveland Clinic. Retrieved March 8, 2025, from https://my.clevelandclinic.org/health/diseases/9638-chronic-migraine
2. How to get rid of a migraine. (n.d.). Cleveland Clinic. Retrieved March 8, 2025, from https://my.clevelandclinic. org/health/diseases/5005-migraine-headaches
3. The link between obesity and migraine | amf. (n.d.). American Migraine Foundation. Retrieved March 8, 2025, from https://americanmigrainefoundation.org/resource-library/migraine-obesity/
4. https://www.healthline.com/nutrition/omega-3-6-9overview#omega-6
5. Faurot, K. R., Park, J., Miller, V., Honvoh, G., Domeniciello, A., Mann, J. D., Gaylord, S. A., Lynch, C. E., Palsson, O., Ramsden, et al. 2003. Front. in Pain Res (Lausanne, Switzerland), 4, 1231054. https://doi.org/10.3389/ fpain.2023.1231054
6. Interview with Keturah R Faurot, Ph.D. 2/21/25.
By Shadi Darawsheh
Image courtesy of Freepix

Every parent hopes for a smooth journey when it comes to their child’s health, but for many families, receiving an autism diagnosis can feel like stepping into a maze with no clear way out. From long wait times to systemic obstacles, the journey from initial screening to intervention is riddled with delays, delays that are even more severe for Black families, who historically face the greatest health disparities for timely autism care.2
At the forefront of addressing these disparities is Dr. Kelly Caravella, a clinical psychologist and researcher at the University of North Carolina at Chapel Hill. Dr. Caravella has spent her career studying early childhood development, autism, and intellectual disabilities. She currently leads a groundbreaking study designed to expedite care and access to autism interventions and treatments for Black families, as early access to treatment has been proven to improve patient outcomes.
In an ideal world, children between the ages of 18 to 24 months receive standardized developmental screenings during pediatric checkups3. If these screenings raise concerns about potential autism, children should be referred to a specialist for further evaluation. If diagnosed, they should then be connected to early intervention services designed to help them develop crucial skills. Unfortunately, this process, which Dr. Caravella called the “diagnostic odyssey” frequently breaks down at multiple points.1


Figure 1. Addressing barriers faced by underserved populations, creating a more equitable system. Photo courtesy of Freepik.
The odyssey takes its hit from multiple systemic delays as some pediatricians delay referrals, opting for a “wait and see” approach instead of early screening, causing crucial months of intervention to be lost. Even when children are referred, the wait to see an autism diagnostician can stretch beyond 12 months, leaving families in limbo. Once a diagnosis is even confirmed, securing intervention services poses another challenge due to insurance limitations or provider shortages. Families often face difficulties in navigating these barriers, leading to prolonged delays in accessing necessary care.2
“And that’s before you even start intervention. We know that the earlier children receive support, the better their developmental outcomes. But for many families, access to these services is anything but easy.”1,4
For Black families, these challenges are magnified. Studies show that Black children with autism are diagnosed later than their white counterparts and are twice as likely to have intellectual disabilities alongside autism.5,6 This disparity has long-term consequences: children who receive late diagnoses are more likely to require higher levels of support throughout their lives.5,4 Dr. Caravella’s research seeks to dismantle these barriers by utilizing a novel intervention: family navigation
The family navigation model, originally developed in
cancer care, provides structured guidance to help families navigate complex medical and social systems.7 Dr. Caravella believes this model can play a transformative role in autism care by streamlining accessibility for barriers in evaluations, therapies, transportation and other essential services. Family navigation also offers a promising strategy to improve early autism diagnoses for children from low-income and minority backgrounds.7
“Imagine having concerns about your child’s development and then being told you need to wait over a year just to get an answer.”
In a multisite randomized clinical trial involving 249 children aged 15 to 27 months, family navigation significantly reduced the time to diagnostic confirmation and increased the likelihood of receiving a diagnosis within one year7. Since early identification is strongly linked to improved cognitive and behavioral outcomes, targeted interventions like family navigation can help ensure more equitable access to diagnostic services to ensure that children from low-income and racial/ethnic minority families receive the benefits of early ASD identification and treatment.
Dr. Caravella believes that utilizing the family navigation framework can play a crucial role in early intervention services1. This model not only helps ease the barriers and systemic challenges parents face when navigating an autism diagnosis, but it also connects families to a strategic and comprehensive range of local resources and supports. This approach forms the basis of Dr. Caravella’s current study, “Expediting Enrollment into Autism-Specific Intervention for Black Toddlers: A Telehealth-Based Family Navigation Approach,” which aims to group and expedite access to essential services such as ABA clinics, occupational, speech, and feeding therapy for young children with autism.
However, one surprising challenge has emerged in these interventions: not all families are immediately ready to begin intervention. While early intervention is widely recognized as critical, receiving an autism diagnosis can be overwhelming, and some parents need time to process the information before committing to structured therapies. “We sometimes forget that families are absorbing life-changing information,” Dr. Caravella notes “Not every parent is ready to immediately begin services, even though they’re given that health based recommendation, it doesn’t mean they’re ready to make that change.”1

To address this, Dr. Caravella is exploring motivational interviewing, a well-established technique in behavioral health. Motivational interviewing helps individuals work through hesitations by addressing barriers and assessing their readiness8. “If a parent isn’t ready to engage in services, throwing information at them won’t help,” she explains.
“We need to meet families where they are and help them move towards readiness.”1
Dr. Caravella aims to broaden the reach of family navigation by integrating it earlier in the diagnostic process, ensuring families receive support from the moment concerns arise. She also sees potential for applying this model beyond autism, helping families of children with other developmental disabilities and chronic conditions. “The goal is to support families throughout the entire process,” she explains. “So we can reduce delays across the whole trajectory and not just at individual points.”1 By refining these interventions, her research has the potential to reshape how families access care, making early intervention more equitable for all.
“We’ve come so far in recognizing the importance of diversity research,” Dr. Caravella says. “The idea that studying the most vulnerable populations is somehow ‘excluding’ others is completely backward. Researching disparities is how we create equity for everyone.”1
At its core, Dr. Caravella’s work is about inclusion, not exclusion. By identifying and addressing the most significant barriers faced by underserved populations, researchers can improve outcomes for all children with autism, regardless of background. “If we can solve the biggest disparities,” she emphasizes, “we can solve the broader problem much more effectively.”1 With promising results on the horizon, Dr. Caravella hopes that this research will redefine how families move through the healthcare system, ensuring that all children receive the support they need, before it’s too late.
1. Interview with Dr. Caravella, Ph.D. (2025, February 13).
2. Aylward, B.S.; Gal-Szabo, D.E.; Taraman, S. J Dev Behav Pediatr. 2021, 42, 682-689.
3. Kim, S. Clin Exp Pediatr. 2021, 65, 10-20.
4. National Institute of Child Health and Human Development. (2025, March 17). Early intervention for autism. 5. https://www.nichd.nih.gov/health/topics/autism/conditioninfo/treatments/early-intervention
6. Constantino, J.N.; Abbacchi, A.M.; Saulnier, C. Pediatrics. 2020, 146, 1-9.
7. Maenner, M.J.; Warren, Z.; Williams, A.R. MMWR Surveill Summ. 2023, 72, 1-14.
8. Feinberg, E.; Augustyn, M.; Broder-Fingert, S. JAMA Pediatr. 2021, 175, 1-8.
9. Larson, E.; Jeglum, N.; Shmays, C. PEC Innov. 2023, 21, 1-6.

In a constantly evolving world, the topic of high-quality early childhood education has become increasingly important. Ethnic and racial diversity in the United States is increasing, showing no signs of stopping. However, despite this growing diversity, not everyone is afforded the same educational opportunities as others. For Black children, there are many systematic barriers in place to prevent them from getting a high-quality early childhood education that can arise even from

By Aria Dhupkar
Image courtesy of Adobe Stock. Image courtesy of Adobe Stock
birth. Only if children are born without complications can they do well in the future. It is important to address those barriers to alleviate the disparities present in education. At the forefront of this movement is Dr. Iheoma U. Iruka, a tenured professor in the Department of Maternal and Child Health at Gillings School of Global Public Health at the University of North Carolina at Chapel Hill, as well as the Founding Director of the Equity Research Action Coalition (ERAC) at the Frank Porter Graham (FPG) Child Development Institute at UNC.
Before going further into the avenues of advancing equity in education, it is important to define what makes up a “high-quality” early childhood education. According to Dr. Iruka, it is “being able to have a safe environment that reflects their cultural background...” Alongside that, the way the teacher and students interact and the content in class should reflect the way students talk and the history of their community. When schools have a primarily Eurocentric curriculum, it cannot effectively meet the needs of Black students, as it is not reflective of the children’s own lived experiences. Having teachers who are well-trained in the students’ background and can adequately handle their
needs is thus highly necessary because it will allow the students to connect with what they are learning.1 However, one of the most important aspects of high-quality early childhood education is the “agency” that children have in their education. Here, agency refers to the degree of choice that students have. They should have some freedom in how they are learning while still receiving a well-structured education. Accounting for these factors will allow for improvements in early childhood education, especially for minorities. Her research aims to better understand how different factors, such as economic background, safety of educational environment, training level of teachers, and relatability of curriculum, can affect the quality of early childhood education, which is something she has been interested in since getting her Ph.D. at the University of Miami. The impact of systemic racism in education is something that Dr. Iruka has a focus on in her research as a director of ERAC and co-founder of the Researchers Investigating Sociocultural Equity and Race (RISER) Network. Racism is usually seen as a more personal concept, but it can also be present in systems and structures.2
The R3ISE Integrative Model – Racism + Resilience + Resistance Integrative Study of Childhood Ecosystem – that Dr. Iruka and her colleagues developed is an integration of multiple frameworks, such as critical race theory, cultural access, and bio-ecological. The R3ISE model was named very intentionally –it defines racism and brings to light its effects on education so changes can be made. This is important for creating and improving policies that can influence the safety of housing, health care, and high-quality early childhood education. It can highlight different aspects of racism, including cultural, interpersonal, institutional, etc. This model can inform educators of different ways that racism can arise in educational settings so they can work on methods to combat it. While it may seem like the R3ISE model only outlines shortcomings, a unique aspect of this model is that it also highlights cultural assets of minorities. By doing this, the R3ISE model can also be used as an uplifting tool to help minorities “rise” to their full potential.
“What makes up a ‘highquality’ early childhood education... is ‘a safe environment that reflects their cultural background.’”
Classroom level change is extremely important, but Dr. Iruka also emphasizes the importance of looking at this issue from multiple standpoints. Making change on a larger scale through policy is also immensely important for her and says that “this is how the research can reach those who need it.” Through her role as the founding director of the Equity Research Action Coalition at the Frank Porter Graham Child Development Institute, Dr. Iruka has created a “Black Child National Agenda” in collaboration with the National Black Child Development Institute in Maryland, which is a set of goals and policies that aims to dismantle systemic inequities that are hindering black children from succeeding. She also worked with the Children’s Equity Project at Arizona State University, specifically looking at the impact of COVID on early childhood programs, showing collaboration with other

educators and individuals in healthcare. Another project she was involved in is studying the effects of cash transfers on infant health outcomes with colleagues at UC Berkeley. Here, she was looking at the influence of economic principles and infant health on child development and education. In her work, Dr. Iruka values an interdisciplinary approach to her research, as this is what allows findings to be synthesized for the public. This interdisciplinary approach is something that continues with her current projects. More recently, Dr. Iruka and her team have received a grant from the Bill and Melinda Gates Foundation to develop an African-centered practice guide that has strategies and materials to allow proper implementation.3
In current times, the importance of early childhood education cannot be exaggerated. In the words of Dr. Iruka, “children are the future,” so it is important to do whatever it takes so that all children get an equal opportunity to receive a highquality education. In a time of discourse surrounding the importance of diversity in education, Dr. Iruka continues to push back and continue the fight to provide high-quality education for all.
1. Interview with Dr. Iheoma Iruka, Ph.D., 02/21/25
2. Curenton, S. M.; Iruka, I. U.; Sims, J.; Ibekwe-Okafor, N. Introduction to the Supplemental Issue: Advancing Developmental Science on the Impact of Racism in the Early Years. Early Childhood Research Quarterly 2024, 69, S1–S5. https://doi.org/10.1016/j. ecresq.2024.06.001.
3. African-Centered Racial Equity Justice Project: Embracing Culturally Responsive Practices to Improve Early Learning and Child Outcomes | Frank Porter Graham Child Development Institute. Unc.edu. https://fpg.unc.edu/ projects/african-centered-racial-equity-justice-project-embracing-culturally-responsive-practices.
By Ryan Parsaee

Dr. Claudia Yaghoobi is the Roshan Distinguished Professor of Persian Studies and serves as the director of the Center for the Middle East and Islamic Studies at the University of North Carolina, Chapel Hill. Dr. Yaghoobi is a scholar of Iranian cultural studies, and gender and sexuality studies with a focus on the members of sexual, ethnic, and religious minoritized populations. Currently, she researches the experiences in the lives of Iranian women in the modern era. Through a multidisciplinary methodology including literary analysis, historical inquiries, oral history, and ethnographic studies, her work breaks down the structural forces shaping these women’s experiences across the Iranian national contexts as well as the mass international immigration, also known as the diaspora.

Iranian Armenians are an ethnic and religious minority in Iran, tracing their ancestry to Armenians who have lived in the region for centuries. Their presence in Iran became more pronounced in the 17th century when Shah Abbas I forcibly relocated large numbers of Armenians from their homeland to strengthen Persia’s economy and cultural landscape. Over time, Iranian Armenians built thriving communities, particularly in cities like Isfahan and Tehran, maintaining their distinct identity while also integrating into Iranian society.
Despite their contributions, Iranian Armenians have long existed in a precarious position, granted certain protections under Islamic governance as “People of the Book” while remaining outsiders in many aspects of public and political life. Many have since migrated to the United States and other countries, where they must discover their identity within new cultural and racial frameworks. The experience of displacement and the constant negotiation of belonging are central themes in Dr. Yaghoobi’s work.
Dr. Yaghoobi’s upcoming book, Lives in Translation: Voices of Armenian Women in Iran and the US (under contract with UNC Press), interrogates the intersectional discrimination experienced by Iranian Armenian women under the Islamic Republic. Scholarship on Iranian Armenians has often overlooked women’s experiences, treating them as part of a broader Iranian or Armenian history rather than as a distinct group during this time period. Dr. Yaghoobi challenges this by centering her and their voices through autoethnography, a research method that incorporates her personal narratives to understand broader cultural and social phenomena, and oral history, which records firsthand accounts from women who have lived through historical events. By employing these methods, she presents a more nuanced understanding of
Iranian Armenian women’s lives and identities.
A central concept in Dr. Yaghoobi’s research is verants’ughi, a term which she coined in the context of Iranian Armenian cultural productions in her third monograph, Transnational Culture in Iranian Armenian Diaspora (Edinburgh UP, 2023). It describes the continual evolution of identity as they navigate life in different sociopolitical landscapes. In Iran, they are minorities, balancing their Armenian heritage with the dominant Iranian culture. Upon immigration, they often find themselves racialized in new ways, sometimes grouped under a broad Middle Eastern identity and subject to Islamophobic biases despite being Christian.
Dr. Yaghoobi’s work challenges rigid definitions of identity, instead presenting Iranian Armenian women as active participants in shaping their cultural belonging. Through their stories, she highlights how identity is not static but is continually being reshaped by historical, political, and personal experiences.
The mechanisms of gendered oppression play a central role in Dr. Yaghoobi’s research. In her second book, Temporary Marriage in Iran: Gender and Body Politics in Iranian Film and Literature (Cambridge UP, 2020), she critically examines sigheh, or temporary marriage, as both a means of patriarchal control and a site of female agency. While sigheh has been promoted by the Islamic Republic, Dr. Yaghoobi demonstrates how literature and film portray it as a mechanism for regulating women’s sexuality. By analyzing these representations, she highlights the ways in which Iranian women negotiate their position within restrictive legal and cultural systems. Similarly, her edited volume, The #MeToo Movement in Iran (Bloomsbury, 2023), places Iran’s feminist discourse within a global framework, documenting the institutional and social barriers that silence survivors of sexual violence. Her research also examines how digital activism and transnational advocacy have reshaped feminist resistance and challenged government suppression of gender-based violence.
In her first book, Subjectivity in ‘Attar, Persian Sufism, and European Mysticism (Purdue UP, 2017), Dr. Yaghoobi explores themes of gender and power through medieval Persian Sufi poetry and its engagement with subversive identities, laying the groundwork for ideas she would further develop in her later work. In this book, she examines the works of ‘Attar,
and reveals how they engage with themes of marginality, transgression, and divine love. By comparing these texts to contemporary theoretical concepts, Dr. Yaghoobi illustrates their continued relevance to discussions of identity in the modern Middle East. Her analysis further situates her research within broader conversations on historical resistance to normative structures and how literature provides a space for identity negotiation.
Through her interdisciplinary approach, Dr. Yaghoobi’s scholarship bridges multiple academic disciplines, including ethnic studies, feminist theory, diaspora studies, and Middle Eastern literary criticism. Her research explores Iranian culture, identity, and diaspora, while also contributing to broader conversations on migration and intersectionality.

1. Harris, Adrienne. Racializing Religion: Islamophobia and the Middle Eastern Diaspora in America. Oxford UP, 2018.
2. Lewisohn, Leonard. Beyond Faith and Fidelity: Sufism and Gender in Persian Literature. I.B. Tauris, 2014.
3. Najmabadi, Afsaneh. Women with Mustaches and Men Without Beards: Gender and Sexual Anxieties of Iranian Modernity. U of California P, 2005.
4. Paidar, Parvin. Women and the Political Process in Twentieth-Century Iran. Cambridge UP, 1997.
5. Tölölyan, Khachig. The Nation as an Imagined Community: Diaspora and Nationalism in a Transnational Age. Duke UP, 2000.
6. Yaghoobi, Claudia. Lives in Translation: Voices of Armenian Women in Iran and the US. UNC Press, forthcoming.
7. Virtual Interview with Dr. Yaghoobi

Editor-in-Chief

Daniela Danilova Managing Editor

Ria Patel Fundraising Chair

Julia Boltz Associate Editor


Natalie Druffner Treasurer

Kirina Shah Online Content Manager

Sprihaa Kolanukuduru Associate Editor



Alex Li Associate Editor



Publicity Chair

Esha Agarwal Associate Editor
Are you interested in communicating science to a broad audience?
Do you want to engage in thought-provoking investigations?
Does your passion for the sciences extend into the world of research?
Do you want to combine your creative talents with your fascination with science? Carolina Scientific is always looking for staff writers, designers, and illustrators! If you are interested, please contact carolina.scientific@gmail.com Follow us on Instagram @carolinascientific Find us on Facebook facebook.com/CarolinaScientific Follow us on Twitter @UNCSci Check out our website carolinascientific.org




“No thief, however skillful, can rob one of knowledge, and that is why knowledge is the best and safest treasure to acquire.”
- L. Frank Baum


Spring 2025 | Volume 20 | Issue 2
This publication was funded at least in part by Student Fees which were appropriated and dispersed by the Student Government at UNC-Chapel Hill as well as the Carolina Parents Council.