CRITICAL REVIEW: PERINATAL MENTAL HEALTH IN HAMILTON & MONTREAL
IN COLLABORATION WITH THE MCGILL SCIENCE UNDERGRADUATE RESEARCH JOURNAL
MEDUAMPLIFY: HEALTHCARE BARRIERS OF SEX WORK
CRITICAL REVIEW:
α -GALCER, AN
α -CANDIDATE IN TUMOUR SUPPRESSION
CRITICAL REVIEW: MAGIC MUSHROOMS
A MAGICAL THERAPEUTIC OPTION FOR MENTAL HEALTH AND SUBSTANCE USE DISORDERS


APRIL 2023 | ISSUE 43 WWW.THEMEDUCATOR.ORG
CONTENTS 01 INTRODUCTION 02 MEDPULSE 04 PATHOPROFILE 06 IWCH ABSTRACTS 08 MEDUGALLERY 10 MEDUAMPLIFY 14 CRITICAL REVIEW: α-GALCER, AN α-CANDIDATE IN TUMOUR SUPPRESSION 18 CRITICAL REVIEW: MAGIC MUSHROOMS 22 CRITICAL REVIEW: PERINATAL MENTAL HEALTH IN HAMILTON & MONTREAL 26 BIOTECH BLUEPRINT 29 CONTRIBUTORS ARTIST: ASEEL ABONOWARA Bachelor of Health Sciences (Honours), Class of 2024, McMaster University TABLE OF
DEAR READER,
Dear Reader,
As this year comes to a close, we must confront the need to change and grow. Change —as exciting as it can be— means we must bid farewell to the people and places we have grown to cherish. It is, however, essential for us to brave these changes to carry through the journey of life. As universities foster academic advancement, it is easy for us to be overwhelmed by the successes of others. We often forget to acknowledge our own success unless tangible gains are attached, whether that be a grade, scholarship, or job offer. Whether you are a student who has persevered through the academic year or a staff member who has persevered through the publication cycle, we applaud your unwavering efforts along the way. You have gained invaluable knowledge, grown in wisdom, and forged meaningful connections with peers and faculty. Your individual qualities make you incredible, regardless of any accolades you may or may not have received.
We take immense pride in our dedicated staff for embracing our vision to address critical social issues in healthcare. The cover art by Creative Directors Arim and Natalie, along with the table of contents by Aseel Abonawara, demand immediate action on the climate crisis to preserve our natural world and combat pollution. Katelyn Moore’s MeduGallery sheds light on the challenges elderly folk face as they age in place, while Jacqueline Chen, Florence Deng, and Dalraj Dhillon’s MeduAmplify examines the stigma and violence sex workers face in healthcare.
Through familiar article formats, our authors brave new territories of health and research. MedPulse features Audrey Dong and Aisling Zeng in their coverage of global healthcare and research news. In Pathoprofile, Olivia Kim and Rida Tauqir examine prion diseases, while David Gou and Matthew Olejarz present a Critical Review of α-GalCer in tumour suppression. Bhavana Soma and Zahra Alam tackle the use of psilocybin in mental healthcare in our Opinion Piece.

We welcome collaborations, new and old, with other organizations as well. It is our pleasure to feature abstracts from the International Women and Children’s Health Conference, covering important topics such as fetal alcohol spectrum disorder, childhood dyslipidemia, and early hospital discharge after birth. We are thrilled to have the McGill Science Undergraduate Research Journal joining us to deliver a Critical Review on perinatal mental health.

To Aisling, Arim, Carolyn, David, Diane, Eric, Gurleen, James, Ken, Leena, Natalie, Olivia, Shanzey, Suraj, and Yiming —thank you for your exceptional leadership and resilience. It was a great privilege to serve all of you and the McMaster community this past year. As we exit stage right, we welcome Natalie Chu and Suraj Bansal as the new Editors-in-Chief. We expect nothing less than greatness from them as they will continue to grow The Meducator beyond its limits.
Though we bid farewell, we will forever cherish the memories we have formed with you throughout this year. Thank you.
All the best,
MADELINE CHAN
Bachelor of Life Sciences
Class of 2024
INTRODUCTION meducator | april 2023 01 &
(Honours)
JEFFREY SUN Bachelor of Health Sciences (Honours) Class of 2024
 Lycaenidae (Canada)
California Dogface (USA)
Lycaenidae (Canada)
California Dogface (USA)






References can be found on our website: www.themeducator.org
Glassy Bluebottle (China)
Giant Blue Swallowtail (Uganda)
Green-Veined White (UK)
Danube Clouded Yellow (Germany)
ABSTRACT
Prions refer to abnormal misfolded proteins which propagate rare, rapidly progressive, and inevitably fatal neurodegenerative infectious diseases affecting both humans and non-human mammals.1-3 The most common human prion disease is Creudtzfeldt-Jakob disease (CJD), aetiologically categorized as either (1) sporadic (sCJD), (2) acquired via infection (aCJD), (3) hereditary (hCJD), or (4) variant (vCJD).1,2 vCJD, in particular, is commonly known due to its contraction via consumption of beef infected with Bovine Spongiform Encephalopathy, also known as Mad Cow Disease: a similarly fatal prion disease affecting cows.2 Regardless of the causative mechanism, all CJDs are characterized by the rapid decline in cognitive function, myoclonus (involuntary twitching and/or jerking of muscles), akinetic mutism, and ultimately, death in all cases.1-3 As suggested by the aforementioned symptoms, CJD is considered a rapidly progressive dementia (RPD), alongside Alzheimer’s, Huntington’s, and Parkinson’s disease.4
RISK FACTORS
Although sCJD accounts for 85% of CJD cases, current literature has not identified concrete risk factors due to the stochastic misfolding of prions.2 However, age has been shown to influence sCJD, with an average age of onset of 60 years old.5 Numerous genetic factors have also been implicated in sCJD. Specifically, a heterozygous genotype at codon 129 of the PRNP gene, the prion protein gene, has displayed protective factors against the spontaneous prion misfolding in sCJD.6 Furthermore, a genomewide association study conducted by Jones et al. identified two loci that may increase risk of sCJD.7 These include risk variants located in, or nearby, STX6 and GAL3ST1.6 As for aCtJD, risk factors are virtually absent due to advances in clinical practices which mitigate risk of infection, such as the sanitization of neurosurgical instruments previously used on patients with CJD.2
DIAGNOSIS
CJD is difficult to diagnose as it shares numerous symptoms with RPD. To provide a definitive diagnosis of CJD, a brain biopsy or autopsy must be performed so a pathologist can examine the brain tissue.8,9 Typical histopathological findings suggesting CJD
doi: 10.35493/medu.43.4
AUTHORS:
OLIVIA KIM 1 & RIDA TAUQIR 2
1 Bachelor of Health Sciences (Honours), Class of 2026, McMaster University
2 Bachelor of Health Sciences (Honours), Class of 2024, McMaster University
ARTIST: MISHAL HOSSAIN 3
3 Bachelor of Health Sciences (Honours), Class of 2025, McMaster University
include neuronal loss, spongiform degeneration, and astrogliosis.10 Due to this challenging nature of confirming diagnosis, medical professionals must rely on probable diagnostic criteria, which consists of a conjunction of laboratory testing and identification of clinical features. According to the Centers for Disease Control and Prevention, this diagnostic criteria includes a positive result on an electroencephalogram, a cerebral spinal fluid assay, or a magnetic resonance imaging brain scan. In addition to the aforementioned laboratory tests, identifying symptoms such as rapidly progressive cognitive impairment, myoclonus, and visual or cerebellar problems offer a more probable diagnosis of CJD.11
MECHANISM
Part 1: Prion Proteins
CJD arises from the conversion of normal cellular prion proteins (PrPC) into a misfolded aggregated and pathogenic form called scrapie (PrPSc).12 PrPC are cell-surface glycoproteins, which are proposed to be involved in protection against apoptosis, transmembrane signalling, and synaptic formation.13 To complete the previously mentioned functions, PrPC are characterized by their highly α-helical structure, detergentsolubility, and susceptibility to protease digestion. On the other hand, PrPSc are conformationally altered isoforms, effectively adopting the opposite characteristics with a β-sheet structure, detergent-insolubility, and resistance to protease digestion.10,
Part 2: Transformation of PrPC to PrPSc
Represented by the different classifications of CJD, PrPSc can be acquired in several different ways, denoted by the four characterizations of CJD. Regardless of the categorization of CJD, the transformation process of the prion proteins remains consistent in which the PrPSc acts as a template for the conversion of PrPC, seeding the formation of an alternative self-replicating state with a different protein folding pattern.12,14 Although the exact molecular mechanism of the conversion of PrPC to PrPSc is unknown, a study using molecular-dynamics simulations by Chen et al. suggests large conformational changes of the C-terminal globular domain and
PATHOPROFILE meducator | april 2023 04
other structural domains in response to harsh conditions of high temperatures and low pH.15 Ultimately, as the PrPSc conformation self-propagates, there is exponential accumulation of the misfolded isoform in the neurons of the central nervous system (CNS).12
Part 3: Degeneration of the CNS
The beginning stages of CJD appear to be associated with synaptic dysfunction. The human prion protein is enriched in the synapses of neuromuscular junctions and the CNS and thus, the conversion of PrPC to PrPSc results in the accumulation of PrPSc in synaptic structures.16 The toxicity of the accumulated PrPSc begins to induce the release of pro-inflammatory cytokines and reactive oxygen species by activated microglial cells, resulting in neuronal cell death by apoptosis.17 CJD is also characterized by spongiform degeneration in which small vacuoles occupy the gray matter of the brain, which is hypothesized to be caused by autophagic cell death.16 As the degree of neuronal cell death progresses, initial symptoms of slurred speech, dizziness, and vision problems rapidly become more severe with the complete loss of coordination and speech. Finally, patients enter a vegetative state in the final stages of CJD before their death.18 The fatal outcome of this disease can be attributed to extensive neuronal death by autophagy and apoptosis.
TREATMENT
Clinical studies investigating potential CJD treatments are hindered by its scarcity and rapid prognosis. duration of patient survival is 4.5 months following symptom onset, with 90% of patients surviving less than 1 year. there are no known treatments to impede or stop the destruction of neurons as a result of prion diseases. opt to alleviate symptoms and support patients and their families in coping with CJD.6 For example, opiates and anti-seizure medication may be prescribed to diminish pain and myoclonus, respectively.6 Other typically treated symptoms include urinary and bowel inconsistency, dysphagia, and blindness or vision loss. Eventually, once patients cannot move and/or speak, full-time care is administered to attend to their daily needs. patients may draw up an advance directive: a treatment plan detailing preferences in care for when that the patient enters a vegetative state and cannot communicate anymore. also worthy to acknowledge current exploration of potential CJD treatments. Notably, Mead et al. conducted the very first experimental treatment targeting human prion diseases in 2022, administering anti-PrPC monoclonal antibody (mAb) therapy to 6 CJD patients.20 Their findings suggest favorable concentrations of anti-PrPC mAbs in CSF and brain tissue, encouraging future exploration in this potentially groundbreaking CJD treatment.
REVIEWED BY: DR. ALBERT AGRO (MD, PHD)
Dr. Albert Agro is an assistant professor specializing in pathology and molecular medicine. He received his PhD in the Department of Medicine at McMaster University, and currently holds a position of chief medical officer of Cynapsus, a pharmaceutical company, as well as CEO of HNZ Strategic Holdings, Inc., a clinical consulting firm. He possesses a wide range of interests, particularly the pathology and treatment of Parkinson’s disease.
1. Iwasaki Y. Creutzfeldt-Jakob disease. Neup. 2016;37(2):174-88. Available from: doi:10.1111/ neup.12355.
2. Vacca VM. CJD: Understanding Creutzfeldt-Jakob disease. Nurse. 2016;46(3):36-42. Available from: doi:10.1097/01.NURSE.0000480598.84274.0f.
3. De Villemeur TB. Creutzfeldt-Jakob disease. Handb Clin Neurol. 2013;112:1191-3. Available from: doi:10.1016/B978-0-444-52910-7.00040-4.
4. Hermann P, Zerr I. Rapidly progressive dementias aetiologies, diagnosis and management. Nat Rev. 2022;18:363-76. Available from: doi:10.1038/s41582-022-00659-0.

5. Alzheimer’s Association. Creutzfeldt-Jakob Disease [Internet]. 2023. Available from: https:// www.alz.org/alzheimers-dementia/what-is-dementia/types-of-dementia/creutzfeldt-jakobdisease [cited 2023 Feb 22].
6. Jones E, Mead S. Genetic risk factors for Creutzfeldt-Jakob disease. Neurobiol Dis. 2020;142:104973. Available from: doi:10.1016/j.nbd.2020.104973.
7. Jones E, Hummerich H, Viré E, Uphill J, Dimitriadis A, Speedy H, et al. Genome-wide association study identifies risk variants for sporadic Creutzfeldt-Jakob disease in STX6 and GAL3ST1. Lancet Neurol. 2020;20:30273-8. Available from: doi:10.1016/s14744422(20)30273-8.
8. Tyler K. Creutzfeldt-Jakob disease. N Engl J Med. 2003;348(8):681-2. Available from: doi:10.1056/NEJMp020187.
9. Sitammagari KK, Masood W. Creutzfeldt Jakob disease. 1st ed. Treasure Island (FL): StatPearls Publishing; 2022
10. Budka H. Neuropathology of prion diseases. Br. Med. Bull. 2003;66(1):121-30. Available from: doi:10.1093/bmb/66.1.121
11. Centers for Disease Control and Prevention. CDC’s diagnostic criteria for Creutzfeldt-Jakob disease (CJD) [Internet]. 2018. Available from:https://www.cdc.gov/prions/cjd/diagnosticcriteria.html [cited 2023 Feb 22].
12. Atkinson CJ, Zhang K, Munn AL, Wiegmans A, Wei MQ. Prion protein scrapie and the normal cellular prion protein. Prion. 2016;10(1):63-82. Available from: doi:10.1080/19336896.20 15.1110293.
13. Westergard L, Christensen HM, Harris DA. The cellular prion protein (PrPC): Its physiological function and role in disease. Biochim Biophys Acta. 2007;1772(6):629-44. Available from: doi:10.1016/j.bbadis.2007.02.011.
14. Spagnolli G, Rigoli M, Inverardi GN, Codeseira YB, Biasini E, Requena JR. Modeling PrPSc generation through deformed templating. Front Bioeng Biotechnol. 2020;8:590501. Available from: doi:10.3389/fbioe.2020.590501.
15. Chen W, Van der Kamp MW, Daggett V. Structural and dynamic properties of the human prion protein. Biophys J. 2014;106(5):1152-63. Available from: doi:10.1016/j.bpj.2013.12.053.
16. Soto C, Satani N. The intricate mechanisms of neurodegeneration in prion disease. Trends Mol
PATHOPROFILE meducator | april 2023 05
SUPPORTING HEALTHY PREGNANCIES: UNDERSTANDING PREGNANT WOMEN AND NEW MOTHERS’ PERSPECTIVES REGARDS FETAL ALCOHOL
SPECTRUM DISORDER PREVENTION CAMPAIGNS TO INFORM EFFECTIVE AND NON-STIGMATIZING APPROACHES IN NORTHEASTERN ONTARIO
BACKGROUND: Fetal Alcohol Spectrum Disorder (FASD) is a diagnostic term used to describe the lifelong impacts on fetal development from prenatal alcohol exposure. Alcohol use during pregnancy has been identified as a significant public health concern, as up to 15% of Canadian women report consuming alcohol during pregnancy. Current FASD prevention efforts have been criticized for their harmful and stigmatizing nature as emotional aspects (e.g., fear, guilt, and shock) have been relied on to discourage individuals from consuming alcohol during pregnancy. Consequently, pregnant individuals and new mothers may be reluctant to disclose information about their alcohol consumption, which may prevent them from receiving support. Therefore, improving current FASD prevention initiatives could help improve supports for pregnant individuals, new mothers, and individuals with FASD.
RESEARCH OBJECTIVES: The objectives of this study include:
(1) to explore pregnant and postpartum women’s attitudes about alcohol use during pregnancy, and their perspectives on existing FASD prevention campaigns; and (2) to generate recommendations for non-stigmatizing FASD prevention campaigns for Northeastern Ontario.


METHODS: Using a basic qualitative approach (Merriam & Tisdell, 2016), this study has employed small group and individual semi-structured interviews via Zoom. Participant recruitment was conducted utilizing social media platforms and through the assistance of community partnering agencies and local organizations. To date, 12 pregnant women and new mothers between the ages of 17 and 45 (Mage = 30, SD = 4.85) across the Sudbury and Manitoulin regions of Northeastern Ontario have participated in this study. Messaging and imagery from 10 existing prevention campaigns were employed to facilitate discussion. Data from this study are being analyzed using Bengtsson’s (2016) qualitative content analysis to generate salient themes from participants’ responses.
RESULTS: At the time of this submission, data analysis is ongoing. However, preliminary findings have revealed that participants have favourable attitudes towards abstaining from alcohol during pregnancy. Findings indicate that participants associate the effectiveness of FASD prevention efforts at preventing alcohol use during pregnancy with the strength of the campaign messaging, if the campaign has an emotive impact, and the overall relatability of the imagery used. For instance, campaigns with a strong message were perceived as being more effective at preventing alcohol use during pregnancy than those with a perceived weak message. Additionally, FASD prevention campaigns that evoked a strong emotional response were perceived as more effective at preventing alcohol use during pregnancy than FASD prevention campaigns that did not have an emotive impact. Preliminary findings revealed that the more relatable the campaign imagery is, the more effective the campaign is perceived to be at preventing alcohol use during pregnancy. Lastly, findings show that current FASD prevention initiatives are lacking and require enhanced accessibility and messages of support.
CONCLUSIONS: Although participants perceive these things as more effective, they can conflict with best practices for FASD prevention messaging, as evocative messages and imagery can reinforce stigma about FASD and alcohol consumption during pregnancy. In summary, the current study will contribute to the growing discourse on informing nonstigmatizing FASD prevention initiatives for Northeastern Ontario. Alcohol use during pregnancy is a growing concern among many Northern Ontario communities; therefore, it is crucial to acquire an understanding of pregnant women and new mothers’ attitudes about alcohol use during pregnancy to help inform non-stigmatizing FASD prevention efforts.
TAYLOR WATKINS1, DR. KELLY HARDING1,2, DR. SHELLEY WATSON3, & CELISSE BIBR1,2 1Laurentian University; 2Canada FASD Research Network; 3Cambrian College
06 IWCH ABSTRACTS meducator | april 2023
ARTIST: MISHAL HOSSAIN Bachelors of Health Sciences (Honours), Class of 2025, McMaster University
COMMUNITY CLINICIAN MANAGEMENT PATTERNS OF CHILDHOOD DYSLIPIDEMIA
BACKGROUND: Childhood dyslipidemia increases the risk of atherosclerosis in childhood and cardiovascular disease (CVD) in young adulthood. The atherosclerotic process begins in childhood. However, adverse health outcomes due to disease are rare in early life. Unmanaged lifelong atherosclerotic processes can result in myocardial infarction and stroke. Management of risk factors including childhood dyslipidemia can decrease the risk of CVD and adverse health outcomes in later life. At the time of the study, there were no Canadian paediatric guidelines for lipid screening. Children with abnormal lipid profiles may be overlooked. Despite childhood dyslipidemia identification, early intervention and management may not be initiated. Primary care physicians (PCP) are optimally positioned to educate and reinforce health behaviours that minimize the risk of CVD and promoting lifelong cardiovascular health.
OBJECTIVES: To describe clinician management patterns for childhood dyslipidemia in the community setting.
METHODS: A retrospective chart review was conducted for children 2 to 10 years of age with abnormal lipid profiles between 2008-2021. Participants were from the TARGet Kids! cohort, Canada’s largest primary care research network for children. Participants in the cohort had completed annual non-fasting blood samples and questionnaires. The primary study outcome was the proportion of physicians engaging in each management practice. R version 3.6.2 (R Foundation for Statistical Computing, Vienna, Austria) was used for statistical analysis.
RESULTS. Within the TARGet Kids! cohort, 790 children were identified with dyslipidemia. Among these children, 768 were seen by PCP at their next follow-up visit while 22 children had no follow-up visit. PCP rarely informed families about abnormal lipid profiles (n=11, 1.43%). All families notified about abnormal lipid profiles were informed at a follow-up visit (n=4, 36.4%), through a phone call (n=6, 54.5%), or through both methods (n=1, 9.1%). PCP frequently counselled on diet and eating habits (n=535, 95.0%), but less often on physical activity (n=160, 28.4%), sleep (n=108, 19.2%), and screen time (n=24, 4.3%). Family history of CVD, diabetes, high cholesterol, or hypertension was occasionally discussed (n=11, 2.0%). PCP repeated fasting lipid profiles uncommonly (n=23, 3.0%). Management plans for abnormal lipid profiles were infrequently documented (n=4, 0.5%), and all involved dietary counselling. Only 3 participants had a follow-up visit booked (n=3, 0.4%). Referrals were rarely made to dieticians and feeding clinics (n=6, 0.8%) and were not in response to abnormal lipid levels.
CONCLUSION. Childhood dyslipidemia is a risk factor for cardiovascular disease in later life. Our study showed that among children identified with dyslipidemia, PCP rarely identified and initiated early management for abnormal lipid profiles. Our results may inform the need for dissemination of paediatric lipid screening and management guidelines to support best clinical practice. There is no actual or potential conflict of interest in relation to the findings presented.
EARLY HOSPITAL DISCHARGE FOLLOWING UNCOMPLICATED BIRTH
KESHINI SRIARULNATHAN1, ANNE M. MALOTT RM PHD2
1Department of Science, McMaster University, 2Department of Family Medicine, McMaster University
BACKGROUND: The current rise of COVID-19 coronavirus has impacted the experiences of new parents in Canada with restrictions on hospital visitors and concerns of nosocomial infections. Early hospital discharge has the potential to reduce exposure, promote the transition to parenthood and breastfeeding duration, and reduce healthcare costs due to shorter hospital length of stay. However, little is known about the impact of early discharge on health outcomes for parturients, neonates, or the healthcare system.
AIM: This review examines existing literature on early postnatal discharge programs following uncomplicated vaginal births as relevant to the Canadian context to determine how it has impacted the clinical outcomes of parents and newborns, patient satisfaction, and the health system.
METHODS: A literature search of electronic databases: PubMed, Scopus, ScienceDirect, Web of Science, and CINAHL evaluated peer-reviewed, primary research published in English from 1976 through 2021. A total of 40 studies were yielded and content analysis identified the population, location, study design, methodology, and significant findings of each with attention to relevance to the Canadian context to determine the generalizability of the findings.
RESULTS: There is a dearth of well-designed studies that include consistent definitions of early discharge and uniform policies and practices for follow-up care for birthing people and their babies.
Conclusion: There is a need for further research exploring the health outcomes of Canadian birthing people and their neonates following early hospital discharge after uncomplicated births. There is also a need to examine the impact of early discharge on the healthcare system in the Canadian context that includes a clear definition of early discharge and specification of care provided in the community following discharge.
IWCH ABSTRACTS meducator | april 2023 07
TOM KN1, DESILVA N2, POLACK A3, SINGH K4, KEOWN-STONEMAN C4, MAGUIRE J4, BIRKEN CS3, WONG PD3
1Michael G. DeGroote School of Medicine, McMaster University; 2Faculty of Medical Sciences, Western University; 3Hospital for Sick Children; 4Li Ka Shing Knowledge Institute, Unity Health Toronto,
ARTIST: KATELYN MOORE
Bachelor of Kinesiology (Honours)
Class of 2023, McMaster University
With the risks that aging poses to health, elderly individuals often find themselves with a difficult choice to make: stay home or admit into a nursing home. With limited at-home resources available in today’s healthcare, several choose to move to long-term care homes to avoid risk of at-home dangers such as injuries and falls. Unfortunately, this transition often proves to be mentally challenging for many retired individuals. Between social disonnection, loss of familiar environments and memories, progression of disease/injury, and altering of financial autonomy, it is reasonable that elderly individuals often feel out of control of not only their health, but also their happiness when moving out of their homes.1
Progression of aging differs greatly between indviduals – there is no way of predicting how one person may develop with age in comparison to another – thus, elderly couples often face risk of separation due to differences in care needs. Along with moving between a familiar home to an unfamiliar care home environment, symptoms such as confusion and anxiety can be aggravated with separation from loved ones, making already-isolating cognitive disorders such as dementia even more challenging to manage.
In light of the COVID-19 pandemic, feeling out of place was particuarily easier for those making the transition from personal homes to nursing homes.2 With the isolation that quarantine demanded of communities, it was even more common for elderly individuals to be placed in vulnerable and confusing situations.2
Managing the phenomenon of aging is by no means an easy feat – when caring for an aging loved one, it’s hard to know what is the “right” decision when it comes to care homes and separation. Likewise, it’s difficult for elderly individuals to know when it is the right time to seek extra care outside of home. As such, the message of this piece is not one to bespeak a right and wrong answer, but rather highlight the importance of us to consider the needs of the people at the centre of the wake: our parents, our grandparents, relatives, siblings, friends, for it those people where home truly is.

MEDUGALLERY 08 meducator | april 2023

MEDUGALLERY meducator | april 2023 09
1. Newman M, Zainal N. The value of maintaining social connections for mental health in older people. The Lancet Public Health. 2020;5(1): 12-13. Available from: doi: 10.1016/s24682667(19)30253-1
2. Van der Roest H G, Prins M, Van der Velden C, Steinmetz S, Stolte E, Van Tilburg T G, de Vries D H. The impact of covid-19 measures on well-being of older long-term care facility residents in the Netherlands. Journal of the American Medical Directors Association. 2020;21(11): 1569-1570. Available from: doi: 10.1016/j.jamda.2020.09.007
HEALTHCARE BARRIERS OF SEX WORK
doi: 10.35493/medu.43.10
AUTHORS: JACQUELINE CHEN 1, FLORENCE DENG 1 & DALRAJ
DHILLON 2

1 Bachelor of Health Sciences (Honours), Class of 2026, McMaster University
2 Bachelor of Health Sciences (Honours), Class of 2024, McMaster University
ARTIST: FAN ZE (ALEX) WANG 3
3 Bachelor of Health Sciences (Honours), Class of 2026, McMaster University
INTRODUCTION
Sex workers are a heavily stigmatized and marginalized group that shoulder the burden of extreme health inequalities and unmet health needs.1 Sex work is defined as “the consensual exchange of sexual services between adults for money or goods,” with sex workers being individuals working in a variety of venues to provide such an exchange.2 Due to substantial systemic and judicial barriers, poor public perception, accessibility to proper health maintenance, and preventative services for sex workers is lacking and calls for reform.



SOCIAL STIGMAS
There are many social stigmas surrounding the sex industry and its workers, which prevents transparency between them and their physicians. In one study conducted by Benoit et al. which surveyed sex workers aged 19 years or older, 37% of participants did not disclose their occupation to healthcare providers.3 Despite knowing the potential harms of nondisclosure, disclosure has also negatively impacted the care that sex workers received on many occasions. Given the discrimination faced by these individuals due to the perception of their employment as propagating
MEDUAMPLIFY meducator | april 2023 10
sexually-transmitted infections and transgressing social norms, they can face many accessibility barriers to healthcare. For 11% of workers who did disclose, health care providers allowed their preconceived notions about sex work coupled with intersecting stigmas such as substance abuse to influence their perception of the person’s integrity or misinform them of the type of health care they were seeking.3 Moreover, these social stigmas impact sex workers’ accessibility to healthcare. A study by Socías et al. evaluating healthcare barriers among female sex workers in Vancouver, Canada found that even within settings established to provide universal health coverage, there are institutional barriers to sex workers receiving quality care.⁴ Of the 723 included study participants, 70.4% reported one or more institutional barriers to care.⁴ Of these, 54.6% included long wait times, 36.5% described limited hours of operation, and 26.1% reported perceived disrespect by health care providers.⁴ Ultimately, these experiences leave sex workers shouldering the responsibility of researching their health concerns, forgoing testing for sexually transmitted infections (STIs), or seeking therapy for mental illness. Given the fraught relationships these individuals have with their physician and the healthcare system, many sex workers face issues around self-disclosure, a challenge also cited by 20% of the study’s participants.3 Many sex workers are also extremely wary of trusting their physicians despite patient-physician confidentiality agreements. For many, a record of sex work activity on their medical records could be a threat to legal proceedings, such as custody cases or even post-secondary applications.3 Without quality healthcare access or care, many sex workers have unaddressed mental health needs, are more likely to suffer from substance abuse, and experience violence within and outside their profession.5
VIOLENCE AND CRIMINALIZATION
The high prevalence of violence amongst sex workers and sexual health-related consequences renders it a healthcare issue. Sex workers face disproportionately high lifetime rates of workplace violence, with the prevalence ranging from 45-75% globally.⁵ The most common forms of violence include physical and sexual assault, rape, deceptive condom removal, and robbery.⁶ Subsequent adverse health effects can manifest as depression, posttraumatic stress disorder, STIs, unplanned pregnancy, and death.⁶ This is further exacerbated by the pre-existing vulnerabilities amongst the sex worker demographic, whom are commonly exposed to extensive trauma such as child abuse, domestic, and sexual violence.⁷
Furthermore, given the nature of their work, another major area of concern for the sex worker population is sexual and reproductive health. Inaccessibility to trauma-informed care, mental health services, and sexual health services is detrimental to the workplace safety and mental and physical well-being of sex workers.⁷ Unmet health needs, as defined by Health Care for Women International, encompasses the disparity between “services deemed necessary to deal with a defined health problem and the services actually received.”⁸ Canadian researchers suggest that sex workers frequently have improper access to sexual and reproductive health and preventative services, such as cervical screenings and HIV testing.⁸ Hence, the healthcare system fails to address the sexual risks existing within this occupation.
The issue of violence and subsequent health concerns for sex workers is interrelated with the criminalization of sex work, which largely influences patterns of violence.⁵ As sex workers are considered illegal under the law, violent acts occuring within the context of sex work are not monitored nor regulated by formal entities. A lack of legal protection for sex workers by police and judicial systems leaves the population highly vulnerable.⁵ A 2014 study done in Vancouver following a sex work enforcement policy prioritizing targeting of clients suggests heavy policing may have unintended dangers. The percentage of workers reporting physical abuse or rape prior to and post-policy did not reveal a statistical significance.⁹ Emphasis on criminalization of sex work clients rather than worker safety has escalated dangers faced by sex workers. Targeting by police has resulted in an inability to screen clients and negotiate terms of sexual transactions given clients’ hesitancy to attract police attention. This results in displacement to isolated areas for the sexual transaction to take place, leaving the sex worker with few resources for help and at increased risk of violence and rape.⁹ Immigrant sex workers are further documented as being even more likely to face reduced access to certain health-related prevention services (i.e., HIV, HCV testing) compared to Canadian-born counterparts.⁸ This calls into attention additional barriers such as language, unfamiliarity with local health systems, lack of insurance, bringing in potential racial and ethnic prejudices that perpetuate inaccessibility.⁸

MEDUAMPLIFY meducator | april 2023 11
IMPLEMENTED LEGISLATURE/MITIGATION OR AWARENESS STRATEGIES
As mentioned above, the overwhelming bulk of the issue lies in the criminalization of sex work. In 2014, the Canadian government passed the Protection of Communities and Exploited Persons Act as a form of end-demand legislature focused on dismantling the sex work industry by making purchasing services illegal.10 While the sale of sex work is legal, the act exacerbated the powerful stigma around sex work and sex workers, which has since limited their ability and willingness to access health resources.11 This strategy closely resembles the Nordic approach to sex work legislature that was implemented in countries such as Norway and Sweden, which similarly focuses on ending demand for sex work.12 This approach has been largely critisized for its lack of efficacy in dwindling the sex work industry while also putting sex workers at higher risks for violence and poor health outcomes. Evidently, major changes should be made to the Canadian legislature to decrease the impact of criminalization on sex workers’ health and reduce stigma around the profession. Current interventions are aimed primarily at aiding current sex workers looking to leave the industry. The Exit Doors Here: Helping Sex Workers Leave Prostitution program is centered on counseling and social work, and uses therapy, support groups, skills training, and other strategies to help support people wishing to leave the industry.13 While programs like this have shown some success, they fail to target the underlying social

factors which lead to individuals pursuing sex work as a career. Thus, adopting other approaches to sex work legislature has been proposed as a possible solution. For example, in the Netherlands, adult prostitution is recognized as a legitimate occupation. This consequently results in employers in the sex work industry being required to follow strict guidelines and by-laws which aim to protect workers, such as mandatory hygiene regulations, taxes, and social insurance requirements.12 This approach ultimately gives sex workers comparable rights and protection as other occupations and removes many of the barriers which prevent these individuals from accessing necessary support services.

CONCLUSION
Overlooked, stigmatized, and underrepresented, sex workers deserve the same access and support to healthcare resources as the rest of Canadians. Current legislation reinforcing the criminalization of sex work contributes to the stigmatization, violence, and consequent negative health outcomes disproportionately faced by sex workers. Moving forward, the Canadian government must look towards adopting a new approach to sex work legislation and increase access to healthcare for individuals in sex work. As citizens, we should urge those in power to make these changes and vocalize our support for sex workers’ health rights. Ultimately, as Canadians we must advocate for healthcare as a right which is based on need, not the occupation which one pursues.
MEDUAMPLIFY meducator | april 2023 12
REVIEWED BY: ELENE LAM
EDITED BY: ALLISON FANG & ZAHRA TAUSEEF
1. Potter LC, Horwood J, Feder G. Access to healthcare for street sex workers in the UK: Perspectives and best practice guidance from a national cross-sectional survey of frontline workers. BMC Health Serv Res. 2022;22(178). Available from: doi:10.1186/s12913-022-07581-7.
2. Sex work in Canada: The public health perspective. Ottawa: Canadian Public Health Association; 2014. 14 p.
3. Benoit C, Smith M, Jansson M, Magnus S, Maurice R, Flagg J, et al. Canadian Sex Workers Weigh the Costs and Benefits of Disclosing Their Occupational Status to Health Providers Sex Res Soc Policy. 2019;16:329-41 Available from: doi:10.1007/s13178-018-0339-8.
4. Socías ME, Shoveller J, Bean C, Nguyen P, Montaner J, Shannon K. Universal coverage without universal access: institutional barriers to health care among women sex workers in Vancouver, Canada. PloS one. 2016;11(5). Available from: doi:10.1371/journal.pone.0155828.

5. Deering KN, Amin A, Shoveller J, Nesbitt A, Garcia-Moreno C, Duff P, et al. A systematic review of the correlates of violence against sex workers. Am J Public Health. 2014;104(5):42-54. Available from: doi:10.2105/ AJPH.2014.301909.
6. Bungay V, Guta A. Strategies and challenges in preventing violence against Canadian indoor sex workers. Am J Public Health. 2018;108(3):393-8. Available from: doi:10.2105/ AJPH.2017.304241.
7. Potter LC, Horwood J, Feder G. Access to healthcare for street sex workers in the UK: Perspectives and best practice guidance from a national cross-sectional survey of frontline workers. BMC Health Serv Res. 2022;22(178). Available from: doi:10.1186/s12913-022-07581-7.
8. Sou J, Goldenberg SM, Duff P, Nguyen P, Shoveller J, Shannon K. Recent im/migration to Canada linked to unmet health needs among sex workers in Vancouver, Canada: Findings of a longitudinal study. Health Care Women Int. 2017;38(5):492-506. Available from: doi:10 .1080/07399332.2017.1296842.
9. Krüsi A, Pacey K, Bird L, Taylor C, Chettiar J, Allan S, et al. Criminalisation of clients: Reproducing vulnerabilities for violence and poor health among street-based sex workers in Canada–a qualitative study. BMJ Open. 2014;4:e005191. Available from: doi:10.1136/ bmjopen-2014-005191.
10. Sarai R. Preventing harm in the Canadian sex industry: a review of the Protection of Communities and Exploited Persons Act. House of Commons Canada; 2022 Jun.
11. Pearson J, Shannon K, McBride B, Krüsi A, Machat S, Braschel M, et al. Sex work community participation in criminalized environments: a community-based cohort study of occupational health impacts in Vancouver, Canada: 2010–2019. Int J Equity Health. 2022 Dec;21(1):18. Available from: doi:10.1186/s12939-022-01621-8.
12. Sex Work in Canada: The Public Health Perspective. Canadian Public Health Association; 2014 Dec.
13. Government of Canada. Exit Doors Here: Helping Sex Workers Leave Prostitution [Internet]. Public Safety Canada. 2018. Available from: https://www.
Culture that includes Research that impacts Education that inspires surgery.mcmaster.ca @mcmastersurgery


Elene Lam is a PhD student currently studying at the School of Social Work at McMaster University. She is also the founder of Butterfly, a grassroots group advocating for the rights of Toronto’s Asian and migrant sex workers.
MEDUAMPLIFY meducator | april 2023 13
CRITICAL REVIEW
α-GalCer, AN α-CANDIDATE IN TUMOUR SUPPRESSION
CRITICAL REVIEW meducator | april 2023 14
ARTIST: STEPHANIE ALELUYA Bachelor of Health Sciences (Honours), Class of 2026, McMaster University
doi: 10.35493/medu.43.14
DAVID GOU & MATTHEW OLEJARZ
olejarzm@mcmaster.ca, goud@mcmaster.ca
Bachelor of Health Sciences (Honours), Class of 2026, McMaster University
ABSTRACT
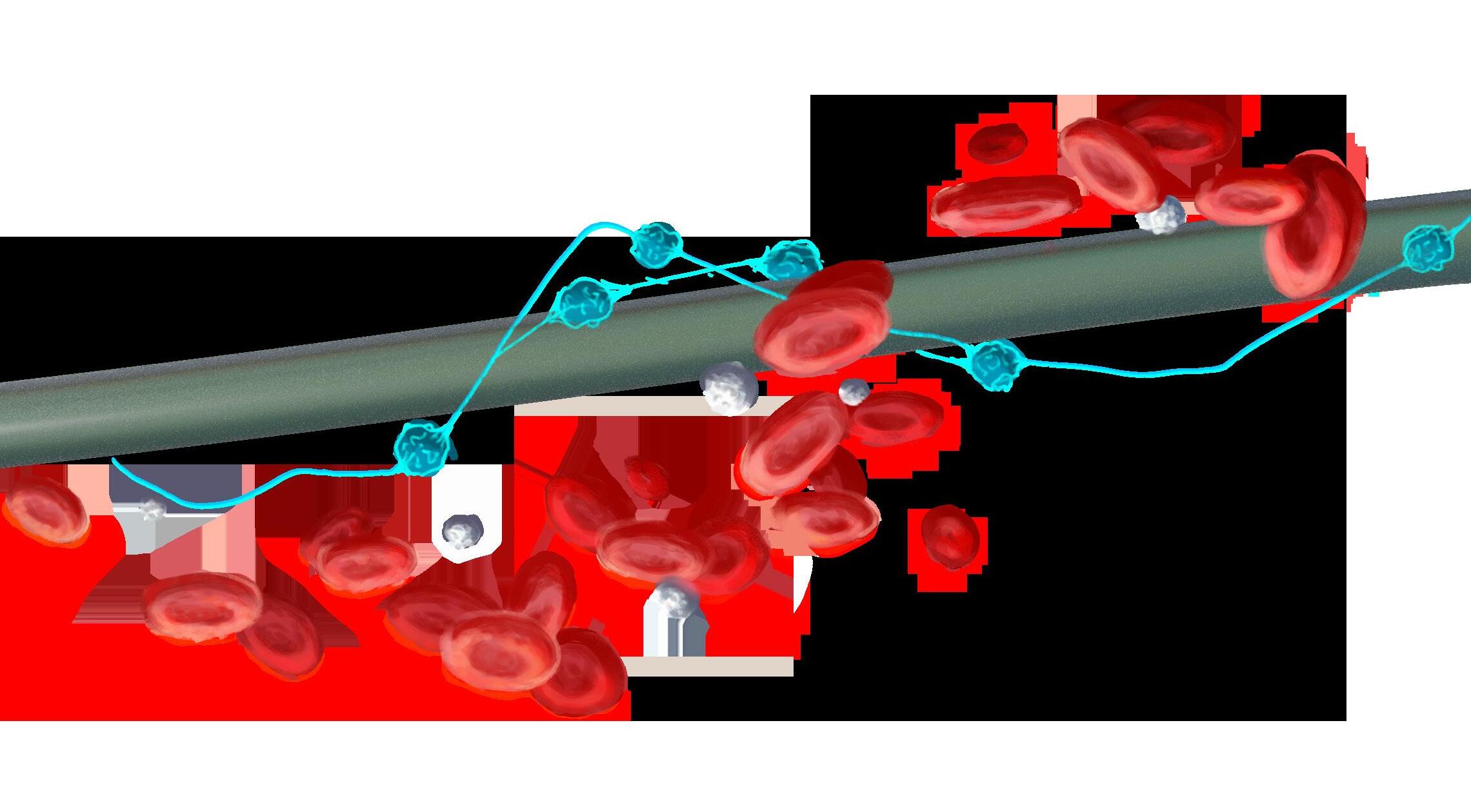
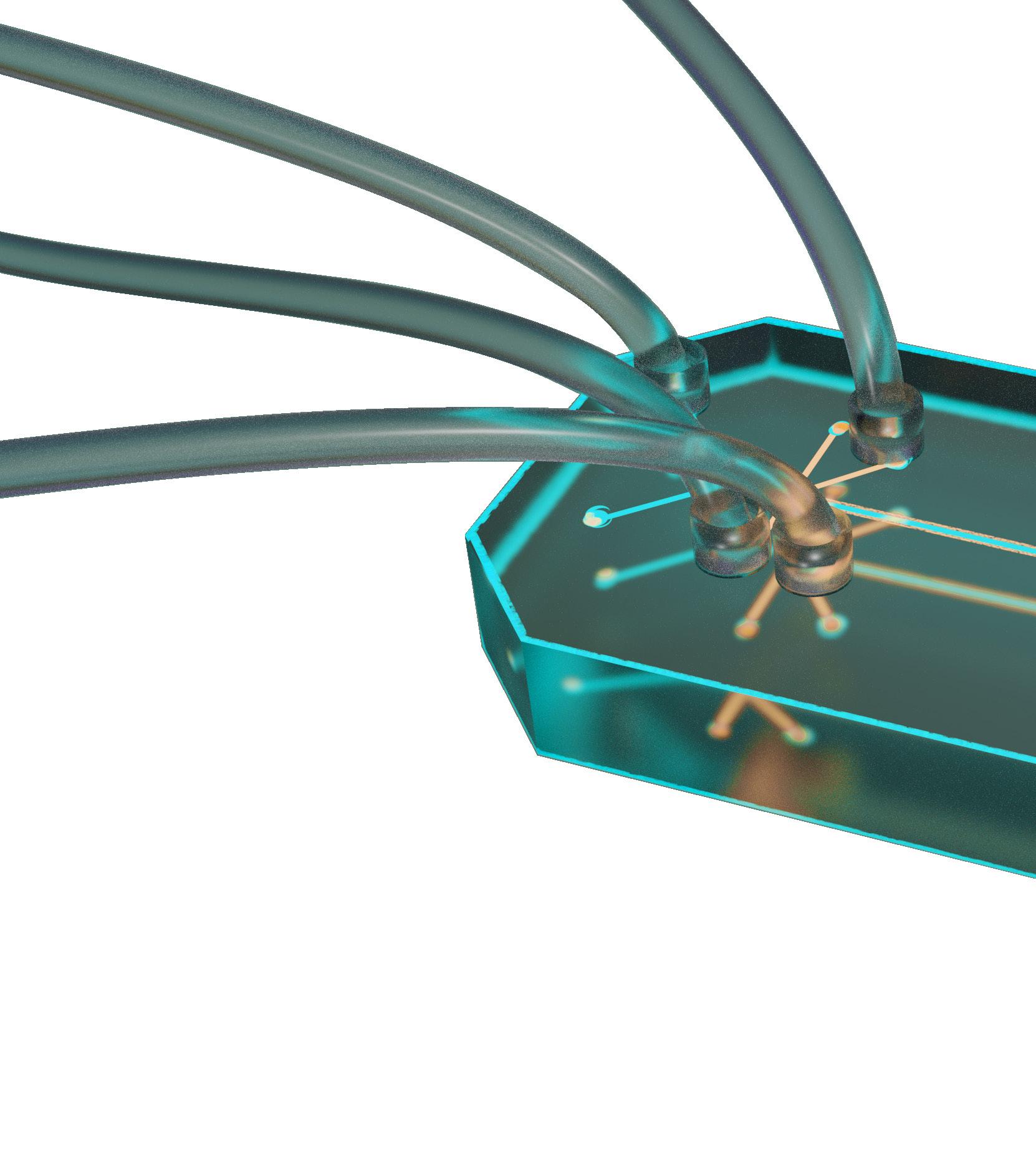
Alpha-Galactosylceramide (α-GalCer, KRN7000) is an exogenous glycolipid ligand that is presented by CD1d molecules in antigen-presenting cells (APCs). It activates invariant natural killer T (iNKT) cells, characterized by semi-invariant T cell receptors (TCRs), which often leads to further downstream activation of the immune system. For example, iNKT cells release cytokines that regulate myeloid-derived suppressor cells (MDSCs) to promote tumor suppression. This critical review aims to clarify the observed effects of α-GalCer by examining recent studies, ranging from in vitro experiments with mice to in vivo clinical trials with humans. Within the current literature, α-GalCer has demonstrated beneficial effects toward tumour suppression. Most pre-clinical studies evaluating α-GalCer have seen success in suppressing tumour growth and increasing patient lifespan, although clinical trials yield inconclusive results. For example, the use of α-GalCer comes with severe limitations, including the induction of immune cell anergy amongst other unwanted side effects. Future studies and trials will be necessary to evaluate the full potential of α-GalCer. Nonetheless, α-GalCer may be a promising agent in combating cancer.
BACKGROUND

One of the most destructive leading causes of death worldwide is cancer, a group of diseases that involve the rapid and abnormal proliferation of cells beyond their usual boundaries.1 These cells can grow and spread to other organs through metastasis, which is the primary cause of death from cancer.1 Unfortunately, difficulty targeting cancer cells and the severe side effects of existing treatments make cancer difficult to cure, contributing to the annual death toll of over 10 million patients globally.1,2 While cytotoxic immune cells are theorized to control tumor development, cancer cells have developed numerous strategies to avoid detection from the immune system.3,⁴
A promising field of immunotherapy research involves iNKT cells and α-GalCer. iNKT cells are a unique type of killer T cell with a semi-invariant TCR and they play important immunoregulatory roles by producing cytokines that influence the actions of other immune cells.⁵,⁶ Almost all iNKT cells respond to α-GalCer, a potent glycolipid agonist that initiates a cascade of strong anti-tumor activity.⁵,⁷ Agelasphins, including α-GalCer,
were first isolated by the marine sponge Agelas mauritianus and exhibited high in vivo antitumour properties against murine B16 melanoma.⁸,⁹ Further investigations showed that α-GalCer was not directly cytotoxic to tumour cells, but rather stimulated the immune system via activation of natural killer (NK) cells.⁸,⁹


While the fundamental mechanisms and interactions of iNKT cells and α-GalCer are documented, studies have shown mixed results. This critical review will analyze the strengths and areas for further research of in vitro studies, murine models, and human clinical trials in this field of research.
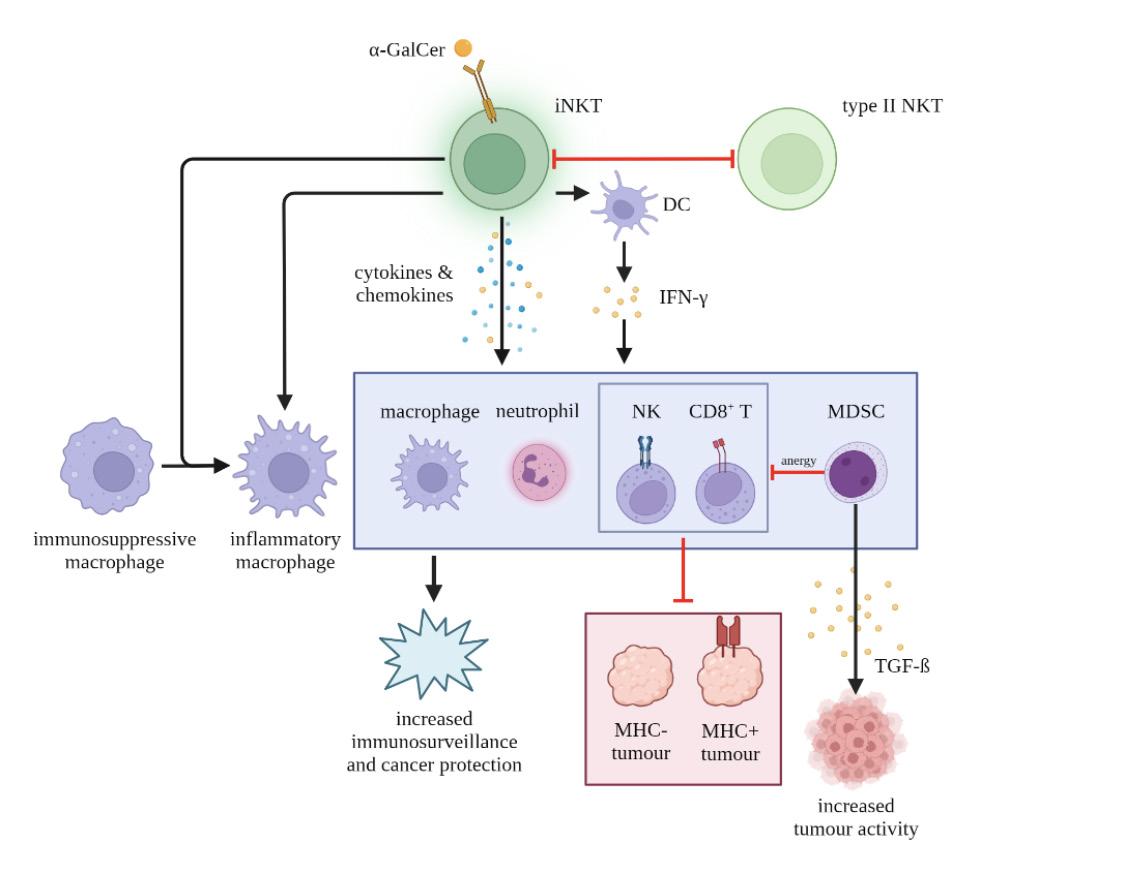
INKT MECHANISMS OF ACTION
iNKT cells commonly operate in the tumor microenvironment (TME) by recognizing glycolipid antigens most commonly presented on APCs or tumour cells by the CD1d protein. This response mechanism allows for the upregulation of immunosurveillance and activation of downstream effectors.
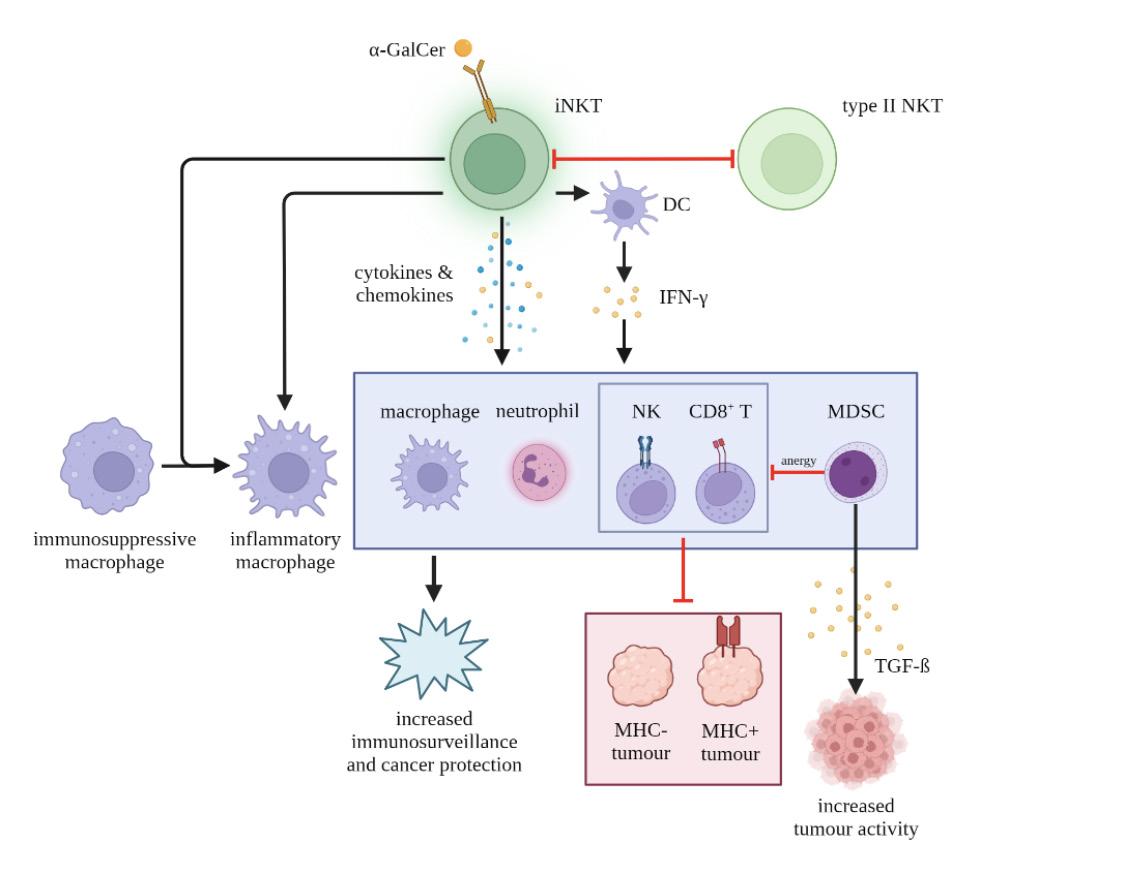
Stimulated iNKT cells can rapidly produce cytokines and chemokines. One example is interleukin 12 (IL-12), an important cytokine for type 1 T helper (Th1) responses, including cancer protection.12 It can be produced directly by iNKT cells or through intermediates, such as activated dendritic cells (DCs).13,1⁴ Cytokines activate or recruit immune cells including NK cells, CD8+ T cells, B cells, macrophages, neutrophils, and MDSCs.13,1⁵ In particular, NK cell and CD8+ T cell activation is critical for the targeting and lysis of tumour cells, including major histocompatibility complex (MHC) negative tumours.13,1⁵ These notoriously difficult targets lack peptide fragments that T cells recognize as pathogenic, enabling them to hide from the immune system.1⁶ Furthermore, iNKT cells can reprogram immunosuppressive tumor-associated macrophages to become inflammatory macrophages, reducing immunosuppression.1⁵,1⁷ As a result of iNKT cells’ wide range of functions, they have been coined the “Swiss Army knife” of the immune system.1⁴
However, other cells in the TME can antagonize the antitumour response of iNKT cells. MDSCs secrete transforming growth factor beta (TGF-β), a potent immunosuppressive cytokine that promotes tumour growth.1⁵ MDSCs also induce anergy in NK and T cells, increasing the rate of metastasis.1⁵ Additionally, type II NKT cells, which lack the semi-invariant TCR, suppress tumour immunosurveillance.13 An immunoregulatory axis exists between iNKT and type II NKT cells: these cells operate antagonistically and downregulate each other, which can explain why cancer therapies which neglect to target type II NKT cells have been largely ineffective.13,1⁵
APPLICATIONS OF α-GALCER IN INKT PATHWAYS
α-GalCer is well-known as an exogenous glycolipid mediator for potent iNKT response.6,13 α-GalCer(Bf), an α-GalCer compound, is produced at various sites within humans,
CRITICAL REVIEW meducator | april 2023 15
including by the gut bacteria Bacteroides fragilis and Bacteroides vulgatus.18-20 Figure 1 summarizes the effects of α-GalCer as an exogenous iNKT cell ligand.
α-GalCer can serve as a “jump start” molecule for iNKT antitumour immune responses.21 It interacts with iNKT cells primarily through APCs, particularly DCs.1⁸ Clinical trials involving free α-GalCer or α-GalCer-pulsed DC (DCs with α-GalCer loaded in their CD1d proteins) administration in humans have shown that detection of the α-GalCer antigen by iNKT cells rapidly stimulates their proliferation and production of granzymes (Gzms) A and B.13,1⁵,1⁸ In this pathway, Gzms A and B promote lysis and apoptosis of CD1d-expressing tumours.1⁵,1⁸ Furthermore, α-GalCer-pulsed DC reduces the inhibitory nature of MDSCs.1⁵ DC-mediated T and B cell activation are well-established strategies for effective immune memory development, protecting against tumor relapses.1⁵ Although there is no dose-limiting toxicity level, free administration of α-GalCer induces anergy in iNKT cells, greatly decreasing the ability of restimulation for up to two months.13,1⁵,22
Α CRITICAL ANALYSES OF α-GALCER STUDIES

α-GalCer studies related to various cancers have been conducted at in vitro and in vivo levels, including human clinical trials. However, the complicated nature of immune pathways in humans has yielded largely inconclusive results; murine studies are often more insightful due to higher levels of experimental control.
In 2022, Li et al. conducted an in vitro and in vivo study
on melanoma and lung cancer tumour-bearing humanized


In the in vitro approach, α-GalCer administration enhanced cytotoxic function and Gzm B levels in PBMC-iNKT cells, confirming α-GalCer’s antitumour capabilities in cell lines.⁶ In the in vivo approach, transferring human iNKT cells with a single dose of localized α-GalCer resulted in rapid iNKT cell recruitment into solid tumours within 24 hours, causing reduced tumour growth.⁶ The treatment group with α-GalCer had higher iNKT cell counts and enhanced cytokine production compared to the PBMC-iNKT and PBMC-T cell negative controls and the phosphate-buffered saline (PBS) placebo control.⁶ However, the sample sizes for each test group ranged between 3 and 4 mice, resulting in decreased confidence in the results.⁶
These results correspond with another murine study conducted by Haghighi et al., which concluded that the combination of α-GalCer and Lactobacillus casei, a probiotic species of bacteria, was highly effective against cervical cancer.23 L. casei is a safe probiotic that exhibits anti-cancer properties and may modulate immune responses against solid tumours in humans.23 The test group received heated cytotoxic type 1 T cells (Tc1s) with α-GalCer and L. casei and was compared against a PBS placebo control, a Gardasil human papillomavirus (HPV) vaccine positive control, and various combination treatment groups, allowing for high confidence in results.23 The treatment group receiving both α-GalCer and L. casei with heated Tc1s experienced the greatest increase in pro-inflammatory cytokine stimulation and nitric oxide levels, activating both innate and adaptive immune branches.23 Further testing should seek to establish the method by which α-GalCer and L. casei interact to better understand this combination treatment and investigate additional anticancer probiotics.
α-GalCer is not limited to murine environments. In 2020, Toyoda et al. examined the effects of α-GalCer on an in vivo, phase II human trial of non-small cell lung cancer cases.2⁴ 34 patients were given four doses of α-GalCer-pulsed APCs.2⁴ Overall, the median survival increased to 21.7 months from the expected 17 months for untreated patients.2⁴ In addition, only nine patients reported minor side effects, indicating that α-GalCer is a relatively safe treatment for tumour suppression.2⁴ Despite these positive results, the single-arm design does not provide sufficient confidence in this treatment compared to traditional protocols.2⁴ Furthermore, the open label design and lack of a placebo group could result in biases in physician and patient reporting of results.2⁵
In contrast to these findings, a 2019 study by Biagioli et al. found that α-GalCer induced acute hepatitis in mice, which reduces the viability of α-GalCer as a treatment.2⁶ However, this study also demonstrated that selective agonists of GPBAR1, a G proteincoupled receptor activated by bile acid, were able to diminish liver damage.2⁶ Since GPBAR1 regulates liver iNKT activities, there may be additional opportunities to mitigate the negative effects of α-GalCer elsewhere in the body.2⁶ Furthermore, the concentration of α-GalCer used to induce acute hepatitis was 0.01g/L2⁶, whereas the concentration used in Toyoda et al.’s human trial was 0.0002g/L.2⁴
Overall, α-GalCer shows strong potential as a cancer treatment following in vitro, murine, and human models. However, studies should seek to compare α-GalCer-based treatment against traditional approaches in a double-arm design.2⁷ Appropriate negative control and test groups should be selected to illustrate the relative efficacy of proposed treatments.
NEXT STEPS
Current studies focus on the short-term effects of single doses of α-GalCer, which neglects the long-term impact of anergy. Since cancer patients generally require treatments for up to six months, anergy would result in significantly decreased effectiveness of immune and cellular responses to α-GalCer.28 Since free α-GalCer induces anergy in iNKT cells, the efficacy of subsequent doses is diminished.17 To combat this, Fujii et al. found that α-GalCer-pulsed DCs reduced tumor growth and metastasis with minimal induction of anergy.15,29 α-GalCer analogs are another
CRITICAL REVIEW meducator | april 2023 16
Figure 1: α-GalCer presentation by APCs with CD1d proteins activate iNKT cells, inducing a cascade of downstream cell behavior, resulting in increased immunosurveillance and cancer protection. iNKT cells also upregulate MDSCs, which contribute to NK and CD8+ T cell anergy. iNKT and type II NKT cells are antagonistic to each other.
alternative avenue of study; analogs such as β-mannosylceramide (β-ManCer) induce almost no long-term anergy of iNKT cells.30 However, this glycolipid uses a nitric oxide synthase (NOS)dependent mechanism, raising the need for further research.13 Because of α-GalCer’s broad range of interactions, there is no standard delivery method. For example, the adoptive transfer of iNKT cells may complement α-GalCer treatments since cancer patients often have decreased function and number of iNKT cells.15,31 Alternatively, while α-GalCer-pulsed DCs are a highly effective delivery method, it is difficult to obtain sufficient quantities of DCs. While this lack of a standard delivery method has opened up various intriguing research pathways to pursue, it clouds objective assessments and comparisons of different trials. Some notable areas for investigation to increase α-GalCer effectiveness include alternative delivery methods, combination treatments, and iNKT cell production. Delivery vectors such as nanoparticles, artificial APCs, exosomes, and liposomes should be explored to address the low efficacy of free α-GalCer administration.15,32,33Since chemotherapy continues to be a major component of cancer treatment, studies need to consider the interactions between them. Early studies of head and neck carcinoma suggest that this chemotherapyα-GalCer combination treatment results in increased iNKT cell and IL-12 production at the cost of increased adverse events.34 Since α-GalCer modulates iNKT activity, the low quantity of endogenous iNKT cells in peripheral circulation presents a barrier to α-GalCer treatment efficacy in humans.6 Various pluripotent stem cellderived iNKT cell production methods should be researched.15
CONCLUSION
α-GalCer therapy is a promising treatment pathway for a variety of cancers. α-GalCer’s effects have been demonstrated in cell lines, murine models, and human clinical trials, increasing iNKT cell-mediated anti-tumour activity. However, additional research is required to further investigate improved α-GalCer delivery methods and strategies to increase patient iNKT cell counts. Within the broader scope of cancer treatment, α-GalCer treatment will likely be coupled with traditional chemotherapy; the potential adverse side effects of the co-administration of the two therapies should be investigated in the future.
1.
Cancer
Chakraborty S, Rahman T.



3. Gonzalez H, Hagerling C, Werb Z. Roles of the immune system in cancer: from tumor initiation to metastatic progression. Genes Dev. 2018;32(19–20):1267–84. Available from: doi:10.1101/gad.314617.118.
4. Tontonoz M. The immune system can fight cancer. So why doesn’t it? [Internet]. 2018 Dec 11. Available from: https://www.mskcc.org/news/immune-system-can-fight-cancer-so-why-doesn-t-it [cited 2022 Dec 12].
5. Haygreen E. NKT cells: Invariant [Internet]. Available from: https://www.immunology.org/public-information/ bitesized-immunology/cells/nkt-cells-invariant [cited 2022 Dec 12].

6. Li Y-R, Zhou Y, Wilson M, Kramer A, Hon R, Zhu Y, et al. Tumor-localized administration of α-GalCer to recruit invariant natural killer T Cells and enhance their antitumor activity against solid tumors. Int J Mol Sci. 2022;23(14):7547. Available from: doi:10.3390/ijms23147547.
7. Kain L, Webb B, Anderson BL, Deng S, Holt M, Costanzo A, et al. The Identification of the endogenous ligands of natural killer T cells reveals the presence of mammalian α-linked glycosylceramides. Immunity. 2014;41(4):543–54. Available from: doi:10.1016/j.immuni.2014.08.017.
8. Natori T, Morita M, Akimoto K, Koezuka Y. Agelasphins, novel antitumor and immunostimulatory cerebrosides from the marine sponge Agelas mauritianus. Tetrahedron. 1994;50(9):2771–84. Available from: doi:10.1016/ S0040-4020(01)86991-X.
9. Cheng-Sánchez I, Sarabia F. Chemistry and biology of bioactive glycolipids of marine origin. Mar Drugs. 2018;16(9):294. Available from: doi:10.3390/md16090294.
10. Crosby CM, Kronenberg M. Tissue-specific functions of invariant natural killer T cells. Nat Rev Immunol. 2018;18(9):559–74. Available from: doi:10.1038/s41577-018-0034-2.
11. Cortesi F, Delfanti G, Grilli A, Calcinotto A, Gorini F, Pucci F, et al. Bimodal CD40/Fas-dependent crosstalk between iNKT cells and tumor-associated macrophages impairs prostate cancer progression. Cell Rep. 2018;22(11):3006–20. Available from: doi:10.1016/j.celrep.2018.02.058.
12. Trinchieri G. Interleukin-12 and the regulation of innate resistance and adaptive immunity. Nat Rev Immunol. 2003;3(2):133–46. Available from: doi:10.1038/nri1001.
13. Terabe M, Berzofsky JA. Tissue-specific roles of NKT cells in tumor immunity. Front Immunol. 2018;9.
14. Matsuda JL, Mallevaey T, Scott-Browne J, Gapin L. CD1d-restricted iNKT cells, the ‘Swiss-Army knife’ of the immune system. Curr Opin Immunol. 2008;20(3):358–68. Available from: doi:10.1016/j.coi.2008.03.018.
15. Nelson A, Lukacs JD, Johnston B. The current landscape of NKT cell immunotherapy and the hills ahead. Cancers. 2021;13(20):5174. Available from: doi:10.3390/cancers13205174.
16. Charles A Janeway J, Travers P, Walport M, Shlomchik MJ. The major histocompatibility complex and its functions. Immunobiol Immune Syst Health Dis 5th Ed. 2001;
17. Anderson NR, Minutolo NG, Gill S, Klichinsky M. Macrophage-based approaches for cancer immunotherapy. Cancer Res. 2021;81(5):1201–8. Available from: doi:10.1158/0008-5472.CAN-20-2990.
18. Ustjanzew A, Sencio V, Trottein F, Faber J, Sandhoff R, Paret C. Interaction between bacteria and the immune system for cancer immunotherapy: The α-GalCer alliance. Int J Mol Sci. 2022;23(11):5896. Available from: doi:10.3390/ijms23115896.
19. Kuwahara T, Yamashita A, Hirakawa H, Nakayama H, Toh H, Okada N, et al. Genomic analysis of Bacteroides fragilis reveals extensive DNA inversions regulating cell surface adaptation. Proc Natl Acad Sci U S A. 2004;101(41):14919–24. Available from: doi:10.1073/pnas.0404172101.
20. Elsaghir H, Reddivari AKR. Bacteroides fragilis. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2022. Available from: http://www.ncbi.nlm.nih.gov/books/NBK553032/ [cited 2022 Dec 12].
21. McEwen-Smith RM, Salio M, Cerundolo V. The regulatory role of invariant NKT cells in tumor immunity. Cancer Immunol Res. 2015;3(5):425–35. Available from: doi:10.1158/2326-6066.CIR-15-0062.
22. Huang J-R, Tsai Y-C, Chang Y-J, Wu J-C, Hung J-T, Lin K-H, et al. α-Galactosylceramide but not phenyl-glycolipids induced NKT cell anergy and IL-33–mediated myeloid-derived suppressor cell accumulation via upregulation of egr2/3. J Immunol. 2014;192(4):1972–81. Available from: doi:10.4049/jimmunol.1302623.
23. Haghighi D, Yazdani S, Farzanehpour M, Esmaeili Gouvarchinghaleh H. Combined extract of heated TC1, a heatkilled preparation of Lactobacillus casei and alpha-galactosyl ceramide in a mouse model of cervical cancer. Infect Agent Cancer. 2022;17:51. Available from: doi:10.1186/s13027-022-00464-w.
24. Toyoda T, Kamata T, Tanaka K, Ihara F, Takami M, Suzuki H, et al. Phase II study of α-Galactosylceramide-pulsed antigen-presenting cells in patients with advanced or recurrent non-small cell lung cancer. J Immunother Cancer. 2020;8(1):e000316. Available from: doi:10.1136/jitc-2019-000316.
25. Roydhouse JK, Fiero MH, Kluetz PG. Investigating potential bias in patient-reported outcomes in open-label cancer trials. JAMA Oncol. 2019;5(4):457–8. Available from: doi:10.1001/jamaoncol.2018.6205.
26. Biagioli M, Carino A, Fiorucci C, Marchianò S, Di Giorgio C, Roselli R, et al. GPBAR1 functions as gatekeeper for liver NKT Cells and provides counterregulatory signals in mouse models of immune-mediated hepatitis. Cell Mol Gastroenterol Hepatol. 2019;8(3):447–73. Available from: doi:10.1016/j.jcmgh.2019.06.003.
27. Shi H, Zhang T, Yin G. START: single to double arm transition design for phase II clinical trials. Pharm Stat. 2020;19(4):454–67. Available from: doi:10.1002/pst.2005.
28. Cancer Research UK. Your chemotherapy plan [Internet]. 2020 Jul 2. Available from: https://www. cancerresearchuk.org/about-cancer/cancer-in-general/treatment/chemotherapy/planning/yourchemotherapy-plan [cited 2022 Dec 12].
29. Fujii S, Shimizu K, Smith C, Bonifaz L, Steinman RM. Activation of natural killer T Cells by α-Galactosylceramide rapidly induces the full maturation of dendritic cells in vivo and thereby acts as an adjuvant for combined CD4 and CD8 T cell immunity to a coadministered protein. J Exp Med. 2003;198(2):267–79. Available from: doi:10.1084/jem.20030324.
30. O’Konek JJ, Kato S, Takao S, Izhak L, Xia Z, Illarionov P, et al. -Mannosylceramide activates type I natural killer T cells to induce tumor immunity without inducing long-term functional anergy. Clin Cancer Res. 2013;19(16):4404–11. Available from: doi:10.1158/1078-0432.CCR-12-2169.
31. Molling JW, Kölgen W, van der Vliet HJJ, Boomsma MF, Kruizenga H, Smorenburg CH, et al. Peripheral blood IFN- -secreting Vα24+V 11+ NKT cell numbers are decreased in cancer patients independent of tumor type or tumor load. Int J Cancer. 2005;116(1):87–93. Available from: doi:10.1002/ijc.20998.
32. East JE, Sun W, Webb TJ. Artificial antigen presenting cell (aapc) mediated activation and expansion of natural killer T cells. J Vis Exp JoVE. 2012;(70):4333. Available from: doi:10.3791/4333.
33. Gehrmann U, Hiltbrunner S, Georgoudaki A-M, Karlsson MC, Näslund TI, Gabrielsson S. Synergistic induction of adaptive antitumor immunity by codelivery of antigen with α-Galactosylceramide on exosomes. Cancer Res. 2013;73(13):3865–76. Available from: doi:10.1158/0008-5472.CAN-12-3918.
Carolina De Amat Herbozo is a PhD candidate in the Department of Immunology at the University of Toronto. She works in Dr. Thierry Mallevaey's lab where she studies the development and effector functions of iNKT cells, particularly in the context of cancer.
CRITICAL REVIEW meducator | april 2023 17
[Internet]. 2022 Feb 3.
from:
REVIEWED BY: CAROLINE DE AMAT HERBOZO Dec 12].
Available
https://www.who.int/news-room/fact-sheets/detail/cancer [cited 2022
2.
The difficulties in cancer treatment. ecancermedicalscience. 2012;6:ed16. Available from: doi:10.3332/ecancer.2012.ed16.
34. Kunii N, Horiguchi S, Motohashi S, Yamamoto H, Ueno N, Yamamoto S, et al. Combination therapy of in vitroexpanded natural killer T cells and α-Galactosylceramide-pulsed antigen-presenting cells in patients with recurrent head and neck carcinoma. Cancer Sci. 2009;100(6):1092–8. Available from: doi:10.1111/j.13497006.2009.01135.x.
OPINION

OPINION meducator | april 2023 18
MUSHROOMS
doi: 10.35493/medu.43.18
AUTHORS:
ZAHRA ALAM & BHAVANA SOMA
Bachelor of Science (Honours), Class of 2024, McMaster University
ARTIST:
HAMNA MALIK
Bachelor of Engineering and Biomedical Engineering, Class of 2025, McMaster University
ABSTRACT

Psilocybin is a naturally occurring compound present in numerous mushroom species characterised by its hallucinogenic and psychedelic effects. Although it has a negative reputation, psilocybin has demonstrated therapeutic potential for treating mental health disorders by allowing the brain to make new neural connections which help the neural pathways adapt and break out of certain cognitive patterns related to mental illness. In recent studies, psilocybin has shown antidepressant effects, significantly reducing depressive and anxious symptoms in affected individuals. After single or low dosage, mood disorder symptoms remained in remission for 6 to 12 months. In contrast, conventional antidepressants often require multiple doses over long treatment periods to achieve similar effects. Other findings have shown that therapeutic use of psilocybin helps combat substance abuse and addictive disorders and can be applied as a cessation tool. Despite years of controversy surrounding the benefits of psilocybin, recent scientific evidence supports psilocybin’s immense potential in helping those with mental health disorders like Major Depressive Disorder (MDD), Generalised Anxiety Disorder (GAD), Post Traumatic Stress Disorder (PTSD), Obsessive-Compulsive Disorder (OCD), and addiction disorders. With such promising results, psilocybin could be incorporated into clinical use and its therapeutic effects should continue being researched.
INTRODUCTION
Known for its hallucinogenic and psychedelic effects, psilocybin is a naturally occurring compound produced in over 180 species of mushrooms worldwide.1 The psychedelic effects of psilocybin are attributed to the similarity of its molecular structure to serotonin, which allows it to bind to the serotonin 2A receptor (5-HT2AR). 5-HT2AR modulates various cognitive processes, including perception, learning, mood, and imagination, meaning that it is expressed widely throughout the brain. Thus, alterations in pathways involving 5-HT2AR can distort one’s perception of the environment, possibly leading to hallucinations, euphoria, and intense feelings of wonder.2 These effects are dose-dependent and influenced by the user’s expectations of the experience of using psilocybin. Additionally, long-term changes in sensory perception and thought after the experience are not uncommon.

Ongoing research shows that psilocybin has an effect on the brain’s Default Mode Network (DMN). This network allows
us to reflect on the past and plan for the future as it compiles and consolidates information in the background of everyday life. It has also been proposed that the DMN is responsible for the sense of self or individuality.3 Studies suggest that the 5-HT2AR receptors are involved in and influence connections in the DMN.4 Psilocybin may disable some of the connections in this network, which forces new connections to form within the brain, thereby allowing one’s sense of self to shift.3
Mushrooms containing psilocybin are hypothesised to have been used by humans for 5.3 million years.5 They have also been used in medicinal, spiritual, and ceremonial practices around the world for thousands of years.6 Today, however, the majority of psychedelic substances, including psilocybin, have been categorised as controlled and illegal with no recognised medical value.7 Before prohibitive laws ended psychedelic research programs in the 1970s, psychedelics showed initial therapeutic promise as a supplement to psychotherapy for mood disorders and
OPINION meducator | april 2023 19
the treatment of alcohol dependence. Human psychedelic research has been slowly, but steadily, reviving since the early 1990s due to growing recognition of its clinical potential.8 This has led to the subject of recent controlled clinical studies exploring psilocybin’s effects on the mind, and its therapeutic efficacy in aid of existing psychotherapeutic approaches.7 Despite years of controversy surrounding the drug, it has shown immense potential in treating various medical conditions, such as those involving mental health, and holds significant promise for continued investigation. programs in the 1970s, psychedelics showed initial therapeutic promise as a supplement to psychotherapy for mood disorders and the treatment of alcohol dependence Human psychedelic research has been slowly but steadily reviving since the early 1990s due to growing recognition of its clinical potential.8 This has led to the subject of recent controlled clinical studies exploring psilocybin’s effects on the mind, and its therapeutic efficacy in aid of existing psychotherapeutic approaches.7 Despite years of controversy surrounding the drug, it has shown immense potential in treating various medical conditions, such as those involving mental health, and holds significant promise for continued investigation.
USING PSILOCYBIN TO TREAT MOOD DISORDERS
Psilocybin was first reported to have antidepressant properties in a study carried out at Johns Hopkins University in 2016. In patients who developed anxiety disorders associated with their advanced-stage cancer diagnosis, controlled amounts of psilocybin significantly reduced anxiety and depressed mood.9 Additionally, Griffiths et al. demonstrated that 92% of the cancer patients who received a high dose of psilocybin showed a clinically significant decrease in depressive symptoms after the first session.9 Furthermore, there was a sustained symptom remission rate of 65% at the six-month follow-up assessment.9 By demonstrating an enhanced quality of life in these patients, the study provided a catalyst for new research aimed at replicating these findings. Psilocybin may also be effective for a larger demographic beyond cancer patients. A one-time high dose of psilocybin was shown to be associated with remission in mood disorders in patients with long-term depression at six and twelve months after treatment.10 The magnitude of the effect observed was approximately four times greater than what clinical trials have previously demonstrated for conventionally available antidepressants on the market that target the serotonergic system, similar to psilocybin.10 Given that there has been little advancement in mental health treatment over the last three decades, these findings were deemed to be remarkable by the media. This is because most other antidepressant treatments take weeks to work and require more doses that result in a high incidence of unwanted side effects.10 Further research into the therapeutic potential of psilocybin for mood disorders is, therefore, warranted.
PSILOCYBIN AS A TOOL FOR ADDRESSING SUBSTANCE USE DISORDERS

Another area in which psilocybin may have a therapeutic advantage is in managing substance use disorders (SUDs). An online survey conducted in 2020 by Garcia-Romeu et al. examined self-reported instances of psychedelic use followed by a cessation or reduction in use of other substances, including cannabis, opioids, or stimulants. Results indicated that before using psychedelics, 29% of which was psilocybin, 96% of subjects met the criteria for a SUD, whereas only 27% did after use. Greater psychedelic doses were linked to lower drug consumption.
While this survey can only serve to establish a correlation between psychedelics and SUDs, the findings make a case for further clinical research on treatment with psychedelic aids.11

OPINION meducator | april 2023 20
HOW PSILOCYBIN REWIRES THE BRAIN: NEUROPLASTICITY
While psilocybin has been shown to be a promising tool in addressing mental health-related conditions, serving
CONCLUSION

Psilocybin has shown immense potential in helping those with mental health disorders, like MDD, GAD, PTSD, OCD, and addiction disorders. Many other drugs may display similar therapeutic promise if used under controlled conditions; one example is the street drug “ketamine”.17 Recent studies have exhibited interest in using specific doses of ketamine to treat MDD. Although these substances have gained notoriety in the public, they hold potential in modern medical treatment. More clinical trials are needed to further investigate the mechanisms and long-term effects of psilocybin; thus, it should be safely integrated into phase 2 and 3 trials.
REVIEWED BY: DR. KATJA LINHER-MELVILLE (PHD)
A past research scientist in pathology and molecular medicine, Dr. Katja Linher-Melville is currently a sessional instructor in the BHSc program at McMaster University (she teaches Biochem Inquiry, Cell Bio Inquiry, Symptomatology, and Research Skills & Application). Dr. Linher-Melville conducted preclinical research into cancer-induced and neuropathic pain.
PM, Burmester D, Dyssegaard A, Stenbæk DS, Kristiansen S, et al. Psychedelic effects of psilocybin correlate with serotonin 2A receptor occupancy and plasma psilocin levels. Neuropsychopharmacol. 2019;44(7):1328-44. Available from: doi:10.1038/ s41386-019-0324-9.
Gattuso JJ, Perkins D, Ruffell S, Lawrence AJ, Hoyer D, Jacobson LH, et al. Default mode network modulation by psychedelics: A systematic review. Int J Neuropsychopharmacol. 2022. Available from: doi:10.1093/ijnp/pyac074.
Miller MW, Sperbeck E, Robinson ME, Sadeh N, Wolf EJ, Hayes JP, et al. 5-HT2A gene variants moderate the association between PTSD and reduced default mode network connectivity. Front. in Neurosci. 2016;10. Available from: 10.3389/fnins.2016.00299.
Rodríguez Arce JM, Winkelman MJ. Psychedelics, sociality, and human evolution. Front Psychol. 2021;12:729425. Available from: doi:10.3389/fpsyg.2021.729425.
Lowe H, Toyang N, Steele B, Valentine H, Grant J, Ali A, et al. The therapeutic potential of psilocybin. Molecules. 2021;26(10):2948. Available from: doi:10.3390/ molecules26102948.
Tupper KW, Wood E, Yensen R, Johnson MW. Psychedelic medicine: A re-emerging therapeutic paradigm. CMAJ. 2015;187(14):1054-9. Available from: doi:10.1503/cmaj.141124. Carhart-Harris RL, Goodwin GM. The therapeutic potential of psychedelic drugs: Past, present, and future. Neuropsychopharmacol. 2017;42(11):2105–13. Available from: doi:10.1038/npp.2017.84.
Griffiths RR, Johnson MW, Carducci MA, Umbricht A, Richards WA, Richards BD, et al. Psilocybin produces substantial and sustained decreases in depression and anxiety in patients with life-threatening cancer: A randomized double-blind trial. J Psychopharmacol. 2016;30(12):1181-97. Available from: doi:10.1177/0269881116675513.
Gukasyan N, Davis AK, Barrett FS, Cosimano MP, Sepeda ND, Johnson MW, et al. Efficacy and safety of psilocybin-assisted treatment for major depressive disorder: Prospective 12-month follow-up. J Psychopharmacol. 2022;36(2):151-8. Available from: doi:10.1177/02698811211073759.
Garcia-Romeu A, Davis AK, Erowid E, Erowid F, Griffiths RR, Johnson MW. Persisting reductions in cannabis, opioid, and stimulant misuse after naturalistic psychedelic use: An online survey. Front Psych. 2020;10:955. Available from: doi:10.3389/fpsyt.2019.00955.
Jones G, Ricard JA, Lipson J, Nock MK. Associations between classic psychedelics and opioid use disorder in a nationally-representative U.S. adult sample. Sci Rep. 2022;12(1):4099. Available from: doi:10.1038/s41598-022-08085-4.
Johnson MW, Garcia-Romeu A, Griffiths RR. Long-term follow-up of psilocybin-facilitated smoking cessation. Am J Drug Alcohol Abuse. 2017;43(1):55-60. Available from: doi:10.31 09/00952990.2016.1170135.
Bogenschutz MP, Forcehimes AA, Pommy JA, Wilcox CE, Barbosa PCR, Strassman RJ. Psilocybinassisted treatment for alcohol dependence: A proof-of-concept study. J Psychopharmacol. 2015;29(3):289-99. Available from: doi:10.1177/0269881114565144.
Mateos-Aparicio P, Rodríguez-Moreno A. The impact of studying brain plasticity. Front Cell Neurosci. 2019;13:66. Available from: doi:10.3389/fncel.2019.00066.
Catlow BJ, Song S, Paredes DA, Kirstein CL, Sanchez-Ramos J. Effects of psilocybin on hippocampal neurogenesis and extinction of trace fear conditioning. Exp Brain Res. 2013;228(4):481-91. Available from: doi:10.1007/s00221-013-3579-0.
Shin C, Kim Y-K. Ketamine in major depressive disorder: Mechanisms and future perspectives. Psychiatry Investig. 2020;17(3):181–92. Available from: doi:10.30773/pi.2019.0236.
Metzner R, Darling D. Sacred mushroom of visions: Teonanácatl: A sourcebook on the psilocybin mushroom. Rochester (USA): Park Street Press; 2006. Madsen MK, Fisher
OPINION meducator | april 2023 21
CRITICAL REVIEW:
PERINATAL MENTAL HEALTH IN HAMILTON AND MONTREAL

ARTISTS: ELAINE WANG 1 & ARIM YOO 2
1Bachelors of Health Sciences (Honours), Class of 2026, McMaster University
2Bachelors of Health Sciences (Honours), Class of 2024, McMaster University
CRITICAL REVIEW 22
meducator | april 2023
doi: 10.35493/medu.43.22
SHANZEY

1 Bachelors of Health Sciences (Honours), Class of 2024, McMaster University
2 Bachelors of Health Sciences (Honours), Class of 2025, McMaster University
3 Department of Physiology, Class of 2025, McGill University
4 Department of Biology, Class of 2023, McGill University
5 Department of Pharmacology, Class of 2025, McGill University
INTRODUCTION
Mental health concerns experienced by individuals during or up to one year after pregnancy fall under the umbrella of perinatal mental health. Estimates suggest that one in five people will experience a perinatal mental illness at some point during their pregnancy or up to one year postpartum.1 Racialized individuals with low socioeconomic status are at an increased risk to perinatal mental health.2,3 Perinatal mental illness is becoming an incredibly relevant topic in the sphere of public health and policy. Recently, the Canadian Task Force on Preventive Health Care released a recommendation against screening individuals for depression during pregnancy and the postpartum period (up to 1 year after childbirth), stating that there is low certainty of evidence for such screening measures.4 This received backlash, with groups like the Canadian Perinatal Mental Health Collaborative (CPMHC) speaking out.5 Prime Minister Justin Trudeau and the Minister of Mental Health and Addictions aim to “ensure timely access to perinatal mental health services”, as identified in a recent mandate letter.6 Given its current salience, this piece seeks to explore perinatal mental health programs in Ontario and Quebec, critically analyze their effectiveness, and suggest future areas of improvement.
IMPORTANCE OF INTERVENTIONS FOR PERINATAL MENTAL ILLNESS
A growing body of research indicates a link between perinatal mental health and child health, both psychologically and biologically. Perinatal depression in pregnancy has been shown to disrupt state-regulation, sleep, autonomic stability, and neurobehavioral maturity of the newborn. Studies have also reported that the child’s motor skills may also be affected later in life, depending on the status of maternal perinatal mental health. Maternal distress may also predict behavioral problems in the first ten years of life. All of the aforementioned changes may be explained by functional and structural alterations of the brain that take place in offspring that are prenatally exposed to maternal distress. According to animal studies, this includes changes in neuronal and synaptic development in the limbic system, epigenetic changes, programming of large-scale neuronal networks, and more. Studies in humans support these findings, demonstrating that prenatal exposure to maternal anxiety or depression is associated with many aspects of child brain function, such as impulsivity, attention, and endogenous cognitive control. There are also links between offspring autonomic nervous system function and perinatal exposure to maternal mental illness. Some studies suggest that the maternal perinatal mental health affects the fetus’ immune system, gut microbiome, and increased risk of mortality
and hospitalization during the first year of life. These associations clearly outline the possible adverse effects of perinatal mental illness, suggesting the need for proper interventions against it.7,8,9
SCIENTIFIC BACKGROUND
Postpartum disorders are classified into four main categories: postpartum blues (PBs), postpartum depression (PPDs), postpartum psychosis (PP), postpartum post-traumatic stress disorder (PTSD), and postpartum anxiety (PA). Perinatal mental health is crucial because it not only affects the mother's well-being but could also impact the health and development of the baby. Much of the research focuses on epigenetic modifications such as DNA methylation, though the specific effects remain unclear.23 One study did find that maternal mental health was a predictor of childrens’ epigenetic age acceleration.24 As well, researchers have investigated maternal mental health in the emotional and behavioral development of the fetus, finding a correlation between maternal anxiety and anomalies in neurodevelopment, cognitive function, structural brain connectivity, and changes in the HPA-axis.25 Other studies aim to understand the dynamic changes of maternal anxiety throughout pregnancy and two years postpartum, as well correlations to increased anxiety with maternal early adverse life experience.26 Maternal anxiety and depression have also been examined for their roles in hypertensive disorders of pregnancy. Anxiety was linked to preterm birth and low percentile for gestational age and sex, while depression was only linked with preterm birth.27 Other studies disagree on the contribution of maternal anxiety to hypertensive disorders, but suggest a novel link between maternal anxiety and the development of the maternalfetal-placental vascular unit.28 Although disagreement remains surrounding the specific effects of perinatal mental health on the fetus, researchers agree further data and research into the field is required and that supporting maternal mental health is essential.
HAMILTON PROGRAMS
To examine Hamilton’s currently offered support programs, holistically understanding the state of perinatal support services in the province of Ontario is imperative. Based on a 2021 report by the CPMHC, both Ontario and Quebec provide screening guidelines for individuals suffering from perinatal mood and anxiety disorders (PMADs). However, only Ontario has screening recommended on antenatal and perinatal records, specifically in the second and third trimesters and once more at six weeks postpartum. Nevertheless, a 2016 provincial evidence brief described specific interventions to address perinatal mental health in a public health context that Hamilton equally applies. In Hamilton, three principle methods are observed: online perinatal modules, group therapy or support groups, and 1-on1 sessions. However, there are various challenges associated with each option. Patients reported concerns with privacy and self-consciousness among support groups, along with overall skepticism towards the intervention. Furthermore, mixed results on long-term benefits of both in-person support groups and pre-recorded educational modules have been previously reported, particularly for the latter. Support groups have been shown to improve personal adjustment and perceived selfefficacy, although due to limits in consistency, they may require coupling with additional techniques to provide true benefits. Barriers to access, including but not limited to personal preference,
CRITICAL REVIEW meducator | april 2023 23
ALI 1, SURAJ BANSAL 2, INES DURANT 3, SOFIA REYNOSO 4, TIFFANY SPECTOR 5, JEFFREY SUN 1 & YIMING ZHANG 1
medication concerns, fear of judgment, and timeliness of provided interventions have all been reported throughout the province. Systemic limitations remain rooted in said concerns, and obstacles for those at social and economic disadvantages have been consistently reported. Concerning where inequalities lie, social factors may be extrapolated with some skepticism from other provinces. A recent Manitoba study described a list of factors associated with inadequate perinatal care: northern or rural residence, young maternal age, lone parent, parity >4, short inter-pregnancy interval, receiving income assistance, and living in a low-income neighborhood. Medical conditions such as multiple birth, hypertensive disorders, and diabetes were also associated with lower odds of inadequate perinatal care. In other words, the social determinants still act as strong deterrents for mental healthcare, impairing access and willingness to seek out support for mothers requiring said services. The city of Hamilton, while governed by the Ontario healthcare system, presents unique challenges due to its demographics. As the third least affordable city in North America, Hamilton possesses a growing homeless population, including young, pregnant individuals facing the additional stress of surviving on the streets. Although the prevalence of maternal mental health in Hamilton is yet to be studied, there is reason to believe that the stringent living conditions put patients at a higher risk than the provincial standard. Despite these concerns, Nussey notes in her interviews with Hamilton care providers that most physicians are unaware of mental health services to refer their patients towards. The inaccessibility of mental health, therefore, results from both structural factors and a lack of provider knowledge outside the medical context. Ultimately, these issues underscore the need for common knowledge to customize patient care.
MONTREAL PROGRAMS

In Montreal, hospitals and independent clinics provide mental health services for pregnant women, similar to Hamilton. These include, but are not limited to, La Maison Bleue, Mama Joia, West Island Women’s Centre, and more. The services vary from individual/couples therapy to support groups. The Quebec government also provides a general guide to pregnancy, childbirth, and parenthood for prospective parents known as From Tiny Tot to Toddler. Although these can still be effective, some pregnant women may require more tailored care to address all of their concerns. The Jewish General Hospital (JGH), for example, provides perinatal mental health services during pregnancy and six months postpartum. These services are tailored towards mothers who have previously sought psychiatric help and have diagnosed psychiatric disorders. However, the services are primarily reserved for mothers already followed by an OB/GYN or family doctor at the JGH. In addition to the services offered by the JGH, there is a division at the hospital dedicated to conducting research on perinatal mental health known as The CIHR Team in Perinatal Mental Health. Alongside these programs is Toi, Moi, et Bébé, a program developed by CHU Sainte-Justine, Université de Montréal, and the Observatoire pour l'éducation et la santé des enfants. This online program, akin to online modules developed in Hamilton, consists of 10 modules based on cognitive-behavioral therapy provided to pregnant women. In addition to the online platform, participants can receive phone calls by coaches throughout the program.
perinatal mental health care, including cultural differences, migrant-related stressors, and accessibility/quality of care. Another population that could benefit from tailored care is the indigenous community. A 2020 meta-analysis indicated that indigenous women are at a higher risk of developing perinatal mental health conditions. The perinatal period is crucial for providing appropriate support to Indigenous mothers, especially in response to a biomedical model based on non-Indigenous perspectives and needs. In 2021, a Quebec group, the Val d’Or Native Friendship Centre, started an initiative known as Abinodjic to restructure perinatal and perinatal care for pregnant women in their center. In the program, they used a holistic model of perinatal care to incorporate cultural knowledge, healthy lifestyles, parental experiences, and support networks into perinatal care. By incorporating an “ecosystemic approach, social innovation, and cultural safety,” this initiative provided a safe space for Indigenous parents to discuss their concerns with a larger community entrenched in “lived realities”.1 The success of the program could warrant expansion into other communities, such as those based in the Hamilton area. Alongside these successful programs, researchers based in Montreal recently started a longitudinal cohort study known as

CRITICAL REVIEW meducator | april 2023 24
the Montreal Antenatal Well-Being Study to identify the many intersecting biological and psychosocial factors behind perinatal mental health. The project has already released preliminary results, indicating depression and anxiety as relatively frequent conditions during pregnancy and a moderate increase in scores associated with anxiety and depression when the COVID-19 pandemic began. This study could hopefully contribute to improving services and guidelines surrounding perinatal mental health care, particularly in Montreal. As in Hamilton, there is certainly need for improvement in the access, quality, and diversity of mental healthcare options for pregnant individuals. The development of more tailored services informed by extensive research is needed in both Montreal and Hamilton.
CONCLUSION

As the CPMHC Time for Action National Report describes, Canada as a whole varies in prenatal and perinatal mental healthcare, with more than 95% of healthcare practitioners believing Canada offers insufficient perinatal mental health services. In both Hamilton and Montreal, structural barriers in access to care, such as weaknesses in group support offered in Hamilton or linguistic hurdles in Montreal’s online modules, prevent said healthcare services from reaching or treating their target patients optimally. Furthermore, many individualized approaches are barred by expansion due to limitations in healthcare providers: although previously-observed success has been reported with community-based care for mothers in both cities, more options are required to fully support mothers’ mental health during and after pregnancy. Canada’s overall perinatal support services require improvements in accessibility, diversity, and affordability, with the biological and psychological well-being of the mother and their offspring at the forefront of incentives.
REVIEWED BY: DR. CONNIE WILLIAMS (MD, PHD) & DR. JUDY HAGSHI (MD)
Dr. Connie Williams is a staff neonatologist at the McMaster Children’s Hospital, and a director of “Teaching Bioethics” of the MHSc program at the Joint Centre for Bioethics in Toronto. She currently holds a PhD in Health Policy and Bioethics at the University of Toronto, with numerous publications in perinatal and neonatal health. Her specialties include bioethics and social issues in healthcare systems. Dr. Judy Hagshi is a family doctor at the Herzl Family Practice Centre at the Jewish General Hospital (JGH) and a member of the Family Medicine Obstetrics team. She is additionally involved in medical residents at McGill University’s Department of Family Medicine.
1. The Ottawa Hospital Foundation. Perinatal Mental Health at The Ottawa Hospital [Internet]. Available from: https://ohfoundation.ca/perinatal-mental-health-at-the-ottawa-hospital/ [cited 2023 Mar 2].
2. Ban L, Gibson JE, West J, Fiaschi L, Oates MR, Tata LJ. Impact of socioeconomic deprivation on maternal perinatal mental illnesses presenting to UK general practice. Br J Gen Pract. 2012;62(603):e671-8. Available from: doi:10.3399/bjgp12X656801.
3. Segre LS, O’Hara MW, Losch ME. Race/ethnicity and perinatal depressed mood. J Reprod Infant Psychol. 2006;24(2):99-106. Available from: doi:10.1080/02646830600643908.
4. Lang E, Colquhoun H, LeBlanc JC, Riva JJ, Moore A, Traversy G, et al. Recommendation on instrument-based screening for depression during pregnancy and the postpartum period. CMAJ. 2022;194(28):E981-9. Available from: doi:10.1503/cmaj.220290.
5. Canadian Perinatal Mental Health Collaborative. Press Releases [Internet]. Available from: https:// cpmhc.ca/press-releases/ [cited 2023 Mar 2].
6. Government of Canada. Minister of Mental Health and Addictions and Associate Minister of Health Mandate Letter [Internet]. 2021 Dec 16. Available from: https://pm.gc.ca/en/mandateletters/2021/12/16/minister-mental-health-and-addictions-and-associate-minister-health [cited 2023 Mar 2].
7. Van den Bergh BRH, van den Heuvel MI, Lahti M, Braeken M, de Rooij SR, Entringer S, et al. Prenatal developmental origins of behavior and mental health: The influence of maternal stress in pregnancy. Neurosci Biobehav Rev. 2020;117:26-64. Available from: doi:10.1016/j.neubiorev.2017.07.003.
8. Howard LM, Khalifeh H. Perinatal mental health: A review of progress and challenges. World Psychiatry. 2020;19(3):313-27. Available from: doi:10.1002/wps.20769.
9. Aktar E, Qu J, Lawrence PJ, Tollenaar MS, Elzinga BM, Bogels SM. Fetal and infant outcomes in the offspring of parents with perinatal mental disorders: Earliest influences. Front Psychiatry. 2019;10:391. Available from: doi:10.3389/fpsyt.2019.00391.
10. O’Hara MW, Schlechte JA, Lewis DA, Wright EJ. Prospective study of postpartum blues. Biologic and psychosocial factors. Arch Gen Psychiatry. 1991;48:801–6. Available from: doi:10.1001/ archpsyc.1991.01810330025004.
11. Kendell RE, McGuire RJ, Connor Y, Cox JL. Mood changes in the first three weeks after childbirth. J Affect Disord. 1981;3:317–26. Available from: doi:10.1016/0165-0327(81)90001-x.
12. Henshaw C. Mood disturbance in the early puerperium: A review. Arch Womens Ment Health. 2003;6(Suppl 2):S33–42.Available from: doi:10.1007/s00737-003-0004-x
13. Kendell RE, Chalmers JC, Platz C. Epidemiology of puerperal psychoses. Br J Psychiatry. 1987;150:662–73. Available from: doi:10.1192/bjp.150.5.662.
14. A prospective study of postpartum psychoses in a high-risk group 2. Relationships to demographic and psychiatric history characteristics. Acta Psychiatr Scand. 1987;75:35–43. Available from: doi:10.1111/j.1600-0447.1987.tb02748.x.
15. Nonacs R, Cohen LS. Postpartum mood disorders: Diagnosis and treatment guidelines. J Clin Psychiatry. 1998;59(Suppl 2):34–40. Available from: https://pubmed.ncbi.nlm.nih. gov/9559758/.
16. Friedman SH, Cavney J, Resnick PJ. Child murder by parents and evolutionary psychology. Psychiatr Clin North Am. 2012;35:781–95. Available from: doi:10.1016/j.psc.2012.08.002.
17. Wisner KL, Peindl K, Hanusa BH. Symptomatology of affective and psychotic illnesses related to childbearing. J Affect Disord. 1994;30:77–87. Available from: doi:10.1016/01650327(94)90034-5.
18. Creedy DK, Shochet IM, Horsfall J. Childbirth and the development of acute trauma symptoms: Incidence and contributing factors. Birth. 2000;27:104–11. Available from: doi:10.1046/j.1523536x.2000.00104.x.
19. Menage J. Post-traumatic stress disorder in women who have undergone obstetric and/or gynaecological procedures. A consecutive series of 30 cases of PTSD. J Reprod Infant Psychol. 1993;11:221–8. Available from: doi:10.1080/02646839308403222.
20. Matthey S, Barnett B, Howie P, Kavanagh DJ. Diagnosing postpartum depression in mothers and fathers: Whatever happened to anxiety? J Affect Disord. 2003;74:139–47. Available from: doi:10.1016/s0165-0327(02)00012-5.
21. De Armond M. A type of postpartum anxiety reaction. Dis Nerv Syst. 1954;15:26–9.
22. Weightman H, Dalal BM, Brockington IF. Pathological fear of cot death. Psychopathology. 1998;31:246–9. Available from: doi:10.1159/000029046.
23. Cao-Lei L, van den Heuvel MI, Huse K, Platzer M, Elgbeili G, Braeken MAKA, et al. Epigenetic modifications associated with maternal anxiety during pregnancy and children's behavioral measures. Cells. 2021;10(9):2421. Available from: doi:10.3390/cells10092421.
24. McGill M, Pokhvisneva I, Clappison A, McEwen L, Beijers R, Tollenaar M, et al. Maternal prenatal anxiety and the fetal origins of epigenetic aging. Biological Psychiatry. 2022;91:303–12. Available from: doi:10.1016/j.biopsych.2021.07.025.
25. Cao-Lei L, Massart R, Suderman M, Machnes V, Elgbeili G, Laplante D, et al. DNA methylation signatures triggered by exposure to a natural disaster: Project Ice Storm. PLOS ONE. 2014;9(9):e107653. Available from: doi:10.1271/journal.pone.0107653.
26. Agrati D, Browne D, Jonas W, Meaney M, Atkinson L, Steiner M, et al. Maternal anxiety from pregnancy to 2 years postpartum: Transactional patterns of maternal early adversity and child temperament. Arch Womens Ment Health. 2015;18:693–705. Available from: doi:0.1007/ s00737-014-0491-y.
27. Raina J, Elgbeili G, Montreuil T, Nguyen TV, Beltempo M, Kusma D, et al. The effect of maternal hypertension and maternal mental illness on adverse neonatal outcomes: A mediation and moderation analysis in a U.S. cohort of 9 million pregnancies. Journal of Affective Disorders. 2023:326:11-17. Available from: doi:10.1016/j.jad.2023.01.052.
28. Bilbul M, Caccese C, Horsley K, Gauvreau A, Gavanski I, Montreuil T, et al. Maternal anxiety, depression and vascular function during pregnancy. Journal of Psychosomatic Research. 2022:154:110722. Available from: doi:10.1016/j.jpsychores.2022.110722.
CRITICAL REVIEW meducator | april 2023 25
ORGAN-ON-A-CHIP
BIOTECH BLUEPRINT

INTRODUCTION
Organ-on-a-chip (OoC) is a novel branch of biotechnology with the potential to improve the efficiency of biomedical research, particularly in drug discovery.1 In contrast to conventional methods like animal drug testing, plastic well plates, and simple assays before clinical trials, OoCs mimic the complex functions of human organs and tissues.2 Although this technology requires further refinement before it can effectively complement animal models, it shows great promise in accelerating the bench-to-bedside pipeline of drug discovery.1
MODE OF ACTION
OoC is an emerging interdisciplinary platform that will serve as an important tool in tissue analysis and drug screening.3,4 OoCs combine human-derived cells with microfluidic networks of perfused chambers that recreate physicochemical microenvironments to mimic the microarchitecture and function of specific tissues or organs.4-6 Physiological functions and mechanical stimuli of organs can be recreated and manipulated by altering various characteristics of OoCs, including their 3D microarchitecture or fluidic channels.6 Many design variations in 3D microarchitecture exist depending on which specific tissue interaction the OoC is designed to recreate.4 For example, multilayered microfluidic devices are compartmentalized by porous membranes that can recreate natural barrier structures, such as the blood-brain or intestinal mucosal barrier.4,7,8 Variables such as barrier integrity can then be measured with transendothelial/ epithelial electrical resistance to assess material transport between tissues in drug screening.4,7 Furthermore, the various gradients in biological organs are replicated by the flowing culture medium in microchannels via engineered pumps.9 These channels enable long-term culture of cells in the chip through the refreshment of a flowing culture medium, while also replicating the fluid shear stress that cells may experience in the body.4,9 Mechanical functions of organs, such as the breathing motion in the lungs or the peristaltic motion in the gut, may also be mimicked through the use of a micro-diaphragm or side vacuum channels to stretch porous membranes.4 Although OoC is a relatively new field of study, researchers have made rapid progress in terms of developing more specific mechanisms to model various types of organs and tissue samples in a chip microenvironment.6
doi: 10.35493/medu.43.26
AUTHORS:
ANNA McCRACKEN 1 & RAYMOND QU 2
1 Bachelor of Health Sciences (Honours), Class of 2025, McMaster University
2 Bachelor of Health Sciences (Honours), Class of 2026, McMaster University
ARTIST:
JULIO DIAZ 3 & ELAINE WANG 4
3 Bachelor of Health Sciences (Honours), Class of 2025, McMaster University
4 Bachelor of Health Sciences (Honours), Class of 2026, McMaster University
APPLICATIONS
OoC has been employed to simulate the cellular microenvironment of many organs and tissues of the human body, including the heart.1 Emerging research has used cardiomyocytes (CMs) implanted in a polydimethylsiloxane (PDMS) model to create a heart-on-a-chip (HoC), used to evaluate the efficacy of cardiac drugs and their toxicity to CMs.10,11,13,14 In a study conducted in 2016, HoC was used to measure CM response to both verapamil—a calcium channel blocker—and doxorubicin—an anticancer drug with known adverse effects on the heart, including arrhythmia and cardiomyopathy.14 In HoC, individual CMs aggregate and form a functional syncytium to perform tissue-level contraction—the status of this contraction upon drug administration was assessed by rate, magnitude, and pattern.14 This technology provides more information compared to the typical electrophysiological recording of individual CMs, which does not tell us how these cells work together as a tissue and are, therefore, less predictive
BIOTECH BLUEPRINT meducator | april 2023 26
as a technology.14 Thus, the ability to assess the mechanical contraction status of CMs using HoC will play a crucial role in cardiac drug development. Further, doxorubicin is known to be toxic to CMs. HoC proved to be an effective way to test for this cardiotoxicity, as it was able to detect arrhythmia after 60 minutes of doxorubicin administration.14 This is a promising application for HoC since cardiotoxicity is among the most common explanations for cardiac drug attrition and market withdrawal, and animal models have had a historically poor predictive value of this outcome.14-16 In addition to the use of CMs in HoC, Zhang et al. utilized endothelial cells to form networks emulating vasculature, and added neonatal rat CMs to gaps in the vascular network.11 This endothelialized myocardium HoC has promising implications for cardiovascular drug screening and pathophysiological modelling. HoC could be particularly useful in the testing of nanomedicine, as the vessel network in this model can provide an accurate assessment of the translocation of nanoparticles across tissues under in vivo shear flow.11,12 Therefore, the use of OoC technology to simulate conditions of the heart may prove to have vast benefits towards expediting the translation of cardiovascular therapeutics into the clinic.
Further, the application of OoC technology has shown promise in the research of various pathologies. For example, despite many medical advances in research, cystic fibrosis (CF) remains a health complication with no remedy and continues to limit the life expectancy of those affected.17-19 This autosomal genetic disease is characterized by mutations of the gene encoding the CF transmembrane conductance regulator (CFTR) protein, leading to the misregulation of chloride and bicarbonate ions of epithelial cells in areas such as the lungs.19,20 Translational research towards interventions for patients with CF is especially difficult due to the pathophysiological differences between human and animal models, with mice models exhibiting normal lung function compared to the symptoms of respiratory failure found in humans.21,21 In this sense, OoC is a solution to recreate human-relevant CFTR defects to be examined in vitro.20 This can be achieved through the use of induced pluripotent stem cells from patients with CF on lung-on-a-chip (LoC) models to explore personalized medicine approaches to CF treatment.20,23 One study at Harvard University showed that OoC models lined with CF patient cells recapitulate many features of CF symptoms including impaired airway mucociliary clearance, inflammation, and respiratory insufficiency.23 This study highlighted that genetic diseases could be modelled via OoCs using different cell linings, and that their accuracy was closely related to the clinical symptomatology of CF.23 CF LoCs featured higher levels of pro-inflammatory cytokines and a favourable bacteria growth environment as compared to normal LoCs.23,24 As the research behind OoC progresses, their ability to mimic various human diseases and compare their mechanisms to healthy organ chips in vitro will prove to be vital for the translational medicine of many specific diseases.6,23
LIMITATIONS AND FUTURE DIRECTIONS
Since animal models often provide inaccurate information regarding the efficacy and toxicity of drugs in humans, OoC provides an opportunity to remedy this research gap and vastly reduce the unnecessary costs of pre-clinical trials due to both drug attrition and animal models.16,25 While some key applications of OoC have been outlined in this review, many speculate that the future of this technology could extend across many interdisciplinary fields in medicine.2 Although some experts postulate the possibility of a human-on-a-chip, this is not the goal of OoC. Rather, the goal is to better understand inter-organ interactions and address the specific research questions at hand. However, there are still major developments that must occur to achieve this goal.1
For example, while PDMS has proven to be a valuable material
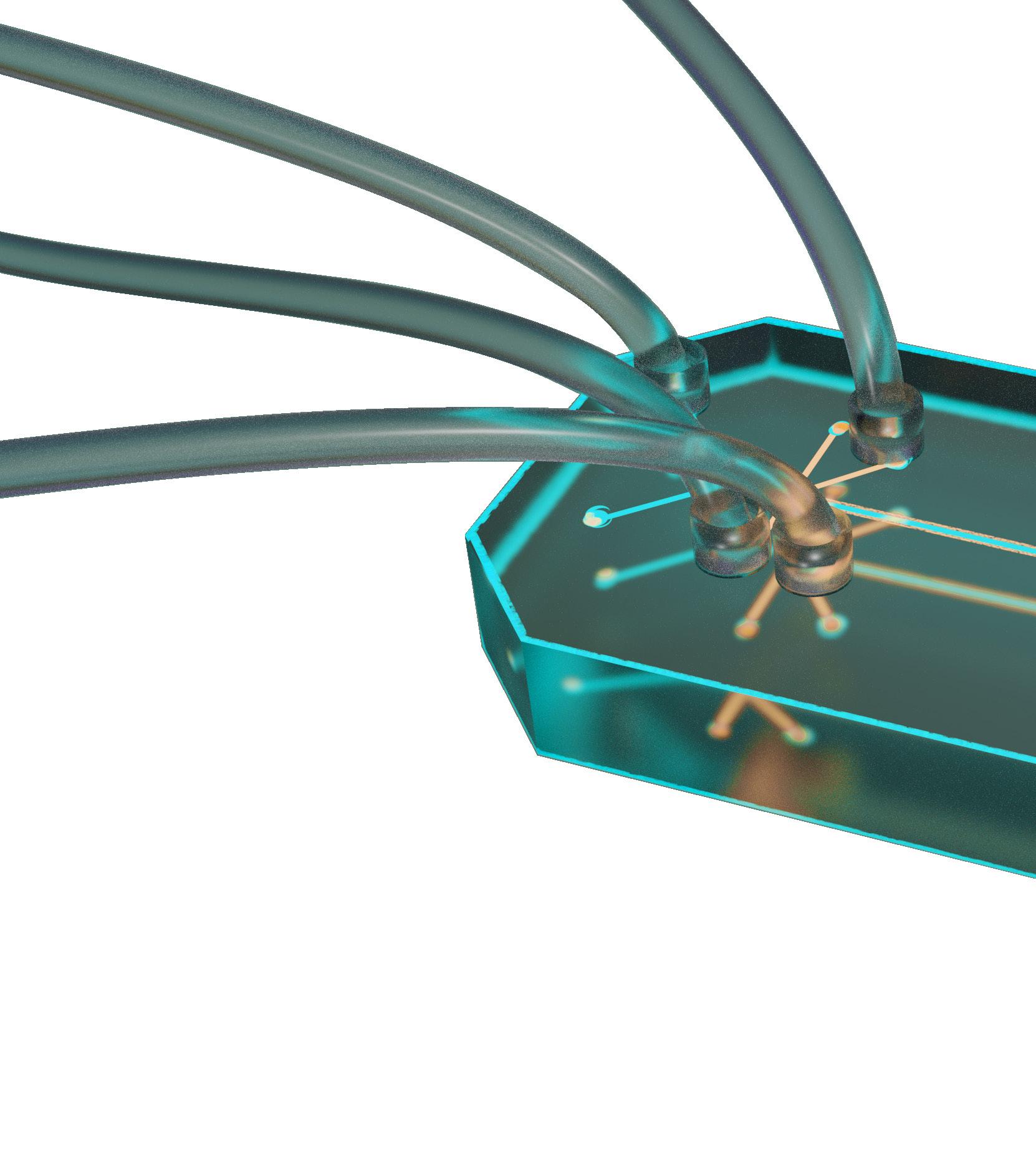
BIOTECH BLUEPRINT meducator | april 2023 27
for OoC, it has several limitations, including a decreased absorbance of small hydrophobic molecules.1 Furthermore, the small dimensions of this technology results in a larger surface area to volume ratio, thus misrepresenting the accurate amount of a drug being absorbed as compared to in vivo studies.26 Further research into alternative materials is necessary to construct more complex OoC models.2,27 For novel drugs, OoC allows for human-relevant drug experimentation even before clinical trials and may aid researchers in predicting drug response variations before the clinical stage. Moreover, when targeting rare disorders where obtaining sufficient participant numbers is difficult, OoC could provide a forum for pre-clinical trials using cells from patients all around the world.2 Thus, OoC has the potential to revolutionize the process of pre-clinical drug discovery.
1. Wu Q, Liu J, Wang X, Feng L, Wu J, Zhu X, et al. Organ-on-a-chip: Recent breakthroughs and future prospects. Biomed Eng OnLine. 2020;19(1):9. Available from: doi:10.1186/s12938-020-0752-0.
2. Ingber DE. Human organs-on-chips for disease modelling, drug development and personalized medicine. Nat Rev Genet. 2022;23(8):467–9. Available from: doi:10.1038/s41576-022-00466-9.
3. Ahadian S, Civitarese R, Bannerman D, Mohammadi MH, Lu R, Wang E, et al. Organ-on-a-chip platforms: A convergence of advanced materials, cells, and microscale technologies. Adv Healthc Mater. 2018;7(2):1700506. Available from: doi:10.1002/adhm.201700506.
4. Cho S, Lee S, Ahn SI. Design and engineering of organ-on-a-chip. Biomed Eng Lett. 2023;1-13. Available from: doi:10.1007/s13534-022-00258-4.
5. Park J, Kim KB, Lee J, Kim HC, Huh D. Organomimetic microsystems technologies. Biomed Eng Lett. 2012;2(2):88–94. Available from: doi:10.1007/s13534-012-0059-6.
6. Maschmeyer I, Kakava S. Organ-on-a-chip. Adv Biochem Eng Biotechnol. 2022;179:311-42. Available from: doi:10.1007/10_2020_135.
7. Ahn SI, Sei YJ, Park H, Kim J, Ryu Y, Choi JJ, et al. Microengineered human blood-brain barrier platform for understanding nanoparticle transport mechanisms. Nat Commun. 2020;11(1):175. Available from: doi:10.1038/ s41467-019-13896-7.
8. Shin W, Hinojosa CD, Ingber DE, Kim HJ. Human intestinal morphogenesis controlled by transepithelial morphogen gradient and flow-dependent physical cues in a microengineered gut-on-a-chip. iScience. 2019;15:391-406. Available from: doi:10.1016/j.isci.2019.04.037.
9. Shao J, Wu L, Wu J, Zheng Y, Zhao H, Jin, Q et al. Integrated microfluidic chip for endothelial cells culture and analysis exposed to a pulsatile and oscillatory shear stress. Lab Chip. 2009;9(21):3118-25. Available from: doi:10.1039/ b909312e.
10. Grosberg A, Nesmith AP, Goss JA, Brigham MD, McCain ML, Parker KK. Muscle on a chip: In vitro contractility assays for smooth and striated muscle. J Pharmacol Toxicol Methods. 2012;65(3):126–35. Available from: doi:10.1016/j.vascn.2012.04.001.
11. Zhang YS, Arneri A, Bersini S, Shin SR, Zhu K, Goli-Malekabadi Z, et al. Bioprinting 3D microfibrous scaffolds for engineering endothelialized myocardium and heart-on-a-chip. Biomaterials. 2016;110:45–9. Available from: doi:10.1016/j.biomaterials.2016.09.003.
12. Chen X, Zhang YS, Zhang X, Liu C. Organ-on-a-chip platforms for accelerating the evaluation of nanomedicine. Bioact Mater. 2020;6(4):1012–27. Available from: doi:10.1016/j.bioactmat.2020.09.022.
13. Zhang D, Shadrin I, Lam J, Xian HQ, Snodgrass R, Bursac N. Tissue-engineered cardiac patch for advanced functional maturation of human ESC-derived cardiomyocytes. Biomaterials. 2013;34(23):5813–20. Available from: doi:10.1016/j.biomaterials.2013.04.026.
14. Zhang X, Wang T, Wang P, Hu N. High-throughput assessment of drug cardiac safety using a high-speed impedance detection technology-based hearton-a-chip. Micromachines. 2016;7(7):122. Available from: doi:10.3390/ mi7070122.
15. Candarlioglu PL, Negro GD, Hughes D, Balkwill F, Harris K, Screen H, et al. Organ-on-a-chip: Current gaps and future directions. Biochem Soc Trans. 2022;50(2):665–73. Available from: doi:10.1042/BST20200661.
16. Tzatzalos E, Abilez OJ, Shukla P, Wu JC. Engineered heart tissues and induced pluripotent stem cells: Macro- and microstructures for disease modeling, drug screening, and translational studies. Adv Drug Deliv Rev. 2016;96:234–44. Available from: doi:10.1016/j.addr.2015.09.010.
17. Naehrig S, Chao CM, Naehrlich L. Cystic fibrosis. Dtsch Arztebl Int. 2017;114(33–4): 564–74. Available from: doi:10.3238/arztebl.2017.0564.
18. Standen J. Cystic fibrosis. InnovAiT. 2020;13(1):39–46. Available from: doi:10.1177/1755738019883322.
19. Bell SC, Mall MA, Gutierrez H, Macek M, Madge S, Davies JC, et al. The future of cystic fibrosis care: A global perspective. Lancet Respir Med. 2020;8(1):65–124. Available from: doi:10.1016/S2213-2600(19)30337-6.
20. Ramalho AS, Amato F, Gentzsch M. Patient-derived cell models for personalized medicine approaches in cystic fibrosis. J Cyst Fibros. 2023;22(1):S32–8. Available from: doi:10.1016/j.jcf.2022.11.007.
21. Silva IAL, Laselva O, Lopes-Pacheco M. Advances in preclinical in vitro models for the translation of precision medicine for cystic fibrosis. J Pers Med. 2022;12(8):1321. Available from: doi:10.3390/jpm12081321.
22. McCarron A, Donnelley M, Parsons D. Airway disease phenotypes in animal models of cystic fibrosis. Respir Res. 2018;19(1):54. Available from: doi:10.1186/s12931-018-0750-y.
23. Plebani R, Potla R, Soong M, Bai H, Izadifar Z, Jiang A, et al. Modeling pulmonary cystic fibrosis in a human lung airway-on-a-chip. J Cyst Fibros. 2022;21(4):606–15. Available from: doi:10.1016/j.jcf.2021.10.004.
24. Tabary O, Zahm JM, Hinnrasky J, Couetil JP, Cornillet P, Guenounou M, et al. Selective up-regulation of chemokine IL-8 expression in cystic fibrosis bronchial gland cells in vivo and in vitro. Am J Pathol. 1998;153(3):921–30. Available from: doi:10.1016/S0002-9440(10)65633-7.
25. Human organs-on-chips [Internet]. Wyss Institute. 2014. Available from: https://wyss.harvard.edu/technology/human-organs-on-chips/ [cited 2023 Feb 21].


26. Danku AE, Dulf EH, Braicu C, Jurj A, Berindan-Neagoe I. Organ-on-achip: A survey of technical results and problems. Front Bioeng Biotechnol. 2022;10:840674. Available from: doi:10.3389/fbioe.2022.840674.
27. Koyilot MC, Natarajan P, Hunt CR, Sivarajkumar S, Roy R, Joglekar S, et al. Breakthroughs and applications of organ-on-a-chip technology. Cells. 2022;11(11):1828. Available from: doi:10.3390/cells11111828.
REVIEWED BY: DR. BOYANG ZHANG (PHD)
Dr. Boyang Zhang (PhD) is an Assistant Professor in the department of Chemical Engineering at McMaster University. As the principal investigator of the BZhang lab, some of his research interests include tissue engineering, microfluidics, and organ-on-a-chip technology. In 2022, Dr. Zhang was awarded the Ontario Early Career Outstanding Research Award by the Government of Ontario.
EDITED BY: AISLING ZENG & AUDREY DONG
BIOTECH BLUEPRINT meducator | april 2023 28
STAFF
EDITORS-IN-CHIEF
Jeffrey Sun & Madeline Chan
EDITORIAL BOARD
Managing Editors
Shanzey Ali, Suraj Bansal & Yiming Zhang
Editors
Aisling Zeng
Alexander Xiang
Allison Fang
Anna McCracken
Audrey Dong
Dalraj Dhillon
Fan Ze Wang
GRAPHICS & DESIGN
Creative Directors
Arim Yoo & Natalie Chu
Graphic Designers
Aseel Abonowara
Ashley Low
Elaine Wang
Fan Ze (Alex) Wang
Hamna Malik
MEDUCOLLAB Directors
Florence Deng
Jacqueline Chen
Olivia Kim
Raymond Qu
Sepehr
Rida Tauqir
B. Khoshhal
Zahra Tauseef
VIDEO TEAM
Video Managers
David Klitovchenko, James Wang & Ken Yu
Video Producers
Brooke D’Mello
Charles Cai
Cindy Lin
Diane Kim
Kian Torabiardkani
Neil Lin
Nishaad Sheth
Serena Bansal
MEDUPROMO Director
Carolyn Wang & Leena Ghani
Medupromoters
Kaitlyn Eng
Kevin Yang
Mike Cho
Sadia Ahmad
Serena Wei
Tharani De Silva
MEDUCURRENT Directors
Julio Diaz
Katelyn Moore
Katie Lin
Mishal Hossain
Stephanie Aleluya
Eric Zhang & Gurleen Bhogal
ONLINE MANAGER
Aisling Zeng
Basant Dhillon
Eric An
Diane Kim & Olivia Chung
Larissa Rodrigues
Content Creators
Myra Agarwal
Najifah Tasnim
Nyla Syed
SENIOR ADVISOR

David Klitovchenko
ADDRESS
The Meducator, BHSc (Honours) Program

Michael G. DeGroote Centre for Learning and Discovery Room 3308
Faculty of Health Sciences
1280 Main Street West Hamilton, Ontario L8N 3Z5
CONTACT US THROUGH EMAIL the.meducator@gmail.com
VISIT OUR WEBSITE FOR PAST ISSUES www.themeducator.org
FOLLOW UPDATES ON FACEBOOK www.facebook.com/themeducator
FIND US ON YOUTUBE Meducator Official Channel
INTERESTED IN WRITING FOR OUR NEXT ISSUE? Visit www.meducator.org/ submit-now
WE WOULD LIKE TO GIVE A THANK YOU TO OUR SPONSORS FOR THEIR GENEROUS SUPPORT
Bachelor of Health Sciences (Honours) Program

McMaster Student Union

Bachelor of Health Sciences Society
Office of the President
CONTRIBUTORS meducator | april 2023 29





 Lycaenidae (Canada)
California Dogface (USA)
Lycaenidae (Canada)
California Dogface (USA)