medical link

Workplace Diversity: It’s More Than Meets the Eye
"Everyone has diversity. Yes, everyone. To fully optimise the current and future medical workforce, we must understand two important concepts, intersectionality and equity."


"Everyone has diversity. Yes, everyone. To fully optimise the current and future medical workforce, we must understand two important concepts, intersectionality and equity."
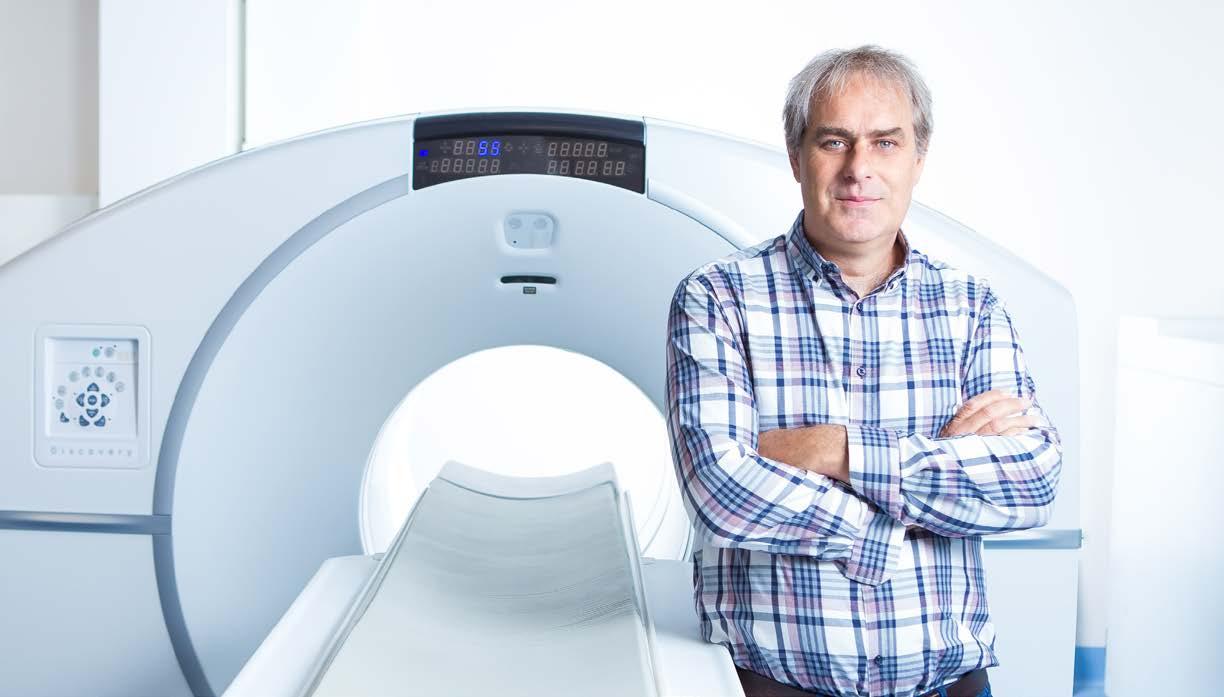
South Coast Radiology is excited to announce a 5-ring upgrade to our PET/CT scanner at John Flynn Hospital’s Nuclear Imaging and Therapy Center. This improvement will see an enhancement in clinical work via newly incorporated digital technology, the latest in diagnostic CT and advanced software, making it one of the most sensitive PET/CT scanners on the Gold Coast.
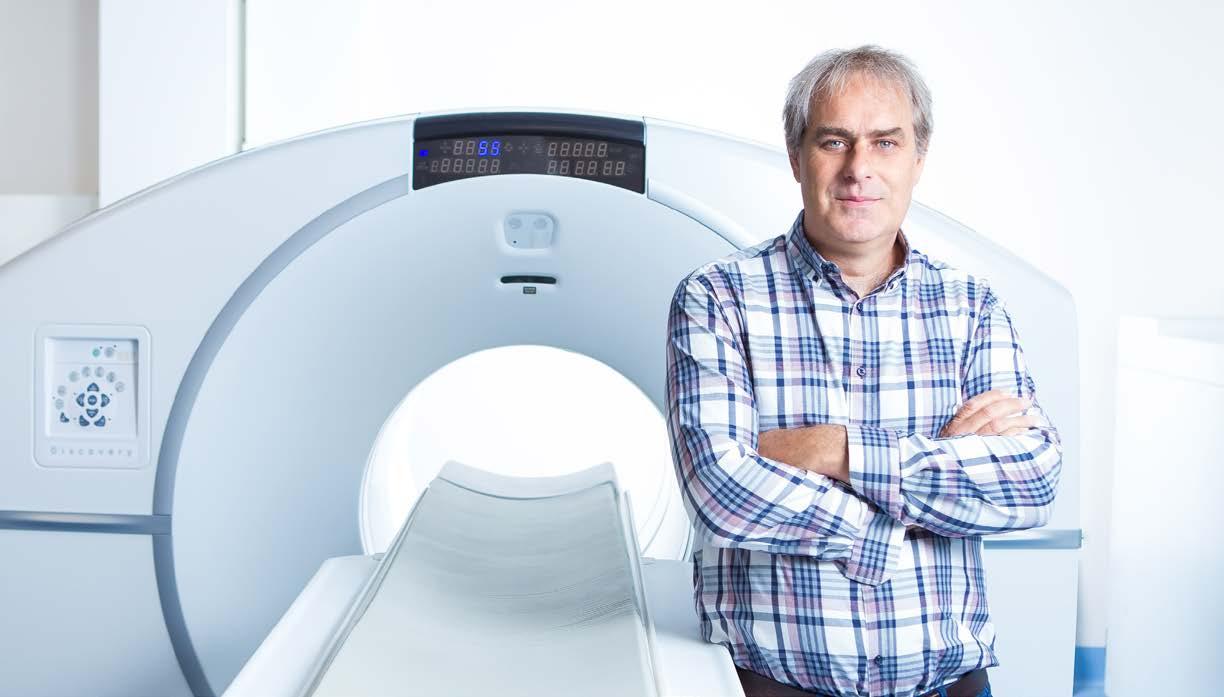
This premium scanner will offer several benefits including an increase in the field of view from its current 15cm to 25cm. Other benefits include:
• Longer field of view resulting in reduced scan time for patients
• Increased appointment availability for more timely patient management

• Class leading sensitivity - 2.8x increase over current system resulting in greater lesion detectability and improved clinical outcomes










Dear GCMA Colleagues,
2023 is here and another active year is planned for the Gold Coast Medical Association. We will encourage a more diverse and inclusive approach to our membership. Our monthly Thursday evening dinner meetings start again on Thursday 16 March at the Southport Golf Club. We anticipate a blockbuster special dinner speaker (following the brief AGM of the association). Please come along and bring your spouse or partner. Monthly Thursday evening meetings will continue throughout the year but we are considering running these meetings on second-monthly basis.
A major focus for the GCMA this year is our medical conference in Apia, Samoa from 29-30 September at the Taumeasina Island Resort. We are running this meeting in collaboration with the Samoan Medical Association, the Oceania University of Medicine, the National University of Samoa Medical School, and the Samoan Ministry of Health. Bond University is a generous sponsor of this meeting. We hope other local Gold Coast medical education institutions will be sponsors too.
Please put this meeting date in your diary. Direct flights from Australia will be available and the accommodation at the resort has been obtained at ‘local’ room rates. This is a conference
NOT TO MISS. Please support this way of advancing medical education in the South Pacific region. A draft conference program will be available soon.
The Medical Link is being enhanced with lots of photos of participants at GCMA functions and articles reflecting medical topics presented at our monthly meetings and other topical matters. I would like to thank Aaron Chapman for the extra attention he is putting into our association magazine. We encourage GCMA members to write articles or advertorials for The Medical Link. Contact Aaron at admin@themedicallink.com.au to make an editorial contribution.
We are always looking to expand our membership. I encourage you to invite your doctor colleagues to join the GCMA. It is very easy to do. Just go to the GCMA website (www.gcma. org.au) and click through to the ‘Become a Member’ page to join. The registration page can take credit card payments. The $150 annual membership is extremely good value. It covers monthly evening meetings where salient updates on clinical and professional matters are presented as well as a two-course meal and complimentary beverage, and the opportunity to interact with colleagues from all professional disciplines.
There are a plethora of benefits gained from tailored and clinically justified exercise programs delivered by Exercise Physiologists.
This can be applicable to people in stages of prerehabilitation, during treatment, survivorship phase, and palliative care. The benefits of exercise address the detrimental side effects of treatment:

C a r d i o r e s p i r a t o r y
f i t n e s s
M u s c u l a r s t r e n g t h
B o n e h e a l t h
M e n t a l h e a l t h
I m m u n e f u n c t i o n
Q u a l i t y o f l i f e
T r e a t m e n t t o l e r a n c e
R a t e o f c o m p l e t i o n
T h e r e l a t i v e r i s k o f
r e c u r r e n c e
T h e r e l a t i v e r i s k o f
m o r t a l i t y
N a u s e a
C a n c e r - r e l a t e d
f a t i g u e
P o s t o p e r a t i v e
c o m p l i c a t i o n s
D a y s s p e n t i n
h o s p i t a l
I would like to thank those members who have renewed their membership for 2023. Your support is always appreciated.
The GCMA is always ready to welcome new members to the leadership team. In particular, we would encourage members to nominate themselves or their colleagues for the positions of secretary, treasurer, vice president, president, junior doctor representative, GP specialist representative, specialist representative, and academic representative at our next AGM in March 2023. Please give me a call on phone number is 0422 545 753 if you are interested.

I look forward to seeing you at our March dinner meeting.
Yours sincerely,
 Prof Philip Morris AM President GCMA
Prof Philip Morris AM President GCMA
"This is a conference not to miss. Please support this way of advancing medical education in the South Pacific region."
If you would like to advertise your products or services, positions vacant, rooms for rent etc. in The Medical Link, please feel free to contact us at admin@themedicallink.com.au.
Advertising of medical services in The Medical Link should comply with the same advertising guidelines released in the Medical Board of Australia Code of Conduct:
Be factual and verifiable | Not include testimonials | Only make justifiable claims regarding quality and outcomes | Not raise unrealistic expectation | Not offer inducements | Not make unfair or inaccurate comparisons between your services and those of colleagues
The Medical Link is designed and published by Swan Management Services. It is the advertiser’s responsibility to ensure that advertisements comply with the Trade Practices Act 1947 as amended. All advertisements are published on the condition that the advertiser indemnifies the publisher and its servants against all claims, suits, actions, loss and/ or damages as a result of anything published on the advertiser’s behalf. DISCLAIMER: The contents of articles and opinions published are not necessarily held by the publisher, editor or the Gold Coast Medical Association. No responsibility is accepted by the publisher, editor or Gold Coast Medical Association for the accuracy of information contained in any opinion, information, editorial or advertisement contained in this publication and readers should rely upon their own enquiries in making decisions touching own interest. Unless specifically stated, products and services advertised or otherwise appearing in The Medical Link are not endorsed by the publisher, editor or the Gold Coast Medical Association.

ADVERTISING
advertising@themedicallink.com.au
FINAL DESIGN & LAYOUT Cabin Studio cabinstudio.com.au
DESIGN & CUSTOMER LIAISON design@themedicallink.com.au
PUBLISHER Swan Management Services admin@themedicallink.com.au
MEDICAL EDITORIAL COMMITTEE
Philip Morris, Geoff Adsett, Stephen Withers, John Kearney, Maria Coliat GCMA MEMBERS gcma.org.au
GCMA EXECUTIVE COMMITTEE
President Prof Philip Morris 5531 4838
Vice-President Dr Maria Coliat 5571 7233 Secretary Prof Philip Morris 5531 4838
Immediate Past President Dr Sonu Haikerwal 5564 6255
Treasurer Dr Geoff Adsett 5578 6866
Specialist Representative Prof John Kearney 5519 8319
GP Representative Dr Katrina McLean 5564 6501
Academic Representative Prof Gordon Wright 5595 4414
The Medical Link enriches the Gold Coast medical community by uniting the voice of its doctors.
Here you will find insightful stories and the latest trends in field research conducted abroad, and of course, right here on the Gold Coast. Keep informed of new health services, developments in the medical profession, and general interest items.
We invite you to submit your company updates, new recruits and promotions to the following email: admin@themedicallink.com.au
And if you would like to advertise your products or services, positions vacant, rooms for rent etc. in The Medical Link, please feel free to contact us admin@themedicallink.com.au.
"Everyone has diversity. Yes, everyone."
But I don’t have any diversity’ responded a colleague when I suggested he come with me to a recent conference session titled Diversity in Surgery. This common misunderstanding may underlie some of the difficulties with improving diversity, not just in surgery but in the whole profession of medicine.
Everyone has diversity. Yes, everyone. Two decades ago, when I was often ‘the only woman in the room’ in surgical teams, it was thought that just getting more women in the room would also ‘get’ diversity. As the numbers of women slowly increased, the same argument was applied to different groups- Indigenous people, those from lower socioeconomic backgrounds, LGBTQI+, those from rural areas and so on.
There has been improvement in measurable characteristics, for example, the number of women surgeons in Australia has more than doubled, from 6% to 15%1, so men ‘only’ comprise 85% of active surgeons nowadays. However, the increase in raw numbers has not translated to leadership and academic roles, even though the first generations to benefit are now in their 50s and 60s2,3 This effect remains even in specialties such as anaesthesia (33% women), and obstetrics and gynaecology (gender parity achieved 2020)4,5
It is becoming clear that there is no ‘pipeline effect’. Simply getting more people with a specific characteristic is insufficient to create meaningful diversity 10 or 20 years later. There are deeper
systemic influences which require a more nuanced understanding of diversity to effectively address.
Developing this understanding is worthwhile because the benefits of diversity are well known. Workforce diversity improves workplace cultures, improves organisational performance, and improves patient outcomes6. The Ottawa Consensus 2010 states that the medical workforce should be broadly representative of the population that they serve7, and it is known, for example, that the mortality penalty for black newborns cared for by black doctors is halved compared to white newborns8 and that women having acute myocardial infarctions have a higher survival when cared for by women doctors9. In Australia, lack of diversity similarly contributes to stubborn problems – rural areas underserved by doctors, a persistently high proportion of patient complaints relating to miscommunication, ingrained disrespectful workplace cultures arising from socialisation into ‘the’ (singular) culture of medicine.
At the same time, there is evidence that targeted programmes for diversity must be very carefully implemented to avoid unintended harms. My research published in the Lancet showed that ‘women in surgery’ programmes have contributed to women leaving surgical training through an ‘othering’ effect. The same research showed that many of the factors affecting women are common to all trainees, not just women10
It has been gratifying to see this research taken up by RACS, which has moved towards policies focused on common values such as respect, flexibility, and educational outcomes. This approach avoids implying that every member of a specific group requires special assistance based solely on a group characteristic, something known as a ‘deficit narrative’. The drawbacks of a deficit narrative become clear if you imagine the outcry that would arise if RACS set up a ‘men in surgery’ programme to give all men special support in view of their 10% lower pass rate in the general surgical Fellowship examination1. Equitable policies that apply to everyone, resulting in targeted support for individuals who require it – regardless of gender or any other characteristic – is more likely to achieve diversity than applying broad brushstrokes to entire groups defined by a nominal characteristic.
Everyone has diversity. Yes, everyone. To fully optimise the current and future medical workforce, we must understand two important concepts, intersectionality and equity.
Consider Figure 1. If a diversity committee were to choose the most diverse candidate for a position they would likely choose the Chinese woman (me), considering that the two men on the left were ‘lacking diversity’. However, it is likely that Philip Morris and I share more in common in terms of educational background and beliefs about equality than Kyle Sandilands in the centre, who is a shock jock well known for racist and sexist slurs on-air. This is the idea of thought diversity – that different ways of thinking contribute more to the benefits of diversity than visibly identifiable characteristics such as age, race, and gender.

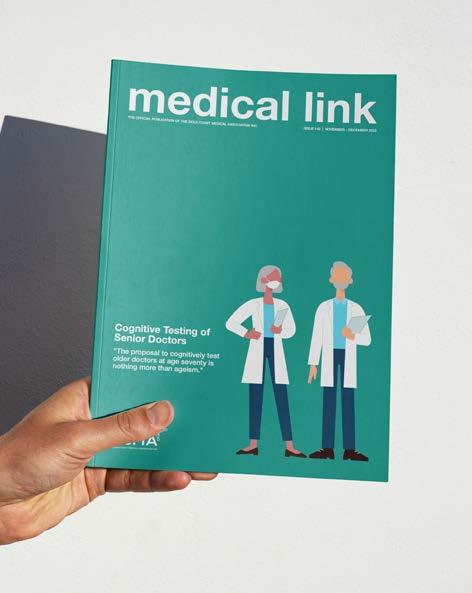
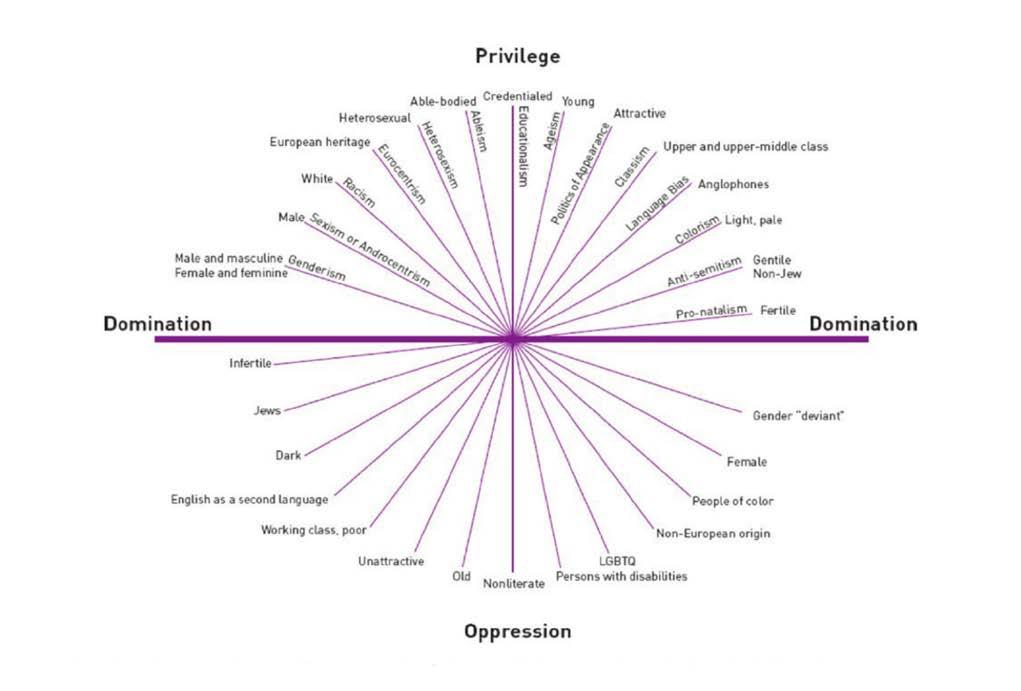
It may be noted that the language of ‘lacking diversity’ is a deficit narrative in itself. It does not make any more sense to say that someone is lacking diversity on the basis of being a man, than it did to say that women all required special assistance to be surgeons. A more contemporary view of diversity is shown in Figures 2 and 3. The Diversity Iceberg shows how people who look similar may in fact have very different backgrounds and ways of thinking, and that much diversity is invisible; ‘below the waterline’. The Intersectionality Wheel shows that there are characteristics that may be more privileging or oppressing in any given context. It is important to note that the composition of the wheel constantly changes depending on the situation. Having
English as a second language, for example, may be oppressing when trying to understand complex legal documents in English, but it may be a privilege when working as a medical translator. For any given time and situation, the ‘heat map’ will look different for individuals, each of whom sits at the intersection of all the many characteristics that make up who they are.
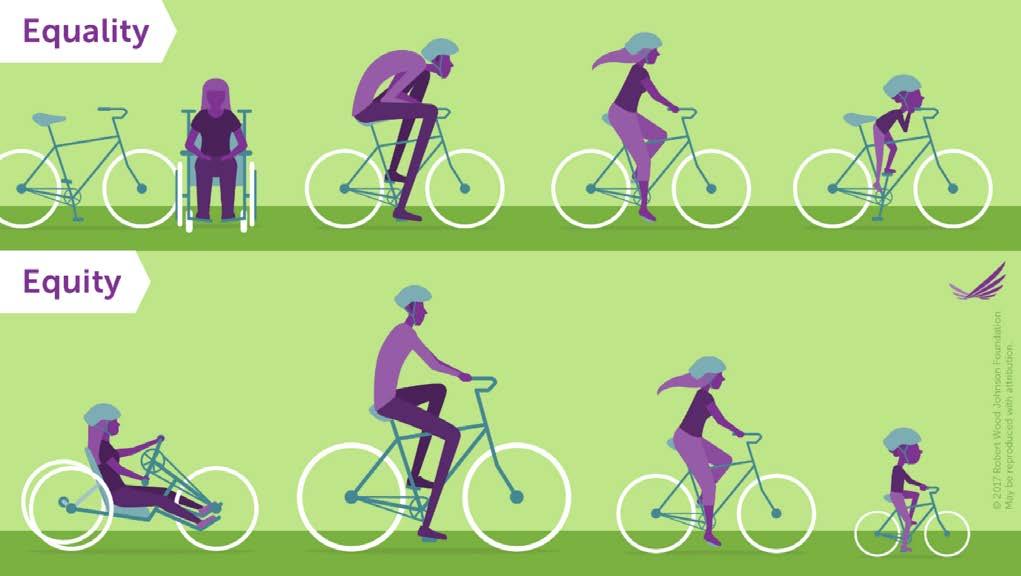
The concept of intersectionality is why claims that ‘we treat everyone the same’ cannot be sustained. We don’t, and nor should we, because to provide a level playing field we need equity, not equality. Unsure about the difference? Equality is treating everyone the same, which seems to make sense at face value but doesn’t bear logical scrutiny, because it merely reproduces existing privileges and oppressions. For example, if the aim is to select ‘the best’ for specialty training by awarding points for first-authored research publications, but some candidates live in metropolitan areas with much better access to research labs, are we selecting ‘the best’ in applying the same points system, or ‘the best located’?
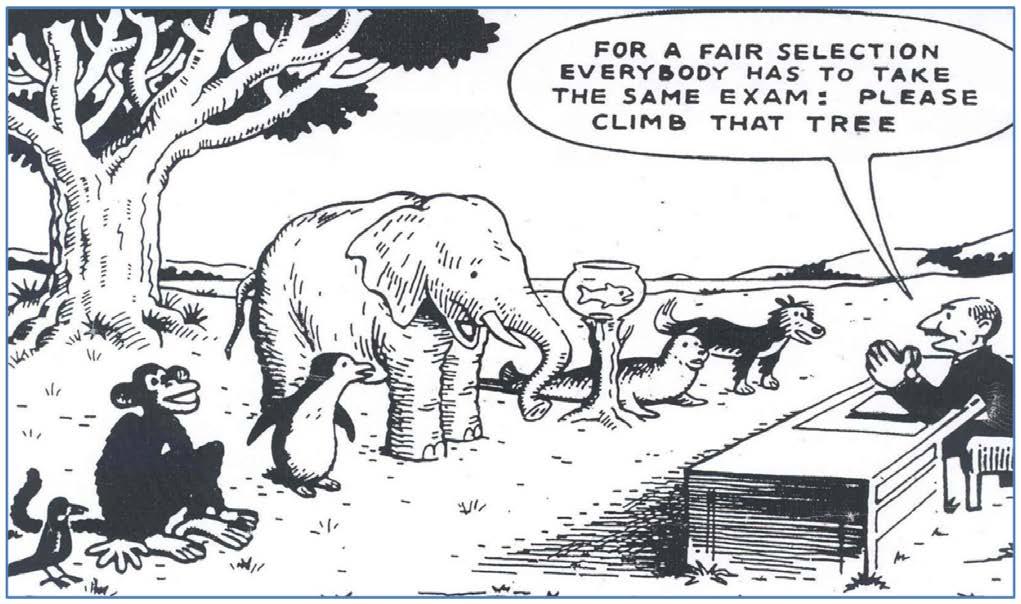
Equity, on the other hand, is treating everyone towards the same common goal, and this is an actual levelling of existing privileges and oppressions to see who can then thrive when given the same opportunities. This may require some people to be given different resources to others. Figure 4 shows how, for a common goal of ‘riding a bicycle’, an equality approach means only one person achieves the goal, while an equity approach means everyone can achieve the goal by getting a different bicycle that suits them. Figure 5 is a humorous take on the same concept; many of us will remember some point in our medical training when we felt like the goldfish being asked to climb the tree. For me, it was being told as a fourth year student that I couldn’t scrub because my glove size wasn’t on the shelves, but I would still be expected to somehow demonstrate ‘gloving and gowning’ to pass the surgical rotation (an equality approach; everyone must be treated the same). Thank goodness I had excellent surgical mentors who perceived the difficulty and found ways to address it (an equity approach; different resources for different needs).
What, then, does this mean for efforts towards diversity going forward? Some practical suggestions:
1. Develop an equity approach. ‘I’m a good guy, I don’t see gender/race’ is an equality approach and continues the status quo; ‘I’m going to look for under-recognized good people and give them a hand’ is active mentorship based on an equity approach and leads to positive change.
2. Avoid making assumptions based on appearances. Broad statements such as ‘women tend to…’ or ‘you look like an orthopod’ ignore all the underwater parts of the Diversity Iceberg. By the same token, don’t accept disrespectful tropes such as ‘boomers’ or ‘dinosaurs’. Everyone has diversity. Yes, everyone!
3. Encourage thought diversity. We are not good at this in medicine. If a student or colleague offers a view that you disagree with, pause a little longer to consider whether it is wrong, or simply different. Wrong views should be appropriately addressed, but many things that were once considered ‘wrong’ in medicine (showing emotions in consultations, permitting trainees to take parental leave, being a doctor with visible tattoos) are now considered a normal part of our workforce diversity. It’s OK to disagree; it’s not OK to be disrespectful in expressing that disagreement.
As for my colleague who believed that he had no diversity? He came with me to the Diversity in Surgery session and was pleasantly surprised that it was not ‘just for women’ as he had feared. ‘I think I get it’, he said as we were exiting towards the exhibition hall for morning tea. ‘I was told I had to shave off my moustache for the Fellowship examination and I did it, even though I felt like a bald alien for the whole exam. My facial hair had nothing to do with my competence. I guess I need to stop putting the same illogical expectations on others?’
He had, indeed ‘got it’.
References
1. Royal Australasian College of Surgeons, 2022. Activities Report 2021. Available at https://www.surgeons. org/-/media/Project/RACS/surgeons-org/files/reportsguidelines-publications/workforce-activities-censusreports/2021-12-31_RACS_ActivitiesReport_2021_V4_ Final.pdf?
2. Teede HJ. Advancing women in medical leadership. Medical Journal of Australia. 2019 Nov;211(9):392-4. doi: 10.5694/mja2.50287
3. Bismark M, Morris J, Thomas L, Loh E, Phelps G, Dickinson H. Reasons and remedies for underrepresentation of women in medical leadership roles: a qualitative study from Australia. BMJ open. 2015 Nov 1;5(11):e009384. doi: 10.1136/bmjopen-2015-009384
4. Bosco L, Lorello GR, Flexman AM, Hastie MJ. Women in anaesthesia: a scoping review. British Journal of Anaesthesia. 2020 Mar 1;124(3):e134-47. doi: 10.1016/j. bja.2019.12.021
5. Modra LJ, Austin DE, Yong SA, Chambers EJ, Jones D. Female representation at Australasian specialty conferences. The Medical Journal of Australia. 2016 Jun 6;204(10):385. doi: 10.5694/mja16.00097
6. Gomez LE, Bernet P. Diversity improves performance and outcomes. Journal of the National Medical Association. 2019 Aug 1;111(4):383-92. doi: 10.1016/j. jnma.2019.01.006
7. Prideaux D, Roberts C, Eva K, Centeno A, Mccrorie P, Mcmanus C, Patterson F, Powis D, Tekian A, Wilkinson D. Assessment for selection for the health care professions and specialty training: consensus statement and recommendations from the Ottawa 2010 Conference. Medical teacher. 2011 Mar 1;33(3):215-23. doi: 10.3109/0142159X.2011.551560
8. Greenwood BN, Hardeman RR, Huang L, Sojourner A. Physician–patient racial concordance and disparities in birthing mortality for newborns. Proceedings of the National Academy of Sciences. 2020 Sep 1;117(35):21194-200. doi: 10.1073/pnas.1913405117
9. Greenwood BN, Carnahan S, Huang L. Patient–physician gender concordance and increased mortality among female heart attack patients. Proceedings of the National Academy of Sciences. 2018 Aug 21;115(34):8569-74. doi: 10.1073/pnas.1800097115
10. Liang R, Dornan T, Nestel D. Why do women leave surgical training? A qualitative and feminist study. The Lancet. 2019 Feb 9;393(10171):541-9. doi: 10.1016/ S0140-6736(18)32612-6
Medical Suite – 78m2
Osler House – Southport
• Air Conditioned
• Good Car Parking
• Large Rooms incl. Fit-Out
• Close to Private Hospitals
• Hygienic Facilities
• Specialised Meadical Centre
• Close to Light Rail
Other Features Include:
• Ambulant Common Facilities
• Wheel-Chair Ramp Access
• Alarm System Throughout (Internally & Externally)
• Small Complex with Similar Specialised Medical Uses
• Good Access & Visibility
• Covered Ambulance Bay
• Staff & Patient Covered Parking (No Metered Areas)
• Recently Refurbished Externally
Contact: 0413 155 200
Figure 5ICON Cancer Centre
Gold Coast Private Hospital
Lower Ground 3, 14 Hill Street, Southport (07) 5634 2400 | admin.goldcoastprivate@icon.team
This World Cancer Day, Saturday 4 February, Australia’s largest dedicated cancer care provider, Icon Group is championing deeper integration of healthcare and innovation to help close the cancer care gap.
Icon Group’s continued focus follows the recent release of a national survey highlighting the obstacles to accessing cancer treatment.
Of the 600 Australia cancer patients surveyed, nearly half (45%) found living life around their care to be one of the hardest parts of their experience.
Up to 69% want to see changes to the healthcare system during the COVID-19 pandemic incorporated into future cancer care of the future. Specifically, increased use of virtual and digital services (76%) and greater flexibility in accessing holistic support (35%).
Icon Group CEO, Mark Middleton said that despite Australia having one of the best healthcare systems in the world, there are still significant gaps in the cancer experience that need to be addressed.
“We’re committed to providing patients greater access to integrated cancer care and working with our partners at local and national levels to connect patients to all aspects of their care,” Mr Middleton said.
“This year we’re continuing to expand our national network of cancer centres (currently at 36 centres), working alongside likeminded patient advocacy groups to improve the patient experience wherever people live.”
This focus on deeper relationships with patient advocacy groups will help connect patients with the services they need in a timely manner.
It’s enhanced by a strategic focus to providing comprehensive cancer care under one roof and using the latest technology and techniques, including centralised remote radiation therapy, to help close the care gap.
“Innovation is key to change,” Mr Middleton said.
“We’ve built a genuinely integrated network of cancer centres and expert clinical teams to eliminate the barriers faced by more remote communities.
“Our way of delivering care addresses workforce shortages and improves patients' ability to access care with greater ease.”
To mark World Cancer Day, Icon Group is running a ‘Blooms of Hope’ campaign.
Icon Cancer Centre teams across the country, including Southport, Gold Coast Private and Gold Coast University Hospital are encouraging staff, patients and visitors to contribute a piece of advice or a message of hope on a paper flower, which will be prominently displayed in their centres, highlighting Icon’s commitment to reducing the global cancer burden.
“Every cancer patient has a unique perspective and story to tell. By bringing together advice, learning and hope from across our network of integrated care services, we’re taking another step forward in closing the care gap,” Mr Middleton said.
Graeme Buntine was treated for prostate cancer at Icon Cancer Centre Gold Coast Private last year.
In mid-2021, Graeme visited his GP to seek treatment for knee pain. The father-of-three has been an avid runner for over 40 years.
The GP suggested a full medical examination, which discovered Graeme’s Prostate-Specific Antigen (PSA) had gone up since his last test.
Upon seeing a urologist, it was discovered Graeme had prostate cancer. Graeme chose to have his prostate removed, but when a check-up after the operation discovered his PSA was still rising, Graeme was referred to Icon Cancer Centre Gold Coast Private radiation oncologist, A/Prof Jim Jackson for radiation therapy.
“It was a big shock to the system,” Graeme said.
“I have always tried to keep myself fit through running and going to the gym three times a week for 40 years. I’ve always been careful with my diet.
“It’s so prevalent these days. Of the 45 members of my running club, 13 have been diagnosed with prostate cancer at some stage or another,” Graeme said.
Last year Graeme completed 35 sessions of radiation therapy at Icon over eight weeks.
While his cancer treatment has finished, he laughs when he points out that he still battling “dodgy knees, which I went to the GP about in the first place.”
"Every cancer patient has a unique perspective and story to tell."












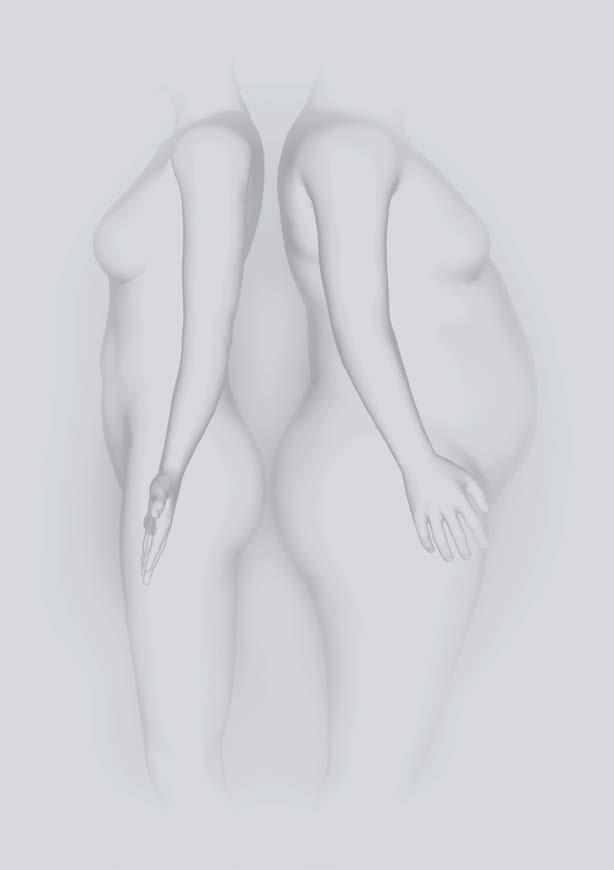
An experienced general surgeon with a sub-specialist interest in bariatric and upper gastrointestinal surgery.

Using the latest surgical techniques, including minimally invasive treatment technologies, Harald has helped thousands of people achieve the best health outcomes. Bariatric patients especially benefit from his close partnership with bariatric dietitians, exercise physiologists and psychologists. It is this dedication to holistic care, and Harald’s compassionate manner, that give his patients individual solutions for long-term results.
PHONE (07) 5667 9766
No or reduced medication for:
• Type 2 diabetes
• Hypertension
• High cholesterol
• Osteoarthritis / joint pain
• Decreased risk of heart attacks, strokes, blood clots
• Decreased risk of developing 13 types of cancer (e.g. large bowel, ovarian)
• Better quality of life and increased physical activity
• Prolonged life expectancy (calculated from the age of 40 years)
• Improved fertility female (polycystic ovarian syndrome) and male
F (07) 5636 6275
E admin@generalsurgerygoldcoast.com.au


"Colorectal cancer is a devastating disease which contributes to the third highest cause of cancer-related death for both men and women in Australia1."
Mohammed Islam MBBS, FRACP Icon Cancer Centre Lower Ground 3, 14 Hill Street Southport (07) 5634 2400 | admin.goldcoastprivate@icon.team
Colorectal cancer is a devastating disease which contributes to the third highest cause of cancer-related death for both men and women in Australia1
Unfortunately, many patients who develop colorectal cancer are asymptomatic until the disease is advanced or metastatic. If detected early, however, colorectal cancer is easy to treat with curative intent. So, while a patient may not exhibit symptoms, screening is critical to ensure early detection and improved patient outcomes.
The risk of developing colorectal cancer increases at 45 years of age. As a result, screening for colorectal cancer in Australia is recommended every two years from the ages of 50 to 74. It is recommended patients who present high-risk factors begin screening earlier. These factors include:
• Previous history of colorectal cancer or adenomatous polyp
• Family history or genetic risk of colorectal cancer
• Abdominal radiation in childhood
• HIV infection
• Lifestyle habits – obesity, dietary fat, alcohol & smoking
The screening process involves a Faecal Occult Blood (FOB) test. This non-invasive test seeks to identify blood in a miniscule sample from two separate bowel motions (faeces). While usually caused by something less serious than cancer, blood may be an early sign of bowel cancer or a polyp (a growth on the inside of the bowel that could develop into cancer).
If the FOB test indicates blood in the bowel motions, a colonoscopy is recommended for diagnosis. Gastroenterologists can perform other tests if required.
In such a deadly disease, it is critical patients are given the best possible chance to beat their cancer. If colorectal cancer is found, there are advanced treatment options available including surgery, radiation therapy, chemotherapy, targeted therapy and immunotherapy.
An experienced multi-disciplinary team (MDT) can help determine the best course of treatment for the patient depending on their individual circumstances, stage of cancer, health factors and treatment preferences.
Dr Mohammed Islam is an experienced medical oncologist who consults and treats patients at Icon Cancer Centre Southport. He is experienced in caring for a wide range of solid tumour malignancies, with a special interest in urogenital cancers, colorectal cancer, head and neck cancer and lung cancers.
For more information or to refer a patient, visit iconcancercentre. com.au/centre/southport, email admin.southport@icon.team or call 07 5657 6400
References
1. Australian Institute of Health and Welfare. (2021). Cancer in Australia. Retrieved from https://www.aihw.gov.au/ getmedia/0ea708eb-dd6e-4499-9080-1cc7b5990e64/ aihw-can-144.pdf.aspx?inline=true
Efficient document management is a key component to running a quality healthcare practice. While more practices have gone ‘paperless’, many still store their digital documents inefficiently and unsecured on computers, which can lead to:
• time wasted trying to locate the current version of a file
• greater risk of data or privacy breaches if anyone can access a document
• data loss if files aren’t backed up
• human error with tasks being missed or performed incorrectly
• interrupted workflows
• not meeting compliance or accreditation requirements
Using a centralised document management system can help streamline your practice processes and ensures your practice and patient data is stored securely.
Below are some benefits of an online document management system in more detail.
A data breach can cost a business in excess of $2 million, depending on the severity. Using a centralised management platform like PracticeHub, practices can load and store all their confidential documents on to the system and can authorise certain employees to view specific documents depending on their role. Any amendments that are made to any documents, can be tracked via an audit trail.
By storing and managing your practice documents on a cloudbased platform, the hassle of manual file backups is often removed, and you can relax knowing that your documents are stored securely. It’s important to perform your due diligence on any supplier before moving your documents to a cloud-based platform. Understand what security protocols the supplier has in place, what location your data is stored and that it meets any regulatory requirements for your practice.
With a document management system, automation saves time and improves efficiencies in workflow. A platform like PracticeHub lets you link relevant tasks and documents to your practice policies and procedures. You can assign tasks to staff roles and monitor compliance and completion. Alerts and reminders ensure you meet compliance or insurance renewals and task deadlines.
Policies are regularly and automatically updated in line with regulatory changes. PracticeHub’s audit history displays all the changes made to the policy, procedure or document. To ensure that the practice’s staff are continually up to date with any amendments made, staff are required to read, understand and agree to the changes. By having a singular and updated copy of documents loaded in the system, it can reduce the risk of human error or compliance breaches.
Storing and managing your practice documents in one place online makes them more accessible to your team and you – wherever you’re working from. PracticeHub’s dashboard gives an overview of tasks and their status, for easy tracking.
Centralised sharing of documents promotes efficiency and collaboration which can in turn enhance team building, morale and better performance – making staff feel like their input matters.
Paper-based or inefficient digital filing can cost you more hours in staff wages which could be better spent on patient care and ensuring compliance. Utilising a document management system, enables practice owners and managers to spend less time on practice administration and more time on big-picture strategy to grow the business. You also save money on paper and printing costs.
Well managed practice policies and procedures improves the quality of your service to patients, and your regulatory compliance. This is easier with a document management system. The customisable policies and procedures templates in PracticeHub are written by practice management experts, providing bestpractice processes for patient care and business management.
The integrated registers streamline insurance renewals management for clinicians and equipment maintenance tasks. PracticeHub also includes eight training modules on common risk areas. This saves you time and money on external training and
ensures staff stay compliant in their roles.
Ahpra Alerts features automatically update practitioner registration status helping to streamline regulatory compliance for a practice.
We’ve seen how a document management system improves compliance, and it stands to reason that this helps make it easier for your practice to not only meet accreditation or quality requirements, but also to prepare for assessment.
With PracticeHub’s Standards-aligned policies and procedures, task monitoring, training modules and audit trail, you have a record of what you need to prepare for, and meet accreditation –all in one place, for quick, easy access.
Discover how PracticeHub’s document management system streamlines your processes, saving you time so you can focus on improving patient outcomes. Visit the PracticeHub website or call 1300 96 86 36.
Persons implementing any recommendations contained in this publication must exercise their own independent skill or judgment or seek appropriate professional advice relevant to their own particular practice. Compliance with any recommendations will not in any way guarantee discharge of the duty of care owed to patients and others coming into contact with the health professional or practice. Avant and PracticeHub are not responsible to you or anyone else for any loss suffered in connection with the use of this information. Information is only current at the date initially published. © Avant Mutual Group Limited 2023
"Lung cancer is the leading cause of death in adults in Australia1."
Icon
Cancer CentreLower Ground 3, 14 Hill Street Southport (07) 5634 2400 | admin.goldcoastprivate@icon.team
Lung cancer is the leading cause of death in adults in Australia1 Fortunately, the earlier lung cancer is detected (especially if it is small and has not spread) the more likely it is for a patient to receive successful treatment and remain disease-free.
Screening can ensure early detection of lung cancer. The screening process involves a low-dose CT (LDCT) scan to generate detailed images of a patient’s lungs. While the scan only takes a few minutes and is not painful, it can subject patients to physical and emotional risks.
In addition to detecting lung cancer, a LDCT scan can also detect small benign lesions (non-cancerous nodules). While these lesions pose no harm to the patient, they must be in investigated by a biopsy and further CT scan if detected. This may result in unnecessary anxiety for patients, health insurance issues and potential over-treatment. Cumulative exposure to radiation, through multiple scans, may also impact on a patient’s health.
The results of over seven large-scale clinical trials indicate that screening for lung cancer did not provide any mortality benefit.
Fortunately, lung cancer is a highly preventable disease. In Australia, approximately 90% of lung cancer cases in males and 65% in females are estimated to be a result of tobacco smoking2 Thus, prevention by advocating to quit or avoid smoking, rather than screening, is the most effective way to reduce lung cancer in Australia.
As a result, screening is typically not recommended for lung cancer as a population-based program. However, there are circumstances where screening can be rationalised. These are typically in high-risk patients who:
• are current, former or passive tobacco smokers
• have had environmental or occupational exposures
• have a family history of lung cancer
• have a history of chronic lung disease3
If there is potentially no, or minimal, mortality or survival benefit for the patient, the decision to screen must be shared between the clinician and patient based on benefit and harm.
If lung cancer is found, it is critical patients are given the best possible chance to beat their cancer. There are advanced treatment options available including surgery, thermal ablation, radiation therapy, chemotherapy and targeted therapies.
An experienced multi-disciplinary team (MDT) can help determine the best course of treatment for the patient depending on their individual circumstances, stage of cancer, health factors and treatment preferences.
Dr Mohammed Islam is an experienced medical oncologist who consults and treats patients at Icon Cancer Centre Southport. He is experienced in caring for a wide range of solid tumour malignancies, with a special interest in colorectal cancer, head and neck cancer, lung cancers and urogenital cancers.
For more information or to refer a patient, visit iconcancercentre. com.au/centre/southport, email admin.southport@icon.team or call 07 5657 6400.
References
1. Australian Institute of Health and Welfare. (2021). Cancer in Australia. Retrieved from https://www.aihw.gov.au/ getmedia/0ea708eb-dd6e-4499-9080-1cc7b5990e64/ aihw-can-144.pdf.aspx?inline=true
2. Cancer Council. (n.d.). Smoking and tobacco. Retrieved from Cancer Council: https://www.cancer.org.au/cancerinformation/causes-and-prevention/smoking
3. Cancer Australia. (2020). What are the risk factors for lung cancer? Retrieved from Cancer Australia: https:// www.canceraustralia.gov.au/cancer-types/lung-cancer/ awareness
Dr Adriana Olog
Maternal Fetal Medicine
Specialist, Obstetrician
Designed by women for women, Grace Private is a dedicated specialist practice offering integrated healthcare for the women of the Gold Coast and surrounding areas.
Gynaecology Obstetrics Fertility
Dietetics
Physiotherapy
Psychology
Endocrinology Women’s Health GPs
(07) 5594 7632
Gold Coast Private Hospital, Suite 5, 14 Hill St, Southport, QLD 4215
graceprivate.com.au
Shop 9.06, The Brickworks Shopping Centre, 107 Ferry Rd, Southport, QLD 4215
Dr Tina Fleming
Obstetrician & Gynaecologist Fertility Specialist
Dr Yasmin Pilgrim
Dr Tania Widmer
Obstetrician & Gynaecologist Fertility Specialist Gynaecological Oncologist

Dr Helen Green
Dr Bridget Gilsenan
Obstetrician & Gynaecologist Obstetrician & Gynaecologist
Dr Priya Sokhal Obstetrician & Gynaecologist


Dr Aakansha Zala Endocrinologist

Dr Shian Miller Gynaecologist
Dr Frances Knight
Dr Elise Turner Specialist Women’s Health GP

Dr Anna Alderton Specialist Women’s Health GP Specialist Women’s Health GP










Elle Pidgeon Debra Miller Women’s Health Physiotherapist Women’s Health Physiotherapist

Karen White Clinical Psychologist


Sharnie Dwyer
Dietitian
"... individuals, patients, families, carers and support groups from all around Australia are saying that the care of mentally ill individuals is a disgrace."
Australia has a mental health crisis. Despite a number of national mental health plans and a decade of changes to public mental health services, individuals, patients, families, carers and support groups from all around Australia are saying that the care of mentally ill individuals is a disgrace. The experience of these groups is backed up by recent reports into the state of mental health nationwide (see recent “Not for Service” report and the Senate Select Committee report on mental health). This crisis primarily affects public mental health services.
In my opinion the problems in mental health stem from the following difficulties.
There are not enough mental health services to meet the needs of patients. This leads to rationing. In the current situation resources are so limited that rationing has to be tightened to extreme degrees and as a result only the most severely ill patients are offered treatment. Other patients who are very ill but fall under the rationing threshold may not get appropriate care. This rationing is most acutely felt when decisions are made to admit patients to psychiatric inpatient care from hospital emergency departments, when decisions are made to discharge patients from inpatient care, and when decisions are made to determine which patients are
offered intensive case management by community mental health clinics. The severity of rationing nowadays means that patients who need hospital admission may not get it, that patients who need longer stays in hospital may be discharged too early, and those patients who need intensive community case management and follow-up may not get it. These flaws in the provision of treatment can have disastrous consequences; an article in The Australian newspaper (Kate Legge, July 19, 2005) drew attention to 42 suicide deaths in Victoria in young people under age 30 over a two year period where inadequate treatment was linked to the suicide. Lack of mental health beds for high risk patients, too rapid discharge, and lack of intensive treatment were problems identified. A Queensland Health report in early 2007 highlighted the problems for patients trying to access a health system under pressure. The report identified 140 unexpected deaths of patients treated by Queensland Health in the previous year. More than half of these deaths (86) were of mentally ill patients who accessed Queensland Health. Most of the deaths were by suicide; either within a week of a patient being assessed in Queensland Health emergency departments and not being admitted, or within a week of discharge from a psychiatric admission. This disproportionate number of deaths of psychiatric patients raises the question of how well Queensland Health services are serving mentally ill individuals. One of the major problems is the lack of acute psychiatric beds (and back-up extended care beds) across Queensland, making admission of very ill individuals difficult and potentially forcing early discharge of inpatients. It is amazing that psychiatric inpatient units are continually at 100% occupancy,
making them unable to meet the demands of fluctuating clinical pressures. Increasing inpatient bed numbers would allow inpatient units to operate at the more conventional 85% occupancy –allowing admission of patients when needed without rationing. Inadequate intensive community follow-up case management of these highly vulnerable individuals means that too few patients are managed closely in the community and are open to the possibility of self harm.
New revisions of state mental health acts have been introduced around Australia over the past two decades. These acts are often more ‘enlightened’ than the ones they replace in that they give more weight to patient autonomy and to the least restrictive forms of treatment being used. However, these acts can be misused because of the pressures of rationing that apply at the moment and this can lead to patients being treated inappropriately. The mental health acts may be used as a 'fig leaf' to cover inadequate inpatient beds ("your son doesn't meet criteria for admission"), or mental health act provisions may be invoked for patients who do not need to be involuntary just in order to access community case management. Another article in The Australian (Clara Pirani, July 4, 2005) highlighted psychiatrists needing to use these practices in order to get appropriate care for their patients. Unfortunately, across the world the introduction of new mental health policies, acts and plans are associated with increased suicide rates compared with national drug policies that are associated with lowered suicide rates. Drug policies usually reduce drug supply and provide more rehabilitation treatment whereas new mental health acts and plans tend to make treatment more difficult to access.
Over the past 20 years there has been a push by public mental health services to ‘mainstream’ the care of individuals suffering from mental illness. This means providing services for them within the general health system rather than a separate service for psychiatric illness. While this has emphasized the role of the general practitioner in providing treatment, and had some (limited) benefit of reducing stigma and curtailing the excesses of some treatment practices in the older, or more isolated, stand alone psychiatric facilities, the policy more broadly has been a failure. The unique needs of individuals suffering mental illness have not been fully appreciated and provided for and this has led to a secondary marginalization of mentally ill patients in general health services. One needs to look no further than the way patients with mental illness and substance abuse are treated in busy public hospital emergency departments to see evidence of this marginalization. Indeed, belatedly, there is now recognition that separate psychiatric emergency departments need to operate in public hospitals. But beyond the emergency department the mentally ill need inpatient units with plenty of space, sub acute and extended care treatment facilities, and properly supervised community residential accommodation – all features that are not usually offered or supported by general health services.
Mortality figures for individuals under the care of public mental health services have been kept very quiet. In NSW, for example, although figures for deaths occurring in people while theoretically under the care of the mental health services have been collected since 1992, systematic publication has always been refused.
A particularly alarming development was that the only paper published on the figures by NSW Health in 1995, covering a 39-month period from 1992 to 1995, had pooled these figures, giving an average of 76 such deaths per year. The paper failed to mention that, as eventually emerged in a 200-page report released very quietly on 23rd December 2003, the figures were actually 68 in 1993, 72 in 1994, jumping to 100 in 1995, i.e. a dramatic and alarming increase of 47% in just three years, which has continued subsequently to a total increase of at least 300% since 1992. Data and trends on mortality from natural causes (including a breakdown of causes of death), suicide, homicide, police shootings, and accidents are not readily available. Nor are data on the number of deaths and severe assaults that are caused by individuals under mental health care.
Australia faces a looming crisis in training of psychiatrists and other mental health professionals. A large number of psychiatrists and psychiatric nurses are reaching retirement age and there are too few coming through to replace them. In addition, the training opportunities for a balanced, comprehensive training experience in psychiatry are limited. Public adult mental health services have gradually but progressively narrowed their clinical focus to patients suffering from drug induced and functional psychoses, patients on forensic orders, and the more severe (often Cluster B – antisocial, borderline) personality disorders. This is an important but very limited view of psychiatry. Many of these services do not provide the breadth of clinical conditions and treatment environments and programs required to provide an attractive and comprehensive training experience for registrars and other mental health professionals. As most training positions are in the public sector (with some exceptions), this is causing serious problems for the training of the next generation of mental health professionals. A recent study from the University of NSW shows that while medical students at the start of their training are favourably disposed to psychiatry, by the end of their clinical training they have a negative view of the discipline! Either the other medical and surgical specialities are better at attracting students, or the experience of clinical psychiatry in the current teaching settings is a ‘turn off’. I suspect the latter. Students find it difficult to identify with aggressive, psychotic, heavily sedated, locked up and often forensic patients that populate public mental health units now. Lack of identification leads to lack of interest in psychiatry as a career.
In my opinion the first action is to emphasise accountability at the point of the patient – clinician contact. The patient placing his or her care in the hands of a doctor, nurse or other mental health professional needs to know that that clinician has the patient’s welfare at heart and that the treatment needs of the patient will not be inappropriately influenced by the demands of rationing applied by the mental health service. This form of accountability will lead to a profound change in the way public mental health services are provided and resourced. Substantial staffing and facility enhancements and additional funding will be required to support this change. As a method of enhancing accountability, the Gold Coast Institute of Mental Health and the Gold Coast Medical Association has called for an audit or commission of inquiry into all suicides to review each pathway to death and any contact the person had with treatment services in order to monitor the quality of mental health care.
An audit or commission of inquiry should be established to examine the pathways to death in all cases of suicide in Australia, whether occurring in hospital or in the community. The inquiry should have the power to call witnesses. The inquiry should be required to focus on the pathway to death of the individual and the nature of contact over the preceding three months between the individual and public (and private) mental health services. The inquiry should make regular comment about the quality of services and make recommendations about improving these services. The inquiry should also examine how the regulations of state mental health acts are being applied to see if they are being used to cover inadequacies in the provision of acute inpatient care and intensive community care. The focus should be on the nature of the contacts with mental health services (and to a lesser extent with other practitioners) in the weeks and months prior to the suicide. In my role as executive director of the Gold Coast Institute of Mental Health and as a private practitioner, I get contacts from families and partners of individuals who have committed suicide, who in the days or weeks prior to the suicide were taken by these relatives/friends to mental health services where they explained to staff the gravity of the situation and the threats of harm to self or others by the individual, yet the individual was not admitted or provided with intensive case management. This is not a unique experience. The Brisbane Courier Mail reported on four suicides in far north Queensland where the adequacy of treatment by mental health services leading up to the suicide is being investigated by the Coroner. Although suicide is a multi-determined behavior, surely the quality of mental health services for those who make contact with them prior to suicide has some role to play in preventing tragic outcomes - if not, then we should not be in the business of providing care. I do not think we can just wash our hands and say that these suicides are "not preventable". Some suicides might be preventable if we hospitalize people at lower levels of concern than we do now. This is an important point: due to limited acute, sub-acute and extended care beds, and perverse use of new (more liberal) mental health acts, access to safe supervised hospital accommodation is so severely rationed that many patients who need this type of care are not getting it. The traditional medical admonition of "when in doubt, play it safe" has been turned on its head in public psychiatry; now it is hard to get at-risk patients admitted unless it has been proved beyond doubt that they will definitely self-harm or harm others. As a result of this situation we have been calling for an audit or standing commission of inquiry into all suicide deaths. A commission of inquiry will provide the opportunity to examine all evidence and witnesses (including health providers and mental health service managers) and to make recommendations about improving services. The advantage of a judicial commission is that it will be independent of government and health services and should be able to make findings and recommendations unbiased by outside influences.
It is important to publish mortality data from natural causes (including a breakdown of causes of death), suicide, homicide, police shootings, and accidents. Mortality data and operative complication rates are now becoming required even for individual surgeons. Anaesthetists for many years have provided a model of how to use their tiny number of deaths to reduce mortality even further. If, as in all other life-threatening illnesses/procedures,
we keep track of all the deaths, note whether the numbers are increasing, and look carefully at each one to see how, when and whether it could have been prevented, then that will tell us clearly how well the system is working. Data should be published on the numbers of deaths or serious assaults caused by individuals suffering from mental illness under care of public mental heath services. In mental illness we also have two other measures which, although social rather than medical, are nevertheless definite enough to be counted as clear indicators of how the system is working. These are the number of gaoled and homeless individuals with a significant mental illness.
Let us acknowledge that the ‘mainstreaming’ policy has its limitations and a move to another model is now needed. An alternate model would recognize the special needs of individuals with mental illness and build a system of care from there while utilizing the strengths and services that comes from close association with general health services. This change in direction would facilitate the development of community, emergency department, inpatient, sub acute, extended care, and residential supervised accommodation services that better meet the needs of the mentally ill. Parallel but integrated services should replace the 'mainstream' model. A major build of clustered 24-hour supervised accommodation around embedded rehabilitation and recovery services is urgently needed for longer stay patients.
A substantial increase in training opportunities beyond public mental health services is required for medical students, registrars, allied health professionals and nurses in order to provide comprehensive knowledge and skills in psychiatry. More training positions in the private sector and in other settings (such as non government organizations [NGO] services) are needed and should be affiliated with learning organizations such as universities and institutes. Methods of funding these positions will be a major challenge, but without this broadening of psychiatric training the profession will wither. With foresight and vision, regional medical communities might just provide the opportunities needed to overcome this looming crisis. The establishment of training positions for doctors, nurses and other mental health professionals in private hospitals and clinics, and NGO services, all affiliated with local medical schools and educational institutes would go a long way to place mental health training on a secure footing. Even within the public sector a change in the teaching environment would help – dedicating some inpatient and outpatient services for voluntary patients only would expand the range of conditions seen and the types of treatment interventions able to be employed, thus offering a more satisfying learning experience.
While a major investment of public resources is required to deal with the mental health crisis, the money will not be well spent unless issues of accountability, service direction and training are addressed.

If you’re considering upgrading your car or practice equipment, now may be the perfect time to make that purchase.
The Temporary Full Expensing Scheme ends on 30 June 2023, and to be eligible to claim an immediate deduction, one qualifying condition is that your car or equipment must be delivered and installed by this date – not just purchased. With the current lengthy wait times, be sure to make your purchase today to take advantage of this attractive incentive
We’ve been tailoring flexible asset finance solutions for medical professionals for over 30 years. Now let us help you make the most of this opportunity.
Visit boqspecialist.com.au to find out more, or speak to your local finance specialist on 1300 160 160.
is the time to ask us how before the