




After more than 14 years at the NSWNMA, including a year as Assistant General Secretary and the past three years as General Secretary, I am resigning to spend more time with my family.
As many of you may now know I will finish my tenure as your General Secretary at the end of this 2025.
It has been an incredibly difficult decision to make but one that is right for me and my family.
The role of General Secretary is all consuming, and I’ve become more realistic about the time and support I need and want to give to my young family.
This union means so much to me, and I’m incredibly proud of the wins we’ve had and the outcomes we’ve delivered for our members.
Together we have secured lasting improvements. In the NSW public sector, they include the commencement of nurse-to-patient ratios and our largest ever strikes for fair pay. These strikes led to our historic legal case now under way to correct deep-seated gender undervaluation in nurses’ wages. In the private sector, we have mobilised members to successfully campaign for better enterprise agreements, while in aged care our pay and staffing wins have also been historic.
It has been a privilege and a joy to share this special journey with you over these years. We have had to fight hard because no one is going to give nurses and midwives what they are entitled to on a silver platter. But we should all be proud of what we have achieved, together writing our own chapter in the history of this great union.
No one who bore witness to our strikes and actions over the last few years could deny what a courageous, energetic, caring and astute membership we have, totally committed to the wellbeing of our patients and residents and unswerving in their resolve to defend and improve our health and aged care systems. You are inspiring – to me and to many others.
It has been a privilege and a joy to share this special journey with you over these years.
I would like to acknowledge Assistant General Secretary, Michael Whaites for his unwavering support, loyalty and friendship during my tenure. I am extremely proud of the powerful partnership we developed and the collective work we achieved together.
I’d also like to thank the NSWNMA Council, the Association’s hardworking staff, the brave and selfless activists of our union and all our 82,000 members.
The NSWNMA Council has accepted my resignation and has unanimously appointed Michael Whaites as the incoming General Secretary, and Katrina Bough as Assistant General Secretary.
Michael and Katrina will commence in their new roles at the Association from 1 January 2026.
Michael has a wealth of experience as both a clinician and a union leader. He has worked as a registered nurse and midwife in aged care, neonatal intensive care, and maternity services, mainly at RPAH, where he was a CME for antenatal and postnatal services.
He was a branch official at RPAH –an organised and active branch that commanded the respect of management and effectively and responsibly wielded power and influence in the interests of members.
Michael has been exemplary in the role of Assistant General Secretary over the last three years and has been tireless in his efforts to strengthen this union and to win outcomes that will improve the lives of our members and our patients.
Katrina is a third-generation nurse having followed her mother and grandmother into the profession.
Her union activism was tempered in the forge of our campaign against the privatisation of rural and regional hospitals.
In that campaign Katrina learned about organising, the importance of relationships and networks, engaging community and power of collectivism, working together with other unions and lobbying politicians.
Over the last five years she has been a senior member of my team.
This new leadership team has my full support. I wholeheartedly believe they will do a tremendous job, and this union will go from strength to strength under their united leadership.n
On behalf of the Hornsby Ku-ring-gai Branch of the NSWNMA, I write with heartfelt emotion to thank and say farewell to our General Secretary, Shaye Candish.
I first had the privilege of sitting beside Shaye when ICU nurses met with then–Health Minister Brad Hazzard. Even in those early meetings, she demonstrated the sharp insight and steady resolve that would come to define her leadership. Shaye proved herself a skilled negotiator — her calm strength and strategic thinking outshining the weary rebuttals of denial from the Minister. She spoke with conviction, representing nurses with intelligence, integrity, and purpose.
Over the past three years, Shaye has led the state’s largest union through a period of immense challenge and transformation. Under her guidance, the Association has undergone a true paradigm shift — one that strengthened its voice and influence across every area of the health care sector. Shaye’s leadership has empowered members to stand tall, speak out, and fight for safe workplaces and professional respect.
She has kept us all accountable in the most positive and inspiring way, reminding us of the power of unity and the importance of courage in the face of adversity. Shaye has led with strength, compassion, and authenticity.
As Shaye steps forward to embrace the next chapter, we stand proud of all that she has achieved. Her legacy will continue with Michael, to inspire us to lead with heart, speak with honesty, and act with integrity.
Michelle Rosentreter, RN, NSWNMA Hornsby Ku-ring-gai Branch
In recent months, most members of our branch have been informed that their eligibility to receive packages from the NSW Rural Health Workforce Incentive Scheme (RHWIS) has been reviewed, and that these payments will cease in 12 months’ time.
The governance and decision making around Rural Workforce Incentives was complicated from the start. Our hospital is big enough to have multiple wards and work groups, yet small enough to have recruitment and retention difficulties due to rurality. The incentive was not a consistent sum of money, but was awarded between $5000-10,000 per year, paid fortnightly, depending on assessment of recruitment difficulty, whether it was critical or hard to fill.
Initially, a few difficult to staff wards received good bonuses, but wards alongside did not.
Incentives were assessed in work groups, or sometimes line management groups, which saw some staff who worked together and performed many of the same roles, receive differing incentive assessments.
Staff who work across wards missed out entirely, such as our many casual staff who save our rosters week after week. This created a nursing and midwifery workforce receiving differing hourly rates due to incentive assessment, not role designation or experience grading. This has upset and undervalued many people.
In the current reassessment, permanent staff positions are assessed against a criterion of being advertised twice in the previous 6 months without recruitment. i.e. we need to resign to prove our worth! It is the opposite of a retention incentive.
Our members are disappointed and stressed by the discontinuation of an incentive which was initially proposed to respect the work we do and the commitment we have to our rural workplaces and public health.
Emma Ratajczyk, RN, Armidale Community Health & Hospital Branch
I would like to thank my organiser and the whole union team for providing me with an opportunity to attend the event in Canberra last week, which was one of my greatest lifetime experiences.
We were given a brief of information on what to expect throughout the event and what we are hoping to talk to the Minister. In the meantime, I was very nervous and anxious if my voice would really matter, especially being early in my nursing career. But on the day of the event, we spoke with the respective Members of Parliament, and I was also able to share my experiences, challenges I have been facing as a newly graduated Registered Nurse and how the providers have manipulated the care minutes and avoided the obligations putting the residents' quality of life at risk.
I got emotional in between the moments as I shared how unsafe I feel working as a nurse, working short staffed every single day because of providers failing to comply with the care minute reporting standards.
I felt more confident and heard when the MPs were engaging in the conversation, acknowledged our concerns and looked out for investigation, and further follow up discussion.
Advertise in The Lamp and reach more than 80,000 nurses and midwives. To advertise contact 02 8595 2139
While no immediate policy change will occur right now, I believe we had a successful discussion and this will contribute to changes we are hoping for in the near future around improving care minute expectations, so we will be able to give residents the quality time and care they deserve.
Punam Subba, RN
Fulfilling a dream
After nearly five years of studying for my Diploma and Bachelor of Nursing, over 1000 hours of placements, countless assignments and exams and huge amounts of stress, receiving my New-Grad offer felt surreal. I’ll be starting in the Emergency Department next year, which is something I’ve dreamt about since I began nursing.
Before starting my Bachelor of Nursing, I worked as an enrolled nurse, so I’ve already seen how challenging yet rewarding the nursing profession can be. But stepping into a RN role feels like a whole new chapter which brings me both excitement and nerves.
The New Grad application process was tough but rewarding. Writing and rewriting selection criteria answers, waiting for interviews and refreshing my emails every minute
Australia’s one stop nurse shop –for all your nursing and midwifery supplies
If there’s something on your mind, send us a letter and have your say. You could WIN scrubs to the value of $50 thanks to eNurse.
EMAIL YOUR LETTERS TO: Editorial Enquiries at lamp@nswnma.asn.au
Please include a high-resolution photo along with your name, address, phone and membership number. Letters may be edited for clarity and space. Anonymous letters will not be published.
the day offers came out. When the offer finally came through, I was overwhelmed with pride and relief. It felt as though every minute of study, every placement, every long shift and every sacrifice made for my degree had finally paid off.
As I am preparing myself to start in ED next year, I’m feeling equally nervous and excited, I know how fast paced and demanding yet rewarding the environment will be.
To those who will be applying for New Grads in the future – don’t give up. The journey is long but when you receive the offer, it’s worth every moment of hard work.
Brooke Erichsen, EN
Our Special Case witnesses made us proud
As a delegate, I personally felt obliged to travel to the IRC hearings to represent my branch, support my friends, and attend as many of the hearings as I could. I think our witnesses felt supported when they saw us sitting in the courtroom, wearing our blue scrubs. Though we could not interact with them in any way while they were on the stand, most of the members thanked us for being there after they were finished.
This case is so important for all nurses and midwives, regardless of the area they are employed in. Nursing is ever evolving, and we are not paid appropriately for our ever increasing clinical and computer workload.
As far as I am aware, over fifty of our NSWNMA members and other professions submitted statements in support of our cause. The NSW Health legal team then decided who they would question, no doubt to try and pick holes in their witness statements.
Our witnesses were fantastic. From NUMs, ADONs, CNC, CNE, CNS nurses from hospital wards, midwifery, ICU, ED, to those from pall care community, mental health, child and family health, theatres, cardiology, and NICU. It was also amazing to see Professors from Sydney Uni, School of Nursing and Midwifery, Australian College of Critical Care Nursing and many more take the stand.
Our witnesses made us proud. They answered in a polite, knowledgeable, intelligent manner, and I am very grateful to each and every one of them advocating for us all.
Kathy Triggell, RN, Wyong NSWNMA Branch

The NSW Industrial Relations Commission (IRC) has heard all the evidence in our landmark work value case for a 35 per cent pay increase over three years and will hand down a decision in 2026.

On 7 November the IRC finished hearing evidence in the NSWNMA’s historic Special Case – one of the biggest legal cases in NSW industrial relations in decades. Final submissions from legal teams representing the Union and NSW Health were due in early December. The case is being heard by two Judges and one Commissioner, referred to as the ‘Full Bench’.
NSWNMA General Secretary, Shaye Candish, said there is no decision deadline but “given the importance of the case the Full Bench is expected to take some time to consider all the evidence put before them.”
A similar case prosecuted by the Fire Brigade Employees Union required five months between the ending of the hearings and the decision.
The Association’s legal team compiled more than 17,400 pages of evidence, including statements from a dozen experts and academics and 39 witness statements from nurses and midwives.
The Ministry of Health’s evidence totalled about 6000 pages.
The NSWNMA presented compelling evidence of:
• the gendered undervaluation of nurses and midwives’ work
• the work value increase over the past 16 years
• the impacts of productivity and inflation
• recruitment and retention across the Public Health System.
Members will not need to vote to accept the IRC’s Special Case decision.
Once a decision is handed down, any updated wage rates and clauses will be put into the new Award which will cover three years – 2024/25, 2025/26 and 2026/27.
Shaye said the NSWNMA had thrown everything at the legal case, after being unable to resolve its pay dispute by negotiation.
“It’s disappointing we weren’t able to settle our pay claim out of the courts, after almost two years of campaigning for a decent pay offer for our members,” she said.
“We put the best possible case forward to deliver public sector nurses and midwives across NSW the recognition, pay, and conditions they rightly deserve.
“In order to boost recruitment and retention and reduce workforce shortages, nurses and midwives must receive a competitive wage that addresses the wage stagnation our members have experienced under the previous Coalition government’s wages policy.” n
Adjunct Professor Debora Picone AO – former NSW Health DirectorGeneral and former NSWNA President (1987-1992)
“Over the past decade, NSW nurses have faced mounting pressures as healthcare demand outpaced staffing growth. An ageing population with more chronic illness has increased patient acuity and hospital admissions. Yet, resourcing has struggled to keep up.”
Professor Rae Cooper AO –University of Sydney Business School “Feminised frontline sectors including nursing (and) midwifery, are essential for the functioning of the national economy and the wellbeing of our communities.”
Professor Caroline Homer AO –Burnet Institute
“The increased amount of screening (for perinatal mental health and domestic violence) increases the emotional work for midwives. It is tiring asking difficult screening questions all day long and responding to the challenging situation that many women are facing.”
Dr Zachary Byfield – Australian College of Nursing
“The move to skills that involve putting things in people’s bodies and taking them back out was a real change in the work of ENs. ENs now can insert and remove invasive devices such as nasogastric tubes and do venipuncture. In 2025 these are now fundamental parts of the EN role and training.” n
The NSWNMA gave the Full Bench detailed written statements from 39 members. They testify to the increased complexity and difficulty of nurses and midwives’ work and reflect the views and experience of members from a wide range of specialties, facilities and locations.
Excerpts from witness statements of four members who participated in the Special Case have been highlighted for you here and over the page.
Erin Bonett graduated as a midwife in 2018. She resigned from her permanent position with NSW Health in 2025 and moved to Mount Isa, Queensland, where her contract to work as a midwife comes with a “significantly higher” salary and free accommodation.
In her witness statement, Erin outlined:
“The main thing that has changed in midwifery from 2018 to 2025 is the complexity of the women giving birth. More women are getting pregnant who previously wouldn't get pregnant, due to advances in technology (such as women with fertility issues falling pregnant with IVF) and it is hard to care for them.
Previously we had “high risk” patients now we have “high highrisk” patients. For example, women with low platelets are now getting pregnant and having the baby, which is a very risky pregnancy... gestational diabetes (diabetes for the first time during pregnancy), is a risk factor for preeclampsia, and has also increased with unhealthy lifestyles in the overall population.
Women with low platelets are now getting pregnant and having the baby which is a very risky pregnancy…

“The main thing that has changed in midwifery from 2018 to 2025 is the complexity of the women giving birth.” — Erin Bonett
Gestational diabetes…is a risk factor for preeclampsia and has also increased with unhealthy lifestyles in the overall population.
Women with polycystic ovarian syndrome, who previously struggled to get pregnant and are now getting pregnant with IVF, are at a higher risk of gestational diabetes and therefore also preeclampsia.
“ Women with kidney problems are choosing to stay pregnant, which makes them at a high risk of developing preeclampsia.”
“From 2018 to 2025 I estimate that I saw the high-risk patients go from being 60 per cent of the workload at RPA to 80 per cent of the workload.”
“ Because there are so many high-risk patients I am in constant consultation with the multidisciplinary team…
These different patients require observations that are different to the standard observations, require a lot of different care and I am exposed to different outcomes for the babies because of risks for the mum.”
“Because of the high rate of highrisk and IVF women, there are more inductions of labour… An induction increases the job of a RM tenfold compared to a spontaneous labour and puts the woman more at risk of needing instrumental intervention or a cesarean section (which also increases the RM’s workload).”
“ I have acquired a significant number of additional skills since I completed university in 2018 but I have never been remunerated for having these.n
RN/M Kathryn Fifield is the facility manager of the multipurpose service in the southwestern NSW town of Henty. Her witness statement described the impact of increasing patient acuity on the MPS, which has 12 aged care beds, three acute beds and two ED beds. In her witness statement, Kathryn outlined:
“Five years ago I saw that the patients in the acute beds were sub-acute. These patients were likely a step up in assistance from home care, were waiting for an aged care bed or had a disease such as gastroenteritis.
Today I see that we are holding higher acuity patients including those with mild sepsis, congestive heart failure or renal failure. This has meant the workload at Henty MPS has also increased.
Patients in the aged beds are people that can't live at home and who need increased assistance. Five years ago, I observed that we used to have low and high-acuity patients in the aged care beds.
Today I observe that they are all high-acuity patients as chronic and complex conditions have increased across the board tenfold due to new medical interventions and people staying alive longer.”
“I have experienced that there is a higher level of medical intervention and we nurses are expected to care for these patients. This means nurses need to be upskilled and there is a requirement for further education for more complex interventions.

‘I have seen a 50 per cent increase in the number of bariatric patients which are obese patients with a body mass index greater than 40… If you put two or three bariatric patients in a ward this is a lot of additional work.’ — Kathryn Fifield
This has increased the knowledge base people need as there are many more procedures and things people have now that nurses have had to learn to do.”
“I have seen a 50 per cent increase in the number of bariatric patients which are obese patients with a body mass index greater than 40… If you put two or three bariatric patients in a ward this is a lot of additional work.
An increase in bariatric patients increases safety fatigue and manual handling risks for staff.
When I did a medication round in Deniliquin in the early 2000s I gave out half the medication I see that is given now…nurses now need to know a wide variety of medications (and) understand those and their interactions.”n
Kellie Toole is a Clinical Midwifery Specialist 2 in Dubbo.
In her witness statement, Kellie outlined:
“Between 1995 and 2020 I have seen a closure of 15 maternity services in Western NSW LHD. The LHD started virtual care (Vcare, which uses video or phone technology to provide care to patients) in 2008.
When I first started working in remote midwifery in 2015 an obstetrician travelled to see women. Now there is either no obstetrician or the obstetrician doesn't travel. The midwife is expected to do those case reviews.

At the moment a registered midwife 8th year earns around $51 per hour as their base rate without penalty rates. I have observed that a lot of midwives I work with have to work shifts that have penalty rates attached to them in order to afford to live.
Working Monday to Friday day shifts does not give me enough income to pay rent in Dubbo… It would be worse for midwives in (Sydney).
As a midwife I am expected to have a high level of skill. I am expected to make decisions and be the devil's advocate to the obstetricians and doctors. As a midwife I have a high level of accountability (however) the pay doesn't recognise that responsibility or compensate me for the times I've missed Christmas and Easter with my family.n
Julia Costello, a Nurse Practitioner at Port Macquarie Hospital, has worked continuously in emergency departments since she graduated in 2008.
Her witness statement described the increased expectations on ED nurses to be able to de-escalate patients, recognise mental health issues and apply mental health first aid to patients experiencing grief, anxiety, depression or psychosis.
“Most emergency nurses I know have had some kind of physical thing happened to them, I’ve seen people punched in the face, I've seen someone attacked with an IV pole. I worked with a colleague who has a large scar on her face after sustaining a 10-centimetre cut on her forehead after she was assaulted by a patient.”
“I have been punched in the head multiple times. I have been kicked in the chest. I have been spat on. I have had people try and rip the skin off my arm.”
“There has however been an increase in training directed at assisting nurses to become more skilled in managing aggressive patient behaviour.

‘The
skill of communicating with and deescalating aggressive patients is a skill that comes with time and experience. It isn't something that can be simply taught in a once-off training session.’
— Julia Costello
This training is excellent but it is it is once-only training, there is no follow up. I am expected to do the training and then retain the skills and knowledge forever.
I have seen in my own practice that the skill of communicating with and deescalating aggressive patients is a skill that comes with time and experience. It isn't something that
can be simply taught in a once-off training session. it is something that I have learned through practice and role modelling over many years. In this way managing aggressive patients went from being a difficult part of my job to an expectation that I will participate in these kind of situations because nurses now have received explicit training, it becomes an expectation that training will be used to deescalate violent and or aggressive patience in EDs.
Aggressive patients used to be managed via a physical restraint. Now this is only done until the patient can be chemically sedated and is only done so the chemical sedation can be administered in a way that is safe for the health staff administering the chemical restraint and the patient.”n
The Association welcomes the facility’s transfer to public ownership but questions remain about proposals to retain private beds within the public hospital.
In October 2025, the state government announced it would spend $190 million to buy back Northern Beaches Hospital (NBH).
The government said it would put the entire 488-bed hospital under the direct control of Northern Sydney Local Health District by mid-2026. All hospital clinical and support staff would be offered jobs by NSW Health at the facility and staff entitlements would be transferred to NSW Health.
As The Lamp goes to print the NSWNMA has become aware that some doctors are pushing for exclusively private beds and services to remain within the public hospital.
“This would have serious ramifications for the operating capacity of the public hospital,’ said NSWNMA General Secretary Shaye Candish.
The state government promised that there would a three-week consultation period on the operating models within the new entity.
“We will continue to advocate for Northern Beaches Hospital to be a public hospital which allows for patients to elect and access private services as we see in other NSW public hospitals,” Shaye said.
Healthscope, which went into receivership in May 2025 with $1.6 billion in debt, will exit its contract to operate the hospital until 2038. The announcement followed months of negotiations between the government, Healthscope and its receivers, to unwind what Health Minister Ryan Park called one of NSW’s worst privatisation experiments.
Mr Park said the in-principle agreement marked the beginning of NBH’s transition into the public health system.
“I want to be upfront that this will not be without its challenges, but patient safety sits at the very heart of this hand-back to public ownership,” he said.
“We have worked with urgency and speed to provide certainty for the community, patients and staff.
“We thank the staff for their hard work and cooperation as we continue to work through the transition.”
Shaye Candish said the government had assured the union that no nurse or midwife at Northern Beaches Hospital would lose their job and leave entitlements would be transferred when the hospital transitions to the public system.
“We are pleased to see Healthscope and the state government working collaboratively to reach an outcome and provide job security to the thousands of staff employed at NBH,” Shaye said.
The NSWNMA campaigned against the Baird Liberal government’s public private partnership (PPP) deal with Healthscope in 2014 (see story p14).
A report by the Auditor-General this year justified the union’s opposition to the deal.
The Auditor-General found that the privatisation model did not allow NBH to deliver adequate health services and created tension between profit motives and health outcomes.
“We warned the previous government this would be detrimental to the community and people of the Northern Beaches, but we were ignored,” Shaye said.
Our Public Health System is NOT FOR SALE

“We
warned the previous government this would be detrimental to the community and people of the Northern Beaches, but we were ignored.”
— NSWNMA General Secretary Shaye Candish
She said transitioning to the public system gives Northern Beaches nurses and midwives “hope for stability, transparency and accountability”.
“We also look forward to the implementation of the public system’s nurse-to-patient ratios which will provide safer workplaces and quality care that our Northern Beaches community deserves.”n
Many
North Shore residents fell for the Baird government line that privatised healthcare services would be ‘the same but better’.
When nurse Robyne Brown heard the state government was taking over Northern Beaches Hospital (NBH), “I ran into the stockroom and said, I told you so!” she said.
As NSWNMA branch secretary at Mona Vale Hospital, Robyne was an early and prominent opponent of the Baird government’s 2013 decision to establish NBH as a so-called publicprivate partnership.
She feared the consequences for patients and nurses if services delivered at Mona Vale and Manly public hospitals were handed to a profit-driven private operator such as Healthscope.
“Soon after the government announcement, a community meeting was held to sell the concept of the new hospital to the public. We had NSWNMA members dotted around the floor to try and ask questions,” Robyne said.
“I think our campaign against the privatisation after that meeting did really well. However, NSW Health was adamant that the privatisation was happening and they weren’t going to budge.
“Our campaign got a lot of support, but as much as we tried, many people failed to realise what impact a private hospital delivering public services would have on the community.
“People believed the government line that everything would be ‘the same but better’ because NBH would be a bigger and fancier hospital.
“A lot of people got a shock after it opened, when suddenly patients were asked to pay for all sorts of things that they would never have paid for in a public hospital.

“I worked in day surgery where we would have a patient covered by a private fund and paying an excess while the public patient having the same procedure next to them paid nothing.
“If you were a public patient everything was free, including medications to take home. But private patients had to pay for them.”
As Mona Vale branch secretary, Robyne battled to get answers to nurses’ questions about employment and working conditions at NBH.
“Before NBH opened in 2018 we had two very frustrating years of so-called planning talks with Healthscope and NSW Health,” she said.
“Every two months Lyn Hopper (Manly Hospital branch president) and I would join the NSWNMA officers and go to a planning meeting, where Healthscope did not want to tell us anything.
“Many people failed to realise what impact a private hospital delivering public services would have on the community” — Robyne Brown
“They wouldn't give us any of the models of care or tell us how many staff we were going to have.
“We had some arbitrary person telling us which field every nurse would be transferred to.
“Most people had to accept the job they were offered and then apply later if they wanted a different job.”
Once NBH opened, Robyne became secretary of the NBH branch and remained at the hospital until arranging a new job in the public system a year ago.
“Staffing levels at NBH were not as good as the public system and the poor communication and lack of transparency made life difficult –especially for branch officials seeking information,” she said.
“There was a lot of frustration with changing management; we had three directors of nursing in the first few months.
“The staffing profile got progressively worse as senior staff left because they were not prepared to put up with inferior conditions.”n
‘Yes’ vote protects pay and annual leave for staff at troubled private hospital operator.
Nurses and midwives at Healthscope, which went into receivership in May, have voted for a new enterprise agreement that locks in pay increases and back pay and protects annual leave.
More than 80 per cent of eligible staff participated in the ballot, with more than 90 per cent voting ‘Yes’ to the agreement.
The vote followed long negotiations included industrial action by NSWNMA members in 2024 and 2025.
Main features of the agreement include a 16 per cent increase to pay and allowances over four years.
Healthscope has told the NSWNMA that back payments of 5.5 per cent from 1 July 2024 and 4.5 per cent from 1 July 2025 would be made no later than 20 November 2025.
Existing entitlements including annual leave and payment of overtime for part-time employees are protected under the new agreement.
The agreement also contains improvements to parental leave and family and domestic violence leave, paid lactation breaks, and improved rights for NSWNMA branch officials.
Speaking to Healthscope members by video, NSWNMA General Secretary Shaye Candish said the union campaign for a new agreement had taken many twists and turns since it started in early 2024.
In particular, Healthscope going into receivership “changed the nature of your campaign”. It became focused on protecting back pay, locking in a pay rise and protecting existing entitlements – especially annual leave and accrued entitlements.

“It would not have been possible to secure these essential improvements without your unwavering persistence.”
— Shaye Candish to Healthscope members
Union pressure via the Fair Work Commission brought Healthscope back to the bargaining table when it seemed the company would not commit to paying back pay in a reasonable time and sought to change annual leave conditions. Those changes “would have meant even a member working 50 weekends and three public holidays a year still would not be entitled to six weeks of annual leave,” Shaye said.
Healthscope dropped its proposed annual leave changes and committed
in writing to paying increases and back pay no later than 21 days after a ‘Yes’ vote.
Shaye described the agreement as “the best to chance to lock in a pay rise, back pay and conditions in these uncertain times”.
The campaign was “a mammoth effort and it would not have been possible to secure these essential improvements without your unwavering persistence.”
She said the union will “continue to work as hard as we can, both here in NSW and at the national level with ANMF and the federal government, to protect your jobs and entitlements”.
Healthscope is reportedly carrying $1.6 billion in debt but the company says its hospitals will operate “as normal” while buyers are found.
Shaye said the Healthscope campaign “has taught us the importance of being organised and ready to take action”.n
Healthscope members can help to enforce their rights in the new agreement by strengthening their local branches. This includes:
• becoming a branch representative/steward for your ward/unit
• regularly attending your local branch meetings
• raising issues through your branch and taking them forward collectively
• talking to your colleagues about joining the Union.n
After three years in the top job, our General Secretary Shaye Candish is leaving the position to spend more time with her young family.
Shaye Candish says that when she assumed the leadership of the Association, in August 2022 she felt compelled to make improvements that ensured the Union worked for members and “gave them a voice”.
Organisationally, it started by giving “our excellent councillors” the training and knowledge “to hold our Union to account and to make sure the Union was doing what was required to deliver for its membership”.
Next, it was to develop a strategic plan - endorsed by council and by delegates - with a very clear set of goals to improve the lives of nurses and midwives.
“I continue to fight for the goals crystallised in that strategic plan, be it about improving pay, getting better conditions for our members, or being involved in the big social justice issues that we know make our members’ lives better outside of work,” Shaye told The Lamp. “We’ve done a few of those things which is pretty exciting.”
STRIKES SUPPORTED BY THE COMMUNITY
Over the last three years nurses and midwives in both the public and private sectors have taken to the streets in massive numbers to pressure the government and employers into fixing the health system’s woes.
These strikes, Shaye says, “were remarkable moments”.
“In aerial shots you could just see this wave of blue walking through the streets of CBD.
“The government was so immoveable the only way we were going to get anything was to turn out in numbers. It was pretty exciting when we did.

“Shaye has created the foundations for a progressive and innovative Union that will continue to lead and grow the nursing and midwifery professions.” — O’Bray Smith, NSWNMA President
“We hadn’t had those sorts of numbers at strikes in our Union for decades.”
This resolve and militancy has also grown dramatically in the private sector.
Ramsay nurses and midwives took strike action – a step they had never taken before.
“People were out for the first time and seeing what it was like to be part of the collective fighting for and winning incredible improvements to their pay offer.
“In both our public and private hospital campaigns, our members political consciousness was lifted with the understanding that this is how you win, you win together.
“That was a really fine thing to be able to share with the members. I hope we have been able to create new generations of people who have experienced the power of unions.”
The strikes, Shaye says, were about more than putting pressure on the government – they were also about reaching out to the community.
“The strikes were critically important to raise awareness about what was happening to nurses and midwives, about the disparity in pay between states and about the disconnection with community expectation of nurses and midwives wages, particularly after COVID, when compared to the reality.
“All that had to be told, and in a very public way, to get community support on our side and to give voice to our members.”
Shaye, a former ED nurse who lives in the Illawarra, says when she came in as the general secretary she fought “really hard to give a platform to aged care and really lift the expectations about the work our Union does in aged care.”
This increased focus has led to strong outcomes, she says.
“We’ve had incredible growth. There’s been some exciting work with our members of culturally diverse backgrounds to bring diversity to member leadership. We have some fantastic and inspiring member leaders. We’ve had some fantastic pay wins and we’ve worked as part of the ANMF nationally on a work value case which has delivered real pay improvements in aged care. The type of improvements that make a real and meaningful difference to peoples’ lives.

“We’ve also had the implementation of care minutes as a first step in government reform, which puts us on a critical path to getting staffing enhancements that allow aged care nursing the time they need deliver great care that residents benefit from
“I hope we have been able to create new generations of people who have experienced the power of unions.”
— Shaye Candish
Shaye says the role of General Secretary is all consuming and she now wants to give time back to her family including two sons at primary school in the Illawarra.
Highlighting the impact of gender on the nursing and midwifery professions has been a feature of the Union’s work over the past few years.

“We have been able to give a voice to the experiences of our members most of whom are women with significant caring responsibilities. People who hold multiple qualifications and yet are not suitably compensated for their skills, knowledge and experience when compared to other professions, this flows onto the males working in our industry too.
“We have highlighted the female dominated nature of our workforce and explained and educated people on the impact of this - our work has historically been perceived as women’s work and therefore has been devalued by decision makers over the years, which still continues in 2025.
“The combination of those factors, year on year on year, has meant that women’s wages have been kept really low while male-dominated workforces have moved ahead quite significantly,” says Shaye.
“Evidence of wage disparity due to gender has been widely used in our campaigning, media and policy advocacy. In the aged care work value case, pivotal evidence around gender inequity was crucial to the outcome. The Association is now using similar arguments in our special case before the NSW IR Commission.”
“My family has often had to sacrifice a lot and that’s tricky. Both of my boys are at a point where they need support. I need to give my kids what they need at the moment.”
NSWNMA President, O’Bray Smith said the Union’s Council had accepted Shaye’s resignation with a heavy heart but fully supported her decision to put her family first.
“Shaye has created the foundations for a progressive and innovative Union that will continue to lead and grow the nursing and midwifery professions,” she said. Her comments were echoed by Assistant General Secretary Michael Whaites.
“Shaye’s commitment to the membership, her tenacity in taking on politicians and national employers, and her dedication to achieving change and advocating robustly for our professions, has been truly inspiring,” Michael said. n
Many nurses and midwives have sent Shaye their best wishes on social media. If you too want to do so, email gensec@nswnma.asn.au.
The NSWNMA is working with the Australian College of Midwives to promote midwifery-led care and the role of endorsed midwives.

An acute shortage of maternity services in regional areas presents an opportunity to promote midwifery-led continuity of care, said Assistant General Secretary Michael Whaites.
He described endorsed midwives as “an extremely under-utilised resource” who could “champion the way” for the spread of midwifery-led care – especially in regional Australia.
Midwifery-led care means care provided to a woman by a single midwife or small group of midwives through pregnancy, birth and the early parenting period.
An endorsed midwife is a midwife with an additional postgraduate qualification for an endorsement for scheduled medicines.
Endorsed midwives have MBS access, can prescribe some medications and order diagnostic tests relating to pregnancy, birth and the neonatal period.
Michael, who is a Midwife and Registered Nurse, was speaking during a panel discussion on midwifery at the NSWNMA’s 2025 annual conference professional day.
He said the Association was working with the Australian College of Midwives to promote “clear pathways for midwifery leadership and endorsed midwives”.
“We have got to make sure that midwives who are prescribing and referring are getting paid for that work because it is adding value and they should be remunerated.”
Michael said the 2024 Midwifery Futures report found shortages of midwives in places across Australia – particularly in nonmetropolitan areas.
“The report also found though that based on current uni enrolment rates, and looking at current retention rates, we've got enough midwives to last us and be in surplus by 2030.
“However, the report also noted that if the attrition rates get worse then the profession is in a catastrophic position.”
This was worrying because NSW Health data showed a 10 per cent reduction in the number of senior midwives over the past 10 years.
“Senior midwives are reducing their hours or leaving the industry. And they are doing that because of burnout, lack of job satisfaction, poor workplace culture and poor workplace safety,” Michael said.
“Early career midwives are also dropping their hours or leaving the industry and they are doing that because they are not able to work the way they were trained to work.
“And when they look over their shoulders in a moment of crisis, guess what? The senior midwives aren't there.
“We've got really intelligent young people wanting to do midwifery, but we just can't hang on to them.”
— NSWNMA Assistant General Secretary Michael Whaites

“To get into midwifery you need a really high ATAR score and we've got really intelligent young people wanting to do midwifery but we just can't hang on to them.”
Michael cited a 2022 report on “Future proofing the midwifery workforce in Victoria”, which said three quarters of managers reported their services were inadequately staffed with midwives.
“The key challenge again was trying to get experienced midwives to work.
“All the research shows we simply need to pay midwives better and give them a better working experience.”
Another speaker at the panel discussion was Dr Alison Teate, an experienced endorsed midwife and lactation consultant working in private practice.
Dr Teate is the vice president of the Australian College of Midwives, has held midwifery academic roles at two universities and is co-director of a collaborative GP-midwife practice.
She said the number of endorsed midwives (in NSW?) had grown from 600 in 2020 to 1502 in 2025.
Emma Gedge is a midwife and lactation consultant in public and private practice and a member of the NSWNMA state council.
She told the annual conference panel discussion that midwives’ inability to work to their full scope of practice left them feeling undervalued.
“When you come out of university either as a direct entry midwife – or as a mid-start – you have a lot of skills that that lend themselves to autonomy,” she said.
“Then, when you work within a health service, your hands are quite often tied.
“There are lots of things you can't do because you're at the mercy of the overarching obstetric model of care that you're working under.
“That's a really soul-destroying way to work and it gradually eats away at you until you either quit or you … just do your job.
“We really do need to recognise that midwifery is a distinct profession and we have a very distinct set of skills."n
She said that to maintain continued growth and innovation governments need to be held accountable.
Governments also need to continue providing primary care scholarships for nurses and midwives.

“The Australian College of Midwives wants to remove the requirement of 5000 hours of clinical practice in order to gain endorsement ”
— Dr Alison Teate, Vice President Australian College of
Midwives
Dr Teate described the process midwives need to follow to gain endorsement.
In her case, she undertook a Nursing and Midwifery Board-approved postgraduate qualification in prescribing and also in referrals for pathology and radiology.
She then needed to apply to APHRA (Australian Health Practitioner Regulation Agency) with evidence she had completed 5000 hours of midwifery practice in the six years before her application (amounting to three years full time in that six years).
“And then with my endorsement that I got through the NMBA I was able to do applications to Medicare and to the Pharmaceutical Benefits Scheme to enable me to get my provider and prescriber numbers,” she said.
Dr Teate added that the Australian College of Midwives wants to remove the requirement of 5000 hours of clinical practice in order to gain endorsement.
“We would like to replace that with enabling our new career midwives to come into the profession from an undergraduate course – being able to learn to prescribe and provide diagnostic support.
“We should have early career mentorship support and probably have a transition to practice year in regard to that prescribing.”n
Culturally safe care for Aboriginal families was a focus of a panel discussion on midwifery at the NSWNMA 2025 annual conference professional day.
The annual conference midwifery session was addressed by Aboriginal midwife Tamara Blanch who has worked for Binji and Boori Aboriginal Maternal Infant and Child Health Service for 20 years.
Binji and Boori is part of Illawarra Shoalhaven Local Health District. It does not birth babies but provides continuity of care in the antenatal and postnatal periods.
Staff include Aboriginal health workers, child and family health nurses, midwives, social workers, an occupational therapist and a speech pathologist.
Tamara started her career as an Aboriginal health worker at Binji and Boori 20 years ago and completed a bachelor of midwifery in 2012.
She said the service supports families “from pregnancy testing to when baby starts school”.
The centre started by talking to community elders, women, and men’s groups “to find out from the community what they wanted,” Tamara said.
“We wanted to provide a family service; it wasn't just for the women.
“We have a lot of cultural events rolled into our care.
“We provide a lot of education and a lot of our women go into that birthing space so well educated and so empowered that they come out the other side and say, ‘We had such a good experience’.
“One of the biggest successes I see in our program is that we have families who bring their babies in 18 years later and say, ‘This was your Aboriginal health worker, or this was your midwife’.
“They don’t say that just to me; it is to our non-Aboriginal staff as well.
“They come up, and they throw their babies over the table at Emma and Katrina and our other staff members for cuddles. This shows me that our service is successful.
“The families are comfortable coming to us and they refer the majority of our clients on to us, [which] shows trust.”
Tamara was asked what healthcare staff can do to provide culturally safe care in services that are often restricted by red tape.
“Each interaction that we have with every family is an opportunity to build trust, to listen deeply, to build respect and to be respectful of everybody's cultural identity,” Tamara replied.
“Just sitting and listening to someone’s story can open doors. It can make such a huge difference."
She urged members to “advocate for change in your services”.
“Do it in your staff meetings, collaborate with your Aboriginal health workers, collaborate with your Aboriginal hospital liaison officers, take it to your Aboriginal executive directors.
“Listen to the wants and needs of your community.
“There are Aboriginal working groups across the state; go to them, listen to their wants and needs and take them to the meetings in your area.
“If we've got clients who are requesting things outside of normal care, I will request an MDC [multidisciplinary meeting] with the stakeholders at the hospital.

“Just sitting and listening to someone’s story can open doors. It can make such a huge difference.”
—Tamara Blanch
“I will pull in my manager, the manager of the maternity unit, the manager of the birthing unit and I will put the woman's wants and cultural needs on the table …
“If the woman is at a place where she's able to come to those meetings she will sit next to me, and we will discuss … what needs to happen.”
“All these things take time but … you can pull those Aboriginal health workers in to help you to do those meetings.”n
In July, NSWNMA Councillor Rebekah Henderson travelled to Kaurareg Country, Waibene (Thursday Island) where 200 Aboriginal and Torres Strait Islander nurses, midwives and health professionals discussed putting Indigenous practitioners at the centre of health care delivery to their communities.
The event was the annual conference of the Congress of Aboriginal and Torres Strait Islander Nurses and Midwives (CATSINaM).
“The theme of the Regional Congress was The Power of Bringing your Practice Home,” Rebekah says. “It highlighted the importance of Aboriginal and Torres Strait Islander nurses and midwives using their skills to improve the health and wellbeing of Mob.”
CATSINaM and Torres Strait Islander Elder Aunty Professor Doseena Fergie, a registered nurse and midwife who holds a PhD in nursing research, argued for more Aboriginal and Torres Strait Islander nurses and midwives to be elevated to higher positions in health.
Rebekah attended the conference with Keith Wicks, the NSWNMA Aboriginal and Torres Strait Islander Engagement Officer, NSWNMA

organiser Jo Perdue and members Michelle Cutmore and Jo Burton (a nurse practitioner who also happens to be Rebekah’s mother).
“Keith presented on a panel that explored what a cultural safety looks like in the workplace,” Rebekah says. “He shared his experience and insights into how cultural safety may be developed through organisational commitment and willingness and, conversely, the risks presented when Aboriginal and Torres Strait Islander workers become isolated in their workplace.”
AND CATSINAM
CATSINaM and the NSWNMA have a long association. “CATSINaM had their first meeting at the Association headquarters,” says Rebekah.
“Dr Aunty Sally Goold, who recently passed away, and Aboriginal and Torres Strait Islander nurses and midwives founded CATSINaM to have a formal representative body for Aboriginal and Torres Strait Islander voices.”
“While we spent a lot of time throughout the Congress continuing to develop the NSWNMA relationship with CATSINaM, I have come away feeling there is much to be done in this space,” Rebekah adds.
As well as being a NSWNMA councillor, Rebekah, a dualregistered RN and midwife, works to amplify the voices of Aboriginal and Torres Strait Islander members within the NSWNMA as a founding
member of the Association’s Aboriginal and Torres Strait Island Member Circle. All new members who identify as Aboriginal and Torres Strait Islander are automatically included in the Circle.
Rebekah says the Circle, which will celebrate a two-year anniversary in January, “is a really important voice within the union”.
“The recent creation of two Aboriginal and Torres Strait Islander councillor positions is another important step, but there is always more we can do to make sure that we have an Aboriginal and Torres Strait Islander lens not just on Indigenous, but on all issues.”
There are some NSWNMA members who aren’t aware that they can be a part of the circle as well as a member of their local branch.
“We would love to welcome people to come to our meeting and talk about Aboriginal and Torres Strait Islander issues in nursing and midwifery,” Rebekah says.
“We would love more active members,” Rebekah says of the group, which meets online bimonthly.n
The next CATSINaM Congress in 2026 will held in Alice Springs, NT. For more information about taking part in the Aboriginal and Torres Island Circle, contact Keith Wicks at the Association.n
There are there are 200,000 survivors of Female Genital Mutilation in Australia, says Khadija Gbla.

“Female genital mutilation is a brutal form of discrimination and an attack on autonomy, sexual rights, and so much more.”
—Khadija Gbla
Khadija Gbla’s activism against female genital mutilation (FGM) began when they were 13 years old and they told their mother that the practice that women in their family had undergone for generations had to end. “I looked her in the eye and said: ‘No more’.”
Like their mother, as a child Gbla experienced what they call a form of gender-based violence. They told their mother: “I did not consent to this being done. A child cannot consent.”
“I was the circuit breaker,” says Gbla, who identifies as non-binary.
Gbla, who was born in Sierra Leone and fled war as a child before settling in Adelaide, has become one of Australia’s leading voices in the fight to end female genital mutilation (FGM). Earlier this year they spoke to an audience of nurses and midwives at a NSWNMA professional day.
WHAT IS FGM?
Gbla describes FGM as “a brutal form of discrimination and an attack on autonomy, sexual rights, and so much more”.
According to the World Health Organization (WHO), FGM includes all procedures that involve partial or total removal of the external female genitalia or other injury to the female genital organs for nonmedical reasons.
Type 1 (Clitoridectomy) – “Type one involves the partial or total removal of the clitoris,” Gbla says. “People use that to liken it to male circumcision. It’s a way to minimise what is a brutal act being done to children.”
Type 2 (Excision) – Partial or total removal of the clitoris and labia minora. This is the type Gbla personally experienced at nine years old in Gambia, when “an old lady was paid money to use a rusty knife to mutilate me.”
Type 3 (Infibulation) – This type involves the removal of external genitalia and sewing the vaginal opening closed. “We have people walking around who are infibulated,” Gbla says. This procedure has serious implications, often causing difficulties urinating.
Type 4 – Includes harmful procedures such as pricking, piercing or cauterising the genital area.
A PRACTICE WITHOUT BORDERS
FGM is often mistakenly seen as an issue confined to regions in Africa or the Middle East, but Gbla says this is not correct. FGM has been documented in “every continent except Antarctica”, and it occurs

across communities of different races, religions, and social classes.
“When people think about this, they think of third-world countries. They think of where I was born,” they explain. And yet “labiaplasty for kids under the age of 18, without medical reasons, will fit the definition of FGM if it’s been done for non-medical reasons.”
Gbla says that in Australia “there are 200,000 survivors of FGM”. At last count “11 girls a day were at risk of being mutilated in Australia”.
The immediate risks of FGM include haemorrhage, infection, shock, and death. Long-term complications encompass infertility, fistula, painful periods, sexual dysfunction, and childbirth complications.
“You might not even get to childbirth because one of the health consequences of FGM is infertility,” warns Gbla.
Survivors often experience complex post-traumatic stress disorder, loss of trust in caregivers, and deep emotional trauma. “Remember,” Gbla says, the practice is “predominantly done by caregivers, who you should feel safe with.”
In Australia, FGM is illegal in every state and territory, and it is a criminal offence to perform or assist in performing FGM, to take a child overseas for the procedure, or to fail to protect a child from it.
Gbla reminds healthcare workers of the importance of understanding and communicating the law clearly. “Ensure that girls, women
understand the law and how it may help them but understand that people may feel pressured.”
For Gbla, health professionals are critical agents of change. “You are at the forefront of the battle to eliminate female genital mutilation,” they say. Nurses and midwives are the frontline workers who provide care to survivors of FGM.
This requires sensitivity, cultural awareness, and a trauma-informed approach, they say. “Sometimes in our battle or fight to eliminate FGM, we sometimes alienate,” Gbla cautions.
“We can come in so strong; we push people back. People can feel ashamed and judged. And you can’t make change where there’s no safety. So, we must make people feel safe.”
Gbla encourages nurses and midwives to ask direct but respectful questions when taking a patient history. For example:
• Have you had the practice of FGM?
• Have you had any gender alterations done to you?
• Have you had any problems passing urine or difficulties during childbirth?
They emphasise the importance of documentation, noting the type of FGM, scar tissue, and any evidence of re-suturing. “Be mindful that dark-skinned people have keloids,” they add.
In
Australia, FGM is illegal in every state and territory, and it is a criminal offence to perform or assist in performing FGM, to take a child overseas for the procedure, or to fail to protect a child from it.
Gbla advises healthcare providers to approach survivors without judgment. “Be aware of your own feelings and responses. We think we’re poker face, but people watch us. They go, ‘Oh, you’re about to judge me.’ Don’t make assumptions; ‘Oh, you’re African, you must have had FGM.’ Please don’t.”
“You could be the person speaking to a grandma and changing their mind about this. You could be the person speaking to a mom or a father or a sister. But it will matter how you hold this conversation, which is complex and nuanced.”
Gbla left the audience with a message about why the role of nurses and midwives matters so profoundly to protect children, just as it was their role as a 13-year-old who spoke up to their mother: “Child abuse is my place. Child protection is all our place.”n
We need to inoculate ourselves from online disinformation, argues journalist Van Badham.
When protestors in hi-vis vests and work boots assembled outside the Melbourne headquarters of the CFMEU’s construction division in the early months of the COVID lockdowns, journalist Van Badham was researching a book about conspiracy theorists and rightwing extremists.
The protest, which turned violent, was demanding the “CFMEU fight the lockdowns and fight all the health restrictions … at a time when COVID was killing hundreds of people every day in Victoria”, she says.
When Van saw images of the protest on the news, she recognised that the ring leaders belonged to extremist groups she had been researching for her book.
“They had bought their hi-vis on the Internet. They had bought it from Amazon. They were pretending to be union members, and they were not,” she said.
Van used the story to illustrate just how easily disinformation can spread in a highly online world. And now, “AI (artificial intelligence) is changing the game of disinformation and supercharging it rather extraordinarily”.
Speaking to the NSWNMA 2025 annual conference, Van said there had been a “concerted effort” to attack unions with disinformation – false information intended to mislead.
“Unions are a problem for authoritarians,” she said.
“There was a reason why the Nazi party came after us first; we're strong and we're powerful, we’re full of

believers, we are people who put the collective ahead of the individual.
“That makes us very dangerous to projects that want to prioritise the power of a small group of individuals.
“Unions are democratic organisations that by their very existence prove the value of democracy. So demobilising, disenfranchising and dividing unions is absolutely crucial to the anti-democratic project.”
Van said unions have industrial and economic power to “stop corporations from doing things that hurt us”.
“We also have cultural power; every single union member is an advertisement to the rest of the community about the values of equality, about the values of
democracy, about the values of enfranchisement, about the values of feminism and anti-racism and antihomophobia and anti-transphobia and anti-bigotry.
“We stand for a cultural principle that we are all equal and that is a powerful principle.”
In another protest outside an Ikea store in Melbourne during the COVID pandemic, a crowd of about 700 spread the message that vaccinations are dangerous. “This protest, it turned out, was actually organised by a far-right group in Germany, and the Australians who participated did not even know who was calling the shots,” Van said.
She said health workers and the CFMEU were not the only workers to be targeted by disinformation.
“Librarians never thought they would be dealing with bomb threats at work. They are because of the crazy scare campaigns around drag queen story hour in Victoria.”
Because of disinformation, “council workers who are members of the Australian Services Union have been targeted with the most extreme threats of violence merely for working for councils that host drag queen story hours”.
She added that as a result of “disinformation about gender relations” some teenagers were refusing to be taught by female teachers “because the internet has told them those women are lesser and inferior to them”.
During the 2023 Voice campaign, majority support for a Voice to Parliament swung to a majority No vote because the No campaign was so effective at spreading disinformation online, Van said.
“The point is not that people believe it. The point is that people do not have the time to check if it was true.”
“Disinformation is not just about the people who believe the nonsense. It's also about the people who get confused by the nonsense and it's about the people who see the nonsense, want absolutely no part of it and drop out.”
The 60 per cent No vote in the Voice to Parliament referendum was not due to racism or hatred of Aboriginal people, “but because [voters] were subjected to the most feral onslaught of disinformation in Australian history”.
Van Badham called for a “counter disinformation body”, the equivalent of an ICAC [Independent Commission Against Corruption], to independently monitor disinformation.
We need to support institutions such as the ABC, she argued.
“Disinformation thrives when people don't believe in institutions … or don't believe media mastheads, or don't believe the ABC. That's how these messages get out.”
Her headline message, however, is “Don't share”.
“Leave, go outside, reconnect with the world, find a friend. Do not share it. Do not ‘Like’ it. Do not be part of that system.”
“Unions are democratic organisations that by their very existence prove the value of democracy.”
Use fact-checking sites, she encouraged. When the topic is a workplace issue affecting nurses and midwives, get out ahead of disinformation when you can.
“Inoculation is everything. It doesn't matter what it is – vaccination, working conditions – whatever people are trying to politicise, if you know it's a lie, get out ahead of it.”n
“Unions are a problem for
authoritarians.”—Van Badham



Working consecutive shifts
I am a registered nurse working in a public hospital and my manager has rostered me to work eight shifts in a row. Can they do this?
No. As per subclause 4(iv)(a) of the Public Health System Nurses’ and Midwives’ (State) Award 2023, an employee cannot be required to work more than seven consecutive shifts unless the employee requests this and management agrees.
You can agree to work this shift pattern, but you should not be required or pressured to do so. Under no circumstances, though, can an employee work more than 10 shifts in a row.
You should direct your manager’s attention to this subclause and contact NSWNMA if further assistance is needed.
Requesting leave without pay
I work in a public hospital in Sydney and want to take six months off for a road trip with my family. I do not have enough annual leave to cover the full six months. Can I ask for leave without pay to give me enough time off to go on my road trip?
You may request leave without pay in these circumstances.
Section 8 of NSW Health Leave Matters for the NSW Health Service PD2024_046 sets out various conditions in relation to leave without pay, including the following:
• a maximum of three years' leave without pay can be granted
• a sufficient reason for the leave must be demonstrated
• the employer must be satisfied that the employee intends to resume duty at the conclusion of the leave
• excess annual leave and accrued ADOs must be taken prior to commencing leave without pay
When it comes to your rights and entitlements at work, NSWNMA General Secretary Shaye Candish has the answers.
• the conduct and performance of the employee must be satisfactory.
If you meet these conditions and your manager unreasonably refuses to approve your request, please contact NSWNMA for further advice and support.
My manager has been rostering me under my contracted hours. I have tried to raise this with them, but they say they don’t have shifts available for me. What are my rights in this situation?
A contract is a legal and binding agreement between an employer and an employee. Each party must meet their obligations under the contract unless the two parties mutually agree to a change to the contract. If your manager does not have shifts available for you and you are ready, willing and able to work, your employer must still meet your contracted hours in wages. If you are unable to resolve this with your manager, you could escalate your concerns managerially or to your pay office. Please contact NSWNMA for advice specific to your situation or if you’re not able to resolve the issue with management.
I work as a registered nurse for NSW Health, and I have been injured at work. I am receiving workers compensation payments and working reduced hours at work while I recover. Can I access my sick leave to top up the difference between my compensation payments, and my normal fortnightly wage?
Yes, you have a right to access your sick leave to top up your pay but only to the base rate. You can always request to use your sick leave to top up to a higher rate,
but your employer is not required to grant this. Additionally, you may take annual leave or long service leave while on workers compensation and receive the workers compensation benefits and payment for the leave simultaneously. In the public health system, there is an option to take long service leave at half pay if requested by the employee. If your employer refuses your application, please contact NSWNMA for advice.
My employer has told me I must sign a new contract which is different from my current contract. I am not happy with some of the terms. Do I have to sign the new contract?
An employment contract is made when the employer makes an offer that is accepted by the employee. A contract must be entered into by mutual consent between the parties, free of pressure or coercion. A contract can be oral or in writing and does not necessarily require signatures to be legally binding. An employer cannot force or compel you to sign any contract or document that you are not comfortable signing. If you don’t agree, then you should let your employer know that you decline to sign as you wish to remain on the terms of your current contract. NSWNMA is here to assist if your employer makes any changes to your employment without your agreement.

Branch Beat with NSWNMA Assistant General Secretary Michael Whaites
Winning an adequately staffed, safer workplace sometimes comes down to a battle of numbers.
NSWNMA branches may need to collect a lot of data to show that a ward or unit is understaffed, or that management practices are unsafe and need to be changed.
Public sector branches can put their case to a hospital-level Union Specific Consultative Committee (USCC) – a forum for consultation and discussion between management, a specific union, and its delegates.
The NSWNMA branch at Tomaree Community Hospital has shown how effective use of a USCC can win improvements when combined with the reasonable workloads clause in the PHS Award.
Located in the Port Stephens region north of Newcastle, Tomaree Hospital is somewhat unique: it is a Peer D hospital with a level 2 emergency department.
The ED sees about 18,000 patients per year – more than some level 3s – but must get by with level 2 staffing. Night shifts were under the greatest strain. By mounting a strong case based on careful data collection, Tomaree branch achieved more hospital funding, more staff, and improved criteria for patient admissions. Improvements included:
• an increase in funded beds – from six to 10
• four nurses on night shift – up from three
• permanent FTE allocation for current staffing of five on morning and afternoon shifts
• safer admission criteria.
In 2024, Tomaree branch sent hospital management a written proposal for a safer workplace and asked management to convene a USCC.
The NSWNMA team for USCC meetings comprised Branch President Megan Chippindale, Branch Delegate Tracey Richardson, an NSWNMA organiser, and an Association lawyer.
Across the table were hospital and regional health service management representatives.
The branch put a case for more funding for the ward, which was funded for only six of 14 physical beds.
Branch officials had collected data to prove that:
• the ward had 10 patients per day on average
• nurses were working 200 to 300 over-contracted and overtime hours each month, showing they were routinely understaffed
• many nurses missed meal breaks, particularly on night duty, because of insufficient staff to provide relief.
“We made our case in numbers – language the health service understands.”
—Tomaree Branch Delegate Tracey Richardson
“When you care deeply about your patients and colleagues, you’re willing to give up your time to ensure patients receive the right care at the right facility and to maintain a safe workplace.”
The branch argued that the LHD needed to apply to the Health Ministry for more funding. As a result, the Ministry increased funding from six to 10 beds.
“We made our case in numbers – language the health service understands,” Tracey said.
“We got an extra night nurse, and bed numbers capped at 10 with two surge beds, as a result.”
Tracey said the extra staffing has had “a massive impact, specifically on night shift, especially around direct patient care and staff wellbeing”.
“However, we continue to face unsafe staffing levels on the ward for morning and afternoon shifts,” Tracey said.
“At full 12-bed capacity, each patient receives only 4.33 hours of nursing care in 24 hours – well below safe standards.
“While the ward isn’t classed as NHPPD, we’re demanding urgent action to increase nurse allocation to ensure a safe workload, reduce falls risk, and provide safe, quality care.”
The branch put patient admission criteria high on the USCC agenda.
“Patients were being admitted to the ward who were inappropriate for our staff to manage,” Tracey said.

“While the facility has some diagnostic and clinical services, these are limited, and our nurses and locum doctors do not have the specialised clinical skills required to safely care for complex patients. This puts both patients and staff at risk.
“Some patients experienced adverse outcomes because they were unable to access the specialist teams they required. These incidents prompted London Protocol reviews of critical events.”
The USCC tasked a team to write a new admission policy. The team included a clinical nurse specialist, clinical nurse educator, discharge planner, nursing unit manager, medical officers, and Tracey, who represented the branch.
“Every one of us had to review, research, and re-write a section of the policy,” she said.
“It was a complicated process that took about nine months of writing and meetings before a new set of admission protocols was accepted by the health service and USCC.
“Now, any time we are getting pushed to admit, we can refer to the policy and point out that this patient is outside of our admission criteria.
“If a patient is admitted outside policy, we record it in the incident system.
“Our admission criteria provide safeguards for patients and staff, but these can be bypassed when decisions are made offsite, overriding the clinical team on the floor who understand the patient’s clinical needs and our facility’s limitations.”
Tracey said the USCC experience has boosted members’ confidence in the union and strengthened their understanding of their rights to a safe workplace, while empowering them to advocate effectively for their patients.
“Members have a better understanding of the process they should follow if there is a staffing problem or a breach of the admission policy,” she said.
“Our staff have always put patient safety first. Now, they are also more likely to make a record of an incident and to let the union know what happened.”
“When you leave work, you want to switch off,” Tracey said. “But as a branch official, there’s a sense of pride when your team calls when you’re not on shift – seeking guidance that follows local health service and union policies.
“When you care deeply about your patients and colleagues, you’re willing to give up your time to ensure patients receive the right care at the right facility and to maintain a safe workplace.
“Megan and I might be the face and voice of the branch, but we are far from alone.
“We’re proud of our team and the commitment they show every day in providing excellent nursing care and taking union action to protect it.” n



Who should attend? Both new and existing members, delegates, and Branch Officials. This is an ideal starting point for new activists and a valuable opportunity for experienced members to reflect and strengthen their skills. Join us to build a foundation for meaningful union involvement and collective action.
Wednesday 25 February 2026, 9am – 4pm
Riverside Function Centre – Ballina RSL Club 1 Grant Street, Ballina NSW 2478
Cost: Members $95 / non-members $190 Lunch and refreshments provided
Speakers and topics:
This workshop explores the importance of the legal and ethical frameworks around communication and documentation that govern nursing and midwifery practice.

This workshop covers:
• ISBAR: Learn how it helps with providing comprehensive health communication;
• Unpack clinical handover and the exchange of information and what the responsibilities and accountabilities are for nurses and midwives;
• Understanding your obligations with professional standards in regards to documentation;
• The patient’s records and what is documentation to provide a full story;
• Report writing: Learn how to keep it simple but tell the whole story;
• Q&A.
A CPD Certificate will be provided to attendees at the end of the seminar.
Who should attend? Delegates, Member Leaders and Branch Officals seeking to enhance their confidence and capability in supporting members and resolving workplace issues. Through interactive discussions and practical exercises, you will refresh essential skills and explore real experiences of member representation.
Who should attend? Current and aspiring Branch Delegates who want to enhance their knowledge and engagement within the Association. You will gain a clear understanding of your responsibilities, the democratic processes within the Association, and the rules that guide your role. You will be equipped to actively contribute to our democratic structure.
This SafeWork NSW approved course aims to provide Health and Safety Representatives (HSRs) or deputy HSRs elected under the WHS Act with the knowledge and skills necessary to fulfil your role.
It provides:
• an understanding of the Work Health and Safety (WHS) legislation
• an understanding of how it applies to your role as an HSR or deputy HSR
• the knowledge and skills necessary to assist you to improve safety outcomes in your workplace.
Waterloo
9 – 13 February, 9am – 4.30pm
4 – 8 May, 9am – 4.30pm
17 – 21 August, 9am – 4.30pm
2 – 6 November, 9am – 4.30pm
This course is available to elected HSRs who have completed the 5-day SafeWork NSW approved HSR Training greater than 12 months prior.
Participants must provide evidence of completing the 5-day HSR Training by providing a copy of their original certificate.
It provides a refresher of:
• Understanding WHS legislation
• Understanding how it applies
• Knowledge and skills.
Waterloo
18 June, 9am – 4.30pm 16 October, 9am – 4.30pm
*WHS Act stipulates that HSR course fees are covered by the employer
Thursday 12 March 2026, 9am – 4pm
Cost: members $45 / non-members $60 associate student members $30
NSWNMA , 50 O’Dea Avenue, Waterloo NSW 2017
Join us for this interactive conference where you will learn about the prevalence of violence and aggression in our industry, hear about some practical measures being taken to mitigate the risks associated with violence and workshop processes and procedures to minimise violence in the workplace and manage its effects.
Hear from a range of professional speakers, workshops on speaking up and managing occupational violence incidents in the workplace
Who should attend? Any nurse or midwife interested in learning more about occupational violence and how violence should be managed when working in healthcare.
Event rescheduled from 30 October 2025.





There are two services providing free support to nurses, midwives and students in NSW. And the good news is they could both be right for you!
Getting support – there’s no wrong door
Support services designed specifically for nurses, midwives and students are available in Australia. But which one is right for you? The good news is that they both are. And that you can choose; the right service depends on what you need right now.
h2 Your support service options
Free and confidential, delivered by trained nurses and midwives, these services offer you a safe space to talk.
h3 Ongoing peer-to-peer support - Nurse Midwife Health Program
Australia (NMHPA)
If you want to talk things through and receive ongoing support, NMHPA may be right for you. Their peer-to-peer counselling and health support services are
delivered by experienced nurses and midwives who understand the realities of the profession.
NMHPA is independent from employers, Ahpra and universities. They are a safe, confidential place where you can talk openly.
NMHPA are available across Australia and offer continuity; you can build a connection with the same clinician over time. Support is available Monday to Friday, 9am to 5pm (local time), face-to-face over the phone or via telehealth.
h3 Need support right nowNurse & Midwife Support (NMS)
If you need to speak to someone straight away, NMS provides 24/7 national phone and email support. You can remain anonymous if you choose. Their team of nurses and midwives offer confidential brief intervention and referrals. NMS can also support you during an Ahpra notification, are launching a graduate mentorship program in 2026, and offer a wellbeing portal for self-guided care.
Nurses and midwives are used to coping. We push through double shifts, emotional load, ethical pressure and life outside of work. We tell ourselves, “Others have it worse,” or “I’ll be fine once things calm down.” But sometimes things don’t settle and coping alone can become difficult.
Reaching out for support isn’t a sign of weakness. It’s a professional strength and part of safe practice. Just like reflection or escalation, seeking support is essential to sustaining ourselves in this profession.n
Reaching out early can be a protective step – don’t have to wait until you’re not coping. One conversation can change things.
NMHPA
1800 001 060
www.nursemidwifehpa.org.au
NMS 1800 667 877
www.nmsupport.org.au
A responsible person as defined by the Aged Care Act
I am a nurse in charge of a shift in residential aged care, does this make me a responsible person under the new Aged Care Act from 1 November?
The new Aged Care Act, effective 1 November, does not change current obligations around the definition of a responsible person. A responsible person, as defined under the Aged Care Act 2024 is an individual with authority over, or significant influence over, a provider's planning, directing, or controlling activities, including those on a governing body or in senior management. These individuals have a statutory duty to exercise "due diligence" to ensure the provider complies with its legal obligations, such as maintaining safety and quality of care. They also have their own obligations, including following the Aged Care Code of Conduct and not threatening whistleblowers.
A responsible person is:
• a member of a registered provider’s governing body (such as a board member)
• an individual with executive decision-making authority
• someone who has authority, responsibility for, or significant influence over the planning directing or controlling of a provider’s activities
• an individual in charge of overall management, such as a director of nursing or nurse manager.
This change was made in response to union advocacy and ensures nurses who do not hold any kind of management positions (or are not in a position with the decision-making power to influence daily operations of a registered provider) are not inadvertently subject to obligations placed on responsible persons under the new Aged Care Act.
More information can be found here: www.health.gov.au/sites/ default/files/2025-07/new-agedcare-regulatory-modelfrequently-asked-questions.pdf
services and care minutes
I am a registered nurse providing on-call telehealth service to a group of residential aged care facilities in a rural area. I have heard this can count towards the facilities direct care minutes, is this correct?
Only direct on-site ‘clinical care’ and ‘personal care’ activities provided by specified workers (RNs, ENs or PCWs/AINs) can count as care minutes.
This means support provided through on-call and virtual telehealth arrangements cannot count towards care minutes targets.
There’s a regularly updated online guide produced by the federal government which outlines the latest advice about direct care minutes and RN 24/7 responsibilities that you can use to assist. You can access this this information via the Commonwealth Department of Health, Disability and Aged Care website. If you need more support, contact the union.
https://www.health.gov.au/ resources/publications/ care-minutes-and-247-registerednurse-responsibilities-guides-forresidential-aged-careproviders?language=en
Social support and care minutes
I work in aged care. Recently my employer has changed my role and I now provide some social support to my residents – both group and individual activities. Do these count as direct care for the care minute calculation?
Personal care services for the purpose of counting direct care
minutes include one-on-one social and emotional support activities if an individual receives direct support from an RN/EN or PCW/AIN as part of a group activity being held, or as an individual activity. Providing social activities to a group, such as a group bingo session does not count toward direct care minutes.
There’s a regularly updated online guide produced by the federal government which outlines the latest advice about direct care minutes and RN 24/7 responsibilities that you can use to assist. If you need more support, contact the union.
https://www.health.gov.au/ resources/publications/ care-minutes-and-247-registerednurse-responsibilities-guides-forresidential-aged-careproviders?language=en
Responsibilities of a prescribing RN
Now that prescribing has started for RNs what are my responsibilities if I choose to take up this endorsement?
If you’re endorsed as a prescribing RN, you carry important responsibilities to ensure safety and accountability. These include:
• prescribing only within your scope of practice and under a formal prescribing agreement with another authorised health practitioner
• working within a clinical governance framework that provides oversight and supports safe decision-making
• completing ongoing CPD specifically related to the prescribing of schedule medicines to keep your knowledge and skills current
• understanding the legal, ethical, and medicines/poisons responsibilities that apply in NSW.
With the added responsibility, it’s about practising safety –ethically, and collaboratively.
Endorsed RN prescribers must balance their expanded role with clear professional boundaries and continued learning, ensuring people in their care receive the safest and most effective care. You can read more about the new registration standard on the NMBA website: https://www. nursingmidwiferyboard.gov.au/ Registration-Standards/ Endorsement-for-scheduledmedicines-designated-RNprescriber.aspx
standards
The NMBA has announced a new prescribing standard for RNs. When will this start, and what does it actually mean for me as an RN?
From 30 September 2025, RNs who meet the Registration standard: Endorsement for scheduled medicines – designated registered nurse prescriber requirements are now able to apply for endorsement to obtain, possess, supply and prescribe Schedule 2, 3, 4, and 8 medicines. Prescribing must be done in partnership with an authorised
The Association’s professional team answers your questions about professional issues, your rights and responsibilities.
health practitioner, under a clinical governance framework, and with a prescribing agreement. This must be done in accordance with the relevant standards, guidelines, and applicable state and territory legislation.
You can read more about the new registration standard on the NMBA website.
https://www. nursingmidwiferyboard.gov.au/ Registration-Standards/ Endorsement-for-scheduledmedicines-designated-RNprescriber.aspx
Qualifications and experience needed to be an RN prescriber
If I want to apply to be an RN prescriber, what qualifications and experience do I need to have already completed?
To be eligible for this endorsement, you will:
• hold general registration as an RN with no conditions
• have completed an NMBAapproved postgraduate qualification (or equivalent)
It is with such sadness that we share the passing of Professor Deborah Hatcher, Dean of the School of Nursing and Midwifery at Western Sydney University. Deb passed away peacefully at home, surrounded by her family after a battle with illness.
A deeply respected leader, educator, and mentor, Deb dedicated 38 years of service to Western Sydney University and the nursing profession. Her visionary leadership helped shape the School of Nursing and Midwifery into the internationally recognised leader it is today. She will be remembered for her wit, strength, wisdom, and unwavering dedication to others. No matter how demanding her role, Deb always made time for people - offering guidance, encouragement, and genuine care to all who crossed her path.
Deb’s legacy lives on through the countless nurses, colleagues, and students she inspired, and through the compassion they bring to their communities every day. School of Nursing and Midwifery, Western Sydney University
that meets the Registered Nurse Prescribing Accreditation Standard
• have completed at least three years full-time equivalent clinical experience (5000 hours) in the past six years
• have demonstrated relevant clinical experience (assessed on context of practice)
• undertake the required sixmonth clinical mentorship with an authorised prescriber. You can read more about the new registration standard on the NMBA website. https://www. nursingmidwiferyboard.gov.au/ Registration-Standards/ Endorsement-for-scheduledmedicines-designated-RNprescriber.aspx

A new study published in the respected medical journal The Lancet has found that international sanctions “have substantial adverse effects on public health, with a death toll similar to wars”.
A large number of the deaths due to sanctions were attributed to malnutrition and decreased access to healthcare, with a disproportionate impact on children and the elderly, the report says.
The study, by US researchers, analysed the impact of sanctions on 152 countries between 1971 and 2021. Interestingly, the research found “the strongest effects for unilateral, economic and US sanctions whereas (we) found no statistical evidence of an effect for UN sanctions”.
The study attributed this to the widespread use of the US dollar and Euro in international finance and the extraterritorial application of sanctions.
The study “estimated that unilateral sanctions were associated with an annual toll of 564,258 deaths, similar to the global mortality burden associated with armed conflict”.
The study's central estimate found that unilateral sanctions imposed by the US and EU since 1970 are associated with 38 million deaths.
The deaths were not from direct violence, but were linked to factors like malnutrition, infectious disease and lack of access to medicine, which are consequences of economic hardship caused by sanctions.
Children and the elderly were the most vulnerable groups, with the study finding that over half of the victims were children and the elderly.
The household, income and labour dynamics in Australia (HILDA) survey gives fascinating insights into Australians’ lives.
Here are some of the results from this year’s report: Financial stress: There is plenty of evidence that many Australians are increasingly struggling to deal with the high cost of living, not least rising rents and the prices of other necessities.
One in eight people reported two or more indicators of financial stress in 2023 – the second-highest rate in nearly 20 years.
Stress indicators include not being able to pay utilities or mortgage or rent on time, skipping meals, being unable to heat the home, or having asked for financial help from friends, family or welfare organisations.
Childcare costs: The average family is spending $171 a week on childcare, or nearly $100 more than two decades ago – a 40 per cent increase.
Fewer children: Australia’s total fertility rate, or the average number of children a woman will have in her lifetime, dropped to a record low of 1.5 in 2023 –down from 2.02 in 2008.
Retiring older: In 2003, 70 per cent of women and 49 per cent of men aged 60–64 were retired. But by 2023, these figures had dropped to 40 per cent and 27 per cent, respectively, the survey showed.

“We estimated that unilateral sanctions were associated with an annual toll of 564,258 deaths, similar to the global mortality burden associated with armed conflict.”
“There is plenty of evidence that many Australians are increasingly struggling to deal with the high cost of living.”
Millions of lower-income workers in Australia are set to benefit from proposed superannuation changes, primarily through an increase in the Low-Income Superannuation Tax Offset (LISTO).
Starting 1 July 2027, the eligibility threshold for LISTO will rise from $37,000 to $45,000 a year, and the maximum tax offset will increase from $500 to $810.
The Treasury says the reform will help deliver a more secure retirement for 1.3 million Australians, of which about 60 per cent are women, with the total number of Australians becoming eligible for LISTO increasing to 3.1 million.
It will benefit workers with incomes between $28,000 and $45,000, with an average increase in the LISTO payment of $410.
According to Super Members Council modelling, the changes could mean some lifetime low-paid workers could have up to $60,000 more in their super savings by retirement.
The ACTU welcomed the changes to LISTO, which it says was designed to ensure workers on low income paid less tax on their super than they did on their take-home pay, however, hadn’t been adjusted to keep up with the rest of the tax system.
“Super has always been about everyone having a dignified retirement, not a tax minimisation scheme for the ultra-wealthy,” Secretary Sally McManus says.
Super fund HESTA said the important equity measure was a significant step forward in addressing the gender super gap.

“Super has always been about everyone having a dignified retirement, not a tax minimisation scheme for the ultra-wealthy.”— ACTU secretary Sally McManus
Civilian injuries in Gaza similar to those of soldiers in war
Civilians in Gaza have sustained injuries of a type and on a scale more usually seen among professional soldiers involved in intense combat operations.
Research published in the British Medical Journal – based on the type of injuries observed by international healthcare workers during the conflict in Gaza – found that wounds such as burns or leg injuries are more common in Gaza than among US soldiers who fought in Iraq and Afghanistan.
“Injured civilians in Gaza are experiencing a pattern of wounds that you would expect in intense combat with military professionals. The distribution and nature [of injuries] is almost the same or worse,” Bilal Irfan, one of the study’s authors, told The Guardian.
Irfan said the data did not include most fatal injuries. “This is data for the patients who made it to hospital and so survived. We don’t even have a full profile of the serious injuries of those who died without any medical attention,” he said.
Overall, almost 24,000 trauma-related injuries were reported in the study, of which 18 per cent were burns. About two-thirds of injuries were from explosions.
Burns were particularly common and severe, in particular among children, the authors found. More than 10 per cent of burn injuries were fourth degree, meaning they penetrated all tissue layers down to the bone.
The extent of traumatic injury victims reflects “the impact of indiscriminate aerial and heavy explosive bombardment in civilian areas”, the study said.
Almost 24,000 traumarelated injuries were reported in the study, of which 18 per cent were burns. About two-thirds of injuries were from explosions.

American nurses and midwives fear the future of an already vulnerable health system as the Trump administration slashes funding.
President Trump’s budget bill – the so-called One Big Beautiful Bill Act – included a raft of reductions and restructures to healthcare funding in the US.
This includes cuts to funding for schemes which encourage prospective students into nursing courses at university through loan repayment support.
“Cutting hundreds of millions of dollars that support nurse faculties, nursing students and nurses in loan repayment areas is detrimental. If we don’t get it back, it could have a decades-long impact on the number of nurses [we have],”
Dr Jennifer Kennedy, president of the American Nurses Association told Nursing Times.
The administration also announced deep cuts in its budget to Medicaid, the country’s public health insurance system.
Dr Kennedy said the cuts to Medicaid – which is predominantly used by older people and those on low incomes – could have a severe impact on both the nursing workforce and the general public.
“This bill will make care unreachable for many and add even more pressure on an already overburdened nursing workforce.”
She warned that cuts to Medicaid did not only impact the ability for an American to receive healthcare – it would also lead to hospital closures and job losses for nurses.
“This bill will make care unreachable for many and add even more pressure on an already overburdened nursing workforce.”
— Dr Jennifer Kennedy, president of the American Nurses Association
It’s never been a better time to be a billionaire, reports anti-poverty agency Oxfam.
Billionaire wealth has risen three times faster in 2024 than 2023, according to a study by Oxfam. Five trillionaires are now expected within a decade.
Trillions are being gifted in inheritance, “creating a new aristocratic oligarchy that has immense power in our politics and our economy”, the report found.
Meanwhile, the number of people living under the World Bank poverty line of US$6.85 today is the same as it was in 1990: almost 3.6 billion people. This represents 44 per cent of humanity. Meanwhile, the richest 1 per cent own almost an identical proportion – 45 per cent of all wealth.
Most billionaire wealth is taken, not earned - 60 per cent comes from either inheritance, cronyism and corruption or monopoly power, the study says.
Oxfam calculates that:
• 36 per cent of billionaire wealth is derived from inheritance
• 6 per cent is from crony sources
• 8 per cent is from monopoly power.
The report also highlights wealth transfers not just to the ultra-rich, but disproportionately to the ultra-rich in the Global North.
“Ours is the age of billionaire colonialism. Unchecked, we are about to see the biggest transfer of the largest generational wealth in human history handed over – hardly earned, hardly taxed,” it claims.
“Most billionaire wealth is taken, not earned - 60 per cent comes from either inheritance, cronyism and corruption or monopoly power,”

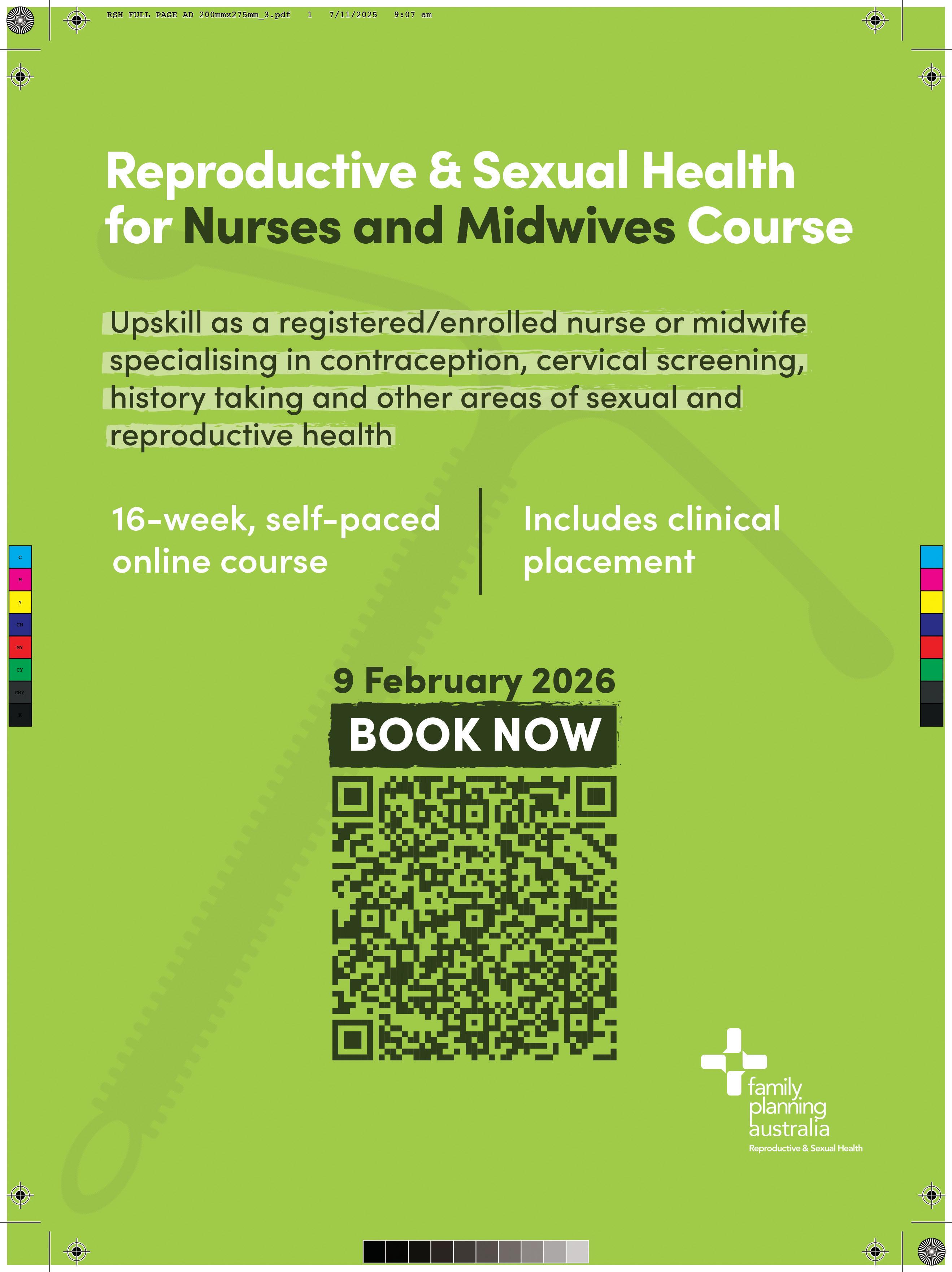



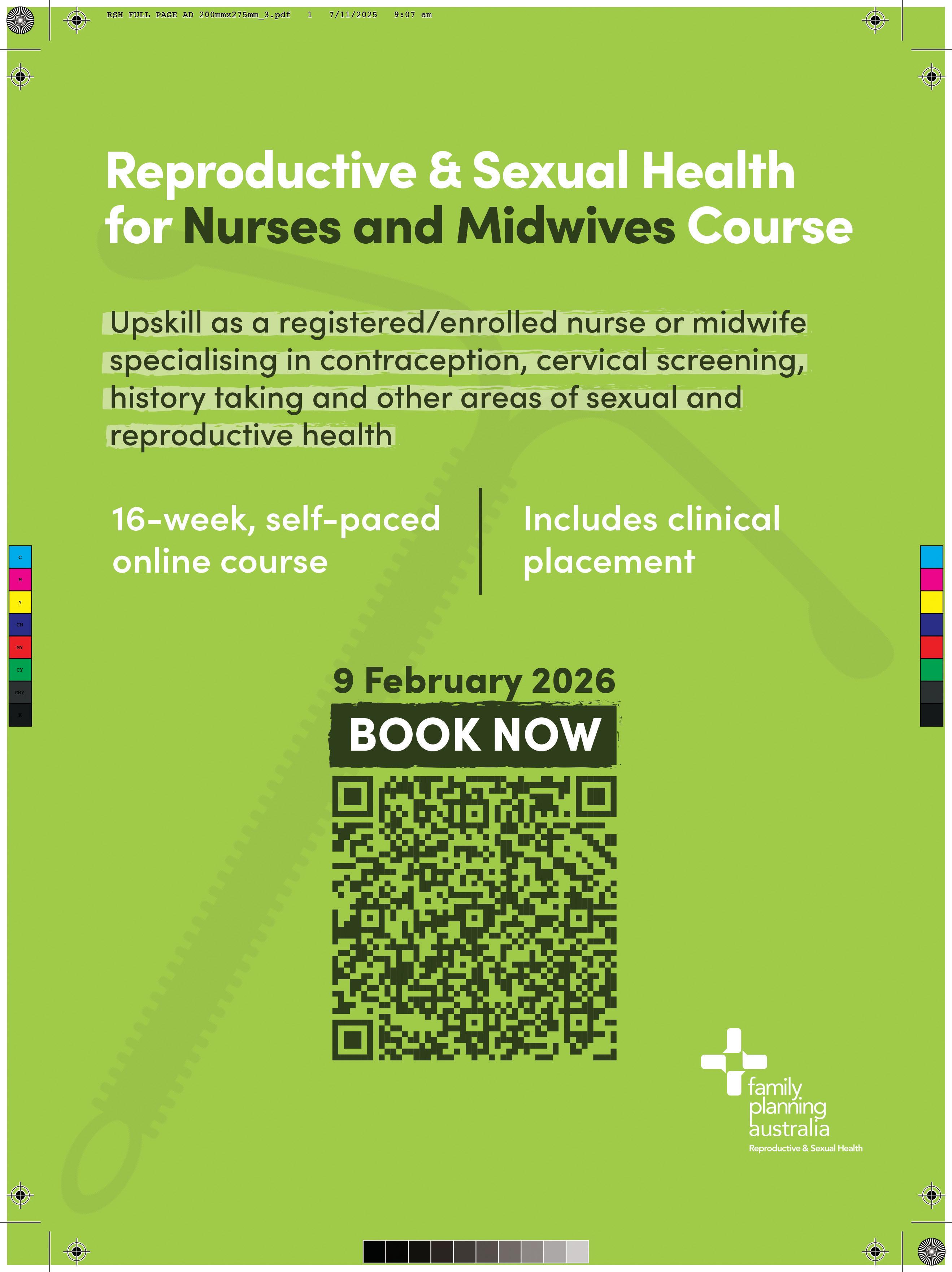


ACROSS
1 Machine that records brain waves (21)
12 Resembling cells that form the covering of all internal and external surfaces of the body (11)
17 Having eight cells (11)
19 Through unbroken skin (11)
23 Symbol for radium (2)
24 Functional group in aspirin (11)
27 A small travelling bag (11)
28 A dilated lymph space (5)
29 X Unit (1.1)
30 A unit of radioactivity (1.1.1)
32 Sensitivity to stimuli originating outside of the body (13)
36 Symbol for tantalum (2)
38 A blood disorder (1.1)
39 A nursing qualification (1.1)
41 The basis of locomotion in vertebrates, body’s framework (15.6)
45 Towards, upon (2)
46 Fireflies (10)
49 Bones (4)
53 Arterial Hypertension (1.1)
54 Nutrient that fights free radicals (11)
55 Without glands (11)
57 Intrathecal (1.1)
58 Hospital's critical care section (1.1.1)
59 In its original place (2.4)
60 Immersed, engrossed (11)
63 A crib (3)
64 Drying up, vaporising (11)
67 Common medication for high blood pressure (10)
71 Ethinyl Estradiol (1.1)
72 The symbol for aluminum (2)
73 Neck vessel (8.13)
DOWN
1 Galvanic skin response (13.8)
2 Vapes (11)
3 Total Laparoscopic Hysterectomy (1.1.1)
4 Lubricating liquid (3)
5 New (3)
6 Situated or occurring within the heart (11)
7 Estrus (4)
8 Lupus erythematosus (1.1)
9 Animal starch (8)
10 Condition of stunted growth with normal body proportions (9)
11 Arthroplasty (3.11.7)
13 Pregnancy due date (1.1.1)
14 Isoflavone reductase (1.1.1)
16 The outer portion of an organ (6)
18 Blueprint, design (6)
20 Echolocation (5)
21 Cellular transit hub between the ER and Golgi (1.1.1.1.1)
22 Multifocal atrial tachycardia (1.1.1)
26 Lethal dose (1.1)
31 Thorax (5)
33 A congenital gap in the cranium with herniation of brain substance (13)
34 Petroleum extraction (3.10)
35 Lessen pain or discomfort; alleviated (5)
37 Any anatomic structure in the form of a loop or an arc (4)
40 Ankle bones (5)
42 Oculus (3)
43 A coding part of a gene (4)
44 Family of viruses that includes rubella (5)
47 A disease or disorder (3)
48 Deprivation of possession (7)
50 Thyroid enlargements (7)
51 Acute occlusive thrombosis (1.1.1)
52 Spleen (4)
54 Apart (5)
56 Labium (3)
61 Cause of death (1.1.1)
62 Not fluid or gaseous; not hollow (5)
65 A vote that blocks a decision (4)
66 A seaweed extract (4)
68 The adipose tissue of the body (3)
69 Sick (3)
70 A period of time (3)






We want to wish you and your loved ones a happy and safe festive season. It’s been an eventful year, from launching a major special case in the public health system, widespread bargaining campaigns in the private sector, and more historic wage increases in aged care. In 2026 we’ll continue with the same determination to achieve real change for our members.

NSWNMA offices will be closed 25 December 2025 – 1 January 2026 inclusive. If you require urgent assistance during this time, please call the office during business hours on 27, 30, or 31 December and the message will detail the options available to you. Our office number is 1300 367 926











