TINY LIVES DESERVE SAFE CARE

Contacts
NSW Nurses and Midwives’ Association
For all membership enquiries and assistance, including The Lamp subscriptions and change of address, contact our Sydney office.
Sydney Office
50 O’Dea Avenue, Waterloo NSW 2017 (all correspondence)
T 8595 1234 (metro) 1300 367 962 (non-metro)
F 9662 1414 E gensec@nswnma.asn.au
W www.nswnma.asn.au
Hunter Office
8–14 Telford Street, Newcastle East NSW 2300
NSWNMA Communications Manager
Danielle Blasutto
T 02 8595 1234 (metro) T 1300 367 962 (regional)
For all editorial enquiries, letters and diary dates
T 8595 1234 E lamp@nswnma.asn.au
50 O’Dea Avenue, Waterloo NSW 2017
Produced by
Hester Communications T 0414 550 376
Press Releases
Send your press releases to: F 9662 1414 E gensec@nswnma.asn.au
Editorial Committee
Shaye Candish, NSWNMA General Secretary
Michael Whaites, NSWNMA Assistant General Secretary O’Bray Smith, NSWNMA President
Michelle Cashman, Long Jetty Continuing Care
Michelle Cutler, Tweed Hospital
Karen Hart, Wagga Wagga Base Hospital
Robyne Brown, Maitland Hospital
Printed by
Printed by IVE Group Sydney
Advertising
T 8595 2139 E nswnursescomms@nswnma.asn.au
Information & Records Management Centre
To find archived articles from The Lamp, or to borrow from the NSWNMA nursing and health collection, contact: Adrian Hayward, Coordinator. T 8595 2175 E gensec@nswnma.asn.au
The Lamp ISSN: 0047-3936
General Disclaimer
The Lamp is the official magazine of the NSWNMA. Views expressed in articles are contributors’ own and not necessarily those of the NSWNMA. Statements of fact are believed to be true, but no legal responsibility is accepted for them. All material appearing in The Lamp is covered by copyright and may not be reproduced without prior written permission. The NSWNMA takes no responsibility for the advertising appearing herein and it does not necessarily endorse any products advertised.
Authorised by S. Candish, General Secretary, NSW Nurses and Midwives’ Association, 50 O’Dea Avenue Waterloo NSW 2017
Privacy Statement
The NSWNMA collects personal information from members in order to perform our role of representing their industrial and professional interests. We place great emphasis on maintaining and enhancing the privacy and security of your personal information. Personal information is protected under law and can only be released to someone else where the law requires or where you give permission. If you have concerns about your personal information, please contact the NSWNMA office. If you are still not satisfied that your privacy is being maintained, you can contact the Privacy Commission.
Subscriptions for 2025
Free to all Association members. Professional members can subscribe to the magazine at a reduced rate of $30. Individuals $84, Institutions $140, Overseas $150
VOLUME 82 NO. 4
AUGUST / SEPTEMBER 2025

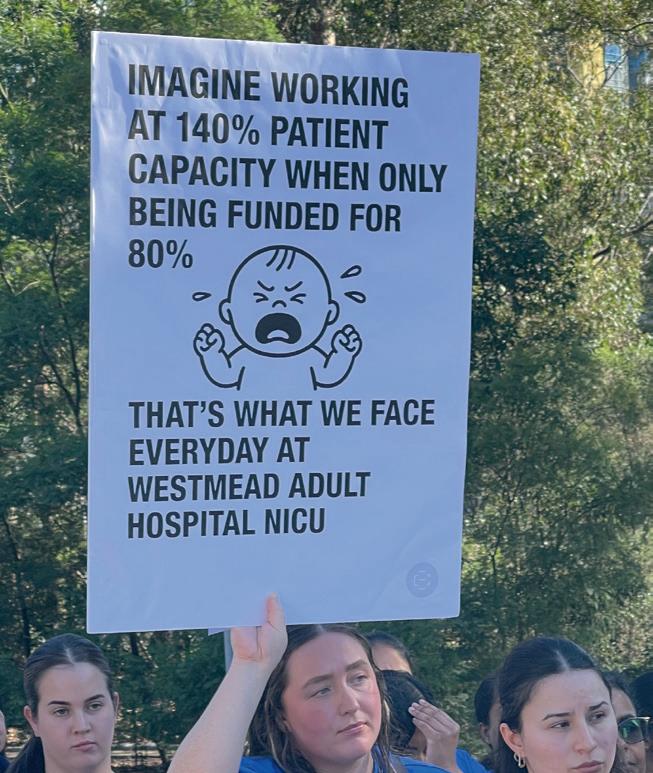
COVER STORY Action wins staffing boost for Western Sydney Public pressure and lobbying by NSWNMA members has won a commitment to boost staffing at Westmead Hospital’s Neonatal Intensive Care Unit.
10 COVER STORY
Tiny lives deserve safe care
Nurses warn of severe understaffing at Western Sydney neonatal intensive care unit.
12 HEALTHSCOPE
Unions and governments seek stability during Healthscope’s administration
The interests of patients and staff are paramount in the period leading to the sale of the troubled company.
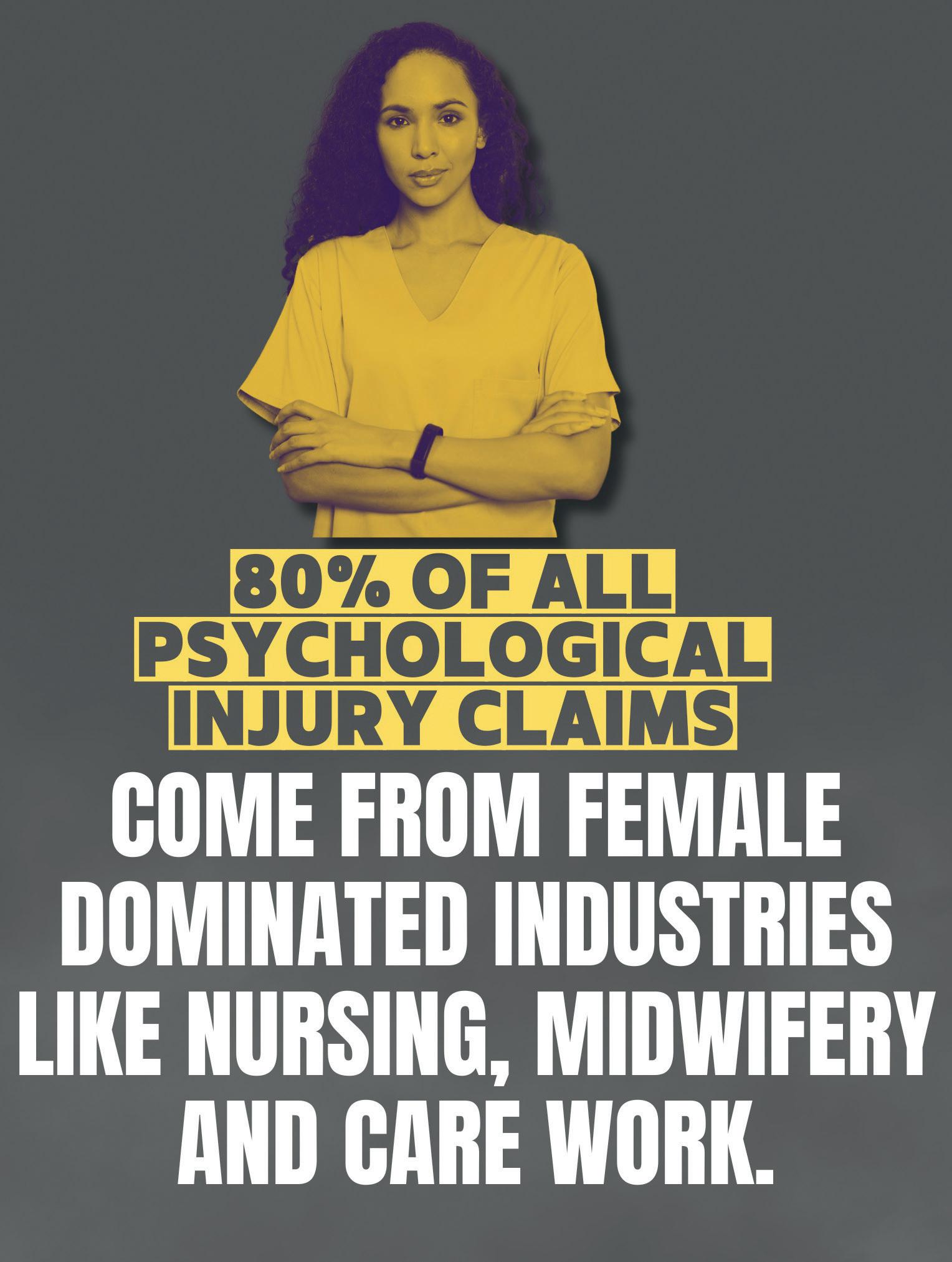
18 WORKERS COMP
Compo ‘reform’ would hit women hardest
The Minns government’s proposed ‘reform’ to workers compensation would drastically curtail the ability of psychologically injured workers to access long-term payments
22 IR LAWS
Union-backed laws seek pay justice for ‘women’s work’, combat bullying and sexual harassment
The Minns government should look at what causes so many psychological injuries in the health service rather than making it harder for staff to access workers compensation.
25 RECONCILIATION
Working towards Closing the Gap
Like many organisations around the country, the union is developing a Reconciliation Action Plan as a practical and structured approach to reconciliation.
COVER : Jessica Charlston and Alicia Rodgers Photographed by Sharon Hickey

Candish
GENERAL SECRETARY
A big step forward to improve the working lives of women in NSW
New laws address gender inequality and undervaluation of work in a significant way.
It has been described as the “most significant increase in industrial rights in NSW in over 30 years” (see p22).
New amendments to the NSW IR Act are good news for NSW workers, especially those working in female dominated sectors like nursing and midwifery.
In the federal IR system, we have seen how the Fair Work Commission has been able to grant substantial wage increases to aged care workers in order to redress historic undervaluation of work in the sector.
New amendments to the NSW IR Act give us the potential to pursue similar cases in the NSW IR system which could benefit members in the Public Health System.
Currently, we are pursuing a 35 per cent pay rise over three years via a special case in the NSW Industrial Relations Commission. These new laws will strengthen one of our principal arguments: there needs to be a correction of the gender-based undervaluing of nursing and midwifery in NSW.
A new object of the Act will be to achieve gender equality in the workplace and in particular, to “ensure equal renumeration for men and women doing work of equal or comparable value and to eliminate gender-based undervaluation of work”.
There are also improvements to prevent and eliminate discrimination, bullying and sexual harassment with strong sanctions including damages of up to $100,000 to be awarded in such cases. There are also important improvements to Workplace Health and Safety which will aim to strengthen compliance and enforcement and give unions significant new powers and influence.
The Association has been championing these changes for some time along with our colleagues at the Teachers’ Federation. We have garnered support across the union movement and have
New amendments to the NSW IR Act are good news for NSW workers, especially those working in female dominated sectors like nursing and midwifery.
been able to convince key government figures including the Premier, the Treasurer and the Minister for Industrial Relations. There has also been solid support from the crossbenchers.
The State government’s track record on reducing the gender pay gap has, up to now, been less than stellar but these new laws have real teeth and will give the Association fresh avenues to pursue pay claims that would address the historical anomalies.
NICU MEMBERS FIND THEIR POWER
Congratulations to our members working in Neonatal Intensive Care Units in Western Sydney (see p8).
Their crowded and critically understaffed units were at a tipping point until members took things into their own hands and initiated action on behalf of their vulnerable patients.
At Westmead babies were often “double parked” or “triple parked” – two or three babies to a bed space – even within a converted cupboard, a totally unacceptable clinical situation.
The staff response was decisive, inspirational and effective in defence of their voiceless patients.
Branches at Westmead and Nepean held rallies in their own time and lobbied Western Sydney MPs for improved funding and more staff to improve safety.
Initially, the response of those MPs was disappointing. They trotted out the same old mantra the Association has been hearing for the last two years – “There is no money”.
But pressure works. The media coverage our branches generated garnered the community support needed to bring the government to its senses and to allocate more funding, at least for a start at Westmead.
For our NICU members it is a reminder that the community values them and will listen to their analysis of what is happening at the frontline. The government needs to do the same.
SUPPORT IN A TIME OF UNCERTAINTY
The failure of the private equity model in health implemented by Healthscope was both predictable and avoidable.
But all that matters at this moment is protecting the interests of patients and staff as the administrators prepare the company for sale (see p12).
This can and should be done in an orderly way that maintains the stability of the company’s hospitals, allows staff to deliver their high-quality care as they always do and for patients to be well looked after as they deserve.
The administrators say there are adequate funds within the company to maintain this stability and the federal government has been unequivocal in prioritising the interests of patients and hard-working staff.
The NSWNMA and the ANMF have been active and vigilant to give our Healthscope members a voice with the company, the state and federal governments and the administrators during this difficult period.
It’s a difficult time but we are rock solid behind you to help you get through it.n SHAYE

Have your Say
Featured Letter
A rewarding job, but emotionally devastating
I work with children battling cancer. The job is incredibly rewarding, but also emotionally devastating.
The work is a constant balancing act of delivering lifesaving care, managing the workload and stress, and trying to preserve my own well-being along the way. I value the privilege of working with sick children and their families during the toughest time of their lives.
The emotional toll nursing takes is incalculable. It is devastating to see that a child has relapsed or has passed away, but that is the daily reality of my work.
I often feel burnt out and tired, and this feeling is compounded by the knowledge that my empathy and dedication to the nursing profession are being exploited because I am not compensated fairly for what I do.
I have seen many of my colleagues leave the profession entirely or migrate to other states where conditions and pay are more reasonable.
Why should nurses and midwives be forced to choose between fair pay and safe staffing levels?
We are worth the investment; the (government) knows it, and the community knows it, too. But this government continues to refuse to sit down and resolve our claim with us directly. And I, for one, am sick of the cowardice of our elected representatives on Macquarie Street.
Charley Hirst, Registered Nurse, Sydney Children’s Hospital
Speaking truth to Allegra Spender
I am writing this letter following a meeting between NSWNMA private hospital members and Member for Wentworth, Allegra Spender.
It was amazing to have a politician so eager to hear from nurses and learn more about the struggles we face when it comes to securing minimum safe staffing ratios in private hospitals.
I spoke about my experience working at both St Vincent’s Public Hospital with no ratios and then moving to St Vincent’s Private which won some ratios in their EBA agreement. I spoke about what a difference it makes.
In the public system, the burden constantly falls on the nursing staff to compensate for the unreasonable workloads, increased patient load and acuity.
At St Vincent’s Private I witnessed and experienced the benefits of ratios: more staff on of the floor per patient, improved staff morale, improved staff safety and of course achieving the ultimate goal: improved patient safety. The other issue I raised was housing affordability for nurses. Working in the inner city of Sydney in one of the most affluent electorates in Australia, for which Ms Spender is the MP, one thing has also become clear to me: not only
Featured Letter
it is impossible to live near my work, but it is also impossible for me to live in Sydney at all.
I told this to Allegra Spender, that sadly I am another nurse on the way out, due to low pay.
Jack Fullerton, Registered Nurse, NSWNMA St Vincent’s Private Branch
Speaking out Is an empowering experience
At Westmead we have a problem: too many babies with not enough space or staff to care for them. The branch raised concerns locally on many levels but our calls for support for the littlest patients, continue to fall on deaf ears.
As a branch, we invited local Western Sydney MPs to come and hear our story.
Only one MP accepted the invitation and attended. We then brought our stories to the MPs who didn’t show up, attending NSW Parliament House, but it still fell on deaf ears, so we made the decision to go public.
On 24 June, we rallied outside our workplace, attracting media attention and spreading the word about the crisis in our NICU. Standing together and speaking out was an empowering experience.
Following media scrutiny, our branch was invited back to Parliament House, this time to meet with the Minister
If there’s something on your mind, send us a letter and have your say. You could
for Health, Ryan Park and our Local Health District Chief Executive.
As a result of the meeting, we have had a commitment to fast track the advertising for the current vacancies and approval to increase our staffing profile.
As I write this, the state has run out of neonatal intensive care beds, with all funded beds occupied and several units well over their capacity. Westmead NICU currently has 30 babies requiring intensive care with only 24 beds. This math doesn’t work. NSW urgently needs investment in its neonatal services. Because the smallest and sickest patients deserve better.
Jessica
Charlston, RN, Westmead NSWNMA Branch
Prac payment is crucial to retaining students
I am a recent graduate of a Bachelor of Nursing program and active participant in the recent NSWNMA campaign ‘End Placement Poverty’, which resulted in the government’s introduction of the Commonwealth Prac Payment (CPP) for nursing and midwifery, teaching and social work students.
We had over 8000 students sign the NSWNMA petition to end placement poverty.
I wanted to share my thoughts now that eligible students can apply.
The CPP, providing $331.65 per week to eligible students on clinical placements, is a direct response to campaign pressure from students and union members demanding fair recognition of the burdensome costs associated with undertaking unpaid placement for weeks at a time.
All nursing and midwifery students on placement work full-time hours without pay, often traveling long distances, paying out of pocket for transport, parking, accommodation, uniforms, and more. Many have no choice but to reduce paid work or forego it entirely. This immense financial pressure is driving capable, passionate students out of the profession before they even graduate.
In a profession that has seen a mass exodus of skilled professionals in recent years, it is crucial we retain the students we recruit.
Angelique Dumas, New Grad, Sutherland Hospital
Advertise in The Lamp and reach more than 80,000 nurses and midwives.
To advertise contact 02 8595 2139 nswnursescomms@nswnma. asn.au

Action wins staffing boost for Western Sydney
Public pressure and lobbying by NSWNMA members has won a commitment to boost staffing at Westmead Hospital’s Neonatal Intensive Care Unit.
The NSW Health Ministry has agreed to fund a significant increase to nursing staff at Westmead Hospital’s Neonatal Intensive Care Unit in Western Sydney Local Health District.
This follows a rally by NSWNMA members outside the hospital which drew public attention to the NICU’s desperate shortage of nurses.
Westmead NICU is the only Level 6 referral unit in metropolitan Sydney apart from the Royal Hospital for Women NICU in Randwick.
During their own-time rally outside the hospital, Westmead NICU nurses called on Health Minister Ryan Park to urgently intervene with increased funding to employ more nurses.
NSWNMA Assistant General Secretary, Michael Whaites, told the media that members had been raising the staffing issue with hospital management and Western Sydney Local Health District on a weekly basis “but their repeated calls for help have gone unanswered.”
“The NICU is funded for 44 beds, but it regularly must open up to 50 beds or more due to the demand from surrounding Western Sydney hospitals, or the babies requiring cardiac care from the Children’s Hospital next door,” Michael said.

“We often have to put two or three babies in one bed spot, which has oxygen and other equipment designed for one baby.” — Jessica Charlston, NSWNMA Westmead Hospital branch
“The unit is currently staffed for 80 per cent capacity but has been surging to 130-140 per cent thanks to a sharp increase in acuity of babies needing critical care.”
Earlier, a delegation of Westmead NICU nurses appealed to western Sydney MPs for help at meeting in parliament house.
The MPs were Edmond Atalla (Mount Druitt), Stephen Bali (Blacktown), Lynda Voltz (Auburn), and Dr Michael Holland as Parliamentary Secretary for Health.
MP for Parramatta, Donna Davis, was invited but did not attend.

WESTERN SYDNEY LHD AND THE CHILDREN'S HOSPITAL AT WESTMEAD DELEGATION TO PARLIAMENT
“We are getting more and more babies and more of those are needing 1:1 care.” —
Jessica Charlston
DEMAND HAS INCREASED
NSWNMA member Jessica Charlston said the delegation of members were very disappointed in the MPs’ response to nurses’ pleas for more funding.
“Westmead is a major referral hospital and the NICU staff shortage is an issue for the entire Western Sydney LHD,” she said.
“We look after babies from all over the district including Blacktown and Auburn hospitals, and those from outside the district needing the specialist services of Westmead Hospital.
“We suggested to the MPs that the government provide additional funding to allow Blacktown Hospital to open up and staff spare bed spaces.
“That would allow us to backtransfer babies to Blacktown and for Blacktown to look after more of their own babies instead of sending them to us.
“The MPs basically said there is no more money and we will have to make do with our current funding.”
Speaking before the Ministry’s commitment to fund more nurse positions, Jessica said the staff shortage was the worst she had experienced since she started at the NICU as a casual in 2008.
“The population of western Sydney has increased a lot since the current NICU was opened in June 2007.
“We are getting more and more babies and more of those are needing 1:1 care, yet our nursing numbers have stayed the same.
“Staff are working under extreme pressure, the mood of the unit has deteriorated and people are no longer enjoying the work.
“We often have to put two or three babies in one bed spot, which has oxygen and other equipment designed for one baby.
“We even have to put two babies in the resuscitation room, which is a converted cupboard where we used to store our resuscitation equipment.
“It was never designed for ongoing care for babies. It gets very crowded and has no windows.
“When you have two babies in incubators with the monitors and other equipment you need, plus the clinical staff, there isn’t even room for parents at the bedside.”n

What Westmead nurses gained for western suburbs
The NSW Health Ministry agreed to fund significant improvements to NICU staffing in Western Sydney in July.
The Ministry agreed to:
• advertise to fill current vacant positions in the Westmead NICU
• expand the Westmead NICU staffing profile by another 15 full-timeequivalent nurses on every shift and to advertise for those positions. Westmead NICU would then be adequately staffed providing it is not over-capacity
• allocate $50 million to build a new NICU at Westmead to replace the current facility which has operated for 17 years
• consider additional funding for Blacktown Hospital’s Newborn Care Unit in order to open surge beds when Westmead NICU is at full capacity
• raise the status of the newborn special care unit in the future Rouse Hill Hospital also in the Western Sydney LHD from Level 2 to Level 3. Rouse Hill Hospital is in the planning stages. n
Critically ill babies ‘double parked’
At Westmead Hospital’s Neonatal Intensive Care Unit (NICU), critically ill and/or premature babies often have to be ‘double parked’ in one bed space.
Babies requiring 1:1 or 1:2 nursing care may even be ‘triple parked’ under the care of a single nurse who might be working a double shift.
“We only have 44 bed spots but often have up to 50 babies or more,” said NSWNMA member Emily, who asked that her last name be withheld for personal reasons.
“It’s not uncommon for nurses to have to work from 1.30 in the afternoon to 7 the next morning,” she added.
“When we are full, we don’t have anywhere else to send a baby –and when we’re full, more babies keep coming to us.”
Emily was speaking before the Health Ministry’s commitment of additional funding for Westmead NICU, which followed media publicity generated by the NSWNMA’s push for more staff for the neonatal unit.
Emily works at the NICU as a casual, which used to mean she wasn’t rostered on any shifts and would only be called upon to plug gaps. Now, she is on a Monday to Friday roster and is asked to extend her 8-hour shift to a 12-hour shift every time.
“I could work seven days a week and pick up any shift I wanted. It’s not overtime pay because I’m casual but a lot of staff are on overtime. Sometimes four to seven nurses are on overtime each shift.”
THE WEST’S POPULATION HAS GROWN
She said the NICU is funded for 44 beds and has been at 44 or above for at least a year.
“We are staffed on 80 per cent capacity and the roster is capped at 21 nurses per shift, though we need 24 to 26 per shift.
“However, when Monday comes along, we might have one or two nurses sick leave and then we’re down to 19 or 20.
“When we are full, we don't have anywhere else to send a baby – and when we’re full, more babies keep coming to us.
“The government needs to invest in neonatal services in western Sydney as the population has grown and continues to grow.
“We are currently unable to safely meet the demands of our community.
“We are led to believe that one in four dollars of the state budget is spent on health but clearly it is not being spent where it is needed. It’s not being spent on the front line.”n

Tiny lives deserve safe care
Nurses warn of severe understaffing at Western Sydney neonatal intensive care unit.
Tiny lives deserve safe care was the theme of a rally by nurses at Nepean Hospital’s Neonatal Intensive Care Unit (NICU), which cares for some of the state’s sickest babies.
The rally called for more staff to ensure safe staff to patient ratios for sick and preterm babies.
Nepean Hospital is located at Kingswood in western Sydney and its NICU receives sick babies from all over NSW.
The hospital’s NSWNMA branch organised the protest, which members attended in their own time. Some came into the rally on their day off while others had just finished a long shift.
As of July 2025, the hospital was funded for 38 beds in the NICU. They included 25 special care nursery beds and 13 intensive care beds.
However, patient numbers often exceed funded bed capacity.
“These are the most vulnerable patients in the health system – tiny, sick and pre-term babies who don't have a voice and are reliant on their caregivers for all their daily needs," said Branch Secretary and Delegate Alicia Rodgers.
“Often, they're as sick as adult intensive care patients, but they don’t get the same level of safe staffing as their adult counterparts.

“These are the most vulnerable patients in the health system –tiny, sick and pre-term babies who don’t have a voice.” — Alicia Rodgers, NSWNMA Nepean Hospital branch
“The state government has agreed to roll out minimum staffing ratios of one-to-one care to adult ICUs but not NICUs.

“At Nepean NICU we absolutely strive to give our sickest babies 1 to 1 care. However, staff and/or patient numbers don’t always guarantee that level of care.
“We are seeking a government commitment so that its guaranteed that we can nurse the most critically ill patients on a one-to-one basis.”
FAMILIES NEED CARE TOO
Alicia said NICU patients receive similar levels of medical care as adult ICU patients and have additional needs such as neurodevelopmental care for very pre-term babies.
“We also provide care to entire families; for example, we support them to care for their preterm babies and we provide breastfeeding support,” she said.
“In order to meet these demands, we desperately need more staff to stop the reliance on overtime, extra shifts and deployed staff from other units.
“Constantly surging beyond our funded intensive care beds and our overall bed capacity within the NICU and special care nursery really stretches our ability to be able to provide the safest and most effective care to our most vulnerable patients.
“The neonatal unit is funded for 38 beds but we sometimes surge up to 43 beds. We might have between 14 to 16 staff on the floor for that many patients.”
Alicia said nurses enthusiastically supported the Nepean Hospital rally and hoped that a government promise to increase staffing at Westmead NICU would lead to a similar commitment for Nepean NICU.
“There is a real sense of anticipation at Nepean as to what our action might be able to achieve for us given the result at Westmead.”n
Unions and governments seek stability during Healthscope’s administration
The interests of patients and staff are paramount in the period leading to the sale of the troubled company.
The NSWNMA and the ANMF have been in regular contact with Healthscope management and the NSW and federal governments to advocate on behalf of our members since the private hospital operator's parent companies went into receivership, says NSWNMA General Secretary Shaye Candish.
“We’ve spoken with the state government about the potential impact on the publicprivate partnership at Northern Beaches Hospital.
“Separately, we have also held talks with the federal health minister, Mark Butler. He has told Healthscope administrators they must do the right thing by the community, nurses and midwives. We welcome this support,” she said
“We will continue to hold regular meetings with the federal health minister during this process. We’re also coordinating our efforts on behalf of nurses and midwives with other unions representing non-nursing/midwifery employees as part of an Australian Council of Trade Unions affiliates group, and this is central to our advocacy efforts.”
Healthscope's parent companies went into receivership on May 26 after accumulating $1.6 billion in debt and defaulting on its lease payments.
“This is the outcome of a series of poor financial decisions by the previous owners, Brookfield. Instead of investing in the company to ensure it could provide quality patient care for the community in the long-term, Brookfield decided to strip Healthscope of its key assets by selling off its hospitals and entering lease agreements with the new owners,” Shaye said.
“This is a typical strategy that private equity firms like Brookfield use when ‘investing’ in healthcare – they want to secure short-term gains for their investors.”
Shaye said the union was focussed on supporting our members during this uncertain time.
It had prepared resources to answer members’ numerous questions, had conducted several webinars and had prepared services for members to access if they were anxious or stressed by the insecurity surrounding the company.
Federal Health Minister Mark Butler said the company had adequate funds to maintain operations during the administration process leading to a sale and he expected “that the interests of patients and hardworking staff will be the highest priority through this process”.n

“Mark Butler has told Healthscope administrators they must do the right thing by the community, nurses and midwives. We welcome this support.”
— Shaye Candish
Huge win on annual leave at Healthscope
After two years of fighting, Healthscope members have secured a huge win on annual leave accrual and loading in the Fair Work Commission.
The case was initiated by the Northern Beaches Hospital branch of the NSWNMA in mid-2023. The key findings of the FWC are:
• Full-time employees accrue six weeks leave if they “work according to a seven-day roster”
• Annual leave must accrue progressively, not retrospectively, after 12 months’ service
• There is “no warrant for imposing a requirement that an employee work a particular number of Sundays or public holidays” before they can be considered as working on a seven day basis
• Annual leave loading must be paid on all annual leave accrued by employees who work on a seven-day basis.
• Bargaining continues despite receivership.
The Association is in talks with the company to discuss any impacts the decision may have on any new agreement arising from current bargaining.
NSWNMA General Secretary Shaye Candish said that despite the current receivership, Healthscope have continued to communicate to employees and the Association that employees’ pay and entitlements will be respected.
“There have been several bargaining meetings with the company. There are no plans to halt the bargaining process, but that will be a decision made with members as the situation evolves,” she said.
Union officers will continue discussions with Healthscope’s lawyers about remediation of underpayments for full-time and part-time employees.n
Big wins come when members are active
“The union’s case that Healthscope was incorrectly calculating staff annual leave began when the Northern Beaches Hospital branch started looking through payslips and seeing people were only accruing four weeks of leave a year.
Full-time employees who work according to a seven day roster are entitled to six weeks annual leave a year.
Because leave is allocated progressively, rather than as a lump sum, it was easy to miss this mistake. With union organisers and then industrial officers involved, we started a big audit.
Once we discovered the same leave accrual was being applied across the entire Northern Beaches Hospital, we moved onto other sites and realised the error was occurring across the entire Healthscope nurses
and midwives’ workforce, both currently and previously employed over the past six years.
We lodged a dispute in the Fair Work Commission, which came down to the definition of what it meant to be employed on a seven day basis.
Healthscope interpreted the definition very narrowly, arguing that to be employed across a seven day basis you had to work at least 34 Sundays and six public holidays. We argued that we were available seven days, whether we worked or not, and the Commission found in our favour.
The decision will have to be retrospectively applied. It means all full time employees who work across all seven days have under-accrued annual leave by two weeks a year.
Someone who has worked for six years has been entitled to twelve more weeks leave than they have been given.

BRADY
Our part time staff are entitled to five weeks, and they were also only getting four weeks.
The result shows the strength of what we can do when you have members who are active and bring their issues forward.”
Sheridan Brady, NSWNMA Councillorn
SHERIDAN
Patients and staff will be protected from Healthscope’s demise: Minister Butler
The federal Minister for Health Mark Butler has emphasised that an orderly sale of Healthscope is essential to protect the interests of patients and hard-working staff.
There will be no bailout of private equity-owned Healthscope, but the federal government will “be looking over the shoulder” of all the actors in the administration and sale of the company “to make sure the interests of staff and patients going forward are protected”, Mark Butler said.
The Minister said private hospitals had an important part to play in the health system and received “very significant taxpayer support amounting to about $8 billion through the private health insurance rebate”.
“All of these parts of our system are interconnected, and there's a very strong national interest in ensuring that every part of it, including the private hospitals component of the system is functioning well,” he said. Butler said that the government was aware that a disorderly sales process would have an impact on public hospitals.
“(I am) determined to make sure that if there is a sale of Healthscope hospitals, which is now clear there will be, that it's undertaken in an orderly, stable way that protects the operations of those hospitals, and through that the interests of patients and the very hard-working 19,000 staff members.”
He pointed out that these hospitals had been part of the Australian

“Many of these hospitals have been operating in communities for decades.”
— Mark Butler
health system for a long time, predating Healthscope.
“Many of these hospitals have been operating in communities for decades. They’ve only been owned by Healthscope in its current ownership structure through Brookfield, the Canadian private equity firm, for several years since 2018 or so,” he said.
Healthscope’s woes highlighted the risks to the viability of hospitals in the private sector, he said.
He said private health insurers needed to lift the amount they “actually paid out to hospitals rather than going into profits or management expenses”.
He also cast doubts on “the wisdom of such important assets being held in the hands of overseas private equity firms”.
“There is a strong national interest in the operation of private hospitals, And, with that, comes some social licence that obligates operators of private parts of the system to do so in a way that benefits the interests of patients, not just their owners or their lenders or their shareholders.”n
Find out more
The Association has created a resource area for Healthscope members on our website. There, you can find a large amount of information about the company’s administration process and its consequences and about support that is available to our members. There are FAQs about Healthscope in general and about Northern Beaches Hospital in particular, as well as regular updates.
Visit: https://www.nswnma.asn. au/campaigns/private-sector/ healthscope/
Support in a time of uncertainty
“When we first heard about Healthscope going into receivership, people’s biggest concern was ‘What is happening with our jobs, do we have a job?’ The prospect of not knowing what is going to happen in the next few months or years makes people very worried.
When the news came out, the Union was all over it. The Union had some information in advance and quickly put up FAQs on the website. Pretty much straight away, we had an organiser walking the hospital and in the tearooms, just talking to members and non-members about what was going on. And we had information flyers that were distributed straight away.
We had mass member meetings pretty soon after the receivership was announced. And we put up some flyers about people with visas sponsored by Healthscope, advising then to contact the Union.
People are worried too about what happens with their long service leave: do they get it, or do your entitlements disappear? The union’s industrial officers are advising that, if we get bought out by another company, the new business should honour our entitlements.
We are advising members to take regular screenshots of leave accrual on our Dimensions app, so you have an up-to-date record of your leave entitlements.
The union is advertising peer support through a counselling hotline run by nurses, particularly after there was so much negative media around Healthscope at the Northern Beaches Hospital. The negative public opinion was like a slap in the face.”
Sarah Keevers, Secretary of Norwest NSWNMA branchn

“We are advising members to take regular screenshots of leave accrual.”
— NSWNMA Norwest Private Branch Secretary
State government “eager” Northern Beaches Hospital transfers to public ownership
A complex contract complicates the roll back of the Northern Beaches Hospital privatisation but the state government says it wants it back in public hands.
“Private equity shouldn’t be running acute emergency care.”
That was the blunt message NSW Treasurer Daniel Mookhey delivered to a community forum on the future of the Northern Beaches Hospital.
At the same forum Health Minister Ryan Park said the privatisation of the Northern Beaches Hospital “was a bad decision that had detrimental outcomes”.
“This is a model of care that, unfortunately does not deliver the benefits to the community in the way that the public health system does. When private firms are involved, there is obviously going to be a focus on the bottom line,” he said.
Daniel Mookhey said unravelling the contract was not simple.
“We’re eager to ensure that the hospital returns to public hands. We are also mindful that we don’t think private equity deserves a windfall gain,” he said.
“In order to exit we are obliged to follow the contract we inherit. That has a lot of complexity around it. The contract wasn’t written so it could easily be broken. It contains
“Private equity shouldn’t be running acute emergency care.”
— NSW Treasurer Daniel Mookhey

clauses that require the state, if it decides to terminate it, to pay what was the expected profits from the time at which the contract was signed”.
The contract was signed by Liberal Premier Mike Baird in 2024. Technically it runs to 2058. The Baird government intended Northern Beaches Hospital to be the first of five hospitals that would be built under this model across NSW. The contract has been renegotiated a few times according to a recent Auditor-General’s report.n
We’re here to help
When a company fails it doesn’t mean the end of the services it provides for the community. Particularly so in health, they must be continued by some other entity.
In the uncertain period until these services are reorganised under a different management structure, whether that be another private company, by reabsorption into the public health system or a combination of both, the NSWNMA will be here to support our Healthscope members and to keep them informed of developments in the process to the next stage.
Naturally we will also mobilise our resources and activate our networks in the union movement and step up our advocacy with governments to ensure the interests of the workforce are prioritised and to ensure our members voices are heard.

Frequently Asked Questions by Healthscope members
What is the ANMF and the NSWNMA doing about this situation?
The NSWNMA is working with the ANMF and the federal and state governments to ensure there is a plan in place to protect members at Healthscope hospitals across the country. Conversations with all levels of government have been going for some time.
An urgent meeting of the ANMF Federal Executive put together a plan in order to coordinate the union response. Members are encouraged to come to scheduled member meetings to hear more about what’s being discussed.
Will my hospital close?
There are no plans to close hospitals, and the services that you provide are still a vital part of the health system. The NSWNMA and the ANMF are working hard with the federal and state governments to keep hospitals open and ensure your jobs are protected through this period of uncertainty. Current expectations are that Healthscope will continue to operate as normal while its financial affairs are being reorganised. The Minister of Health Mark Butler has stated that the company has sufficient funds to do so.
What will happen to patients?
Hospitals should continue to operate as normal while under receivership and/or administration. Your hospitals are still an integral part of the health system. We know members care deeply about what happens to your patients and we’ll be working with all the stakeholders to make sure the interests of both members and patients are at the heart of any solution.
I want to keep a record of my entitlements. How do I do that?
Members should download and use the Dimensions App and follow these steps:
• Tap my schedule
• Tap 3 horizontal lines. It may appear in top left or in the bottom right corner
• Tap my time card
• Tap accruals tab centre bottom
• This brings up all of your accruals. Please screen shot and save. You may need to update this save each pay day to make sure you have the most current balance.
What should I say if I’m asked by patients or other members of the public about Healthscope’s
financial situation?
Employees are not authorised to speak on behalf of Healthscope about its financial situation. You should respond by explaining that you’re not able to comment, but that you’ll continue to work as normal providing patient care. Any questions should be referred to the appropriate people within Healthscope who are authorised to speak on behalf of the company (e.g. Healthscope’s communications team).
Resources
WHERE TO FIND SUPPORT
Support available to members feeling stressed or anxious
We know it is a very difficult time for members when their company is in difficulties and there is uncertainty in the workplace. If you’re feeling stressed or anxious and need support, you can contact Nurses and Midwives Support at www.nmsupport.org.au or 1800 667 877.
For those currently on a working visa
If you are an NSWNMA member, you can access the Immigration Advice and Rights Centre (IARC), a free immigration and visa service. Their lawyers provide expert advice for all types of visas provided to workers in Australia such as student, working holiday and sponsorship visas.

Stop press
Healthscope bargaining update
The NSWNMA/ANMF has asked the Fair Work Commission to step in and end Healthscope’s delay on members’ pay increases and back pay.
We have now lodged an application in the Fair Work Commission (FWC) for an Intractable Bargaining Declaration (IBD) because of Healthscope’s refusal to let nurses and midwives vote on the agreement unless we support changes to annual leave. This means that there is no prospect of an agreement being reached.
If the IBD is granted, a full bench of the FWC will decide Healthscope nurses and midwives’ pay and conditions. Importantly their decision must only include terms that are ‘not less favourable’ to each employee which means it is likely your existing annual leave entitlements, and all other existing conditions will be protected.
All protected industrial action (including the wearing of union scrubs) will need to stop once an Intractable Bargaining Declaration is issued, as such action will no longer be protected industrial action.
Compo ‘reform’ would hit women hardest
The Minns government’s proposed ‘reform’ to workers compensation would drastically curtail the ability of psychologically injured workers to access long-term payments.
Women workers including nurses and midwives would be hit hard by the NSW government’s “appalling” workers compensation plans, said NSWNMA Assistant General Secretary, Michael Whaites. He urged the government to focus on preventing psychological injuries in the workplace rather than making it harder for nurses and other essential workers to access support. Under the government proposal, nurses, midwives and carers would automatically be denied access to workers compensation for psychological injuries arising from excessive workloads.


“Those workloads are injuring our members. They will not be compensable injuries under the proposed legislation. Members will just be left to the social security services and no longer work.”
— NSWNMA Assistant General secretary Michael Whaites
Workers who were bullied or sexually harassed at work would have to prove it in court before being eligible for workers compensation, and the injury threshold to continue receiving payments would double to 31 per cent.
In evidence to the parliamentary Standing Committee on Law and Justice, Michael said 85 per cent of people who suffer a psychological injury at work were women.
“We see the proposed changes as, quite frankly, abhorrent,” he said.
“There are systems of work within health, whether it is NSW Health or other healthcare providers, that are injuring nurses, midwives and carers, who are predominantly women. This
proposed legislation will exclude them from compensation.”
He said the NSWNMA gave NSW Health a copy of a report the Association commissioned in 2023 which showed that 15 per cent of nurses had indications of posttraumatic stress disorder.
“A significant other amount had indications of burnout. This was related, in the post-COVID setting, to workloads: workloads generated by being short-staffed, a poor skill mix and increasing activity through those hospitals and aged-care facilities.
“We provided that to government. Health representatives dismissed it out of hand.”
GOVERNMENT DOESN’T VALUE NURSES
Michael said excessive workloads could be fixed by pay increases to restore wages after a decade of “wage suppression”, and more nurses and midwives on the floor.
“But we see through the government's actions that they don't actually value nurses and midwives, because they are fighting the pay rise that will fix the issue.
“With the changes to this [workers comp] legislation, we see they just don't care.
Those workloads are injuring our members. They will not be compensable injuries under the proposed legislation. Members will just be left to the social security services and no longer work. It's appalling.”
Speaking elsewhere, Michael said the Labor Party pledged to stand by injured workers at the last state election.
“It cannot go down the path of inflicting cruelty on its essential workers,” he added.
When The Lamp went to press the workers compensation ‘reforms’ were under consideration by the Public Accountability and Works Committee in state parliament’s upper house.n
Experts slam proposed changes
Experts have slammed the government’s proposed overhaul of workers compensation in evidence to a parliamentary inquiry.
One proposed change, to take benefits away from psychologically injured workers after 2½ years unless they reach a higher 31 per cent Whole of Person Impairment (WPI) rating, came in for particular criticism at the inquiry by the parliamentary Standing Committee on Law and Justice.
The vice-president of the Australian Association of Psychologists, Katrina Norris, said raising the threshold of permanent impairment to 31 per cent could conceivably exclude almost all workers from making a legitimate mental health claim.
“An impairment of 15 per cent requires an individual to be unable to function independently in almost all domains of life,” she wrote in a submission quoted in The Guardian newspaper.
Doug Andrews, a senior medical assessor for the Personal Injury Commission told the committee anyone with a WPI of 21 per cent or more would have no capacity to work and would be pushed onto other government welfare programs if their support was removed.
“I’ve been doing this for many years. I’ve done many, many hundreds of assessments. I can’t recall anybody who had more than 21 per cent impairment who was able to work,” The Sydney Morning Herald reported him as saying.
The Herald also highlighted evidence by Kim Garling, the inaugural independent watchdog of the workplace compensation system.
Garling said the government’s argument about the need to urgently reform the scheme to ensure its sustainability was “misplaced”, adding that it had “been in deficit for most of the time it’s been in existence”.
Garling said the scheme had been underfunded for four years and the simple solution available to the government was to increase premiums paid by businesses.n
Key facts about psychological injuries
The state government’s proposed amendments to workers compensation legislation would severely limit access to compensation for psychological injuries.
In a submission to a parliamentary inquiry, the NSWNMA noted:

• The changes would require workers to prove their injury arose from a narrowly defined ‘relevant event’.
• The proposal reflects a misunderstanding of how psychological injuries occur, which are often cumulative rather than from a single event.
• A 150.6 per cent increase in psychological injury claims among nurses and midwives in the periods 2013–2015 and 2019–2021, indicates systemic failures rather than malingering.
Nurses and midwives face numerous factors that contribute to psychological harm including:
• Chronic understaffing which exacerbates risks, leading to unmet patient needs and increased occupational violence.
• Excessive workloads and “moral injury” arising from systemic failures, forcing nurses to provide care below professional standards.
• Poor management of psychosocial hazards which results in inadequate support for workers who report issues, further compounding their psychological distress.n
Fix system failures that cause psychological injury
The Minns government should look at what causes so many psychological injuries in the health service rather than making it harder for staff to access workers compensation.
Pippa* was the first clinician on the scene when a critical incident occurred in a NSW acute mental health unit in 2014.
Psychological injury later forced Pippa to be medically retired. Her 40-year career as a registered nurse ended nine years earlier than her planned retirement age.
However, it wasn’t the critical incident that caused Pippa’s injury.
“I didn't feel badly affected by the incident – I dealt with it as most nurses do,” she said.
“It was the way the management of the mental health service treated me and my colleagues after the incident that forced me and others to retire early.
“They gave us little care, compassion or consideration of what we had been through.
“They committed multiple breaches of their own policy concerning management of critical incidents and duty of care to staff involved.
“I was the NSWNMA delegate, and when I tried to facilitate workplace safety, I was accused of trying to stir up trouble and having time management issues.
“It was typical of the bullying culture inside the health service.”
Three months after the critical incident, the stress brought about by management’s attitude and failure in its duty of care, forced Pippa to go on workers compensation leave.
‘It is time stories like mine are told and management are made to face up to the practices that cause so many psychological injuries.’
“Management’s behaviour resulted in about four of us being on workers comp,” she said.
PROCESSES EXACERBATED THE ANXIETY
After six weeks on workers comp, Pippa asked to return to work to a vacant position which she was qualified for, in a different area within the Local Health District.
“The GP and psychologist advised me not to return to my old unit because the same managers who caused my stress were still there.
“Despite this, management refused to allow me to transfer to any available position.
“I was a veteran nurse with three certificates and two master degrees and despite my repeated requests they couldn’t find me a job anywhere.
“I believe it was because I was the union delegate and was outspoken about safety issues.
“While I was on workers comp the Local Health District stopped my compensation payments without
the insurance company’s knowledge and made false statements about me to the insurance company.
“They also cut off my work email despite the fact that I was still employed.”
The NSWNMA helped Pippa to resolve these issues in the Industrial Relations Commission.
However, her dealings with the LHD and the difficult return to work process caused her so much distress that the health professionals involved in her care advised her to leave all communications with the LHD to the NSWNMA Industrial Officer dealing with her case.
Pippa said she would strongly advise any nurse making a workers comp claim to get the NSWNMA involved as early as possible.
“The Union’s knowledge and support when going through something like this is invaluable,” she said.
RESOLUTION COMES WITH A GAG
After five years on workers comp, Pippa launched a work damages claim in the NSW Industrial Commission.
Her claim maintained that the health service had failed in its duty of care –including by refusing to offer her any available job.
The court action dragged on for two years – which made her injury worse – until the health service offered an out of court financial settlement with a non-disclosure clause, which she reluctantly accepted.
‘Management committed multiple breaches of their own policy concerning management of critical incidents and duty of care to staff involved.’
“From what I hear, 17 years on, nothing much has changed.
“Nurses are rarely valued or appreciated, and instead of looking for ways to fix a broken system, the Treasurer is proposing even bigger hurdles for injured workers to access the compensation they are entitled to.
“If the current workers comp insurance system is unsustainable, the government should look at what is causing the number of psychological injuries and fix a broken system, rather than punishing the workers which is what NSW Health seems to do.
“Instead of acknowledging systemic failures, through root cause analysis and examinations of critical incidents – which in my experience are simply box ticking exercises – the buck usually stops with nurses on the floor.
“Time and time again systemic failures are swept under the carpet, and nurses are the fall guys.
“It seems that in NSW Health, there always has to be a scapegoat.”
*Name changed for legal reasons.n
“They settle out of court because they don't want it on the public record,” Pippa said.
“The gag clause means nurses and other workers don’t get to tell their story, management never have to learn from their mistakes and the whole thing just keeps repeating.
“In my situation and I believe it to be true in many cases, the managers within NSW Health are not accountable and instead blame the nurses who are working within a failed system much of the time.
“It is time stories like mine are told and management are made to face up to the practices that cause so many psychological injuries.”
Changes to workers comp legislation currently proposed in NSW would force people to prove a psychological injury by going through the Industrial Relations Commission.
Pippa said: “That would just make the whole process more difficult and exacerbate their injuries.”
“There are already so many hurdles to navigate when negotiating workers compensation claims, and when it’s a psychological injury, workers often don’t feel up to the challenge and resign, which seems to be what NSW Health is aiming for.”
Pippa referred to the 2008 Special Commission of Inquiry into Acute Care Services in NSW Public Hospitals, also known as the Garling inquiry.
“Garling found that a culture of blame, bullying and harassment existed in NSW Health,” she said.
Union-backed laws seek pay justice for ‘women’s work’, combat bullying and sexual harassment
Changes to industrial relations law championed by the NSWNMA are expected to improve the working lives of nurses and midwives in NSW.
Parliament has passed amendments to the NSW Industrial Relations Act after extensive lobbying by unions including the NSWNMA. The amendments apply to workers in the NSW industrial relations system, such as state and local government employees.
The Act now has the explicit objectives of achieving gender equality in the workplace and eliminating gender-based undervaluation of work.
‘We have won significant tools to improve the working lives of women in NSW.’
The elimination of workplace bullying and sexual harassment are other new objectives of the Act.
The amendments give the NSW Industrial Relations Commission (IRC) the power to issue binding orders against bullying and sexual harassment in the workplace and award compensation of up to $100,000.
NSWNMA General Secretary Shaye Candish said the Union worked closely with the NSW Teachers’ Federation to win reforms that will benefit working women in particular.
“We have won significant tools to improve the working lives of women in NSW,” she said.
WOMEN DOMINATED INDUSTRIES EARN 36 PER CENT LESS
Shaye said the Act’s objectives are to achieve gender equality, including by eliminating gender-based undervaluation of work.
“This is especially relevant for our profession where almost 90 per cent of nurses and midwives are female,” she said.
“Feminised industries have historically been undervalued.
“The NSW Gender Equality Budget Statement for 2023 -2024 acknowledged this when it stated that nursing has historically tended to be undervalued and seen as ‘women’s work’.
“The gender equality statement revealed that workers with a bachelor’s degree or higher, working in female dominated industries earned 30 per cent less per hour than their counterparts working in male dominated industries.
“Workers with a Certificate III/ IV working in female-dominated industries earned 36 per cent less per hour.
“The Minns government says it is committed to reducing the public sector’s gender pay gap, which was 6.2 per cent in 2023 - the highest median gender pay gap for over a decade.
‘The new antibullying/antisexual harassment provisions are changes with real teeth.’
“We expect the government to live up to its commitment to close the gap.”
The amended Act has another new objective to prevent and eliminate discrimination, bullying and sexual harassment in the workplace.
In line with this objective, workers can now take complaints of sexual harassment and bullying to the IRC.
“This new jurisdiction is expected to produce faster and more traumainformed approaches to resolving these types of matters, where nurses and midwives are in extremely vulnerable situations,” Shaye said.
“Previous arrangements involved a variety of bodies including the NSW Anti-Discrimination Board, the NSW Civil and Administrative Tribunal, the Australian Human Rights Commission and the Federal Court of Australia and were often subject to lengthy delays.
“The new anti-bullying/anti-sexual harassment provisions are changes with real teeth.”
STOP-BULLYING ORDERS
In introducing the amendments, NSW Industrial Relations Minister Sophie Cotsis told parliament that workplace bullying is estimated to cost up to $36 billion annually in Australia and “causes serious harm to workers' health and to the organisations that employ them”.
The amended Act provides that an employee is bullied at work if an individual or group of individuals repeatedly behaves unreasonably towards the employee or a group of employees at work, and the behaviour creates a risk to health and safety.
The IRC must first try to deal with bullying matters by conciliation and, if this fails, by arbitration.
The Act provides that the IRC may make a stop-bullying order to remedy and prevent bullying if it is satisfied there is a risk that the employee will continue to be bullied at work. It can also order a public apology be made.
SEXUAL HARASSMENT DAMAGES
There are financial penalties for contravening a Commission order and victims of sexual harassment and bullying can receive damages of up to $100,000 via the Commission. The amendments give the IRC the jurisdiction to hear workplace sexual harassment claims and deal with all stages of the claim, conciliation and final determination.
Unions get new safety powers
NSW parliament has passed amendments to the Work Health and Safety (WHS) Act which aim to strengthen compliance and enforcement and give unions significant new powers and influence.
It will now be easier for unions to prosecute an employer if the regulator declines to prosecute or does not prosecute within 12 months.
The amendments allow courts to order a portion of a fine or other penalty be paid to the prosecuting union.
“This recognises the significant resources required to bring a successful prosecution,” said Industrial Relations Minister Sophie Cotsis.
The amended Act strengthens the ‘right of entry’ for union officials to collect evidence relating to suspected contraventions of the Act, including conducting tests, measurements and taking photos or videos at a workplace.
It also relaxes confidentiality provisions, allowing information disclosure about inspections and investigations to unions, health and safety representatives and families of deceased workers (so long as it does not prejudice an ongoing investigation or prosecution).
The limitation period for prosecutions under the Work Health and Safety Act remains at two years. However, the amendments allow a court to grant leave to bring proceedings outside the limitation period “if it is in the interests of justice”.n
As with bullying complaints, the commission must first deal with sexual harassment matters by conciliation and, if this fails, via arbitration.
The commission can make an order to remedy and prevent sexual harassment.
The order may apply to individuals and/or employers. n
Data snapshot





Till now, all talk, little action on gender pay gap
Majority-female professions such as nursing are undervalued compared to male-dominated professions, and the state government is not doing enough to close the gap.
As the largest employer of women in Australia, the NSW government is “committed to being a model employer by paying female dominated workforces in the public sector fairly and providing economic security.”
So says the NSW Government’s most recent Gender Equality Budget Statement (2024-25).
“Gender equality is central to our wellbeing, the performance of our state’s economy and the safety of our society,” the Budget statement adds. Noble sentiments – but is the Minns government living up to them?
Karen Hart is among many nurses who don’t think so.
Karen is president and delegate of the NSWNMA’s Wagga branch in the Riverina region.
She points to the NSW public sector gender pay gap – the difference in median remuneration between men and women.
The gap was 6.2 per cent in favour of male employees in June 2023 – up from 4.5 per cent in 2022.
“On average, women in the NSW public sector women earn $217 less than men,” Karen says.
“Majority-female professions such as nursing are still undervalued compared to male-dominated professions, and the state government clearly is not doing enough to close the gap.
“The Gender Equality Budget Statement says that almost 78 per cent of NSW school teachers are women.
“The statement adds that NSW teachers are now the best paid in Australia as a result of an ‘historic’ pay rise.
“The statement also says almost 90 per cent of public sector nurses and midwives are women. However, our wages have been suppressed to such an extent that they don’t even keep up with inflation.”

‘‘Midwives and many nurses have got postgrad qualifications and yet their pay is low compared to
other occupations
that
require university degrees.’’
— Karen Hart
COUPLES WORKING 7 DAYS A WEEK
Karen says low wages paid to NSW nurses are a frequent topic of conversation among her colleagues.
“Midwives and many nurses have got postgrad qualifications and yet their pay is low compared to other occupations that require university degrees.
“Some nurses say they have to seek out weekend work because they need the penalty rates to make ends meet – and because their husband can look after the kids on weekends, which is the only affordable childcare option available to them.
“That means that between the two of them they're working seven days a week with no day off to spend together as a family.
“People say, nurses don’t earn a bad wage because they get penalty rates.
“They seem to forget that penalty rates are being paid for the atrocious hours and the effects on our families and our health.
“Our low rates of pay prevent a lot of nurses from even trying to go into high grade duties because some of those positions are Monday to Friday only, no penalty rates.”
The Gender Equality Budget Statement says 17 per cent of women are living in poverty, compared to 14 per cent of men.
Karen says the reasons include undervalued female-majority professions, loss of pay and superannuation related to having children, and unaffordable childcare.
“Trying to make ends meet is particularly tough for single mothers in lower-paid, female dominated professions.
“Nurses who are single mothers have limited options for childcare due to shift work hours and high fees and they struggle to earn an income above the poverty line.”n
Working towards Closing the Gap
Like many organisations around the country, the union is developing a Reconciliation Action Plan as a practical and structured approach to reconciliation.

Like many organisations around the country, the union is developing a Reconciliation Action Plan as a practical and structured approach to reconciliation. The plan, or ‘RAP’, is being developed in consultation with Aboriginal and Torres Strait Islander members.
Working towards reconciliation includes the establishment of an Aboriginal and Torres Strait Islander Member Circle, as well as empowering leaders such as the recently appointed First Nations councillors, Mat Grant, a nurse manager and Wiradjuri man, and Rebekah Henderson, a dualregistered RN and midwife and a Wiradjuri woman.
“Our reconciliation plan includes acknowledging the impact that nursing and midwifery have had on the inequalities of the past, and working towards Closing the Gap,” says Assistant General Secretary Michael Whaites.
“We recognise that First Nations nurses and midwives are leading the way in health equality and respect,
and providing healing care to their communities and helping women birth on country for generations.”
During NAIDOC week in July, the association held a staff education day, which included a Welcome to Country from Uncle Brendan Kerin and an address from Aunty Donna Ingram.
On Torres Strait Islander Flag Day, 29 May, the association raised the Torres Strait Islander flag outside the NSWNMA head office. Michael spoke to NSWNMA staff about the flag’s design of blue and green and black panels, representing the sea, the land and Torres Strait Islander people, along with a white dhari, a dancer’s headdress, and a five-pointed star, a symbol of sea navigation that also represents the five island groups in the Torres Straits.
Referring to the history of colonisation, stolen generations and indentured labour that came from the Torres Strait Islands, Michael said: “Raising the flag today helps us reflect on the past, and think about the future, and that is part of our Reconciliation Action Plan.”
The association also marked National Sorry Day with an acknowledgement of the stark reality of the Aboriginal and Torres Strait Islander health outcomes, where life expectancy is, on average, eight years less than nonIndigenous communities, and the disease burden is more than double. Michael says: “The union will continue to advocate for more equitable healthcare in remote and regional settings, to uplift Aboriginal and Torres Strait Islander nurses, midwives and carers, and for Aboriginal and Torres Strait Islander people to have a greater say in the way we address complex and intergenerational mental health care.”n


WELCOME TO COUNTRY FROM UNCLE BRENDAN KERIN
THE PLAN, OR ‘RAP’, IS BEING DEVELOPED IN CONSULTATION WITH ABORIGINAL AND TORRES STRAIT ISLANDER MEMBERS.
ADDRESS FROM AUNTY DONNA INGRAM

Branch Beat
Branch Beat with NSWNMA Assistant General Secretary Michael Whaites
Closing beds on a severely understaffed ward is an option open to members when management fails to act in the interests of patient and staff safety.
If managers insist on filling more beds regardless of the staff available, a hospital’s NSWNMA branch may consider closing beds.
The aim would be to align bed numbers with the number and qualifications of the available nursing workforce.
The branch is more likely to decide to close beds if nurses have already put a case to management through all available channels with no relief. Members can expect to come under pressure from management not to close beds.
However, as Bathurst Base Hospital branch has shown, management pressure can be resisted if branches have done the necessary networking to get members on board and members stay united.
Closing beds to protect patients and staff
A Bathurst Hospital branch decision to close beds led management to abandon hardline positions, take a fresh look at staffing solutions and implement bed closures themselves.
“It is still a work in progress, but so far we have pretty much got the outcome that we wanted,” said branch secretary James Adams.
The branch met last October to discuss concerns raised by members in the surgical ward.
The ward had failed to meet its required nursing hours per patient per day (NHPPD) for 40 weeks of 2024.
“There was constant use of unfunded beds despite members raising the issue through reasonable workloads meetings,” James said.
“There was excessive overtime, and the surgical ward basically absorbed the hospital’s entire casual pool which impacted every other department.
“For instance, our clinical nurse educators were being redeployed to
the floor most of the time – despite an Award provision that they are only to be allocated to direct patient care in an emergency.
“At the same time, the CNEs were held accountable as to why their education workload wasn't being met, which was a ridiculous situation.”
WORK HEALTH AND SAFETY ACT GIVES PROTECTION
James said the branch voted unanimously to immediately close non-funded beds to improve NHPPD and protect patient and staff safety.
“We have the right under the Work Health and Safety Act to refuse an unsafe workload.
“Our branch resolution included a proviso that we were willing to negotiate beds being opened when we had a Step Level Black situation.
“We closed beds for about half a week. One bed-closure day had a real impact, which prompted management to come to us for a meeting.”
James said bed closures are one of the hardest things a branch can do.
“There was pressure from management on individual members to ignore the branch resolution.
“Some members initially didn't understand their rights and backed away a bit, but other members really stood their ground.
“We had to be unified in our approach, and we did a lot of networking to coordinate everybody at the ward level.

“Our team leaders were the key because they were the ones who interacted with management. They had to be able to stand strong and say no, that bed is closed.”
The branch advised members to communicate with management about bed closures by email with copies to branch officials.
“This gave us an evidence base that helped us in our subsequent meetings with management,” James said.
Following the bed closures, branch officials and NSWNMA staff held four meetings with management.
OPERATING WITHOUT MODELS OF CARE
“Management let us lead the first meeting and they actually listened to everything we had to say. I think we showed them that we had a whole evidence base behind our decision [to close beds],” James said.
“We argued that key areas of the hospital including surgical, medical and rehab were operating without models of care.
“For example, the rehab ward had a mixed patient cohort with medical patients sometimes outnumbering rehab patients. However, it was staffed as if all patients were rehab.

BATHURST HOSPITAL RANCH SECRETARY JAMES ADAMS WITH BRANCH PRESIDENT KATHI HAMILTON
“Management are now committed to dividing the ward with medical patients staffed with the appropriate NHPPD ratio and no nurse to be given a mixed patient load.”
James said management also agreed to cap surgical ward beds at the funded 20 beds and not surge unless appropriately staffed.
“This was the cap we sought when we decided to close beds,” he said.
“The hospital is developing a model of care as well for rehab, surgical and medical wards which will be finalised through the Staff Consultative Committee. The aim is to make patients safer and reduce staff workload.”
James said branch stewards and key members were monitoring the implementation of agreed staffing improvements.
“We have a good group of stewards and key members who are doing great work on the ground.
“They collect a lot of data, which they put in the IMS (incident management system) for the workload committees to review.
“They also email suggestions to the staff consultative meeting and email the branch regularly to keep us up to date with their actions.”
“We had to be unified in our approach, and we did a lot of networking to coordinate everybody at the ward level.”
— James Adams, Bathurst Hospital branch
And the branch and management have agreed that CNEs are only to be deployed to the floor in an emergency, which must be clearly documented.
Meanwhile, the casual pool has increased and “management are looking at new approaches to recruitment.”
James said some branch stewards had benefited by attending NSWNMA training sessions.
“We encourage as many stewards as possible to attend union training courses and workshops.” n

Ask Shaye
Changing rosters
I am a registered nurse in a public hospital. Recently we were told that the hospital wants to change the starting time and finishing times of our rostered shifts generally, as well as varying the changeover times. Can they do this?
Yes, it is possible for the Local Health District to change the roster generally, however, there needs to be consultation with employees and the Association.
Clause 6 of the Public Health System Nurses’ and Midwifes’ (State) Award requires the employer to consult with staff and their representatives about such change. Some examples of a change requiring consultation under the Award include:
• major changes in the composition, operation or size of the employer’s workforce or in the skills required
• the alteration of hours of work for a class, or group of employees
• transfer of a group of employees to other work, or location
• restructuring of jobs.
In the case of a change to the general rostering times, the employer is seeking ‘the alteration of hours of work for a class or group of employees’.
Feedback from employees and the Association may lead to a consideration of different views and possibly a different roster outcome.
When it comes to your rights and entitlements at work, NSWNMA General Secretary Shaye Candish has the answers.
Changing rosters
In the Public Health system, can a casual employee get overtime?
Unfortunately, casual employees are not entitled to overtime under the Public Health System Nurses & Midwives’ (State) Award. Casuals are instead paid an hourly rate plus 10 per cent with a minimum 2-hour start, as per clause 29 Part II.
If a casual employee is working regularly and systematically for more than six months however, they may elect to apply for casual conversion to permanent employment provided they are not backfilling another employee temporarily. If they become a permanent employee, they would then become eligible for overtime if such circumstances arose.
If a casual is asked to continue working beyond the normal length of a shift and they do not wish to, then they should simply advise the relevant manager that they wish to proceed home and they would just be paid for all time worked.
Long Service Leave for Casual Employees
I have been employed in private clinic on a casual basis with the same employer for 11 years. Am I entitled to long service leave?
Just like full and part-time employees, casuals are also entitled to 2 months paid long service leave on completion of 10 years continuous service, and one month of paid leave for each additional 5 years' service. A worker who has completed between 5 and 10 years of continuous service may be entitled to a long service leave payout if they are terminated, or resign on account of illness, incapacity, or domestic or other pressing necessity.
Usually, continuous service is not broken merely due to:
• irregularity in shifts
• brief periods your employer did not offer you work
• brief periods you were unavailable, such as holidays.
However, continuous service is broken if you resigned and were re-employed.
Long service leave must be taken and cannot be paid-in-lieu or cashed-out unless the employee resigns or their employment is terminated. For casual workers, long service leave pay is generally based on your average weekly wage over the previous 12 months or 5 years, whichever is greater. This amount however can vary depending on individual circumstances.
You should contact the Association if you have any questions about your entitlements to long service leave.
Determining grades
I am a public sector Clinical Nurse Consultant Grade 2. Management have indicated that they are considering downgrading my position to a Clinical Nurse Specialist Grade 2 on the basis that the position does not fulfill all the domains under IB2024_009 List of Domains and Functions for Clinical Nurses and Midwives. Is my manager correct?
Your manager is wrong. Some history is required to explain the domains. The Clinical Nurse/ Midwife Consultant position was first created in 1985. It was a single grade. Around 2000, the Clinical Nurse/Midwife Consultant position was expanded from one single grade to three grades. To grade a particular position, NSW Health and the Association created the domains, as a way to differentiate the grades from each other by looking at where
the majority of functions fell in a particular position. The latest version of the policy is now found in IB2024_009. This policy states:
The domains / functions have been selected to differentiate between the grades of CNC/ CMC and are not intended to describe the whole range of functions undertaken by CNC/CMC.
In the original policy when the Clinical Nurse/Midwife Consultant grades expanded and NSW Health and NSWNMA were educating the workforce about the positions, Circular 2000/1 (the predecessor of the current policy) explicitly identifies the position of NSW Health and NSWNMA:
“It is acknowledged … that not all functions listed at higher grades are necessarily required for the Area Health Service to establish a higher-grade Clinical Nurse Consultant position.
When determining the grade of a Clinical Nurse Consultant position to be established, the Area Health Service should clearly establish its requirements and then have due regard to the level that contains the majority of functions listed in the domains”
Classification upgrades
I am seeking career advancement. How do I get a classification upgrade?
The best time to commence an upgrade is at your annual performance appraisal review. Reviews should include changes and updates to your position description (PD).
If there is substantial change to your PD then an upgrade may be warranted. This would be processed by your Line Managers and ultimately go to the Local
Health District Grading Committee for adjudication. Committee adjudicators include some representatives from the Association.
All upgrades do require incorporation of the Award’s minimum criteria into the PDs. Minimum criteria are relevant post registration qualifications and experience, including in the specialty field.
Position upgrades of 5 per cent or more pay increases are to be advertised. Subsequently the incumbent seeking the upgrade must apply for the advertised position in accordance with PD2023_024 Recruitment and Selection of Staff to the NSW Health Service.
Separate from the above processes are Clinical Nurse/Midwife Specialist Grade 1 classifications. These classifications are personal grades. They are an extension of the applicant’s Registered Nurse position and classification. Personal grades are subject to the Award criteria of experience and/or qualifications and being a specialist, leader and resource to the unit. The upgrading process is to apply via line management.
Free from on-call on days off
I am a senior Nurse Manager in the public sector. I work Monday to Friday. I have now been asked to be on-call over the weekends when I am not rostered to work. This is too much. Aren’t I entitled to have some downtime?
Yes, you must be completely free from work, including free from being placed on-call in accordance with the Public Health System Nurses’ and Midwives’ (State) Award. Firstly, when you are on annual leave, you cannot be placed on-call (clause 4 (xvii)). Secondly, while there is a possible exception in extreme circumstances to remain on-call on rostered days
off to provide clinical services, the general arrangement provides the following in clause 4(xvii)(b):
“…no employee shall be required to remain on call whilst on a rostered day off or from the completion of the employee’s shift on the day preceding a rostered day off.”
Therefore, if you work Monday to Friday, you must be free from oncall on Saturday, Sunday and on Friday night.
There is a special allowance for being on-call during a rostered day off. This allowance can only be utilised in circumstances agreed between the Local Health District and the head office of the Association (see clause 4(xvii)(c). This is quite rare.
Failure to meet medical exam
What if I fail to attend an independent medical examination (IME) as part of my workers’ compensation claim?
If you are unable to attend an appointment that has been organised for you as part of your workers’ compensation claim, you should contact your case manager as soon as possible.
Failure to attend an IME may affect benefits payable in accordance with the Workplace Injury Management and Workers Compensation Act of 1998. Your employer is likely become aware of the non-attendance, as they have a role in facilitating your safe return to work and understanding the medical advice related to your injury or illness.


Professional Perspectives
Career break: Registration options
I am taking a career break to care for my elderly parent and am thinking of letting my registration lapse but may want to return to practise at some point in the future. What is the best option for me?
There are several options depending on your individual circumstances and how long you wish to take off. Here are a couple of the more common approaches available to you.
If you can maintain your continuing professional development (CPD) and recency of practice requirements, it may be more appropriate for you to retain general registration. You may wish to choose this option if you are unsure how long you need to take off and how you will feel about returning to practice at a later stage.
You may also consider becoming a non-practising registrant. As a non-practising registrant, you are not required under the National Law to meet the registration standard requirements of CPD, professional indemnity insurance or recency of practice. However, if you hold nonpractising registration and would like to return as a practising registrant, you must meet all the requirements of the following NMBA registration standards:
• criminal history
• professional indemnity insurance arrangements
• recency of practice.
If you do not meet the recency of practice registration standard requirement, you will need to follow the NMBA re-entry to practice requirements: https://www. nursingmidwiferyboard.gov.au/ Registration-and-Endorsement/ reentry-to-practice.aspx.
All nurses and midwives must renew their registration each year regardless of the type of registration they hold. If you do
not renew your registration, your registration will lapse, and you will no longer be able to use any of the protected titles that apply for nurses and/or midwives. Your details will be removed from the Register of Nurses and/or Register of Midwives.
English language competency
I am from a non-English speaking background and have just completed my Bachelor of Nursing in Australia. I am seeking registration through Ahpra for the first time, and I am being asked to provide evidence of English language competency. Why do I need to do this when I graduated in Australia?
To get registration in Australia, every applicant must meet the NMBA English language skills standard. This includes Australian-trained or overseas qualified applicants. This standard supports registered health practitioners to practise safely in Australia. The standard does not apply to students but does apply to graduates and anyone seeking registration in Australia for the first time. There are various pathways to proving English language competency so it’s best to check out the NMBA ‘English language skills pathway selection tool’ online: https://www.ahpra.gov.au/ Registration/RegistrationStandards/English-languageskills.aspx#form-top and see which best applies to you. We advise any member who is seeking registration for the first time to check out the requirements in advance, allowing sufficient time to get all requirements completed to avoid delays gaining registration. If you need help with the process, you can contact the NSWNMA.
Coronial Investigation
There was an unexpected and unexplained death at work that was reported to the coroner. I was on duty at the time. What do I do? Can the NSWNMA help me?
Your membership with the NSWNMA provides you with legal representation for coronial inquests. Please call to speak to one of our legal officers who will advise and support you through the process with the police, providing a statement to the coroner, preparing you to give evidence in court and representing you at the Coroners Court if you are a party of sufficient interest.
Even if you are required to appear as a witness only, the NSWNMA will provide advice and support to you during the coronial process.
When there is an unexpected death there is also a Root Cause Analysis (RCA) or Serious Adverse Event Review (SAER) process. There may even be a fact finding or Managing Complaints and Concerns about Clinicians (MCCC) process. This can be overwhelming. The NSWNMA member rights centre can provide support so please reach out.
Sometimes while the coronial and employer investigations are happening there can be a complaint to the Health Care Complaints Commission (HCCC). If this occurs the NSWNMA can advise, assist and represent you at the HCCC and Nursing and Midwifery Council (NMC).
Political activism
I am interested in being engaged in political rallies and activities – what do I need to consider?
When engaging in political activities, it is important to consider your obligations as an employee, and professionally as a nurse or a midwife. From an employee perspective, you must ensure you don’t breach any
relevant workplace code of conduct (for example, don’t wear work uniform to a protest or rally and don’t identify your workplace to the media).
From a professional perspective, the Nursing and Midwifery Board of Australia (NMBA) professional standards outline the practice and behaviour expectations of all nurses and midwives: (https://www. nursingmidwiferyboard.gov.au/ Codes-Guidelines-Statements/ Professional-standards.aspx).
These professional standards outline that nurses and midwives should promote health and wellbeing and understand and apply the principles of public health. Nurses and midwives should also participate in health advocacy for community and
The Association’s professional team answers your questions about professional issues, your rights and responsibilities.
addresses health inequality. Nurses and midwives must not participate in unlawful behaviour and understand that unlawful behaviour may be viewed as unsatisfactory professional conduct or professional misconduct and have implications for their registration.
Criminal charges and your NMBA Registration
I have recently been charged with a criminal offence, and I am concerned that this will impact on my registration and ability to practice – what should I do?
If you are charged with an offence, we recommend you contact the NSWNMA as soon as possible for individual advice from a Legal Officer. Depending on your
offence you have been charged with, you may be required to inform the Nursing and Midwifery Board of Australia (NMBA) before renewal. At renewal, all changes to criminal history must be declared.




AUSTRALIA
Student prac payment begins

From July 1, the new Commonwealth Prac Payment (CPP) system became available to nursing and midwifery students across Australia to assist them with much-needed financial support while undertaking their mandatory clinical training.
The NSWNMA and the ANMF were instrumental in advocating for the CPP, to help eligible students experiencing ‘placement poverty’, to manage the significant financial burden associated with completing their clinical placements, including the loss of regular income and out-of-pocket costs.
ANMF Federal Secretary Annie Butler welcomed the introduction of the CPP scheme as a ‘positive first step’ in financially supporting nursing and midwifery students but said there should be broader eligibility criteria for all students needing to access the payment.
“This financial burden has resulted in growing numbers of students failing to complete their qualifications and walking-away from the profession.
“While we welcome the start of the CPP scheme, we know we need to do more to support nursing and midwifery students through their studies to ensure they have ongoing access to quality education programs, quality clinical placements and training, and sufficient financial assistance to address the increasing challenges they face.”
Eligible students will receive $331.65 a week.
University students (Bachelor and Masters) can apply via their education provider.
For students enrolled in a Diploma of Nursing at TAFE or Registered Training Organisation (RTO), the CPP (VET) is being delivered by the Department of Employment and Workplace Relations.
More info:
For more information on the CPP, including eligibility and the tax implications go to: nswnma.info/3ZWtZOa
AUSTRALIA
Ramsay to close psychology units
Australia's largest private hospital operator will shut down 17 of its 20 psychology clinics across the country by September, reports the ABC .
Ramsay Health Care is Australia's largest private provider of psychology services, and its clinics see a range of high-risk patients with various mental health conditions.
The provider also runs separate mental health clinics. They will not be affected by the change.
A Health Department review into the viability of the private hospital system, commissioned by the Albanese government and published in summary last year, identified declining mental health services as a major issue.
It noted the sector had raised concerns about access to private hospital psychiatric services, and the difficulty in attracting and retaining psychiatrists prepared to work in a hospital setting. While the number of Medicare-subsidised psychiatric services increased by almost 20 per cent from 2018-19 to 2021-22, the number of services delivered in a private setting dropped by about 15 per cent over the same time period.
Psychiatrist and former Australian of the Year, Patrick McGorry told the ABC there was a "great risk" Ramsay’s clinic closures would see some patients left without care.
"It'll throw more patients potentially back on a public sector that's severely underfunded at a state level and in crisis in several states,” he said.

“It'll throw more patients potentially back on a public sector that's severely underfunded at a state level and in crisis in several states”
—
Psychiatrist, and former Australian of the Year, Patrick McGorry.
AUSTRALIA
People with disability are dying from cancers we can prevent

People with disability are dying from preventable cancers at higher rates than the general population due to systemic barriers in accessing preventative care and treatment.
People with disability are missing out on screening programs that could help detect cancer early, and after diagnosis are less likely to survive, according to a new study.
Researchers say their study shows “the striking inequity at the heart of current approaches to controlling cancer”.
They reviewed evidence from 73 studies from around the world that compared cancer outcomes in people with disability to those without.
They found people with disability are missing out on these life-saving screening programs all around the world, including for breast, cervical and bowel cancer.
In fact, some studies showed these cancers are more likely to be diagnosed at an advanced stage in people with disability. Once diagnosed, people with disability are still at a disadvantage with lower survival rates than cancer patients without disability.
A UK study of cancer deaths in people with intellectual disability found more than a third had their cancer diagnosed after going to the emergency department. Almost half of the cancers in the study were already at an advanced stage when diagnosed.
Another review of global evidence found cancer patients with disability receive poorer quality cancer care. This included delays in treatment, being undertreated or having excessively invasive treatment.
From diagnosis to treatment, global evidence shows people with disability are being excluded from health services that many people without disability routinely access and benefit from.
AUSTRALIA
Minimum wage increases by 3.5 per cent
Fair Work Commission (FWC) says said the decision will help claw back the loss of real incomes over the past few years.
The new minimum wage from July 1 will be $24.95 an hour ($948 per week) up from $24.10 ($915.90) respectively –a weekly increase of about $32.
The increase is about one percentage point above inflation.
Workers who will benefit most are concentrated in labour-intensive and female-dominated industries such as hospitality, health and social assistance, and administrative services.
The Reserve Bank recently projected inflation will climb from 2.4 per cent in the year to March, to 3.1 per cent by mid-2026 following the end of government cost of living measures, such as energy subsidies.
The president of the FWC, Justice Adam Hatcher, said with inflation back under control, it was time to make up for that hit to living standards.
“We are satisfied that the level of wage increase we have determined is sustainable,” he said.
ACTU secretary Sally McManus credited union pressure for the real minimum wage rise.
“With unions delivering strong real wage growth in collective agreements and now with real award wages growing, working people have turned the corner and are seeing decent real wage growth for the first time in more than a decade,” she said.
The ABS Wage Price Index had previously shown that wages for workers on collective agreements rose by 3.8 per cent over the year to March 2025. Real wages grew by one per cent in that time.

A UK study of cancer deaths in people with intellectual disability found more than a third had their cancer diagnosed after going to the emergency department. “Working people have turned the corner and are seeing decent real wage growth for the first time in more than a decade.”
— ACTU secretary Sally MacManus

Union support for global action to tax the super-rich
Public Services International (PSI) throws its weight behind push to tax the mega wealthy.
Spain and Brazil have launched a joint initiative at a United Nations conference “to promote higher tax contributions from the super-rich worldwide, aimed at tackling soaring inequality by ensuring those with the most pay their fair share”.
“Our countries need more and more public revenues to meet their needs. Inequality is a problem everywhere and the richest pay less than the middle class – even less than lower-income taxpayers,” said Spain’s Secretary of State for Finance Jesús Gascón.
The two governments point to a stark reality: the wealthiest one per cent of the global population owns more than 95 per cent of humanity combined.
The initiative prioritises information sharing to help expose gaps in tax systems, close loopholes and combat evasion and avoidance.
This will help tax administrations identify where and how wealth is concentrated, how much is currently being paid and what needs to change.
The initiative has a clear aim: more transparency, more accountability and fairer contributions from the richest.
The PSI says the proposal marks a historic step toward addressing extreme wealth inequality that threatens both public services and democracy itself.
“This builds directly on years of union-led tax justice campaigning that has already yielded significant victories, including the OECD global minimum corporate tax and Australia's public country-bycountry reporting initiatives,” it said.
“This builds directly on years of union-led tax justice campaigning that has already yielded significant victories.” — PSI
AUSTRALIA

QACAG finishes on a high
After 20 years of successful advocacy, the Quality Aged Care Action Group (QACAG) has finished up after some historic achievements in the sector.
The group was established in 2005 for carers, consumers, aged care nurses and advocacy groups to raise awareness and lobby for improvements in residential aged care.
The group included current and retired nurses and care staff, and other community members concerned with improving aged care. The group also had representatives from the Older Women’s Network, Combined Pensioners & Superannuants Association of NSW, Senior Rights Service, NSW Nurses and Midwives’ Association and the Retired Teachers’ Association, Multicultural Communities of the Illawarra and Kings Cross Community Centre.
The group made significant contributions to the Aged Care Quality and Safety Commission and the Productivity Commission inquiries into aged care.
As fellow travellers with aged care workers and their unions QACAG was able to celebrate some historic achievements for the sector including an injection of more than $11 billion by the federal government into the sector to finance pay rises for aged care workers and a raft of reforms to improve the lives of residents.
Its unspent funds will be donated to Older Women’s Network (NSW) who are very active partners in the NSW Aged Care Roundtable. QACAG members are welcome to work with OWN to continue this work under the umbrella of OWN.
The group made significant contributions to the Aged Care Quality and Safety Commission and the Productivity Commission advocating for better quality care for older Australians.
AUSTRALIA
Abortion law reform expands role of nurses

Nurse practitioners (NPs) and endorsed midwives may now prescribe the abortion drug MS-2 Step thanks to law reform backed by the NSWNMA.
Legislation to expand abortion services in NSW, introduced by Greens MP Amanda Cohn, allows NPs and endorsed midwives to supply medication to terminate pregnancies up to nine weeks' gestation.
The NSWNMA lodged a submission in support of the legislation.
NSWNMA General Secretary Shaye Candish said the reform means endorsed midwives and NPs can now work to their full scope of practice and provide comprehensive reproductive health services, with prescribed medication subsidised under the pharmaceutical benefits scheme.
“This will especially benefit women in rural areas where a GP may not be available or the best choice for a woman in her local area,” Shaye said.
The NSWNMA submission said women living rurally and remotely with limited access to GPs are often compelled to travel long distances to access the care they need.
“To enhance women’s access to abortions, the NSWNMA advocates for changes in MS-2 Step prescribing, to encompass prescriptions by both nurse practitioners and endorsed midwives,” the submission said.
“Nurse practitioners and endorsed midwives have the necessary qualifications, clinical experience, training, and lawful authority to safely prescribe MS-2 Step for medical terminations of pregnancy.
“Such a legislative change would additionally ensure that our nursing and midwifery workforce is working to full scope of practice, ultimately addressing service gaps and an historic over-reliance on medical practitioners.”
“This will especially benefit women in rural areas where a GP may not be available.”
— NSWNMA General Secretary Shaye Candish
AUSTRALIA
Australia’s bowel cancer rates are world’s highest for under-50s
A study of 50 countries – published recently in Lancet Oncology – revealed Australia ranked the worst for having incidences of early-onset bowel cancer.
An early release of findings from an Australian study shows the incidence of bowel cancer is up to three times higher among Australians born in the 1990s compared with the 1950s cohort.
The study, led by the University of Melbourne, analysed government data on all diagnoses of bowel cancer in Australia from 1990-2020.
While over-50s make up the majority of diagnoses these rates have begun to decline. National screening was lowered from 50 to 45 in 2023.
Early-onset cases, however, are increasing by up to 8 per cent per year, the study found.
Bowel cancer is now the deadliest form of cancer for people aged 25 to 44 in Australia.
Julien Wiggins, the chief executive of Bowel Cancer Australia, told The Guardian : “The data is now starting to really unfortunately confirm what we’ve been seeing.”
Dr Lisa Mielke, the head of the mucosal immunity and cancer laboratory at the Olivia Newton-John Cancer Research Institute, said: “The study highlights that it is not just one type of bowel cancer that is on the rise in younger people. Overall, the incidences of bowel cancers in all regions of the large bowel, rectum and anus are increasing,” she said.
‘Early-onset cases of bowel cancer are increasing by up to 8 per cent per year.’
One people enriched, one people erased
The UN Special Rapporteur Francesca Albanese has called on unions, civil society and ordinary citizens to press for boycotts, divestment and sanctions to make the Israeli government accountable for its genocidal war in Gaza.
The UN Food and Agricultural Organisation estimates that, since the blockade of humanitarian aid in Gaza by the Israeli army, the average caloric intake per person per day in Gaza has plummeted to 67 per cent of the minimum required for survival.
A recent editorial in The Lancet points out that “starvation is only one aspect of this grim reality”.
“The attacks on health care facilities and workers have been relentless. Many hospitals have either been bombed or destroyed. Specialised care is almost non-existent. The already moribund health system has been further weakened by the aid blockade and the unacceptable killing of more than 1400 healthcare workers,” it said.
“Israel has dismantled the last function of the UN in Gaza –humanitarian aid.”
According to The Lancet, the Israeli Government has also targeted civilian infrastructure required for the survival of Palestinians, with 89 per cent of the water and sanitation systems and 92 per cent of housing destroyed or damaged.
The UN Relief and Works Agency for Palestinian refugees found that between 2023 and 2024 cases of acute watery diarrhoea increased 36-fold, while acute jaundice syndrome (indicative of hepatitis A) increased 384-fold
The Lancet also pointed out that

https://anmf.org.au/media/ nurses-andmidwives-for-peace
“every day, on average, 35 children are killed in Gaza, amounting to a total of at least 18,000 children killed in this conflict.
“Pre-teen children are being admitted with gunshot wounds. Children are dying of chronic malnutrition and those who survive might never fully recover. Gaza is also home to the largest cohort of child amputees in modern history.”
The respected medical journal had harsh words for the “many medical academies and health professional organisations that claim a commitment to social justice (but) have failed to speak out. Their silence is morally unacceptable.”
CORPORATIONS PROFIT FROM GAZA’S MISERY
Earlier this year, the UN Special Rapporteur Francesca Albanese also emphasised the responsibility of the medical profession in light of the relentless violence towards health facilities and health workers.
“I urge medical professionals worldwide to pursue the severance of all ties with Israel as a concrete way to forcefully denounce Israel’s full destruction of the Palestinian healthcare system in Gaza, a critical tool of its ongoing genocide.” she said.
The UN Special Rapporteur released a report in July called “From Economy of Occupation to Economy of Genocide” that investigates the corporate machinery that sustains and has profited from “Israel’s economy of illegal occupation, apartheid and now, genocide”.
“Official figures count over 200,000 people killed or injured. Leading health experts estimate the true toll is far higher. Israel has dismantled the last function of the UN in Gaza –humanitarian aid,” she said.
“Its so called “Gaza Humanitarian Foundation” is nothing else than a death trap engineered to kill or force the flight of a starved, bombarded, emaciated population marked for elimination.
“At the same time since October 2023, the Tel Aviv Stock Exchange has soared by 213 per cent in US dollars amassing 225.7 million in US dollars in market gains including $US67.8 in the last month alone.
“One people enriched. One people erased.
“At this existential moment for the Palestinian people trade unions, lawyers, civil society groups and ordinary citizens should encourage behavioural change from the side of corporate entities and governments by pressing for boycotts, divestment, sanctions and accountability.”n

ACTU condemns Israeli government blockade of humanitarian aid to Gaza
Australian union movement warns two million Palestinians are at risk of starvation.
“We continue to be horrified by the humanitarian catastrophe facing Palestinians in Gaza,” the ACTU said in a statement released in late May.
“The Israeli Government has sought to shut down the existing aid and distribution system run by the United Nations and humanitarian partners and establish its own delivery mechanisms by the Israeli military, contravening fundamental humanitarian principles, and meaning large parts of Gaza will go without supplies,” it said.
“We continue to be horrified by the humanitarian catastrophe facing Palestinians in Gaza.” — ACTU
“The ACTU condemns the use of starvation as a weapon of war and urges Israel to comply with the International Court of Justice’s order to take immediate steps to prevent acts of genocide, punish incitement to genocide, and facilitate the provision of basic services and humanitarian assistance to Palestinians in Gaza. Israel must immediately provide food and essentials to people in Gaza and ensure unimpeded access for humanitarian aid.
“We stand in solidarity with workers such as health workers who are both dealing with the immediate risk to their own health and safety and of caring for those injured, dying and facing starvation.”
Read the full ACTU statement : https://www.actu.org.au/ speeches-and-opinion/actu-statement-on-gaza/ n
ANMF launches Nurses and Midwives for Peace campaign
The campaign is a response to the attacks on healthcare facilities and staff in war zones. In Gaza, hospitals have been bombed, ambulances fired on and nurses, midwives and doctors killed while trying to save lives.
These attacks are not just violations of international law — they are attacks on our professions, on humanity, and on the principle that healthcare must remain neutral and protected. As nurses and midwives, we are bound by a commitment to health, healing, and human rights. That commitment doesn’t stop at borders.
TAKE ACTION:
Show your support: Sign our letter or write your own personal message to nurses and healthcare workers on the frontline in Gaza
Join the movement online: support our social media campaign by sharing posts on Facebook and Instagram
Hear their stories: Read firsthand accounts from Australian nurses who have recently returned from working in Gaza
Support humanitarian efforts: Volunteer with or donate to the Red Cross to help provide vital aid.
Visit: https://anmf.org.au/media/nurses-andmidwives-for-peace n
health+wellbeing
Dealing with menopause

The Australian nursing and midwifery workforce is predominately female. It is also ageing, which means that many will be going through menopause.
Menopause can affect your health greatly, which in turn can affect your experiences at work and the rest of your life. Here is some information on menopause and what you can do to offset its effects.
The gender composition of our workforce
As at June 2016, 89 per cent of registered nurses and midwives were female, and 11 per cent were male.
The average age of a registered nurse or midwife in Australia is 44 years of age, with 37 per cent of registrants aged between 45 and 60 years.
When
does menopause occur?
Menopause naturally occurs between the ages of 45 and 55 years of age, with the average age of onset occurring at 50 years. Perimenopause, which is also referred to as menopausal
transition, may occur over five to 10 years before the final menstrual period. Perimenopausal signs and symptoms may include irregular periods, or a change in flow, hot flushes, night sweats, body aches and painful breasts. A woman is considered to be post-menopausal when she has had no periods for 12 months.
Early menopause occurs between 40 to 45 years of age. This can occur due to a natural loss of ovarian function, surgical removal of ovaries and some cancer treatments.
Symptoms of menopause
The symptoms outlined below will not occur for every woman, and not all symptoms may be experienced.
Research suggests that 60 per cent of women report experiencing mild symptoms usually lasting four to eight years. A further 20 per cent report no symptoms, and 20 per cent of women report severe symptoms (Col et al., 2009).
The physical and psychological symptoms of perimenopause and menopause may include:
Physical symptoms
• hot flushes and night sweats
• body aches and joint pains
• osteoporosis
• muscle tension
• dry skin
• itchy skin
• headaches or migraines
• dizziness and vertigo
• digestive problems
• heart palpitations
• sleeping difficulties
• fatigue
• loss of libido
• vaginal dryness
• urinary frequency
• unwanted hair growth
• thinning of scalp and pubic hair
• tingling extremities
• bloating, and
• breast tenderness or pain.
Psychological symptoms
Lower levels of oestrogen also reduce or lower the level of serotonin. Serotonin is an important neurochemical that regulates mood, emotions and sleep. Symptoms include:
• anxiety
• irritability
• depression
• mood swings
• forgetfulness, and
• trouble concentrating or ability to make decisions.
What can I do next?
You may want to know about menopause and managing it. The Australasian Menopause Society has a range of information sheets that can get you started: https:// menopause.org.au/
Nurse & Midwife Support provides free and confidential support 24/7, to nurses, midwives and students Australia wide. If you would like to speak to someone, call 1800 667 877, or you can request support via email (https://www.nmsupport. org.au/support).




test your Knowledge
ACROSS
1. Medical term for cryptorchidism (11.6)
9. Thoughtful and reflective (13)
12. Set out on a journey (6)
13. Renewed outbreak of a disease (13)
18. Sound
19. Materials that harden on heat (9)
20. Form a mental picture (7)
22. Relating to the bladder and vagina (13)
24. A suspension of colloidal particles in a liquid (3)
25. Cold-induced skin condition
27. Removal of waste from the body (9)
29. Delicate as in a fine net or weave
31. As a result, consequently (4)
33. Mimicking or resembling (9)
34. Crosses or moves across (9)
35. Numbing technique for lower body surgeries (6.11) DOWN
1. Chronic inflammation of the colon (10.7)
2. A compound formed from an alcohol and an acid (5)
3. Inability to speak despite understanding (10.7)
4. Genetic blueprint for life (1.1.1)
5. An antiviral used with other drugs for HIV infection treatment (1.1.1)
6. Basic or fundamental (9)
7. The sum of all parts (10)
8. Inherited condition affecting hemoglobin shape (6.4.7)
10. Digitus pedis (3)
11. Visceral Epithelial Cell (1.1.1)
14. Masticates (5)
15. Type of acid found in soil (5)
16. The origin and development of cells
17. Not able to spread disease (13)
21. Milliampere (1.1)
23. A graft of bone into a bone cavity (5)
26. Replayed competition (7)
28. Inflammation of the iris (6)
30. Raccoon-like mammal (5)
32. Fluids from clotted blood (4)



The NSWNMA is committed to protecting the interests of nurses and midwives by purchasing a range of insurances to cover members.
Journey Accident Insurance
provides cover for members who are injured as a result of an accident while travelling between their home and their regular place of employment.
Professional Indemnity Insurance*
provides legal representation and protection for members when required.
Make sure your membership remains financial at all times in order to access the insurance and other benefits provided by the NSWNMA.