ON PAGE 3...)


The CQC's decision to issue Blackpool Council with the first 'inadequate' rating for adult social care since assessments began in December 2023 makes for sobering reading.
Yet as I absorbed the details of this hard-hitting report, I found myself reflecting not on the failings of the service itself, but on the crushing reality of the social and economic context in which it operates.
Blackpool is England's most deprived authority, with the highest rate of drug-related deaths in the country and healthy life expectancy levels for men and women that are 10 years short of national averages.
These are not just statistics – they represent a community grappling with profound challenges that would stretch any social care system to breaking point.
Perhaps most tellingly, senior leaders told the regulator that people with care and support needs moved to Blackpool seeking low-cost housing, adding to demand for adult social care, which was significantly above the national average.
The numbers speak for themselves: in 2023-24, the authority received 2,980 requests for support per 100,000 people aged 18-64, compared with 1,785 across England, and 15,795 requests per 100,000 people aged 65 or over, as against 13,285 nationally.
For someone like me, who grew up in one of Europe's most deprived areas, Blackpool holds particularly fond memories. Just 53 miles from my childhood home, it represented a welcome escape – a place of joy and respite from the harsh realities of deprivation.
To see it now struggling under such enormous social care pressures is deeply saddening, yet sadly unsurprising given the broader crisis engulfing our sector.
The report's findings must be viewed against the backdrop of systemic underfunding that has been laid bare repeatedly this year.
Regular readers will recall the hard-hitting parliamentary report in May that we published that warned about the "cost of inaction" in social care.
A cross-party group of MPs warned that attempts to reform adult social care were doomed to fail unless ministers accepted that major investment was needed to overhaul a "broken" system that was failing millions of people.
More recently, the ADASS Autumn Survey 2024 painted an even bleaker picture: 81% of councils were on course to overspend their adult social care budget in the 2024/25 financial year, rising from 72% in 2023/24 and 63% in 2022/23.
On current trends, within a couple of years, all council adult social care budgets will be overspent. Against this backdrop, Blackpool's plight becomes not an anomaly, but a harbinger of what awaits other authorities.
The CQC found evidence of a "crisis intervention" approach to adult social care across the authority, with the council struggling to provide preventive services and reablement support.
Yet this reactive approach is precisely what happens when resources are stretched beyond capacity – services focus on immediate crises rather than the early intervention that could prevent greater problems down the line.
Particularly concerning were the findings around cultural competence and equality of access. The regulator found that people were "not being treated equally" in relation to standards of care, with people with learning disabilities or autistic people waiting longest for Care Act assessments.
However, again I would argue this reflects resource pressures rather than deliberate discrimination.
What gives me hope is that satisfaction with care in Blackpool is above the national average, with 90% of people telling the inspectors that they felt safe.
This suggests that frontline staff are working heroically within impossible constraints –a testament to their dedication rather than evidence of systemic failure.
The council has committed to developing an improvement plan scrutinised by an independently-chaired board, focusing on safeguarding training, reducing waiting times, and embedding strengths-based practice.
These are worthy goals, but without addressing the fundamental funding crisis, we risk simply rearranging deck chairs on the Titanic.
I would direct your attention to our article on page [5], featuring a podcast interview with Nadra Ahmed Chair of the National Care Association, who "pulls no punches" in her condemnation of the government's approach to sector funding. As she so eloquently put it, cutting through political rhetoric with stark clarity: "Social care has continued to deliver, continues to deliver and does not need fixing. It needs to be funded."
The Blackpool report should serve as a wake-up call, not just for that council, but for policymakers across the country.
We cannot continue to expect miracles from a sector starved of resources while dealing with England's most vulnerable citizens. The inequalities and challenges faced by places like Blackpool demand a national response – one that acknowledges that some communities need significantly more support than others.
Until we address the fundamental funding crisis and the growing demand pressures on adult social care, more councils will follow Blackpool's path. The question is not whether this will happen, but when.
On a lighter note, have you sent in your "Afternoon Tea Week" entry yet? We'd be delighted to share your celebrations with us, and a £50 Marks & Spencer voucher awaits the winner. You have just 5 more days to send us your celebration – just a small paragraph and a couple of photographs, and "That's it"! (See page 9 for details.)
I can always be contacted at editor@thecareruk.com


(CONTINUED FROM FRONT COVER)
Conducting the investigation, the CQC examined nine areas spread across four themes, to assess how well the authority was meeting its responsibilities.
SIGNIFICANT SHORTFALLS
The regulator gave the areas a score out of four, with one representing “significant shortfalls”, and four showing an “exceptional standard”. The scores were as follows:
1. Assessing people’s needs: 1
2 Supporting people to lead healthier lives: 1
3. Equity in experience and outcomes: 1
4 Care provision, integration and continuity of care: 2
5. Partnership and communities: 2
6. Safe pathways, systems and transitions: 2
7. Safeguarding: 1
8. Governance, management and sustainability: 1
9. Learning, improvement and innovation: 1
The statistics exposed the difficulties the council face: Blackpool received 2,980 support requests per 100,000 working-age residents in 2023-24, compared to the national average of 1,785. For older residents, the figure reached 15,795 requests per 100,000 people aged 65-plus, substantially higher than England's 13,285 average.
NATIONAL AVERAGES
The CQC identified a fundamental shift away from preventative care towards crisis intervention.
Data reveals Blackpool supports significantly more residents in longterm care arrangements – 1,465 working-age adults and 9,185 older people per 100,000 – compared to national averages of 855 and 5,185 respectively.
Inspectors found limited evidence of strategies to reduce or delay care needs. A prevention strategy had remained in draft form for over a year without implementation, while practitioners rarely considered how interventions might reduce future support requirements.
The assessment highlighted particular concerns around reablement provision – services crucial for preventing unnecessary care home admissions. Only 60% of Blackpool residents completing reablement programmes avoided subsequent long-term support, compared to 79% nationally.
Hospital discharge outcomes also fell short of standards. Just 78% of older residents remained at home 91 days after discharge into reablement services, against an 84% national benchmark. The CQC noted declining reablement uptake and fragmented service delivery, with therapy services delivered through NHS trusts rather than integrated council provision.
The inspection revealed concerning trends in permanent care home placements, with rising admissions among working-age adults. Some
reablement staff reported that existing care package holders were inappropriately excluded from services, contradicting official guidance.
The regulator also identified significant disparities in service quality across different user groups. People with learning disabilities and autism faced the longest delays for Care Act assessments, while LGBTQ+ residents encountered barriers highlighted in previous reviews that remained unaddressed.
Inspectors noted what they termed "a culture of making decisions for people" rather than supporting individual choice. Two care home residents specifically told inspectors their placements did not reflect their preferences, while partner agencies reported that assessments sometimes proceeded without meaningful service user involvement. The report identified systemic safeguarding weaknesses affecting the care sector. Partner organisations, including care providers, reported poor communication about referred concerns, with unclear feedback on whether issues met investigation thresholds.
Delays were evident in processing Section 42 safeguarding enquiries under the Care Act 2014, from initial assessment through case allocation to conclusion. While improvements were noted during the March 2024 inspection period, the regulator remained concerned about harm reduction for adults awaiting case outcomes.
Staff consistently reported lacking confidence in safeguarding work, with no specific induction or competency training identified for this critical area.
The inspection found limited senior management oversight of frontline practice. Some practitioners received one-to-one supervision only every six months, with others missing six-weekly supervision targets. Leaders attributed gaps to workload pressures, though electronic monitoring systems remained unimplemented.
James Bullion, CQC’s chief inspector of adult social care and integrated care, said: “When we carried out our assessment of Blackpool Council, we found stronger leadership was needed to drive rapid improvements in how people were able to access adult social care services across the borough.”
“Strong leadership is especially important given the authority needs to make these improvements against a challenging backdrop. Blackpool is the most deprived local authority in England, and five areas in the borough have NHS priority ward status due to the level of deprivation and health inequalities. Leaders weren’t working well with partner organisations to provide person centred care and tackle these inequalities. This meant the authority weren’t able to ensure people had access to the care or support they needed, which was having a negative impact on their health and wellbeing”
“We have told leaders at Blackpool Council where they need to improve, and we expect to see rapid and widespread improvements
when we return.”
Cllr Neal Brookes, Deputy Leader of Blackpool Council and Cabinet Member for Adult Social Care, said: “This report is a difficult read and we take the findings exceptionally seriously. “Adults in Blackpool deserve the highest quality of care when they need it and I am committed to putting the processes in place to make sure that happens.”
“There are areas of good work highlighted in the report, including the care and passion of our staff. In fact Blackpool Council performs well and above average in most of the government’s surveys looking at adult social care performance, including people’s satisfaction of care. “But there are also areas where we need to improve and do better. We won’t shy away from the work we need to do.”
“Our independently chaired improvement board is already meeting and we will be assessing each risk that has been raised by the CQC and addressing it. “It is very important to note that the inspectors found no evidence to suggest adults were unsafe. “Our staff have focused on keeping people safe and solving their immediate problems, but we need to do more to work with people to create care packages that are tailored to them.”
“Care users will be at the heart of our improvement journey and their lived experience as recipients of our care will shape our future actions and processes “Blackpool has an above average number of adults requiring care, but below average funding to deliver that support. While the funding deficit is not an excuse for having the right processes in place, the demand for adult social care services will continue to grow in the near future as our population gets older. With that aging population brings even more pressure on our processes and staff.”
Blackpool Council has informed key stakeholders of the judgement, including the independent chair of Blackpool’s Safeguarding Adults Board.
The Safeguarding Adults Board includes key partners involved in protecting adults across the town, including the NHS trusts, police, fire service, ambulance service and others. Its role is to ensure all parties work together to ensure vulnerable people are protected and safe. Stephen Chapman, Independent Chair of the Blackpool Safeguarding Adults Board, added: “I have received a copy of this inspection report and read it in full. “There are areas of concern and work to do to improve processes. However, I have spoken to the council about the improvement plans. I have confidence that the council is committed to putting the foundations in place to correct the concerns raised, and the board is ready to play its part in supporting the improvement plan.”

By Charlotte Greatorex, Associate, Devonshires (www.devonshires.com)

The Care Quality Commission (CQC) has published new local authority assessments, focusing on how local authorities (LAs) meet their responsibilities under Part 1 of the Care Act (2014), ensuring access to adult social care and support.
The CQC evaluates nine areas across four key themes. Each area is graded on a scale from 1 to 4, with 1 representing a significant shortfall and 4 indicating exceptional standards. Once a score of 1 –4 is awarded, the ratings are converted into a percentage, with 25 to 38% = 1 (Inadequate), 39 to 62% = 2 (Requires Improvement), 63 to 87% = 3 (Good), and over 87% = 4 (Outstanding). In looking at the CQC gradings, local authorities are being assessed as falling short in some clearly identifiable areas.
The first theme the CQC evaluates is the way in which the LA works with people. This theme includes three areas: assessing needs, supporting people to live healthier lives, and equity in experience and outcomes, but in recent assessments, most LAs scored 2. This was often due to poor record keeping, limited access to equipment or digital services, and difficulties recruiting the right staff.
What is clear from the gradings is the areas the CQC values, and addressing these areas can provide higher scores. The CQC awarded higher scores to LAs that offered strength-based assessments centred around people to deliver personalised care plans. Where staff were qualified in their specialist area, with strong multi-disciplinary and inter-agency working, the CQC also awarded higher scores, particularly with good use of advocacy services and communication aids. LAs that used clear triage systems and had a strong understanding of the local population to prioritise cases and facilitate access also scored highly.
PROVIDING SUPPORT
In contrast to the theme above, LAs in recent assessments largely performed well in this area. Common themes included in the assessments included effective methods of commissioning and monitoring services, diverse support with adaptable resources, and strong sense of community, with understanding of local needs, regular contact, and strong and respectful relationships.
However, there were also issues recognised in the provision of support. Aside from the usual improvements to be made in record keeping and training, the CQC found that there remains a significant shortage of
residential care and nursing homes, and the delivery of care and support is not meeting the demand. This is not a new problem and ultimately will continue to come down to the cost of provision and funding.
When reviewing recent assessments, this theme has been a mixed bag when looking at scores. Well-performing LAs have a clear understanding and robust management of the risks people face in care. They regularly monitor risks, ensuring multi-disciplinary working with shared learning. Regular audits are conducted to identify risks with good responsiveness to feedback and good links with transition teams and health partners to ensure safe hospital discharges.
Yet there are still areas where improvements were identified as necessary. These include access to systems and record keeping, as well as staying up to date on procedures such as hospital discharges, in order to ensure the correct care and support is in place. Staffing gaps were also an area of concern, particularly in regard to the transition from children’s care to adult care services
Recent assessments showed most LAs performed well in this area, all scoring 3. This theme incorporates governance, management and sustainability, as well as learning, improvement and innovation. To improve performance to a score of 4 however, suggested areas for more growth included increasing the oversight of externally commissioned services and audits, as well as improving mechanisms for risk review with higher training levels for safeguarding. In a broader sense, improving staff involvement understanding of organisational operation was also an area to be bettered.
In recent evaluations, most LAs scored 3, falling within the “Good” range. However, some areas scored lower, reflecting common challenges, such as record keeping, adequate systems, access to care and support, recruitment, staffing and training, and community engagement. This perhaps suggests the key areas important to the CQC when assessing the provision of care from local authorities.
These common issues are often linked to funding constraints which affect staffing, training and the availability of care and support services. Time is another key issue: LAs need sufficient time to update records, recruit and train staff, and strengthen community relationships.
While many LAs are performing well, ongoing challenges in record keeping, staffing, and funding continue to affect their ability to meet demand for care services. The CQC’s assessment process is ongoing for many LAs and will be uploaded to the CQC’s website in due course, no doubt providing further detail on the problem areas in care provision.
A Fleet care home resident scored big when he returned to his favourite football club.
Peter Swan, 92 and resident at Care UK’s Bourley Grange on Bourley Road in Church Crookham, is one of the oldest and longest-serving Chelsea FC fans.
When the team members at the home heard about Peter’s wish to visit their stadium for the first time in 60 years, they reached out to the football club to organise a special surprise.
Peter was given the full VIP experience during his trip to Stamford Bridge, enjoying a tour of the dressing room, press room, players’ tunnel and pitch
Peter said: “I always loved watching the cup finals between Liverpool and Manchester United as the crowds used to go crazy.
“When I walked onto the steps and looked out at the football pitch, it all came back to me – all the cheering and singing.”
Peter’s special day was part of the home’s Wishing Tree initiative, which enables residents to put forward their desires to revisit old

hobbies or try something completely new.
To show his appreciation, Peter wrote a letter to the team at the home.
It read: “I would like to thank the staff of Bourley Grange for organising a wonderful day out to the home of Chelsea FC.
“It’s over 60 years since I last watched a match at Stamford Bridge, and the place has changed beyond belief.
Many thanks to Chelsea Harris for organising it and a special thanks to Sajal and Paul for looking after me. It really was a dream come true.”
Racquel Merdegia, Home Manager at Bourley Grange, said:
“Peter is a massive Chelsea fan, so we knew we had to do something special for him to get him back to the place where he has many happy memories.
“I’d like to thank the team for working hard to make this day a reality for Peter. It was great to see him reconnect with something he has such a deep love for. He was truly in his element at the stadium.”
In April 2025, the Supporting the Provider Market (STPM) team in County Durham published a new report evaluating the use of pobroll® — a waterproof bed-bathing wrap designed to improve dignity, comfort, and ease during personal care.
This evaluation was carried out across 10 care homes with high numbers of residents living with dementia. Each setting was given one or more pobroll® units and invited to share feedback through a structured survey. The findings reveal how even simple tools can make a significant difference in everyday care.
How was pobroll® used?
Most care homes used pobroll® daily or several times per week, showing it quickly became part of regular practice. Staff noted that one of the biggest challenges was not having enough units — all homes requested additional stock after the trial, highlighting a clear appetite for wider adoption. What did care teams think?
Feedback from the care homes showed strong support for the tool:

Ease of use was rated highly, with an average score of 4.4 out of 5. Staff found pobroll® straightforward to incorporate into care routines.
Training was rated slightly lower, at 3.8 out of 5, suggesting that while the wrap is easy to use, additional training resources could improve onboarding for new users. Resident response was positive. Three in ten care homes reported improved mood or behaviour during bed
Written by Pat O’Brien of pobroll
bathing for dementia patients.
• Key benefits included greater warmth, coverage, and dignity for residents, especially those who might find conventional methods distressing. Some teams also found it particularly useful for end-of-life care
Would they recommend pobroll® for bed bathing for dementia patients?
Absolutely. Homes rated their likelihood to recommend pobroll® at 4.3 out of 5, with half of respondents giving it a full 5 out of 5. The overall feedback was clear: this is a valued, meaningful addition to personal care.
Would they recommend pobroll® for bed bathing for dementia patients?
The results of this trial reinforce what many professionals already believe — that small, thoughtful design changes can significantly improve care. For residents who are bedbound or living with dementia, personal care can often be a distressing experience. But with the right tools, it doesn’t have to be. The pobroll® isn’t a complex device. It’s a simple, dual-layered cotton towelling wrap. But its thoughtful design — offering full coverage, comfort, and support — makes a real difference where it matters most. If you’re part of a care home, hospice, or hospital and would like to explore how pobroll® could benefit your residents or service users, get in touch. We’re here to support compassionate, dignified care — one small change at a time. See the advert on the facing page for details, or visit www.pobroll.co.uk
One of the sector’s most recognisable voices has delivered an uncompromising message to Government: stop the rhetoric and start providing proper funding for social care.
Nadra Ahmed CBE, Chair of the National Care Association and a nationally recognised leader with over four decades in the sector, has launched a blistering critique of Government policy, warning that the social care crisis is worsening despite official claims of increased investment.
Speaking on Newcross Healthcare’s Voices of Care podcast with host Suhail Mirza, Ahmed revealed the frustration that drove 250 care providers to take unprecedented action earlier this year.
“We had about 250 people on a call saying, we’ve got to do something. Let’s go march on Parliament,” Ahmed revealed, describing the moment that sparked the Providers Unite movement – a watershed moment for a sector that felt words were no longer enough.

The march represented thousands of care professionals taking their concerns directly to the Palace of Westminster in an unprecedented show of unity and defiance.
Ms Ahmed pulled no punches when addressing Government announcements about increased social care funding, declaring bluntly: “somebody is not telling us the truth” about whether additional funding is actually reaching frontline providers.
“When it comes to the frontline, the money is insufficient – that’s a polite way of saying it,” she stated. “The reality is, it’s not even a drop in the ocean. Someone in there is lying.”
At the heart of her message lies a fundamental challenge to how social care is perceived within the broader health and care system.
“The role of social care is not only to support the NHS, it is a role in its own right,” she declared. “They only invest in us to support the NHS.”
This struggle for recognition comes as the sector faces mounting pressures, with Ahmed highlighting that “we’re probably closer to about three quarters of a million people who can’t even be assessed for social care.”
Ms Ahmed emphasised the increasing complexity facing care homes and domiciliary providers: “We’re looking after people who have very complex healthcare needs. And the need is growing.”
This growing complexity coincides with what Ahmed describes as a disturbing abandonment of vulnerable people: “We’re allowing, enabling, by keeping quiet, vulnerable people to be ignored.”
The NCA Chair didn’t spare the Home Office from criticism over visa policy changes that have exacerbated workforce shortages in the sector.
“I would say the Home Office got it wrong when they first put the visas out, they should have been much more careful and we wouldn’t have had this problem,” Ahmed stated.
Despite the challenges, she remains passionate about the sector’s mission: “Why would you be a carer? You’d be a carer because it’s one of the most rewarding jobs that you’ll ever do.”
However, she insists systematic change is needed: “They need to have the professional ladder, they need to be paid properly. And all of that should be funded through government.”
When challenged about her outspoken approach, Ahmed was characteristically direct: “As soon as you raise your head above the parapet, there’s always somebody to shoot it down. So is it going to shut me up? Is it hell.”
Ms Ahmed’s message cuts through political rhetoric with stark clarity: “Social care has continued to deliver, continues to deliver and does not need fixing. It needs to be funded.” She added.
Godden Lodge Care Home in Benfleet, Essex, part of the HC-One family, recently opened its doors to the local community for a special Coffee Morning, bringing together representatives from local organisations for a morning of connection, conversation, and collaboration. Guests included representatives from Stibbards & Sons, Paul Robinson Solicitors, Abbey Funeral Services, The Salvation Army, and Thundersley Methodist Church. The event provided a relaxed setting for attendees to share ideas on how best to work together for the benefit of the community and the people each organisation serves.
Home Manager Lewis Chester welcomed attendees and gave a short presentation on Godden Lodge, highlighting the care and support the home provides. Julie Barnard, Senior Activities Coordinator, spoke about the variety of activities and events available to residents, before leading a guided tour of the home.

Throughout the morning, guests enjoyed freshly brewed coffee and tea, accompanied by an assortment of delicious cakes and biscuits, while engaging in friendly discussions and exploring opportunities for future partnerships.
Speaking after the event, Lewis Chester said:
“We were delighted to welcome so many members of the community into our home. Events like this help build stronger relationships between local organisations and give us the chance to share ideas that will benefit everyone. We look forward to continuing to work together for the good of our residents and the wider community.”
Godden Lodge Care Home is committed to being an active part of the local community and plans to host further events to strengthen these valuable connections.


Working as a carer, whether that be as a paid carer or unpaid carer for a family member, can be challenging for some people’s mental wellbeing. It has been reported that many of those who work in the care sector are experiencing burn out and other negative emotions whilst working in the profession.
But how can you take steps to negate these feelings and look after yourself and the person you are caring for? Michael Berkley-Blezard at the Elmfield care group home Old Sarum Manor (www.elmfieldcare.co.uk/old-sarum-manor), shares his tips for protecting your wellbeing when working in care.
THE SIGNS OF BURN-OUT
Michael says: “Becoming burnt-out is something that happens over time, and the signs can include anxiety or depression. These can show up at work and at home and symptoms include severe exhaustion, feeling cut off from others, having no hope, energy, or reason for things to change.
Burnout can also look less obvious, for instance being unusually forgetful, catching more colds than usual, struggling to make simple decisions, or even feeling guilty for taking breaks. Sometimes carers don’t realise they’re burnt out because they don’t recognise the less common signs.”
1. TAKE TIME FOR YOURSELF
Michael shares: “Taking time for self-care is essential in preventing burn-out. This can look different for different people but simply taking time to exercise, focusing on proper nutrition and establishing a sleep
routine will all help to make you feel more regulated.
“Trying to spend time doing hobbies is also a great way to practice self-care. Whether it be reading or playing 5-a-side with your friends, it can help you feel more like yourself. Even if you can only do it for a couple of hours a week, it is important to carve out that time for yourself.”
2. SPEAK UP
Michael explains: “Whilst it may feel difficult, sometimes the best thing you can do is talk. Whether it be to your friends and family or you seek out additional support. Charities such as The Care Workers charity, Carers trust and Carers UK are accessible for all carers across the UK.
“If there is a serious issue or matter that is affecting your mental health and needs to be resolved, this is when you need to take things higher up to your manager or wider management. This will allow for any significant and drastic issues to be dealt with in a professional way, which will also take some of the pressure and stress off yourself. Whilst it may be tough to do this, it is always the route to take to ensure that problems are solved properly and stops them from impacting on your personal wellbeing.”
3. KEEP LEARNING
Michael says: “Knowledge is power, sometimes learning and developing is a great way to support your mental wellbeing and reduce the likelihood of burn-out. This is for multiple reasons, one being that attending training courses may help you understand why situations are dealt with in a certain way. This will help you learn best practices which as a result, can lessen the stress associated with trying to make the right decision. A second reason being that continuously learning and widening your scope helps to keep your days varied and more exciting.
“You can also join support groups and learn from other people’s experiences, and share your knowledge with others. Connecting with other people in the same industry or position as you also creates a sense of community, which is seen to be beneficial in supporting men-
tal wellbeing.”
4. REFLECTION TIME
“Taking time to reflect on your day or week, or maybe month if you struggle to find time for it, is a great way to be able to check in with yourself and identify how you are feeling before you reach the point of burn-out,” Michael explains. “Journaling and writing down your thoughts, feelings and things that have happened allows you to process and understand them more.
“Whether you're an unpaid carer or working within a care home, remembering the importance of what you do and how you care for and support the people you look after also helps to put feelings into perspective.”
5. SET BOUNDARIES
Michael says: “Whilst it can be difficult, it is essential to advocate for yourself and your mental wellbeing and know your limits before you do become burnt-out. If you are consistently working more hours than you are supposed to or you are not taking any time to do activities that you enjoy, you need to be able to recognise this and try and put a stop to it.
“The simple act of only working your set hours and trying to not think about work or talk to people from work when not there, will contribute greatly to finding a work-life balance which ultimately leads to better mental-wellbeing and prevents burn-out. If you are an un-paid carer, respite care could be something that may benefit you and the person you care for.”
Karolina Gerlich, CEO of The Care Workers’ Charity, shares: “Looking after your wellbeing as a care worker is vital, not just for your own health, but for the people you support every day. The emotional and physical demands of care work can be overwhelming, and without proper support, burnout becomes a real risk. At The Care Workers’ Charity, we’re here to ensure no care worker faces those challenges alone. Whether it's through mental health support, financial grants, or simply a listening ear, we are committed to helping carers take care of themselves, too.”
We are delighted to share that Jubilee Court Care Home, part of the Runwood Homes Group has attained the GSF Accreditation Quality Hallmark Award following a successful GSF Accreditation Assessment. This recognition highlights the home’s commitment to ensuring residents live with dignity and comfort until the end of their lives.
The evaluation praised Jubilee Court for its exceptional clinical care, compassionate support for families, and comprehensive approach to social and emotional wellbeing. The inspection report noted, “A high level of excellence in clinical care for residents to ensure that they are comfortable and that their symptoms are managed proactively. Social and emotional care is embedded in daily routines, with activities adapted for those who remain in their rooms.”
“Compassionate, dignity-enhancing care is delivered by all staff, who are supported through reflective practice and self-care within a compassionate culture.”
Heather Limb, Home Manager at Jubilee Court said, “The entire team have

worked incredibly hard to meet the standards showcasing the outstanding, person-centred and compassionate care provided to residents and their family members. This accreditation reflects the tireless dedication of our staff. From nursing and care staff to our lifestyle coordinators, everyone at Jubilee Court works together to ensure residents and their families receive the highest standard of care during such an important stage of life.”
The home’s staff have been recognised for their outstanding efforts with a celebratory event, and a wider community party is planned to share this achievement with residents, families, and local supporters.
Jubilee Court Care Home continues to set the standard for excellence in palliative and end-of-life care, demonstrating dedication, professionalism, and a deep commitment to its residents and the local community.
The whole team were incredibly proud of their accomplishment and celebrated with delicious pizza.
In retail, bigger is often equated with better. But in continence care, size alone does not equal performance. What matters is fit, appropriateness, and clinical suitability. At Ontex, we believe continence care should be clinically sound, cost-conscious, and centred on the individual. We support care providers through practical training, formulary-aligned product design, and assessment-led solutions that preserve dignity and comfort.
Addressing Common Misconceptions in Care Settings

Here are some frequently encountered misconceptions about absorbent continence solutions:
1. "The bigger the resident, the bigger the pad."
This is a frequent misunderstanding. Correct sizing depends on accurate waist, hip, and thigh measurements. In many cases, a smaller, well-fitted solution provides better containment. Selection should also be based on the individual’s continence profile and type- not just physical stature.
2. "Belted products fit anyone if tightened enough."
Tightening at the waist does not guarantee security around the legs.
A proper fit should allow a one-finger gap at the leg and a two-finger gap at the waist. Belted options are often higher-cost items and should be used only when clinically appropriate.
3. "Double padding keeps residents drier."
Layering pads undermines containment. Once fluid reaches the
waterproof backing of the upper pad, it is diverted laterally often leading to leaks, moisture-related skin compromise, and reactive containment changes that increase staff burden. A single, well-matched product is always the safer choice.
4. "Pull-ups are the best option for everyone."
Pull-on formats suit some profiles but may hinder others. They are not ideal for individuals with reduced dexterity or limited mobility. Two-piece systems offer greater flexibility and allow for the use of personal
underwear—supporting comfort, autonomy, and dignity.
Why Assessment Is Essential
A thorough continence assessment rather than assumption-based product selection is key to improving outcomes, optimising cost, and protecting resident wellbeing.
Key Assessment Components:
- Measurements: Capture accurate waist, hip, and thigh data. Always refer to product-specific sizing guidance.
- Bladder Diaries: Maintain a 3-day fluid intake and output record to determine actual absorbency needs. This often reveals a lighter option may suffice.
Clinical and Operational Benefits:
- Prevents unnecessary product usage
- Reduces reactive containment changes
- Minimises moisture-related skin issues and infection risk
- Improves comfort, dignity, and independence for residents
Our guidance aligns with NHS England policy on absorbent containment: assessment-led provision, a maximum of four pads per 24 hours unless clinically justified, and prioritisation of adaptable two-piece systems wherever appropriate.
Broader Considerations
- Infection Risk: Continuous use of containment products without regular reassessment can increase the likelihood of urinary tract infections. A structured, assessment-led approach helps mitigate this risk.
- Skin Health: Selecting the right containment format supports skin preservation. Regular skin checks should accompany each pad change.
- Cost and Resource Efficiency: Product selection tailored to individual need reduces waste, optimises staff time, and supports broader NHS resource stewardship. NHS formularies consistently prioritise flexible, fit-for-purpose solutions.
Final Thought
In continence care, assumptions cost more than time they impact dignity, safety, and outcomes. Assessment-led, evidence-based selection reflects best practice and ensures the right solution, for the right person, at the right time. Want to support your team with continence product fit checks or product training delivered by our Nurse Advisors? Ontex provides practical resources and training, tailored to your care setting. Contact your local nurse advisor to arrange a session. For further information
Crisis and inpatient mental health services require a major overhaul to provide care which is timely, compassionate and effective, a new report has said today.
Crisis and acute mental health care by Centre for Mental Health says that people in a mental health crisis are facing a postcode lottery of care, with certain groups (including children and young people) sometimes unable to access care suited to their needs.
Crisis and acute mental health care summarises research from the NIHR Policy Research Unit in Mental Health about ways of supporting people in a mental health crisis. The report sets out the evidence about community-based alternatives to hospital care (such as crisis houses, day units, home treatment teams and crisis cafes), which enable people to get support closer to home.
But it finds that the provision of alternatives to hospital care is inconsistent, and what’s commissioned doesn’t correspond with the available evidence of what’s effective.
The report says that rising levels of need for emergency mental health care, coupled with short-staffing and dilapidated buildings in inpatient services, are placing current systems under major pressure. And too often, people’s experience of inpatient care can be coercive and re-traumatising.
The report comes in the midst of major challenges in crisis care, with people in a mental health crisis twice as likely to wait over 12 hours in an emergency department. And the withdrawal of police from some aspects of crisis care – driven by the ‘Right Care, Right Person’ approach – has exacerbated pressures on
Residents at HC-One’s Fosse Way View Care
Home, in Bingham, Nottingham, raised their glasses last week to celebrate International Beer Day in style, with a special visit from one of Bingham’s best-known locals – Niall from The Wheatsheaf.

As the oldest pub in Bingham and freshly crowned Vale of Belvoir CAMRA’s Pub of the Year 2025, The Wheatsheaf is steeped in local history and beer expertise. Niall gave an engaging and informative talk to Fosse Way View residents, lifting the curtain on life behind the bar – from caring for the pumps to explaining why a cloudy pint is no
longer something to send back.
Resident Pat Weightman shared memories of their time running a pub in Newcastle named The Robin Hood, while resident James Hutton happily sampled a taste of the past with a pint of Shipstones Original, generously brought in by Niall for residents to try.
Fiona Benning, HC-One’s Fosse Way View Wellbeing Coordinator, said: “It was such a lovely afternoon – not just for the beer tasting, but for the stories, laughter, and sense of community it brought. We’re so grateful to Niall for taking the time to bring the pub to us – without the walk home!”
individuals, families and services.
Crisis and acute mental health care says that major investment in services, staffing and buildings is needed to move towards compassionate and timely care in a crisis.
However, it also cautions that superficial changes or tokenistic attempts at reform will fail to achieve systemic change.
Andy Bell, chief executive at Centre for Mental Health, said: “Acute and crisis care are essential elements of our mental health care system. At their best, they save lives and are there for people when they most need urgent help. Too often, however, people struggle to get help in a crisis, and many report that their experiences of crisis care and hospitalisation create traumas of their own.”
“We urge the NHS to invest effectively in mental health crisis care, addressing gaps in provision and updating estates which are no longer fit for purpose. But we also need a radical rethink of inpatient and crisis care to achieve the Government’s ambition of shifting treatment from hospital to communities. To do this, the NHS needs to invest in what works and ensure provision is consistent across the country.”
“At a time of limited budgets and rising need, we urge the Government to invest in evidence-backed interventions to better support people in a mental health crisis. Before embarking on plans to build new ‘mental health emergency departments’, it must ensure that investment is used wisely to provide the right help in the right places.”


By Emma Streets, Associate Director, Tigerbond

The care sector’s ability to achieve mainstream media attention continues to grow. The combination of high public awareness of its challenges, links to the NHS and sensitive, highly emotive individual stories make reputation management increasingly important to consider for the independent care homeowners and operators that account for 90% of the market today*.
With individual stories and homes often subject to the court of public opinion, and news frequently being shared across multiple channels, from family WhatsApp groups to social media, managing communications when an issue arises is complex and requires speed and efficiency to reach the relevant audiences whilst monitoring ongoing conversation.
Safety failures are the most common theme that generates huge visibility and can not only negatively impact individual home reputations but also tarnish the sector. Understanding the complex care system is a message that can be lost in translation when news reaches the general public and headlines are designed to attract maximum attention and clicks.
However, there are steps that can be taken to mitigate reputational risk and ensure that you’re approaching communications issues with a clear process and perspective that includes awareness of how the media landscape works in 2025.
For example, CQC reports adopt a typical process that includes right of reply within set timeframes.
Communications experts can support within this process to ensure that any potential media interest is prepared for in advance and then managed once the report is published with agreed statements and language that is based on fact and accuracy. This ensures that your stakeholders, including the public, have your full response and that you’re prepared for questions that may arise, from press to Facebook comments.
Monitoring social media is particularly important to ensure that you’re aware of public perceptions as well as able to potentially rebuff false information when appropriate and pending investigations which can mean you’re unable to provide specific details.
Engaging with communications experts as part of your business planning enables these professionals to understand your organisation, processes and valuable context that can support future communications ahead of time. Context is crucial, particularly given the spread of false information online that’s being increasingly driven by AI generated content. Within the communications industry, this is a growing trend that brands are facing and given the nature of the care sector, it’s one that has many potential implications for individuals and their families.
Maintaining factual accuracy and ensuring your right to reply on historic media stories is another area where communications experts can add value, to ensure that the digital record is correct and that your online reputation reflects reality.
Given the pace of growth in the sector, aligned with the pace of change in the way that we communicate and consume news and information online, taking a proactive approach to reviewing how negative and positive news is shared for your brand across all your channels is an essential element of futureproofing your organisation.
* Sources: Carehome.co.uk: Care home stats: number of settings, population and workforce Care homes for older people, UK market report (34th edition), LaingBuisson 2024
Residents and team members at Chorleywood Manor Care Home recently completed a charity event to raise crucial funds for Great Ormond Street Hospital’s new children’s cancer centre.
The team took on a 10-mile journey, crossing 10 London bridges, starting at Vauxhall Bridge and finishing at Tower Bridge.
The aim was to raise £2,500 to support the hospital’s work in providing life-saving treatments for young cancer patients. Thanks to generous donations and the determination of everyone involved, they surpassed this goal, raising a total of £3,800.
Nicole Moosbrugger, CCC Project Support Officer, and her team, including Diana Saenz-Herrera and Lottie from Great Ormond Street Hospital, visited Chorleywood Manor Care Home to collect the cheque.
The donation was proudly presented by residents Eric, Yvonne, Jill, Joyce and Shirley, who all took part in the fundraising efforts.
The event, organised by Chorleywood Manor Care Home, part of Avery Healthcare, one of the UK’s leading providers of residential, dementia, and respite care, demonstrated the care home residents’ incredible determination.

During the cheque presentation, the team from Great Ormond Street Hospital took the time to speak personally with each resident involved in the walk. They listened as residents shared stories from their 10-
mile adventure, recounting memorable moments from the day, the bridges they crossed, and the friendships that kept them going.
Resident Eric Heather, aged 93, said, “This was about showing that we can still contribute, no matter our age or ability.”
Fellow resident Yvonne Field, aged 89, who has faced mobility challenges following a stroke, said, “I didn’t let anything stop me from participating. I wanted to make a difference for these children.”
“We knew this walk would be a real challenge, but the incredible team spirit among our residents, staff, and supporters made all the difference,” said Patrick Maher, Well-being Manager at Chorleywood Manor Care Home. “The way the local community rallied behind us was truly heart warming; their encouragement kept everyone motivated from start to finish.”
Great Ormond Street Hospital (GOSH) is one of the largest paediatric cancer centres in Europe, treating over 400 children with cancer each year.
Funds raised through this challenge will help create a state-ofthe-art children’s cancer centre at GOSH, bringing together worldleading research and specialised care in one place.
Eric added, “I’m proud to have taken part in this challenge. It’s been a meaningful experience, and I hope it encourages others to get involved and support such an important cause.”
Blueleaf, a leading provider of cleaning solutions, consumables, equipment and services to the care sector, is proud to announce a new strategic partnership with Renray Healthcare, one of the UK’s foremost manufacturers of furniture for healthcare environments. Together, they are launching a comprehensive range of care home furniture that combines outstanding quality with seamless service and delivery.
This collaboration brings together Blueleaf’s trusted nationwide distribution network and commitment to customer service with Renray’s decades of expertise in designing and manufacturing furniture that enhances care environments. The partnership aims to make it easier than ever for care homes to access stylish, durable and compliant furniture –delivered on time, fully assembled, and ready for immediate use.
Ellen Brown, Sales and Marketing Director at Blueleaf, commented:
“This partnership is about more than just products - it’s about ensuring our customers receive the highest standards of service from start to finish. Renray shares our commitment to the care sector and understands the importance of creating spaces that are both functional and homely. Together, we’re bringing furniture to the forefront - where quality products meet quality service.”

The new range officially launched in this month - July 2025, offering a wide selection of bedroom furniture, chairs, tables, and soft furnishings, all designed specifically for the needs of care home residents and operators. Each item reflects Renray’s design-led approach and Blueleaf’s understanding of what care homes need to operate efficiently and compassionately.
Nick Frogbrook, CEO of Blueleaf, added:
“At Blueleaf, we exist to help care homes run smoothly. This partnership allows us to expand that support with trusted furniture solutions that are built to last and backed by the high level of service our customers rely on.”
Jackie Dearden, Director of Renray, commented:
"Our new collaboration reflects a mutual commitment to advancing healthcare through smarter solutions, greater efficiency, and unwavering dedication to those working in care."
For more information about the new Blueleaf furniture range, contact your Blueleaf account manager or reach out at:
T: 0330 55 22 88





As the summer months unfold, care homes across the UK observed one of the most beloved celebrations of the year – Afternoon Tea Week, taking place from 11-17 August. This quintessentially British tradition, which has graced our culture since the 1840s, holds particular significance within residential and nursing care settings, offering far more than just a delightful culinary experience.
MORE THAN JUST TEA AND CAKE
Within the care home environment, Afternoon Tea Week serves multiple vital purposes that extend well beyond the obvious pleasure of fine food and drink. This celebration creates a natural opportunity for residents and staff to come together in a relaxed, social atmosphere where conversation flows as freely as the tea itself.
The informal setting encourages residents to share stories, connect with peers, and engage with care staff on a
anniversary of Victory over Japan (VJ)
Colten Care’s homes Abbey View in Sherborne and Newstone House in Sturminster Newton were decorated with Union flags, bunting and 1940s memorabilia for the occasion.
At Abbey View, residents enjoyed the opportunity to sing classic favourites at an afternoon concert in the garden led by Colten Care’s Music & Arts Partner Fiona Pritchard on vocals and guitar.
The list included Land of Hope and Glory, Pack up your Troubles, It’s a Long Way to Tipperary, Jerusalem, Daisy Daisy, White Cliffs of Dover and We’ll Meet Again. “Everyone sang with great gusto,” said Abbey View Companionship Team Leader Bev de Bruyn. “We’ve organised similar VJ Day anniversary events in the past and they’ve always proved very popular with residents sharing memories and reflecting on how their younger years were affected by World War Two and

its aftermath.
“This year, being the 80th anniversary of the end of the war, had added interest. What a profoundly heartwarming day we had, shared with our wonderful Abbey View family.”
Among the Abbey View residents who took part was 94-year-old David Froud, a former Captain in the Parachute Regiment.
As an ex-soldier, David was invited to address the garden gathering and spoke of the importance of honouring those who fought for our freedom.
Fellow resident Wendy Ash thanked Fiona and all involved in staging the anniversary event, adding: “Well done! That was just so lovely.”
Residents at Newstone House meanwhile took part in Sturminster Newton community events including a service of remembrance.
One resident, Tony, who served in the Navy, said: “You don’t know how much this means to me.”






The care sector is no stranger to demanding schedules. Long hours, irregular shifts and constant time pressures can make traditional classroom-based training a significant challenge for staff. However, the introduction of personalised, digital learning offers an innovative solution, which aligns with the unique demands of the care industry.
Caroline Evans, VP of Enterprise Sales at FutureLearn (www.futurelearn.com), discusses how mobile-first platforms and microlearning techniques are reshaping how care professionals acquire new skills and knowledge. Here, she explores the importance of personalised learning, and the benefits it can bring to care homes across England and Wales.
ADDRESSING UNIQUE NEEDS
Traditional, generic training programmes often fail to address the unique needs of individual employees. This lack of personalisation can limit engagement and significantly reduce the return on investment for learning spend. As an example, according to recent research, insufficient investment in soft skills alone is costing the UK £22.2bn annually.
When training programmes are irrelevant to their day to day roles, care staff may feel undervalued, leading to disengagement, poor knowledge retention and difficulty thriving in their roles. Ultimately, this contributes to a gap in skills that organisations struggle to close effectively.
MAKING PERSONALISATION SCALABLE
Advances in digital tools and data analytics have revolutionised corporate learning by making personalised training at scale a reality. For example, at FutureLearn, we apply learning management systems, artificial intelligence and data insights, to help care providers tailor training to meet the diverse needs of their teams.
The numbers speak for themselves. Research reveals that 74% of employees feel unable to reach their full potential due to limited development opportunities, despite 68% expressing a desire to embed learning into their daily routines. Personalised learning addresses this disconnect, by seamlessly integrating professional growth into everyday work.
Organisations can overcome key barriers, such as limited mentoring opportunities and difficulty in recognising individual skills gaps, by implementing personalised development plans. These tailored plans, which 96% of professionals deem valuable for career mobility, allow care staff to take actionable steps towards achieving their goals, while addressing organisational needs.
Personalised learning empowers care workers by giving them greater ownership over their professional development. By providing easily accessible, flexible and relevant training, which is tailored to individual roles and goals, care home leaders can help employees to build confidence and competency.
For a care worker managing demanding schedules and emotionally challenging work, digital platforms offer the advantage of flexibility. Training can be completed between visits, shifts or during short breaks, while bite-sized micro-courses can reinforce key skills, without requiring lengthy classroom sessions. McKinsey highlights that “the most effective organisations encourage personalised, adaptive learning.” By connecting training directly to daily responsibilities and career progression, organisations can boost motivation and engagement, helping care professionals feel more invested in their work and development.
When learning is deeply integrated into the flow of work, and tailored to meet the specific needs of care workers, the results are transformational. Personalised approaches can help to keep skills sharp, improve operational efficiency and support staff retention by fostering job satisfaction and career progression. For care homes across England and Wales, investing in personalised digital learning is more than an operational improvement. It’s an essential strategy for providing high-quality care, while valuing and empowering those who make it possible.
Residents at an Altrincham home made the short trip to the Imperial War Museum North to brush up on their modern British history.
Eight residents from MHA Handsworth, accompanied by staff and volunteers visited the museum.
They spent the day learning about modern British history, including artefacts from World War I and II.
Amongst the visitors were two residents who did national service in their younger days and recognised various medals, which were given to all civilians that did their national service.
In line with South Asian Heritage Month, the group watched an exhibition called ‘Chila Welcomes You’ which took them on a journey from a personal perspective of Indian migration to Britain after the Second World War.
MHA Handsworth provides residential care for our 43 residents. Charlotte Fowke, activities coordinator said: “ The trip came off the back of one of our residents who mentioned wanting to go to the Imperial War Museum North.
“I then asked around, put posters up around the home to get oth-

ers interested and away we went.
“It’s around 30 minutes away from us which isn’t too far at all.
“The visit lasted around four hours and we had a great time. The residents really enjoyed learning and taking in all the facts.
“The residents spoke about their own memories of wars and recognised items that they had themselves used when they were carrying out National Service.
“Hearing their stories and the memories from times such as the war was really nice and helped us to get to know the residents a little better.
“We spent time watching short videos that have been created for the museum’s use which gave us an insight to the sounds and emotions in the battlefields.
We ended our trip with a talk on the different helmets used by different countries where residents were encouraged to try on and handle the artifacts.
“It was a lovely trip out, one that was enjoyed by us all, and definitely something we would do again.”
Residents at an Ilkley home can visit places such as Scotland and the North York Moors without leaving their home thanks to a new train experience.
MHA Glen Rosa have installed the Jolly Journey Train Experience, a new initiative by Little Islands, who specialise in creating unique interactive environments.
The train experience showcases journeys across the UK from the viewpoint of a passenger looking out of the window.
The team from Little Islands installed and decorated a part of the home’s dementia unit and converted it into a train carriage with props such as suitcases, train times and journey information displays.
MHA Glen Rosa provides residential and residential dementia care for 47 residents.
Adam Carling, home manager said: “The Jolly Journey Train experience is a new initiative and one that is proving to be very popular here.

“We have received some great feedback since the experience has been installed.
“Our residents love it, you will often see a number of them sat in the carriage and watching a journey.
“The idea came to me from my area who forwarded it to me, and I decided to look into it.
“I then contacted the team at Little Islands and the whole process took a couple of months from start to finish.
“We are quite privileged here at MHA Glen Rosa, where thanks to the generosity of the local community we are able to provide services such as this for our residents.
“We received a very generous donation via our Legacy Fund which enabled us to go for this experience.
“The location of the experience is really good as it’s in a high footfall area, where both residents and their relatives can sit and enjoy it.
“Alongside the Train Experience, we have also prepared a sensory garden thanks to funds we received.
“I do think this is something other MHA homes can look into having, it’s something quite unique and I
More than 10,000 people have signed a petition demanding the UK Government gives unpaid carers the legal right to a break, following a one-of-a-kind protest outside Parliament.
The petition, set up by national charity Carers Trust and Uncommon Creative Studio, calls for carers in England to have a right to access properly funded replacement care and a break away from their caring role. Signatures surged past the 10,000 mark in a matter of days and the campaign is now backed by more than 12,000 people.
The petition was launched on 22nd July – just before MPs headed off for recess – in a unique protest which saw carers holding up placards in their living rooms and kitchens saying what they’d do if they had time for a break. It made the point that they can’t protest in person because they’re too busy caring.
Films of eight carers holding up placards, along with pictures of scores of others, were broadcast on giant LED screens mounted on vans which drove around Parliament.
The protest was created by Uncommon Creative Studio and national charity Carers Trust. The petition will remain open for signatures until it is handed in to the Department of Health and Social Care next month.
A survey of unpaid carers in England has shown two-thirds (67%) said even planning a holiday feels like a pipe dream, while 60% reported feelings of burnout. Almost 1 in 3 (29%) rarely take a respite break, with 1 in 7
(15%) admitting they never take a break from their care duties.
Kirsty McHugh, CEO of Carers Trust, said:
“We’re delighted that over 10,000 people have already added their voice to our petition. This shows just how urgent the issue is. Carers are exhausted and face relentless demands, often having to give up their jobs to look after those family and friends. Despite this, they don’t get nearly enough support in return.”
“The UK Government now needs to listen to the British public and ensure carers are able to take a break from their caring role. If they don’t, many more will face burnout which will only heap even further pressure on our struggling health and social care system.”
Duncan Clark, Creative at Uncommon Creative Studio and part-time carer, added:
“I’ve been a carer for 15 years, but am fortunate enough to not only be paid, but able to take holiday, and return home after my shift has finished. I have endless respect for those who dedicate their lives to supporting those they love, but I’m really frustrated at the lack of support they are given by the Government”
“Unpaid carers aren’t asking for much – our research found that if they had some more time off, 44% would just want to get outside for a walk. This protest demands Government attention for unpaid carers, at a time when it feels like the whole country is getting a break, apart from them.”
DOVES took flight at a Saltburn-by-the-Sea care home as elderly residents commemorated the 80th anniversary of VJ Day with a symbolic tribute to peace.
Hazelgrove Court Care Home, on Randolph Street, marked the occasion with a dove release, chosen by residents as a meaningful way to remember the end of the Second World War.
Staff contacted Joanne Smith from Blessed with Wings, based in Billingham, who brought nine white doves to the home for the ceremony.
Six birds were released by residents and staff, while Betty Wood, 102, and Judith Pearson, 81, opened baskets containing three more.
Verses were read aloud before the release, including: “We release these doves as a symbol of peace and new beginnings.”

Sharon Lewis, activities coordinator at Hazelgrove Court Care Home, said: “The residents felt that releas-

ing white doves was deeply symbolic, representing peace and new beginnings, which everyone hoped and prayed for after the ending of the Second World War. The release of the doves was very emotional.”
Resident David Rigg, 78, who held and released one of the doves, said: “I felt as though I was setting the world free.”
Judith Pearson, 81, added: “Opening the basket and watching them fly brought a tear to my eye.”
Resident Ann Thomson, 87, shared her memories of VJ Day in 1945. She said: “I was seven and can remember going down to The Stray in Redcar with family where everyone celebrated round a bonfire.”
Everyone who attended the ceremony received an organic bag containing three white feathers to remember the occasion.
Among those present was Jules Walker, Veteran Friendly Framework (VFF) support project officer, who joined residents and staff for the tribute.

International real estate advisor Savills reports that the UK healthcare real estate market experienced a significant upswing in investment volumes in the first half of 2025.
The senior housing and care home sector saw £1.5 billion deployed, marking the strongest performance in a decade, according to MSCI data. Care homes led the charge, buoyed by robust private pay pricing, improved operator performance and favourable market dynamics.
Savills notes that international investors, particularly from the US, are increasingly targeting UK healthcare REITs that are trading at discounts to net asset value. Notably, US-based CareTrust REIT acquired CareREIT, while UK REIT Assura’s board initially recommended a bid from KKR and Stonepeak, before pivoting to a merger with PHP, which recently received a 63% majority vote from shareholders in favour. This wave of cross border activity signals significant confidence in the UK healthcare sector’s long term value and resilience.

Another area of strength in H1 2025 was the private hospital sector, fuelled by NHS outsourcing of elective procedures and rising private pay demand. Non-NHS inpatient admissions hit a record 939,000 in 2024, up 3% year-on-year and marking the third consecutive year of record volumes.
Despite positive sentiment, healthcare development activity remains subdued. Rising build costs, challenging debt conditions, ongoing planning constraints, and land values not adjusting to a more difficult macroeconomic environment have slowed development progress in the UK since 2022. New care home
delivery has primarily focused on private-pay schemes in London and the South, where development economics are more viable, exacerbating the existing North–South supply imbalance. This said, Savills suggests that signs of recovery, such as easing debt markets and renewed investor confidence are beginning to support new build pipelines.
Savills suggests that recent government initiatives including the Spending Review, UK Infrastructure Strategy, and the NHS’s 10-Year Plan have signalled renewed commitment to healthcare investment, with a focus on technology, primary and community care, and public private partnerships.
Caryn Donahue, Head of Senior Housing and Healthcare Transactions, Savills, says, “Investor interest in UK healthcare real estate remains very strong, supported by a stabilising macroeconomic backdrop and growing policy support for public private delivery, particularly in primary and acute care. In the care home sector, rising wages and immigration changes may put pressure on margins, especially for providers that are reliant on Local Authority funding, but private providers will see less impact.”
Tom Atherton, Strategy & Market Intelligence Manager, Savills, adds, “Strategies focused on private pay demand and operational upside remain well-positioned. With dry powder available and financing conditions improving, momentum in the UK healthcare sector is expected to continue as we head towards the end of the year and beyond.”
Featherton House care home in Deddington, Banbury, has collaborated with local florist Steve Wheeler to create beautiful, professional floral arrangements to raise money for chosen charity Breast Cancer Now.
Every few weeks, local florist Steve visits Featherton House to run hands-on floral workshops with residents to bring creativity and colour into the home. In each session, Steve works with around five residents who each receive a foam block and a selection of fresh flowers to create their own stunning arrangement.
The most recent session featured beautiful, pink-themed arrangements, honouring breast cancer awareness. These handmade displays now decorate the home with purpose and pride, and Steve kindly donated his own display as a prize in recent the coffee morning raffle, which raised £367 for Breast

Cancer Now.
It was a big success, with a wonderful turnout from friends, families, and the wider Deddington community. Guests were treated to live music by entertainer Vintage Ruby, as well as tea, coffee, and a selection of cakes.
Activities officer Tracey Harbert said: “We’re so grateful to everyone for attending our Breast Cancer Now coffee morning. The support and generosity from the community was overwhelming. Big thanks to the Deddington Arms, Co-op, Medipill, and local firefighter Chris Fenemore and team, along with many kind individuals from the village who donated incredible prizes for the event’s charity raffle. And of course, to Steve at DBS Flowers, for the beautiful flower arrangements, not only for the home but for the coffee morning and Breast Cancer Now.”

The Gold Standards Framework (GSF) Charity equips your team with the skills, confidence, and compassion to deliver person-centred care that truly makes a difference.
For a limited time, the GSF Care Homes Training & Accreditation Programme is available at 50% off – now only £1,095 + VAT. This affordable, high-impact training is designed for your whole organisation (offer expires October 2025).
GSF Accreditation is CQC-recognised, endorsed by leading care organisations, and more than 97% of accredited teams report better experiences for people and their families.
For more information, visit: www.goldstandardsframework.org.uk / 020 7789 3740
Future-proof your care. Empower your workforce. See the advert on the facing page for more information.

A new care home hosted a pop-up Cat Café in aid of a local charity last week, raising money on International Cat Day.
Langtree Care Home, part of the Millennium Care Group, which has five homes across Lancashire and Greater Manchester, hosted the purpose-driven event that supported cats, the community and the home’s residents.
Hosted in aid of Avid’s Angels Cat Rescue, a Bolton-based charity which supports cats in the North West, residents and people from the local area indulged in sweet treats, refreshments while getting to know some of the organisation’s cats.
The event raised awareness and £100 for the charity, while several cats are being considered for adoption by attendees.
The recently completed Langtree Care Home specialises in advanced nursing and dementia care and is part of the Standish Care Village.
The Village comprises three homes catering for different needs, which deliver unrivalled continuity in the North West.

Sabrina Myers, Lifestyle & Enrichment Coordinator at Langtree Care Home, said: “It was wonderful hosting our first event at Langtree Care Home and even more special due to the
good it created. Our residents really enjoyed it. One resident, Winnie, got so much from it with a smile plastered all over her face from start to finish!”
Jenny Rimmer, Co-Founder & Trustee, at Avid’s Angels, said:
“Avid’s Angels Cat Rescue was thrilled to attend the recent Pop-up Cat Café hosted by Langtree Care Home, in aid of our rescue work. The event brought together care home residents, their families, and our friendly feline companions for a heartwarming afternoon of tea, cake, and cat cuddles.
“We believe strongly in the importance of enrichment activities for care home residents, and it was wonderful to witness the joy and connection the café brought – not just to the residents, but also to their visiting families. The smiles, laughter, and gentle moments of affection truly reflected the uplifting power of animal companionship.
“We would be delighted to visit Langtree Care Home again in the future and continue building on the bond between our cats and the community. Avid’s Angels Cat Rescue currently has many adorable cats looking for loving forever homes. Details can be found on our website!”
The Welsh Government is making £30 million in additional funding available to local authorities to strengthen community-based social care services and improve hospital discharge processes.
Local Authorities are investing their allocation towards actions that will support timely assessments and the availability of packages of care to ensure people can leave hospital when they are clinically able to, helping to reduce the number of delayed hospital discharges.
The funding will be used to strengthen community-based social care and support services to help people to stay well at home.
Local authorities will direct funding towards their specific regional challenges, building on progress made under the 50-day challenge and aligning with integrated care models.
During a visit to Bridgend, Minister for Children and Social Care, Dawn Bowden, met Mr Howard Pring who is receiving vital support from the local authority’s Home Support Team. Through daily visits, the team provides help with essential tasks, enabling the individual to continue living independently at home.
The funding will also support the development of a multi-disciplinary prevention team in Bridgend which is designed to reduce hospital admissions by providing targeted support to individuals in care homes and the wider community.
Similar projects across Wales will benefit from the £30m, with local authorities focusing on preventative and early intervention initiatives as well as actions that enable people to leave hospital as soon as they are clinically able, helping individuals live healthier lives at home and within their communities.
The support being made available demonstrates the Welsh Government’s ongoing commitment to improve patient flow and develop and grow support for individuals receiving care in the community.”
Minister for Children and Social Care, Dawn Bowden said:
“The funding we are making available to local authorities will make a real difference to people across Wales who need care and support.”
“By investing in community-based support, we can help more people return home from hospital when they’re medically ready and enable others to remain independent in their communities.”
“This will not only improve experiences for individuals but also help patient flow through our hospitals.”
Director of the Welsh NHS Confederation Darren Hughes said:
“We welcome the additional funding from the Welsh Government to strengthen community-based social care services and improve hospital discharge processes.”
“Social care is about much more than hospital discharge; care workers play a crucial role in supporting people to remain independent for longer and preventing hospital admissions in the first place.”
“Local authorities and health boards must work together to invest the funding to strengthen communitybased health and social care and support services to enable the best outcomes for people and communities.”
“In our survey of NHS leaders from across Wales, the sustainability of the social care sector was the number one priority. So, although welcome, we need to find a long-term solution, including a move to parity between the NHS and social care. This means ensuring the workforce feel properly valued, paid and respected for their important work.”
“Unless we move to a longer-term vision for health and social care, we will still be fighting the same battles in years to come.”
Staff at a specialist dementia care home in Wellington are celebrating confirmation of their fifth successive accreditation, with full marks for the third time in a row, from national standards body the Gold Standards Framework (GSF), awarded for the outstanding quality of palliative care they provide for residents.
Camelot House and Lodge now qualifies as a finalist in October’s national awards for Care Home of the Year.
The home was first accredited in 2013 by GSF – which exists to promote delivery of the very best end-of-life care – and it has been consistently accredited at three-yearly intervals ever since.
The assessor, Gaynor Pitman, said: “It was clear from the outset that the home has not lost its enthusiasm for GSF and ensuring that their residents live and die well, and are consistently seeking ways to improve.
“They certainly deserve their fifth accreditation. Well done team.”


Paul Teasdale, director of Camelot Care, said: “This fifth successive reaccreditation by GSF is proof of the long-term commitment of our colleagues at Camelot House and Lodge.
“It gives such reassurance to residents’ families about how genuinely dedicated the team is to providing the highest quality palliative and end-of-life care.
“Huge congratulations to our home manager Zillah Oakes and her team – we are very proud of them.”
As part of her inspection, Ms Pitman interviewed the daughter of resident for whom end of life care was in place at the time of her visit.
The interviewee, who was spending long hours at her dying mother’s bedside, said: “I’ve been sat here for hours and never once have I heard a staff member be unkind or rude to anyone, they are just wonderful, kind human beings.”



By Chris Hornung, Managing Director – Public Sector,

When the government released its long-awaited 10Year Health Plan this month, headlines focused on GPs, waiting times, and workforce investment. On paper, the ambition was welcome: shift care out of hospitals, treat people earlier, and move more services into communities. But for those working in the system, there’s one service area that still feels overlooked. Care at home.
If we want to take real pressure off our acute services, we can’t treat care at home as an add-on. It needs to become a central part of how we manage health.
WHY HOME NEEDS TO BE THE FRONT LINE
For decades, the NHS has been trapped in a reactive model, scrambling to treat illness once it reaches a crisis point. But care at home flips that logic. It’s about managing long-term conditions earlier. Preventing deterioration. Keeping people well enough not to need a hospital bed at all.
We now have the technology to do this well. People can track their own blood pressure, oxygen levels, and mobility from home and be alerted if something’s not right. But this isn’t about replacing people with machines. It’s about creating the conditions for earlier, better care, without needing a hospital stay. The NHS Fit For the Future plan talks about “closer to home” models, but doesn’t go far enough in making homebased care the default.
A GAP IN THE FUNDING CONVERSATION
What the plan doesn’t address clearly is how this shift will be funded. Yes, we’re seeing more talk about community health. But in England, much of that work is commissioned by local authorities, not the NHS. At the moment, there's little sign that local authorities will get the extra support they need to make this work. Most adult social care is delivered by private providers, commissioned locally. If we’re serious about care at home, we have to fund local authorities to commission and monitor that care properly. Otherwise, we risk creating a pipeline out of hospitals with nowhere for people to go. For instance, this year, 13,000 beds a day were occupied by patients medically fit for discharge, slowing patient flow and leading to bottlenecks in service.
WHAT GOOD COULD LOOK LIKE BY 2035
A strong care-at-home model is about more than just devices. It’s about designing a system that’s flexi-
ble, responsive, and person-centred.
Right now, many people receive a fixed “package of care” that doesn’t change, even when their needs do. That’s not the fault of the care providers, but the system currently in place, but that’s not how health works in real life. People have good weeks and bad weeks. They recover, relapse, and improve again.
What we should aim for is real-time care planning. We’re working with several local authorities to build a system where carers can record someone’s daily condition - how they’re managing meals, hygiene, and mobility - and adjust their support accordingly.
If someone’s doing well, reduce visits. If they catch a cold or show signs of decline, increase support early before a hospital trip becomes necessary. These small, real-time changes can make a big difference. They’re better for the patient, and they cost far less than emergency care.
This approach has also been backed by a recent clinical trial published in The Lancet, which found that flexible home care packages led to a 35% reduction in unplanned hospital visits, leading to an average saving of £586 per person to the NHS over the year of the study.
Ultimately, technology should support the people who deliver care, not complicate their work. Take continuity. We know it matters that people see the same carer when possible. But that’s not always realistic. Staff have holidays and sick days. What matters then is that whoever steps in understands the person they’re visiting.
For instance, we’ve recently piloted a tool that condenses six months of care records into a short, clear summary. A carer can read it in two minutes and walk in already knowing what’s changed, what to expect, and how best to help. That gives confidence to the carer, reassurance to the person receiving care, and flexibility to the service.
It’s a small feature, but it shows what thoughtful technology can do - remove friction and improve care.
WHAT NEEDS TO CHANGE NOW
We need to stop dividing funding into NHS and local authority pots. It doesn’t reflect how people live. Someone recovering from surgery at home doesn’t care who’s funding their physio or their meals; they just need it to work together so they can get the support they need.
We should treat health funding as one national pot. Decide what we want to spend on hospitals, on community care, and on care at home and allocate accordingly. Right now, we’re seeing money flow into one part of the system while another is left short. That isn’t sustainable.
The vision in the NHS 10-Year Plan is the right one. But without real investment in care at home, we’re asking hospitals to do too much, too late.
We have a chance now to shift the system before it breaks. That means giving people the support they need, where they live and using technology to make that care smarter, faster, and more human. If we get care at home right, everything else starts to work better.
A Selston-based care home has received accreditation from the Veteran Friendly Framework (VFF), recognising its commitment to supporting veterans, reservists and their families.
Described as ‘outstanding’ in their approach, Wren Hall’s accreditation highlights its personalised care for those who have served in the military, helping them feel respected and understood.
The Veteran Friendly Framework (VFF), developed in collaboration with NHS England, the Royal British Legion and Care England, sets a high standard for care providers, promoting greater awareness and support around the unique challenges faced by veterans.
A proud supporter of the Armed Forces Covenant, Wren Hall has embedded its values of dignity and respect through its service, ensuring veterans are acknowledged and supported.

The home has also recently welcomed a veteran onto the team. New Head Chef Steve Wright brings extensive culinary expertise, gained through RAF training, as well as a personal understanding of the veteran experience. His presence within the team further strengthens Wren Hall’s veteran-friendly ethos,
Social care collaboration and use of an “outside the box” approach to recycling of community equipment means daily life is now safe for teenager Rhianna Maness.
The 17 year-old has complex disabilities, including seizures and being non-verbal. Her parents Melissa and Darren themselves have health issues.
Getting Rhianna up and down stairs was becoming a risk, but the conventional solutionsa stairlift or through-floor lift- were not viable.
Rhianna’s Occupational Therapist at Calderdale and Huddersfield NHS Trust found out about AAT’s Sella stairclimber, and reached out for assessment support. It worked!
A Sella was available at Medequip’s stores for Kirklees’ Council, as were some of the accessories needed to ensure Rhianna was sat secure and properly supported as she needed. As a result, using the re-issue capability of the stairclimber, Rhianna’s carers can now transfer her up and down the stairs without risk to her or themselves. Should Rhianna have a seizure en route, the stairclimbing process can be safely paused for as long as required.
“It’s been a real life saver,” says Melissa. “Rhianna’s face shows that she enjoys it, and it’s
bringing lived experience to its care offering.
Steve said: “My time in the RAF taught me discipline, precision, and the importance of serving others - values I bring to the kitchen every day at Wren Hall. Whether it’s preparing a comforting meal or planning a nutritious menu, it’s all about care and respect for those we serve.”
For residents with military backgrounds, Wren Hall continues to offer and develop a program of veteran-specific activities, including military history talks, veteran breakfast clubs and regular visits from local ex-forces groups. The home also proudly displays military memorabilia and personal mementos in its communal spaces.
Anita Astle, manager of Wren Hall, part of Church Farm Care, which offers specialist care across 5 homes in Nottinghamshire, said: “We’re incredibly proud to receive this accreditation, which not only celebrates the work of our team but reinforces the importance of recognising the unique journeys and experiences of our veteran residents. At Wren Hall, we strive to create a place where everyone feels seen, valued and at home - and this is especially important for those who’ve given so much through military service.”

made the world of difference to us all.
“It was a bit scarey to start with at the top of the stairs, but AAT trained us fully in how to use the stairclimber safely. If Rhianna has a seizure, we just stop until it’s passed and we can resume.”
Adds Gareth Brown of AAT, “Rhianna requires significant support to sit. We had most of the accessories she needed in stores @ Kirklees, so there was only need to purchase a couple of small additions. Her access to all levels of the family home has been made safe, including assessment, equipment and training, for around £1000- a fraction of the cost of other solutions, had they been viable.”
AAT’s re-issue facility for stairclimbers is unique within the sector. It means that- where appropriate- necessary, reasonable and practical changes can be made to make stairs safe for someone with reduced mobility, for <£1000/ £650 pa(1). There are no structural alterations nor permanent restriction of the stairs for other members of the household. Full details can be found


Summer brings plenty of opportunities to get stuck into the garden, with sunshine and rain helping everything come to life. From tending to flower beds to pruning, feeding and watering, there’s always something to keep green fingers busy, and many find great satisfaction in the daily rhythm of caring for a garden.
However, gardening isn’t just about keeping things tidy, even the smallest tasks can be incredibly rewarding as they offer a great way to boost our mental and physical wellbeing, explains Lisa Harding, Danforth Care Regional Manager for three care homes in Yorkshire.
HOME GROWN PRODUCE
“We’ve recently been working on our Ground to Plate initiative, which celebrates sustainable living through homegrown produce. It’s been amazing to see each care home growing a selection of fruit and vegetables which have been chosen and cared for by the residents, to later be used in the home’s kitchens.
"To coincide with this, we’ve also had professional chef, Theo Michaels, visit several of our care homes to perform live cooking demonstrations using the produce grown by the residents he’s visiting.” GARDENING IN CARE HOMES
“You can enjoy the emotional and physical benefits of gardening at any age, anywhere, and it’s particularly important for the residents in our care homes. For many, gardening has long been a meaningful part of their lives, offering a sense of purpose, promoting well-being, and helping them stay active.
“Some residents bring decades of gardening experience and relish in sharing tips and tricks with us and their neighbours. Others are completely new to it but have really enjoyed being hands-on with planting and pruning for the first time.”
“It’s wonderful to see the happiness it brings our residents, and the pride they take in their garden spaces and the things they grow. Being part of that experience is truly special, and I find real fulfilment in helping everyone in our community make the most of their outdoor environments.”
WHY IS GARDENING GOOD FOR OUR PHYSICAL HEALTH?
“Gardening is a great exercise for the full body,” says Lisa, Regional Manager at Danforth’s care homes in Yorkshire. “It builds strength in key muscles such as your quadriceps and your hamstrings, and enhances flexibility – stretching out your back, hips and shoulders. Gardening for even ten minutes can be a full body work out!”

“Simple gardening tasks such as weeding and cutting the grass have you pushing, pulling and carrying –all of which add to your strength and your mobility. It also gets you walking around, adding to your step count, which is great for your heart health.”
“Since it’s not exercise in the traditional sense, many people prefer it as it doesn’t feel like a workout, and it can be as gentle or as challenging as you’d like. You can see the fruits of your labour (sometimes literally!), and this helps to keep people motivated. Keeping fit is almost a biproduct of tending to the garden.” WHY IS GARDENING GOOD FOR OUR MENTAL HEALTH?
“There are many reasons gardening is so good for our minds. For example, sunshine reduces blood pressure and increases our vitamin D levels, which lifts our mood, and the physical exercise provides mind boosting endorphins as well. The presence of plants and a natural landscape reduces our stress levels and
Britain’s National Health Service experienced significant disruption during the latest round of junior doctor strikes, with an average of 16,162 resident doctors absent from work daily, leading to the rescheduling of over 6,420 inpatient procedures and 47,675 outpatient appointments across five days of industrial action.
Despite the industrial disruption being less severe than June’s strikes, the NHS continues to grapple with mounting pressures as the total waiting list climbed to 7.37 million patients by June, though there were some positive signs with emergency department performance improving to 76.4% of patients being seen within four hours in July and ambulance response times for Category 2 calls dropping to 28 minutes and 40 seconds, beating both the previous month and the government’s 30-minute target for the first time in recent memory.
Rory Deighton, acute director at the NHS Confederation, said:
“These new figures show that NHS leaders and their teams have left no stone unturned to treat patients and keep services open in the face of continuing high demand and a fresh round of industrial action from resident doctors. “
“This has been possible with lower staff absence during this round of strike action than in June 2024. As in previous rounds of strike action by resident doctors, consultants have stepped in to cover rotas
often making quicker decisions to admit or discharge patients which has helped ease both demand on urgent and emergency care and the flow of patients throughout hospitals.”
“But the real impact of this further industrial action will be seen on elective care. Although the NHS has worked hard to minimise cancelled appointments, a slow down in the reduction of waiting list numbers is still anticipated. It is disappointing that despite the hard work of NHS leaders and their teams to deliver more treatments than in previous years, the waiting list has still increased slightly. Increasing productivity is going to be vital if the NHS is going to bring down waiting lists long term, and our members tell us that additional capital funding will be key to unlocking that potential.”
“Emergency department teams managed to reduce bottlenecks and free up beds to improve performance against the four-hour target despite having one of the busiest months on record. Category two response times were faster last month, which has eased pressure on wider urgent and emergency care services and enabled quicker triage and treatment for patients.”
“But while there are some promising signs, health service leaders are under no illusion how far there is to go to tackle the backlog, bring down waiting lists, improve productivity and hit the government’s 18
week target.”
Tim Gardner, Assistant Director of Policy at the Health Foundation, said:
‘While summer is often a time for the NHS to catch its breath, today’s data shows hospitals and ambulance services remain under relentless pressure.”
‘July brought modest improvements in A&E waiting times and ambulance response times, but performance is still well below NHS constitutional standards, and many patients are waiting far too long for treatment.”
‘Despite a small fall in waiting times for routine hospital treatment in June, the waiting list remains stubbornly high at 7.37 million. Our recent analysis found the impact is felt more acutely in the most deprived communities, where people consistently face longer waits for treatment than those in more affluent areas.”
‘The slight improvements seen this summer offer a glimmer of hope. However, the commitment to tackling waiting lists needs to ensure that more timely treatment becomes a reality for every patient, regardless of where they live.’
A family-run West Devon care home has joined the elite few UK social care settings to have adopted of the acclaimed ‘Butterfly Approach’ – establishing an exemplary dementia care culture where people can thrive.
West View Care Home, in Bere Alston, recently completed the significant 18-month transformation to provide a more personcentred care model and elevate its “excellent” offering even further.
Following rigorous monthly support with the team at the 28-bed home, along with those who live there, West View received accreditation in the prestigious Butterfly Approach from Meaningful Care Matters. The care and culture consultancy group specialise in focusing on the development of resilient, relationship-centred cultures of care shaped by the people living and working within them.
The Butterfly Approach has a meticulous focus on creating a culture where people are ‘free to be me’. It values emotional intelligence and the core belief that everyone has a unique story that has meaning and matters. It also encourages care providers to put the focus back on the people they care for and their emotions, by engaging in the reality of people’s lived experience in the ‘here and now’.
The transformation at West View included splitting the home into two separate living areas – Wren and Robin – where people with earlyonset dementia or without dementia live together and people who experience more complex needs or later stage dementia live together. This fundamental change to a small household approach has enabled holistic care to flourish, where emotions-based care is balanced with clinical care best practice.
The home has also been decorated with vibrant colours and murals to bring warmth, with items of interest all around representing each individual and their life story – what Meaningful Care Matters calls the

‘stuff of life’, creating a family atmosphere.
Diane Kehoe, Manager at West View Care Home, said: “As a secondgeneration family-run business, we always aspire to create a stimulating, engaging and enjoyable environment – and the Butterfly Approach has provided us with the platform to offer that around the clock. I was already familiar with the approach and saw the potential West View had in achieving it. The transformation was not easy, and we had a few challenges along the way, but the rewards upon completion have made it so worthwhile.
“We believed in the whole process from the outset and the staff embraced it – showing so much patience and kindness. They treat the residents like family, enjoying life together with lots of laughter and fun. When you step into the home now you can really sense the buzz of the place, and the level of care is both phenomenal and heartwarm-
ing.”
The overall findings from Meaningful Care Matters during a final audit last month identified the home as “excellent”, offering a highly engaged service that prioritises meaningful moments and where emotion-focused care is consistently seen, felt and heard in interactions with people. It also reported that individuality and self-expression are encouraged within the home, allowing people to freely be themselves.
Peter Bewert, Managing Director of Meaningful Care Matters, said: “West View has transformed into a truly wonderful home. The team have clearly embraced the desire to change and have achieved amazing results, being guided and supported by Diane. They have also lifted their CQC rating from ‘Requires Improvement’ to ‘Good’ and are aiming over the course of the year to reach ‘Outstanding’. They have also been supported by the local service improvements team, who were so impressed at the transformation that they plan to use West View as a role model for other homes.”
Peter continued: “The journey has been incredible. From what we would call a ‘traditional’ care home, West View has come alive and now has a genuine feeling of family, togetherness, love and purpose for the people living there.”
The home aims to continue elevating its high standard of care, with ambitious plans to be acknowledged and approved by the National Dementia Care Accreditation Scheme. It also plans to achieve the ‘gold standard’ for end-of-life care by the Gold Standards Framework.
For more information on West View Care Home, please visit https://westviewcarehome.co.uk/.
For more information on Meaningful Care Matters and its cultural transformation models, visit https://meaningfulcarematters.com/.
The National Institute for Health and Care Research (NIHR) has signed a joint statement alongside other major UK research funders, committing to greater inclusion of older adults in health and care research. This builds on our announcement in November 2024 that inclusion needs to be considered in all applications for our funding.
This move follows the Chief Medical Officer’s Annual 2023 report on healthy ageing, which highlighted that older people, particularly those living with multiple long-term conditions (MLTC), are routinely underrepresented in clinical trials and research studies. This is despite multiple long-term conditions becoming increasingly common and something that many people in the population are likely to live with as they age. Isolating diseases for research purposes is not reflecting the reality of experience and treatment of an ageing population.

The underrepresentation of older people in research and clinical trials makes findings less relevant and less effective for the people who need them most. It can also contribute to inequalities in how healthcare is delivered, particularly as more people reach older age with complex health needs, with differences in healthy life expectancy across communities.
Chief Medical Officer Professor Chris Whitty said:
“Despite often having the highest levels of need, older adults are frequently left out of research that directly affects their care. This exclusion can lead to gaps in evidence, less effective treatments, and care that isn’t properly tailored to those who use services the most. As the population ages, it’s essential that
research reflects the people it aims to serve.”
The joint statement sets out a shared commitment from the participating UK research funders to:
• actively support the inclusion of older adults in research,
• challenge unjustified exclusion, particularly where older adults have complex health conditions,
• and ensure that research is designed with equity in mind and better reflects the diversity of the UK
Professor Lucy Chappell, Chief Scientific Adviser at the Department of Health and Social Care (DHSC) and Chief Executive Officer of the NIHR, said:
“The NIHR is proud to champion the inclusion of older people in research, recognising that their meaningful involvement enriches our understanding and enhances the relevance of findings to improve health outcomes and tackle health inequalities. We are pleased to stand alongside research funders across the UK in this joint statement, reaffirming our shared commitment to making research more inclusive, impactful, and reflective of all stages of life.”
The joint effort follows a roundtable discussion of research funders in 2024, where gaps in how older people are included in health and care research were discussed. The aim is to improve the quality of research while making it more inclusive, ensuring diverse representation of the public across various demographic groups and helping everyone in the UK age well. Including older people more routinely in research will lead to more effective, social and public health strategies and help improve quality of life as people age, ensuring that we support the health of the oldest members of society.
Chester resident, singer, and ‘grandfriend’ Doreen Barnes has had the adventure of a lifetime with a trip to Buckingham Palace to mingle with Their Majesties the King and Queen, thanks to her dedication to the development of the city’s children.
The sunny summer reception saw the 89-year-old make her way to the capital from her home, Belong Chester care village, to represent the Sankofa Songsters, the city’s intergenerational choir featuring fellow residents, children, and other members of the wider community.
Speaking of the experience Doreen said: “We walked into the Palace gardens to the sound of music from the band and then we saw the King and Queen on the garden steps, waving to everyone. It was a lovely day, and I’ve never had one like it – to sum it up in one word: unforgettable!”

The retired civil servant spends much of her time fulfilling duties as a designated intergenerational champion and ‘grandfriend’, a moniker given to her by the cohort of children at the Nursery in Belong, the early years care setting integrated within her home, operated by national charity Ready Generations. In addition to singing alongside the young-
sters in the choir, Doreen plays and dines with them and shows them the ways of the world.
Joining her at the place were choir lead, Amanda Wrigley, volunteer pianist, Pete Legge, and singer Hollie McDiarmid. The invitation came after the choir performed at last year’s Royal Carols: Together at Christmas ceremony, the annual event hosted at Westminster Abbey by Catherine, Princess of Wales.
Sankofa Songsters’ choir lead, Amanda Wrigley of Live the Beat, commented:
“What an honour it was to have been invited to the palace! Special thank you to Cheshire Community Foundation and Healthbox CIC for their role in supporting the choir’s work.”
Caroline Ray, general manager at Belong Chester, added:
“We are thrilled to have had Doreen representing us. We are all about community and since day one moving in, she has immersed herself in village life, encouraging others to join in and make it what it is. Congratulations to Doreen and the Sankofa Songsters.”


According to business rates experts at Colliers, latest figures just announced by the government reveal that the business rates appeal system: Check Challenge Appeal (CCA) is storing up “a tsunami” of appeals over the next seven months as we approach the final stretch of the 2023 list which ends on 31st March 2026. According to government (VOA) statistics, in the 27 months since the beginning of the 2023 list (1st April 2023 to 30th June 2025), 162,440 Checks (the first part of the appeal process) were registered of which 17,330 are still outstanding. More concerning is that of the 35,910 of these which progressed to the Challenge (second) stage of the process, well over half – 20,160 (or 56 %), were still outstanding 9 months before the end of the three year list. And only 9,340 (26%) of Challenges had been resolved so far, with 6410 (18%) labelled as “incomplete” by the VOA and therefore struck out/ declared void.
Given the difficulty for businesses in registering a Check in CCA in the first place- the amount of detailed information businesses now need to provide means that most have to use professional rating surveyorsColliers believes many businesses have up to now held back from registering their appeals. But in the next seven months new Checks will begin to flood the already creakingly slow system as the deadline approaches.
According to John Webber, Head of Business Rates at Colliers, “Many businesses have only recently finished disputing their values from the 2017 list and are only now turning to look at the 2023 list. And for those
businesses in the RHL (retail, hospitality and leisure) sectors who received reliefs on their business rates bills in the first two years of this list, the economic picture is now getting much tougher as the reliefs have been significantly cut and will soon disappear altogether. They will undoubtedly now consider disputing current rateable values.
We think as businesses return from their summer holidays in September, they will start to put their appeals in against their current valuations. And looking at the numbers we at Colliers are already advising, we estimate there will be about 100,000 new appeals (checks) across the industry lodged over the next seven months.”
Webber advises that businesses would be sensible to challenge their rates bills if they can. As the VOA’s own figures reveal: 60% of businesses who challenged their business rates valuations saw a reduced RV (rateable value) as a result and only 0.6% saw an increase, and 54% of those who went onto the appeal stage also saw a reduction to their RV, with 0% seeing an increase. Success rates are therefore high.
However, Colliers is concerned about how slow the system is to get such challenges resolved.
As Webber continued, “If 56% of Challenges have still not been resolved 27 months on from being registered, how will the VOA cope with the expected 100,000 of new businesses disputing their 2023 valuations in the next 7 months? By next April the VOA will also need to start working on the 2029 list, for which the law will change giving businesses only a 6-month window in which to appeal. It’s going to be carnage.”
“The burden of business rates is too high and the lack of transparency about how bills are arrived at remains the root cause of this shocking number of people trying to appeal their rate bills. We believe the VOA is severely under resourced to deal with these numbers in the timeframe and will struggle. Businesses will miss out.
We believe businesses need and deserve a better appeals system- and they need it now.”
Foundation Partners and Deer Capital have acquired five fully operational homes across Kent from The Graham Care Group, in a move which takes their total investment to over £300m in the last 12 months under the Hartford Care brand. The sale reinforces Hartford Care’s ambitious expansion strategy and adds a further 513 bedrooms to its growing portfolio which now comprises 29 homes in the UK (over 1,800 bedrooms).
The purpose-built homes acquired are Cornford House and Hazeldene House in Pembury, Woodchurch House in Ashford, Hawkinge House on the outskirts of Folkestone and Hawkhurst House in Hawkhurst. The homes have a current occupancy in excess of 95%, reflecting the high quality of the service and environment on offer to residents; the experienced and valued staff in every home will be retained.
All the homes offer studio and one-bedroom suites, which include a kitchenette, living and dining area. These provide a home for life for residents with nursing needs, while Hawkinge House and Hawkhurst House include a Proactive Assessment Unit, offering hospital discharge patients access to primary assessment and treatment capabilities. Hawkinge House also offers an innovative short-term unit, for those requiring rehabilitation before returning home.
Ben Puddle, Managing Partner, Foundation Partners, said: “We are very pleased with this acquisition, which broadens the scope of our services to include complex care alongside our established provision of residential, nursing and dementia care. This milestone brings us one step closer to realising our ambition of delivering a truly national, fully integrated, full-service care offering across the UK. Together with our partners at Deer Capital, we have a strong pipeline of near-term acquisitions that we hope to announce in the coming weeks that will further expand our capabilities and enhance the services and locations we
provide to the communities we serve.”
Kevin Shaw, Chief Executive of Hartford Care, comments: “The acquisition of these homes from The Graham Care Group represents another exciting milestone in our growth plan and marks our geographical expansion into Kent for the first time. It enables us to offer our expert care and ‘home from home’ environment to even more residents in new communities. We’re proud to carry on the legacy of Graham Care Group’s expertise and are working closely with the team to ensure a smooth transition as we bring the homes into the Hartford Care family.”
Ernie Graham, Founder and Owner, The Graham Care Group, comments: “Hartford’s philosophy of care for the entire local community in which each home is based aligns closely with our own. This ethos is evident across their homes and in the expert support and care their residents receive. We’re looking forward to continuing to collaborate with the Hartford Care team during the acquisition period and wholly supporting our staff, residents and families through a seamless handover while we continue to operate in other areas of the South East running our existing homes and developing new ones.”

Care Inspections UK (CIUK), the UK’s only accredited inspection body for care homes, has launched a pay-as-you-go inspection service aimed at helping care homes improve quality, performance, risk management, and regulatory ratings in the face of the increasing costs affecting the social care sector.
To ease cash flow during rising National Insurance and wage pressures, the subscription service offers care homes structured, evidence-based support to navigate compliance challenges effectively. To add to this support, CIUK is offering up to £100 per month off all new subscriptions for twelve months for sign-ups in May 2025.

Designed to accommodate a range of operational needs and budgets, the three-tiered subscription model, Silver, Gold, and Platinum, offers varying levels of inspection frequency, expert guidance, and action plans tailored to each home’s requirements.
Under the Silver plan, care homes receive an annual comprehensive inspection carried out by experienced, accredited professionals. The resulting detailed report includes a full breakdown of every aspect of the care home, along with easy click-through access to relevant standards, regulations, and best practices. An action plan is provided to cover any non-conformances, with ongoing review and support to
ensure continuous progress. Homes that meet the required thresholds will be awarded a certification, signifying excellence in care provision. Additional benefits include advisory support before and after inspections, access to exclusive online events and forums for networking and best practice sharing, and participation in CIUK-led publicity initiatives designed to highlight high standards of care. CIUK also guarantees that, by fully implementing all aspects of the action plan, homes will see improvements in their regulatory ratings (CQC, CI, CIW, RQIA), giving providers added assurance that their investment in quality improvement will yield tangible results.
The Gold tier builds upon the Silver plan by offering additional regulatory and commissioning pre-inspection tools. This deeper level of service helps care providers prepare more effectively for formal inspections, giving them an edge in demonstrating compliance with industry standards. Gold members benefit from an in-depth assessment of their readiness for external regulatory visits, with tailored support that helps anticipate potential concerns and address them proactively. In addition to all the features of the Silver package, Gold subscribers receive a more comprehensive level of preparatory guidance, ensuring that homes meet and exceed industry expectations.
The Platinum package is the most comprehensive offering, providing
two inspections per year to ensure that care homes maintain consistently high standards throughout the year. Alongside the core benefits found in the Gold and Silver plans, Platinum members gain access to detailed analysis of inspection trends, helping care homes identify recurring issues and implement long-term solutions for sustained compliance and excellence. Additional advisory support is extended to Platinum members, ensuring they have ongoing expert guidance in regulatory matters, risk management, and quality improvement. This elite tier is particularly beneficial for larger care providers or those undergoing transitions, such as ownership changes or expansion, who require higher scrutiny and support.
Kevin Groombridge, chief executive at Care Inspections UK, said: “Our mission is to raise standards in the care sector by providing accessible, evidence-based support. This subscription model equips care homes with the tools to enhance compliance and deliver the highestquality care.
With rising costs placing additional pressure on the sector, for only a couple hundred pounds a month, our service offers expert guidance and regular inspections to help providers navigate these challenges. By following our structured action plan, care homes can guarantee an improvement in their regulatory ratings, ensuring better outcomes for both residents and staff.”
Visit www.careinspections.co.uk or see the advert on the facing page for details.

Cats with dementia have brain changes similar to those of people with Alzheimer’s disease, offering a valuable model for studying the condition in humans, a study says.
Scientists discovered a build-up of the toxic protein amyloid-beta in the brains of cats with the condition – one of the defining features of Alzheimer’s disease.
The findings offer a clearer picture of how amyloid-beta may lead to age-related brain dysfunction and memory loss in cats, experts say.
Many older cats develop dementia, leading to behavioural changes such as increased vocalisation – or meowing – confusion and disrupted sleep – symptoms similar to those seen in people with Alzheimer’s disease.
Scientists at the University of Edinburgh examined the brains of 25 cats of different ages after they had passed away, including those with signs of dementia.

Powerful microscopy images revealed a build-up of amyloid-beta within the synapses – connections between brain cells – of older cats and cats with dementia.
Synapses allow the flow of messages between brain cells and are vital to healthy brain function. Their loss strongly predicts reduced memory and thinking abilities in humans with Alzheimer’s disease.
The research team also found evidence that astrocytes and microglia – types of support cells in the brain – engulfed or ‘ate’ the affected synapses. This process, called synaptic pruning, is important during brain development but can contribute to synapse loss in dementia.
Experts say the findings will not only help to understand and manage dementia in cats but, given their similarities, could also contribute to the development of future treatments for people with Alzheimer’s disease.
Scientists studying Alzheimer’s disease in the past have relied heavily on genetically modified rodent models. Rodents do not naturally develop dementia, and studying cats with dementia has the potential to advance knowledge and help develop treatments for both cats and people, experts say.
The study, funded by Wellcome and the UK Dementia Research Institute, included scientists from the Universities of Edinburgh and California, UK Dementia Research Institute and Scottish Brain Sciences.
Dementia is a devastating disease – whether it affects humans, cats, or dogs. Our findings highlight the striking similarities between feline dementia and Alzheimer’s disease in people. This opens the door to exploring whether promising new treatments for human Alzheimer’s disease could also help our ageing pets. Because cats naturally develop these brain changes, they may also offer a more accurate model of the disease than traditional laboratory animals, ultimately benefiting both species and their caregivers.
Dr Robert McGeachan Study lead from the Royal (Dick) School of Veterinary Studies said:
“Feline dementia is so distressing for the cat and for its person. It is by undertaking studies like this that we will understand how best to treat them. This will be wonderful for the cats, their owners, people with Alzheimer’s and their loved ones. Feline dementia is the perfect natural model for Alzheimer’s, everyone benefits.”
A relaxation of rules to allow overseas health and social care professionals now residing in the UK earlier access to funded training will be a boost to the struggling sector, according to an industry expert.
The Government’s Department for Education recently announced simplification of the residency rules for Adult Skills funding.
It means health and social care workers with Ordinarily Resident status in non-devolved areas will no longer have to wait three years to be able to claim funding for training as they had to before.
A number of devolved areas have already followed suit, including Tees Valley, Liverpool City Region, West Midlands and West Yorkshire.
Angela Kaine, Director of Health & Social Care at leading training provider Realise, said a relaxation of long-standing residency rules is one step closer to creating greater equality of opportunity and would allow care homes to develop their people.

Angela said: “This is a valuable improvement and extremely welcome news for both health and social care workers from overseas and care providers.
“This will help ensure that individuals who have come to the UK to perform vital roles in health and social care can access the same training opportunities as others and potentially remain longer in their roles once they have secured Ordinarily Resident status.
“Previously, people in the UK with Ordinarily Resident status were expected to fund the training them-
selves for the first three years - or secure employer backing - which was clearly a barrier for many.
“Care managers have huge concerns over deficits in staffing. This offers a short-term solution that eases the problem. It’s a relief for the sector, which relies heavily on large numbers of committed and skilled workers from overseas, and the increasing number of people who are being granted residency status.”
Realise can deliver funded staff training in the West Midlands, West Yorkshire, Tees Valley, Liverpool City Region, as well as all non-devolved areas.
The most recent figures showed there are around 300,000 non-EU nationals working within health and social care.
Angela said many people who come to the UK to work within health and social care already have years of valuable experience in the sector.
“Many have worked in care in their country of origin,” said Angela. “Legislation and practices might differ, but they have a fantastic basis of knowledge and they are keen to forge a career with the right values and compassion.”
Realise is one of the largest and most respected providers of health and social care training providers in the UK and holds the new Quality Assurance Care Learning Services (QACLS) endorsement for many of its programmes, including the Level 2 Adult Social Care Certificate.
For more information, visit www.realisetraining.com
Spellman Care has announced that all four of its homes have been re-accredited under the Veteran Friendly Framework. This achievement comes one year after the group became only the second care home group in the country to receive the initial accreditation.
Fran Sharp, Project Officer at the Veteran Friendly Framework, praised Spellman Care’s dedication and the team’s passion when delivering the news of their re-accreditation. She highlighted the amount of innovative and engaging projects the group has undertaken, which truly make a difference to the lives of veterans in their care.
A key part of Spellman Care’s efforts this past year has been the successful launch of the Spellman Care Veterans Cafes. These monthly gatherings circulate between the four homes, providing a dedicated space for veterans to connect and socialise. Peter Chadwick, representing Spellman Care, shared his delight at the news. “The entire Spellman Care team is thrilled to receive our one-year re-accreditation. A lot of hard work has gone into this project, and this recognition is a testament to the whole team, especially our Activity Coordinators who have worked tirelessly to provide the very best person-centred care for our veterans. We were particularly proud this year to see our first resident become an Armed Forces Champion, which is a wonderful example of the impact our work is having.”

In a letter to the homes, Fran Sharp extended her congratulations, stating:
“It is our pleasure to congratulate you on your continuous commitments to your VFF Status, as a Veteran Friendly Framework Care Home in July 2025. We thank you for continued commitment to the Armed Forces Covenant. This accreditation recognises your continued work identifying and sharing best practice within your care home to enable the best standards of care for the Armed Forces community.” She added that the national team will continue to support Spellman Care’s veteran-aware activities and assist with establishing a program that delivers a lasting impact.
Chadwick concluded with a look to the future. “While we are delighted with this re-accreditation, our commitment to outstanding care for our veterans—and indeed, for all our residents—is a journey with no end. We are always looking for ways to expand and improve. We’d also like to extend a huge thank you to all the new contacts and partners we’ve made this year for their incredible support, including the Keighley Sea Cadets and Royal Marine Cadets and the members of the Ilkley Armed Forces Breakfast Club. The whole team is looking forward to growing our Veterans Cafes and building even more links within the veteran community. We will continue to work closely with the VFF for many years to come as we strive to provide the best possible care for everyone in our homes.”
A care assistant at a Stafford home who "wasn't sure what to expect” when she started her journey with the home has marked 10 years’ service.
Charlotte Gittins joined MHA Weston and Queensway House in 2015 from community care and despite her reservations to begin with has marked 10 years with the home.
To mark her service Charlotte was awarded with her long service certificate and a gift voucher from the management team.
MHA Weston and Queensway House provide dementia nursing care for 70 residents.
Speaking after the ceremony she said: “It does feel like I have been here for years, and to be honest I knew I was coming up to 10 years.
“I didn't know the exact date, so yeah it was a nice surprise when I was presented with my certificate and voucher.
“I applied for the job on the off chance, I wasn't even aware if the home had any vacancies at the time.
“Initially I wasn't sure what to expect as I hadn't worked in full time care before, as my background was in community care.
“I am so happy I work at MHA Weston and Queensway, I love my job.
“The residents and my colleagues make the home and the job very special to me.
“Working for an organisation like MHA has been a very enjoyable experience so far, I haven't got a bad word to say about the organisation or the home.”

Members of the Royal Electrical and Mechanical Engineers (REME) corps have ‘geared up’ to donate £200 towards a sensory garden at a Somerset nursing home.
The dementia-friendly garden at Avalon Nursing Home in Bridgwater will offer a safe, calming space for residents, with plants, scents and sensory features to enhance well-being.
The REME donation came about through Netta Merrick, a close friend of a late resident’s family, who wanted to give back to the home for the care and compassion shown him.
Netta, a friend of Angela Lovell, first visited Avalon to visit Angela’s late husband Chris, who was a resident there and says she immediately felt a strong connection to the home.
A keen lover of the outdoors, Netta married a soldier in 1972 and spent 24 years living in properties without a garden while travelling the world to support his military career.
“Having a garden is like having a sanctuary, somewhere to be quiet,



find peace, and reconnect with nature, like having a little piece of the countryside right at home,” said Netta.
“It’s a place where you can let out your frustration or anger, and it doesn’t matter.”
So far, Avalon has raised £11,545 for a sensory garden with calming plants, seating, and features for residents and guests; currently work is being carried out to lay down a path in the garden.
“The money we raise will go towards things like landscaping, plants, seating, and sensory touches such as water features and wind chimes,” said Avalon’s activities team leader, Lisa Priddice.
“We want to create a lovely garden that’s not only safe and welcoming for our residents, but also a special place where families and carers can spend time together.”
The Corps of Royal Electrical and Mechanical Engineers provides engineering support to maintain and repair the vast array of British Army equipment.

• We specialise in the sale and purchase of quality used wheelchair accessible vehicles and ambulances.
• They can be bought as seen or refurbished and sign-written to your own requirements.
• Fully serviced, new mot & warranty
• Engineers inspection supplied if required.
• Free delivery service available
• All buses comply with new legislation
•
• Lease hire and purchase


By Nikki Walker - CEO of QCS, an RLDatix Company

The social care sector stands at a turning point. With rising demand, increasing regulatory scrutiny, and ongoing staffing pressures, providers are being asked to do more, with less. In this environment, the way forward isn’t just about working harder it’s about working smarter.
One of the most transformative shifts on the horizon is the move towards truly integrated care systems: digital platforms that bring together compliance, care planning, risk management, training and quality monitoring in one unified place. More than just a convenience, this integration is fast becoming essential. Currently, many providers juggle multiple systems or rely on a mix of digital tools and paper-based processes. Information is scattered. Teams duplicate effort. Vital data goes unnoticed.
The result? Frustration, inefficiency and risk.
A connected system solves this by creating a single source of truth, where care delivery and compliance are not just stored, but actively linked. Changes in a policy can automatically update associated risk assessments. Notes in a care plan can prompt training needs. Audit trails are clear and accessible. For staff, it means less time on admin. For managers, better visibility. For individuals receiving care, more consistent, safer support.
Adding artificial intelligence (AI) into the mix elevates this even further. AI can help spot patterns in care records, prompt best practice actions and reduce the burden of documentation. Crucially, AI isn’t there to replace human decision-making it’s there to support it. By giving frontline teams real-time, intelligent guidance, it helps ensure nothing is missed and quality remains high.
Of course, technology alone isn’t enough. These systems must be built on deep sector knowledge and shaped by those working in care. Platforms like QCS, for instance, combine expert-backed content with intelligent tools to provide not just data, but insight. It’s this fusion of trusted information and digital innovation that’s beginning to change how care is delivered.
But a connected future is about more than software. It’s a cultural shift towards a care environment that is proactive rather than reactive, where data drives improvement, and where teams feel confident and supported.
In a sector where every moment counts, integrated systems offer more than efficiency, they offer the chance to focus on what matters most: people. When technology works seamlessly in the background, it frees carers to do the deeply human work that technology can’t replicate.
The future of care is not just digital. It’s intelligent. And most importantly, it’s integrated.
To see how QCS are integrating care planning, rostering. audits, mock inspection, surveys, training, compliance, dementia care and more into one integrated system backed by AI technology, follow the link. www.qcs.co.uk/what-we-do/
A resident who lives at Roman House in Basingstoke, part of Salutem Care and Education, has completed an extraordinary challenge scaling the O2 in London in a wheelchair and raising an impressive £1000 for the Salvation Army.
With the backing of an incredible support team, including Christopher Bell who climbed with him, and the use of a specially designed off-road wheelchair provided by the O2 climbing team, Simon ascended to the 171 ft summit. From the top, he was rewarded with breathtaking panoramic views of London’s iconic skyline.
Simon is no stranger to daring challenges. A self-confessed thrill-seeker, he has previously tackled abseiling, gliding, and quad biking, and already has his sights set on his next big adventure which he hopes will be zip lining. True to his fearless spirit, the extreme heights of the O2 did not faze him in

the slightest; in fact, he loved every second.
Trudy Hobday, registered manager of Roman House, said: “This inspiring achievement is a powerful reminder of what can be accomplished with determination, courage, and the right support. Here at Salutem we are very proud to support Simon in living his life to the fullest and committed to empowering the individuals we support to push boundaries and achieve extraordinary goals.”
Beyond the personal triumph, Simon’s climb raised an impressive £1000 for the Salvation Army, a charity close to his heart. He said: “I always want to push myself and prove that I can do anything. It’s something different and I love the adventure. Adventure is for everybody and climbing the O2 was an amazing experience for me, and I hope it inspires others to do something different and push the boundaries.”

Ben Smith, a dedicated support worker at High View in Truro, part of Salutem Care and Education, has been nominated for the prestigious Support Worker of the Year award at the Proud to Care Cornwall Awards.
Ben, who was recently promoted to a senior role at High View, a residential care home supporting up to five people with a learning disability or autism, was nominated by the family of one of the individuals he supports.
The heartfelt nomination reads:
“Ben has supported my son Joe for many years, both at High View and at Chylidn, where Joe lived previously. Joe has autism, a learning disability, and struggles with behavioural difficulties. Ben understands Joe’s needs completely and supports him with a high level of skill, care, and confidence –especially when Joe is having a difficult time.
“Nothing is too much trouble for Ben. He consistently delivers an exceptionally high standard of care with a positive attitude. Always upbeat and happy, Ben makes
sure Joe is having the best time. Whether it’s swimming, cycling, sailing, dance classes or his farm placement, Ben is always keen to get involved – he treats taking Joe out like spending time with a friend.
“Joe clearly loves Ben’s company and enthusiasm. Ben combines his professionalism with a relaxed sense of fun, helping Joe build trust and feel completely at ease.
“As a senior team member, Ben is incredibly supportive of his colleagues – offering advice even on his days off and attending voluntary training in his own time. He’s always willing to cover shifts at short notice, putting the people he supports before himself.
“He’s so thoughtful, regularly checking in on Joe’s family and updating us on what Joe has been up to. Ben is a consummate professional, a key member of the staff team, and an outstanding mentor who fully deserves to be recognised for his hard work, commitment, and genuine love of his role.”
John Godden, chief executive of Salutem Care and Education said: “We are incredibly proud of Ben and delighted to see his dedication recognised in this way, particularly by the family of one of the individuals he supports. His passion, kindness and commitment embody the very best of social care.”
The Proud to Care Cornwall Awards celebrate the outstanding contributions of care professionals across the county, honouring those who go above and beyond to make a difference in the lives of others. The award ceremony will take place at the iconic Eden Project on Friday 19 September 2025, during Professional Care Workers Week.
Residents at Boroughbridge Manor in Boroughbridge marked Indian Independence Day which took place on August 15th. Independence Day is celebrated on August 15th, the anniversary of the day in 1947 when the provisions of the Indian Independence Act, which transferred legislative sovereignty to the Indian Constituent Assembly, came into effect and India gained its Independence from the United Kingdom. It is a public holiday in India. The Prime Minister raises the red national flag of India and addresses the nation.
Residents, relatives and members of staff celebrated the homes Indian colleagues in a celebration, whilst wishing to embrace their culture.

To honour the occasion, the homes colleagues from India shared elements of their rich cultural heritage with residents and staff. The afternoon featured traditional dance performances, a cultural fashion showcase where members of the team enjoyed an Indian glow up!
Susan Carter, General Manager at Boroughbridge Manor said: “We celebrate all cultures and religions and we try to mark as many cultural events as possible. Indian Independence Day has given our residents a wonderful opportunity to find out more about India and its traditions, whilst celebrating the homes Indian colleagues.”

NIHR-funded research project will explore barriers and resources for young people seeking mental health support in England.
The University of Birmingham, in collaboration with the universities of Bristol and Kent, has launched a landmark 18-month research project to explore how care-experienced young people (CYP) aged 13 to 25—including those who are LGBTQ+, racially minoritised, neurodivergent, or disabled—seek help for mental health problems.
The study has been funded by the NIHR Research Programme for Social Care (RPSC).
The project, called COLLAGE (Care-experienced yOung peopLe’s mentaL heAlth help-seekinG bEhaviours), will aim to bring together diverse voices and experiences to build a fuller, more inclusive picture of the challenges CYP face when looking for mental health support, and the things that help them access it. The project is also co-produced with CYP, who are involved as partners in shaping the research, not just participants.

Dr Willem Stander, who is leading the study at the University of Birmingham, said: “Care-experienced young people have some of the highest mental health needs in the UK, yet many struggle to get the support they need. Only around one in three young people with diagnosable mental health conditions receive services—and for CYP, barriers like instability, disrupted relationships, and gaps in care make access even harder. This is amplified further for those with multiple minoritised identities, as these young people often face unique challenges when seeking help for mental health problems.
“Despite this, there is still a critical lack of evidence about how they seek or access help, and even less that centres their views and lived perspectives. Understanding their experiences is essential to designing support that truly meets their needs. This study is about listening to CYPs’ lived experiences and underrepresented voices, and working with them to co-design services that are inclusive, accessible, and reflect their needs.”
The study is one of the first UK studies to address this gap by exploring help-seeking across all types of care placement, including foster care, residential homes, kinship care, and care leavers. It will use a mixed-methods approach, including a large-scale national survey, in-depth interviews, and an international systematic review of the research evidence base.
The COLLAGE study will:
• Investigate how care-experienced young people seek and access mental health support
• Identify what makes it easier or harder to get support
• Explore the experiences of CYP with multiple marginalised identities
• Co-produce digital resources and policy recommendations to improve support
Running up to November 2026, the study will deliver:
• A comprehensive evidence base on mental health help-seeking across a wide range of out-of-home care placements
• Co-designed digital resources for young people, professionals, and the public
• A free online event to share findings, featuring presentations and reflections from CYP
• Academic, practice, and policy-focused outputs to support real-world impact
The project team includes Professor Jason Schaub (University of Bristol), Dr Jolie Keemink (University of Kent), Omar Mohamed (a Children and Families Social Worker), and Emma Wallace (Research Fellow, University of Birmingham).
Dr Stander concluded: “In the context of growing national concern around youth mental health, health inequalities, and social care reform, this project and its findings will be crucial to developing an accurate picture of care-experienced young people experiences of mental health support. Our findings will be able to help inform policy, improve practice, and promote equity in mental health access for some of the UK’s most underserved young people.”
Residents at HC-One’s Coppice Lodge Care Home in Arnold, Nottingham, brought history to life on Friday, August 15, with a heartfelt celebration to honour Victory over Japan Day (VJ Day), commemorating the end of World War II in true style.
VJ Day (Victory over Japan Day) in 2025 marks the 80th anniversary of Japan's surrender during World War II. It is observed on August 15, 2025, in the UK and Commonwealth, while in the United States, it is celebrated on September 2, 2025. This day is significant as it commemorates the end of the war in the Pacific and is marked by various events and activities to honour the WWII generation.
Coppice Lodge residents, along with their families and friends, were treated to an unforgettable afternoon filled with music, nostalgia, and community spirit. The event featured a captivating performance by the talented Amy

Evans, who delighted guests with classic wartime hits that echoed the spirit of the era.
The atmosphere was alive with smiles, laughter, and plenty of toe-tapping as everyone savoured delicious refreshments and nibbles. The celebration provided a meaningful tribute to a remarkable generation who lived through extraordinary times.
Ken Buxton, HC-One’s Coppice Lodge Care Home Manager, stated: "It was a beautiful way to reflect on such an important moment in history. Events like this give our residents the chance to share memories, feel connected, and simply enjoy life surrounded by loved ones."
Resident Doreen said: “The event was brilliant – they had lovely cakes and white wine spritzers for us to enjoy, and they all wore hats. The singer Ami was very clear, and she could hear everyone word that she sang.”
OneAdvanced, the leader in AI-powered healthcare IT solutions supporting over 40 million UK patients annually, has completed the purchase of certain assets of INPS, relating to the Vision electronic patient record (EPR) system used by GP practices across the UK. This puts an end to six months of uncertainty for GPs using the Vision EPR software and provides an exceptionally strong partner for the future.
This strategic move further enhances the delivery of OneAdvanced's next-generation healthcare platform and reinforces OneAdvanced's commitment to reimagining healthcare services through technology. Combining the Vision EPR solution with OneAdvanced's extensive healthcare portfolio, creates a powerful healthcare platform, aligned directly with the NHS's 10-year plan to create the world’s most digitally accessible healthcare service, as launched by Wes Streeting on 3 July 2025.

OneAdvanced’s healthcare platform underpins the transformation to neighbourhood care, supporting local GP’s, pharmacies and local communities in support of improved patient experience. In providing secure, trusted, real-time patient insights across primary, community, secondary and social care settings, the OneAdvanced healthcare platform aids the NHS in its quest to enhance patient care services across the UK. The OneAdvanced platform paves the way for a unified, AI-driven national health system, and is fundamental to achieve the governments neighbourhood care ambitions.
Ric Thompson, SVP of Health & Care at OneAdvanced, remarked confidently on this pivotal step for UK healthcare innovation:
"We are pleased to add this mission critical solution used by hundreds of GP practices across the UK to our healthcare portfolio. We are on the brink of a generational leap in healthcare technology, by integrating Vision EPR expertise with OneAdvanced’s existing healthcare solutions, such as document management [Docman], secondary care electronic patient management [Adastra], online GP consultation [Patchs] and clinical triage and decision support [Odyssey], we deliver the backbone for a future defined by intelligenceled, highly personalised, and efficient healthcare delivery.”
This announcement carries immediate benefits for GPs across the UK, especially in Scotland, where the
Vision platform is playing a vital role in NHS Scotland's national technology programme. Around 900 GP practices are undergoing a crucial transition from legacy EMIS technology to the Vision cloud-based EPR system, backed by this purchase.
"GPs in Scotland can rest assured knowing this vital transition will be seamless, with no interruptions to clinical care," Thompson asserted. "Our existing relationship with NHS National Services Scotland will ensure the INPS Vision platform will not only be fulfilled, it will also be accelerated with innovative enhancements only OneAdvanced can deliver."
Steven Flockhart, Director of Digital and Security, NHS National Services Scotland, said:
"A stable and effective GP IT system is essential to supporting Primary Care across Scotland. We look forward to working closely with OneAdvanced on this next phase of service delivery."
With over 35 years' experience in healthcare technology, OneAdvanced is bringing its deep industry expertise and modern AI-powered innovation together to tackle the complex challenges facing the NHS, unlocking the full potential of digitalisation for enhanced patient care.
Integrating Vision into OneAdvanced’s existing Primary Care portfolio enhances their world-class national health platform, addressing the increasing demand for seamless, data-driven healthcare solutions. By leveraging AI, OneAdvanced’s healthcare platform empowers clinicians with actionable insights, reduces administrative burdens on NHS staff and ensures patients receive more consistent, proactive, and personalised care. No other provider in the UK has the capability to deliver such a platform.
Thompson adds, "Adding Vision EPR to our existing Primary Care solutions, ensures OneAdvanced is directly connected to the NHS 10-year vision for improved patient outcomes through better neighbourhood care. Key to this is empowering GPs to proactively manage complex patient needs, with accurate and timely interventions, ultimately enhancing the patient experience whilst also reducing hospital admissions and waste."
For more information about OneAdvanced, visit www.oneadvanced.com

National Care Group, one of the UK’s leading adult social care providers for adults with learning disabilities, mental health diagnoses, acquired brain injuries, and autistic people, has released its first Impact Report. The report is a comprehensive overview of the organisation’s significant progress in sustainability and social contribution.
The inaugural report for 2024/25 builds on the previous Quality Account 2023/24 and the commitments made within the organisation’s Corporate Social Responsibility Strategy.
National Care Group’s Impact Report details its first sustainability steps and meaningful progress made through environmental, community, growth and people initiatives.

“The introduction of our first Impact Report is a significant moment for National Care Group. It brings to life the progress, decisions and the first steps in sustainability that are shaping and supporting a brighter future for all associated with our organisation,” said James Allen, Chief Executive Officer. Key highlights from the Impact Report include:
Community: A total of 105 supported people logged a volunteering or work interaction on their digital care plan, and 100% of learners at Regent College, a specialist education centre in Stoke-on-Trent, participate in some form of volunteering.
Environment: A five-year carbon reduction plan was launched, and an enhanced waste management trial in Stoke-on-Trent achieved an 82% reduction (measured by the number of bedrooms in the residential services). Amongst other carbon reduction initiatives, enhanced recycling will be rolled out nationally during 2025/26.
Growth: The organisation reports that it is supporting more people following the opening of four new supported living services, creating 14 new tenancies and 30 new jobs in 2024/25. This was in addition to the expansion of its existing services.
People: The people section of the report celebrates an improved retention rate, the significant reduction in time to hire and a collective 935 years of colleagues celebrating long service milestones. Now employing 2,978 colleagues, the numbers were boosted thanks to the acquisition of Apple House in Dorset in February 2025.
James Allen added: “The release of the Impact Report marks the beginning of a new chapter for National Care Group, reinforcing our mission to unlock the potential of the people we support and our colleagues, while making a positive contribution to the planet.
“We will use our new carbon reduction plan to guide future decision-making, enhance sustainability, and further embed our values of passion, empowerment, respect and collaboration into every aspect of operations.”
In care homes, where hygiene, safety, and reliability are paramount, it’s essential that laundry operations run seamlessly. Forbes Professional’s Complete Care solution is tailored to meet the specific demands of this environment, offering fully supported and cost-effective laundry systems.
With Complete Care, care homes benefit from access to premium commercial laundry appliances without upfront capital expenditure. The allinclusive rental plan covers installation, routine servicing, maintenance, and repairs; enabling staff to focus on resident care rather than laundry appliance logistics. Unexpected breakdowns can severely disrupt operations, which is why Forbes provides nationwide, award-winning support with a same or next-day engineer response to minimise downtime.
Preventative servicing is central to Forbes’ approach. Their offering includes routine maintenance, full certification, annual gas safety checks, and professional dryer duct cleaning - ensuring systems meet all legal and regulatory standards. Whether supporting existing machines or those rented through Forbes, this proactive strategy improves operational efficiency and reduces risk.

Under Regulation 35 of the Gas Safety Regulations 1998, annual gas inspections are mandatory. Forbes’ Gas Safe-registered engineers conduct these checks to ensure safe, legally compliant environments. Additionally, regular duct cleaning - often overlooked - is vital not only for performance but also for fire prevention. Forbes’ nationwide service mitigates these risks while optimising dryer efficiency.
Whether you need new rental equipment, service and maintenance for existing appliances, or a full purchase, Forbes offers flexible procurement routes to suit different operational models and budgets. Their expert consultants work closely with care providers to design tailored solutions for each setting.
With decades of experience in the care sector, Forbes Professional is a trusted partner to care homes across the UK; delivering dependable, fully supported laundry solutions that prioritise safety, compliance, and peace of mind. forbespro.co.uk | info@forbes-professional.co.uk | 0345 070 2335
See the advert on the facing page for more information.


HipSaver Soft Hip
Protectors protect the elderly and disabled people from fall-related hip fractures.
Designed to protect elderly people

Available as comfortable underwear or long casual pants in several sizes for men and women, HipSavers feature soft protective airPads permanently sewn into the garments over the hip areas prone to injuries and fractures. HipSaver TailBone models have an additional protective airPad over the coccyx on
Since our founding in 2010, Activities to Share has been dedicated to enhancing the lives of those in care by providing thoughtfully designed activity products. Our mission is to support activity coordinators in delivering uplifting, engaging experiences that foster connection, joy, and well-being. We achieve this by listening closely to your feedback and evolving with your needs. Whether over the phone, via email, WhatsApp, or

hip fractures.


In a care home, catering can be the difference between mealtimes that are anticipated with pleasure and those that are simply endured. Care itself is rightly personalised, tailored to the needs and preferences of each resident. The same principle should apply to the food they eat. Residents and their families are entitled to expect meals which reflect dietary needs, medical conditions, and personal tastes. But delivering that level of personalisation at scale, within budget, is no small task.
The Healthcare Management Trust acquired St Quentin Care Homes almost a year ago and has made significant improvements in care delivery, infrastructure, and leadership. Catering was a big area of focus and has brought tangible results: residents returning for second helpings, heartfelt thanks from families, and a noticeable reduction in food waste. These results haven’t happened by chance; they are the outcome of deliberate choices in how we source ingredients, design menus, and create the overall dining experience.
FRESH INGREDIENTS AND A VARIED MENU
The value of using fresh ingredients over pre-packaged or heavily processed alternatives cannot be overstated. Fresh produce boosts nutritional quality, enhances flavour, and increases the likelihood that residents will eat and enjoy their meals. Variety is equally important. A repetitive or bland menu fails to tempt people to the dining room. Similarly, introducing a rotating weekly menu with diverse flavours and textures, including vegetarian and vegan options, will create something for everyone, which is especially important where care homes support residents of varying ages and cultural backgrounds.
PRESENTATION MATTERS
Style should never overtake substance, but presentation matters and plays a vital role in whether a meal
By Charlotte McKay,
is eaten. An unappealing plate can lead to food being left untouched, no matter how nutritious it is.
Small touches make a big difference. Balancing colours on the plate, arranging food attractively, and serving it on crockery that complements the meal will encourage meals to be finished. Even something as simple as offering a platter of sandwiches with varied fillings, so residents first see vibrant colours rather than just bread, can boost appetite and engagement.
Many care home residents are unable to visit restaurants, and for them, mealtimes are often the closest equivalent to dining out. Recreating elements of that experience can lift the mood and turn a necessary routine into a highlight of the day.
Printed menus with clear, attractive typography help residents feel they have real choice and control. For some, reading a menu may even stir fond memories of past outings and family meals. This small detail reinforces the dignity and pleasure of the dining experience.
Sharing food is a social occasion. In care homes, shared meals can foster community spirit, reduce loneliness, and spark conversation. Making mealtimes engaging and enjoyable benefits both emotional wellbeing and nutritional intake.
This means paying attention to more than just the food. Lighting, music, table layout, and staff interaction all contribute to the atmosphere. A team that works seamlessly from kitchen to dining room by greeting residents warmly, knowing their preferences, and encouraging participation can transform mealtime into a joyful daily event.
Great catering doesn’t happen in isolation. It relies on strong collaboration between chefs, care staff, activities teams, administrators, residents, and families. Open communication ensures dietary needs are met, allergies are avoided, and preferences are respected.
When everyone takes shared responsibility, residents benefit from meals that are not only safe and nourishing, but also deeply satisfying. The catering team gains valuable insight from care staff who know residents well, while residents themselves feel heard and valued.
Ultimately, catering in a care home is about far more than providing three meals a day. It’s about respecting individuality, supporting health, and creating moments of joy. When meals are thoughtfully planned, beautifully presented, and shared in a warm environment, they nourish the body and the mind.

In the care sector, food is more than just nutrition - it’s comfort, dignity, and a way of bringing joy to residents every day. That’s why chefs can’t afford to compromise. From flavour and safety to consistency and versatility, every ingredient has to deliver. When it comes to bouillon, Knorr Professional refuses to settle for anything less than the best and so do the chefs who use it.
Knorr Professional Bouillon is the UK’s number one bouillon brand*, trusted in kitchens nationwide for its rich depth of flavour, outstanding versatility, and chef-trusted consistency. It’s made to work hard in every service, withno allergens to declare¹ options that give chefs peace of mind when catering for residents with diverse needs.
NEVER SETTLE FOR BLAND DISHES
As residents age, their sense of taste can diminish. That’s why flavour has to work harder in care - it’s not just about nutrition, it’s about enjoyment. Knorr Professional Paste Bouillon brings bold, balanced flavour that cuts through reduced senses, ensuring dishes remain satisfying and memorable. Whether it’s used as a base, rub, seasoning, glaze, or marinade, it delivers the same consistent, chefapproved results. From soups and stews to roasted vegetables and marinades, this is one product that performs across the menu - helping chefs adapt quickly without losing quality. NEVER SETTLE FOR UNCERTAINTY
In care kitchens, allergen safety isn’t negotiable. Theno allergens to declareoptions in Knorr Professional Paste Bouillon make it simple to create inclusive dishes without sacrificing flavour. This helps reduce the risk
of cross-contamination and ensures every resident can enjoy the same great taste.
For Knorr Professional Care Ambassador Preston Walker, that confidence is invaluable:
“With ‘no allergens to declare’ options available across the range, Knorr Professional Paste Bouillon is easy to introduce into dishes that need to be suitable for varying needs and preferences,” says Preston. “It gives me peace of mind that I can create flavourpacked dishes for all residents, without excluding anyone due to allergens.”
NEVER SETTLE FOR INCONSISTENCY
Care kitchens can be high-pressure environments, where time is short and the need for consistency is constant. Knorr Professional Bouillon’s paste format makes it easy to store, measure, and use, ensuring the same flavour profile in every batch. Its consistent yield also helps with budget control - delivering premium quality without waste.
Preston sums it up simply:

“We use the Knorr Professional Bouillon paste range for one simple reason - it delivers. Quality, flavour, consistency, and the confidence of knowing exactly what you’re going to get, every time.”
NEVER SETTLE FOR SECOND BEST
Every plate in a care home matters. It’s an opportunity to provide comfort, joy, and nourishment - and that means every ingredient has to earn its place. With Knorr Professional Bouillon, chefs can be sure they’re serving the very best in flavour, safety, and reliability. Because when it comes to care catering, settling for less is never an option.

How one simple training game is helping care homes improve outcomes for residents—and staff
In care homes dehydration remains a quietly persistent danger. While often invisible on the surface, its effects can be devastating—both for older adults and for the staff who care for them.
Despite being entirely preventable, dehydration continues to cause avoidable harm, hospital admissions, and even deaths among vulnerable care home residents. It can also impact staff wellbeing, concentration, and performance—making it a risk that affects the entire care environment. So why does dehydration still slip under the radar? And what practical steps can care homes take to tackle it head-on?
A QUIET EPIDEMIC IN CARE SETTINGS
Older adults are particularly vulnerable to dehydration for a range of reasons. As we age, our sense of thirst diminishes, and many residents have underlying conditions—such as dementia, stroke, or mobility impairments—that make it harder to ask for, reach, or consume drinks. Medications like diuretics or laxatives increase fluid loss, while difficulties swallowing (dysphagia) make drinking unpleasant or risky.
A study published in Age and Ageing (El-Sharkawy et al., 2015) found that over a third of older adults admitted to hospital were already dehydrated on arrival, and two-thirds remained so 48 hours later. More recent studies confirm that this remains a pressing issue. For example, care home residents are still five times more likely than community-dwelling older adults to arrive at hospital with dehydration, particularly with dangerously elevated sodium levels—known as hypernatremia—which significantly increases the risk of in-hospital death.
Despite public health campaigns and growing awareness, more recent reviews suggest the problem has not improved. As recently as 2022, a UKwide review of hydration practices in residential care estimated that around 20% of older adults remain clinically dehydrated at any given time. Some studies, depending on the criteria used, report prevalence rates as high as 34%.
Put simply, dehydration in care homes hasn’t gone away. It remains a widespread, under-addressed issue that continues to harm some of the most vulnerable people in our society.
IT’S NOT JUST THE RESIDENTS
While most dehydration efforts focus (rightly) on residents, it's important to recognise that care home staff are also at risk.
Working long shifts in hot, fast-paced environments, care staff often delay drinking water or miss breaks altogether. Some worry about not having time for toilet breaks. Others are simply too focused on their residents’ needs to think about their own.
The effects of even mild dehydration on staff can include fatigue, headaches, poor concentration, irritability, and slower decision-making— none of which is ideal in a safety-critical setting. Dehydrated staff may not perform at their best, and over time this can impact both care quality and wellbeing.
Supporting hydration in care homes, then, means supporting everyone—residents and staff alike.
A SIMPLE GAME, A BIG IMPACT
So how can care homes raise awareness of hydration risks, improve practice, and make learning more engaging?
One increasingly popular approach is The Hydration Game, developed by Focus Games. Designed specifically for health and social care staff, the game takes the form of a fun, team-based learning session that helps players explore the causes, risks, and solutions related to dehydration in care settings.
The Hydration Game prompts discussion, sparks reflection, and encourages staff to share their experiences and insights in a relaxed, collaborative way.
Players take turns answering questions, tackling realistic scenarios, and discussing how they might handle various hydration-related situations— from supporting a resident who refuses drinks, to spotting early signs of dehydration, to thinking about their own hydration habits during shifts.
The game typically lasts 45–60 minutes and is suitable for 2–12 players. It works well across all roles—care assistants, nurses, kitchen staff, cleaners, and even admin or maintenance teams—because everyone in a care home can play a part in hydration care.
There’s also an online version (ZeST) for teams who work remotely or across multiple sites.
REAL-WORLD RESULTS
Beyond awareness and engagement, hydration-focused training can produce measurable results. A notable example comes from Torbay and South Devon NHS Trust, which in 2021–2022 supported a hydration project across 33 care homes. The results were striking: a 63% reduction in falls requiring hospitalisation, an 18.5% decrease in urinary tract infections (UTIs), and zero UTI-related hospital admissions during the project period. What made the difference? A blend of simple changes: structured drink
At Simply Food Solutions, we believe that everyone deserves access to delicious meals tailored to their specific dietary requirements. Founded over 20 years ago, the company began with a vision to provide high-quality halal meals to hospital patients. Today, as part of the Bidfood family, Simply Food Solutions offers an extensive range of food solutions designed to meet the diverse needs of healthcare providers, care homes and individuals across the UK.
Our Product Ranges
SIMPLY PUREE
Designed for individuals with swallowing difficulties (dysphagia), the Simply Puree range offers texture-modified meals compliant with IDDSI guidelines. From Level 3 (Liquidised) to Level 7 (Regular), our meals ensure safety without compromising on taste. Options include soups, main courses, desserts and snacks, all crafted to the highest safety standards. Additionally, the Simply Puree Junior line caters to paediatric needs, providing
rounds, flavour and temperature choices, staff reminders, visual prompts, and team training.
The Hydration Game fits perfectly into this approach, helping staff explore and embed hydration-friendly practices in a way that’s memorable and motivating.
IDEAS FOR USING THE HYDRATION GAME IN YOUR HOME
Care homes that adopt The Hydration Game often find that it quickly becomes a flexible, well-used tool across their organisation. Here are some creative and effective ways it can be used:
As part of induction or refresher training, the game helps new staff understand hydration risks from day one—and makes mandatory learning more enjoyable. Many homes use it during Care Certificate sessions. During staff meetings or team huddles, a few game cards can be used to prompt a five-minute discussion. These quick conversations often uncover issues or ideas that otherwise go unspoken.
To promote staff wellbeing, the game can also prompt teams to think about their own hydration habits. “When did you last drink water?” or “How do you remind yourself to hydrate?” are simple but important questions that encourage better self-care.
Some care homes even use the game to identify “hydration champions”—staff members who demonstrate a real interest in promoting better hydration, and who can lead initiatives, monitor intake, or coach colleagues.
SHIFTING THE CULTURE
Ultimately, hydration in care homes is not just about checking drink charts or offering fluids at mealtimes. It’s about embedding a culture of attentiveness—where hydration is seen as an essential act of care, not an afterthought.
Games like The Hydration Game make this easier by turning serious issues into opportunities for learning, connection, and shared responsibility. They give staff the space to speak, reflect, and come up with practical ideas that make sense in their setting.
And when residents are better hydrated, they are safer, happier, more comfortable, and more independent. Staff are sharper, more resilient, and more engaged. Everyone benefits.
By making learning enjoyable and practical, The Hydration Game is helping care homes across the UK improve hydration outcomes and build stronger, more confident teams.
Want to learn more or get started? See the advert on the front cover and use the code for a 20% discount.
Visit www.hydrationgame.com for details and ordering options.
meals that are both safe and appealing for children.
SIMPLY HEALTHCARE
Meeting the needs of patients with allergies, intolerances, or specific dietary requirements, the Simply Healthcare range includes gluten-free, allergen-aware and renal-suitable meals. Each dish is pre-plated and ready to serve, ensuring convenience and consistency in meal preparation. The range encompasses a variety of meat, fish and vegetarian options, all designed to support patient health and satisfaction.
SIMPLY WORLDFOODS
Reflecting the UK's rich cultural diversity, Simply Worldfoods offers a selection of cultural meals, including halal, kosher and AfroCaribbean meals. This range allows healthcare providers to offer patients a taste of home, enhancing mealtime experiences and promoting cultural inclusivity.The range also provide multiportion dishes that are ideal for staff or visitor feeding cafes.

Explore our full range of products and discover how Simply Food Solutions can enhance your mealtime offerings, please visit https://simplyfoodsolutions.co.uk
Our son Rune is nearly six. He lives with a rare neuromuscular condition called Nemaline Myopathy, which affects his movement and strength. He needs round-theclock care, someone awake even through the night to manage his ventilator, medication, and medical equipment.
But the biggest threat to Rune’s health hasn’t been his condition. It’s been what he was being fed.
FORMULA NEARLY BROKE HIM
For the first few years of his life, Rune was in and out of hospital. He suffered from constant vomiting, painful tummy issues, repeated chest infections, and dangerous aspiration (when food or liquid enters the lungs). These episodes were terrifying, and they were all made worse by the “nutritionally complete” formula feeds he was given through his feeding tube. These formulas, the kind given to most tube-fed children and adults in the UK, are ultra-processed and heavy in dairy. For Rune, they made everything worse. He was deeply unwell, and we were told this was just part of his condition. But what if it wasn’t?

calories are made of, how they digest, and how they make you feel. Think about how you eat. Smelling, tasting, chewing, it all signals your body to start digesting. Tube-fed individuals miss out on that entirely, which means their bodies have to work harder. And if all they’re being given is sweetened shakes or oil-heavy blends, it’s no wonder they struggle to thrive.
TRIAL, ERROR, AND TRANSFORMATION
We had a lot to learn. Creating tubefriendly meals isn’t just about chucking leftovers in a blender. It takes careful attention to texture, nutrition, timing, and safety. But with help from open-minded professionals and a lot of research, we began to build blends tailored for Rune’s needs.
And the change was incredible.
The vomiting stopped. The chest infections slowed. His bowels started to work more normally. He had more energy for therapy. And for the first time in a long while, Rune felt more like himself.
Now, Rune shops with us. He picks out vegetables by smell and colour. He helps decide what goes into his blends. And incredibly, he’s even started tasting small amounts of purée by mouth, something we never imagined would be possible. He’ll always use his feeding button, but now he calls it his “powerup button.” He’s proud of it. And so are we.
FROM PERSONAL JOURNEY TO SHARED PURPOSE
Rune’s journey changed how we think about food, not just as nutrition, but as comfort, culture, and connection. We began to see how many tube-fed people, like him, are offered only one option: formula. For many, it’s essential. But it shouldn’t be the only choice.

Let’s be clear formula isn’t the enemy. For many people, it’s an absolute lifeline. It saves lives. It provides critical nutrition in a manageable, measurable, and medically supported way. This isn’t about demonising formula, it’s about recognising that one size doesn’t fit all. And for too long, that fact has been overlooked.
After one particularly rough hospital stay, we started researching alternatives, and that’s when we discovered the blended diet. In simple terms, it means blending real, cooked food so it can go through a feeding tube. It’s more common in places like the US, but at the time it was almost unheard of in the UK due to old guidelines and fears around safety. That’s changed in recent years. New evidence and updated NICE guidance now support the use of real food blends in medical care. Why? Because people do better. It's not just about calories, it’s about what those
This wasn’t just a lucky break. Study after study shows that real food can offer major benefits for tube-fed people, especially children, where most of the research has focused so far. But the logic applies to adults too. Imagine being used to eating normal food your whole life, only to be switched to synthetic-tasting formula with no smell, no flavour, no connection to the food you once loved. What does that do to your appetite? Your wellbeing? Your sense of self?
FOOD IS CONNECTION
In our home, food isn’t just fuel. It’s comfort. It’s an experience. It’s care. When Rune first started tube feeding, his feeds were done in private, away from the dinner table. That’s what his school and carers had been taught, to keep it discreet, hidden. But we didn’t want Rune to feel ashamed about how he eats. He deserves variety, flavour, and choice just like everyone else.
So we brought him into the heart of mealtimes.
Plenty of tube-fed people can still taste, smell, and even enjoy small amounts of food by mouth. So why shouldn’t they have access to real ingredients, varied flavours, and meals that reflect the same dignity as those who eat by mouth?
Together with a close family friend, we’ve started a small company Food Untethered, not just to create meals, but to rethink what it means to eat when you're tube-fed. Our aim is to support those on liquid diets to live fully, with options that nourish both body and spirit.
This all started with Rune, but it’s something so many others deserve too.

Sophia Johnston Co-founder of Food Untethered Parent carer for Rune Johnston www.fooduntethered.com contact@fooduntethered.com 07846690988




We’ve
But
Mobile Kitchens Ltd specialises in the hire or sale of temporary catering facilities and foodservice equipment.
Ideal for events or to provide temporary catering facilities during your kitchen refurbishment, our versatile units and equipment offer an efficient and economic solution to the caterers’ needs.
Production Kitchens, Preparation Kitchens, Warewashing Units, Dry Store Units, Cold Rooms and Restaurant Units are available as individual units in their own right or they can be linked together on site to form a complete complex.

Alternatively, we can offer modular, open-plan facilities, usually for larger, longer-term hires.
We offer a free design service, and project management from concept through to delivery and installation on site, plus full technical support throughout the hire period.

By Gill Ireson, Head Of Sales at cleaning manufacturer Robert Scott

Strong odours in care homes don’t just offend the nose –they can significantly affect the mental and emotional wellbeing of residents. Gill Ireson from Robert Scott explores how businesses can win the battle with advanced hygiene technologies.
Care homes should be places of comfort, dignity, and well-being for elderly residents.
Yet unpleasant odours can quickly erode that sense of home, creating an environment that feels unwelcoming and unhygienic. Care home managers face a complex mix of challenges - ranging from incontinence and bodily fluids to poor ventilation, food waste, and certain medical treatments. All of these can contribute to persistent odour problems, especially in communal areas where residents spend most of their time.
These lingering smells compromise air quality and can deeply affect residents’ emotional and mental well-being, often causing discomfort,
distress, and feelings of neglect. Visitors and staff, too, may interpret persistent odours as a sign of poor hygiene or substandard care, potentially harming the facility’s reputation.
For cleaning professionals, maintaining high standards of hygiene in this environment is no easy task. Regular cleaning alone is often not enough. Tackling the root causes of unpleasant odours, while also preventing the spread of germs in enclosed, high-use areas, requires both consistency and innovation.
Even spaces that appear clean can still suffer from foul smells caused by airborne bacteria, hidden contaminants, or poor drainage. To truly overcome these issues, care homes may need to go beyond traditional cleaning methods and adopt more advanced, targeted solutions. Ventilation and odour control technologies
While regular cleaning routines play a vital role in hygiene, they often fall short when it comes to long-lasting odour control in care homes. Odours can build up quickly, and traditional methods rarely offer continuous protection. To effectively manage this challenge, facilities managers are increasingly turning to advanced, automated solutions.
Precision fragrance systems provide consistent and controlled scent delivery, maintaining a fresh environment throughout the lifespan of each cartridge. These systems, based on fuel cell technology used in the pharmaceutical sector, ensure a steady and precise release of fragrance, making them a reliable, low-maintenance option for odour
management.
The technology operates through a generator that delivers a measured dose of oxygen, compressing a fragrance-filled pouch. This releases scent onto a cellulose pad, which gradually disperses a pure, clean fragrance into the space - ensuring consistent freshness without manual intervention.
In addition to scent systems, care homes are also adopting advanced air and surface purification technologies that neutralise odours and pathogens at their source. These environmentally friendly systems use UV light to treat airborne contaminants, combined with ozone disinfection and photoplasma generation to break down organic matter both in the air and on surfaces.
Such innovations can reduce airborne micro-organisms by up to 70%, effectively targeting viruses like influenza, E. coli, Listeria, and Salmonella, as well as bacteria, fungi, and algae. By removing odours and contaminants directly at the source, without relying on harsh chemicals, these systems provide a powerful, eco-conscious solution for maintaining cleaner, fresher environments, especially in high-use areas like washrooms or canteens.
Maintaining a fresh, welcoming environment has a lasting impact on the well-being of both residents and visitors in care homes. By integrating advanced odour control technologies, facilities can ensure a consistently pleasant and hygienic atmosphere - supporting emotional comfort, promoting dignity, and reinforcing a sense of home.
Smell Away Ltd. has unveiled its latest innovation: a dual-action HEPA air purifier designed homes and residential care homes across the UK and Ireland. Combining advanced allergen filtration with trusted odour control, this new solution promotes cleaner, fresher indoor air – crucial for the health and comfort of vulnerable residents and staff alike
As hay fever season intensifies and indoor air quality becomes a growing concern, the Smell Away® purifier addresses both allergen exposure and persistent odours in care environments. Its High-Efficiency Particulate Air (HEPA) filter captures 99.97% of airborne particles as small as 3 microns, effectively removing pollen, dust and mould spores. For elderly residents, especially those with respiratory conditions, this protection can ease symptoms and enhance wellbeing.
Long praised for its odour-neutralising technology, Smell Away® now integrates its premium RC412 Australian activated carbon with a proprietary additive to tackle common

care home smells – from food and cleaning agents to incontinence and smoke – discreetly and efficiently.
Designed for ease of use, the compact, quiet unit fits seamlessly into bedrooms, treatment rooms, and communal areas. It requires no installation, operates with low energy consumption, and offers a long filter life of up to two years. Free delivery is available across the UK and Ireland, with special rates for care homes purchasing multiple units. "Air quality has a direct impact on wellbeing," says Gareth Williams of Smell Away Ltd. "This filter isn’t just about cleaner air – it’s about creating a more dignified, comfortable environment for residents and staff."
With growing attention on indoor air standards, Smell Away® provides a practical, cost-effective tool for care homes committed to delivering safer, more pleasant living spaces – one breath at a time.
For further information see the advert below or visit www.smellaway.com/carer

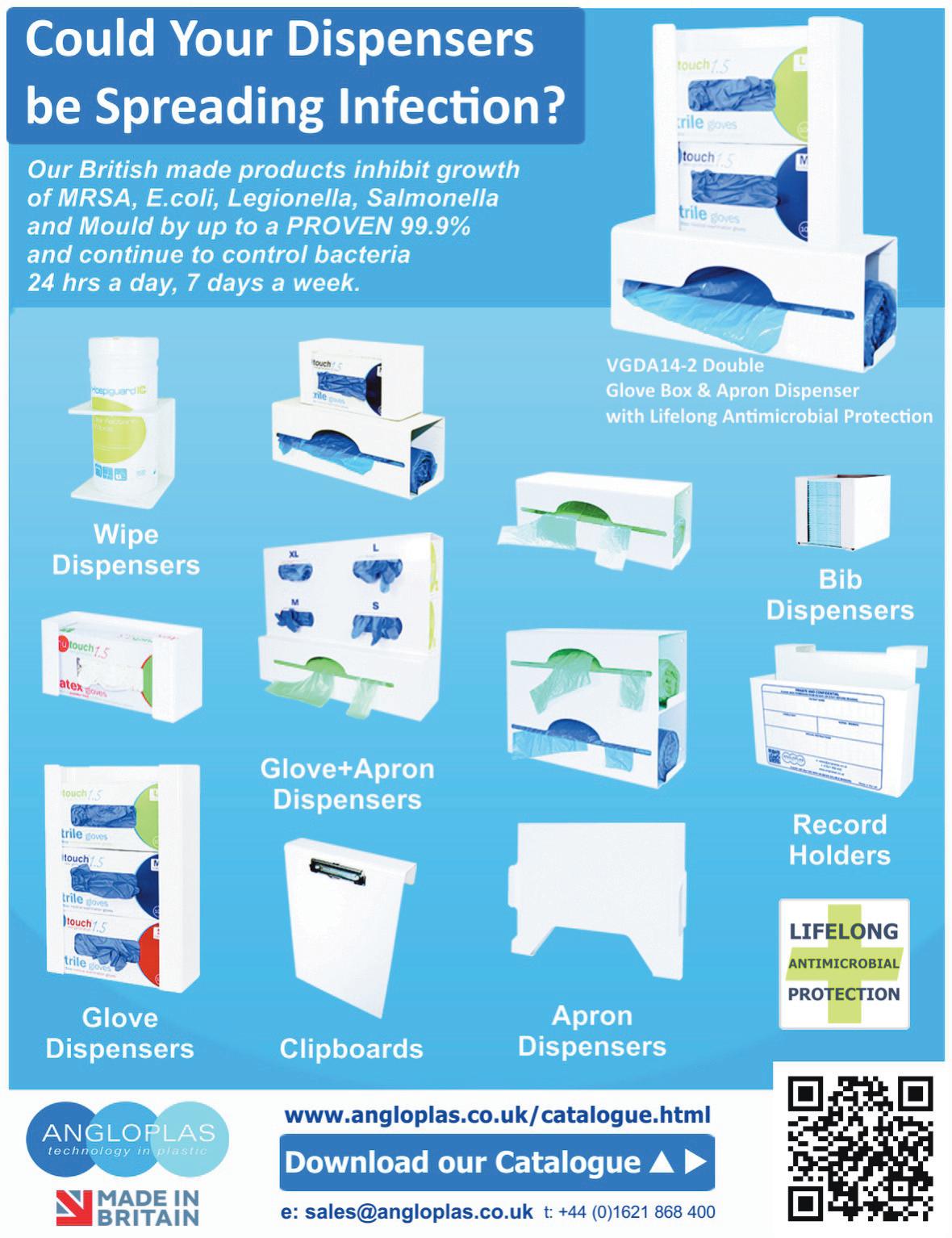
Part of Velair Group Limited, established 2012. Enviro-Save supplies costeffective and environmentally friendly washroom solutions, as well as being the Master Distributor for the Oxy-Gen Powered® air-care range in the UK and Republic of Ireland.

Oxy-Gen Powered® is the only technology that harnesses the power of pure oxygen to guarantee the delivery of fragrance into the air continuously, consistently and accurately for the entire duration of the cartridge life.
This innovative system is based on fuel cell technology that is used in the pharmaceutical industry to deliver drugs to human beings and animals.
Oxy-Gen Powered® technology is simple, reliable and cost-effective.
All Oxy-Gen Powered® fragrance cartridges contain Neutra-Lox, our proprietary odour eliminating ingredient that is extremely effective against the smell of urine, faeces, body odour, tobacco, pet malodour, kitchen odour, mould, mildew and more. Unlike other systems that only mask odours, Oxy-Gen Powered® cartridges eliminate odours and release fragrance effectively and continuously. Carbon footprint approved, and 100% recyclable cartridges; choose Oxy-Gen Powered® for cleaner air and a cleaner earth.
With no added solvents, alcohols, CFCs, VOCs or propellants, our Oxy-Gen Powered® cartridges contain 100% pure fragrance oil and are a safe choice for any facility.
See the advert on this page for further information.
Angloplas are a UK manufacturer who specialise in producing dispensers for the health and hygiene industry. Although these are designed to keep the workplace tidy and uncluttered they are, more importantly, built knowing the control of healthcare-associated infections (HCAIs) are a priority for healthcare providers, and who are employing a combination of infection prevention and control strategies, including hand hygiene, cleaning, training and the adoption of new technologies, to tackle the problem.

proven Antimicrobial PVC with silver ion technology and which is exclusive to Angloplas. This helps reduce the risk of cross infection by stopping the growth of bacteria and mould and works continuously for the lifetime of the product, reducing levels of bacteria such as MRSA, E Coli, Legionella, Salmonella and mould by up to 99.99%.
For non-clinical environments
As a result, a wide range of infection control products and technologies are emerging on the market, including antimicrobial technology. Angloplas’ range of dispensers are produced in the world’s first
Angloplas has recently launched its new Budget Range of products which are made to the same exacting standards as the antimicrobial protected ones but with lower price tags.
You can order Angloplas products directly from its website at www.angloplas.co.uk

Alarm Radio Monitoring is the market leader in the design, manufacture and installation of bespoke, endto-end, wireless alarm systems and solutions for the healthcare, leisure, custodial and education industries.
We have been providing wireless alarm and nurse call systems for over 30 years. Supplying care homes and hospitals with an essential lifeline that supports the delivery of outstanding care.

We believe in excellence which translates into:
Advanced Technology
Industry-leading wireless alarm technologies and software
Bespoke Solutions
We design systems to your needs rather than your team having to work around the system
Innovative Design
Pushing boundaries with the reliability that comes from decades in the industry
Flexible Finance Options
Ensuring organisations of any size can provide safety for their staff and clients
24 Hours a Day, 365 Days a Year Service
Your ARM service team is on hand, on the phone, on-site or return to base, whether you have a service contract or not
For further information, see the advert below or visit www.arm.uk.com
Modern nurse call monitoring systems represent a transformative advancement in residential care, bridging the gap between resident independence and professional oversight. These sophisticated platforms extend far beyond traditional emergency buttons, offering comprehensive monitoring solutions that support dignity whilst ensuring safety and prompt response to care needs.
The fundamental purpose of nurse call systems lies in empowering residents to maintain control over their care environment. When individuals can easily summon assistance, anxiety decreases and confidence increases, directly supporting psychological wellbeing and independence. This empowerment proves particularly vital for residents with mobility limitations or cognitive concerns who may otherwise feel vulnerable or isolated.
Recent Care Quality Commission reports consistently highlight response times to resident calls as key indicators of care quality. Effective monitoring
systems provide objective data demonstrating compliance with regulatory requirements whilst supporting continuous quality improvement initiatives.
Medpage’s commitment to innovation and quality is evident in their product range. Each solution is designed with the user’s safety and convenience in mind, making them a trusted choice for caregivers and healthcare providers alike.
By investing in these advanced fall prevention tools, families and facilities can create safer environments for those at risk. Medpage continues to lead the way in providing practical, reliable solutions that make a real difference.
For more information, visit Medpage’s official website or contact their team to explore these products further. Safety starts with the right tools, and Medpage delivers just that. www.easylinkuk.co.uk T: 01536 264 869
For more information, see later in this feature.


Data Analysis software provides a full audit trail of events
The all-new call logging software from ARM enhances the functionality of your care call system dramatically.
• It can help you track the quality of your service to your residents.
• It can help you demonstrate compliance with your aims and best practices, both to relatives and to authorities.
• It can help you find bottlenecks in service provision, track staffing requirements, and allow you to ensure staff are meeting expectations.
• Most importantly, it provides assurance that you know and can demonstrate what is happening in your care home.
The wireless ARM Nurse Call system has been developed over 30 years with both the client and user in mind.
It enables staff to efficiently answer calls, making the management of resources more flexible and provides the functionality you would expect of any nurse call system.
The system is quick and easy to install and works wirelessly, using radio communication between both the call points and the system infrastructure.
Call messages can be sent direct to staff to speed up response times and can also be integrated to work with smart phones & messaging.
Fall Savers®, are an experienced market leading healthcare provider of resident safety solutions for over 15 years.
FALL SAVERS ® WIRELESS MONITOR
Eliminate all cables with our new generation falls management solutions!
Upgrade your falls programme with the latest technology from Fall Savers®. The NEW Fall Savers®
Wireless eliminates the cord between the monitor and sensor pad. This results in less work for nursing staff, improved safety for patients and reduced wear and tear on sensor pads. Wireless advantages include the ability to use one monitor with two sensor pads simultaneously and support for many new wireless devices.
BENEFITS INCLUDE:
Safer for patients; less work for staff Bed and chair pads available
One monitor works with two sensor pads Integrates with most nurse call systems
A variety of options, including:

Floor sensor mat
Wireless door/window exit alerts
TREADNOUGHT
®FLOOR SENSOR PAD
The TreadNought® Floor Sensor Pad is built to last with a durable construction that far out lasts the competition. Our anti-bacterial floor sensor pad is compatible with most nurse call systems or can be used with a portable pager to sound an alert when a person steps on to the sensor pad. Caregivers typically place the sensor pad at the bedside, in a doorway or other locations to monitor persons at risk for falls or wandering. An optional anti-slip mesh reduces the potential for slippage on hard surface floors.
FEATURES INCLUDE:
Connects directly to most nurse call systems
High Quality anti-bacterial Floor Sensor Pad
Large Size Pad: Measures (L)

Blaucomm’s Nurse Call Messaging Service (NMS) is the market leading solution to remove the dependency on noisy nurse call panels and pagers, through its intelligent software, which delivers the alerts straight to the care staff who need them.
Care homes are rapidly introducing smartphones for digital care planning and eMar - now, the same devices can be used to receive the nurse call alerts they need for the residents under their care.
Furthermore, Blaucomm NMS is deeply linked into Person Centred Software MCM, so call bell data is linked straight to care plans. This unlocks a huge benefit to care homes to enhance the staff performance with how they accept and respond to residents, which ultimately promotes better response times and visibility for management to audit their performance.
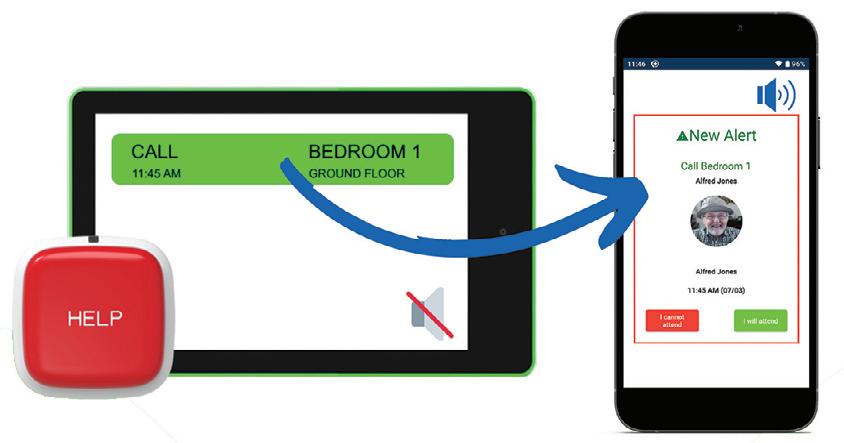
The best part is that Blaucomm NMS links into your existing nurse call system - we work with all major
brands such as Aidcall, ARM, Courtney Thorne, C-TEC, ENS, Intercall, Medicare, SAS and TeleAlarm.
Care operators are constantly recognising Blaucomm NMS for its reliability and dependability to their care operations, which is why we’ve been chosen time and time again over other solutions.
Head of IT Trudi Harrow at WCS Care had this to say about Blaucomm NMS:
“We find Blaucomm is a genuinely fantastic company with a reliable product.
"We would highly recommend this to anybody who wants to replace expensive pagers and silence those annoyingly loud nurse call screens!” To find out more about Blaucomm NMS, visit

Falls are a significant concern for vulnerable individuals, especially seniors and patients at risk. Medpage, a leader in assistive technology, offers a range of cuttingedge products designed to enhance safety and provide peace of mind for caregivers and families. Here’s an in-depth look at some of their standout solutions:
MPRCG1 (2023) BED LEAVING DETECTION ALARM WITH CAREGIVER RADIO PAGER
The MPRCG1 is a comprehensive system tailored for fall prevention in domestic, commercial, and NHS care settings. This all-inclusive kit includes a bed pressure mat sensor, a BTX21-MP alarm sensor transmitter, and an MP-PAG31 radio pager. The system is designed to alert caregivers when a patient leaves their bed, reducing the risk of falls. Key features include:
Wireless Alerts: Notifications are sent to the caregiver’s pager via tone or vibration.
Customizable Alarm Delays: Options for instant, 15-minute, or 30-minute delays.
Durable Design: Antimicrobial and disinfectant-resistant materials ensure longevity. Ease of Use: Minimal installation required, making it user-friendly and portable.
HDKMB2 HOSPITAL DISCHARGE KIT FOR FALLS RISK PATIENTS

The HDKMB2 is a thoughtfully curated kit aimed at supporting patients transitioning from hospital to home care. It includes essential tools to mitigate fall risks and promote recovery. This kit is ideal for caregivers seeking a comprehensive solution to enhance patient safety during the critical post-discharge period.
CMEX-21 MULTI-PORT WIRELESS SENSOR INPUT EXPANDER FOR NURSE CALL CONNECTION
The CMEX-21 is Medpage’s latest innovation, designed to integrate seamlessly with existing nurse call systems. This multi-port expander allows for the connection of multiple wireless sensors, enhancing the
monitoring capabilities of healthcare facilities. Its versatility makes it a valuable addition to any care environment, ensuring timely responses to patient needs.
RON-WC2 WATERPROOF DISABLED PULL CORD ALARM TRANSMITTER WITH WIRELESS ALARM RECEIVER
The RON-WC2 is a robust solution for disabled individuals requiring immediate assistance. This waterproof pull cord alarm is ideal for use in bathrooms and other high-risk areas. Paired with a wireless alarm receiver, it ensures that help is just a pull away. Features include:
• Waterproof Design: Suitable for wet environments.
Wireless Connectivity: Reliable transmission to the alarm receiver.
• Ease of Installation: Simple setup for quick deployment.
WHY CHOOSE MEDPAGE?
Medpage’s commitment to innovation and quality is evident in their product range. Each solution is designed with the user’s safety and convenience in mind, making them a trusted choice for caregivers and healthcare providers alike.
By investing in these advanced fall prevention tools, families and facilities can create safer environments for those at risk. Medpage continues to lead the way in providing practical, reliable solutions that make a real difference.
For more information, visit Medpage’s official website or contact their team to explore these products further. Safety starts with the right tools, and Medpage delivers just that. www.easylinkuk.co.uk
T: 01536 264 869
Courtney Thorne, a long-standing innovator in healthcare communication systems, is setting new standards in the care home sector with its advanced wireless nurse call technology—designed to improve resident safety, enhance staff efficiency, and support a more responsive care environment.
With over 30 years of experience serving the UK healthcare market, Courtney Thorne’s systems are now trusted by thousands of care homes nationwide. Unlike traditional hardwired solutions, their wireless nurse call systems offer non-invasive installation, scalability, and smart analytics—making them ideal for both new builds and retrofit projects.
“At the heart of our technology is the belief that better communication leads to better care,” says Graham Vickrage, Managing Director at Courtney Thorne. “Our wireless systems not only reduce response times but also empower staff

with the tools they need to deliver safe, person-centred care.”
Care providers are increasingly choosing wireless systems for their flexibility, reliability, and cost-effectiveness. With a full suite of accessories—including neck pendants, door monitors, fall detection, and bed sensors—Courtney Thorne systems can be tailored to meet the specific needs of each home and resident.
In an industry where compliance, safety, and staff pressures are always front of mind, Courtney Thorne provides more than just products—they offer ongoing support, training, and a commitment to innovation that helps care homes futureproof their operations.
For more information or to book a free demo, visit www.c-t.co.uk or contact info@c-t.co.uk.

Adult social care is changing fast. Across England, providers are swapping paper and patched-together systems for complete digital records, in step with the government’s Digitising Social Care programme.
Primera Healthcare, which supports people at home in Birmingham and London, has moved early and decisively.
The team started 2025 by upgrading their older care system to Allin-one PASS, adding digital care planning, rostering and finance tools so that every part of the service now sits under a single platform.
The switch felt less like a software update and more like turning on the lights. Travel times, staff skills and visit continuity now feed automatically into the rota, so late or missed calls are spotted and fixed before they become problems.

Medication notes flow straight into electronic MAR charts, and live GPS data shows managers exactly where carers are, cutting the need for frantic phone calls on busy shifts.
Most striking of all is GP Connect. With one tap, authorised staff can see up-to-date diagnoses and prescriptions, saving time and keeping visits focused on the person rather than the paperwork.
“The transition was seamless,” says Shaelene Dewar, Quality Assurance Auditor. “The journal view gives us a live window on the whole business, and the Data Creation Team at PASS built our new
3. ENHANCED MONITORING
is
finding its
care settings, the impact it can have is huge.
Here’s a closer look at why AI is set to make waves in social care:
1. BOOSTING EFFICIENCY
AI can help handle those resource-draining tasks in seconds. Whether it’s crunching a mountain of data, summarising care notes, or suggesting next steps, it frees up your team to do what they do best.
It can also improve communication, such as helping new team members quickly access policies or answer routine questions without waiting for assistance. By handling these background tasks, AI allows organisations to redirect resources to other core priorities.
2. ENSURING PERSON-CENTRED CARE
AI can support your teams when providing persona-centred care by analysing data over time, so they can build tailored plans that align with each individual’s goals, preferences, and abilities. It can even predict future needs, flagging issues before they arise so your team can act proactively.
Care organisations often operate round-the-clock, and AI can offer real-time monitoring to support this. For example, AI can highlight subtle behavioural changes, like someone sleeping poorly or becoming more withdrawn. These insights can alert your teams to potential concerns early, which means better, faster decisions can be made to support your clients.
For organisations, this level of tracking ensures care quality stays high, without adding to the workload. It’s like having an extra layer of support that’s always on duty.
4. EMPOWERING TEAMS
AI is here to help empower your care teams, not replace them. AI tools can provide instant recommendations or resources, which could help your newer employees confidently manage unexpected situations. Similarly, AI can assist with summarising care notes or giving quick access to up-to-date best practices, helping your teams provide the high-quality care they work so hard to deliver.
5. OPTIMISING COSTS
One of the big wins of AI is its ability to do more with less. By automating tasks and making resource allocation more efficient, it
forms in record time. GP Connect is brilliant. Reliable information in seconds, and the new charts help us spot patterns we never saw before.”
Those changes have delivered quick, concrete gains. Oversight is tighter, risk is lower, and staff spend more minutes each day with the people they support.
Everything is logged, time-stamped and ready for inspection, which reassures families and pleases regulators.
As everyLIFE Technologies marks ten years of PASS, Primera’s experience shows what the next decade can look like when digital tools are placed at the heart of care.
Good care can always get better, and better starts with digital.
Ready to explore your own next step? Visit www.everylifetechnologies.com or call the everyLIFE team to see how PASS can help your service.
can help organisations manage tight budgets without compromising on care.
AI can even help reduce staff turnover by easing workload pressures, which means savings on recruitment and training costs too. Plus, because AI solutions are scalable, it can adapt to your organisation's needs.

AI in social care isn’t about replacing people with tech. It’s about giving your teams the time, insights, and tools they need to focus on the people they care for. That’s why OneAdvanced AI, the first UK hosted fully secure, private AI tool for businesses, was created. OneAdvanced AI can help care providers improve efficiency, deliver person-centred care, and empower teams, all while safeguarding your data. This marks a significant step towards a more innovative and sustainable future in social care.
Find out more at: www.oneadvanced.com/ai
See the advert on the back cover of this issue for further info.




A new report from the Digital Care Hub, Online But Unsupported, highlights the vital role care homes and other care providers play in supporting people with learning disabilities to stay safe online.
Digital access is now a routine part of life. People use the internet to keep in touch with family and friends, follow hobbies, do their shopping, and increase their independence. But alongside the many benefits come real risks—and people need the right support to manage them.
The research, commissioned by Better Security, Better Care and delivered by Cyber Champions, found that while many people with learning disabilities feel confident using the internet, fewer feel confident about keeping themselves safe.
Key challenges identified include:
• Only 31% of people knew how to spot a fake email or scam
Nearly 30% didn’t know how to change privacy settings on social media
Almost a quarter weren’t sure how to update device security

Some people had been tricked into sharing inappropriate images, not realising the risks or consequences
Others struggled to tell the difference between online and real-life friends
Carers also raised concerns about online grooming, sexting, bullying via messaging apps, and people oversharing personal information.
Care home staff, volunteers and family members are central to helping people manage these risks. But the report found that carers often don’t get the practical training or support they need.
• 89% of staff support people online at least once a month
25% had received little or no training in digital safety
• 69% said their training was annual but not tailored to real-life situations
• Around 30% said they didn’t know how to set up two-factor authentication or update device security
“We need to make online safety part of everyday conversations in care,” said Samantha Leonard, new Director of ARC England. “Staff need to be seen as the experts, but they do not need to feel confident talking about online risks, noticing red flags, and knowing where to go for trusted support.”
Anu Khurmi, CEO of Cyber Champions, added: “Cyber Champions is a notfor-profit initiative encompassing organisations from the private, voluntary and public sectors. Its goal is to make a difference to local communities and future generations by promoting best practices in digital literacy, online safety and cyber skills.”
The report calls for care providers to invest in regular, scenario-based training for staff—moving beyond tick-box approaches. It recommends using roleplay and real-life stories to help people with learning disabilities understand online safety in simple, everyday terms.
“We need to make online safety part of everyday conversations in care,” said Samantha Leonard, CoDirector of Cyber Champions. “Staff don’t need to be tech experts, but they do need to feel confident talking about online risks, noticing red flags, and knowing where to go for trusted support.”
The report also encourages care organisations to build a culture where staff can share new threats, ask questions, and learn together. By doing so, care providers can help people with learning disabilities enjoy the digital world safely and confidently.
Free resources and guidance are available at: www.digitalcarehub.co.uk/OnlineButUnsupported

In today’s regulated care environment, having clear, current, and wellcommunicated health and social care policies is essential for delivering safe, compliant services. The Care Quality Commission (CQC) now places increasing emphasis on how policies are implemented and understood—especially during registration and inspections.
Outdated or poorly communicated policies can significantly impact your CQC rating. Even if documentation is comprehensive, failure to ensure staff understand and follow procedures may lead to a “Requires Improvement” or even “Inadequate” rating under the ‘Effective’ domain. Well-maintained policies promote consistent standards across care teams and help safeguard services when incidents arise. In regulatory investigations, the first request is often to review relevant policies—making accuracy and accessibility key to reducing legal and compliance risks.

However, keeping policies up to date is challenging. Constant changes in legislation, best practice guid-
ance, and case law mean that policies can quickly become obsolete. W&P has been a trusted provider of CQC-ready care policies and procedures for over 20 years. Our expert team monitors industry developments to ensure your policies remain fully compliant.
Our Online Policy Portal simplifies policy management. With just a few clicks, providers can update content, distribute documents to staff, track confirmations, and monitor compliance via a real-time dashboard. You can even provide temporary read-only access to inspectors—demonstrating transparency and accountability instantly.
Ensure your care service meets CQC expectations with fully up-to-date, easily accessible, and well-communicated policies.
Email: info@wandptraining.co.uk
Call: 01305 767104
for details.

By Becky Mundie, RotaCloud (https://rotacloud.com)

How much time do you spend on admin?
How long are you locked away in your office to make the rota, only having to go back again and again for amends? How often have you realised you’re understaffed, resulting in overspending on agency staff? How frequently do payroll errors, messy audit trails, and chasing staff who missed a shift update occur?
It’s constant, the stress of it all. It’s enough to carry the care of your service users on your shoulders without being overwhelmed every day by repetitive admin and errors. You never thought you’d be spending more time amending schedules, chasing for cover, and correcting issues than your actual job.
But those inefficiencies — staff shortages, payroll errors, missed shift updates, and multiple spreadsheets you juggle — cost you money, time, staff retention, and, in some cases, compliance.
It’s easy to suggest investing in budgeting tools or certain tech to help you understand spending before it happens and to automate certain processes. Budgets are tight in care, after all. But there are simple fixes to cut your operating costs without cutting back on care if you can’t yet turn to digital systems.
Cutting costs doesn’t just mean spending less. It’s about making smarter decisions – reacting to and fixing
the cause of the problem, not the effect. And it all starts with your rota.
There are ways to take better care of your rota, which will, in turn, improve efficiency and staff morale.
One main way: putting your staff first.
First, give your team more say in when they work by allowing them to submit their availability. Try making a rolling rota with a mix of most and least preferred shifts so everyone gets a fair share of them. It means far less admin for you when the rota repeats, far fewer last-minute amends, a more accurate payroll, an easier audit trail, and no more miscommunications on when everyone’s working.
Second. Share rotas at least two weeks in advance. Doing so allows enough time to make amends and for everyone affected to be updated. Sticking to this process is more efficient, which means less admin – which means more time to focus on service users.
Third. Put in a more seamless process for holiday requests. Whether a submitted form or limiting to one means of messaging, sticking to one process means fewer lost or forgotten requests and much less paperwork. Plus, allow staff to arrange shift swaps themselves, leaving managers to simply approve or deny. Again, less time on admin means more time for service users.
All in all, your saviour is flexibility. Flexibility in rotas means less admin for managers, more efficient teams and safe staffing levels, happier staff (and higher retention rates), and, in return, happier service users – all saving costs in the process. After all, when you aren’t making last-minute changes or relying on agency staff to cover no-shows, you stick to the staffing levels and labour budgets you’ve forecast. So long, overspending, lost time, and inefficient processes.
Technology is a key part of the CQC’s improvement agenda; especially when it comes to how care services record performance during inspections.
THE PROBLEM
Many care providers want to move away from pen and paper-based audits and spreadsheets, but most software lacks the capability and flexibility to handle the complexity of the CQC requirements and ratings structure – leading to gaps in oversight and accountability.
THE SOLUTION
Drawing on our experience providing CQC improvement support, we developed an easy-to-use care audit platform designed to help care providers stay on top of their compliance obligations with the user in mind and the CQC framework at its core.

Our Enterprise Care Audit Tool enables care providers to improve oversight and respond to CQC requirements with confidence — delivering greater visibility, accountability, and control.
Now, we’ve made that same expertise and capability more accessible.
Our new cloud-based version is built on the same trusted foundation, giving providers of all sizes a faster, more flexible way to manage compliance with ease.
KEY FEATURES
• CQC-Aligned Dashboard - View audit outcomes and actions against CQC rating thresholds, with drill-down visibility for full organisational oversight.
• 100+ Ready-to-Use Audits - Covering all core operational areas including Care, Health & Safety, Estates, Catering, HR, and more.
• 2,000+ Question Library - Choose from a comprehensive library of questions, each aligned to statutory regulations and the CQC inspection framework.
• Automated Action Management - Audit outcomes that require follow-up are automatically fed into the dashboard and actions portal for clear accountability and tracking.
Reporting - Access a suite of structured reports to support internal reviews and inspection readiness.
• Engagement Surveys - Collect feedback from staff, service users, and relatives STRESS LESS. TRACK MORE. BE READY.
If you’re spending hours chasing paperwork or stressed about being prepared for any inspection any day
- Care Audit Tool can help.
Website: careaudittool.co.uk
Email: info@careaudittool.co.uk
Phone: 0333 577 0807

QCS x Carebeans, the UK’s leading digital provider of compliance, care management and workforce solutions for the adult social care and support sector, announces the launch of QCS Learning Centre - a powerful new addition to their growing ecosystem of connected tools built to help providers deliver safer, smarter care.
Developed in partnership with CareTutor, a trusted training expert with over 20 years’ experience in the care sector, QCS Learning Centre offers accessible, accredited and engaging video-based training designed specifically for frontline care teams.
“We’re building the future of digital care,” says Nikki Walker, CEO at QCS. “The QCS platform is about more than just ticking boxes. We’re creating an intelligent, joined-up system where compliance, care management and training all work together – backed by rich data that powers our AI integrations, all driven by realworld care and support challenges, designed to give time back to providers when they need it most.”
A CONNECTED ECOSYSTEM – SMARTER TOGETHER

QCS Learning Centre is fully integrated into the wider QCS x Carebeans platform, which brings together care planning, rostering, audits, mock inspections, policies and training into one seamless digital experience. This connected approach means that care and support teams can respond faster, train smarter and make better decisions - all in one place.
Whether you’re running a care home, a domiciliary service or supported living provision. Every part of the system works together to reduce admin, keep you inspection-ready and support better outcomes for the
people you care and support for.
Luke Bond, Managing Director at CareTutor, adds “QCS Learning Centre is more than just another training tool. It’s the next step in supporting a stronger, more confident workforce - providing engaging and interactive, video-led courses designed and created by CareTutor specifically for the adult social care sector”.
What QCS Learning Centre Delivers:
Accredited, video-led training developed by sector experts
• Smart tracking and reporting to keep training up to date and inspection-ready
Designed for real-world care and support - simple to use and quick to deploy
Supports staff development, retention and quality improvement
Future integration roadmap with the full QCS x Carebeans system planned BUILT FOR THE SECTOR. BACKED BY AI.
With AI-powered features running across QCS x Carebeans platforms – the rich data within the system enables intelligent audit tools to real-time alerts and automated policy updates - QCS Learning Centre is part of a long-term vision to reduce admin, raise care quality and give providers back the time they need to provide and evidence quality care and support.
READY TO SEE IT IN ACTION?
Explore the QCS Learning Centre today and see how it can support your service so you can be assured your team is skilled, confident, and able to provide higher-quality care and support.

https://www.qcs.co.uk/qcs-learning-centre/
By Eleanor Stephens, Senior Solicitor – Insolvency at law firm Harper James

The UK care sector is under significant financial pressure with rising costs, workforce shortages, and longterm underfunding pushing many care providers towards breaking point. These challenges have only intensified following recent Budget announcements, with increases in the National Living Wage and National Insurance placing further pressure on already resource-stretched organisations.
Recent findings from the Care Provider Alliance paint a stark picture.
A survey of over 1,100 care providers revealed that 73% expect to refuse new care packages, 77% are drawing on reserves, 64% anticipate redundancies, and 22% are considering closing altogether. These figures represent more than just operational strain; they signal a threat to vulnerable adults who rely on essential care, families who depend on support, and dedicated staff who risk losing their livelihoods.
Despite the severity of these challenges, care providers are not powerless. There are practical steps and strategies that can help navigate financial distress and build resilience for the future. In this article, Insolvency Solicitor Eleanor Stephens discusses how you can identify if there are cash flow issues in your business and the steps you can take as a care home provider.
HOW CAN CARE HOME OPERATORS RECOGNISE THE EARLY WARNING SIGNS OF FINANCIAL DISTRESS?
Financial distress rarely arrives without warning, recognising the signs early allows care providers to take action before problems escalate. Common warning signs include difficulties managing cashflow, increasing reliance on short-term borrowing or reserves, and delays in paying suppliers, landlords or HMRC. Indirect indicators, such as rising staff turnover, difficulties recruiting, or pressures around meeting regulatory standards, can also point to underlying financial stress. Directors, no matter the sector, have a legal duty to act in the best interests of creditors once a business faces potential insolvency. Ignoring warning signs not only reduces the chance of recovery but also increases the risk of wrongful trading, which can lead to personal liability.
What steps can care home providers take?
Start with a detailed financial health check, this includes reviewing cashflow forecasts, profit margins, and liabilities. Identify immediate pressures and longer-term risks. This step is not just for the finance team, senior leadership, including operations and HR, should understand the business’s financial position to work together on solutions. Its imperative to ensure you maintain an accurate and up to date financial picture so all directors are aware of the realistic financial situation and
can make decisions based on up to date information.
Engaging with key stakeholders early is an important step. Open conversations with lenders, landlords, suppliers, and local authority commissioners can create opportunities to renegotiate terms, extend payment deadlines, or secure additional support. Many stakeholders would rather help a business recover than see it fail.
Cost structures should be reviewed carefully. Are there areas of spend that can be reduced without affecting care quality? Are contracts still fit for purpose, or could they be renegotiated? Are there opportunities to refinance or access new funding?
UNDERSTANDING YOUR BUSINESS’ RESTRUCTURING AND INSOLVENCY OPTIONS
In the care sector, financial pressure can build gradually, rising operating costs, staffing shortages, and delayed local authority payments can impact cash flow. For many business owners, the word ‘insolvency’ can feel like a last resort, or something to be avoided at all costs. But in reality, insolvency and restructuring processes are there to help businesses, not punish them.
If your care home is facing financial difficulties, understanding your options early can make all the difference. A legal process such as administration is designed to give viable businesses the breathing space they need to stabilise, restructure, and recover.
Here are the most common routes and options: COMPANY VOLUNTARY ARRANGEMENT (CVA)
A CVA is a legally binding agreement between a company and its unsecured creditors, typically to repay debts over a fixed period, often at reduced amounts.
The key advantage is that the business can continue trading while the CVA is in place. Directors stay in control, and staff, residents, and suppliers can experience minimal disruption.
How it works:
• The company proposes a repayment plan, usually spread over 3–5 years
• Creditors vote on the proposal at least 75% (by value) must agree for it to proceed
• Once approved, all unsecured creditors are bound by the terms
• The business continues to operate under the supervision of an insolvency practitioner
Why it works well in the care sector:
• Preserves continuity of care and minimises disruption for residents
• Retains jobs and protects staff morale
• Can prevent reputational damage by avoiding formal insolvency proceedings like liquidation
• Shows creditors that you’re taking proactive steps to meet obligations ADMINISTRATION
Administration is a formal insolvency process where control of the business passes to a licensed insolvency practitioner (the administrator). Their role is to act in the best interest of creditors and try to rescue
the business where possible.
During administration, the company is protected by a legal “moratorium”, meaning creditors can’t take enforcement action without the administrator’s consent or court approval.
What administration can achieve:
• Restructure the business to cut costs or exit loss-making contracts
• Sell the business as a going concern, preserving value and jobs
• Deliver a better return to creditors than an immediate liquidation Why this matters for care homes:
• Resident care can continue while the administrator explores rescue or sale
• It creates space to secure investment, agree a pre-pack sale, or restructure leases and liabilities
• Essential suppliers (e.g. food, utilities, medical services) are more likely to continue supply during a managed process LIQUIDATION
Liquidation is the process of closing down a company in a structured and lawful way. Assets are sold, creditors are repaid in order of priority, and the business is removed from the Companies House register. There are two main types:
• Creditors’ Voluntary Liquidation (CVL): initiated by directors when the business is insolvent and can’t continue trading
• Compulsory Liquidation: initiated by a creditor via court proceedings
What happens in liquidation:
• All trading ceases
• A liquidator is appointed to sell assets, settle debts, and distribute any remaining funds
• Employees are made redundant (with access to redundancy pay and other statutory entitlements)
• Directors’ duties continue during the process and are reviewed by the liquidator
When liquidation is appropriate:
• The business has no realistic prospect of recovery
• There are more liabilities than assets
• Continuing to trade would risk further losses or wrongful trading by directors
For care businesses, liquidation should be a last resort, but if recovery isn’t possible, it can allow directors to close the company in a way that meets legal obligations and limits personal risk.
SUMMARY
Many care homes in the UK are under real financial pressure. Rising costs and cash flow issues are making it harder to keep things running smoothly. Acting early is key: review your finances, talk to lenders and suppliers, and seek professional advice. Options like CVAs and administration can help restructure and protect your business, while liquidation should only be a last resort. Throughout the process, maintain clear communication with residents, families, and staff prioritising their wellbeing.

The Home Office has announced major reform of the Immigration Rules and the changes came into effect on 22 July 2025.
New rules were laid in Parliament on the 1st July 2025, which see skills and salary thresholds rise to the previously set RQF level 6, overseas recruitment for care workers to end, and between 100 and 180 occupations no longer eligible under the skilled worker visa route.
The new Immigration Rules came into force on 22 July 2025.
There is no doubt that the UK’s social care system will suffer from the UK government tightened immigration rules.
One of the major changes which will directly affect the social care sector is the Skilled Worker entry clearance applications for care workers (SOC code 6135) and senior care workers (SOC code 6136) being closed on 22 July 2025.
The government’s position is that care providers can recruit from the regional care partnerships which have a significant pool of displaced care workers. Furthermore, the government believe that resident workers can be trained to carry out these roles. However, both of these approaches are flawed.
The displaced workers pool will eventually diminish and there is no real plan to identify where the social scare sector will recruit for the carer and senior carer roles.
Key Takeaways: What Steps Should Care Providers Take Now
Providers holding a sponsor licence should carry out a full audit of their HR processes and the five areas of compliance under the sponsor guidance. Take advantage of the Aston Brooke Solicitors UKVI mock audit service. Please contact Mr Kashif Majeed and email km@astonbrooke.co.uk to book an appointment.
In addition to the above, the following action must be undertaken as a matter of urgency:
Global assists clients throughout the U.K. who specialise in the healthcare sector to achieve their objectives of purchase, development and refinance.
We have organised over £1.8bn for clients in the past 30 years, providing clients with competitively priced funding to refinance existing debt, ease cashflow and develop businesses further. From helping clients make their first purchase through to allowing groups to grow significantly in size we assist at every stage of your business expansion.

Every proposal is individual and deserves to be treated that way, so we hope you will allow us to be of assistance to you and call us to chat through your plans and requirements, I am sure we will be able to tailor a facility to your requirements. Call us on 01242 227172 or e-mail us at enquiries@globalbusinessfinance.net

1. Sponsored Migrants Salary Audit
As there are no transitional arrangements for the new salary thresholds, employers must review the salaries of all sponsored workers. If you are assigning CoSs on or after the 22 July 2025, you must meet the new salary thresholds to ensure compliance of the rules.
2.Compliance of the Skill Level Threshold
Please ensure compliance of any roles filled which fall below RQF level 6 and that they also appear on the Temporary Shortage List and the Immigration Salary List.
Please ensure that any roles sponsored under SOC code 6135 and 6136 are for existing staff who have been employed in the business for at least three months.
There are more changes to come later this year which include:
1. Increasing the immigration skills charge
2. Increasing the English language requirements across the immigration system.
For clear and comprehensive advice on the new rules, its implementation and how it affects your business,
please contact Mr Kashif Majeed, Director at Aston Brooke Solicitors. Email: km@astonbrooke.co.uk
"23 years, operating 4 Devon Nursing homes, has been pretty tough, as anyone in social care, knows, only too well. And if it was hard already, after 2024 budget, it's just got harder. Anyway, at heart, I am just customer of Eden Alternative, and it was a stroke of luck to come across this whilst on holiday in New Zealand in 2009. It started in USA in 1994 and now runs in 22 countries.

it's a programme that is straight forward, tried and tested for 30 years and really works. Its member care organisations generally become trainers for their own teams, and run it themselves. The programme is run in person over 2-3 days or online 1 hr a wk for 7 weeks. You choose.
The fact that I am now involved with this not-forprofit organisation (in the UK area) came about when one of the 2 main UK directors died suddenly just before Covid. But it's something I have run with for 11 years to help make 'vision' a reality, not a struggle. So, being both a customer and helping the admin seems quite natural.
It is a modern philosophy of care, but moreover,
It addresses loneliness, helplessness and boredom and operates through 10 principles to underpin 7 critical domains of wellbeing. Moreover, it's effective, transformational and really works. As residents, and team members wellbeing, matter so much it's a must, in my opinion. Geoffrey Cox Southernhealthcare.co.uk eden-alternative.co.uk"