



















Today's Skills for Care report brings welcome news for our sector – a 2.2% increase in total posts and a £77.8 billion contribution to the UK economy.
These are encouraging figures that demonstrate the continued growth and vital importance of adult social care.
Last week, whilst exhibiting at the CARE Show at Birmingham's NEC, the issue of overseas recruitment was highly topical among delegates and exhibitors alike.
The timing couldn't have been more pertinent given today's findings. The report has been positively, albeit cautiously, greeted by leading sector organisations and spokespersons who have shared their views with THE CARER (see page 4).
In Birmingham, I was speaking with a leading immigration lawyer who, I hope, will be writing a comment piece for us in the coming weeks.
They were quite outspoken regarding the government's policy on overseas workers in the care sector, raising a question that many in our industry are now asking: did the government "throw the baby out with the bathwater" when it revised its policy in July?
The UK government ended overseas recruitment of care workers on 22 July 2025 by removing the role from the list of eligible occupations for the Health and Care Worker visa.
This means care providers can no longer sponsor new staff from abroad for these roles, although existing visa holders can continue to work and switch employers until July 2028.
However, as today's report shows, the numbers tell a concerning story. While improvements in workforce capacity continue to be supported by international recruitment, the number of new international recruits fell from 105,000 in 2023/24 to 50,000 in 2024/25.
Over the same period, the number of workers with British nationality declined by 30,000 – a 2.6% decrease. With the sector projected to need around 470,000 new posts by 2040 (an increase of 27%), the mathematics simply don't add up. Scotland has been the first to "break ranks".
First Minister John Swinney has announced that the Scottish Government will directly sponsor visas for overseas care workers to counter Westminster's immigration restrictions.
The SNP leader described his intervention as a necessary "solution" to what he called a staffing crisis, with care homes across Scotland desperately short of workers following the UK Government's tightened immigration controls.
To quote a well-known phrase: "the road to hell is paved with good intentions".
While I understand the government's intentions to train a domestic workforce, it was, as observers say, badly thought out and implemented.
Critics and providers contend that current domestic recruitment efforts are insufficient and will exacerbate shortages and impact the quality of care.
What is abundantly clear from today's report is that vacancy rates remain three times higher than the wider economy, with tens of thousands of British workers leaving the sector each year and demand only set to rise. Without urgent action to revise the current overseas recruitment policy and simultaneously build capacity at home, the progress seen in this report risks being short-lived.
On a brighter note, congratulations to Allegra Care's nursing homes Olive Tree House and Rose Garden, winners of our coffee morning competition. (See pages 18-22.)
We again had a fantastic response from care homes all over the UK – every one a winner, but sadly we could only pick one (well, in this case, two) since the homes collaborated with a sustainable fashion show which took TWO months to prepare.
Very well done, and once again thank you for all the wonderful nominations – a testament to the dedication, commitment and hard work of those in the sector who do so much to enhance the wellbeing of their residents and to support the amazing work of Macmillan.

I would encourage our readers to sign up for our bi-weekly digital newsletter at www.thecareruk.com and follow us on social media for all the latest news.
The Carer is published by RBC Publishing Ltd, 3 Carlton Mount, 2 Cranborne Road, Bournemouth, Dorset BH2 5BR.
I can always be contacted at editor@thecareruk.com
damage. Views expressed within this publication are not necessarily those of the publisher or the editorial team.
responsibility for any effects, errors or omissions therefrom. All rights reserved, reproduction is forbidden unless

£77.8
(CONTINUED FROM FRONT COVER)
Vacancy rates have also returned to pre-Covid levels at 7% (as reported in our ‘Size and structure of the adult social care sector and workforce report’) and the proportion of men in the workforce reached a new record for the third successive year – now at 22%.
INTERNATIONAL RECRUITMENT
While improvements in workforce capacity continue to be supported by international recruitment, the number of new international recruits fell from 105,000 in 2023/24 to 50,000 in 2024/25. Over the same period, the number of workers with British nationality declined by 30,000 (a 2.6% decrease).
With the vacancy rate still around three times that of the wider economy, the report’s findings demonstrate how, rather than overseas recruits taking jobs from British people, international recruitment has continued to benefit employers struggling to recruit domestically. The lack of growth in domestic recruitment highlights the need to build a more sustainable, long-term workforce.
For the first time, the report includes figures on employer sick pay and pension contributions which show that 62% of care providing establishments using the Adult Social Care Workforce Data Set (ASCWDS) don’t offer enhanced sick pay and 57% don’t offer enhanced employer pension contributions (more than 3%).
The proportion of care and support workers with a Level 2 qualification has fallen to 38% – down from 41% in 2023/24 and 48% 2018/19.
As part of the report, Skills for Care analyses ‘Five factors affecting turnover’. These are:
• pay up to 30% below the local authority average not being on a zero-hours contract receiving training having a qualification relevant to social care
• working full-time.
The latest findings show a contrast in turnover rates: people with none of these factors in place are almost three times more likely to leave their jobs compared to people with all five factors (42.2% vs 14.4%).
Other key findings from the report include:
The vacancy rate for 2024/25 fell to 7%. This was a return to similar levels seen prior to 2021/22, when the rate had peaked at 10.5%.
The total number of vacant posts in 2024/25 was 111,000, which is a 12.4% decrease on the previous year.
The number of filled posts grew by 3.4% to 1.6 million. This growth was smaller than the previous year, but still the second highest increase on
record.
The turnover rate in the independent sector decreased from 25.8% in 2023/24, to 24.7% in 2024/25.
The total number of posts in adult social care in England – comprising filled and vacant posts – was 1.71m in 2024/25.
The sector still faces long-term recruitment and retention challenges as it is projected to need around 470,000 new posts – an increase of 27% – by 2040 to keep up with the projected growth in the population over the age of 65.
Professor Oonagh Smyth, Skills for Care’s CEO, says: “Our latest report highlights the complex nature of the social care sector today, with encouraging signs of progress for our workforce, alongside challenges that still need to be addressed.
“It’s positive to see our workforce growing, and vacancy and turnover rates continuing to fall. However, much of this improvement is being driven by international recruitment and, as both domestic and international recruitment are slowing, we need to explore new pathways to build sustainable workforce capacity.
“At the same time, falling qualification levels – when care roles are becoming more complex – suggest that capability, as well as capacity, is likely to be a challenge in the future. We have to ensure that people have the skills, values and confidence to do these essential roles in social care.
“To meet growing and changing care needs, we must prioritise domestic recruitment and invest in learning and development for our workforce.
“That’s why initiatives such as the Workforce Strategy that we published last year, and steps towards a Fair Pay Agreement and a National Care Service are so important. They are vital to building a thriving, skilled workforce that plays a central role in neighbourhood health – and ultimately supports people to live a good, independent life in a place they can call home.
“Skills for Care will continue to work with partners across the sector to support workforce development in practice and ensure the insights from this report inform future planning and policy.”
Dr Wendy Taylor, Chair of the LGA’s Health and Wellbeing Committee, said: “The care workforce plays a fundamental and invaluable role in supporting people who draw on social care to live the independent lives they want to lead.
"Growth in the care workforce is a positive reflection of recent progress in improving capacity, stability and quality in the sector. However, urgent action is still needed to tackle long-standing serious
recruitment and retention challenges, particularly around fair pay, access to training, and employment rights for all care workers.
“The Government's ambition to deliver a Fair Pay Agreement (FPA) for adult social care workers will be the cornerstone of this, but its success hinges on its costs being fully funded.
“We need a financially sustainable care system that is rooted in prevention and personalised care, and one that delivers for both workers and those who draw on care and support, now and for years to come.”
STORM CLOUDS “GATHERING”
Professor Martin Green OBE, Chief Executive of Care England, said: “This report tells the story of a sector that is holding the line, but only just. The international recruits who helped plug the gaps are no longer arriving in the same numbers, and we’re losing too many home-grown staff. With fewer people coming in, more leaving, and the domestic workforce shrinking, pressure is mounting. The storm clouds are already gathering, and unless action is taken now, providers will once again be forced to rely on costly agency cover; and the impending wave of pressure will bring with it greater instability and, ultimately, less consistency for the people we support.”
“These figures show how even small pay rises can tip a sector already on a knife-edge. Providers want to pay their staff fairly, they know how hard they work and how much they give, but they can’t do it without proper support. Every increase brings huge financial strain for services already stretched to their limits. Unless the government sets out a clear plan to meet these rising costs, providers will be pushed into making impossible choices, and the fragile stability we’ve worked so hard to rebuild will start to fall away.”
DEEPER FRAGILITY
Karolina Gerlich, CEO of The Care Workers’ Charity, said “this report confirms what we already know; that social care stands on the dedication of its workforce, yet too many care workers still lack the pay, protections, and recognition they deserve.
Falling vacancies are a positive sign, but they mask deeper fragility. The workforce’s growth continues to rely on international recruitment, while domestic recruitment and retention remain under strain. Migrant care workers make an invaluable contribution and deserve fair treatment, clear routes to settlement, and protection from exploitation. We urgently need investment in training, fair pay, and wellbeing support to build a sustainable future for care.
Every data point in this report represents a person; a care worker balancing compassion with exhaustion. They deserve more than survival; they deserve respect, security, and opportunity.”
To view care sector industry response to today's Skills for Care report, see page 4.

Sector leaders have offered a cautiously optimistic response to today’s publication of Skills for Care’s annual workforce data report, with many welcoming signs of progress whilst warning against complacency in the face of persistent fragility within the care sector.
The report reveals a 2.2% increase in total posts and a fall in vacancy rates to 7% – returning to pre-pandemic levels – yet sector leaders sharing their views with THE CARER have emphasised that such improvements mask deeper vulnerabilities, particularly around the sector’s heavy reliance on international recruitment and a worrying decline in domestic workforce numbers. With international recruitment having halved from 105,000 to 50,000 in the past year, and British nationals in the workforce falling by 30,000, leaders have stressed that whilst the data offers encouragement, the sector remains in a precarious position that demands urgent action on domestic recruitment, training, and sustainable workforce planning if it is to meet the projected need for 470,000 additional posts by 2040.
Vic Rayner, National Care Forum CEO commented:

“Skills for Care’s State of Care report highlights both the progress and persistent challenges facing the social care sector. It is encouraging to see workforce growth, falling vacancy rates, and reduced turnover; all of which deserve celebration. Yet the report also underlines the fragility of our care system; a system still struggling to recruit and retain the sustainable domestic workforce needed to meet the current and future demands of an ageing population.
“Much of the recent improvement has been driven by international recruitment, over this last year with 50,000 new international recruits joined our workforce. However, with tighter immigration restrictions now in place, the sector faces a stark reality: vacancy rates remain three times higher than the wider economy, tens of thousands of British workers leaving the sector each year, and demand only set to rise. Without urgent action to build capacity at home, the progress we see in this report risks being short lived.
“One of the clearest ways forward is to improve pay, terms and conditions for our dedicated workforce. The report shows that experienced care workers earn barely more than new care workers; this is unsustainable.
The government’s Fair Pay Agreement offers a vital opportunity to invest in the workforce, but it must be backed by long term funding, robust infrastructure, and immediate interim measures.
“The government must work with the sector to deliver a sustainable workforce plan, that ensures we have the right people, with the right skills, in place for the future.
The measures contained within the workforce strategy collectively created by a range of social care organisations, including Skills for Care, are a starting point the government can build upon. We need new future-focussed approaches that embrace the role of technology, that pay attention to the changing nature of care and support work, expertise of our care and support workforce and ultimately, what people need and want to live full and independent lives.
The Chancellor’s Autumn Budget provides another opportunity to bring forward the resources to drive this work forward now, rather than waiting until a Fair Pay Agreement is in place.”
Kathryn Marsden OBE, Chief Executive of SCIE, said:
for all care employers, along with a pay structure that rewards increasing skills.
“We know that pay is a principal driver of reducing turnover and improving recruitment. The Fair Pay Agreement, due to be introduced under the Employment Rights Bill, is a welcome step towards recognising care as a skilled profession. That said, the £500 million announced in September to fund the Fair Pay Agreement translates to an estimated average increase of just 20p per hour, according to think tanks. This will not scratch the surface of being able to bring care worker pay in line with equivalent roles in the NHS, nor address the pay disparity in the sector.
“As the Fair Pay Agreement enters into its consultation phase and the Casey Commission begins to build in momentum, the Workforce Strategy for Adult Social Care, led by Skills for Care, should be seen as a guidebook for action. Delivering solutions for our workforce is not something we can continue to stray from; with 470,000 new posts needed by 2040, we need bold, funded solutions that will secure the future sustainability of the sector.
“The workforce is our sector’s beating heart. Every day, those working in care go above and beyond to provide the support that transforms lives, enabling people to live with greater independence, dignity and purpose. Their work sustains families and communities, eases pressure on our other public services and, as this report evidences, contributes £77.8 billion each year to the wider economy—more than the accommodation and food service industry.”
Rory Deighton, acute and community care director at the NHS Confederation, said:

“This report shows the scale of improvements that have been made to boost recruitment and retention across the adult social care sector while also highlighting the challenges that remain. The fragility of the social care sector is one of key issues facing the health and wellbeing of our population.
“Low pay and long hours have led to huge gaps in staffing, with more and more social care providers closing, feeding instability into a struggling system.
“A strong adult social care sector is crucial to solving the challenges facing the NHS and achieving the government’s ambitions – including preventing ill health, moving care closer to people’s homes and getting healthy patients out of hospital more quickly.
“We hope that the government’s forthcoming Casey Review of social care will build upon the progress that has already been made to tackle recruitment and retention challenges, including the government’s recent fair pay agreement.”
Simon Bottery, Senior Fellow at The King’s Fund, said:

at the earliest.
“There are also still glaring issues with pay and working conditions, with care workers with over five years’ experience earning only 7p per hour more than those with under one year of experience. For wages, sick pay and pensions, social care does poorly compared to the NHS. But the Fair Pay Agreement aimed at enhancing pay, terms and conditions in social care won’t be implemented for over three years, supported by only a modest sum of money. Today’s report captures data from before the government increased Employer National Insurance, which is set to add almost £1bn to the care sector’s employer costs in 2025/26. With such tight finances, it’s likely that we’ll start to see a reversal in fortunes on workforce trends in the next years.
“It’s projected that social care will need 470 thousand more workers by 2040, so the Skills for Care findings underscore the need for rapid action and a comprehensive, government-backed workforce strategy that comes alongside wider reform for the sector.”
Director of Policy and Research at the Health Foundation, Hugh Alderwick, said:

‘The Skills for Care report paints a mixed picture for social care. The care workforce is growing and vacancies are falling, but vacancy rates are still around three times higher than in the wider economy and recent progress is fragile. The continuing decline in the number of British workers poses a major challenge given the government’s decision to end international recruitment of care workers.
‘Poor pay and conditions contribute to chronic workforce challenges in the sector and have an impact on people’s care.
Today’s data show fewer care staff are getting the training and qualifications they need, and most of their employers don’t offer enhanced sick pay or pension contributions above the legal minimum. In March 2025, median hourly pay for care workers was 56p above the National Living Wage.
Our analysis finds that 1 in 5 residential care workers live in poverty.
‘The government’s Employment Rights Bill and the planned Fair Pay Agreement for social care offer a vital opportunity to tackle these issues. If backed by investment from government and care providers, these measures could help improve the lives of the 1.5 million people employed in social care and the people they care for.’
Emily Hindle, Head of Policy at Alzheimer’s Society, said:

“This report shows that dementia training levels remain worryingly low for the social care workforce in England.
Around two thirds of social care workers haven’t received any dementia training, meaning people living with dementia are going without the high-quality, personalised care they need and deserve.
“Social care helps people living with dementia who need extra support to live safe, more independent and fulfilling lives. It supports them with daily activities like washing, dressing, and eating, as well as helping them to do activities they enjoy. High-quality, evidence-based dementia training reduces the inappropriate use of antipsychotics and restraints and can even help lower the need for GP or hospital visits.

“Despite some good news about the care workforce in this report, we shouldn’t be complacent. The workforce has grown for the third consecutive year, and average vacancy and turnover rates have continued to fall.
However, a detailed look at the underlying workforce pressures suggests breathing easy would be premature. A relentless focus on improving care workers’ pay, working conditions and career opportunities remains critical to stabilising the social care system.
“One driver of the workforce trends is international recruitment, but we cannot rely on international workers for the long term. As the report describes, the domestic workforce is still shrinking, and routes for international recruitment are being sealed off, reducing the pool of people available to work in the sector. Renewed attention to recruiting a home-grown workforce is urgently needed.
“Of great concern is that workers’ pay has not kept pace with increasing experience. The report highlights that care workers with five or more years of experience are only earning 7p more per hour than new starters. A recognised career path that recognises workers’ experience with better pay is sorely needed.
“Equally as concerning is the decline in workforce qualification levels, which raises questions about the sector’s capability for meeting the people’s social care needs. Increasingly, care workers require skills for delegated health tasks and caring for people with complex conditions. Investing in training and skills development must remain a top priority
‘This report shows that, once again, the reduction in the vacancy rate in adult social care has come about through the recruitment of overseas rather than British staff, highlighting the crucial role they play in the running of adult social care services. Yet, with recent changes to visa rules, the government has effectively turned off the tap for international recruits without implementing sufficient measures to fill the gap with domestic workers.
A promised fair pay agreement, while welcome, will not arrive until 2028 and the £500m budget for it is unlikely to allow the scale of pay increase that appears necessary if vacancies are to be filled.
‘Given the report’s forecast that 200,000 more care workers will be needed by 2030, there is little realistic hope that this demand will be met.
We will need to rethink the wider funding of social care, develop a wider workforce strategy and consider how the workforce can be better deployed to support those who rely on it, particularly as demand will grow as the population ages.
‘Without a stable, well-supported workforce, the pressure on services will only intensify, and the quality and availability of care for people requiring support will be compromised.’
Nuffield Trust Deputy Director of Policy, Natasha Curry said:

“There are some positive signs in today’s findings, with the number of social care jobs continuing to increase and vacancies falling again last year from the 2021/22 peak.
“Although international recruitment declined steeply last year following immigration policy change, it still drove much of the growth in filled social care roles, with 50,000 people joining the workforce from abroad. As even tighter immigration restrictions kick in, the sector’s overreliance on overseas staff is looking increasingly risky, and firm plans to boost the domestic workforce won’t take effect until 2028/29
“Training is not only beneficial for those receiving care, but also for those providing it. Social care workers who receive training are more likely to stay in their roles, with retention improving as training levels increase. High-quality dementia training can also lower burnout, increase job satisfaction, and provide cost savings to the social care sector.
“It will take a society to beat dementia. That’s why we’re calling for a statutory duty to provide dementia training for all social care workers –so that everyone living with dementia receives the best possible care and support.”
Cllr Dr Wendy Taylor, Chair of the LGA’s Health and Wellbeing Committee, said:

“The care workforce plays a fundamental and invaluable role in supporting people who draw on social care to live the independent lives they want to lead.
"Growth in the care workforce is a positive reflection of recent progress in improving capacity, stability and quality in the sector. However, urgent action is still needed to tackle long-standing serious recruitment and retention challenges, particularly around fair pay, access to training, and employment rights for all care workers.
“The Government's ambition to deliver a Fair Pay Agreement (FPA) for adult social care workers will be the cornerstone of this, but its success hinges on its costs being fully funded.
“We need a financially sustainable care system that is rooted in prevention and personalised care, and one that delivers for both workers and those who draw on care and support, now and for years to come.”
Half of people in the UK say dementia is the condition they fear most, according to findings from Alzheimer’s Research UK, with women, over65s, and those with personal experience of the condition particularly likely to share this concern.
The fear is well-founded, given that dementia is currently the leading cause of death in the UK. Women face a particularly elevated risk, accounting for two out of every three dementia diagnoses. Contributing factors include longer life expectancy, social isolation, and emerging research suggesting menopause may play a role in the condition’s development.
Hilary Evans-Newton, Chief Executive of Alzheimer’s Research UK, explained that people fear dementia “because there is still no cure. Dementia continues to rob people of their independence and place an immense strain on families and society.”

She added: “By 2040, 1.4 million people in the UK are expected to be living with dementia, making progress more urgent than ever.”
While most UK adults say they would feel comfortable discussing a dementia diagnosis, with 59% of respondents expressing comfort, stigma remains a considerable obstacle, particularly within minority ethnic communities.
Among Black African, Black Caribbean, and Black British adults, only 46% said they would feel comfortable discussing a diagnosis, with more than a third (35%) saying they would not – compared with 23% of white respondents.
Age also influences attitudes towards diagnosis. Around nine in 10 people aged 35-64 said they would likely seek a formal diagnosis if worried about early-stage Alzheimer’s or another form of dementia. Among
adults 65 and over, this figure falls slightly to eight in 10.
Older adults are also twice as likely to say they wouldn’t seek a diagnosis: only 7% of people aged 35-64 said they probably wouldn’t speak to a doctor, compared with 14% of those aged 65 and over.
To address these barriers, Alzheimer’s Research UK has established its Dementia Community Champions programme, which supports dedicated volunteers who bring conversations about dementia, stigma, and research into their own communities.
Samantha Turner, who leads the programme, said: “There is still a significant amount of fear and stigma surrounding dementia, and for many, it’s something to be kept quiet.”
She explained that the latest findings underpin why the programme is so important: “By building on the trust and relationships that already exist within communities, we can create spaces where people feel supported and confident talking about dementia – and start to dismantle the stigma that has gone unchallenged for too long.”
When asked to identify the most important priorities for dementia research from a list of eight options, the public was clear: finding a cure comes first. Some 43% of respondents chose a cure for dementia as either the most or second-most important area for research, followed closely by finding a way to prevent the condition.
Since the last wave of the research in 2023, there has been landmark progress towards a cure. In 2024, two new treatments – lecanemab and donanemab – were licensed in the UK. While these treatments are not currently available on the NHS, they mark an important milestone in dementia research and may help explain why the public continues to prioritise finding a cure.
Staff and residents at Barchester’s Hazel Lodge care home in Battle, cheered on local farmers when the home provided a welcome stop for the tractor run. The event organised by the team at Rural Past Times, brought so much excitement to everyone as they watched tractors of all shapes, sizes and ages chug down the drive and into the car park.
Hazel Lodge residents, their families and staff enjoyed chatting to the farmers about their tractors and the struggles of British Farmers today, many residents reminiscing about their own farming experiences and memories of owning a ‘little grey Fergie’. Showing their support, the home provided freshly cooked bacon muffins and a well needed hot drink to their visitors, whilst residents were able to take a closer look at the characterful workhorses, some of which were decorated with flow-

ers, whilst others displaying banners, having just returned from a visit to London to highlight their plea.
Home Services Advisor, Sharon Ward said: “As always, we’ve all been looking forward to the tractors arriving and get very excited when we think we hear them! Autumn is such a lovely time of year and important time for the farming community– our residents and the team are all so passionate about supporting our rural community and British Farmers.” Jean, resident at Hazel Lodge said: “I love watching all the tractors arrive, it reminds me of so many years on the farm. I love seeing the tiny vintage ones parked up next to the big modern ones…. it shows how things have changed! It is always sad to see them go but they always give us a little toot and wave when they leave for another year.”

By
The UK’s adult social care sector is wide ranging and supports older adults and people living with disabilities or other long-term health conditions. As the sector faces pressures around staffing, retention, funding and succession planning, two in five care business owners are considering exiting the market, prompting the government to explore alternative models that could diversify and strengthen the sector with incentive schemes and employee ownership trusts (EOTs) gaining traction.
A recent paper by Care England suggests that selling care businesses to employees could offer a sustainable, valuesdriven solution to succession. But what exactly is employee ownership, how does it work, and is it a viable option for adult social care?
WHAT IS AN EOT?

An EOT is a legal structure that enables a business to be owned collectively by its employees. The EOT must hold a majority share in the company and treat all beneficiaries equally. This model allows founders to sell their business in a tax-efficient way, with proceeds paid over time from company profits, and which are free from capital gains tax.
Employees also benefit directly, with the potential to receive annual bonuses of up to £3,600 tax-free. Beyond financial incentives, EOTs foster a sense of shared purpose and long-term commitment.
WHY EMPLOYEE OWNERSHIP WORKS SOCIAL CARE
Despite its essential role, the social care sector is often marked by low wages, limited career progression, and high staff turnover which are factors that undermine continuity of care. With overseas recruitment routes now closed, providers must invest in domestic workforce development to fill the gap.
At the same time, financial pressures, especially stagnant local authority fees and rising workforce costs, are prompting many owners to consider exiting. These twin challenges of retention and succession demand innovative solutions.
Employee ownership offers a compelling response. It promotes long-term thinking, deeper engagement, and a stable workplace culture. Businesses owned by their employees tend to experience higher morale, lower turnover and greater accountability. These qualities translate into better care outcomes and stronger organisational resilience.
REGULATORY ALIGNMENT AND CULTURAL FIT
Employee ownership should be positively received by the Care Quality Commission (CQC), especially

given its established acceptance of ownership changes, provided the registered manager, registered provider, and the registered individual remain unchanged. Under an employee-owned model, accountability among these key figures is likely to be more transparent, empowering those closest to service users to influence strategic decisions. This alignment between frontline insight and leadership can drive meaningful innovation and enhance service quality.
Employee ownership is a natural fit for social care businesses, which are built on values of dignity, compassion and community. By transitioning to employee ownership via an EOT, founders can preserve these principles while securing a future where staff who are most committed to the mission take greater accountability.
Employee owners tend to be more innovative and invested in delivering high-quality care, and EOTs offer a compelling and tax-efficient succession option that keeps the business intact, avoiding the disruption of selling to external buyers or passing it on to reluctant family members.
The EOT model typically relies on the business’s own profits to pay the outgoing owner. In low-margin sectors like care, this can be slow and risky and may lead to a breach of the sale agreement terms if the business does not perform in accordance with the forecasts.
Securing external funding for EOT transitions can be difficult. Those looking to transition to employee ownership may have to accept that it will not be possible to secure funding with the transaction relying on vendor debt paid over time.
As the adult social care sector confronts urgent workforce shortages, succession challenges, and the need to preserve its deeply rooted values, employee ownership via an EOT offers a promising path forward. By placing ownership in the hands of those who deliver care, EOT owned businesses can strengthen accountability, improve service quality, and foster innovation, all while maintaining the cultural integrity of the business. Though funding hurdles remain, particularly in a low-margin environment, the long-term benefits of employee ownership make it a compelling option for founders seeking a values-led exit strategy. In a sector where continuity and compassion are paramount, who owns the business truly matters and who cares, wins.
Elizabeth Finn Homes held its inaugural employee awards ceremony on 11th September at St Hilda’s College, Oxford, recognising staff for their commitment and embodiment of the organisation’s key values.
Elizabeth Finn Homes operates eight residential homes across the South of England and the Midlands, offering residential, respite and end of life care for those in later life.
Each home nominated a quarterly winner, all of whom were then entered into the final awards with winners selected by a panel of sector experts. The three overall winners were chosen based on how their actions, practices, and dedication reflected and upheld the values that define the culture and purpose of Elizabeth Finn Homes. Kim Arthur, a Carer at Merlewood Home in Virgina Water, Surrey, won the first place Gold Award. Kim’s dedication to the home, the residents and their families is hard to match, she makes them her absolute priority. Described by colleagues and residents as inspiring, supportive, and as going above and beyond even when off duty. Lynne Hall, Clinical Training

Coordinator at The Cotswold Home (Oxfordshire), received the Silver award and Paulina Hartshorne, Carer at Rashwood (Worcestershire), received Bronze.
The Home of the Year award was won by The Cotswold Home, rated Outstanding by the CQC. This award recognises a collective team effort in carrying out the EFH values, overcoming challenges, supporting new colleagues, and consistently upholding high standards of care and culture.
“This fabulous event was such a special opportunity to celebrate the dedication, passion and excellence shown by our teams across the country” said Olivia Curno, Chief Executive.
“It was inspiring to see how our winners and finalists put our values into practice every day. Our homes are all about people, and at Elizabeth Finn Homes we’re so lucky to have the most amazing people that create loving homes where people flourish.
Congratulations to all our winners.”
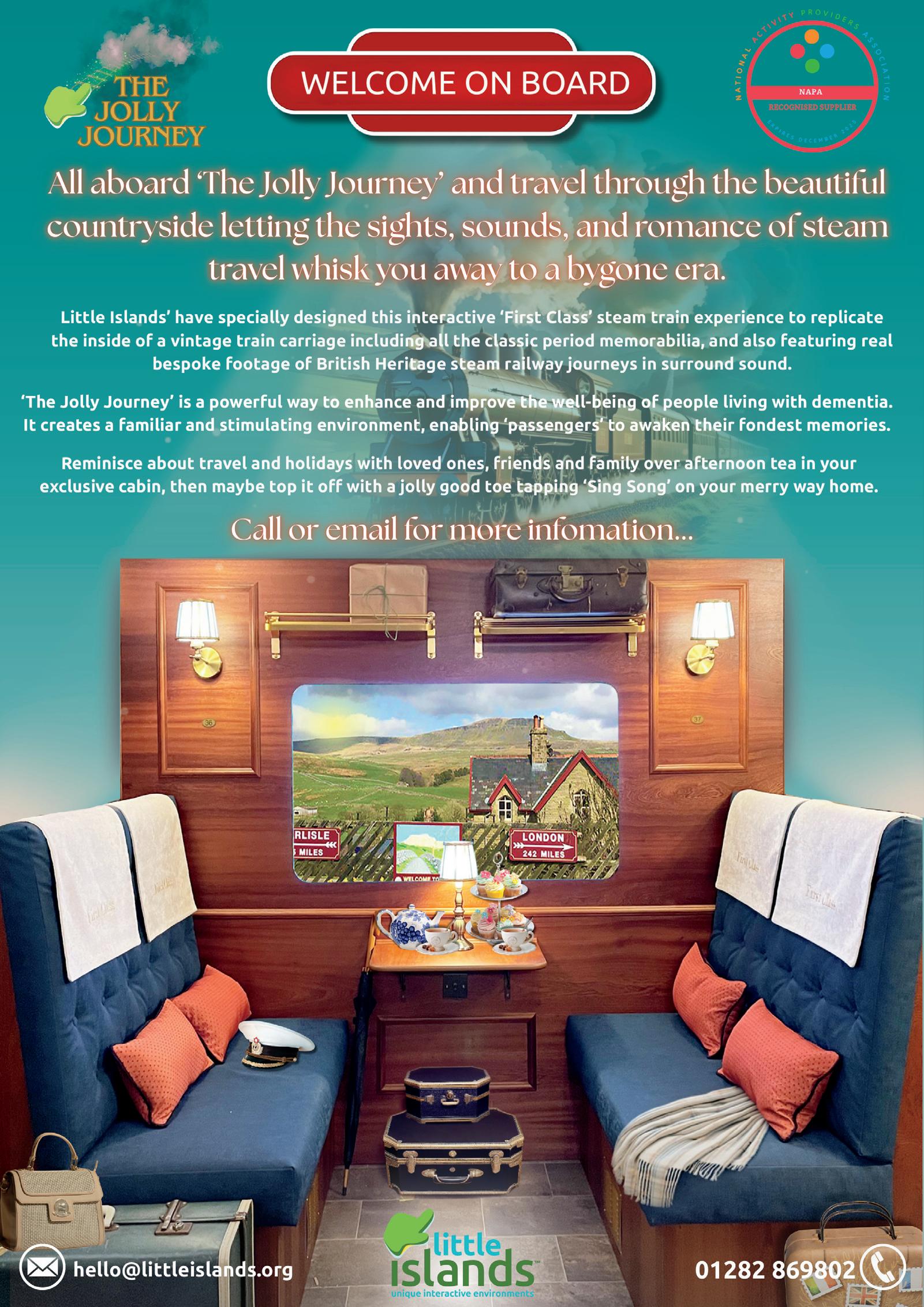
Residents at an Ilkley home can visit places such as Scotland and the North York Moors without leaving their home thanks to a new train experience.
MHA Glen Rosa have installed the Jolly Journey Train Experience, a new initiative by Little Islands, who specialise in creating unique interactive environments.
The train experience showcases journeys across the UK from the viewpoint of a passenger looking out of the window.
The team from Little Islands installed and decorated a part of the home’s dementia unit and converted it into a train carriage with props such as suitcases, train times and journey information displays.
MHA Glen Rosa provides residential and residential dementia care for 47 residents.
Adam Carling, home manager said: “The Jolly Journey Train experience is a new initiative and one that is proving to be very popular here.
“We have received some great feedback since the experience has been installed.

“Our residents love it, you will often see a number of them sat in the carriage and watching a journey.
“The idea came to me from my area who forwarded it to me, and I decided to look into it.
“I then contacted the team at Little Islands and the whole process took a couple of months from start to finish.
“We are quite privileged here at MHA Glen Rosa, where thanks to the generosity of the local community we are able to provide services such as this for our residents.
“We received a very generous donation via our Legacy Fund which enabled us to go for this experience.
“The location of the experience is really good as it’s in a high footfall area, where both residents and their relatives can sit and enjoy it.
“Alongside the Train Experience, we have also prepared a sensory garden thanks to funds we received.
“I do think this is something other MHA homes can look into having, it’s something quite unique and I do feel other homes will see the benefits just
Scotland’s First Minister John Swinney announced that the Scottish Government will directly sponsor visas for overseas care workers in a bold move to counter Westminster’s immigration restrictions.
The SNP leader described his intervention as a necessary “solution” to what he called a staffing crisis, with care homes across Scotland desperately short of workers following the UK Government’s tightened immigration controls.
In the year ending June 2025, the number of Health and Care Worker visas issued to migrant workers in Caring Personal Service Occupations fell by 88%, following restrictions introduced by the UK Government to the visa route.
The subsequent decision by the UK Home Office in July to close the Social Care Visa Route altogether will have a further impact on the social care sector.
According to a Scottish Care survey, more than a quarter of the social care workforce in Scotland is made up by international workers – with many sector leaders citing concerns with workforce shortages and recruitment.

The Scottish Government is continuing to call on the Home Office to reverse its decision to close the route and is investing £500,000 to fund a tailored offer to help ‘displaced’ international social care workers who have found themselves without sponsored employment elsewhere in the UK at no fault of their own.
The funding will be used to help support international social care workers meet the costs associated with
moving to and working in Scotland’s social care sector.
Health Secretary Neil Gray said: “The UK Government’s hostile and restrictive migration policies are damaging Scotland’s health and social care sector.
“In Scotland we need a migration system that works for our NHS, our social care sector, our businesses and third sector. Until we have the full powers over migration that will come with independence, we will do all we can within the devolved powers of the Scottish Parliament to mitigate the UK Government’s harmful approach to migration.
“I am therefore pleased to confirm today that the Scottish Government will create a bespoke offering to help social care workers who have been displaced to come to Scotland and contribute to our care sector.
“We will provide £500,000 to mitigate the devastating impact of the UK Government’s closure of the care worker visa route and provide targeted support to help displaced social care workers.
“This will support international social care workers already in the UK who have lost their social care jobs as a result of their employer losing their visa sponsor licence, to come to Scotland and contribute their valuable skills to our social care sector.
“It is our intention for this work to begin immediately so that social care workers can settle into new jobs before Christmas.”
House Care Home Staff Raise Over £2,000 for Alzheimer’s Society
Staff at Potter House care come in Yeovil have gone to new heights for charity, raising over £2,000 for Alzheimer’s Society through a daring 15,000-foot skydive.
Four members of the Potter House team, including Front of House Manager Jess Stuart, took part in the skydive to show their support for people living with dementia.
Their fundraising will help Alzheimer’s Society continue its vital work, providing care, support, and research for those living with dementia.
Reflecting on the achievement, Jess Stuart said: “We are incredibly proud to have taken part in this challenge and even more grateful for the amazing support we’ve received. Every donation will make a real

difference for people living with dementia, and we want to thank everyone who contributed so generously to this cause.”
Siân Johnson, Regional Fundraiser at Alzheimer’s Society, added, “We are hugely grateful to Potter House Care Home for helping to raise awareness and vital funds for Alzheimer’s Society.
“There are over 101,500 people living with dementia in the Southwest. Alzheimer’s Society provides vital support to people living with dementia, funds groundbreaking research and campaigns to make dementia a priority. We simply can’t reach everyone without the continued support of our incredible fundraisers.”

By Sharif Ahmed, owner of Jothno Care & Support

South Asian elders are underrepresented in London’s adult social care when compared to local demographics. This matters because it has an impact on their wellbeing, their independence and their health outcomes. Recent research has highlighted the need for service improvement in diverse boroughs like Barking & Dagenham.
RESEARCH ON SOCIAL CARE IN LONDON FOR SOUTH ASIANS
Healthwatch in Barking & Dagenham undertook in-person surveys, ran focus groups and engaged with elders at community venues and places of worship. Their target was the South Asian population in Barking & Dagenham including Indian, Pakistani, Bangladeshi, and other Asian / Asian British populations.
LANGUAGE AND COMMUNICATION
They found that there was a language mismatch between clients and providers. This had an impact on understanding, service uptake and informed decision making.
83% of those surveyed thought that their social worker either did not understand the challenges that those from South Asia face or only partly understood it. 48% said they would approach their GP for guidance, but even then “The GP doesn't understand your problem and doesn't really take your problem seriously as some people might not be able to speak fluent English as they are not British born and come from another country and find it difficult to explain their problems and therefore don't get treated that easily.” 22% would seek help from the local council and 22% would turn to family and friends.
CULTURAL STIGMA AND FAMILY EXPECTATIONS
A study at Brunel University in London found that families in some South Asian communities felt that social care was a “public admission” of their failure to uphold family values. They carried a stigma about care homes, mental health and ‘outsider’ intervention.
These concerns can influence family opinions and decision making, preventing the family from seeking help when it is needed. They found that social care was seen as a last resort.
“People were very worried that if they were seen to have social care professionals entering their home or to receive services such as meals on wheels they would be seen by the wider community as being bad parents or having children who were unwilling to care for them.”
The approach the report recommended to professional carers was to suggest support is supplementary to the family, rather than replacement for family care. Respite care can offer this type of supplementary support.
The inconsistent recognition of dietary (halal, vegetarian) and religious (prayer, gender of carers) needs was widespread. There was a perceived lack of awareness by some professionals and a need for more staff from similar backgrounds. Survey participants said “We need to have professionals from that background.”
Navigational challenges and trust issues
Survey participants had difficulty finding the right information to direct them to the service they required. This was especially relevant when they were outside familiar environments e.g. their local GP or local health clinic and seeking specialist care.
The older generation wanted to be seen face-to-face and not have phone appointments. They accepted that they were more likely to need social care services but they were not able to access information online as low users of the internet. They trusted familiar settings like community centres and places of worship and suggested that healthcare professionals came to give talks there.
The survey highlighted positive and negative experiences of health care.
The positive feedback talked about tailored support and how the service user felt empowered in their decision making. “I get care 3 times a day, I don`t have any next of kin, I am getting help managing finances and going to hospital appointments. I had a stroke following which I was provided with an adapted home.”
The negative experiences talked about delays, miscommunication, lack of continuity or unmet needs. “My experience with social care services for her was a nightmare. The carers that came to look after her did not have any experience. On some days they would just not turn up at all.”
Participants who received care from professionals in the Muslim community felt comfortable and wanted it to continue. Many participants want more bilingual and bicultural staff and more outreach in community languages, and a regular presence in community spaces.
There was an emphasis on culturally sensitive service design and carer recruitment from a diverse cultural background.
The findings from the report suggest that there is a greater need for culturally diverse provision in Barking & Dagenham and it would suggest, across London. The South Asian community is underrepresented and that impacts on families who need to access information and make decisions about care for their families.
Enfield care home residents have jazzed things up a bit thanks to a gift from the famous Ronnie Scott’s club.
Residents at Brookwater House Care Home, Oakthorpe Road, are thrilled they can now strike up a chord thanks to the Yamaha piano.
The generous gift is now filling the home full of music, proving a tonic to players and listeners alike.
Resident Gizzy Williams, aged 76, said: “It’s wonderful to sit down at the keyboard again and enjoy playing.
“I used to play piano at home.”
Fellow resident May Doyle, aged 93, lives with dementia and started playing the piano at primary school. May later played at her local church so the chance to
tinkle the ivories again is very welcome.
Brookwater House Customer Relations Manager Amba Shaw said everyone is delighted with the gift, which is now in the Bistro, the social hub of the home.
She said: “It’s wonderful to have music in our lives. It can offer so many benefits for our mental and physical well-being.
“Also, playing an instrument can be physically demanding, so it’s good for promoting movement, too, as well as bringing people together.
“We love having the piano and we would like to say a huge thank you to Ronnie Scott’s for this incredible gift.
“Listening to May and Gizzy play has certainly made everyone smile here at Brookwater House.”

for their commitment and embodiment of the organisation’s key values.
Elizabeth Finn Homes operates eight residential homes across the South of England and the Midlands, offering residential, respite and end of life care for those in later life.
Each home nominated a quarterly winner, all of whom were then entered into the final awards with winners selected by a panel of sector experts. The three overall winners were chosen based on how their actions, practices, and dedication reflected and upheld the values that define the culture and purpose of Elizabeth Finn Homes.
Kim Arthur, a Carer at Merlewood Home in Virgina Water, Surrey, won the first place Gold Award. Kim’s dedication to the home, the residents and their families is hard to match, she makes them her absolute priority. Described by colleagues and residents as inspiring, supportive, and as going above and

beyond even when off duty. Lynne Hall, Clinical Training Coordinator at The Cotswold Home (Oxfordshire), received the Silver award and Paulina Hartshorne, Carer at Rashwood (Worcestershire), received Bronze.
The Home of the Year award was won by The Cotswold Home, rated Outstanding by the CQC. This award recognises a collective team effort in carrying out the EFH values, overcoming challenges, supporting new colleagues, and consistently upholding high standards of care and culture.
“This fabulous event was such a special opportunity to celebrate the dedication, passion and excellence shown by our teams across the country” said Olivia Curno, Chief Executive. “It was inspiring to see how our winners and finalists put our values into practice every day. Our homes are all about people, and at Elizabeth Finn Homes we’re so lucky to have the most amazing people that create loving homes where people flourish. Congratulations to all our winners.”
Splitting county councils into multiple small unitary councils could hit millions of vulnerable people with a triple whammy of worse services, higher costs for care, and not enough staff to deliver support, a new report warns.
The County Councils Network (CCN), which commissioned the research, say the report’s findings are a stark warning for the government if it does not stick to its original plans of creating councils with populations over half a million, with the first wave of councils submitting competing proposals to ministers two weeks ago.
The network argues that these plans to overhaul local government structures will ‘make or break’ care services depending on which proposals ministers decide to implement. But a survey contained in the report reveals that the most senior care professionals in England, have little to no confidence that the risks of breaking up vital care services into smaller councils will be fully considered by ministers.
Last year’s English Devolution White Paper outlined plans for a radical overhaul of council structures, with government committing to end ‘two-tier’ local government: replacing 185 county and district councils with new unitary authorities in 21 areas.
Official government guidance had set out that new unitary councils should have a population of 500,000 or more and ‘avoid’ the fragmentation of vital care services. However, this guidance outlined that there may be ‘flexibility’ on this number in certain scenarios. District councils across the country are proposing to break up county councils who deliver social care into new unitary councils with populations of 300,000 or lower. Each of these new authorities will deliver care services, rather than one single upper tier council as is the case today.
The report by Newton concludes that the government’s forthcoming decisions about the size of new unitary councils will have ‘profound, long-lasting impacts on the most vulnerable members of society’. It argues that the evidence strongly suggests larger-scale councils are ‘essential’ to preserve service quality, prevent rising costs, and ensure financial sustainability of people-based services.
Previous research for the network by PwC has shown that splitting county councils into multiple authorities as small as 300,000 could result in hundreds of millions extra costs every single year for local taxpayers.
And now current research, which draws on local data from half a million residents across 146 possible new unitary footprints, lays bare a further triple whammy of risks for care services and special educational needs:
New unitary councils with populations substantially below 500,000 people will increase the price councils pay for care, putting further financial costs on these under-pressure services. Modelling suggests that if all new unitary councils had a population below this figure, this would result in additional unit costs of between £180m and £270m
annually solely as a result of reductions in purchasing power. In contrast, if all new unitary councils had a population above 500,000, it would reduce care fees by £65m a year across England.
Splitting county councils into smaller local authorities will require hundreds of new senior roles as councils already grapple with a shortfall in care staff. Modelling shows that if all new unitary councils had a population of below 500,000, this would result in a requirement of between 500 – 1,100 additional management and senior roles in care services – which the CCN warns will be impossible to fill. In contrast, if all new unitary councils had a population of above 500,000, fewer senior managers than are currently in place will be required, saving those areas money to reinvest in care services.
Breaking up ‘high-performing’ county councils into substantially smaller councils could lead to worse services. The report reveals that larger authorities are more likely to receive ‘Outstanding’ or ‘Good’ ratings from Ofsted for children’s care services and currently 16 of the 21 county councils are already Good or Outstanding for these services. Consequently, directors of care and special needs services warn in the report that smaller services could struggle to attract staff and invest in improving services.
Splitting county councils into smaller unitaries covering populations as small as 300,000 or lower could see some of these new authorities overwhelmed with demand. The report finds that the smaller the council, the more they could experience extreme concentrations of care users: effectively meaning care costs are highly variable between new authorities and may exceed planned budgets. This could leave some councils exposed to unaffordable costs and the use of expensive out of area placements. This could challenge their financial sustainability from inception.
The CCN says that instead of running the risk of worsening services, government should grasp the nettle and ensure that the reforms are a catalyst to transform the way in which vulnerable people are supported with local authority care. However, they say this research shows this can only be achieved by ensuring the government stick to their own statutory criteria and ‘rigorously evaluate’ all proposals against it.
A survey carried out for the research reveals that whilst senior care professionals are cautiously optimistic about the potential benefits of reorganisation – if delivered in the right way – there are widespread concerns that the risks to care services will not be adequately considered by ministers when they make their decisions on competing proposals. Less than one in 10 (6%) of county council chief executives and directors of adult social care and children’s services are confident they will be fully recognised.
The report recommends that the government avoid, where possible, splitting up people-based services. Where this cannot be avoided, the government must ensure that all new authorities are above their stated
criteria of 500,000 or more.
The study also recommends that given the level of competing proposals, and the risks highlighted by the report, minister should give a heavy weighting towards the impact on splitting up these care services when they decide on proposals and should even consider appointing an independent body to evaluate the proposals.
Cllr Matthew Hicks, Chair of the County Councils Network said: “Local government reorganisation has the potential to deliver significant benefits for local taxpayers and improve every day services residents rely on. However, it also carries with it significant risks if it’s not delivered in the right way. This report should focus minds on the impact that these proposals will have on the lives of the most vulnerable people who depend on local authority care and support day in, day out.
“With several areas now submitting competing proposals, the study clearly shows the stark choice facing the government. It provides clear evidence that there are very real risks to care services if county councils are split into multiple small unitary councils. Those that depend on care could face worse services, be met with significant upheaval, and have too few staff to adequately deliver their support. At the same time, councils and local taxpayers could be loaded with substantive extra costs.
“Put simply, reorganisation plans could make or break care services unless the government gets these reforms right.
“It is therefore vital that the government sticks to the criteria it set out earlier this year whereby new councils cover populations of over 500,000 people. Considering these are the most important and expensive local authority services, ministers must ensure they rigorously evaluate all proposals and heavily weight their decisions based on the risks to people-based services.”
President of the Association of Directors of Adult Social Services (ADASS), Jess McGregor said:
“This report reinforces concerns we raised with Ministers in August about the risks local government reorganisation poses to hundreds of thousands of people who are older-aged, disabled or in vulnerable situations that draw on care and support. The findings highlight important issues government must address: developing a pipeline of Directors of Adult Social Services, a plan to address disproportionate impacts of ordinary residence decisions, and ensuring adult social care can contribute to the shift from hospital to community care.
“New councils must be financially sustainable from day one and able to meet their legal duties to provide care and support. It’s vital that Ministers engage adult social care leaders in this process by inviting them to sit on Joint Committees and help assess all proposals. ADASS will continue to work with Ministers and civil servants as so many of the people our members serve rely on us getting this right.”

By Catia Pereira, Home Manager of Aria Care’s Huntercombe Hall in Henley-on-Thames
(www.ariacare.co.uk)

Leadership in the care sector is both uniquely challenging and deeply rewarding. It requires leaders to balance operational pressures with the wellbeing of vulnerable individuals and the teams who support them. A recent reflection on the journey of Catia, Home Manager at Aria Care’s Huntercombe Hall, provides her insight into the realities of care leadership and what makes it effective.
Catia’s journey into leadership began with a nursing career spanning more than 15 years. Having trained in Portugal and later moving to the UK, she developed her passion for caring for the elderly through years of clinical and managerial roles. Her path, from dementia unit manager, to clinical manager, to deputy, and now home manager, has been driven by purpose and a genuine commitment to the people she serves.
Today, she leads a home with 54 staff members and 41 residents, where every decision she makes has a direct impact on the safety, happiness, and quality of life of those in her care. For her, this responsibility is not simply a job, but a calling saying,
“The wellbeing of residents is always at the heart of what I do, and I am committed to being involved in every aspect of care.”
SHAPED BY PERSONAL EXPERIENCE
Catia’s passion for care is deeply rooted in her own experience of ill health as a teenager. Born with a rare knee condition, she spent several years in and out of hospital, including long periods confined to a wheelchair. During this time, she experienced first-hand what it felt like to be treated as a case study rather than as a person. Doctors often spoke about her but not to her, leaving her feeling invisible and unheard. By contrast, it was the nurses who made her feel seen. They stayed by her side, offered encouragement, and gave her the sense of being valued as a person rather than just a patient. This contrast left a lasting impression. Catia says, “I really felt not listened to. There was no empathy. Everyone was asking how I was, but never asking me directly. The nurses were always there, and that’s when I developed my passion for nursing.”
These experiences have shaped her leadership today. Her empathy for residents and her insistence that staff communicate openly and respectfully stem from her determination that no one in her care should ever feel invisible or diminished.
BUILDING TEAMS AND CELEBRATING DIVERSITY
Among her biggest challenges as a leader has been managing a multicultural team. While this diversity can be a strength, it also brings the risk of misunderstanding if not carefully nurtured. Catia has responded with creativity and empathy. She has introduced regular cultural days, team activities, and events where
both staff and residents can join together, sharing food and stories from the cultures that have shaped them and helped make them who they are.
“Culture plays a huge part in the way we do things, how we communicate, it is subtle but powerful. Fostering understanding is essential. When staff are happy at work and feel valued, everything else improves. These shared activities foster a team spirit; a sense of belonging. We embody one team, one vision. A recent success has been a team-building programme, where over four weeks we explored what it means to be a high-performing team.”
Catia’s leadership philosophy is clear, “Good leadership, to me, means truly knowing your team, understanding their skills, strengths, and potential, so that we can work together effectively. It’s about creating a positive environment, being present, and inspiring others to perform at their very best.” She believes the best leaders are visible and approachable, and she works alongside her team. “By adopting a hands-on approach I feel it has earned me greater respect and trust, as the team sees that I am willing to put on a uniform, share in the work, and show up fully for both the challenges and the successes.”
As a manager, she takes pride in strong organisation and planning, ensuring tasks are completed efficiently. As a leader, she seeks to inspire and innovate, driving progress while keeping the team engaged. She has even implemented thoughtful activities such as offering head and shoulder massages, organising social activities such as BBQs, and these gestures have gone a long way in reducing turnover and strengthening bonds among staff. She is 10 months into her leadership role at Huntercombe Hall which has already seen an increase in occupancy and a reduction in the need for Agency staff.
Effective communication, Catia emphasises, is the foundation of strong leadership. She ensures policies and practices are communicated clearly through both formal meetings and informal briefings. She has created visible mechanisms for feedback, such as her “You said, I did” board, which demonstrates how staff input leads to action. These practices not only build trust but also encourage accountability and shared ownership.
In her words: “Leadership is about guiding, supporting, and leading by example.”
Catia starts each day by spending time on the floor with staff and residents. This visibility is not about micromanaging but about being present to understand the daily realities, offering support, and ensuring that residents’ care remains central. At the same time, she believes in empowerment, trusting her staff to take responsibility for their roles while supporting their continuous development through training and education. She also recognises that strong leadership requires balance. For Catia, family plays a vital role in sustaining her energy and resilience. “My fiancé is my anchor, and when I’m home, I take that time to reconnect and restore my energy so I can give my best to my team the next day.” With her wedding on the horizon, she acknowledges that personal milestones can help leaders stay grounded, motivated, and connected to life beyond work.
“My passion for supporting the elderly is limitless, and I see it as a true honour to care for a generation that has given us so much. I want to make sure our residents live in an environment where they enjoy their community, feel safe and happy in their surroundings, and maintain good health, while also feeling valued, respected, and truly at home.”
A staff member at a Toton home bought some special sentimental items to discuss and share her heritage as part of Black History Month.
Black History Month, is an annual observance, held in the month of October of African American history and Black history in the U.S. and other countries.
Selina O’Loughlin works as a care assistant at MHA The Herons and has English, Irish and Jamaican heritage.
She is very proud of her roots and brought in with her a Jamaican flag, a handmade doll which she got from Jamaica over 30 years ago and also a Jamaican top, which her uncle, who visits Jamaica every year bought for her.
The residents at the home were very intrigued by Selina’s heritage and asked Selina plenty of questions on what the items meant to her as well as talking about the different foods and culture.
MHA The Herons provides residential care for 39 residents.
Speaking about the session Selina said: “The idea came about after I was having a conversation with Mandy, the activities coordinator at the home.

“We spoke about Black History Month, she knew about my Jamaican heritage, and we thought it would be a good idea for me to do a session like this.
“Here at MHA The Herons, we are always keen for residents and staff members to share their experiences, and we are quite lucky to have a very diverse workforce.
“Celebrating or observing Black History Month is very important to me, and I feel very proud of my heritage and who I am.
“The residents were very intrigued with what I had bought in and were very keen to know about the types of food we eat in Jamaica, and they absolutely loved the doll.
“I felt very proud to answer any questions the residents had, and it was nice to educate people.
“I really enjoyed it, and as mentioned before having such a diverse workforce is great and gives us all a lot of comfort to be ourselves.”

The Gold Standards Framework (GSF) Charity equips your team with the skills, confidence, and compassion to deliver person-centred care that truly makes a difference. For a limited time, the GSF Care Homes Training & Accreditation Programme is available at 50% OFF – now only £1,095 + VAT This affordable, high-impact training is designed for your whole organisation (for training in April 2026 - places limited). GSF Accreditation is CQC-recognised, endorsed by leading care organisations, and more than 97% of accredited teams report better experiences for people and their families. For more information, visit: www.goldstandardsframework.org.uk / 020 7789 3740 Future-proof your care. Empower your workforce. See the advert on page 7 for more information.

A major UK study of more than 165,000 dementia patients has found that Risperidone raises stroke risk without exception, challenging safety assumptions by leaving no ‘safe group’.
The powerful anti-psychotic is commonly used to treat dementia patients experiencing severe agitation, especially in care homes where other strategies have failed.
But stroke risk among dementia patients taking Risperidone rose even in people with no history of heart disease or stroke. This counters assumptions about safety and raises questions about how the drug, the only licensed drug of this type for use in dementia, is used and monitored.
The findings, out today in the British Journal of Psychiatry, will likely prompt calls for changes in clinical practice.
Most striking was how consistent the risk was across all groups.“We knew Risperidone causes stroke, but we didn’t know whether some groups of people might be more at risk than others. We thought if we might identify characteristics that make people more at risk, doctors could avoid prescribing to patients with those characteristics,” said Dr Byron Creese from the College of Health, Medicine and Life Sciences at Brunel University of London.
Fifty per cent of people with dementia experience agitation, often causing severe distress. When nondrug treatments don’t work, doctors may turn to Risperidone as a last resort. The findings sharpen the already difficult choices facing doctors and families, who must weigh the serious stroke risks of Risperidone against its potential to relieve extreme distress.
The drug, used to calm aggression, carries known risks of stroke in older patients. Yet there is still no dementia-specific guidance on how doctors should monitor those dangers. NHS guidelines limit Risperidone use to six weeks for severe symptoms, but many patients take it for longer, with monitoring standards varying across the country.
There are no UK licenced alternatives for Risperidone in such cases, says Dr Creese, so it is about making sure the risks are clearly explained and carefully weighed up. People with a history of stroke already face a high risk of another stroke. If a stroke happens after taking Risperidone, it may not be just because of the drug. Doctors only use Risperidone as a last resort. “These findings give clearer information about who is most at risk, which helps everyone make more informed choices. Every decision should be based on what is right for each person, through honest conversations between doctors, patients, and families.”
The team analysed anonymised NHS records between 2004 and 2023, comparing patients prescribed Risperidone with matched controls who were not. In people with a history of stroke, the annual rate per 1000 people jumped to 22.2 per cent on Risperidone, compared with 17.7 per cent in those not taking it. In patients who’d not had a stroke, the rates were lower but still significant—2.9 per cent versus 2.2 per cent.
And the risk was higher in patients taking the drug over the short term (12 weeks).
“We hope that these data can be used in updated guidance that is more person centred and based on particular patient characteristics,” said Dr Creese.
Clarendon Hall Care Home in Grimsby, North East Lincolnshire, part of HC-One, hosted a heartwarming coffee afternoon in support of the Alzheimer’s Society, bringing together residents, relatives, and the local community for a special fundraising event.
The afternoon was filled with joy, laughter, and entertainment, with live performances from talented singer George and the Clarendon Hall choir, who helped set a lively and celebratory atmosphere. Guests were also treated to a wonderful selection of homemade cakes, alongside fundraising activities including a raffle and a name card for a luxury hamper.
Thanks to the generosity of all who attended and donated, the event raised an impressive total of over £1,000 for the Alzheimer’s Society. The charity works tirelessly to support those living with dementia and their fami-

lies, making this achievement particularly meaningful to everyone at Clarendon Hall.
One of the residents shared: “It was such a lovely afternoon – the singing, the cakes, and being surrounded by family and friends made it so special.”
Hayley Sandison, Senior Wellbeing Coordinator at HC-One’s Clarendon Hall Care Home said:
“We are so proud of our residents, relatives, and colleagues who came together to support such an important cause. The Alzheimer’s Society is close to many of our hearts, and raising over £1,000 is a fantastic achievement that will make a real difference.”
The event was a wonderful celebration of community spirit and kindness and will be fondly remembered by all who attended.


Compassion forms the backbone of the care industry, but what does this look like in practice?
Here, Bethan Evans, CEO of My Choice Healthcare (www.mychoicehealthcare.co.uk), discusses how care home staff can tend to the needs of both residents and their families with compassion, how to handle the challenges of care home life sensitively, and why empathy is essential for both physical and mental wellbeing.
1. How does compassionate care enhance residents’ wellbeing, both physically and emotionally?
“Compassion helps people connect. The warmth, openness and kindness shown through compassionate care help residents feel supported, and this is a powerful foundation for wellbeing.
“Those who feel supported are more likely to feel settled in their surroundings and are better able to build fulfilling relationships – these feelings of belonging and support are cornerstones of wellbeing. If residents aren’t treated with compassion, they can be left feeling isolated, misunderstood, fearful or neglected, and this is a risk we simply can’t take.
“In terms of physical wellbeing, studies have shown that compassionate relationships influence heart rate and breathing, as well as brain health and function. Compassionate care has also been linked to faster recovery times and the prevention of health issues.
“Treating residents with care and empathy is all about being sensitive to their unique needs, handling any worries with respect, and going above and beyond to ensure they feel supported.”
2. Care home staff are busier than ever as the system struggles to cope with demand. How do you ensure residents are treated with the compassion and time they deserve under such testing conditions?
“Compassionate care is a cultural approach rooted in a home’s values and, as such, doesn’t take any longer to deliver.
“A compassionate approach should be present in every element of operations and depends on having the right culture. It’s about the way we do things, rather than what we do.
“If residents aren’t treated with compassion, they are more likely to become distressed or fearful, and their behaviour will reflect this. It’s in these instances that staff are more likely to feel under increased pressure, rather than the other way round.
“Treating residents with compassion and care isn’t time-consuming or a burden. It’s a natural human instinct and is the kind of support everyone deserves.”
3. Do you have any examples of where compassionate care has made a real difference to the day-to-day life of a resident?
“A manager at one of our homes introduced a ‘wish tree’ for residents to request their one big wish –something they would really like to do or achieve.
“We’ve seen countless examples of residents experiencing wonderful outcomes through this initiative, including one resident with dementia who was able to attend a football match with his best friend.
“A compassionate approach to granting these wishes means residents are supported to achieve their aspirations, rather than being told something is too difficult or off limits. This has undoubtedly had an impact on their overall quality of life and wellbeing, ensuring they’re treated with dignity and respect.”
4. What are some of the biggest challenges you see for those in residential care, and how do you handle these with compassion?
“Feelings of loneliness and isolation can be quite common. It’s a big change to move away from family and friends into a new setting, and it’s inevitable that some residents will find this challenging.
“We adopt a compassionate approach to help alleviate these feelings, particularly when it comes to communication. Taking the time to get to know our residents, including their likes and dislikes, their personalities, and their backgrounds, can help reduce these feelings of loneliness.
“Loss of independence or dignity is another challenge many residents come up against as any age-related conditions develop, and this can impact their confidence.
“Taking a compassionate approach here means continuing to see and celebrate the person behind the condition. As people age, their health or ability can become their defining feature, but we want to change this. It’s about seeing each person for who they are as a whole.”
5. Adapting to residential care can be tough for families of residents too. How do you ensure their needs and worries are treated with empathy?
“It’s a real adjustment for families when a relative moves into residential care. Open and consistent communication is crucial to providing the support they need, and every step of the process needs to be explained thoroughly.
“Prior to move-in we must have a solid understanding of the family’s expectations, and they need to be involved in all discussions around the care and life of their relative. An honest and transparent approach is best and helps families feel included.
“We also have an open-door policy which helps families feel welcome and reassures them that they can talk to staff whenever they need. It’s understandable that families may have worries, but handling any concerns with compassion can help alleviate some of this stress.”
6. What do you think is the most important action care providers can take to develop a culture of empathy in residential care, and why does this matter?
“Culture and tone start at the top and need to be set by the leadership team – managers who lead by example will ensure the wider team adopt the same approach. Creating an open, honest, warm and responsive environment is down to the whole team and benefits everyone.
“This is important because we’re supporting people who are often at their most vulnerable. Human kindness goes a long way in reassuring residents and helping them see that they matter. We place them at the heart of all that we do, and this is non-negotiable.”

Supporting residents to get out and about and feel part of the community is a key focus for staff at St Cecilia care
A recent trip saw them on a day trip to Wells Cathedral to feed the famous swans, with a picnic in the grounds of the Bishops Palace, and tea and cakes at the city’s Conservative Club.
“Getting out into the world gives residents a real boost,” said Tracy Woofrey, manager of the 17-bed specialist dementia care home run by White Care Group.
“There was a real sense of excitement. Trips out bring so much joy and anticipation for our residents and helps connect them to the wider community.”
For many, the highlight of the day was making the six-mile trip on board First Bus’s 174 Bath to Wells service.
“It might sound a small thing, but going by bus was a real highlight for everyone. They loved watching the world go by out the window and pointing out places they know.”
Tracy also has praise for the First Bus drivers who brought them there and back.
“The drivers were absolutely marvellous and so kind and courteous. They helped make the journey stress-free and are a credit to their company.”

In April 2025, the Supporting the Provider Market (STPM) team in County Durham published a new report evaluating the use of pobroll® — a waterproof bed-bathing wrap designed to improve dignity, comfort, and ease during personal care. This evaluation was carried out across 10 care homes with high numbers of residents living with dementia. Each setting was given one or more pobroll® units and invited to share feedback through a structured survey. The findings reveal how even simple tools can make a significant difference in everyday care.
How was pobroll® used?
Most care homes used pobroll® daily or several times per week, showing it quickly became part of regular practice. Staff noted that one of the biggest challenges was not having enough units — all homes requested additional stock after the trial, highlighting a clear appetite for wider adoption. What did care teams think?
Feedback from the care homes showed strong support for the tool:

Ease of use was rated highly, with an average score of 4.4 out of 5. Staff found pobroll® straightforward to incorporate into care routines.
Training was rated slightly lower, at 3.8 out of 5, suggesting that while the wrap is easy to use, additional training resources could improve onboarding for new users.
Resident response was positive. Three in ten care homes reported improved mood or behaviour during bed
Written by Pat O’Brien of pobroll
bathing for dementia patients.
• Key benefits included greater warmth, coverage, and dignity for residents, especially those who might find conventional methods distressing. Some teams also found it particularly useful for end-of-life care
Would they recommend pobroll® for bed bathing for dementia patients?
Absolutely. Homes rated their likelihood to recommend pobroll® at 4.3 out of 5, with half of respondents giving it a full 5 out of 5. The overall feedback was clear: this is a valued, meaningful addition to personal care.
Would they recommend pobroll® for bed bathing for dementia patients?
The results of this trial reinforce what many professionals already believe — that small, thoughtful design changes can significantly improve care. For residents who are bedbound or living with dementia, personal care can often be a distressing experience. But with the right tools, it doesn’t have to be.
The pobroll® isn’t a complex device. It’s a simple, dual-layered cotton towelling wrap. But its thoughtful design — offering full coverage, comfort, and support — makes a real difference where it matters most.
If you’re part of a care home, hospice, or hospital and would like to explore how pobroll® could benefit your residents or service users, get in touch. We’re here to support compassionate, dignified care — one small change at a time.
See the advert on the facing page for details, or visit www.pobroll.co.uk
Millions of carers are locked out of paid work according to a new report, which results in their households lose vital income, and the government loses tax income.
Across all working age carers, this is worth up to £47.7bn a year –equivalent to 1.7% of the UK’s entire GDP – which would further boost economic growth, contributing an additional £20.4bn in Gross Value Added across the economy from carers having a higher income to spend, a major new study has found.
Just getting those unpaid carers closest to the job market back into employment could boost the UK economy and household incomes by up to £16.9bn a year, leading to a further £7.2bn increase in GVA across the rest of the economy.

‘The hidden cost of unpaid care: The economic price of locking carers out of work’ research was commissioned by national charity, Carers Trust, and funded by savings and retirement business Phoenix Group as part of its ‘Caring for Carers’ initiative. It shows the UK could reap huge financial benefits by giving carers more support to enter, and remain in, employment.
Of the nearly six million carers in the UK, almost half (2.7 million) are not in paid employment, researchers found. Of those, 524,000 are currently unemployed but could work with the right support.
If all of these 524,000 carers were able to get full-time work, their household income would rise by up to £10.1bn. This would also result in up to £2.8bn in reduced welfare payments and as much as £4bn in increased Income Tax and National Insurance contributions – a total gain of £16.9bn for the economy and carer household incomes.
Increased household income from unpaid carers being supported to work could also support household
consumption and further economic growth in the wider economy. That includes up to £7.2bn in Gross Value Added to the economy and as much as £494m in increased VAT revenue.
For young carers, in particular, there is an economic cost of up to £1.1bn due to being out of the workforce. Their employment prospects are often blighted by the disruption caring causes to their education opportunities.
The State must, the report says, invest in specialist employment support for carers. Carers need support from initiatives that understand the challenges and barriers they face.
Supporting more carers into paid work would play a vital part in achieving Government ambitions. This vital support would get more people into employment, reduce poverty rates among carers, and help reduce spend on welfare.
Previous Carers Trust research has shown around two-thirds of carers have had to cut back on working hours or give up employment completely because of the difficulty of balancing care with a career.
Carers Trust’s CEO, Kirsty McHugh, said: “Up and down the country, millions of carers have been forced to give up paid work because of the overwhelming pressures of their caring role and the huge gaps in UK social care provision. This vital research shows for the first time the huge financial benefits of helping them back into paid work. The proceeds of that growth could be put towards finally fixing the creaking social care system which forces so many people into unpaid care in the first place.
“Employers can also play a huge part by offering flexible, carer-friendly working practices. Carers have so many skills to offer. It’s time they were given the opportunity to put them into action so everyone can benefit.”
Hartford Care has appointed Vishul Seewoolall as Chief Operating Officer, a newlycreated role that supports the care home group’s continuing growth strategy.
With over 20 years’ experience in the care industry, Vishul joins Hartford Care from Signature Senior Lifestyle, where he was the Chief Operating Officer and held various director roles throughout his seven years with the company. He previously worked for Bupa as Regional Director of Operations. Vishul will work alongside Chief Financial Officer, Amanda Smith, with a particular focus on Hartford Care’s newly built homes in Aldershot, Alton, Southampton and Swindon.
Vishul Seewoolall, Hartford Care’s new Chief Operating Officer, comments: “It’s a very exciting time to join the team at Hartford Care. Even as the company continues


to expand at pace, increasing its capabilities and service offering in new locations, it hasn’t lost sight of its commitment to a ‘home from home’ ethos and to building lasting partnerships across its communities. I look forward to being a part of Hartford’s ongoing evolution.”
Kevin Shaw, Chief Executive of Hartford Care, comments: “It’s a pleasure to have Vishul on board. With our most recent acquisition of five homes from The Graham Care Group in Kent, we’ve increased our geographical reach and now have 29 homes across the south of England and Isle of Wight, with over 1,800 bedrooms. Vishul is exceptionally well placed to help us deliver our ongoing, ambitious growth strategy, enabling us to offer high-quality, expert care to existing and future residents.”


• We specialise in the sale and purchase of quality used wheelchair accessible vehicles and ambulances.
• They can be bought as seen or refurbished and sign-written to your own requirements.
• Fully serviced, new mot & warranty
• Engineers inspection supplied if required.
• Free delivery service available
• All buses comply with new legislation
•
• Lease hire and purchase



A leading all-inclusive care provider has relaunched its annual staff-shadowing programme under a new name, ‘B:
In Your Shoes’, giving central support colleagues the chance to step into frontline roles and experience daily life in its homes first-hand.
As part of this, members of Berkley Care Group’s central team took part in the initiative across all 12 of their homes, working alongside teams in housekeeping, reception, hospitality, kitchens, and care.
Chief Executive Officer Laura Perry spent the day as a care assistant at Leycester House in Warwick, while Marketing Manager Rachel Clinton joined the housekeeping team at Blenheim House, one of Berkley’s luxury care homes in Melksham. They were joined by senior leaders from across the group, each stepping into very different frontline roles.
At Blenheim, Chief Financial Officer Stuart Devon supported the dementia care floor, while at Ryefield Court in Uxbridge, Financial Controller Wendy Lee Ping Sang swapped spreadsheets for spanners, assisting the maintenance team with the daily running of the home.
Others included Group IT Manager Adam Collett, who tried his hand as a chef at Worcestershire care home Burcot Grange, and People Resourcing Director Laura Purvis, who took on an events role at Portobello Place, in Chesham.
Together, the experience gave the central team a powerful perspective on the diverse and demanding roles that make Berkley homes run smoothly and, most importantly, on the compassion, skill, and dedication that enable residents to live well every day.
The initiative was designed with several clear aims. At its heart is the commitment of Berkley’s central team to maintain close connection with the realities of living and working in Berkley homes. While col-
leagues visit regularly, the programme provides dedicated time to understand the demands and achievements of frontline roles.
It also ensures that decisions made at group level are grounded in lived experience. By stepping into these positions, leaders gain valuable perspective on the challenges and impact of policies on colleagues and residents alike.
The shadowing days also celebrate the exceptional work of Berkley’s care home teams. From the compassion of carers to the attention to detail of housekeepers, every role plays a vital part in creating homes where residents feel valued, comfortable, and supported.
Feedback from earlier years of the initiative has already led to meaningful improvements across the group. These include introducing ‘Management Matters’ workshops to support line managers, upgrading IT, care and people systems, and investing in new estates and facilities processes to strengthen daily operations.

Commenting on the day, Laura Perry, Chief Executive Officer at Berkley Care Group, said:
“B: In Your Shoes was, once again, an incredibly eye-opening and humbling experience. Spending a day as part of our care team reminded me not only of the physical demands of the role, but also of the attention to detail and genuine compassion that underpin everything we do at Berkley.
“These small, everyday acts are what make our homes feel truly special. For me, B: In Your Shoes is about more than shadowing a role. It’s about listening, learning, and ensuring that our leadership decisions reflect the real experiences of our teams and residents.
“I’ve come away with an even deeper admiration for our colleagues, particularly in seeing how much of a difference the smallest gestures - like a shared laugh, a kind word, or a moment of reassurance - can make. Those interactions define life in our homes just as much as the care we provide and show why initiatives like this matter so much.”
Karolyn Sisto, Home Manager at Eastham Care Home, part of the Runwood Homes Group, has achieved an extraordinary personal and professional milestone by successfully completing an 18-hour trek to the summit of Mount Toubkal, North Africa’s highest peak, all in support of her residents.
On 6th–7th October 2025, Karolyn took on the gruelling challenge of scaling the 4,167-metre (13,671 feet) Moroccan mountain, battling through altitude sickness, blistered feet, and extreme temperature shifts. The trek began with a 7-hour ascent to the refuge at base camp, followed by a short rest before continuing the final and most difficult leg of the climb, starting at 3:00 AM in total darkness.
“The trek was gruelling, but thinking about our residents and the joy a summer house would bring them kept me going,” said Karolyn Sisto, Home Manager at Eastham Care Home

The fundraising climb was part of Karolyn’s personal mission to raise money for a summer house to be built in the home’s garden, a peaceful and accessible space where residents and their families can enjoy quality time outdoors.
So far, the effort has raised £675, bringing the home one step closer to making the vision a reality.
The atmosphere throughout the challenge was extremely tough, with high altitudes, steep terrain, and rapidly changing weather conditions. But the highlight, according to Karolyn, was reaching the summit which was an emotional and fulfilling moment made even more meaningful by the cause behind it.
Karolyn has gone to incredible lengths, literally, to improve the lives of residents at Eastham Care Home . Her team, and the wider community, are incredibly proud.
Leading mobility provider AAT is stepping up to help deliver the Government’s new value-based model of care, shifting hospital to community and sickness to prevention. And it is uniquely positioned, as its equipment- the top-selling stairclimbing wheelchair S-Max Sella- is already in almost every local authority social care department and NHS Trust across the UK.
In addressing hospital to community, one of the primary causes for delay in hospital discharge is the social care support needed for patients, be it short- or long-term. NHS data reports changes to stairs is the first change required to a home.
In addressing prevention, mobility is the biggest limitation affecting people in their homes. There are 1m+ accidents on stairs every year, resulting in 43,000+ hospitalisations. AAT’s S-Max Sella makes stairs safe for almost anyone with impaired mobility, with the help of a carer. The battery-powered stairclimbing wheelchair is “plug and play”, requiring no structural alteration nor installation. It can cope with almost every common staircase design, even turns and spirals.
It reduces risk and manual handling as it can traverse onwards from the flight of stairs

into whichever room is the final destination. It can even navigate external steps.
AAT’s unique re-issue capability for the Sella further delivers value: when the original recipient no longer needs the equipment, it can be re-prescribed to another person. AAT assesses each potential recipient, their carer and their home environment, and personally trains the carer(s) in the Sella’s safe operation as part of the process. No other stair solution has that capability.
“Making stairs safe is one of the biggest obstacles to all involved in social care- be it effecting efficient hospital discharge or preventing hospital admission in the first place,” says Peter Wingrave, AAT Director.
“With our existing presence within social care equipment stores, our nationwide team and speed of resolution, we are perfectly positioned to be the first call in addressing this element of the new Plan for Change. All it takes is a telephone call…”
Full details of AAT’s S-Max Sella and its re-issue can be found @ www.aatgb.com/ots/



When THE CARER invited care homes around the country to share their Coffee Morning celebrations on 26th September, coinciding with Macmillan's annual Coffee Morning, we knew the sector would rise to the occasion!
After all, care homes understand better than most the importance of community, compassion, and supporting those who need it most.
With a £50 Marks & Spencer prize on offer, we were inundated with nominations from dedicated care homes nationwide, each showcasing the creativity, heart, and community spirit that makes this sector so special. The entries were truly outstanding, making our decision incredibly difficult.
A FASHION SHOW TWO MONTHS IN THE MAKING
We are absolutely thrilled to announce that this year's winners are Allegra Care's nursing homes Olive Tree House and Rose Garden in Patchway, near Bristol, who went above and beyond with their joint Upcycled Fashion Show – an event that took two months of preparation and captured the imagination of their entire community.
The homes transformed recycled materials into stunning fashion pieces for their catwalk extravaganza. Residents breathed new life into old clothes, adding fresh buttons, decorative trims, and hand-painted designs. In a powerful environmental statement, they even created a giant plastic bottle sculpture made entirely from plastic bottles, highlighting that 34 million plastic bottles are used daily in the UK, with only half being recycled.
A COMMUNITY AFFAIR




Catherine Crawshaw, Regional Resident Liaison Manager, painted a vivid picture of the day's festivities: "There was also lots of fun with a summer holiday theme of fish 'n' chips and ice creams and the only song to accompany these models was 'We're all going on a Summer Holiday'! The models were residents, family members, team members, church and college volunteers all of whom made the event such a success."
But the star performers were undoubtedly the children from neighbouring Happy Days Nursery. "A special shout out has to go to the children of neighbouring Happy Days Nursery who all designed their own t-shirts and walked down the catwalk with Home Manager, Vlad, who dressed as a box to go with their catwalk song 'Big Fish, Little Fish'!" Catherine enthused. "The children were amazing to take part in two fashion shows and raise money from the sale of their t-shirts – what absolute super stars."
MAKING A DIFFERENCE
The combined efforts of Happy Days Nursery, Olive Tree House, and Rose Garden have raised over £150 for Macmillan Cancer Support –funds that will make a real difference to people living with cancer across the UK.
Once again, the care sector has demonstrated that when it comes to bringing communities together for a worthy cause, you simply cannot be beaten.
Congratulations to everyone at Allegra Care, and thank you to every care home that participated in this year's Coffee Morning competition. You truly did not disappoint us – you inspired us.


This year, Belong Wigan wanted to do something a bit different for their Macmillan World's Biggest Coffee Morning. The village's experience team consulted with their residents and apartment tenants who agreed they wanted to invite their friends from Platt Bridge Community Centre. Belong Wigan customers can often be found at the centre, enjoying bowls, bingo, shuffleboard and many of the activities available.
Customers wanted to share the special fundraiser with their friends and so welcomed them with open arms to join them for their coffee morning, featuring a fun raffle, a (lively) game of bingo, plenty of cuppas and of course, delicious cakes!
Charlene Frodsham, experience coordinator at Belong Wigan, said: "It was a fabulous morning, full of smiles, laughter, and community spirit – all while supporting such an amazing cause. We raised £236 and it was wonderful to have the Platt Bridge community as our guests. A big thank you to everyone who joined in and made it so special!"


Residents, relatives, colleagues, and local friends gathered at HCOne’s Millcroft Care Home in Redditch to take part in the World’s Biggest Coffee Morning in aid of Macmillan Cancer Support.
Held in the home’s welcoming Café, the event was a true celebration of community spirit, featuring delicious cakes, freshly brewed tea and coffee, and plenty of lively conversation. The Café was decorated for the occasion, creating a warm and friendly atmosphere where everyone could come together to enjoy themselves while supporting an incredible cause.
The Coffee Morning was part of Macmillan Cancer Support’s national fundraising campaign, which takes place annually to help provide vital services for people living with cancer and their families. Every slice of cake and every donation helps ensure Macmillan can continue offering emotional, medical, and financial support to those who need it most.
Residents and visitors alike commented on how enjoyable the day was. Many shared stories and laughter over tea and cake, with some even baking their own contributions for the table. Families of residents also joined in, making it a truly intergenerational gathering that highlighted the importance of connection and kindness.
The event raised valuable funds to support Macmillan’s work raising a total of £100, and the day captured
the fun, laughter, and sense of belonging that filled the home.
With the arrival of autumn, Millcroft is looking forward to marking special seasonal traditions such as Harvest Festival, while also preparing the home for the colder months with a calendar of cosy, community-focused events.
Millcroft is one of over 280 kind and cosy HC-One care homes across the UK, providing the kindest care to older people. This autumn, new residents can take advantage of a special welcome offer, enjoying 4 weeks for the price of 3 when joining before 30th November 2025.
Embrace the warmth of a kind community this autumn. Visit Millcroft - Care Home in Redditch, Worcestershire| HC One today to find out more about life at Millcroft.
Lyndsay Sard, Home Manager at HC-One’s Millcroft Care Home, said:

“We are so grateful to everyone who came along to support our Macmillan Coffee Morning. It was lovely to see our residents, families, and the local Redditch community come together. These events mean so much – not only do they raise money for a cause close to many hearts, but they also bring joy and togetherness for everyone involved.”


A recent Macmillan Coffee Morning at Five Oaks care home in Barnet raised £270 for Macmillan Cancer Support.
The UK’s leading cancer charity provides specialist health care, information and financial support to people affected by cancer. Macmillan also looks at the social, emotional and practical impact cancer can have, and campaigns for better cancer care.
“Macmillan does such amazing work, and we knew our coffee morning in support of the charity would be popular,” said Five


Oaks care home manager, Rahima Mulindwa
Residents, relatives, staff and healthcare professionals enjoyed a sumptuous spread of cakes, pastries, tea and coffee.
“We had a fantastic turnout – the car park was full and the room was buzzing with conversation and laughter,” said Rahima.
“We’re so grateful to everyone who attended for their generosity and support. Thanks to them, we raised an amazing £270. It’s truly inspiring to see how a great cause can bring so many people together.”

At Sussex Grange in Selsey, we held a fantastic Macmillan Coffee Morning on Tuesday (Tuesday September 30) with our wonderful residents, their friends and family. The event included a raffle and Bring and Buy sale, with many members of our marvellous Care Home team modelling some of the clothes and shoes which were available to buy.
Our kitchen staff whipped up a storm, too, with an amazing array of delicious cakes and treats to go with guests' teas and coffees and so far, the event has raised over £130 for Macmillan Cancer Support!
At Sussex Grange in Selsey, West Sussex, we love having lots of fun with the wide range of daily activities which are always going on and, judging by all of the laughter and singing that was coming from all who attended, this morning was no different!


HUNDREDS of pounds were raised for Macmillan Cancer Support thanks to a joint fundraising event hosted by two North East care homes and a church group.
St Francis of Assisi Church Friendship Group, Ingleby Care Home, and Hazelgrove Court Care Home brought residents, families, staff, and supporters together for the fundraiser.
Held at St Francis of Assisi Church, Ingleby Barwick, dozens of attendees enjoyed various games, sweet and savoury treats, hot and cold drinks, and catching up with friends.
The event raised £500 for Macmillan Cancer Support, which provides practical, emotional and financial support to people living with cancer and their families across the UK.
Ingleby Care Home, on Lamb Lane, provided a “guess how many sweets in the jar” game, along with a tombola and raffle prizes.
Hazelgrove Court Care Home, on Randolph Street, Saltburn-by-the-Sea, contributed a “guess the weight of the cake” challenge, a “guess the name of the teddy” game and additional raffle prizes. And the St Francis of Assisi Church Friendship Group hosted and provided the refreshments. Guests also enjoyed a lively game of Spanish bingo, with the winner required to shout “Olay, Olay, Olay,
Olay!” to claim their prize.
Olive Smith, 89, a resident at Ingleby Care Home, said: “I love playing Spanish bingo, even though I didn’t win.”
Joyce Tibbett, 91, from Hazelgrove Court Care Home, added: “I love supporting Macmillan as everyone knows someone who has been affected by cancer in their lives.”
John Hymes, 70, also from Ingleby Care Home, said: “It has been a wonderful event and the food provided by St Francis Friendship Group was amazing.”
Mike English, home manager at Ingleby Care Home, was delighted to win a raffle prize, while staff from all three organisations praised the success of the event.
Kirsty O’Connor, Angela Hudson, Sharon Lewis and Sue Dixon – representing Ingleby Care Home, Hazelgrove Court Care Home, and the St Francis Friendship Group, respectively – all agreed it was a fantastic opportunity to work together for a good cause.
Sharon Lewis, activities coordinator at Hazelgrove Court Care Home, said: “It’s amazing what can be achieved when care homes and the community come together.
“Supporting Macmillan means so much to so many, and we’re proud to have played a part in raising funds for such an important charity.”

Rownhams Manor Care Home recently hosted a heartwarming Macmillan Coffee Morning, bringing together residents, staff, and members of the local community. The event was a delightful success, filled with delicious treats, laughter, and meaningful conversations. Everyone who attended—whether living at the home or visiting from the public—truly enjoyed the occasion.
It was more than just coffee and cake; it was a celebration of community spirit and support for a vital cause. Residents prepared for the event by helping support with decorations and cake decorating. This event was meaningful to our residents as some have experienced cancer personally whilst others have had other people dear to them effected.

Macmillan Coffee Morning –Mission Cake Accomplished!
At Lycroft Care Home in Wisbech what a morning it was! Our very first Macmillan Coffee Morning and the cakes didn’t stand a chance – gone faster than you can say Victoria Sponge!
Huge thanks to our residents’ families who baked like Bake Off finalists, to our staff who whipped up good ies (and sneakily bought a few… we saw you!), and to everyone who came along armed with forks and big appetites. Between the laughter, chatting, and cake demolishing, we raised a WHOPPING £156 for such a fantastic cause! Not bad for a few hours of coffee, crumbs, and cake-induced joy.



Temple Ewell Nursing Home was delighted to host a Macmillan Coffee Morning on 26th September 2025, with coffee and cakes galore! It was wonderful to see so many of our residents, relatives, and staff come together to support such an amazing cause.
Alongside the delicious treats, we held a fun quiz and two competitions for everyone to take part in, which really brought out the competitive side of both residents and visitors, it was fantastic to see!
Many of our residents also got involved in the making, baking, and decorating of the cakes on show it was like an episode of Great British Bake Off, with the fruit scones proving to be a particular highlight and firm favourite though the banana bread was a close second.
A truly memorable moment of the morning was when our Head of Services joined the celebrations, singing along to the music, dueting, and even dancing with residents, bringing so much joy and energy to the event.It was a wonderful day of community spirit, laughter, and togetherness, and we were proud to open our doors to the wider community for such a worthy cause..

At Thornhill House residents and families enjoyed the coffee morning for Macmillan with residents baking and decorating the cakes and enjoying karaoke.
The event raised £210 for Macmillan, which is close to residents' hearts
The home manager is now raising money for breast cancer by doing Strictly for Barnsley hospital.
The home involved the local community joining in with local bakeries donating cakes and families also baking with a bake off competition.





Residents at a Cheltenham care home enjoyed homemade cakes and bakes with families and friends at their annual Macmillan Coffee Morning fundraiser.
Chefs Manuela Deriu and Jade Robbins, who work at Wentworth Court specialist dementia nursing home on Village Road, provided a lavish table of tray bakes, chocolate truffles, frosted cupcakes and a show-stopping Victoria sponge topped with fresh fruit, to tempt visitors to donate to the cause.
Wentworth Court Managing Director, Mitesh Dhanak said: “Our coffee morning for Macmillan is a highlight in our calendar. It’s an annual event that brings residents, families and our team together to support a good cause while enjoying conversation over a cafetière of coffee or a pot of tea.
“Today’s event raised close to £100 along with money raised throughout September from donations to our café.”


Coppice Lodge Care Home in Arnold, Nottinghamshire, part of HC-One, proudly joined thousands of people across the UK in support of Macmillan Cancer Support by hosting a special Coffee Afternoon as part of the charity’s annual fundraising campaign.

The event brought together residents, families, colleagues, and members of the local community, who gathered to enjoy freshly brewed tea and coffee alongside a tempting variety of homemade cakes and biscuits. The home’s lounge was decorated for the occasion, creating a warm and welcoming atmosphere where guests could relax, chat, and enjoy each other’s company. Laughter and conversation filled the room as everyone came together to support a cause close to many hearts.
Generous donations were made throughout the afternoon, with all proceeds going directly to Macmillan Cancer Support. These vital funds will help the charity continue its work providing practical, medical, and emotional support to people living with
cancer, as well as their families.
Combined with the Macmillan Cancer Support Coffee Afternoon event, the home also hosted a Kitty Café Afternoon including a visit from the cat rescue charity, Meow and Furever.
Ken Buxton, Home Manager at HC-One’s Coppice Lodge Care Home, said: “We’re so proud to support Macmillan Cancer Support and the incredible work they do. Cancer affects so many lives, and it means a lot to us to be able to give something back. Our residents loved being part of the fundraising and welcoming visitors into the home for such an important cause.”

Angela Allen, Front of House Manager at HC-One’s Coppice Lodge Care Home, added: “It was wonderful to see our residents, families, and neighbours come together to enjoy such a positive event. The generosity shown was truly inspiring, and we want to thank everyone who came along, donated, or baked cakes to make the afternoon a success.”




Chefs at Colten Care’s 21 care homes across the south put a Willy Wonka-style twist on the Macmillan Coffee Morning.
Residents, team members and visitors raising a mug at the annual charity fundraiser were served with freshly prepared homemade cakes, cookies and pastries.
At each home, one of the tasty treats was a ‘Golden Cup Cake’, containing a layer of edible gold leaf, sugar balls or cherry guaranteeing the lucky recipient a prize bottle of bubbly.
The added interest prompted smiles all round as, together, the homes raised hundreds of pounds for the charity appeal in aid of people living with cancer.
At Fernhill, a dedicated dementia care home in Longham near Bournemouth, Companionship Team Leader Cara Duroe said: “We always support the Macmillan Coffee Morning. It’s a fantastic community initiative that brings together families, friends and local contacts. Everyone has great fun while doing their bit to help with cancer support.”
Along with the cupcake fun at Woodpeckers in Brockenhurst, New Forest, residents enjoyed a quiz and sweepstake with prizes awarded. The coffee morning also coincided with the birthday of resident June Farrow, adding to the party atmosphere.
Over at Kingfishers in New Milton, the coffee morning raised more than £250 with the home staging a performance by guest singer Kelly Lorraine.
Resident Jack Phillips summed up the event, saying: “It was a lovely morning, the lounge was full of people, and the music was excellent.”
Other Colten Care homes staging coffee mornings for Macmillan included Amberwood House in Ferndown, Brook View in West Moors and Lymington homes Court Lodge and Belmore Lodge.
Team members at the provider’s Ringwood head office also held an event in support.



Residents, families, and team members at HC-One’s Ebor Court Care Home in Nether Poppleton, York, came together to host a Macmillan Coffee Morning, raising an impressive £250 in support of Macmillan Cancer Support. The event, part of Macmillan’s annual nationwide fundraising campaign, saw Ebor Court filled with the delicious aroma of freshly baked cakes and treats. Head Chef Ian Munro prepared a fantastic selection of bakes that delighted everyone who attended. Residents, relatives, and colleagues enjoyed a morning of coffee, cake, and conversation — all in aid of a worthy cause.
Lifestyle Manager Denise Cooper, who helped organise the event, shared why the fundraiser was especially meaningful to her:
“It was such a pleasure to raise these funds. Having personally experienced cancer and received support from Macmillan, I truly understand how crucial fundraising is for this fantastic charity.”
The Ebor Court community was proud to contribute to Macmillan’s mission of providing vital support to those affected by cancer. The event was filled with smiles, laughter, and a shared sense of purpose.


Compton View recently hosted a wonderful MacMillan Coffee Morning, bringing together residents, families, and the wider community for a morning of fundraising and fellowship. The event saw a steady stream of visitors throughout the morning, with families eagerly joining in the festivities to support this important cause. The atmosphere was warm and welcoming from the start, with everyone united in their commitment to raising funds for MacMillan Cancer Support while enjoying quality time together.
The morning was made even more special by the appearance of Tina Jay, who came along to entertain everyone with her musical talents. Her performance brought an extra sparkle to the occasion, filling the room with melody and joy. Adding to the excitement, organizers had arranged a chocolate raffle that proved extremely popular with attendees, giving everyone the chance to win some sweet treats while contributing to the fundraising efforts. The combination of live entertainment and fun activities helped create a truly festive atmosphere.
One of the highlights of the event was the magnificent selection of homemade cakes on offer. All the residents thoroughly enjoyed the opportunity to choose from the tempting array of baked goods, each one lovingly prepared by volunteers and supporters.
The residents were particularly animated during Tina's performance, dancing and singing along with enthusiasm and delight. The music sparked poignant moments too, as it provided an opportunity for residents to share cherished memories of family members and friends they had lost to cancer. These touching exchanges reminded everyone of why MacMillan's work is so vital and meaningful. By the end of the morning, it was clear that the event had been a complete success, not only in raising funds but in bringing people together, creating joyful memories, and honoring those who had been affected by cancer.


Residents, their families and staff at the Healthcare Management Trust’s care homes came together to have a cuppa and raise funds for Macmillan Cancer Support.
Macmillan Coffee Morning took place at the Trust’s four care homes: Norden House in West Sussex, Marie Louise House in Hampshire, Coloma Court in Bromley and St Quentin’s Care Homes in Newcastleunder-Lyme.
Staff and residents’ family members donated homemade cakes and biscuits for the events and raised more than £200 for the charity, which supports almost 3.5 million people in the UK living with cancer.
Adam Bloor, Director of Community and Complex Care at HMT, said: “We’re delighted to see so many of our resident and their families come together with our care home staff to support such a worthy cause. So many of us have been affected by cancer, and Macmillan Cancer Support provides vital support to those who need it.”




At Park View in Gloucester we had a wonderful time celebrating The World’s Biggest Coffee Morning with residents, staff, families, and friends. Everyone got involved, staff and residents baked at home and brought in a delicious variety of cakes, while others shared their favourite recipes and enjoyed tasting all the different bakes together. We also invited families and friends to join in, making it a truly warm and social morning filled with chatter, laughter, and the smell of fresh baking.

The atmosphere was fantastic, with residents proud to contribute and excited to welcome guests into the home. Thanks to everyone’s generosity, we raised £150 in cash on the day, with even more donations continuing online. It was a wonderful example of our community coming together for a special cause, enjoying good company, great cake, and raising funds to support those affected by cancer.

Allegra Care’s St Georges’ Nursing Home near Weston-super-Mare stepped back in time to the 1950s for their “Moment in Time” Coffee Morning to raise funds as part of the Macmillan World’s Biggest Coffee Morning. Elvis, Marilyn Monroe, James Dean and Humphrey Bogart were just some of the stars that joined residents for a fun packed morning.
The home also opened their Boots Memory Box. The pharmacy chain have sent care homes a memory box with replica boxes and advertising materials. It was fun to reminisce about products from Ponds Cream to Gripe Water! The home’s kitchen team followed the 1950s theme with homemade milkshakes and cakes.


Brockington House Care Home in Hereford has once again participated in Macmillan's World's Biggest Coffee Morning, continuing its tradition of supporting the cancer charity.
The event, which has become an annual fixture at the care home, brought together residents and their families for an afternoon of refreshments, homemade cakes, games and quiz activities, all aimed at raising funds for Macmillan Cancer Support.
Tara, Activity Lead at Brockington House, emphasised the importance of the event.
"The home is very supportive of different charities but MacMillan is always one they wish to support.
I always inform my residents that whatever we raise all amounts to something. They are always fantastic in supporting and wanting to give something back. Although we enjoy the afternoons events and try and make it a fun- event we don’t lose sight of the importance of why we have come together. The residents at Brockington House and staff all show respect and compassion for any individuals that are dealing with cancer, we are all living or working in a Care Community so fully understand what this disease can do, that’s why we will always support. "


Residents, colleagues, families, and friends came together at HC-One’s Foley Grange Care Home in Kidderminster to host a Macmillan Coffee Morning, raising funds and awareness for Macmillan Cancer Support.
The home was filled with the aroma of freshly brewed coffee and a colourful display of homemade cakes, cupcakes, biscuits, and sweet treats, lovingly baked and donated by colleagues, residents’ families, and members of the local community. Guests enjoyed an afternoon of conversation, laughter, and entertainment while making a meaningful contribution to an important cause.
The event not only raised funds to support Macmillan’s vital work but also created a warm and vibrant atmosphere for residents and visitors alike. For many of the residents, the occasion sparked fond memories of family gatherings, tea parties, and community get-togethers.


Staff and residents at Elgar Court Residential Care Home in Malvern in held a charity coffee morning and bake last Friday 26 September to raise money for Macmillan Cancer Support.
Residents enjoyed spending time with friends and relatives, and members of the local community. Head chef and staff had baked lots of lovely cakes, biscuits and pastries with a special focus on those that were Gluten intolerant diets – for everyone to sample and for guests to buy and take home everyone’s needs were catered for! Some residents had baked cakes and biscuits for the occasion too along with their visitors and members of the community, everyone was spoilt for choice!
Elgar Court Residential Care’s coffee morning was a big success, raising money for this charity and, most importantly, everyone had a great time doing it! Jenny Fletcher a resident at the home, commented: “MacMillan is such a fantastic
in the community, we all love raising money for them and



Care sector leaders convened in Westminster last week for a roundtable discussion on the development of a Care Professionals Register (CPR) in England.
Hosted by the National Association of Care & Support Workers (NACAS) and chaired by the Rt Hon Damian Green, former MP and Chair of The Social Care Foundation, a UK-wide think tank, the meeting marked a significant milestone in the sector’s efforts to professionalise the workforce and protect the public.
Liz Blacklock, CEO of NACAS, a professional body committed to raising the standards and status of care professionals across the UK, opened the session by outlining the progress of the CPR initiative.
She highlighted the creation of a voluntary register in partnership with the Institute of Health & Social Care Management in 2021 and the successful completion of the Professional Standards Authority’s Public Interest Assessment in July this year.
To date, over 500 professionals have joined the CPR pilot, with a majority being self-employed or Personal Assistants.
NACAS believes the register will play an important role in both safeguarding the public and building trust, while also raising the status of care as a skilled profession.
It aims to promote accountability and high standards, giving confidence to employers, people drawing on care, and their families. At the same time, the register will support career development by fostering a stronger sense of professional identity and give the sector a more unified voice in calling for better working conditions.
Registered Care Professionals will need to go through robust verifications and checks, and adhere to a code of conduct and defined set of standards as determined by a sector-wide steering group Liz Blacklock said: “We fully recognise that registration is not a silver bullet, but it’s a vital step toward recognising care work as a profession and safeguarding those who rely on it.
“The aim isn’t to make registration difficult or to put barriers in the way of people needing care; it’s about finding the right balance — protecting the public and raising standards, while still making it straightforward for care professionals to join and keep their registration, and for families to access the support they need.”
The roundtable meeting confirmed strong sector interest in the CPR, while also highlighting the need to clarify scope, purpose, and practicalities.

Attendees discussed how the register might align with wider sector reforms, including the Covid-19 Public Inquiry, the Casey Commission, and Skills for Care’s Workforce Development Strategy.
Notable attendees included: Fraser Rickatson, Policy Manager at Care England; Daisy Cooney, Head of Policy, Practice and Innovation at the Homecare Association; Finn Turner-Berry, Policy, Research and Projects Officer at the National Care Forum; Dan Archer, CEO of Visiting Angels; Natasha Southall, Registered Nurse Avery Healthcare; and Sarah Gilbert, Head of Workforce Strategy at Skills for Care.
“Damian Green, Chair of the Social Care Foundation (SCF), said: “I believe the register will play a crucial role in raising the status of care workers, as recommended in the SCF’s report, ‘Who Cares’, and making social care a more attractive career destination.
“That’s why I’m fully supportive of NACAS and its commitment to setting up a professional register, in collaboration with the sector.”
The meeting also featured a powerful testimony from Louise Woollam, whose Campaign for Richard’s Law demands an official register for carers. She shared her personal experience of hiring a private carer for her husband, who lives with Alzheimer’s, only to discover that they had stolen from her family home.
The carer, who was handed a 12-month suspended sentence by Weymouth magistrates in July, was previously convicted of a similar crime in 2010, but a basic DBS check did not reveal their unlawful past.
Louise said: “Without a register, families like mine are left vulnerable. This initiative could help drive accountability and prevent future harm.”
Next on the agenda for NACAS is to establish focus groups tasked with developing a fitness-to practice-framework and define agreed standards. These groups will report back to the main CPR Working Group, made up of attendees from the roundtable meeting.



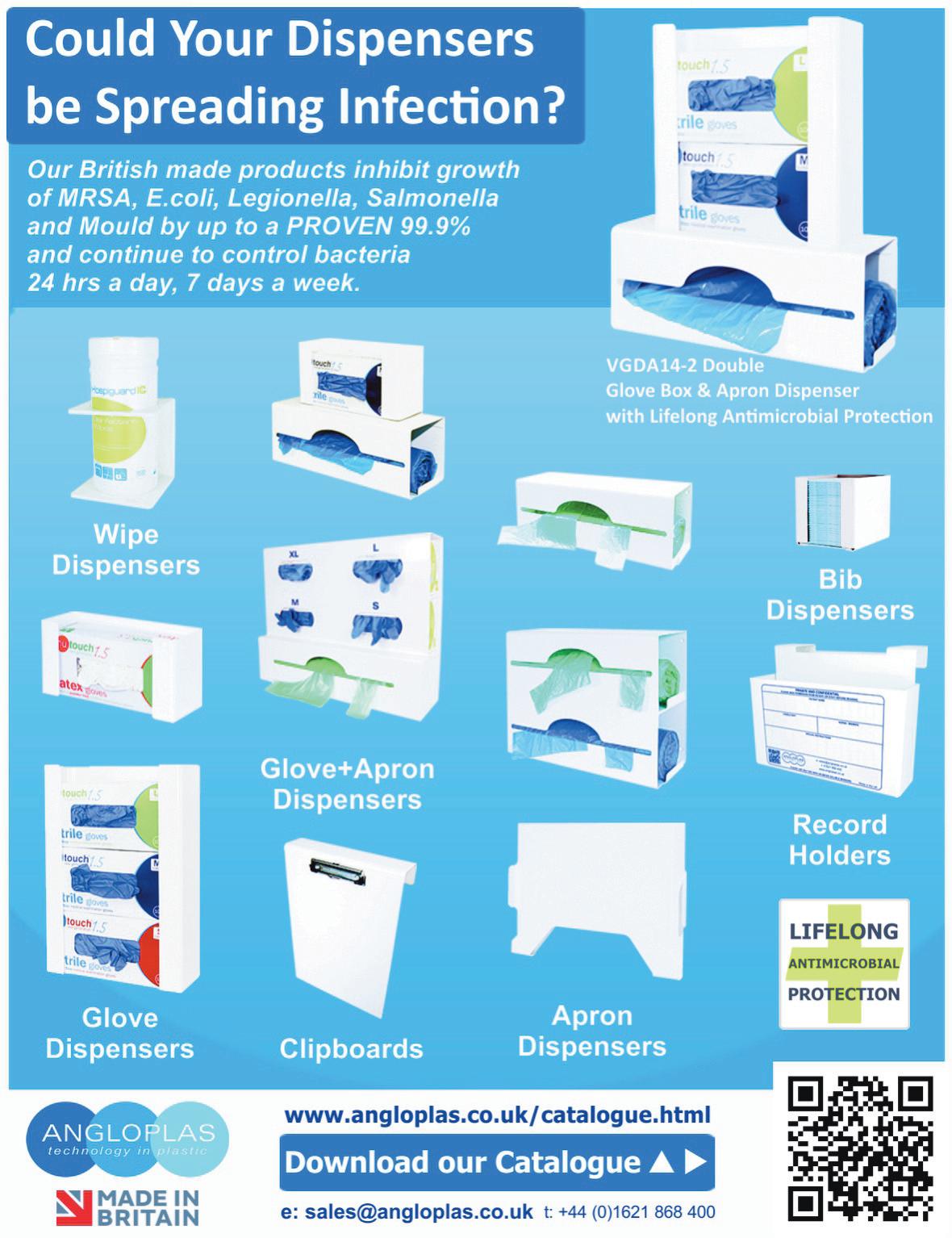
When Howard Ross moved into Cumbrae House care home in Glasgow’s west end on 10th September 2024, it followed a serious fall at home that left him with seven broken ribs, delirium and severely reduced mobility. He was confused, struggling with balance and considered at high risk of further falls, experiencing eight in his first six weeks at the home.
His wife, Mags, was unsure what to expect. Their shared life, built through decades of working together as accountants, had changed overnight. Howard’s condition had declined so quickly that Mags described feeling like she’d lost her husband.
The decision to move into care was difficult but made with safety and stability in mind. In the early stages, Howard was often disoriented and unsure why he had been admitted. Mags did what she could to help bridge the gap by bringing in profit and loss sheets from their former work, hoping that the familiar material might help him reconnect with a part of himself.
Meanwhile, the care team at Cumbrae House - in partnership with specialists from the Glenkirk Centre - supported Howard through a formal dementia diagnosis and developed a focused care plan tailored to his needs. With consistent physiotherapy and a regular routine, his strength and balance began to improve. The steady involvement of staff, alongside Mags’ presence, helped rebuild his confidence and trust.
As Howard’s condition stabilised, so too did the couple’s outlook on the future. Mags began speaking to Karen Mackie, manager at Cumbrae House, about whether it might be possible to return to Madeira - their long-time favourite holiday destination. Rather than see it as unrealistic, Karen and the team worked to make it possible.

They arranged for Howard’s medication to be pre-packed into clearly labelled blister packs, with simple written instructions to support safe use while abroad. They also helped Mags plan for logistical challenges, ensuring the trip could be both manageable and enjoyable. Now, less than a year after Howard’s fall, the couple are preparing to board a flight back to the island they love.
Mags said: “A year ago, I couldn’t imagine us being where we are now. Nobody ever wants to see their other half go into a care home, it was a really difficult decision and I was heartbroken. But for Howard’s safety, it had to happen.
“I used to think care homes meant the end of independence, but what we’ve experienced has been completely different. From day one, the support here has helped us get back to something that feels close to normal. It didn’t take long to realise that the person-centred care wasn’t about taking things away, it was about working with experts to in fact improve Howard’s quality of life.”
Cumbrae House is part of Oakminster Healthcare, a group of five care homes located throughout Glasgow. At the heart of Oakminster Healthcare’s philosophy is a commitment to personalised, resident-led care that goes beyond meeting basic needs. Each care plan is built around the individual, with a strong focus on health, wellbeing, and meaningful daily experiences.
By listening closely to residents and their families, Oakminster Healthcare ensures that support is not only clinically sound but also deeply personal, helping people maintain independence, reconnect with cherished routines, and embrace opportunities that bring joy and purpose.
Karen Mackie, manager at Cumbrae House, said: “Our job is not just to provide support, but to help people continue living their lives in a way that feels meaningful to them.
“For Howard, that meant more than just meeting his daily needs, it was about helping him reconnect with the things that made him feel like himself. That included familiar routines and the freedom to enjoy holidays.
“We spent time getting to know Howard, listening to his story, understanding what brings him comfort and joy. That’s the heart of what we do here at Oakminster. We don’t believe in a one-size-fits-all approach to care. Every person who comes through our doors is treated as an individual with their own preferences, memories and goals.”
The upcoming trip to Madeira isn’t just a holiday. For Howard and Mags, it marks the return of something they thought they had lost and a quiet reminder that, with the right support, life doesn’t stop in care.
Staff and residents at Barchester’s Hilton Park Care Home in Bottisham have been marking World Mental Health Day by taking part in a range of different activities to promote good mental health. World Mental Health Day took place on Friday 10 October, the idea behind the day is to encourage people around the word to talk about mental health in general and how we all need to look after our mental health by talking about things and sharing our challenges. The theme this year is ‘Access to Services – Mental Health in Catastrophes and Emergencies’ as set by the World Federation for Mental Health. The WFMH has been working for over 70 years to make sure mental health is treated on a par with physical health. World Mental Health Day is also an opportunity to ask for help if you are struggling.

Residents and staff embraced the spirit of the day by taking part in a variety of activities. These included a visit to Tenpin Bowling, where residents enjoyed a wonderful evening, as well as relaxation sessions such as gentle exercise and arts and crafts. There was also a music session led by music therapist Julie Bristow, and open discussions about mental health, where participants shared their feelings and challenges.
Geanina Tinca, General Manager at Hilton Park Care Home, said: “Our residents have had a wonderful day. It’s so important to take time to focus on our mental health, talk about our feelings, and practise selfcare. Everyone thoroughly enjoyed the day, and it was a meaningful reminder of the importance of looking after our wellbeing.”
In today’s highly regulated health and social care environment, providers face the dual challenge of ensuring compliance while striving to deliver safe, high-quality, and commercially sustainable services. Care Inspections UK Limited (CiUK) has emerged as a trusted partner in this landscape, providing a professional and independent inspection service that goes beyond the standard requirements of the Care Quality Commission (CQC), The Care Inspectorate Wales (CIW) and the Care Inspectorate (Scotland), collectively “The Inspectorates”
What sets CiUK apart is its status as a registered inspection body, operating with the highest levels of professionalism and governance. This official recognition imbues care providers with confidence that inspections are carried out with rigour, objectivity, and an unwavering focus on evidence. Every report is underpinned by validated, research-based methodology, ensuring the outcomes are credible, balanced, and practical.
BEYOND CQC/ CIW/ CI STANDARDS

• Operational risk management involves identifying risks before they become incidents, reducing exposure for service users and providers.
• Quality enhancement: Assessing opportunities to raise standards in care delivery, staff engagement, and governance.
• Commercial sustainability: Offering insight into how operational practices influence financial performance, helping providers balance compliance with business viability.
The result is an inspection report that is not only regulatory-ready but also a strategic tool for improvement.
Professionalism is at the heart of CiUK’s ethos.
Inspections are conducted by highly experienced professionals who bring frontline expertise from clinical, managerial, and governance roles in the care sector. This depth of knowledge allows CiUK to deliver meaningful feedback that resonates with staff at every level, from frontline carers to boardroom directors.
Care providers today operate in an environment of heightened scrutiny and rising expectations. CIUK’s inspections do more than highlight compliance gaps; they provide a clear roadmap for reducing risk, enhancing quality, and driving organisational improvement.
By identifying weaknesses early, providers can take corrective action before issues escalate. At the same time, CiUK’s focus on strengths and opportunities supports a culture of positive development. This balanced approach ensures that inspection outcomes are constructive, not punitive, fostering continuous organisational improvement.
SUPPORTING COMMERCIAL
One of the most overlooked aspects of care provision is its commercial dimension. Poor compliance and weak governance inevitably carry financial consequences, from reputational damage to contract loss. CiUK recognises this and integrates commercial insight into every inspection. CiUK helps providers achieve operational excellence and commercial resilience by aligning care quality with business performance.
THE CIUK
While CQC/ CIW/ CI inspections focus on fundamental areas such as safety, effectiveness, responsiveness, and leadership, CiUK’s approach extends further. Each CiUK inspection covers all the domains CQC/ CIW/ CI would expect, but also incorporates additional layers of analysis essential for continuous improvement. This Includes:
Independence is equally vital. As an external registered inspection body, CiUK reassures providers that its findings are unbiased and transparent. In a sector where credibility matters, this impartiality is invaluable in preparing for CQC inspections and demonstrating accountability to commissioners, investors, and the wider community.
Choosing Care Inspections UK Limited means selecting a partner committed to professionalism, independence, and comprehensive excellence. CiUK inspections do more than prepare organisations for regulatory visits—they empower providers to deliver safer, higher-quality care while protecting their reputation and commercial future. CiUK delivers evidence-based assurance and actionable insight for providers who want more than compliance.
Guidance to support acute teams to deliver optimal care for older people living with frailty has been developed by Getting It Right First Time (GIRFT) in collaboration with the BGS.
The new guidance, Co-ordinated frailty care for better outcomes, offers tools, practical advice and checklists to support a system-wide approach, ensuring older people with frailty receive timely access to care in the right setting.
It also features a set of actions to improve key areas: identifying frailty, preventing deconditioning, delirium, falls and bone health, end of life care and advance care planning, community-based care, and working with care homes.
IN ADDITION TO OPTIMISING HOSPITAL CARE, ITS OVERARCHING PRINCIPLES ARE:
• Early identification of the severity of frailty

• Adopting a ‘home first’ approach to avoid unnecessary emergency department (ED) attendance or hospital admission.
• Delivering care outside hospital at an appropriate scale, to meet local demand and avoiding long waits in EDs, which cause delay-related harm.
• Early discharge planning using a ‘home first’ principle.
• This latest guide builds on our 2023 collaboration with GIRFT and the Royal College of Physicians (RCP), which produced the Hospital Acute Care Frailty Pathway, and the linked Six Steps to Better Care. It should also be used in conjunction with our Joining the dots: A blueprint for preventing and managing frailty in older people resource.
The guide can support the move towards developing neighbourhood teams, as outlined in NHS England’s Neighbourhood health guidelines 2025/26.
Dr Adrian Hopper, GIRFT’s clinical lead for geriatric medicine, said: “The demographic changes we are already seeing mean all healthcare professionals, regardless of their specialty, need the knowledge and skills to deliver effective care to older people.
“Now is the time to tackle variation in care we have seen across the country – issues like older people with frailty being conveyed to hospital disproportionately or deteriorating in hospital – and to adopt system-wide best practice.
We hope that integrated care systems review their existing services against this GIRFT guide and will work with their partners to embed an approach that will help us to deliver optimal care for older people living with frailty, now and into the future.”

Residents at a Sanctuary Care home in East Kilbride recently enjoyed a unique and exciting outing - ice skating in their wheelchairs at East Kilbride Ice Rink.
Jo Sloan (91) and Irene Cassells (80), who live at not-for-profit Forefaulds Care Home, enjoyed the incredible experience with the home’s Activities Coordinator Kirsty Bagan and Care Assistant Argie Fermil. Kirsty was inspired following visits to the local shopping centre, where she often saw wheelchair users on the ice rink and thought, “What a brilliant idea!”
She said: “When I showed Jo the videos of them skating the next morning, she laughed and said she’d love to do it again. That means the world to me.
“Irene was all smiles on the day, waving to her husband, daughter, and grandson who came to watch. Their families were deeply grateful, saying
the outing looked brilliant.”
“I was nervous,” Kirsty admitted. “It’s been over 25 years since I last skated, but seeing their smiles made it all worthwhile.”
The residents were joined by another group in wheelchairs, who offered encouragement and joined Jo and Irene around the rink.
“They were so friendly and gave us tips - it really added to the experience,” Kirsty said.
Jo and Irene are active members of the Forefaulds community, enjoying arts and crafts, cooking sessions and live entertainment.
“Whether it’s a craft session at home or something extraordinary like our recent ice-skating trip,” said Kirsty, “taking part in meaningful activities gives our residents joy, confidence, and a renewed sense of purpose. These experiences prove that age is no barrier to adventure - and the smiles say it all.”
Crystal Care Collection reached a major milestone as they received the keys to their fifth care home, Fairwood Fields in Pontefract.
Set to welcome its first residents in the coming weeks, Fairwood Fields is the first Yorkshire based care home to be operated by Crystal Care Collection.
The new home features 66 en-suite bedrooms, landscaped gardens, a cinema room, a beauty salon, and the latest in care technology to support residents’ wellbeing and independence.
General Manager at Fairwood Fields, Lynn Robinson, said, ‘We’re abso-
lutely thrilled to take the keys to Fairwood Fields, where we’ll be representing the values of Crystal Care Collection in Yorkshire – clarity, community, and compassion.’
‘Our home will be a place for exceptional care and a hub for people in the area, starting with our ‘Reyt Yorkshire’ themed Grand Opening on Saturday 25th October. All are welcome to join us for a day packed with family fun, live entertainment, delicious Yorkshire food like parkin and liquorice cake, and VIP tours of Fairwood Fields, and we can’t wait to welcome our first residents to their new home.’


Repose Furniture is one of the UK’s leading manufacturers of bespoke seating solutions, with a reputation built on craftsmanship, innovation, and a strong commitment to improving the quality of life for its customers. Established in 1999 and based in the West Midlands, the company has grown from a small family business into a trusted supplier to both the domestic and healthcare markets. Every chair produced by Repose is handmade in the UK, with an emphasis on quality, durability, and comfort, ensuring that each product meets the specific needs of its user. Whether for home use or demanding healthcare environments, Repose combines skilled upholstery techniques with modern engineering to create chairs that provide postural support, pressure management, and ease of use. Their wide product portfolio includes rise and recline chairs, hospital and care home seating, bariatric solutions, and specialist products designed to address particular medical and lifestyle needs. An essential element of their offering is flexibility: customers can choose from a range of back styles, seat cushions, mechanisms, and fabrics, allowing each chair to be tailored to the individual. Interchangeable parts mean that a chair can adapt as a user’s requirements change, extending the product’s longevity and ensuring value for money. The healthcare sector is a particular area of expertise for Repose. They strive to design chairs that balance comfort with clinical functionality. Features such as tilt-in-space mechanisms, adjustable cushioning, and pressure relief options make their healthcare seating particularly suited to long-term use in hospitals, hospices, and care homes. The company’s bariatric range demonstrates the same careful attention to

detail, offering robust yet comfortable solutions for larger users.
While customisation is the centre of the Repose offering, they also recognise the urgency often faced in healthcare settings. To address this, Repose have developed their Healthcare Express Chairs, designed to deliver highquality healthcare seating at speed. The models in this range can be despatched within just five working days. The Multi Bari Express and bestselling Boston Express, for example, are available on this five-day lead time, offering care providers a rapid solution without sacrificing quality or functionality. For less specialist needs, some homecare models are even available on faster turnaround times, demonstrating Repose’s ability to balance responsiveness with craftsmanship.
Repose’s reputation is further reinforced by its after-sales support, 5-year manufacturing warranty, and commitment to ethical and sustainable practices. With a UK-based factory, a dedicated distribution network, and close relationships with healthcare professionals, the company continues to be a trusted partner in multiple sectors throughout the country and beyond. In combining bespoke design with reliable express options, Repose Furniture stands out as a manufacturer

University College London has published a study, part funded by Alzheimer’s Society’s Heather Corrie Impact Fund, which shows it’s possible to cut the time for diagnostic MRI scans for dementia to one third of their standard length.
The findings have been described as a step towards ending ‘the postcode lottery in dementia diagnosis’. Shorter scans would be easier and more comfortable for patients and also mean more people could be scanned at a lower cost. The team behind the study say this could at least double the number of dementia scans able to be done in one day.
MRI scans often play a key role in an accurate dementia diagnosis, including ruling out other causes of symptoms and assisting in diagnosing the type of dementia. Emerging disease-modifying treatments such as lecanemab and donanemab also require an MRI scan before starting treatment and for safety monitoring during the course of treatment.Reducing the cost of scanning would contribute to lowering the total cost of delivering for such treatments.

The ADMIRA study (Accelerated Magnetic Resonance Imaging for Alzheimer’s disease) aimed to understand the reliability of fast MRI scans compared to standard-of-care clinical scans.
The research team scanned 92 people in an outpatient setting where an MRI brain scan was planned as part of their routine clinical assessment. The accelerated scans were carried out and enhanced to increase the quality of the image using new scanning methods. Three neuroradiologists examined these scans, and weren’t aware if they were looking at fast or standard-of-care scans.
The team found that the quicker scans reduced time in the scanner by 63% and they were as reliable as the standard-of-care scans for diagnosis and visual ratings.
Richard Oakley, Associate Director of Research and Innovation at Alzheimer’s Society, said: “Dementia is the UK’s biggest killer, but one in three people living with the condition haven’t had a diagnosis. An early and
accurate diagnosis isn’t just a label, it’s the first step to getting vital care, support and treatment.
“While MRIs aren’t the only way to diagnosis dementia, very few people with concerns about their cognitive health are offered one as part of the diagnosis process, mainly because they are expensive and not widely available. These faster MRIs, which take less than half the time of standard scans, could help end this postcode lottery in dementia diagnosis, cut costs and potentially give more people access to them.
“MRI scans can be an uncomfortable and daunting experience for patients, so anything we can do to make it an easier process is really positive.
“So far, this shortened MRI scan has been tested at one specialist centre with one type of MRI scanner, so more research is needed to make sure this works across different types of scanners and a diverse range of people. We’re hugely encouraged by this progress and eager to see how it continues.”
Professor Nick Fox, Professor of Neurology and Director of the Dementia Research Centre at the Institute of Neurology, University College London, said: “As more treatments that can slow or change the course of dementia are being developed, it’s important to make sure MRI scans are available to everyone. This is because people living with dementia often need an MRI scan as part of their diagnosis before they can access these treatments.
“To help make this possible, our team carried out the first study looking at how new imaging techniques –called parallel imaging – could speed up MRI scans in clinics. Their goal is to move closer to a future where every person with dementia can get a diagnosis through a scan.”
The team will now build on their early results by making sure the approach works across different types of MRI machines, so it can benefit as many hospitals and clinics as possible.
The residents and staff at Elm Bank care home in Kettering were delighted in welcoming the Seventhday Adventist Church choir to their home who filled the air with beautiful sounds.
A group of children adults and children from the congregation visited the residents, providing a truly uplifting morning of songs and spiritual fellowship. The choirs beautiful voices brought smiles to every face, and the residents thoroughly enjoyed the heartfelt performance. The children in particular were a delight, their sweet voices adding a special touch to the event. Afterward, the children personally handed out beautiful, handcrafted cards and flowers to each resident. The cards made with care and creativity, served

as a tangible reminder of the day’s warmth. Tina, Activities Co-ordinator said, “The visit was a powerful reminder and an example of the importance of faith and spiritual activities within a care home setting. These moments of connection and joy are invaluable, providing not just entertainment but a deeper sense of peace and community.
The Seventh-day Adventist Church’s generosity and compassion created a day that will be remembered by both residents and staff.” ur varied life enrichment programme keeps residents active, and provides a daily choice of engaging physical, mental and spiritual activities tailored to residents’ interests and abilities.
Croner-i was founded in 2017 as a proud part of the Peninsula Group. Since its beginning, it has supported thousands of care providers across the UK to stay compliant with Care Quality Commission (CQC) requirements and wider regulatory obligations, setting a standard in the industry.
Through their Navigate-Care platform, Croner-i specialises in providing practical, accessible and easy-to-understand guidance that enables care services to exceed their compliance responsibilities. From residential care homes, and domiciliary care agencies to supported living providers and other care services, thousands of care providers rely on Croner-i’s resources to maintain quality, safety, and best practice across their operation.

“We understand that compliance can be a challenging and time-consuming process for care providers,” said Andrew Murphy, Head of Content at Croner-i. “Our mission is to take the complexity out of CQC and regulatory requirements, giving providers the clarity and confidence they need to deliver outstanding care.”
With Croner-i’s Navigate-Care platform, care services have access to a comprehensive library of policies,
toolkits, and expert guidance written by industry and care specialists. This includes practical step-by-step advice on preparing for CQC inspections, meeting the new Single Assessment Framework (SAF) and implementing robust quality assurance processes.
Being part of Peninsula Group allows Croner-i to benefit from decades of experience in employment law, HR, and business compliance. This ensures the advice and support given is both legally and operationally practical.
With the care sector under increasing scrutiny and public pressures, Croner-i remains committed to empowering providers with the tools they need most, to operate efficiently, protect service users, achieve inspection success and grow their care service.
Look out for more details from Croner-i in the coming weeks.
For more information about Croner-i Navigate-Care, get in touch with the partnership team at partnerships@croneri.co.uk.
According to data from carehome.co.uk, there are approximately 441,479 people residing in care homes across the UK.
For these individuals, the supported, structured environment of a care facility affords them a degree of independence and autonomy, alongside the medical and professional assistance needed to lead a healthy, safe, and fulfilling life.
Yet care homes are not without risk. Research suggests care home residents are three times more likely to experience a fall compared to those living in their own homes. Fortunately, advancements in technology, engineering, and facility design are actively tackling these risks, increasing the safety for those living in supported environments.
Pinpoint’s P2 alarm system is one of these solutions.

Enabling care home residents to summon professional support instantly, the Pinpoint System establishes a clear line of communication between residents and care staff.
By pressing a button on a Patient Call Button, the user alerts staff members to the need for help and the exact location of an active call. This information, displayed on a staff communication device, elicits an immediate response to deliver the required support.
For individuals more vulnerable to falls or accidents, the Pinpoint System ensures that medical assistance is readily available, offering reassurance to care home residents and their families that help is always at hand and that high-risk incidents are handled efficiently.
On a day-to-day basis, the Patient Call Buttons are used by residents in need of extra assistance, such as when using the bathroom, to get out of bed or to access certain rooms within the facility. In this way, the Pinpoint System gives individuals a greater degree of control over their routine and avoids the need for 1-1 supervision, enhancing their quality of life.
The Pinpoint Patient Call Buttons come in various forms, including Wrist PITs, which are worn on the wrist of the individual, and wall-mounted alarms. Wander Leads of up to 2 metres in length can also be plugged into wallmounted alarms to allow resident with limited mobility to activate the alarm from their bed or armchair.
Biomaster technology provides 24/7 antimicrobial protection for all devices, preventing the spread of bacteria in care facilities, while an Ingress Protection rating of 67 allows Patient Call Buttons to be installed in bathroom and kitchen facilities where residents may be more vulnerable to slipping.
The presence of the Pinpoint System gives care home residents the chance to maintain a level of independence, while being safe in the knowledge that professional assistance can be accessed quickly and easily. This balance between site security and individual autonomy instils residents and their families with confidence that support is always available, and the peace of mind that the wellbeing, safety and health of the individual is the care home’s top priority.
Please see the advert on the facing page or visit www.pinpoint.ltd.uk
By Nikki Walker - CEO of QCS, an RLDatix Company (www.qcs.co.uk)

The social care sector stands at a turning point. With rising demand, increasing regulatory scrutiny, and ongoing staffing pressures, providers are being asked to do more, with less. In this environment, the way forward isn’t just about working harder it’s about working smarter.
One of the most transformative shifts on the horizon is the move towards truly integrated care systems: digital platforms that bring together compliance, care planning, risk management, training and quality monitoring in one unified place. More than just a convenience, this integration is fast becoming essential.
Currently, many providers juggle multiple systems or rely on a mix of digital tools and paper-based processes. Information is scattered. Teams duplicate effort. Vital data goes unnoticed. The result? Frustration, inefficiency and risk.
A connected system solves this by creating a single source of truth, where care delivery and compliance are not just stored, but actively linked. Changes in a policy can automatically update associated risk assessments. Notes in a care plan can prompt training needs. Audit trails are clear and accessible. For staff, it means less time on admin. For managers, better visibility. For individuals receiving care, more consistent, safer support.
Adding artificial intelligence (AI) into the mix elevates this even further. AI can help spot patterns in care records, prompt best practice actions and reduce the burden of documentation. Crucially, AI isn’t there to replace human decision-making it’s there to support it. By giving frontline teams real-time, intelligent guidance, it helps ensure nothing is missed and quality remains high.
Of course, technology alone isn’t enough. These systems must be built on deep sector knowledge and shaped by those working in care. Platforms like QCS, for instance, combine expert-backed content with intelligent tools to provide not just data, but insight. It’s this fusion of trusted information and digital innovation that’s beginning to change how care is delivered.
But a connected future is about more than software. It’s a cultural shift towards a care environment that is proactive rather than reactive, where data drives improvement, and where teams feel confident and supported.
In a sector where every moment counts, integrated systems offer more than efficiency, they offer the chance to focus on what matters most: people. When technology works seamlessly in the background, it frees carers to do the deeply human work that technology can’t replicate.
The future of care is not just digital. It’s intelligent. And most importantly, it’s integrated.
To see how QCS are integrating care planning, rostering. audits, mock inspection, surveys, training, compliance, dementia care and more into one integrated system backed by AI technology, follow the link. www.qcs.co.uk/what-we-do/

Residents at a Chippenham home were delighted when they saw a pair of furry alpacas visit their home.
MHA The Fairways welcomed Caramac and Liquorice, a pair of Alpacas from Alpaca Adventure based in Dorset.
The pair were accompanied by their handler and owner of Alpaca Adventure, Wendy Williams.
The home tends to arrange animal visits for residents on a monthly basis, but this is the first time they have had alpacas visit the home since the pandemic.
The pair spent their time surrounded by residents and going for a stroll around the home.
MHA The Fairways provides residential and residential dementia care for 60 residents.
Tamara Eggleston, activity coordinator said: “Our residents love animals and animal visits in general are always a big hit with them.
“We are always planning different types of animal visits and decided to go with alpacas.
“From the moment they saw the alpacas they were all very excited and loved meeting and stroking them.
“Some of the residents were a little surprised, but in a good way.
“The alpacas brought so many smiles, laughter, and cuddles, making it a truly memorable day.
“It was wonderful to see the joy on everyone’s faces as they spent time with these gentle animals.
“The alpacas were really well behaved and gave us no issues or accidents!
“We are definitely going to bring them back for another visit, maybe later on in the year as we want to explore other options and keep a nice variety of visits for our residents.”

Residents at HC-One’s Kirkwood Court Care Home in Kenton, Newcastle upon Tyne, have launched their very own walking club, making the most of the beautiful weather by enjoying time outdoors together.
The group recently set off for a gentle stroll around the local park, where they took in the scenery, enjoyed fresh air, and spent quality time chatting with each other and colleagues who accompanied them. The residents especially enjoyed watching children play in the park, which brought smiles all around.
One resident even suggested that next time the group could bring along a picnic to enjoy together in the park. The idea was warmly welcomed, as residents expressed how much they valued both the company and the chance to be out in nature.
Gladys Duffy, a resident at HC-One’s Kirkwood Court Care Home, shared: “It was nice to get some fresh air and chatting with others whilst sitting in the park.”

The walking club not only offers residents the opportunity to stay active but also encourages meaningful social interactions and a stronger sense of community. The initiative has been well received by residents, families, and colleagues alike, and there are already plans to make the walks a regular activity.
Lauren Proctor, Wellbeing Coordinator at HC-One’s Kirkwood Court Care Home, shared: “It was wonderful to see our residents enjoying the sunshine, chatting together, and appreciating the simple joys of being outdoors. Activities like these are so important for wellbeing, and we are delighted that the walking club has brought so much happiness already.”
HC-One’s Kirkwood Court Care Home is proud to continue offering opportunities that enrich residents’ lives and help them stay connected with both nature and the local community.
To learn more about Kirkwood Court Care Home or other HCOne homes in your area, visit: www.hc-one.co.uk/carehomes.

SEE US ON STAND J20 AT THE CARE SHOW
A SPONSORED walk turned into a nostalgic journey for Thornaby care home residents – when they pounded the pavements to raise funds.
A group of residents, staff, and their families from Mandale House Care Home covered more than four miles in a loop to the Tees Barrage and back for the fundraiser.
From the care home, on Acklam Road, they walked north towards Stockton Riverside College and then onwards to Tees Barrage International White Water Centre, with a stop at The Talpore Beefeater along the way. The journey took the team over three hours and raised £330 for the residents’ fund – which contributes towards activities and outings for those living at the care home.
Phillip Thornton, 70, was among the residents who took part. He said: “It’s been a trip down memory lane, walking past the places where I grew up, and up to the new areas of Thornaby that have changed over the years.” Jean Brand, 70, also joined in the walk, pushed along by the staff team, which

included home manager Anita Clarkson, deputy manager Donna Clayton, care assistant Susan Chapman, and kitchen assistant Carol Lewis. Anita’s four-year-old grandson, Brooklyn, also took part in the challenge.
Donna said: “It was a lovely walk and it was a nice day. The sun was on our side and shone all the way there and back.
“Our residents Jean and Phillip thoroughly enjoyed the stroll, the sunshine and particularly the frothy coffee at the pub, when we took in the sights, watching canoeing on the river and dogs having their daily walks.
“The staff said it was a lovely walk, just what was needed, and we’re all already busy thinking of the next adventure out with residents – maybe a train ride to the beach.
“We’d like to thank everyone who sponsored us. We raised an amazing amount of money for our residents’ fund, which will make a big difference to the experiences we can offer – from day trips and entertainment to little treats that brighten our residents’ days.”
Resident Graham, at Hickathrift House located in Marshland St James, loves nothing more than visiting the coast for fish and chips. He often reminisces about taking the children and grandchildren to Hunstanton and of course tasting the local cuisine while walking along the promenade, so staff at the home made his wish a reality through their ‘Post a Wish’ initiative proving the old adage, it’s never too late.
Hickathrift House ‘Post A Wish’ initiative helps residents complete their lifelong dreams, from going ice skating to meeting a pony. In 2024 the home successfully granted 30 wishes for residents and so far in 2025 have granted 16 wishes and hopes to grant even more. Graham’s wish will make the 20th wish granted this year.
Graham has lived at Hickathrift House for less than a year and is beloved by staff and residents alike. Staff at the home were delighted to be a part of making his dream come true, as they knew how much it meant to him, and they all wanted to be there to see the smile on Graham’s face when his dream was realised. Staff discussed with Graham some of his favourite activities to do at Hunstanton and discovered the Sea Life Centre was always a favourite. Together the staff arranged a visit with the team at the Sea Life Centre

Husnstanton, including a tour of the facilities. The staff at the Sea Life Centre surprised Graham with an extravagant opportunity to feed the seals.
Afterwards they enjoyed a scrumptious fish and chips, Graham’s favourite. Graham was also accompanied by friends and staff, who were there to witness this momentous occasion and listen to his memories.
In response to this beautiful surprise, Graham said: “I was on the verge of tears. It is such an amazing feeling to know that such a loving group of people care so much about me that they helped me to live out a dream – and I didn’t even ask.
The Sea Life Centre has changed for the better but it’s clear the staff still know their stuff and the fish and chips tastes better than ever.”
Staff from the Sea Life Centre said: “It was a pleasure to be part of Graham’s “Post a Wish” dream”.
Paula Melerski General Manager at the home, said: “We believe that every moment is worth cherishing. We want everyone we care for to know how important they are to us here at Hickathrift House.
It is testament to the hard work and dedication of the team here in making our residents’ dreams come true. It was fantastic to see how happy Graham was –and the staff loved being a part of this as well.”
A resident at an Altrincham home went on a trip down memory lane as she visited a sunflower trail.
Sue Rowe lives at MHA Handsworth and visited Dunham Massey Farm, in Dunham Massey.
Sue lived in Dunham Massey for more than 50 years before moving to MHA Handsworth in April.
She remembered going for walks around the trail with her 2 children, Lizzie and Louise when they were young children.
Sue spent time strolling round the trail and admiring the sunflowers and finished the day off with a visit to the ice cream shop onsite, where she had her favourite, chocolate ice cream.
MHA Handsworth provides residential care for 43 residents Charlotte Fowke, activity coordinator who accompanied Sue said: “Sue is an avid gardener who enjoys spending her time in our own garden, so while the weather was on

our side we enjoyed a trip to the sunflower trail.
“The visit brought back a lot of happy memories which Sue was very happy to share with me.
“Sue recalled how she used to walk around Dunham Massey with her children and spoke of picnics that they enjoyed with family.
“She also remembered walking down the canal and she had a huge smile on her face throughout the trip.
“To cool off from our walk we stopped in the farms café where they sell an array of flavours of homemade ice cream.
“Sue enjoyed her favourite, chocolate which had real chocolate chunks to Sue’s surprise.
“She enjoyed spending time in the shade watching other visitors enjoying their visit and watching the world go by.
“It was a lovely trip and one that we both really enjoyed.”
The team at Rosedale Court Care Home, part of the Runwood Homes Group, came together to celebrate the incredible birthday of much-loved resident Ivy Smith, who turned 102 years old.
The Lifestyle Team arranged a lovely party on the top floor of the home, where Ivy’s friends, carers, and fellow residents joined her. There was music, dancing and plenty of hugs. The team also presented Ivy with balloons, flowers, thoughtful gifts, and of course a birthday cake.
Everyone joined in singing Happy Birthday and She’s a Jolly Good Fellow to mark the special occasion.
The day was made even more memorable by a visit from seven-year-old Heath Chatern, who lives next door to Rosedale Court, and has a very special bond with Ivy. Heath surprised Ivy at her party, delighting her with a dance as they held a
giant balloon together. Ivy commented on the day: “I’ve had a lovely day, thank you so much for organising my special party. It was wonderful that Heath came to see me too. I am a very lucky lady.”
Heath Chatern (age 7) said: “Thank you for letting me come and see Ivy for her birthday today. I hope she liked my dance at her party! I had a lovely time and can’t believe she is 102!” Louise Healy, Lifestyle Lead at Rosedale Court,, said:
“Reaching the age of 102 is an incredible achievement, and Ivy is a truly remarkable lady who still loves to party and share stories about her life. It was important to us to make this day as special as possible for her, surrounded by friends and with a wonderful surprise from Heath, who means so much to her.”



Scott Hulin, a Mental Health Nurse at Sanctuary Care’s Trewartha Residential and Nursing Home in Carbis Bay, Cornwall has scooped a prestigious nursing award.
Scott was crowned winner of the Social Care Nurse of the Year Award at Cornwall Council’s Proud to Care Awards recently.
This esteemed award recognises nurses in adult social care who demonstrate exceptional clinical care and leadership.
Scott’s holistic approach sets him apart, deeply connecting with residents by understanding their life stories, wellbeing, and emotional needs.
Scott, who has worked at the not-for-profit home for two years said:
“I feel privileged and grateful to have been even nominated for this award.
“I believe that we can’t achieve much in healthcare on our own, and this award belongs to the whole team at Trewartha.
“Thank you to my home manager Julia Tyldesley for her support and leadership – and thank you to all of my amazing colleagues who work so hard every day.
“We get many opportunities throughout each day to enrich someone’s life, and that’s so important.”
Joining Scott at the ceremony was Cat Rowe, Care Assistant at Sanctuary Care’s The Green Residential Care Home in Redruth, who was proud to be named runner up in the Care Worker of the Year Award. Congratulations to both!
Residents of HC-One’s Foley Grange Care Home in Kidderminster, Worcestershire, enjoyed a fantastic afternoon of music, laughter, and nostalgia when they were warmly invited to Berrington Court for a lively Elvis tribute performance.
The event brought together residents from both care homes to celebrate the timeless music of the King of Rock ’n’ Roll. The tribute artist delivered an energetic performance filled with familiar hits, toe-tapping tunes, and plenty of opportunities for residents to sing and dance along.
The atmosphere was one of pure joy and community spirit, as the room filled with smiles, laughter, and the sound of Elvis classics. For many residents, the afternoon stirred fond memories and a wonderful sense of togetherness.
The visit highlighted the importance of music, friendship, and social engagement in supporting residents’ wellbeing. Everyone left looking forward to more community events like this in the future.

CareZips® Classic are patented, easy dressing unisex adaptive pants designed for older and disabled people suffering with problems associated with continence, mobility, mental function and cognition. Suitable for persons living in care institutions, receiving care at home or living independently at home, CareZips® Classic enable people to dress themselves or with assistance from carers.
CareZips® Classic feature patented 3-zipper system, which opens the front of the pants from the waist to the knees for quicker access during toileting, continence pads changes and personal hygiene. The forward positioning of the two side zippers lessens pressure on sensitive hip areas, helping to eliminate discomfort. The third zipper facilitates simple full frontal opening for faster more dignified diaper changes, catheter adjustments, personal cleansing and hygiene routines.

cal functionality and versatility of the CareZips® Classic, all day comfort and easy garment care.
• People dependent on assisted dressing appreciate quick easy dressing process with less stress, embarrassment and greater dignity offered by CareZips® Classic.
• CareZips® Classic offer practical gains to the carers, helping them to provide better care, whilst reducing physical efforts and saving valuable time.
CareZips® Classic are unisex, available in 6 sizes and 3 practical colours (i.e. black, charcoal and navy). Tapered fit at the ankles gives a tidy appearance. Made from breathable moisture-wicking 4-way stretchy crease-free and easy-care durable fabric, CareZips® Classic are comfortable, practical and conveniently functional.
For more information, contact Win Health Medical Ltd - 01835 864866www.win-health.com
In today’s care sector, where equipment failure can directly impact patient safety and service quality, proactive asset management is non-negotiable. Enter Assetain, Medaco’s pioneering solution designed to manage the complete lifecycle of patient-handling equipment - from first supply to planned obsolescence.

assessments, which are promptly linked to each record. This approach adds both accountability and immediate insight for stakeholders.
CareZips® Classic have many benefits for the older and disabled users and their carers:
• People dressing themselves enjoy the practi-
See the advert on page 3 for further information on Win Health’s product range.
Angloplas are a UK manufacturer who specialise in producing dispensers for the health and hygiene industry. Although these are designed to keep the workplace tidy and uncluttered they are, more importantly, built knowing the control of healthcare-associated infections (HCAIs) are a priority for healthcare providers, and who are employing a combination of infection prevention and control strategies, including hand hygiene, cleaning, training and the adoption of new technologies, to tackle the problem.

As a result, a wide range of infection control products and technologies are emerging on the market, including antimicrobial technology. Angloplas’ range of dispensers are produced in the world’s first
proven Antimicrobial PVC with silver ion technology and which is exclusive to Angloplas. This helps reduce the risk of cross infection by stopping the growth of bacteria and mould and works continuously for the lifetime of the product, reducing levels of bacteria such as MRSA, E Coli, Legionella, Salmonella and mould by up to 99.99%. For non-clinical environments Angloplas has recently launched its new Budget Range of products which are made to the same exacting standards as the antimicrobial protected ones but with lower price tags. You can order Angloplas products directly from its website at www.angloplas.co.uk See page 17.
Launched in August 2025, Assetain delivers three core benefits: comprehensive asset visibility, budget-wise maintenance, and strategic replacement planning. Rather than reactively repairing faulty devices, care homes, NHS Trusts, and SEND schools can now oversee the health of all moving and handling equipment with confidence and clarity.
At its heart lies a meticulously maintained, datarich register. The programme initiates with a full audit of existing assets; each entry is ported into a dynamic system setting tailored maintenance thresholds, repair-vs-value benchmarks, and clear end-of-life triggers.
Field engineers play an essential role - capturing photographic evidence of faults and functional
Timely alerts are a standout feature. When equipment approaches “no-longer-manufactured” status or reaches its recommended service term, Assetain sends clear notifications - empowering teams to anticipate challenges before they arise. Regular updates of the full asset register ensure stakeholders remain fully informed of the condition and availability of their entire fleet.
Assetain isn’t just maintenance - it’s strategic careasset stewardship that saves time, reduces costs, and safeguards patient well-being. A smart, forwardthinking programme like this helps care providers shift from reactive firefighting to purposeful planning.
In short, Assetain elevates care facility operations into a new era of efficiency and confidence - where every asset is seen, scheduled, and systematically sustained.
www. medaco.co.uk/solutions/assetain/
Consort Claudgen now offers Wi-Fi-enabled low surface temperature heaters that can be controlled through a digital control panel on the heaters or the Consort Connect app. Features include a 7-day timer with 24 daily heating periods, a lock function, open window detection, custom automation, and energy consumption statistics.
Additionally, LST heaters with Wi-Fi and occupancy sensor have a self-learning control ability which uses inbuilt occupancy sensors to detect and learn a

user’s weekly presence in a room. It then creates a heating schedule and automatically warms the room according to the detected or predicted occupancy. When the space is unoccupied, the heater will conserve energy by switching to a setback temperature or frost protection mode. Consort's website also offers BIM objects for download.
See page 17 or 01646 692172 | sales@consortepl.com | www.consortepl.com

The Care Show Birmingham 2025 once again stood as a beacon of innovation and excellence in the care sector. The twoday event attracted care professionals from across the country, who gathered to explore the latest developments in care delivery, technology, and best practice. Attendees engaged with a comprehensive educational programme covering critical topics including regulatory compliance, design innovations, and care management strategies.
A highlight of this year's show was the third annual Care Show Thirty Under 30 Awards, which recognised 30 exceptional young professionals making significant contributions to the sector.
From care workers who go the extra mile every day, to innovators finding new ways to deliver support, to advocates fighting for a stronger voice for the sector – these 30 individuals show just how much talent and heart the next generation is bringing into care.
Adam Camel, Show Manager, Care Show Birmingham said:
The Care Show Thirty Under 30 awards is one of the highlights of Care Show Birmingham. It’s so inspiring to see the energy and compas-
sion that these young professionals bring to social care. They remind us all why this sector matters so deeply, and it’s a privilege to celebrate their achievements on stage this year.
The Care Show Thirty Under 30 Class of 2025:
Adam Batey, Operations Manager, Dale Care
Amie Elson, Care Manager, Hengoed Park Ltd
Annie Aston, Lead Activities Coordinator, Hengoed Park Ltd
Ayana Mohamed, Director, Standard Care Ltd
Bailey Greetham Clark, Founder, Be Great Fitness
Callum Pearce, General Manager, Oyster Care Homes
Chloe Hart, Deputy Manager, Shores Homecare Ltd
Chris Brown, Registered Manager/Business Development
Manager/Director, Alternative Care Ltd and Auralis Homes
Colby Ebsworth, Senior Support Worker, Ryde House Group
Deanna Murray Wiggins, House Manager, Aspects Care
Dominic North, Client Liaison Manager, Signature Senior Lifestyle
Dr Jade Okene, Operations Director – Service Transformation & Partnerships, Passion Tree Care Services
Gemma Bell, Senior Carer, St Michaels Homes Ltds
Gemma Hebron, Deputy Manager, West Park Care
Grace Evans, Managing Director, Salveo Care Ltd
Isaac Hemper, Home Manager, Ryde House Group
Jasmin Cartwright, Senior Carer, DKL Healthcare Ltd
Jodie Ebsworth, Home Manager, Ryde House Group
Kara Cave, Registered Manager, Unique Senior Care
Katie Bedwin, Clinical Educator, Superior Healthcare
Katie Oerton, Business Manager, Forevermore Care
Katy Hague, Chief of Staff, Oyster Care Homes
Kush Patel, Deputy Manager, Cherrytree Care Home/Kara Healthcare
Olivia Walsh, Branch Manager, Agincare
Rhiannon Corns, Deputy Manager, Lavender Hills Care Home
Sean Gilfillan, Care Coordinator, Unique Senior Care
Sinead Nealon, Pharmacy Manager, Kara Healthcare
Summer Smith, Registered Manager Trinity Homecare Limited
Taylor Turner, Service Lead, Forevermore Care
Zachary Dawson, Operations Director, Bloom Care Solutions
The exhibition floor featured both established sector suppliers and emerging companies, providing attendees with opportunities to discover new solutions and strengthen industry connections.
The event's continued growth and positive reception from delegates reinforces Care Show Birmingham's position as an essential fixture in the care sector calendar. Organisers have confirmed plans to build on this year's success when the show returns in 2026.Show Manager, Adam Camel, commented after the event:
“Care Show Birmingham was an all-around success this year, with stellar feedback from the visitors and exhibitors alike - I could not be prouder of the Care Show team for putting together another fantastic show. It's wonderful seeing the entire care community come together year after year in such a joyous and celebratory fashion. I can't wait to do it again next year!”
Introducing Access Smart Notes for Care Planning.
We’re excited to introduce the upcoming release of Access Smart Notes - A new AIpowered tool designed to reduce admin, saving time and money for care providers like you.
Smart Notes helps you create accurate, detailed notes, using AI to write up forms in moments and and deliver them directly into Access Care Planning. That means less time writing, and more time with the people who matter most.
Access Smart Notes key features and benefits:
• Save thousands of pounds every year on Care Assessments without a drop in quality.
• Capture detailed notes quickly and efficiently in the moment.
• Reduce errors and missed details with templates customised to your service
• Integrated with Access Care Planning for real-time updates saving hours of admin time.
• Built-in AI accuracy to streamline the documentation process to reduce risks and improve the quality of your notes
• Full audit trail for peace of mind and transparency Visit www.theaccessgroup.com

Since 2008, Satellite Finance has been a trusted commercial finance broker specialising in funding solutions for care homes and healthcare providers. Based in Newport, Wales, Satellite Finance has a range of tailored business finance services from asset finance, business loans, and mortgage funding to support care home acquisitions, refurbishments, and equipment purchases.
If you’re looking for Asset Finance to help grow your business, new equipment is a must. Satellite Finance can help you to get all the equipment you need, without making large dents to your cashflow. With Asset Finance you don’t have to pay for everything upfront, you can spread the cost of your equipment over the period of time its expected to be used for which can be from 12-72

months, allowing you to spend more money on higher standard equipment without feeling the economic pinch.
Perhaps you’re looking for a loan for a new building, or to make a refurbishment in a care home or surgery? Satellite Finance works with you to choose the best loan for your project. Choose from either a Business, Professional, Personal, or Corporate & VAT loan, and because Satellite Finance has access to over 40 specialist lenders that have facilitated over £100 million in funding for more than 4,500 clients, you know you’re in good hands.
For a Mortgage Loan, Satellite Finance can help you to request a loan for anything between £50,000 – £40 million. With rates starting from just 2.25% above Bank of England base rate, your repayment period




can be anywhere between 5 and 30 years. Unlike other finance companies, Satellite Finance’s terms won’t feel like a burden, as they’re both competitive and flexible, ensuring you get an arrangement that is affordable and convenient for you. Having close relationships with over 40 high street banks, challenger banks, and regional lenders all over the UK, Satellite Finance is experienced and up to date with the best lenders who offer the best rates to the healthcare sector.
Every day, care organisations are working tirelessly to deliver essential support in the face of growing needs and rising costs. However, too many providers are stuck balancing tight budgets, having ‘just enough’ to stay afloat. The hard truth is, just enough isn’t enough—not for the providers, not for the employees, and certainly not for the clients who depend on them.
Rising operational costs—from wages and the Fair Pay Agreement to energy bills—compound historic underfunding and financial pressures. And demand for care continues to increase, creating a widening gap that organisations are often forced to fill with limited resources.
Providers then end up in survival mode, unable to invest in improving their services for today and the future.
THE NEED TO RETHINK FINANCIAL STABILITY
Care providers need to have healthy finances in social care, and that doesn’t come at odds with delivering compassionate care.
A financially strong organisation has the breathing room to improve services, retain employees, and innovate to make a meaningful difference to the lives of people they support. And having this financial security means providers can actually plan for the future rather than constantly reacting to the present.
BENEATH THE SURFACE
Social care organisations face a web of financial intricacies. Local authority
Fran
discusses how financial pressures continue to challenge social care providers.
support often comes with layers of red tape. Managing aged debt and resolving invoicing errors take a significant amount of time that few organisations can spare. Regulation and compliance require meticulous reporting, and the sheer volume of admin work to manage all these leaves teams stretched thin. At the same time, there’s an expectation for providers to keep doing more. But without the right tools and systems in place, these compounded financial struggles threaten to overwhelm this indispensable sector.
Social care providers aren’t just keeping their organisations alive; they’re safeguarding the wellbeing of countless individuals and families.
Providers need to be able to prioritise long-term financial resilience. And part of this means having the tools—including robust financial management softwaresimplify manual processes, optimise resources, and reduce inefficiencies.
By championing financial sustainability, we’re creating conditions where employees can thrive, where clients receive the quality of care they deserve, and where the sector can confidently meet future challenges.
Find out more at: www.oneadvanced.com/ai
See the advert on the facing page.
We were excited to be heading to the Care Show in Birmingham on 8–9 October bringing something brand new with us.
At this year’s event, we launched the Data Policy Builder, a powerful new tool designed to make data protection policies simple, practical, and meaningful for your organisation. Too often, policies sit on a shelf, written in complex language that no one reads. The Data Policy Builder helps you create living documents that reflect your service, speak to your staff, and actually shape day-to-day practice.
By guiding you step by step through the process, the tool ensures your policies are DSPT-compliant and tailored to your unique risks and needs. Whether you run a single care home, a homecare service, or a larger group, this tool will help you write policies that your team can understand and use – supporting safer care and better data security. LIVE DEMO – DATA POLICY BUILDER

The Care Show offered a first look at the Data Policy Builder in our live demo session. We’ll be focusing
on Bring Your Own Device (BYOD) policies, an area many care providers struggle with. You’ll learn:
• The risks of staff using personal devices for work
• What should be included in a robust BYOD policy
• How the tool can generate a clear, easy-to-read document for you – in minutes We’ll also be sharing which other policies we’ll be adding to the tool in the future, so you can start planning ahead.
DROP-IN HUB – YOUR QUESTIONS ANSWERED
Throughout the Care Show, the Digital Care Hub team ran a drop-in hub where you could ask all your questions about digital technology, data protection, and cyber security. Whether you need help with the Data Security and Protection Toolkit (DSPT), want advice on cyber security risks, or just want to sense-check your approach to data sharing, we’ll be there to support you.
For further information, please see the advert below.


Sensore launches a smart pressure ulcer prevention system, a breakthrough technology combining a smart fabric sensor mat with an intuitive app and powerful AI analytics.
Today’s best practice is reactive: manual checks and frequent repositioning. Sensore flips the model - continuously monitoring pressure distribution in real-time and providing simple preventative alerts, so users stay protected while easing the daily vigilance demand on users and carers.
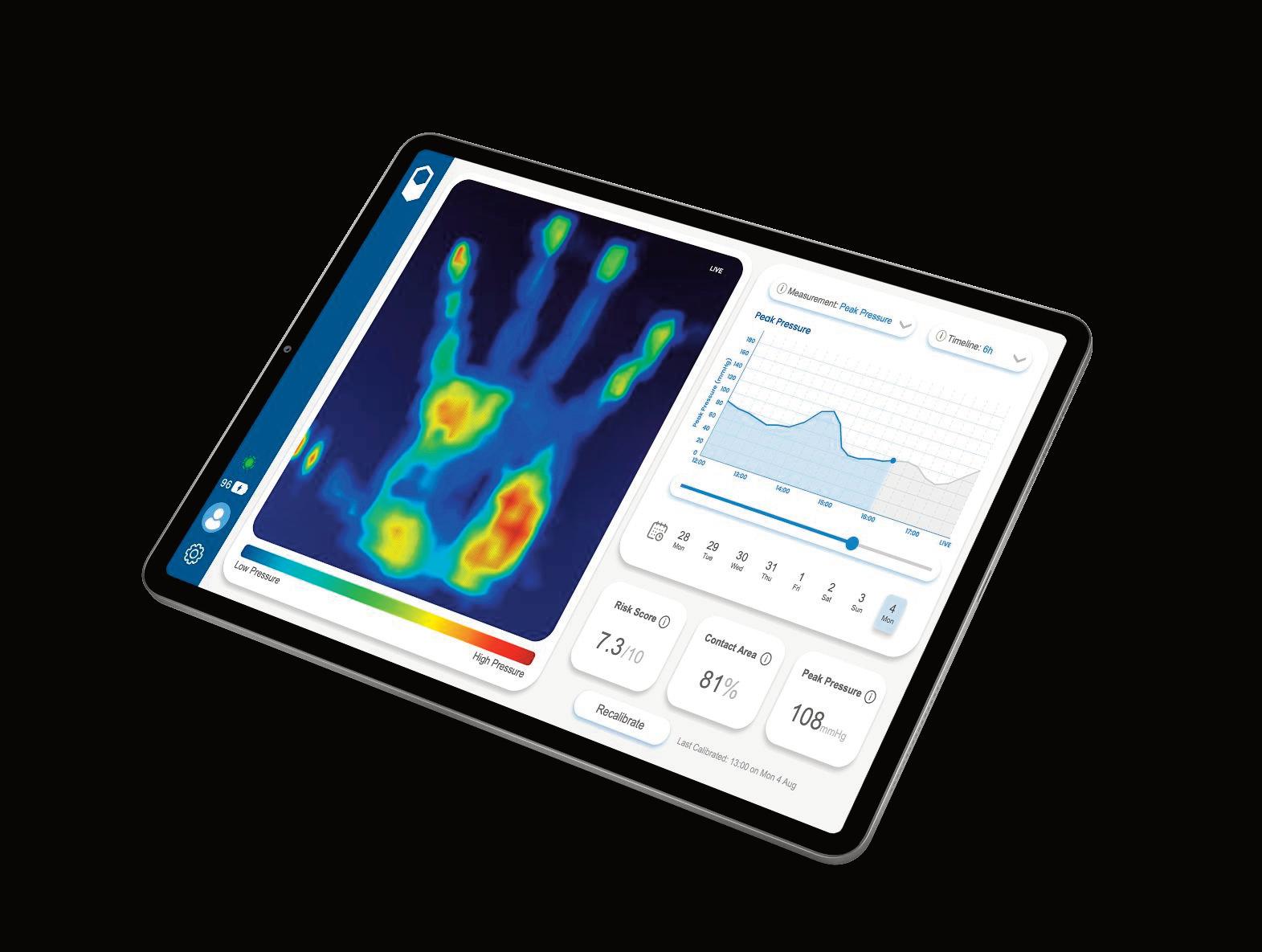

A personal early-warning system that integrates seamlessly into any wheelchair or bed, Sensore is built for elegant simplicity - restoring peace of mind for wheelchair users and supporting higher-quality, more
consistent care. For care providers, Sensore can help standardise prevention workflows and contribute to meaningful cost savings, while building a unique dataset to advance pressure-injury research.
Sensore is supported by clinical experts: "We believe Sensore’s continuous pressure monitoring will have a transformational impact on our ability to prevent and manage pressure ulcers effectively, while driving measurable improvements in patient care quality" - NHS Consultant Clinical Scientist Specialist in Clinical Biomedical Engineering
Visit www.sensore.health for more information, to sign up for early access and book a free demo.
For over 60 years, Fowler UK has been proud to support the care sector with dependable commercial laundry and catering equipment, backed by expert service that puts people first. As a family-run business, we understand the pressures care providers face, and we’re committed to delivering solutions that keep vital operations running smoothly.

From supply and installation of equipment, ongoing servicing and repairs, detergent packages, right through to our in-house CAD design team, we offer a ‘one-stop-shop’ solution for all of our clients laundry and kitchen facilities.
Reliability and customer service the heart of what we do. Our fast response times and high first-time fix rate mean care providers can trust us to minimise downtime and keep essential services running without interruption. By stocking a vast range of manufacturer parts on our vans and in-house, we’re able to resolve issues quickly and effectively.
“Supporting the care sector has always been central to our business,” said William Fowler, Director at Fowler UK. “We know how important reliable equipment is for both residents and staff, and we’re proud to play our part in helping care homes provide safe, efficient, and welcoming environments.”
With a proven track record, family values, and a commitment to service, Fowler UK remains a trusted partner for care providers nationwide.
We’d be delighted to discuss how Fowler UK can support your facility. Visit our stand - G02 at The Care Show, NEC, on 8–9 October, or contact our team today to find out more.
Beyond equipment sales, we support care facilities with comprehensive compliance and maintenance services such as gas safety inspections, preventative maintenance visits, duct cleaning and kitchen deep cleaning. This all-in-one approach provides peace of mind for our customers, ensuring they can focus on delivering high standards of care while we take care of the rest.

Each year Skopos launch new fabric collections, developed specifically with Care interiors in mind. Specialists in key attributes which help keep homes looking fresh and stylish (soil resist, antimicrobial) interior schemes can easily be pulled together using a mixture of prints, textures and plains. Leading the way at this year’s show, Skopos will be highlighting their new range of printed designs, from the Skopos STUDIO. Available on basecloths for upholstery, bedding and curtains, the fabric choices have grown, to include a waterproof and antimicrobial velvet upholstery and a textured woven upholstery. Designs from the STUDIO are split into different categories, including stripes, florals, geometric and textures.

Skopos can offer a fabric-only service or a full service; with site measure, product manufacture and installation. The Skopos team produce
approximately 25,000 made-up items each year, including bedthrows, cushions and pairs of curtains, all manufactured by a highly-skilled team of machinists, cutters and pattern makers; items that are delivered and installed into different contract environments.
As with all Skopos prints, the lead-times are under one week and everything is produced locally, in Yorkshire.
Skopos also offers a Bespoke design service, for statement interiors that require something different. Our design team will work alongside you to develop ideas which can make your caring interior personal, branded and unique. For samples of any of our collections visit www.skoposfabrics.com
PASS by everyLIFE Technologies, UK and Ireland’s leading digital care management platform, will be showcasing its award-winning software at this year’s Care Show in Birmingham.

Used by over 1,200 services and supporting more than 85,000 care professionals every day, PASS brings care planning, medication management, rostering and finance together in one simple system. The platform helps providers save time, reduce risk, and improve compliance - giving care teams more time to focus on the people they support.
Visitors to the Care Show will also be able to see PASSgenius™, the suite of AI-powered insights now
built directly into the platform. PASSgenius™ analyses care notes and rostering data to highlight risks, changes, and trends that may otherwise be missed. From punctuality dashboards to health note summaries, it turns everyday information into clear, actionable insight. Robin Batchelor, CEO at everyLIFE Technologies, said: “The Care Show is always a fantastic opportunity to meet providers, share ideas, and demonstrate how digital tools can make a real difference to quality of care.” For more information, visit www.everylifetechnologies.com.


The NHS Long Term Plan is reshaping healthcare to make it more personal, preventative, and accessible. At the heart of this transformation are three strategic shifts: delivering more care in the community, embracing digital solutions, and focusing on prevention rather than treatment. For patients and carers, these changes mean more support at home, fewer hospital visits, and better tools to manage health.
One innovation helping to make this vision a reality is Evondos—an automated medication dispensing service and virtual care platform designed to support safe, timely, and consistent medicine use at home.
SUPPORTING INDEPENDENCE AND SAFETY
Evondos Anna Medicine Dispensing Robot is installed in the patient’s home and dispenses pre-packed doses at the right time. It provides spoken instructions and visual cues, making it easy to use for people of different ages and abilities. If a dose is missed, the medication is stored safely and securely inside the device until a carer or healthcare professional can follow up. This is especially important for patients with time-sensitive or multi-dose medication schedules, such as those managing diabetes, Parkinson’s, or heart conditions. Evondos ensures that every dose is delivered as prescribed, helping prevent complications and hospital admissions.
PEACE OF MIND FOR CARERS

For carers—whether family members or professionals—Evondos offers reassurance. You don’t need to be present for every dose, and you’ll be notified if a dose is missed. This reduces stress and allows carers to focus on other aspects of support, knowing that medication is being managed reliably.
Evondos also supports virtual care through its built-in two-way video camera, allowing care professionals to check in with patients remotely. This adds a personal touch to digital care and helps maintain strong relationships between patients and their carers.

Care home residents, new staff and visitors can all benefit from clear way-finding signage, which is why the Care Quality Commission places great importance on a well thought out signage scheme – especially where memory care needs demand specialist input. Add the need to reflect a group's branding objectives whilst working within interior design guidelines, and the challenge for managers tasked with sourcing signage is knowing who to call.
With nationwide coverage, Taylor and Pickles have a reputation for well thought out signage schemes which effectively and discreetly direct people around care homes for many of the UK’s leading care providers.
Starting with a client’s briefing, Taylor and Pickles carry out a comprehensive site survey and develop
Evondos includes a built-in roaming cellular SIM card, which means it connects automatically—no home internet or technical setup is required. Patients don’t need to understand or manage any digital connectivity. This makes Evondos accessible to everyone, including those who are not confident with technology or live in areas with limited digital infrastructure.
TRAVEL MODE FOR FLEXIBILITY
Evondos also includes a travel mode, allowing patients to take their medication with them when away from home—whether visiting family, going on holiday, or staying in respite care. This keeps routines consistent and supports independence, even when life changes temporarily.
EQUALITY
Evondos is built with equality at its core. Its intuitive design, secure medication handling, automatic connectivity, and virtual care features make it accessible to people from all backgrounds. Whether you’re living alone, supported by carers, or part of a busy household, Evondos fits into your life and helps you stay well.
Evondos supports the NHS’s three strategic shifts by delivering smarter, safer, and more accessible care. For patients, it means more independence and better health. For carers, it means peace of mind and less pressure. With support for complex medication schedules, secure storage, travel flexibility, virtual care, and no need for internet knowledge, Evondos is helping bring the future of healthcare into everyday life.
If you or someone you care for could benefit from help with medication, speak to your local care team about Evondos. It’s a powerful solution designed with real people in mind.
See the advert on the facing page for details.
detailed design proposals. Often working with a client’s interior designers, the team at Taylor and Pickles create options for bespoke signs which provide clear directions and are sympathetic to the client’s creative concepts. This custom approach prevents signs looking out of place, or like “off the shelf” stock items.
Of course, there are times when greater visual contrast is essential. Residents with memory care needs require a bold and sometimes bright scheme which might seem heavy handed elsewhere. When the special needs of these residents are added to the brief, clients can be confident that Taylor and Pickles’s approach, guided by leading academics and their experience of helping many homes through the Care Quality Commission signage inspection process, will pay off. Often a multi-tiered approach allows signs across different zones in a development to have a cohesive look yet serve differing care needs.
Taylor & Pickles also recognise a client’s commercial needs. Timely, unobtrusive surveys – effective design and tidy installation by in-house teams make Taylor and Pickles the chosen signmaker for many of the UK’s leading care home groups.
See the advert below for details.









In the complex world of care-home medicine management, consistency and reliability are everything. From ensuring the right medicines arrive on time, to providing specialist support and training for staff, a single weak link can jeopardise the safety and well-being of residents. That is why more and more care providers are turning to Care Quality Pharmacy – a national, care-home-only distance-selling pharmacy – to deliver a true one-pharmacy solution.
CONSISTENCY AND SIMPLICITY
Running multiple homes often means juggling relationships with several local pharmacies. This can lead to variations in service levels, communication gaps and unnecessary administrative burden. By partnering with a single specialist pharmacy, care providers enjoy a unified approach across every home. Care Quality Pharmacy provides guaranteed monthly delivery dates, centralised prescription management and a dedicated Key Account Manager, ensuring that every home receives the same high standards of service.
ADVANCED TECHNOLOGY AND COMPLIANCE

Care Quality Pharmacy harnesses advanced AI-driven prescription checking and integrates seamlessly with leading electronic MAR (eMAR) systems. These innovations reduce the risk of dispensing errors and give care teams real-time oversight of residents’ medication records. The pharmacy’s robust auditing and returns collection processes support full regulatory compliance, while scheduled annual training sessions
keep staff confident and up to date with best practice.
OPERATIONAL EFFICIENCY AND COST SAVINGS
A one-pharmacy solution eliminates duplicated processes and frees up valuable staff time. With Care Quality Pharmacy’s dedicated communications team liaising directly with GPs, homes save hours previously spent chasing prescriptions or clarifying medication queries. Interim requests are handled swiftly – often the same day –and returned medicines are collected routinely, further reducing workload and waste.
A PARTNERSHIP BUILT ON TRUST
Perhaps the greatest benefit is peace of mind. Care Quality Pharmacy’s national infrastructure, experienced team and proactive approach mean care-home operators can focus on delivering exceptional care while knowing that every aspect of their medicines management is in expert hands.
In a sector where safety, compliance and resident well-being are paramount, a one-pharmacy solution is not just convenient – it is transformative. Care Quality Pharmacy brings together specialist knowledge, cutting-edge technology and a commitment to personalised support, making it the trusted partner for care homes across the UK.
See the advert on the back cover for further details.

Blended learning recognises that effective training goes beyond theory. Knowledge is important; staff must first understand the what and the why, however knowledge alone doesn’t always prepare them for the realities of a care setting. Skills need to be practised, rehearsed and refined in an environment that’s safe before they are put into practice with residents or service users. When staff build confidence through role play, simulation, and guided practice, the leap from theory in the classroom to the real world becomes less daunting. The next step is proving capability on the job. Competency assessments connect learning with practice, giving managers assurance, regulators evidence, and service users confidence in the care they receive. But learning shouldn’t end there; structured pathways that map skills to roles, prompt refreshers, and track development over time keep staff on course,
turning their training into a process of continual growth which is also aligned with Skills for Care standards and expectations set out by CQC.
The impact on organisations is clear – teams feel supported and this improves retention, which in the Health and Social Care sector is more important now than ever. Families, inspectors, and service users see a higher quality of care, and managers gain reassurance that their workforce is competent and confident. Ultimately, blended learning creates safer, kinder, and more consistent outcomes for everyone, meaning higher care standards and greater satisfaction all round.
Which is why your team deserves myAko. Blended learning is more than just an approach, it’s essential for everyone in our sector!
ww.myako.online
hello@myako.com 01202 283283





By Gemma Christie, Business Account Manager at Miele

In the care sector, operational decisions carry significant weight. Whilst frontline care rightly takes centre stage, it’s also important to remember that the kitchen plays a vital role in maintaining hygiene, supporting staff efficiency, and ensuring resident wellbeing. Among the many moving parts of the care home kitchen, dishwashing is often overlooked. This is likely because it operates behind the scenes and isn’t seen as a direct part of resident care, yet it’s a key consideration for care homes looking to provide a safe, smooth service.
With multiple meal services each day, the kitchen is one of the busiest areas in a care home. Relying on manual washing not only slows down operations but also increases the risk of hygiene lapses. That’s why investing in the right dishwashing solution is critical.
For care homes looking for reliability, hygiene assurance and longterm value, commercial solutions are the smart choice. Here are five key reasons why investing in a professional dishwashing solution can make a meaningful difference.
WHY DOMESTIC DISHWASHERS FALL SHORT
It’s not uncommon for care homes to rely on domestic dishwashers, especially when budgets are tight. But these machines are rarely up to the task. Designed for occasional household use, they struggle with the frequency and intensity of care home operations. Over time, this can lead to breakdowns, inconsistent results, and even hygiene risks. Commercial dishwashers, by contrast, are built for durability and performance. They’re tested to withstand thousands of cycles and are engineered to maintain consistent cleaning standards, even under intense pressure. For care homes, this means fewer disruptions, lower
long-term costs, and greater piece of mind.
HYGIENE RESULTS YOU CAN TRUST
It’s no secret that infection control is always a top priority in any care or medical settings, especially with residents that are often more vulnerable to illness, and where outbreaks can have serious consequences. Dishwashing equipment can help to fight against these infections and play a big role in preventing cross contamination. But only if it’s up to the job.
High-performance commercial machines, such as the MasterLine range by Miele Professional offer disinfection-grade wash cycles that eliminate harmful bacteria and pathogens. Some models also feature advanced drying systems that remove the need for manual handling, further reducing the risk of contamination. These features aren’t just nice to have, they’re essential for maintaining compliance and protecting residents.
SPEED AND EFFICIENCY IN THE KITCHEN
Care homes run on tight schedules. Mealtimes are fixed, and delays can have a knock-on effect across the day. That’s why turnaround time is a key consideration when selecting dishwashing equipment.
Modern commercial dishwashers can complete a full cycle in as little as five minutes, ensuring that clean items are always available when needed. This reduces the need for excess crockery and helps staff stay focused on resident care rather than kitchen logistics.
Supporting staff and reducing their workload
The right equipment doesn’t just improve hygiene standards, it also helps to support staff wellbeing. In a sector where recruitment and retention are constantly ongoing challenges, anything that eases the daily workload is a welcome investment.
User-friendly controls, intuitive interfaces, and automated features such as detergent dosing or drying programmes can make a real difference to staff efficiency and satisfaction. When equipment actually works with your team, and not against them, it frees up critical time and energy for what matters most, caring for their residents.
A LONG-TERM INVESTMENT
While the upfront cost of commercial dishwashing equipment may be higher, the long-term benefits are clear. Reduced maintenance,

lower energy and water consumption, and extended service life all contribute to a more sustainable and cost-effective operation. For example, Miele Professional’s MasterLine dishwashers can complete a full cycle in just 5 minutes and use as little as 5.0 litres of water per cycle, depending on the model. Their energy-efficient design helps reduce utility costs while maintaining top-tier hygiene performance. Some dishwasher manufacturers offer extended parts availability and nationwide service networks, ensuring that support is always close at hand. Miele Professional offers spare parts available for up to 15 years after production ends and a UK-wide service network with a 90%+ first visit fix rate meaning that care homes can rely on consistent, expert support when it matters most.
Dishwashing may not be the most visible part of care home life, but it’s one of the most vital. By investing in the right equipment and processes, care homes can enhance hygiene, improve efficiency, and create a safer, smoother environment for both residents and staff.
To explore how Miele Professional's commercial dishwashing solutions can enhance your care home, please visit: https://www.miele.co.uk/p/retirement-care-homes-4053.htm

In the care sector, food is more than just nutrition - it’s comfort, dignity, and a way of bringing joy to residents every day. That’s why chefs can’t afford to compromise. From flavour and safety to consistency and versatility, every ingredient has to deliver. When it comes to bouillon, Knorr Professional refuses to settle for anything less than the best and so do the chefs who use it.
Knorr Professional Bouillon is the UK’s number one bouillon brand*, trusted in kitchens nationwide for its rich depth of flavour, outstanding versatility, and chef-trusted consistency. It’s made to work hard in every service, withno allergens to declare¹ options that give chefs peace of mind when catering for residents with diverse needs. NEVER SETTLE FOR BLAND DISHES
As residents age, their sense of taste can diminish. That’s why flavour has to work harder in care - it’s not just about nutrition, it’s about enjoyment. Knorr Professional Paste Bouillon brings bold, balanced flavour that cuts through reduced senses, ensuring dishes remain satisfying and memorable.
Whether it’s used as a base, rub, seasoning, glaze, or marinade, it delivers the same consistent, chef-approved results. From soups and stews to roasted vegetables and marinades, this is one product that performs across the menu - helping chefs adapt quickly without losing quality.
NEVER SETTLE FOR UNCERTAINTY
In care kitchens, allergen safety isn’t negotiable. Theno allergens to declareoptions in Knorr Professional Paste Bouillon make it simple to create inclusive dishes without sacrificing flavour. This helps reduce the risk of cross-contamination and ensures every resident can enjoy the same great taste.
For Knorr Professional Care Ambassador Preston Walker, that confidence is invaluable:
“With ‘no allergens to declare’ options available across the range, Knorr Professional Paste Bouillon is easy to introduce into dishes that need to be suitable for varying needs and preferences,” says Preston. “It gives me peace of mind that I can create flavour-packed dishes for all residents, without excluding anyone due to allergens.”
NEVER SETTLE FOR INCONSISTENCY
Care kitchens can be high-pressure environments, where time is short and the need for consistency is constant. Knorr Professional
Bouillon’s paste format makes it easy to store, measure, and use, ensuring the same flavour profile in every batch. Its consistent yield also helps with budget control - delivering premium quality without waste.
Preston sums it up simply:

“We use the Knorr Professional Bouillon paste range for one simple reason - it delivers. Quality, flavour, consistency, and the confidence of knowing exactly what you’re going to get, every time.”
NEVER SETTLE FOR SECOND BEST
Every plate in a care home matters. It’s an opportunity to provide comfort, joy, and nourishment - and that means every ingredient has to earn its place. With Knorr Professional Bouillon, chefs can be sure they’re serving the very best in flavour, safety, and reliability. Because when it comes to care catering, settling for less is never an option.
Care home budgets are under mounting pressure. Food supply constraints, inflation, and rising labour costs are combining to create a perfect storm for operators already working to tight margins.
The British Retail Consortium’s latest survey paints a concerning picture: 85% of retailers have raised prices in response to increased costs, fuelled by rises in employer National Insurance contributions and the National Living Wage. In the catering sector, which is heavily dependent on lower-wage roles, these changes are having a pronounced impact.
The Office for National Statistics’ July CPI figures show food inflation at 4.9%, with forecasts suggesting this could reach 6% by the end of the year. According to food procurement expert allmanhall’s Managing Director, Oliver Hall says:
“Based on recent and forecasted inflation spikes, care groups may want to revisit what they have budgeted for annual food inflation for the coming months. allmanhall consistently outperform inflation with price rises lower than inflationary rates, ensuring every pound of catering spend goes as far as possible.”.

Global factors are adding further uncertainty. Extreme weather patterns are disrupting crop yields and threatening food supply chains. The resulting price volatility is not limited to raw ingredients - distribution, packaging, and processing costs are also climbing.
Faced with these pressures, some care providers may be considering outsourcing catering as a cost-saving measure. However, as Oliver cautions:
“Pause before you add a management fee on top of rising labour costs on someone else’s payroll.”
Just because you eat less, or eat differently, it doesn't mean you should settle for less.
At Food Untethered, we believe that everyone – regardless of how they eat –deserves access to real, organic, and nourishing food. Whether you are tubefed, or simply need liquid nutrition on the go, our meals are made with care, using nothing artificial and held to the highest of safety standards.
We’ve launched our first three meals: a Coconut & Banana Smoothie, a Carrot & Coriander Soup, and a Mexican Bean Stew. Each is packed with whole ingredients, made for both taste and tolerance, and suitable for use orally or via a feeding tube.
But this is just the beginning. Over the next year, we’re releasing a full range of meals that can be consumed hot or cold, snacks, smoothies, and drinks –designed with real people, real needs, and real lives in mind.
Instead, the focus should be on smarter procurement strategies that deliver sustainable, long-term cost control.
Taylor & Taylor Care provide a strong example. Partnering with allmanhall, they benefit from comprehensive supply chain management, proactive supplier negotiations, and regular consultative advice - all designed to keep costs down without compromising quality.
“From day one, the care and attention provided by allmanhall has been exceptional… I’ve been impressed by the savings we’ve already seen, the flexibility regarding suppliers and by the excellent quality.”
Click here for the full video case study:
https://www.youtube.com/watch?v=NkroiOj26fs&t=1s
In today’s climate, expert food supply chain management is more than a support service - it’s a necessity. By tracking every penny of spend, identifying efficiencies, negotiating competitive pricing, and managing suppliers, care homes can protect their budgets while maintaining quality for residents.
As Oliver concludes:
“The effects of Government policy will likely be felt in the form of higher food prices in the coming years... choices made today will play a pivotal role in shaping the future of food security”.
With the right partner, care groups can ensure good food remains affordable, responsible, and sustainable - because quality meals for residents shouldn’t cost the Earth.
See the advert on the facing page for more information.

Our food is safe, shelf-stable, recyclable, and above all, human. It's not synthetic formula. It's not baby food. It’s real food, reimagined for different appetites.
If you or someone you care for lives with dysphagia, is tube-fed, or simply needs an easier way to stay nourished, we’re here to help.
Call us today – we’re a small team, and we love to talk. Whether you’re new to this or a seasoned pro, we’ll help you find something that works.
You don’t need to compromise.
You just need food that works for you.
Food Untethered
Real food. For every way of eating. www.fooduntethered.com
Please see our advert below.


Infection control remains a vital concern in care homes, where laundry plays an essential role in preventing the spread of harmful pathogens. With the Care Quality Commission continuing to raise expectations through a more rigorous inspection framework, laundry operations must meet high standards for both hygiene and regulatory compliance. Forbes Professional is helping care providers across the UK achieve exactly that.
Many care homes still rely on domestic washing machines that are ill-suited for the demands of a clinical environment. These machines often lack the ability to maintain the thermal disinfection temperatures required in care settings and are not compliant with WRAS Category 5 regulations. In addition, domestic models are not built for the volume of laundry processed in care homes, leading to higher operational costs, increased breakdowns, and invalidated warranties.

Forbes Professional supplies Miele commercial laundry equipment that is purpose-built for healthcare environments. These machines offer validated thermal disinfection cycles and include Type A air gaps for full WRAS compliance. Forbes also offers high-performance detergents which can be used in conjunction with the Miele appliances to deliver a comprehensive solution that supports effective infection control even at lower temperatures.
Some care operators have explored ozone-based disinfection as an alternative. While ozone can be effective, it introduces additional responsibilities around safe use and regulatory compliance. Systems must be carefully managed to mitigate potential risks to staff and residents. Forbes offers tried-and-tested alternatives that eliminate complexity while delivering proven results in a care environment. A major differentiator for Forbes is the company’s nationwide service infrastructure. They understand that equipment failure in a care home laundry room can quickly escalate into a serious operational issue. To minimise disruption, Forbes provides same- or next-day engineer call-outs as standard. Their extensive team of qualified field engineers and well-stocked service vehicles ensures swift, expert support across the UK.
Forbes also offers comprehensive rental and service contracts that include all maintenance and repairs, helping care homes manage costs and reduce administrative burden. These end-to-end solutions provide care operators with peace of mind, knowing their laundry systems are compliant, efficient, and fully supported. By partnering with Forbes, care homes benefit from expert guidance, market-leading equipment, and dependable service; ensuring hygiene standards are met and residents are protected. forbespro.co.uk | info@forbes-professional.co.uk | 0345 070 2335
SOUTHERN Contracts is one of the UK’s leading suppliers of industrial laundry, catering and commercial cleaning equipment.
Founded in 1964 to initially supply and maintain commercial cleaning equipment to the marine industry, we have since grown to become a well-respected and trusted partner to leading manufacturers.
We have consistently been the top performing Laundry Partner to Electrolux Professional and again achieved their top Laundry Partner Award for 2024. We’ve now won this accolade consistently for well over 20 years.

Now in our third generation and still very much a family run business, we are proud to now be a global supplier of not only laundry equipment, but with knowledge gleaned over the years, we are also a go-to company for professional kitchen appliances and commercial cleaning equipment. With our knowledge of most market products, we pride ourselves on delivering the very best solutions and service to our customers.
Already working for many of the national Care and Nursing Homes, as well as the hospitality industry such as hotels, restaurants and holiday parks, we understand the importance of keeping ‘down time’ to a minimum and by keeping in stock the leading commercial washing machines, tumble dryers and cleaning equipment we can sometimes just swap machines over to keep your business up and running.
We are able to offer independent and unbiased advice to ensure your purchase precisely meets your
requirements and budget, across a complete array of different products and models. Our expert team of technical staff are on hand to ensure your business is supported through every aspect of your purchase or rental agreement.
From advising on current government standards (eg. infection control for commercial washing machines and meeting government legislation for kitchen appliances) our team fully support you throughout the whole journey, from initial advice to delivery, installation, customer training, ongoing maintenance, service and repair. We hold many accreditations for safety and service excellence, providing peace of mind to all our customers, whether existing or potential.
For more information regarding our services for :
- Commercial laundry equipment
- Commercial kitchen appliances and warewashing/dishwashing
- Commercial cleaning equipment
Please visit our website at southerncontracts.co.uk and see previous projects we’ve worked on and our enviable testimonials received from happy clients across a plethora of sectors.
Contact us now on 03301 222888
Follow us on : Facebook, Twitter, Instagram and LinkedIn
See the advert on the previous page for information.
At PDS, we understand the challenges that come with managing laundry in a care home. From bedding, towels and tablecloths, to cleaning the clothes of residents, we appreciate that you need a care home laundry repair service and care home laundry equipment you can rely on.
Here at PDS, we provide care home laundry equipment to suit the needs of your setting. We offer many big-name industrial brands such as Alliance, Electrolux, Miele, Girbau, Grandimpianti and Schulthess.
As your trusted care home laundry repair services partner, we can help you with more than just supplying equipment. Our care home laundry services include laundry consultations, project design and management, equipment supply and installation, spare parts and more.
Our care home washing machines range from 6kg to 30kg drums for small to medium-sized care settings, and from 26kg to 40kg ones for larger care homes with more demanding laundry needs. We offer a full range of care home laundry equipment to meet your needs. Our equipment includes:
• Washing machines
• Tumble dryers
• Stacked equipment

• Ironers
We supply everything from compact care home washing machines to larger ironers and stacked systems, tailored to suit your available space, daily routines and laundry demands. Our aim is to make laundry simple and efficient, so your team can focus on providing the best care for your service users.
With more than 30 years of experience, our in-house engineers offer expert support nationwide. Wherever you’re based, we’re here to keep your laundry equipment performing at its best.
If you run or manage a care home and are looking for a care home laundry repair services partner, then look no further than PDS. We’ve been helping care homes just like yours since 2007 and are one of the most trusted suppliers of care home laundry repairs and care home laundry equipment. We are here to help keep your care home running smoothly. Please get in touch

If you are looking for high quality wash results that remove stubborn stains then speak with MAG for their recommendations. Complete thermal disinfection is a standard feature on their washing machines for nursing homes. To find out more about how MAG can support your care home telephone 01353 883025 or

We




•
•



Falls Prevention Awareness Week took place this year between the 22nd and the 26th of September, and as the autumn months are upon us, the weather is beginning to change, making it important to address the types of hazards that are now more likely to occur.
Things like snow, ice and fallen leaves can cause serious accidents for both residents and colleagues and Falls Prevention Awareness Week looks to raise awareness of these hazards to protect those who may be affected.
In 2024 the Health and Safety Executive estimated the cost of slips and trips in the workplace to the UK economy was £500 million in terms of employee absence, lost production, and other costs to business.
Slips and trips in the workplace were also estimated to have cost the NHS over £800 million in 2024 hospital admission and treatment costs.
Phil Clarke, Head of Health and Safety at Care UK (www.careuk.com) says: “It’s important that we are proactive in helping our colleagues through the winter months. By reducing the number of slips and trips we can make sure everyone is safe when
they’re moving around within the homes which, most importantly, helps colleagues to ensure that residents can lead fulfilling lives.”
As part of Phil’s plans to help Care UK-run homes with their awareness of hazards posed during the winter months, he has launched Sliptember, a campaign that aims to keep people safe and aware during the month of September and beyond.
Phil says: “The main thing we can do is plan to deal with these potential issues ahead of time. This includes stocking up on grit or salt and clearing up fallen leaves regularly. A combination of rotting leaves and frozen ground provides a dangerous slip and trip hazard to both residents and colleagues.”
As part of this campaign, Phil is using the acronym CHIMES to create an easy way for people to remember what we can be doing to prevent slips and trips.


Fall Savers®, are an experienced market leading healthcare provider of resident safety solutions for over 15 years.
FALL SAVERS ® WIRELESS MONITOR
Eliminate all cables with our new generation falls management solutions!
Upgrade your falls programme with the latest technology from Fall Savers®. The NEW Fall Savers® Wireless eliminates the cord between the monitor and sensor pad. This results in less work for nursing staff, improved safety for patients and reduced wear and tear on sensor pads. Wireless advantages include the ability to use one monitor with two sensor pads simultaneously and support for many new wireless devices.
BENEFITS INCLUDE:
Safer for patients; less work for staff
Bed and chair pads available
One monitor works with two sensor pads
Integrates with most nurse call systems
A variety of options, including:

Floor sensor mat
Wireless door/window exit alerts
TREADNOUGHT ®FLOOR SENSOR PAD
The TreadNought® Floor Sensor Pad is built to last with a durable construction that far out lasts the competition. Our anti-bacterial floor sensor pad is compatible with most nurse call systems or can be used with a portable pager to sound an alert when a person steps on to the sensor pad. Caregivers typically place the sensor pad at the bedside, in a doorway or other locations to monitor persons at risk for falls or wandering. An optional anti-slip mesh reduces the potential for slippage on hard surface floors.
FEATURES INCLUDE:
Connects directly to most nurse call systems
High Quality anti-bacterial Floor Sensor Pad
Large Size Pad: Measures (L) 91cm x (H) 61cm
Options (sold separately):
Anti-slip mesh for hard surface floors
See the advert on this page for further details or visit www.fallsavers.co.uk.
Courtney Thorne, a long-standing innovator in healthcare communication systems, is setting new standards in the care home sector with its advanced wireless nurse call technology—designed to improve resident safety, enhance staff efficiency, and support a more responsive care environment.
With over 30 years of experience serving the UK healthcare market, Courtney Thorne’s systems are now trusted by thousands of care homes nationwide. Unlike traditional hardwired solutions, their wireless nurse call systems offer non-invasive installation, scalability, and smart analytics—making them ideal for both new builds and retrofit projects.
“At the heart of our technology is the belief that better communication leads to better care,” says Graham Vickrage, Managing Director at Courtney Thorne. “Our wireless systems not only reduce response times but also empower staff

with the tools they need to deliver safe, person-centred care.”
Care providers are increasingly choosing wireless systems for their flexibility, reliability, and cost-effectiveness. With a full suite of accessories—including neck pendants, door monitors, fall detection, and bed sensors—Courtney Thorne systems can be tailored to meet the specific needs of each home and resident.
In an industry where compliance, safety, and staff pressures are always front of mind, Courtney Thorne provides more than just products—they offer ongoing support, training, and a commitment to innovation that helps care homes futureproof their operations.
For more information or to book a free demo, visit www.c-t.co.uk or contact info@c-t.co.uk.

Falls are a significant concern for vulnerable individuals, especially seniors and patients at risk. Medpage, a leader in assistive technology, offers a range of cutting-edge products designed to enhance safety and provide peace of mind for caregivers and families. Here’s an in-depth look at some of their standout solutions:
MPRCG1 (2023) BED LEAVING DETECTION ALARM WITH CAREGIVER RADIO PAGER
The MPRCG1 is a comprehensive system tailored for fall prevention in domestic, commercial, and NHS care settings. This all-inclusive kit includes a bed pressure mat sensor, a BTX21-MP alarm sensor transmitter, and an MP-PAG31 radio pager. The system is designed to alert caregivers when a patient leaves their bed, reducing the risk of falls. Key features include:
Wireless Alerts: Notifications are sent to the caregiver’s pager via tone or vibration.
• Customizable Alarm Delays: Options for instant, 15-minute, or 30-minute delays.
Durable Design: Antimicrobial and disinfectant-resistant materials ensure longevity. Ease of Use: Minimal installation required, making it user-friendly and portable.
HDKMB2 HOSPITAL DISCHARGE KIT FOR FALLS RISK PATIENTS

The HDKMB2 is a thoughtfully curated kit aimed at supporting patients transitioning from hospital to home care. It includes essential tools to mitigate fall risks and promote recovery. This kit is ideal for caregivers seeking a comprehensive solution to enhance patient safety during the critical post-discharge period.
MULTI-PORT WIRELESS SENSOR INPUT EXPANDER FOR NURSE CALL CONNECTION
CMEX-21
The CMEX-21 is Medpage’s latest innovation, designed to integrate seamlessly with existing nurse call
systems. This multi-port expander allows for the connection of multiple wireless sensors, enhancing the monitoring capabilities of healthcare facilities. Its versatility makes it a valuable addition to any care environment, ensuring timely responses to patient needs.
RON-WC2 WATERPROOF DISABLED PULL CORD ALARM TRANSMITTER WITH WIRELESS ALARM RECEIVER
The RON-WC2 is a robust solution for disabled individuals requiring immediate assistance. This waterproof pull cord alarm is ideal for use in bathrooms and other high-risk areas. Paired with a wireless alarm receiver, it ensures that help is just a pull away. Features include:
Waterproof Design: Suitable for wet environments.
• Wireless Connectivity: Reliable transmission to the alarm receiver.
Ease of Installation: Simple setup for quick deployment.
WHY CHOOSE MEDPAGE?
Medpage’s commitment to innovation and quality is evident in their product range. Each solution is designed with the user’s safety and convenience in mind, making them a trusted choice for caregivers and healthcare providers alike.
By investing in these advanced fall prevention tools, families and facilities can create safer environments for those at risk. Medpage continues to lead the way in providing practical, reliable solutions that make a real difference.
For more information, visit Medpage’s official website or contact their team to explore these products further. Safety starts with the right tools, and Medpage delivers just that. www.easylinkuk.co.uk
T: 01536 264 869
Alarm Radio Monitoring is the market leader in the design, manufacture and installation of bespoke, end-to-end, wireless alarm systems and solutions for the healthcare, leisure, custodial and education industries.
We have been providing wireless alarm and nurse call systems for over 30 years. Supplying care homes and hospitals with an essential lifeline that supports the delivery of outstanding care.
We believe in excellence which translates into:
Advanced Technology
Industry-leading wireless alarm technologies and software
Bespoke Solutions
We design systems to your needs rather than your team having to work around the system Innovative Design

Pushing boundaries with the reliability that comes from decades in the industry Flexible Finance Options
Ensuring organisations of
or

Data Analysis software provides a full audit trail of events
The all-new call logging software from ARM enhances the functionality of your care call system dramatically.
• It can help you track the quality of your service to your residents.
• It can help you demonstrate compliance with your aims and best practices, both to relatives and to authorities.
• It can help you find bottlenecks in service provision, track staffing requirements, and allow you to ensure staff are meeting expectations.
• Most importantly, it provides assurance that you know and can demonstrate what is happening in your care home.
The wireless ARM Nurse Call system has been developed over 30 years with both the client and user in mind.
It enables staff to efficiently answer calls, making the management of resources more flexible and provides the functionality you would expect of any nurse call system.
The system is quick and easy to install and works wirelessly, using radio communication between both the call points and the system infrastructure.
Call messages can be sent direct to staff to speed up response times and can also be integrated to work with smart phones & messaging.
Falls are one of the biggest challenges facing care providers – and they’re not just an issue for older people. They can affect anyone receiving care and support, including working-age adults with disabilities or longterm conditions. A fall can change someone’s life in an instant, leading to injury, hospitalisation, or loss of confidence. For staff, falls mean stress, paperwork, and the urgent task of helping someone recover safely. This September’s Falls Awareness Week is a chance to shine a light on the issue and explore new ways of keeping people safe. At the Digital Care Hub, we’re supporting the week with practical resources and a twopart mini-webinar series designed to spark ideas and share real-world success stories from across the sector.
LEARNING FROM EACH OTHER
On Tuesday 23 September at 2pm, we’ll host Wellbeing in Focus: Sensor Technology and the Care Journey. This session will explore the benefits of sensor-based technology from both care provider and resident perspectives. Speakers include Sensio, Lovett Care and Dormy Care, with an introduction from the National Care Forum.

On Wednesday 24 September at 2pm, we’ll run Beyond Falls: How Sensor Tech is Unlocking Safer, Calmer Care. This goes beyond basic fall prevention, exploring how sensors can improve sleep, reduce anxiety and even help spot health risks earlier. Care England will open the session, and Ally Cares will share powerful insights from care homes already using these systems. Both webinars are free to attend and are aimed at managers, owners and care teams who want practical, evidence-based solutions.
THE CHALLENGE ON THE GROUND
Anyone working in care knows that preventing falls isn’t easy. Staff need to balance safety with independence, spot risks early, and respond quickly when incidents happen. For many providers, night-time
checks can disturb residents’ sleep and still miss the moment when a fall happens. Long-lie incidents, where someone is not discovered for hours, are a particular concern and can have serious health consequences.
TECHNOLOGY MAKING A DIFFERENCE
The good news is that technology is helping providers change the story.
At The Lawns Care & Nursing Home in Worcestershire, the team introduced Ally Cares, an AI-powered acoustic monitoring system. It alerts staff to unusual sounds or movement at night, so they can intervene before someone gets hurt. Over six months, falls dropped by two-thirds, with the biggest impact for residents most at risk.
Hartland House Care Home in Cumbria went a step further with Nobi Smart Lamps, which combine AI and smart lighting to detect when someone gets out of bed and automatically light the room. They reported an 84% reduction in falls, no long-lie events, and response times falling from nearly an hour to just two minutes.
Technology alone isn’t the answer – it needs the right culture, training and care planning to be truly effective. That’s why conversations like those taking place during Falls Awareness Week are so important.
By sharing stories, data and lessons learned, we can make care safer, calmer and more dignified for everyone – whether they live in a care home, supported living, or their own home.
Join us at the Digital Care Hub webinars and be part of the conversation. Together, we can turn the tide on falls.
Find out more on the Digital Care Hub website at www.digitalcarehub.co.uk/falls-awareness-week-the-power-of-tech/
See us n Stand B11 at The Care Show. See the advert on page 28.
Technology has made people more connected with the world around them and the revolution in assistive care devices has made it possible for the elderly to spend their last years in a comfortable and familiar environment. These devices have also made it easier for home carers to provide quality care for their loved ones while managing their own lives. They allow you to care for your elderly whether they are travelling in the city for errands, staying alone at home, or staying in the same home as you. They are also helping nursing homes provide better care for them with discrete monitoring and quick responses to emergencies.

If you’re looking for these kinds of assistive care devices for your loved ones or nursing home, Frequency Precision produce some of the best systems available to help you with elderly care and mobility monitoring, ranging from bed, chair and floor sensor mats through fall monitoring and GPS tracking to fully integrated nurse call plug or wireless systems.
Phone: 01837 810590
Email: contact@frequencyprecision.com
Website: www.frequencyprecision.com

By

The care sector in the UK is facing a growing crisis. With an aging population, rising demand for services, and chronic staff shortages, pressure on providers has never been greater. In 2023, Skills for Care reported around 152,000 vacancies in adult social care in England alone. These challenges not only strain the system but also compromise the quality and continuity of care. Yet, a powerful and often underutilised solution lies in education and training pathways, particularly Foundation Apprenticeships, full Apprenticeships, and vocational work-based learning such as college placements and T Levels.
These routes into the care profession not only address immediate staffing shortages but also support the longterm sustainability and professionalism of the sector. By combining academic learning with hands-on practical experience, these pathways provide young people with the skills, confidence, and motivation to build fulfilling careers in care. In turn, employers benefit from a pipeline of wellprepared, passionate, and loyal workers.
FOUNDATION APPRENTICESHIPS: ENGAGING FUTURE TALENT EARLY
Foundation Apprenticeships (FAs), offered to school leavers (and up to the age of 19 or 24 with an EHCP), provide an invaluable early introduction to the care sector. These programmes combine classroom learning with structured work placements, giving apprentices the chance to gain practical experience in real care settings in an 8-month window. By engaging with the profession early on, students gain a realistic and positive understanding of what care work involves, dispelling myths and building confidence in their abilities.
This early engagement is crucial. Foundation Apprenticeships help students make informed career choices and allow employers to spot and nurture young talent as they enter the workforce. For the care sector, which traditionally struggles to attract younger workers, FAs serve as a vital bridge between education and employment. They also broaden access to the profession, particularly among school-leavers who may not have considered care as a viable or attractive career path.
COLLEGE PLACEMENTS AND T LEVELS: BUILDING REAL-WORLD EXPERIENCE
Further education colleges play a key role in preparing students for care roles. Health and Social Care students typically complete structured placements in settings such as care homes, day centres, and domiciliary services. These experiences allow learners to apply theory in practical environments and develop essential interpersonal skills.
T Levels, introduced in 2020, are two-year programmes for 16-19 year-olds that include a minimum of 315 hours of industry placement. The Health and Science T Level equips students with both technical knowledge and soft skills like empathy, patience, and communication - all vital for high-quality care.
For employers, T Level placements offer a low-risk way to assess potential recruits in real working contexts. Students who complete meaningful placements are often more confident and better prepared for full-time roles, leading to improved retention and smoother transitions into employment.
APPRENTICESHIPS: STRENGTHENING AND RETAINING THE WORKFORCE
While Foundation Apprenticeships and T Levels lay the groundwork, full Apprenticeships serve as a critical tool for both recruitment and retention in the care sector. Apprenticeships offer a blend of paid work and formal study, allowing individuals to "earn while they learn" and progress toward nationally recognised qualifications in adult care, childcare, and support work.
Crucially, apprenticeships cater to a wide age range and can be used both for new recruits and for upskilling existing staff. This makes them incredibly versatile. For young people who may not thrive in traditional academic routes, apprenticeships offer a clear, supported pathway into meaningful employment. For care providers, investing in apprenticeships can help fill vacancies with committed, well-trained individuals while demonstrating a commitment to workforce development.
Apprenticeships also promote staff loyalty. When employees are supported to learn and develop within their role, they are more likely to stay with their employer long-term. This helps to reduce the high turnover rates that plague the care sector and improves continuity of care for service users.
In a sector crying out for skilled, compassionate workers, the potential of Foundation Apprenticeships, college placements, T Levels, and full Apprenticeships cannot be overstated. These pathways equip learners with the necessary skills and values while embedding them in the culture of care from an early stage. By integrating education with employment, we can reshape how the care sector recruits and retains its workforce. This is not a short-term fix but a sustainable, future-focused strategy.
The care sector cannot afford to wait. By actively engaging with local education providers such as colleges, schools, and apprenticeship training organisations, care employers can build a robust pipeline of skilled, motivated individuals ready to make a difference. Whether it’s offering a placement, mentoring a student, or hiring an apprentice, every action contributes to a stronger, more sustainable workforce. Reach out to Exeter College today and start shaping the next generation of carers.
Sam has been part of the apprenticeship world for over 25 years, having gained vast experience in teaching, designing and managing the quality of apprenticeship curriculum in both independent training provider & College settings. Sam joined Exeter College over 4 years ago and played a key role in the Ofsted Outstanding grading for Apprenticeships. Apprentices@exe-coll.ac.uk https://exe-coll.ac.uk/apprenticeships/
See the advert on the facing page
PIONEERING TECHNOLOGY-ENHANCED CARE FOR THE FUTURE
Multisensory Care Solutions represents a significant advancement in specialist care provision, founded by industry veterans Karen Bradley and Brian Lumb. Drawing upon their exceptional track record of operating a CQC Outstanding-rated residential care home for complex care residents over three decades, the company brings unparalleled expertise to the care sector.
PROVEN LEADERSHIP IN CARE EXCELLENCE
Karen Bradley brings over 45 years of comprehensive experience working with individuals living with dementia, autism, learning disabilities, and other specialist needs. As a former Registered Manager and certified trainer across multiple care disciplines, her deep understanding of person-centred care principles has consistently delivered outstanding outcomes for residents and their families. Brian Lumb contributes extensive technical expertise from his background in multimedia systems, touchscreen displays, and point-of-information technologies. His proven track record in developing and implementing innovative digital solutions—both as a business owner and senior executive within major PLCs—provides the technical foundation for revolutionary care applications.
INNOVATION-DRIVEN CARE EXCELLENCE
The founders' unique combination of care expertise and technological innovation has enabled them to integrate cutting-edge solutions into their care delivery model. This pioneering approach to person-centred care through technology played a crucial role in achieving their CQC Outstanding rating, demonstrating measurable improvements in quality of life for residents and enhanced support for families.
INTRODUCING MULTISENSORY MAGIC
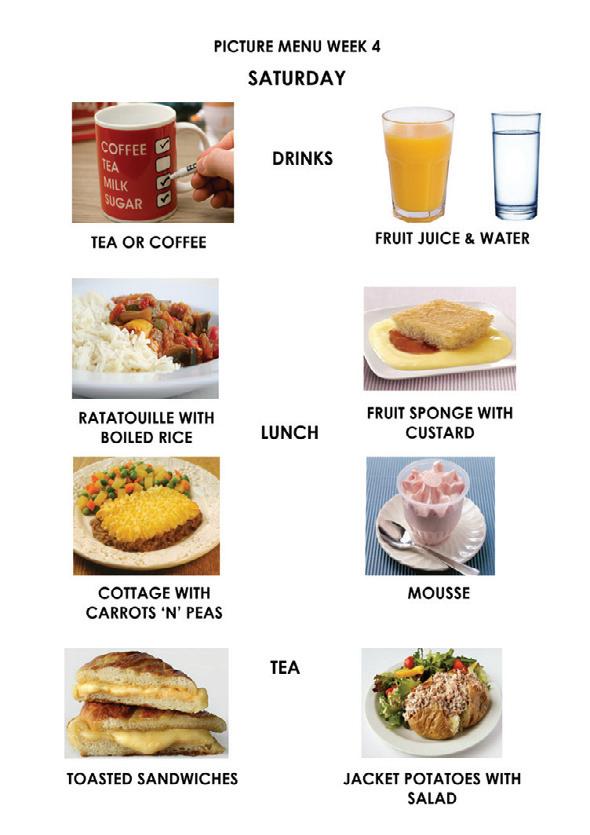
Building upon decades of practical experience, Multisensory Care Solutions has developed "Multisensory Magic"—an accessible software application designed to democratise technology-enhanced care. This cost-effective solution makes advanced multisensory interventions available to care providers across the sector, extending beyond premium facilities to benefit a broader range of residents.
Meeting Critical Care Challenges
With approximately one million people currently living with dementia in the UK—a figure projected to reach 1.5 million by 2040—the need for innovative care solutions has never been more urgent. Technology-enhanced interventions offer proven benefits in:
Sensory stimulation and engagement
Cognitive function support
Enhanced communication pathways
Improved resident wellbeing outcomes
A TIMELY CALL TO ACTION
As the care sector observes World Alzheimer's Month in September 2025, culminating in World Alzheimer's Day on 21st September, the opportunity to transform dementia care through accessible technology solutions represents both a professional imperative and a moral responsibility.
Multisensory Care Solutions stands ready to support care providers in achieving improved CQC ratings whilst delivering meaningful enhancements to resident care and family satisfaction. For more information see the advert on the facing page or please call or email Brian Lumb - 07801 498483 or Email - brian@multisensorycaresolutions.com www.multisensorycaresolutions.com
Restrictive practices such as physical restraint, bed rails, or lap belts remain one of the most challenging aspects of health and social care. Intended to keep patients safe, they can also cause harm, distress, and loss of dignity when used unnecessarily. Across the UK, the principle is clear: care must always use the least restrictive option.
Legislation provides the framework, but culture and staff behaviour shape daily practice. Nurses, carers, and clinicians often make quick decisions balancing safety with autonomy. Without training, restrictive practices risk becoming routine. To change this, staff need better understanding of the human impact and confidence to use alternatives. That’s where Restrictive Practice makes a difference. Developed through co-design workshops with patients and carers, this gamified e-resource gives a voice to those most affected by restraint. Their lived
experiences shaped the learning, helping staff see restraint not as a neutral safety tool, but often as something frightening or disempowering.
The results are powerful. Staff trained with the resource led Quality Improvement projects, achieving measurable reductions:
- Bed rails dropped from 360 to 277 incidents
- Bed bumpers from 303 to 227
- Lap belt use halved, from 46 to 22
These improvements represent safer, more compassionate care and reassurance for families.
Restrictive practices may never disappear entirely, but they should be the exception, not the rule. With the right knowledge and tools, staff can choose safer alternatives and build a culture of dignity, compassion, and respect across UK care services. See our advert on the front cover or visit www. RestrictivePractice.com


Users / providers are enabled to ‘CONJURE
and reminiscence therapy sessions. Audio, video, slide shows, text, images and aromas can all be blended
using multiple screen displays.



A new apprenticeship has been launched for adult care support workers who assist people with mental health challenges, including dementia and neurodiversity.
Leading training provider Realise has revealed its new Level 3 Senior Healthcare Support Worker Apprenticeship which features a specialist mental health pathway.
The apprenticeship aligns with The Care Workforce Pathway - developed by Skills for Care and the Department of Health and Social Care –which emphasises the importance of equipping staff who support people with mental ill health with the right knowledge and skills.
The programme’s focus on mental health makes it ideal for those working in complex care services or supporting individuals living with dementia or mental health conditions. It also benefits those supporting individuals with a dual diagnosis.
Standard apprenticeship funding rules apply with no age restrictions. However, learners aged 16–22 are eligible for 100% government funding, meaning non-levy employers are not required to pay the usual 5% co-investment. This is available in England only.

While a few other providers offer the Level 3 Senior Healthcare Support Worker Apprenticeship in Mental Health Pathway, the Realise progamme was developed in collaboration with leading industry provider Barchester Healthcare, ensuring it is closely aligned with the real-world demands of the role, particularly in complex care.
Angela Kaine, Director of Health & Social Care at Realise, said: “We fully support The Care Workforce Pathway, which emphasises the importance of people being able to receive training in areas in which they
specialise.
“Care workers supporting individuals with dementia or other mental health conditions benefit greatly from targeted training in crisis intervention, mental capacity and de-escalation techniques.
“Offering this apprenticeship can help adult care providers recruit individuals for specialised roles and improve retention - two major challenges within the sector.
“There is a wide variety of opportunities within adult care, and we’re proud to support those looking to develop both their technical skills and their chosen specialism.”
This comprehensive 18-month apprenticeship is designed to provide a rich and supportive learning experience. Learners will benefit from a blend of face-to-face support and interactive webinars, creating the perfect balance between in-person guidance and flexible online learning.
These sessions not only enhance understanding but also offer valuable opportunities to connect, collaborate, and network with peers from across the sector- helping to build confidence, share best practices, and develop lasting professional relationships.
Modules include quality improvement - where learners are challenged to identify small changes to enhance performance - and team leadership, which encourages them to take on more responsibilities.
Realise can tailor programmes to suit the employer’s needs by utilising unit selection through the diploma.
The apprenticeship is available throughout England.
For more information, visit www.realisetraining.com
In today’s regulated care environment, having clear, current, and wellcommunicated health and social care policies is essential for delivering safe, compliant services. The Care Quality Commission (CQC) now places increasing emphasis on how policies are implemented and understood—especially during registration and inspections.
Outdated or poorly communicated policies can significantly impact your CQC rating. Even if documentation is comprehensive, failure to ensure staff understand and follow procedures may lead to a “Requires Improvement” or even “Inadequate” rating under the ‘Effective’ domain.
Well-maintained policies promote consistent standards across care teams and help safeguard services when incidents arise. In regulatory investigations, the first request is often to review relevant policies—making accuracy and accessibility key to reducing legal and compliance risks.

However, keeping policies up to date is challenging. Constant changes in legislation, best practice guid-

page
ance, and case law mean that policies can quickly become obsolete. W&P has been a trusted provider of CQC-ready care policies and procedures for over 20 years. Our expert team monitors industry developments to ensure your policies remain fully compliant.
Our Online Policy Portal simplifies policy management. With just a few clicks, providers can update content, distribute documents to staff, track confirmations, and monitor compliance via a real-time dashboard. You can even provide temporary read-only access to inspectors—demonstrating transparency and accountability instantly.
Ensure your care service meets CQC expectations with fully up-to-date, easily accessible, and well-communicated policies.
Email: info@wandptraining.co.uk
Call: 01305 767104
for details.
Since our founding in 2010, Activities to Share has been dedicated to enhancing the lives of those in care by providing thoughtfully designed activity products. Our mission is to support activity coordinators in delivering uplifting, engaging experiences that foster connection, joy, and well-being.
We achieve this by listening closely to your feedback and evolving with your needs. Whether over the phone, via email, WhatsApp, or Live Chat on our website, our team is always ready to offer advice and help you find just the right products to bring your ideas to life.

While we embrace the convenience of technology to expand our resources and share knowledge, we remain firm believers in the irreplaceable power of sensory engagement. That’s why we continue to make our Reminiscence Kits and Sensory Bags with
real, tactile items that stimulate the senses. Some experiences—like popping bubbles for the splash, breathing in a familiar scent, or piecing together a puzzle with others—simply can’t be replicated on a screen. These sensory moments are invaluable in encouraging storytelling, sparking memories, and fostering conversation. Our values remain rooted in this commitment to meaningful connection. We’re here to partner with you—the professionals on the front lines of care—to create a sense of structure, well-being, and fun for those who need it most.
Are you longing for your activity diary to be full?
Look no further
www.activitiestoshare.co.uk are here for you! Call 0117 966 6761


Rebecca Pallot, a partner and employment lawyer at Mills & Reeve

The much-debated Employment Rights Bill promises to bring widespread reforms to employment law. As it reaches the final stages of the Parliamentary process, Rebecca Pallot, employment lawyer at Mills & Reeve, looks at three groups of measures which will have a particularly significant impact on employment relationships in the adult social care sector.
The Government intends to use the Bill to abolish the two-year qualifying period for unfair dismissal, making the entitlement to bring a claim effective from the first day of employment. It also proposes to introduce a new framework for a lighter touch unfair dismissal regime during an “initial period of employment”. That lighter touch process has been described as a “probationary period exemption”.
Under the proposals, a care home provider will be able to dismiss fairly during the initial period if they can demonstrate a potentially fair reason for dismissal which relates to the individual employee. It will also be possible to bring claims in respect of dismissals for redundancy from the first day of employment.
Regulations will define the length of the initial period of employment and how it is calculated. This is likely to be a minimum of six months and could be as long as a year, with the Government currently supporting a compromise of nine months.
(www.mills-reeve.com) assesses three groups of measures in the Bill which are particularly significant for the adult social care sector.
It remains to be seen what the exact process will be to make a dismissal fair in the initial period but it is clear, that there is growing concern amongst care home operators about the increased risk of unfair dismissal claims. While some think that this change could be cost-neutral, because it will give employers a greater incentive to manage probationary periods effectively, much will depend on the design of the regulations, on which the Government will be consulting shortly.
There are three groups of measures to protect zero-hours and low hours workers, as well as agency workers employed in the adult care sector on similar arrangements:
the right to guaranteed hours after the end of every reference period, which reflects the hours worked during that period the right to reasonable notice of shifts (including change and cancellation), and the right to payment for cancelled, moved and curtailed shifts where sufficient notice has not been given
The new regulations will define the reference period for calculating guaranteed hours and other conditions of entitlement, as well as the procedural requirements around the offer of a new contract. They will also specify the minimum notice period for the cancellation of shifts, the compensation due and when it must be paid.
According to the Bill’s impact assessment, these measures will have a disproportionate impact on the social care sector, where over a fifth of its workforce are believed to be engaged on zero-hours contracts or similar arrangements which would be in scope.
There will be significant direct and indirect costs in complying with these measures, which are among the most complex in the Bill.
The three-day waiting period to qualify for SSP will be abolished so that it is paid from the first day of sickness. The Lower Earnings Limit, which
prevents those who earn below a certain amount from claiming SSP, will also be removed. Once these changes take effect, SSP will be paid at 80% of average weekly earnings or the current flat rate, whichever is lower.
As with the measures in respect of zero hour contracts, the Government’s plans to reform SSP will have a significant effect on the social care sector, because of its relatively high proportion of lower paid workers. However, it is possible that the resulting improvements in staff welfare will bring productivity gains to offset at least some of the additional costs.
According to the Government’s implementation timetable, published in July, changes to SSP eligibility will be brought into effect in April 2026, giving care home providers a small window in which to prepare for these reforms.
Other measures in respect of zero hours contracts and unfair dismissal will not be brought into force until 2027. As such, employers have more time to implement any necessary changes. In the meantime, it’s important for providers to keep an eye on this constantly evolving area of law, while engaging with the Government’s consultation on the regulations required to implement these measures, which is expected shortly.
Employers could consider taking the following steps:
• assess your organisation’s dependence on workers who are not permanent employees with predictable hours
• review procedures for probationary periods and ensure that line-managers are trained to implement them, and
• align your sickness absence procedures with the changes to SSP being introduced in April.
While the Bill also creates the framework for establishing a negotiating body to set pay and conditions across the entire adult care sector in England, it remains to be seen what impact the proposed measures will have on the sector.

Specialist business property adviser, Christie & Co, has launched its Care Market Review 2025 report, which analyses a range of topics relating to the UK healthcare business market, including capital markets, land and development, the transactional market, shifts in local authority fee rates, operator sentiment and the finance landscape. Healthcare the report reveals, remains a compelling investment due to strong demographic drivers, particularly the ageing population and rising life expectancy, with the over-80s population expected to more than double by 2050. Investor interest is further supported by ESG credentials and inflation-linked, long-income lease structures the report reveals.
The 12 months to July 2025 marked a period of strategic realignment amid ongoing macroeconomic and geopolitical shifts, with the market evolving via increased M&A, joint ventures, and a growing focus on management contracts.
Overseas capital significantly boosted deal activity during this time, with sector-specialist REITs like Welltower and Omega leading major acquisitions, including Care UK and 45 Four Seasons care homes respectively. H1 2025 also saw robust investor activity, including notable M&A deals like Care Trust REIT’s acquisition of Care REIT plc and the Aedifica-Cofinimmo merger. While operators are increasingly using lease-based models and sale-and-leaseback structures to unlock capital, looking ahead, Christie & Co expects to see more investors exploring sale and manage-back models, offering higher returns with greater operational exposure. Christie & Co’s report goes on to analyse the transactions that it has conducted over the past year. Deal activity surged, with completions at their highest level, and Christie & Co’s pipeline 24 per cent ahead of where it was in 2024. 49 per cent of deals involved homes with 20 to 39 beds, while only 17 per cent were for homes over 60 beds.
A notable shift occurred in the profile of homes entering the market, with a rise in smaller care homes (under 20 beds) making up 38 per cent of instructions, an increase from 12 per cent in early 2024. Larger homes (over 60 beds) comprised just 5 per cent of instructions, down from 15 per cent, reflecting a shortage of purpose-built facilities. Homes with 20 to 59 beds accounted for 56 per cent of instructions, down from 73 per cent in 2024.
First-time buyers represented 17 per cent of deals in H1 2025, up from 11 per cent in 2024 and just 4 per cent in 2023. Small and medium-sized groups (those with 3 to 19 homes) were the most active buyers (32 per cent of deals), followed closely by independent operators (those with 1 to 2 homes) at 31 per cent. Large groups and corporates saw a decline in activity, accounting for only 20 per cent of deals, down from 36 per cent in 2023.
Homes sold with vacant possession rose to 21 per cent in 2025, up from 13 per cent in 2024. Of these closed homes, 60 per cent remained in care use, 24 per cent were converted to residential dwellings, and 16 per cent repurposed for other uses. This high closure rate in the sector is something that Christie & Co expects will continue.
Christie & Co also conducted and analysed a Freedom of Information Act survey, covering all 174 local authorities across England, Wales, and Scotland. It revealed an average residential fee increase in England of 8.6 per cent compared with 9 per cent in 2023/24. There were some notable fee rate uplifts in certain local authorities, albeit from a low base level.
The burden on the self-funded client base is likely to rise, with the majority of providers achieving private fee increases of between 5 per cent and 10 per cent, sometimes more.
A segment from Christie Finance on the finance landscape notes that the care sector continues to attract strong interest from the finance market, with both new and established operators seeking debt funding to sup-
Global assists clients throughout the U.K. who specialise in the healthcare sector to achieve their objectives of purchase, development and refinance.
We have organised over £1.8bn for clients in the past 30 years, providing clients with competitively priced funding to refinance existing debt, ease cashflow and develop businesses further.
From helping clients make their first purchase through to allowing groups to grow significantly in size we assist at every stage of your business expansion.

Every proposal is individual and deserves to be treated that way, so we hope you will allow us to be of assistance to you and call us to chat through your plans and requirements, I am sure we will be able to tailor a facility to your requirements.
Call us on 01242 227172 or e-mail us at enquiries@globalbusinessfinance.net
port growth. However, securing finance remains challenging due to increasingly rigorous lender requirements. Richard Lunn, Managing Director – Care at Christie & Co, comments,
“We have seen extremely positive market activity throughout the year, as many operators look to grow their portfolios. By the end of August, we had already transacted more deals than in 2024, and our forward pipeline is the highest ever, reflecting the investor and operator desire to acquire care services. On a recent trip to the USA, investors called this a ‘Goldilocks period’ for senior care providers and investors, with the much-heralded arrival of the huge demographic wave of elderly people requiring care and support and limited quality supply to meet this demand in future years.”
To read the full Care Market Review 2025, visit: www.christie.com/sectors/care/care-market-review-2025
