83/224 - MAY/JUNE 2025



83/224 - MAY/JUNE 2025



Join JCI for a comprehensive two-day workshop designed to provide you with the knowledge and strategies to establish a standardized approach to managing patient safety events, including sentinel events.
Why Attend:
• Learn from JCI experts who will guide you through the process of conducting a root cause analysis (RCA) and implementing corrective actions
• Engage in hands-on activities and discussions that will deepen your understanding of RCA methodologies
• Gain practical insights and strategies to apply RCA in your healthcare organization, improving patient safety and quality of care
What Will You Learn:
• Define 7 organizational requirements to effectively manage patient safety events
• Interpret relevant Joint Commission International standards
• Apply the 4-phase approach to root cause analysis
• Illustrate the use of 5 essential tools
Continuing Education Credits Available ACCME: 6 CME credit(s) ANCC: 6 CE credit(s)
LEARN MORE:


According to the World Health Organization, cancer claims the lives of approximately 10 million people every year. This stark reality drives scientists to intensify efforts in improving treatments for better healing and overall health. As stated in a World Economic Forum report, seven out of ten cancer-related deaths occur in low- and middle-income countries. This highlights how increased investment in healthcare and wise management can significantly reduce cases and improve survival rates.
At the same time, the number of new cancer cases is expected to rise by more than 75% annually by 2050. These alarming projections have doubled the urgency among researchers and accelerated medical advancements in the fight against cancer. Encouraging indicators have emerged, such as vaccines designed to stimulate the immune system to target cancer cells and reduce the risk of recurrence.
These vaccines are also expected to have fewer side effects than traditional chemotherapy. In addition, a new test developed by U.S. researchers can detect 18 types of cancer in their early stages, paving the way for multi-cancer early detection screenings. This test has proven to be both cost-effective and accurate. Artificial intelligence is also significant in this progress; it is not a side player but a core driver of innovation.
While cancer cases may be on the rise, so are medical science breakthroughs. Hospitals are advancing their technologies and capabilities to offer better care, and related investments are growing rapidly. Awareness, early detection, and patient education are becoming increasingly impactful in managing the disease. As a result, hope is growing, and so are recovery rates.
Together, we can achieve more!

The Publisher
Publisher Arab Health Media Communication
President Simon Chammas schammas@tahmag.com
Executive Vice President Mirna Khairallah mirna@tahmag.com
Senior Editor Elham Najem editorial@tahmag.com
Content Executive Jessica Achkar editorial@tahmag.com
Editors Aline Debes, Mark Steven, Don Karn, Andrew Weichert, Colette Semaan, Abbas Moussa
Senior Director of Content Marketing Jessie Chlela jessie@tahmag.com
Creative Director Rania Khalil rania@tahmag.com
Business Development Manager Wadih Chammas wadih@tahmag.com
IT Manager Elie Yammine elie@tahmag.com
Photographer Hanna Nehme
Advertising advertising@thearabhospital.com
OFFICES
IHMC, Cyprus +357 96 158661
Dubai
Expert Media Communication Services-FZCO
Dubai Silicone Oasis +971 50 2971007
Printing
Distribution KSA - UAE - OMAN - TURKEY
LEBANON - JORDAN - KUWAIT
BAHRAIN - QATAR - EGYPT
All images from shutterstock© unless provided by clients .
All rights reserved by the HOSPITALS magazine. No part of this publication can be reproduced in any form without prior permission in writting from the publisher.




Dr. Hassan Galadari


32 M42 appoints Dr. Moza Ajaif Al Zaabi as CEO of Sheikh Sultan bin Zayed Hospital to drive healthcare excellence
104 MedTech World: Fueling MedTech Investment Momentum Across Borders
24 Former U.S. attorney general chooses UChicago Medicine for robotic and minimally invasive heart surgery
28 Istiklal Hospital Hosts Cochlear Implant Project for Palestinian Children with a Grant from King Salman Humanitarian Center
40 UCLA Health: Functional MRI provides ‘roadmap’ for surgery in previously inoperable areas of the brain
50 Henry Ford Health: Healing Beyond Boundaries, Leading the Future of Medicine
56 ACIBADEM GROUP: We Care for Blood Diseases
62 ACIBADEM TURKIYE: A Preeminent Center for Adult and Pediatric Liver and Kidney Transplantation
42 Dr. Clement Khoury, Head of Radiation Oncology at Clemenceau Medical Center Beirut
54 Dr. Momen Wahidi, Medical Director, Canning Thoracic Institute, Northwestern Medicine
58 Hein Van Eck, Chief Executive Officer, Mediclinic Middle East
Dr. Elias Zgheib



64 Diala Atassi, Chief of Global and National Programs, University of Chicago Medicine
68 Dr. Hassan Galadari, Assistant Professor of Dermatology at the College of Medicine and Health Sciences of United Arab Emirates University
72 Mark Adams, CEO of CMC Hospital Dubai
76 Ramsey Hout, Founder of Applied Healthcare Solutions
80 Dr. Elias Zgheib, Plastic and Reconstructive Surgeon
36 A New Era in Brain Tumor Breakthroughs
46 International Accreditation: Elevating Healthcare Quality to Global Standards
84 Obesity Treatment: A Comprehensive Approach to Lifestyle Change
102 Toward Better Management of Hypertension: Lifestyle Changes and the Latest Therapeutic Innovations
Baylor St. Luke's Medical Center
88 Three things to know about the renal diet
90 How Dialysis Works in Patients With Kidney Failure
Al-Ahli Hospital/Qatar
92 Cesarean Section Cons and Pros
96 Al-Ahli Hospital Launches Qatar’s First Comprehensive Well Child Preventive Wellness Package
100 Al-Ahli Hospital Unveils Qatar’s First Photon Scanner CT





When technological precision meets the compassion of medicine, healing becomes a story worth telling. This is what unfolded at King Faisal Specialist Hospital & Research Centre (KFSHRC) Riyadh, where an eight-year-old child underwent a life-saving liver lobe transplant using an advanced robotic surgical system, after liver failure had exhausted his small body and deprived him of his childhood. The high-precision technology enabled the young patient to be discharged just two weeks after surgery, half the usual recovery time, allowing him to return to a normal childhood. The medical team described the outcome as the essence of their striving to achieve.
The child’s condition required urgent intervention, complicated by the small body size and the limited space available for surgical access. However, KFSHRC’s extensive experience with robotic organ transplants in adults paved the way for adapting the technology to a paediatric case. A tailored surgical plan was developed, involving precisely repositioning the robotic instrument entry points to accommodate the child’s anatomy.
Professor Dieter Broering, Executive Director of the Organ Transplant Centre of Excellence and lead surgeon on the case, explained: "Robotic surgical techniques have traditionally been limited to adults, but we succeeded in adapting them for children, offering exceptional precision and a marked reduction in complications. The transplant required redesigning the surgical approach to suit the child’s small body and confined space, which we addressed by meticulously adjusting the entry sites for the robotic tools to ensure maximum safety."
The procedure was successfully performed by extracting the left lobe from a living donor and fully transplanting it into the child, using a robotic surgical system, without any direct manual intervention. This approach significantly minimized the size of surgical incisions. It

accelerated the recovery process, allowing the child to be discharged within two weeks, compared to the usual month-long hospital stay for similar transplants.
This operation represents a groundbreaking model for expanding robotic surgery in paediatric care. The technology offers exact control, reduces surgical complications, and enhances overall safety, paving the way for the future development of child-specific robotic surgical systems.
This achievement is part of a series of milestones positioning KFSHRC as a global leader in robotic surgery. The hospital previously performed the world’s first fully robotic heart transplant and the world’s first robotic liver transplant, advancements that garnered attention from both local and international media. These breakthroughs reflect KFSHRC’s commitment to pioneering innovative medical solutions and delivering world-class specialized healthcare. The accomplishment also represents a success of the Health Sector Transformation Program, one of the key initiatives under Saudi Vision 2030, launched by H.R.H. Crown Prince Mohammed bin Salman, Prime Minister of the Kingdom. It stands as a testament to the quality of healthcare provided to all people in Saudi Arabia.
IT IS NOTEWORTHY THAT KFSHRC HAS BEEN RANKED FIRST IN THE MIDDLE EAST AND AFRICA AND 15TH GLOBALLY IN THE LIST OF THE WORLD’S TOP 250 ACADEMIC MEDICAL CENTRES FOR THE THIRD CONSECUTIVE YEAR AND RECOGNISED AS THE MOST VALUABLE HEALTHCARE BRAND IN THE KINGDOM AND THE MIDDLE EAST, ACCORDING TO THE 2025 BRAND FINANCE RANKINGS. ADDITIONALLY, IT WAS INCLUDED IN NEWSWEEK MAGAZINE'S WORLD’S BEST SMART HOSPITALS LIST FOR 2025.


As part of its commitment to advance healthcare innovation, the Department of Health – Abu Dhabi (DoH), the regulator of the healthcare sector in the Emirate, has announced a dual Memoranda of Understanding (MoU) with Gilead Sciences, a global biopharmaceutical company, on the sidelines of Abu Dhabi Global Healthcare Week 2025 (ADGHW). As part of the agreement, both parties aim to broaden collaboration in clinical research, advanced therapies and healthcare accessibility, while also enhancing treatment options and driving cutting-edge medical innovation in the emirate
Reflecting Abu Dhabi's standing as a global leader in healthcare innovation, these agreements are set to propel the emirate to the forefront of medical research and development. By focusing on advancements in virology and cell therapies, the partnership aims to expand access to pioneering treatments and enhance community healthcare outcomes. This strategic collaboration reinforces Abu Dhabi's commitment to integrating state-of-the-art medical technologies and research capabilities, thus ensuring the emirate remains a hub for healthcare excellence and a model for worldclass healthcare practices.
Dr. Asma Ibrahim Al Mannaei, Executive Director of the Health Life Sciences Sector at the Department of Health – Abu Dhabi (DoH), said: “Research and development are crucial for fostering innovation and ensuring the sustainable advancement of the health and life sciences ecosystem. This commitment ultimately supports proactive and holistic care for our communities. In alignment with Abu Dhabi’s vision to establish one of the world’s smartest healthcare systems, we are dedicated to empowering our community with the tools necessary for maintaining healthy populations for generations to come. Furthermore, we continue to forge strategic partnerships that enhance our capacity to deliver

best-in-class care to community members in the emirate and beyond.”
IN THE PRESENCE OF H.E. DR. NOURA KHAMIS AL GHAITHI, UNDERSECRETARY OF THE DEPARTMENT OF HEALTH – ABU DHABI (DOH), THE MOU WAS SIGNED BY DR. ASMA IBRAHIM AL MANNAEI, EXECUTIVE DIRECTOR OF THE HEALTH LIFE SCIENCES SECTOR AT THE DEPARTMENT OF HEALTH – ABU DHABI (DOH) AND VITOR PAPAO, GENERAL MANAGER, MIDDLE EAST, RUSSIA, TURKIYE AT GILEAD SCIENCES.
Vitor Papao, General Manager, Middle East, Russia, Turkiye at Gilead Sciences commented: “These MoUs reaffirm Gilead and Kite’s commitment to healthcare innovation and underscore our contribution to the healthcare ecosystem in Abu Dhabi. By collaborating with leading institutions, we are proud to support Abu Dhabi’s vision of becoming a leader in medical research and advanced therapeutics backed by a robust knowledge economy. This collaboration aligns with national efforts to strengthen healthcare systems, advance medical research, and expand access to lifechanging treatments, such as our innovative CAR T-cell therapies.”
ADGHW is a major government initiative from DoH and serves as a platform for innovation and collaboration under the theme ‘Towards Longevity: Redefining Health and Well-being.’ It places a strong emphasis on community-driven health and well-being, with a proactive approach centred around preventive, personalised, and holistic care. Four core themes will guide discussions and initiatives: Longevity and Precision Health; Health System Resilience & Sustainability; Digital Health & AI; and Investment in Life Sciences. By convening diverse stakeholders worldwide, ADGHW is a community without borders that seeks to advance the future of health and well-being.














A n exc e ptio n al g ro u p devote d to





ACIBADEM MOBIL
provides emergency and home care services outside of the hospital.

ACIBADEM APLUS
addresses the hygiene and catering requirements of the hospitals.
ACIBADEM HEALTH POINT ensures continuous support for patients from their arrival at Istanbul Airport until they return home, guiding them through their entire healthcare journey in Türkiye.
ACIBADEM TECHNOLOGY
develops and improves inhouse softwares including Hospital Information System and healthcare command center.
ACIBADEM UNIVERSITY
trains healthcare students to be future healthcare professionals.

ACIBADEM LABMED
offers a wide range of services including pathology, food control, stem cell and cord blood bank within the laboratory framework.
develops turnkey hospital establishment projects.
Step into a world where healthcare is not just a service, but a carefully designed ecosystem centered around Patient Safety and Patient Satisfaction – Welcome to ACIBADEM. At the forefront of innovative medical care, ACIBADEM's healthcare model is a testament to its unwavering commitment to excellence. Every facet of the healthcare journey is seamlessly integrated, with ACIBADEM collaborating with its supporting institutions at every step to mitigate risks and ensure service quality that aligns with ACIBADEM standards. Embark on a journey of cutting-edge medical services that transcend borders, as ACIBADEM extends its reach across Türkiye, Bulgaria, Macedonia, Serbia, and the Netherlands. Experience healthcare like never before, where your well-being takes center stage.

At UCLA Health, rare conditions meet expert care and real solutions.




Cedars-Sinai has been named to the Honor Roll for the ninth consecutive year in U.S. News & World Report’s “Best Hospitals 2024–25” rankings. As a global leader in healthcare, we offer a full range of services to patients from around the world. Whether we’re providing clinical services in your region via video visits or at our renowned medical center, our mission remains unchanged: to give patients access to excellence in healthcare—wherever they may be. Located in iconic Beverly Hills, Cedars-Sinai blends cutting-edge medicine in a vibrant setting known for its rich culture, famous landmarks and year-round warm weather—making it a leading destination for international patients seeking world-class treatment.


•
•
•
•
•




When former U.S. Attorney General John Ashcroft needed heart surgery, he considered only one place: the University of Chicago Medicine.
He also knew the surgeon he wanted: robotic cardiac surgery pioneer Husam H. Balkhy, MD.
“My aspiration was to go to the very best place possible,” said John Ashcroft, who served under former President George W. Bush from 2001 to 2005.
Ashcroft recently came to UChicago Medicine for removal of a papillary fibroelastoma, a growth on his aortic valve that put him at risk of a heart attack or stroke.
While reviewing images before surgery, Balkhy and his team found another problem. The patient’s aortic valve didn’t close tightly, causing blood to leak backward with each
heartbeat instead of moving out of the heart to oxygenate the body.
Balkhy, the director of robotic and minimally invasive cardiac surgery at UChicago Medicine, recommended replacing the entire aortic valve. Ashcroft was on board.
Ashcroft, who turned 82 in May, knew he wanted minimally invasive surgery that would spare him the long and sometimes difficult recovery from an open-heart procedure.
Those surgeries include a long incision and a sternotomy, where the breastbone is split and the halves spread apart to access the heart. Ashcroft worried he might never recover enough to wield a chainsaw and drive tractors on his 230-acre farm in Missouri.
Two days after Balkhy performed robotic heart surgery on March 25, Ashcroft was discharged to a Chicago hotel. The patient was
A QUICK RECOVERY FROM ROBOTIC AORTIC VALVE REPLACEMENT LEFT ASHCROFT IN GOOD SHAPE TO RECEIVE HIP REPLACEMENT SURGERY IN JULY. SIX WEEKS LATER, HE DROVE 12 HOURS TO COLORADO. HE ALSO BEGAN TEACHING THIS MONTH IN VIRGINIA.
back home three days after that, and he was able to give a speech the next month.
“We drove 500 miles at a time when, if I’d had a normal open-heart procedure, I don’t think I’d have been in any condition to do that,” Ashcroft said.
UChicago Medicine is unique in its 11 years of experience using surgical robots to perform all kinds of heart surgeries, rather than focusing on just one type of operation such as mitral valve repair. Balkhy adds that it is one of the only places in the country to perform fully endoscopic aortic valve replacement — the operation that Ashcroft had.
Endoscopic means the surgeon uses tools to look inside the body, rather than cutting it open. The patient’s breastbone remains intact, and five small incisions between the ribs allow placement of ports for the robot’s three thin “arms,” a camera and a spot to insert the replacement valve. Ashcroft's new valve is made of tissue from a cow's heart.
At the console with a high-definition, magnified view of the heart, Balkhy uses a set of controllers to precisely move the robotic arms to perform the surgery.
“Using a totally endoscopic approach leads to quick recoveries and return to activity and work,” said Balkhy, who uses robots for all of his surgeries.
Balkhy has performed more than 2,400 minimally invasive, robot-assisted cardiac procedures — including coronary artery bypass; aortic, mitral and tricuspid valve repair and replacement; ablation to correct arrhythmia; and repair of congenital defects.
The complexity of Ashcroft’s diagnosis would have ruled him out for treatment at most robotic heart surgery programs that use the technology only on the most straightforward cases, Balkhy said.
The papillary fibroelastoma erased the possibility of performing transcatheter aortic valve replacement (TAVR), a minimally invasive
procedure in which a new valve is placed, but the old one is not removed.
A quick recovery from robotic aortic valve replacement left Ashcroft in good shape to receive hip replacement surgery in July. Six weeks later, he drove 12 hours to Colorado. He also began teaching this month in Virginia.
“He’s just loving life,” said Brooke Patel, MSN, APN, CNP, a robotic nurse practitioner coordinator at UChicago Medicine. “That man, you can't keep him still. He's traveling all over the place, and he’s thankful for everything that he's been given.”
Ashcroft, who served as a U.S. senator for Missouri (1995 to 2001) and governor of Missouri (1985 to 1993), was first referred to UChicago Medicine in 2020 by John Garner, MD, Ashcroft’s cardiac electrophysiologist in Springfield, Missouri.
At UChicago Medicine, doctors performed cardiac ablation to correct an arrhythmia, and Balkhy waited in the next operating room in case further intervention was needed.
Having access to deep and specialized expertise compelled Ashcroft to stick with UChicago Medicine for his future needs.
“I just felt a real sense of confidence that this was a place that was at the very front end of the technology and was very experienced in deploying it,” Ashcroft said.
The recent surgery marked a homecoming for Ashcroft, who was born in Chicago. He attended law school at the University of Chicago, where he met his wife, Janet. Both graduated in 1967, and they were married the same year.
“Good things happen to me in Chicago,” Ashcroft said.
In a handwritten letter to University of Chicago Health System President Tom Jackiewicz, Ashcroft expressed his appreciation for Balkhy and members of the robotic cardiac surgery team “who were flawlessly helpful and patient and kind.”
“I have great appreciation for U of C,” Ashcroft wrote. “Thank you for sustaining a commitment to quality.”



Husam H. Balkhy, MD
Professor of Surgery Director, Robotic and Minimally Invasive Cardiac Surgery
Husam H. Balkhy, MD, is a pioneer in the field of minimally invasive and robotic cardiac surgery. He specializes in the treatment of coronary artery disease, heart valve disorders, atrial fibrillation and other cardiac diseases, using robotic and less invasive techniques in order to reduce pain, disability, and recovery time.























On the morning of Monday, April 14, 2025, the Jordanian capital, Amman, witnessed a distinguished humanitarian event hosted by Istiklal Hospital, the executive partner of the King Salman Humanitarian Aid and Relief Center. The event marked the official launch of the cochlear implant project for Palestinian children, made possible through a generous grant from the King Salman Center, in collaboration with the Saudi volunteer medical team and executive partnership with Istiklal Hospital.
This pioneering project aims to restore hope and hearing to Palestinian children suffering from hearing loss. It reflects the Kingdom of Saudi Arabia's deep humanitarian commitment and its strategic partnership with Jordan in the field of humanitarian healthcare.
The ceremony highlighted two core aspects of the initiative: First, the generous funding and steadfast humanitarian support provided by the King Salman Center, which continues to champion humanitarian causes across the region, and second, the advanced medical implementation by Istiklal Hospital, which provided state-of-the-art facilities and expert medical and nursing staff to ensure the project’s success at the highest standards.
A group of elite volunteer Saudi doctors participated in performing the cochlear implant surgeries at the hospital. These procedures followed a precise medical plan and were
closely monitored by both Jordanian and Saudi teams, creating an atmosphere of unity and shared humanitarian values that underscored the spirit of Arab solidarity.
Speakers at the ceremony praised Istiklal Hospital’s exceptional organizational and technical capabilities, its vital role in the project’s success, and its ability to provide a comprehensive therapeutic environment aligned with the initiative’s noble goals.
This humanitarian medical project is a practical embodiment of a comprehensive humanitarian vision and a shining example of cooperation between brothers in serving the most vulnerable groups; especially children, whose lives and futures will be profoundly transformed by these procedures.
Through this achievement, Istiklal Hospital reaffirms its status as a leading humanitarian medical center in the Kingdom and a key partner in regional and international efforts to uphold human dignity and serve those in need.
ISTIKLAL HOSPITAL
THIS HUMANITARIAN MEDICAL PROJECT IS A PRACTICAL EMBODIMENT OF A COMPREHENSIVE HUMANITARIAN VISION AND A SHINING EXAMPLE OF COOPERATION BETWEEN BROTHERS IN SERVING THE MOST VULNERABLE GROUPS—ESPECIALLY CHILDREN, WHOSE LIVES AND FUTURES WILL BE PROFOUNDLY TRANSFORMED BY THESE PROCEDURES.



April 8-11, 2025
Shanghai, China
Sept. 26-29, 2025
Guangzhou, China
Exhibitors












M42, a global health leader powered by artificial intelligence (AI), technology and genomics, announced the appointment of Dr. Moza Ajaif Al Zaabi as Chief Executive Officer of Sheikh Sultan bin Zayed Hospital in Al Batayeh, Sharjah.
Dr. Moza Ajaif Al Zaabi brings over 20 years of experience spanning clinical practice, hospital commissioning, and executive leadership. She previously served as the founding CEO of both Al Jalila Children’s Specialty Hospital and Adam Vital OrthoSpinal & Sports Medicine Hospital, where she played a pivotal role in guiding these institutions from conception to full operational excellence. A specialist in pediatrics, Dr. Moza holds a postgraduate qualification from the Royal College of Paediatrics and Child Health (UK), and a master’s degree in healthcare management from the Royal College of Surgeons in Ireland. She is also a proud alumna of the UAE Women’s Leadership Program, delivered by the Mohammed bin Rashid Center for Leadership Development - an initiative designed to empower the next generation of national leaders.
Commenting on her appointment, Dimitris Moulavasilis, Group Chief Executive Officer of M42, said: “We are thrilled to welcome Dr. Moza Ajaif Al Zaabi as the Chief Executive Officer of Sheikh Sultan bin Zayed Hospital in Sharjah. Dr. Moza's extensive experience, track record in establishing and operating major hospitals in the UAE, and dedication to healthcare excellence, make her the ideal leader to drive our mission of providing patientcentered, specialized world-class services. Her appointment underscores M42's commitment to expanding and enhancing healthcare in the region. Under her guidance, Sheikh Sultan bin Zayed Hospital will continue to thrive and set new standards in healthcare delivery."
Prior to her new role, Dr. Moza served as a Consultant Pediatrician at Al Qassimi Hospital and held an academic position as Adjunct
SHEIKH SULTAN BIN ZAYED HOSPITAL PLAYS A VITAL ROLE IN IMPROVING ACCESS TO SPECIALIZED, LONGTERM, AND POSTACUTE CARE IN THE EMIRATES. WORLDCLASS CLINICAL EXPERTS FROM M42’S NETWORK OF ESTEEMED HOSPITALS, INCLUDING IMPERIAL COLLEGE LONDON DIABETES CENTRE (ICLDC), AMANA HEALTHCARE, MUBADALA HEALTH DUBAI AND HEALTHPOINT, ARE DELIVERING ADVANCED TREATMENTS AND SPECIALIZED MEDICAL EXPERTISE FOLLOWING M42’S STRATEGIC INVESTMENT PARTNERSHIP WITH THE UAE’S MINISTRY OF DEFENCE TO MANAGE AND OPERATE THE HOSPITAL.

Clinical Assistant Professor at the University of Sharjah. She currently chairs the Innovation Panel for Healthcare Solutions, reinforcing her dedication to progressive, future-focused leadership in the healthcare sector.
Reflecting on her appointment, Dr. Moza said: “It is a privilege to lead Sheikh Sultan bin Zayed Hospital at such a dynamic point in its development. I am committed to enhancing our services, empowering our teams, and ensuring every patient receives the highest standard of care. Together, we will build upon a strong foundation and shape a forward-thinking healthcare model for the community.”
Sheikh Sultan bin Zayed Hospital plays a vital role in improving access to specialized, long-term, and post-acute care in the Emirates. World-class clinical experts from M42’s network of esteemed hospitals, including Imperial College London Diabetes Centre (ICLDC), Amana Healthcare, Mubadala Health Dubai and Healthpoint, are delivering advanced treatments and specialized medical expertise following M42’s strategic investment partnership with the UAE’s Ministry of Defence to manage and operate the hospital. This partnership marked M42’s strategic expansion into the UAE’s northern areas to transform healthcare delivery and make high-quality healthcare accessible to all segments of society.
Liquid biopsy in breast cancer – Less invasion more precision
Liquid biopsy in breast cancer – Less invasion more precision

The Plasma-SeqSensei Breast Cancer IVD Kit is an NGSbased liquid biopsy assay that focuses on highly sensitive detection of clinically relevant mutations in TP53, ESR1, PIK3CA, AKT1 and ERBB2 from blood plasma.


Learn more about the unique advantages of Plasma-SeqSensei technology
The Plasma-SeqSensei Breast Cancer IVD Kit is an NGSbased liquid biopsy assay that focuses on highly sensitive detection of clinically relevant mutations in TP53, ESR1, PIK3CA, AKT1 and ERBB2 from blood plasma.
High sensitivity at low MAFs
Learn more about the unique advantages of Plasma-SeqSensei technology
Down to 0.06% - 0.07% Mutant Allele Fractions.
High sensitivity at low MAFs
Down to 0.06% - 0.07% Mutant Allele Fractions.
Absolute quantification
Short and standardised workflow
From cfDNA samples to results in two days.
Short and standardised workflow
From cfDNA samples to results in two days.
Data analysis and reporting made easy
Generate report designed for clinicians with just a few clicks.
Absolute quantification
Meaningful comparison of ctDNA levels per millilitre of plasma.
Meaningful comparison of ctDNA levels per millilitre of plasma.
Data analysis and reporting made easy
Generate report designed for clinicians with just a few clicks.

Expert voices

‘We know that tissue samples cannot be taken regularly, but liquid biopsy is easy to take, it is simply a sample of blood. And it gives you real-time information.’
Dr Bhuwnesh Agrawal Member of The Supervisory Board


‘Even low levels of ctDNA could have given an indication of the coming progression in the follow-up.’

‘There is much more diagnostic power in the absolute quantification.’

‘We know that tissue samples cannot be taken regularly, but liquid biopsy is easy to take, it is simply a sample of blood. And it gives you real-time information.’
Sysmex Inostics and MD, Germany
Dr Bhuwnesh Agrawal Member of The Supervisory Board
Sysmex Inostics and MD, Germany
‘Even low levels of ctDNA could have given an indication of the coming progression in the follow-up.’
‘There is much more diagnostic power in the absolute quantification.’
Prof. Christopher Gebhardt UKE Hamburg, Germany
Prof. Christopher Gebhardt UKE Hamburg, Germany
Prof. Geert A. Martens AZ Delta General Hospital, Belgium
Prof. Geert A. Martens AZ Delta General Hospital, Belgium


Turnkey Healthcare Solutions
Custom solutions tailored to healthcare providers' needs

Medical Equipment Distribution
Partnerships with leading global brands to ensure quality and innovation
Pharmatrade offers a diverse portfolio of over 5000 high-quality medical and pharmaceutical products, tailored to meet the needs of both the Government and Private sectors in the UAE.
Pharmaceutical & Healthcare Product Supply
Compliance with international healthcare standards for safety and efficacy
48 Years of Excellence in UAE
Trusted partner in healthcare excellence since 1977

Research into brain tumors is progressing rapidly, fueled by a deeper understanding of the complex molecular and cellular mechanisms that lead to the development and growth of these tumors. These advances include intensive efforts to develop new and more effective treatments that target the unique characteristics of cancerous brain cells. These therapies include immunotherapy, gene therapy, and targeted therapy. Moreover, there has been significant progress in developing advanced imaging technologies that allow for earlier and more accurate diagnoses, as well as better monitoring of treatment effectiveness. Researchers are also exploring innovative methods to deliver drugs to the brain more efficiently by overcoming the blood-brain barrier, which is notoriously difficult to penetrate. Together, these developments offer promising improvements in treatment outcomes, including higher survival rates and better quality of life for patients with brain tumors.
A brain tumor is an abnormal growth of cells within the brain or central nervous system. Tumors can be either benign (non-cancerous) or malignant (cancerous). They may originate in the brain itself (primary brain tumors) or spread from other parts of the body (secondary or metastatic tumors).
There are over 120 different types of brain tumors, each with unique characteristics, growth rates, and treatment approaches. Common types include gliomas (such as astrocytomas, oligodendrogliomas, and glioblastomas), meningiomas, and pituitary adenomas. In children, the most frequent types include astrocytomas, gliomas, ependymomas, and medulloblastomas.
Benign tumors are generally slow-growing, with well-defined borders, and they rarely spread. However, they can still be dangerous if they press on vital areas of the brain. Malignant tumors, on the other hand, are cancerous, tend
to grow quickly, and can invade surrounding brain tissue.
Benign tumors typically grow slowly and are often encapsulated, making them easier to remove surgically. They do not usually spread to other parts of the brain or body. However, the term "benign" can be misleading, if such a tumor grows in a sensitive area or causes increased pressure inside the skull, it can still be life-threatening. For example, a benign tumor pressing on the brainstem can affect vital functions like breathing and heart rate. Symptoms may include severe headaches, nausea, vision problems, and seizures. As a result, even benign tumors may require treatment, such as surgery or radiation, to control their growth and relieve symptoms.
Malignant tumors are cancerous and typically grow rapidly. They often have irregular borders, making complete surgical removal more difficult. These tumors can infiltrate and destroy nearby brain tissue and, in some cases, spread to other parts of the central nervous system, such as the spinal cord. Although rare, some may metastasize outside the CNS.
Treatment for malignant tumors is usually more aggressive and may involve surgery, radiation therapy, chemotherapy, immunotherapy, targeted therapy, or a combination of these. The choice of treatment depends on the tumor’s type, size, location, spread, and the patient’s overall health.
Symptoms of brain tumors vary depending on their size, location, and growth rate. Common symptoms include persistent headaches, seizures, personality changes, muscle weakness or paralysis, vision or hearing problems, balance issues, nausea, vomiting, and cognitive difficulties. Some people may experience no symptoms in the early stages. Common symptoms include:
• Persistent Headaches: Often mild at first but become more severe over time. Headaches may worsen in the morning
A BRAIN TUMOR IS AN ABNORMAL GROWTH OF CELLS WITHIN THE BRAIN OR CENTRAL NERVOUS SYSTEM. TUMORS CAN BE EITHER BENIGN (NON-CANCEROUS) OR MALIGNANT (CANCEROUS). THEY MAY ORIGINATE IN THE BRAIN ITSELF (PRIMARY BRAIN TUMORS) OR SPREAD FROM OTHER PARTS OF THE BODY (SECONDARY OR METASTATIC TUMORS).
or with changes in position, coughing, or straining. It is important to note that most headaches are not caused by brain tumors.
• Seizures: These may be among the first symptoms. They can be localized (affecting one part of the body) or generalized (involving loss of consciousness and convulsions).
• Personality or Behavioral Changes: Tumors in the frontal lobe can alter mood, personality, decision-making, and social behavior.
• Weakness or Paralysis: Tumors can disrupt motor pathways, causing weakness or loss of movement in one limb or an entire side of the body.
• Vision or Hearing Loss: Symptoms include blurred or double vision, peripheral vision loss, hearing impairment, or ringing in the ears (tinnitus). Balance

THERE ARE OVER 120 DIFFERENT TYPES OF BRAIN TUMORS, EACH WITH UNIQUE CHARACTERISTICS, GROWTH RATES, AND TREATMENT APPROACHES.

and Coordination Issues: Tumors affecting the cerebellum or brainstem can impair balance, walking, and coordination.
• Nausea and Vomiting: These symptoms often occur in the morning and may be linked to increased intracranial pressure.
• Cognitive Impairment: Patients may experience memory issues, concentration difficulties, language problems, and reduced ability to plan or organize.
Diagnosis usually begins with a neurological examination, followed by imaging techniques such as MRI or CT scans. A biopsy is often performed to determine the tumor’s type and grade. PET scans may also be used in certain cases, especially for high-grade tumors. Diagnostic steps include:
This is a fundamental part of evaluating any suspected brain or nervous system disorder. A neurologist assesses multiple brain functions, including:
• Mental status: Assesses awareness, memory, attention, language, and thinking.
• Motor function: Evaluates muscle strength and movement.
• Reflexes: Checks for abnormalities in reflex responses.
• Coordination and balance: Tests walking ability and stability.
• Sensory function: Assesses responses
MRI is the most commonly used imaging method. It provides detailed images of the brain’s structure and is essential in identifying the size, location, and characteristics of the tumor. CT scans may be used if MRI is not possible.
A tissue sample is often required to determine the exact nature of the tumor. This can be done through a surgical procedure or a needle biopsy guided by imaging.
These are sometimes used to assess the tumor’s activity and distinguish between active tumor cells and treatment-related changes, such as necrosis or scar tissue.
• Cranial nerves: Tests functions like vision, hearing, taste, smell, eye and facial movement, swallowing, and speech.
DIAGNOSIS USUALLY BEGINS WITH A NEUROLOGICAL EXAMINATION, FOLLOWED BY IMAGING TECHNIQUES SUCH AS MRI OR CT SCANS. A BIOPSY IS OFTEN PERFORMED TO DETERMINE THE TUMOR’S TYPE AND GRADE. PET SCANS MAY ALSO BE USED IN CERTAIN CASES, ESPECIALLY FOR HIGHGRADE TUMORS.


September 18-21, 2025

Visit healthexpoiraq.iq to find out all country pavilions participating.
Iraq stands at a pivotal moment in its healthcare journey. With unprecedented government investment, ambitious national healthcare programs, and a commitment to modernization, the opportunities are extraordinary. Health Expo Iraq 2025 is your gateway to this transformative market Alongside the Exhibition, As we celebrate our milestone 5th edition, we’ve evolved from an exhibition into the region’s most influential healthcare platform -where policy meets innovation, where partnerships are forged, and where the future of Iraqi healthcare takes shape.
Comprehensive Healthcare Showcase :
• Pharmaceuticals & Medications
• Hospital Build & Infrastructure
• Healthcare IT & Digital Solutions
• Specialized Care & Services
• Medical Supplies consumables
• Medical Equipment & Devices
• Education & Training
+300
Leading Exhibitors
9
National Pavilion
+25
Participating Countries
+18K
Professional Visitors
+35 Delegates

serves as a strategic platform, bringing together health leaders, decision-makers, and experts from both the

Private hospitals across Iraq are working to enhance healthcare services and expand their capacity to meet the growing needs of citizens. These efforts align with the Iraqi government’s directives to strengthen the health sector, support the implementation of health insurance, and encourage greater integration between the private and public sectors. With the direct support of His Excellency the Prime Minister, Mr. Muhammed Shiaa Al-Sudani, and in coordination with the Iraqi Ministry of Health, private healthcare institutions aim to provide high-quality medical services and contribute to building a more sustainable and accessible healthcare system for all Iraqis.
Functional MRI provides ‘roadmap’ for surgery in previously inoperable areas of the brain
Adèle Noyer’s parents noticed the indentation in her chest as a baby. Both her father and grandfather had slight hollows, a condition called pectus excavatum, or “sunken chest syndrome,” where rib cartilage pushes the breastbone inward.
By third grade, Adèle struggled to keep up with friends and became easily breathless. Her pediatrician referred her to a surgeon at UCLA Health. The dip in her chest was measured annually, and by seventh grade, it had deepened
3 inches, reducing her stamina. In March 2024, 13-year-old Adèle underwent surgery at UCLA Mattel Children's Hospital, where surgeons placed a custom-bent titanium bar beneath her sternum.
“The bar is custom-bent to the patient's shape, and the correction is immediate,” said her pediatric general surgeon, Justin Wagner, MD.
“But the remodeling of the chest shape is the process that takes a little bit longer. That's why we'll leave the bar in for three years to allow it to heal, scar and set. Then we'll take the bar out at a second procedure.”

UCLA HEALTH’S PECTUS PROGRAM TREATS CONDITIONS IN CHILDREN AND ADULTS, FROM NON-SURGICAL INTERVENTIONS FOR MILD DEFECTS TO SEVERE CASES.
Chest wall abnormalities are fairly common, affecting 1 in 300 to 500 people, predominantly males. UCLA Health’s pectus program treats conditions in children and adults, from nonsurgical interventions for mild defects to severe cases where the breastbone compresses the heart and lungs.
“Most people going through this have a fear that there's no way the chest can look normal,” said pediatric general surgeon Veronica “Ronnie” Sullins, MD. “The majority of them are not dangerous. But, they also change over time. The ideal time to evaluate patients is during adolescence when the chest wall is changing quickly, but we care for patients from childhood to older adults.”
UCLA Health’s pectus program began in the 1960s with Eric Fonkalsrud, MD, an international authority on the management of chest wall deformities. “His teaching is so ingrained in pediatric surgery that it's hard to come across somebody who hasn't learned from him,” said Dr. Sullins, associate clinical professor of pediatric surgery at the David Geffen School of Medicine at UCLA.
Surgeons diagnose pectus excavatum through physical exams and imaging, such as X-rays or CT scans.
“The question always comes up about whether this is a functional problem or an aesthetic one, and there's definitely a component of both,” said Dr. Wagner, assistant clinical professor of pediatric surgery at the David Geffen School of Medicine at UCLA. “The first consideration is the way a patient feels and the way it's affecting their lives. If a patient says to me that they're really unhappy, that they're unable to keep up with their peers and have trouble breathing, these are major contributors to the decision to have surgery.”
Sunken chest syndrome is commonly treated with the minimally invasive Nuss procedure, which involves the insertion of a titanium bar. Surgeons use nerve cryoablation
and Enhanced Recovery After Surgery (ERAS) protocols to reduce pain and opioid use, allowing next-day discharge.
“We're correcting a defect that is formed over time,” said Dr. Sullins, “so suddenly moving the chest wall up, when it was down, can be kind of painful, especially with nerves coming around each rib. So we use a probe to freeze the nerves and make them numb for about three months.”
Most pediatricians now recognize pectus excavatum early, but older generations may delay treatment until daily life is impacted. Leigh Dannhauser, 32, dismissed her chest divot as “weird cleavage” until declining endurance and heart palpitations interfered with daily activities.
Given Dannhauser’s family history of cardiac disease, cardiologist Megan Kamath, MD, referred her to thoracic surgery. Imaging showed her sternum compressing her heart and pushing it into her lung.
Because surgeons for adult and pediatric patients collaborate closely, Dannhauser saw both during her appointment. Dr. Sullins performed the Nuss procedure in July 2022.
“When it’s a very focal defect, we sometimes need two bars to get a good correction across the entire length of the sternum,” explained Dr. Sullins. “Like a seesaw, if you put a bar where it's pointiest, then there might be some instability of that bar. We need to put in two bars so both of them can be stable.”
Dannhauser saw her smooth chest immediately after surgery, and the heart palpitations were gone. Recovery during the first month was difficult, she said, but she made it to the start of her final law school year. By graduation, she was doing CrossFit again — and even climbed Mt. Fuji.
For more information, please visit https://www.uclahealth.org/international-services/ or call +1 310-794-8759

SUNKEN CHEST SYNDROME IS COMMONLY TREATED WITH THE MINIMALLY INVASIVE NUSS PROCEDURE, WHICH INVOLVES THE INSERTION OF A TITANIUM BAR. SURGEONS USE NERVE CRYOABLATION AND ENHANCED RECOVERY AFTER SURGERY (ERAS) PROTOCOLS TO REDUCE PAIN AND OPIOID USE, ALLOWING NEXT-DAY DISCHARGE.

Dr. Clement Khoury,

The Radiation Oncology Department at Clemenceau Medical Center is equipped with cutting-edge radiation therapy technologies. Key among these is the state-of-the-art TrueBeam STx linear accelerator, featuring a high-definition multileaf collimator for precise dose modulation. The department has fostered a more integrated, patient-centered approach by expanding multidisciplinary tumor board meetings. These combined efforts have led to enhanced clinical outcomes and a better overall patient experience. “Hospitals” magazine interviewed Dr. Clement Khoury, Head of Radiation Oncology at Clemenceau Medical Center Beirut, who talked about the department and the latest advances in radiation oncology.
What are the most prominent developments the Radiation Oncology Department at Clemenceau Medical Center has witnessed recently? Over the past few years, our department
has seen transformative advancements in technology and patient care. We have adopted sophisticated techniques such as Stereotactic Radiosurgery (SRS), Volumetric Modulated Arc Therapy (VMAT), Stereotactic Body Radiation Therapy (SBRT), and Image-Guided Radiation Therapy (IGRT), which have significantly enhanced the accuracy and efficacy of cancer treatment. Furthermore, we have expanded our multidisciplinary tumor board meetings and implemented a more integrated, patientcentered care model. These changes have collectively elevated our clinical outcomes and patient experience.
What are the most important and latest devices and equipment currently available in the Radiation Oncology Department? What are their capabilities and features?
Our facility is equipped with some of the most advanced radiation therapy technologies available today. This includes a state-of-theart linear accelerator TrueBeam STx equipped with a high-definition multileaf collimator for precise dose modulation. We utilize an advanced planning system the Eclipse version 18.0.1, which support complex treatment modalities including Intensity-Modulated Radiation Therapy (IMRT) and VMAT. Daily cone-beam CT imaging is also employed for image-guided treatments to ensure precise targeting and facilitate adaptive treatment planning. Most recently, we have integrated the Varian Perfect Pitch 6 degreesof-freedom treatment couch, allowing for highly accurate patient positioning, and the Brainlab ExacTrac Dynamic system, which provides real-time tracking and submillimetric precision for intracranial and extracranial treatments by merging surface and x-ray tracking. Another feature of ExacTrac Dynamic is allowing skin marker free prepositioning for our daily treatments providing a more easy and pleasant
OUR FACILITY IS EQUIPPED WITH SOME OF THE MOST ADVANCED RADIATION THERAPY TECHNOLOGIES AVAILABLE TODAY. THIS INCLUDES A STATE-OF-THE-ART LINEAR ACCELERATOR TRUEBEAM STX EQUIPPED WITH A HIGH-DEFINITION MULTILEAF COLLIMATOR FOR PRECISE DOSE MODULATION. WE UTILIZE AN ADVANCED PLANNING SYSTEM THE ECLIPSE VERSION 18.0.1, WHICH SUPPORT COMPLEX TREATMENT MODALITIES INCLUDING INTENSITYMODULATED RADIATION THERAPY (IMRT) AND VMAT.

experience for our patients. These innovations collectively enhance our ability to deliver safe, precise, and effective radiation therapy.
Can you provide specific examples of the types of cases or tumors that are successfully treated using the technologies available in CMC?
We treat a wide array of cancer types with a high degree of success. Notable examples include the treatment of brain tumors both benign and malignant such as meningiomas and brain metastases using Stereotactic Radiosurgery (SRS). We treat early-stage lung, liver tumors and oligometastatic disease using SBRT. Head and neck malignancies, prostate and gastrointestinal primaries with VMAT. Deep Inspiration Breath Hold (DIBH) for advanced lung disease and left-sided breast tumors. The advanced technology we use allows us to deliver effective doses while minimizing damage to surrounding healthy tissue, making it especially beneficial for tumors near critical structures.
How is coordination and collaboration carried out between the Radiation Oncology Department and other departments at Clemenceau Medical Center, such as Oncology and Surgery, to ensure the best patient care?
We maintain a highly collaborative, multidisciplinary approach to cancer care. Weekly tumor board meetings bring together specialists from medical oncology, surgical oncology, radiology, and pathology to design comprehensive, individualized treatment plans. Additionally, our electronic health record system enables seamless information sharing and coordination, ensuring continuity of care and optimal treatment outcomes for our patients.
What are the procedures and protocols followed to ensure the highest levels of quality and patient
safety during treatment?
CMC is in affiliation with Johns Hopkins International and has achieved accreditation from Joint Commission International (JCI), USA. With this, CMC joins an exclusive group of hospitals worldwide, which have passed JCI's stringent clinical quality standards. Patient safety and quality assurance are foundational to our practice. We implement rigorous protocols including daily machine calibration, patientspecific quality assurance testing, and adherence to international standards such as those from AAPM and ASTRO. Every treatment plan undergoes peer review, and a safety checklist is completed before each session to confirm patient identity, treatment site, and delivery accuracy.
How do you see the role of Artificial Intelligence (AI) in improving radiation oncology processes in the near and distant future?
Artificial Intelligence is already beginning to reshape our field. AI-driven tools now assist in contouring, treatment planning, and workflow optimization. In the near term, I foresee AI enhancing our ability to tailor treatments based on predictive modeling and patient-specific data. Looking further ahead, AI will likely play a key role in real-time adaptive therapy and biologically guided radiation, ultimately driving more precise and personalized cancer care.
What is your vision for the future of radiation oncology?
My vision is for radiation oncology to evolve into a highly adaptive, biologically personalized discipline. As imaging, AI, and systemic therapies continue to advance, we will be able to tailor treatment more precisely to each patient’s tumor biology and real-time response. At CMC Beirut, we are fully committed to this future and are continually investing in the latest technologies and training to lead innovation in the region.
www.cmc.com.lb www.cmc.com.lb www.cmc.com.lb
CMC IS IN AFFILIATION WITH JOHNS HOPKINS INTERNATIONAL AND HAS ACHIEVED ACCREDITATION FROM JOINT COMMISSION INTERNATIONAL (JCI), USA. WITH THIS, CMC JOINS AN EXCLUSIVE GROUP OF HOSPITALS WORLDWIDE, WHICH HAVE PASSED JCI'S STRINGENT CLINICAL QUALITY STANDARDS. PATIENT SAFETY AND QUALITY ASSURANCE ARE FOUNDATIONAL TO OUR PRACTICE. WE IMPLEMENT RIGOROUS PROTOCOLS INCLUDING DAILY MACHINE CALIBRATION, PATIENT-SPECIFIC QUALITY ASSURANCE TESTING, AND ADHERENCE TO INTERNATIONAL STANDARDS SUCH AS THOSE FROM AAPM AND ASTRO.







International accreditation plays a vital role in raising the quality of healthcare and patient safety to global standards. By adopting the stringent standards and evaluation processes of internationally recognized bodies, healthcare institutions can demonstrate their commitment to excellence, build trust, and ultimately deliver better care to their patients in an increasingly interconnected world.
International accreditation in healthcare is a process through which healthcare institutions are evaluated by an independent external body according to a set of internationally recognized standards. Obtaining this accreditation signifies a commitment to providing safe, high-quality care that meets global benchmarks. It is a proven and effective means of elevating healthcare quality to align with international standards. Accreditation significantly contributes to improving treatment outcomes, enhancing operational efficiency, and increasing patient satisfaction, while also establishing a safe and accountable work environment.
Amid growing challenges faced by health systems worldwide, accreditation remains a key strategic option to ensure excellence and maintain public trust in the healthcare services provided. Accrediting any hospital to international standards requires strict criteria, as international accreditation bodies set comprehensive standards that cover various aspects of healthcare delivery, including patient safety, quality of care, infection control, medication management, facility safety, and ethical practices. Healthcare institutions undergo extensive on-site surveys conducted by experienced professionals from the accrediting body. These surveys assess the institution's compliance with established standards through observation, interviews, and document review.
However, accreditation is not a one-time event. Accredited institutions are usually required to demonstrate continuous efforts to monitor, evaluate, and improve their processes
and outcomes. Numerous studies indicate that accreditation programs lead to measurable and observable improvements in the quality of care for various diseases and medical conditions, such as acute heart attacks, traumatic injuries, infection control, and pain management. Accreditation encourages healthcare facilities to adopt evidence-based treatment practices, implement standardized procedures, and activate continuous quality improvement mechanisms, contributing to reduced error rates and unwanted complications.
International accreditation offers an objective and independent assessment from an external body, enabling institutions to measure their performance against globally recognized standards. Additionally, accreditation is a vital tool for risk reduction by identifying areas needing improvement and minimizing the chances of professional errors or unfavorable treatment outcomes. Key benefits of international accreditation for healthcare institutions include:
• Enhancing Patient Safety and Quality of Care: Compliance with international standards leads to the adoption of best practices, resulting in safer care environments and improved patient outcomes.
• Increasing Credibility and Trust: International accreditation serves as a mark of excellence that enhances the institution’s reputation among patients, families, healthcare professionals, and the broader community. It reflects a commitment to quality and accountability.

• Competitive Advantage: In a globalized healthcare landscape, international accreditation can distinguish an institution and attract patients seeking high-quality care. It also facilitates partnerships with international stakeholders.
• Improving Efficiency and Effectiveness: The accreditation process often drives institutions to streamline operations, optimize resource use, and enhance overall operational efficiency.
• Attracting and Retaining Talent: Healthcare professionals are often drawn to accredited institutions that demonstrate a commitment to quality and professional development.
• Risk Management and Reduction: With its focus on safety protocols and quality improvement, accreditation helps institutions mitigate risks and reduce the likelihood of adverse events.
• Access to International Markets: For institutions aiming to attract medical tourists or collaborate with international healthcare providers, accreditation can be a critical requirement.
• Optimizing Operations & Resource Use: Accreditation encourages hospitals to standardize and enhance both clinical and administrative operations, leading to more efficient resource utilization and better workflow.
• Improving Quality Management and Organizational Structure: Accreditation
drives improvements in management quality, strategic planning, and leadership, all contributing to more effective and productive hospital operations.
• Positive Impact on Service Quality and Outcomes: About three-quarters of reviewed studies indicate that accreditation enhances service quality at both organizational and administrative levels, often translating into higher productivity as processes become smoother and outcomes improve
• Fostering a Culture of Continuous Improvement: Accreditation instills a culture that values collaboration, communication, and skill development, essential elements for sustained efficiency gains.
• Sustainable and Long-Term Impact: The benefits of accreditation on efficiency and productivity extend beyond the accreditation preparation phase. They tend to persist over time, fostering organizational learning and continuous improvement.
Studies show that accredited hospitals achieve measurable improvements in operational performance, such as reduced patient length of stay and better utilization of human resources and supplies.
Accreditation fundamentally influences the quality of planning and strategy within
ACCREDITATION IS NOT A ONE-TIME EVENT. ACCREDITED INSTITUTIONS ARE USUALLY REQUIRED TO DEMONSTRATE CONTINUOUS EFFORTS TO MONITOR, EVALUATE, AND IMPROVE THEIR PROCESSES AND OUTCOMES. NUMEROUS STUDIES INDICATE THAT ACCREDITATION PROGRAMS LEAD TO MEASURABLE AND OBSERVABLE IMPROVEMENTS IN THE QUALITY OF CARE FOR VARIOUS DISEASES AND MEDICAL CONDITIONS, SUCH AS ACUTE HEART ATTACKS, TRAUMATIC INJURIES, INFECTION CONTROL, AND PAIN MANAGEMENT.


institutions by promoting integration, accountability, and continuous improvement. Its specific impacts are evident in the following areas:
• Strategic Integration and Focus: Accreditation requires institutions to align their strategic plans with defined standards, ensuring that their vision, mission, objectives, and values correspond with quality benchmarks. This integration helps institutions identify gaps and use accreditation as a tool for strategic development.
• Enhanced Accountability and Monitoring: Accreditation links planning with evaluation, holding institutions more accountable for achieving strategic goals. It ensures that plans are regularly monitored and adjusted based on assessments from accreditation activities
• Improved Stakeholder Engagement: Involving stakeholders in the accreditation process strengthens collaboration and mutual trust. These stakeholders contribute to strategic planning by
providing feedback on how accreditation standards align with the institution’s goals, ensuring comprehensive and effective planning.
• Continuous Quality Improvement: Accreditation pushes institutions to embed continuous quality improvement principles into their strategies, shifting the focus from short-term operational goals to sustained efforts toward excellence. Leaders play a key role in driving cultural changes that prioritize long-term quality improvement.
• Operational Efficiency in Planning: Incorporating accreditation into planning reduces redundancy and streamlines procedures. It enables institutions to prepare for reviews as part of routine operations rather than concentrating efforts into short timeframes.
Accreditation strengthens long-term focus on core competencies and systematic analysis, positioning institutions to effectively address future challenges.
STUDIES SHOW THAT ACCREDITED HOSPITALS ACHIEVE MEASURABLE IMPROVEMENTS IN OPERATIONAL PERFORMANCE, SUCH AS REDUCED PATIENT LENGTH OF STAY AND BETTER UTILIZATION OF HUMAN RESOURCES AND SUPPLIES.
Founded in 1915 by the legendary auto pioneer Henry Ford, this world-renowned institution transformed the way healthcare was delivered in America. With a century-long legacy of pioneering innovation, Henry Ford Health has become an epicenter for high-acuity care, groundbreaking medical research, and patientcentered healing; welcoming individuals from all corners of the world.
The Trusted Healthcare provider Henry Ford Health is a leading academic medical center serving Michigan and beyond with a full range of care; from primary and preventive services to advanced treatment in cancer, heart surgery, neurology, orthopedics, and transplant. It also offers virtual care, home healthcare, dialysis centers, comprehensive pharmacy services, and eye care for a seamless, patientcentered experience. With 50,000+ team members including over 10,000 physicians and researchers and 15,000 nurses, it ranks among Michigan’s largest employers. The system leads in medical education, training 6,000+ students and fellows annually, conducting over 3,000 research projects, and ranking among the top three NIH-funded institutions in the state.
Guided by CEO Robert G. Riney, the system operates over 550 locations, including 13 acute care hospitals and 3 behavioral health facilities. More than a healthcare provider, Henry Ford Health is a lifelong partner on each patient’s journey; delivering care that is personalized, science-driven, and compassion-led.
• Mission: To improve people’s lives through excellence in the science and art of health care and healing.
• Vision: The trusted partner in health, leading the nation in superior care and value.
• Compassion: We provide a heartfelt experience to every patient, member and each other.
• Relentless Innovation: We continuously pursue what’s possible through research, education, clinical and operational excellence.
• Global Standard of Quality: We deliver beyond expectations.
• Health Equity for All: We provide access, respect, and dignity across every culture.
• Results: We reliably deliver on our promise as leaders in safety and affordability, ensuring the health of all communities.

AT HENRY FORD HEALTH, EVERY INNOVATION, EVERY DIAGNOSIS, AND EVERY HEALING TOUCH IS GUIDED BY A CENTURY-OLD PROMISE: TO TREAT EVERY PERSON WITH DIGNITY, PRECISION, AND HOPE.
World-Class Infrastructure: A Health System Without Limits
• 13 Hospitals including the flagship Henry Ford Hospital, a major academic medical center
• 550+ Outpatient and Specialty Centers across Michigan
• Academic Alliance with Michigan State University Health Sciences
• Henry Ford Innovations: A global hub for healthcare technology and medical device development
Advance Treatment Available
• Gene therapy
• CAR T-cell therapy
• Gamma Knife
• Precision medicine
• Robotic surgery

• Henry Ford Cancer Institute
• Heart & Vascular Institute
• Neuroscience Institute
• Orthopedic and Sports Medicine Institute
• Transplant Institute- all solid organs, bone marrow and intestinal transplant
• Urology Institute
• More than $150 million in annual research awards
• 3000 active research projects
• 400+ active clinical trials
• 7,000+ learners trained annually, including 1300+ medical students and 2000+ residents and fellows
Henry Ford Health welcomes international patients seeking advanced medical expertise, with a dedicated multilingual team ensuring white-glove service:
• Virtual consultations and second opinions
• Visa assistance and personalized care navigation
• Access to clinical trials and high-acuity treatments
• Embassy and health authority support
• Interpreters, care coordinators, nurse navigators and cultural accommodation

AT HENRY FORD HEALTH, WE BELIEVE HEALING EXTENDS BEYOND MEDICINE. IT’S IN THE WAY WE LISTEN, INNOVATE, AND RELENTLESSLY PUSH THE BOUNDARIES OF WHAT’S POSSIBLE. FOR OVER 110 YEARS, WE’VE REDEFINED HEALTHCARE; NOT JUST BY TREATING ILLNESS, BUT BY EMPOWERING PEOPLE TO LIVE FULLY, WITH DIGNITY, STRENGTH, AND HOPE. WHETHER YOU’RE ACROSS THE STREET OR ACROSS THE WORLD, OUR COMMITMENT TO YOU REMAINS THE SAME: WORLD-CLASS CARE WITH A HUMAN HEART.
Key Specialties for International Patients:
• Oncology (including precision cancer therapy)
• Complex cardiac & vascular surgery
• Neurology & neurosurgery
• Organ transplants
• Orthopedic & spine surgery
• Advanced robotic and minimally invasive surgery
Awards, Accreditations and Global Trust
• Magnet® Designation for Nursing Excellence.
• Joint Commission Gold Seal of Approval.
• Top Rankings by U.S. News & World Report.
• Leapfrog “A” Ratings for Patient Safety.
• Recognized globally for cutting-edge clinical outcomes.
• Malcolm Baldrige National Quality Award recipient. One of the most prestigious awards for performance excellence, the Baldrige Award is a Presidential award presented annually to U.S. organizations by the office of the President of the United States.
• Over $500 million invested each year in community health, education, and equity to expand access, support underserved populations, and improve health outcomes.
• Leading health equity programs tackling disparities in chronic illness, maternal health, and access to care
• Reaching communities through mobile clinics and education.

More than a hospital; it's a destination of hope.
• Over 110 years of experience.
• Globally recognized experts.
• Advanced technology & personalized care.
• Seamless international patient journey.
• Unwavering commitment to preserving the dignity, respect, and humanity of every person we serve.
In 2024, Henry Ford Health launched a transformative $3 billion “Future of Health” initiative in Detroit’s New Center area. At its core is a new one-million-square-foot expansion of Henry Ford Hospital, redefining the academic healthcare campus. This visionary project includes a residential development in partnership with the Detroit Pistons (the city's professional basketball team) and a cuttingedge research facility with Michigan State University. With $375 million in philanthropic support, it will also house the world-renowned Shirley Ryan AbilityLab and the Nick Gilbert Neurofibromatosis Research Institute.
WITH OVER 10,000 PHYSICIANS, RESEARCHERS, AND ADVANCED PRACTICE PROVIDERS, THE HENRY FORD MEDICAL GROUP IS A NATIONAL LEADER IN CLINICAL EXCELLENCE AND INNOVATION. SINCE 1915, IT HAS SHAPED ADVANCES IN CANCER, NEUROSCIENCE, TRANSPLANT, AND CARDIAC CARE; SERVING PATIENTS WORLDWIDE.
With over 10,000 physicians, researchers, and advanced practice providers, the Henry Ford Medical Group is a national leader in clinical excellence and innovation. Since 1915, it has shaped advances in cancer, neuroscience, transplant, and cardiac care; serving patients worldwide.
Henry Ford Health supports over 3,000 active research projects and 400 clinical trials. In 2023 alone, it secured over $151 million in research funding. More than 7,000 medical learners, including 1,300 students and 2,000 residents; train within Henry Ford Health each year.
Henry Ford Health is extending its impact worldwide with licensed hospitals in India and the Middle East. It is advancing innovation through global tech partnerships and health initiatives in over 15 countries focused on supporting research and sustainable initiatives.
Established in 2012, Henry Ford Innovation Institute drives the commercialization of new healthcare solutions. With 50+ commercial agreements, 225 active patents, and six spin-off companies, it connects clinical discovery with real-world applications worldwide.


"I’m very excited to share that I have joined Henry Ford Health as the Director of International Business Development. The decision to make this move was an easy one, the more I learned about Henry Ford Health, the more I was inspired by its mission and commitment to patient centered care and innovation. It is an incredible honor to be part of a center that offers some of the most advanced treatments available today, including gene therapy, CAR T-cell therapy, Gamma Knife, solid organ, stem cell and bone marrow transplant, and many other groundbreaking procedures. In addition, it gives me great pleasure to share that many of our renowned physicians and wonderful nurses and clinical staff are very diverse and share the same values and culture. I’m looking forward to reconnecting with our valued partners in the Middle East and continuing to strengthen these important relationships. I’m truly excited for this new chapter and the opportunity to contribute to a world-class organization".

IN 2024, HENRY FORD HEALTH LAUNCHED A TRANSFORMATIVE $3 BILLION “FUTURE OF HEALTH” INITIATIVE IN DETROIT’S NEW CENTER AREA. AT ITS CORE IS A NEW ONEMILLION-SQUAREFOOT EXPANSION OF HENRY FORD HOSPITAL, REDEFINING THE ACADEMIC HEALTHCARE CAMPUS. THIS VISIONARY PROJECT INCLUDES A RESIDENTIAL DEVELOPMENT IN PARTNERSHIP WITH THE DETROIT PISTONS (THE CITIES PROFESSIONAL BASKETBALL TEAM) AND A CUTTING-EDGE RESEARCH FACILITY WITH MICHIGAN STATE UNIVERSITY.
In a time when respiratory diseases are surging, driven by post-COVID complications, rising air pollution, and an aging population, Northwestern Medicine is leading the charge in innovative lung care. At the helm of this mission is Dr. Momen Wahidi, an internationally recognized interventional pulmonologist and the Medical Director of the Canning Thoracic Institute. In this exclusive interview with Hospitals Magazine, Dr. Wahidi shares how multidisciplinary care, groundbreaking lung transplant programs, and cuttingedge minimally invasive technologies are transforming outcomes for patients with the most complex pulmonary conditions.
Dr. Wahidi, please tell us about yourself?
I’m an interventional pulmonologist with 20 years of experience. I joined Northwestern Medicine two years ago as Medical Director of the Canning Thoracic Institute, overseeing lung care across 11 hospitals.
How does Northwestern approach care for patients with complex lung diseases? Through a multidisciplinary approach. We build care teams that include pulmonologists, rheumatologists, surgeons, nutritionists, social workers, and others to manage every aspect of a patient’s health.
Are there treatments available before needing a transplant?
Yes. We use advanced techniques like robotic bronchoscopy and endobronchial ultrasound for early diagnosis and staging.
We’re also seeing progress with inhaled medications and biologics.
What makes Northwestern a leader in lung transplant?
We’re the top center in the U.S. by transplant volume and the first to offer post-COVID and cancer-related lung transplants. Our DREAM

program offers hope to patients with advanced lung cancer limited to the lungs.
What are the most common reasons for lung transplant today?
Severe COPD, interstitial lung disease like pulmonary fibrosis, and in some cases, lung cancer. We’re proud to be the first center globally offering lung transplants for advanced lung cancer cases.
COMPREHENSIVE INTERNATIONAL PATIENT SERVICES AVAILABLE AT NORTHWESTERN.
What are the main challenges in performing lung transplants, and do they involve living donors?
One of the biggest challenges in lung transplantation is proper patient selection. Not every patient qualifies, so a thorough evaluation is essential to ensure they are fit for surgery and free of contraindications.
Lung transplants do not involve living donors; we rely entirely on deceased donors, often individuals who have experienced catastrophic events but had healthy lungs.
We are deeply grateful to these donors and their families for their life-saving generosity.
What does the recovery process look like for patients after undergoing a lung transplant, including hospital stay, survival rates, rehabilitation, follow-up care, and physical activity?
Recovery following a lung transplant is a comprehensive and carefully monitored process that begins with a hospital stay lasting approximately 13 to 14 days, including several days in the intensive care unit.
During this critical period, patients are closely observed to manage potential complications and stabilize organ function. Once discharged, the focus shifts to meticulous follow-up care. This phase involves regular visits, bronchoscopies, and infection management protocols due to the essential use of immunosuppressants.
At Northwestern Medicine, our multidisciplinary team has achieved a remarkable one-year survival rate of around 90%; a testament to the excellence of our comprehensive care approach. Equally vital to recovery is rehabilitation, which plays a pivotal role throughout the entire journey. It starts even before surgery, addressing pre-existing symptoms, and continues post-operatively to help patients regain strength, mobility, and

lung function. To further support patients during this transition, we provide both inperson and telehealth follow-up appointments. Additionally, we incorporate home spirometry tools for remote monitoring, allowing us to track lung function in real time. For added convenience, our suburban hospital services extend care closer to patients’ homes.
Lastly, physical activity is another key component of the recovery process.
Exercise regimens are personalized to each patient’s specific needs and capabilities, with a focus on gradual but consistent movement. This structured, individualized approach not only aids in the healing process but also fosters long-term health and overall quality of life.
Do you support international patients?
Yes. We work closely with our international office, which handles coordination, language support, and cultural sensitivity. We also have partnerships in the UAE and beyond.
Would your team travel abroad for transplants?
We’re open to it; if the local infrastructure supports long-term care. We can assist with program development, training, and surgery collaboration in regions like the UAE.
What advice would you give young doctors interested in this field?
It’s an incredibly fulfilling specialty. There’s rapid advancement in tech like robotics and AI, but also growing public health risks like smoking and vaping.
Preventive care and patient education; especially about shisha and vaping; must be prioritized.
NORTHWESTERN MEDICINE PERFORMED 148 TRANSPLANTS MAKING IT THE HIGHEST-VOLUME LUNG TRANSPLANT CENTER IN THE UNITED STATES AND HAD THE SHORTEST WAIT TIME FOR A LUNG TRANSPLANT, WITH A MEDIAN WAIT TIME OF 4 DAYS
MINIMALLY INVASIVE TECHNOLOGIES LIKE ROBOTIC BRONCHOSCOPY ARE IMPROVING EARLY DETECTION. FIRST IN THE WORLD TO OFFER LUNG TRANSPLANTS FOR ADVANCED LUNG CANCER.
For more information please contact our International team on the following email; international@nm.org, or visit our website; www.northwesterninternationalhealth.com
Acıbadem Group is dedicated to fighting blood cancer and blood disorders in both adults and children through its expert teams, advanced chemotherapy and radiotherapy units, bone marrow transplantation centers, and innovative procedures such as CAR T-cell therapy.
There are various types of blood diseases, which can be either benign or malignant. In some cases, blood cells may become cancerous; in others, the body may not produce enough blood cells, or the cells produced may be defective. The most common malignant blood diseases are leukemia, lymphoma, and multiple myeloma, which are known as blood cancers. Common benign blood disorders include thalassemia, aplastic anemia, and myelodysplastic syndrome. The treatment of blood disorders requires a comprehensive and personalized approach. Depending on the condition, treatment may involve medications, chemotherapy, radiotherapy, or surgery. When these options are not sufficient, bone marrow transplantation may offer a potential cure. At Acıbadem, we provide all of these treatment modalities under one roof, eliminating the need for patients to move from one hospital to another.
In Türkiye, Acıbadem has four fully equipped Bone Marrow Transplant Centers, addressing a significant demand from patients with various conditions, including blood cancers such as leukemia, lymphoma, and multiple myeloma, as well as benign hematologic disorders like thalassemia. One of these centers, located in İstanbul, stands out as the facility performing the highest number of bone marrow transplants in the country. Every year, hundreds of families from around the world apply to Acıbadem for the treatment of complex hematologic conditions.
The most critical step in bone marrow transplantation is finding a human leukocyte antigen (HLA) matched donor for the patient. However, this can also be one of the biggest challenges. Without a fully HLA-matched donor, transplantation was traditionally not possible.

IN TÜRKIYE, ACIBADEM HAS FOUR FULLY EQUIPPED BONE MARROW TRANSPLANT CENTERS, ADDRESSING A SIGNIFICANT DEMAND FROM PATIENTS WITH VARIOUS CONDITIONS, INCLUDING BLOOD CANCERS SUCH AS LEUKEMIA, LYMPHOMA, AND MULTIPLE MYELOMA, AS WELL AS BENIGN HEMATOLOGIC DISORDERS LIKE THALASSEMIA.
Thanks to advancements in this field, even in the absence of a fully matched donor, halfmatched (haploidentical) related donors can now be safely used in stem cell transplantation. This development has significantly expanded the donor pool. Potential donor matches are primarily sought among first-degree relatives, including siblings, children, or parents.
Over the past 10 years, advances in technology, the development of new medications, and increased clinical experience have significantly improved the outcomes of haploidentical stem cell transplantation. Today, this method is widely used and achieves high success rates. At Acıbadem, nearly 25% of all allogeneic bone marrow transplants are currently performed using haploidentical donors.
Even though families are ready to donate bone marrow to save a loved one, a matching relative may not always be found. In this scenario, there is one final option: stem cells can be sourced from national or international bone marrow banks, which may have an unrelated fully matched donor. In such cases, Acıbadem focuses on identifying suitable donors through national and international registries and succeeds in finding matches for nearly half of the patients

who apply. One key resource is TÜRKÖK, Türkiye’s national bone marrow bank, which is the sixth largest in the world. Thanks to TÜRKÖK, matched donors are found for a significant number of patients from around the globe receiving care at Acıbadem.
Despite today’s advanced chemotherapy, radiotherapy, and bone marrow transplantation methods, these treatments may not always lead to the desired outcome. In such cases, CAR T-cell therapy offers a promising and innovative option. This treatment involves enhancing the ability of T cells, which are found in the blood, to recognize and destroy cancer cells by genetically modifying them in the laboratory. Acıbadem is among the few hospitals worldwide that not only administer CAR T-cell therapy but also have the capability to produce CAR T-cells on site. This allows Acıbadem to create personalized CAR T-cells specifically for patients with lymphoma or leukemia when needed.
OVER THE PAST 10 YEARS, ADVANCES IN TECHNOLOGY, THE DEVELOPMENT OF NEW MEDICATIONS, AND INCREASED CLINICAL EXPERIENCE HAVE SIGNIFICANTLY IMPROVED THE OUTCOMES OF HAPLOIDENTICAL STEM CELL TRANSPLANTATION. TODAY, THIS METHOD IS WIDELY USED AND ACHIEVES HIGH SUCCESS RATES.


With over two decades of experience in global healthcare and an unwavering commitment to innovation, Hein van Eck is at the helm of Mediclinic Middle East, steering one of the UAE’s most respected healthcare providers into a new era. From his early career as a healthcare actuary in South Africa to leading one of the region’s largest healthcare ecosystems, Van Eck’s journey is rooted in data-driven decision-making and people-centered care. In this exclusive interview with Hospitals Magazine, he discusses Mediclinic’s expansive vision, the integration of AI and digital health, and the Middle East’s unique position to lead global transformation in healthcare delivery.
Mr. Van Eck, can you tell us about your background and your journey to becoming CEO of Mediclinic Middle East?
I’m from South Africa, my accent usually gives that away quickly. I started my career as a
healthcare actuary, initially working on the insurance side of the industry. Back in 2005, I was part of a team that negotiated provider tariffs, which led me to encounter Mediclinic. They eventually offered me a role, and I’ve now been with the organization for 20 years. I moved to the Middle East in 2014 to support the development of insurance pricing, analytics, health policy, and revenue cycle management.
I’ve been in my current position as CEO for two years now, and it’s been an incredibly rewarding experience.
How do you view the current healthcare landscape in the Middle East?
It’s an exceptionally exciting time for healthcare in this region. One of the biggest advantages here is the absence of legacy systems that often hinder innovation elsewhere. In many parts of the world, introducing new technologies can be challenging due to regulatory inertia and entrenched systems. In contrast, the Middle East is forward-looking,
MEDICLINIC IS PART OF A LEADING INTERNATIONAL HEALTHCARE GROUP WITH OPERATIONS IN SWITZERLAND, SOUTH AFRICA, AND OF COURSE, THE MIDDLE EAST. HERE IN THE UAE, WE’VE BUILT A COMPREHENSIVE ECOSYSTEM ACROSS THE CONTINUUM OF CARE; WITH 7 HOSPITALS AND 29 CLINICS.
with governments that embrace innovation and digital transformation. The willingness to implement AI and data-driven systems, combined with agile governance, is propelling the region ahead, and I believe it will soon outpace many global healthcare systems in areas like Artificial Intelligence and machine learning.
Where does Mediclinic position itself in this dynamic market?
Mediclinic is part of a leading international healthcare group with operations in Switzerland, South Africa, and of course, the Middle East. Here in the UAE, we’ve built a comprehensive ecosystem across the continuum of care; with 7 hospitals and 29 clinics. But it doesn’t stop there: we’re involved in IVF through our Bourn Hall brand, home-based care, telemedicine, home dialysis, and even command centerstyle patient coordination through our Care Collaboration Centre. Our strategic focus is personalization, offering tailored clinical and administrative experiences for our customers, not just our patients. We believe in being a healthcare partner for individuals across all stages of health, including when they’re well.
So, personalized care is the foundation of Mediclinic’s future?
Absolutely. Personalized care, supported by advanced AI, is the future. We’re entering a phase where lab testing will become more affordable and accessible, and AI will assist, or even lead clinical decision-making. Family medicine, while irreplaceably human in many ways, will increasingly benefit from AI support. We aim to proactively serve patients based on their preferences, medical history, and behavioral data, instead of sending standard communications. It’s about relevance, convenience, and outcomes.
How has the transition from Chief Strategy Officer to CEO changed your perspective? It’s been a whirlwind - challenging, but incredibly energizing. I’ve been fortunate to work alongside an exceptional team. I’m naturally collaborative, and I don’t pretend to have all the answers. But I do know the right questions to ask and when to rely on the data.
One of the biggest differences is the breadth of responsibilities that come with the CEO role. The data-driven mindset that I developed as an actuary continues to serve me well, especially when navigating complex decisions. You don’t always have perfect data, but knowing how to evaluate it and when it’s sufficient to act is key.
Can you share examples of how Mediclinic is using AI to enhance operations?
One standout case is our “no-show bot,” developed using the DataRobot AI platform and UiPath automation. No-shows—patients who book appointments and don’t arrive—are a major issue in healthcare. Our predictive model analyzes patient behavior to estimate the likelihood of attendance with up to 96% accuracy. This allows us to free up appointment slots, optimize scheduling, and ultimately reduce waiting times for others. It’s a great example of how AI can solve real-world healthcare inefficiencies.
And how has Mediclinic scaled its digital health infrastructure post-COVID? COVID was a turning point. We significantly expanded our digital health strategy. Today, our Care Collaboration Centre—essentially a command hub staffed by doctors and nurses remotely monitors hundreds of chronic patients. During COVID, we cared for over 1,000 elderly patients remotely. Today, we’re still managing around 500 patients this way. We conduct about 20,000 teleconsultations and nearly 100,000 online bookings monthly. Digital health is now deeply embedded in our ecosystem, from virtual consults to home care, pharmacy delivery, and in-home doctor visits. But we’re also focused on seamless Integration - digital health must complement physical care, not replace it.
Has demand for telemedicine remained steady post-pandemic?
It has come down, but settled at a higher base than pre-Covid levels and continued increasing over time. While in-person consultations remain the preferred choice for many, telemedicine has found a strong niche, particularly for chronic and follow-up cases. We use it strategically where it
WE ARE PROUD TO BE A LONG-TERM PARTNER IN THE UAE’S HEALTHCARE ECOSYSTEM. WE WORK CLOSELY WITH THE GOVERNMENT ON INITIATIVES SUCH AS EMERGENCY PREPAREDNESS, ORGAN TRANSPLANTATION, AND THE PROMOTION OF DIGITAL AND VIRTUAL HEALTH. WE’VE PERFORMED OVER 70 KIDNEY TRANSPLANTS AND ARE STRONG ADVOCATES FOR PRIMARY AND PREVENTATIVE HEALTHCARE.
enhances convenience without compromising care. That said, widespread adoption also depends on reimbursement models. Currently, teleconsultations are reimbursed at about half the rate of physical ones. Closing that gap would incentivize broader adoption.
How does Mediclinic balance growth and innovation with maintaining high standards of care?
Quality is deeply rooted in our DNA, thanks to our founder, Dr. Edwin Hertzog. His philosophy still guides us: when a doctor is with a patient, the only focus should be on quality care. Only outside that consultation room should we consider financial sustainability, efficiency, or business concerns. That principle allows us to act ethically, even when insurance coverage is limited. We provide care first, because it’s the right thing to do.
What are the key challenges facing the healthcare sector in the region?
Margin squeeze is a pressing issue, rising costs, pricing pressures, and increasing competition make efficiency critical. AI and automation offer tremendous potential to reduce administrative overhead. Another challenge is managing the influx of new technologies. Every day, we receive proposals from tech companies pitching innovations. Evaluating and integrating the right ones without missing the next breakthrough, is a constant balancing act.
What role does Mediclinic play in supporting the UAE’s healthcare strategy?
We are proud to be a long-term partner in the UAE’s healthcare ecosystem. We work closely with the government on initiatives such as emergency preparedness, organ transplantation, and the promotion of digital and virtual health. We’ve performed over 70 kidney transplants and are strong advocates for primary and preventative healthcare. However, the funding model for primary care still needs to evolve to better incentivize its utilization. Formalizing that structure will be key to longterm sustainability.
Sustainability is an important aspect of
modern healthcare. How is Mediclinic addressing environmental responsibility?
We’re deeply committed to sustainability. During COP28, two of our hospitals received the Department of Health’s Emerald Award for environmental excellence. We’re implementing solar panel infrastructure, using clean energy across our campuses, and recycling tens of thousands of liters of water daily from our air conditioning systems, used for irrigation and cleaning. Sustainability is not a side project; it’s an operational priority.
How does your participation in Abu Dhabi Global Health Week align with Mediclinic’s mission?
This event resonates strongly with our vision. We’re proud to be long-standing partners with the Department of Health, and the caliber of speakers and participants here is world-class.
The conference reflects where UAE healthcare is headed, and we’re proud to help shape that future.
What upcoming initiatives can we expect from Mediclinic?
We’re continuing to grow. We’re investing AED 120 million into expanding Mediclinic Airport Road Hospital, adding operating theatres and 50 more beds to meet increasing demand. That facility is evolving into a major healthcare campus. We’re also looking to expand some of our other hospitals by nearly 50% and are exploring new hospital opportunities. We’ll be announcing more details later this year, inshallah.
Finally, what advice would you give to aspiring healthcare leaders entering the industry?
First, take the time to understand the Big picture, how healthcare systems function, how regulators think, and how policies are shaped. Healthcare is incredibly complex, and leaders need to be informed across all levels. Second, stay connected to the ground. Don’t just rely on PowerPoint presentations. Visit clinics. Talk to staff. Observe patients. The reality on the ground often tells a more accurate story than the boardroom ever will. It’s a lesson I live by every day.
FIRST, TAKE THE TIME TO UNDERSTAND THE FULL PICTURE, HOW HEALTHCARE SYSTEMS FUNCTION, HOW REGULATORS THINK, AND HOW POLICIES ARE SHAPED. HEALTHCARE IS INCREDIBLY COMPLEX, AND LEADERS NEED TO BE INFORMED ACROSS ALL LEVELS. SECOND, STAY CONNECTED TO THE GROUND.


Acıbadem Healthcare Group is a leading destination for kidney and liver transplantation worldwide. Many patients from across the world choose Acıbadem in Türkiye for their treatment, attracted by their multidisciplinary approach, extensive experience, innovative surgical techniques, high success rates, and patient-centered international service.
Organ transplantation is a deeply emotional journey. A healthy donor willingly undergoes surgery to give part of their organ, offering someone else a chance to survive. The recipient, in turn, holds on to life through this act of generosity. Today, organ transplantation is possible for various organs. However, the two organs with the highest need for
transplantation, as well as the most frequently transplanted and with the highest success rates, are the kidney and liver.
Professor Hamdi Karakayalı, one of the pioneers in organ transplantation in the country and the head of Acıbadem Atakent Hospital Organ Transplantation Center, highlights the center’s capacity and expertise: “At Acıbadem, we perform both liver and kidney transplantations, primarily relying on living donors in our transplantation program. Acıbadem serves as a referral center not only for Türkiye but also for the wider region. Many patients travel from abroad with their donors to undergo transplantation at our center. My team and I have extensive experience
KIDNEY TRANSPLANTATION IS THE TRANSFER OF A HEALTHY KIDNEY TO A PERSON WHOSE KIDNEYS HAVE NO ACTIVITY. ALTHOUGH DIALYSIS CAN PARTIALLY COMPENSATE FOR THE LOSS OF KIDNEY FUNCTION, IT IS NOT A PERMANENT CURE.
in this field. I have performed more than 2,500 liver transplantations and over 4,000 kidney transplantations. At Acıbadem, in this hospital alone, we have conducted 1,500 liver transplantations and more than 1,000 kidney transplantations in the past 10 years.”
Acıbadem has impressive success rates in both kidney and liver transplantation. The survival rate for kidney transplantation is nearly 99%, and for liver transplantation, our success rate is almost 90%, both of which are especially notable compared to the success rates of other countries performing living donor transplantations.
When the liver can no longer function properly, it is called liver failure. If it is not treated, it will progress to death. A liver transplant is the only solution, as survival is not possible without a functioning liver. There are two types of liver transplants based on the donor source: living donor and deceased donor transplantation. The liver is uniquely suited for living donor transplants because it is the only organ in the human body that can regenerate. When a donor gives more than half of their liver for transplantation, the remaining portion can continue functioning without serious complications. In fact, the liver can still perform its functions even when up to 70% of it is removed.
Kidney transplantation is the transfer of a healthy kidney to a person whose kidneys have no activity. Although dialysis can partially compensate for the loss of kidney function, it is not a permanent cure. There are two types of kidney transplantation regarding the donor types: from living donors and from deceased donors. A living person can donate a kidney because, after donating one, they can continue to live a healthy, normal life with the remaining kidney. More than 3.500 kidney transplants are performed in Türkiye annually, and 85% of them are done with living donors. This number makes Türkiye first country for living donor kidney transplantations in the world.
Beyond performing thousands of surgeries, having an expert team, using state-of-the-art technology, and achieving success rates of up to 99%, perhaps our most remarkable aspect is our ability to touch lives by performing surgeries on babies as young as 5–6 months old, weighing only 4.5 kilograms. Babies may suffer from congenital genetic diseases that lead to liver or kidney failure, requiring organ transplants. However, only a limited number of centers worldwide perform these surgeries. At Acıbadem, our team has extensive experience in this field. Today, liver and kidney transplantation procedures are performed at Acıbadem’s four organ transplantation centers: two in Istanbul and one each in Izmir and Bursa. If you’d like to learn more, visit acibademinternational.com and share your condition with us through the contact form. Our expert team will get in touch with you within a few hours.
ACIBADEM HAS IMPRESSIVE SUCCESS RATES IN BOTH KIDNEY AND LIVER TRANSPLANTATION. THE SURVIVAL RATE FOR KIDNEY TRANSPLANTATION IS NEARLY 99%, AND FOR LIVER TRANSPLANTATION, OUR SUCCESS RATE IS ALMOST 90%, BOTH OF WHICH ARE ESPECIALLY NOTABLE COMPARED TO THE SUCCESS RATES OF OTHER COUNTRIES PERFORMING LIVING DONOR TRANSPLANTATIONS..


In an era of rapidly evolving healthcare landscapes, academic medical institutions are redefining their global footprint. At the forefront of this shift is the University of Chicago Medicine, an academic powerhouse that is not only delivering world-class care, but also creating new pathways in healthcare diplomacy, international education, and advanced medical technology. Dialla Atassi, Chief of Global and National Programs at UChicago Medicine, has spent the past decade expanding the institution’s reach across five continents. In this exclusive interview with Hospitals Magazine, she discusses the strategic balance between national and global healthcare initiatives, the power of culturally sensitive patient care, and how technology and AI are shaping the future of academic medicine.
Ms. Atassi, can you tell us about your background and your role at the University of Chicago Medicine?
My name is Dialla Atassi, and I joined the University of Chicago Medicine ten years ago. For the past four years, I have been leading our
Global and National Programs. Over this time, we have dramatically expanded our reach across the world. Our focus spans three major pillars: patient care services, training and education— both clinical and non-clinical—under our Global Education Center, and international advisory and consultancy services. Our mission is to share our expertise and extend our academic medicine model beyond borders.
How do you manage and differentiate strategies between national and international healthcare partnerships?
While national and international collaborations share some commonalities, they are inherently distinct markets. For our national initiatives, we build upon the strong reputation of our physicians and Centers of Excellence, which are widely recognized throughout the U.S. Our strategy for global expansion, however, involves a completely different approach. Internationally, we must understand and adapt to diverse healthcare systems, regulatory frameworks, and cultural contexts. We’re not just competing with other U.S. institutions— we’re entering entirely different ecosystems across continents, which requires agility, sensitivity, and deep-rooted partnerships.
Can you tell us about some of your most impactful international programs?
One of our most meaningful recent initiatives is our telestroke program between Chicago and the United Arab Emirates. This program allows for real-time, virtual stroke care; from diagnosis to post-stroke management between our clinical teams and physicians abroad. The ability to respond quickly to stroke symptoms can dramatically improve outcomes or even save lives. This kind of program reflects our core mission: to offer world-class care, no matter the geography, and to do so with urgency and precision.
ONE OF OUR MOST MEANINGFUL RECENT INITIATIVES IS OUR TELESTROKE PROGRAM BETWEEN CHICAGO AND THE UNITED ARAB EMIRATES. THIS PROGRAM ALLOWS FOR REALTIME, VIRTUAL STROKE CARE; FROM DIAGNOSIS TO POST-STROKE MANAGEMENT BETWEEN OUR CLINICAL TEAMS AND PHYSICIANS ABROAD. THE ABILITY TO RESPOND QUICKLY TO STROKE SYMPTOMS CAN DRAMATICALLY IMPROVE OUTCOMES OR EVEN SAVE LIVES. THIS KIND OF PROGRAM REFLECTS OUR CORE MISSION: TO OFFER WORLD-CLASS CARE, NO MATTER THE GEOGRAPHY, AND TO DO SO WITH URGENCY AND PRECISION.
How do you identify promising opportunities for global partnerships?
We’ve built a trusted global network over the years, rooted in the strength of the University of Chicago brand, consistently ranked among the top ten universities in the world. This network includes existing partners who actively seek collaboration with us, as well as regional offices in five continents that help us build new connections. Our presence on the ground, combined with our academic and clinical reputation, makes us a sought-after partner in many regions.
What metrics do you use to evaluate the success of these partnerships?
Several key performance indicators guide us. These include brand recognition in international markets, the strength and loyalty of our partner relationships, and patient return rates. One of the most important indicators of success is patient trust. When patients and partners continue to return and recommend our services, it’s a testament to the quality and consistency of the care and collaboration we provide.
How is technology transforming your global outreach efforts?
Technology is one of the core pillars of our global strategy. We offer a robust remote second-opinion program in multiple languages, operating 24/7. We also provide comprehensive telehealth services: doctorto-doctor, doctor-to-patient, telestroke, telepathology, and teleradiology. These virtual services allow us to expand our reach and offer continuity of care in real time. They’re not supplemental, they’re essential to how we deliver academic medicine globally.
And how does artificial intelligence fit into your operations?
AI is deeply embedded in our day-to-day work. In fact, the University of Chicago has developed proprietary AI software integrated into our electronic medical records. These tools help with everything from auto-diagnosis to clinical documentation optimization. AI enhances
efficiency and precision in both clinical decision-making and patient workflows. It’s not just a trend, it’s the future, and we’re actively shaping how it will be used in healthcare.
Cultural sensitivity is vital in global healthcare. How do you ensure that across programs?
Cultural sensitivity is a cornerstone of our international approach. Our global team collectively speaks nine languages, and we’ve created a workforce that reflects the cultural, religious, and dietary needs of our patients. We tailor each consultancy or partnership proposal to fit the unique culture of the country we’re working with.
On the patient services side, we ensure accommodations for religious practices, provide access to halal meals, and create a welcoming environment for every patient, whether they are inpatient or outpatient. This cultural adaptability is part of our everyday operations.
Can you share a success story from one of your global patient programs?
One of the strongest indicators of our success is the consistent return of patients and the growth of our program through word-ofmouth. Our international program operates 24 hours a day, 365 days a year, in multiple languages. Patients know they can rely on us, even if they call at 3 a.m., there’s someone available to support them. That level of responsiveness and trust is something we’ve worked hard to build and maintain.
What are the biggest challenges you face when managing national and international programs?
One major challenge is the increasing level of global competition among healthcare providers. Another is the evolution of healthcare systems in many of the countries we work with. As these countries develop their own infrastructures and services, we must stay agile and adapt our models to complement, rather than compete with, local systems. That includes providing support in capacity building, training, and longterm development strategies.
TECHNOLOGY IS ONE OF THE CORE PILLARS OF OUR GLOBAL STRATEGY. WE OFFER A ROBUST REMOTE SECONDOPINION PROGRAM IN MULTIPLE LANGUAGES, OPERATING 24/7. WE ALSO PROVIDE COMPREHENSIVE TELEHEALTH SERVICES: DOCTORTO-DOCTOR, DOCTOR-TO-PATIENT, TELESTROKE, TELEPATHOLOGY, AND TELERADIOLOGY. THESE VIRTUAL SERVICES ALLOW US TO EXPAND OUR REACH AND OFFER CONTINUITY OF CARE IN REAL TIME. THEY’RE NOT SUPPLEMENTAL, THEY’RE ESSENTIAL TO HOW WE DELIVER ACADEMIC MEDICINE GLOBALLY.

How do you view the future of academic medicine on a global scale?
Academic medicine holds a unique and powerful position in the future of healthcare. Unlike standalone hospitals, academic institutions are anchored by research, innovation, and evidence-based care. The integration of AI, telemedicine, and clinical trials will further strengthen this role. The institutions that can rapidly adapt to these innovations will lead the way—and I believe the University of Chicago is already doing just that.
What kind of support does your team provide for international patients seeking care in Chicago?
We offer a complete 360-degree patient experience. Before patients even arrive, our intake team proactively connects with them
to understand their medical needs and ensure every detail is prepared; from arranging dialysis or oxygen support to accessibility needs like wheelchairs. We also provide complimentary transportation between the airport, housing, and medical appointments. Every patient is assigned a coordinator who speaks their language, and our on-call system operates around the clock, every day of the year.
Once the patient arrives, we assist with housing, cell phone service, banking, and even meal planning. Throughout their treatment, we ensure they follow their doctor’s care plan, and after discharge, we support them through virtual follow-up consultations. We also coordinate communication with their home physicians to ensure a seamless transition and continuity of care. This is academic medicine with a mission, and it extends far beyond clinical walls.
WE OFFER A COMPLETE 360-DEGREE PATIENT EXPERIENCE. BEFORE PATIENTS EVEN ARRIVE, OUR INTAKE TEAM PROACTIVELY CONNECTS WITH THEM TO UNDERSTAND THEIR MEDICAL NEEDS AND ENSURE EVERY DETAIL IS PREPARED; FROM ARRANGING DIALYSIS OR OXYGEN SUPPORT TO ACCESSIBILITY NEEDS LIKE WHEELCHAIRS. WE ALSO PROVIDE COMPLIMENTARY TRANSPORTATION BETWEEN THE AIRPORT, HOUSING, AND MEDICAL APPOINTMENTS. EVERY PATIENT IS ASSIGNED A COORDINATOR WHO SPEAKS THEIR LANGUAGE, AND OUR ON-CALL SYSTEM OPERATES AROUND THE CLOCK, EVERY DAY OF THE YEAR.



In the pursuit of optimal skin health and rejuvenation, innovative treatments continue to emerge. One such advancement is the Morpheus8 treatment, a revolutionary approach combining microneedling and radiofrequency energy. This technique, highlighted by Dr. Hassan Galadari, offers a comprehensive solution for various skin concerns, addressing both superficial imperfections and deeper structural issues. This overview delves into the specifics of Morpheus8, exploring its benefits, suitability, and the science behind its effectiveness.
What is Morpheus8 treatment, and how does it improve skin health?
Morpheus8 is an innovative skin treatment that blends microneedling with radiofrequency
(RF) energy to remodel and rejuvenate the skin at multiple depths. It stimulates collagen production, tightens tissue, and enhances overall skin quality. Morpheus8 delivers deep fractional remodeling unlike other treatments, addressing surface imperfections and underlying structural concerns. The result? Smoother, firmer, and more youthful-looking skin with long-lasting benefits. For those looking for overall skin tightening and lifting, Morpheus8 Prime offers a tailored approach for delicate areas like under the eyes and around the lips.
Who is a good candidate for Morpheus8? What skin concerns does it help with?
Morpheus8 is ideal for improving skin texture, firmness, and elasticity. It’s a perfect treatment for males or females. I had it myself. It treats
MORPHEUS8 IS IDEAL FOR IMPROVING SKIN TEXTURE, FIRMNESS, AND ELASTICITY. IT’S A PERFECT TREATMENT FOR MALES OR FEMALES. I HAD IT MYSELF.
fine lines, wrinkles, acne scars, enlarged pores, and skin laxity. Whether you’re in your 30s trying to maintain youthful skin or in your 50s looking to restore firmness, Morpheus8 is a highly adaptable treatment that can cater to various skin types and concerns. For those struggling with uneven skin tone, texture, or superficial imperfections, Morpheus8 Resurfacing is an excellent choice for refining and smoothing the skin.
How does Morpheus8 combine microneedling and radiofrequency, and why is this effective?
Morpheus8 integrates the precision of microneedling with the deep-penetrating power of RF energy. The microneedles create micro-injuries, triggering the body's natural healing response, while RF energy heats the deeper layers, tightening existing collagen and stimulating new production. This powerful combination enhances skin remodeling, improving both surface-level imperfections and deeper structural concerns for maximum rejuvenation. Morpheus8 (24 tips) is designed for faster treatments with enhanced comfort, making it a great option for those looking for efficiency without compromising results.
What kind of results can patients expect from Morpheus8 treatment, and how soon do these results become noticeable?
Everything is a journey. Patients typically notice improvements in skin texture and firmness within a few weeks. The most dramatic results appear over the next three months as collagen regeneration continues. Expect a more lifted, smoother, and refreshed look with benefits that last up to a year or more. Consistency and proper post-care can further enhance and extend the results. Morpheus8 Body specifically targets larger treatment areas like the abdomen, arms, and thighs for those looking for the best in body contouring and skin tightening.
Is Morpheus8 treatment painful, and are there any downtime or side effects associated with the procedure?
Morpheus8 is designed to be a comfortable experience, with a topical anesthetic applied beforehand to minimize discomfort. Some patients may feel a mild heat sensation, which is generally well tolerated. Post-treatment, you may experience slight redness, swelling, and pinpoint bruising, which typically subsides within 24 hours. Most patients return to their normal activities quickly, making it a convenient option for those with busy schedules.
How many sessions of Morpheus8 treatment are recommended to achieve optimal results?
Every skin type is unique. For the best outcome, three sessions spaced four to six weeks apart are typically recommended. However, some patients significantly improve with just one session, while others may benefit from additional treatments depending on their skin concerns and goals.
Are there any age restrictions for patients considering Morpheus8 treatment, or is it suitable for people of all ages?
Morpheus8 is suitable for adults of all ages. While it is commonly sought after by individuals in their 30s and beyond for anti-aging benefits, younger patients with acne scars or early signs of skin laxity can also benefit from its collagenboosting effects. However, always consult with your doctor first.
Can Morpheus8 be used to treat different areas of the body, or is it mainly for the face? What areas tend to see the most significant improvement?
Morpheus8 is not just for the face, it can treat various body areas, including the neck, chest, arms, abdomen, and knees. Morpheus8 Body offers a specialized approach to improve skin laxity, reduce stretch marks, and smooth out irregular textures for those seeking a targeted body treatment. Here are four essential Morpheus8 tips for achieving the best results: 1. Hydration is Key: Drink plenty of water before and after your treatment to help your skin recover and maximize collagen production.
MORPHEUS8 DELIVERS DEEP FRACTIONAL REMODELING UNLIKE OTHER TREATMENTS, ADDRESSING SURFACE IMPERFECTIONS AND UNDERLYING STRUCTURAL CONCERNS. THE RESULT? SMOOTHER, FIRMER, AND MORE YOUTHFUL-LOOKING SKIN WITH LONGLASTING BENEFITS. FOR THOSE LOOKING FOR OVERALL SKIN TIGHTENING AND LIFTING, MORPHEUS8 PRIME OFFERS A TAILORED APPROACH FOR DELICATE AREAS LIKE UNDER THE EYES AND AROUND THE LIPS.

2. Sun Protection Matters: Avoid direct sun exposure post-treatment and always wear SPF to prevent hyperpigmentation.
3. Consistency Enhances Results: A series of Morpheus8 Body sessions delivers the best long-term firming and smoothing effects.
4. Pair with Lifestyle Choices: Healthy nutrition and regular exercise can further enhance and prolong the skin-tightening benefits.
What are the long-term benefits of Morpheus8 treatment for skin health?
Will patients need to schedule follow-up treatments?
Morpheus8 delivers long-term benefits, including improved skin texture, firmness, and a youthful glow. While results are long-lasting, maintenance sessions once or twice a year can help sustain collagen production and keep skin looking its best.
Are there any pre-treatment or posttreatment care instructions that patients must follow for the best outcome?
Before your Morpheus8 session, avoid excessive sun exposure and discontinue retinoid use a few days prior. After treatment, hydration is essential, and applying sunscreen diligently will
help protect the skin as it heals. Patients should also avoid strenuous activities and excessive heat exposure for several days.
Can Morpheus8 be combined with other skin treatments for better results?
Absolutely! Morpheus8 pairs well with IPL treatment (before the treatment), exosomes, PRP, and injectables like botulinum toxins or dermal fillers. These complementary treatments can amplify rejuvenation and provide even more dramatic results.
What sets Morpheus8 apart from other skin rejuvenation treatments available today, and why should consumers consider it part of their skincare routine?
Morpheus8 is unique because it penetrates deeper than traditional microneedling or lasers, providing superior collagen stimulation and lasting skin tightening.
It is effective for all skin types and has minimal downtime, making it an excellent choice for those seeking a high-tech, noninvasive solution to aging and skin texture concerns. Whether for the face or body, Morpheus8 delivers exceptional, sciencebacked results, making it a powerful tool in any skincare routine.
MORPHEUS8 IS UNIQUE BECAUSE IT PENETRATES DEEPER THAN TRADITIONAL MICRONEEDLING OR LASERS, PROVIDING SUPERIOR COLLAGEN STIMULATION AND LASTING SKIN TIGHTENING. IT IS EFFECTIVE FOR ALL SKIN TYPES AND HAS MINIMAL DOWNTIME, MAKING IT AN EXCELLENT CHOICE FOR THOSE SEEKING A HIGHTECH, NON-INVASIVE SOLUTION TO AGING AND SKIN TEXTURE CONCERNS. WHETHER FOR THE FACE OR BODY, MORPHEUS8 DELIVERS EXCEPTIONAL, SCIENCE-BACKED RESULTS, MAKING IT A POWERFUL TOOL IN ANY SKINCARE ROUTINE.


Migraines are more than just headaches, they are a chronic and often debilitating neurological condition that affects nearly 15% of the global population, with a significant impact on quality of life. While various non-invasive treatments offer temporary relief for some, a large proportion of patients continue to suffer despite medication, alternative therapies, and lifestyle changes.
In this exclusive interview with HOSPITALS Magazine, Mark Adams, CEO of CMC Hospital Dubai, sheds light on one of the most promising developments in migraine care: nervedecompression surgery. Once an accidental discovery during cosmetic procedures, this technique has evolved into a precise and potentially life-changing intervention for chronic migraine sufferers.
SURGERY IS THE ONE THAT CAN REALISTICALLY BE CONSIDERED A POTENTIAL CURE RATHER THAN A TEMPORARY RESPITE.
Can migraine surgery end the misery of headache pain?
The severe and debilitating effects of migraine attacks can severely impair quality of life. A chronic neurovascular disorder, migraine largely occurs in adults between the ages of 20 and 50. It affects around 15% of the global population, with women suffering disproportionately.
Causing intense headache pain and nausea, as well as hypersensitivity to light or noise, migraines have long been treated with a combination of pain relief and preventative medication. Quick relief is elusive for many sufferers, and where traditional medications have failed, people have often turned to non-traditional methods in a search for pain relief and a long-term cure. Chinese herbal medicine (CHM) has emerged in Western cultures as a viable alternative for some patients, and there is a body of evidence from clinical trials in China that suggests CHM, commonly used to treat migraines in China outside clinical settings, can be an effective shortterm and long-term treatment.
But despite the pervading narratives that often champion “non-invasive” treatments, migraine surgery – technically known as nervedecompression surgery – can provide the relief that many fail to find from alternative therapies. Indeed, it’s estimated that up to one-third of migraine sufferers in the US find no relief at all from existing non-invasive treatments. Elsewhere, the proportion of patients who don’t respond to pharmacologic treatments ranges from 20% to 50%. And whilst there’s a chance that nerve-decompression surgery won’t always provide a long-term cure for the misery of chronic migraines, around 60% to 80% of people who’ve undergone migraine surgery report that, one year on, they experienced no further migraines.
What non-invasive treatments are available?
Short-term prescription or over-the-counter pain relief is the most common treatment for one simple reason: it allows some patients to return to a semblance of normality and enjoy a better quality of life in the short term. But overuse of these medications can, in many

cases, cause so-called rebound headaches, leaving sufferers back at square one. CHM can offer temporary or longer-term respite for some sufferers, and clinical trials have shown that patients reported improvements in severity and frequency after taking commonly used herbs fu ling and chuan xiong, as well as herbal formulae such as chuan xiong cha tiao san and yi qi cong ming tang. An array of preventative treatments can be prescribed depending on the frequency, intensity, and nature of a patient’s migraines, as well as the patient’s health profile and comorbidities. For example, simple blood-pressure medication can be effective in some cases, as can antidepressants and antiseizure drugs. Even Botox injections at 12-week intervals have helped reduce or cure migraines in some patients.
External, drug-free tech devices controlled by smartphones are also available as an alternative to pharmacological treatments. These rely on electrical magnetic stimulation of the nerves to target migraine pain at a patient’s trigger points. Known as neuromodulation, these devices usually cause no side effects. With some targeting prevention and others designed to offer acute relief, there’s little doubt that they offer some sufferers another option to manage migraine pain more effectively.
And in this digital age, it’s probably not surprising that there’s a digital treatment as an adjunct to standard migraine treatments for episodic migraines – fewer than 15 headache days per month – that remaps the brain, based on research that faulty brain circuits are the root cause of many diseases. In short, there’s now an app that can help retrain and rewire the brain by guiding sufferers through a carefully curated set of in-app tasks.
Nerve-decompression surgery: a viable treatment for a permanent cure
IT’S ESTIMATED THAT UP TO ONETHIRD OF MIGRAINE SUFFERERS IN THE US FIND NO RELIEF AT ALL FROM EXISTING NON-INVASIVE TREATMENTS. ELSEWHERE, THE PROPORTION OF PATIENTS WHO DON’T RESPOND TO PHARMACOLOGIC TREATMENTS RANGES FROM 20% TO AS HIGH AS 50%. AND WHILST THERE’S A CHANCE THAT NERVEDECOMPRESSION SURGERY WON’T ALWAYS PROVIDE A LONG-TERM CURE FOR THE MISERY OF CHRONIC MIGRAINES, AROUND 60% TO 80% OF PEOPLE WHO’VE UNDERGONE MIGRAINE SURGERY REPORT THAT, ONE YEAR ON, THEY EXPERIENCED NO FURTHER MIGRAINES.

Migraine surgery is suitable for candidates already diagnosed with migraines or occipital neuralgia by a neurologist, and for whom alternative therapies either give no relief or cause unbearable side effects. Also commonly referred to as nerve-release surgery, it began life as an accidental by-product of cosmetic-surgery techniques during brow-lift procedures in the US; it transpired that releasing a nerve behind a patient’s eye also gave unexpected relief from migraine pain. To this day, nerve decompression procedures are carried out by qualified cosmetic surgeons rather than neurologists.
Migraine surgery has come a long way since then, with a greater understanding of how compression and irritation of sensory nerves, such as the trigeminal and occipital nerves around a sufferer’s head, can cause migraines and their associated pain. Known as trigger points, surgery can release the compression across a variety of sites where trigger pain is found through the neurolysis of sensory
branches of the occipital and trigeminal nerves at temporal and endonasal sites. These principal pain zones are typically located in the back of your head, spreading to behind the eyes (occipital); around the temples (temporal); above the eyes or forehead (frontal) or inside a patient’s nose and behind the eyes (rhinogenic). Of course, patients can often present with more than one trigger point, and such symptoms will dictate how surgery is ultimately conducted.
That surgery involves either an open or endoscopic procedure to decompress and relieve the pressure in nerves and blood vessels at frontal or temporal trigger sites, via an uppereyelid incision or small, discrete incisions above the hairline. If both sites need simultaneous treatment, based on a patient’s symptoms, a surgeon may choose the same upper-eyelid incision to deal with both sites. The occipital and rhinogenic trigger sites are treated slightly differently, with the former performed via a discrete vertical or horizontal incision across the
EVIDENCE FROM A WIDE ARRAY OF CLINICAL STUDIES CARRIED OUT OVER MORE THAN 20 YEARS SUGGESTS SUCCESS RATES FOR COMPLETE AND PERMANENT ELIMINATION OF MIGRAINE SYMPTOMS CAN BE AS HIGH AS 80%. IN SHORT, THERE’S CAUSE FOR CAUTIOUS OPTIMISM.
back of the skull, while the latter is personalised depending on how a cosmetic surgeon assesses individual patients.
It’s worth mentioning here that candidates for nerve decompression surgery should have a realistic expectation of surgery, as even the most minor of procedures bear a degree of risk that it may not achieve the desired outcome. That said, with debilitating, chronic life-changing pain, the risk-reward equation will often favour intervention, and evidence from a wide array of clinical studies carried out over more than 20 years suggests success rates for complete and permanent elimination of migraine symptoms can be as high as 80%. In short, there’s cause for cautious optimism.
And whilst the obvious corollary to that success rate is the fact that one-fifth of patients undergoing surgery see no lasting difference at all, research has found that the most likely causes of failure in migraine surgery stem not from a patient’s suitability for surgery or otherwise, but rather from an inability to accurately determine the migraine trigger sites. As one recent paper on the efficacy of triggersite surgery published in the US National Library

of Medicine notes, “the most common reason for a partial clinical response is the failure to identify all trigger sites or inadequate surgery on the trigger sites.” That, or when pain in one site is so acute, it masks symptoms at another.
Surgical intervention for migraines has emerged as a viable treatment option for patients with a clinical diagnosis of neuralgia, and for whom pain relief and preventative pharmacological treatment are ineffective or, worse still, cause undesirable side effects. With most procedures completed on an outpatient basis in just a few hours, the vast majority of patients who choose surgical intervention as a long-term cure for migraine pain will see either immediate results or will experience a gradual but inexorable improvement during their recovery. As far as anti-migraine options go, surgery is the one that can realistically be considered a potential cure rather than a temporary respite.

WITH MOST PROCEDURES COMPLETED ON AN OUTPATIENT BASIS IN JUST A FEW HOURS, THE VAST MAJORITY OF PATIENTS WHO CHOOSE SURGICAL INTERVENTION AS A LONG-TERM CURE FOR MIGRAINE PAIN WILL SEE EITHER IMMEDIATE RESULTS OR WILL EXPERIENCE A GRADUAL BUT INEXORABLE IMPROVEMENT DURING THEIR RECOVERY. AS FAR AS ANTI-MIGRAINE OPTIONS GO, SURGERY IS THE ONE THAT CAN REALISTICALLY BE CONSIDERED A POTENTIAL CURE RATHER THAN A TEMPORARY RESPITE.

Applied Healthcare Solutions, is a dynamic force in the Middle Eastern healthcare landscape. The company has strategically positioned itself as a key player in the UAE with a significant reach across the entire MENA region, leveraging deep industry expertise and cutting-edge technology to deliver premium medical equipment and services. “Hospitals” magazine interviewed Ramsey Hout, founder of Applied Healthcare Solutions, who shared his insights and how they are shaping healthcare solutions across the region.
What are the key priorities for Applied Healthcare Solutions in serving the healthcare needs?
Based in the UAE with reach across the entire
MENA region, Applied Healthcare Solutions is a dynamic medical equipment distributor leveraging deep industry expertise and cuttingedge technology to provide premium products and services. Our commitment to consultancy and project management allows us to offer tailored solutions, driving operational efficiency and market growth for our clients.
What are the specific areas covered by your company?
Operating within the healthcare sector, our organization delivers value through four distinct service lines:
1. Medical Equipment Distribution: In today's rapidly advancing healthcare
WE’RE TRANSFORMING HOSPITAL OPERATIONS THROUGH SMART LOGISTICS SOLUTIONS THAT REDUCE MANUAL WORKLOAD, SPEED UP WORKFLOWS, AND LET HEALTHCARE PROFESSIONALS FOCUS ON WHAT MATTERS MOST; PATIENT CARE.
landscape, access to top-tier, dependable medical equipment is paramount. Applied Healthcare Solutions ensures healthcare professionals are equipped with state-of-the-art tools that enhance diagnostic precision, surgical efficacy, and ultimately, patient well-being. Our distribution service offers a carefully selected range of advanced products that meet both global benchmarks and specific local healthcare requirements.
2. Parapharma Distribution:
As healthcare increasingly emphasizes prevention and comprehensive wellness, parapharmaceuticals are vital in supporting medical treatments and promoting patient recovery. Applied Healthcare Solutions offers a wide array of para-pharmaceutical products, blending medical effectiveness with consumer appeal, including dietary supplements, nutraceuticals, and advanced skincare solutions that cater to the growing demand for scientifically validated wellness products.
3. Consulting:
Healthcare organizations navigate a challenging environment of regulations, operational hurdles, and rapidly evolving technologies. Applied Healthcare Solutions provides expert consultation services designed to guide them through these complexities. We offer customized, data-driven strategies aligned with their objectives and the specific dynamics of the Middle East market.
4. Project Management:
Achieving successful healthcare projects requires meticulous planning, precise execution, and the ability to adapt to the sector's evolving needs. Applied Healthcare Solutions delivers comprehensive project management services, ensuring that initiatives, from hospital renovations to technology deployments and supply chain transformations, are completed on schedule, within budget, and in alignment with client goals.
How do you specifically invest in technological advancements, expertise,
and strong relationships to achieve your mission of boosting healthcare in the Middle East?
At Applied Healthcare Solutions, we invest in technological advancements by carefully selecting innovative, clinically proven medical equipment and digital health solutions that address real operational gaps in healthcare facilities. We prioritize partnerships with global manufacturers that offer next-generation technologies; such as smart disinfection systems, automated lab solutions, to ensure our clients stay at the forefront of medical innovation. We build expertise through continuous training, both internally and with our partner suppliers. Our team undergoes regular product certifications and hands-on training to ensure we can offer not just equipment, but endto-end consultation, implementation, and aftersales support tailored to each market’s needs. We foster strong relationships by maintaining a close and transparent dialogue with hospitals, clinics, procurement authorities, and medical professionals across the region. By understanding their evolving challenges, we act not just as a supplier, but as a strategic partner committed to elevating care standards and driving long-term impact in the Middle East healthcare ecosystem.
What specific aspects of healthcare excellence in the Middle East do you aim to revolutionize, and what will that revolution look like in practice?
Applied Healthcare Solutions is enhancing healthcare in the Middle East by focusing on several key areas, some of which are integrating technologies like lab automation and intelligent storage to streamline operations and improve patient care. Our deployment of advanced UVC LED disinfection systems offers rapid, chemicalfree disinfection in critical areas such as ICUs and emergency rooms, reducing the risk of hospitalacquired infections. Additionally, we provide ergonomic medical furniture and pediatric solutions designed to boost patient comfort and well-being. Together, these initiatives aim to elevate care quality, reduce errors, and increase patient satisfaction across the region. More advanced technologies tailored to the region are on the way.

THIS IS JUST THE BEGINNING; MANY MORE INNOVATIONS ARE ON THE WAY AS WE CONTINUE TO SOURCE AND DELIVER ADVANCED HEALTHCARE TECHNOLOGIES TAILORED TO THE REGION’S EVOLVING NEEDS.

During an interview with ‘Hospitals’ magazine, Dr. Elias Zgheib, plastic and reconstructive surgeon, discussed RevolaxTM filler, emphasizing its strong safety record and established presence in the market. He explained that, unlike many fillers that utilize biphasic hyaluronic acid, RevolaxTM employs a monophasic structure where all hyaluronic acid chains are of uniform length, have greater long-term stability, and more predictable outcomes than biphasic fillers.
Could you share a concise overview of your professional journey and current focus?
I'm a plastic and reconstructive surgeon with over a decade in the field, having completed my plastic surgery studies at the American University of Beirut Medical Center. My advanced training includes plastic and reconstructive surgery, cleft work at Great Ormond Street Hospital in the UK, and trauma reconstruction at the Royal London Hospital. For the past ten years, my focus has been on aesthetics. I've also been a Key Opinion Leader for injectables for about five to six years, most recently with Botulax and RevolaxTM, and I serve on the medical advisory board for injectables in the UAE. I am the representative for Aesthetic Plastic Surgeons of Lebanese Descent (APSLD) in the GCC region, which includes the UAE, Oman, Saudi Arabia, Qatar, and Kuwait. While my current practice is primarily cosmetic and aesthetic surgery, I continue to be involved in cleft lip with the Global Smile Foundation.
What is RevolaxTM, and how does it differ from other dermal fillers?
RevolaxTM, a hyaluronic acid dermal filler manufactured by the South Korean company Hugel (a major player in the industry), has been available since around 2017. Unlike many fillers that use biphasic hyaluronic acid, RevolaxTM features a monophasic structure where all the hyaluronic acid chains are the same length. This manufacturing difference results in a more uniform consistency and, importantly, contains less of the free cross-linking agent BDDE. Consequently, RevolaxTM is associated with reduced inflammation and swelling, greater long-term stability, and more predictable outcomes than biphasic fillers.
What types of RevolaxTM fillers are available, and how do you choose the right one for a patient?
The success of a RevolaxTM treatment hinges on a thorough consumer examination to pinpoint the areas needing filler and to select the most suitable RevolaxTM type. There are three types – Fine, Deep, and Sub-Q – each with the same
hyaluronic acid concentration but different levels of thickness and firmness, making them appropriate for different skin layers. The doctor's expertise is crucial not only in choosing the right RevolaxTM product for the specific treatment area and skin thickness but also in determining the correct amount and injection technique. Experience allows practitioners to achieve optimal results, sometimes even surpassing outcomes from treatments using larger quantities of filler administered by less experienced individuals.
How soon after the injection can consumers expect to see results with RevolaxTM?
Unlike toxins, which typically take several days to a week to show effects, dermal fillers like RevolaxTM provide almost immediate results. This initial outcome represents about 80% to 90% of the final result. Over the following 10 days to two weeks, the filler integrates well with the tissues and, being hydrophilic, attracts some water, leading to a further increase of 5% to 10% in volume. The ultimate result is usually visible after about two weeks, once any injectionrelated swelling or bruising has subsided.
How long do the results of RevolaxTM fillers typically last?
Research suggests that monophasic fillers like RevolaxTM tend to last at least 20% longer than other available fillers.
The duration of filler results varies depending on the specific type used. The finer RevolaxTM tends to have a shorter lifespan compared to the firmer Sub-Q, which has more cross-linking. The injected area also plays a role; for instance, lip fillers typically don't last as long as those in the under-eye area or cheeks due to movement breaking down the filler.
Regarding downtime, there isn't a specific recovery period. Consumers are generally advised to refrain from exercise for about 24 hours. Any downtime experienced is usually related to potential bruising from the injection itself, not the filler product.
Are RevolaxTM fillers safe? What kind of
UNLIKE TOXINS, WHICH TYPICALLY TAKE SEVERAL DAYS TO A WEEK TO SHOW EFFECTS, DERMAL FILLERS LIKE REVOLAXTM PROVIDE ALMOST IMMEDIATE RESULTS. THIS INITIAL OUTCOME REPRESENTS ABOUT 80% TO 90% OF THE FINAL RESULT.
testing and approvals do you have?
RevolaxTM is a certified product, having passed ISO and CE testing, and is the top-selling filler in the UK. It's distributed across 29 countries, with a production volume exceeding 30 million syringes. A key aspect of RevolaxTM's safety profile lies in its distinct manufacturing process. After the initial 24-hour cross-linking, the filler undergoes a thorough two-week dialysis purification. This crucial step eliminates residual unbound materials, specifically BDDE (known to cause inflammation), and any other nonhyaluronic acid components. Furthermore, RevolaxTM utilizes a sterilization technique involving high heat followed by rapid cooling, which contributes to its enhanced safety and stability. Consequently, it's considered a very safe and pliable filler with no reported adverse bodily reactions.
How does the texture and feel of RevolaxTM compare to other popular fillers?
The G prime value of RevolaxTM, which indicates the filler's firmness, varies by type: Sub-Q has a G prime of 300, Deep is 200, and Fine is 100. Importantly, when injected correctly, the product does not clump and is highly moldable. This moldability is a key feature, allowing for easy adjustment if a small lump is felt after injection. The texture is such that it integrates seamlessly with the surrounding tissues, feeling natural and without causing lumps, granulomas, or other complications.
What should the consumer do before and after the procedure to ensure the best results?
All right. So, if the lady is taking any anticoagulation that can be stopped or if she is basically exercising, She should preferably stop any anticoagulation. She should not exercise the day of the procedure. Obviously, after the filler is injected, in certain areas I tell the ladies to massage it so that there's not much swelling and so that it is distributed evenly. But then again, if the filler is injected properly in the right place and in the right amount, there shouldn't be any issues and the results should last long.
Do you have any further thoughts or comments regarding RevolaxTM?
When we look at the dermal fillers available on the market, there's a significant number of them. And it's common to see several new fillers, at least four or five, being introduced regularly. One of the positive aspects of RevolaxTM is that, despite it being a Korean product – and some people might initially have reservations about Korean beauty products, the reality is quite different. Korea has an exceptionally high standard of aesthetics. I visited there a couple of months ago, and the level of advancement in this field is unparalleled globally.
While perhaps earlier technologies weren't as advanced, Korea now possesses the leading technology worldwide. So, in terms of product development and manufacturing, RevolaxTM is extremely safe and has been on the market for a considerable time. From a practitioner's perspective, I appreciate RevolaxTM because I haven't observed any adverse reactions in my consumers, it is safe and gives me reproducible and controllable results This isn't the case with all fillers; some don't respond well to manipulation and are difficult to control after injection So, overall, I have a genuine positive opinion of RevolaxTM."
THE G PRIME VALUE OF REVOLAXTM , WHICH INDICATES THE FILLER'S FIRMNESS, VARIES BY TYPE: SUB-Q HAS A G PRIME OF 300, DEEP IS 200, AND FINE IS 100. IMPORTANTLY, WHEN INJECTED CORRECTLY, THE PRODUCT DOES NOT CLUMP AND IS HIGHLY MOLDABLE.

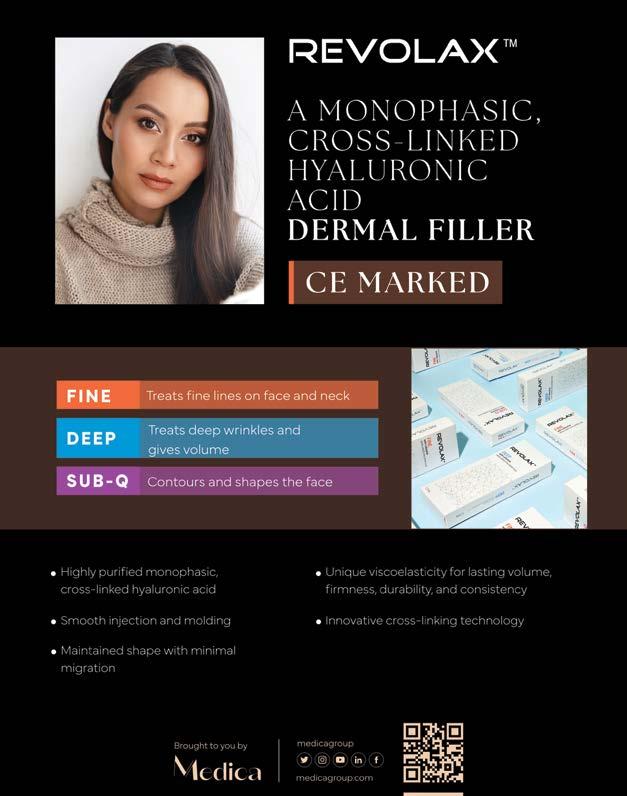


Treating obesity requires a comprehensive and integrated approach that focuses on long-term lifestyle and health behavior changes. The main methods of treating obesity:
A healthy diet is based primarily on reducing daily calorie intake so it is less than what the body burns, this is the foundation of weight loss. Equally important is focusing on increasing the consumption of nutrient-rich foods, such as:
• Fresh fruits
• A variety of vegetables
• Whole grains that provide energy and fiber
• Lean proteins that help build muscle and increase satiety
• Low-fat dairy products that provide calcium and essential vitamins
It is also essential to learn how to control portion sizes. Knowing how much food is appropriate and avoiding overeating helps maintain caloric balance and prevent weight gain.
Regular physical activity is a key part of a healthy lifestyle and is effective for both weight loss and maintenance. This includes aerobic exercises such as:
• Brisk walking
• Running
• Swimming
• Cycling
It is recommended to engage in at least 150 minutes of moderate aerobic exercise per week, or 75 minutes of vigorous-intensity exercise per week. Strength training is also important for increasing muscle mass, which boosts the basal metabolic rate (BMR), meaning the body burns more calories even at rest. It's recommended to engage in strength training that targets major muscle groups at least twice per week.
Behavioral change is a key component of achieving and maintaining weight loss.
It starts with:
• Setting realistic and measurable goals, which help track progress and maintain motivation
• Self-monitoring to understand behaviors related to eating and physical activity by:
1. Logging meals and food types
2. Recording exercise (type, duration, and intensity)
3. Regularly tracking weight
In addition to lifestyle changes, medication may be used as a supplemental method for people with severe obesity or health conditions requiring medical intervention. Weight-loss medications work through various mechanisms such as:
• Suppressing appetite
• Inhibiting fat absorption in the intestines
Weight-loss injections have become increasingly common. These are subcutaneous injections that help individuals with obesity or related conditions lose weight by:
• Regulating appetite
• Reducing food intake
These medications are used in conjunction with a reduced-calorie diet and increased physical activity. It is essential to consult a specialist before starting any medication to determine its suitability, explain proper use, and discuss potential side effects. It's important to remember that medication is only one part of a comprehensive weight-loss plan that includes continued commitment to healthy habits for long-term success.
There are several non-surgical procedures for weight loss, such as:
A relatively non-surgical weight-loss treatment. When injected into the stomach muscles, Botox works by:
• Slowing gastric emptying, helping food stay in the stomach longer and creating a feeling of fullness
IT IS ESSENTIAL TO CONSULT A SPECIALIST BEFORE STARTING ANY MEDICATION TO DETERMINE ITS SUITABILITY, EXPLAIN PROPER USE, AND DISCUSS POTENTIAL SIDE EFFECTS. IT'S IMPORTANT TO REMEMBER THAT MEDICATION IS ONLY ONE PART OF A COMPREHENSIVE WEIGHT-LOSS PLAN THAT INCLUDES CONTINUED COMMITMENT TO HEALTHY HABITS FOR LONG-TERM SUCCESS.
• Reducing the secretion of ghrelin, the hormone responsible for stimulating appetite
The procedure is done via upper endoscopy, where a flexible tube with a camera is inserted through the mouth into the stomach. Botox is then injected into specific areas of the stomach wall. It takes about 15–20 minutes and typically requires only mild sedation or local anesthesia.
Who qualifies for gastric Botox?
• Individuals with a BMI between 27 and 35
• Those who did not succeed with diet and exercise alone
• People looking for a less invasive alternative to surgeries like gastric sleeve or bypass
• Those who are medically fit for Botox and endoscopy
A non-surgical method that involves inserting a medical-grade silicone balloon into the stomach and filling it with sterile saline. The balloon:
• Takes up space in the stomach, helping the patient feel full faster
• Reduces the amount of food consumed in each meal
• May delay gastric emptying, which increases the sense of satiety
The gastric balloon is a temporary method. It is removed after 6 to 12 months, depending on the type and the physician's recommendation.
Bariatric surgery is often reserved for individuals with:
• A BMI of 40 or higher, or
• A BMI of 35 or higher with serious obesityrelated health problems
• Who have not succeeded with other weightloss methods
Sleeve Gastrectomy (Gastric Sleeve)
One of the most commonly performed and effective surgeries for treating severe obesity. It is approved by health authorities globally due to its significant impact on:

• Weight loss
• Improving or curing type 2 diabetes Reducing blood pressure
• Improving lipid profiles
How it works: Approximately 80% of the stomach is removed, leaving a narrow tube or "sleeve" that limits food intake and reduces the secretion of the hunger hormone ghrelin, resulting in reduced appetite.
Surgery results: Most patients lose 50–70% of their excess weight within the first 12–18 months post-operation. It also leads to significant improvement in overall quality of life.
Treating obesity requires a personalized and integrated approach. Although diet, exercise, and behavior change are essential, many people may need additional medical, minimally invasive, or surgical treatments to achieve lasting results. Choosing the appropriate treatment should be made in collaboration with healthcare professionals, taking into account the individual's medical condition, personal goals, and commitment to long-term change. A comprehensive approach ensures not only weight loss but also improved quality of life, health, and well-being.
IT IS RECOMMENDED TO ENGAGE IN AT LEAST 150 MINUTES OF MODERATE AEROBIC EXERCISE PER WEEK, OR 75 MINUTES OF VIGOROUS-INTENSITY EXERCISE PER WEEK. STRENGTH TRAINING IS ALSO IMPORTANT FOR INCREASING MUSCLE MASS, WHICH BOOSTS THE BASAL METABOLIC RATE (BMR), MEANING THE BODY BURNS MORE CALORIES EVEN AT REST. IT'S RECOMMENDED TO ENGAGE IN STRENGTH TRAINING THAT TARGETS MAJOR MUSCLE GROUPS AT LEAST TWICE PER WEEK.

Provided by Baylor St. Luke's Medical Center
Along with medical support, nutrition is key to managing kidney disease. For those with compromised kidney function, the foods you eat or avoid can even prevent kidney disease from progressing. The renal diet exists to help people with diabetes or kidney disease and can be customized for each individual’s health needs. Read on to learn how this diet works and what it can include.
What is the renal diet?
Kidneys filter and remove waste from the blood, so waste can build up and cause issues when they don't function properly. A renal diet focuses on reducing the amounts of sodium, phosphorus, and protein a person consumes to make their kidneys’ work easier. It also emphasizes the importance of limiting fluids and eating high-quality protein. Some people may also benefit from limiting potassium and calcium in their diets; it’s important to work with your doctor or dietitian to develop the right diet for your individual needs.
What foods should I avoid in a renal diet?
Foods containing the following substances are typically limited in a renal diet.
Sodium is one of the three major electrolytes in the body. Too much sodium can build up in people with compromised kidney function, leading to symptoms like excessive thirst, swelling, high blood pressure, heart failure, and shortness of breath. To limit sodium, try these tips:
• Choose fresh fruits and vegetables or canned and frozen produce with no salt added.
• Always read food labels to understand how much sodium is in a product.
• Limit sodium to 150 mg per snack and 400 mg per meal.

• Cook at home and do not add salt to your food.
This mineral is found naturally in the body, as well as in the foods we eat. It helps to keep the heartbeat regular and muscles working properly. It also helps maintain the balance of fluid and electrolytes. When the body cannot remove excess potassium from the bloodstream, it can cause muscle weakness, irregular heartbeat, a slow pulse, or a heart attack. To limit potassium, avoid salt substitutes and seasonings with potassium, and limit foods that are high in potassium. These can include:
• Citrus juices
• Bananas
• Fish
• Avocado
• Potatoes
• Spinach
Phosphorus aids bone development and maintenance and supports the development of connective tissues and organs. High levels of
SODIUM IS ONE OF THE THREE MAJOR ELECTROLYTES IN THE BODY. TOO MUCH SODIUM CAN BUILD UP IN PEOPLE WITH COMPROMISED KIDNEY FUNCTION, LEADING TO SYMPTOMS LIKE EXCESSIVE THIRST, SWELLING, HIGH BLOOD PRESSURE, HEART FAILURE, AND SHORTNESS OF BREATH.
phosphorus can pull calcium from the bones, weakening them, and can lead to calcium deposits in the lungs, heart, eyes, and blood vessels. To prevent a buildup of this mineral, pay attention to food labels to avoid packaged foods that are high in phosphorus. Some foods that are high in phosphorus include:
• Soda
• Cheese
• Fast food
• Meat
• Seeds
• Canned fish
• Milk
Protein
Kidney patients typically need a low-protein diet, but the amount of protein recommended in a renal diet changes based on what stage of kidney disease a person is in. Protein is an essential nutrient that promotes tissue maintenance, so work with your nephrologist and dietitian to learn how much protein is recommended for you. As always, read nutrition labels to see how much protein is in the foods you’re eating.
As you can probably tell from the previous foods to avoid, controlling the amount of fluid in the body is vital for people with kidney disease. When fluid builds up, it can put pressure on the heart and lungs. While maintaining a healthy level of electrolytes is essential, you should also consider the amount of fluids you’re consuming as well. Your nephrologist can help you understand how much fluid your body needs. Here are things to be aware of when monitoring fluid intake:
• Count all foods that melt at room temperature (for example, popsicles or gelatin).
• Consider all fluids used in cooking.
• Do not drink more than your doctor orders.
What foods are good to include in a renal diet?
Depending on your overall health, your doctor or nutritionist may recommend different diets.

One diet that is common for people with kidney disease is the DASH (Dietary Approaches to Stop Hypertension) diet. This way of eating is rich in produce, low-fat dairy, whole grains, beans, and nuts. However, talk to your doctor to learn what’s right for you. In general, here are a few things to eat that can help you balance the nutrients in your body.
Foods low in potassium
If you’re used to drinking citrus juice to regulate blood sugar, you can easily switch to apple, grape, or cranberry juice instead. These juices are lower in potassium and can help you regulate this mineral. Other foods low in potassium include peaches, carrots, green beans, white bread and pasta, rice milk, cooked rice and wheat cereals, and grits. Foods low in phosphorus
Some packaged or deli foods can have phosphorus added to them, so always check the label for words with “phosphorus” or “PHOS” in the ingredients. Some foods that are lower in phosphorus include fresh fruits and vegetables, bread, pasta, rice, and corn and rice cereals.
Healthy amounts of protein
To protect your kidneys, it’s important to regulate the amount of protein you consume. A portion of chicken, fish, or meat is about 2-3 ounces; roughly the size of a deck of cards. Understand how much protein is in the foods you eat, including plant-based protein, which is found in foods like beans, nuts, and grains. Because the amounts of these nutrients suggested for you vary based on what stage of kidney disease you’re in, as well as numerous other health factors, it’s important to discuss the renal diet with a St. Luke’s Health nephrologist. They can recommend what’s right for you and help answer any questions about meal planning, keeping a food diary, and followup care. Before making any changes to your regular diet or lifestyle, talk with a Baylor St. Luke's Medical Group primary care physician.
TO PROTECT YOUR KIDNEYS, IT’S IMPORTANT TO REGULATE THE AMOUNT OF PROTEIN YOU CONSUME. A PORTION OF CHICKEN, FISH, OR MEAT IS ABOUT 2-3 OUNCES; ROUGHLY THE SIZE OF A DECK OF CARDS. UNDERSTAND HOW MUCH PROTEIN IS IN THE FOODS YOU EAT, INCLUDING PLANTBASED PROTEIN, WHICH IS FOUND IN FOODS LIKE BEANS, NUTS, AND GRAINS. BECAUSE THE AMOUNTS OF THESE NUTRIENTS SUGGESTED FOR YOU VARY BASED ON WHAT STAGE OF KIDNEY DISEASE YOU’RE IN, AS WELL AS NUMEROUS OTHER HEALTH FACTORS, IT’S IMPORTANT TO DISCUSS THE RENAL DIET WITH A ST. LUKE’S HEALTH NEPHROLOGIST.

Provided by Baylor St. Luke's Medical Center
According to the National Kidney Foundation, chronic kidney disease (CKD) affects about 37 million people in the U.S. alone, and about 90% of those don’t even know they have it. The only cure for stage 5 CKD is a kidney transplant, but before that, many people receive ongoing treatment through dialysis, a simple procedure that performs the functions of a healthy kidney.
If you receive a CKD diagnosis, your nephrologist will work to determine what stage you are currently experiencing. There are five stages, with stage 1 meaning your kidneys are functioning at about 90-100% of their normal capacity due to some kidney damage and stage 5 meaning your kidneys are functioning at less than 15%. Stage 5 CKD is also known as kidney failure. To determine what stage of CKD you are currently in, your doctor will take a blood sample and measure the amount of creatinine in your blood and factor in your age, body size, and gender.
The kidneys are responsible for filtering excess fluids, salt, and waste products from the blood. When someone has kidney failure, their kidneys can’t remove these items efficiently, causing them to build up in the body.
“Dialysis is a treatment option for those with significant kidney failure, and the process of dialysis is to replace many functions of normal kidneys,” said Dr. Jingyin Yan, Nephrologist at Baylor St. Luke’s Medical Center.
While there are different types of dialysis, all of them begin with a doctor creating an access port in the body through which your blood can travel into an artificial kidney or dialysate (a liquid that absorbs the waste products) can enter the body.
There are two main types of dialysis:

1. Hemodialysis (HD). This form of dialysis typically occurs in a hospital or an outpatient dialysis center but can also happen at home. You go in for this procedure about three times a week, and it lasts for about four hours. While there, a medical professional will use an access point in your arm, leg, or neck and connect it to a device that functions as an artificial kidney. It slowly removes blood from the body, runs it through a filter, and then returns it.
2. Peritoneal Dialysis (PD). This type of dialysis typically occurs at home and happens several times a day. Before a patient can begin PD, their doctor places a catheter into the abdomen. Using this entrance, patients can insert dialysate, a cleansing fluid, into their abdominal cavity. The dialysate uses the peritoneum, the abdominal lining, to filter waste products from the blood. After a set period, the person drains the fluid into a bag and disposes of it properly.
Every month, our nephrology team at Baylor St. Luke’s Medical Center performs over 800 inpatient dialysis treatments. We offer all dialysis procedures, including continuous filtering therapies.
As a U.S. News & World Report High Performing Hospital in nephrology for 20192020, our team can provide the support you need in any stage of CKD.
If you notice signs of kidney disease, such as cramps, nausea, vomiting, loss of appetite, blood in the urine, or swelling, schedule an appointment with your primary care physician for evaluation and diagnosis.

IF YOU HAVE CHRONIC KIDNEY DISEASE, REQUEST A CONSULTATION WITH A ST. LUKE’S HEALTH NEPHROLOGIST TO LEARN ABOUT YOUR TREATMENT OPTIONS, INCLUDING YOUR ELIGIBILITY FOR TRANSPLANTATION. OUR KIDNEY TRANSPLANT PROGRAM IS DEDICATED TO PROVIDING THE HIGHEST LEVEL OF PATIENT CARE AND EXPANDING THE FRONTIERS OF RESEARCH IN NEPHROLOGY.

Cesarean section is the most common surgical procedure performed in obstetrics. It is a life-saving operation for both the mother and the fetus.
Globally, the recommended cesarean section rate should not exceed 23% of all deliveries. Unfortunately, cesarean section rates have been increasing dramatically worldwide.
At the same time, a low cesarean section rate may reflect issues within the healthcare system. Mainly, shortage of resources.
Cesarean section can be classified as either emergency or elective (planned), additionally; it can be categorized based on the type of uterine incision into:
• Classical cesarean section: Involves an incision in the upper uterine segment (now largely abandoned due to high risks).
• Lower uterine segment cesarean section: The routine and safer incision.
Obtaining Informed consent is necessary before proceeding with surgery, explaining the indications, necessity and possible complications.
The preferred anesthesia for a cesarean section is spinal or epidural anesthesia, which allows the mother to remain awake, initiate skin-to-skin contact, and begin breastfeeding immediately. Administration of General anesthesia is more risky than regional anesthesia, only given when epidural or spinal anesthesia is contraindicated, patient request, failed regional anesthesia, or high emergencies.
A cesarean section involves delivering the baby through a surgical incision in the lower abdominal wall and involving a transverse incision in lower uterine segment.
Lower segment scar weather longitudinal
or transverse promote better healing and a stronger scar.
Delivery of The baby head-either first or breech, depending on its position. Once the baby is out, extraction of the placenta ensuring complete removal with membranes, followed by closing of the lower uterine segment incision in two layers, ensuring proper hemostasis. Finishing by cleaning of the abdominal cavity, checking urine output and inspection of the ovaries and finally counting the towels and instruments before closing the abdominal wall.
Enhancement of early recovery after surgery is an evidence based beneficial practice to promote maternal wellbeing, minimize hospital stay, and facilitate early discharge. It includes encouraging early ambulation, resuming food intake, and initiating breastfeeding as soon as possible after surgery. Women should receive home postnatal visits and care to address common concerns such as pain, breastfeeding challenges, and early detection of serious complications like post-partum depression, puerperal sepsis and thrombosis.
Maternal and fetal indications for cesarean section include:
1. Previous cesarean sections or uterine surgery – Any prior operation on the uterine muscle (myometrium) may result in a weak fibrotic scar, which can rupture during next labor.
2. Cephalo-pelvic disproportion (CPD): A small or narrow pelvis that prevents the baby’s head from passing through the birth canal.
3. Obstructing pelvic tumors: Uterine fibroids or other pelvic tumors that hinder and interfere with fetal head descent.
4. Maternal infections: Active genital herpes simplex virus infection, which could cause severe neonatal encephalitis.
5. Abnormal fetal presentations: Breech, transverse, or brow presentations.
6. Multiple pregnancies: Twin or higherorder gestations.
7. Macrosomia: Large babies that increase the risk of birth trauma.
8. History of poor obstetric outcomes: Recurrent pregnancy loss or stillbirth.
9. Fetal distress: Umbilical cord issues, such as cord prolapse or abnormal fetal heart rate.
10. Placental abnormalities: Placental abruption, placenta Previa, or placenta accrete.
Although cesarean sections are generally safe and improve pregnancy outcomes, they still pose significant risks, including the following intraoperative and Postpartum Risks:
• Hemorrhage: Excessive bleeding may require blood transfusion, increasing the risk of anemia.
• Infections; Higher risk of surgical site infections, endometritis, and puerperal sepsis.
• Deep vein thrombosis (DVT) and pulmonary embolism: prolonged immobility together with increase of coagulations factors during pregnancy will increase risk of thrombosis.
• Bladder and bowel injuries: More common in repeat cesarean sections.
• Long-Term Risks: include chronic pelvic pain and adhesions that may affect fertility.
• Uterine niche formation – Can affect future pregnancies and menstrual pattern.
• Scar rupture in future pregnancies –Particularly in cases of poorly managed vaginal birth after cesarean (VBAC).
To minimize unnecessary cesarean sections, healthcare providers should:
• Provide comprehensive antenatal care and risk assessment.
• Offer antenatal classes to educate expectant mothers about labor and delivery.
• Follow evidence-based medical practices and avoid unnecessary interventions.
• Use oxytocin judiciously to induce or augment labor only when medically necessary.
THE PREFERRED ANESTHESIA FOR A CESAREAN SECTION IS SPINAL OR EPIDURAL ANESTHESIA, WHICH ALLOWS THE MOTHER TO REMAIN AWAKE, INITIATE SKIN-TO-SKIN CONTACT, AND BEGIN BREASTFEEDING IMMEDIATELY. ADMINISTRATION OF GENERAL ANESTHESIA IS MORE RISKY THAN REGIONAL ANESTHESIA, ONLY GIVEN WHEN EPIDURAL OR SPINAL ANESTHESIA IS CONTRAINDICATED, PATIENT REQUEST, FAILED REGIONAL ANESTHESIA, OR HIGH EMERGENCIES
• Ensure proper fetal heart monitoring and accurate interpretation of cardiotocography (CTG).
• Perform external cephalic version (ECV) when appropriate to correct breech presentation.
• Educate women who request cesarean sections without medical indications about the short- and long-term risks affecting their future fertility.
• Encourage trial of labor after cesarean (TOLAC) when appropriate, with careful risk assessment.
Finally to unify the fees to be the same for both cesarean section and normal vaginal delivery.
A ruptured uterine scar is a serious complication of VBAC, posing life-threatening risks to both the mother and fetus. Therefore, the decision to attempt VBAC should be made carefully, with detailed counseling and a thorough risk
evaluation. VBAC should be conducted inside well-equipped hospitals with blood transfusion service, intensive care unit and well-qualified surgeons capable to deal with high-risk near miss complications.
The possibility of successful VBAC increases if there is history of previous normal vaginal delivery, if there is a history of previous successful VBAC, lapse of 18 months interval or more between the cesarean section and the VBAC and if the previous cesarean section was done for temporary reason like Breech presentation or fetal distress
VBAC is contraindicated if the previous cesarean section was done in upper segment of the uterus, or because of obstructed labor or during second stage of labor with failure to progress and descend, or after ruptured uterus and if the woman has history of previous two cesarean sections or more.
A RUPTURED UTERINE SCAR IS A SERIOUS COMPLICATION OF VBAC, POSING LIFE-THREATENING RISKS TO BOTH THE MOTHER AND FETUS. THEREFORE, THE DECISION TO ATTEMPT VBAC SHOULD BE MADE CAREFULLY, WITH DETAILED COUNSELING AND A THOROUGH RISK EVALUATION





Dr. Mohammad Anas Barakat, Consultant Pediatrician Al-Ahli Hospital/Qatar

Empowering Families. Preventing Illness. Protecting Futures.
Doha, Qatar Al-Ahli Hospital proudly leads the way in pediatric care with the launch of Qatar’s first fully integrated Well Child Preventive Wellness Package a groundbreaking initiative offering children a full-circle health experience focused on early detection, prevention, and long-term wellness.
Recognizing that healthy childhoods lead to healthier societies, this one-of-a-kind program is designed to screen for physical, emotional, sensory, developmental, and even dental issues before they evolve into chronic or lifelong conditions.
While many healthcare services respond to illness after it arises, Al-Ahli Hospital’s Well Child Package is proactive, preventive, and holistic. It offers a multidisciplinary, age-specific approach that includes eight interconnected specialties; all delivered in one seamless, childcentered experience. From behavioral health to dental checks and lab diagnostics, this package ensures nothing is overlooked in your child’s developmental journey.
This package uniquely combines the expertise of eight vital disciplines, working together to provide a full-picture understanding of your child’s health:
1. Pediatric Growth & Developmental Assessment: Experienced pediatricians conduct full evaluations focusing on growth charts, neurological milestones, immunization status, and behavioral screening; looking deeper than surface-level symptoms to uncover subtle
indicators of concern.
2. ENT – Advanced Hearing & Balance Screening: Our ENT specialists use modern technology to detect hearing loss, balance disturbances, or inner ear conditions that may affect language development, attention, and school performance.
3. Vision Testing by Ophthalmologists: Poor eyesight is often misdiagnosed as a learning issue. Our team screens for strabismus, refractive errors, and early signs of eye disease, helping protect your child’s visual and cognitive development.
4. Nutritional Assessment & Diet Counseling: Our clinical dietitians evaluate nutritional intake, BMI, and family dietary patterns. They offer personalized nutrition plans to support healthy growth and help prevent obesity, diabetes, and future cardiovascular risks.
5. Pediatric Dentistry Screening: Oral health plays a critical role in overall wellbeing. Our dental team checks for cavities, bite problems, hygiene habits, and gum conditions; educating children and families on proper dental care routines that support lifelong oral health.
6. Laboratory Tests (Basic Wellness Panel): Key laboratory diagnostics are included to assess internal health, screen for anemia, vitamin deficiencies, glucose levels, and general indicators of systemic issues. These tests support clinical findings and reinforce early prevention strategies.
7. Integrated Report & Personalized Recommendations: All results are compiled into a cohesive wellness report, reviewed jointly across specialties. Parents receive clear action steps, lifestyle guidance, and referrals if any risk factors are detected.
The Well Child Package is ideal for:
• 4- 15 years old kids
• School-age children facing academic or behavioral transitions
• Preteens preparing for puberty and emotional growth
• Any child needing a full preventive check; even without noticeable symptoms
Whether it’s routine screening or early detection, this package acts as a health shield, catching what parents might miss and addressing issues before they escalate.
• The First in Qatar to offer this fully integrated pediatric wellness model
• Multidisciplinary team: Pediatrics, ENT, Ophthalmology, Nutrition, Dentistry, Hearing and Balance, as well as the following tests: Ferritin, (for Iron levels), Vitamin D, and Complete Blood Count CBC.
• ISO-Certified for quality, safety, and patientcentered care
• Stress-free, child-friendly environment
• Single-visit experience with comprehensive reporting
More Than a Check-Up. It’s a Commitment.
At Al-Ahli Hospital, we believe pediatric wellness is a shared responsibility—between hospitals, families, and communities.
Our Well Child Preventive Wellness Package is part of a broader vision to create a healthier, happier future generation by shifting from reactive to proactive pediatric care. This initiative encourages families to see wellness checks as essential; not optional; and empowers parents with education, support, and peace of mind.
Because Prevention is the Best Protection Healthier childhoods start with smarter choices band earlier interventions. The Well Child Preventive Package is not just a healthcare offering, it’s a promise: to protect your child’s full potential, to support families at every step, and to reduce the risk of preventable illnesses before they begin.
Because when it comes to children, the best medicine is prevention.
DOHA, QATAR AL-AHLI HOSPITAL PROUDLY LEADS THE WAY IN PEDIATRIC CARE WITH THE LAUNCH OF QATAR’S FIRST FULLY INTEGRATED WELL CHILD PREVENTIVE WELLNESS PACKAGE A GROUNDBREAKING INITIATIVE OFFERING CHILDREN A FULLCIRCLE HEALTH EXPERIENCE FOCUSED ON EARLY DETECTION, PREVENTION, AND LONG-TERM WELLNESS



In line with its mission to deliver cutting-edge healthcare, Al-Ahli Hospital proudly becomes the first hospital in Qatar to introduce the revolutionary Photon Scanner CT, a major advancement in diagnostic imaging technology. This photon-counting computed tomography system sets a new benchmark for image clarity, patient safety, and clinical efficiency; reinforcing the hospital’s status as a national leader in precision diagnostics. The Photon Scanner CT isn’t just a new tool it’s a paradigm shift that reshapes the landscape of radiology.
AL-AHLI HOSPITAL’S RADIOLOGY SERVICES, INCLUDING THE PHOTON SCANNER CT SUITE, ARE PART OF AN ISO-CERTIFIED MEDICAL IMAGING DEPARTMENT; DEMONSTRATING A CONSISTENT COMMITMENT TO QUALITY, SAFETY, AND INTERNATIONAL STANDARDS.
Unlike conventional CT systems that use energy-integrating detectors, photon-counting CT technology registers each individual X-ray photon and analyzes its energy profile. This allows for the creation of ultra-high-resolution, multi-energy images that dramatically enhance tissue contrast and reduce noise. By capturing more detailed, energy-sensitive data, this scanner provides richer diagnostic insights, even in the most complex clinical scenarios.
Scan times are significantly reduced, enabling rapid imaging with less motion artifact; especially beneficial in emergency cases, pediatric care, and elderly patients.
With up to 60% less radiation compared to traditional CT scanners, the system ensures maximum patient safety without compromising image quality. This makes it ideal for patients requiring repeated imaging, including those undergoing oncology or cardiac monitoring.
The system offers unmatched resolution and contrast, allowing physicians to detect smaller lesions, microfractures, and subtle tissue changes that would otherwise go unnoticed.
Al-Ahli Hospital’s radiology services, including the Photon Scanner CT suite, are part of an ISO-certified medical imaging department; demonstrating a consistent commitment to quality, safety, and international standards.
The Photon Scanner CT is already transforming care across multiple specialties at Al-Ahli Hospital:
• Oncology: Early tumor detection, treatment response evaluation, and follow-up scans with lower radiation burden.
• Cardiology: Clear visualization of coronary arteries, even in fast-moving hearts, supporting earlier and more accurate detection of arterial plaque.
• Neurology: Precise differentiation of soft tissues aids in stroke evaluation, hemorrhage detection, and neurodegenerative disease diagnosis.
• Pulmonology: Superior lung imaging assists in the assessment of interstitial lung disease, embolisms, and nodules.
• Orthopedics & MSK Imaging: Enables highdetail evaluation of bone integrity, joint pathology, and post-operative follow-up.
This level of diagnostic accuracy empowers physicians to tailor treatment plans confidently, reducing delays and improving outcomes.
At Al-Ahli Hospital, clinical innovation goes hand in hand with patient comfort. The Photon Scanner CT was designed with patient needs at the center:
• Quieter scan environment for reduced anxiety
• Shorter procedure times for enhanced comfort
• Weight-adjustable tables and open designs accommodate patients of all sizes and mobility levels
• Lower radiation dose protects vulnerable populations, such as children and patients requiring serial imaging
• These features make the scanner a patientfriendly solution, delivering not just superior imaging; but peace of mind.
The acquisition of the Photon Scanner CT aligns with Al-Ahli Hospital’s broader strategic vision;
to remain at the forefront of medical technology and provide world-class diagnostic services right here in Qatar.
Being the first in the country’s private sector to implement this cutting-edge system, Al-Ahli reinforces its commitment to:
• Innovation in clinical practice
• Investments that improve patient care and safety
• Supporting Qatar’s national healthcare transformation goals
Faster, more accurate diagnoses allow for earlier interventions and personalized treatment planning. Whether it's oncology, cardiology, or emergency medicine, the Photon Scanner CT empowers doctors with greater confidence and sharper decision-making tools. This is not just about better pictures; it’s about better lives.
At Al-Ahli Hospital, radiology is more than diagnostics it’s the foundation of proactive, life-saving medicine. Every scan matters. Every detail is vital. And every patient deserves clarity and care.
With the Photon Scanner CT, the radiology department takes a giant leap forward; enhancing not only how we see, but how we heal. And just as Al-Ahli’s IVF services are known for their high number of take-home baby successes, our diagnostic capabilities now offer an equally high standard of clinical precision, early detection, and care planning—building a consistent record of outcomes that matter.
To our patients, referring physicians, and the broader medical community: this is your technology, your hospital, your future.
IN LINE WITH ITS MISSION TO DELIVER CUTTING-EDGE HEALTHCARE, AL-AHLI HOSPITAL PROUDLY BECOMES THE FIRST HOSPITAL IN QATAR TO INTRODUCE THE REVOLUTIONARY PHOTON SCANNER CT, A MAJOR ADVANCEMENT IN DIAGNOSTIC IMAGING TECHNOLOGY. THIS PHOTON-COUNTING COMPUTED TOMOGRAPHY SYSTEM SETS A NEW BENCHMARK FOR IMAGE CLARITY, PATIENT SAFETY, AND CLINICAL EFFICIENCY; REINFORCING THE HOSPITAL’S STATUS AS A NATIONAL LEADER IN PRECISION DIAGNOSTICS
Recent advancements in hypertension management include the development of new drug classes, minimally invasive procedures for specific causes, enhanced methods for blood pressure monitoring, and improved strategies to support treatment adherence. These innovations hold promise for better blood pressure control, particularly in patients with resistant or secondary hypertension, and are expected to reduce the global burden of cardiovascular disease.
Hypertension is a significant risk factor for cardiovascular diseases. Effective management, particularly for hard-to-treat patients, can reduce the incidence of heart attacks, strokes, and kidney failure, improving population health and lowering global healthcare costs. Modern treatments have advanced, providing targeted options that enhance patient outcomes while minimizing complications. It is crucial to choose the right treatment under the guidance of a specialized physician, taking into account individual assessments. Historically, hypertension treatment options were limited, but scientific progress has introduced new drug classes and a growing focus on personalized medicine that addresses unique patient characteristics.
Hypertension occurs when the long-term force of blood against artery walls is high, leading to potential health problems like heart disease. Blood pressure is the force of circulating

blood on blood vessel walls, and sustained high pressure can damage arteries and cause various health issues.
Blood pressure is typically measured using two numbers:
• Systolic pressure: the top number, which indicates the pressure in the arteries when the heart beats (contracts) and pumps blood.
• Diastolic pressure: the bottom number, which reflects the pressure in the arteries when the heart rests between beats.
A normal blood pressure reading is around 120/80 mmHg. Hypertension is generally defined as consistent readings of 130/80 mmHg or higher over time.
There are two main types of hypertension:
• Primary (essential) hypertension: the most common form, developing gradually over many years. Its exact cause is not always clear but is likely a combination of genetic predisposition, lifestyle choices (such as unhealthy diet, physical inactivity, obesity, smoking), and age-related changes in the body.
PHARMACOLOGICAL AND THERAPEUTIC OPTIONS REPRESENT A SIGNIFICANT LEAP IN HYPERTENSION CARE, OFFERING MORE EFFECTIVE TREATMENT CHOICES THAT TARGET SPECIFIC DISEASE MECHANISMS. THIS PAVES THE WAY FOR BETTER PATIENT OUTCOMES AND FEWER LONG-TERM COMPLICATIONS.
• Secondary hypertension: caused by an underlying medical condition. These may include kidney disease, adrenal gland tumors, obstructive sleep apnea, thyroid disorders, certain medications (such as contraceptive pills, decongestants, pain relievers), and illicit drugs (like cocaine or amphetamines). Secondary hypertension often develops suddenly and tends to be more severe than primary hypertension.
Hypertension is often called the “silent killer” because many people with the condition exhibit no symptoms for years, even when the condition is severe. Uncontrolled high blood pressure can significantly increase the risk of life-threatening conditions, including:
• Heart attacks and strokes: damaged arteries may become narrowed or blocked, leading to such events.
• Heart failure: the heart must work harder to pump blood against elevated pressure, which may weaken or enlarge it over time.
• Kidney disease: high blood pressure can damage kidney blood vessels, impairing their function.
• Vision problems: it may damage blood vessels in the eyes, leading to vision loss.
• Vascular dementia: reduced blood flow to the brain, due to arterial damage, can contribute to cognitive decline.
The good news is that hypertension can often be effectively managed through lifestyle changes and medication.
A healthy diet is essential for managing hypertension. It should include fresh fruits, vegetables, whole grains, and lean proteins like poultry and fish. Reducing sodium intake from processed foods and limiting saturated fats are also crucial, as they contribute to heart disease. The DASH diet is often recommended for its effectiveness in lowering blood pressure and improving heart health.
Consistent physical activity is integral to blood
pressure control. It is recommended to engage in at least 150 minutes of moderate-intensity aerobic exercise per week (e.g., brisk walking, cycling, swimming), or 75 minutes of vigorous aerobic activity (e.g., running, high-intensity workouts). Exercise strengthens the heart muscle, improves circulation, helps maintain a healthy weight, and contributes to lowering blood pressure and reducing cardiovascular risk.
Weight plays a critical role in blood pressure regulation. For individuals who are overweight or obese, losing even a modest amount of weight can significantly improve blood pressure levels. Weight loss reduces strain on the heart and blood vessels, enhancing their function and lowering the risk of hypertension-related complications.
Chronic stress can negatively affect blood pressure. Therefore, learning and practicing stress reduction techniques is vital for maintaining healthy levels. These techniques include relaxation exercises such as yoga, meditation, and deep breathing. Such practices help calm the nervous system, reduce the release of stress hormones that may raise blood pressure, and promote a sense of well-being.
Excessive alcohol intake negatively affects health, particularly by raising blood pressure. Hypertension is a major risk factor for heart disease and stroke. Therefore, it's advisable to limit or avoid alcohol to manage hypertension effectively. Research shows that reducing alcohol improves blood pressure and decreases the risk of related health issues. By making informed choices about alcohol, individuals can enhance their health and well-being.
Smoking is a major contributor to vascular damage and significantly increases the risk of hypertension and its complications, including heart attacks and strokes. Quitting smoking is one of the most important steps a person can take to protect cardiovascular health and reduce overall disease risk.
CHRONIC STRESS CAN NEGATIVELY AFFECT BLOOD PRESSURE. THEREFORE, LEARNING AND PRACTICING STRESS REDUCTION TECHNIQUES IS VITAL FOR MAINTAINING HEALTHY LEVELS. THESE TECHNIQUES INCLUDE RELAXATION EXERCISES SUCH AS YOGA, MEDITATION, AND DEEP BREATHING. SUCH PRACTICES HELP CALM THE NERVOUS SYSTEM, REDUCE THE RELEASE OF STRESS HORMONES THAT MAY RAISE BLOOD PRESSURE, AND PROMOTE A SENSE OF WELL-BEING.

In 2024, California’s medtech sector defied expectations and exceeded previous funding benchmarks. According to the J.P. Morgan Medtech Industry insights, a staggering $19.1 billion was raised across 691 funding rounds, surpassing 2023’s figures despite a drop in deal volume. Instead, investors shifted their focus toward fewer but more substantial investments, prioritizing quality and long-term growth potential. Alongside this, the M&A landscape flourished with 305 acquisitions totalling $63.1 billion, largely driven by smaller, strategic deals. The IPO front, too, is regaining its footing with $744.5 million raised through four medtech IPOs. Particularly promising are AI-powered diagnostics and personalized medicine startups that continue to generate optimism on the public markets.
Southern California remains a powerhouse within this investment surge, generating over $20 billion in annual revenues. Its medtech ecosystem is known for its capacity to produce strong shareholder returns and foster
MEDTECH WORLD’S EFFORTS AREN’T CONFINED TO NORTH AMERICA. EARLIER THIS YEAR, AT ITS DUBAI EDITION, THE PLATFORM COLLABORATED WITH AMCHAM DUBAI TO ENCOURAGE CROSSBORDER INVESTMENT BETWEEN THE U.S. AND THE GCC REGION.
innovation at scale. This dynamic environment reflects broader industry trends: a more mature, measured, and innovation-focused investment cycle.
Amid this flourishing investment activity, MedTech World is positioning itself as the international gateway that brings together the most relevant stakeholders in the sector, from startup founders and academic leaders to investors and global health authorities. Its growing global footprint and emphasis on meaningful engagement have cemented its place as a connector of high-potential companies and visionary backers.
MedTech World’s approach is rooted in creating deliberate connections across geographies and specialisations. In a year where funding growth has increasingly relied on large-scale, targeted investment, the need for a trusted, curated platform for introductions and dialogue has
never been greater. With that in mind, MedTech World has partnered with MedTech Innovator for an exclusive event taking place on June 27th in San Jose, California.
This event brings together 100 carefully selected startups and a robust network of investors and key industry figures, creating the ideal environment for substantive conversation and deal-making. MedTech Innovator, the world’s largest accelerator for medical device, digital health, and diagnostics companies, is known for propelling transformative healthcare ventures. Together, the partnership exemplifies what MedTech World has consistently championed, platforms that connect innovative ideas with the resources they need to scale, sustainably and globally.
But MedTech World’s efforts aren’t confined to North America. Earlier this year, at its Dubai edition, the platform collaborated with AmCham Dubai to encourage cross-border investment between the U.S. and the GCC region. This event opened up new channels for emerging technologies and underscored the platform’s role in fostering dialogue between historically underconnected markets. By bridging these gaps, MedTech World contributes not just to investment but also to the globalisation of healthcare innovation.
"At MedTech World, we’ve always believed that opportunity isn’t bound by geography. Whether in California, Dubai, or Malta, our mission is to build an ecosystem where investors and startups don’t just meet, they build meaningful partnerships. As the industry becomes more complex, curated spaces like ours help stakeholders navigate risk, identify transformative potential, and build long-term value. We are proud to work alongside global partners to create events that are not only relevant but also future-facing."
Dr. Dylan
Attard, CEO and Co-founder, MedTech World
The major touchpoint in MedTech World’s calendar is MedTech Malta 2025, taking place from 12 to 14 November. Set against the backdrop of Malta’s growing reputation as a
hub for innovation, this flagship event offers a compelling opportunity for investors to engage with promising startups, participate in strategic discussions, and expand their networks across continents.
Malta’s strategic location between Europe, Africa, and the Middle East provides a unique convergence point for international delegates. For investors, it presents a rare opportunity to evaluate cross-border deals and gain visibility into MedTech trends emerging from diverse markets. The event will include keynote sessions, investor roundtables, and startup showcases tailored to facilitate dialogue and action, in addition to the MedTech startup pitch competition.
As global interest in healthcare technology continues to rise, investors need platforms that offer more than exposure; they need relevance, curation, and access. MedTech World continues to deliver just that.
THIS EVENT OPENED UP NEW CHANNELS FOR EMERGING TECHNOLOGIES AND UNDERSCORED THE PLATFORM’S ROLE IN FOSTERING DIALOGUE BETWEEN HISTORICALLY UNDERCONNECTED MARKETS. BY BRIDGING THESE GAPS, MEDTECH WORLD CONTRIBUTES NOT JUST TO INVESTMENT BUT ALSO TO THE GLOBALISATION OF HEALTHCARE INNOVATION.

Healthcare providers and payers have made significant strides. Clinical innovation, expanded access to care, and digital health solutions have transformed the care landscape in positive ways. Providers deliver more advanced interventions than ever before, while insurers have introduced promising population health models and chronic care strategies. Yet we stand at a crossroads: These gains risk stagnation if we continue to blend patient satisfaction with meaningful outcomes. The focus must shift from how the system appears to how well it functions; clinically, ethically, and structurally.
“Patient-Centered Care” has long served as the favorite child of healthcare reform, etched into mission statements, policy frameworks, and accreditation checklists. In theory, it embodies an ideal where medical decisions, treatment plans, and organizational priorities revolve around patient needs and experiences. In practice, however, the concept has strayed.
Globally across public and private systems, in developed and emerging economies “patientcenteredness” has been diluted into a buzzword. It is too often reduced to hospitality features and superficial satisfaction metrics rather than a structural commitment to clinical outcomes, shared decision-making, and long-term wellbeing. This raises urgent questions: Has our obsession with patient satisfaction tangibly improved care? Or have we merely rebranded hospitality as healthcare? Comfort, respect, and kindness matter. Patients deserve dignity. But comfort is not care, and a pleasant experience is no substitute for medical progress.
Modern hospitals and clinics invest heavily in patient experience infrastructure: plush waiting rooms, high-end menus, valet parking, and realtime feedback systems. While these efforts hold value, they are not the essence of healing. Too often, patients are discharged with unanswered questions, fragmented care plans, or confusion about next steps, yet leave with a tote bag, a smile, and a text prompting them to rate their
“experience.” This is not patient-centered care. It is aesthetic care. In this misguided transaction, clinical excellence has become secondary, a dangerous imbalance the healthcare industry can no longer afford.
The future demands a universal framework for patient-centered care, one rooted not in brand image or PR language but in clinical integrity, operational transparency, and cultural humility. This framework must:
• Prioritize Clinical Outcomes
• Amplify the Patient’s Voice
• Align Provider and Payer Incentives
• Leverage Technology Responsibly
Building a truly patient-centered system is not the duty of one stakeholder but a collective mission:
• Providers must transcend procedural efficiency to reclaim their roles as advocates, educators, and partners in recovery.
• Payers must move beyond bureaucratic denial models and fund evidence-based solutions.
• Patients must engage as active participants, not passive recipients.
• Policymakers must ensure licensing, accreditation, and quality benchmarks reflect genuine care not superficial service polish.
Patient-centered care isn’t about kiosks or wellness lounges; it’s about patients feeling healed and heard. True care is personalized, evidence-based, and focused on outcomes. Success should be measured by recovery, not throughput, and by real patient experiences, not data alone. We can choose surface fixes or rebuild healthcare around the patient’s journey; with truth, courage, and collaboration. Patientcentered care demands an unflinching definition, it is not a slogan; it's justice. "Every life entrusted to healthcare deserves systems that see them, hear them, and relentlessly fight for their dignity without compromise, without delay."

Ali Elhaj is a healthcare strategist and policy advisor advocating for structural transformation in care delivery. With expertise in government leadership, payer strategy, and health system reform, he focuses on ethical, comprehensive and sustainable system that align stakeholder collaboration.
Our experts get to know you, then tailor treatments to help fit your needs—which could include radiation, surgery, chemotherapy, immunotherapy, cellular therapy, genetic counseling, or a customized lifestyle management plan. In collaboration with Baylor College of Medicine, we’re equipped to pave the way for even more revolutionary discoveries and groundbreaking approaches to cancer prevention, diagnosis, and treatment.
Learn more about the NCI-designated Dan L Duncan Comprehensive Cancer Center at Baylor College of Medicine at stlukeshealth.org/bslmcinternational


