Excellence in Healthcare
Cedars-Sinai has been named to the Honor Roll for the ninth consecutive year in U.S. News & World Report’s “Best Hospitals 2024–25” rankings. As a global leader in healthcare, we offer a full range of services to patients from around the world. Whether we’re providing clinical services in your region via video visits or at our renowned medical center, our mission remains unchanged: to give patients access to excellence in healthcare—wherever they may be. Located in iconic Beverly Hills, Cedars-Sinai blends cutting-edge medicine in a vibrant setting known for its rich culture, famous landmarks and year-round warm weather—making it a leading destination for international patients seeking world-class treatment.
•
•
•
•
•
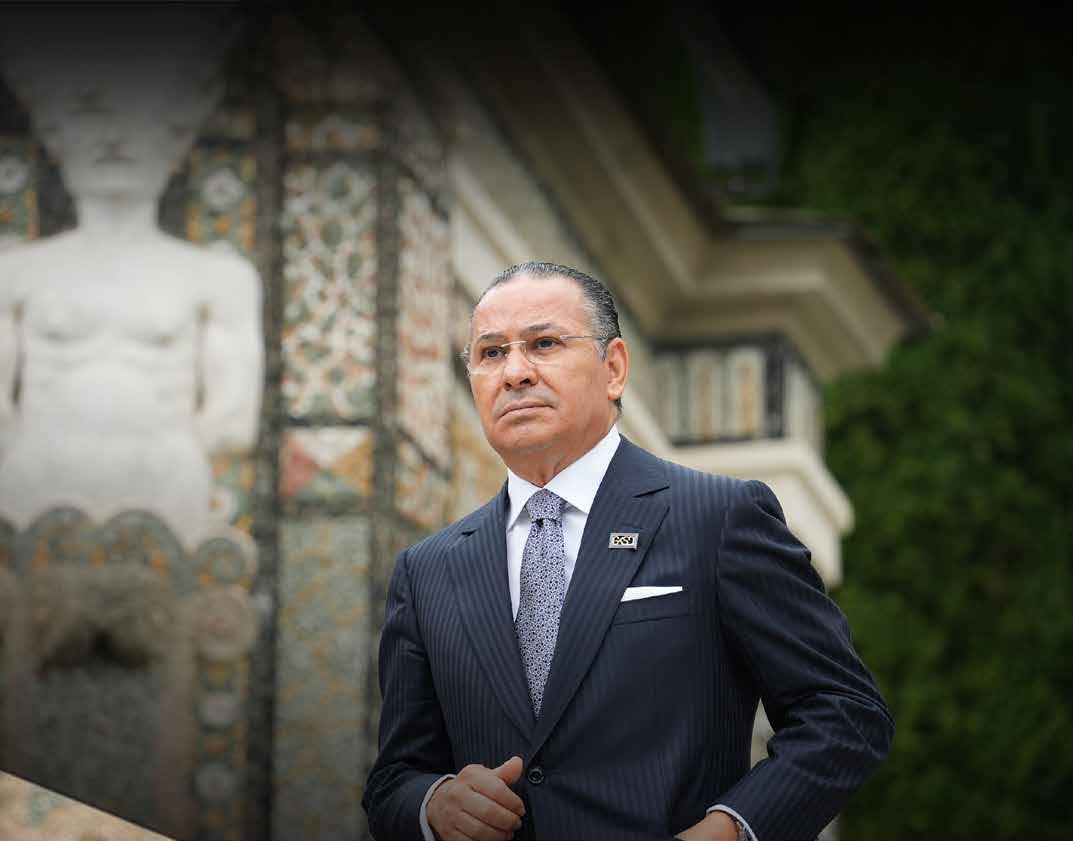
amel Ghribi’s journey from humble beginnings in Tunisia to becoming a pivotal fgure in global healthcare, business, and philanthropy is a testament to his unwavering commitment and visionary leadership. Born in 1962 in Sfax, Tunisia, Ghribi's early exposure to a strong work ethic and perseverance shaped his future endeavors. His impact now spans multiple sectors, from advancing medical infrastructure to fostering international cooperation and education. Over the past year, his achievements have continued to reshape the landscape of healthcare and investment, reinforcing his legacy as a leader who prioritizes people, progress, and positive change.
Ghribi’s ability to integrate his deep-rooted values with professional accomplishments sets a blueprint for responsible leadership in today’s interconnected world. As he continues to infuence and inspire, Kamel Ghribi remains a beacon of innovation and philanthropy, paving the way for a healthier, more educated, and more cooperative global community.
commitment to enhancing global healthcare systems, driving investment, and supporting communities worldwide. His career began in the energy sector, where he held executive roles in leading petroleum companies. At just 29, he became Vice President of Olympic Petroleum Corporation in New York while simultaneously serving as President of Olympic Management in Italy. Later, as President of Attock Oil Company in the UK, he led signifcant expansions, refning his expertise in global trade and strategic investment.
Kamel Ghribi is the President of GKSD Investment Holding Group, the President of IRCCS San Donato Hospital, and the Vice President of both GSD IRCCS San Rafaele University Hospital and IRCCS Galeazzi Sant’Ambrogio Hospital. His leadership underscores a deep
In 2015, Ghribi founded GK Investment Holding Group in Switzerland, focusing on exporting essential commodities and establishing industrial projects in emerging markets. His strategic investments have driven economic development across Africa, the Middle East, and Europe, reinforcing his reputation as a visionary leader.
In Italy, Ghribi expanded his business empire through GKSD Investment Holding, a multidisciplinary group specializing in healthcare, engineering, infrastructure, and construction. Under his leadership, GKSD became a key player in managing complex healthcare projects and advancing medical institutions, overseeing cutting-edge research at institutions like Vita-Salute San Rafaele University. His strategic acumen and passion for healthcare accessibility continue to shape global medical advancements.


GKSD Healthcare Management & Consulting, a vital entity within GKSD Investment Holding Group and the San Donato Hospital Group, leverages its expertise to provide top-tier healthcare solutions. Established in 2020, it has become a hub for strategic advisory services, integrating cutting-edge technology and AIbased diagnostic care in collaboration with Microsoft. Meanwhile, Gruppo San Donato (GSD), the largest private hospital group in Italy, operates 58 facilities in Italy and 77 in Poland, treating over 5.6 million patients annually. Its commitment to medical excellence, gene and cell therapy, and sustainable healthcare solutions has made it a global leader in research and innovation. With a workforce of over 26,000 professionals, including more than 8,000
doctors, GSD plays a critical role in advancing patient-centered healthcare and medical research worldwide.
Kamel Ghribi’s enduring infuence and innovative spirit have not only transformed traditional sectors but also laid the groundwork for pioneering advancements in integrated healthcare. His strategic vision seamlessly bridges decades of leadership with a forwardthinking approach, setting the stage for a revolutionary model of patient care that blends state-of-the-art technology with the warmth of personalized service. This evolution of thought and practice naturally culminates in the inception of Hospital Healthcare Holdings, where his commitment to excellence and transformative impact fnds a dynamic new expression.
WE DO NOT SIMPLY INVEST IN INFRASTRUCTURE; WE INVEST IN PEOPLE. HEALTHCARE IS NOT A PRIVILEGE; IT IS A RIGHT THAT MUST BE ACCESSIBLE TO ALL. KAMEL GHRIBI
ospital Healthcare Holdings (HHH) heralds a new chapter in integrated health excellence. Under the leadership of Kamel Ghribi, the pioneering HHH brand combines the expertise of Gruppo San Donato, Italy's largest private hospital group, and GKSD Holding, a leading provider of advisory services, project management, and consultancy services. Gruppo San Donato (GSD), a key player in the Italian National Health Service (NHS) and part of GKSD Investment Holding, was established in 1957 and operates a network of future-focused healthcare facilities, hospitals, smart clinics, universities, and research centers in Italy, Poland, Romania, and Iraq. By integrating world-class clinical care with scientifc research through its private, not-forproft Vita-Salute San Rafaele University, GSD remains at the forefront of healthcare innovation.
GKSD Investment Holding is a multidisciplinary group with diverse activities ranging from healthcare to engineering, infrastructure, and construction. Since its inception in 2011, GKSD has become the provider of choice for the conception, creation, and management of complex healthcare projects across Italy, Africa, and the Middle East & North Africa region. As the frst global brand to bring together luxury, elegance, and healthcare excellence, HHH’s portfolio of premium hospitals refects the fnest in holistic health and signature hospitality.
Expanding the Future of Luxury Healthcare: 10 state-of-the-art HHH Hospitals & Smart Clinics set to open by 2030, redefning premium medical excellence.
A Vast Network of Cutting-Edge Care: 161 world-class medical facilities under Gruppo San Donato, delivering unparalleled healthcare solutions across multiple regions.
Transforming Lives on a Global Scale: Over 5.8 million patients receive top-tier medical treatment annually, ensuring accessibility and quality at every level.
An Elite Force of Medical
Experts: A prestigious global network of 10,000+ physicians, providing expertise, innovation, and groundbreaking medical care.
Unmatched Capacity for Excellence: 8,000+ hospital beds worldwide, ensuring comfort, efciency, and world-leading patient care.
A Thriving Healthcare Powerhouse: €2.7 billion in turnover (2024), solidifying Gruppo San Donato as a leader in sustainable and innovative healthcare investment.
A Global Leader in Research & Innovation: Ranked #4 in the world for ‘Research Quality’ by THE World University Rankings 2025, positioning Vita-Salute San Rafaele University at the forefront of medical advancements.
Our integrated health hospitals are designed to deliver a seamless patient experience that blends world-class medical expertise with the latest technological innovations. These hospitals are not just treatment centers; they are holistic health hubs that prioritize both physical and emotional well-being. Every facility is built to the highest standards of clinical care, equipped with cutting-edge surgical units,
intensive care wards, and specialized centers for precision medicine. Our multidisciplinary approach ensures that every patient receives a fully customized treatment plan, integrating diagnostics, therapy, and rehabilitation under one roof.
We understand that premium healthcare extends beyond hospital walls. Our exclusive
FROM ANTIAGING THERAPIES TO ADVANCED REGENERATIVE MEDICINE, OUR BOUTIQUE CENTERS REDEFINE THE STANDARDS OF OUTPATIENT CARE.
24/7 Health Concierge service provides patients with round-the-clock medical assistance, ensuring they receive top-tier medical support anytime, anywhere. Whether it’s arranging priority consultations with world-renowned specialists, facilitating travel for medical procedures, or providing remote health monitoring, our concierge service is dedicated to enhancing the patient journey. With a personal health manager assigned to every patient, we guarantee an unparalleled level of support and accessibility.
Our smart clinics and boutique medical centers are designed for patients seeking high-end medical care in a sophisticated and convenient setting. These centers focus on precision diagnostics and personalized treatments, integrating cutting-edge medical technologies such as AI-powered diagnostics, robotic-assisted procedures, and telemedicine services. Patients
receive tailor-made treatment plans from leading specialists, all within an environment that embodies luxury and exclusivity. From anti-aging therapies to advanced regenerative medicine, our boutique centers redefne the standards of outpatient care.
At HHH, luxury and healthcare go hand in hand. Our hospitals and medical centers are modeled after fve-star hotels, ofering private suites with high-end furnishings, gourmet dining options, and wellness services that
OUR INTEGRATED HEALTH HOSPITALS ARE DESIGNED TO DELIVER A SEAMLESS PATIENT EXPERIENCE THAT BLENDS WORLD-CLASS MEDICAL EXPERTISE WITH THE LATEST TECHNOLOGICAL INNOVATIONS. THESE HOSPITALS ARE NOT JUST TREATMENT CENTERS; THEY ARE HOLISTIC HEALTH HUBS THAT PRIORITIZE BOTH PHYSICAL AND EMOTIONAL WELL-BEING.
cater to every aspect of patient recovery. We collaborate with the world’s most prestigious brands in fashion, hospitality, and wellness to create an environment of elegance and relaxation. Our philosophy is to treat patients not just as individuals receiving medical care but as distinguished guests experiencing the highest standard of personalized service.
We oversee the management and development of premium hospitals and clinics, from acquisition and construction to daily operations. Our primary focus is on creating a network of hospitals renowned for VIP services and exclusive care, integrating advanced technologies with precision medicine.
OUR PRIMARY FOCUS IS ON CREATING A NETWORK OF HOSPITALS RENOWNED FOR VIP SERVICES AND EXCLUSIVE CARE, INTEGRATING ADVANCED TECHNOLOGIES WITH PRECISION MEDICINE.
As pioneers in healthcare innovation, we are committed to advancing medical training and education. Through strategic partnerships with Vita-Salute San Rafaele University, we ofer specialized training programs for healthcare professionals, integrating virtual reality (VR) surgical simulations, AI-driven diagnostics, and remote learning platforms.
Our Visiting Consulting program brings world-renowned specialists to train local physicians, ensuring that cutting-edge techniques and best practices are shared across our global network. By investing in continuous professional development, we are shaping the next generation of medical excellence.
With extensive experience in hospital management, we implement a model of excellence and operational optimization for existing hospitals and healthcare facilities. Our approach ensures the highest operational performance, improving processes and procedures to deliver an exceptional patient experience while driving fnancial success.
We ofer franchising opportunities for highend hospitals and clinics around the world, granting the use of our prestigious brand while overseeing quality and operational standards.
Vice President of HHH President of GSD
GSD Operations Strategy Supervisor & International Development Coordinator
Global Head of Strategic Investments and Presidential Advisor
Chairman of HHH Chairman of GKSD Group
CEO of GSD Sistemi e Servizi GKSD Holding Executive Director & CFO
CEO of HHH General Manager of GKSD Healthcare
CEO of the San Rafaele Teaching Hospital (IRCCS)
Saudi Arabia’s healthcare sector is undergoing a remarkable transformation as part of Vision 2030, presenting unprecedented investment opportunities for international players. As a leading European healthcare and investment group, GKSD sees immense potential in the Kingdom’s evolving medical landscape. From the expansion of specialized hospitals and research centers to the integration of smart healthcare solutions, the demand for cutting-edge facilities continues to grow. Key investment areas include advanced diagnostics, AI-powered healthcare, robotic surgery, and luxury medical services that align with Saudi Arabia’s ambition to become a global healthcare hub.
GKSD is emerging as a transformative force in reshaping healthcare across the Middle East. With rapid technological advancements, the future of healthcare in the region is shifting towards AI-driven diagnostics, smart hospitals, and digital health ecosystems. GKSD envisions a healthcare landscape that prioritizes accessibility, patient-centered innovation, and sustainable medical advancements. By leveraging AI, telemedicine, and roboticassisted surgery, the company aims to bridge healthcare gaps, improve patient outcomes, and introduce next-generation medical solutions across Saudi Arabia and beyond.

As GKSD continues its global expansion, Saudi Arabia stands out as a strategic market within the Gulf Cooperation Council (GCC). The Kingdom’s rapid infrastructure development, combined with the government’s increasing focus on public-private partnerships (PPPs), makes it a prime destination for high-end hospital investments, medical education programs, and healthcare consulting services. Recognizing the existing gaps in Saudi Arabia’s specialized medical care and advanced research capabilities, GKSD aims to introduce state-ofthe-art medical centers, high-tech hospitals, and cutting-edge training programs to address the country’s evolving healthcare needs.
With artifcial intelligence (AI) and digital healthcare reshaping the industry, GKSD is committed to integrating these technologies into its projects. The rise of smart hospitals and AI-driven healthcare solutions in Saudi Arabia will signifcantly improve efciency, early disease detection, and precision medicine. Digital platforms will also enable seamless patient experiences, from remote monitoring to AI-assisted diagnostics, making high-quality healthcare more accessible and efective.
AS GKSD CONTINUES ITS GLOBAL EXPANSION, SAUDI ARABIA STANDS OUT AS A STRATEGIC MARKET WITHIN THE GULF COOPERATION COUNCIL (GCC). THE KINGDOM’S RAPID INFRASTRUCTURE DEVELOPMENT, COMBINED WITH THE GOVERNMENT’S INCREASING FOCUS ON PUBLIC-PRIVATE PARTNERSHIPS (PPPS), MAKES IT A PRIME DESTINATION FOR HIGH-END HOSPITAL INVESTMENTS, MEDICAL EDUCATION PROGRAMS, AND HEALTHCARE CONSULTING SERVICES.
GKSD’s multi-vertical approach ensures that healthcare management, hospital operations,
and academic research work in synergy. The group’s investment in university-afliated medical research and innovation hubs fosters the development of new treatments, breakthrough therapies, and next-generation medical training programs.
As Saudi Arabia strengthens its focus on medical education and workforce training, GKSD is looking to introduce specialized training programs in collaboration with top-tier local institutions, bringing world-class expertise to the region.
ofering an efcient, high-quality alternative to traditional hospital visits. With the rising adoption of telemedicine and wearable health technology, smart clinics are set to play a pivotal role in Saudi Arabia’s healthcare evolution, ensuring faster, more personalized medical care for patients across the Kingdom.
Expanding into new markets requires a wellstructured approach, and GKSD’s entry strategy in Saudi Arabia revolves around partnerships, acquisitions, and direct investments. By carefully assessing market needs, government regulations, and investment incentives, GKSD is identifying the most impactful and sustainable ways to contribute to the Kingdom’s healthcare development. The company is also exploring strategic collaborations with government entities and private sector partners to support the country’s growing healthcare infrastructure and service diversifcation eforts.
In response to the increasing demand for premium medical services, GKSD is preparing to launch a luxury healthcare brand that merges state-of-the-art medicine with high-end hospitality. This new concept will set a global benchmark for elite healthcare, combining world-class clinical care, personalized concierge services, and fve-star wellness experiences. Saudi Arabia is a key market for this initiative, with Riyadh, Jeddah, and the Eastern Province being prime locations for the brand’s expansion. While exclusivity remains at the core of this model, GKSD is also committed to ensuring that cutting-edge treatments and specialized care remain accessible to a wider audience.
THROUGH STRATEGIC INVESTMENTS, CUTTING-EDGE RESEARCH, AND WORLD-CLASS EXPERTISE, GKSD IS FULLY COMMITTED TO SHAPING THE FUTURE OF HEALTHCARE IN SAUDI ARABIA, ENSURING THAT QUALITY CARE, INNOVATION, AND ACCESSIBILITY REMAIN AT THE HEART OF ITS MISSION. AS PART OF OUR UNWAVERING COMMITMENT TO REVOLUTIONIZING HEALTHCARE WORLDWIDE, WE ARE EMBARKING ON AN AMBITIOUS EXPANSION, BRINGING OUR SIGNATURE BLEND OF LUXURY AND MEDICAL EXCELLENCE TO NEW DESTINATIONS.
In line with its expansion strategy, GKSD has already secured a major SAR 1 billion investment agreement with King Saud Medical City, aiming to transform healthcare delivery in Saudi Arabia. This partnership is expected to enhance medical research, improve hospital facilities, and introduce world-class healthcare solutions. In addition to this milestone, GKSD continues to explore new collaborations that align with its long-term vision for healthcare innovation and accessibility in the Kingdom.
Looking ahead, GKSD envisions Saudi Arabia as a leading destination for advanced healthcare, research, and medical innovation. Over the next fve to ten years, the company aims to establish a robust network of high-tech hospitals, smart clinics, and luxury medical centers that redefne patient experiences and set new standards in medical excellence.
Following its successful implementation of smart clinics in the UAE, GKSD is looking to introduce the same innovative healthcare model in Saudi Arabia. These next-generation medical centers provide AI-driven diagnostics, advanced imaging, and remote consultations,
Through strategic investments, cuttingedge research, and world-class expertise, GKSD is fully committed to shaping the future of healthcare in Saudi Arabia, ensuring that quality care, innovation, and accessibility remain at the heart of its mission. As part of our unwavering commitment to revolutionizing healthcare worldwide, we are embarking on an ambitious expansion, bringing our signature blend of luxury and medical excellence to new destinations. These strategic openings will not only provide state-of-the-art facilities but will also set a new benchmark in patient-centric care, seamlessly integrating the latest medical advancements with world-class hospitality.
A Landmark in Egyptian Healthcare - Our Cairo hospital (Opening 2025) will redefne medical excellence in North Africa, ofering cutting-edge treatments in a facility designed to prioritize comfort and innovation.
A Smart Approach to Premium Healthcare – Our Smart Clinic in Riyadh (Opening 2027) will introduce a groundbreaking outpatient experience, merging telemedicine, precision diagnostics, and boutique-style patient services.
Advancing Care in Iraq – The Baghdad hospital (Opening 2026) will be a beacon of modern healthcare in the region, equipped with advanced medical technology and specialized treatment programs.
Elevating European Healthcare – The Tiranë hospital (Opening 2026) will bring unparalleled medical expertise and world-class healthcare infrastructure to Albania, reinforcing our commitment to international healthcare excellence.
With these new openings, we continue to push boundaries, ensuring that our hospitals and clinics are not just centers of healing but symbols of innovation, quality, and unparalleled patient care.
Kamel Ghribi's leadership is not just about business growth, it is about reshaping industries, transforming communities, and driving sustainable progress. His strategic vision has revolutionized healthcare, investment, and philanthropy, leaving an indelible mark across Europe, the Middle East, and Africa.
As GKSD and Hospital Healthcare Holdings (HHH) continue to expand, Ghribi remains steadfast in his commitment to building a world where innovation meets accessibility, where luxury healthcare is redefned, and where quality medical services are no longer a privilege but a fundamental right. His work serves as a blueprint for ethical leadership, collaboration, and global impact, ensuring that progress extends beyond infrastructure to truly change lives.
Looking ahead, Kamel Ghribi envisions a future where healthcare, investment, and humanitarian eforts converge, creating a sustainable, patient-frst ecosystem that sets new global standards. His dedication to bridging continents, fostering partnerships, and empowering the next generation of leaders ensures that his legacy will not just be remembered—it will continue to inspire and evolve. As he often says: "True success is not measured by wealth or power, but by the lives we uplift and the legacy we leave behind."
AS GKSD AND HOSPITAL HEALTHCARE HOLDINGS (HHH) CONTINUE TO EXPAND, GHRIBI REMAINS STEADFAST IN HIS COMMITMENT TO BUILDING A WORLD WHERE INNOVATION MEETS ACCESSIBILITY, WHERE LUXURY HEALTHCARE IS REDEFINED.
he Arab African Council for Awareness (AACA) is proud to announce Dr. Ossama Shaheen's appointment as its President for the current session. Dr. Shaheen brings a wealth of distinguished experience in marketing, communications, and the health sector, making him an invaluable leader for the council’s mission. The Arab African Council for Awareness looks forward to a promising future under Dr. Shaheen’s leadership as it champions knowledge, education, and sustainable progress. In an interview with ‘Hospitals’ magazine, Dr. Shaheen expressed his gratitude for the trust placed in him, stating: “I am deeply honored to take on this leadership role and work alongside esteemed colleagues to drive meaningful change. Through collaboration and dedication, we will continue to strengthen awareness eforts and create a lasting impact across our communities.”

AACA is a non-proft organization committed to promoting awareness, education, and innovation across various felds at the regional level. Its core mission is to empower Arab and African communities with the knowledge and resources essential for sustainable development across diverse sectors. We aim to expand the council’s outreach, foster knowledge-sharing, and drive impactful initiatives that align with the United Nations' Sustainable Development Goals (SDGs).
unity, sustainability, and equitable growth in the Arab and African regions.
Our methodology is to involve harnessing the diverse expertise of infuential members to promote awareness aligned with the Sustainable Development Goals. Combining experiences, our initiatives aim to empower communities and individuals for comprehensive benefts. Through collaboration and dedication, we strive for transformative change, encouraging positive developments, inclusivity, unity, sustainability, and equitable growth in the Arab and African regions.
With a vision to inspire transformative change, AACA focuses on nurturing informed and engaged communities through diverse awareness programs and initiatives. The council’s methodology leverages the expertise of its infuential members to implement strategic initiatives that promote inclusivity,
We believe in the power of education as a tool for raising awareness and fostering knowledge in diverse felds for the betterment of Arab and African communities. Education is the cornerstone upon which individuals and societies can progress and thrive.
amantha Chatman noticed that her smooth, warm timbre was becoming increasingly hoarse.
The weekend morning anchor and investigative reporter for Chicago’s ABC7 initially thought the cause was her allergies or asthma. But after the hoarseness grew worse, she took the advice of her pastor in February 2024.
“He said, ‘You probably want to see an ear, nose and throat specialist to get that checked out,” Chatman said.
A scope passed through her nose revealed the cause: a polyp on her vocal cords.
TESTS REVEALED A RARE GROWTH: AN INFLAMMATORY MYOFIBROBLASTIC TUMOR, WHICH HAS ONLY BEEN DESCRIBED IN A HANDFUL OF MEDICAL JOURNALS
Chatman’s doctor recommended she sees the “Michael Jordan of vocal surgery,” aka University of Chicago Medicine otolaryngologist Brandon Baird, MD, to have it removed.
Baird cautioned Chatman that any polyp surgery would be followed by roughly three weeks of complete vocal rest. Chatman, an Emmy-winning journalist, had never taken more than a few days of, and she’d have to communicate via a text-to-speech app and a whiteboard.
“I wasn't thrilled with everything going on, but we had a plan,” Chatman said.
Chatman, a Hyde Park native, trusted Baird, and she was comforted by having a Black doctor — “someone who looks like you” — performing her surgery at the UChicago Medicine Center for Care and Discovery in April 2024.
When Chatman awoke from surgery, she learned that the centimeter-large round mass was more serious than her care team initially thought.
“The mass had grown notably in those three weeks between our two preoperative ofce visits, and that’s very unlikely for a polyp,” Baird said. “While we were thinking it might be a mass, we didn’t know whether or not it was benign while we awaited the fnal pathology.”
Baird told Chatman it was important to meet with UChicago Medicine’s cancer team while awaiting the biopsy results.
Chatman wept; she couldn’t believe the news.
“I remember writing, ‘You think it’s cancer?’” she said.
Tests revealed a rare growth: an infammatory myofbroblastic tumor, which has only been described in a handful of medical journals. But the tumor was benign, meaning the focus could shift from saving Chatman’s life to preserving her career by surgically removing the tumor without causing excess collateral damage.
“We were a little bit more at ease,” Baird said. “But the voice box is very important real estate, and millimeters matter when it comes to the vocal cords. You take an extra millimeter from the wrong part and you can have a permanently hoarse voice and scarred vocal cord for the rest of your life.”
WHEN CHATMAN AWOKE FROM SURGERY, SHE LEARNED THAT THE CENTIMETER-LARGE ROUND MASS WAS MORE SERIOUS THAN HER CARE TEAM INITIALLY THOUGHT.
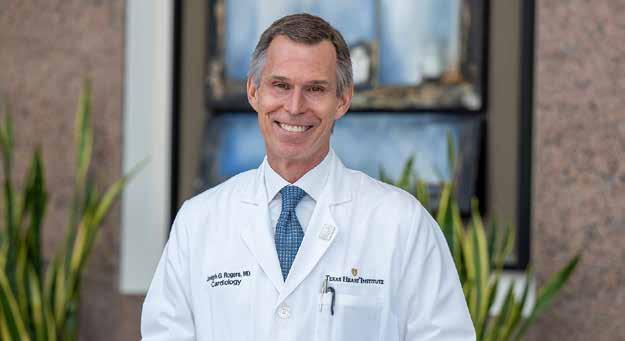
Assistant Professor of Surgery - Co-Director, Voice Center
Otolaryngologist
Brandon Jackson Baird, MD, is a laryngeal surgeon specializing in a wide range of laryngeal diseases with an emphasis on medical and surgical management of voice and swallowing disorders.
University of Chicago Medicine otolaryngologist Brandon Baird, MD, performed Samantha Chatman's vocal cord surgery
On April 24, 2024, after a preoperative prayer with Chatman and her family, Baird used microsurgical instruments and a carbon dioxide laser to surgically remove the mass without damaging Chatman’s vocal cords.
“I woke up and he said that it went really, really well,” Chatman said. “He was smiling, so it was diferent from the frst surgery.”
The recovery plan included voice rest for two months and avoiding foods that cause refux, such as carbonated drinks and spicy foods. Chatman also limited her use of pain medication, despite initial soreness.
Her voice preserved, Chatman fnally went back on air in June at ABC7, and she even shared her story on the Tamron Hall talk show in November.
Looking back, Chatman said remaining silent wasn’t all that bad.
“It gives you a lot of time to refect, listen,
observe and take in,” she said. “That period was a life-changing experience.”
With time and the help of monthly vocal therapy sessions, Chatman’s vocal cords are back to their normal function.
“She’s been able to get a higher part of her range back,” Baird said. “And she's been able to do her job, which is ultimately the goal.”
Still, Chatman does occasionally notice that she can become vocally fatigued after a long day. She isn’t sure if that's due to the tumor or whether she is now more aware of the health of her vocal cords. Like Baird, she urges anyone who begins to experience a hoarseness that will not go away to get checked out by a doctor.
“Pay attention to your symptoms; you’ve got to put your health frst and let the doctors do what they need to do, because everything else will fall into place,” Chatman said.
ON APRIL 24, 2024, AFTER A PREOPERATIVE PRAYER WITH CHATMAN AND HER FAMILY, BAIRD USED MICROSURGICAL INSTRUMENTS AND A CARBON DIOXIDE LASER TO SURGICALLY REMOVE THE MASS WITHOUT DAMAGING CHATMAN’S VOCAL CORDS.
Samantha Chatman is back on the job again at Chicago's ABC7 studio
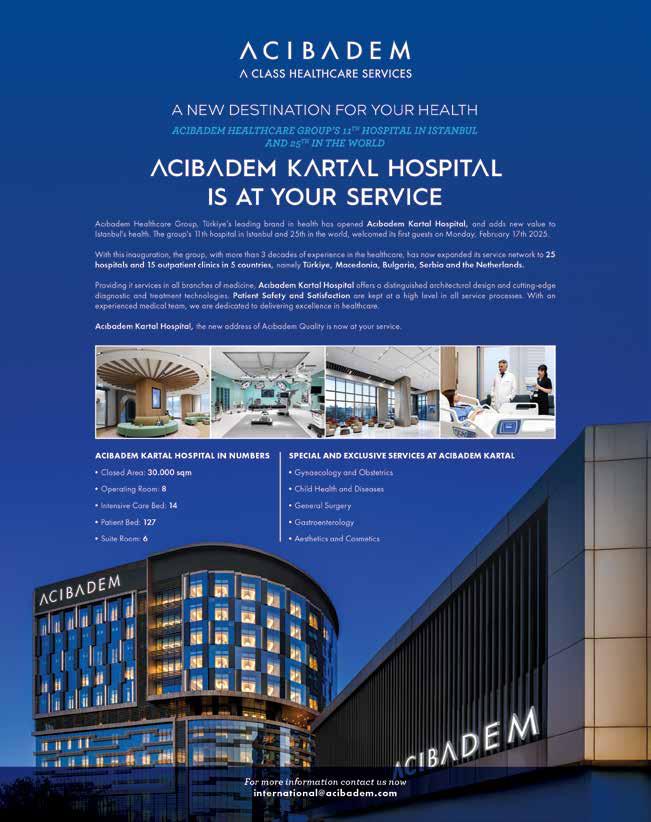
Hôtel-Dieu de France (HDF) and Saint Joseph University (USJ) proudly announce the signing of a groundbreaking agreement to introduce Lebanon’s frst and latest generation Cambridge Medical Robotics (CMR) Versius® Surgical Robot system. This cutting-edge technology, provided by PROMEDZ in Lebanon, as the ofcial representative of CMR Surgical (UK), positions HDF and USJ as regional pioneers in robotic surgery.
Known for its versatility, the system is set to be applied across several key specialties, including minimally invasive procedures in colorectal, urological, gynecological, thoracic, and general surgeries. This advanced approach enhances precision and reduces recovery times, benefting both patients and healthcare providers, marking a new era of healthcare excellence in Lebanon.
“We are thrilled to lead the way in advanced surgical care by introducing the CMR Versius® system at our hospital. This robot will enhance the quality of care we provide to our patients, further solidifying our commitment to excellence in healthcare,” said Mr. Nassib Nasr, CEO of Hôtel-Dieu de France.
The project also extends to the academic sector through a collaboration with the Faculty
of Medicine of Saint Joseph University, which will host a frst of its kind dedicated animal lab training facility for robotic surgery in the region. This training hub will include an identical CMR Versius Surgical robot, separate from the hospital facility, and will serve not only Lebanese surgeons but also aspiring robotic surgeons from across the region.
“This initiative will establish Lebanon as a reference point for surgical robotics training,” emphasized Prof. Elie Nemer, Dean of the Faculty of Medicine at Saint Joseph University and Head of the Urology Department at HôtelDieu de France. “It will allow surgeons to gain invaluable hands-on experience with the most advanced surgical technology available to enhance performance on the patient and ensure that it’s never the frst time on the patient; The frst surgeries with the robotic system at HDF were successfully conducted on prostate cancer patients during February”.
“PROMEDZ and CMR Surgical worked closely with HDF and USJ to ensure the seamless integration of the Versius® system. This includes comprehensive training and support for medical teams and the launch of the “Train the Trainer” program, further emphasizing Lebanon’s strong position in the region” said Mr. Hady Bsat, Chairman of PROMEDZ.
KNOWN FOR ITS VERSATILITY, THE SYSTEM IS SET TO BE APPLIED ACROSS SEVERAL KEY SPECIALTIES, INCLUDING MINIMALLY INVASIVE PROCEDURES IN COLORECTAL, UROLOGICAL, GYNECOLOGICAL, THORACIC, AND GENERAL SURGERIES. THIS ADVANCED APPROACH ENHANCES PRECISION AND REDUCES RECOVERY TIMES, BENEFITING BOTH PATIENTS AND HEALTHCARE PROVIDERS, MARKING A NEW ERA OF HEALTHCARE EXCELLENCE IN LEBANON.
Boehringer Ingelheim, a leading researchdriven biopharmaceutical company, has collaborated with Emirates Thoracic Society (ETS) and social media infuencer Ghaith Marwan, to raise awareness of Interstitial Lung Disease (ILD) through a community engagement initiative achieving 1 million steps and culminating in a breathtaking installation unveiling at Dubai Miracle Garden on 22 February 2025.
ILD is an umbrella term used for several diseases that cause scarring, or fbrosis, of the lungs. The scarring causes stifness in the lungs which makes it difcult to breathe and deliver oxygen to the bloodstream. Lung damage from ILDs is often irreversible and progresses over time. Common symptoms of ILD are shortness of breath, consistent dry cough, chest discomfort, fatigue and occasionally weight loss. Early diagnosis and treatment of many ILD diseases, such as Idiopathic pulmonary fbrosis (IPF), can slow disease progression and preserve quality of life for patients .
Under the theme ‘Think Lungs’, the social media campaign encouraged the public to share their breathtaking moments together with their daily step count to reach the collective goal of one million steps. The campaign concluded at the Dubai Miracle Garden in the presence of ETS representatives, renowned pulmonologists, Boehringer Ingelheim representatives and Ghaith Marwan. The event saw the unveiling of a 5-meter lung installation made entirely of colorful and blossoming fowers. Following the event, in line with Boehringer Ingelheim’s commitment to sustainability, the fowers from the installation were gifted to Rashid Centre For People of Determination.
Derek O’Leary, Regional Managing Director, Boehringer Ingelheim in India, Middle East, Turkey and Africa, said: “Lung health shouldn’t be an afterthought—it should be a priority. At Boehringer Ingelheim, we launched "Think Lungs" to spark a movement, because awareness leads to action, and action can improve lives.
Seeing people come together to join our 1 Million step for ILD awareness movement and stand before the lung installation at Dubai’s Miracle Garden was a powerful reminder of what’s possible when people come together for a cause. Our vision is a future where early diagnosis is the norm, individuals take charge of their lung health, and communities replace stigma with support and hope.”
Dr. Bassam Mahboub, Head of the Pulmonology, Department at Rashid Hospital and Vice President of the Emirates Thoracic Society, said, “Diagnosing ILD can be a challenge given the shared symptoms with other lung diseases and delays in treatment can hinder eforts to improve outcomes. It is encouraging to see key healthcare stakeholders come together with a shared vision to raise public awareness of lung diseases which are often overlooked. Awareness campaigns like ‘Think Lungs’, empower communities to seek expert opinions early and to ask their physicians the right questions which can potentially lead to earlier diagnosis and better treatment outcomes.”
THE CAMPAIGN HIGHLIGHTED THE NEED FOR PROACTIVE ATTENTION TO LUNG HEALTH, ENCOURAGING INDIVIDUALS TO RECOGNIZE SYMPTOMS AND SEEK TIMELY MEDICAL ADVICE. THROUGH THIS INITIATIVE, BOEHRINGER INGELHEIM AIMS TO INSPIRE BEHAVIORAL CHANGE, HIGHLIGHT THE POWER OF EARLY DETECTION, AND UNITE COMMUNITIES IN A SHARED COMMITMENT TO LUNG HEALTH.
Liquid biopsy in breast cancer – Less invasion more precision
HEALTHCARE PARTNER
Our Best Services
Turnkey Healthcare Solutions
Custom solutions tailored to healthcare providers' needs
Medical Equipment Distribution
Partnerships with leading global brands to ensure quality and innovation
Pharmatrade offers a diverse portfolio of over 5000 high-quality medical and pharmaceutical products, tailored to meet the needs of both the Government and Private sectors in the UAE.
Pharmaceutical & Healthcare Product Supply
Compliance with international healthcare standards for safety and efficacy
48 Years of Excellence in UAE
Trusted partner in healthcare excellence since 1977
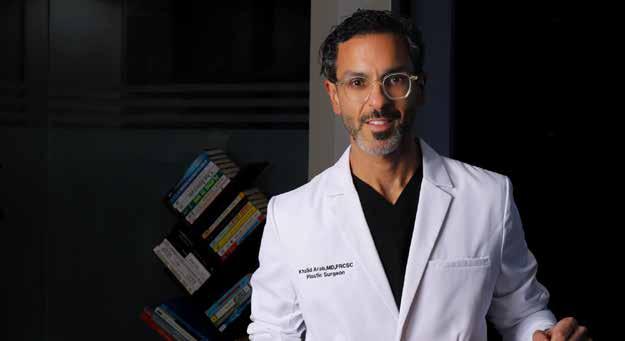
besity remains a global epidemic, impacting millions of lives and posing signifcant health risks. In recent years, bariatric surgery and weight-loss treatments have evolved dramatically, integrating cutting-edge surgical techniques, advanced medications, and a comprehensive, multidisciplinary approach to patient care. In this exclusive interview with "Hospitals" Magazine, Dr. Samer Gamil Mattar, Professor and Chief of the Division of Metabolic and Bariatric Surgery, discussed the latest innovations in the feld, the impact of GLP-1 medications, and the future role of AI in personalized obesity treatment. With decades of experience, Dr. Mattar shares insights on how modern bariatric surgery has transformed into a safe, efective, and lifelong solution for patients seeking better health and improved quality of life.
My role focuses on ensuring high-quality patient care, expanding access to our services, and continuously improving outcomes.
This includes reaching out to the community, building relationships with referring providers, and tracking patient data to optimize treatments. We also integrate medical weightloss therapies, which have become a key component of obesity management.
Despite being a recognized epidemic, obesity still faces misconceptions and stigma.
Many people blame themselves, believing it’s solely a lifestyle issue, which prevents them from seeking treatment. In reality, obesity is multifactorial—genetics, metabolism, and environmental factors all play a role.
Processed foods and changing dietary habits have also contributed to rising obesity rates worldwide.
OUR TEAM INCLUDES DIETITIANS, PSYCHOLOGISTS, AND EXERCISE SPECIALISTS, ENSURING COMPREHENSIVE PATIENT CARE. WE’VE ALSO REFINED SURGICAL TECHNIQUES TO REDUCE COMPLICATIONS AND IMPROVE RECOVERY
The most important shift has been adopting a multidisciplinary approach. Previously, surgery was a standalone procedure, but now we understand that lifelong support is crucial.
Our team includes dietitians, psychologists, and exercise specialists, ensuring comprehensive patient care.We’ve also refned surgical techniques to reduce complications and improve recovery.
Additionally, weight-loss medications have played a major role in optimizing patient results.
We follow a patient-centered approach, often referred to as the “white glove treatment.” Every patient is assigned a navigator to guide them through their journey, ensuring they receive the right care at every stage.
More importantly, we emphasize that obesity is a medical condition, not a personal failure. We treat it like any other disease, providing compassionate and bias-free care.
In the past, bariatric surgery had a higher risk of complications, and patients often lacked longterm follow-up. Today, it is as safe as natural childbirth and even safer than gallbladder surgery. Previously, patients were left to manage on their own, leading to nutritional defciencies and weight regain. Now, we focus on extensive preoperative education and lifelong follow-ups, signifcantly improving longterm success.
We now perform 100% laparoscopic procedures and rely heavily on robotic-assisted surgery, which enhances precision and reduces recovery time. A key advancement is the Single Anastomosis Duodenal Ileostomy (SADI), a procedure designed to maximize weight loss while preserving nutrition. We are also exploring endoscopic treatments and magnetic technology, which ofer less invasive alternatives for weight loss.
Bariatric surgery resets metabolism, reducing hunger and improving overall health. Patients often experience:
• Diabetes remission – Many stop using insulin.
• Blood pressure and cholesterol improvement – Reducing cardiovascular risks.
• Sleep apnea resolution – Many no longer need CPAP machines.
• Joint pain relief – Less strain and infammation.
• Psychological benefts – Increased energy, confdence, and mental well-being. Interestingly, many female patients receive job promotions or salary increases within a year post-surgery, highlighting how appearance infuences workplace opportunities.
WE NOW PERFORM 100% LAPAROSCOPIC PROCEDURES AND RELY HEAVILY ON ROBOTIC-ASSISTED SURGERY, WHICH ENHANCES PRECISION AND REDUCES RECOVERY TIME. A KEY ADVANCEMENT IS THE SINGLE ANASTOMOSIS DUODENAL ILEOSTOMY (SADI), A PROCEDURE DESIGNED TO MAXIMIZE WEIGHT LOSS WHILE PRESERVING NUTRITION.
It is already the present. Robotic-assisted surgery has become the standard of care, and the future lies in minimally invasive and endoscopic innovations.
Patients need to be motivated and meet specifc BMI criteria. Previously, BMI requirements were 40+ or 35+ with health conditions like diabetes. However, new guidelines lower the BMI threshold, allowing more patients to qualify. Before surgery, we ensure patients are medically optimized and fully educated on
postoperative lifestyle changes.
These drugs are among the most signifcant medical advancements of the century. We discovered that bariatric surgery naturally boosts GLP-1 levels, reducing hunger and improving metabolism. Pharmaceutical companies have now replicated this efect with injectable weight-loss medications. However, the key diference is sustainability. Surgery provides a lifetime efect, while medications require ongoing use. Many patients struggle with side efects or the high cost of these drugs, making surgery a more practical solution for long-term success.
metabolic improvements.
• Long-term success rates for diferent approaches.
No. Surgery remains the superior option for signifcant weight loss. However, medications work well for patients with moderate weight concerns and can be used before and after surgery as part of a comprehensive plan.
This will make decision-making more precise and improve overall patient outcomes.
Previously, we required patients to stop them two weeks before surgery to prevent aspiration risks. However, new guidelines suggest discontinuation is no longer necessary.
Future medications will be more powerful and better tolerated.
Pharma companies are using AI-driven drug development to minimize side efects while enhancing efectiveness. We are also exploring advanced endoscopic procedures and magnetic technologies, which could ofer non-surgical solutions for weight loss.
WE FOLLOW A PATIENT-CENTERED APPROACH, OFTEN REFERRED TO AS THE “WHITE GLOVE TREATMENT.” EVERY PATIENT IS ASSIGNED A NAVIGATOR TO GUIDE THEM THROUGH THEIR JOURNEY, ENSURING THEY RECEIVE THE RIGHT CARE AT EVERY STAGE. MORE IMPORTANTLY, WE EMPHASIZE THAT OBESITY IS A MEDICAL CONDITION, NOT A PERSONAL FAILURE. WE TREAT IT LIKE ANY OTHER DISEASE, PROVIDING COMPASSIONATE AND BIAS-FREE CARE
AI will be a game-changer. Even with 25 years of experience, I sometimes struggle to determine the best surgical approach for each patient. AI will analyze millions of patient cases and provide personalized recommendations for:
• The best procedure based on individual health factors.
• Expected weight loss outcomes and
Obesity is not your fault. It is a medical condition that requires professional care.
With advancements in surgery, medications, and multidisciplinary support, there are more treatment options than ever.
If you are struggling with weight-related health issues, don’t hesitate to seek medical guidance—there is a solution tailored for you.
r. Joseph G. Rogers, Director of the Texas Heart Institute at Baylor College of Medicine, is a leading cardiologist and an internationally recognized expert in heart failure, heart transplantation, and mechanical circulatory support. In this exclusive interview, he discusses the latest challenges and breakthroughs in cardiovascular medicine, the future of heart transplantation, and the impact of artifcial intelligence in cardiology.
and a half years, I have been leading The Texas Heart Institute, working to advance research, education, and clinical innovation in cardiovascular medicine.
I have dedicated my career to the study and treatment of advanced heart failure, heart transplantation, and mechanical circulatory support. Before joining The Texas Heart Institute, I spent nearly two decades at Duke University and a decade at Washington University in St. Louis. For the past three
The biggest challenge is prevention. Ideally, we would prevent heart disease before it even occurs rather than just treating it after diagnosis. Cardiovascular disease is primarily driven by cardiometabolic conditions—high blood pressure, high cholesterol, diabetes, and obesity. These conditions are often linked to lifestyle factors such as poor diet, lack of exercise, and smoking.
We are seeing groundbreaking innovations, but one of the biggest concerns is accessibility. For example, the recent development of GLP-1 receptor agonists, such as semaglutide (Ozempic), is transforming the management of
THE BIGGEST CHALLENGE IS PREVENTION. IDEALLY, WE WOULD PREVENT HEART DISEASE BEFORE IT EVEN OCCURS RATHER THAN JUST TREATING IT AFTER DIAGNOSIS. CARDIOVASCULAR DISEASE IS PRIMARILY DRIVEN BY CARDIOMETABOLIC CONDITIONS—HIGH BLOOD PRESSURE, HIGH CHOLESTEROL, DIABETES, AND OBESITY
obesity and metabolic disease, but their cost limits access for many people worldwide. At the end of the day, the most efective solution is promoting healthy lifestyles—ensuring access to nutritious foods, encouraging physical activity, and eliminating smoking.
One of the most exciting breakthroughs has been the use of SGLT2 inhibitors, which were originally developed to treat diabetes but have shown remarkable benefts in heart failure patients, even those without diabetes. What’s fascinating is that we still don’t fully understand their exact mechanism of action, but the clinical results are undeniable.
Lifestyle changes are essential, but they require a multi-faceted approach. It’s not just about telling people to eat better or exercise more— it’s about ensuring they have the means to do so. I recall a patient I treated in North Carolina who struggled with severe obesity. She told me it was more afordable to feed her children at fast-food restaurants than to buy fresh ingredients and cook at home.
This highlights a deeper systemic issue. We need policies that improve access to afordable, healthy food and create environments where people can exercise safely. In Houston, for instance, I spoke with community members who said stray dogs in their neighborhoods prevented them from going outside for walks. These are real-life barriers that policymakers must address to make a signifcant impact on public health.
Mechanical circulatory support has evolved tremendously over the years. The current leading device is a continuous-fow left ventricular assist device (LVAD), which has proven to be a life-saving bridge to transplant and even a long-term alternative for some patients.
At The Texas Heart Institute, we are at the forefront of artifcial heart development. One of the most promising innovations is the BiVACOR Total Artifcial Heart, which is based on magnetic levitation (maglev) technology. This device supports both the right and left sides of the heart and has the potential to be a durable alternative to transplantation.
AT THE TEXAS HEART INSTITUTE, WE ARE AT THE FOREFRONT OF ARTIFICIAL HEART DEVELOPMENT. ONE OF THE MOST PROMISING INNOVATIONS IS THE BIVACORE TOTAL ARTIFICIAL HEART, WHICH IS BASED ON MAGNETIC LEVITATION (MAGLEV) TECHNOLOGY. THIS DEVICE SUPPORTS BOTH THE RIGHT AND LEFT SIDES OF THE HEART AND HAS THE POTENTIAL TO BE A DURABLE ALTERNATIVE TO TRANSPLANTATION
There have been several major advancements in the management of heart failure, particularly in drug therapy. The standard of care now includes four key pillars of medication that can dramatically improve outcomes.
What’s critical is the urgency of initiating treatment. Historically, physicians would introduce one medication at a time over several months or even years. Now, we understand that getting patients on these therapies as soon as possible—within the frst few months of diagnosis—signifcantly reduces hospitalizations and mortality.
The FDA recently approved early feasibility studies, and the initial results have been very encouraging. One patient in Australia has been supported on the device for over two months, which is an exciting step forward.
Two key advancements are reshaping heart transplantation. The frst is non-invasive rejection monitoring.
Traditionally, we’ve had to perform heart biopsies to check for rejection, but now, we can use a blood test that detects donor DNA fragments in the recipient’s bloodstream. This allows us to monitor rejection without invasive procedures, making post-transplant care
safer and more efective. The second major development is in donor organ preservation and transportation.
We have moved away from simply placing donor hearts in ice and now use advanced preservation techniques that keep the heart warm and beating or maintain it in a controlled cold environment. These strategies improve organ viability and allow us to retrieve hearts from farther distances, increasing the available donor pool.
We are involved in several pioneering projects, including:
• Stem Cell Therapy: Researchers have demonstrated that injecting stem cells into the heart reduces infammation and lowers the risk of heart attacks and strokes.
AI is already making a signifcant impact, particularly in diagnostics. For example, electrocardiograms (ECGs) have been interpreted using AI-based algorithms for years, and now, machine learning is being applied to echocardiograms to enhance the detection of abnormalities.
In the future, AI could play a crucial role in personalized medicine, integrating genetic and clinical data to tailor treatment plans for individual patients. We are just scratching the surface, but I believe AI will become a standard tool in cardiology within the next decade.
• Gene Therapy: Scientists have identifed a molecular pathway that stops heart muscle cells from regenerating. By turning of this “stop signal,” they have successfully regenerated heart tissue in animal models, with human trials set to begin soon.
• Heart Regeneration: Our researchers are working on creating bioengineered hearts by washing out cells from animal hearts and repopulating them with human stem cells. This could one day lead to lab-grown hearts for transplantation.
These are exciting developments that could completely transform cardiovascular medicine.
IN THE FUTURE, AI COULD PLAY A CRUCIAL ROLE IN PERSONALIZED MEDICINE, INTEGRATING GENETIC AND CLINICAL DATA TO TAILOR TREATMENT PLANS FOR INDIVIDUAL PATIENTS. WE ARE JUST SCRATCHING THE SURFACE, BUT I BELIEVE AI WILL BECOME A STANDARD TOOL IN CARDIOLOGY WITHIN THE NEXT DECADE
Birthing couches: Versatile Medical Equipment for Natural Birth Positions
Birthing couches are adaptable medical aids equipped with additional features that support physiological positions during childbirth. They help women relax more easily and choose the position that feels most natural at any given moment.
These specialized pieces of equipment are designed for use during childbirth, allowing women to adopt various positions that are both physiological and comfortable. Birthing couches are crafted to promote the physiological process of labor while enhancing the comfort of the birthing woman. They also enable close proximity to a partner or companion.
Birthing couches are commonly utilized in maternity wards that prioritize physiological birthing practices and value the comfort of the mother.
The LINDU Medical Birthing Couches features armrests and a range of accessories. It is foldable and portable. The couch is covered with a two-layer medical-grade material with certified quality, bonded seams, and foam padding. It is fully disinfectable to meet the needs of hospitals and maternity wards. The material is flexible and pleasant to the touch.
Additional components of the couch come in various shapes, are refillable, and can be supplemented as needed.
The positions in which women give birth are not just a result of the physiology and function of the female body and the birth process. They are influenced by the culture we live in, the images and understanding of birth that we have and, of no less importance, by the training of midwives and medical professionals. It is time to base our care on evidence and facts.
Benefits of vertical birth positions
• Active vertical positions support the natural biomechanics of labour, which means less complications and healthier both, baby and mother.
• The foetus has more room to rotate in the birth canal as there are increases in most pelvic measurements.
• Labour is shorter and less painful.
• Due to evidence, it is more beneficial to move and change birthing positions than to stay in one specific position.
David Winkler CFO Lindu medical
Currently, over 50% hospitals in the Czech republic and 6 in Slovakia are equipped with birthing couches and have undergone the implementation workshop on active vertical birth and practical couch care guidance.
ospitals Magazine had the privilege of speaking with Vivek Kanade, Managing Director of Siemens Healthineers for the Middle East and Africa, during Arab Health 2025. With over 31 years at Siemens Healthineers, Kanade shares insights on the company’s vision, technological advancements, AI integration, and the evolving healthcare landscape in the region.
I have been with Siemens Healthineers for 31 years, working across diferent regions, including India, Germany, and Singapore. For the past 18 months, I have been leading the Middle East and Africa operations. Throughout my journey, I have witnessed the evolution of healthcare technologies and how Siemens Healthineers has continuously pioneered breakthroughs in the industry.
Our vision is encapsulated in our purpose statement: “We pioneer breakthroughs in healthcare. For everyone. Everywhere.”
While Siemens Healthineers has long been recognized for its innovation, quality, and robustness, our goal is to ensure that these breakthroughs reach all communities, including underserved regions.
Globally, more than 3.5 billion people still lack access to quality healthcare.
This issue is not limited to developing nations; even in advanced economies, rural and peripheral areas struggle with accessibility. We are addressing this challenge through a multi-faceted approach—providing advanced products, fnancial services, AI-driven solutions, and training programs to bridge the gap.
WHILE SIEMENS HEALTHINEERS HAS LONG BEEN RECOGNIZED FOR ITS INNOVATION, QUALITY, AND ROBUSTNESS, OUR GOAL IS TO ENSURE THAT THESE BREAKTHROUGHS REACH ALL COMMUNITIES, INCLUDING UNDERSERVED REGIONS.
The shortage of medical professionals is one of the most pressing challenges in global healthcare. To address this, we have developed solutions that optimize efciency and reduce dependency on highly skilled resources.
One of our fagship innovations is the Single Virtual Cockpit, which allows trained professionals in urban centers to remotely operate complex imaging systems, such as MRI and CT scanners, installed in remote locations. This technology has been successfully implemented in Brazil, where a central command center in São Paulo manages 70 MRI units located in smaller towns. Instead of requiring over 200 technologists, just 15 experts remotely oversee operations, ensuring standardized image quality and minimizing service disruptions.
Furthermore, we integrate AI-assisted diagnostics, which categorize scans based on complexity, enabling radiologists to focus on cases that require immediate attention. In addition, our education and training programs, often in collaboration with leading universities, help build a sustainable pipeline of healthcare professionals.
Flow MRI system, which eliminates the need for 3,000 liters of liquid helium—previously essential for MRI scanners. Instead, this nextgeneration MRI uses less than a liter of liquid helium in a sealed system, drastically reducing infrastructure and maintenance requirements. This means that MRI units can now be installed in smaller hospitals and rural clinics, expanding access to advanced imaging technology.
Innovation at Siemens Healthineers is focused on two primary goals: enhancing clinical outcomes and making technology more accessible and scalable.
One of our most groundbreaking developments is Photon-Counting CT technology, which signifcantly improves diagnostic capabilities. Traditional CT scans struggle to provide clear imaging in patients with high calcium buildup in their arteries. However, with Photon-Counting CT, we can visualize internal structures with unprecedented clarity, eliminating the need for invasive angiograms in many cases.
Another breakthrough is the Magnetom
AI is becoming an integral part of modern healthcare, but rather than replacing professionals, it acts as an enabler—enhancing accuracy, efciency, and consistency.
At Siemens Healthineers, we leverage AI in multiple areas, from imaging and diagnostics to workfow optimization. Our AI algorithms have been trained on over one billion medical images, making them some of the most advanced in the industry. These algorithms assist radiologists by highlighting anomalies, prioritizing urgent cases, and reducing human error. A great analogy for AI in healthcare is that of a screwdriver—it’s a tool that helps professionals do their jobs faster and better. While AI will never replace radiologists or physicians, it will continue to serve as an essential partner in delivering highquality healthcare.
AT SIEMENS HEALTHINEERS, WE LEVERAGE AI IN MULTIPLE AREAS, FROM IMAGING AND DIAGNOSTICS TO WORKFLOW OPTIMIZATION. OUR AI ALGORITHMS HAVE BEEN TRAINED ON OVER ONE BILLION MEDICAL IMAGES, MAKING THEM SOME OF THE MOST ADVANCED IN THE INDUSTRY. THESE ALGORITHMS ASSIST RADIOLOGISTS BY HIGHLIGHTING ANOMALIES, PRIORITIZING URGENT CASES, AND REDUCING HUMAN ERROR. A GREAT ANALOGY FOR AI IN HEALTHCARE IS THAT OF A SCREWDRIVER—IT’S A TOOL THAT HELPS PROFESSIONALS DO THEIR JOBS FASTER AND BETTER. WHILE AI WILL NEVER REPLACE RADIOLOGISTS OR PHYSICIANS, IT WILL CONTINUE TO SERVE AS AN ESSENTIAL PARTNER IN DELIVERING HIGH-QUALITY HEALTHCARE.
Collaboration is at the heart of healthcare innovation. We work closely with government entities, private healthcare providers, and academic institutions to develop solutions tailored to the region’s unique needs. One of our most ambitious partnerships is with the Dubai Health Authority (DHA), where we are establishing a centralized imaging repository. This system will connect both public and private hospitals, ensuring that every patient’s imaging history is accessible across the network. By streamlining medical data, we improve continuity of care, reduce redundant scans, and enhance treatment planning.
Adoption in the Middle East is exceptionally fast. The region is known for being an early adopter of cutting-edge technologies, which is why innovations such as Photon-Counting CT and Magnetom Flow MRI are expected to be implemented here in a matter of months.
However, technology alone isn’t enough— training is crucial. We provide extensive training through dedicated centers and reference sites, where healthcare professionals can gain handson experience with our latest innovations. Additionally, our in-hospital clinical specialists provide on-site training whenever a new system is installed.
services while maintaining high standards of quality and efciency.
We are witnessing a shift towards valuebased care, where the emphasis is on patient outcomes rather than just service volume. This aligns well with Siemens Healthineers’ strategy of integrating AI, remote technologies, and precision medicine into everyday healthcare.
The Middle East’s healthcare market is dynamic and growing rapidly. Governments and private investors are actively driving advancements in medical infrastructure, AI adoption, and digital health initiatives.
The focus is on scaling up healthcare
Arab Health continues to solidify its position as one of the most infuential healthcare events worldwide. The level of engagement, discussions, and partnerships formed here demonstrate the region’s commitment to advancing healthcare. The energy this year has been incredible. We are thrilled to showcase our latest innovations and collaborate with industry leaders to shape the future of healthcare in the Middle East and beyond.
"Hospitals" Magazine thanks Vivek Kanade for his insights and looks forward to seeing how Siemens Healthineers continues to drive innovation in global healthcare.
ADOPTION IN THE MIDDLE EAST IS EXCEPTIONALLY FAST. THE REGION IS KNOWN FOR BEING AN EARLY ADOPTER OF CUTTING-EDGE TECHNOLOGIES, WHICH IS WHY INNOVATIONS SUCH AS PHOTONCOUNTING CT AND MAGNETOM FLOW MRI ARE EXPECTED TO BE IMPLEMENTED HERE IN A MATTER OF MONTHS. HOWEVER, TECHNOLOGY ALONE ISN’T ENOUGH— TRAINING IS CRUCIAL. WE PROVIDE EXTENSIVE TRAINING THROUGH DEDICATED CENTERS AND REFERENCE SITES, WHERE HEALTHCARE PROFESSIONALS CAN GAIN HANDSON EXPERIENCE WITH OUR LATEST INNOVATIONS. ADDITIONALLY, OUR IN-HOSPITAL CLINICAL SPECIALISTS PROVIDE ON-SITE TRAINING WHENEVER A NEW SYSTEM IS INSTALLED.

Signifcant advancements in cancer treatment have revolutionized how we approach this disease, leading to remarkable improvements in patients’ lives. These advancements have been refected in increased treatment efcacy, as some types of cancer that were once considered fatal are now treatable and curable. Additionally, these modern treatments have greatly enhanced the quality of life for patients by reducing side efects, making the treatment and recovery periods more bearable and comfortable.
Moreover, these developments have played a pivotal role in extending the lifespan of cancer patients. Many patients now live longer after diagnosis and treatment, allowing them more time with their loved ones and the opportunity to enjoy a better quality of life.
According to the World Health Organization (WHO), cancer is one of the leading causes of death worldwide, responsible for nearly 10 million deaths in 2020, which accounts for approximately one in every six deaths.
About a third of cancer deaths are attributed to tobacco use, high body mass index, alcohol consumption, low fruit and vegetable intake, and lack of physical activity. In addition, air pollution is a signifcant risk factor for lung cancer. Cancer-causing infections, such as the Human Papillomavirus (HPV) and hepatitis, are responsible for about 30% of cancer cases in low- and middle-income countries.
Many types of cancer can be treated if detected early and managed efectively. New cancer treatments, improved screening strategies, and the use of the HPV vaccine for cancer prevention are contributing to reducing cancer mortality rates. HPV infection is linked to several diseases, especially cervical cancer and head and neck cancers.
The World Health Organization states that between 30% and 50% of cancer cases can now be prevented by avoiding risk factors and
implementing prevention strategies. Cancer burden can also be reduced through early detection, appropriate treatment, and patient care for those diagnosed with cancer. Many types of cancer have a high cure rate if diagnosed early and treated appropriately.
The signifcant advancements in cancer treatment provide great hope for patients and their families. Thanks to these developments, cancer has become less terrifying, with many cases now being curable. As scientifc research and technological development continue, we expect further progress in the future, leading to better treatment outcomes, higher cure rates, and longer survival for cancer patients. Cancer treatment has undergone unprecedented developments in recent years, revolutionizing the way we handle this disease and signifcantly contributing to higher cure rates and prolonged patient survival.
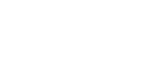
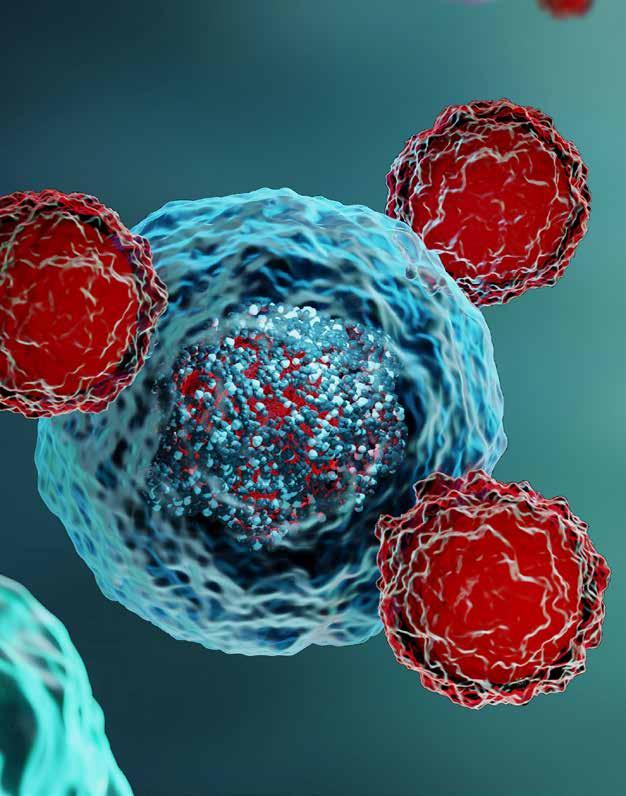
1. Immunotherapy: This treatment harnesses the body’s immune system to attack and destroy cancer cells. It has shown great promise, especially for certain types of cancer such as skin cancer and lung cancer.
2. Targeted Therapy: This type of treatment directly targets cancer cells without afecting healthy cells. It focuses on identifying genetic mutations or proteins on the surface of cancer cells and developing drugs that target these markers, reducing side efects associated with chemotherapy.
3. Precision Radiation Therapy: Uses advanced imaging techniques to precisely target radiation at cancer cells while minimizing damage to surrounding healthy tissues. It reduces side efects compared to traditional radiation therapy.
ABOUT A THIRD OF CANCER DEATHS ARE ATTRIBUTED TO TOBACCO USE, HIGH BODY MASS INDEX, ALCOHOL CONSUMPTION, LOW FRUIT AND VEGETABLE INTAKE, AND LACK OF PHYSICAL ACTIVITY. IN ADDITION, AIR POLLUTION IS A SIGNIFICANT RISK FACTOR FOR LUNG CANCER. CANCERCAUSING INFECTIONS, SUCH AS THE HUMAN PAPILLOMAVIRUS (HPV) AND HEPATITIS, ARE RESPONSIBLE FOR ABOUT 30% OF CANCER CASES IN LOW- AND MIDDLEINCOME COUNTRIES.
4. Robotic Surgery: Used for highly precise surgeries, reducing incision size and recovery time, and allowing for more complex operations to be performed with greater accuracy
5. Personalized Medicine: Based on analyzing the genetic and biological characteristics of each patient to determine the most efective treatment plan for their specifc condition, improving treatment outcomes and reducing side efects.
6. Gene Therapy: Aims to modify the genes responsible for cancer cell growth and replication. While still in the developmental stages, gene therapy holds great potential for treating specifc types of cancer.
Advancements in diagnostic techniques for detecting cancer, coupled with greater awareness of the importance of early detection, have signifcantly changed how this disease is managed. Thanks to these developments, it is now possible to detect cancer at its early stages, increasing the chances of successful treatment and improving patients’ quality of life.
blood samples to detect cancerous DNA or circulating cancer cells. It is a non-invasive method for cancer detection and disease monitoring.
Helps identify genetic mutations associated with specifc types of cancer. It is used to assess cancer risk and guide treatment decisions.
These are substances secreted by cancer cells and can be measured in blood or urine. They are used for detecting certain types of cancer and monitoring patient response to treatment.
• MRI (Magnetic Resonance Imaging) provides detailed images of organs and internal tissues, helping to detect small tumors and determine their extent.
• PET (Positron Emission Tomography) uses radioactive materials to identify active cancer cells, enabling the detection of tumors in their early stages.
• CT (Computed Tomography) Scan ofers three-dimensional images of internal organs, aiding in tumor detection and assessment of size and location.
• Ultrasound generates images of internal organs and is a safe and noninvasive method.
: This technique involves analyzing
Early cancer detection plays a critical role in treatment success. The chances of recovery are signifcantly higher when the disease is detected in its early stages, as treatment is more efective and less complicated. Early detection also reduces the need for intensive treatment, as cancer can often be managed with less invasive therapies, such as targeted surgery or precision radiation, thus minimizing potential side efects. Moreover, early detection contributes to improving the patient’s overall quality of life, as treatments in the early stages are generally less taxing and allow the patient to maintain a better lifestyle. Finally, early detection is more cost-efective. Treating cancer at an early stage is far less expensive than treating it in advanced stages, making it a more economical choice as well.
EARLY CANCER DETECTION PLAYS A CRITICAL ROLE IN TREATMENT SUCCESS. THE CHANCES OF RECOVERY ARE SIGNIFICANTLY HIGHER WHEN THE DISEASE IS DETECTED IN ITS EARLY STAGES, AS TREATMENT IS MORE EFFECTIVE AND LESS COMPLICATED. EARLY DETECTION ALSO REDUCES THE NEED FOR INTENSIVE TREATMENT, AS CANCER CAN OFTEN BE MANAGED WITH LESS INVASIVE THERAPIES, SUCH AS TARGETED SURGERY OR PRECISION RADIATION, THUS MINIMIZING POTENTIAL SIDE EFFECTS.
CLA research fnds that combining immunotherapy with chemotherapy is safe and efective for people with advanced small cell cancers in the bladder and prostate.
A research team led by UCLA Health Jonsson Comprehensive Cancer Center investigators has shown that combining pembrolizumab, an immunotherapy drug, with standard chemotherapy can improve treatment outcomes for patients with small cell bladder cancer and
small cell/neuroendocrine prostate cancer.
Small cell carcinomas can arise in various tissues—including the bladder, prostate, lung, ovaries and breast—and are known for their rapid progression, tendency to relapse after initial treatment and poor overall survival rates. The survival time for patients with advanced small cell bladder cancer is only about 7 to 13 months and only 7 to 9 months for patients with small cell/neuroendocrine prostate cancer.
The early-stage study, published in Cell Reports Medicine, showed that using
IN BLADDER CANCER GROUP, ONLY ONE OUT OF SEVEN PATIENTS EXPERIENCED DISEASE
PROGRESSION AFTER A MEDIAN FOLLOWUP OF ALMOST THREE YEARS.
pembrolizumab with chemotherapy resulted in 43% of patients having a partial or complete regression of disease, with 86% of patients with bladder cancer and 57% of those with small cell/ neuroendocrine prostate cancer living two years.
“The combination of pembrolizumab and chemotherapy presents a promising new treatment approach for these challengingto-treat, rare cancers and could be a major breakthrough for patient care,” said Dr. Arnold Chin, Professor of Urology at the David Gefen School of Medicine at UCLA and senior author of the study.
Immune-based treatment, such as pembrolizumab, has showed success for treating people with a variety of advanced or metastatic cancers, including patients with advanced small cell lung cancer. Previous laboratory-based research at UCLA, led by Dr. Owen Witte, Chin and colleagues, has demonstrated that small cell cancers in the bladder, lung, and prostate share many biological traits. Building on these fndings, Chin and his team pursued the concept that treatment approaches should target cancers based on molecular similarities. They designed a clinical trial across all small cell/neuroendocrine urologic cancers combining pembrolizumab and chemotherapy as a frst-line therapy for bladder and prostate small cell cancers.
The trial involved 15 patients who were separated into two cohorts. The frst included seven participants with advanced or metastatic small cell bladder cancer, while the other group included eight patients with primary small cell or neuroendocrine prostate cancer. The study was designed for patients who would normally receive chemotherapy as part of their standard care.
The researchers found that patients showed favorable responses using this treatment regimen. In bladder cancer group, only one out of seven patients experienced
disease progression after a median follow-up of almost three years.
For the prostate cancer group, the median survival for patients with small cell/ neuroendocrine prostate cancer in the trial reached 27 months, which is longer than expected compared to the historical average of just 7 to 9 months.
The combination treatment was also well tolerated, with no patients needing to stop therapy due to side efects.
“These results suggest that the combination therapy could provide a substantial survival beneft,” said Chin, who is a member of the UCLA Health Jonsson Comprehensive Cancer Center and the Eli and Edythe Broad Center of Regenerative Medicine and Stem Cell Research.
Along with the encouraging survival rates, the team found that the clonal expansion of CD8+ T cells in the blood, a type of immune cell, in response to treatment correlated with better progression-free survival. This indicated that a blood test could be predictive of treatment response for patients in the future.
The fndings support the need for larger clinical trials to confrm these fndings.
The study’s frst authors are Yiqian Gu, a graduate student in the bioinformatics interdepartmental program at UCLA, and Ann Ly, formerly a staf researcher in the department of urology at UCLA and now a doctoral candidate at UC Davis. UCLA authors include Sara Rodriquez, Hanwei Zhang, Jiyoon Kim, Zhiyuan Mao, Ankush Sachdeva, Nazy Zomorodian, Matteo Pellegrini, Gang Li, Alexandra Drakaki, Matthew Rettig, and Sandy Liu, who is now at City of Hope.
IMMUNE-BASED TREATMENT, SUCH AS PEMBROLIZUMAB, HAS SHOWED SUCCESS FOR TREATING PEOPLE WITH A VARIETY OF ADVANCED OR METASTATIC CANCERS, INCLUDING PATIENTS WITH ADVANCED SMALL CELL LUNG CANCER. PREVIOUS LABORATORY-BASED RESEARCH AT UCLA, LED BY DR. OWEN WITTE, CHIN AND COLLEAGUES, HAS DEMONSTRATED THAT SMALL CELL CANCERS IN THE BLADDER, LUNG, AND PROSTATE SHARE MANY BIOLOGICAL TRAITS.
t the forefront of healthcare innovation, oncology has transformed how we approach disease risk and prevention. With tools like genetic analysis, polygenic risk scores (PRS), and artifcial intelligence (AI), cancer care has shifted from a reactive approach to one that emphasizes precision and prevention. However, these advancements don’t just revolutionize cancer care—they are now being applied to chronic metabolic and age-related conditions, such as heart disease and diabetes1.
With these innovative tools, the potential to unlock healthier, longer lives for everyone is becoming within reach. Let’s explore how translating these cutting-edge insights into actionable steps for patients can inspire a new era of preventive care.
the disease.
• 1 in 4 people with coronary artery disease remain undetected through clinical risk evaluations alone. These gaps underscore the need for advanced tools like NGS and AI-driven models3. By ofering deeper insights into genetic and lifestyle risks, these technologies empower patients to take preventive action long before symptoms appear.
When it comes to understanding disease risk, oncology leads the way. Thanks to nextgeneration sequencing (NGS), healthcare providers can now analyze a person’s DNA and RNA to predict their chances of developing specifc cancers.
This isn’t just theoretical—it’s practical. For instance, testing for BRCA1 and BRCA2 mutations enables women at higher risk of breast or ovarian cancer to take preventive action, ranging from lifestyle changes to preventive surgeries. Moreover, in oncology, NGS is not only used to assess disease risk but also to predict treatment responses based on various genomic profles, guiding personalized treatment plans.
AI has taken this progress even further. By analyzing vast amounts of data, AI provides highly accurate risk predictions and tailors interventions to each patient2. The result?
A more personalized approach to care that spans prevention, diagnosis, and treatment, subsequently improving outcomes and reducing overall disease burden. For example, AI in oncology can assist in early cancer detection by analyzing medical images, like CT scans or MRIs, to identify tumors or abnormalities, enabling earlier and more accurate diagnoses.
These are just a few examples of how oncology is driving the transformation in healthcare through the use of advanced technologies in both preventive and predictive medicine. What’s especially inspiring is how this shift—from reactive treatment to proactive prevention— has also been applied to redefne healthcare practices in other medical felds. Traditional methods often fall short in identifying risks for certain diseases. For example:
• 7 out of 10 women diagnosed with breast cancer have no family history of
Disease risk isn’t just about genetics—it’s multifactorial. Poor eating habits, hormonal changes, and environmental exposures all work alongside genetic predispositions to shape our health.
Advanced technologies now integrate these elements—genetics, epigenetics, and lifestyle factors—into comprehensive risk assessments, overall providing a more personalized picture of an individual’s health trajectory.
This holistic approach is transforming how we understand and manage chronic conditions.
THE PRINCIPLES OF PRECISION CARE IN ONCOLOGY ARE NOW BEING APPLIED TO OTHER HEALTH CONDITIONS, ESPECIALLY THOSE LINKED TO AGING.
7 in 10
7 out of every 10 women diagnosed with breast cancer do not have a family history of the disease.
8 in 10
8 out of 10 people with pre-diabetes are not aware of their condition and the possibilities for prevention.
1 in 4
1 out of every 4 people with coronary artery disease is undetected through the evaluation of clinical risk factors.
Many diseases, such as breast cancer or coronary artery disease, remain undetectable through traditional methods, especially in individuals without a family history or obvious symptoms. Advanced technologies like PRS and AI are critical for uncovering risks that might otherwise go unnoticed.
Disease risk is multifactorial, combining genetics, lifestyle, and environmental factors. Incorporating this comprehensive view provides a more accurate and actionable understanding of health risks.
The principles of precision care in oncology are now being applied to other health conditions, especially those linked to aging. Chronic conditions such as heart disease, diabetes, and others, share common biological pathways with cancer, including infammation and oxidative stress. Leveraging similar tools— like PRS and AI—enables more efective prediction and management of these risks3. Take heart disease, with NGS, healthcare providers can identify individuals predisposed to cardiovascular issues5. Instead of waiting for symptoms, targeted prevention strategies— such as dietary changes, exercise programs, or medication—can be implemented5. For example, familial hypercholesterolemia (FH) is a genetic condition caused by changes in the APOB, LDLR, and PCSK9 genes, which lead to very high cholesterol levels early in life. Without treatment, people with FH have a much higher chance of developing atherosclerotic cardiovascular disease (ASCVD), sometimes as early as in their 40s. However, with early and efective cholesterol-lowering medications, this risk can be greatly reduced. This shows how genetic testing can pinpoint those at risk, allowing for early action to prevent serious health issues later on.6
AI is also making strides in managing conditions like diabetes, which afects millions globally. By combining genetic data with patient medical histories, AI can identify risks early and
recommend tailored interventions that range from dietary to lifestyle.
Aging isn’t just about adding years to life— it also amplifes genetic risks for chronic conditions. One major culprit is “infammaging,” a low-grade chronic infammation that has been linked to diseases such as cancer and heart disease. This is where oncology’s focus on early intervention proves invaluable.
By identifying risks tied to infammation, patients can adopt lifestyle changes that tackle multiple issues simultaneously.
For example, an anti-infammatory diet or a tailored exercise routine can reduce cancer risks while improving heart and metabolic health. By helping patients embrace these holistic approaches, healthcare professionals can ensure individuals age with vitality.
The ultimate goal of these advancements is clear: helping people live longer, healthier lives. By combining the power of genetic insights, PRS, and AI, healthcare providers can design personalized health plans that address multiple risks simultaneously. For aging populations, this shift means focusing on prevention rather than waiting for problems to arise. Advanced health programs informed by these cutting-edge tools
PERSONALIZED HEALTH SOLUTIONS ARE PARTICULARLY CRUCIAL FOR PATIENTS WITH HIDDEN OR MULTIFACTORIAL RISKS. ADVANCED TOOLS SUCH AS PRS AND AI CREATE ACTIONABLE ROADMAPS FOR PREVENTION BY ADDRESSING RISKS THAT OFTEN REMAIN INVISIBLE IN CLINICAL EVALUATIONS. WHETHER IT’S IDENTIFYING, OR CATCHING EARLY SIGNS OF CORONARY ARTERY DISEASE.
Shifting from Treatment to Prevention
can help individuals adopt healthier habits and better manage their unique risks. This is the future of healthcare—tailoring health solutions to the unique needs of each individual.
Personalized health solutions are particularly crucial for patients with hidden or multifactorial risks.
Advanced tools such as PRS and AI create actionable roadmaps for prevention by addressing risks that often remain invisible in clinical evaluations. Whether it’s identifying prediabetes, mitigating infammation, or catching early signs of coronary artery disease,
Advanced genetic tests enable the reclassifcation of patients at intermediate risk by traditional methods. Depending on their genetic profle, these patients may be identifed as having a high risk of coronary artery disease, allowing for earlier and more efective interventions.
By identifying high-risk patients through genetic and metabolic markers, tailored nutritional or pharmacological approaches can prevent the development of type 2 diabetes, improving outcomes and reducing longterm complications.
Specialized genetic tests can detect the polygenic risk of breast cancer in women without hereditary mutations, ofering new insights for those at risk of sporadic cases and enabling earlier preventive measures.
Genetic testing provides critical tools for identifying individuals at high risk of prostate cancer, surpassing the limitations of traditional screening methods and supporting earlier detection and intervention.
these technologies empower patients to make informed choices.
Multifactorial risk assessments that combine genetics, lifestyle, and environmental data represent the next frontier of precision medicine. Some health indicators are undetectable through symptoms or traditional tests. Tools like PRS and AI are helping bridge these gaps1, creating a healthcare system that prioritizes prevention and longevity6
The fusion of oncology and preventive medicine is reshaping healthcare. What began as a mission to better understand and treat cancer has evolved into a powerful blueprint for addressing aging and chronic diseases4
By integrating the latest advances in genetic research and AI, healthcare professionals can empower patients to take charge of their health and embrace the opportunities for healthier, longer lives.
WHAT BEGAN AS A MISSION TO BETTER UNDERSTAND AND TREAT CANCER HAS EVOLVED INTO A POWERFUL BLUEPRINT FOR ADDRESSING AGING AND CHRONIC DISEASES4 .
References:
1. Jin, J., & Kim, J. (2024). Multi-omics and Artifcial Intelligence Technology for Elucidating Disease Pathophysiology. Preprints.org.
2. Henry, E. (2024). Utilizing Electronic Health Records for Predictive Modeling of Cancer Risk. ResearchGate.
3. Yurkovich, J. T., Evans, S. J., & Rappaport, N. (2024). The Transition from Genomics to Phenomics in Personalized Population Health. Nature Reviews Genetics.
4. Patrinos, G. P., & Meybodi, H. A. (2024). Introduction to the Future of Medicine. Springer.
5. Verma, M., & Senapati, S. (2024). Integrating Polygenic Risk Scores (PRS) for Personalized Diabetes Care: Advancing Clinical Practice with Tailored Pharmacological Approaches. Diabetes Therapy.
6. Hood, L., & Price, N. (2023). The Age of Scientifc Wellness: Why the Future of Medicine Is Personalized, Predictive, Data-Rich, and in Your Hands. Books.Google.
7. Grzymski, J.J., Elhanan, G., Morales Rosado, J.A. et al. Population genetic screening efciently identifes carriers of autosomal dominant diseases. Nat Med 26, 1235–1239 (2020). https://doi.org/10.1038/s41591-020-0982-5
®
ltherapy PRIME® represents a remarkable advancement in non-invasive skin tightening, ofering precise and naturallooking results without the need for surgery. By stimulating collagen production through ultrasound technology, it provides a safe and efective solution for lifting and rejuvenating delicate areas of the face and neck.
In an interview with "Hospitals" magazine, dermatologist Dr. Tatiana Kuznechenkova praised Ultherapy PRIME, emphasizing its role in providing patients with cutting-edge, efective solutions for improving skin's look and feel.
MY LOVE FOR DERMATOLOGY
BEGAN DURING MEDICAL SCHOOL, WHERE I WAS FASCINATED BY HOW SKIN HEALTH INTERTWINES WITH CONFIDENCE AND OVERALL WELL-BEING.
Absolutely! My love for dermatology began during medical school, where I was fascinated by how skin health intertwines with confdence and overall well-being. After specializing in aesthetic medicine, I found my calling in non-invasive treatments that deliver natural, transformative results. As a Merz trainer, my days blend patient care with mentorship. I educate HCPs on products, protocols, and best practices and deliver hands-on demonstrations for products, covering safety, efcacy, and patient consultation strategies.
®
Ultherapy PRIME® is the next-generation evolution of ultrasound technology! It uses focused ultrasound energy to gently heat deeper layers of skin, stimulating the body’s natural collagen production. it ofers a precise, efective way to lift and tighten skin without surgery or downtime. This treatment provides natural, long-lasting results by enhancing skin elasticity and reducing fne lines.
®
It’s versatile! We commonly treat the face, neck, and décolletage. But with PRIME’s enhanced precision, we’re also seeing beautiful results for brows and submental area.
®
Three words: non-invasive, real-time visualization, and customizable. Unlike lasers or injectables, Ultherapy PRIME® doesn’t target the surface, it works from the inside out for naturallooking lifting. Plus, there’s no downtime. You can literally schedule a session during lunch and return to your day! It’s ideal for patients who want gradual, lasting results without needles or scalpels.
®
Yes! Thanks to smarter technology, treatment times are up to 30% shorter. A full face and neck session now takes about 45-60 minutes. Patients love the efciency, and the enhanced comfort makes the experience smoother.
®
If you’re noticing mild to moderate sagging, loss of defnition, or crepey texture, Ultherapy PRIME®! Good candidates are generally in their 30s to 60s, seeking preventative care. It’s perfect for busy individuals who want to age gracefully but authentically.
facials or fllers. Pair it with good skincare and sun protection, and you’ll maximize that glow!
Most patients see optimal results with just one treatment. Your body continues producing collagen over 2-3 months, so improvements unfold gradually.
Results typically last 1-2 years, mirroring your skin’s natural aging process. Since collagen keeps working long after treatment, many patients feel their results outlast traditional
Keep it simple! Avoid harsh exfoliants or sunburn for a few days prior. We recommend a clean, makeup-free face on treatment day. During your consultation, we’ll tailor prep steps based on your skin type. but there’s no strict regimen.
During the session, you’ll feel warm tingling as the ultrasound energy targets specifc depths, most patients fnd it comfortable, and we adjust settings for sensitivity. Afterward, you might have slight redness or tenderness, but it fades within hours. Zero downtime! Patients can exercise, socialize, or head back to work immediately.
Absolutely! Gentle cleansers, moisturizers, and SPF are recommended post-treatment. Wait 2448 hours before reintroducing retinoids or acids to let your skin settle. And of course, hydration and sunscreen will help protect your fresh, collagen-boosted glow!
ULTHERAPY PRIME® IS THE NEXT-GENERATION EVOLUTION OF ULTRASOUND TECHNOLOGY! IT USES FOCUSED ULTRASOUND ENERGY TO GENTLY HEAT DEEPER LAYERS OF SKIN, STIMULATING THE BODY’S NATURAL COLLAGEN PRODUCTION. IT OFFERS A PRECISE, EFFECTIVE WAY TO LIFT AND TIGHTEN SKIN WITHOUT SURGERY OR DOWNTIME. THIS TREATMENT PROVIDES NATURAL, LONGLASTING RESULTS BY ENHANCING SKIN ELASTICITY AND REDUCING FINE LINES.

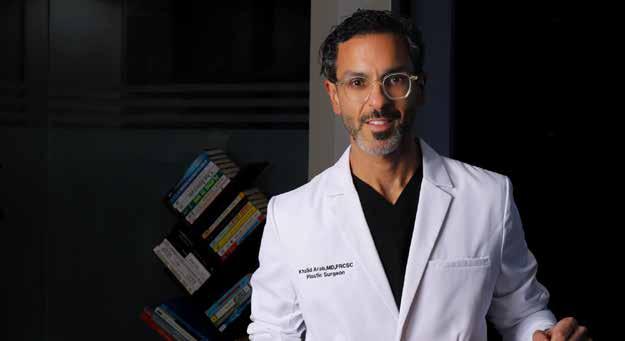
ospitals magazine met Dr. Khaled Arab, Associate Professor, King Saud University- Plastic Surgery Consultant, to discuss Motiva implants and their revolutionary impact on breast augmentation. With advanced technology, these implants have transformed the feld. Dr. Arab has extensive experience, having studied in Saudi Arabia before moving to Canada for further specialization. He has completed fellowships in Sweden and Canada in facial surgery, breast aesthetics, and body contouring. Today, he works as a consultant and professor of plastic surgery at the university and runs a private aesthetic clinic in Riyadh and Dubai.
To understand Motiva’s impact, it’s important to look at the history of breast augmentation. This procedure has been performed since the 1960s, but progress was slow due to regulatory restrictions and challenges in developing implants that were both safe and naturallooking. Until the early 2000s, advancements in this feld were limited, largely due to stringent regulations from authorities like the FDA. However, with Motiva’s introduction, the industry underwent a major shift. Over the past decade, breast implants have evolved at an unprecedented pace, leading to signifcant improvements in both safety and aesthetics. Motiva implants ofer several advantages. They are designed to integrate seamlessly with the body, signifcantly reducing complications. According to studies, the complication
SELECTING THE RIGHT IMPLANT IS NOT A DECISION THAT SHOULD BE TAKEN LIGHTLY. IT REQUIRES CAREFUL COLLABORATION BETWEEN THE SURGEON AND THE CONSUMER.
rate is less than one percent, a signifcant improvement over previous generations of implants. Another key beneft is their natural shape, which aligns with the growing preference among women for a more subtle, realistic look.
Motiva has also pioneered new technologies, making breast augmentation more advanced than ever. Their continuous investment in research and development has allowed them to stay ahead, working closely with specialists across multiple disciplines. Their implants feature cutting-edge gel technology, known as Ergonomix, along with an advanced microchip that enhances safety and tracking.
primary distinction being between Round® and Ergonomix®. The Round® implants are ideal for women who prefer a more prominent and voluminous look, particularly in the upper breast. This option creates a fuller and more defned shape, though it may appear less natural in certain cases.
On the other hand, Ergonomix® implants are designed to replicate the natural shape and movement of real breasts. Their unique structure allows them to adjust dynamically to the body’s motion, providing a teardrop-like shape that enhances natural aesthetics. This option is particularly popular among women who seek a soft, realistic appearance without an overly augmented look.
Selecting the right implant is not a decision that should be taken lightly. It requires careful collaboration between the surgeon and the consumer. Every woman has unique anatomical characteristics, and factors such as breast width, tissue type, and skin thickness must be evaluated to determine the most suitable implant. The woman’s preferences also play a key role. While some women seek a more prominent look, others prefer subtle enhancements that maintain a natural shape. However, expectations must be realistic and aligned with the body’s natural structure.
A surgeon’s expertise is crucial in this process. Experience allows the surgeon to recommend the best options based on the woman’s body type and aesthetic goals. Ultimately, the aim is to achieve a balanced and harmonious result.
Motiva implants have become a preferred choice for those looking for a natural breast appearance, as they are designed to adapt seamlessly to the body’s movement and structure. A detailed physical examination, including precise measurements, is essential in selecting the appropriate size and shape.
Over the years, there has been a noticeable shift in aesthetic preferences, with more women opting for results that look and feel as natural as possible. This has led to a rise in demand for Ergonomix®, as it closely mimics the natural breast contour while still ofering the benefts of enhancement. The main diference between the two lies in the outcome—while Round® implants provide noticeable fullness and projection, Ergonomix® is tailored for those who prioritize natural movement and integration with the body.
Motiva ofers a range of implants to cater to diferent women's preferences, with the
Choosing the right implant requires a comprehensive evaluation that goes beyond just size preferences. The process begins with an open discussion between the woman and the surgeon to understand their goals. Some women seek a more natural, proportionate enhancement, while others prefer a more dramatic transformation. Understanding these desires helps guide the selection process.
A thorough physical assessment follows, where factors like breast width, tissue elasticity, and skin fexibility are carefully examined. These elements help determine the best implant dimensions for a balanced look. Lifestyle is another important consideration. Women who lead an active lifestyle may require a diferent implant placement compared to those with a
MOTIVA IMPLANTS HAVE BECOME A PREFERRED CHOICE FOR THOSE LOOKING FOR A NATURAL BREAST APPEARANCE, AS THEY ARE DESIGNED TO ADAPT SEAMLESSLY TO THE BODY’S MOVEMENT AND STRUCTURE. A DETAILED PHYSICAL EXAMINATION, INCLUDING PRECISE MEASUREMENTS, IS ESSENTIAL IN SELECTING THE APPROPRIATE SIZE AND SHAPE.
more sedentary routine. The choice between placing the implant under or over the muscle depends largely on these factors.
Once all these aspects are evaluated, the appropriate implant type is selected. Whether it’s Round® for a fuller look or Ergonomix® for a more natural result, the decision is tailored to the woman’s anatomy and aesthetic goals. The projection of the implant, which determines how much the breast extends forward, is also an important factor in achieving a proportional and well-balanced result.
and experienced surgeon. Open discussions about expectations, potential results, and surgical options are essential in making an informed choice. It is important to set realistic expectations and choose an implant size that complements one’s natural body proportions. Reviewing before-and-after images of past women can help in understanding potential outcomes. Women considering this surgery should also be mentally prepared for the procedure and the recovery phase. Since the results are long-term, making a well-thought-out decision is crucial. While not a necessity, breast augmentation can have a positive impact on self-esteem when done correctly.
One of the most signifcant advancements Motiva has introduced is its superior safety features. Traditional implants were often associated with complications such as capsular contracture, a condition where scar tissue forms around the implant, causing it to harden and distort. Motiva’s unique design and biocompatible materials have drastically reduced the occurrence of such complications.
Additionally, Motiva implants incorporate antibacterial technology, signifcantly lowering the risk of post-surgical infections, which have historically been a major concern. Their high fexibility and durability further minimize the risk of rupture or leakage. Another standout feature is Q-Code technology, an integrated microchip that allows for easy tracking of implant details, ensuring safety and simplifying future medical follow-ups. By combining innovation with biocompatibility, Motiva has set new standards in breast augmentation, ofering women a safer and more reliable option with fewer long-term risks.
Breast augmentation with Motiva implants is a straightforward procedure with a relatively quick recovery time. The surgery typically lasts about an hour, and most women can return to normal activities within one to four weeks. Post-operative care is essential for ensuring the best outcomes. Women are advised to wear a compression garment for a specifed period to aid healing. Strenuous activities should be avoided initially, and a healthy lifestyle should be maintained. Follow-up appointments with the surgeon are important for monitoring progress. Since the procedure is minimally invasive and often performed as an outpatient surgery, hospitalization is not required. Strict adherence to post-operative instructions ensures optimal healing and long-lasting results.
Breast augmentation is a personal decision and not a medical necessity. However, for many women, it is a procedure that enhances self-confdence and body image. If someone is unsure about undergoing the surgery, the frst step is to consult with a qualifed
Motiva has revolutionized the feld of breast augmentation, and its name refects its mission: Motivation for Technology, Motivation for Inspiration, and Motivation for Involvement. The brand has consistently led advancements in breast implant technology, redefning industry standards and empowering women with safer, more natural-looking options. Ultimately, Motiva is not just about breast augmentation; it represents innovation, excellence, and confdence in modern aesthetic surgery.
ONE OF THE MOST SIGNIFICANT ADVANCEMENTS MOTIVA HAS INTRODUCED IS ITS SUPERIOR SAFETY FEATURES. TRADITIONAL IMPLANTS WERE OFTEN ASSOCIATED WITH COMPLICATIONS SUCH AS CAPSULAR CONTRACTURE, A CONDITION WHERE SCAR TISSUE FORMS AROUND THE IMPLANT, CAUSING IT TO HARDEN AND DISTORT. MOTIVA’S UNIQUE DESIGN AND BIOCOMPATIBLE MATERIALS HAVE DRASTICALLY REDUCED THE OCCURRENCE OF SUCH COMPLICATIONS.
Abu Dhabi is not just keeping pace with the future of healthcare; it is defning it. With a steadfast commitment to innovation, the emirate is leveraging advanced technologies such as genomics, artifcial intelligence (AI), and precision medicine to revolutionize patient care. Through groundbreaking research and strategic initiatives, Abu Dhabi is cementing its position as a global innovation hub for life sciences, setting new standards for prevention, diagnosis, and treatment.
Systems worldwide are under immense
pressure. Abu Dhabi’s forward-thinking approach, fuelled by government support, private sector collaboration, and international partnerships, serves as a model for other nations striving to future-proof their healthcare systems. Its partnership with the World Health Organization (WHO) and other leading global entities ensures that Abu Dhabi remains at the forefront of healthcare advancements.
“Beyond technological innovation, Abu Dhabi is also investing in genomics, clinical trials and medical education, positioning itself as a centre of excellence for biomedical discoveries. The emirate’s commitment to fostering innovation in healthcare start-ups and supporting groundbreaking medical research is cultivating a globally connected ecosystem that attracts top talent and encourages scientifc progress,” says Dr. Asma Ibrahim Al Mannaei, Executive Director of the Health Life Sciences Sector at the Department of Health – Abu Dhabi (DoH).
INNOVATION IS THE BACKBONE OF A RESILIENT HEALTHCARE SYSTEM. BY INTEGRATING GENOMICS, AI, AND DIGITAL TECHNOLOGIES INTO HEALTHCARE, WE ARE NOT ONLY ELEVATING PATIENT CARE BUT ALSO TRANSFORMING THE VERY ESSENCE OF HOW IT IS DELIVERED
Imagine a healthcare system that predicts and prevents disease before symptoms even appear. In Abu Dhabi, this vision is becoming a reality, thanks to the region’s investment in genomics. By decoding the genetic blueprint of individuals, scientists and clinicians can develop highly personalized treatment plans, improving patient outcomes and reducing the burden of chronic diseases. This precision-driven approach is reshaping healthcare, shifting the focus from reactive to proactive care. Dr. Al Mannaei is aware of the signifcance of these advancements: “Innovation is the backbone of a resilient healthcare system. By integrating genomics, AI, and digital technologies into healthcare, we are not only elevating patient care but also transforming the very essence of how it is delivered.”
The Emirati Genome Programme (EGP) – one of the world’s largest programs helping set global standards – is one
DR. ASMA IBRAHIM AL MANNAEI
example of how DoH is trying to understand the genetic makeup of UAE citizens to accelerate the development of integrated services and solutions that address the specifc health needs of the population. Beyond individual patient care, genomics also plays a crucial role in population health. By analyzing genetic data on a broader scale, researchers can identify trends, predict disease outbreaks, and implement preventative public health measures. This proactive approach enables healthcare to prepare for future health challenges, including rare genetic disorders, by developing targeted screening programs and early intervention strategies. This not only benefts individuals but also strengthens Abu Dhabi’s ability to build a healthier society for generations to come.
healthcare and the ‘Voice of the Customer’ platform to streamline health sector processes. These initiatives underscore the nation’s strategic clarity in leveraging technology to enhance healthcare delivery. Furthermore, the integration of AI into telemedicine is expanding access to healthcare, particularly in remote underserved areas, ensuring that every patient can beneft from expert medical consultations regardless of their location.
AI and digital health solutions are central to Abu Dhabi’s transformation of healthcare, beyond genomics. DoH is taking the lead on several innovative projects that improve patient care, optimize medical processes and increase access. Hospitals now employ advanced AI models to predict emergency room demand so they can optimise resources and improve care delivery. From preventive assistance to diagnostics and more, AI is changing the way diseases are detected and treated. Abu Dhabi has established a comprehensive health innovation ecosystem which has facilitated cutting-edge initiatives such as HealthX. The two-year startup program launched by startAD and DoH aims to advance 30 global life science startups into the UAE’s healthcare ecosystem. Additionally, the creation of a digital health ecosystem, including the Malaf digital health exchange platform, allows medical staf to securely access millions of unique patient records.
The healthcare authorities are actively launching strategic initiatives like a smart AI-powered auditing system for health facility engineering plans, an AI-driven project analyzing biometric indicators for preventive
Abu Dhabi Global Healthcare Week (ADGHW) is a platform for open, inclusive exchange and joint action. It is a community without borders that seeks to advance the future of health and well-being. A key highlight of the event is the ADGHW Innovation Awards, which recognize and celebrate the most transformative breakthroughs in global healthcare. By honoring cutting-edge research, emerging technologies, and groundbreaking solutions, the Awards reinforce the Emirate’s commitment to fostering an ecosystem where transformative innovation thrives.
Dr. Al Mannaei emphasized the importance of collaboration in shaping the future of healthcare: “Partnerships between governments, the private sector, and the scientifc community are essential to drive medical breakthroughs. By creating an environment that nurtures research and development, we have a pivotal role in bringing people together to redefne health and wellbeing. Collaboration across borders and across disciplines is crucial in tackling global health challenges, from pandemics to chronic disease management.”
To further enhance the impact of these collaborations, Abu Dhabi is also facilitating investment in biotech hubs and innovation districts, creating a seamless pipeline from research to real-world application. These investments not only accelerate drug discovery and medical device development but accelerate the future of health – making good health and quality care a global priority.
ABU DHABI GLOBAL HEALTHCARE WEEK (ADGHW) IS A PLATFORM FOR OPEN, INCLUSIVE EXCHANGE AND JOINT ACTION. IT IS A COMMUNITY WITHOUT BORDERS THAT SEEKS TO ADVANCE THE FUTURE OF HEALTH AND WELL-BEING. A KEY HIGHLIGHT OF THE EVENT IS THE ADGHW INNOVATION AWARDS, WHICH RECOGNIZE AND CELEBRATE THE MOST TRANSFORMATIVE BREAKTHROUGHS IN GLOBAL HEALTHCARE. BY HONORING CUTTING-EDGE RESEARCH, EMERGING TECHNOLOGIES, AND GROUNDBREAKING SOLUTIONS, THE AWARDS REINFORCE THE EMIRATE’S COMMITMENT TO FOSTERING AN ECOSYSTEM WHERE TRANSFORMATIVE INNOVATION THRIVES.

he landscape of medical travel has evolved signifcantly, with patients increasingly seeking high-quality, patient-centered care beyond their home countries. Patients traveling for care often face greater vulnerabilities than local patients—unfamiliar healthcare systems, cultural and language barriers, continuity-ofcare concerns, and legal uncertainties. Without proper safeguards in place, these risks can lead to miscommunication, compromised patient safety, and reputational damage for healthcare organizations.
This is why accreditation plays a pivotal role in ensuring high standards in medical travel. Accreditation validates a healthcare organization’s ability to provide safe, transparent, and high-quality care while ensuring the patient’s journey is seamless from start to fnish. Global Healthcare Accreditation (GHA) has positioned itself as a leading authority in accrediting healthcare organizations catering to international patients,
ensuring they meet rigorous standards for safety, transparency, and patient experience.
Healthcare organizations looking to attract international patients face a unique set of challenges. Unlike local patients, medical travelers must navigate complex logistical, linguistic, and cultural barriers. Additionally, they require comprehensive pre-travel guidance, seamless in-country coordination, and post-treatment follow-ups. GHA accreditation ensures that hospitals, clinics, and associated service providers optimize these critical aspects, fostering trust and confdence among patients.
Renée-Marie Stephano, CEO of Global Healthcare Accreditation, highlights that today's medical travelers are well informed and selective about their care choices. "Patients are not just looking for afordability; they want assurances of safety, continuity of care, and
GLOBAL HEALTHCARE ACCREDITATION (GHA) HAS POSITIONED ITSELF AS A LEADING AUTHORITY IN ACCREDITING HEALTHCARE ORGANIZATIONS CATERING TO INTERNATIONAL PATIENTS, ENSURING THEY MEET RIGOROUS STANDARDS FOR SAFETY, TRANSPARENCY, AND PATIENT EXPERIENCE.
Renée-Marie Stephano
high-quality outcomes. Accreditation in medical travel is not just about meeting standards— it’s about creating a holistic, patient-frst experience that instills confdence in both patients and stakeholders.”
Accreditation is more than just a certifcate—it is a strategic tool that enhances operational efciency and global marketability. Some key benefts of accreditation include:
• Enhanced Patient Trust & Brand Reputation: Patients and referring institutions prefer accredited facilities, viewing them as reliable and committed to best practices.
• Greater Operational Efciency: Accreditation helps streamline workfows, reduce redundancies, and implement standardized procedures, leading to improved coordination and resource management across departments.
• Alignment with International Health Insurers: Insurance providers are more likely to collaborate with accredited institutions, ensuring patients receive care that meets global benchmarks.
• Optimization of Patient Experience: From pre-arrival consultation to posttreatment follow-up, accreditation ensures a seamless, patient-centered journey.
While the benefts are evident, many healthcare organizations struggle with the accreditation process. Common challenges include:
• Lack of Leadership Buy-In: Without executive-level support, hospitals may struggle to allocate necessary resources for accreditation. Demonstrating the return on investment (ROI) through increased international patient volume can help gain leadership support.
• Absence of a Defned Medical Travel Strategy: Many providers enter the market without a structured business model. GHA assists in developing
comprehensive strategies that align with patient expectations and market demands.
• Gaps in Patient-Centric Services: Cultural competence, multilingual support, and international patient coordination are often overlooked. GHA accreditation ensures that these critical elements are integrated into a hospital’s medical travel program.
• Digital Accessibility and Market Alignment: A hospital’s digital presence plays a crucial role in attracting international patients. A healthcare provider targeting patients from the Middle East, for example, must ensure its website content is available in Arabic, culturally appropriate, and easy to navigate. GHA helps healthcare organizations tailor their digital and marketing strategies to specifc patient demographics, ensuring better engagement and conversions. Overlooking this aspect can result in lost opportunities to connect with international patients seeking care abroad.
Beyond patients, international insurers and corporate healthcare buyers increasingly seek partnerships with accredited providers. Accreditation often signals adherence to key insurer priorities such as:
• Clinical outcomes and readmission rates
• Patient safety, informed consent, and confdentiality
• Continuity of care and medical liability transparency
HEALTHCARE ORGANIZATIONS THAT ACHIEVE GHA ACCREDITATION GAIN EXCLUSIVE ACCESS TO INTERNATIONAL MARKETING INITIATIVES, NETWORKING WITH GLOBAL INSURERS, AND ENHANCED VISIBILITY AMONG PATIENT REFERRAL NETWORKS. LEADING INSTITUTIONS SUCH AS CLEVELAND CLINIC (OHIO-US), BUMRUNGRAD INTERNATIONAL HOSPITAL (THAILAND), AND CEDARS-SINAI (CALIFORNIA-US) HAVE ALREADY ACHIEVED GHA ACCREDITATION, FURTHER SOLIDIFYING CREDIBILITY IN THE INDUSTRY.
With the rising cost of healthcare, multinational employers also prioritize accredited institutions for their globally mobile
workforce. Accreditation assures them that their employees receive standardized, highquality care regardless of location.
Unlike general accreditation bodies that primarily focus on clinical quality, GHA’s accreditation process covers the entire medical travel care continuum. From pre-arrival patient education to transportation, hospitality, and post-treatment follow-ups, GHA ensures every aspect of a patient’s journey is optimized for excellence. Additionally, healthcare organizations that achieve GHA accreditation gain exclusive access to international marketing initiatives, networking with global insurers, and enhanced visibility among patient referral networks. Leading institutions such as Cleveland Clinic (Ohio-US), Bumrungrad International Hospital (Thailand), and Cedars-Sinai (California-US) have already achieved GHA accreditation, further solidifying credibility in the industry.
As medical travel continues to expand, healthcare organizations must stay ahead by prioritizing accreditation. Future trends suggest an increased demand for digital health solutions, including telemedicine and virtual consultations, which will further integrate into the accreditation process.
For hospitals and clinics looking to establish themselves as leaders in medical travel, pursuing GHA accreditation is not just a competitive advantage—it’s a necessity. By fostering transparency, patient trust, and operational excellence, GHA-accredited organizations are setting the gold standard for international patient care.
FOR HOSPITALS AND CLINICS LOOKING TO ESTABLISH THEMSELVES AS LEADERS IN MEDICAL TRAVEL, PURSUING GHA ACCREDITATION IS NOT JUST A COMPETITIVE ADVANTAGE, IT’S A NECESSITY.
Sustainable healthcare has become an urgent necessity in the modern era. The role of hospitals is no longer limited to providing treatment to patients but has expanded to include the responsibility of preserving the environment and reducing its negative impact. This highlights the importance of transforming hospitals into green hospitals, an initiative aimed at integrating sustainability principles across all aspects of hospital operations.
Sustainable healthcare is a concept that seeks to deliver healthcare services while minimizing environmental impact, promoting public health, and optimizing resource utilization. This includes practices such as reducing energy and water consumption, efective waste management, using environmentally friendly materials, lowering carbon emissions, and promoting public health. These practices contribute to environmental preservation and improve the health of the community. Sustainable healthcare also plays a crucial role in transforming hospitals into green hospitals by providing a comprehensive framework for implementing sustainability practices throughout their operations. It involves prioritizing areas of sustainability such as reducing energy and water consumption, managing waste, providing tools and resources for implementation, and helping hospitals measure their performance to identify areas for improvement. These eforts reduce the environmental impact of hospitals and improve public health.
Examples of sustainable healthcare practices include the design of green buildings based on green design principles such as using renewable energy, sustainable materials, and natural lighting. It also involves implementing efective recycling programs for medical waste and other recyclable materials, encouraging staf and patients to use sustainable
transportation options such as bicycles and public transport, and ofering healthy food options for patients and staf while promoting local and organic farming.
These practices help reduce environmental impact and improve public health.
• Reducing Environmental Impact: Transforming hospitals into green hospitals helps minimize the negative environmental impact of the healthcare sector.
• Cost Savings: Implementing sustainability practices can lead to signifcant cost savings, such as reductions in energy and water costs.
• Improving Public Health: Green hospitals contribute to better public health by providing a healthy and safe environment for patients and staf.
• Enhancing Hospital Reputation: Adopting sustainability practices can enhance a hospital’s reputation and attract patients and staf who are environmentally conscious.
Sustainable healthcare is essential for several reasons. It helps mitigate the efects of climate change on human health, as climate change threatens human health by increasing heat-related illnesses, respiratory problems, and the spread of infectious diseases. Sustainable healthcare ensures the responsible use of limited resources such as water, energy, and raw materials.
SUSTAINABLE HEALTHCARE IS A CONCEPT THAT SEEKS TO DELIVER HEALTHCARE SERVICES WHILE MINIMIZING ENVIRONMENTAL IMPACT, PROMOTING PUBLIC HEALTH, AND OPTIMIZING RESOURCE UTILIZATION. THIS INCLUDES PRACTICES SUCH AS REDUCING ENERGY AND WATER CONSUMPTION, EFFECTIVE WASTE MANAGEMENT, USING ENVIRONMENTALLY FRIENDLY MATERIALS, LOWERING CARBON EMISSIONS, AND PROMOTING PUBLIC HEALTH.
Furthermore, sustainable waste management practices protect the environment and public health from the large volumes of waste generated by healthcare, including hazardous materials. Finally, sustainable healthcare can lead to long-term cost savings by reducing waste, improving efciency, and preventing expensive diseases.
Several key elements are involved in achieving sustainable healthcare. This includes investing in prevention to reduce the burden on health systems and improve overall health outcomes. It also includes promoting telemedicine to reduce the need for travel and decrease carbon emissions, while improving access to care, especially in remote areas.
Additionally, healthcare facilities must transition to using renewable energy sources such as solar and wind power to reduce their carbon footprint. It is also crucial to apply green building practices when constructing and renovating healthcare facilities, using sustainable materials and energy-efcient designs. The importance of reducing waste and recycling cannot be overlooked, and efective waste management programs should be implemented. Finally, sustainable procurement practices must be adopted by purchasing supplies and medical equipment from companies that prioritize sustainability.
environmentally friendly, biodegradable, or recyclable, and reducing the use of harmful substances.
• Reducing Carbon Emissions: Adopting practices that reduce carbon emissions, such as using sustainable transport options, decreasing reliance on fossil fuels, and encouraging the use of renewable energy.
• Promoting Public Health: Creating a healthy and safe environment for patients and staf and contributing to the improvement of community health through awareness and health education programs.
• Sustainable healthcare is a vital part of the future of healthcare. By adopting sustainability practices, healthcare institutions and hospitals can reduce their environmental impact, improve community health, save costs, and enhance their reputation. All healthcare professionals must work together to integrate sustainability principles into every aspect of their operations.
THE IMPORTANCE OF REDUCING WASTE AND RECYCLING CANNOT BE OVERLOOKED, AND EFFECTIVE WASTE MANAGEMENT PROGRAMS SHOULD BE IMPLEMENTED. FINALLY, SUSTAINABLE PROCUREMENT PRACTICES MUST BE ADOPTED BY PURCHASING SUPPLIES AND MEDICAL EQUIPMENT FROM COMPANIES THAT PRIORITIZE SUSTAINABILITY.
• Reducing Energy and Water Consumption: Using technologies and practices that help conserve energy and water, such as energyefcient lighting, rainwater harvesting systems, and high-efciency appliances.
• Efective Waste Management: Implementing efective strategies for managing medical waste and disposing of it safely, including sorting, recycling, and responsibly handling hazardous waste.
• Using Environmentally Friendly Materials: Selecting construction materials, medical supplies, and equipment that are
As the UAE’s frst private inpatient and outpatient facility for mental health and addiction treatment, Ardens Medical Center is redefning the path to recovery— combining compassionate care, global expertise and innovative therapies, all within a modern, confdential setting designed to empower healing. Every detail of this pioneering facility is crafted to foster comfort and privacy, ensuring patients feel safe as they work toward recovery.
Ardens Medical Center is the frst private inpatient and outpatient facility in the UAE dedicated to treating mental illness and addiction, a ground-breaking step that flls a crucial gap in the region’s healthcare scene by ofering a local haven where patients can receive comprehensive care under one roof.
Ardens stands as a transformative addition to the UAE’s healthcare landscape, addressing a long-standing need for specialized,
integrated care. By providing inpatient, partial hospitalization, and outpatient services under one roof, the center eliminates the need for patients to seek fragmented treatment elsewhere. Licensed by Dubai’s health authorities, Ardens operates on a foundational belief: healing thrives in environments where individuals feel supported, respected, and free from judgment. Through personalized treatment pathways, partnerships with leading global institutions, and a commitment to confdentiality, Ardens Medical Center is not just a facility—it’s a beacon of hope for those reclaiming their lives.
ARDENS STANDS AS A TRANSFORMATIVE ADDITION TO THE UAE’S HEALTHCARE LANDSCAPE, ADDRESSING A LONG-STANDING NEED FTALIZATION, AND OUTPATIENT SERVICES UNDER ONE ROOF, THE CENTER ELIMINATES THE NEED FOR PATIENTS TO SEEK FRAGMENTED TREATMENT ELSEWHERE.
Ardens’ serene, state-of-the-art facility prioritizes calm and confdentiality. Natural
light foods soundproof therapy rooms and inviting lounges, while safety and comfort rival luxury wellness resorts. With only 17 inpatient beds, the intimate setting ensures personalized attention: all rooms are private (genderseparated), VIP suites ofer premium amenities, and a medical isolation suite addresses specialized needs.
Every treatment is research-backed and refned through partnerships with global clinical partners. Outcomes are tracked rigorously, and protocols evolve with the latest science. Yet Ardens never sacrifces humanity for innovation. Discretion is paramount, externally, the center resembles an upscale wellness retreat, shielding patients and their families from stigma. Internally, encrypted records and strict privacy training ensure patients’ stories stay confdential. In a region where reputation is vital, this sanctuary lets individuals heal without fear. Ardens’ multilingual team of psychiatrists, therapists, and nurses collaborates daily, blending clinical expertise with empathy. Led by veterans with decades of international experience, they
adapt care plans in real time and ofer a unique standard of coordinated care.
Ardens’ defning strength lies in its fullspectrum addiction recovery program, guiding patients through every stage, starting with medically supervised detox in a dedicated unit. Drug and alcohol withdrawal is managed with precision and compassion, ensuring safe, comfortable stabilization.
• Gender-specifc inpatient units with private rooms prioritize dignity, privacy, and cultural sensitivity during vulnerable recovery stages.
• Post-detox, patients enter personalized rehabilitation blending evidence-based therapies:
- Psychotherapy: to uncover root causes.
- Group sessions: fostering peer support.
- Family counselling: repairing relational impacts.
- Mind-body integration: via ftness, mindfulness, and nutrition.
The program emphasizes practical skills from relapse prevention to healthy routines that anchor sobriety long after discharge. By addressing addiction’s physical, emotional, and social dimensions, Ardens creates a resilient foundation for lifelong recovery:
• Medically-Supervised Detox: Roundthe-clock medical care to manage withdrawal symptoms safely.
• Personalized Therapy: One-on-one counselling and psychiatric support to uncover and treat underlying issues.
• Group & Family Therapy: Healing not just individuals but relationships, through group support meetings and family involvement when appropriate.
• Life Skills & Wellness: Workshops on stress management, vocational guidance, ftness, and nutrition to reinforce healthy living.
• Aftercare Planning & Home Health Services: Ongoing recovery coaching, relapse prevention, and at-home wellness consultations for those
needing additional support. This comprehensive approach means that Ardens doesn’t just help patients quit a substance, it empowers them with the tools and support to rebuild their lives. It’s a refuge where someone can arrive in crisis and graduate with confdence, equipped with coping strategies, a healthier body and mind, and a renewed sense of purpose.
Addiction rarely occurs alone, a truth central to Ardens’ design. Many patients face overlapping struggles like depression, anxiety, PTSD, or OCD alongside substance use. Ardens tackles these interconnected challenges through an integrated mental health program, addressing conditions ranging from everyday stress to complex disorders. Every patient is seen as a whole person from day one. A patient with addiction and depression receives simultaneous treatment for both, while someone with severe anxiety (without addiction) accesses tailored
ARDENS’ DEFINING STRENGTH LIES IN ITS FULL-SPECTRUM ADDICTION RECOVERY PROGRAM, GUIDING PATIENTS THROUGH EVERY STAGE, STARTING WITH MEDICALLY SUPERVISED DETOX IN A DEDICATED UNIT. DRUG AND ALCOHOL WITHDRAWAL IS MANAGED WITH PRECISION AND COMPASSION, ENSURING SAFE, COMFORTABLE STABILIZATION.
inpatient or outpatient mental wellness care.
Therapy is customized to each journey, and the integrated approach ensures progress in one area fuels healing in others, addressing psychological roots and emotional fallout together for lasting recovery.
Crucially, Ardens’ team dismantles mental health stigma daily. Patients often arrive burdened by shame, which the staf reframes through education and empathy. They emphasize that mental health struggles are medical conditions, not failures, and seeking help is an act of courage. This nurturing environment fosters meaningful progress, where patients feel safe to heal.
nurses, therapists, dietitians, and more. Patients don’t just address emotions, they improve sleep, nutrition, and coping skills in tandem. If stress or chronic pain fuels depression or relapse risk, activity therapists and nursing staf ofer tailored exercises and relaxation techniques. Ardens integrates art, mindfulness, and spiritual support into recovery, and while focusing on the person, not just symptoms, Ardens crafts deeply personalized care. This intentional approach rejuvenates mind, body, and spirit, building lasting resilience.
Every aspect of Ardens’ program is carefully designed to nurture mind-body wellness. Beyond psychiatrists and psychologists, its multidisciplinary team includes physicians,
Ardens’ treatment philosophy is rooted in global excellence, strengthened by strategic partnerships with pioneers like Connecticut’s Silver Hill Hospital (afliated with Yale University) and Pennsylvania’s Caron Treatment Centers. These alliances deliver real-world benefts: patients gain access to proven, gold-


standard therapies, while Ardens’ clinicians stay ahead through joint training, research, and protocol-sharing. Silver Hill’s century of expertise in complex mental health and addiction cases informs Ardens’ approach, while Caron’s 70+ years of rehab excellence enriches its family support programs and relapse prevention strategies. Critically, these global models are adapted to align with the UAE’s cultural values ensuring care respects local traditions without compromising innovation. For patients, this means world-class treatment rooted in global best practices, ofered in Dubai. For families and regulators, it’s reassurance that Ardens meets rigorous international benchmarks. Ultimately, Ardens ofers the best of both worlds: the warmth and knowledge of local understanding paired with the precision of top-tier global care. Patients heal in an environment where expertise knows no borders, yet feels deeply personal.
Ardens pioneers mental healthcare with advanced therapies like repetitive Transcranial Magnetic Stimulation (rTMS), a non-invasive treatment using magnetic pulses to target brain regions linked to mood.
Efective for treatment-resistant depression, OCD, and anxiety, rTMS ofers hope when medications fail. Specialists administer it over multiple sessions with minimal side efects (light scalp tapping), often yielding renewed clarity and emotional balance. As a leading UAE provider, Ardens brings global treatments home. Partnering with Neurocare Group, Ardens adapts cutting-edge neuromodulation tools (biofeedback, neurofeedback, tDCS) for complex cases.
These augments never replace core therapies: rTMS patients, for example, pair sessions with psychotherapy to turn neurological shifts into practical coping skills.
SILVER HILL’S CENTURY OF EXPERTISE IN COMPLEX MENTAL HEALTH AND ADDICTION CASES INFORMS ARDENS’ APPROACH, WHILE CARON’S 70+ YEARS OF REHAB EXCELLENCE ENRICHES ITS FAMILY SUPPORT PROGRAMS AND RELAPSE PREVENTION STRATEGIES.
• rTMS: Brain stimulation for depression/OCD.
• Biofeedback/Neurofeedback: Self-regulation mastery.
• tDCS: Emerging electrical mood therapy.
For those out of options, Ardens’ blend of tech and human care breaks cycles of despair, turning breakthroughs into lasting resilience.
Prioritizing results over rhetoric, and dismantling taboos, communities will see mental health struggles and addiction not as moral failings, but as treatable conditions. This shift ripples outward: workplaces will embrace open dialogues about well-being, while leaders advocate for policies that mirror Ardens’ compassionate, evidence-based model.
In a region where mental health and addiction treatment is overshadowed by stigma, Ardens Medical Center is swiftly becoming a transformative force. Blending medical detox, psychological therapy, wellness practices, and family support with evidence-based treatments, Ardens is redefning private mental healthcare, not just as a service, but as a sanctuary.
For healthcare professionals and policymakers, Ardens is a critical ally in tackling long-ignored public health challenges.
Ardens’ true power lies in its duality. It is both a state-of-the-art medical facility and a haven of humanity where privacy coexists with community, science harmonizes with empathy, and innovation serves the soul of healing. For those battling addiction or mental illness, and for families clinging to hope, Ardens’ name (rooted in “ardent”) refects its ethos: ferce dedication to recovery, and by merging global best practices with cultural nuance, Ardens isn’t just treating individuals, it’s reshaping the narrative around mental health in the region. One patient, one breakthrough, one reclaimed life at a time, the center illuminates a path forward: where world-class safe and confdential care and unwavering compassion are inseparable.



n the knee and hip joints in particular, wear and tear of the cartilage surfaces over time causes pain, stifness, and limited movement in these joints. In advanced cases of this disease, called osteoarthritis, the cartilage loss can reach serious proportions. Rheumatoid arthritis, an autoimmune disease, can also afect the joint membranes and cause infammation in the joints. This infammation can also cause damage to the joints, resulting in cartilage loss. In addition to severe cartilage loss in joints such as osteoarthritis and rheumatoid arthritis, serious injuries, fractures, or torn ligaments can also cause permanent damage and cartilage loss in the knee and hip joints. These conditions are usually treated with joint replacement surgery.
Arthroplasty is usually performed by implanting a prosthetic device. This involves removing the damaged joint surfaces and replacing them with an artifcial joint implant. Prosthetic implants can be made of materials such as metal, ceramic, and plastic and create a smooth surface in the joint that mimics normal joint movement.
Acibadem Health Group's International Joint Center located at Acibadem Maslak Hospital is a specialized unit for joint surgery. The center includes a modern facility with specialized surgeons, experienced medical staf, and state-of-the-art medical equipment. It performs
ACIBADEM HEALTHCARE GROUP IS KNOWN WORLDWIDE FOR ITS EXPERTISE AND EXPERIENCE IN ARTHROSCOPY.
Professor Javad Parvizi
arthroplasty surgeries on various joint areas such as the knee, hip, shoulder, elbow, hand, and wrist. Acıbadem International Joint Center uses a multidisciplinary approach to create personalized treatment plans for patients and select the most appropriate surgical methods. It also ofers a comprehensive rehabilitation program to manage the post-operative rehabilitation process and ensure the patient's healthy recovery. Known for its high success rates and patient satisfaction, Acibadem International Joint Center strives to restore freedom of movement to patients sufering from joint problems.
Acıbadem Medical Group takes a multidisciplinary approach to joint replacement surgery. This approach includes rehabilitation specialists, physiotherapists, and other healthcare professionals in addition to the surgical team. This team aims to achieve the best results by working together at every stage of the patient's treatment process.
Acıbadem Healthcare Group ofers a combination of expertise, experience, technology, and services required for arthroplasty surgery. Therefore, it ofers the best treatment option for patients with joint problems.
Arthroplasty is a technically demanding procedure, complex inpatient evaluation, important complication management, and requires constant monitoring of new technological developments. Acıbadem Health Group has a team that specializes in this feld. Surgeons who are experienced, trained, and specialized in arthroplasty surgery work to provide the most appropriate treatment for the patient's needs.
Acıbadem Healthcare Group is known worldwide for its expertise and experience in arthroscopy. High success rates have been achieved in arthroplasty surgeries. This success is based on the quality of the surgical equipment, the expertise of the surgeons, and the use of the latest techniques.
Acıbadem Medical Group ofers a state-of-theart infrastructure for joint replacement surgery. Advanced surgical equipment, robotic surgical techniques, and imaging systems allow surgeons to work more precisely and efectively. These technologies support less invasive and faster recovery for patients.
ACIBADEM HEALTH GROUP'S INTERNATIONAL JOINT CENTER LOCATED AT ACIBADEM MASLAK HOSPITAL IS A SPECIALIZED UNIT FOR JOINT SURGERY. THE CENTER INCLUDES A MODERN FACILITY WITH SPECIALIZED SURGEONS, EXPERIENCED MEDICAL STAFF, AND STATE-OF-THE-ART MEDICAL EQUIPMENT.
Joint replacement surgery requires an individualized treatment plan based on each patient's unique needs and health status.
Personalized treatment is important to achieve the most efective results, tailored to the severity of the patient's joint problems, lifestyle, health history, and personal preferences. This approach optimizes the patient's recovery process, reduces the risk of complications, and increases long-term success.
Comprehensive post-arthroplasty rehabilitation increases a patient's range of motion, strengthens muscles, reduces pain, increases independence, and helps prevent complications. This process allows patients to recover faster and more efectively, facilitates their return to daily activities, and improves their quality of life. The rehabilitation process after arthroplasty is important for the success of the treatment. Acıbadem Health Group supports the patient's recovery process by providing comprehensive physiotherapy and rehabilitation services.
Arthroplasty is performed to reduce joint pain, restore joint mobility, and improve a patient's functional status. Arthroplasty is most commonly performed on the knee and hip, but can also be performed on the shoulder, elbow, wrist, and other joint areas. Arthroplasty surgery begins with an evaluation of the patient, followed by a surgical approach under appropriate anesthesia. The surgeon removes the damaged tissue and places an artifcial prosthetic implant in the joint area. After surgery, the surgical site is closed and the patient's recovery process begins. This process helps the patient regain joint function, reduce pain, and return to normal activities of daily living.
such as osteoarthritis, rheumatoid arthritis, traumatic joint injury, or other joint disease. Arthroplasty may be an option for patients who are experiencing joint pain, limited mobility, and a signifcant decrease in quality of life.
The recovery process varies depending on the patient's overall health, the complexity of the surgery, and the prosthesis used. In general, however, patients experience a rapid recovery process with postoperative physical therapy and rehabilitation programs.
Arthroplasty is generally a safe procedure, but as with any surgical procedure, there are risks. The most common risks include infection, bleeding, prosthesis loosening, and nerve damage. However, these risks can be minimized by the careful work of the surgical team and by taking appropriate precautions.
ARTHROPLASTY IS PERFORMED TO REDUCE JOINT PAIN, RESTORE JOINT MOBILITY, AND IMPROVE A PATIENT'S FUNCTIONAL STATUS. ARTHROPLASTY IS MOST COMMONLY PERFORMED ON THE KNEE AND HIP, BUT CAN ALSO BE PERFORMED ON THE SHOULDER, ELBOW, WRIST, AND OTHER JOINT AREAS. ARTHROPLASTY SURGERY BEGINS WITH AN EVALUATION OF THE PATIENT, FOLLOWED BY A SURGICAL APPROACH UNDER APPROPRIATE ANESTHESIA.
When is joint replacement surgery necessary?
Arthroplasty may be necessary for conditions
Good candidates for joint replacement surgery are patients who experience joint pain, limited range of motion, and a signifcant decrease in quality of life. However, the appropriate treatment plan for each patient is determined by a team evaluation.
The length of time you should avoid activities after surgery varies depending on the complexity of the surgery and the speed of the patient's recovery. In general, it is important to exercise according to the rehabilitation program recommended by your surgeon and to avoid heavy lifting.
elisa, a 24-year-old university student born in Germany, lives there with her family. She was diagnosed with Caroli disease, a rare genetic condition that causes the bile ducts in the liver to widen. This led to liver failure, making a transplant essential for her survival. Melisa registered on the transplant waiting list, but being on the list did not guarantee an immediate transplant. She had to wait for her turn. While waiting on the deceased donor list for a liver transplant in Germany, she regained her health in Türkiye through her cousin’s liver donation.
Liver transplantation is a surgical procedure that replaces a diseased or damaged liver with a healthy one from a donor. There are
two types of liver transplants based on the donor source: living donor and deceased donor transplantation. The liver is uniquely suited for living donor transplants because it is the only organ in the human body that can regenerate. When a donor gives more than half of their liver for transplantation, the remaining portion can continue functioning without serious complications. In fact, the liver can still perform its functions even when up to 70% of it is removed.
LIVER TRANSPLANTATION IS A SURGICAL PROCEDURE THAT REPLACES A DISEASED OR DAMAGED LIVER WITH A HEALTHY ONE FROM A DONOR.
When the liver can no longer function properly, it is called liver failure. If it is not treated, it will progress to death. A liver transplant is the only solution, as survival is
not possible without a functioning liver. Liver failure can have various causes, and Melisa’s case was one of the rarer ones.
In Caroli Syndrome, parts of the bile ducts inside the liver become abnormally enlarged, forming cyst-like or sac-like structures. These may contain stones or sludge, leading to serious infections that can progress to blood poisoning and pose a life-threatening risk. Melisa experienced these complications multiple times and spent the past year in hospitals across Germany, undergoing repeated treatments for her bile ducts. She faced life-threatening situations, making a liver transplant urgently necessary. However, the waiting period in Germany extended longer than expected, and she was informed that it could extend even further. Meanwhile, she received great news from Türkiye. Her cousin Oğuzhan had decided to volunteer as a donor for her. The two cousins, living in diferent countries, reunited at Acıbadem İzmir Hospital. Professor Surgeon Murat Kılıç, Associate Professor Cahit Yılmaz, and their team performed the surgery, removing a portion of Oğuzhan's liver and transplanting it into Melisa.
transplantation is a deeply emotional journey. A healthy donor willingly undergoes surgery to give part of their organ, ofering someone else a chance to survive. The recipient, in turn, holds on to life through this act of generosity. Melisa expressed her gratitude, saying, “I now have a second brother. He made sacrifces for me, and I can’t thank him enough. I was deeply moved by his willingness. He was my cousin before, but now he is my brother. I used to play licensed football for a club in Germany, and I was in my fnal year at university. Unfortunately, I had to miss my exams because of my disease, but I will continue my studies.”
Oğuzhan shared his thoughts, saying, “I did what anyone should do. At frst, I was scared and worried about getting hurt. But we shouldn’t let fear hold us back. Saving a life is a privilege not everyone gets.”
THE SURGERY WAS SUCCESSFUL, AND EVERYTHING WENT SMOOTHLY AFTERWARD. TEN DAYS LATER, THEY WERE DISCHARGED FROM THE HOSPITAL. ORGAN TRANSPLANTATION IS A DEEPLY EMOTIONAL JOURNEY. A HEALTHY DONOR WILLINGLY UNDERGOES SURGERY TO GIVE PART OF THEIR ORGAN, OFFERING SOMEONE ELSE A CHANCE TO SURVIVE. THE RECIPIENT, IN TURN, HOLDS ON TO LIFE THROUGH THIS ACT OF GENEROSITY.
The surgery was successful, and everything went smoothly afterward. Ten days later, they were discharged from the hospital. Organ
Each year, more than 1,400 liver transplants are performed in Türkiye, with 80% involving living donors. This places Türkiye second in the world for the highest number of living donor liver transplants. Acıbadem Healthcare Group is a leading destination for liver transplantation in Türkiye. Patients from around the world choose Acıbadem for its multidisciplinary approach, extensive experience, innovative surgical techniques, high success rates, and patientcentered care.
To date, Acıbadem has successfully performed over 2,000 liver transplants for patients from around the world, including children, complex cases, and combined kidneyliver transplants. These procedures are carried out at its three liver transplant centers in Istanbul, Izmir, and Bursa.
If you’d like to learn more, visit www. acibademinternational.com and share your medical fle with us through the contact form. Our expert team will get in touch with you within a few hours.
atty Liver Disease (FLD) is an emerging health challenge in Qatar and the Middle East, characterized by excessive fat accumulation in liver cells, which negatively afects liver function. Its increasing prevalence is linked to modern lifestyles and unhealthy dietary habits, making it a signifcant public health concern.
Fatty Liver Disease, medically known as hepatic steatosis, is classifed into two main types:
• The most common type, associated with obesity, diabetes, and high cholesterol.
• Afects individuals who consume little to no alcohol.
Caused by excessive alcohol consumption, which can lead to severe liver damage.
In Qatar, NAFLD is the predominant concern, driven by increasing obesity and diabetes rates, largely infuenced by local dietary and lifestyle habits.
• Genetic Factors: Research indicates a genetic predisposition among Middle Eastern populations.
Several key factors contribute to its high prevalence:
• Unhealthy Diet: High consumption of processed foods, sugary beverages, and saturated fats leads to fat buildup in the liver.
• Sedentary Lifestyle: Lack of physical activity and long working hours increase the risk.
• Chronic Conditions: High rates of obesity and diabetes, both major risk factors for NAFLD.
Fatty Liver Disease is often called the "silent disease" because it has no symptoms in its early stages. As the condition progresses, patients may experience:
• Persistent fatigue.
• Discomfort or pain in the upper right abdomen.
PREVENTION IS KEY TO MANAGING FATTY LIVER DISEASE, WITH STRATEGIES FOCUSED ON LIFESTYLE MODIFICATIONS AND MEDICAL INTERVENTIONS.
• Unexplained weight loss.
• Abdominal or limb swelling (in advanced stages).
If left untreated, fatty liver disease can progress to:
• Non-Alcoholic Steatohepatitis (NASH) – liver infammation that can cause damage.
• Liver fbrosis or cirrhosis – scarring that afects liver function.
• Liver failure in severe cases.
At Al-Ahli Hospital, we utilize state-of-the-art techniques for accurate diagnosis, including:
• Blood Tests: Detect elevated liver enzymes (ALT, AST) indicating liver stress.
• Imaging Techniques: Ultrasound, CT scans, and MRI to assess liver fat accumulation.
• FibroScan (Elastography): A non-invasive test to measure liver stifness and detect fbrosis.
• Liver Biopsy: Performed in select cases to confrm diagnosis and disease severity.
Control diabetes, high blood pressure, and cholesterol with medical guidance.
Prevention is key to managing fatty liver disease, with strategies focused on lifestyle modifcations and medical interventions:
• Increase fruits, vegetables, lean proteins, and whole grains.
• Reduce sugar, trans fats, and processed foods.
• Include healthy fats (olive oil, nuts, fsh) to support liver function.
Engage in at least 30 minutes of exercise daily (walking, cycling, swimming).
. Losing 5-10% of body weight signifcantly improves liver health.
• Medications to regulate blood sugar, cholesterol, and reduce infammation.
• Vitamin E and experimental drugs for selected patients.
Specialized diet plans from expert nutritionists to support liver health and weight control.
Surgical interventions (e.g., bariatric surgery) for severely obese patients.
Ongoing follow-ups and liver function tests to track disease progression.
Al-Ahli Hospital is committed to reducing the burden of Fatty Liver Disease through:
• Public Workshops & Lectures: Educational sessions on the importance of diet and exercise for liver health.
• Social Media Campaigns: Raising awareness on preventive measures and treatment options.
• Expert Consultations: Providing personalized advice for at-risk individuals.
Early detection and lifestyle changes can reverse Fatty Liver Disease before it leads to complications.
Schedule your consultation today at Al-Ahli Hospital and start your journey toward a healthier liver!
EARLY DETECTION AND LIFESTYLE CHANGES CAN REVERSE FATTY LIVER DISEASE BEFORE IT LEADS TO COMPLICATIONS. SCHEDULE YOUR CONSULTATION TODAY AT AL-AHLI HOSPITAL AND START YOUR JOURNEY TOWARD A HEALTHIER LIVER
uring and after the COVID-19 pandemic, we’ve seen how the role of the World Health Organization (WHO) in global health is indispensable. Yet, the organization faces a recurring challenge—fnancial instability. The past few years have exposed its vulnerabilities, particularly with its reliance on voluntary contributions from member states. This weakness became glaringly evident when former U.S. President Donald Trump withdrew the United States from the WHO during his frst term, stripping away a signifcant portion of its funding. The subsequent reentry under President Joe Biden, accompanied by nearly half a billion dollars in funding, ofered temporary relief, but with another withdrawal by Trump looming as a possibility, the issue remains unresolved.
This unpredictability raises a fundamental question: Can the WHO continue to operate efectively under its current fnancial model?
Unlike private enterprises or even some nongovernmental organizations (NGOs), WHO does not have a strong, independent revenue stream to ensure long-term stability.
A clear example of the pitfalls of this system can be seen in the Global Polio Eradication Initiative. This WHO-partnered program made remarkable progress in reducing polio cases worldwide. However, funding gaps in certain years slowed down its momentum, paving way for outbreaks to persist in countries like Pakistan and Afghanistan.
To create a more sustainable fnancial ecosystem, the WHO ought to embrace a corporate-like strategy that focuses on diversifed funding.
Unlike traditional donor countries that contribute sporadically, the UAE has taken a strategic approach by investing in longterm healthcare projects that align with both national and global health priorities.
In 2017, the UAE pledged $100 million to eliminate river blindness and lymphatic flariasis in Africa. Rather than a one-time donation, the UAE ensured that these funds were disbursed over multiple years.
The results have been transformative, as seen by the reduced disease prevalence and strengthening of the healthcare systems in the afected regions.
Similarly, the Sheikh Fatima Fund in the UAE has taken a sustainable approach in Mauritania by training midwives instead of merely donating mobile health units. So what’s happening here is that skills are being transferred to local professionals, which empowers them to independently manage maternal healthcare programs in the long run.
Going by these examples, it wouldn’t be
wrong to believe that fnancial sustainability is achievable when funding is structured around long-term impact rather than short-term relief. If the WHO were to take advantage of such approaches, it could signifcantly enhance its ability to respond to global health challenges.
To ensure the WHO’s long-term viability, several strategic shifts must be considered:
One of the biggest weaknesses of WHO’s current fnancial system is its overreliance on government contributions. A more diversifed funding model could create a broader fnancial base. An example of this approach is Gavi, the Vaccine Alliance.
Unlike WHO, Gavi has successfully secured long-term partnerships with corporations like the Bill & Melinda Gates Foundation and pharmaceutical companies which ensures a steady stream of funding for vaccine distribution worldwide.
This type of fnancial structure allows Gavi to maintain operations even when government funding fuctuates.
WHO needs to shift away from reactive, short-term funding cycles and develop multiyear fnancial roadmaps. Clear objectives, measurable outcomes, and transparent allocation of funds will make WHO a more attractive partner for long-term investors.
UNICEF, which is another UN-afliated agency, has successfully implemented multiyear funding strategies for global child health initiatives. And with this, UNICEF has been able to sustain life-saving programs such as immunization campaigns and maternal healthcare support in low-income countries.
WHO should also leverage its unique position as a global health leader to spearhead stronger international collaborations.
UNLIKE TRADITIONAL DONOR COUNTRIES THAT CONTRIBUTE SPORADICALLY, THE UAE HAS TAKEN A STRATEGIC APPROACH BY INVESTING IN LONGTERM HEALTHCARE PROJECTS THAT ALIGN WITH BOTH NATIONAL AND GLOBAL HEALTH PRIORITIES. IN 2017, THE UAE PLEDGED $100 MILLION TO ELIMINATE RIVER BLINDNESS AND LYMPHATIC FILARIASIS IN AFRICA. RATHER THAN A ONE-TIME DONATION, THE UAE ENSURED THAT THESE FUNDS WERE DISBURSED OVER MULTIPLE YEARS. THE RESULTS HAVE BEEN TRANSFORMATIVE, AS SEEN BY THE REDUCED DISEASE PREVALENCE AND STRENGTHENING OF THE HEALTHCARE SYSTEMS IN THE AFFECTED REGIONS.
Engaging with countries that prioritize healthcare investments such as the UAE, Switzerland, and Germany—could result in joint ventures that align fnancial resources with shared health objectives.
For instance, the UAE’s partnership with the Carter Center in fghting Guinea worm disease has shown how cross-country collaboration can accelerate disease eradication eforts.
Beyond traditional contributions, WHO could explore modern fnancing tools such as social impact bonds (SIBs) and health investment funds. These mechanisms allow investors to fund health initiatives with returns tied to measurable health improvements.
A prime example of this model in action is the Development Impact Bond (DIB) used in India to improve education and health outcomes. Private investors fund programs upfront, and their returns are paid by donors only when pre-agreed results are achieved.
Platforms like GoFundMe and GiveDirectly have proven that collective small donations can generate millions of dollars for urgent health needs. WHO can take that direction, and create an ofcial global health crowdfunding platform that allows individuals to contribute directly to specifc health programs they care about.
Donors, whether governments or private entities, are more likely to invest in organizations that demonstrate transparency and accountability.
WHO can opt to prioritize real-time reporting on how funds are used, the progress of health initiatives, and the impact achieved. Médecins Sans Frontières (Doctors Without Borders) does this. They publish detailed fnancial reports on how every dollar is spent. This level of transparency has helped the organization build trust with donors and maintain steady fnancial support.
WHO could engage the global public in funding specifc health initiatives through crowdfunding campaigns. Micro-donations from millions of individuals worldwide could provide a steady supplemental revenue stream for emergency responses and long-term projects.
WHO has access to vast amounts of global health data, research, and expertise that could be leveraged for sustainable funding. Instead of ofering all its resources for free, it could create a tiered-access model where premium insights and specialized consulting services are available for a fee to corporations.
The World Bank and IMF generate revenue by ofering consulting and data-driven advisory services to member countries. WHO could similarly ofer specialized health advisory services to governments, particularly in developing countries that seek guidance on health related matters.
WHO’s challenges in the past few years have exposed the urgent need for a more resilient fnancial model that is sustainable and even more importantly—resilient to political shifts. To secure its position as a global health leader for years to come, WHO needs to embrace a more corporate-like approach—one that prioritizes diversifed funding.
The WHO must now take inspiration from other organization’s success stories and chart a new course toward fnancial independence.
A stronger, better-funded WHO is a goal that the whole world will defnitely reap from. Because in a world where pandemics, climaterelated health crises, and emerging diseases are not rare, we need an organization that can act swiftly and decisively, free from the constraints of uncertain funding.
It’s time for the WHO to redefne its fnancial prowess—and with the right strategy, the future looks promising.
WHO NEEDS TO SHIFT AWAY FROM REACTIVE, SHORTTERM FUNDING CYCLES AND DEVELOP MULTIYEAR FINANCIAL ROADMAPS. CLEAR OBJECTIVES, MEASURABLE OUTCOMES, AND TRANSPARENT ALLOCATION OF FUNDS WILL MAKE WHO A MORE ATTRACTIVE PARTNER FOR LONG-TERM INVESTORS. UNICEF, WHICH IS ANOTHER UN-AFFILIATED AGENCY, HAS SUCCESSFULLY IMPLEMENTED MULTI-YEAR FUNDING STRATEGIES FOR GLOBAL CHILD HEALTH INITIATIVES.



The healthcare sector is undergoing a revolutionary transformation, driven by the rapid advancements in artifcial intelligence (AI) technologies. These technologies are being integrated into diverse areas of healthcare, from diagnosis and treatment to data management and patient experience. AI enables healthcare organizations to speed up diagnostics, improve treatment decisions, streamline workfows, reduce staf burnout, and enhance patient outcomes. In other words, AI ofers powerful tools that enhance the quality and efectiveness of healthcare. By analyzing vast amounts of data with accuracy and speed, AI enables physicians to make informed decisions and provide better care. AI applications contribute to improved patient outcomes, driving a paradigm shift in healthcare that enhances patient health and overall well-being.
AI algorithms are revolutionizing the accuracy of medical diagnosis, excelling in the analysis of complex medical images, such as X-rays, MRIs, and CT scans. These algorithms can detect subtle anomalies, helping doctors identify issues earlier, which leads to better disease detection and higher chances of successful treatment. Moreover, AI can analyze extensive patient data, including genetic information and medical history, to identify patterns and relationships that may not be apparent to human observers. This ability to analyze large datasets allows AI to predict the likelihood of patients developing specifc conditions, enabling doctors to take preventive measures early and better tailor treatments. AI allows doctors to create highly precise, personalized treatment plans. By analyzing
extensive patient data—such as genetic makeup, medical history, and lifestyle—AI can identify the best treatment path for each individual. This approach, known as precision medicine, moves beyond the traditional onesize-fts-all model, focusing on the unique needs of each patient. This customization maximizes treatment efectiveness while minimizing undesirable side efects. Thanks to AI, medical treatment becomes more targeted and efective, opening new possibilities for improving patient health and well-being.
AI signifcantly contributes to improving the quality of healthcare in various ways. It is used to develop medical data management systems, facilitating access to patient information and improving the efciency of administrative processes in hospitals and clinics.
Additionally, AI can develop applications and virtual assistants that provide support to patients, such as reminding them about medication schedules and ofering personalized health advice, which helps improve treatment adherence and health awareness.
Furthermore, AI reduces medical errors, as algorithms can analyze medical data with precision and speed, assisting doctors in making more accurate decisions. The role of AI extends beyond this by also contributing to reducing healthcare costs, as it can automate some administrative and diagnostic tasks, saving time and efort for medical staf. In general, AI is a powerful tool for enhancing healthcare quality while delivering it at a lower cost.
In the feld of drug discovery and development, AI stands out as a driving force in accelerating this vital process. AI allows for the efcient identifcation of promising drug candidates by analyzing vast and complex
AI ALGORITHMS ARE REVOLUTIONIZING THE ACCURACY OF MEDICAL DIAGNOSIS, EXCELLING IN THE ANALYSIS OF COMPLEX MEDICAL IMAGES, SUCH AS X-RAYS, MRIS, AND CT SCANS. THESE ALGORITHMS CAN DETECT SUBTLE ANOMALIES, HELPING DOCTORS IDENTIFY ISSUES EARLIER, WHICH LEADS TO BETTER DISEASE DETECTION AND HIGHER CHANCES OF SUCCESSFUL TREATMENT.
chemical databases and accurately predicting how diferent molecules will interact with specifed biological targets. This analytical and predictive capability of AI signifcantly reduces the time and costs associated with traditional drug development processes, which typically require years of experimentation and high costs for trials and analyses.
Thanks to AI, researchers and developers can focus on the most efective and safe molecules, accelerating the pace of innovation and providing new, efective drugs for patients in a shorter time and at a lower cost. Additionally, AI can help identify new drug targets that were previously unknown, opening new horizons for treating rare and chronic diseases.
In the feld of robotic surgery and assistance, AI marks a signifcant advancement in how surgical operations are performed. AI-powered robotic systems enhance surgical precision and enable minimally invasive procedures, signifcantly reducing the damage to surrounding tissues and speeding up the recovery process for patients. This advanced technology reduces the risks associated with traditional surgeries, as robots can perform intricate and complex movements that human surgeons may not be able to execute on their own.
Moreover, AI can analyze data and medical images during the procedure to guide the surgeon and provide vital information that aids in making quick and accurate decisions. This integration of robotics and AI not only improves surgical outcomes but also reduces hospital stays and lowers the likelihood of post-surgical complications, ultimately benefting patients by enhancing their quality of life and reducing recovery times.
AI plays a pivotal role in healthcare data management by enabling the analysis of vast amounts of information generated in healthcare institutions. This capability to handle big data provides valuable, actionable insights to healthcare providers and researchers,
assisting them in making informed decisions and improving the quality of care provided to patients. AI can organize and categorize complex medical data, such as electronic patient records, medical images, and genetic data, making it easier to access and analyze efectively. Additionally, AI can be used to identify patterns and trends within the data, helping to detect diseases early and develop new treatments. It can also contribute to better resource management in hospitals and healthcare centers by analyzing patient data and predicting future needs. This ability to analyze data comprehensively and accurately makes AI an indispensable tool in improving the efciency and efectiveness of healthcare delivery.
AI is poised to revolutionize healthcare by improving diagnostic accuracy, ofering personalized treatments, and enabling continuous patient monitoring, all of which will enhance healthcare quality and reduce costs. Wearable AI-powered technology will further strengthen remote patient monitoring, allowing doctors to track patient conditions continuously and respond promptly to any concerning changes. Additionally, AI is also expected to aid in the early detection of rare diseases and provide virtual health coaches to guide patients toward healthier lifestyle choices. In short, AI will revolutionize healthcare by improving diagnostics, personalizing treatment, and enabling continuous patient monitoring.
IN THE FIELD OF ROBOTIC SURGERY AND ASSISTANCE, AI MARKS A SIGNIFICANT ADVANCEMENT IN HOW SURGICAL OPERATIONS ARE PERFORMED. AIPOWERED ROBOTIC SYSTEMS ENHANCE SURGICAL PRECISION AND ENABLE MINIMALLY INVASIVE PROCEDURES, SIGNIFICANTLY REDUCING THE DAMAGE TO SURROUNDING TISSUES AND SPEEDING UP THE RECOVERY PROCESS FOR PATIENTS.
ry eye syndrome, also known as ocular surface disease, is a common yet often overlooked condition that signifcantly impacts quality of life. It occurs due to insufcient tear production or poor tear quality, leading to discomfort that can worsen if left untreated. At Al-Ahli Hospital, Dr. Hind and her team in the Ophthalmology Department specialize in accurate diagnosis and advanced treatment to ensure lasting relief and optimal eye health.
Dry eye occurs when the eyes don’t produce enough tears or when tears evaporate too quickly. Tears are essential for maintaining a healthy eye surface and clear vision.
• Persistent dryness and irritation
• A gritty sensation or feeling of something in the eye
• Redness or infammation
• Blurred vision or difculty focusing
• Sensitivity to light
"Dry eye is not just a minor inconvenience; if untreated, it can lead to serious complications," explains Dr. Hind.
Several factors contribute to dry eye, including environmental, lifestyle, and medical conditions:
• Environmental Factors: Wind, smoke, or dry climates can cause rapid tear evaporation.
• Digital Eye Strain: Prolonged screen use reduces blinking, leading to tear evaporation.
• Aging: Tear production naturally decreases with age, especially after 50.
• Hormonal Changes: Pregnancy, menopause, or oral contraceptives can impact tear production.
• Medications: Antihistamines,
antidepressants, and diuretics may contribute to dryness.
• Underlying Health Conditions: Autoimmune diseases like Sjögren’s syndrome, rheumatoid arthritis, and lupus can cause chronic dry eye.
• Contact Lens Use: Long-term contact lens wear can reduce tear flm quality and increase dryness.
At Al-Ahli Hospital, our team uses cutting-edge tools to identify the root cause of dry eye:
• Tear Break-Up Time Test (TBUT): Measures
DRY EYE OCCURS WHEN THE EYES DON’T PRODUCE ENOUGH TEARS OR WHEN TEARS EVAPORATE TOO QUICKLY. TEARS ARE ESSENTIAL FOR MAINTAINING A HEALTHY EYE SURFACE AND CLEAR VISION.
how quickly tears evaporate.
• Schirmer’s Test: Assesses tear production using a small strip under the eyelid.
• Fluorescein Staining: Highlights areas of eye damage caused by dryness.
• Meibomian Gland Evaluation: Examines the function of glands responsible for tear flm stability.
Treatment is tailored to each patient based on severity and underlying causes.
• Follow the 20-20-20 rule: Every 20 minutes, look 20 feet away for 20 seconds.
• Use a humidifer to maintain indoor moisture levels.
• Wear protective eyewear to shield against wind and dry environments.
• Over-the-counter lubricating drops for mild cases.
• Prescription eye drops like Restasis or Xiidra to reduce infammation and boost tear production.
Small, dissolvable plugs inserted into tear ducts to prevent tear drainage and retain moisture.
Warm compresses or LipiFlow therapy to unclog oil-producing glands and enhance tear flm quality.
Increasing intake of Omega-3 fatty acids (found in fsh, faxseeds, and walnuts) can improve tear quality and reduce infammation.
• Serum Eye Drops: Made from the patient’s blood to promote healing in extreme cases.
• Intense Pulsed Light (IPL) Therapy: Reduces infammation and improves gland function.
• Personalized Treatment Plans: Designed based on the patient’s condition and contributing factors.
• Regular Follow-ups: Continuous monitoring to adjust treatment and prevent recurrence.
• Patient Education: Guidance on lifestyle changes and preventive measures for longterm eye health.
SEVERAL FACTORS CONTRIBUTE TO DRY EYE, INCLUDING ENVIRONMENTAL, LIFESTYLE, AND MEDICAL CONDITIONS: ENVIRONMENTAL FACTORS, DIGITAL EYE STRAIN, AGING, HORMONAL CHANGES, MEDICATIONS, UNDERLYING HEALTH CONDITIONS AND CONTACT LENS USE.
• Stay Hydrated: Drink plenty of water to support tear production.
• Take Breaks from Screens: Reduce digital strain and blink frequently.
• Protect Your Eyes: Wear sunglasses or protective eyewear in harsh conditions.
• Eat a Healthy Diet: Incorporate Omega-3rich foods for better tear quality.
• Review Medications: Consult your doctor about drugs that may contribute to dryness.
• Expertise: Led by Dr. Hind, our ophthalmology team has extensive experience in diagnosing and treating dry eye.
• Advanced Technology: We use the latest diagnostic tools and treatment methods for precise and efective care.
• Personalized Care: Every patient receives a tailored treatment plan to meet their specifc needs.
• Comprehensive Support: From diagnosis to long-term care, we provide continuous guidance for lasting relief.
"Don’t let dry eye afect your quality of life," says Dr. Hind. "With the right treatment, you can protect your vision and enjoy lasting comfort."
Book your consultation today at Al-Ahli Hospital and experience expert dry eye care!
Polycystic Ovary Syndrome (PCOS) is a common hormonal disorder that afects women of reproductive age. It can cause a wide range of symptoms, including irregular periods, weight gain, acne, and excessive hair growth. While there is no cure for PCOS, various treatments are available to help manage its symptoms and improve quality of life.
PCOS varies in severity and impact from one woman to another. Therefore, continuous communication with a healthcare provider allows for the tailoring of treatment to meet the individual needs of each woman. Regular monitoring also helps in the early detection of potential complications, such as insulin resistance, high blood pressure, or high cholesterol, allowing for timely intervention and prevention. Consistent communication with a specialized healthcare provider is crucial in managing PCOS. Regular follow-up enables the doctor to continuously assess the condition, monitor symptom progression, and adjust treatment plans as necessary. The doctor ofers guidance on healthy living, including nutrition, exercise, and coping strategies for the psychological symptoms of PCOS. Regular healthcare visits are vital for managing PCOS and enhancing quality of life for women afected by it.
Following a low glycemic index (GI) diet is an important step in managing PCOS, as it helps reduce sudden spikes in blood sugar levels, thereby aiding in the control of insulin resistance—a common issue in women with this condition. It is also recommended to include fber-rich foods, such as fruits, vegetables, and whole grains, which help regulate blood sugar levels and improve digestion. By focusing on foods that are digested and absorbed more slowly, women can maintain stable blood sugar
levels, reducing excessive insulin production and alleviating symptoms associated with PCOS.
Regular physical exercise is an essential component of managing PCOS, as it plays a signifcant role in improving overall health, controlling weight, and reducing symptoms linked to the condition. Regular physical activity helps enhance insulin sensitivity, reducing the insulin resistance that is one of the primary issues associated with PCOS.
Exercise also helps burn excess calories, supporting weight loss or maintenance, which is crucial for women with PCOS, as weight gain often exacerbates symptoms. In addition, regular exercise contributes to regulating the menstrual cycle, improving mood, and reducing stress and anxiety—common symptoms experienced by women with PCOS. It is important for women to choose exercise types that they enjoy and that match their physical capabilities, such as brisk walking, running, swimming, cycling, or strength training.
Quitting smoking and reducing alcohol consumption are vital steps for women with PCOS. Smoking and alcohol consumption negatively impact hormonal health and exacerbate the symptoms of this condition. Smoking lowers estrogen levels, crucial for menstrual regulation and ovarian health, while increasing insulin resistance, a common issue in women with PCOS. Alcohol also disrupts hormone levels and the menstrual cycle, and both substances elevate the risks of cardiovascular disease, type 2 diabetes, and endometrial cancer—conditions already more prevalent in women with PCOS. Thus, quitting smoking and reducing alcohol intake are critical for managing PCOS efectively and enhancing overall health.
PCOS VARIES IN SEVERITY AND IMPACT FROM ONE WOMAN TO ANOTHER. THEREFORE, CONTINUOUS COMMUNICATION WITH A HEALTHCARE PROVIDER ALLOWS FOR THE TAILORING OF TREATMENT TO MEET THE INDIVIDUAL NEEDS OF EACH WOMAN. REGULAR MONITORING ALSO HELPS IN THE EARLY DETECTION OF POTENTIAL COMPLICATIONS, SUCH AS INSULIN RESISTANCE, HIGH BLOOD PRESSURE, OR HIGH CHOLESTEROL, ALLOWING FOR TIMELY INTERVENTION AND PREVENTION. CONSISTENT COMMUNICATION WITH A SPECIALIZED HEALTHCARE PROVIDER IS CRUCIAL IN MANAGING PCOS. REGULAR.
ealth, as defned by the World Health Organization (WHO), encompasses physical, mental, and social well-being. Yet mental health remains consistently sidelined. Globally, one in eight people struggles with conditions like depression, anxiety, and addiction, major causes of disability worldwide. Economically, untreated mental illnesses could cost $16 trillion by 2030 due to lost productivity and healthcare expenses. Healthcare stands at a crossroads, shaped by social, political, economic, and technological shifts. These changes necessitate rethinking healthcare delivery, especially in resource-limited nations. Despite evidence supporting universal healthcare as morally and economically vital, policymakers hesitate, particularly on mental health, which remains neglected. Nations allocate vast resources to defense but underfund healthcare, equally critical for national stability. Governments often cite fnancial constraints to avoid healthcare reforms, yet rarely scrutinize military spending. COVID-19 exposed healthcare vulnerabilities, proving that robust healthcare is essential for national security and underscoring the ongoing neglect of mental health in policy and funding.
teletherapy can democratize access, especially in underserved communities.
Governments must prioritize mental health within national healthcare agendas, funding community-based services, training primary providers, and expanding telehealth accessibility. Enforcing mental health parity laws ensures equitable treatment alongside physical health.
Mental healthcare cannot be treated as optional or luxury. Comprehensive coverage including therapy, medication, and crisis intervention must be universally accessible. Closing funding gaps and leveraging digital solutions like
Stigma signifcantly obstructs mental healthcare access, driven by misinformation and cultural biases. Tackling this requires:
• Education: Schools and workplaces must openly address mental health, integrating awareness into daily interactions.
• Employer Responsibility: Businesses must provide fexible leave, antidiscrimination policies, and accessible counselling.
• Cultural Competence: Providers need training to deliver sensitive, bias-free care tailored to diverse communities.
• Collective Accountability: A Shared Path Forward
• Transformative healthcare requires unifed action across society:
• Governments: Enforce parity, invest in mental healthcare infrastructure.
• Insurers: Ofer comprehensive, nondiscriminatory coverage.
• Employers: Promote workplace mental well-being.
• Society: Challenge stigma and advocate equitable care. Mental health is not peripheral, it's central to societal well-being. Universal mental healthcare must be prioritized to ensure inclusive, resilient systems. Incremental reforms are insufcient; decisive, collective action is imperative.
Universal healthcare and mental health parity represent essential economic, social, and moral responsibilities. Recognizing healthcare as foundational to national stability is crucial. We face a clear choice: continue neglect or commit decisively to a healthier, equitable future.