


































> Managing Myths: The Facts About Texas Hospitals

> The Numbers Are In: Our Hospital Workforce Needs Serious Help

> Work to Do in Washington: THA’s Federal Priorities Page 4
Industry Issues
> Reeling in Rural Texas
> The Workforce Problem

> Medicaid Enrollees: How to Keep Your Coverage
> COVID-19 in Texas Hospitals: Three Years Later
> Remaining Resilient in Health Care
> Erin Asprec: Building Something New
> Looking Back at THA’s 2023 Annual Conference
Page 29
Membership Spotlight
> Texas Hospital Association Membership Awards

> 23 Women to Know in Texas Hospitals, Health Care and Public Policy
> Celebrating Black Leaders in Texas Hospitals
> Newsmakers
The
Managing
March 2023
January 2023
February 2023
The Texas Hospital Association’s 2023 board chair, Erin Asprec, reflects on a career built upon a passion for accessible health care and looks forward to a new year, a new legislative session and ensuring hospitals’ needs are well-represented at the Texas Capitol.
Written by Amy RiosNinety-two black and white portraits dating back to 1930 line the hallways at THA’s Austin headquarters, prominently displaying world-class hospital leaders who have spoken for the hospital industry as the organization’s board chairs. In January, THA will hang its 93rd portrait, this one featuring Erin Asprec, executive vice president and chief operating officer of Memorial Hermann Health System. It’s a striking representation of the progress achieved when legacies are built upon one another.

After nearly 100 years since THA was founded, Asprec will be only the twelfth woman to hold the title of board chair.
Fortunately, Asprec thrives in environments marked with uncertainty and challenges.
“I’ve been very fortunate since early in my career to be in roles that involved building something from scratch and creating change by which to improve the available programs and services for patients,” Asprec said. “It’s what I gravitate toward.”
On Jan. 10, when the opening gavel falls to mark the new 140-day legislative session, Texas hospitals will need leaders like Asprec at the forefront of the uphill battle to represent hospitals’ needs.

First-hand experience as a patient informed Asprec’s career choice. Born with a rare congenital heart condition called Tetralogy of Fallot, Asprec observed the patient care experience from years spent in doctor’s offices and hospital
beds. She decided that to create systemic change, she would pursue a career in health care administration.
“If it weren’t for the physicians, clinicians, facilities and care that I was very fortunate to have access to, I probably would not be here today,” Asprec said. “Because of that experience so early in life, I am very passionate about ensuring that everyone has access to high-quality health care.”
Few factors impact the well-being of a state’s citizens as much as health care access. Despite Texas’ renowned hospitals and health systems, many Texans continue to struggle accessing health care. Despite having the highest percentage of uninsured among its population, Texas remains one of 12 states in the U.S. that still has not expanded Medicaid coverage for its estimated 1.2 million uninsured residents.
Asprec’s career trajectory mirrors her deep commitment to making health care accessible for patients. Her health care administration career spans nearly 25 years. In that time, she has collaborated with leadership teams to build and renovate hospitals, innovated processes to be more consumer-centric and established differentiated programs and services for the community. Her ability to innovate and think outside of the box will be crucial as THA prepares to work with the Texas Legislature to address the most pressing pandemic-influenced health care issues.
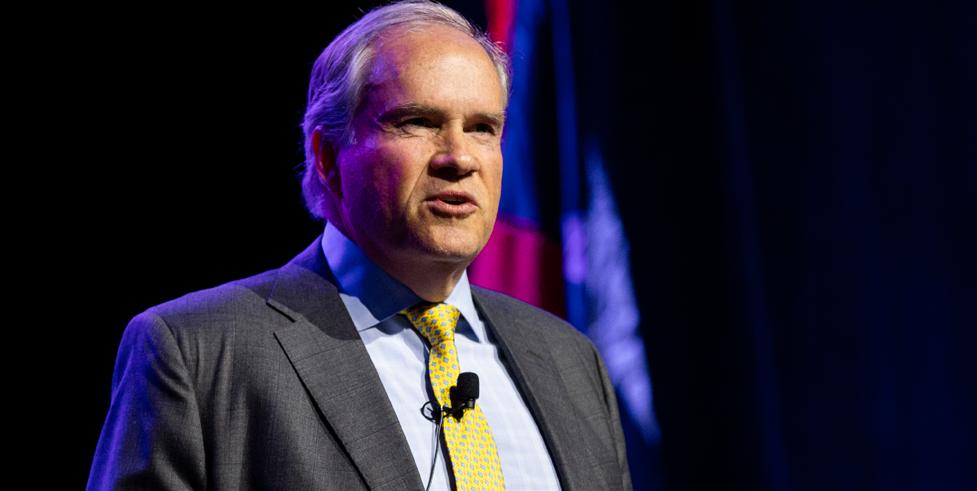
“We’ll need to be aggressive during the 2023 legislative session, and think Erin’s unique insight of THA’s current advocacy priorities will make her an effective board chair,” said John Hawkins, president/CEO of THA. “I recall early on in the
pandemic, Erin would participate on THA’s weekly pandemic calls and identified the issues around workforce inflation and shortages and was instrumental in the formation of THA’s Workforce Task Force, which she chaired.”

Asprec assumed her current role as executive vice president and chief operating officer of Memorial Hermann Health System in January 2020, two months before a global pandemic upended the health care industry. In this role, Asprec oversees the strategic, operational and financial management of all Memorial Hermann operations, which includes 17 hospitals and more than 260 care delivery sites across Southeast Texas. She began her career at Memorial Hermann in 2002 and has built upon each opportunity into increasingly more significant roles within the system. For the past 20 years, Asprec has held integral roles at Memorial Hermann, including key leadership positions—most recently as chief of acute care services and chief transformation officer.
Unsurprisingly, the professional accomplishments that bring her the most satisfaction involve building something new.
In 2004, Asprec was CEO of Memorial Hermann Heart & Vascular Institute-Texas Medical Center. At the time, Memorial Hermann’s Heart & Vascular Institute was under the shadow of two well-regarded, strong cardiology competitors in the Greater Houston market.
In four years, Asprec’s work at the Memorial Hermann Heart & Vascular Institute culminated in the grand opening of a new 230,000 square-foot, eight-story, 147-bed facility that has grown to become one of the country’s top heart and vascular programs.
“That was a very special moment for me because of my heart condition,” Asprec said. “I was proud of the partnerships we formed with physicians to build a program that was top in the country and eventually became a successful, competitive program against two other strong, established competitors.”
For Asprec, building isn’t limited to shiny new hospitals — it also includes re-building processes and service lines to suit the community’s needs.
In 2017, Houston faced the worst oil downturn since the 1980s, and its effects rippled into every industry, even health care. As a result, Houston health systems like Memorial Hermann faced financial uncertainty. At the time, Asprec was the chief transformation officer, and it was clear that, to stay financially solvent, Memorial Hermann needed to transform health care delivery.
Like a good Houstonian, Asprec looked for ways to turn a bust into a boom. She established the health system’s Transformation Office and worked with physicians, clinicians and executives across the system to re-design the health care experience to maximize engagement while reducing waste. As a result, Memorial Hermann decreased its costs and saved a billion dollars over five years.
“It was rewarding not only because it put us back on track in terms of financial stability, but also helped our community,” said Asprec. “It truly improved the care we provide.”
Asprec isn’t just committed to building up hospitals and service lines. She also wants to build a positive corporate culture, particularly for women who still struggle securing a seat at the top.
A 2021 JAMA Network Open study reviewed more than 3,900 health care executives and 3,400 board members across 161 hospitals. The results found that only 15.3% of health system CEOs are women. However, the presence of female CEOs positively influenced gender diversity across the organizational leadership teams.
Asprec, who has been recognized by the Houston Business Journal as one of Houston’s “Women Who Mean Business” and
Asprec says she and the steering committee often field inquiries about Women Leaders of Memorial Hermann and “happily share information” about the program model to help everyone incorporate similar programs in their organizations.
“Erin was instrumental in founding Women Leaders of Memorial Hermann and continues to be a driving force for the program today,” said Teal Holden, senior vice president of Ambulatory Services and Post-Acute Care at Memorial Hermann. “Thanks to her guidance and ongoing dedication, we have proudly supported hundreds of women in their careers, lifting many into leadership roles. Erin’s commitment to mentorship is unmatched, and I can personally say many women within our organization look up to Erin as they work to grow in their respective careers.”
“There is an opportunity here heading into a legislative year with a surplus,” Asprec said. “It’s clearly upon us to be aggressive in advocating for our greatest needs, which right now include opening the workforce pipeline, increased investment in behavioral health, stability for trauma care systems and, as always, pushing for Medicaid expansion in a way that is right for Texas.”
While there is a budget surplus heading into the legislative session, the financial outlook for Texas hospitals is far from ideal. In December 2022, THA released a report compiled by Kaufmann Hall that underscored the existential financial and operational threats Texas hospitals continue to face two and a half years after the beginning of the pandemic. Key findings from the report show that nearly one out of every 10 Texas hospitals is at risk of closure, twice as many as before the pandemic. The report also found that Texas hospital expenses are up 20% over pre-pandemic levels, primarily due to labor, supply and drug increases.
selected among the “Most Powerful and Influential Women in Texas” by the National Diversity Council, wanted to help women navigate their careers. In 2015, she helped spearhead the formation of Women Leaders of Memorial Hermann.
When senior leadership members at Memorial Hermann received feedback from female leaders within the organization that they felt it was difficult to navigate their careers at Memorial Hermann, they knew that feedback must be acted upon.
“We did some research and found that there aren’t many health care organizations that have a leadership group for women,” said Asprec. “So, we looked externally at the programs from other industries like oil and gas or consulting, and we took some of those best practices to found Women Leaders of Memorial Hermann.”
Guided by four tenets: inspiration, mentoring, community service and education, Women Leaders of Memorial Hermann is on a mission to build a culture of excellence among women leaders within Memorial Hermann that has far-reaching, measurable impact.
The program now has over 800 women leaders who circulate through the program. Every year, Women Leaders of Memorial Hermann sponsors two networking events and gives back to the Houston community through partnerships with United Way and Dress for Success, among others.
While everyone would like to put the pandemic in the rearview mirror, its effects are still deeply felt by the hospital industry, left with pervasive workforce shortages and financial instability.
“When I hear people say they are tired of COVID, I want to say, ‘Yeah, no one wants the pandemic to be over more than hospitals,’” Asprec joked. “This misperception that hospitals were financially advantaged due to the pandemic just hurts my soul.”
A self-proclaimed “glass half-full person,” Asprec feels confident that hospitals showed their value during the pandemic, ensuring that the Texas economy could get back on track.
In May 2021, the biennial revenue estimate was increased by $1.67 billion, moving the state from a negative to a positive balance. Texas Comptroller Glenn Hegar credited the improvement to the state’s successful mass COVID-19 vaccination efforts. In the spring of 2021, there were over 70 large vaccine hubs in Texas administering the COVID-19 vaccine. Thirty-six of those hubs were maintained by hospitals and health systems like Memorial Hermann, which hosted a vaccine hub at NRG park in Houston.
It's a formidable challenge, but not beyond Texas hospitals’ capability. Having witnessed Texas hospitals’ collective teamwork to get through the worst of the pandemic, Asprec knows hospitals can work together to get the critical help they need from the legislature.
“There was never a question of if we would help each other,” Asprec said. “And technically we are competitors, but it didn’t matter. In Houston, all the hospitals met, planned and coordinated our response on how to take care of the community together. I will never forget that Texas hospitals and health systems literally banded together and acted as one team. No matter the issue, health care access, corporate culture or organizational alignment, Asprec is compelled by a strong sense of personal responsibility. This sense of duty extends to ensuring hospitals’ needs are well-represented to the 88th Texas Legislature.
“Growing up, it was instilled in me that whenever you see a situation you don’t like or feel should be improved, it is your responsibility to do something about it,” Asprec said. “I deem it my and my colleagues’ responsibility to advocate for our industry. If we are not there advocating and pushing for Texas hospitals’ stability and sustainability, then who will?”


We reminisce on THA’s most popular conference, convening over 300 Texas hospital executives together to network, honor exemplary leaders and examine the most pressing health care policy priorities in the 88th Legislature as we march to Sine Die.
Written by Amy RiosFor the first time since the start of the pandemic, THA hosted its full annual conference without attendance caps or restrictions. After a virtual-only conference in 2021 – which was rescheduled due to Winter Storm Uri – and a smaller-than-usual 2022 conference due to the omicron variant, THA members finally reconvened in Austin, Texas on Valentine’s Day. There was an atmosphere of appreciation for the first semblance of normalcy since 2020.
“While the news media have a reputation for covering only doom and gloom in the health care world, there have been some bright spots peeking out among the clouds,” said John Hawkins, THA president/CEO in his opening remarks. “For starters, we are no longer squarely in the throes of a pandemic. COVID is not gone – but we made it. All Texas hospitals remain open for business.
“And we’re united like never before.”
The timing of THA’s annual conference during a session year affords attendees the unique opportunity to get an inside look at developments in health care policy in real-time. Every day of the 140 days in session are valuable and tumultuous, with news developing by the minute.
By the time conference was underway, the Texas House and Senate’s initial budget bills were reviewed, and assignments were announced for key committees, such as the Senate Committee on Health and Human Services. About 3,200 bills have been filed – approximately half of the average 7,500 bills that are filed throughout session – 642 of which are being tracked by THA. During a typical session, THA will track up to 1,500 bills that impact hospitals. From hospital licensure to medical waste disposal, there are many facets of health care that can be legislated.
Aside from tracking bills, THA is already hard at work combatting the false narrative that hospitals were financially enriched by the pandemic. In early February, a special House Select Committee on Health Care was created and charged with examining “excessive health care costs.” Anticipating this perception, THA released a Kaufman Hall report in December 2022 that demonstrates the financial strain the pandemic put on Texas hospitals.
“The march to May 29 is a long one, but we are proud to work on your behalf,” said Jennifer Banda. “We hope to empower you all to be your legislator’s resource. Make sure they know you are a steadfast leader, resource and infrastructure in the communities you serve.”
The conference culminated with a lively discussion featuring some of Texas’ leading political journalists, including Scott Braddock, editor of The Quorum Report, Sewell Chan, editor in chief of the Texas Tribune and Emily Ramshaw, co-founder and CEO of The 19th News, who provided perspective on the nuances of the current state legislature and its potential downstream effects on Texas hospitals. Panelists pointed out that hospitals are often caught in the crossfire of increasingly polarized and partisan public discourse and bear the brunt of disasters like the pandemic, winter storms, school shootings and controversial politics like the overturning of Roe v. Wade. However, with great responsibility comes great power.
“Hospitals are so critical to the functioning of our communities,” said Ramshaw. “You all yield extraordinary power and you should use it.”

Every year during its annual conference, THA honors exemplary health care leaders and organizations that were nominated and selected by a committee of their peers the year prior.

Earl M. Collier Award for Distinguished Health Care Administration:
Christopher Durovich, FACHE, president and CEO of Children’s Health
The Earl M. Collier Award is the highest honor bestowed by THA. It recognizes outstanding executives who have distinguished themselves through their contributions to the health care industry and their profession, who are leaders in providing quality health care services and active in THA and other industry groups.
For the past 20 years, Durovich has led Children’s Health as president and CEO, guiding the organization through extensive growth and transformation, evolving from a single local children’s hospital to a nationally recognized, award-winning, and market-leading pediatric health system serving one of the nation’s fastest-growing pediatric populations. Today, the system serves more than 300,000 unique patients annually across 800,000 separate patient encounters and contributes $3.3 billion to the North Texas economy.
“I am honored and humbled to receive this recognition,” said Durovich. “I would not be here without the extraordinary work and passion of all those at Children’s Health who fulfill our mission to make life better for children. I am proud to serve with and among them.”

The Pioneer Award is given to a CEO/administrator of a rural hospital or health care system who demonstrates creative and innovative management achievements and leadership within the organization and community. This award is sponsored by the Texas Hospital Insurance Exchange.
Since joining Deaf Smith County Hospital District in 2016 as CEO, Jeff Barnhart has made it his mission to ensure every resident has access to the care they need, when they need it. Barnhart oversees operations of Deaf Smith County Hospital District’s hospital, outpatient clinic, and EMS services. Barnhart never loses sight of the mission to improve the health and quality of life of the individuals and communities DSCHD serves and to be the health care provider of choice for the region. He maintains the necessary big picture, visionary thinking required to run a successful rural hospital while never shying away from the smallest or most menial of tasks if needed to help a patient or team member.
The Excellence in Community Service Award recognizes hospitals and health care systems that have distinguished themselves through contributions to their community.
Texas Health Resources in Arlington was awarded the Texas Hospital Association’s Excellence in Community Service Award for implementation of Blue Zones Project®, a neighborhood-byneighborhood transformation project to improve the health and well-being of people living Fort Worth, Texas.
Hendrick Health received an honorable mention for its ‘A New Day in the Neighborhood’ project which partnered with Day Nursey of Abilene to convert an empty elementary school into a day care facility.
Bill Aston Award for Quality: Academic Institution or Large Teaching Hospital/Health System: University Health

Texas Health Resources in Arlington was awarded THA’s Bill Aston Award for Quality for its Early Recognition and Treatment of Ischemic Stroke project, an innovative approach to improve care and mortality of stroke patients.
The Texas Hospital Association Bill Aston Award for Quality honors hospitals’ measurable success in improving quality and patient outcomes through the sustained implementation of a national and/or state evidence-based patient care initiative.
Texas University Health in San Antonio was awarded THA’s Bill Aston Award for Quality for its Hospital at Home project, a care model that provides hospital-level of care and addresses patient needs in the comfort of their homes.

We hope to see you next year at THA’s 2024 Annual Conference & Expo
Feb. 15 – 16, 2024 at the Hyatt Regency Dallas

There's a clear shift to embrace physical and mental well-being within the health care industry, which was mirrored throughout the exhibit hall with wellness-themed sponsor breaks. Attendees had the opportunity to meet therapy puppies, take a quick yoga or meditation break and win one of two Pelotons.

The Texas Hospital Association recently kicked off the 2023 class of its Leadership Fellows Program, the association’s premier leadership development cohort.

Since 2014, the program has provided health care leaders with in-depth knowledge of the legislative and regulatory process while educating them on priority health care policy issues and connecting them with key stakeholders and policy decisionmakers in Texas. The Leadership Fellows Program also aims to help its participants grow as leaders and become fully equipped to lead policy discussions, drive integration and create environments that enable the best possible patient care outcomes for their hospitals or health systems.
Due to popular demand, THA incorporated two breakout sessions focused on wellness and stress prevention and management for health care leaders and clinicians.
Of course, no trip to the Live Music Capital would be complete without live music. During the Welcome to Austin reception, attendees got to network and listen to the popular local Kristen Gibbs Band.
Thank you to all the attendees, sponsors, speakers and staff who contributed to this year’s conference. Your participation enables us to continue offering educational opportunities, expand our services and advocate on behalf of Texas hospitals.
Each year, the cohort meets in Austin four times for program modules which consist of policy core competencies, real-time legislative updates, communications and presentation strategies, leadership and engagement, and CEO insights. In addition to lectures, panel discussions and project development, fellows participate in competition and mentoring components as well.
As the health care industry and policy landscape evolves, so does the curriculum of the Leadership Fellows Program. Fellows work with THA’s advocacy staff to become familiar with the issues each lobbyist works on so they can engage with them on issues their organizations face. Fellows are also exposed to legislators or legislative staffers, resources at state agencies like HHSC or DSHS as well as established hospital CEOs from across the state.
With 2023 being a legislative session year, there is no better time for participants to observe the legislative process in full swing and gain up-to-the-minute legislative updates on hearings, testimony, bill movement and more.
THA’s Senior Director of Education and Governance Programs Lindsay Thompson shared, “At its core, the Leadership Fellows Program exists to educate hospital leaders on the legislative process so when we’re doing that in a legislative session year, not only do the fellows get to see the process play out in real time but they can use those insights to advance their work on their capstone projects.”
The 2023 class of THA’s Leadership Fellows Program convened in Austin to kick off this year’s iteration of the program which will focus on key policy priorities facing Texas hospitals.Every class of the Leadership Fellows Program completes a capstone project that focuses on key issues facing the health care industry. In the past this has included Medicaid expansion, behavioral health access, the impacts of COVID-19 on Texas hospitals and workforce issues. This year’s group is taking a comprehensive approach with small groups focusing on hospital funding, public and community health, health equity, behavioral health and health care coverage, which parallels the THA’s policy priorities in the current legislative session.
This year, the fellows’ capstone projects involve a new component that requires each participant to put together and deliver mock testimony on the issue they are working on.
“By adding this component in a legislative session year, fellows have the opportunity to witness THA’s advocacy staff and THA member hospitals testifying at the capital on the same issues they are working on,” Thompson explained.

At the conclusion of the program, the cohort has the necessary tools to be effective health care advocates at the community, state and federal levels. The cohort also joins the growing alumni network of over 150 health care executives that provides long-term connections and resources for fellows as they continue in their careers in health care.
Thompson also noted that this year’s class participants are split almost 50-50 between urban and rural hospital leaders, proving the increasing interest and participation by leaders from rural hospitals across the state.
“As I’ve been involved with THA in different capacities over the years, I’ve gained a deeper appreciation for the work that THA does in advocating for its member hospitals and for our patients. I decided to join the Leadership Fellows Program, as a way for me to not only further my relationships within THA and with other hospital leaders across the state, but also to be able to collaborate with these leaders to hopefully help hospitals meet some of the challenges that we’re all facing.”
– Jason Wren, CEO, Wise Health System“I joined THA’s Leadership Fellows Program because I wanted to learn more about the legislative process and how decisions that impact health care delivery and outcomes are made at a level beyond the hospital system that I work in — everything from understanding how decisions are made and what the priorities, trends, and barriers are to making those decisions, to the resources and levers we can use to impact those decisions. I’m also looking forward to the opportunity to connect with peers and colleagues across the state who work in health care and health care leadership.”
- Khalid
Almoosa, M.D., MBA, Chief Medical Officer, Memorial Hermann Katy and Cypress
You can learn more about THA’s 2023 Leadership Fellows Program here or view the Class of 2023 here.
THA launched the weekly recap Jan. 30 and will continue through the end of the regular legislative session, which concludes May 29. Each week during the 2023 session of the Texas Legislature, The Scope’s Cap Recap will take a quick look at the previous week’s most hospital-relevant news under the Pink Dome in Austin.
 Written by Joey Berlin
Written by Joey Berlin
Sen. Lois Kolkhorst (R-Brenham) teased THA General Counsel
Steve Wohleb as he prepared to testify on his third bill of Wednesday’s Senate Committee on Health & Human Services hearing, saying, “I notice you’re not for any of these bills we heard today.”
Some weeks end up like that. For THA, it was a week to repeatedly stand against problematic legislation, and THA membership, THA staff and THA’s written words combined to offer committees detailed descriptions on why myriad bills were so harmful to hospitals.
Sen. Lois Kolkhorst (R-Brenham) teased THA General Counsel
Steve Wohleb as he prepared to testify on his third bill of Wednesday’s Senate Committee on Health & Human Services hearing, saying, “I notice you’re not for any of these bills we heard today.”
Some weeks end up like that. For THA, it was a week to repeatedly stand against problematic legislation, and THA membership, THA staff and THA’s written words combined to offer committees detailed descriptions on why myriad bills were so harmful to hospitals.
Sen. Lois Kolkhorst (R-Brenham) teased THA General Counsel
Sn the midst of about a dozen THA testimonies and a couple of key bill advancements, one fight loomed large above the rest last week at the Capitol, as THA hit back hard against a bill that would institute government rate-setting and depress insurance coverage.
Sen. Lois Kolkhorst (R-Brenham) teased THA General Counsel
Steve Wohleb as he prepared to testify on his third bill of Wednesday’s Senate Committee on Health & Human Services hearing, saying, “I notice you’re not for any of these bills we heard today.”
Some weeks end up like that. For THA, it was a week to repeatedly stand against problematic legislation, and THA membership, THA staff and THA’s written words combined to offer committees detailed descriptions on why myriad bills were so harmful to hospitals.





The 88th Legislative Session has begun and THA’s lobby team is prepared to tackle any challenges on behalf of Texas Hospitals. THA is at the forefront of making sure Texas’ vital health care infrastructure is supported and present in policy decisions. Our lobby team is committed to promoting the interests of Texas hospitals and patients, during and beyond the legislative session.

Three times during the COVID-19 pandemic, Dimmit Regional Hospital came close to taking out a loan just to make payroll. One of those times, the Carrizo Springs facility – tucked deep in rural Southwest Texas – came within mere hours of heading to the bank.
Then, Dimmit’s uncompensated care payment came in the day before the hospital needed to arrange payroll.
For CEO John Graves and his staff, it was a relief – and also a sobering indicator of what rural hospitals faced not just during the worst of the pandemic, but continue to face today as well.
Staffing shortages have long been the norm but are far worse coming out of the pandemic. Inflation is, well, inflating hospital costs. Those and other factors are affecting hospitals across Texas, but are especially hitting the ones that may be the only facility of their kind for miles and miles.
“My hospital, fortunately, we’ve come out of the hole a little bit, despite COVID,” Graves said. “I’m not sure what the future is with all of these continuing costs, when costs are increasing and reimbursements are decreasing. Eventually, that’s going to catch up to us.”
Recent research commissioned by the Texas Hospital Association revealed that more than one in four Texas rural hospitals are at high risk of closure, a game of sustainability Russian roulette that threatens the health of communities all over the state. When rural hospitals are challenged, so are the health and infrastructure of their communities. .
That’s why THA is urging help from the Texas Legislature during the current session, through funding and legislation that can keep rural facilities alive and thriving.
The struggles, explained
A recent report by Kaufman Hall on the financial impact of COVID-19 on Texas hospitals revealed a devastating analysis on the state’s entire hospital landscape. Nearly half of hospitals operated at negative margins in 2022, according to the report; expenses ballooned by more than $33 billion over prepandemic levels; and the number of hospitals at risk of closure nearly doubled compared to 2020, with almost one in 10 hospitals possibly staring at the end of their existence.
But within that last figure contained a specifically eye-opening sign for Texans in the state’s rural communities. Significantly more rural hospitals face the end of the line than facilities in Texas’ major metros – in fact, 26% of rural hospitals are at risk of closure, as compared to 5% of urban hospitals.
“Which means that a rural community hospital is five times more likely to close, or highly vulnerable, than their urban friends,” notes John Henderson, president and CEO of the Texas Organization of Rural & Community Hospitals (TORCH).
Just about every challenge hospitals are facing is exacerbated in the rural setting – whether it’s workforce shortages affecting nurses, physicians and other health care professionals, or rising expenses and other hits to the bottom line. For instance, recruiting workforce to remote areas of Texas is challenging to begin with, and the attrition that came with COVID-19 was another blow to facilities way outside of any major metro.
“We’ve had to make some pretty significant adjustments to our salary structure just to be able to maintain nurses,” Graves said of Dimmit Regional, which has about 9,000 Texas residents in its primary service area. “Because if you’ve ever been to
southwest Texas, you would understand it’s a little difficult trying to recruit people down there, particularly for the physician’s side and the mid-levels. The nurse practitioners and [physician’s assistants], those are just very difficult.”
Sparse housing numbers in such communities mean sparse tax revenue, which also puts rural facilities at a natural disadvantage. “We’re one of the lowest-taxing districts in the state – I think the bottom third,” Graves added. “So our tax revenue is not quite what other folks’ are. So the financial bottom line is a challenge with some of these obstacles.”
And “cash is king,” he said. Dimmit is “in good shape now” due to the strategic and operational changes that the pandemic necessitated. But it’s still among the rural centers that has to watch its cash flow more closely than some others.
“Some of these hospitals [that] are at risk of closure, they’re below 30 cash days on hand. We’re sitting around 40, so we’re not that far above the 30-day threshold,” he said. “So that’s always a concern.”


Much of what rural hospitals need from lawmakers during this session of the Texas Legislature are the same things every hospital needs to combat widespread workforce shortages and financial stability pain points. But rural hospitals have their own unique needs, and THA is striving to make sure legislators follow through on delivering those as well.
Workforce recruitment and retention programs are largely the domain of the state budget. The House and Senate’s respective, highly similar initial budget proposals for 2024-25 contain THA-supported funding levels for these programs, including:
• The Nursing Shortage Reduction Program to increase nursing school graduates: $46.8 million (an increase of about $18 million from 2022-23);
• The Loan Repayment Program for Mental Health Professionals, which encourages those professionals to practice in a health professional shortage area: $28 million (a gigantic increase of $26 million);
• The Nursing Faculty Loan Repayment Program to increase the number of nursing faculty: $7 million (increase of $4 million); and
• The Graduate Medical Education (GME) Expansion Program, funded at a proposed $233 million to help keep Texas medical school students in Texas when they start residency, a strong indicator that they’ll stay there when their career finally begins.
Henderson of TORCH notes that while COVID brought damaging impacts, in some ways, the response to the disease deferred aspects of the current rural-risk crisis, which had started well before the pandemic. Federal relief payments helped keep hospitals afloat for about the first 21 months of the pandemic before those payments ceased in late 2021. And bed capacity was pushed to a breaking point, which forced hospitals – with the blessing of regulatory authorities – to find nontraditional solutions they don’t have in non-pandemic times.
“We needed every bed that we could get our hands on,” Henderson said. “And rural communities, even though it was terrible, probably benefited from that operationally in a way that, as we move out of the pandemic, they [are returning] to that vulnerable state they were experiencing in 2019.”
In a proposed figure that would directly target rural services, Senate Bill 1 and House Bill 1 would also maintain the current $8 million in funding for $500 rural labor and delivery service add-on payments in Medicaid. THA supports that funding, and the ongoing discussions about whether it should be adjusted upward. Rural outpatient add-on payment funding – as well as funding for safety-net and trauma care add-ons – would remain level as well. And money for additional inpatient psychiatric beds across the state would include the dollars for 85 beds in rural communities, with THA asking for a rate increase for those beds as well. Overall Medicaid funding gets a slight bump in the current budget version.
Henderson calls Medicaid “number one” in the state budget for rural concerns, and would also like to see hospitals explore enhanced regional collaboration to address bed capacity challenges. At the federal level, THA continues to advocate for delaying or abandoning harmful cuts that can damage rural hospitals, including federal sequestration cuts. THA is also pushing for Congress and the Centers for Medicare & Medicaid Services to strap a stronger legislative and regulatory leash on Medicare Advantage plans – which are notorious for delaying and denying care and have a significant rural impact.
“There are implications of [Medicare Advantage] for everyone, but it seems like it disproportionately affects rural communities where literally half of the community is Medicare-eligible,” Henderson said.
“Extreme pressure on lifesaving hospitals creates risk for patients and the state’s overall health, hospitals are critical infrastructure for communities and serve as a backbone for health, safety, jobs and stability.”
John Hawkins, President/CEO, Texas Hospital Association
Understanding the depth of today’s hospital workforce problems requires understanding that they didn’t start with the COVID-19 pandemic.
Unlike many societal issues that COVID-19 seemed to foster from scratch, workforce had been an issue for hospitals before the pandemic, with a lack of adequate nursing, medical and other health care staff. Over the past three years, the pandemic’s ripple effects turned Texas’ workforce concerns into a critical need.
Hospitals are struggling, and they need help to replenish their workforce numbers and bolster their health-serving, life-saving mission.
“We have a shortage of nurses, we have a shortage of techs, we have a shortage of physicians. You name it, there’s a shortage of it,” says Cameron Duncan, J.D., THA’s vice president of advocacy and public policy, who focuses on workforce matters.

The pandemic generated new issues contributing to the workforce crisis and intensified old ones: Competition for wages, health care worker burnout and workplace violence all reached new heights and contributed to thinning out the ranks of hospital workers. Nurses left at a record rate due to the pressures of COVID-19, which pushed their colleagues remaining at hospitals to work longer hours and intensified exhaustion and mental strain. Meanwhile, filling the state’s pipeline with replacements has proven to be its own challenge. Texas nursing schools turned away 15,709 qualified applicants in 2021 due to nursing faculty and clinical education capacity shortages.
“There’s been a false narrative that things like vaccines or other social issues have driven health care workers away from their positions,” Duncan says. “But in reality, they’ve left because of greater pay, [or] because they were burned out.”
Additionally – as a survey conducted by the Texas Hospital Association in late 2022 shows – health care workers experienced higher rates of workplace violence during this time, especially nurses. Nearly every hospital responding to the survey – all but one – reported workplace violence had increased or stayed the same during the pandemic, with 61% reporting that violence severity increased. As nurses left, salary competition between hospitals grew. Today, hospitals struggle to keep up with the needs of their communities in both rural and urban settings. THA’s workforce survey showed 64% of hospitals are operating with fewer beds and reduced services because of nurse staffing shortages. Boosting nurse numbers is paramount to Texas hospitals’ efforts to serve communities and save lives.
The shortages in hospitals have created holes in Texas’ health care infrastructure and exacerbated other problems beyond hospital walls. As the Texas Tribune recently reported, mothers in East Texas must drive more than an hour to deliver their babies due to the dearth of obstetricians in the rural east. The Tribune also reported this month that Texas’ jails are holding inmates who must wait over a year for treatment because of lack of staff in psychiatric hospitals.
During this session of the Texas Legislature, lawmakers have a historically massive budget surplus to work with – more than $32 billion. So relative to other legislative years, the Legislature is flush with funds. And, in early iterations of the next budget, lawmakers have demonstrated a heartening commitment to Texas Hospital Association-prescribed solutions to rebuild the state’s hospital workforce.
THA is supportive of the Legislature’s current plans for workforce funding in 2024-25, including:
• $46.8 million for the Nursing Shortage Reduction Program, an increase of more than $26 million;
• More than $7 million for the Nursing Faculty Loan Repayment Program, which more than doubles that program’s current allotment;
• A whopping $26 million increase, to $28 million in funding, for the Loan Repayment Program for Mental Health Professionals, which encourages those workers to practice in a mental health professional shortage area; and
• $233 million for the Graduate Medical Education (GME) Expansion Program, which would maintain the 1.1-to-1 ratio of residency slots to medical school graduates. GME funding is especially important because data has shown that medical students who undertake their residency in Texas typically stay in Texas to practice.
Workplace violence must receive targeted legislation in its own right to be addressed properly. THA supports House Bill 112 by Rep. Donna Howard (D-Austin) and Senate Bill 240 by Sen. Donna Campbell, MD (R-New Braunfels), which require hospitals to create a workplace violence committee and perform individualized training at least annually.
More information can be found in the video below, and in THA’s recent white paper, Soaring Staff Vacancies Results in Reduced Hospital Services.

The state of Texas will soon begin redetermining Medicaid begin redetermining Medicaid eligibility for millions of Texans who have had continuous coverage throughout the COVID-19 public health emergency. Even if you’re still eligible for Medicaid going forward, you may be at risk of disenrollment if the state doesn’t have your updated information.
Previously, while the public health emergency or PHE remained in effect, Medicaid recipients had protected continuous coverage through the calendar month that the PHE ends. But at the end of 2022, Congress ended the continuous-coverage requirement effective March 31 add “of this year” or “2023” just to clarify.
So in April, the Texas Health and Human Services Commission, HHSC, will begin sending out renewal packets to collect updated information necessary to redetermine the eligibility of millions of current Medicaid enrollees, verifying that they meet certain requirements, such as income level, to remain enrolled. If you want to continue receiving Medicaid, the time to act is now. Here are the steps you need to take to stay enrolled:
• The easiest and fastest way to stay up to date on your case is to create an online account. If you haven’t already, create an account at YourTexasBenefits.com. This will allow you to view your account information, update your contact info, submit a renewal and respond to requests from HHSC.
• Once you log in to your account, you should be able to click “Select Details.” There, you’ll see a Time to Renew column, which will say “yes” when it’s time to renew.
HHSC needs Medicaid enrollees’ updated information before the state begins redetermining eligibility for millions of Texans.
 Written by Julia Mann
Written by Julia Mann
• The most important thing you need to do is review and update your information, so it is up-to-date and accurate BEFORE HHSC begins processing your renewal. This will make the process smoother. You can also call 2-1-1 and select option 2 to update your information.
• HHSC is sending renewal packets or requests for information in the mail. Look for these notices – they will be in a yellow envelope. In your account, you can also you can also sign up for electronic alerts and reminders, such as text and email messages, to stay informed about your case.
From the first COVID-19 cases to the development of ground-breaking technology, Texas hospitals have weathered the pandemic’s storm and continue to rebuild in its wake. Three years later, THA reflects on how Texas hospitals and health care workers met the pandemic with resiliency and ingenuity.
This month marks three years since the COVID-19 pandemic irrevocably changed the health care landscape. On March 13, 2020, Gov. Greg Abbott declared a state of disaster for all Texas counties. Schools went online, Texans were urged to stay at home and hospitals paused elective procedures.

The world stopped and waited for an end that took years to arrive.
The effects of the pandemic were felt most acutely by those working in health care. Since March 2020, hospitals have contended with ever-evolving guidance, surges and a pervasive workforce shortage that requires hospitals to do more with less.

The one constant over the past three years is the heroism of our hospitals and health care workers. As cases climbed, Texas hospitals shined, and our state’s health care heroes continue to scrub in and care for patients.
In the early days of the pandemic, photos of health care workers holding signs that said, “We came to work for you. Please stay home for us,” flooded social media feeds and “Heroes Work Here” signage adorned hospital lawns. The public’s heightened awareness of the health care workforce prompted hospitals to use social media to encourage the public to support frontline workers and adhere to preventative measures out of care for them.

Memorial Hermann’s CountingOnHOU campaign featured Memorial Hermann employees and affiliate physicians who reminded the Houston community of the importance of basic safety measures like wearing a mask, hand washing and maintaining social distancing. Frontline health care workers needed support and stability during this time of upheaval.


During surges, many hospital workers had longer shifts and had less time to shop for groceries or pick up their children from school. To help their staff, several Texas hospitals implemented employee support programs to fill in the gaps.
To help hospital staff keep food on the table amid long shifts, worsened by inconsistent grocery store hours and supply chain disruptions, Harris Health offered pre-packaged produce bags that employees could preorder and pick up at the end of their shift.


To show appreciation for its employees and affiliated physicians, the Memorial Hermann Foundation launched “Feeding Frontline Families,” a program that encouraged community members to gift warm meals for health care workers and their families. The effort also encouraged community-support of local restaurants that were also experiencing financial strain due to the pandemic.
With in-person school and daycare suspended, the pandemic put many working parents in a challenging situation, especially frontline health care workers. UMC Health System partnered with the Lubbock Independent School System to provide childcare for the kids of hospital employees for 12 weeks. Tight safety protocols - such as masks, temperature checks and regular hand washing - were followed to ensure the program stayed virus-free.
On Dec. 14, 2020, the first shipments of Pfizer’s COVID-19 vaccine arrived at Texas hospitals. Within the week, nearly a quarter million doses were distributed to 109 hospitals for “first tier” recipients, which included frontline health care workers. For them, the boxes of vaccines were the first sign of hope against a virus that, at the time, claimed the lives of 24,000 Texans and stretched the hospital workforce to unsustainable limits.



As the vaccine rollout progressed, the call to “get shots in arms” was dutifully answered by Texas hospitals. In January 2021, when vaccine eligibility expanded beyond the first tier of recipients, the need for large vaccine hubs became apparent.
In the spring of 2021, there were over 70 vaccine hubs in Texas – approximately half of them were managed by Texas hospitals and health systems. Vaccine providers had to contend with the appreciable challenges of operationalizing a large clinic that processed patients quickly, which included securing a large venue, staffing it and developing an automated system to register patients. In January 2021, Memorial Hermann hosted the first of several mass vaccination clinics, where approximately 14,500 community members were vaccinated in
In May 2021, the biennial revenue estimate was increased by $1.67 billion, moving the state from a negative to a positive balance. Texas Comptroller Glenn Hegar credited the improvement to the state’s successful mass COVID-19 vaccination efforts. Despite its challenges, the vaccine rollout was memorable for patients and providers alike. For vaccine recipients, getting the shot symbolized protection. For vaccine providers, giving the shot to thousands of patients every day is a tangibly gratifying experience for those who’ve dedicated their careers to caring for others.
Expanding its service to the community, Baylor Scott & White launched a unique COVID-19 remote monitoring program through the MyBSWHealth app. To date, the program has supported more than 170,000 adult and pediatric patients with mild illness while in quarantine. Once the COVID vaccine became available, MyBSWHealth enabled patients to schedule their COVID vaccine and boosters. To date, more than 368,000 vaccine appointments have been scheduled via MyBSWHealth.
Now, the MyBSWHealth app provides access to virtual health care 24/7, even to patients who do not have an established relationship with Baylor Scott & White.

2020 proved to be an epoch that will forever change health care delivery. Telemedicine, health care equity, staff retention and burnout have been re-examined more scrupulously with a post-pandemic perspective.
The effects of the pandemic will ripple throughout the health care industry for many years. In a recent survey of member hospitals, over 60% of the 178 hospitals that participated indicated a significant nursing shortage that disrupted health care delivery.

just four days. The drive-through clinics were staffed and made possible by hundreds of volunteers from the community and from the health system. Part of what contributed to the success of Memorial Hermann’s vaccine hub was the development of a homegrown web tool as part of the registration process, which eliminated much of the required paperwork and allowed for each participant to be automatically integrated into Memorial Hermann’s electronic medical records.
When the FDA authorized vaccines for the public, a unique University Health multidisciplinary team came together to make them available. They stood up and operated one of the first and largest vaccination centers in Texas at Wonderland of the Americas, a centrally located shopping mall in San Antonio. The integrated team also routinely delivered vaccines to people in cars outside the mall entrance, and they took doses on the road to the homes of people who were homebound. At its peak, the Wonderland vaccination team was providing thousands of shots a day, with an all-time high of 8,000 doses in a single day. By the end, they had delivered 495,788 doses of COVID-19 vaccine.
From infection prevention to telemedicine, the pandemic dramatically changed health care access and delivery. As hospitals looked to reserve beds, resources and staff for surges, patients embraced staying at home. They opted for more remote health care, including options for care that otherwise would only have been available within a hospital.
The share of Medicare visits conducted through telehealth, skyrocketed from approximately 840,000 in 2019 to 52.7 million in 2020, according to a December 2021 report from the US Department of Health & Human Services.
Not only did shelter at home orders make home care a more attractive choice, but access and reimbursement for telehealth services was expanded.
In the early days of the pandemic, Baylor Scott & White Health was able to quickly leverage its digital health platform. Through MyBSWHealth, Baylor Scott & White became one of the first health systems in the nation to mobilize a COVID-19 screening and drive-thru testing effort for everyone who needed it.
A separate report compiled by Kaufman Hall revealed the devastating financial impact the pandemic had on Texas hospitals. Nearly half of hospitals operated at negative margins in 2022, according to the report; expenses ballooned by more than $33 billion over pre-pandemic levels; and the number of hospitals at risk of closure nearly doubled compared to 2020, with almost one in 10 hospitals at risk of closure. It’s an untenable situation for hospitals and health care workers.

The events of the past three years heavily influenced THA’s policy priorities for the 88th Texas Legislature. Now, 10 weeks into the legislative session, THA is pushing hard to refortify the depleted health care workforce, address the growing need for behavioral health care and protect access to health care for rural Texans because the hospitals that were ground zero amid the pandemic deserve protection and support.
Legislation that’s passed by Sine Die will determine what the next two to three years look like for Texas hospitals. Stay up to date with THA’s Cap Recap, a weekly digest of the most hospital-relevant news under the Pink Dome in Austin.
Tips from THA’s popular resiliency series help health care managers and frontline workers become more resilient against the common contributors of burnout.
We’ve all heard it: the perfunctory instructions given by flight attendants before a plane’s departure. Amid demonstrations of the aircraft’s safety features and what to do if there is a loss in cabin pressure, there is an order that stands out.
Secure your own mask before assisting others.
It’s a phrase reiterated so often it’s become a cliché for the importance of self-care. And, just like preflight instructions, it often goes ignored. Even if we understand the internal logic that care givers must care for themselves first, health care workers consistently experience burnout.
Since the pandemic, health care workers report alarming levels of burnout, which is broadly defined as a state of emotional exhaustion caused by chronic workplace stress. In a recent survey released by THA, which collected responses from 178 hospitals in Texas, 61% of respondents who left hospital employment cited burnout as one of their top reasons for leaving.
The burnout trend isn’t unique to Texas. According to a 2022 Morbidity and Mortality Weekly Report published by the CDC, nearly 53% of health care workers in the United States reported symptoms of at least one mental health condition, such as anxiety, depression and post-traumatic stress disorder, within the past two weeks.
From janitorial staff to nurses and executives, burnout is an existential crisis that everyone in the industry is at risk of experiencing. Like the real estate and banking industries after the Great Recession of 2008, the health care industry will be marked by the adversity of the COVID-19 pandemic for many years.
To help equip health care workers with tools to address this ongoing crisis, THA hosted a workplace resiliency webinar series in collaboration with the Texas Organization of Rural and Community Hospitals, made possible with funding from the U.S. Department of Health and Human Services Administration for Strategic Preparedness and Response (ASPR).
Facilitated by Cindi Baldi, Ph.D., founder of CEO of management science firm Culsure and Geoffrey Tumlin, Ph.D., president of On-Demand Leadership, the six-week series was offered to clinical and non-clinical managers within Texas hospitals and health systems.

All session descriptions, handouts, exercises, speaker information and recommended reading can be found here

Resilience is broadly defined as a collection of qualities that enable a person to adapt and thrive in the face of adversity and stress. Like any characteristic, it can be developed with practice.
Resiliency is not a stable trait; it ebbs and flows depending on the individual and their circumstances. If someone isn’t regularly practicing self-care and “filling the reserves” during good times, it will limit their ability to meet adverse circumstances with resiliency. Additionally, everyone has a breaking point if too much adversity compounds without reprieve. Resiliency is a useful skill for everyone, but it’s especially useful for health care workers because they witness others’ adversity on a daily basis.
To prepare for adversity, follow the “3As” to better respond to the situation with resiliency:
• Acknowledge and affirm the reality of the situation.
• Adjust and reframe the situation from being a threat to being a challenge or an opportunity to grow.
• Act
In the moment of adversity, practice scientifically proven techniques to de-escalate the internal stress response via ACT (Acceptance and Commitment Therapy):
1. Stay in the moment and be mindful of the thoughts and choices you’re making.
2. Don’t judge the thoughts you’re having. Embrace them rather than trying to avoid, deny or alter them.
3. Return to your center by considering your personal values rather than quickly taking action. These values will allow you to take concrete next steps.
To reduce the likelihood of trauma after facing adversity, do the following:
• Reflect on what you’ve learned from the situation and move forward with those lessons. Don’t ruminate on the experience beyond that.
• Try to pull some significance from the experience.
Resources:
You’re not you when you’re exhausted. Symptoms of fatigue, exhaustion and burnout manifest emotionally and physically and impair our ability to meet adversity with resilience. Identifying the early signs of burnout is crucial, particularly in health care because the best and brightest minds have the ability to save lives but might quit their work prematurely due to overexerting themselves.
Understand the difference between common terms:
• Fatigue can be remedied with a few days of rest away from work.
• Exhaustion requires more time away from work and is typically accompanied by lethargy once work resumes.
• Burnout is characterized by a trifecta of professional depersonalization, cynicism and inefficacy. Its accompanying fatigue is not improved by prolonged periods of rest away from work.
To proactively prevent fatigue, exhaustion or burnout, try the following:
• Invest in your work environment by creating a workspace that reflects the mood you want.
• Plan a rest period every month for the next six months.
• Regularly remind yourself of the purpose behind your work and why you’ve chosen to pursue the career you have.
• Understand there is no substitute for regular, high-quality sleep. If your sleep schedule is disrupted, you will feel the effects of fatigue, exhaustion or burnout more acutely.
The importance of investing in relationships, particularly outside of work, cannot be overstated. If we have regularly scheduled meetings with colleagues, we should also have planned time with friends, family and acquaintances outside of work who can later help us through adversity. Even weak connections, people you know but not very well, serve a purpose in your social support system as they can provide an unbiased, objective perspective that is more difficult to get from close connections.
Trouble at home easily transfers to the workplace and vice versa. When you interact with a colleague at work, you aren’t just interacting with them as a professional, you’re interacting with someone who is likely dealing with unseen circumstances at home. Because families are units, when one person within the unit is impacted by adversity, it usually impacts all members. Therefore, a significant component of equipping staff with resiliency training is to teach them how to be resilient at home.
Families are also a resource for one another, so when one member is resilient, they can model that behavior for other members of the family.
The five practices of resilient families:
1. They are connected to each other and to a larger support system.
2. They proactively care for one another.
3. They have confidence that they can get through adversity.
4. They are committed to each other and believe that the family unit matters.
5. They take control and move through adversity together.
Four ways to improve resilient family responses:
1. View your family as a system, not as individual parts.
2. Put the adversity that your family faces in context.
3. See adversity as potential for growth.
4. Remember that families respond to adversity differently. Look at them with a positive framework rather than a negative framework.
While equipping individuals with resiliency tools at the individual level is important, hospitals and health care systems must model resiliency first.


Creating resiliency in the workplace is fairly similar to creating resiliency in the home. It begins with seeing your workplace as a system with a common thread that unites all individual contributors. Just like the family unit is a resource for its members, organizations should be a resource for its staff members.
The success of an organization is not just a reflection of the pooled talent, expertise and ability of its individual members. How the organization facilitates cooperation and communication amongst the individuals determines if the organization will be greater than the sum of its parts.
What resilient organizations do differently:
1. They have routines;
2. The value rest, self-care and the well-being of staff;
3. They embrace the reality of circumstances; and
4. They facilitate relationships and supportive communities.
Organizational agility is characterized by:
1. Rehearsals: the organization emphasizes preparation, pre and post-mortems and contingencies;
2. Reserves: the organization plans for cross-training and diversity of skillsets amongst its workforce;
3. Reflection: the organization facilitates collaborative learning and innovation; and
4. Responsiveness: the organization demonstrates agility in decision-making. Resources:
Since its genesis, the Texas Hospital Association has been advocating on behalf of its member hospitals and health systems, providing them with the latest updates and legislative action in order to drive hospitals and Texas health care forward. THA would not be the strong voice it needs to be for Texas hospitals without the ongoing support, collaboration and input from its members.

75 Years
THA is celebrating Women’s History Month by honoring 23 notable women in Texas hospitals, health care and public policy in 2023.
Written by Julia MannMarie Alvarez Group CEO, Acadia Healthcare
Carla Dawson Chief People Officer, Texas Health Resources


50 Years
25 Years
Erin Asprec Executive Vice President and Chief Operating Officer, Memorial Hermann Health System











Jeanna Bamburg, FACHE, CHT CEO, The Woman’s Hospital of Texas
Jennifer Chapman Banda, J.D. Senior Vice President of Advocacy and Public Policy, Texas Hospital Association
Serena Bumpus, DNP, RN, NEA-BC CEO, Texas Nurses Association
Chani Cordero, FACHE, FCHIME, FHIMSS
Chief Information Officer, Brooke Army Medical Center






Phyllis Cowling
President and CEO, United Regional Health Care System
Cris Daskevich, FACHE, MHA/MBA CEO, Children’s Hospital of San Antonio and Senior Vice President of Maternal Services, CHRISTUS Health
Cecile Erwin Young
Executive Commissioner, Texas Health and Human Services Commission
Dr. Nora Frasier, MBA, RN, FACHE, NEA-BC
Chief Nursing Officer, Methodist Man
Alicia Hernandez, DNP, RN Administrative Director, Nursing Professional Development, Harris Health System, Houston



Sally Hurt-Deitsch, MSN, MHA, RN, FACHE Executive Vice President, Nursing and Operations



Infrastructure, Ascension
Ulondia Lee, DNP, RN Chief Nursing Officer, Medical City Fort Worth


Yasmene McDaniel
CEO, HCA Houston Healthcare Southeast
Emily Ramshaw CEO and Co-Founder, The 19th Cris Rivera CEO, Rio Grande Regional Hospital
Dr. Jennifer Shuford Commissioner, Texas Department of State Health Services
Rhonda Unruh, MHA, RN, CIC Vice President of Quality, Guadalupe Regional Medical Center


Janice Walker, DHA, MBA-HCM, BSN, RN, NEA-BC
System Executive Vice President and Chief Nurse Executive, Baylor Scott & White Health
Carol Porter DNP, RN, FAAN
Chief Nursing Officer and Senior Vice President, The University of Texas MD Anderson Cancer Center





Meghan Weller Director, Government Relations, HCA Healthcare Katherine Yoder Vice President, Government Relations, Parkland Health
 Texas Health Harris Methodist Hospital Cleburne
The CCMCThe Heart Hospital
Texas Health Harris Methodist Hospital H-E-B
Jackson County Hospital District
Baylor Scott & White Medical Center - Taylor
CHRISTUS Spohn Hospital Corpus Christi South
Metropolitan Methodist Hospital
Moore County Hospital District
Medical City Las Colinas
Methodist Specialty and Transplant Hospital
Parmer Medical Center
Corpus Christi Medical Center - Doctors Regional
Medical City Denton
Texas Health Harris Methodist Hospital Cleburne
The CCMCThe Heart Hospital
Texas Health Harris Methodist Hospital H-E-B
Jackson County Hospital District
Baylor Scott & White Medical Center - Taylor
CHRISTUS Spohn Hospital Corpus Christi South
Metropolitan Methodist Hospital
Moore County Hospital District
Medical City Las Colinas
Methodist Specialty and Transplant Hospital
Parmer Medical Center
Corpus Christi Medical Center - Doctors Regional
Medical City Denton


In honor of Black History Month, THA profiles three Black leaders leaving their mark in Texas hospitals and health care
Written by Julia Mann
Hear from three Black leaders making a difference in Texas health care as they discuss what has inspired their careers, the impact they hope to have on their communities and how Texas hospitals can continue to promote diversity, equity and inclusion.

DBA,
In my experience including and involving people from different life experiences to participate in a goal or a desired outcome promotes diversity, equity and inclusion. I personally embrace people with different backgrounds, beliefs, attitudes and experiences. Due to the fact numerous studies have shown that when hospitals promote diversity, equity and inclusion it can benefit the happiness and progress of the community and the workforce. However, we also must be mindful that everyone does not have the same starting line and to be successful we should meet people where they are. As a leader, I would recommend listening more than you tell. Gather as much information as possible and try to make sense of it. Ask tons of questions and listen carefully to the answers. Don't make assumptions, and don't judge. Most importantly, always remember that diversity, equity and inclusion is a journey, not a destination.
Loren K. Robinson M.D., MSHP, FAAP Chief Medical Officer and Vice President of Medical Affairs, CHRISTUS St. Michael Health System
Senior
Vice President and Associate Chief Talent Officer, Parkland Health
Early in my career, I experienced disenchantment with my dream job, so I was pushed to explore other industries, careers and passions. As a result, I was pulled toward health care, and it has truly been life-changing. As with all aspects of change it required transformation and patience. While identifying my desired scope I discovered that human resources (HR) in health care was my calling. Over the years I have been an individual contributor and led multiple teams that were both traditional and non-traditional HR departments. As a result, it allowed me to self-discover my purpose in health care, which aligned with what inspired me to join originally. I have the opportunity to positively impact and add value to the lives of employees, the community and patients. In essence, I can make a difference in the lives of people at work and in the Dallas community.
As a Black leader in health care, I can create and expand spaces and programming aimed at breaking down stigmas. In 2023, health care HR is currently positioned to address the systemic inequities that have been embedded in the workplace for generations. For example, we can establish awareness


especially tied to social change and workplace equity. I use my influence to model appropriate behaviors to discuss race and help build a culture where equity and inclusion are embraced authentically and not avoided. I also hope that we can continue to create initiatives to accelerate progress toward a more inclusive and equitable experience for all races.
I genuinely love working with people at work and in the community. I often immerse myself within the community and surround myself on governing boards with people who are dedicated to enhancing health care, community and HR. When I speak at events or with youth, I strive to provide a unique sense of purpose that hopefully will manifest. also discovered that when you give back it is a great way to get to know your community. In my experience, partnering alongside people with broad open-minded perspectives from different walks of life helps me as an HR Practitioner and as a member of the community, so I strive to have the same impact.
I entered the field of health care inspired by the example and leadership of both my parents, Dr. Luther Robinson, a pediatric geneticist and Mrs. Jan Robinson, a pediatric nurse practitioner. Growing up seeing them take care of other people and give back to the community, inspired me to pursue a similar path. After becoming a mom in 2019, I would say that I continue to be inspired and motivated to improve health care for future generations so that my children and their peers will have equal opportunity for excellent health care options no matter where their lives take them.

Being a Black leader in health care, I constantly reflect on what a different experience in health care many people living today experienced in their youth. I strive to be an example of excellence and professionalism and to advocate not only for health equity, but also for continued commitment to growth and diversification amongst our health care providers and in our C-suites, government, leadership of public and private partners in health care.
I hope that my work continues to strengthen the Texarkana community and Ark-La-Tex/Northeast Texas region as a health care leader. Supporting the growth of health care services provided in our ministry allows our community to get the health care in a region they call home. I want to continually work to eliminate health disparities and promote health equity in our region and across our country. As a Black woman in medicine specifically, I hope that younger generations are inspired to pursue health care fields and return to Texarkana to serve our community. I also hope that the generation that grew up during times of segregation, Jim Crow, and then subsequent integration, know that I respect and honor that legacy and am so thankful for the sacrifices they have made to ensure that I had the opportunity now have to serve as a leader in our community.
Diversity, equity and inclusion is hard, but it is essential work. It can become so easy to get caught up in the demands of finance, growth, staffing, operations and other essential parts of running a hospital day to day. However, by continuing to focus on who is NOT in the room, and seeking input, promoting hires/promotions of people who do not necessarily look like oneself, ensures that leadership teams will continue to have diverse input and opinions that will fuel strategic growth. One of the ways we are able to continue to elevate DEI at CHRISTUS Health is that this work is consistent with our core values. Having the support of a hospital’s CEO is what will make or break a DEI journey. At CHRISTUS St Michael, we have a CEO who is committed to asking the tough questions and making the right decisions in the name of growing our hospital and making it a better and more equitable place not only to seek care, but also to work, no matter your background, training, race, color, or creed.

I first entertained the idea of becoming a physician while in an engineering internship during college. When I asked about how a certain device would feel to the client and what impact it might have on them, the engineer jokingly said that that was for the doctors to figure out. I thought maybe engineering was not the right field for me because I wanted to be a part of the team that would help people feel better in a more tangible way. Shortly after this time, I lost my mother after a short battle with cancer. It was during that time that I realized how the health care system can be so overwhelming to patients and their families during some of their most vulnerable times. I wanted to have a career that would make those times a little less overwhelming by being a compassionate advocate for my patients. Over the years, I've seen how this looks different at the various stages of my career.

As a physician, we use our many years of knowledge and training to help our patients get better and stay healthy, and we hope to have a positive impact on their lives. As a health care leader, that impact goes beyond the individual patient. Now
what inspires me is all the patients we interact with, the families they come from and the environments they live, learn and work in. I'm inspired by the staff that work in our system who show up every day in the face of their own challenges, fears and concerns. Also, I am inspired by the world around us. In my work and background as a pediatrician, I have been involved with the care of some of our tiniest members of society. I know that if we can improve the lives of these little ones and help them achieve their best health, they will be able to become healthy adults who have a positive impact on the next generation and world around us.
You may be familiar with the phrase "representation matters," and that is what being a Black health care leader means to me. As a Black woman in my field, I am able to represent those families who come from diverse racial backgrounds both in clinical spaces and in meeting rooms. It is truly an honor because I realize that I stand on the shoulders of those ancestors who dared dream to not only become a doctor but to be allowed to seek health care in a hospital.

I hope that have a positive impact on the patients and families we serve by being a true advocate for their needs and health. That means that although I may not be directly in front of the patient providing care, still have a hand in improving their health care experience overall. Whether that is by working with our leaders to develop innovative ways of reaching our patients or by identifying and removing the barriers to health care that some of our patients face, hope that my work has played a small part in making health care more accessible to more people regardless of their background. I also hope that I can positively influence others to do the same - to impact the lives of others so that it improves their lives overall.
To promote diversity, equity and inclusion within Texas hospitals, we should start by recognizing that we all need and should want more diverse, equitable and inclusive environments to work and serve in. By recognizing this simple fact, we are allowing the space to figure out what those environments should look like and what they need to thrive. This includes putting the leaders and resources in place to support these initiatives in an ongoing fashion. As Texas and the world around us become more diverse, we must be intentional in making sure we embrace that diversity so that we create space for everyone to thrive.
THA’s Newsmakers highlights leaders from THA member hospitals and health systems making headlines in Texas health care. Congratulations to THA’s Q1 Newsmakers!
 Written by Julia Mann
Written by Julia Mann
Barclay E. Berdan Texas Health Resources

Allen Harrison Medical City Healthcare
Zach Dietze UT Health East Texas
Courtney Head Hendrick Health

Kristin Dyer Medical City Healthcare
Eyal Gottlieb, PhD University of Texas MD Anderson Cancer Center
Tiffany Miller Yoakum Community Hospital
Michael Perez, MBA, PT, FACHE CHRISTUS Spohn Hospital Beeville








David Byrd The Hospitals of Providence Transmountain Campus
Darren DeSimone, BSN, RN HCA Houston Healthcare Kingwood


Kerin Adelson, M.D. University of Texas MD Anderson Cancer Center







Esther Kwon Methodist Hospital Texsan
Nancy Doolittle, DNP, RN UT Health San Antonio Multispecialty and Research Hospital

David McKnight St. David’s Medical Center
Christine Martinez, MSN, R.N. Laredo Medical Center

Dillon Rai Medical City Arlington
Michael
Russ
Kimberly Shaw, BSN, St. Joseph Health John Voight, MSN, RN Memorial Hermann The Woodlands Adam Messer Dell Seton Medical Center Arabinda “Ara” Pani, M.D HCA Houston Healthcare Northwest Wiggins Dell Children’s Williams Texas Children’s Hospital















